Native Mitral Valvular Disease A Focused Review David


- Slides: 35
Native Mitral Valvular Disease A Focused Review David M. Harris MD, FASE, FACC
• Disclosures- None
Goals • Review the physical examine finding of mitral valvular disease. • Learn the evaluation and treatment of mitral valvular heart disease. • Incorporate the information into your daily practice and patient care.
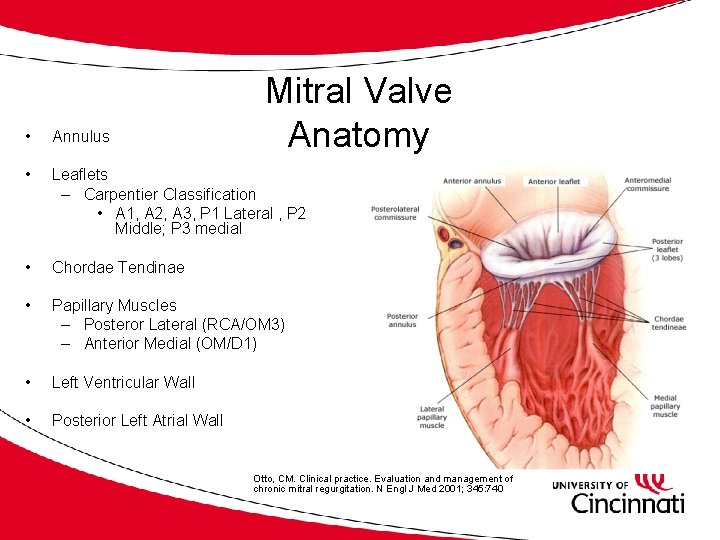
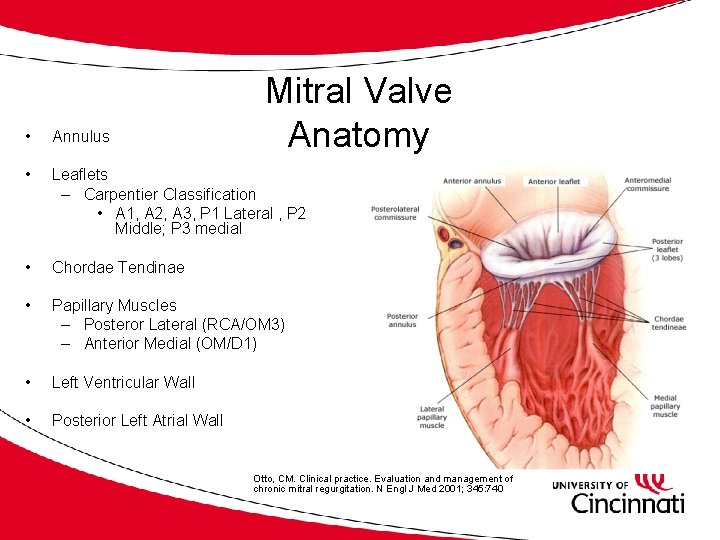
Mitral Valve Anatomy • Annulus • Leaflets – Carpentier Classification • A 1, A 2, A 3, P 1 Lateral , P 2 Middle; P 3 medial • Chordae Tendinae • Papillary Muscles – Posteror Lateral (RCA/OM 3) – Anterior Medial (OM/D 1) • Left Ventricular Wall • Posterior Left Atrial Wall Otto, CM. Clinical practice. Evaluation and management of chronic mitral regurgitation. N Engl J Med 2001; 345: 740
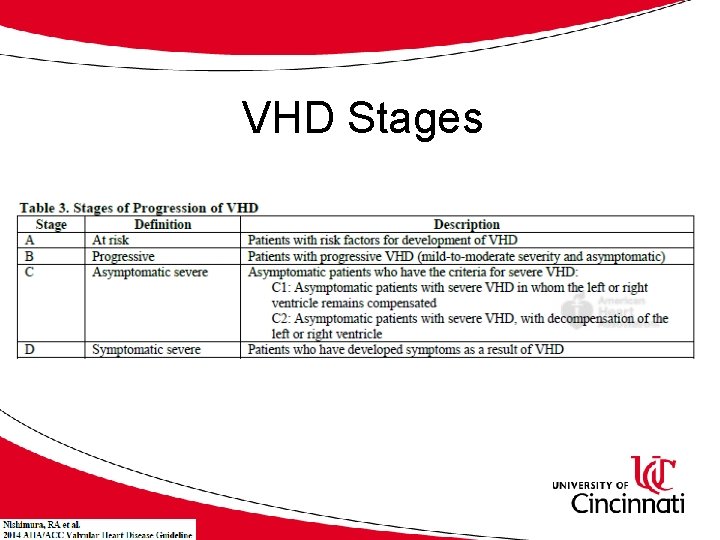
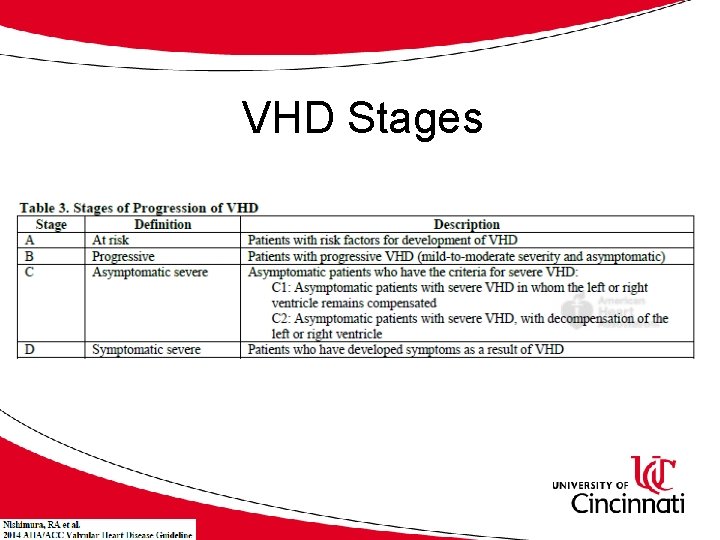
VHD Stages
Assessment for Mitral Valvular Disease • • • History and physical examination Transthoracic Echocardiography Transesophageal Echocardiography Bicycle Stress Echocardiography RHC +/- LHC Stress RHC
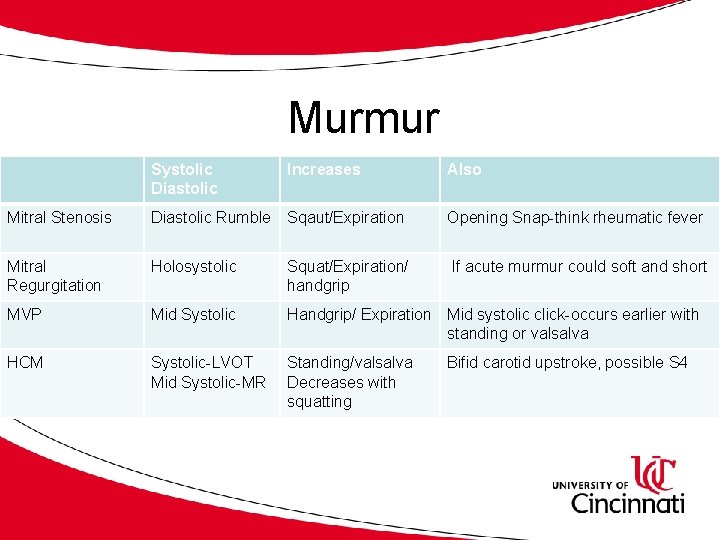
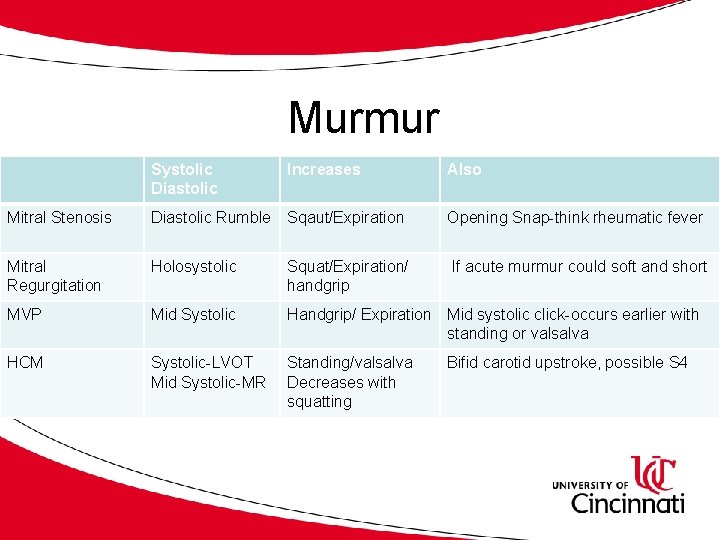
Murmur Systolic Diastolic Increases Also Mitral Stenosis Diastolic Rumble Sqaut/Expiration Opening Snap-think rheumatic fever Mitral Regurgitation Holosystolic Squat/Expiration/ handgrip If acute murmur could soft and short MVP Mid Systolic Handgrip/ Expiration Mid systolic click-occurs earlier with standing or valsalva HCM Systolic-LVOT Mid Systolic-MR Standing/valsalva Decreases with squatting Bifid carotid upstroke, possible S 4
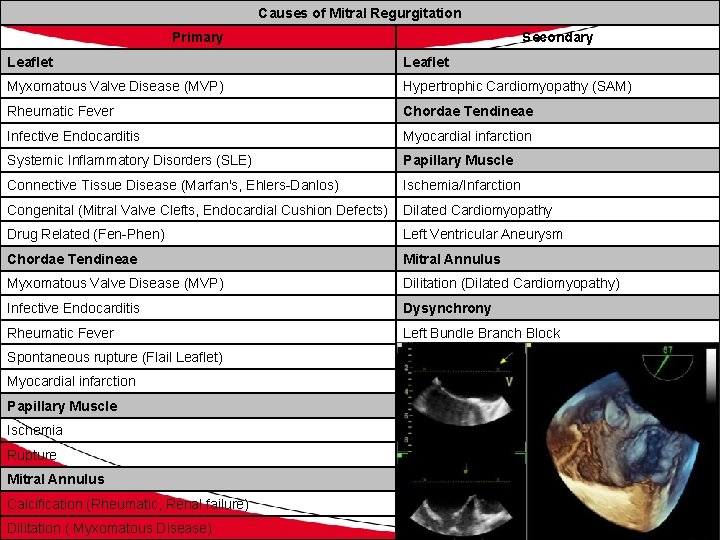
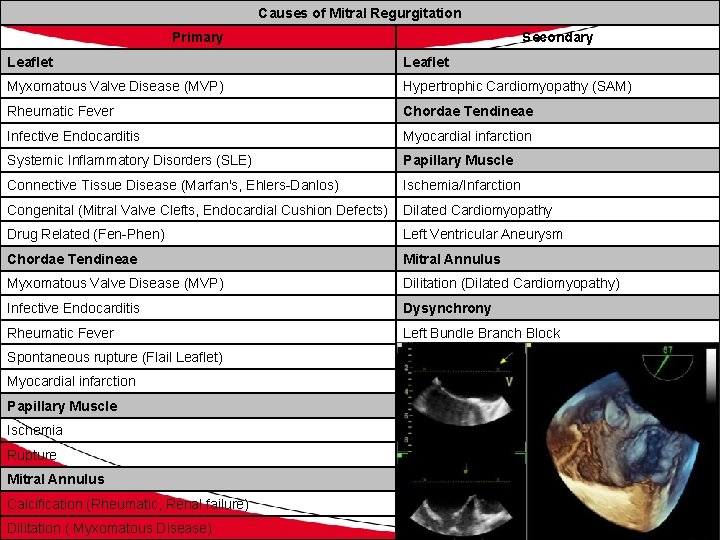
Causes of Mitral Regurgitation Primary Secondary Leaflet Myxomatous Valve Disease (MVP) Hypertrophic Cardiomyopathy (SAM) Rheumatic Fever Chordae Tendineae Infective Endocarditis Myocardial infarction Systemic Inflammatory Disorders (SLE) Papillary Muscle Connective Tissue Disease (Marfan's, Ehlers-Danlos) Ischemia/Infarction Congenital (Mitral Valve Clefts, Endocardial Cushion Defects) Dilated Cardiomyopathy Drug Related (Fen-Phen) Left Ventricular Aneurysm Chordae Tendineae Mitral Annulus Myxomatous Valve Disease (MVP) Dilitation (Dilated Cardiomyopathy) Infective Endocarditis Dysynchrony Rheumatic Fever Left Bundle Branch Block Spontaneous rupture (Flail Leaflet) Myocardial infarction Papillary Muscle Ischemia Rupture Mitral Annulus Calcification (Rheumatic, Renal failure) Dilitation ( Myxomatous Disease)
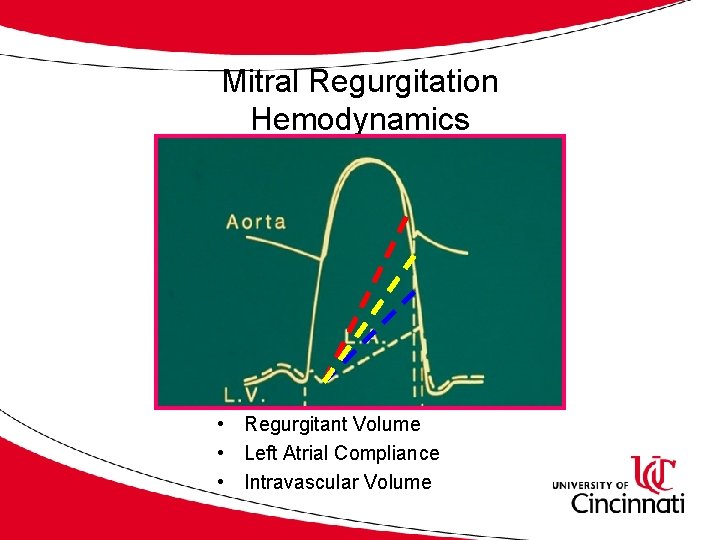
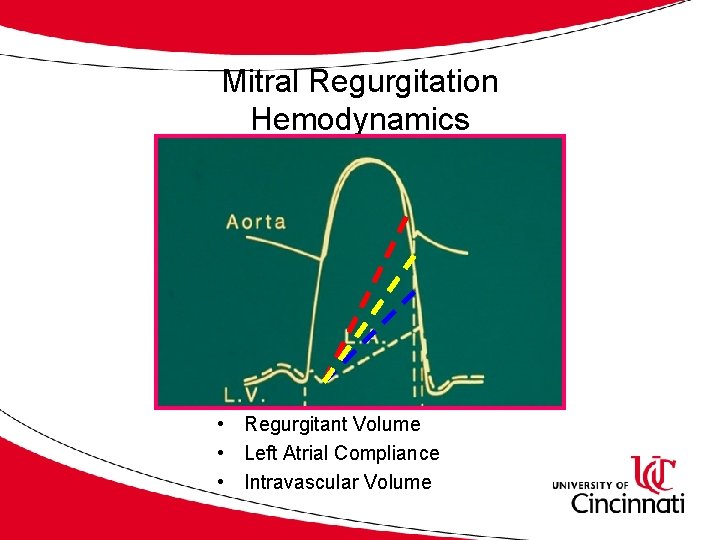
Mitral Regurgitation Hemodynamics • Regurgitant Volume • Left Atrial Compliance • Intravascular Volume
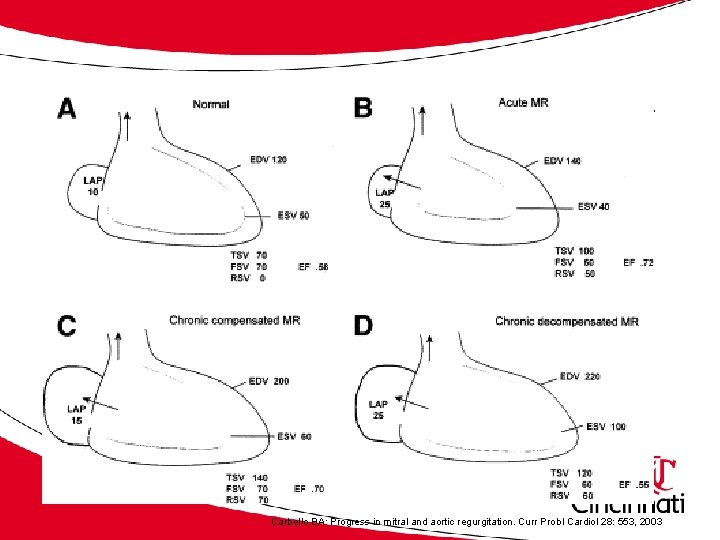
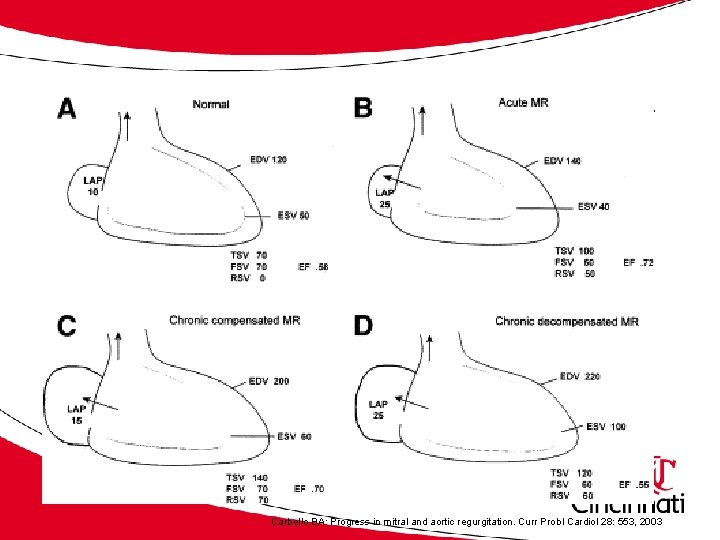
Acute and Chronic Physiology Carbello BA: Progress in mitral and aortic regurgitation. Curr Probl Cardiol 28: 553, 2003
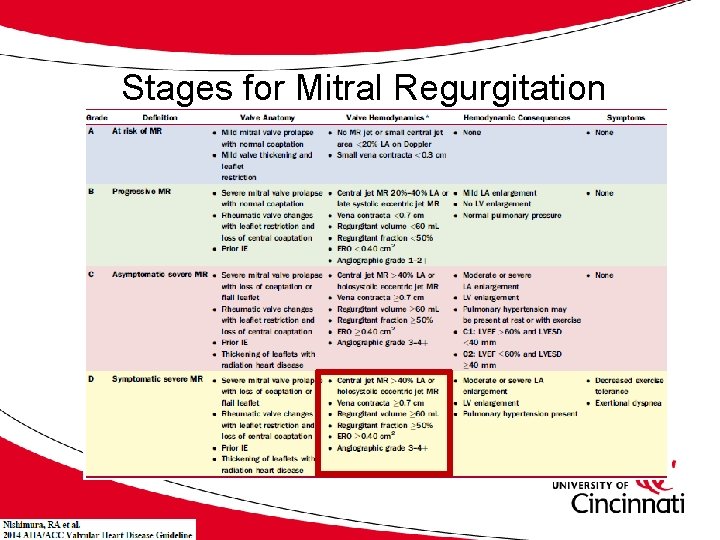
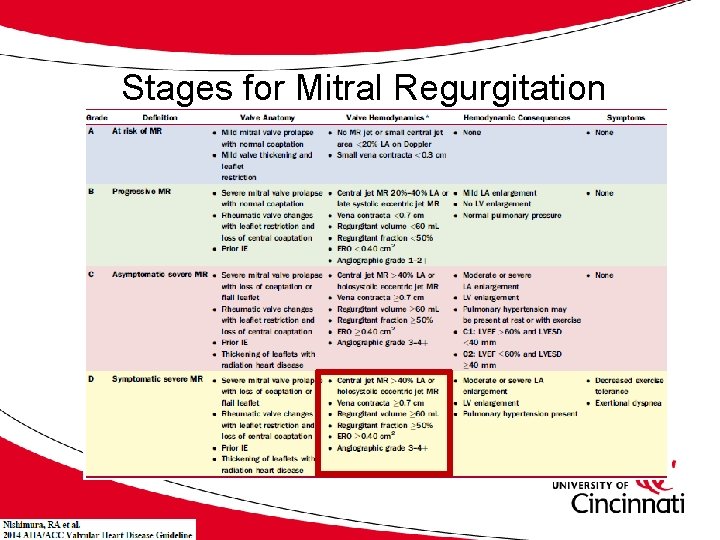
Stages for Mitral Regurgitation
Management of MR • Determine etiology • Decrease afterload (control blood pressure) • Maintain euvolemia (diuretics) • Surgery (Repair over replace) • Mitraclip • Percutaneous Mitral Valvular Replacement
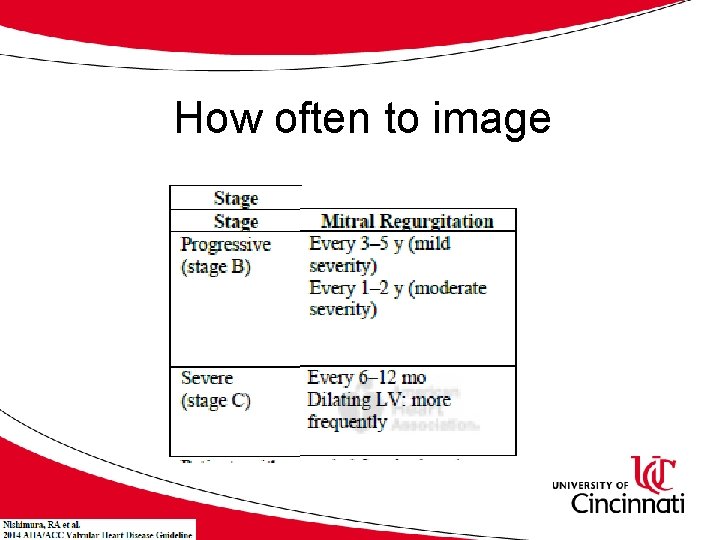
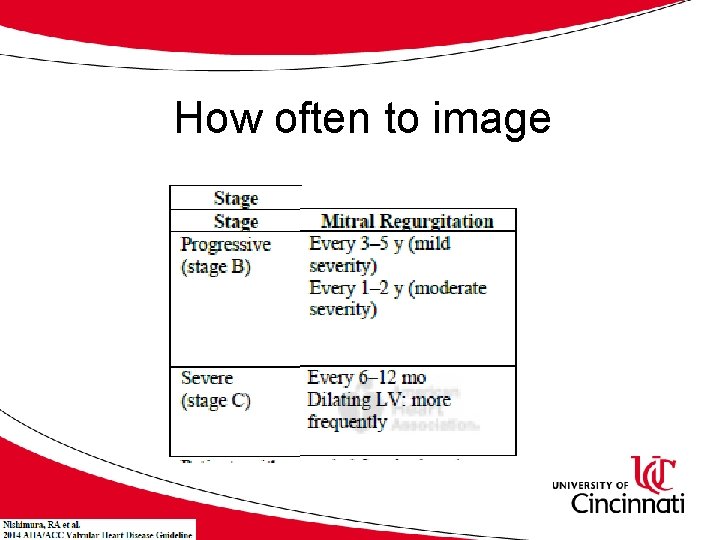
How often to image
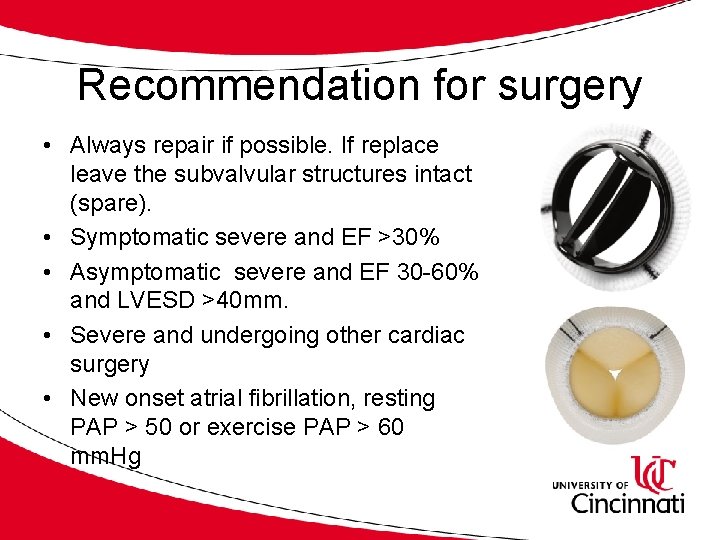
Recommendation for surgery • Always repair if possible. If replace leave the subvalvular structures intact (spare). • Symptomatic severe and EF >30% • Asymptomatic severe and EF 30 -60% and LVESD >40 mm. • Severe and undergoing other cardiac surgery • New onset atrial fibrillation, resting PAP > 50 or exercise PAP > 60 mm. Hg
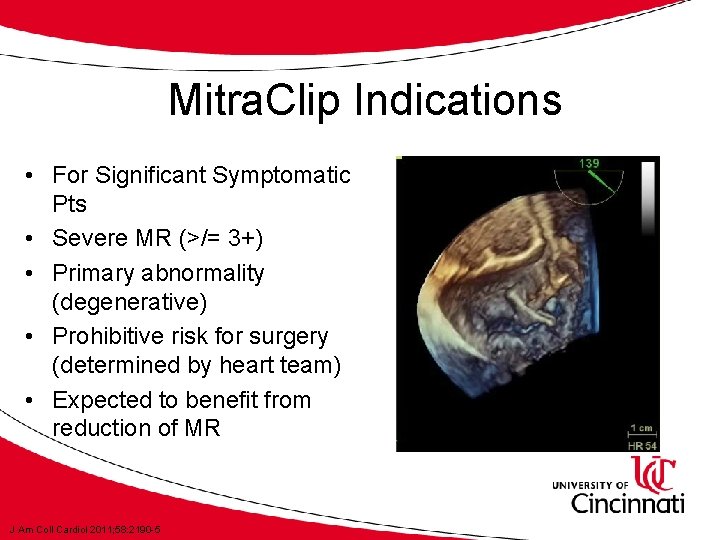
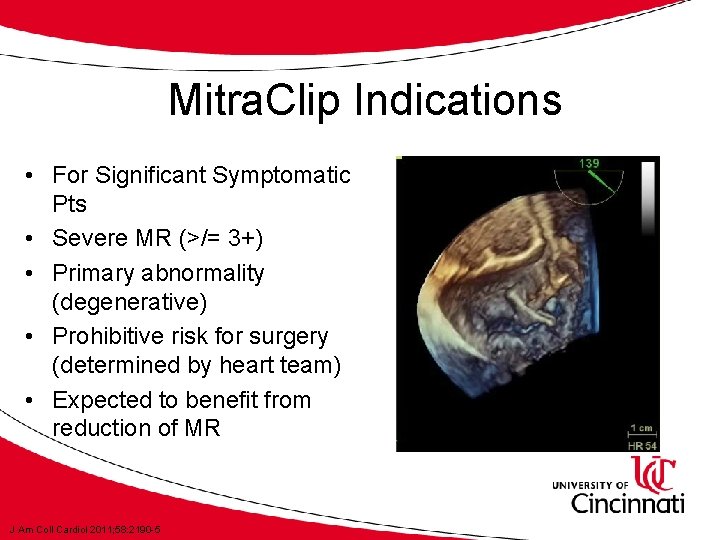
Mitra. Clip Indications • For Significant Symptomatic Pts • Severe MR (>/= 3+) • Primary abnormality (degenerative) • Prohibitive risk for surgery (determined by heart team) • Expected to benefit from reduction of MR J Am Coll Cardiol 2011; 58: 2190 -5

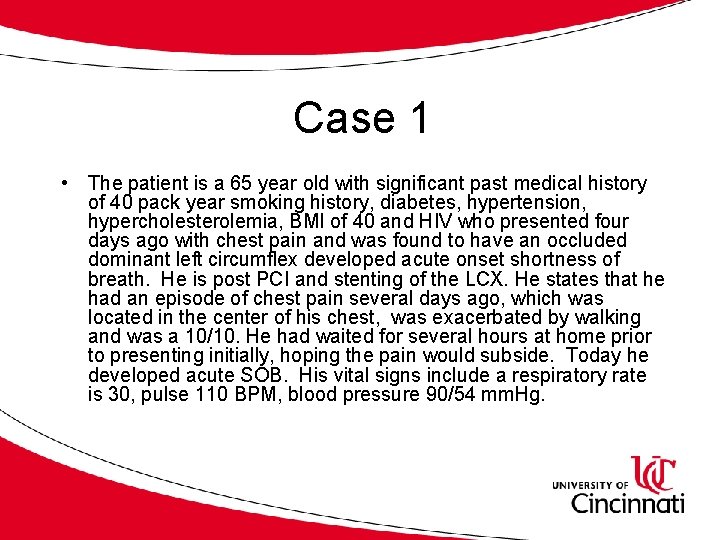
Case 1 • The patient is a 65 year old with significant past medical history of 40 pack year smoking history, diabetes, hypertension, hypercholesterolemia, BMI of 40 and HIV who presented four days ago with chest pain and was found to have an occluded dominant left circumflex developed acute onset shortness of breath. He is post PCI and stenting of the LCX. He states that he had an episode of chest pain several days ago, which was located in the center of his chest, was exacerbated by walking and was a 10/10. He had waited for several hours at home prior to presenting initially, hoping the pain would subside. Today he developed acute SOB. His vital signs include a respiratory rate is 30, pulse 110 BPM, blood pressure 90/54 mm. Hg.
Case 1 Examination • Cardiac: tachycardic with a regular rhythm, there is a new I/VI blowing holosystolic murmur located at the apex which radiates to the axilla, decreases with valsalva and increases with expiration. The PMI is not deviated. JVP measures 16 cm H 2 O. • PULM: Diffuse crackles in the lung fields bilaterally
Echocardiogram Results • Wide open mitral regurgitation-flail posterior leaflet and ruptured posterior lateral papillary muscle
Case 1 What is the initial best medical management? A. Lasix B. Nitroprusside C. Dobutamine D. Bi. PAP E. All of the Above
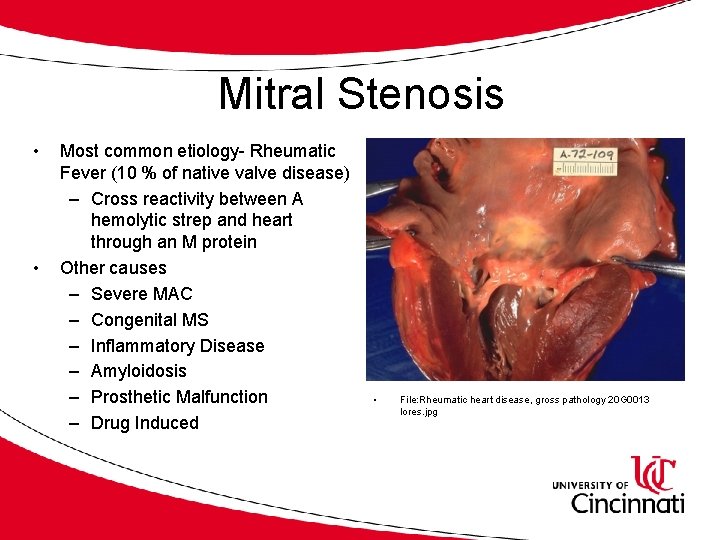
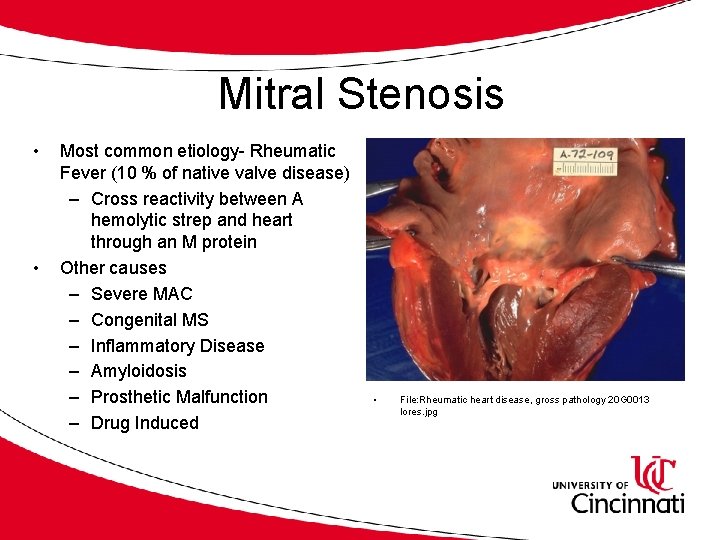
Mitral Stenosis • • Most common etiology- Rheumatic Fever (10 % of native valve disease) – Cross reactivity between A hemolytic strep and heart through an M protein Other causes – Severe MAC – Congenital MS – Inflammatory Disease – Amyloidosis – Prosthetic Malfunction – Drug Induced • File: Rheumatic heart disease, gross pathology 20 G 0013 lores. jpg
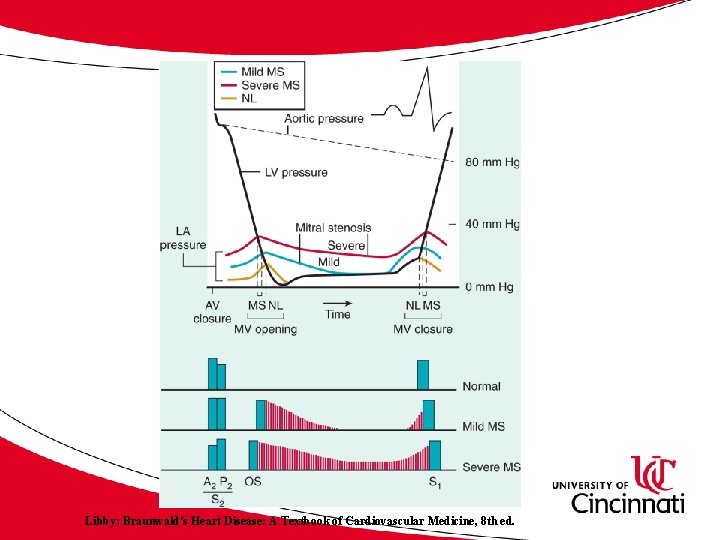
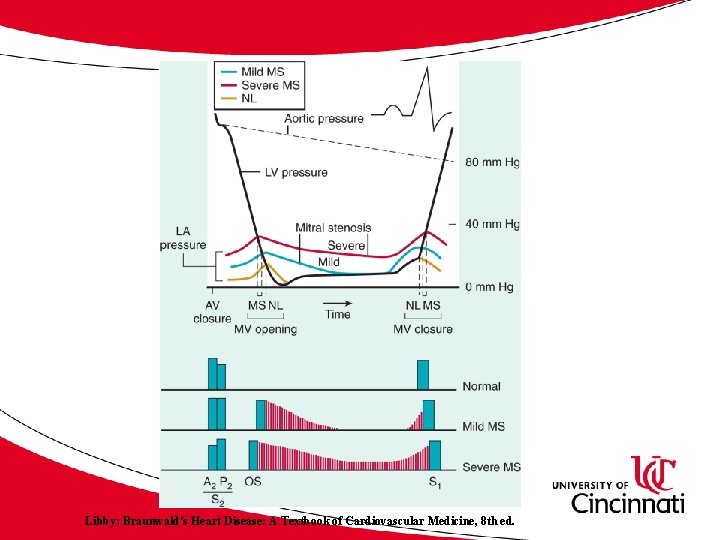
Libby: Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine, 8 th ed.
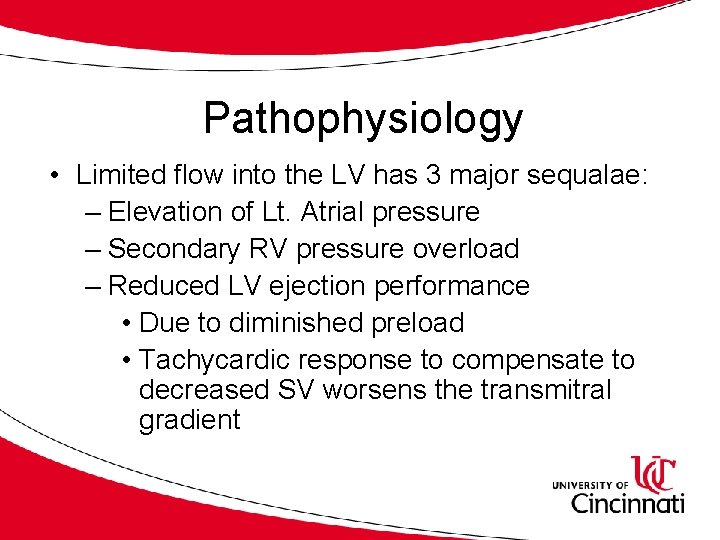
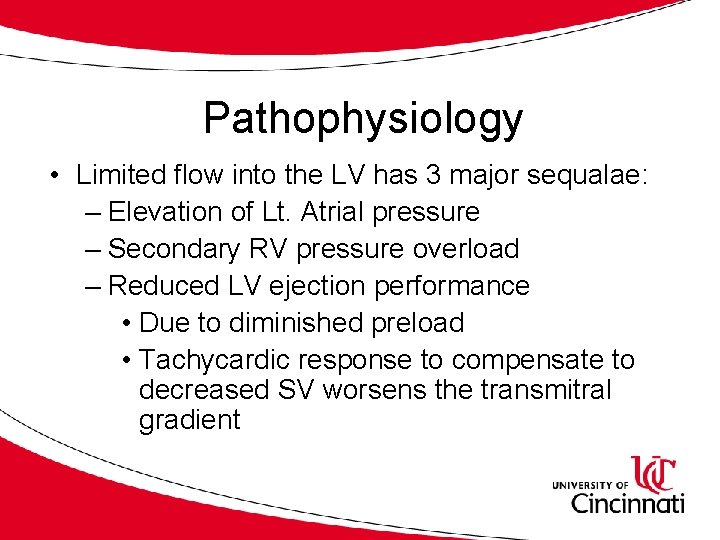
Pathophysiology • Limited flow into the LV has 3 major sequalae: – Elevation of Lt. Atrial pressure – Secondary RV pressure overload – Reduced LV ejection performance • Due to diminished preload • Tachycardic response to compensate to decreased SV worsens the transmitral gradient
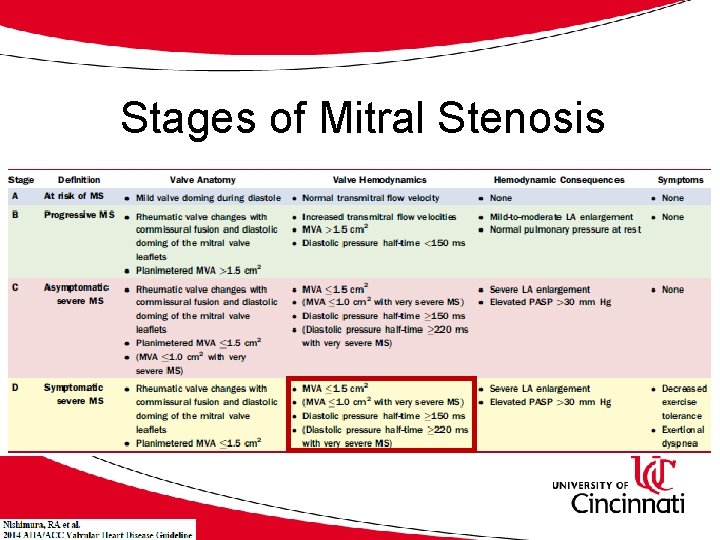
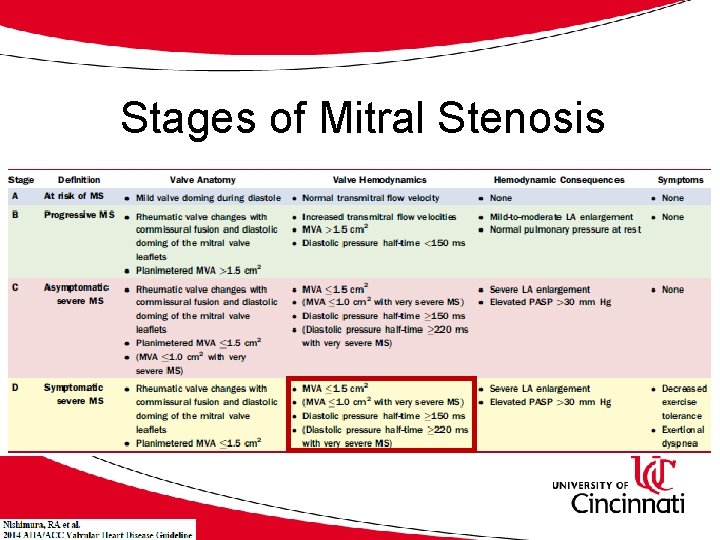
Stages of Mitral Stenosis
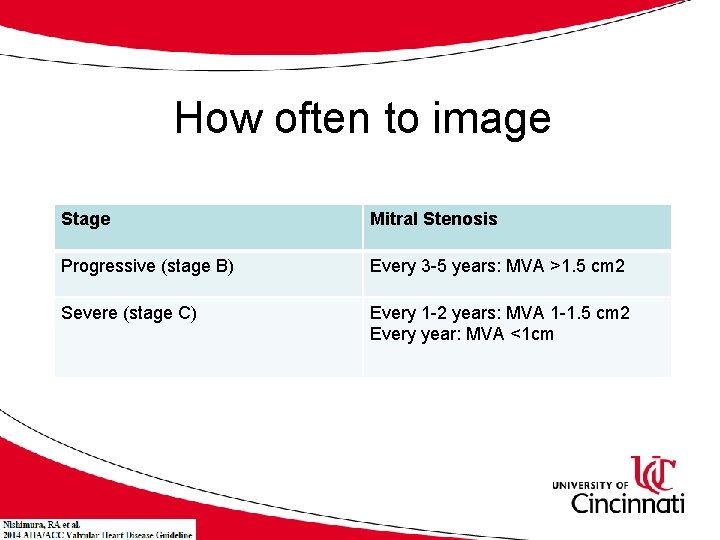
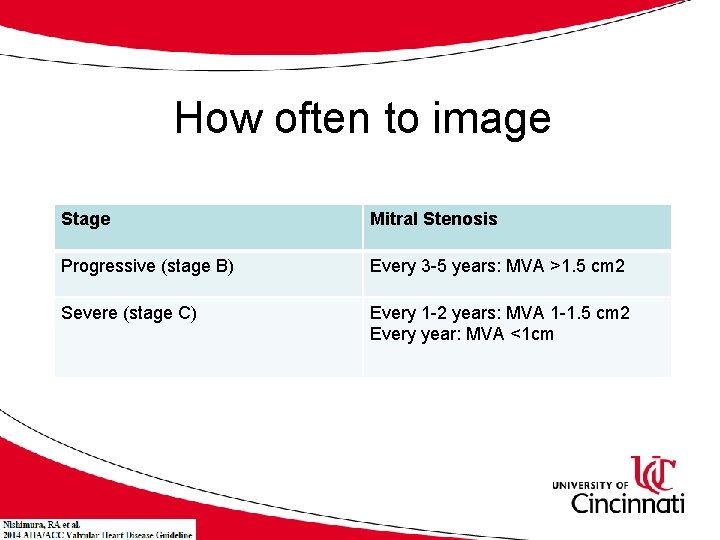
How often to image Stage Mitral Stenosis Progressive (stage B) Every 3 -5 years: MVA >1. 5 cm 2 Severe (stage C) Every 1 -2 years: MVA 1 -1. 5 cm 2 Every year: MVA <1 cm
Anticoagulation and MS • Atrial fibrillation • Prior Embolic Event • LA Thrombus
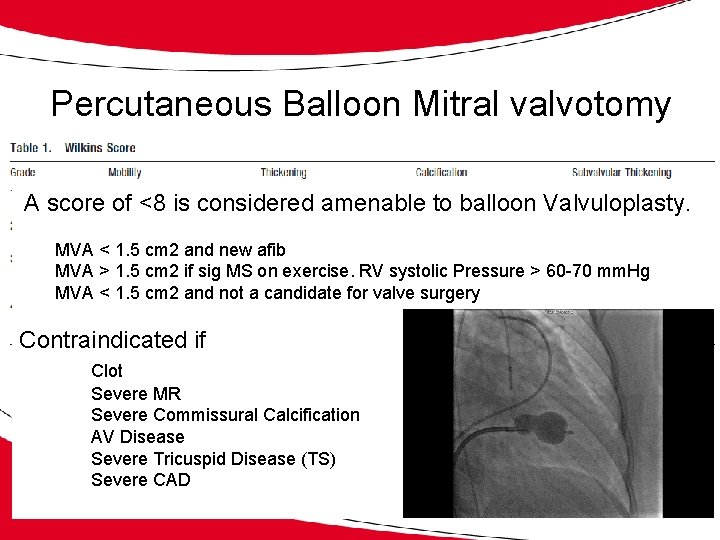
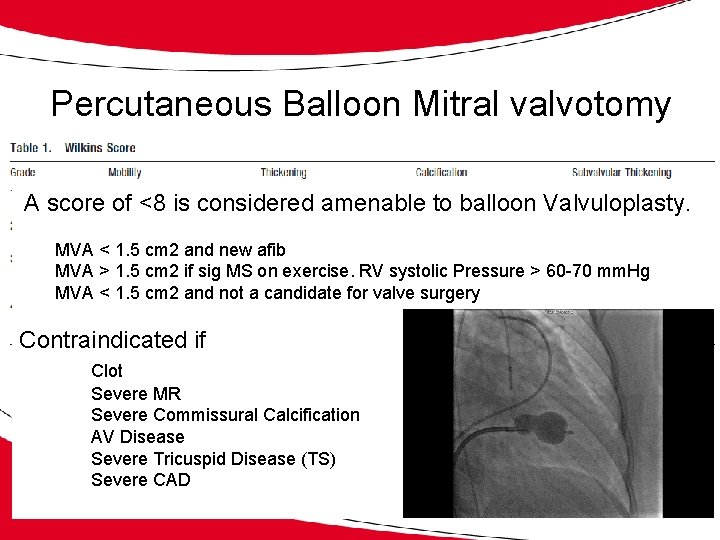
Percutaneous Balloon Mitral valvotomy A score of <8 is considered amenable to balloon Valvuloplasty. MVA < 1. 5 cm 2 and new afib MVA > 1. 5 cm 2 if sig MS on exercise. RV systolic Pressure > 60 -70 mm. Hg MVA < 1. 5 cm 2 and not a candidate for valve surgery Contraindicated if Clot Severe MR Severe Commissural Calcification AV Disease Severe Tricuspid Disease (TS) Severe CAD

Recommendations for Surgery • MVA < 1. 5 cm 2 with symptoms (NYHA class III/IV) • MVA < 1. 5 cm 2 and other cardiac Surgery • MVA < 1. 0 cm 2 and asymptomatic (if favorable anatomy and no contraindications
Case 2 • The patient is a 25 year-old 26 week pregnant G 1 P 0 woman from India without significant past medical history who presents with increasing dyspnea on exertion, shortness of breath, orthopnea, paroxysmal nocturnal dyspnea and lower extremity swelling.
Case 2 Physical examination • Cardiovascular: There is a crisp early diastolic snap followed by a 2/6 diastolic rumble best heard in the axilla. The murmur is loader with squatting and with exercise. JVP is 14 cm H 2 O. • The point of maximal impulse is normal in size and there is no gallop. • There is a right ventricular heave • Pulmonary diffuse crackles bilaterally • +3 bilaterally LE pitting edema
Case 2 What is the best initial step for evaluation A. B. C. D. E. Treadmill Exercise EKG only Stress Transthoracic Echocardiogram Transesophageal Echocardiogram Right Heart Catheterization Chest CT (PE protocol)
Case 2 Echocardiogram Results • LVEF 55 -60%- normal wall motion • Mitral valve decrease leaflet motion with a “hockey stick” appearance to the anterior leaflet; mean gradient of 12 mm. Hg at a heart rate of 108 BPM. Wilkins score= 4. • Left and right atria moderately dilated • Right Ventricle with moderate hypertrophy and normal function.
Case 2 What is the most appropriate management? A. B. C. D. E. Balloon Mitral Valvuloplasty Surgical Valve Repair Surgical Valve Replacement Lasix and Labetolol Watchful waiting-normal in pregnancy
Thank you • Questions