MR COLONOGRAPHY AND COLORECTAL CANCER IOANNA TZOVARA MD

- Slides: 42
MR COLONOGRAPHY AND COLORECTAL CANCER IOANNA TZOVARA, MD RADIOLODIST IASO GENERAL HOSPITAL ATHENS, GREECE.
COLORECTAL CANCER 2 nd most common Ca-related cause of death – major mortality � The time from polyp to cancer development is approximately 10 years. � Early diagnosis of colorectal Ca is important due to the long natural course of the disease. Detection and treatment of adenomatous polyps that have not transformed into Ca yet and early localized Ca are possible through screening programs. �
SCREENING TOOLS � Fecal occult blood tests (FOBT) � Barium double-contrast enema � Colonoscopy (gold standard)
VIRTUAL COLONOSCOPY Bowel cleansing and discomfort of the Colononoscopy procedures lead to poor patient acceptance and low screening rates for colonoscopy. � This led to the development of virtual colonoscopy, which includes both CT colonography and MR colonography. � From the late 1990 s, more studies have been published about CT colonography than on MR colonography. � The CTC appears to be more suitable for colorectal screening than MR colonography. �
CT vs MR COLONOGRAPHY CT colonography has several advantages reduced examination time fewer imaging artifacts higher spatial resolution wider availability less operator dependency lower cost. � However, a major advantage of MR colonography is the lack of ionizing radiation , a potential limitation of screening CT colonography. �
INDICATIONS F 0 R MRC � Indications for MR colonography Inflammatory bowel disease (IBD) Diverticulitis Assessment of colonic anastomoses Colorectal cancer screening Tortuous bowel Severe bowel spasm Extensive diverticular disease Incomplete colonoscopy due to obstructing tumor
INDICATIONS When a tumor occludes the colonic lumen, thereby preventing the colonoscope from being advanced more proximally, MR and CT colonography become very useful tools, since only air or liquid must pass through a stricture to allow visualization of the more proximal colon. � Synchronous lesions that otherwise would have been missed can be identified. �
MRC-CONTRAINDICATIONS Before MR colonography, the patient must be screened for contraindications to MR imaging claustrophobia metallic implants cardiac pacemakers � Patients with hip prostheses are not ideal candidates for either MR colonography or CT colonography due to significant prosthesisrelated artifact, which can obscure views of the rectum and sigmoid colon. �
PREPARATION Patients undego standard bowel preparation with the same diet given by the gastroenterology endoscopy unit and take 3 -4 liters of liquid food daily (water, tea, sour cherry juice, pudding, soup without fiber, and grain) for 2 days prior to the study. Patients take 210 m. L of BT enema solution ) rectally and X-M Diet solution 250 m. L periorally 1 day before the procedure; 210 m. L of BT enema was repeated rectally on the morning of the procedure.
PREPARATION The rigorous bowel preparation associated with colonoscopy and standard virtual colonoscopy remains one of the barriers to widespread acceptance of colorectal cancer screening.
PREPARATION � Preparation-free or limited-preparation techniques have been used. � Similar to stool tagging in CT colonography, ingestion of oral tagging contrast material has been used in MR colonography to adapt the signal of stool to that of the enema fluid. � The results are promising, but further research is required to optimize the technique
MRC PREPARATION � Conscious sedation and � Analgesia are unnecessary for MR colonography.
MR COLONOGRAPHY The most commonly used techniques are dark lumen and white lumen techniques. � In the dark lumen technique, water, air, or carbon dioxide is used in order to provide colon distention. Oral polyethylene glycol solution has been recently added to these techniques. � In the white lumen technique, a 1. 5 -2 -L volume of gadolinium-containing enema is given via perioral or rectal route with 100 -150 cm of hydrostatic pressure. So, the lumen shines with positive contrast medium, and is discriminated from the lesions �
BRIGHT AND DARK LUMEN � � � In MR colonography, the bright and dark-lumen strategy refers to the signal intensity of the bowel lumen at T 1 weighted imaging. In bright-lumen colonography, the bowel lumen is of high signal intensity and the colonic wall remains low in signal intensity. Detection of colonic lesions is based on hypointense luminal filling defects with this approach. Water spiked with paramagnetic contrast is used to distend the bowel lumen and to render the lumen bright. Most bright-lumen MR colonography strategies only administer high-signal contrast material rectally Added paramagnetic oral contrast agent to the major meals before MR colonography to tag fecal residue
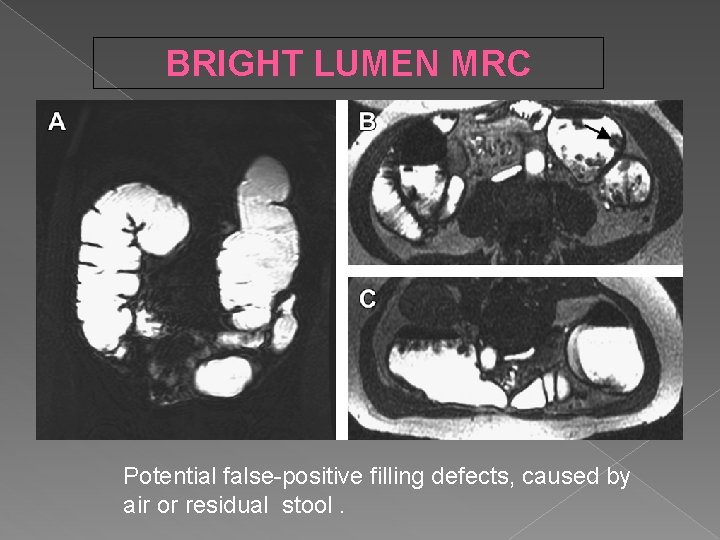
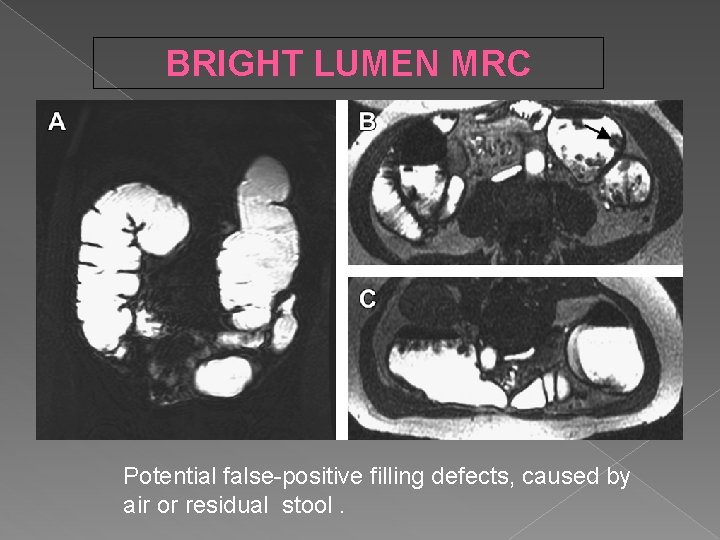
BRIGHT LUMEN MRC Potential false-positive filling defects, caused by air or residual stool.
DARK LUMEN -PROCEDURE Following rectal introduction of a 16 F Foley catheter, the colon is gently filled with 2 -2. 5 l of warm tap water from an enema bag held at shoulder height to distend the colon. Also used room air and carbon dioxide � Bowel motility is abolished by intravenous spasmolytic(Buscopan; Boehringer Ingelheim, Germany) 0. 3 mg kg 21 (max 20 mg) immediately prior to imaging � i. v. gadolinium (0. 2 mg /kg) is also administered. �
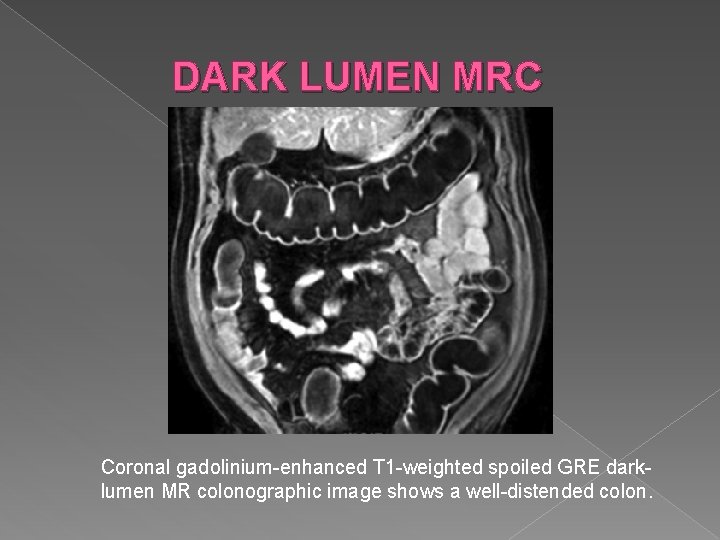
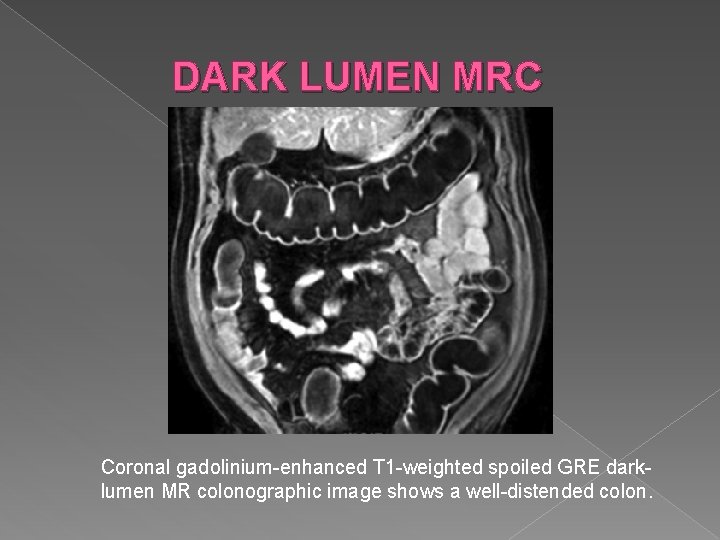
DARK LUMEN MRC Coronal gadolinium-enhanced T 1 -weighted spoiled GRE darklumen MR colonographic image shows a well-distended colon.
DARK LUMEN MRC The aim is to see the lesion by its enhancement in a dark lumen after intravenous contrast administration (Less false neg/pos) � Exam is completed in approximately 20 -30 min after which the water is allowed to drain back into the enema bag. � While the cecum and ascending colon has the most artifacts, the fewest are found in the rectum. � The best distention is obtained in the rectum, and the worst is found in the cecum. �
GADOLINIUM ADMINIDTRATION � By measuring the signal intensities of the lesion on both pre-and postcontrast images, the amount of enhancement can be determined. � True colorectal lesions typically enhance, whereas residual stool particles do not.
DRAWBACKS � Water filling experience. Cramps � Breath holding � Lying still in the MRI scanner (20 min) � Scanner noise � Delay in the results interpretation
1. 5 TESLA vs 3 TESLA � They found no significant difference in image quality at 1. 5 T versus 3. 0 T for polyps 6 mm or larger
MR COLONOGRAPHY T 2 W coronal true fast imaging with steady-state precession (FISP) sequence � Axial T 2 -true-FISP � Axial T 2 HASTE, � Diffusion-weighted images � 3 D T 1 vibe fat suppression coronal sequences � Gadolinium contrast medium administration intravenously. � T 1 vibe fat suppression sequences were repeated on the axial and coronal planes. �
MRC PROCEDURE A large phased-array coil is used to cover the complete abdomen. � For dark- and bright-lumen imaging, dual (prone and supine )positioning is recommended. �
IMAGE EVALUATION � MR colonography data should be evaluated on a workstation that allows for reconstruction of the 3 D-acquired datasets. � 3 D T 1 W sequences are used � 2 D T 2 W sequences can be used for problem solving in cases of motion artifacts � Interpretation times are approximately 20 minutes
IMAGE EVALUATION � An endoluminal fly-through should be performed whenever possible because it enables the radiologist to assess haustral morphologic characteristics more closely, allowing differentiation of haustra from true lesions. � It is recommended that both an antegrade and a retrograde fly-through be performed to allow visualization of both sides of the haustra.
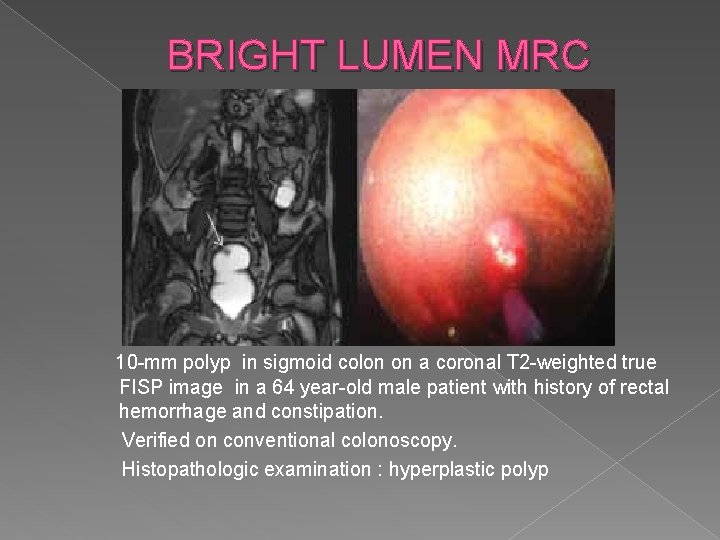
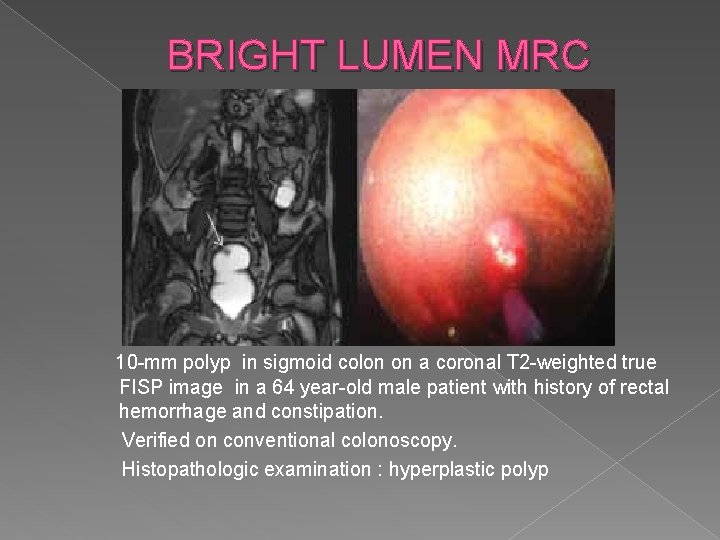
BRIGHT LUMEN MRC 10 -mm polyp in sigmoid colon on a coronal T 2 -weighted true FISP image in a 64 year-old male patient with history of rectal hemorrhage and constipation. Verified on conventional colonoscopy. Histopathologic examination : hyperplastic polyp
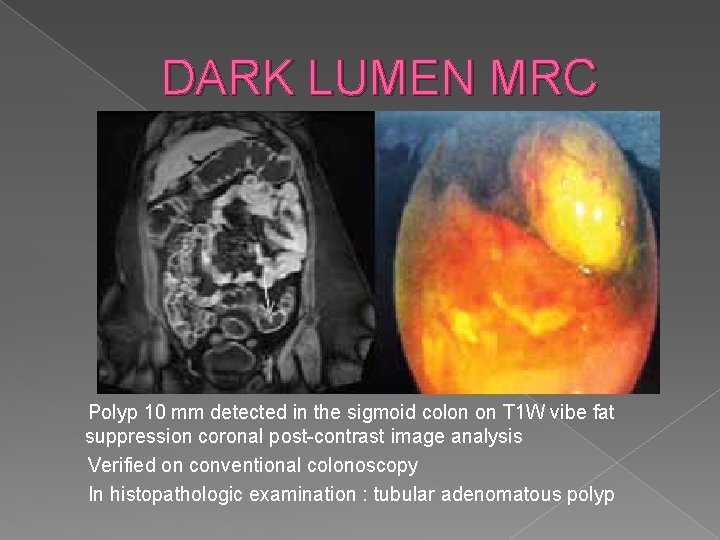
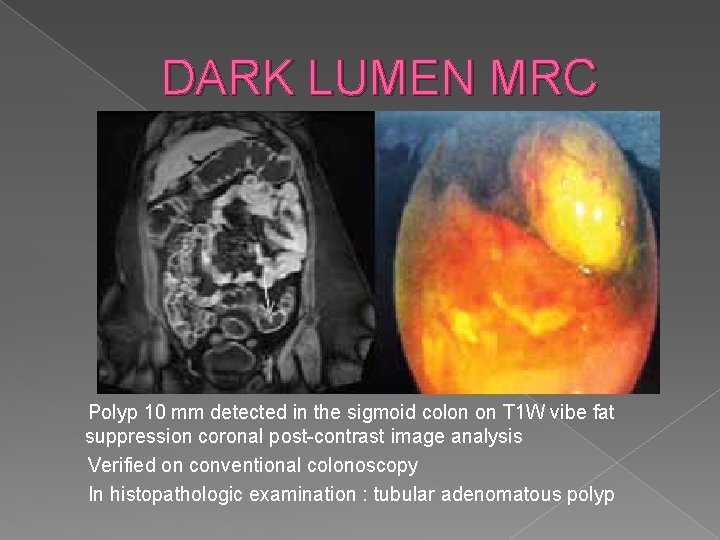
DARK LUMEN MRC Polyp 10 mm detected in the sigmoid colon on T 1 W vibe fat suppression coronal post-contrast image analysis Verified on conventional colonoscopy In histopathologic examination : tubular adenomatous polyp
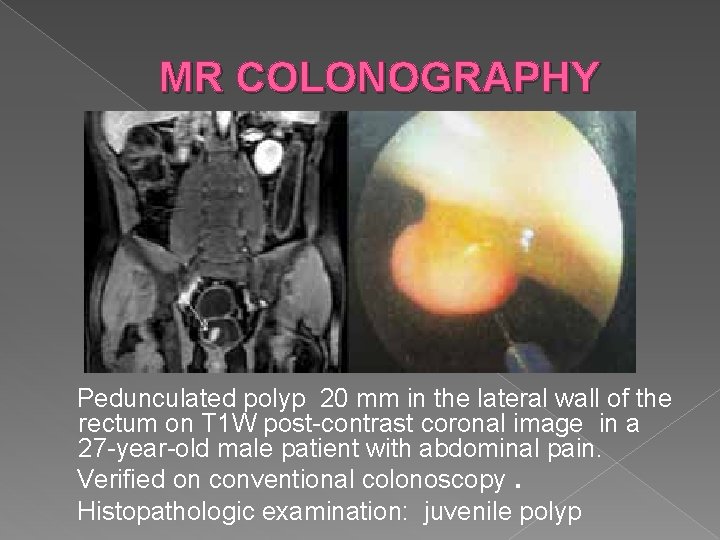
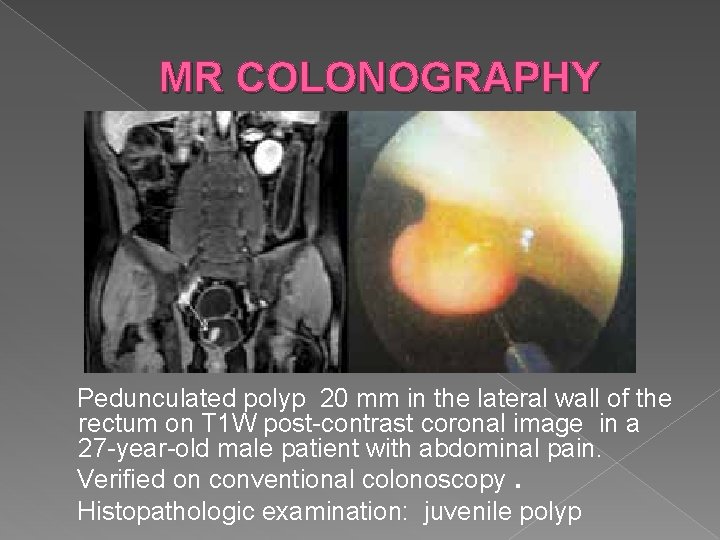
MR COLONOGRAPHY Pedunculated polyp 20 mm in the lateral wall of the rectum on T 1 W post-contrast coronal image in a 27 -year-old male patient with abdominal pain. Verified on conventional colonoscopy. Histopathologic examination: juvenile polyp
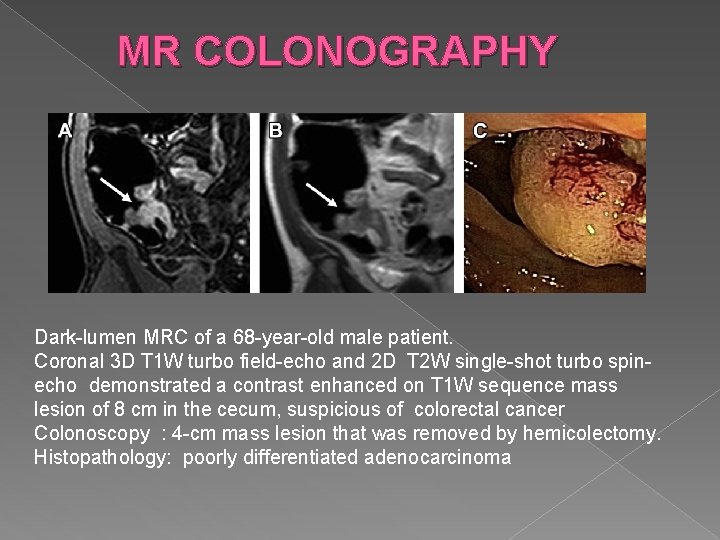
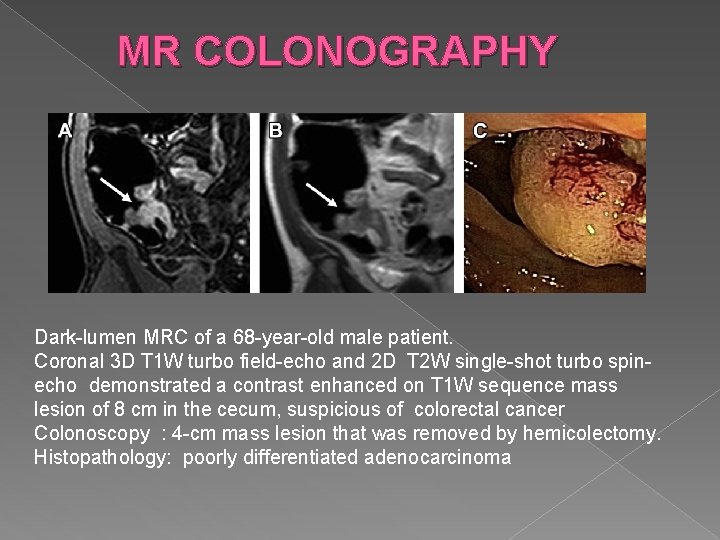
MR COLONOGRAPHY Dark-lumen MRC of a 68 -year-old male patient. Coronal 3 D T 1 W turbo field-echo and 2 D T 2 W single-shot turbo spinecho demonstrated a contrast enhanced on T 1 W sequence mass lesion of 8 cm in the cecum, suspicious of colorectal cancer Colonoscopy : 4 -cm mass lesion that was removed by hemicolectomy. Histopathology: poorly differentiated adenocarcinoma
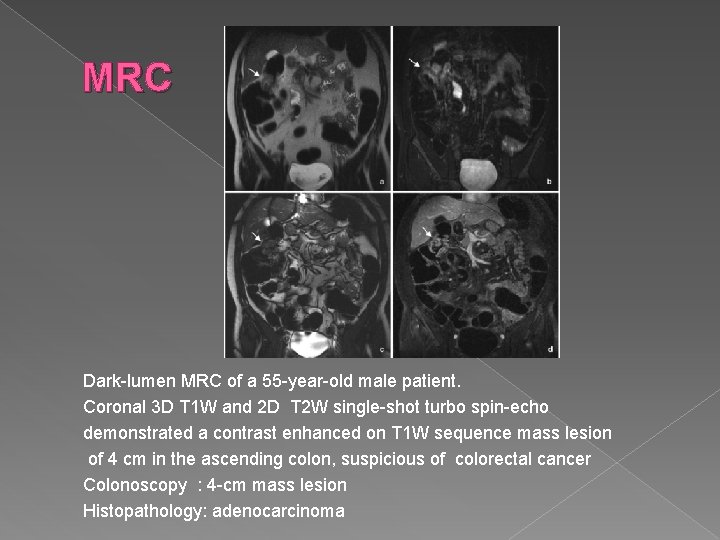
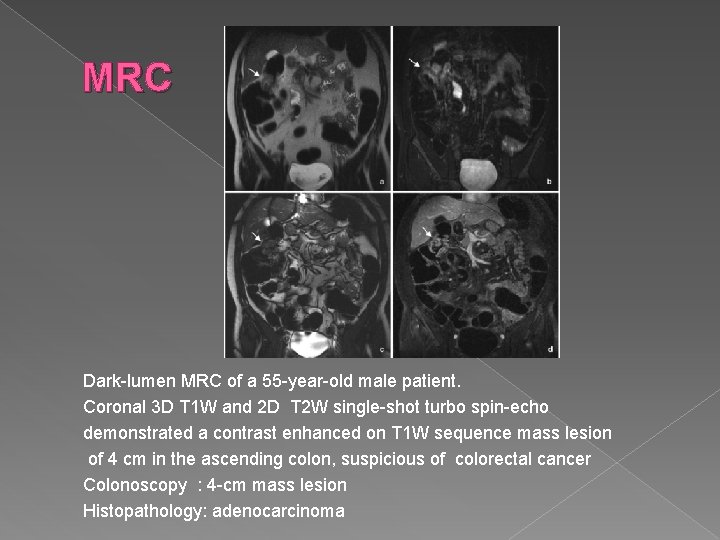
MRC Dark-lumen MRC of a 55 -year-old male patient. Coronal 3 D T 1 W and 2 D T 2 W single-shot turbo spin-echo demonstrated a contrast enhanced on T 1 W sequence mass lesion of 4 cm in the ascending colon, suspicious of colorectal cancer Colonoscopy : 4 -cm mass lesion Histopathology: adenocarcinoma
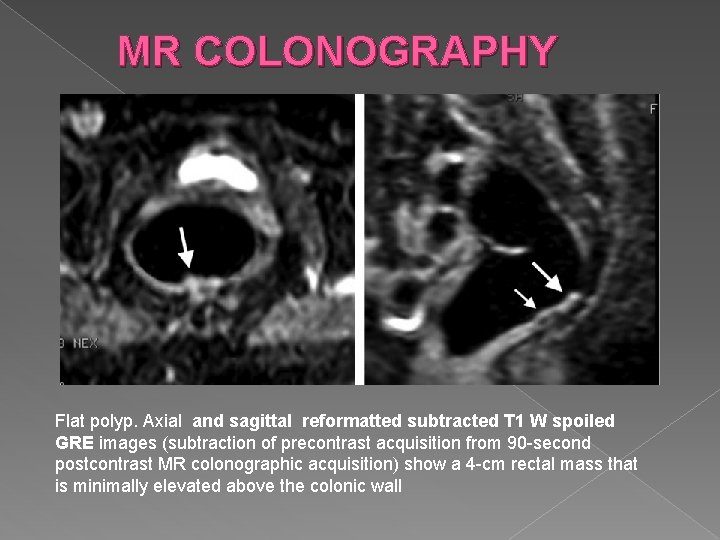
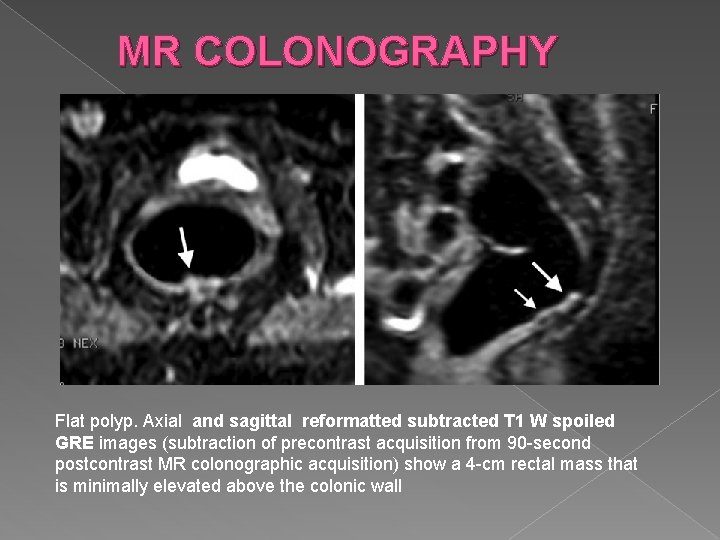
MR COLONOGRAPHY Flat polyp. Axial and sagittal reformatted subtracted T 1 W spoiled GRE images (subtraction of precontrast acquisition from 90 -second postcontrast MR colonographic acquisition) show a 4 -cm rectal mass that is minimally elevated above the colonic wall
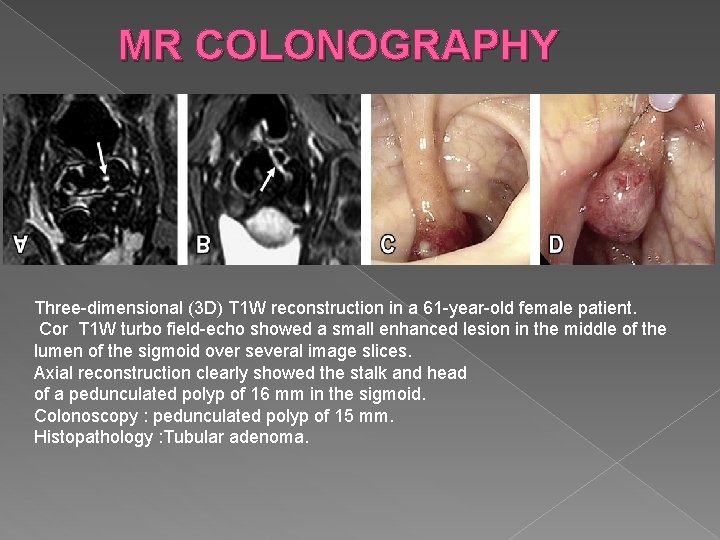
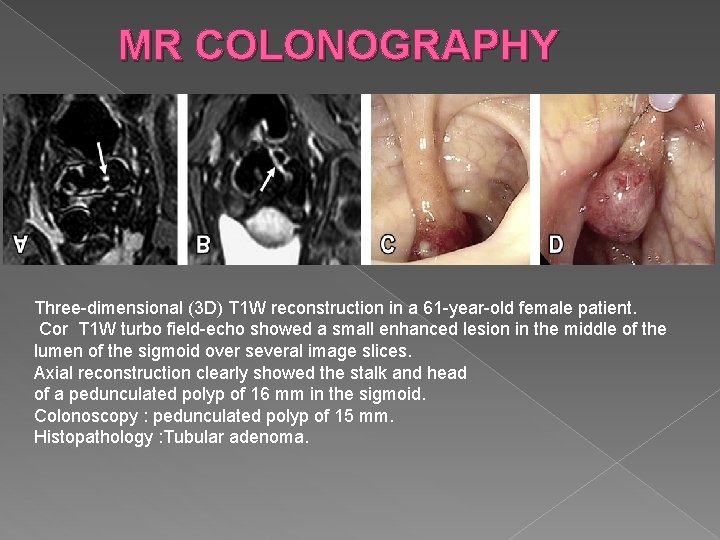
MR COLONOGRAPHY Three-dimensional (3 D) T 1 W reconstruction in a 61 -year-old female patient. Cor T 1 W turbo field-echo showed a small enhanced lesion in the middle of the lumen of the sigmoid over several image slices. Axial reconstruction clearly showed the stalk and head of a pedunculated polyp of 16 mm in the sigmoid. Colonoscopy : pedunculated polyp of 15 mm. Histopathology : Tubular adenoma.
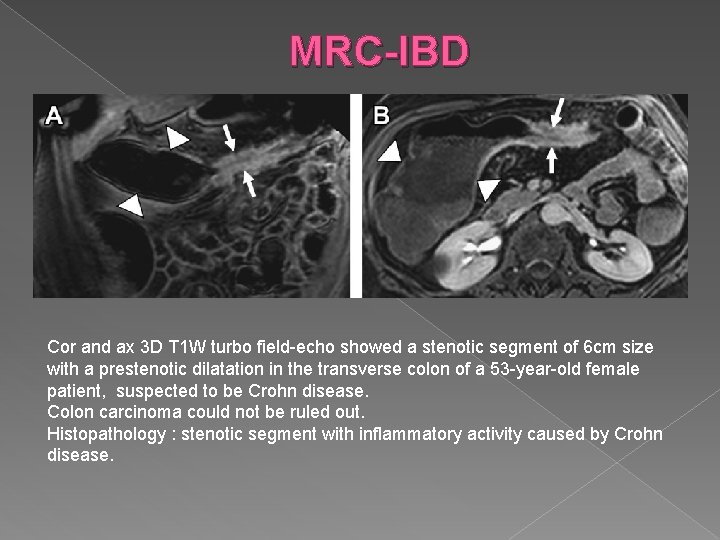
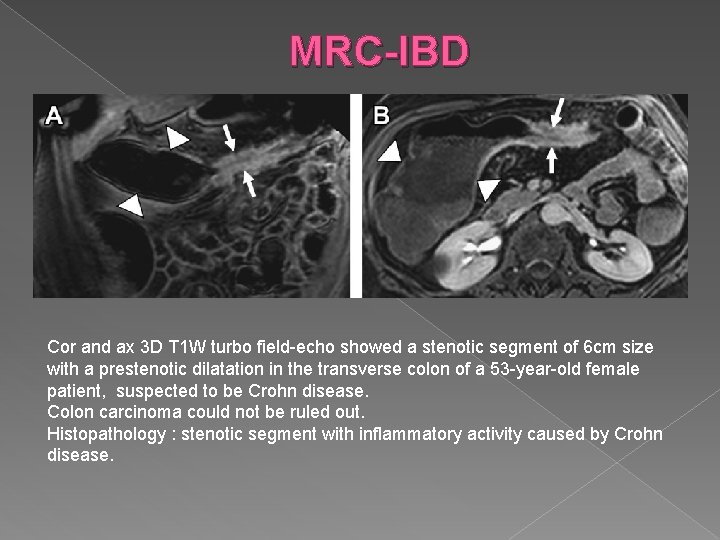
MRC-IBD Cor and ax 3 D T 1 W turbo field-echo showed a stenotic segment of 6 cm size with a prestenotic dilatation in the transverse colon of a 53 -year-old female patient, suspected to be Crohn disease. Colon carcinoma could not be ruled out. Histopathology : stenotic segment with inflammatory activity caused by Crohn disease.
MR COLONOGRAPHY While a significant difference was not found between coronal true FISP and coronal T 1 postcontrast sequences in terms of lesion detection sensitivity, coronal T 1 pre-contrast analysis sensitivity was lower than other sequences. � Extracolonic findings are also detected. Carrying prognostic value for the patient (37%) Findings (63%) have no prognostic values. �
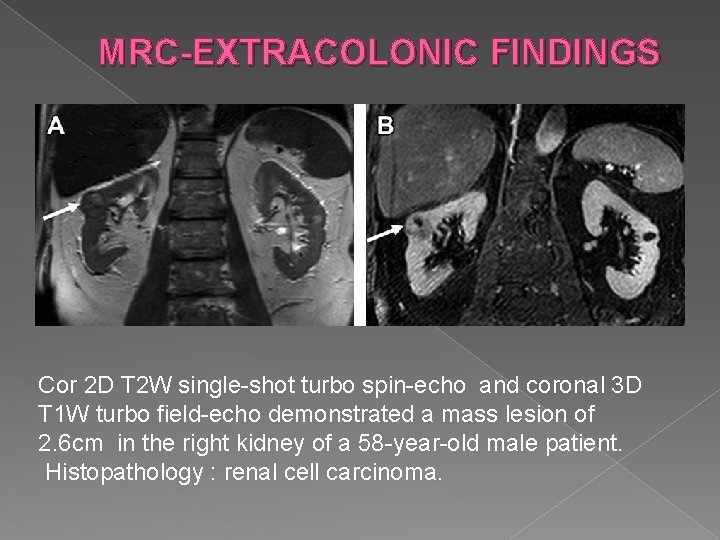
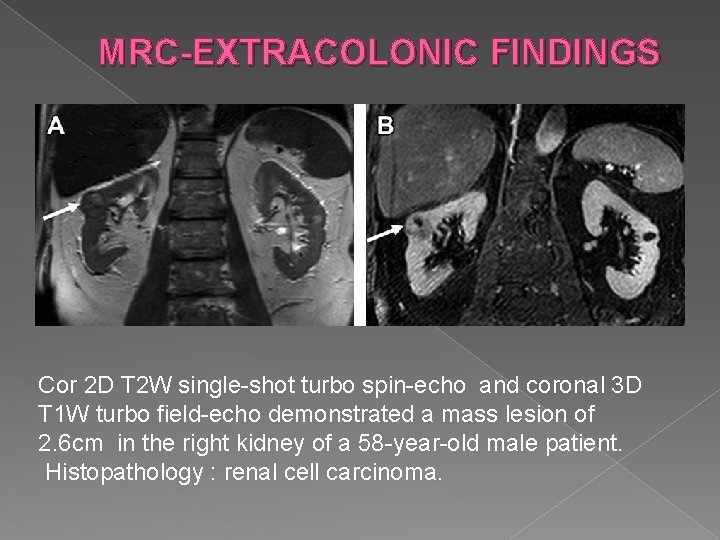
MRC-EXTRACOLONIC FINDINGS Cor 2 D T 2 W single-shot turbo spin-echo and coronal 3 D T 1 W turbo field-echo demonstrated a mass lesion of 2. 6 cm in the right kidney of a 58 -year-old male patient. Histopathology : renal cell carcinoma.
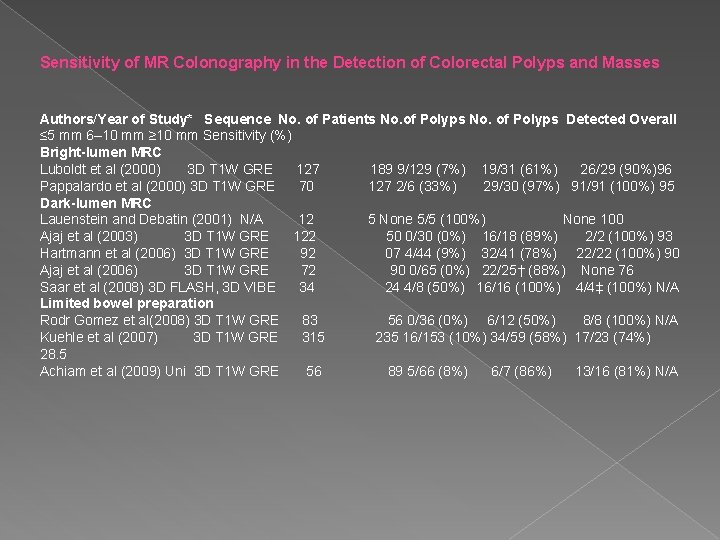
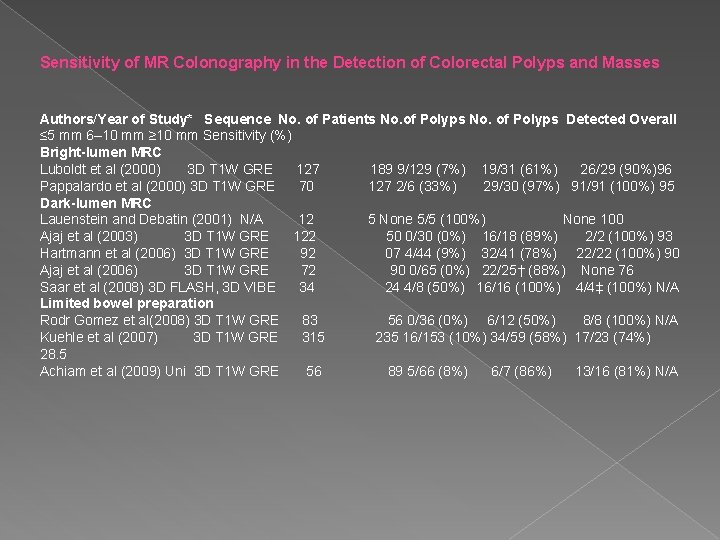
Sensitivity of MR Colonography in the Detection of Colorectal Polyps and Masses Authors/Year of Study* Sequence No. of Patients No. of Polyps Detected Overall ≤ 5 mm 6– 10 mm ≥ 10 mm Sensitivity (%) Bright-lumen MRC Luboldt et al (2000) 3 D T 1 W GRE 127 189 9/129 (7%) 19/31 (61%) 26/29 (90%)96 Pappalardo et al (2000) 3 D T 1 W GRE 70 127 2/6 (33%) 29/30 (97%) 91/91 (100%) 95 Dark-lumen MRC Lauenstein and Debatin (2001) N/A 12 5 None 5/5 (100%) None 100 Ajaj et al (2003) 3 D T 1 W GRE 122 50 0/30 (0%) 16/18 (89%) 2/2 (100%) 93 Hartmann et al (2006) 3 D T 1 W GRE 92 07 4/44 (9%) 32/41 (78%) 22/22 (100%) 90 Ajaj et al (2006) 3 D T 1 W GRE 72 90 0/65 (0%) 22/25† (88%) None 76 Saar et al (2008) 3 D FLASH, 3 D VIBE 34 24 4/8 (50%) 16/16 (100%) 4/4‡ (100%) N/A Limited bowel preparation Rodr Gomez et al(2008) 3 D T 1 W GRE 83 56 0/36 (0%) 6/12 (50%) 8/8 (100%) N/A Kuehle et al (2007) 3 D T 1 W GRE 315 235 16/153 (10%) 34/59 (58%) 17/23 (74%) 28. 5 Achiam et al (2009) Uni 3 D T 1 W GRE 56 89 5/66 (8%) 6/7 (86%) 13/16 (81%) N/A
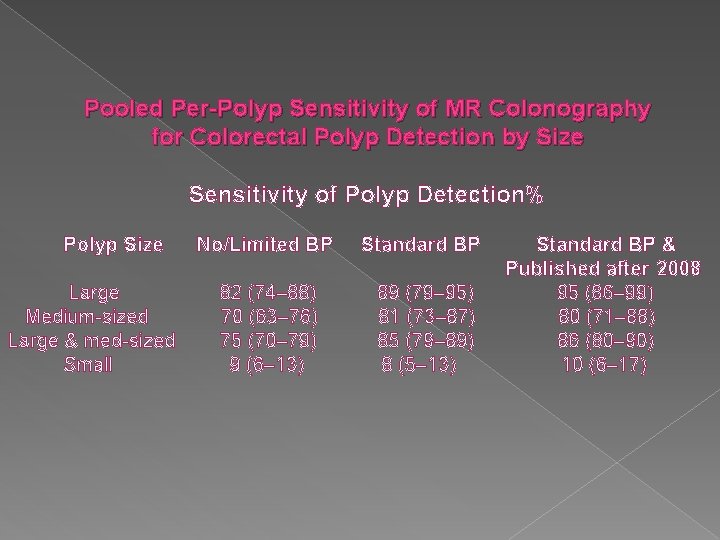
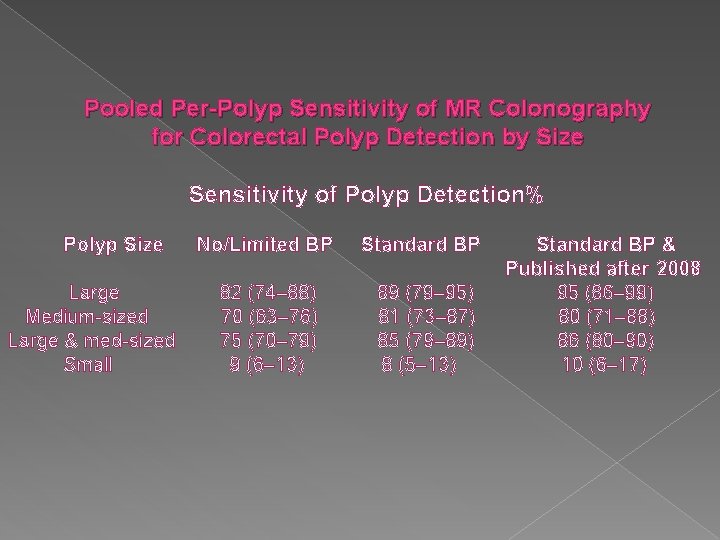
Pooled Per-Polyp Sensitivity of MR Colonography for Colorectal Polyp Detection by Size Sensitivity of Polyp Detection% Polyp Size Large Medium-sized Large & med-sized Small No/Limited BP Standard BP 82 (74– 88) 70 (63– 76) 75 (70– 79) 9 (6– 13) 89 (79– 95) 81 (73– 87) 85 (79– 89) 8 (5– 13) Standard BP & Published after 2008 95 (86– 99) 80 (71– 88) 86 (80– 90) 10 (6– 17)
MR COLONOGRAPHY � � � Sensitivity for the detection of CRC was 100%. Significant heterogeneity was found for overall per patient sensitivity and specificity. For polyps with a size of 10 mm or larger, per patient sensitivity and specificity estimates were 88% (95% CI 63– 97%; I 2=37%) and 99% (95% CI 95– 100%; I 2=60%). On a per polyp basis, polyps of 10 mm or larger were detected with a sensitivity of 84% (95% CI 66– 94%; I 2=51%). The data were too heterogeneous for polyps smaller than 6 mm (0 -10%) and 6– 9 mm(50 -80%). Conclusion: MR-colonography can accurately detect colorectal polyps more than 10 mm in size
Pooled Sensitivity of MR Colonography Compared With CT Colonography MR colonography and CT colonography with 16 -slice or 64 -slice scanners have equal sensitivity for the detection of CRC, as well as for the detection of large and medium sized polyps; however, MR colonography does not carry the associated risks of ionizing radiation. � MR colonography and CT colonography with 16 -slice or 64 -slice scanners can reliably detect most CRCs and large colorectal polyps; however, about 20% of medium-sized colorectal polyps will be missed by both techniques. � None of the techniques can reliably detect small polyps and MR colonography has a much lower sensitivity for the detection of small polyps compared with CT colonography. �
MR COLONOGRAPHY With the integration of 3. 0 -T MR colonography, parallel imaging (an evolving data acquisition and reconstruction technique that makes use of coil arrays to encode and detect multiple data points simultaneously), � Fecal tagging (based on altering the signal intensity of feces by adding contrast material to patients’ meals in the days prior to MRC) � Fecal cracking e administration of stool softeners, both orally and rectally, which leads to hydration of stool and decrease in the signal intensity of stool in T 1 W imaging) � Nanoparticle-based MRC (an experimental method using solid lipid nanoparticles (SLNs) synthesized with loading gadolinium-DTPA to construct Gd-SLNs as an MR T 1 contrast agent) methods into research and clinical settings, MRC gives us the hope of becoming a method that has higher detection ratios and easier clinical use. �
MR COLONOGRAPHY In conclusion, MRC is a good alternative to other colorectal cancer screening methods: It is non-invasive, Has high sensitivity in colorectal lesions measuring 1 cm and above Enables assessment of extracolonic findings and Does not include ionizing radiation. � Sensitivity may be increased by developing methods, like providing a good colonic cleaning and distention and reducing respiratory artifacts through good breathholding. � Future investigations by developing large-scale studies will likely lead to wider acceptance of this method to detect colonic pathologies, including perhaps their use in colon cancer screening programs. �

Thank you for your attention !
 Colorectal cancer drug trial
Colorectal cancer drug trial Colorectal cancer
Colorectal cancer Amsterdam criteria
Amsterdam criteria Ann lyons colorectal surgeon
Ann lyons colorectal surgeon Patho
Patho Ioanna tzoulaki
Ioanna tzoulaki 180-90-64
180-90-64 Ioanna stais
Ioanna stais Adductomics
Adductomics Ioanna miliou
Ioanna miliou Ioanna tzialla
Ioanna tzialla Chapter 24 the immune and lymphatic systems and cancer
Chapter 24 the immune and lymphatic systems and cancer The lymphatic capillaries are
The lymphatic capillaries are National breast and cervical cancer early detection program
National breast and cervical cancer early detection program National breast and cervical cancer early detection program
National breast and cervical cancer early detection program Breast structure
Breast structure Risk factors of head and neck cancer
Risk factors of head and neck cancer Shaukat khanum pharmacy
Shaukat khanum pharmacy Tropic of cancer and capricorn
Tropic of cancer and capricorn What are the tropics of cancer and capricorn
What are the tropics of cancer and capricorn Suspected cancer recognition and referral
Suspected cancer recognition and referral Suspected cancer recognition and referral
Suspected cancer recognition and referral Personal care products and cancer risk
Personal care products and cancer risk Welding causes cancer
Welding causes cancer Tnm staging lung cancer
Tnm staging lung cancer The soldier poem meaning
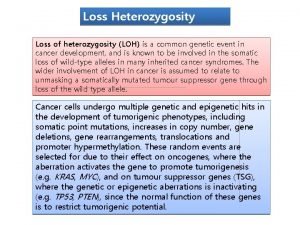
The soldier poem meaning The genetic basis of cancer
The genetic basis of cancer Thames valley cancer network
Thames valley cancer network Indoemtacina
Indoemtacina Cerebral salt wasting
Cerebral salt wasting Clasificacion molecular cancer de endometrio
Clasificacion molecular cancer de endometrio Signo tauro y piscis
Signo tauro y piscis High sierra ahec
High sierra ahec Ca 125
Ca 125 Cdk breast cancer
Cdk breast cancer Breast ca tnm staging
Breast ca tnm staging Two hit hypothesis of cancer
Two hit hypothesis of cancer Glottic cancer staging
Glottic cancer staging T2g3 bladder cancer
T2g3 bladder cancer Luminal a breast cancer
Luminal a breast cancer May cause cancer pictogram
May cause cancer pictogram R
R Borrmann classification of gastric cancer
Borrmann classification of gastric cancer