Optics of Refractive Procedures Amy C Nau OD



![Theoritical basis • Power-[n/(AL-d)]-(n/[n/(K+TR)]-d]) – d is effective lens position – TR = target Theoritical basis • Power-[n/(AL-d)]-(n/[n/(K+TR)]-d]) – d is effective lens position – TR = target](https://slidetodoc.com/presentation_image_h/1a06b3fd1e52fd7c53cc98ebf16ef70e/image-53.jpg)

- Slides: 75
Optics of Refractive Procedures Amy C. Nau, OD, FAAO Clinical Optics 3 rd edition, Elkingtpon, Frank and Greaney
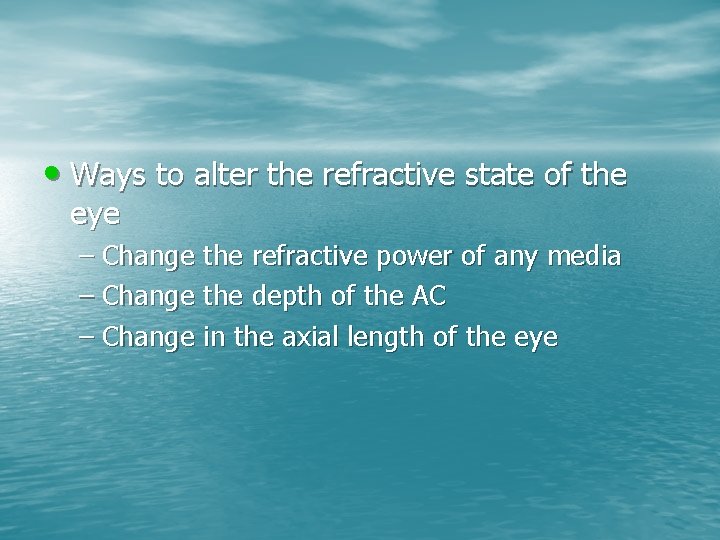
• Ways to alter the refractive state of the eye – Change the refractive power of any media – Change the depth of the AC – Change in the axial length of the eye
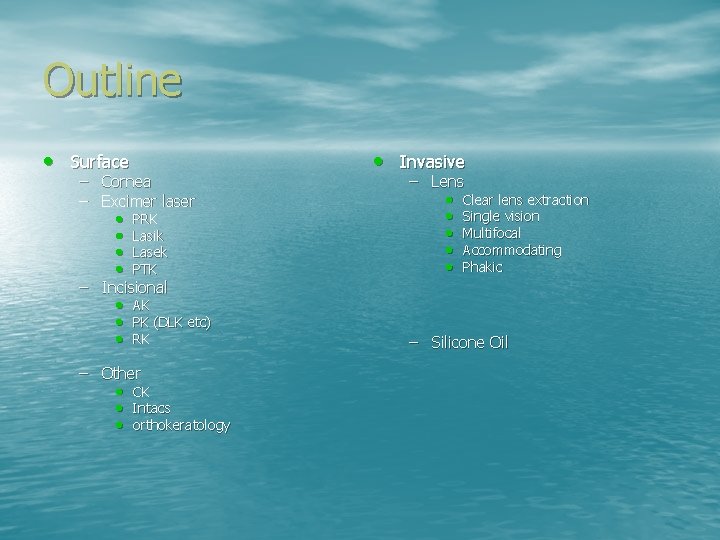
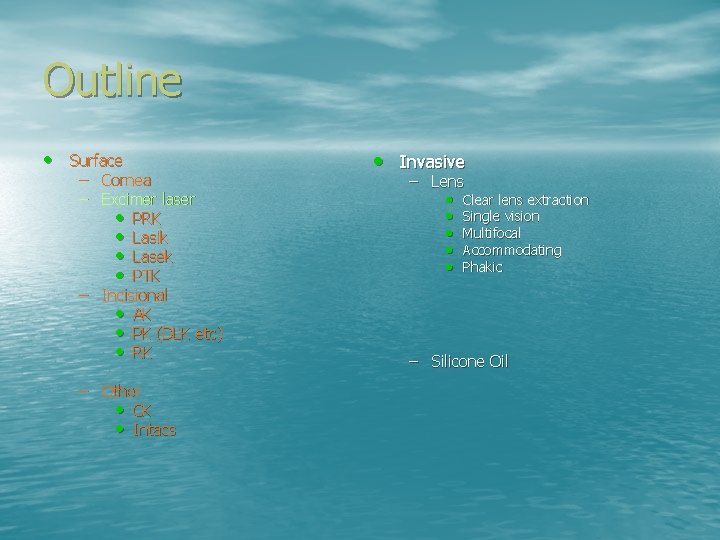
Outline • Surface – Cornea – Excimer laser • PRK • Lasik • Lasek • PTK – Incisional • AK • PK (DLK etc) • RK – Other • CK • Intacs • orthokeratology • Invasive – Lens • Clear lens extraction • Single vision • Multifocal • Accommodating • Phakic – Silicone Oil
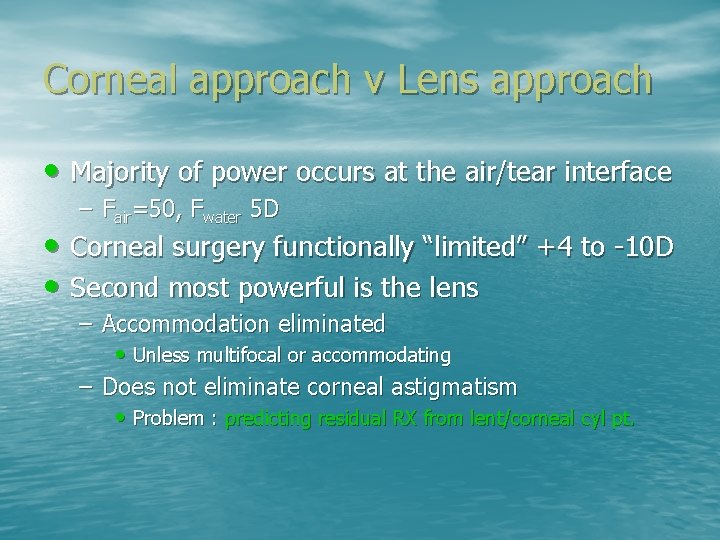
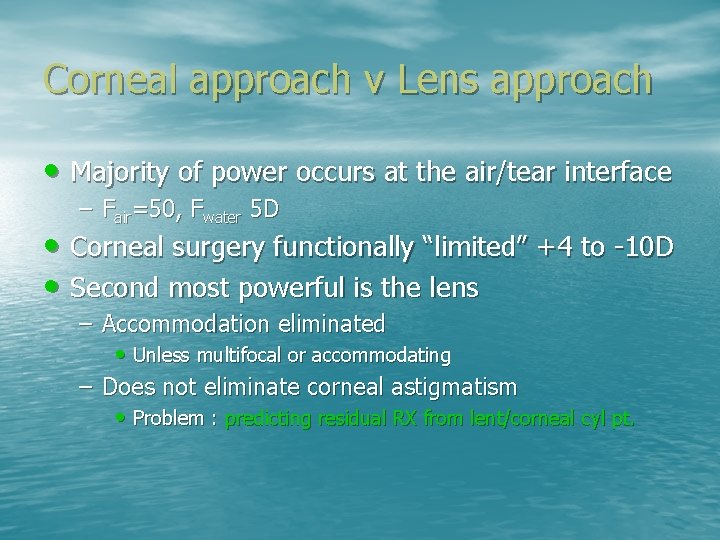
Corneal approach v Lens approach • Majority of power occurs at the air/tear interface – Fair=50, Fwater 5 D • Corneal surgery functionally “limited” +4 to -10 D • Second most powerful is the lens – Accommodation eliminated • Unless multifocal or accommodating – Does not eliminate corneal astigmatism • Problem : predicting residual RX from lent/corneal cyl pt.
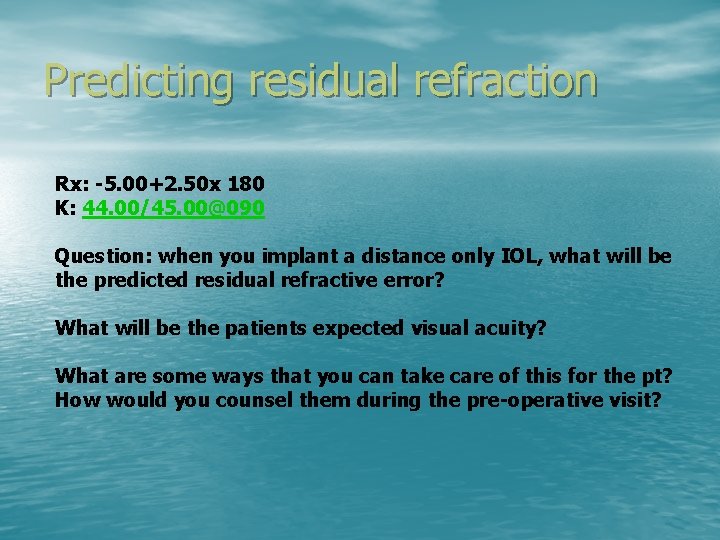
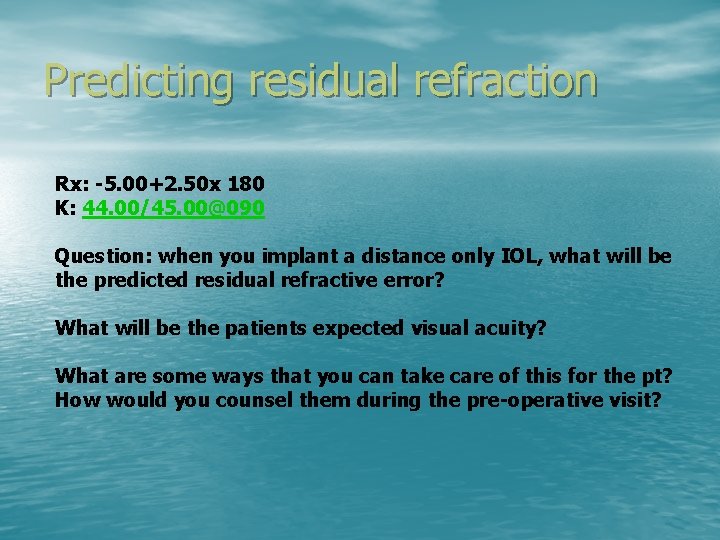
Predicting residual refraction Rx: -5. 00+2. 50 x 180 K: 44. 00/45. 00@090 Question: when you implant a distance only IOL, what will be the predicted residual refractive error? What will be the patients expected visual acuity? What are some ways that you can take care of this for the pt? How would you counsel them during the pre-operative visit?
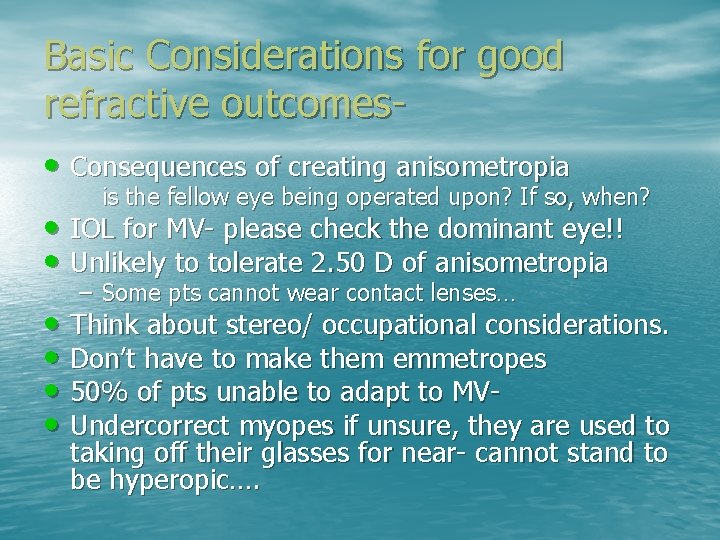
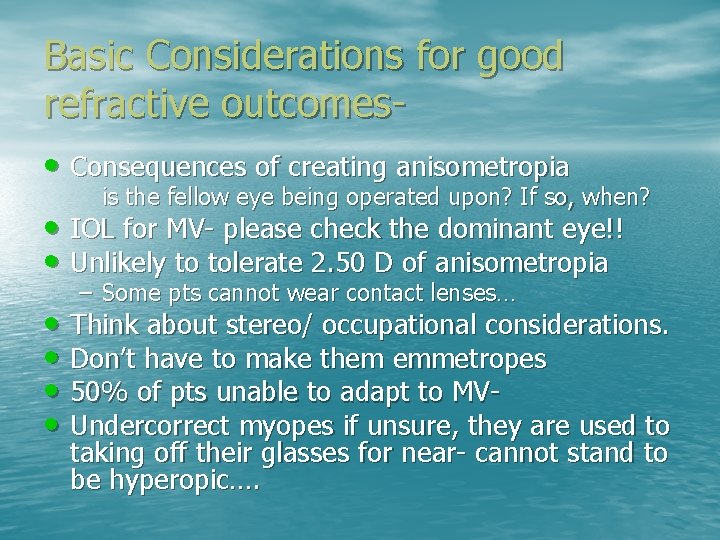
Basic Considerations for good refractive outcomes • Consequences of creating anisometropia is the fellow eye being operated upon? If so, when? • IOL for MV- please check the dominant eye!! • Unlikely to tolerate 2. 50 D of anisometropia – Some pts cannot wear contact lenses… • Think about stereo/ occupational considerations. • Don’t have to make them emmetropes • 50% of pts unable to adapt to MV • Undercorrect myopes if unsure, they are used to taking off their glasses for near- cannot stand to be hyperopic….
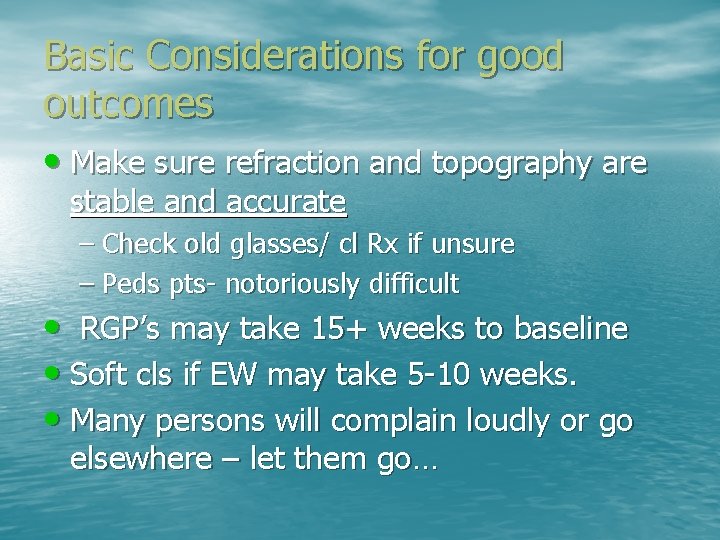
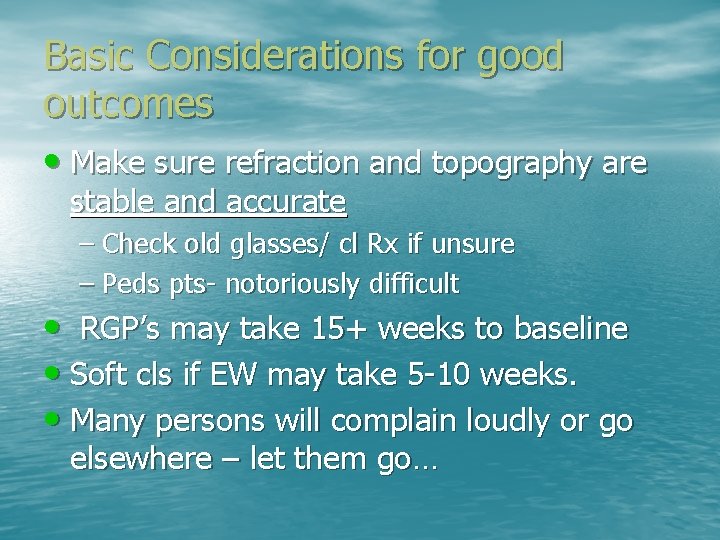
Basic Considerations for good outcomes • Make sure refraction and topography are stable and accurate – Check old glasses/ cl Rx if unsure – Peds pts- notoriously difficult • RGP’s may take 15+ weeks to baseline • Soft cls if EW may take 5 -10 weeks. • Many persons will complain loudly or go elsewhere – let them go…
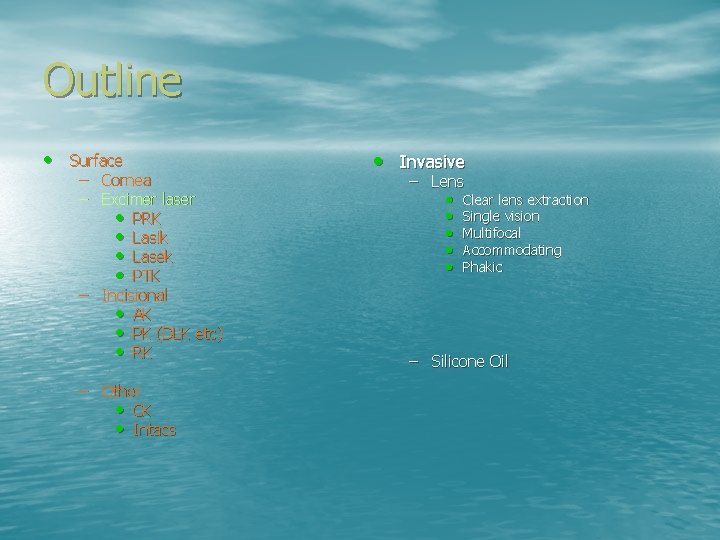
Outline • Surface – Cornea – Excimer laser • PRK • Lasik • Lasek • PTK – Incisional • AK • PK (DLK etc) • RK – Other • CK • Intacs • Invasive – Lens • Clear lens extraction • Single vision • Multifocal • Accommodating • Phakic – Silicone Oil
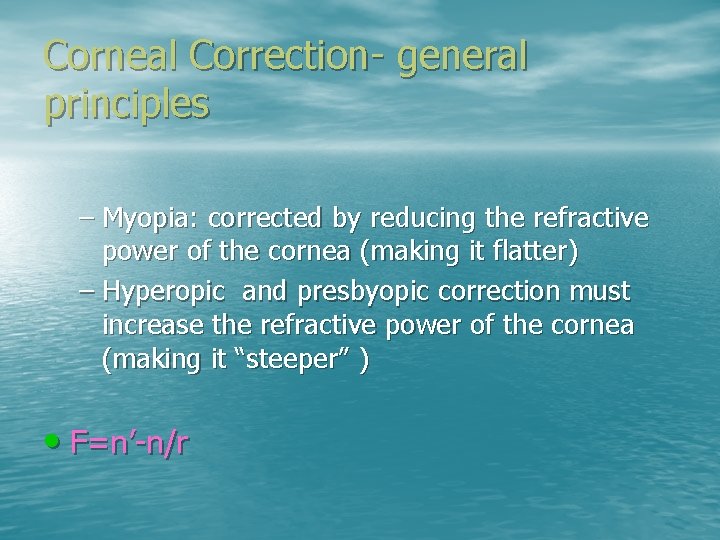
Corneal Correction- general principles – Myopia: corrected by reducing the refractive power of the cornea (making it flatter) – Hyperopic and presbyopic correction must increase the refractive power of the cornea (making it “steeper” ) • F=n’-n/r
Hyperopic correction • Ablate tissue peripherally, making the central cornea “steeper” – Less predictable – More aberrations – Custom preferred over traditional – Try CK…
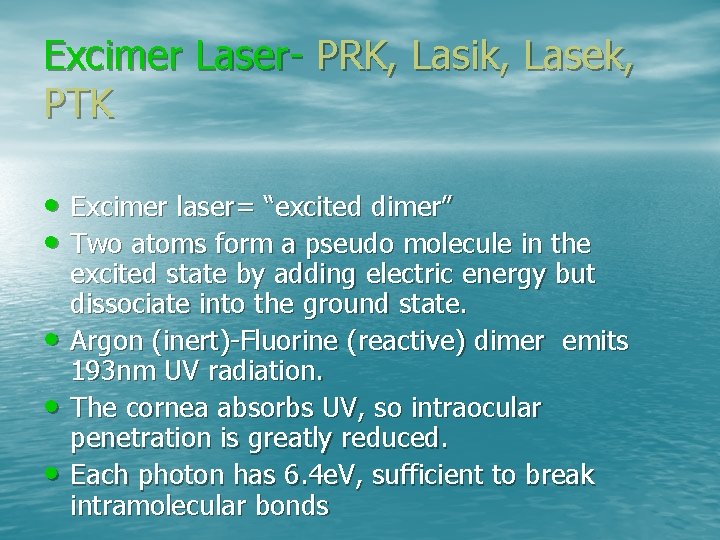
Excimer Laser- PRK, Lasik, Lasek, PTK • Excimer laser= “excited dimer” • Two atoms form a pseudo molecule in the • • • excited state by adding electric energy but dissociate into the ground state. Argon (inert)-Fluorine (reactive) dimer emits 193 nm UV radiation. The cornea absorbs UV, so intraocular penetration is greatly reduced. Each photon has 6. 4 e. V, sufficient to break intramolecular bonds
Excimer Laser • Delivery of high energy to small area causes tissue removal – (ablation/disintigration) • The temperature is very high, but the amount of heat produced is small, minimizing collateral damage. Absorbed in first nanometer of tissue. • USED for PRK, Lasik, Lasek, PTK (phototherapeutic keratectomy)
Excimer • Broad beam- traditional lasik • Scanning Slit- Nidek EC-5000. allows more tissue • removed from center than periphery (or vice versa) Flying Spot – Laser system including a laser bean delivery system and eye tracker responsive to movement of the eye. Shots are fired in a sequence and pattern such that no laser shots are fired in a consecutive location and no consecutive shots overlap. The pattern is a response to the movement of the eye. – http: //www. patentstorm. us/patents/7220255. html
PRK • Each laser pulse ablates surface tissue to a dept of. 4 -. 5 microns • Diameter of the laser is 1 -7 mm (controlled by apeture) – Haloes if apeture is 3. 5 -4 mm • Alphagan, pilo, artificial pupil contact lens – 6 -7 mm is better, but need to ablate more cornea
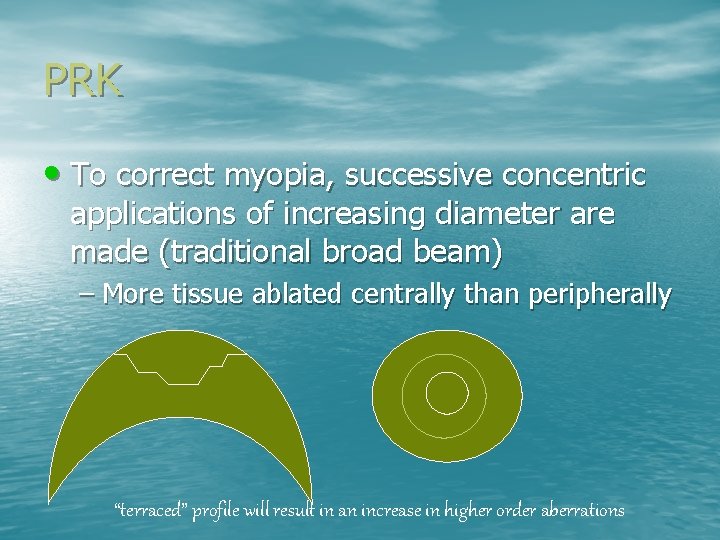
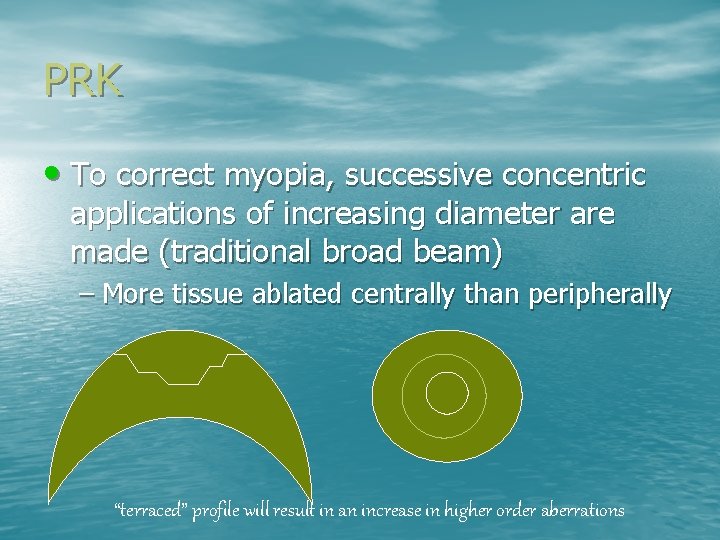
PRK • To correct myopia, successive concentric applications of increasing diameter are made (traditional broad beam) – More tissue ablated centrally than peripherally “terraced” profile will result in an increase in higher order aberrations
PRK • For higher myopia, make more rings and try to smooth out the junctions – Still, less predictable outcome, more likely to regress and higher risk of scarring
Lasik • Same profiles as PRK – Less scarring, regression, earlier stabilization, better predictability Formula for figuring out if sufficient thickness exists- must do for the wavescan data Don’t use pachy- orbscan or pentacam is better (pentacam probably best)
• Larger refractive errors have greater chance of scarring. • Lasik is like a scl, will correct for both internal and lenticular astigmatism. • What power to consider for MV? – 2. 50? 1. 50 (probably better). Leaves margin for hyperopic outcome. Which eye to do first?

Custom Lasik
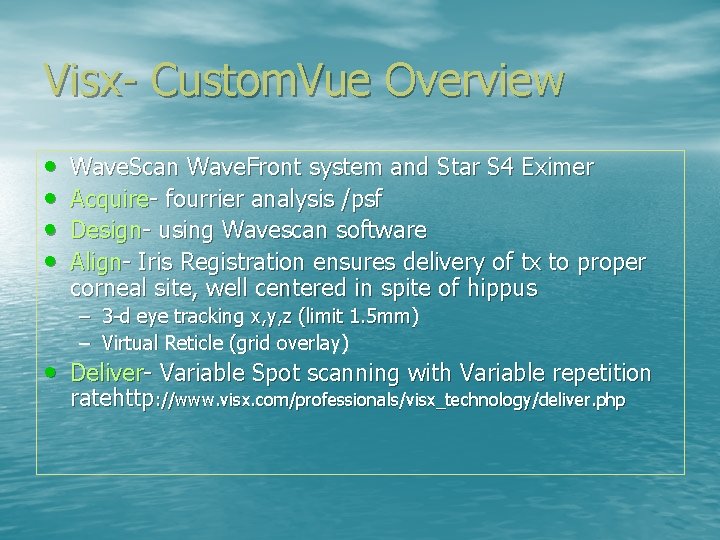
Visx- Custom. Vue Overview • • Wave. Scan Wave. Front system and Star S 4 Eximer Acquire- fourrier analysis /psf Design- using Wavescan software Align- Iris Registration ensures delivery of tx to proper corneal site, well centered in spite of hippus – 3 -d eye tracking x, y, z (limit 1. 5 mm) – Virtual Reticle (grid overlay) • Deliver- Variable Spot scanning with Variable repetition ratehttp: //www. visx. com/professionals/visx_technology/deliver. php
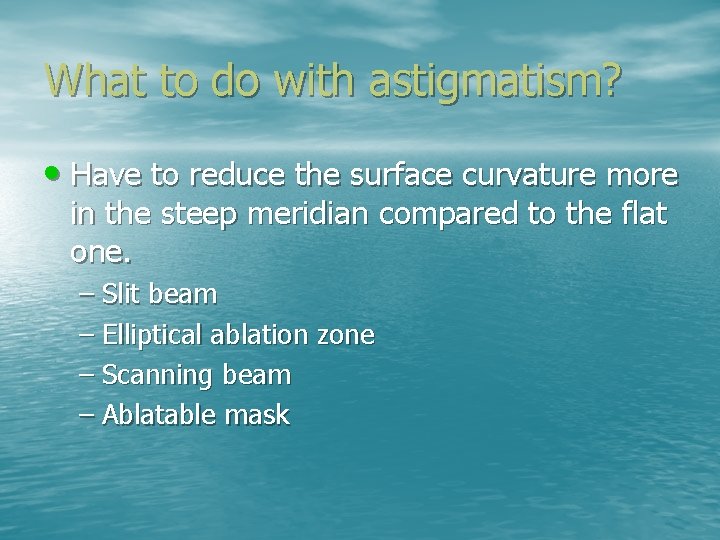
What to do with astigmatism? • Have to reduce the surface curvature more in the steep meridian compared to the flat one. – Slit beam – Elliptical ablation zone – Scanning beam – Ablatable mask
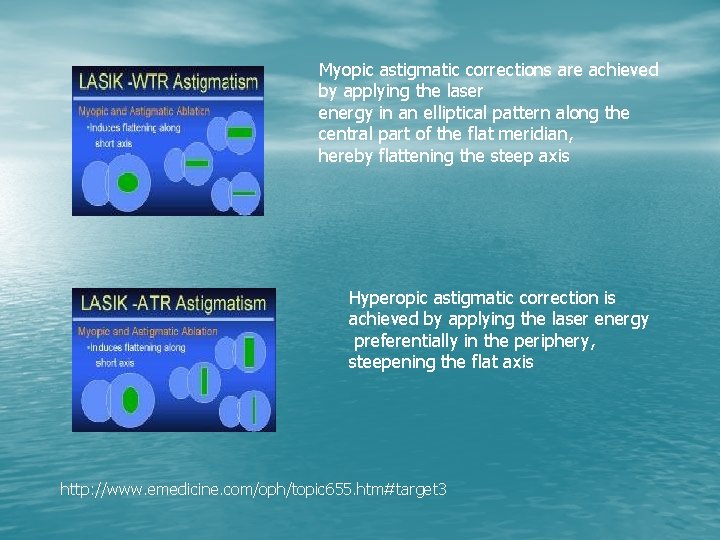
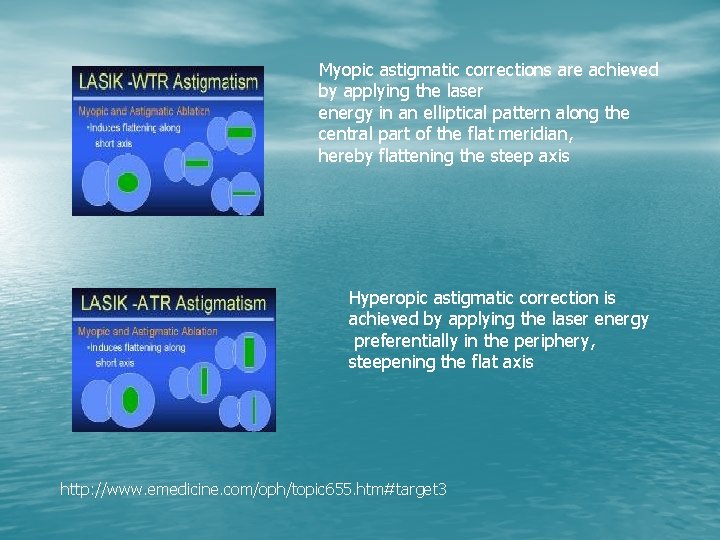
Myopic astigmatic corrections are achieved by applying the laser energy in an elliptical pattern along the central part of the flat meridian, hereby flattening the steep axis Hyperopic astigmatic correction is achieved by applying the laser energy preferentially in the periphery, steepening the flat axis http: //www. emedicine. com/oph/topic 655. htm#target 3
Slit beam • Widens for successive applications • Uniform deep ablation is produced in the long axis of the slit • The surface curvature is reduced only in the meridian where the slit widens
Ablatable mask • A plate of PMMA placed in the path of the laser beam to shield the cornea • Thinner areas of the mask are ablated first and thus allow deeper ablation of the corresponding area of the cornea • Also used to treat hyperopia
Post op irregular astigmatism • Usually because corneal thickness is insufficient • Less than 400 microns pre-op is trouble • 250 microns in bed may be insufficient • Problems seem to occur with thicker than expected flaps- intraoperative pachymetry, post op can do Visante OCT
Outline • Surface – Cornea – Excimer laser • PRK • Lasik • Lasek • PTK – Incisional • AK • PK (DLK etc) • RK – Other • CK • Intacs • Invasive – Lens – Silicone Oil • • • Clear lens extraction Single vision Multifocal Accommodating Phakic
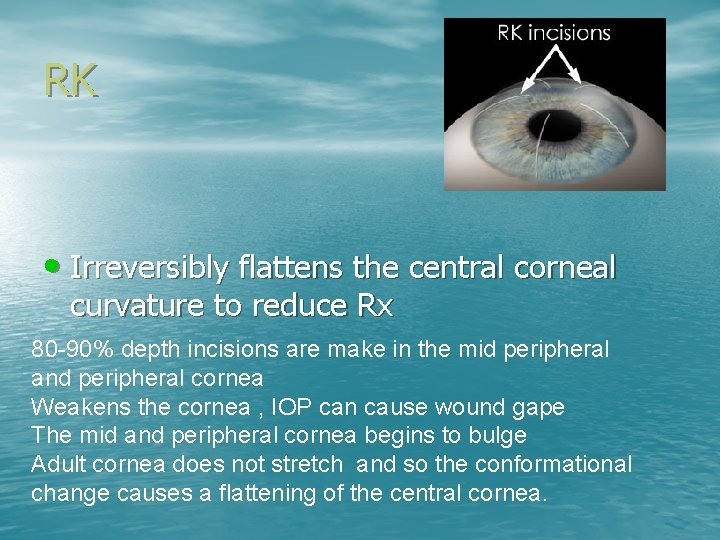
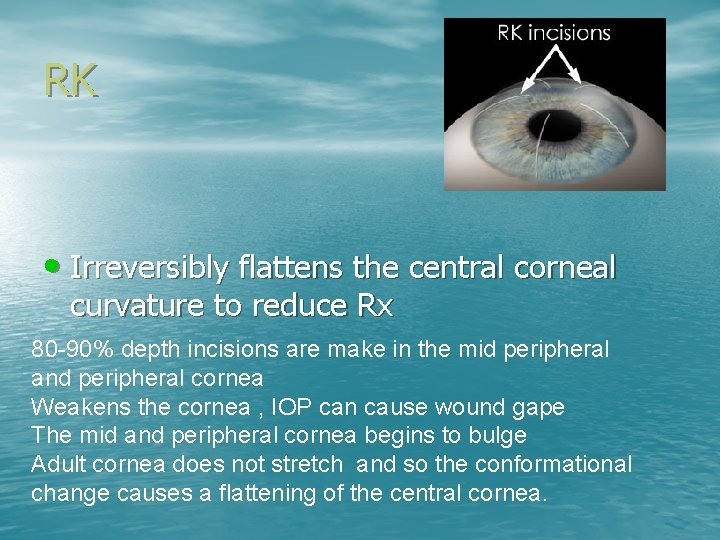
RK • Irreversibly flattens the central corneal curvature to reduce Rx 80 -90% depth incisions are make in the mid peripheral and peripheral cornea Weakens the cornea , IOP can cause wound gape The mid and peripheral cornea begins to bulge Adult cornea does not stretch and so the conformational change causes a flattening of the central cornea.
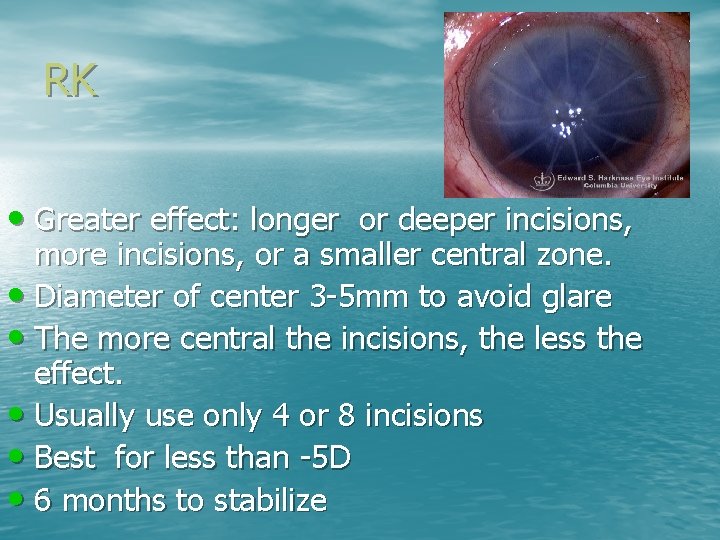
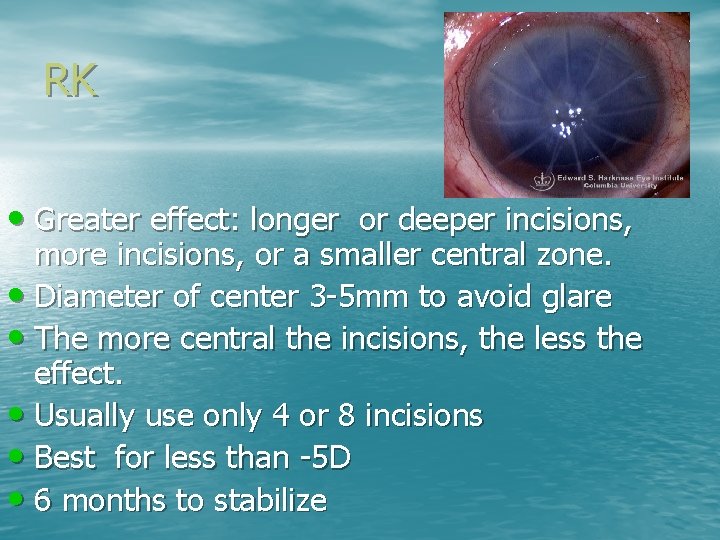
RK • Greater effect: longer or deeper incisions, more incisions, or a smaller central zone. • Diameter of center 3 -5 mm to avoid glare • The more central the incisions, the less the effect. • Usually use only 4 or 8 incisions • Best for less than -5 D • 6 months to stabilize

RK
RK • Consecutive hyperopia – Hyperopic shift continues as cornea loses integrity. – May be difficult or impossible to fit with a lens – May need transplant or running sutures to maintain integrity
Astigmatic (arcuate) Keratotomy • Surgical correction of astigmatism – Cosmetic – Post IOL – Post PK, trauma, etc. – Results somewhat unpredictable. – Hope for CL that fits or spectacles
AK • Place 1 -2 deep curved incisions perpendicular to • the steep meridian Flatten the steep meridia is matched by a steepening 90 degrees away (coupling effect) – Coupling ratio flattening/steepening – SE is about the same ratio about 1 • Effect is immediate • Subsequent healing affects outcome Wilkins, 2005 - nomograms innacurate for PK
Astigmatic keratotomy • all sutures should be removed because they can • be the cause of the astigmatism. Keratoplasty wound should be inspected for focal abnormalities. Wound dehiscence and graft override cause flattening of the central cornea in that meridian and may be best corrected by opening and resuturing the wound, despite the lengthy recovery.
Astigmatic keratotomy Arcuate incisions flatten the steeper meridian the same amount as they steepen the flatter meridian; therefore, the net effect is no change in the spherical equivalent. Arcuate incisions greater than 90° are not recommended because of the risk of late wound dehiscence.
Controlling astigmatism in cataract surgery • Place incision in steepest meridian of the cornea to reduce cyl – May be able to use spherical IOL and get good outcome – Ex: -7. 00+3. 00 x 090 – K 43. 00/44. 00@180 1 D residual cyl – Place incision at 180
Relaxing incisions • An incision causes the cornea to bulge at that site (weakens the structure) • This reduces the surface curvature of the central cornea in the meridian in which the incision is made and induces increased curvature in meridian 90 degrees away
Reducing PK cyl/ scarring cyl • Incising over 60 degrees over the steep meridian • If incisions within the graft (not at junction) effect is more predictable and preserves wound healing • Arcuate is preferred (uniform thickness) • Longer and more axial have greater effect
Wedge resections • >10 D cyl • Remove deep arcuate wedge measuring 60 -90 degrees from the graft/host junction in the FLAT meridian – Opposite of relaxing incision – Wound sutured to shorten the cornea and steepen the curvature in that meridian – The overall effect of wedge resection is to steepen the flat meridian approximately twice as much as it flattens the steeper meridian. The net effect is an increase in myopia or a decrease in hyperopia. The surgical technique involves removing a wedge of tissue along the flat meridian of the cornea.

Compression sutures • Tight suture in the flat meridian will increases the curvature of the cornea adjacent to it and displace the apex away from it – Causes the apex of the cornea to bulge away – Note the topography will change if suture dissolves or breaks – Compression sutures used simultaneously with astigmatic keratectomy can markedly increase the effect of the incisions. Compression sutures are placed 90° from the incisions. Suture depth should be approximately 80% of the corneal thickness. The sutures are tied with a slipknot, and tension is adjusted under intraoperative keratometric or keratoscopic control until an overcorrection of 25 -50% is achieved.
Outline • Surface – Cornea – Excimer laser • PRK • Lasik • Lasek • PTK – Incisional • AK • PK (DLK etc) • RK – Other • CK • Intacs • Invasive – Lens • Clear lens extraction • Single vision • Multifocal • Accommodating • Phakic – Silicone Oil
Conductive Keratoplasty • Increases the asphericity of the cornea • Initially conceived as an alternative to hyperopic excimer procedures. • MV trial with progressive CL useful. • Some glare • Leave room to move • Set up expectations • Nobody really sure how it works
Post operative • Still have to use reading or driving glasses • Glare/ monocular diplopia- usually resolves • Somewhat difficult to fit with lenses • Steep bc with aspheric surfaces • Useful post CE or Lasik
Intacs Up to -3 D myopia (normals) Sufficient thickness (minimum 450 microns) Removable/ adjustable Think about Intacs then Lasik for High myopes with thinner corneas
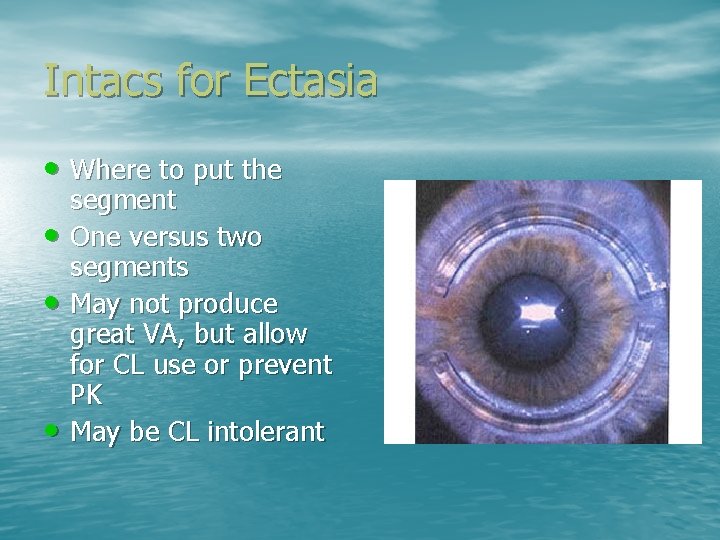
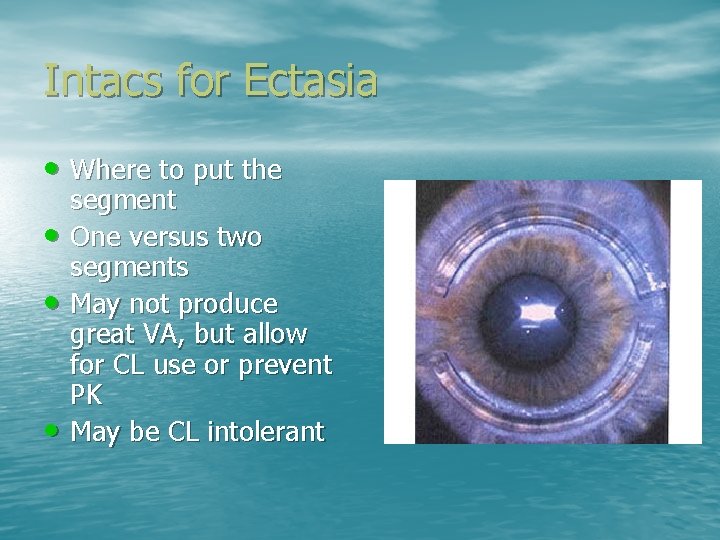
Intacs for Ectasia • Where to put the • • • segment One versus two segments May not produce great VA, but allow for CL use or prevent PK May be CL intolerant
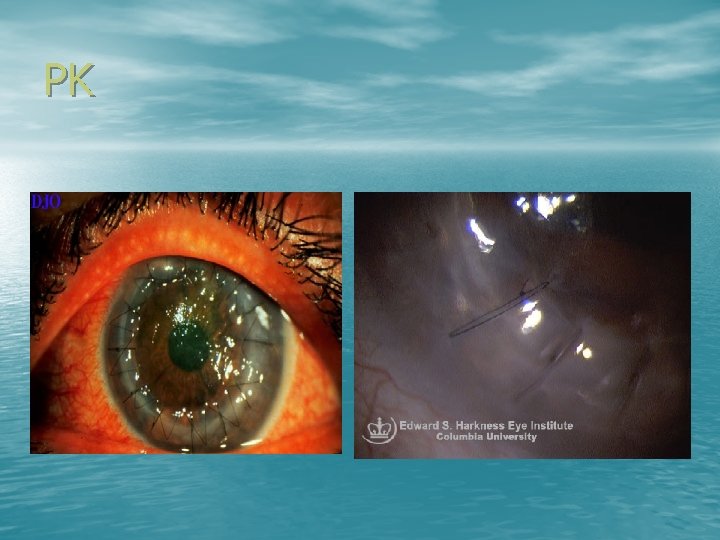
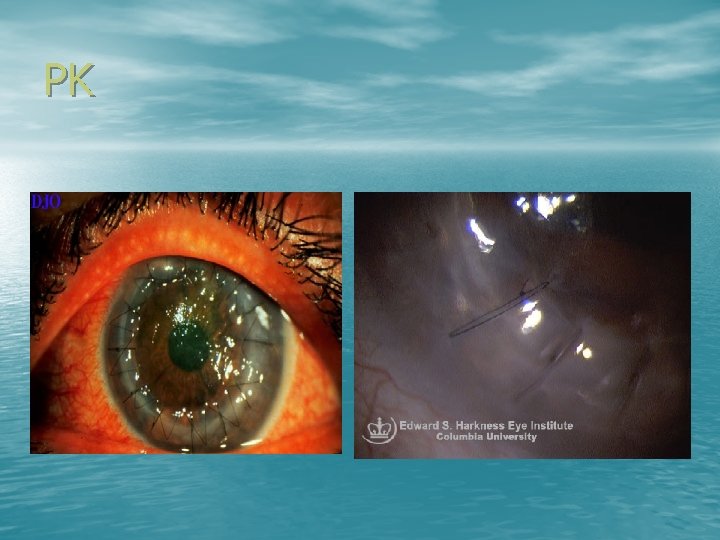
PK
PK • High amounts of irregular cylinder – 19% have 5 D or more • May need subsequent AK • Up to 50% still need RGP design • Expectations • Lamellar techniques promising • Relaxing incisions and/or compression sutures, wedge resection, LK, excimer procedures
Suture Removal (lacs) • Basis is the same as for PK
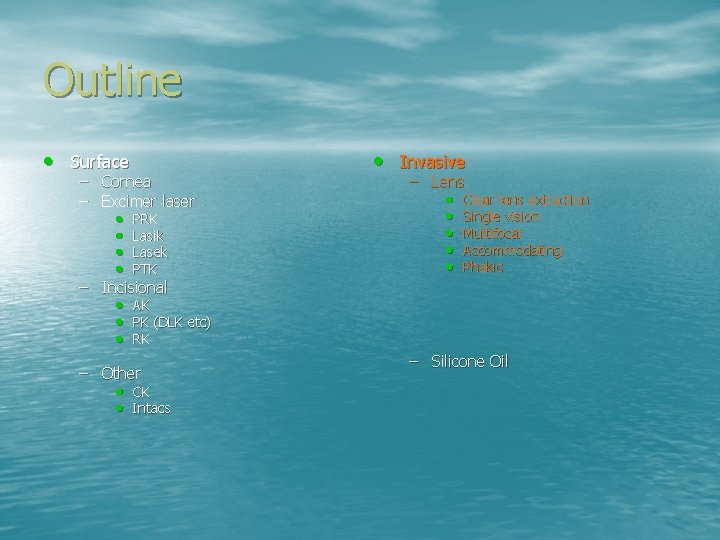
Outline • Surface – Cornea – Excimer laser • PRK • Lasik • Lasek • PTK – Incisional • AK • PK (DLK etc) • RK – Other • CK • Intacs • Invasive – Lens • Clear lens extraction • Single vision • Multifocal • Accommodating • Phakic – Silicone Oil
The lens • Change the power • Change the position • Increasingly, to manage presbyopia
IOL Calculations • Various formulas – Regression (SRK, SRKII) – Theoretical (Hoffer, Haigis, Holladay) • based on reduced eye models – One refractive surface for the cornea and thin lens for IOL
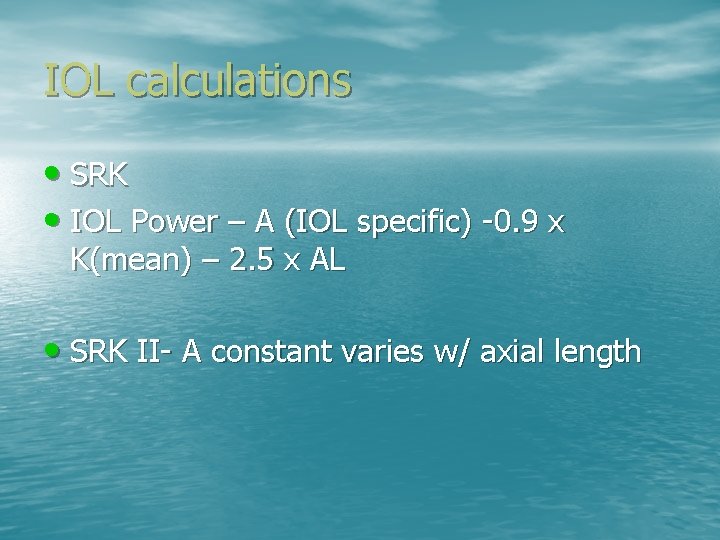
IOL calculations • SRK • IOL Power – A (IOL specific) -0. 9 x K(mean) – 2. 5 x AL • SRK II- A constant varies w/ axial length
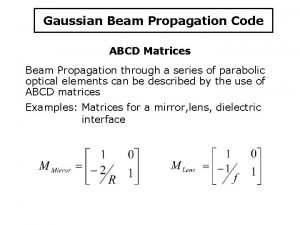
![Theoritical basis PowernALdnnKTRd d is effective lens position TR target Theoritical basis • Power-[n/(AL-d)]-(n/[n/(K+TR)]-d]) – d is effective lens position – TR = target](https://slidetodoc.com/presentation_image_h/1a06b3fd1e52fd7c53cc98ebf16ef70e/image-53.jpg)
Theoritical basis • Power-[n/(AL-d)]-(n/[n/(K+TR)]-d]) – d is effective lens position – TR = target Rx at corneal plane
What’s the difference between various theoretical formulas? • Estimated position of the IOL and the effective refractive index to transform corneal radius to power • In the US (holladay, SRK/T etc) use the AL and K for prediction of IOL position
Post Refractive SX calculations • K’s and topography tend to overestimate corneal refractive power after RS • This will cause underestimation of the IOL power leading to a hyperopic outcome
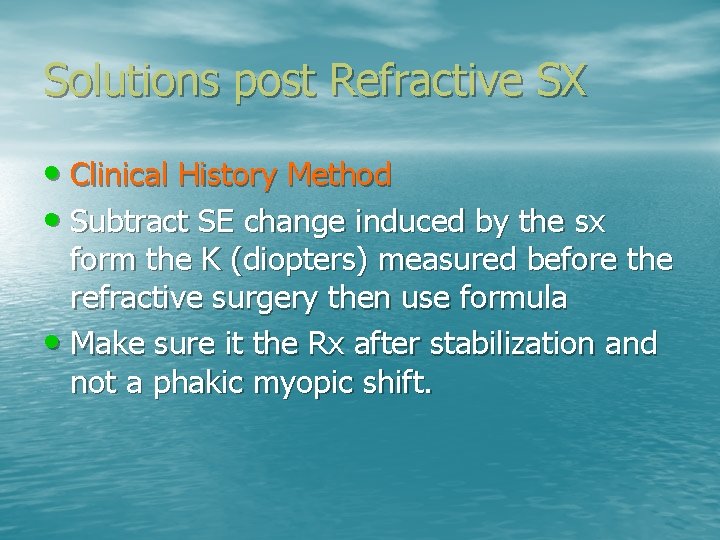
Solutions post Refractive SX • Clinical History Method • Subtract SE change induced by the sx form the K (diopters) measured before the refractive surgery then use formula • Make sure it the Rx after stabilization and not a phakic myopic shift.
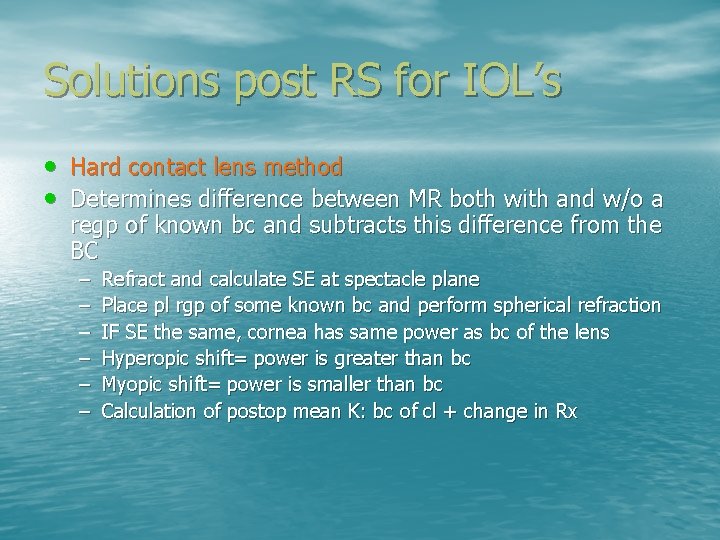
Solutions post RS for IOL’s • Hard contact lens method • Determines difference between MR both with and w/o a regp of known bc and subtracts this difference from the BC – – – Refract and calculate SE at spectacle plane Place pl rgp of some known bc and perform spherical refraction IF SE the same, cornea has same power as bc of the lens Hyperopic shift= power is greater than bc Myopic shift= power is smaller than bc Calculation of postop mean K: bc of cl + change in Rx
Solutions for post RS IOL’s • Look at difference between anterior and posterior lens surface • Pre sx, they should be the same. • Post RX, the posterior should mimic what the pre-op K’s are – Newer topography devices have this capability
Solutions for post RS iol’s • Calculate with std formula using pre-op biometry data • Enter initial ametropia as target refraction
Solutions for post RS IOL’s • Empirical correction • We know that the true corneal power can be predicted from the measured power – The effect of overestimation of corneal power is linear with respect to the amount of correction d/t refractive surgery. - Zeiss instrument : 24% has to be subtracted from measured K’s to get true K’s
Calculation of toric IOLs • Ok to use conventional formulas if all axes of all toric surfaces are aligned. Just calculate each meridian separately If use formula that bases lens position is based on K, you will get two different predicted positions Cylinder of toric lens must be aligned with axis corneal astigmatism
Toric IOL’s • Spherical front and toric back surfaces – May cause meridional magnification issues – Bitoric IOL normalizes meridional differences – Ray tracing schemes
Post Intacs IOL Calculations • Who knows?
Pediatric IOL Calculations • None work well • Issues with emmetropization • PCO • Current formulas based on adult eyes
Monovision IOL Calculations • Try to aim for -1. 50 and set up expectations • Same for any surgical monovision • Can try MF IOL plus modified MV
Re. Stor IOL • Diffraction based system, sort of like simultaneous bifocal soft contact lenses • Again, expectations
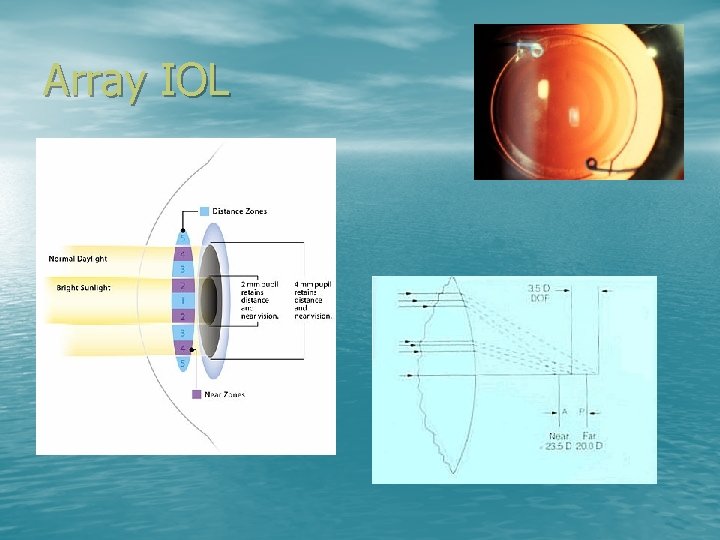
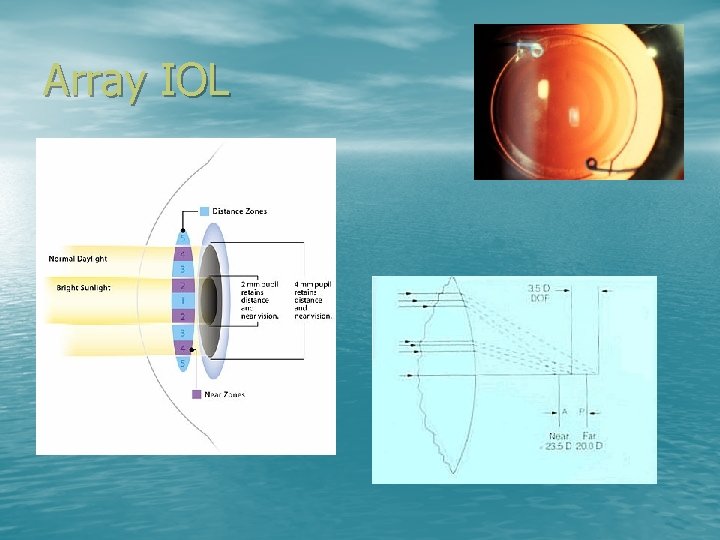
Array IOL
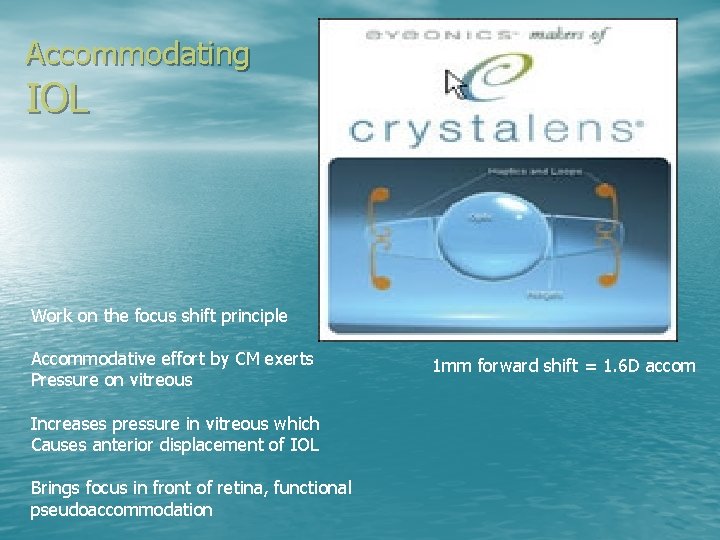
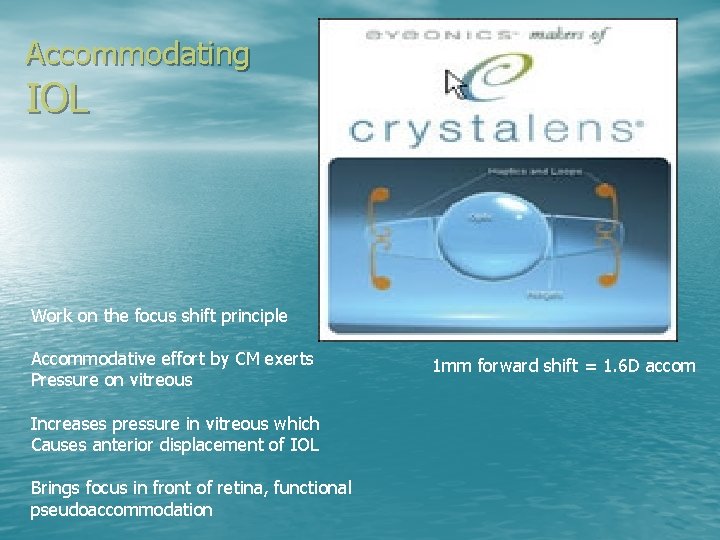
Accommodating IOL Work on the focus shift principle Accommodative effort by CM exerts Pressure on vitreous Increases pressure in vitreous which Causes anterior displacement of IOL Brings focus in front of retina, functional pseudoaccommodation 1 mm forward shift = 1. 6 D accom
• Pseudoaccommodation – Increased depth of focus – Spherical aberration
Crystalens • Silicone • Plate haptics ensure posterior position in capsular bag • Hinged haptic facilitates maximal forward movement
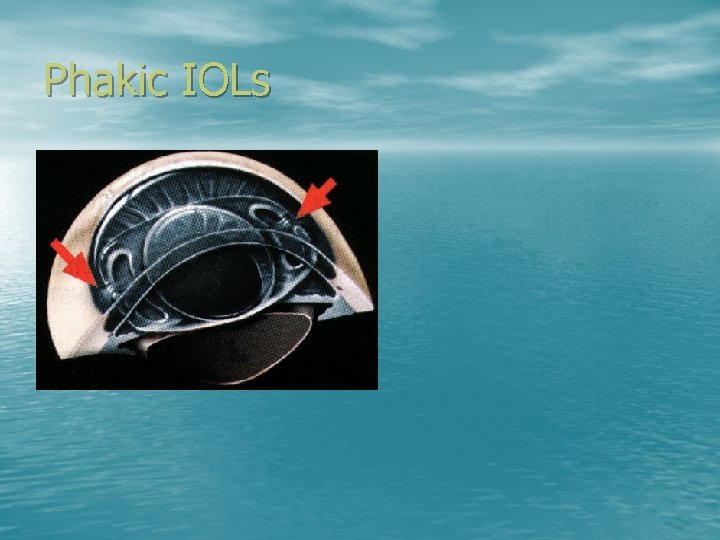
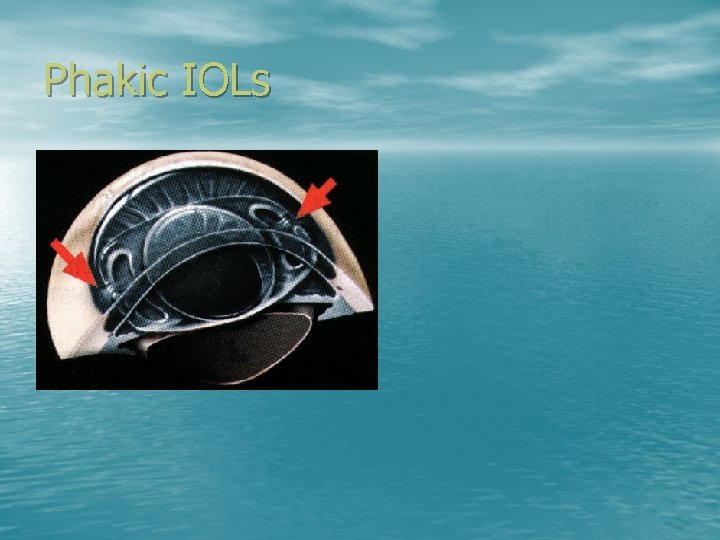
Phakic IOLs

Phakic IOL
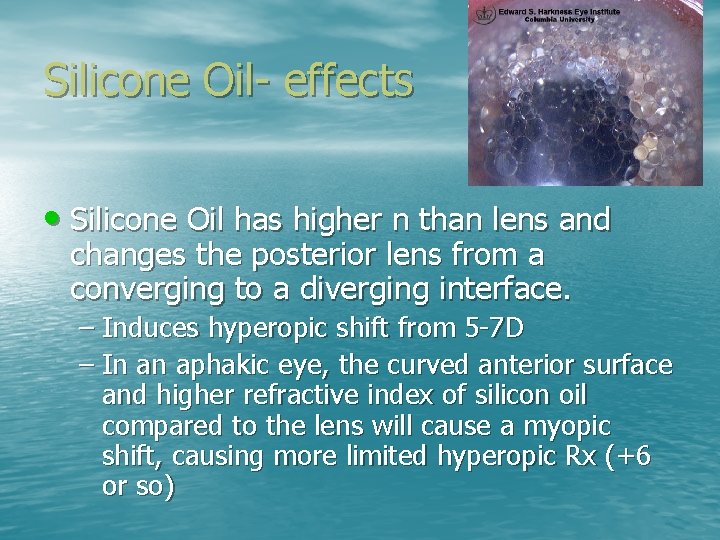
Silicone Oil- effects • Silicone Oil has higher n than lens and changes the posterior lens from a converging to a diverging interface. – Induces hyperopic shift from 5 -7 D – In an aphakic eye, the curved anterior surface and higher refractive index of silicon oil compared to the lens will cause a myopic shift, causing more limited hyperopic Rx (+6 or so)
Scleral Buckles • Induce myopia • Induce Cyl
Gas • Phakic eye will increase the refractive power of the posterior lens surface and cause a large myopic shift – May be able to do indirect w/o a lens! – Aphakic eye will makes posterior cornea highly diverging and almost neutralizes the power of the cornea
 Difference between ray optics and wave optics
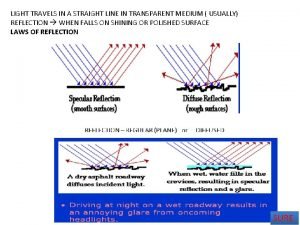
Difference between ray optics and wave optics Reflection and refraction venn diagram
Reflection and refraction venn diagram Maddox rod
Maddox rod Power of lens formula class 10
Power of lens formula class 10 Amy nau
Amy nau Iso-accommodative magnification
Iso-accommodative magnification Amy nau
Amy nau Refractive index of substances
Refractive index of substances Refractive error diagram
Refractive error diagram The refractive indices of crown glass prism for c d f
The refractive indices of crown glass prism for c d f Refractive index applications
Refractive index applications Classement chirurgie réfractive
Classement chirurgie réfractive Drude model refractive index
Drude model refractive index Refractive surprise
Refractive surprise Light refractive
Light refractive Donor acceptor ratio in physical pharmacy
Donor acceptor ratio in physical pharmacy Refractory media of the eye
Refractory media of the eye How to calculate refractive index with speed of light
How to calculate refractive index with speed of light Slimline 750 refractive index
Slimline 750 refractive index Perspex refractive index
Perspex refractive index Strabismus definition
Strabismus definition How to calculate angle of refraction
How to calculate angle of refraction Relation between refractive index and permittivity
Relation between refractive index and permittivity Permittivity refractive index relation
Permittivity refractive index relation Acs comp
Acs comp Refractive surprise
Refractive surprise Conoid of sturm
Conoid of sturm Negative refractive index
Negative refractive index Refractive power formula
Refractive power formula Tempered glass refraction
Tempered glass refraction Index of refraction of polystyrene
Index of refraction of polystyrene A b c d
A b c d Wave optics b.sc physics
Wave optics b.sc physics Geometrical
Geometrical Nonlinear optics
Nonlinear optics Astigmatisml
Astigmatisml Vergence formula
Vergence formula Ion optics simulation
Ion optics simulation Grade 10 optics review
Grade 10 optics review Free space optics
Free space optics John tyndall fiber optics
John tyndall fiber optics Free space optics
Free space optics Introduction to fiber optics
Introduction to fiber optics The spencer optics company produces an inexpensive
The spencer optics company produces an inexpensive Hotwire salisbury nc
Hotwire salisbury nc Ee
Ee Nonlinear optics
Nonlinear optics Losses in optical fiber
Losses in optical fiber Vertical
Vertical Ledlink optics inc
Ledlink optics inc Geometric optics ppt
Geometric optics ppt Optics
Optics Critical angle
Critical angle The computational complexity of linear optics
The computational complexity of linear optics Optics equation
Optics equation Eikonal equation
Eikonal equation Basic electricity and optics
Basic electricity and optics Advantages and disadvantages of optical fiber
Advantages and disadvantages of optical fiber Rainbow optics star spectroscope
Rainbow optics star spectroscope Optics plural or singular
Optics plural or singular Nicolas alba
Nicolas alba Optics
Optics Cauchy formula optics
Cauchy formula optics Maxwell equation derivation
Maxwell equation derivation Single slit envelope
Single slit envelope Geometric optics problems
Geometric optics problems Optics
Optics Curtis parry
Curtis parry Optics poynting's theorem
Optics poynting's theorem Divergin
Divergin Modern optics experiment
Modern optics experiment Cardinal refraction
Cardinal refraction What medical procedure uses fiber optics bill nye
What medical procedure uses fiber optics bill nye Iso 9001 drawing standards
Iso 9001 drawing standards Snell's law
Snell's law Clearly explain what is meant by the term geometric optics
Clearly explain what is meant by the term geometric optics