Introduction to Contact Lenses Amy C Nau History



- Slides: 32
Introduction to Contact Lenses Amy C. Nau
History • 1636 described by Descartes • 1886 first therapeutic lens to aid healing after cataract surgery • 1888 first lens for KC- scleral • 1899 -1912 first concepts of the corneal lens • 1930’s non glass materials • 1948 corneal lenses developed • 1950’s hydrogels • 1970’s rgp • 1990’s silicone hydrogel materials
Demographics • • 32 million Americans wear lenses 98% single vision 2% bifocal 87% soft 12% rgp 1% pmma 66% disposable
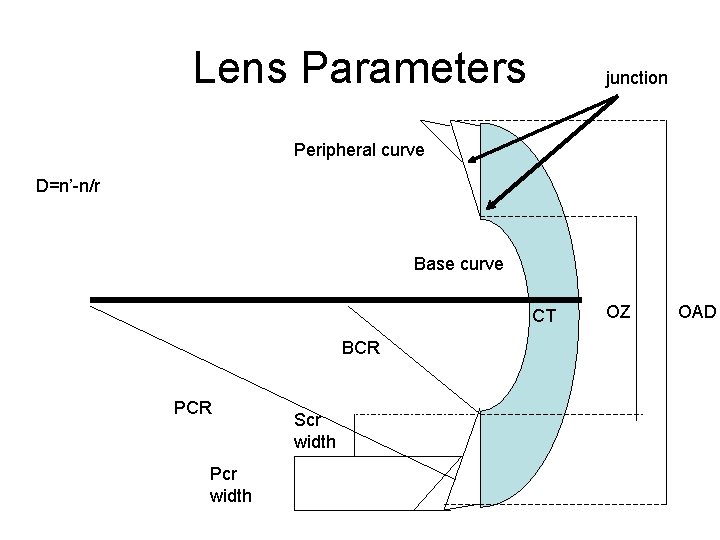
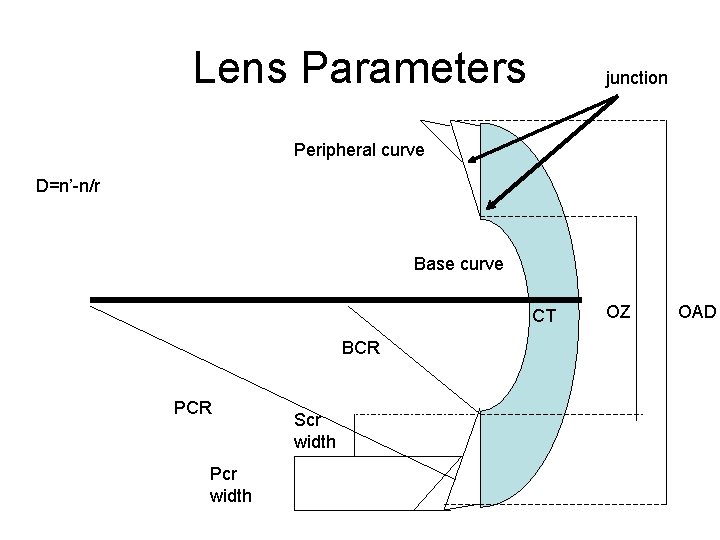
Lens Parameters junction Peripheral curve D=n’-n/r Base curve CT BCR Pcr width Scr width OZ OAD
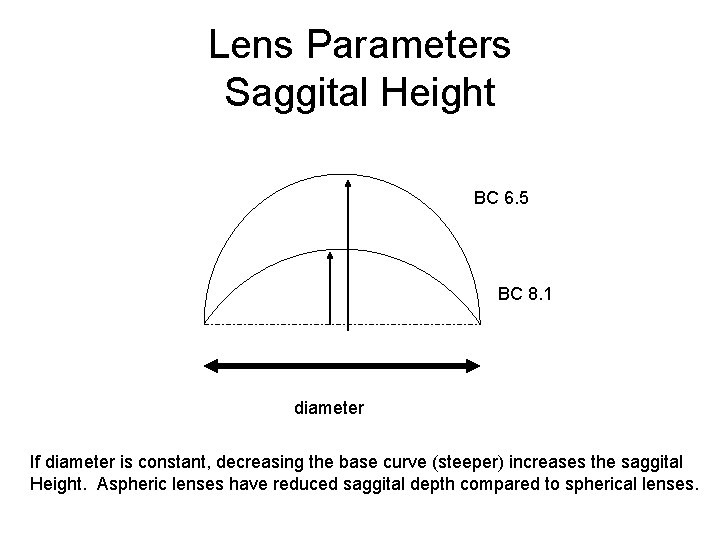
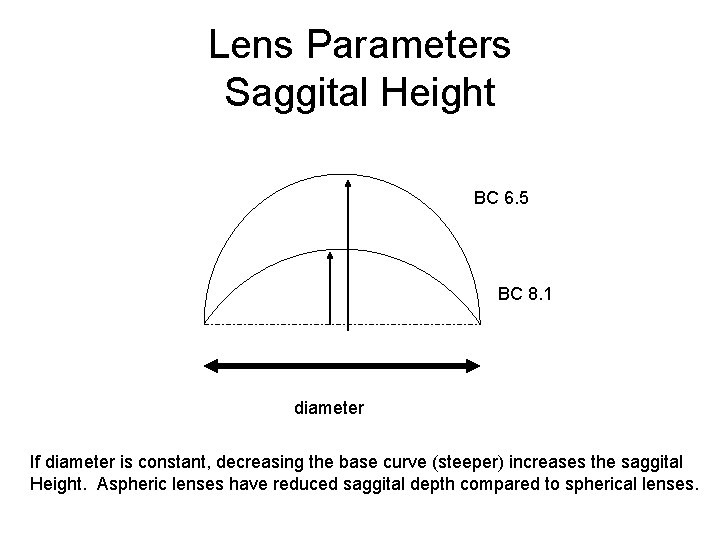
Lens Parameters Saggital Height BC 6. 5 BC 8. 1 diameter If diameter is constant, decreasing the base curve (steeper) increases the saggital Height. Aspheric lenses have reduced saggital depth compared to spherical lenses.
Anatomy of the Contact Rx • Brand/BC/power/diameter/oz/ct/peripheral curve details/material
Oxygen • Dk- measures oxygen permeability of a material. D= diffusion coefficient for oxygen movement in the material k=solubility constant of oxygen in material • Dk/t= the Dk value divided by the center thickness (t). Measures oxygen transmissibility
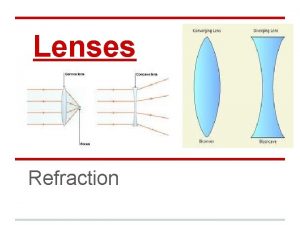
Lens Designs • Aspheric – Peripheral only, total, bi(posterior OZ/ant pc) • • Ballasted (prism) Fenestrated Lenticular (aphakia) Toric – FST, Bi • Truncated
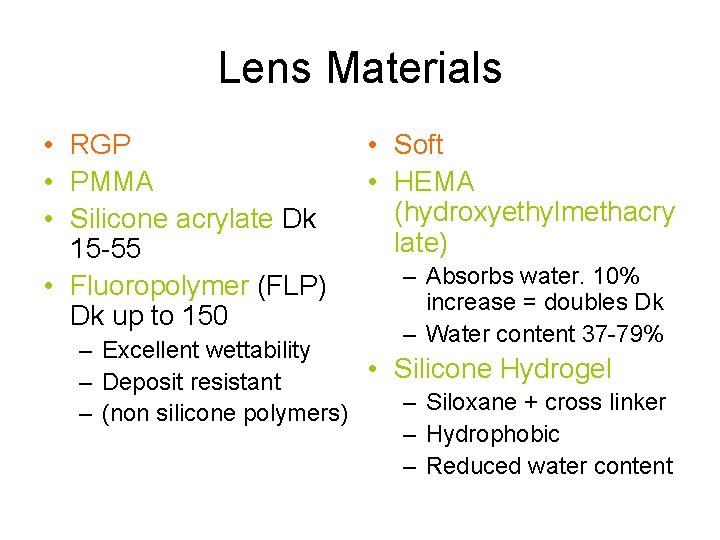
Lens Materials • RGP • PMMA • Silicone acrylate Dk 15 -55 • Fluoropolymer (FLP) Dk up to 150 • Soft • HEMA (hydroxyethylmethacry late) – Absorbs water. 10% increase = doubles Dk – Water content 37 -79% – Excellent wettability • Silicone Hydrogel – Deposit resistant – Siloxane + cross linker – (non silicone polymers) – Hydrophobic – Reduced water content
Instruments • • Keratometer Lensometer- convex side up (bvp) Slit lamp Topography Radiuscope CL comparators-project image 20 x Thickness gauge
Patient Evaluation • Contraindications – – – Chronic blepharoconjunctivitis Recurrent/inflamed pterygium or pinguecula Bells Palsy with corneal anesthesia Poor hygeine Chemical exposures Severe allergy Inability to handle lens Very dry eye TED Uncontrolled Dm AIDS?

History • • Full medical hx Ocular hx Medication hx Contact lens hx Spectacle hx Hobbies/occupational needs Motivation
Conditions that cause problems • • • Chronic allergy Dry eye GPC Recurrent infections Sometimes prior sx Neovascularization Sometimes strabismus Pregnancy Antihistamine use, OCP Mental status Age +/Lens noncompliance
Physical Examination • Visual acuity / MR • Lid assessment (include upper and lower tarsus), blink patterns, mgd/bleph, apeture • Basic dry eye workup (tbut, LG, Na. Fl, Zone quick) • Corneal status/health, esp epi, old scars and neo • Pupil size, HVID • Keratometry/corneal shape
Lens Selection • • Motivation Current lens problems= need to solve Occupational needs Cosmetic needs Maintain health of eye Cost Compliance
Selection Process- Advantages and Disadvantages • SOFT • RGP Once the modality is selected, next step is to pick the material and the solution Finally, brand power
Soft Lenses • BC range 6. 0 to 11. 0 but most are 8. 4 to 9. 0 • Power range -55 D to +60 D but most are +/ - 10 D • Diameter 11. 0 to 24. 00 mm but most are 13. 00 to 15. 00 mm Tyler’s quartery is an invaluable resource
Soft Classifications • Water Content – Low 37 -45% (DW); medium 46 -58%; high 59 -79% (EW) – More water = thicker – Ionicity • Manufacturing process – Spin casting, lathe cutting, cast molding • • Lens design Function (DW, EW, prosthetic etc) Color Bifocal/monovision Therapeutic (bandage, cosmetic Aphakic Toric (double slab off, prism ballast, truncation) Thickness
Extended Wear • • • Use with caution Make sure eye is healthy Compliant pt Understand accept risk Willing to have regular f/u Willing to remove lenses and wear glasses if needed. Remove q 6, clean leave out for 24 h if possible then reinsert EW risk of UK 20. 9/10 K versus 4. 1 per 10 K
F/U visit for EW • • Acute hypoxia (CLARE) Microcystic edema GPC K neo Striae Infiltrates SPK If found, d/c EW.

Soft fitting evaluation • • • Well centered 0. 5 to 1. 0 mm movement with blink Limbal coverage (at least 1. 0 mm beyond) Stable vision Three point touch
Troubleshooting • Decentration- steepen bc or increase diameter, no spin cast lenses • Late decentration- look for deposits, GPC • Minus OR- flatten BC • Unstable VA- flatten BC if sphere (flexure) – Tight lens clear after blink, loose lens burred after blink • Unstable VA (toric) steepen BC, increase diameter, change modality • Too tight- flatten BC or reduce diameter
Follow up • Be clear about lens regimen • Make sure they can I/R • F/U usually about 3 -4 weeks with cls on 4+hours • VA, OR, fit assessment, remove lens, examine for problems, stain with Na. Fl
CL problem • RX: • OD: -6. 75 -2. 75 x 165 • Os: -8. 00 -0. 75 x 180

RGP lenses- fitting philosophies • • Small and thin-max tear circulation and oxygen Vault apex Small cornea= steep; large cornea = flat Small and steep lens ; large and flat lens On flat K Steeper or flatter than K IP, bit steeper than K, smaller diameter, thin edges • LA (increased comfort); flatter than K, larger
RGP fitting technique • Select the fit you want to use for the pt based on physical exam, MR and K. • Select diagnostic lens if available, evaluate fit, perform OR. • Select material you want to use • Select care regimen
RGP fitting- determining lens power and base curve • Must have MR and Keratometry
RGP fitting- problem
RGP fit- troubleshooting • Discomfort- lens edge (too thick, too sharp, poor blend) • Excessive movement- too flat, limbus irritated. Steepen bc or increase diameter. • Too tight- edema, discomfort, redness. Flatten BC, decrease diameter, flatten PC • Vision-OR, flexure, decentration, deposits, incorrect power • Poor wetting d/t partial blink • Deposits- enzyme, surfactants, change material, plasma tx • Flexure- Over K, increase CT, stiffer material, reduce OAD, reduce OZ • Solution hypersensitivity- try one with different preservative.
Solutions/Lens Care • Surfactants to solubilize debris/mucous/lipids. Remove surface contaminants. RUB and RINSE off. • Disinfection-killing infectious organisms – Chemical, hydrogen peroxide, thermal, UV • Enzyme cleaners remove deposits chemically bound to the lens (lipoprotein, denatured lysozyme) – Papain, pancreatin, subtilisin
Solutions/Lens Care • Wetting agents- reduce wetting angle making lens more comfortable (rgp) q
Follow up • Lens care regimen, insertion and removal and wearing schedule should be outlined • F/U in about one month with cls on 4 h • Visual acuity, OR, lens evaluation, remove lens and evaluate eye.
 Amy nau
Amy nau Nau optical
Nau optical Amy nau
Amy nau Contact lens drawing
Contact lens drawing Menicare gp cds
Menicare gp cds Bionic contact lens
Bionic contact lens Advantages of contact lenses
Advantages of contact lenses Which force
Which force Which of the following is sliding contact bearing
Which of the following is sliding contact bearing What is a contact force
What is a contact force Contact and noncontact forces
Contact and noncontact forces Paranochyia
Paranochyia Air resistance contact or noncontact
Air resistance contact or noncontact Dangling bond in fullerene
Dangling bond in fullerene Service marketing chapter 2
Service marketing chapter 2 Contact force
Contact force Air resistance contact force
Air resistance contact force Nau virtual desktop
Nau virtual desktop Toothless hockey players
Toothless hockey players Off campus transfer student housing in flagstaff
Off campus transfer student housing in flagstaff Nau.edu graduate college
Nau.edu graduate college Northern arizona university blackboard
Northern arizona university blackboard Rough endoplasmic reticulum diagram a level biology
Rough endoplasmic reticulum diagram a level biology Nau textbooks
Nau textbooks Nau cayuse
Nau cayuse Nau course evals
Nau course evals Nau course evaluations
Nau course evaluations Nau download microsoft office
Nau download microsoft office Lifelong learning mississauga
Lifelong learning mississauga Nau reverse transfer program
Nau reverse transfer program Me·te·o·riʹzo·mai
Me·te·o·riʹzo·mai Power of lens formula class 10
Power of lens formula class 10 Maddox rod
Maddox rod