New Virtual Histology Findings M Pauliina Margolis MD


- Slides: 26
New Virtual Histology Findings M Pauliina Margolis, MD, Ph. D CMO and VP of Scientific Affairs CRT 2010, Washington DC
DISCLOSURES Paulina Margolis, MD, Ph. D Ownership Interest (Stocks, Stock Options or Other Ownership Interest) – Volcano Corporation Salary – Volcano Corporation
The Vision In vivo knowledge of plaque composition was envisioned to – improve our understanding of atherosclerosis and plaque progression – identify a high risk lesion for plaque rupture, the most common cause of sudden coronary death and myocardial infraction, – recognize lesions with risk for procedural complications before intervention, – identify plaque features which predict the risk of restenosis and stent thrombosis, and – assess the efficacy of systemic therapy in a meaningful, clinically relevant manner
www. vhivus. com Over 150 publications VH IVUS Publications ®
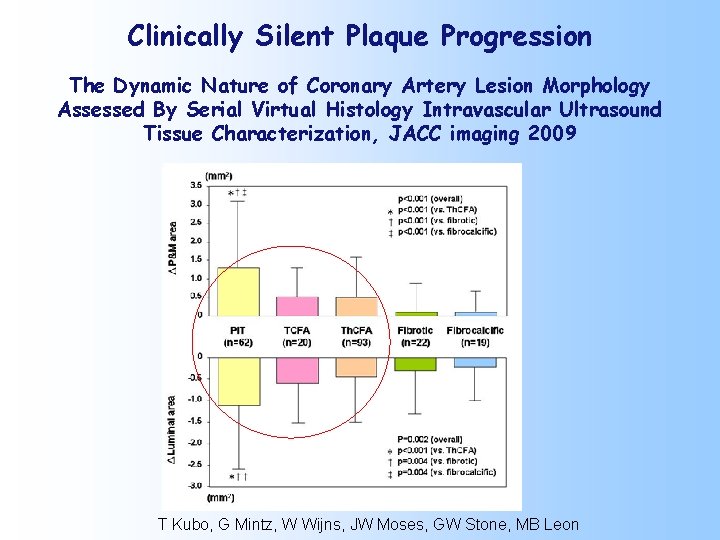
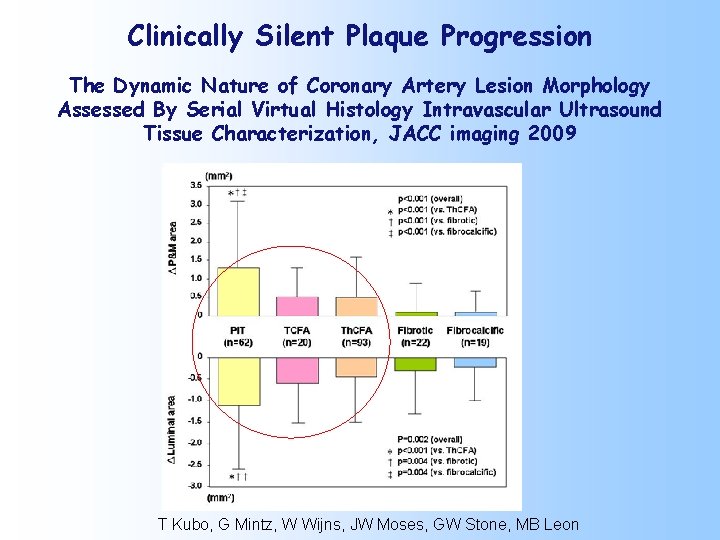
Clinically Silent Plaque Progression The Dynamic Nature of Coronary Artery Lesion Morphology Assessed By Serial Virtual Histology Intravascular Ultrasound Tissue Characterization, JACC imaging 2009 T Kubo, G Mintz, W Wijns, JW Moses, GW Stone, MB Leon

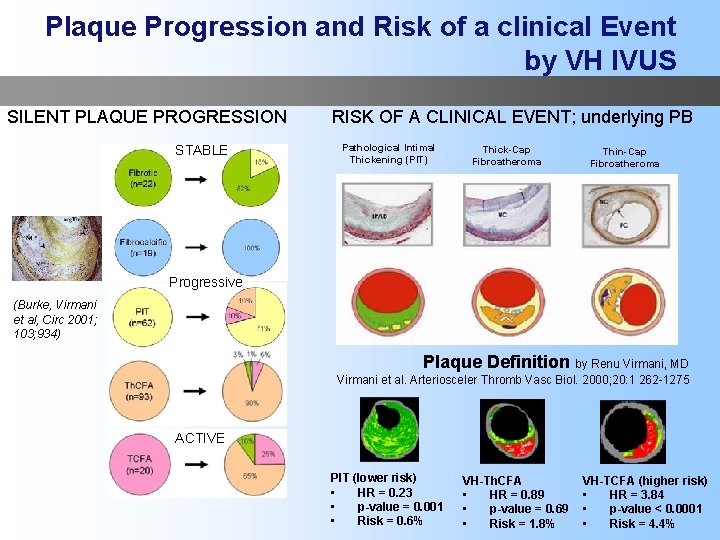
Stable Progressive ACTIVE
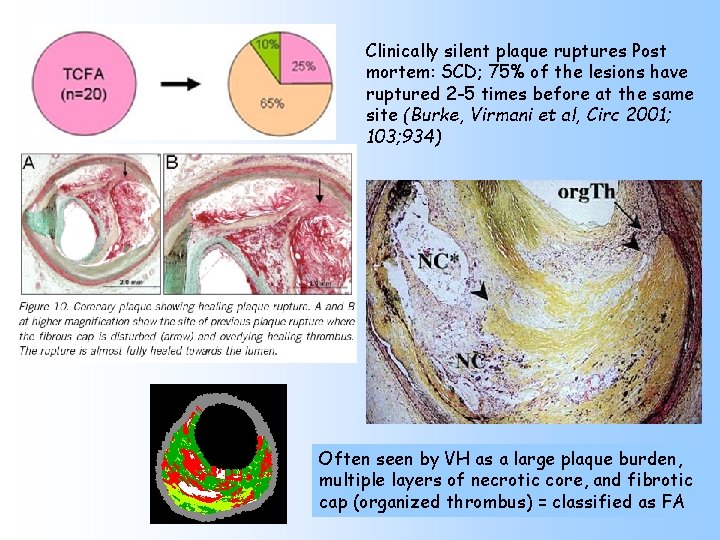
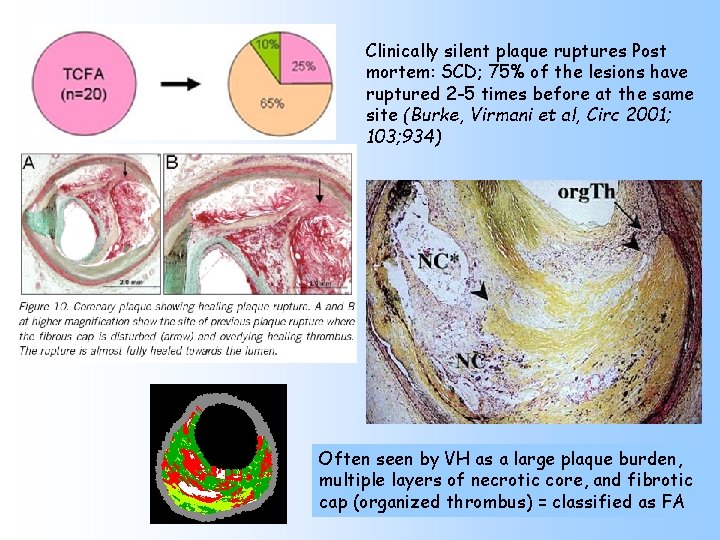
Clinically silent plaque ruptures Post mortem: SCD; 75% of the lesions have ruptured 2 -5 times before at the same site (Burke, Virmani et al, Circ 2001; 103; 934) Often seen by VH as a large plaque burden, multiple layers of necrotic core, and fibrotic cap (organized thrombus) = classified as FA
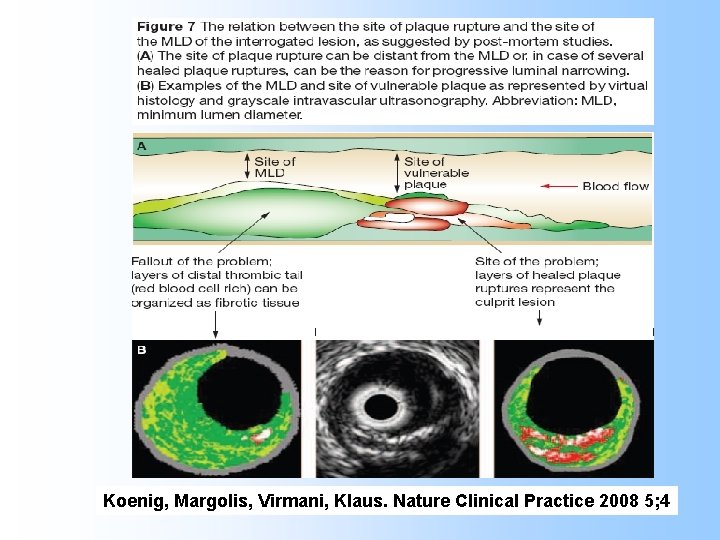
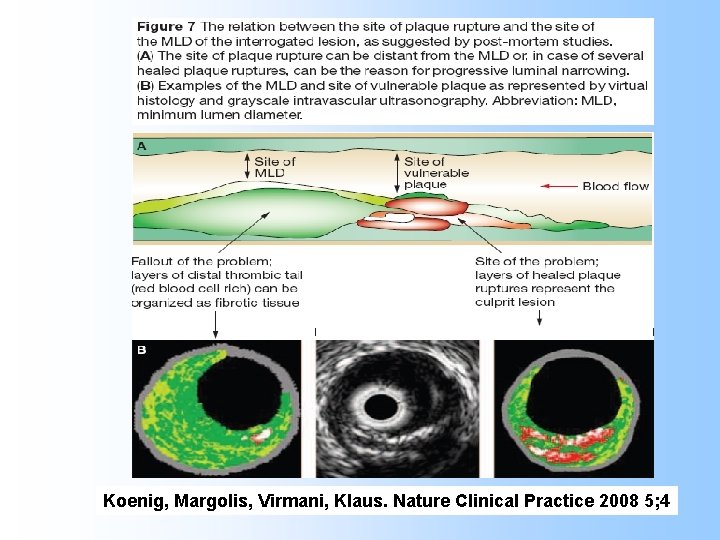
Koenig, Margolis, Virmani, Klaus. Nature Clinical Practice 2008 5; 4
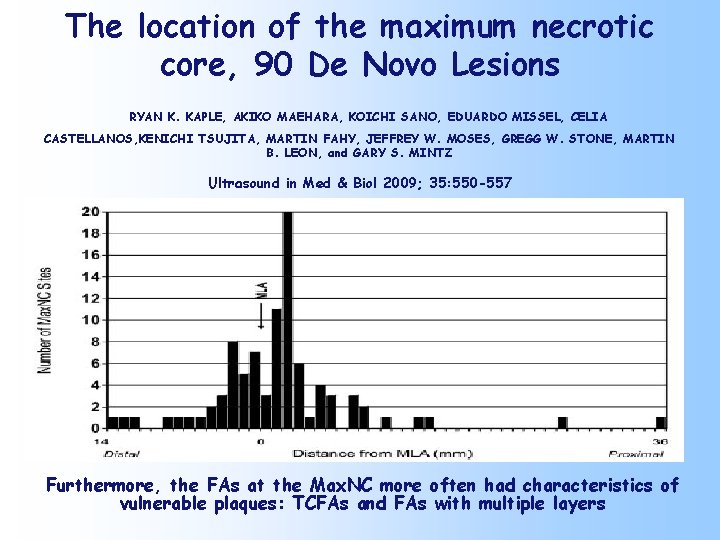
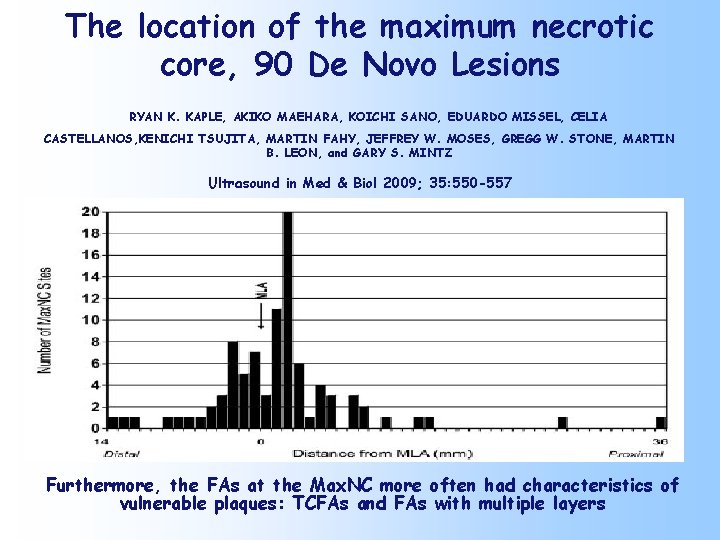
The location of the maximum necrotic core, 90 De Novo Lesions RYAN K. KAPLE, AKIKO MAEHARA, KOICHI SANO, EDUARDO MISSEL, CELIA CASTELLANOS, KENICHI TSUJITA, MARTIN FAHY, JEFFREY W. MOSES, GREGG W. STONE, MARTIN B. LEON, and GARY S. MINTZ Ultrasound in Med & Biol 2009; 35: 550 -557 Furthermore, the FAs at the Max. NC more often had characteristics of vulnerable plaques: TCFAs and FAs with multiple layers
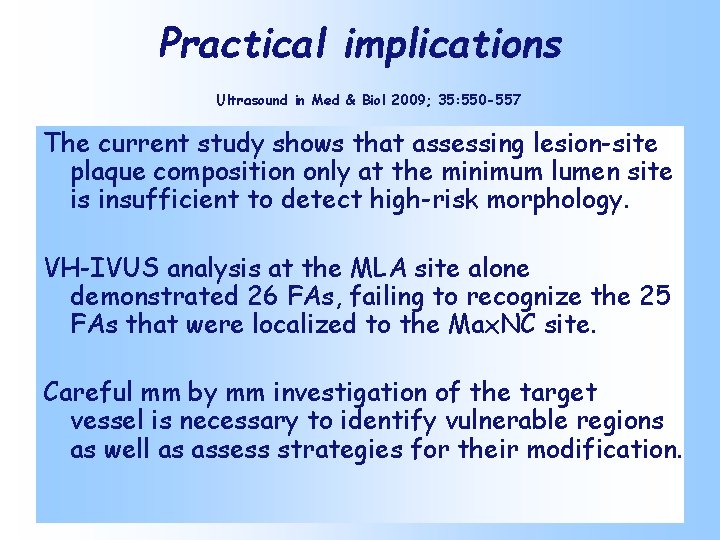
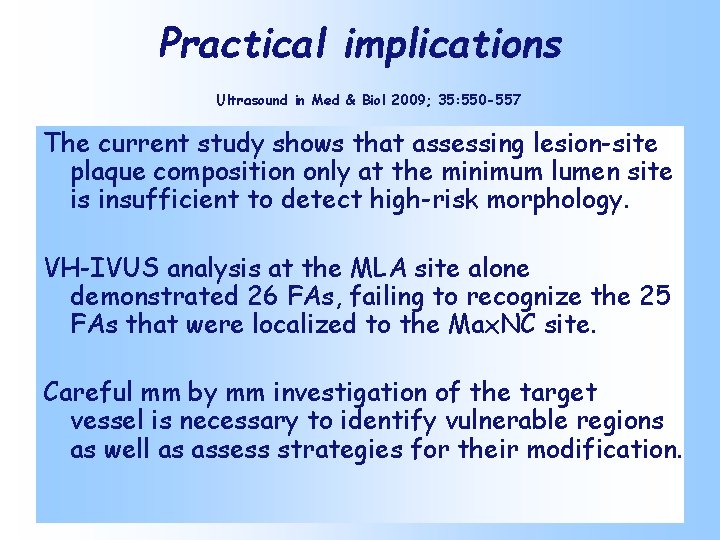
Practical implications Ultrasound in Med & Biol 2009; 35: 550 -557 The current study shows that assessing lesion-site plaque composition only at the minimum lumen site is insufficient to detect high-risk morphology. VH-IVUS analysis at the MLA site alone demonstrated 26 FAs, failing to recognize the 25 FAs that were localized to the Max. NC site. Careful mm by mm investigation of the target vessel is necessary to identify vulnerable regions as well as assess strategies for their modification.
How often do we fail to see and miss treating the ruptured TCFA because thrombus obscures our scenery? • D. Dudek, et al. – n=40 • n=20 STEMI • n=20 NSTEMI – – Aspiration if feasible VH IVUS Stenting by angio guidance only VH IVUS
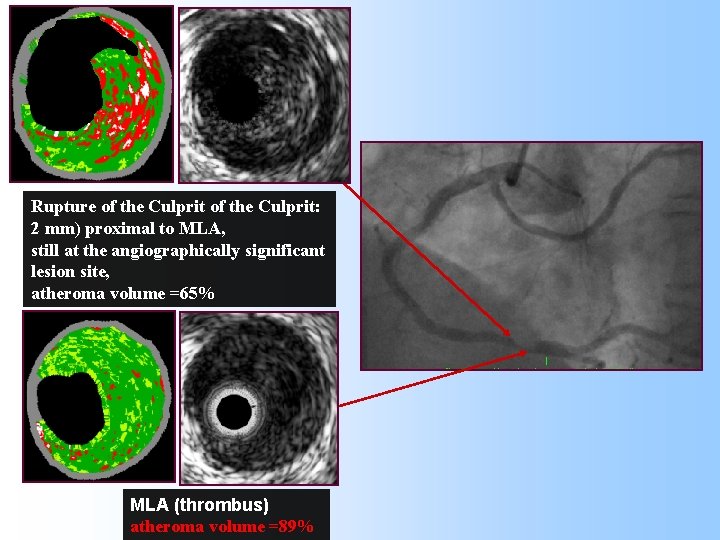
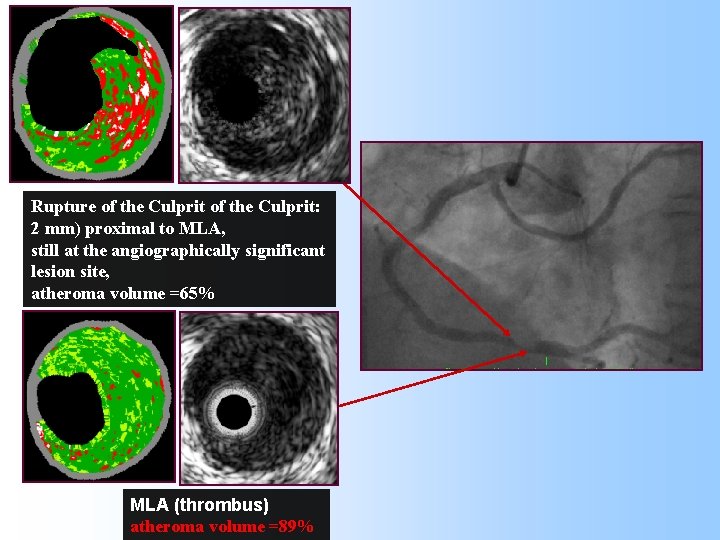
VH IVUS Rupture of the Culprit: 2 mm) proximal to MLA, still at the angiographically significant lesion site, atheroma volume =65% MLA (thrombus) atheroma volume =89%
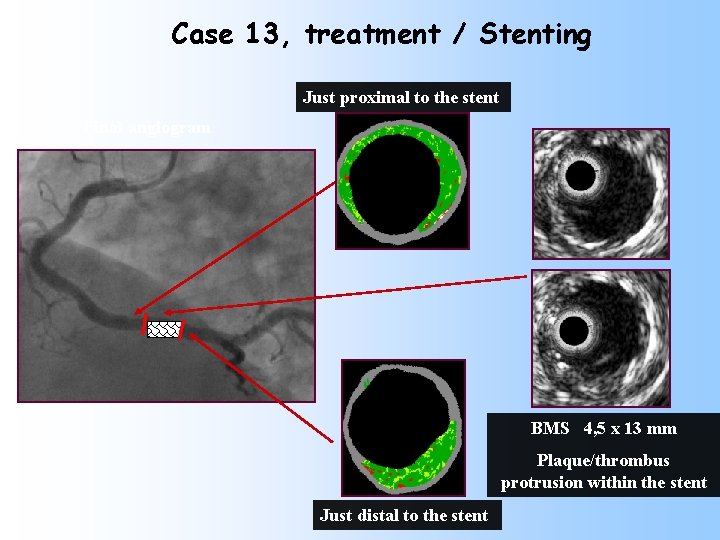
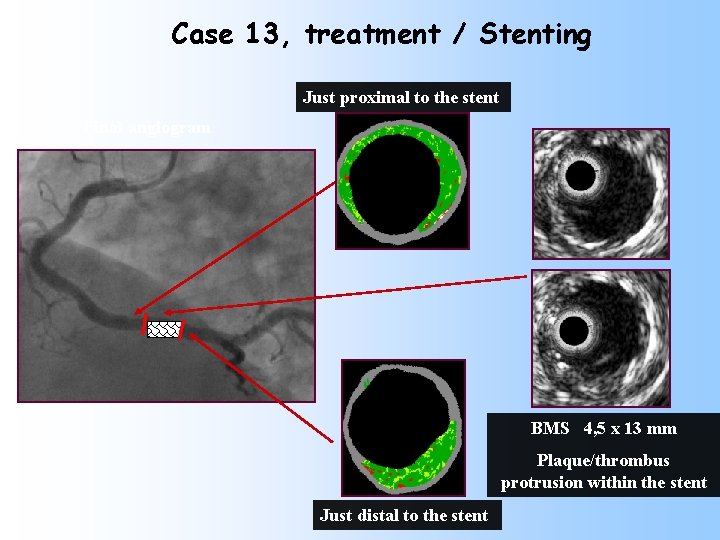
Case 13, treatment / Stenting Just proximal to the stent Final angiogram BMS 4, 5 x 13 mm Plaque/thrombus protrusion within the stent Just distal to the stent
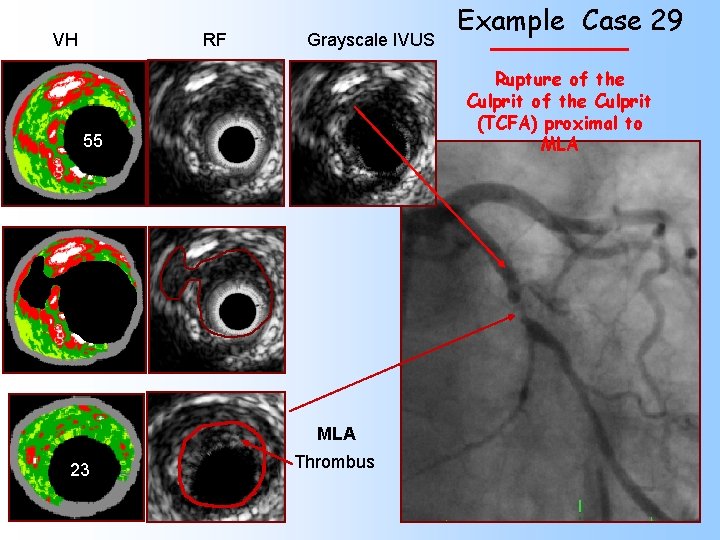
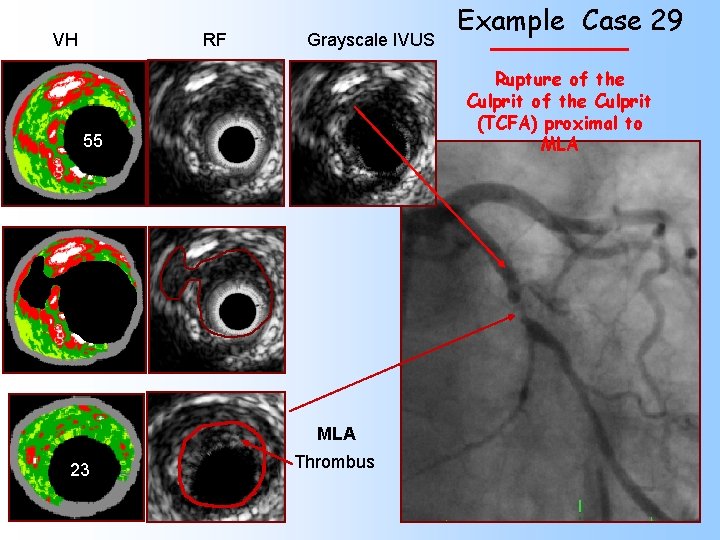
VH RF Grayscale IVUS Rupture of the Culprit (TCFA) proximal to MLA 55 MLA 23 Example Case 29 Thrombus
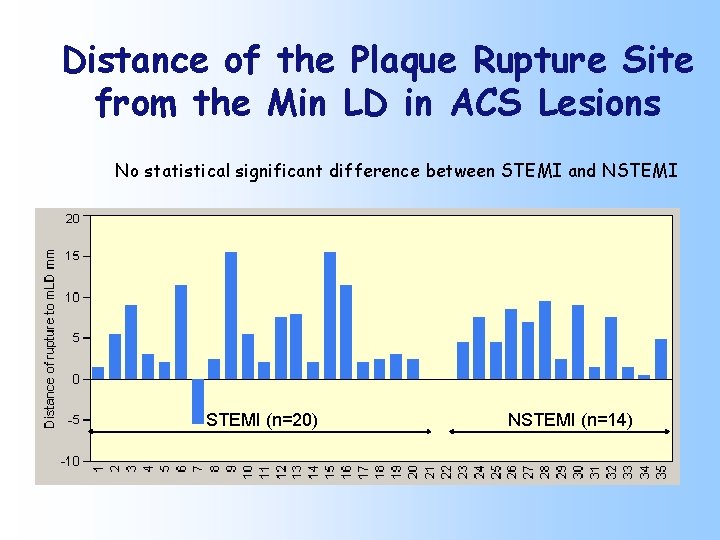
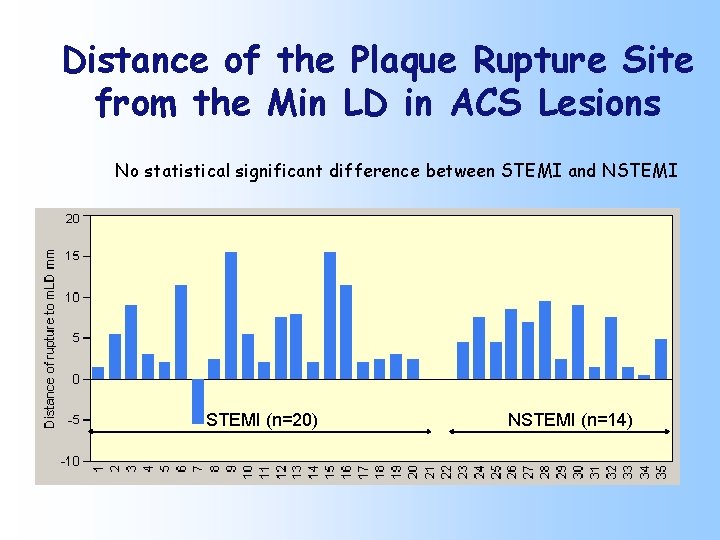
Distance of the Plaque Rupture Site from the Min LD in ACS Lesions No statistical significant difference between STEMI and NSTEMI (n=20) NSTEMI (n=14)
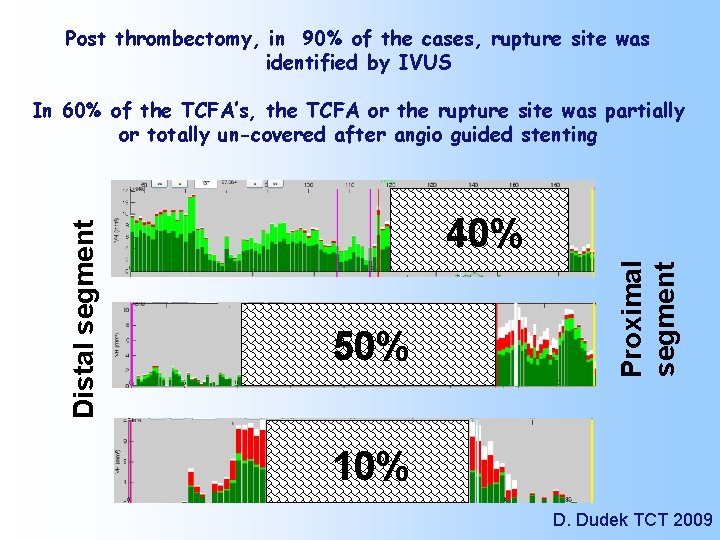
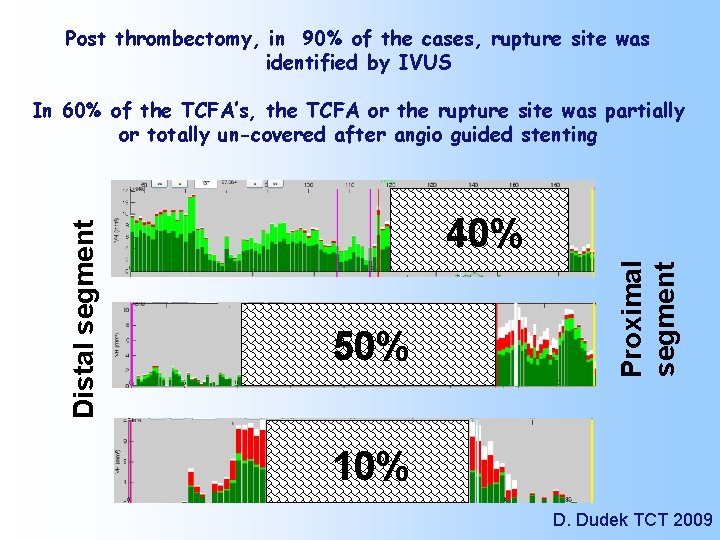
Post thrombectomy, in 90% of the cases, rupture site was identified by IVUS 40% 50% Proximal segment Distal segment In 60% of the TCFA’s, the TCFA or the rupture site was partially or totally un-covered after angio guided stenting 10% D. Dudek TCT 2009
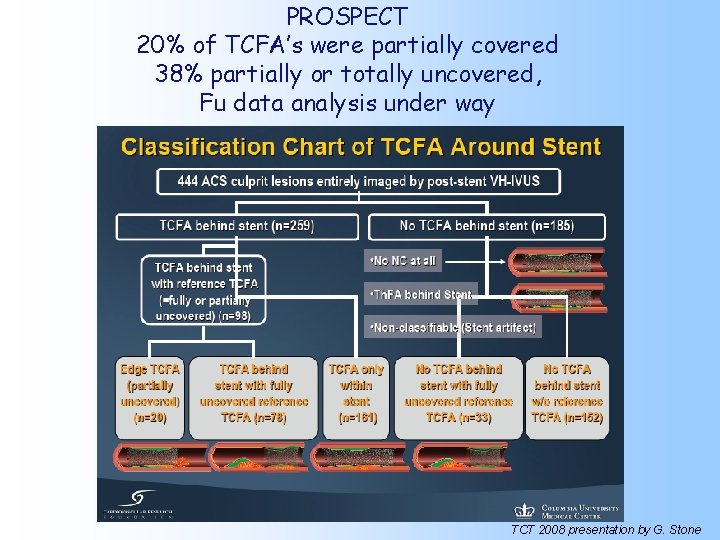
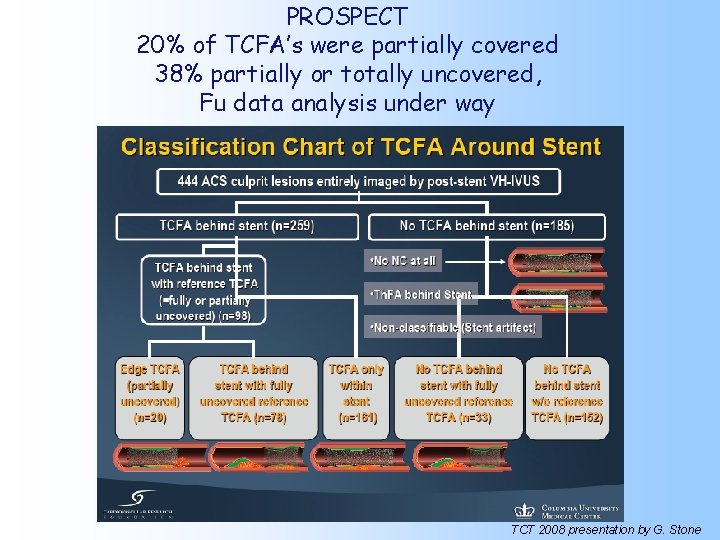
PROSPECT 20% of TCFA’s were partially covered 38% partially or totally uncovered, Fu data analysis under way TCT 2008 presentation by G. Stone
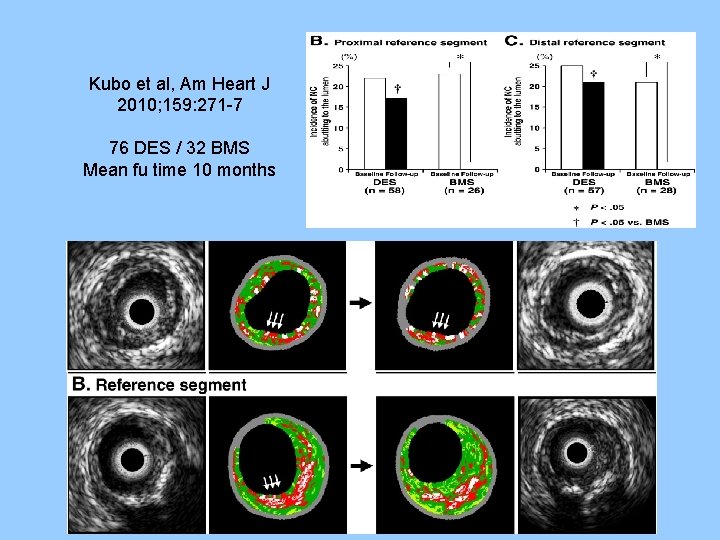
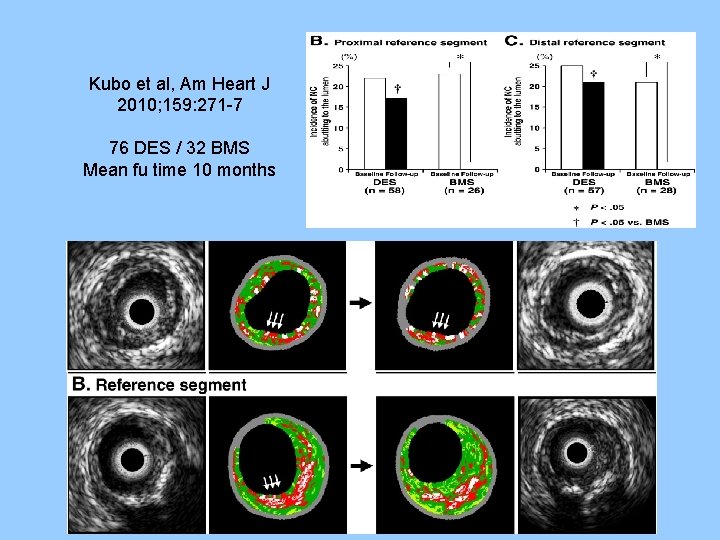
Kubo et al, Am Heart J 2010; 159: 271 -7 76 DES / 32 BMS Mean fu time 10 months
PROSPECT
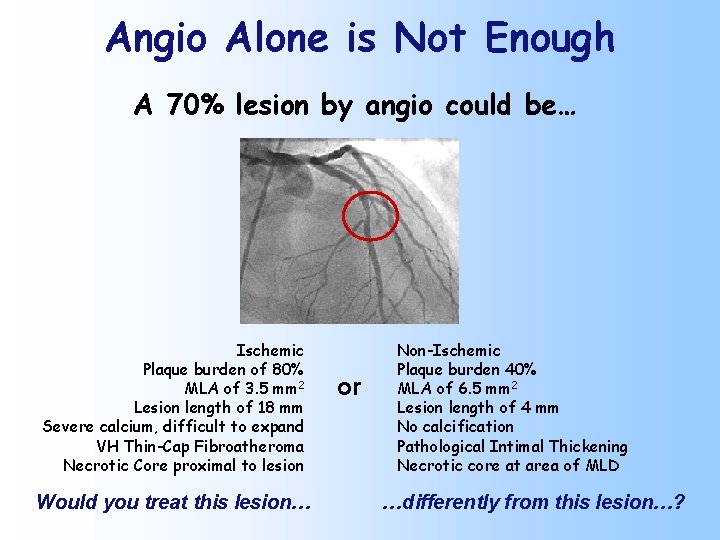
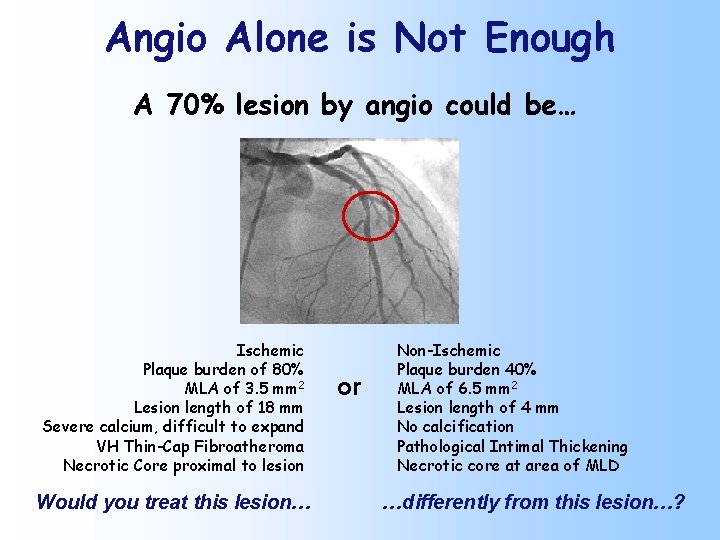
Angio Alone is Not Enough A 70% lesion by angio could be… Ischemic Plaque burden of 80% MLA of 3. 5 mm 2 Lesion length of 18 mm Severe calcium, difficult to expand VH Thin-Cap Fibroatheroma Necrotic Core proximal to lesion Would you treat this lesion… or Non-Ischemic Plaque burden 40% MLA of 6. 5 mm 2 Lesion length of 4 mm No calcification Pathological Intimal Thickening Necrotic core at area of MLD …differently from this lesion…?
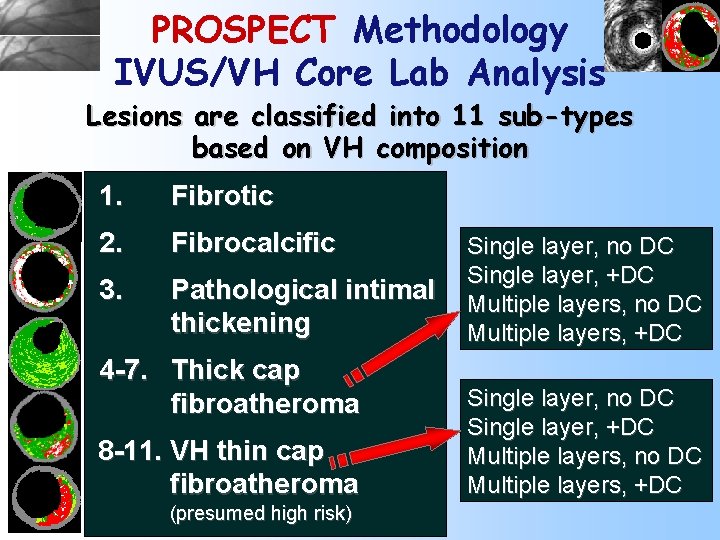
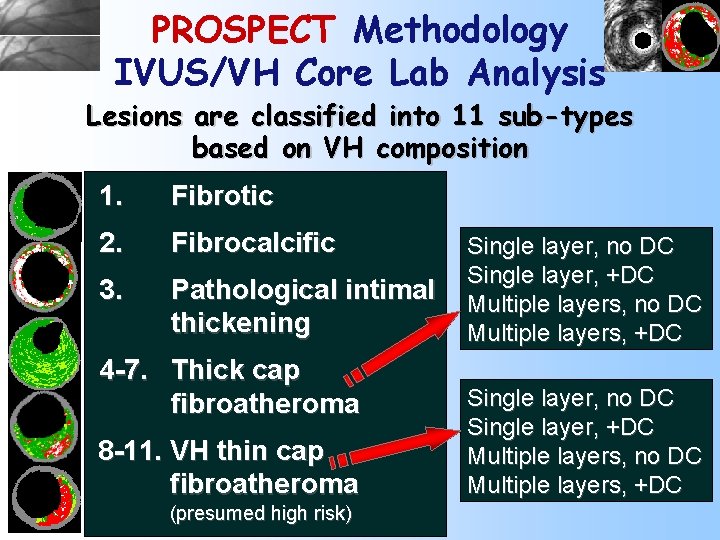
PROSPECT Methodology IVUS/VH Core Lab Analysis Lesions are classified into 11 sub-types based on VH composition 1. Fibrotic 2. Fibrocalcific 3. Pathological intimal thickening 4 -7. Thick cap fibroatheroma 8 -11. VH thin cap fibroatheroma (presumed high risk) Single layer, no DC Single layer, +DC Multiple layers, no DC Multiple layers, +DC
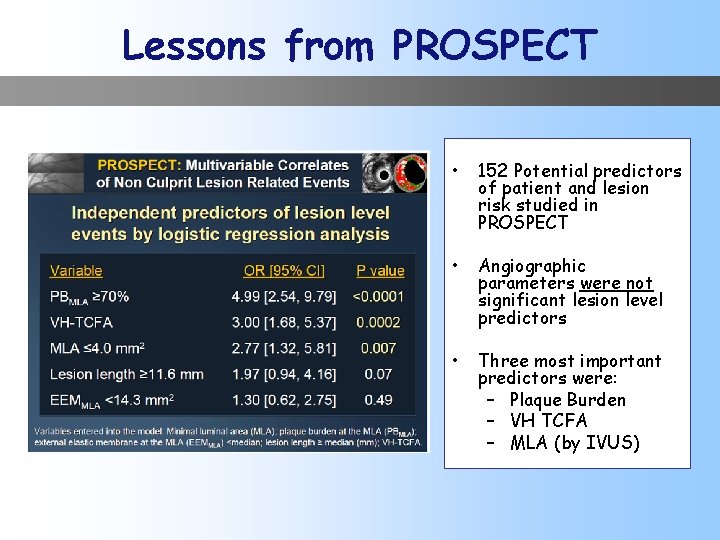
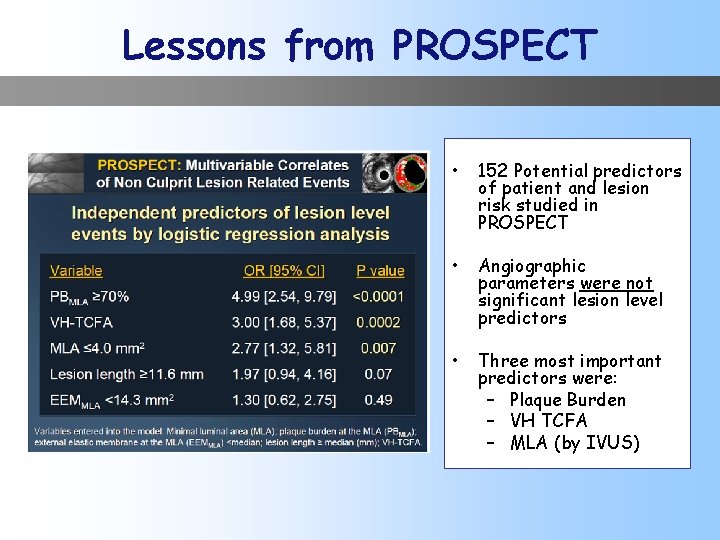
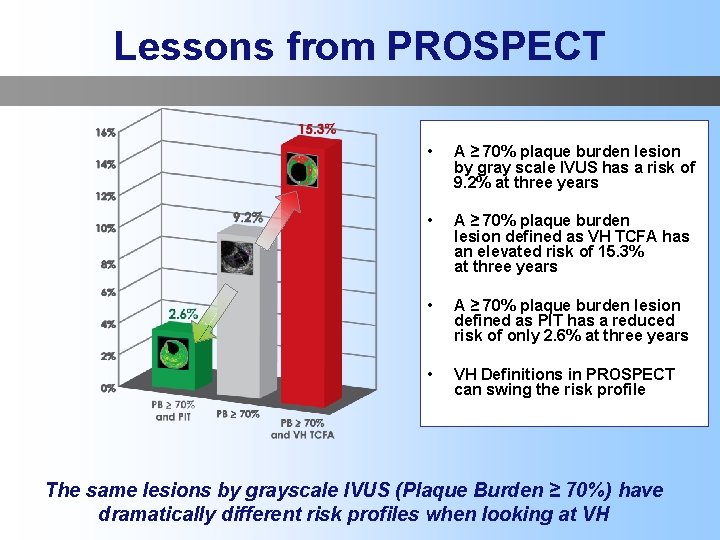
Lessons from PROSPECT • 152 Potential predictors of patient and lesion risk studied in PROSPECT • Angiographic parameters were not significant lesion level predictors • Three most important predictors were: – Plaque Burden – VH TCFA – MLA (by IVUS)
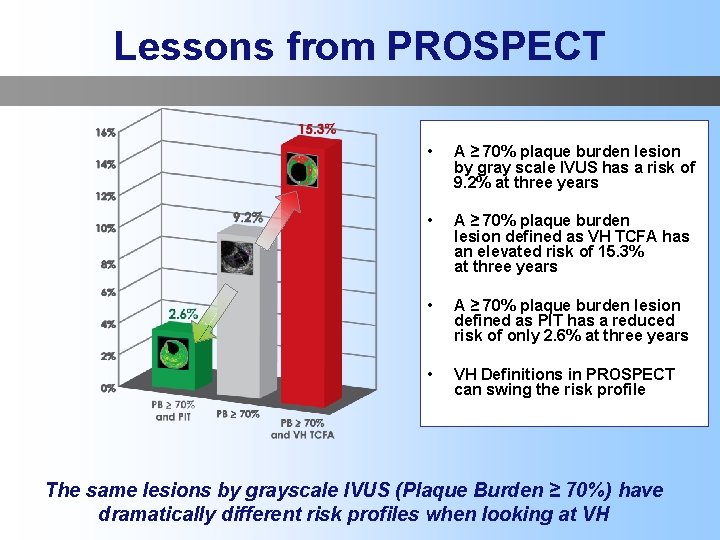
Lessons from PROSPECT • A ≥ 70% plaque burden lesion by gray scale IVUS has a risk of 9. 2% at three years • A ≥ 70% plaque burden lesion defined as VH TCFA has an elevated risk of 15. 3% at three years • A ≥ 70% plaque burden lesion defined as PIT has a reduced risk of only 2. 6% at three years • VH Definitions in PROSPECT can swing the risk profile The same lesions by grayscale IVUS (Plaque Burden ≥ 70%) have dramatically different risk profiles when looking at VH
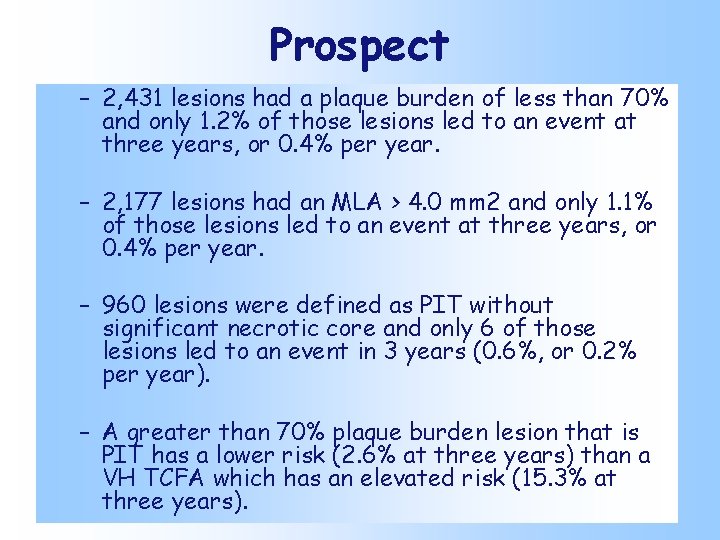
Prospect – 2, 431 lesions had a plaque burden of less than 70% and only 1. 2% of those lesions led to an event at three years, or 0. 4% per year. – 2, 177 lesions had an MLA > 4. 0 mm 2 and only 1. 1% of those lesions led to an event at three years, or 0. 4% per year. – 960 lesions were defined as PIT without significant necrotic core and only 6 of those lesions led to an event in 3 years (0. 6%, or 0. 2% per year). – A greater than 70% plaque burden lesion that is PIT has a lower risk (2. 6% at three years) than a VH TCFA which has an elevated risk (15. 3% at three years).
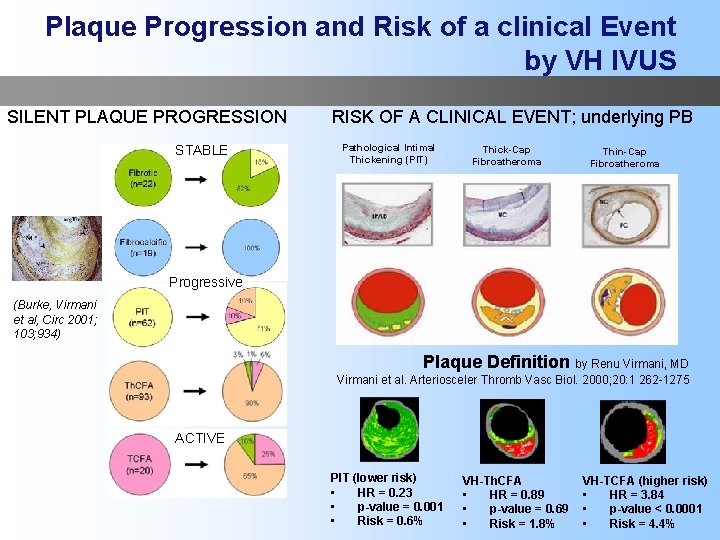
Plaque Progression and Risk of a clinical Event by VH IVUS SILENT PLAQUE PROGRESSION STABLE RISK OF A CLINICAL EVENT; underlying PB Pathological Intimal Thickening (PIT) Thick-Cap Fibroatheroma Thin-Cap Fibroatheroma Progressive (Burke, Virmani et al, Circ 2001; 103; 934) Plaque Definition by Renu Virmani, MD Virmani et al. Arteriosceler Thromb Vasc Biol. 2000; 20: 1 262 -1275 ACTIVE PIT (lower risk) • HR = 0. 23 • p-value = 0. 001 • Risk = 0. 6% VH-Th. CFA • HR = 0. 89 • p-value = 0. 69 • Risk = 1. 8% VH-TCFA (higher risk) • HR = 3. 84 • p-value < 0. 0001 • Risk = 4. 4%

Summary • Over 150 original manuscripts have been published on VH IVUS so far • We can identify a high risk lesion for plaque progression, plaque rupture and risk of a clinical event now with higher accuracy than ever before • We can identify lesions with low risk of an event that may be left untreated • We can place stents with better precision to cover the source of the problem = the location of the TCFA in both stable and ACS patients • Since TCFA’s are related to clinical events and plaque progression, we have now the ability to assess the efficacy of systemic therapy and new pharmaceutical options in a meaningful and clinically relevant manner in every day clinical practice
 Amos anderson omaisuus
Amos anderson omaisuus Pauliina margolis
Pauliina margolis Bruce margolis
Bruce margolis Pauliina stranius
Pauliina stranius Talsta
Talsta Pauliina kanervo
Pauliina kanervo Tuulikulkeumaa vähentävät suuttimet
Tuulikulkeumaa vähentävät suuttimet Pauliina heinänen
Pauliina heinänen Vammaisten lasten ja nuorten tukisäätiö
Vammaisten lasten ja nuorten tukisäätiö Has virtual functions and accessible non-virtual destructor
Has virtual functions and accessible non-virtual destructor Qualitative paper example
Qualitative paper example Tactile fremitus.
Tactile fremitus. Findings in research
Findings in research Communication of research findings
Communication of research findings Words images objects qualitative or quantitative
Words images objects qualitative or quantitative Throax
Throax Causes of rickets
Causes of rickets Results and discussion qualitative research
Results and discussion qualitative research Conncets
Conncets Role of quantitative research
Role of quantitative research Recommendation and conclusion example
Recommendation and conclusion example Tympany sound
Tympany sound Acute interstitial nephritis urine findings
Acute interstitial nephritis urine findings Desiredresults.us
Desiredresults.us Atrial fibrilation ecg
Atrial fibrilation ecg Pernicious anemia vs megaloblastic anemia
Pernicious anemia vs megaloblastic anemia Megaloblastic anemia laboratory findings
Megaloblastic anemia laboratory findings