Managing the Refractive Surprise After Toric IOL Placement
- Slides: 12
Managing the Refractive “Surprise” After Toric IOL Placement Brad H Feldman, MD Derek Del. Monte, MD Alan N Carlson, MD Duke Eye Center Durham, NC Authors have no financial interests
Case Presentation 53 year-old man referred to the Duke Eye Center for 2 nd opinion regarding residual astigmatism after undergoing cataract extraction with Toric IOL left eye Patient originally chose Toric IOL on surgeon recommendation to achieve astigmatic neutrality and decrease spectacle dependence Patient completely unsatisfied with outcome immediately after surgery Surgeon indicated there was nothing more he could offer the patient
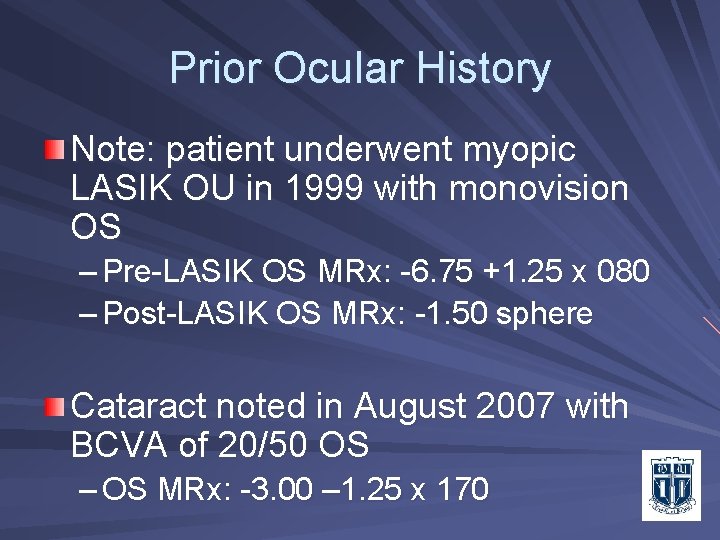
Prior Ocular History Note: patient underwent myopic LASIK OU in 1999 with monovision OS – Pre-LASIK OS MRx: -6. 75 +1. 25 x 080 – Post-LASIK OS MRx: -1. 50 sphere Cataract noted in August 2007 with BCVA of 20/50 OS – OS MRx: -3. 00 – 1. 25 x 170
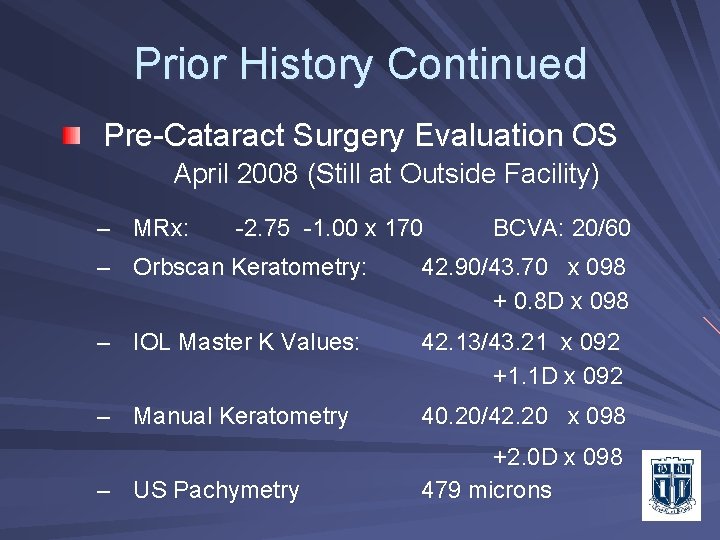
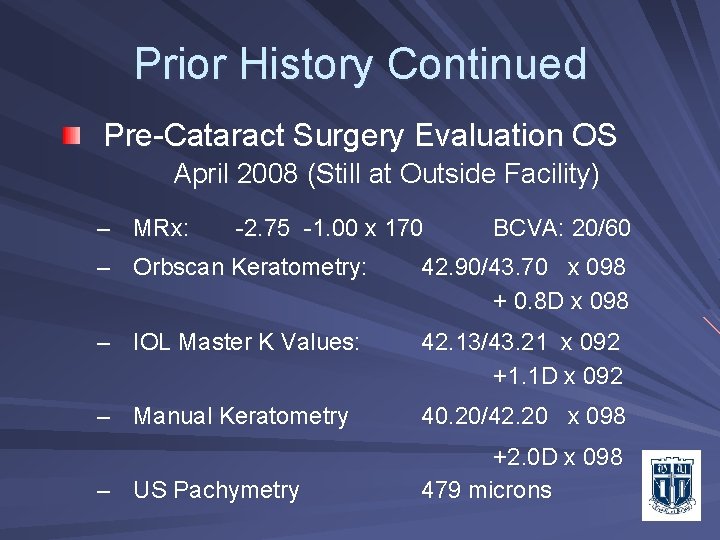
Prior History Continued Pre-Cataract Surgery Evaluation OS April 2008 (Still at Outside Facility) – MRx: -2. 75 -1. 00 x 170 BCVA: 20/60 – Orbscan Keratometry: 42. 90/43. 70 x 098 + 0. 8 D x 098 – IOL Master K Values: 42. 13/43. 21 x 092 +1. 1 D x 092 – Manual Keratometry 40. 20/42. 20 x 098 – US Pachymetry +2. 0 D x 098 479 microns
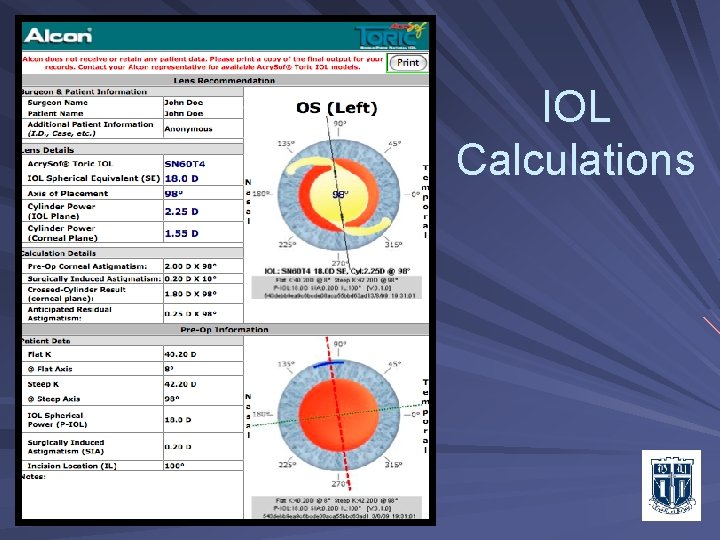
IOL Calculations: (Outside Facility) Patient chose Toric “Premium” Lens Power: – IOL Master Derived – SRK/T Clinical History Method Astigmatism Power: – Alcon Acry. Sof Toric Calculator Used – Based on Manual K’s As per instructions of online calculator Note difference in power of K axes between Orbscan, IOL Master, and Manual K’s (see prior slide)
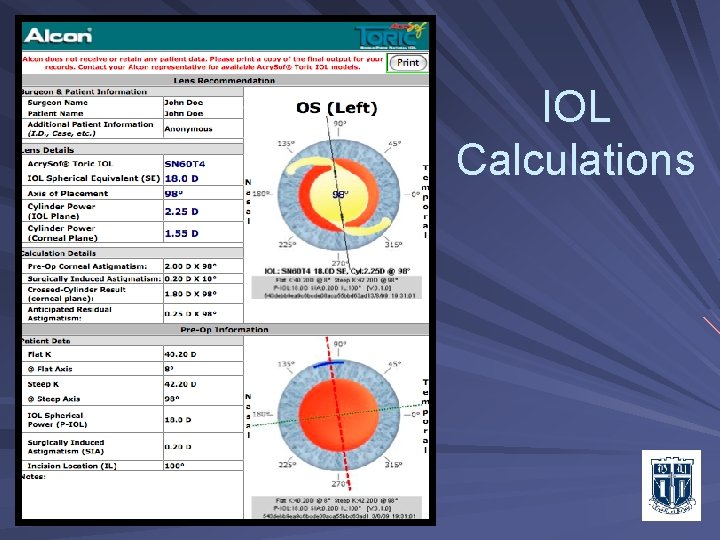
IOL Calculations
Postoperative Course UCVA 20/60; plano – 2. 50 x 100 = 20/20 Examination – Axis flipped despite properly achieving the intended axis – Position: asymmetric fixation, superior loop in sulcus, inferior loop in bag, optic decentered superiorly and tilted Assessment: – Pantoscopic tilt with optic decentration making astigmatic correction by the IOL overly effective, causing over correction and axis flip Plan: Reposition lens for symmetric bag fixation – Please view attached video for details
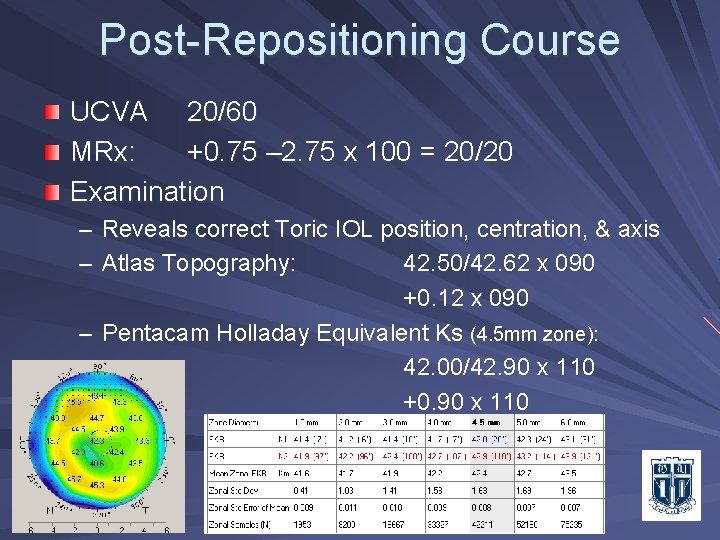
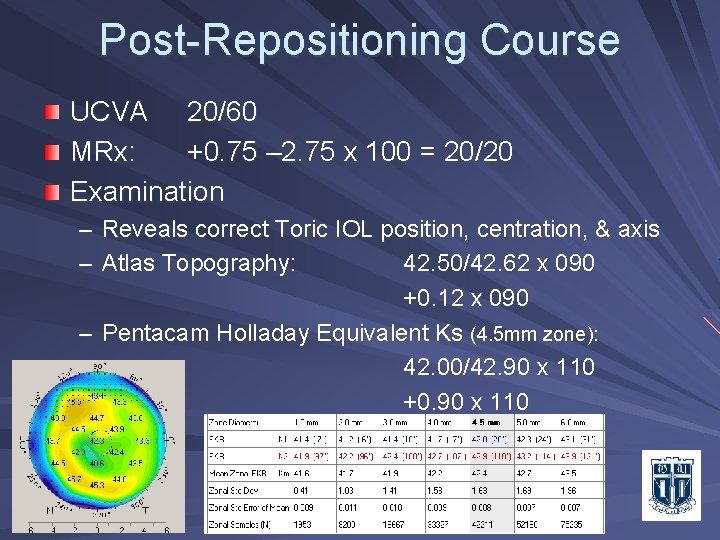
Post-Repositioning Course UCVA 20/60 MRx: +0. 75 – 2. 75 x 100 = 20/20 Examination – Reveals correct Toric IOL position, centration, & axis – Atlas Topography: 42. 50/42. 62 x 090 +0. 12 x 090 – Pentacam Holladay Equivalent Ks (4. 5 mm zone): 42. 00/42. 90 x 110 +0. 90 x 110
Post-Repositioning Course Our initial assessment in consultation supported an improperly implanted IOL as the culprit for the astigmatic axis flip. The patient’s outcome after his second surgery indicates the original IOL selection error was based on using a post-LASIK manual “K” reading. Additional data revealed this was inconsistent with other astigmatism measurements. Patient remains frustrated and is now contemplating IOL exchange.
Discussion The differential diagnosis for a “surprise” result after surgery includes: – Wrong astigmatic power calculation and IOL selection – Incorrect astigmatic axis alignment – Incorrect Toric IOL location resulting from decentration or optic tilt – Surgical or postoperative induction of astigmatism related to wound healing or IOL optic rotation
Summary 53 yo h/o LASIK unsatisfied due to astigmatism following cataract surgery with Toric IOL – Toric IOL was selected on the basis of manual “K” readings as recommended by IOL selection protocol – Original measurements were inconsistent: IOL Master ≠ Orbscan ≠ Pentacam ≠ Manual “K”’s Our error was attributing the initial surgical outcome entirely to faulty IOL fixation and position – There was optic tilt and decentration secondary to asymmetric capsular fixation from the original surgery Astigmatism remained despite proper repositioning – This suggests the original surgeon used manual “K” readings which were incorrect after previous LASIK surgery
Conclusion Measuring corneal astigmatism after refractive surgery requires multiple methods and more critical analysis for consistency before recommending astigmatism-correcting Toric IOLs. Critical analysis and caution are warranted when considering a Toric IOL in cases having discrepancies between different methods of “K” readings