Nephroticnephritic syndrome Hrishi Narayanan Learning Outcomes Understand the






- Slides: 24

Nephrotic/nephritic syndrome Hrishi Narayanan

Learning Outcomes • Understand the key differences between nephrotic and nephritic syndrome (nephritis) • Describe initial investigations and management of nephrotic and nephritic syndrome (nephritis) • Describe the possible complications of nephrotic syndrome

Scenario • 24 year old man • Feeling more tired recently • No systemic symptoms on questioning • Frothy urine, no urinary symptoms, no blood • No past medical history, no medications • Non-smoker, social alcohol use • Examination is unremarkable • Urine dipstick - protein +++
Scenario 1. What are your main differential diagnoses for this gentleman? 2. What are the features of nephrotic syndrome and nephritic syndrome? 3. How would you investigate this gentleman? 4. What would your management plan be for this gentleman? 5. What are the complications of nephrotic syndrome?

Differentials • • • • Emotional stress Exercise Fever UTI Orthostatic Seizures Focal segmental glomerulonephritis Ig. A nephropathy (ie Berger's disease) Ig. M nephropathy Membranoproliferative glomerulonephritis Membranous nephropathy Minimal change disease Haemoglobinuria Multiple myeloma Myoglobinuria Pre-eclampsia/eclampsia • • • Alport's syndrome Amyloidosis Sarcoidosis Drugs (eg non-steroidal antiinflammatory drugs (NSAIDs), penicillamine, gold, angiotensin-converting enzyme (ACE) inhibitors) Anderson-Fabry disease Sickle cell disease Malignancies (eg lymphoma, solid tumours) Infections (eg HIV, syphilis, hepatitis, poststreptococcal infection) Aminoaciduria Drugs (eg NSAIDs, antibiotics) Fanconi's syndrome Heavy metal ingestion
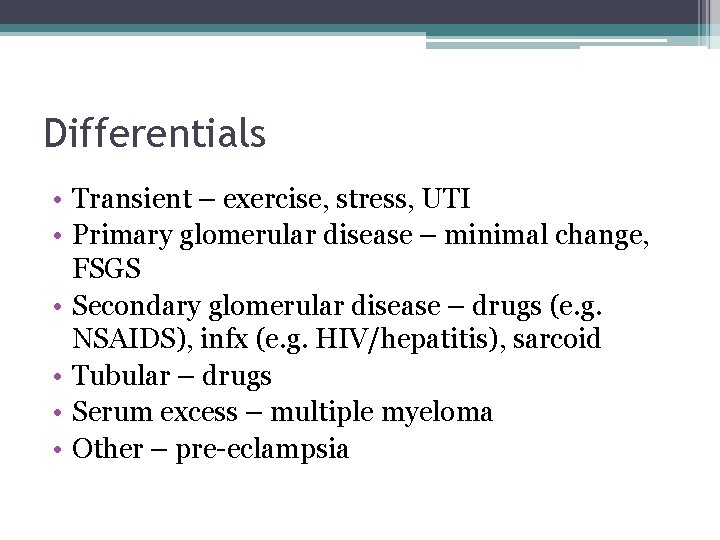
Differentials • Transient – exercise, stress, UTI • Primary glomerular disease – minimal change, FSGS • Secondary glomerular disease – drugs (e. g. NSAIDS), infx (e. g. HIV/hepatitis), sarcoid • Tubular – drugs • Serum excess – multiple myeloma • Other – pre-eclampsia
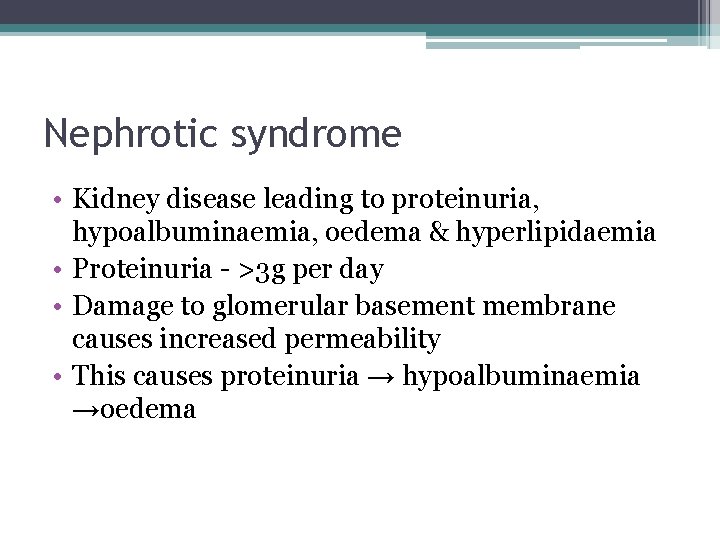
Nephrotic syndrome • Kidney disease leading to proteinuria, hypoalbuminaemia, oedema & lipiduria • Proteinuria - >3 g per day • Damage to glomerular basement membrane causes increased permeability • This causes proteinuria → hypoalbuminaemia →oedema
Nephrotic syndrome • Kidney disease leading to proteinuria, hypoalbuminaemia, oedema & hyperlipidaemia • Proteinuria - >3 g per day • Damage to glomerular basement membrane causes increased permeability • This causes proteinuria → hypoalbuminaemia →oedema
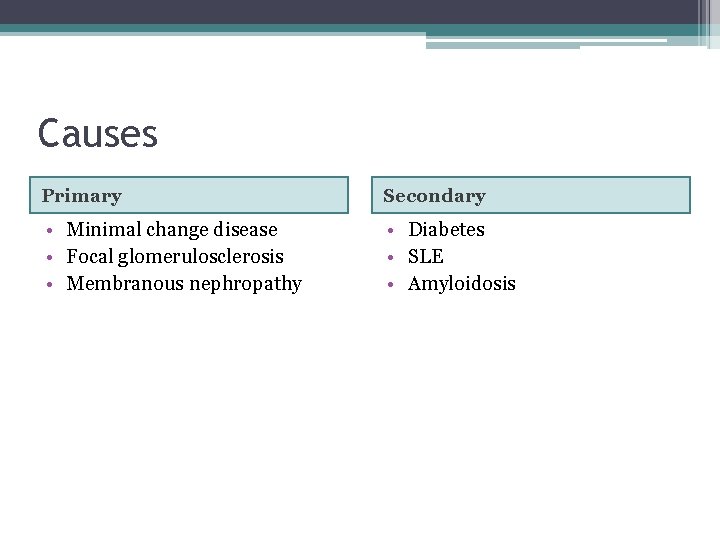
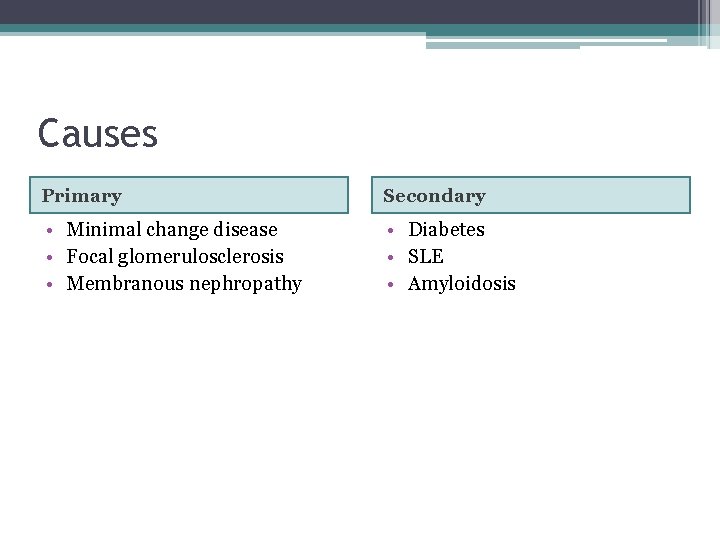
Causes Primary Secondary • Minimal change disease • Focal glomerulosclerosis • Membranous nephropathy • Diabetes • SLE • Amyloidosis
Symptoms • Oedema • Foamy urine • Complications
Nephritic syndrome • Collection of findings associated with glomerular inflammation and glomerulonephritis • Features: ▫ ▫ ▫ Haematuria & red cell casts Proteinuria Hypertension Uraemia Oliguria
Nephritic syndrome • Collection of findings associated with glomerular inflammation and glomerulonephritis • Features: ▫ ▫ ▫ Haematuria & red cell casts Proteinuria Hypertension Uraemia Oliguria
Causes 1. Post-streptococcal 2. Primary: ▫ ▫ ▫ Membranous glomerulonephritis Rapidly progressive glomerulonephritis Ig. A nephropathy (Berger’s disease) 3. Secondary ▫ ▫ HSP Vasculitis
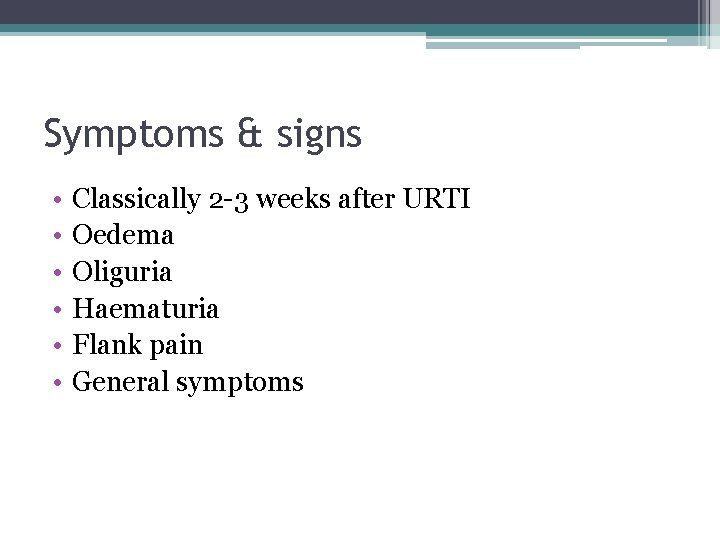
Symptoms & signs • • • Classically 2 -3 weeks after URTI Oedema Oliguria Haematuria Flank pain General symptoms
Investigations • Urine dip • Urine microscopy • Bloods – FBC, U&E, ESR, complement, autoantibodies, myeloma screen, ASOT • Renal Ultrasound • Renal biopsy

Investigations • Urine dipstick • Urine microscopy • Bloods – FBC, U&E, ESR, complement, autoantibodies, myeloma screen, ASOT • Renal Ultrasound • Renal biopsy

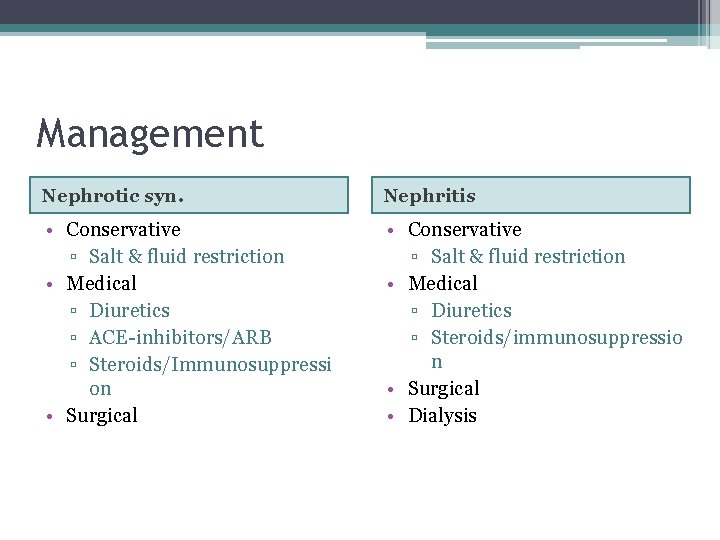
Management Nephrotic syn. Nephritis • Conservative ▫ Salt & fluid restriction • Medical ▫ Diuretics ▫ ACE-inhibitors/ARB ▫ Steroids/Immunosuppressi on • Surgical • Conservative ▫ Salt & fluid restriction • Medical ▫ Diuretics ▫ Steroids/immunosuppressio n • Surgical • Dialysis
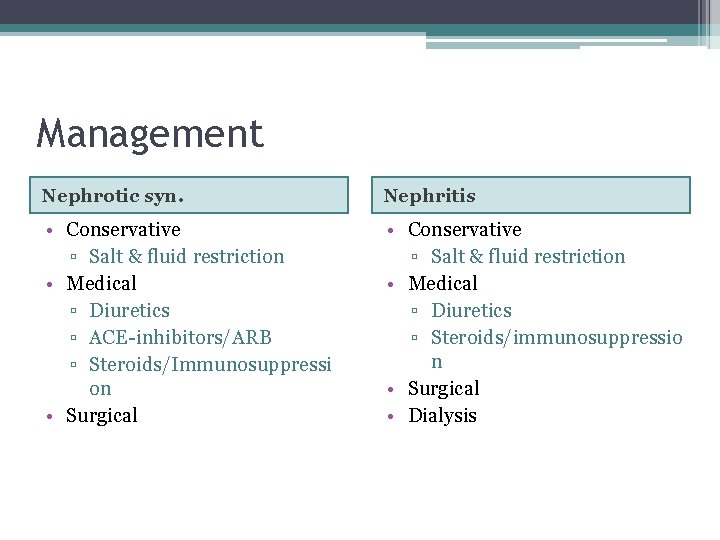
Management Nephrotic syn. Nephritis • Conservative ▫ Salt & fluid restriction • Medical ▫ Diuretics ▫ ACE-inhibitors/ARB ▫ Steroids/Immunosuppressi on • Surgical • Conservative ▫ Salt & fluid restriction • Medical ▫ Diuretics ▫ Steroids/immunosuppressio n • Surgical • Dialysis
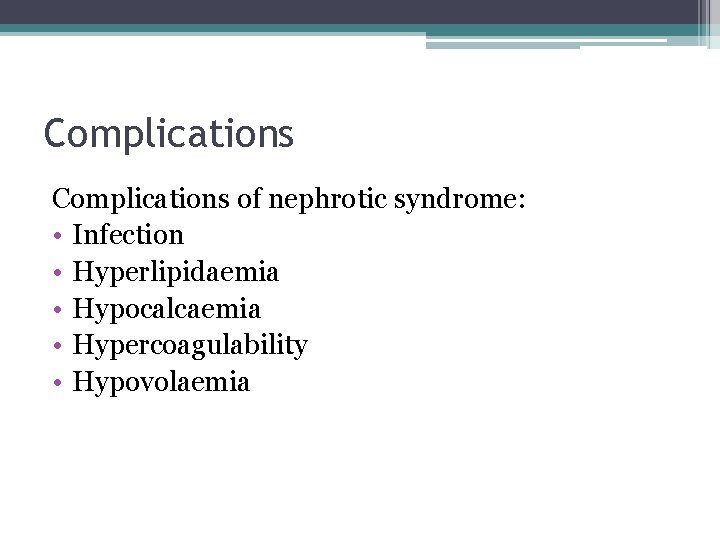
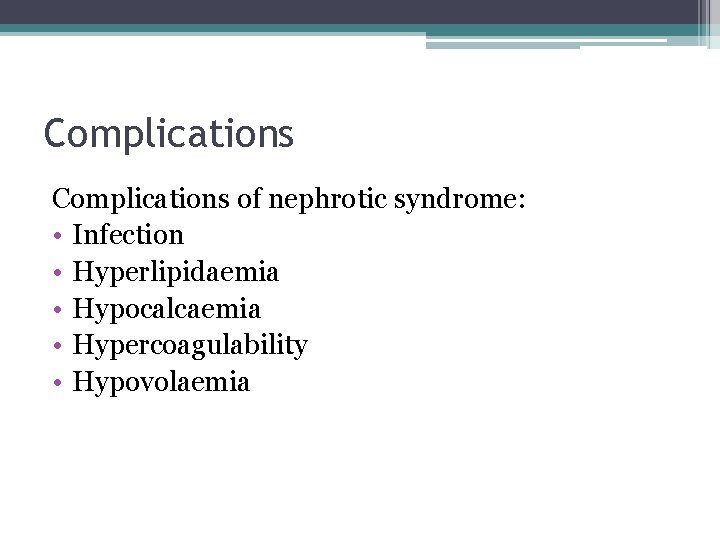
Complications of nephrotic syndrome: • Infection • Hyperlipidaemia • Hypocalcaemia • Hypercoagulability • Hypovolaemia
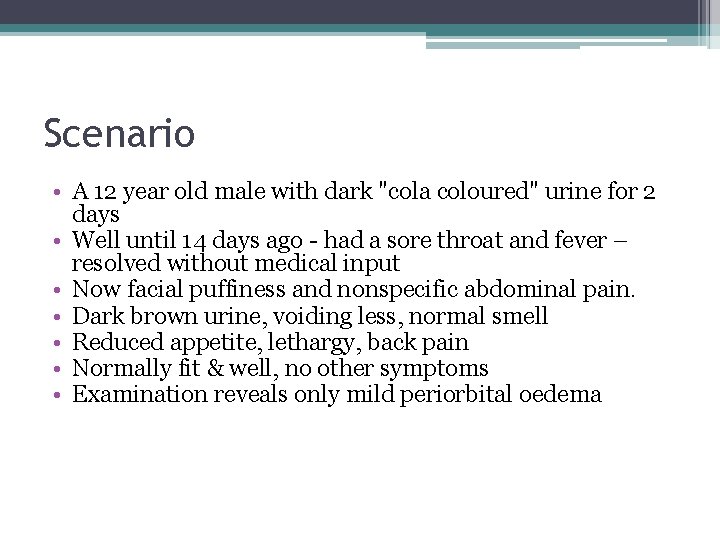
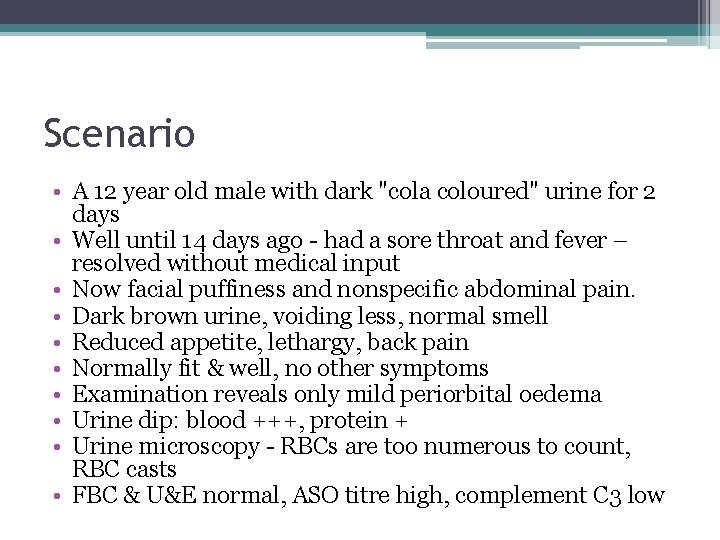
Scenario • A 12 year old male with dark "cola coloured" urine for 2 days • Well until 14 days ago - had a sore throat and fever – resolved without medical input • Now facial puffiness and nonspecific abdominal pain. • Dark brown urine, voiding less, normal smell • Reduced appetite, lethargy, back pain • Normally fit & well, no other symptoms • Examination reveals only mild periorbital oedema Urine dip: blood +++, protein + Urine microscopy - RBCs are too numerous to count, RBC casts FBC & U&E normal, ASO titre high, complement C 3 low
Scenario • A 12 year old male with dark "cola coloured" urine for 2 days • Well until 14 days ago - had a sore throat and fever – resolved without medical input • Now facial puffiness and nonspecific abdominal pain. • Dark brown urine, voiding less, normal smell • Reduced appetite, lethargy, back pain • Normally fit & well, no other symptoms • Examination reveals only mild periorbital oedema • Urine dip: blood +++, protein + • Urine microscopy - RBCs are too numerous to count, RBC casts • FBC & U&E normal, ASO titre high, complement C 3 low
Scenario 1. What are your main differential diagnoses for this patient? 2. How would you investigate this patient? 3. What would your management plan be for this patient?
Key points • Nephrotic syndrome – heavy proteinuria, nephritis (nephritic syndrome) – haematuria • Always do a urine dip for patients with oedema • Important complications include infection and hypoercoagulability
Questions?
 To understand recursion you must understand recursion
To understand recursion you must understand recursion Bhargavi narayanan
Bhargavi narayanan Kaushik narayanan
Kaushik narayanan Dushyanth narayanan
Dushyanth narayanan Slickpic
Slickpic Priya narayanan naac
Priya narayanan naac Neethu narayanan
Neethu narayanan Narayanan raman
Narayanan raman Learning outcome example
Learning outcome example Learning outcomes of water cycle
Learning outcomes of water cycle Notice writing lesson plan
Notice writing lesson plan Learning outcomes of swot analysis
Learning outcomes of swot analysis Nursery rhymes importance
Nursery rhymes importance Planning goals and learning outcomes
Planning goals and learning outcomes Photosynthesis takes place in
Photosynthesis takes place in Learning outcomes of photosynthesis
Learning outcomes of photosynthesis Ncbts stands for
Ncbts stands for Leov math
Leov math Learning outcome generator
Learning outcome generator Learning objectives of reported speech
Learning objectives of reported speech Purpose of learning outcomes
Purpose of learning outcomes Modern input and output devices
Modern input and output devices Biological level of analysis
Biological level of analysis How to write reflective essay
How to write reflective essay Learning outcomes of holy week
Learning outcomes of holy week