Otitis Media and Externa Definitions Middle ear effusion


- Slides: 37
Otitis Media and Externa
Definitions �Middle ear effusion: liquid in the middle ear cavity �Acute otitis media (AOM): rapid onset of signs and symptoms of middle ear inflammation �Recurrent AOM: 3 or more separate episodes of AOM in 6 months OR 4 episodes in 12 months, with at least 1 in the past 6 months �Otitis media with effusion (OME): middle ear fluid that is not infected �External otitis: inflammation of the external auditory canal
Acute Otitis Media �Background: �Most common condition for which antibiotics are prescribed for the pediatric population �Number of visits for AOM have been decreasing �Proportional decrease in antibiotic prescriptions
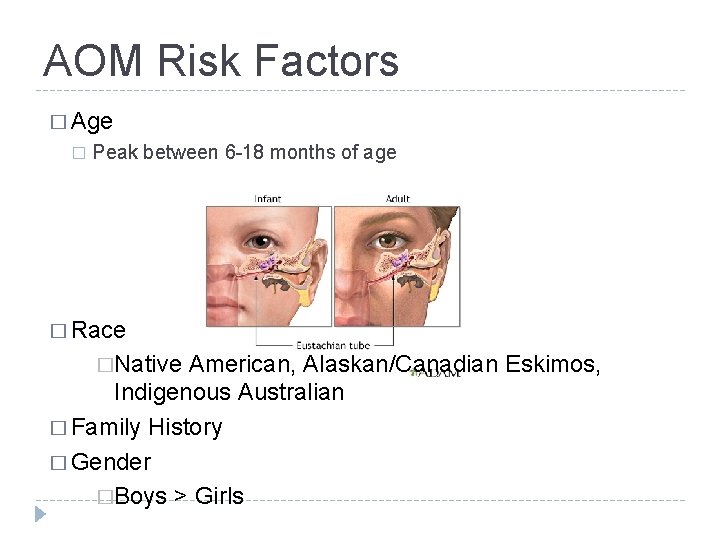
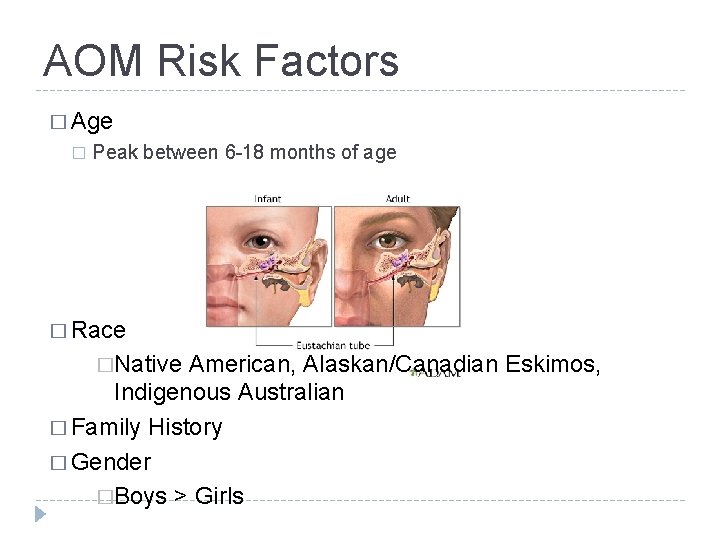
AOM Risk Factors � Age � Peak between 6 -18 months of age � Race �Native American, Alaskan/Canadian Eskimos, Indigenous Australian � Family History � Gender �Boys > Girls
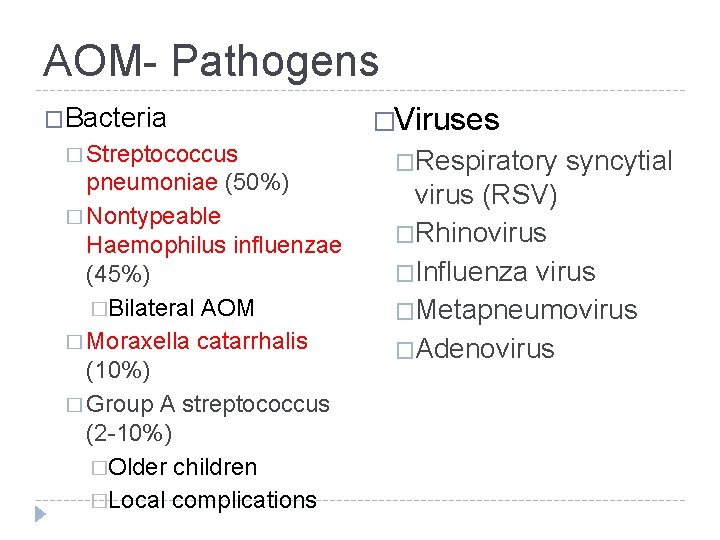
AOM- Pathogens �Bacteria � Streptococcus pneumoniae (50%) � Nontypeable Haemophilus influenzae (45%) �Bilateral AOM � Moraxella catarrhalis (10%) � Group A streptococcus (2 -10%) �Older children �Local complications �Viruses �Respiratory syncytial virus (RSV) �Rhinovirus �Influenza virus �Metapneumovirus �Adenovirus
AOM- Signs and Symptoms �Can be non-specific, especially in infants �Fever �Poor appetite �Poor sleep �Vomiting/diarrhea �Irritability �Ear Pain � Most common complaint, even among preverbal children �Ear tugging has low sensitivity and specificity
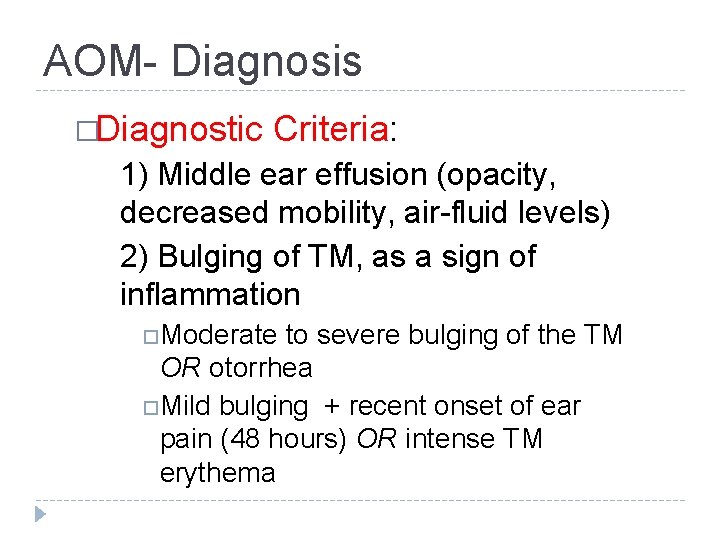
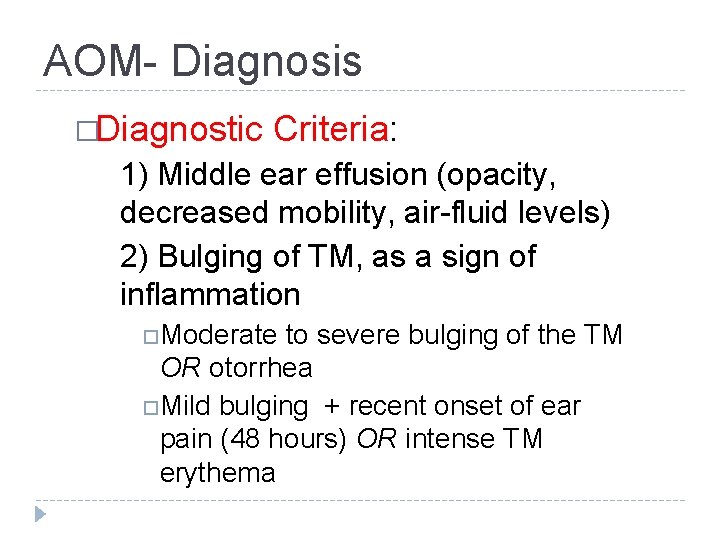
AOM- Diagnosis �Diagnostic Criteria: 1) Middle ear effusion (opacity, decreased mobility, air-fluid levels) 2) Bulging of TM, as a sign of inflammation Moderate to severe bulging of the TM OR otorrhea Mild bulging + recent onset of ear pain (48 hours) OR intense TM erythema
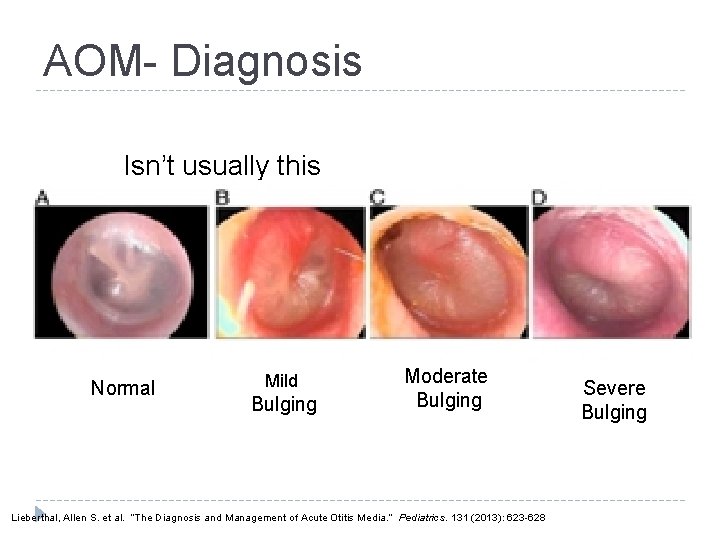
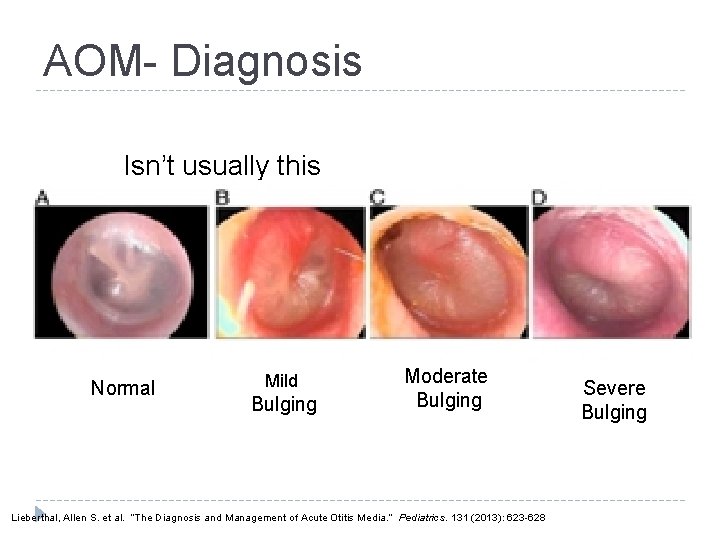
AOM- Diagnosis Isn’t usually this obvious Normal Mild Bulging Moderate Bulging Lieberthal, Allen S. et al. “The Diagnosis and Management of Acute Otitis Media. ” Pediatrics. 131 (2013): 623 -628 Severe Bulging
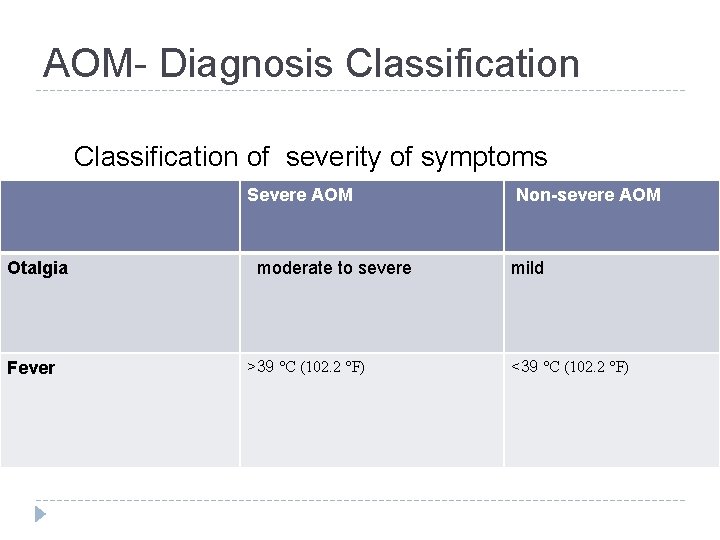
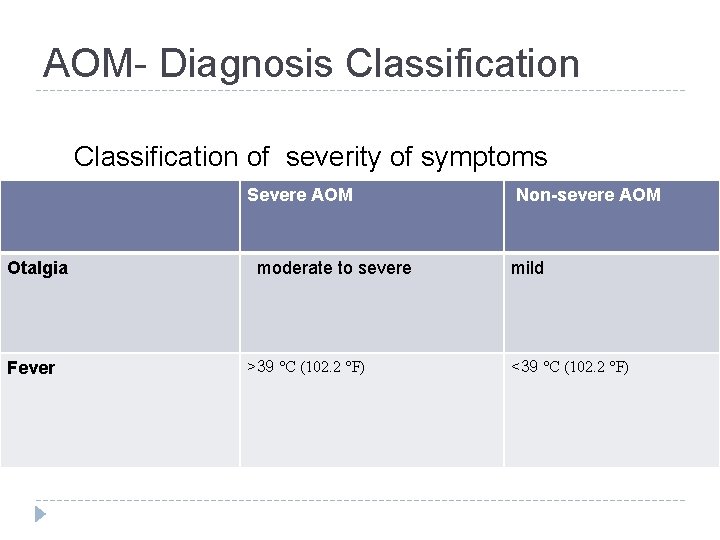
AOM- Diagnosis Classification of severity of symptoms Severe AOM Otalgia Fever moderate to severe >39 °C (102. 2 °F) Non-severe AOM mild <39 °C (102. 2 °F)
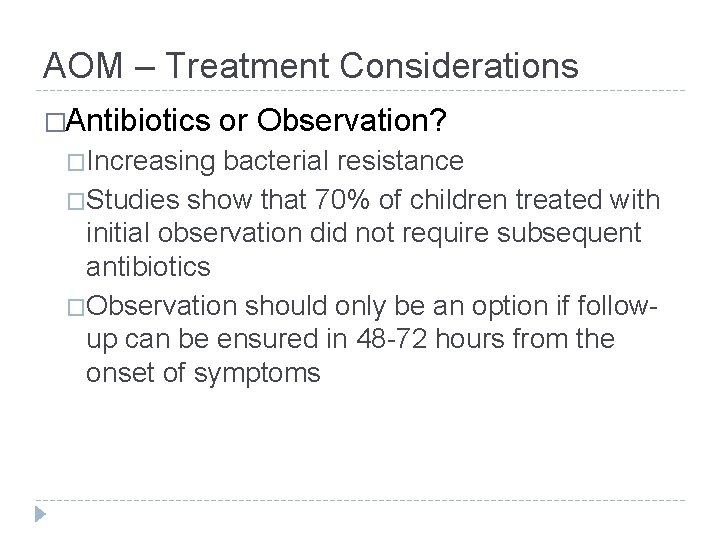
AOM – Treatment Considerations �Antibiotics �Increasing or Observation? bacterial resistance �Studies show that 70% of children treated with initial observation did not require subsequent antibiotics �Observation should only be an option if followup can be ensured in 48 -72 hours from the onset of symptoms
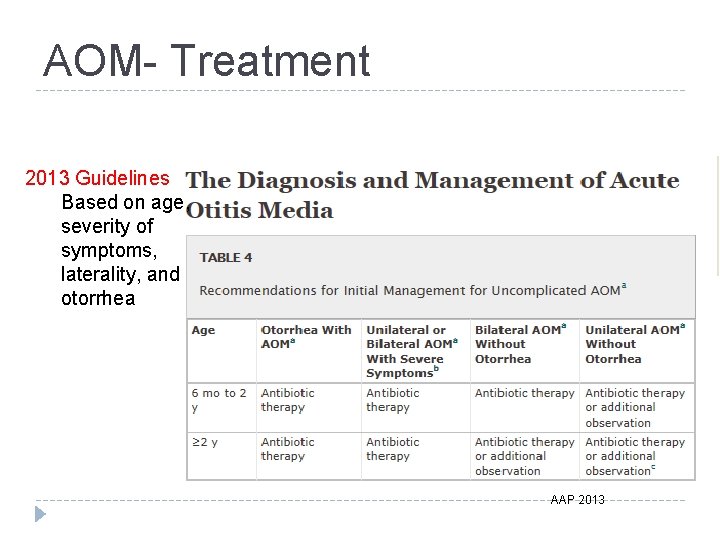
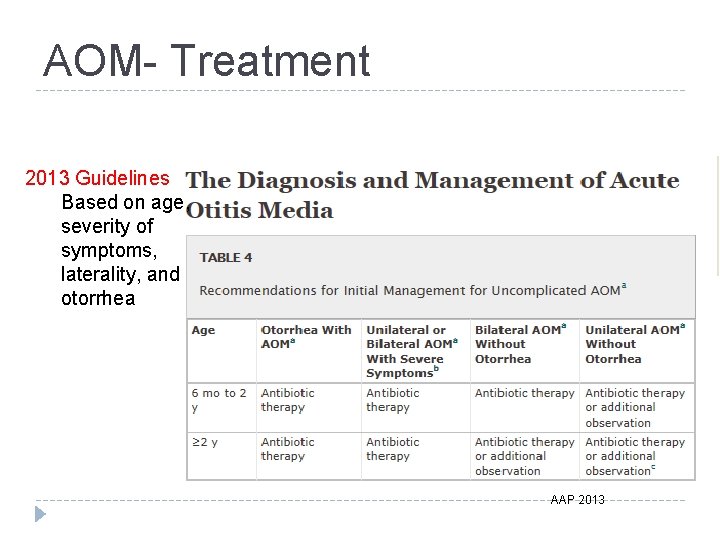
AOM- Treatment 2013 Guidelines Based on age, severity of symptoms, laterality, and otorrhea AAP 2013
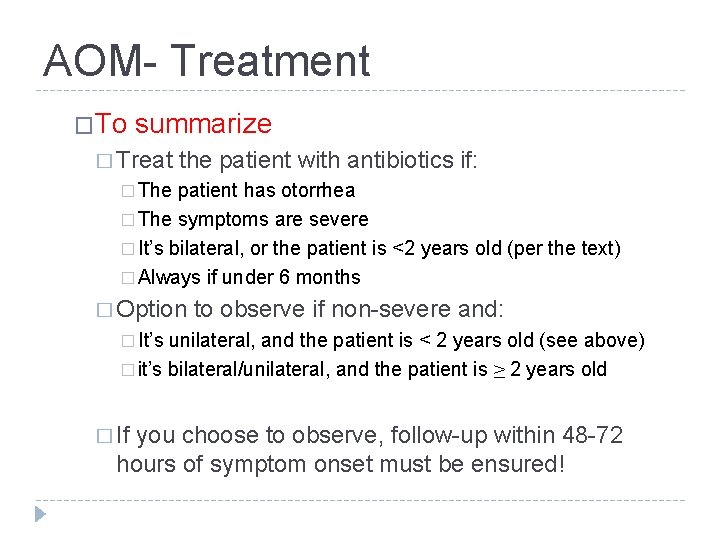
AOM- Treatment �To summarize � Treat the patient with antibiotics if: � The patient has otorrhea � The symptoms are severe � It’s bilateral, or the patient is <2 years old (per the text) � Always if under 6 months � Option to observe if non-severe and: � It’s unilateral, and the patient is < 2 years old (see above) � it’s bilateral/unilateral, and the patient is ≥ 2 years old � If you choose to observe, follow-up within 48 -72 hours of symptom onset must be ensured!
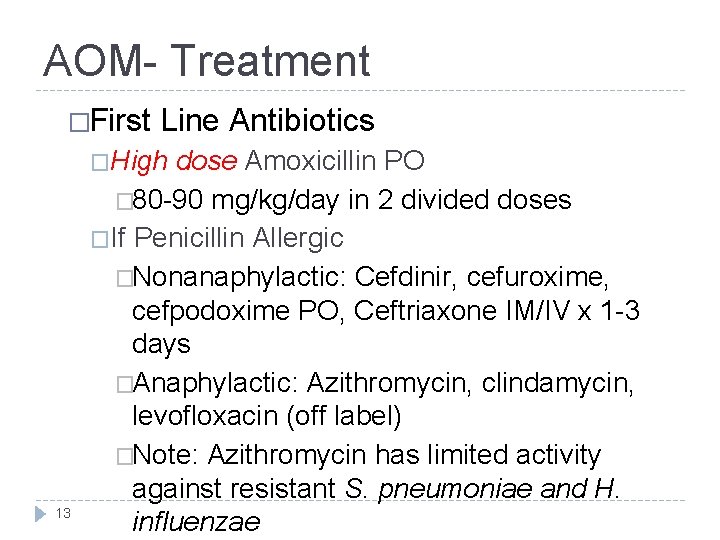
AOM- Treatment �First Line Antibiotics �High 13 dose Amoxicillin PO � 80 -90 mg/kg/day in 2 divided doses �If Penicillin Allergic �Nonanaphylactic: Cefdinir, cefuroxime, cefpodoxime PO, Ceftriaxone IM/IV x 1 -3 days �Anaphylactic: Azithromycin, clindamycin, levofloxacin (off label) �Note: Azithromycin has limited activity against resistant S. pneumoniae and H. influenzae

AOM- Treatment �Second-Line �High Antibiotics dose Amoxicillin-Clavulanate PO or 2 nd generation cephalosporins (see previous slide) � 90 mg/kd/day amoxicillin with 6. 4 mg/kg/day clavulanate in 2 divided doses �For treatment failure �If patient received amoxicillin in the last 30 days �If patient has Hx of AOM unresponsive to amoxicillin
AOM- Treatment �Duration of Treatment �<2 years old or severe symptoms: Standard 10 days � 2 -5 years old: 7 days �> 6 years old: 5 -7 days �Treat Pain �Acetaminophen or Ibuprofen �Topical benzocaine & antipyrine drops �Follow-up �Reassess if very young, severe symptoms, or recurrent AOM
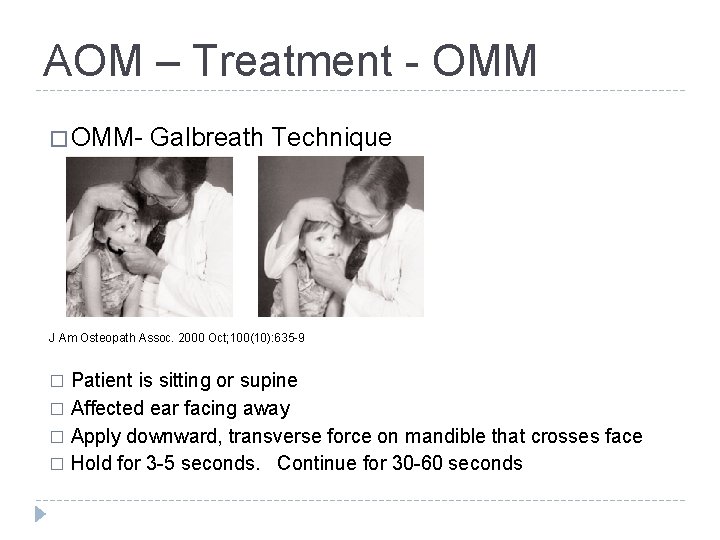
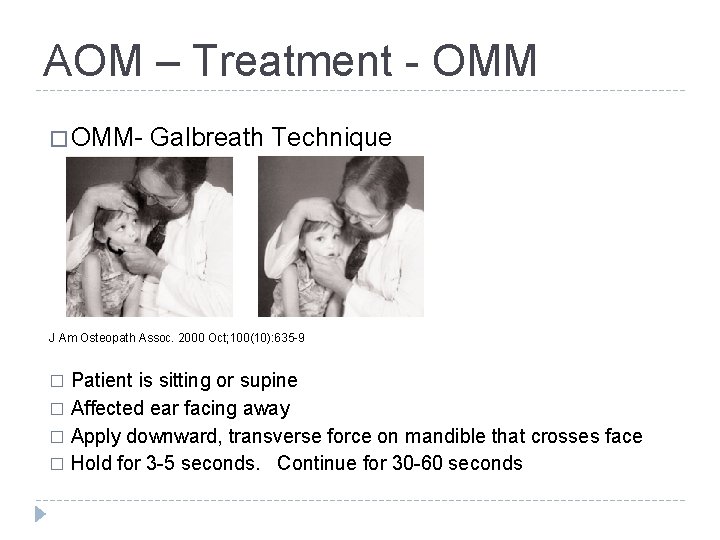
AOM – Treatment - OMM � OMM- Galbreath Technique J Am Osteopath Assoc. 2000 Oct; 100(10): 635 -9 Patient is sitting or supine � Affected ear facing away � Apply downward, transverse force on mandible that crosses face � Hold for 3 -5 seconds. Continue for 30 -60 seconds �
AOM- Prevention �Risk Factors �Encourage exclusive breast feeding for at least 6 months �Avoid exposure to tobacco smoke �Provide pneumococcal vaccine (PCV 13) �Provide annual influenza vaccine �Xylitol gum or lozenges can be helpful in older children with low choking risk 17
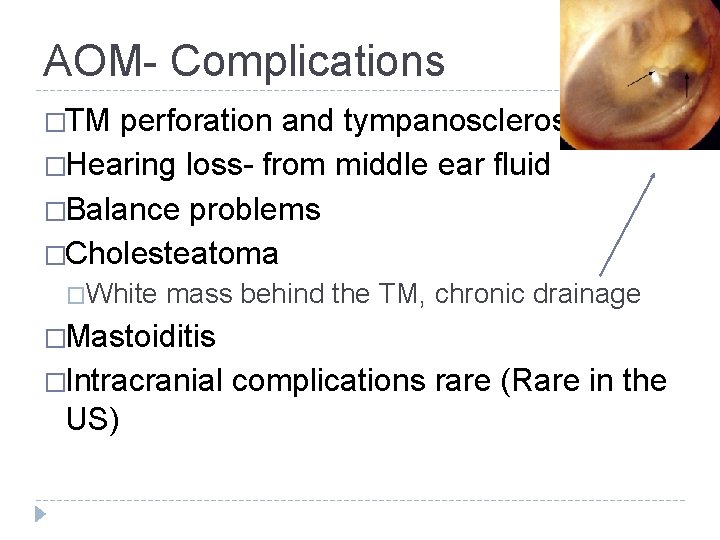
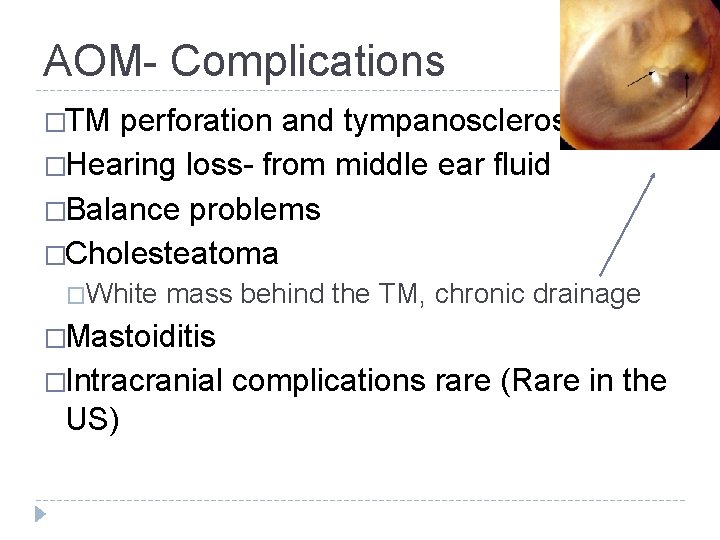
AOM- Complications �TM perforation and tympanosclerosis �Hearing loss- from middle ear fluid �Balance problems �Cholesteatoma �White mass behind the TM, chronic drainage �Mastoiditis �Intracranial US) complications rare (Rare in the
OME Otitis Media with Effusion Remember…. this is NOT infected
OME- Signs and Symptoms �Often asymptomatic �No signs of acute infection �Hearing loss-mild �Conductive �Approximately 25 d. B (plugging ears) �School hearing screening �Ear pain/fullness �Tinnitus
OME- Diagnosis and Treatment �Diagnosis �Otoscopy Decreased mobility of TM-insufflator bulb �Treatment �Commonly resolves spontaneously, but can take weeks to months �Watchful waiting �No medications
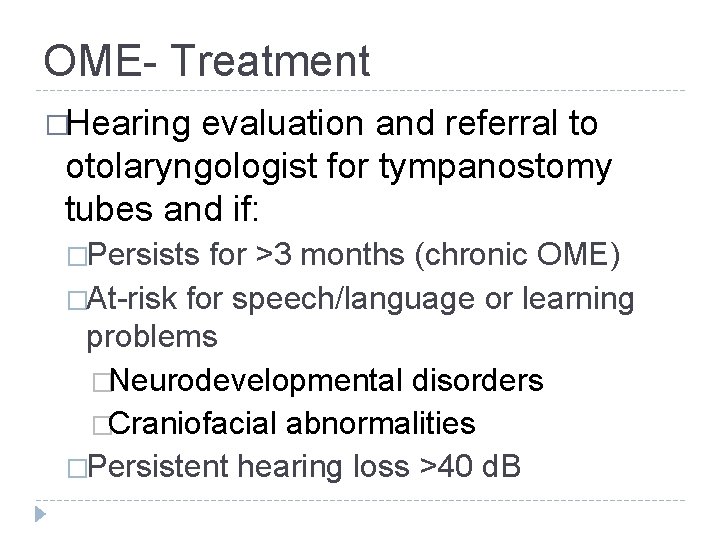
OME- Treatment �Hearing evaluation and referral to otolaryngologist for tympanostomy tubes and if: �Persists for >3 months (chronic OME) �At-risk for speech/language or learning problems �Neurodevelopmental disorders �Craniofacial abnormalities �Persistent hearing loss >40 d. B
Otitis Externa
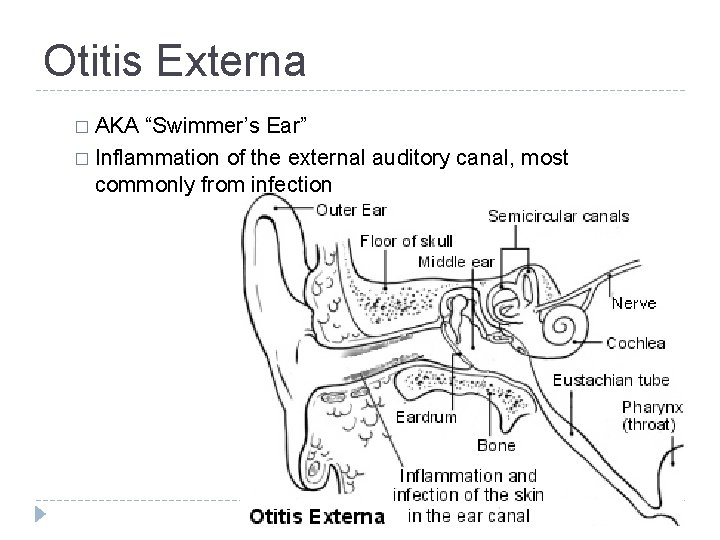
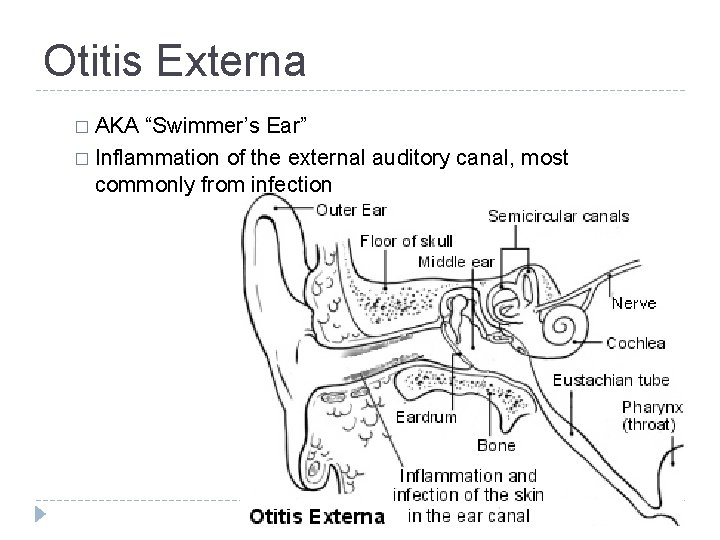
Otitis Externa � AKA “Swimmer’s Ear” � Inflammation of the external auditory canal, most commonly from infection
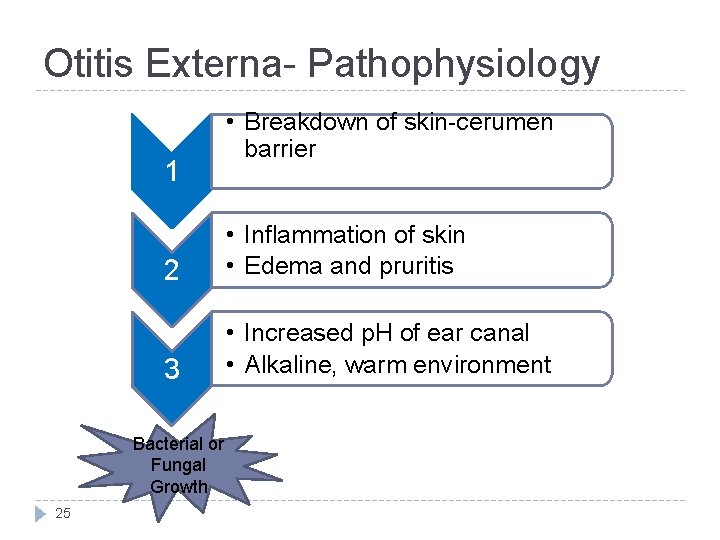
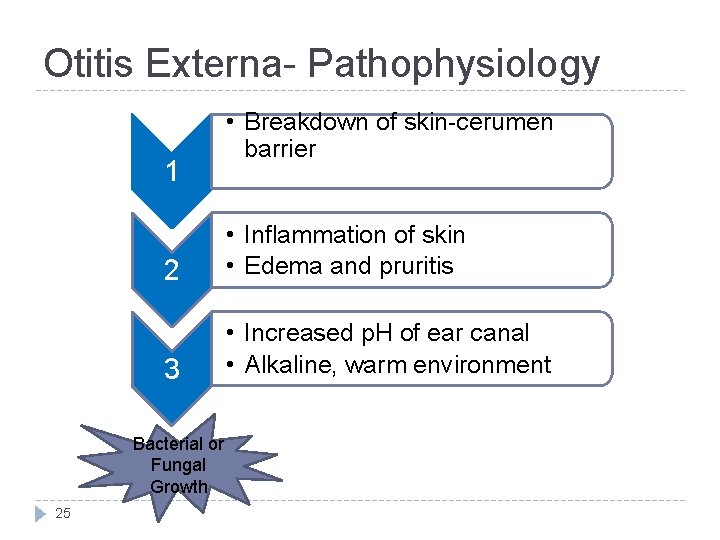
Otitis Externa- Pathophysiology 1 2 • Inflammation of skin • Edema and pruritis 3 • Increased p. H of ear canal • Alkaline, warm environment Bacterial or Fungal Growth 25 • Breakdown of skin-cerumen barrier
Otitis Externa- Risk Factors �Excess moisture (ie. swimming) �Trauma �Skin 26 conditions
Otitis Externa- Pathogens �Pseudomonas aeurginosa (38%) �Staph epidermidis (9%) �Staph aureus (8%) �Fungal (2 -10%) �Candida �Aspergillus 27
Otitis Externa- Diagnosis �Signs and Symptoms �Ear pain �Pruritus �Discharge �Hearing loss �Physical Exam �Tenderness �Swelling of pinna/periauricular skin �Edema and erythema of ear canal �Otorrhea- thick, clumpy, white 28
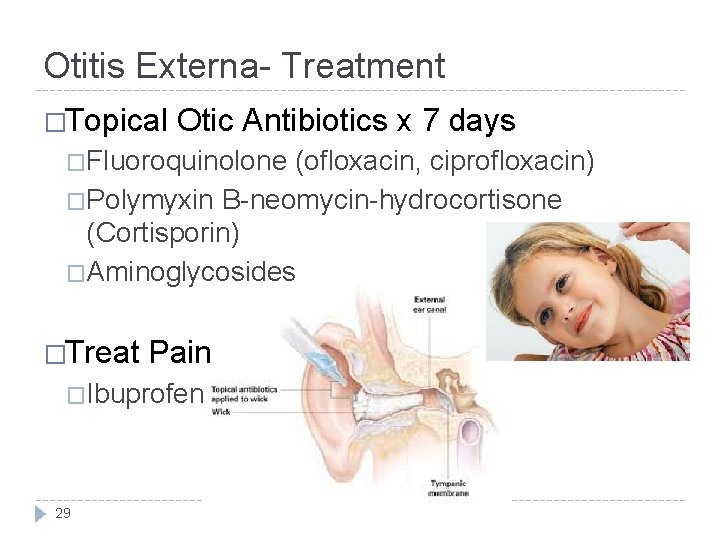
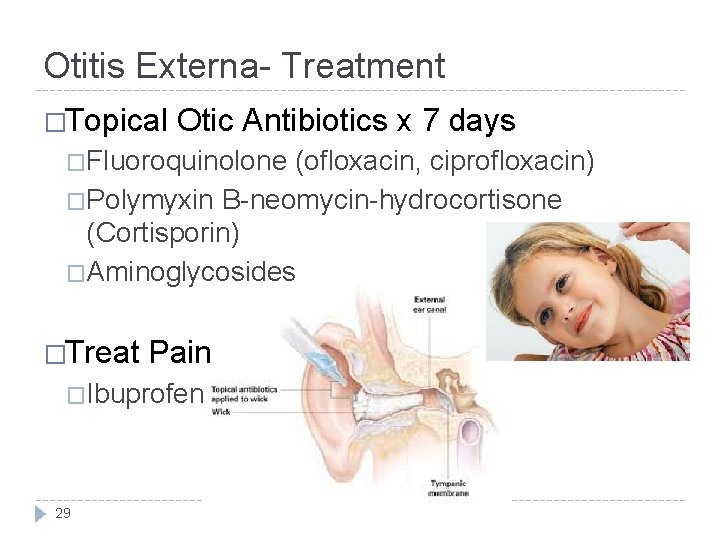
Otitis Externa- Treatment �Topical Otic Antibiotics x 7 days �Fluoroquinolone (ofloxacin, ciprofloxacin) �Polymyxin B-neomycin-hydrocortisone (Cortisporin) �Aminoglycosides �Treat Pain �Ibuprofen 29
Otitis Externa- Prevention �Leave your ears alone! �Keep ears dry �Acetic acid �Diluted isopropyl alcohol (rubbing alcohol) �Blow drying 30
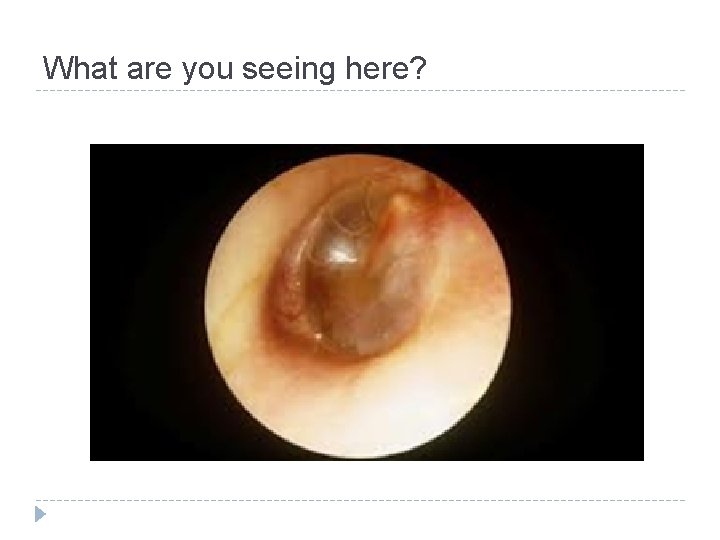
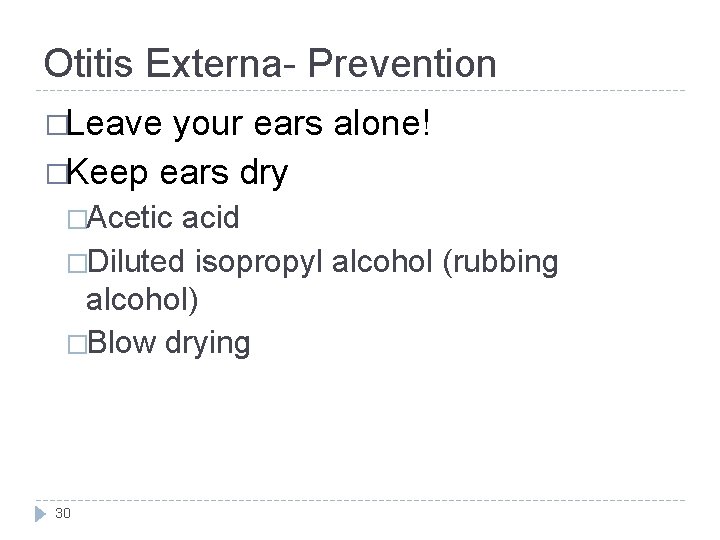
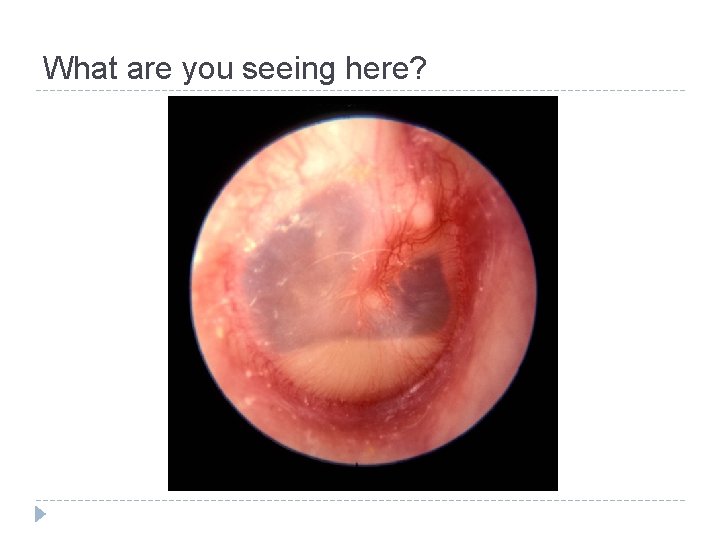
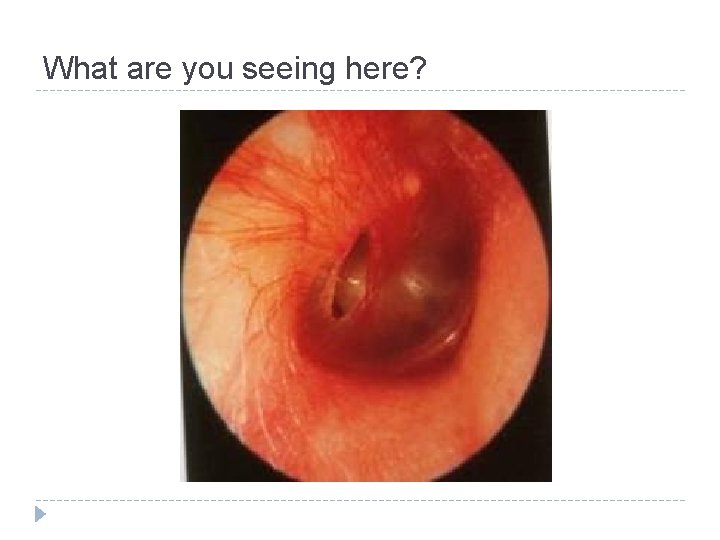
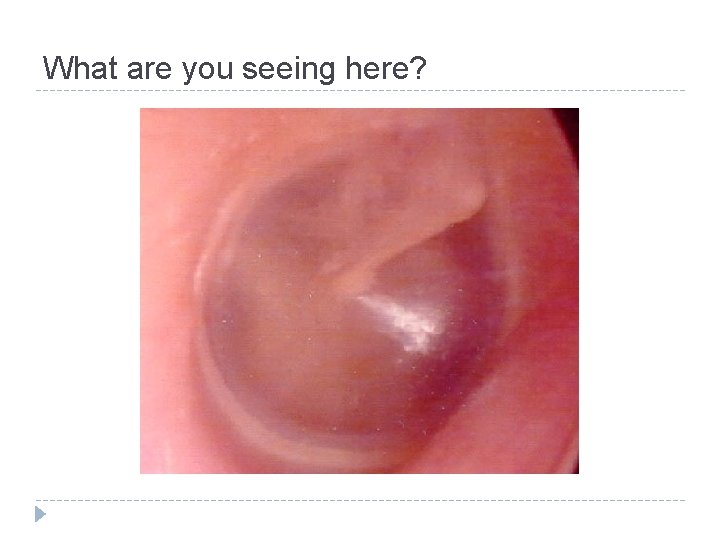
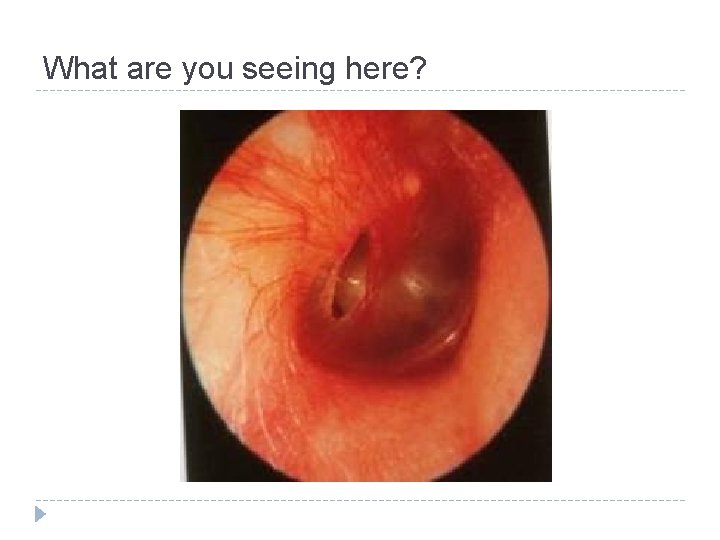
What are you seeing here?

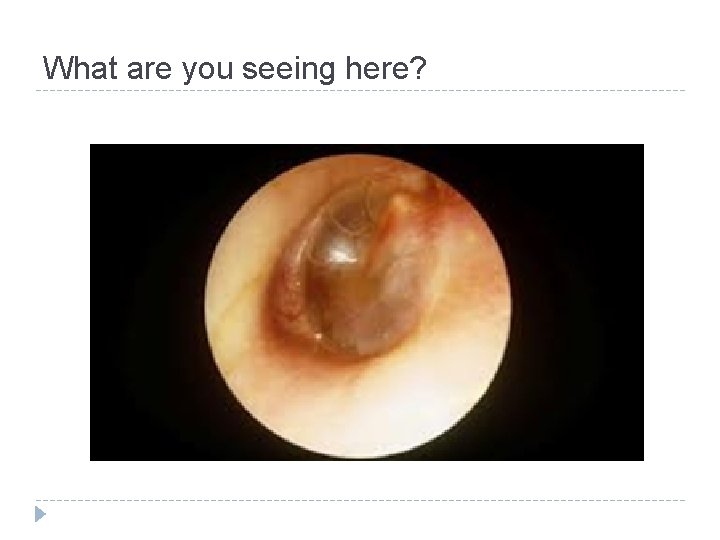
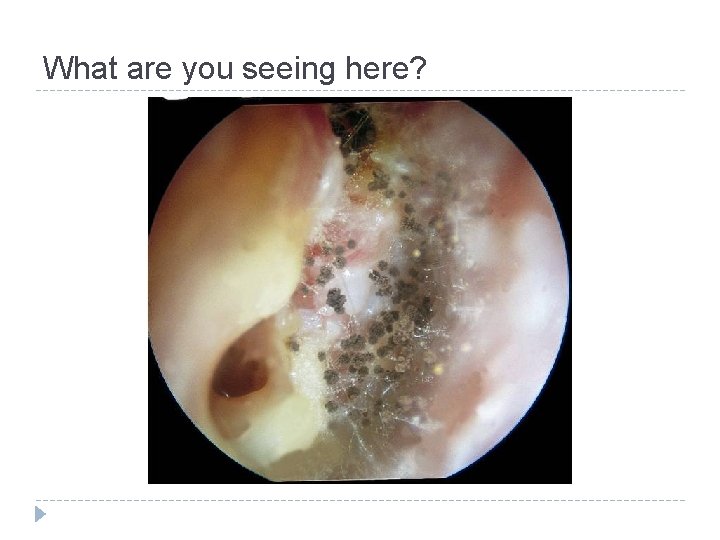
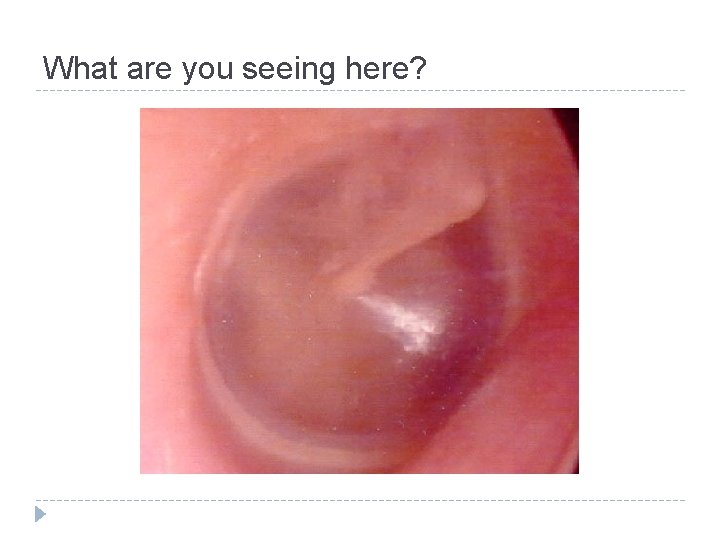
What are you seeing here?
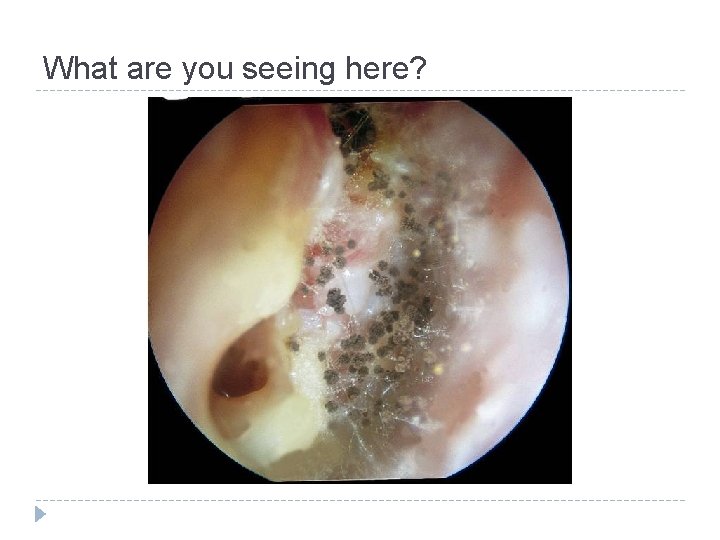
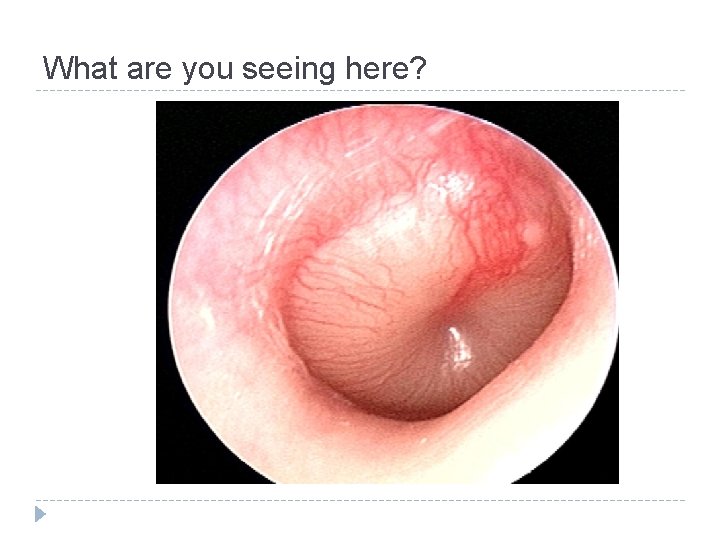
What are you seeing here?
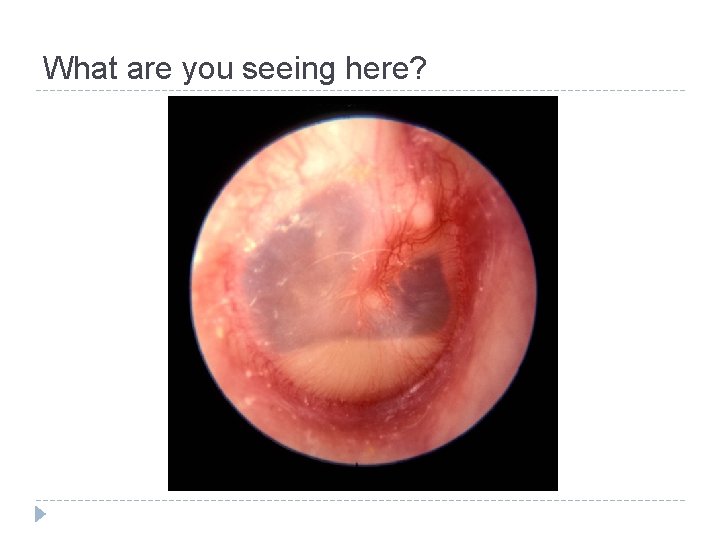
What are you seeing here?
What are you seeing here?
What are you seeing here?
What are you seeing here?