Non viral hepatitis Dr nadia ezzawi gastroenterology department

- Slides: 34
Non viral hepatitis Dr nadia ezzawi gastroenterology department
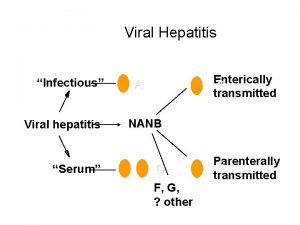
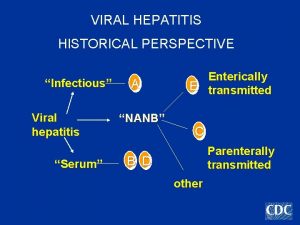
Hepatitis: • It is wide spread liver damage in which variable numbers of hepatocytes undergo necrosis. • Causes: • Viral infection(A, B, C, D, E, CMV, EBV, HSV) • Bacterial(leptospirae , toxoplasma gondii , coxiella burneti) • Drugs : methetroxate , acetaminophen , valporate , diclofenac , INH, anticonvaulsants , sulfonamide , Pyrazinamide , rifampicin. • Toxins : alcohol &other Poisons: mushroms , carbon tetrachloride. • Metabolic : wilsons , fatty changes in pregnancy. • Ischemic: heart failure , shock , budd ghiari syndrome.
Drug induced hepatitis • drug metabolism • is conversion of fat soluble drugs to water soluble metabolites occures in the liver. • This mechanism is mediated by agroup of mixed function oxidase enzymes. • Two types of reaction takes place: • Type I reaction: oxidation or reduction of drugs. • Type II reaction : conjugation ----- metabolites of no pharmacological activity -------excreted in the bile or urine • The rate of drug metabolism varies in relation to : - genetic factors. - nutritional factors. - induction or inhibition of the enzymes. - drug interactions.
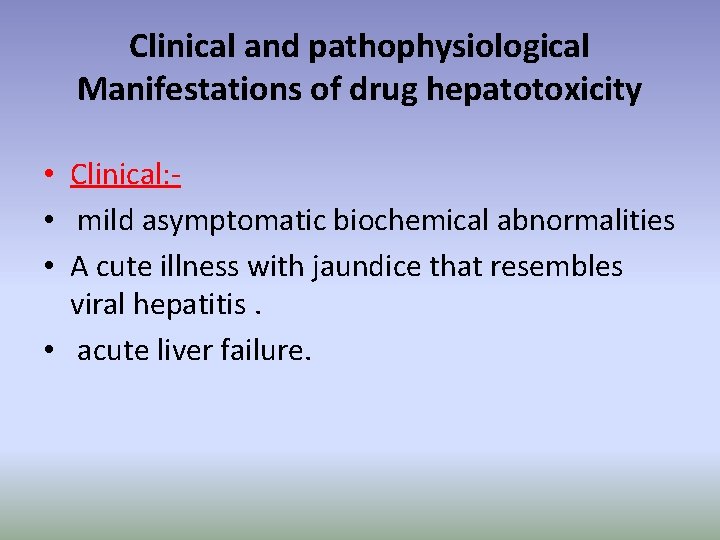
Clinical and pathophysiological Manifestations of drug hepatotoxicity • Clinical: • mild asymptomatic biochemical abnormalities • A cute illness with jaundice that resembles viral hepatitis. • acute liver failure.
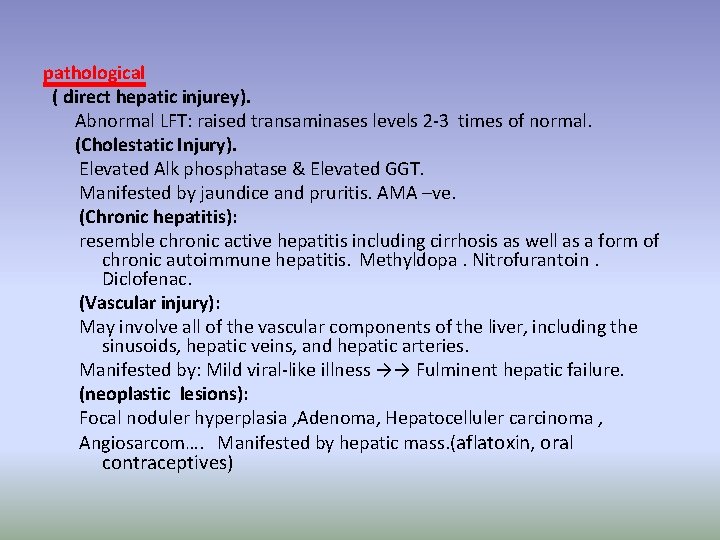
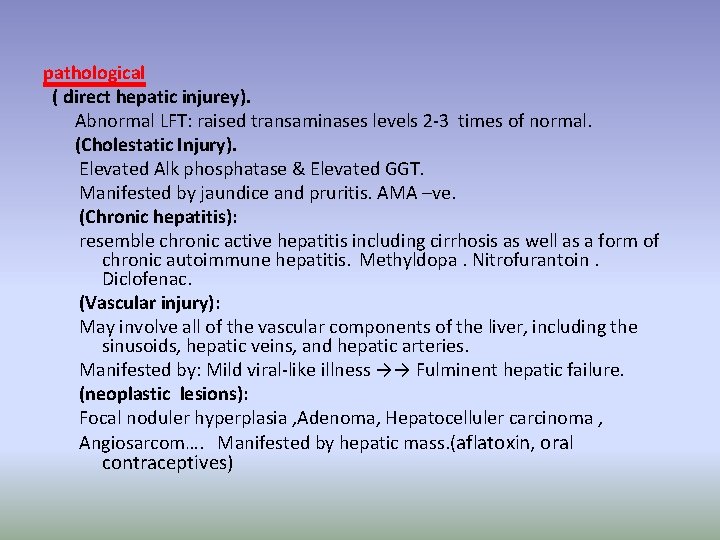
pathological ( direct hepatic injurey). Abnormal LFT: raised transaminases levels 2 -3 times of normal. (Cholestatic Injury). Elevated Alk phosphatase & Elevated GGT. Manifested by jaundice and pruritis. AMA –ve. (Chronic hepatitis): resemble chronic active hepatitis including cirrhosis as well as a form of chronic autoimmune hepatitis. Methyldopa. Nitrofurantoin. Diclofenac. (Vascular injury): May involve all of the vascular components of the liver, including the sinusoids, hepatic veins, and hepatic arteries. Manifested by: Mild viral-like illness →→ Fulminent hepatic failure. (neoplastic lesions): Focal noduler hyperplasia , Adenoma, Hepatocelluler carcinoma , Angiosarcom…. Manifested by hepatic mass. (aflatoxin, oral contraceptives)
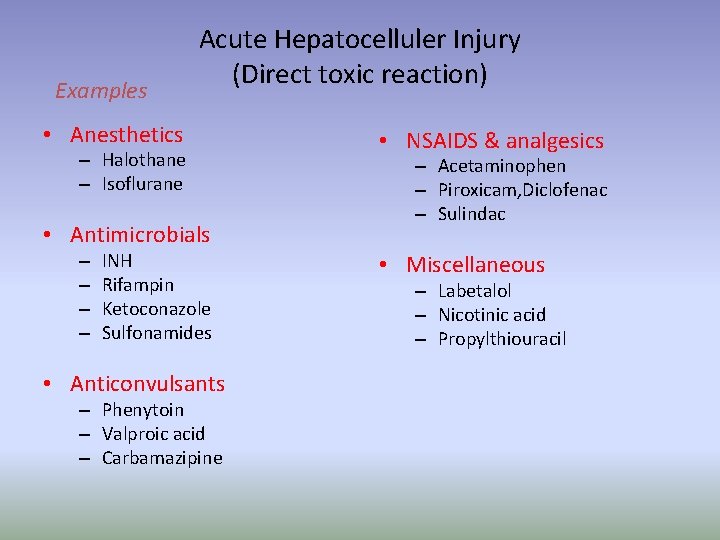
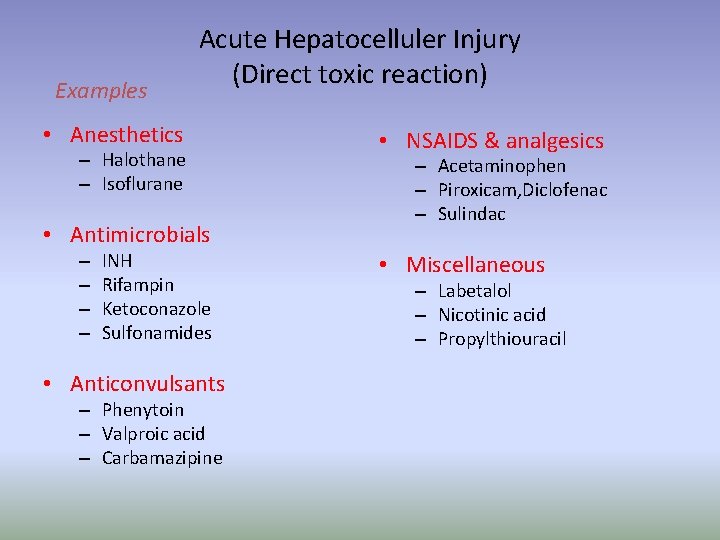
Examples Acute Hepatocelluler Injury (Direct toxic reaction) • Anesthetics – Halothane – Isoflurane • Antimicrobials – – INH Rifampin Ketoconazole Sulfonamides • Anticonvulsants – Phenytoin – Valproic acid – Carbamazipine • NSAIDS & analgesics – Acetaminophen – Piroxicam, Diclofenac – Sulindac • Miscellaneous – Labetalol – Nicotinic acid – Propylthiouracil
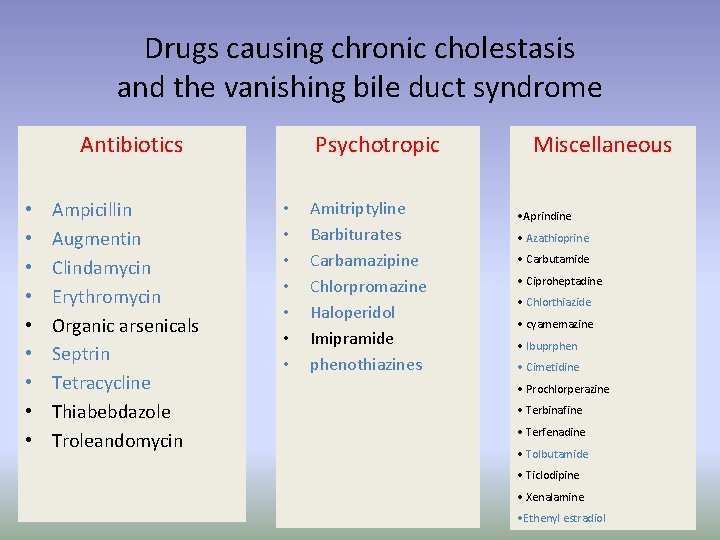
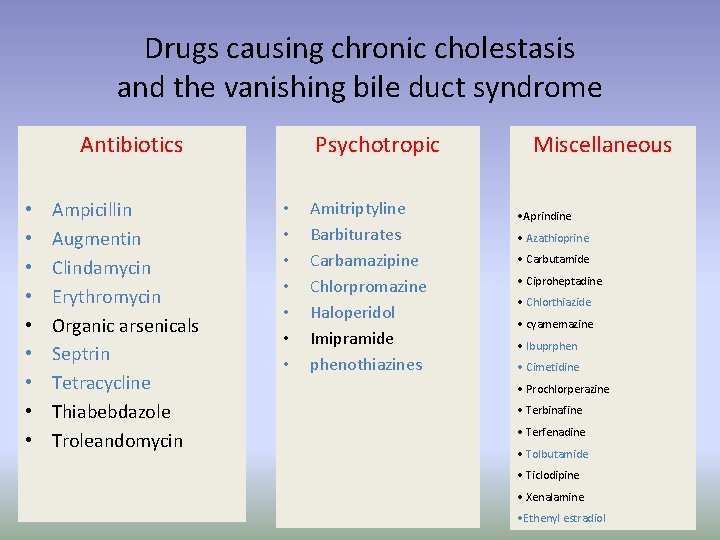
Drugs causing chronic cholestasis and the vanishing bile duct syndrome Antibiotics • • • Ampicillin Augmentin Clindamycin Erythromycin Organic arsenicals Septrin Tetracycline Thiabebdazole Troleandomycin Psychotropic • • Amitriptyline Barbiturates Carbamazipine Chlorpromazine Haloperidol Imipramide phenothiazines Miscellaneous • Aprindine • Azathioprine • Carbutamide • Ciproheptadine • Chlorthiazide • cyamemazine • Ibuprphen • Cimetidine • Prochlorperazine • Terbinafine • Terfenadine • Tolbutamide • Ticlodipine • Xenalamine • Ethenyl estradiol
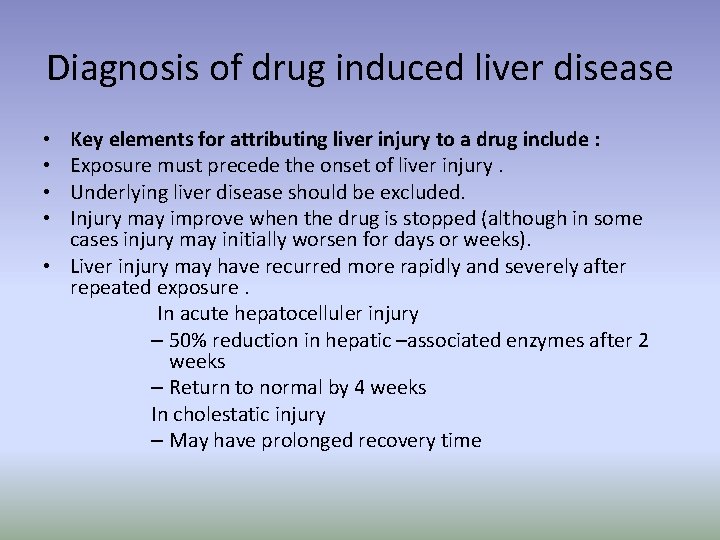
Diagnosis of drug induced liver disease Key elements for attributing liver injury to a drug include : Exposure must precede the onset of liver injury. Underlying liver disease should be excluded. Injury may improve when the drug is stopped (although in some cases injury may initially worsen for days or weeks). • Liver injury may have recurred more rapidly and severely after repeated exposure. In acute hepatocelluler injury – 50% reduction in hepatic –associated enzymes after 2 weeks – Return to normal by 4 weeks In cholestatic injury – May have prolonged recovery time • •
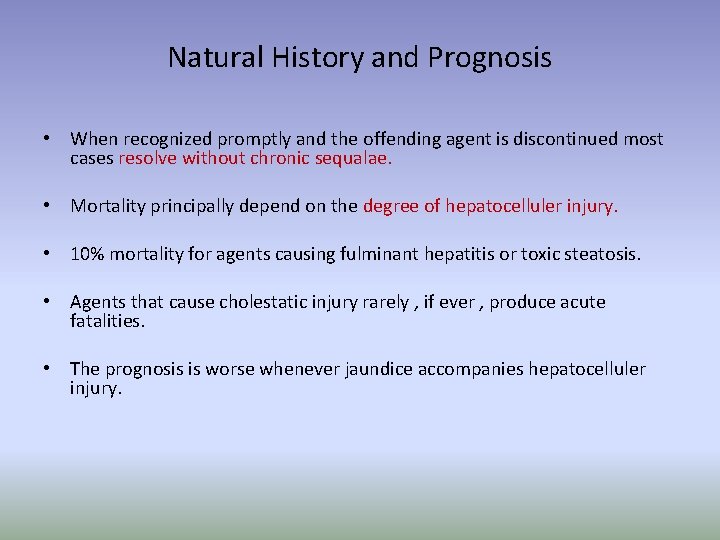
Natural History and Prognosis • When recognized promptly and the offending agent is discontinued most cases resolve without chronic sequalae. • Mortality principally depend on the degree of hepatocelluler injury. • 10% mortality for agents causing fulminant hepatitis or toxic steatosis. • Agents that cause cholestatic injury rarely , if ever , produce acute fatalities. • The prognosis is worse whenever jaundice accompanies hepatocelluler injury.
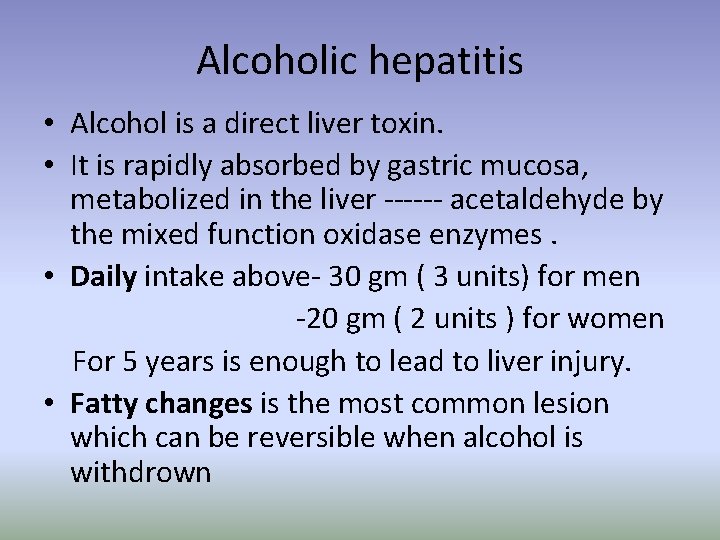
Alcoholic hepatitis • Alcohol is a direct liver toxin. • It is rapidly absorbed by gastric mucosa, metabolized in the liver ------ acetaldehyde by the mixed function oxidase enzymes. • Daily intake above- 30 gm ( 3 units) for men -20 gm ( 2 units ) for women For 5 years is enough to lead to liver injury. • Fatty changes is the most common lesion which can be reversible when alcohol is withdrown
• • clinical feature is: jaundice. plethora. Malaise. confusion. abdominal pain (from capsular distension). anorexia may be present. Signs of chronic liver disease are frequently present as up to 80% of patients with AH will have underlying cirrhosis.
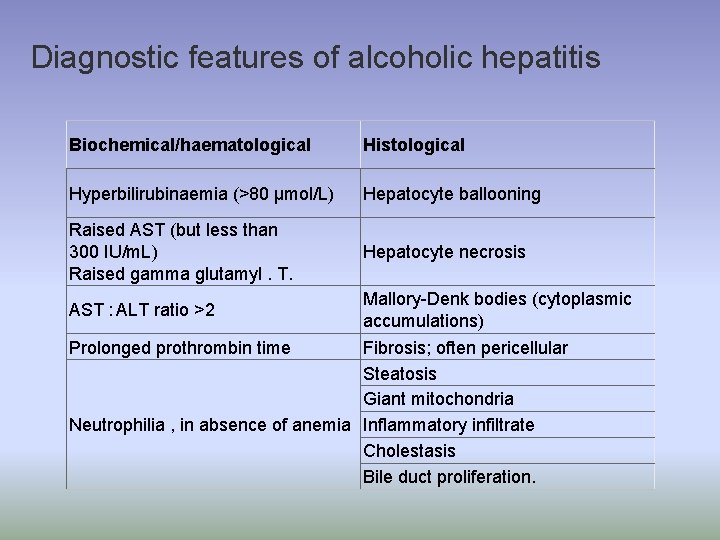
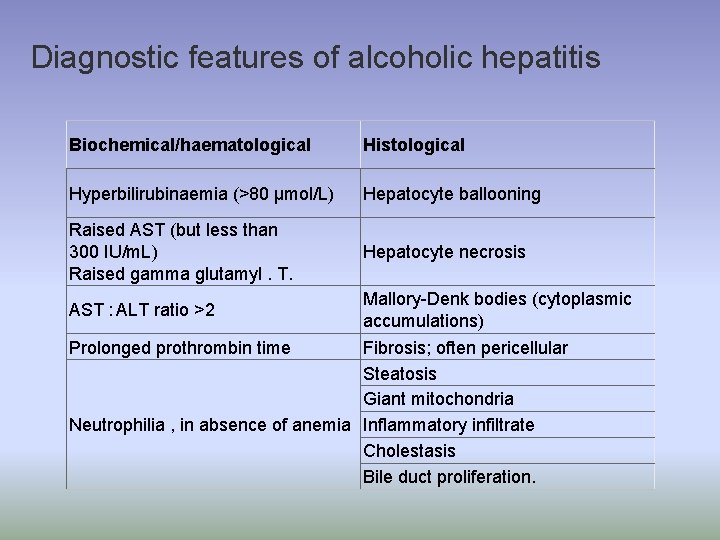
Diagnostic features of alcoholic hepatitis Biochemical/haematological Histological Hyperbilirubinaemia (>80 μmol/L) Hepatocyte ballooning Raised AST (but less than 300 IU/m. L) Raised gamma glutamyl. T. Hepatocyte necrosis Mallory-Denk bodies (cytoplasmic accumulations) Prolonged prothrombin time Fibrosis; often pericellular Steatosis Giant mitochondria Neutrophilia , in absence of anemia Inflammatory infiltrate Cholestasis Bile duct proliferation. AST : ALT ratio >2
Management of ALD • Manage alcohol with drawl. • Screen for other causes of liver diseases (autoimmune , viral , haemochromatosis). • Nutritional suplementations. • Follow up and treatment of chronic liver disease if persist.
metabolic causes of hepatitis • wilson disease : • Autosomal recessive disorder of copper metabolism. - failure of biliary copper excretion----- accumulation. - failure of synthesis of cereluplasmin. • Systemic accumulation of copper Liver, brain, kidneys, cornea, heart, pancreas, and joints • Patients can be asymptomatic or present with a variety of hepatic and extrahepatic manifestations. • Presentatation usually occures in child hood or adolescence. • Diagnosis based upon clinical exam, LFTs, ceruloplasmin, serum and urine copper studies, and liver biopsy
Wilson Disease Neuropsychiatric Manifestations • Movement disorders – Tremors – Involuntary movements • • • Drooling Dysarthria Dystonia Pseudobulbar palsy Seizures • • • Migraine headaches Insomnia Depression Personality changes Psychosis Typically presents later than liver disease
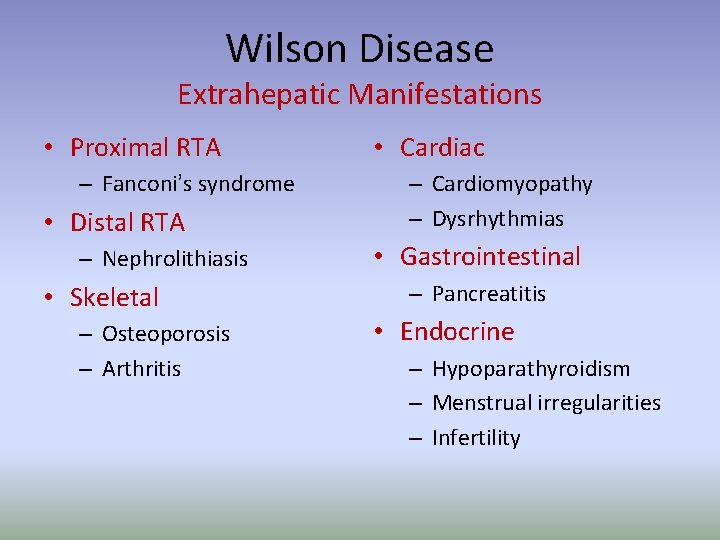
Wilson Disease Extrahepatic Manifestations • Proximal RTA – Fanconi’s syndrome • Distal RTA – Nephrolithiasis • Skeletal – Osteoporosis – Arthritis • Cardiac – Cardiomyopathy – Dysrhythmias • Gastrointestinal – Pancreatitis • Endocrine – Hypoparathyroidism – Menstrual irregularities – Infertility
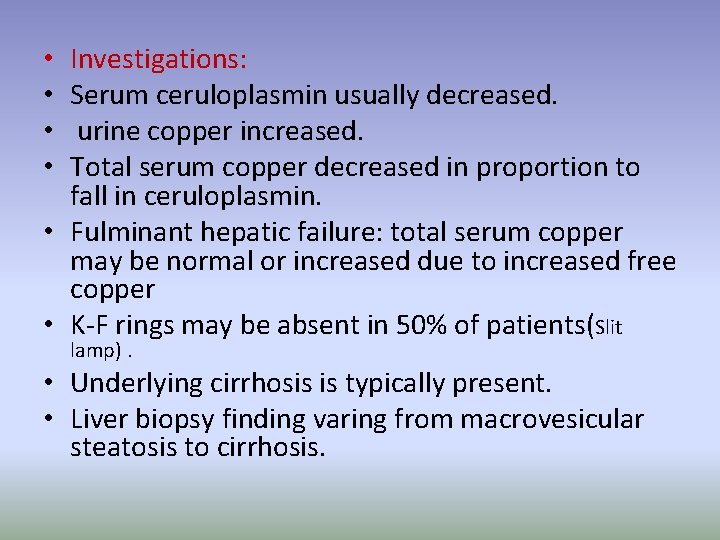
Investigations: Serum ceruloplasmin usually decreased. urine copper increased. Total serum copper decreased in proportion to fall in ceruloplasmin. • Fulminant hepatic failure: total serum copper may be normal or increased due to increased free copper • K-F rings may be absent in 50% of patients(Slit • • lamp). • Underlying cirrhosis is typically present. • Liver biopsy finding varing from macrovesicular steatosis to cirrhosis.
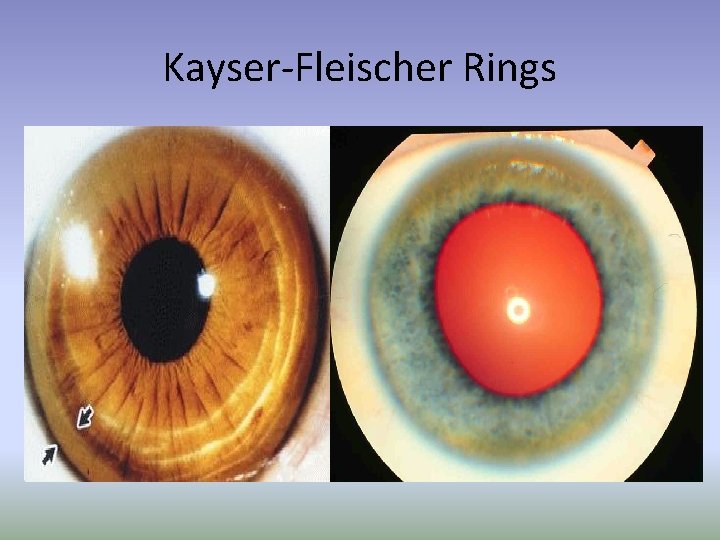
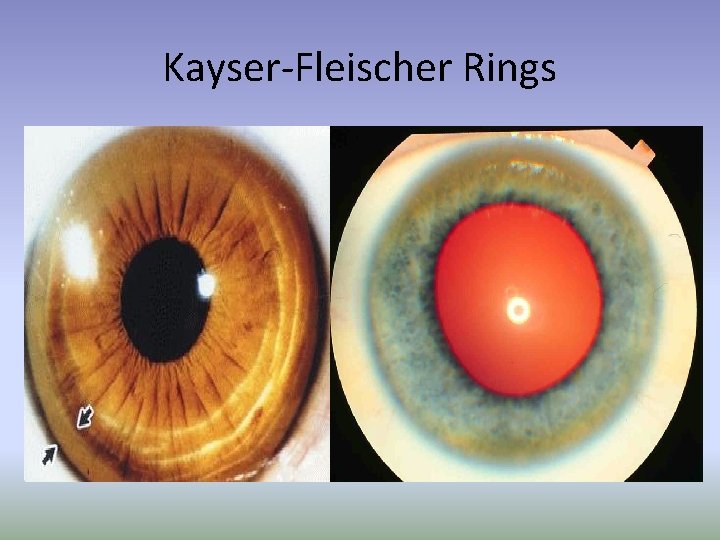
Kayser-Fleischer Rings

Wilson Disease Treatment Options • Medical – Chelators …. Penicillamine, trientine. – Metallothionein inducers …. . Zinc. Used as maintenance therapy after chelation with either penicillamine or trientine. Treatment must be lifelong regardless of choice of therapy • Surgical – Liver transplantation
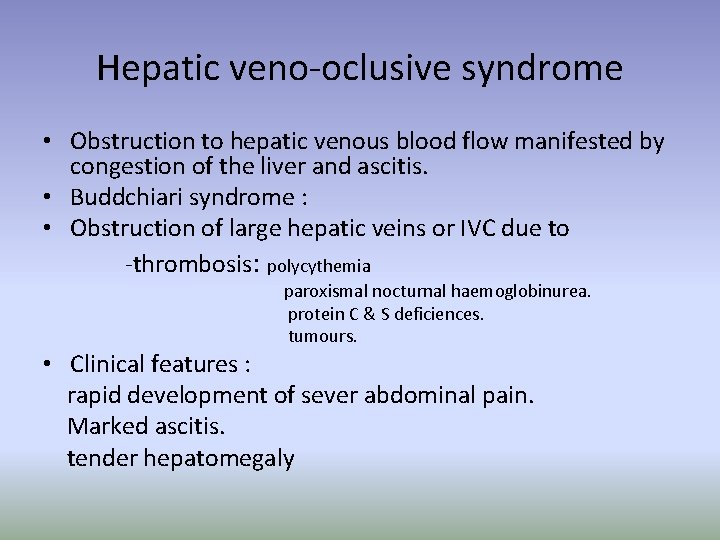
Hepatic veno-oclusive syndrome • Obstruction to hepatic venous blood flow manifested by congestion of the liver and ascitis. • Buddchiari syndrome : • Obstruction of large hepatic veins or IVC due to -thrombosis: polycythemia paroxismal nocturnal haemoglobinurea. protein C & S deficiences. tumours. • Clinical features : rapid development of sever abdominal pain. Marked ascitis. tender hepatomegaly
• LFT: high bilirubin and liver enzymes. • Ascitic fluid analysis – high protein concentration in early stages. • Doppler uss. Obliteration of hepatic veins or reversed flow in portal vein. • Liver biopsy. Centrilobular congestion with fibrosis Management: • Treat the predisposing cause • Anticoagulant. • Treat ascitis. • Prognosis is poor 1/3 ----2/3 of patients die within 1 to 5 years. • Survivors develop liver cirrhosis.
haemochromatosis • hemochromatosis is an Autosomal recessive disorder causing increased intestinal iron absorption. • iron deposited in tissues, especially the liver, heart, pancreas, and pituitary. • Genetic Variants of hereditary hemochromatosis : • Classical hereditary hemochromatosis Low penetrance, clinical onset in adults. • juvenile hemochromatosis • Rapid iron loading, full penetrance, and early onset of hypogonadism and cardiac complications. Liver disease less prominent
Clinical picture • The clinical manifestations of iron accumulation include • liver disease may leads to HCC. • Skin pigmentation. • Diabetes mellitus. • Arthropathy. ( pseudogout, chondrocalcinosis, and chronic arthropathy). • Impotence in males (Iron accumulation is mostly in the anterior pituitary ). • and cardiac enlargement with or without heart failure or conduction defects , due to excess deposition of iron within the myocardium.
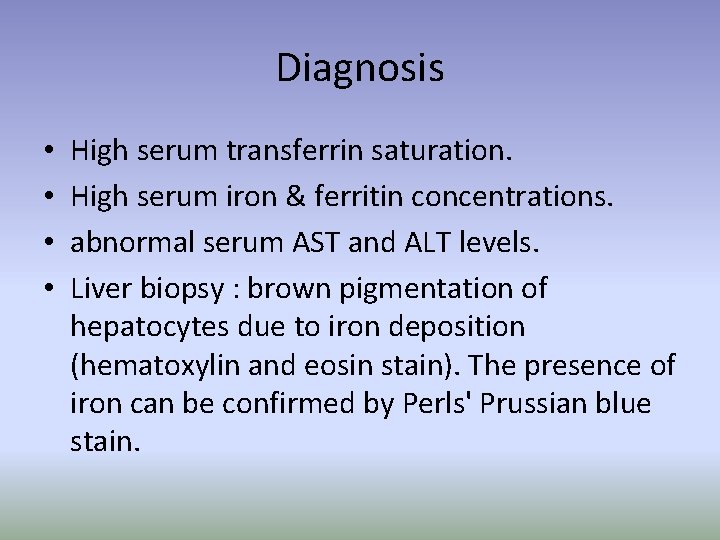
Diagnosis • • High serum transferrin saturation. High serum iron & ferritin concentrations. abnormal serum AST and ALT levels. Liver biopsy : brown pigmentation of hepatocytes due to iron deposition (hematoxylin and eosin stain). The presence of iron can be confirmed by Perls' Prussian blue stain.
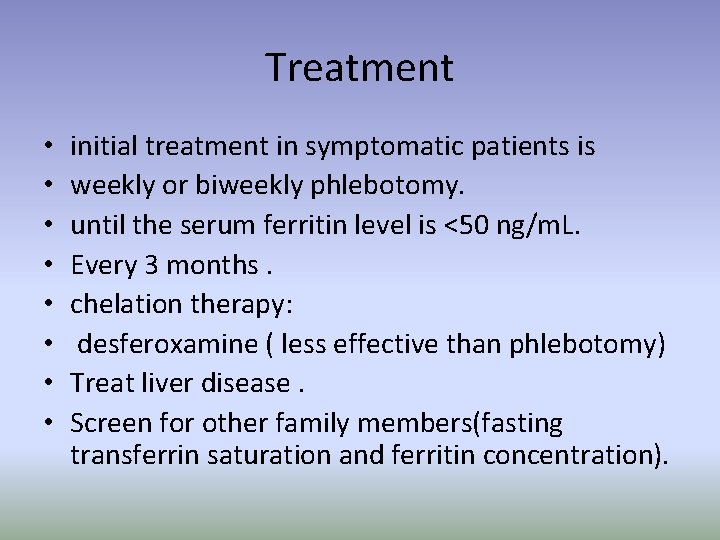
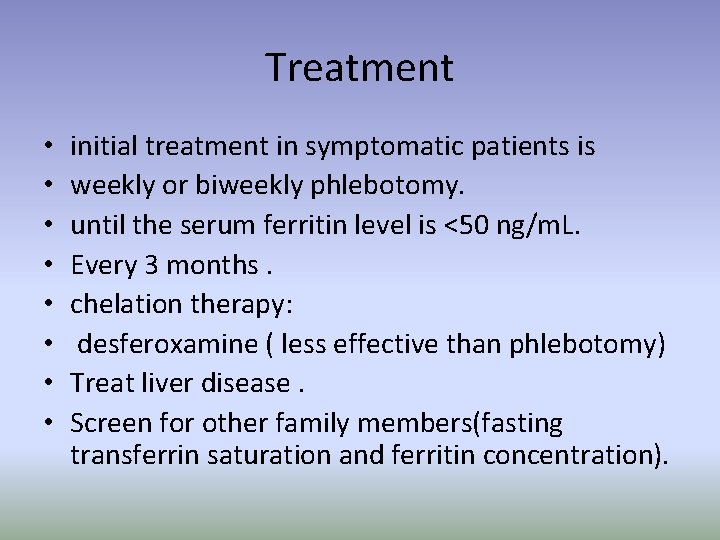
Treatment • • initial treatment in symptomatic patients is weekly or biweekly phlebotomy. until the serum ferritin level is <50 ng/m. L. Every 3 months. chelation therapy: desferoxamine ( less effective than phlebotomy) Treat liver disease. Screen for other family members(fasting transferrin saturation and ferritin concentration).
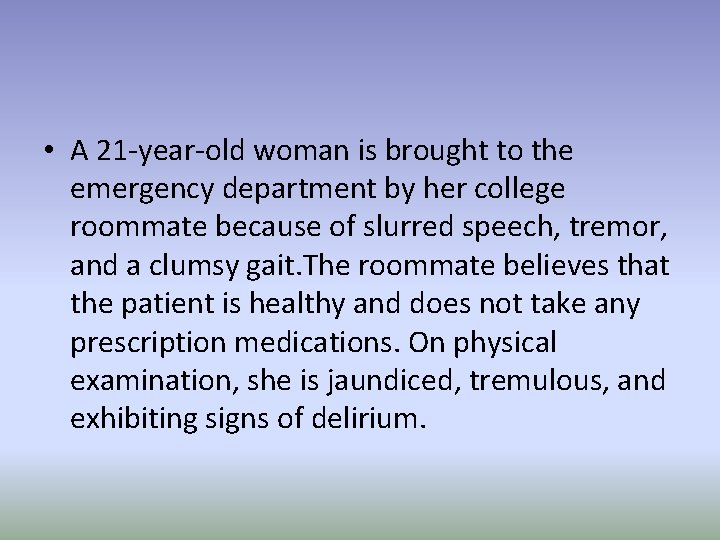
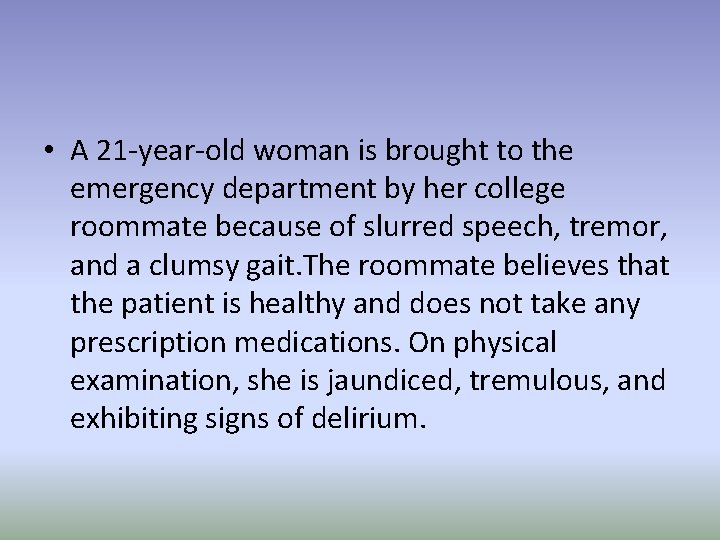
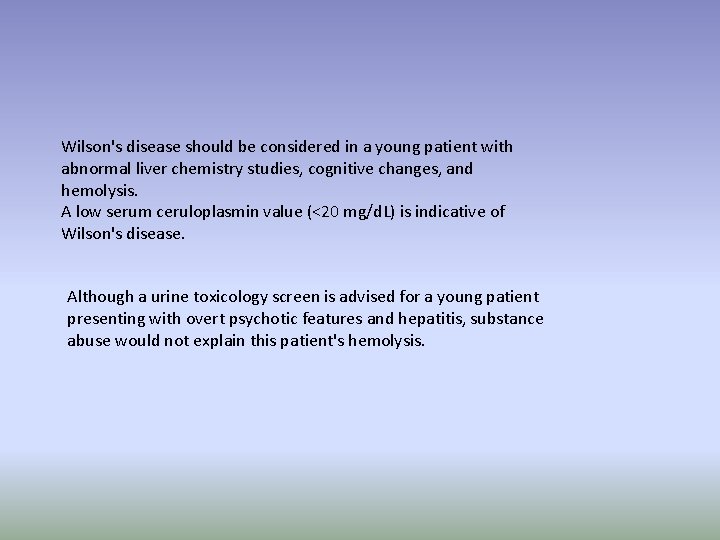
• A 21 -year-old woman is brought to the emergency department by her college roommate because of slurred speech, tremor, and a clumsy gait. The roommate believes that the patient is healthy and does not take any prescription medications. On physical examination, she is jaundiced, tremulous, and exhibiting signs of delirium.
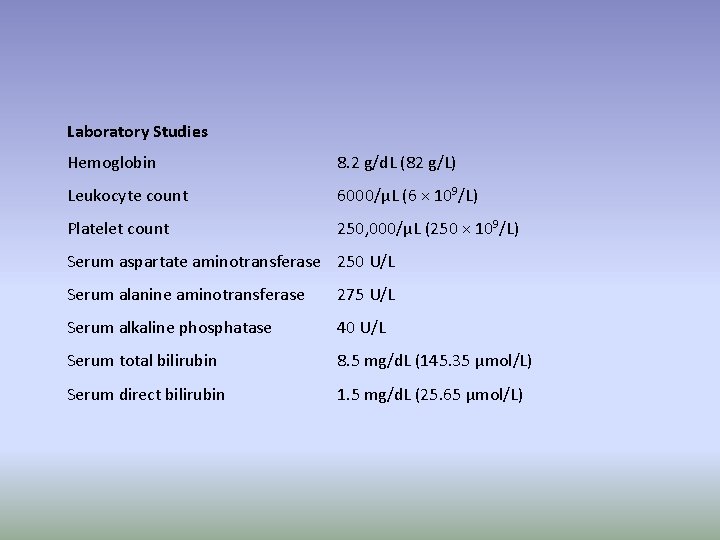
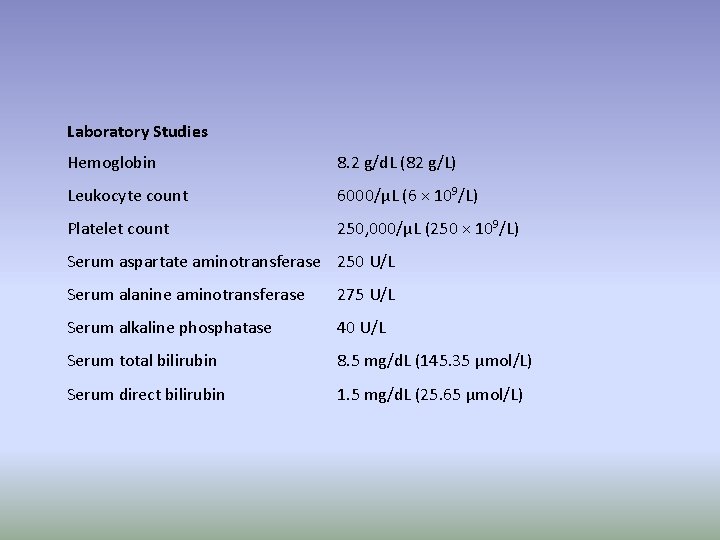
Laboratory Studies Hemoglobin 8. 2 g/d. L (82 g/L) Leukocyte count 6000/μL (6 × 109/L) Platelet count 250, 000/μL (250 × 109/L) Serum aspartate aminotransferase 250 U/L Serum alanine aminotransferase 275 U/L Serum alkaline phosphatase 40 U/L Serum total bilirubin 8. 5 mg/d. L (145. 35 μmol/L) Serum direct bilirubin 1. 5 mg/d. L (25. 65 μmol/L)
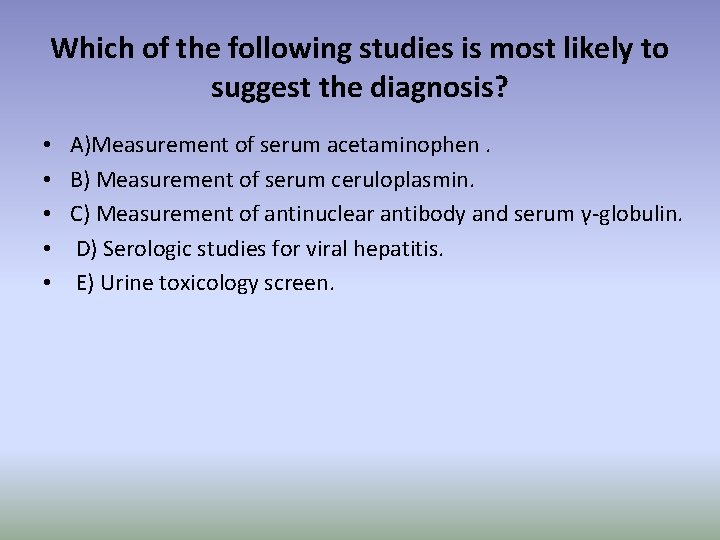
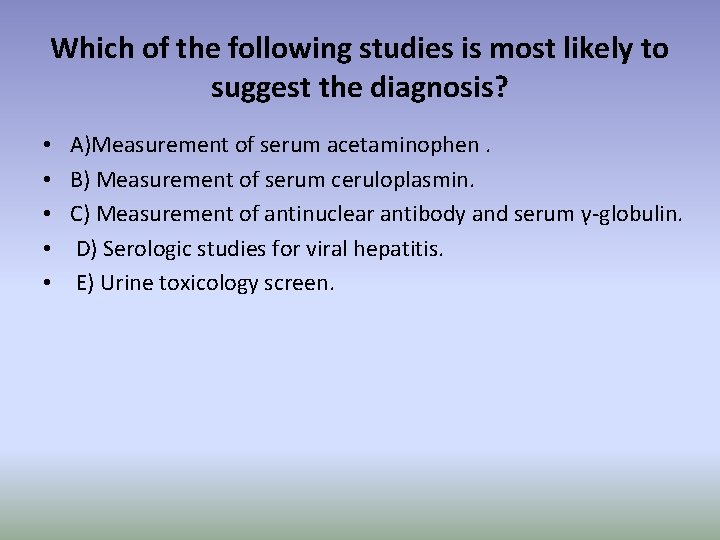
Which of the following studies is most likely to suggest the diagnosis? • • • A)Measurement of serum acetaminophen. B) Measurement of serum ceruloplasmin. C) Measurement of antinuclear antibody and serum γ-globulin. D) Serologic studies for viral hepatitis. E) Urine toxicology screen.
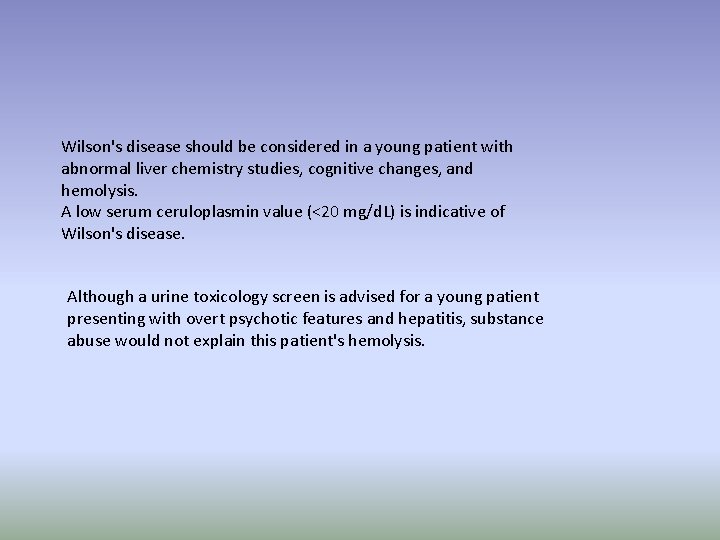
Wilson's disease should be considered in a young patient with abnormal liver chemistry studies, cognitive changes, and hemolysis. A low serum ceruloplasmin value (<20 mg/d. L) is indicative of Wilson's disease. Although a urine toxicology screen is advised for a young patient presenting with overt psychotic features and hepatitis, substance abuse would not explain this patient's hemolysis.
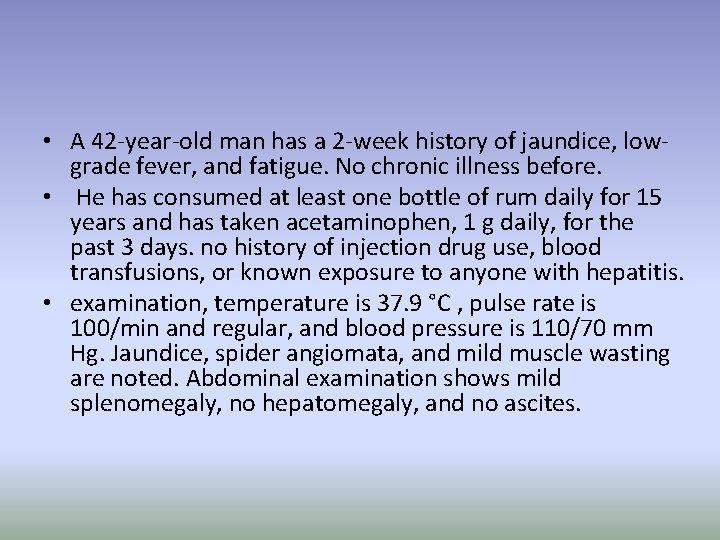
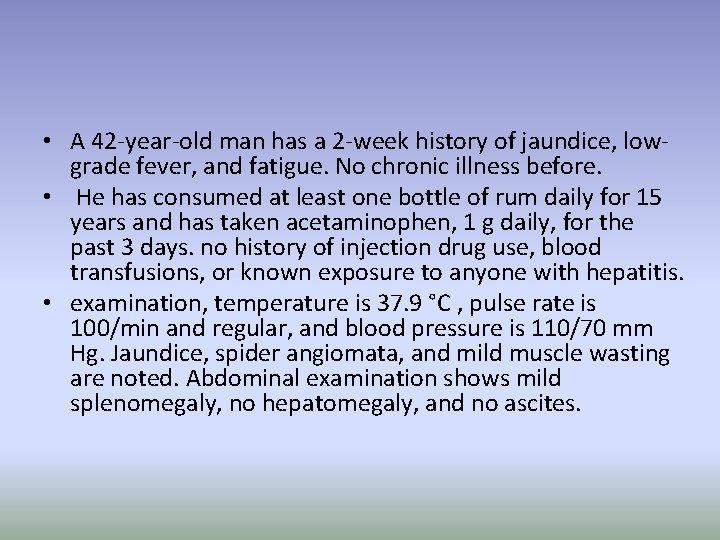
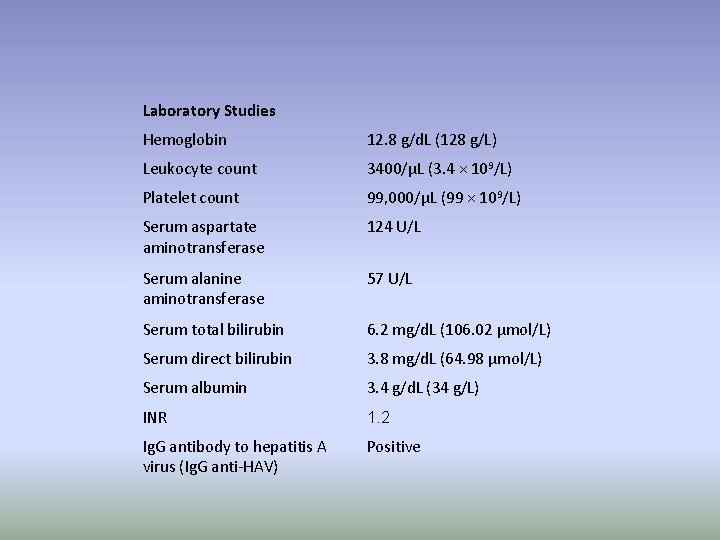
• A 42 -year-old man has a 2 -week history of jaundice, lowgrade fever, and fatigue. No chronic illness before. • He has consumed at least one bottle of rum daily for 15 years and has taken acetaminophen, 1 g daily, for the past 3 days. no history of injection drug use, blood transfusions, or known exposure to anyone with hepatitis. • examination, temperature is 37. 9 °C , pulse rate is 100/min and regular, and blood pressure is 110/70 mm Hg. Jaundice, spider angiomata, and mild muscle wasting are noted. Abdominal examination shows mild splenomegaly, no hepatomegaly, and no ascites.
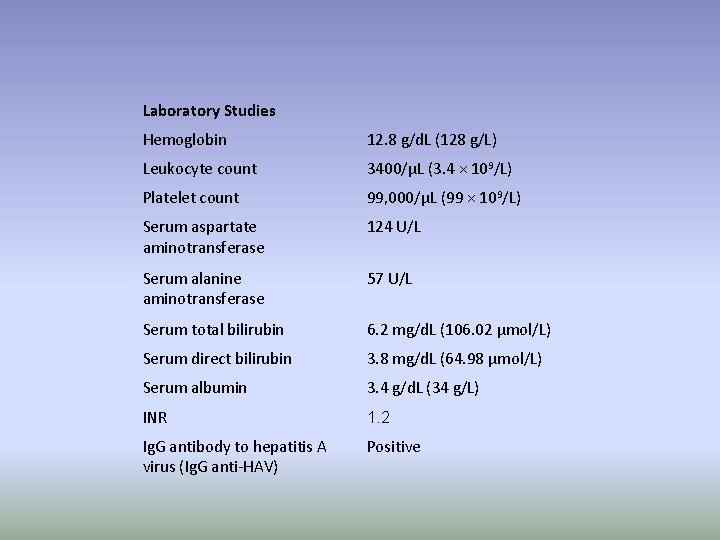
Laboratory Studies Hemoglobin 12. 8 g/d. L (128 g/L) Leukocyte count 3400/μL (3. 4 × 109/L) Platelet count 99, 000/μL (99 × 109/L) Serum aspartate aminotransferase 124 U/L Serum alanine aminotransferase 57 U/L Serum total bilirubin 6. 2 mg/d. L (106. 02 μmol/L) Serum direct bilirubin 3. 8 mg/d. L (64. 98 μmol/L) Serum albumin 3. 4 g/d. L (34 g/L) INR 1. 2 Ig. G antibody to hepatitis A virus (Ig. G anti-HAV) Positive
Which of the following is the most likely diagnosis? • • • A) Hepatitis A. B ) Sepsis. C ) Acetaminophen hepatotoxicity. D ) Alcoholic hepatitis. E ) Autoimmune hepatitis.
• Hepatitis A is associated with both AST and ALT values >500 U/L, with the ALT greater than AST. In addition • a positive Ig. G antibody to hepatitis A virus (Ig. G anti-HAV) is consistent with a remote prior infection. Patients with alcoholism have an increased risk of infection, but sepsis is unlikely because of the absence of leukocytosis. • acetaminophen doses of >3 g/d are probably needed to cause hepatotoxicity, even for patients with alcoholism. • In addition, acetaminophen toxicity typically results in AST and ALT values >5000 U/L. A patient with autoimmune hepatitis would generally have AST and ALT values similar to those of a patient with acute viral hepatitis.
Thank you
 Hepatitis viral
Hepatitis viral Gastroenterology near galt
Gastroenterology near galt Dr vallina gastroenterology
Dr vallina gastroenterology Icd 10 codes gastroenterology
Icd 10 codes gastroenterology Alix lanoue
Alix lanoue Gastroenterology medical terminology
Gastroenterology medical terminology Gastroenterology board review
Gastroenterology board review Bilitec 2000
Bilitec 2000 Les promesses de dieu ne failliront jamais
Les promesses de dieu ne failliront jamais Viral induced wheeze vs asthma
Viral induced wheeze vs asthma Replicação viral ciclo lítico e lisogênico
Replicação viral ciclo lítico e lisogênico Section 24-1 viral structure and replication
Section 24-1 viral structure and replication Inklüzyon cisimcikleri
Inklüzyon cisimcikleri Viral inoculation in embryonated egg
Viral inoculation in embryonated egg Viral inoculation in embryonated egg
Viral inoculation in embryonated egg Viral inoculation in embryonated egg
Viral inoculation in embryonated egg Spasmodic croup vs viral croup
Spasmodic croup vs viral croup Varicela variola
Varicela variola Exocitose
Exocitose Sample rejection criteria
Sample rejection criteria Tratamiento meningitis viral
Tratamiento meningitis viral Causes of viral hemorrhagic fever
Causes of viral hemorrhagic fever Ciclo viral
Ciclo viral Viral infection
Viral infection Viral
Viral Viral recombination
Viral recombination Vaccins à vecteur viral
Vaccins à vecteur viral Viral receptors
Viral receptors Procalcitonin
Procalcitonin Trivalent vaccin herpes
Trivalent vaccin herpes Virus dna
Virus dna Viral gastroenteritis
Viral gastroenteritis Viral entry
Viral entry The dynamics of viral marketing
The dynamics of viral marketing Csf findings in different meningitis
Csf findings in different meningitis