Monitoring Practitioners for Performance Quality Monitoring for Effectiveness




- Slides: 35
Monitoring Practitioners for Performance & Quality
Monitoring for Effectiveness • 1. Medical staff & organization • 2. Peer review • 3. Credentialing

Medical Staff • • • Legislative mandate Structure & organization Medical staff membership Medical Board & committees Medical Departments Joint Conference Committee
Responsibility to Institution • Develop, monitor and reinforce standards of care and professional behavior • Advise institution on care practices & requirements • Refer and admit patients • Support reputation & good will of institution • Review and recommend staff to the hospital
Medical Staff Peer Review • • Patient care evaluation review Surgical case review Drug usage review Blood usage review Medical record document review Utilization review Risk review
Credentialing • • • Issues involved in credentialing Hospital vs. managed care Effective credentialing process Physician profiling Economic credentialing
Who Performs Credentialing? • • Hospitals HMO’s PPO’s PHO’s IPA’s Other Health Plans Ambulatory Care Facilities
Who Credentials • The responsibility for admitting practitioners to the organized medical staff lies with the governing body, as defined by state statutes
Who Is Credentialed? • Medical Staff • Independent practitioners – – – Dentists Psychologists Nurse Midwives Physician Assistants Podiatrists Chiropractors
Why Do We Credential? • Legal issues • Quality issues • Laws, standards, regulations Misrepresenting/falsifying credentials

Legal Issues • Increased litigation due to: • Pressures on health care organizations and practitioners by patients seeking redress of grievance in court • Patients demanding providers monitor practices • Purchasers paying less while scrutinizing more

Darling Case - 1965 Landmark Case • Hospitals have a duty to oversee care provided by physicians and can be liable for patient injury caused by incompetent practitioners • Governing body is ultimately liable for care provided in the hospital

Liability • • Negligent Credentialing --Patient as the Plaintiff Unfair Credentialing --Physician as the Plaintiff
Negligent Credentialing • Negligent selection/retention of practitioners • Organization failed to protect patients from unqualified or incompetent practitioners • Organization falsely represents practitioner’s qualifications and competence
Doctrine of Corporate Liability • Recognizes duties owed to patient – Selection/retention of qualified, competent practitioners – Development and enforcement of policies and procedures to safeguard quality of care – Ongoing oversight and assessment of care
Unfair Credentialing • Adverse credentials decision – Admission to staff – Privileges limited, terminated, restricted • Nature of claim – Loss of income/ability to earn living (antitrust) – Denial of right to due process (defamation) – Loss of reputation From unjustified decision • Violation of due process – Intentional denial of rights granted by statutes and bylaws Decisions not data driven or based on merit – Not informed of rationale – Not afforded opportunity to provide defense
Liability in Managed Care • Wrongful denial of access to needed medical care • Quality of care or provider malpractice • Claims and theories of liability will increase with managed care
Quality of Care Claims • Organization may be held: – Directly liable for quality of care provided – Vicariously liable for care provided by Plan’s health care professionals
Negligent Credentialing • Recent cases demonstrate HMOs have the duty to conduct reasonable investigations of physicians available to enrollees • Accepting physician’s applications without investigation does not meet this duty
Breach of Contract • HMOs and other managed care plans have failed to provide qualified medical providers as required by contract • Quality of coverage, not the failure to provide coverage
Misrepresentation • Health Plan misrepresents its quality of care while enrollees rely on the representations • Areas of claims that are likely to increase with competition and marketing:
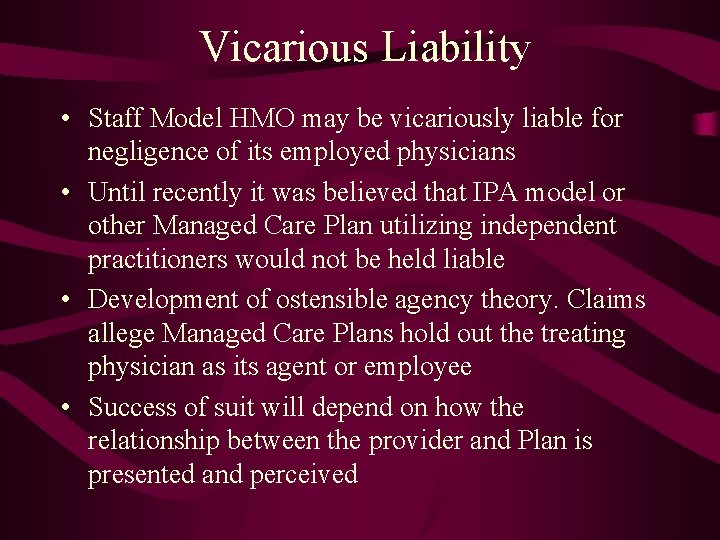
Vicarious Liability • Staff Model HMO may be vicariously liable for negligence of its employed physicians • Until recently it was believed that IPA model or other Managed Care Plan utilizing independent practitioners would not be held liable • Development of ostensible agency theory. Claims allege Managed Care Plans hold out the treating physician as its agent or employee • Success of suit will depend on how the relationship between the provider and Plan is presented and perceived
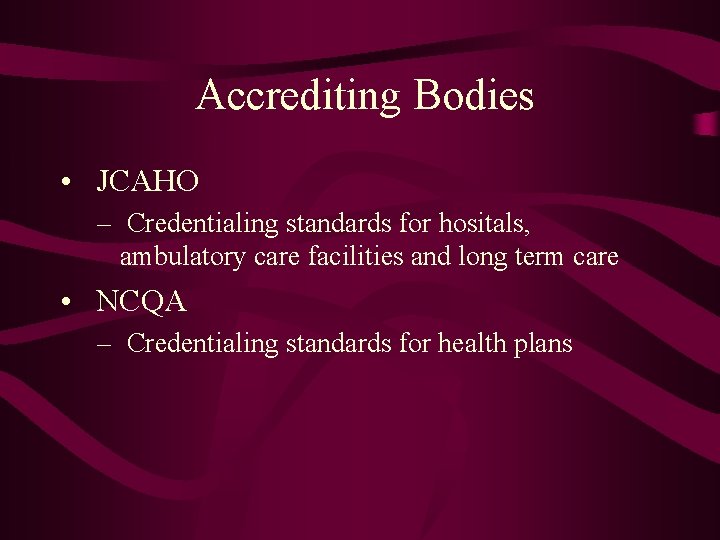
Accrediting Bodies • JCAHO – Credentialing standards for hositals, ambulatory care facilities and long term care • NCQA – Credentialing standards for health plans
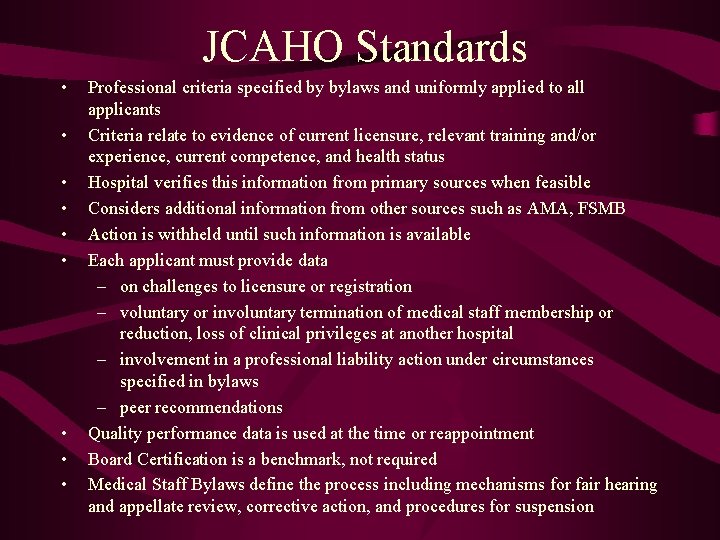
JCAHO Standards • • • Professional criteria specified by bylaws and uniformly applied to all applicants Criteria relate to evidence of current licensure, relevant training and/or experience, current competence, and health status Hospital verifies this information from primary sources when feasible Considers additional information from other sources such as AMA, FSMB Action is withheld until such information is available Each applicant must provide data – on challenges to licensure or registration – voluntary or involuntary termination of medical staff membership or reduction, loss of clinical privileges at another hospital – involvement in a professional liability action under circumstances specified in bylaws – peer recommendations Quality performance data is used at the time or reappointment Board Certification is a benchmark, not required Medical Staff Bylaws define the process including mechanisms for fair hearing and appellate review, corrective action, and procedures for suspension
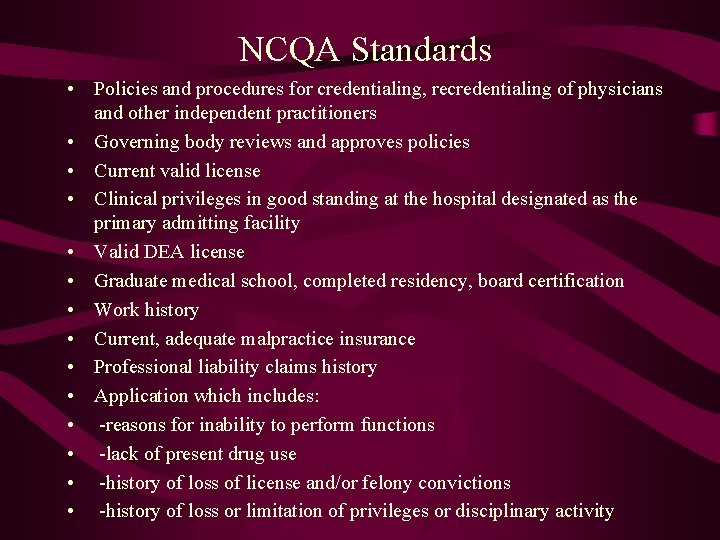
NCQA Standards • Policies and procedures for credentialing, recredentialing of physicians and other independent practitioners • Governing body reviews and approves policies • Current valid license • Clinical privileges in good standing at the hospital designated as the primary admitting facility • Valid DEA license • Graduate medical school, completed residency, board certification • Work history • Current, adequate malpractice insurance • Professional liability claims history • Application which includes: • -reasons for inability to perform functions • -lack of present drug use • -history of loss of license and/or felony convictions • -history of loss or limitation of privileges or disciplinary activity
NCQA Standards- cont. • Query- NPDB, Licensure authority • Review for medicare and medicaid sanctions • Site visit to primary care practitioner’s office and offices of obstetricians/gynecologists and other high volume specialists • Policies and procedures for review of initial quality assessment of health delivery organizations with which it intends to contract • Process for reappointment which includes a review of data • Data – Member complaints – Results of quality reviews – Utilization management – Member satisfaction surveys • Delegation of credentialing activities – Evidence of oversight – Written description of delegated activities – Delegates accountability for activities
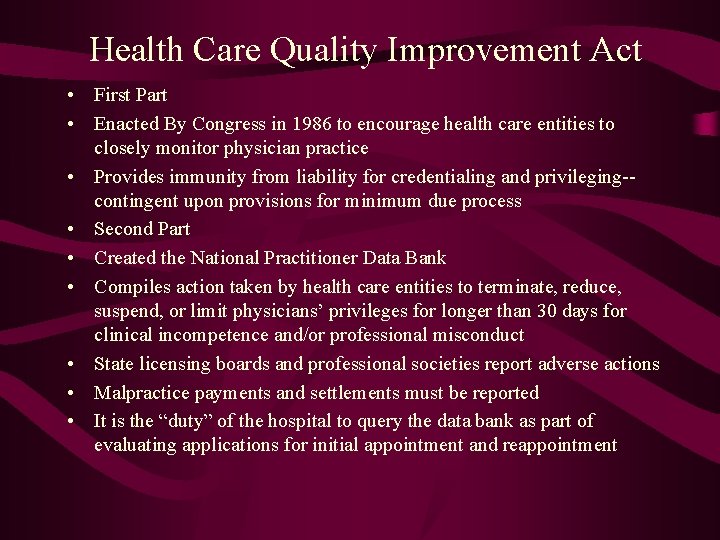
Health Care Quality Improvement Act • First Part • Enacted By Congress in 1986 to encourage health care entities to closely monitor physician practice • Provides immunity from liability for credentialing and privileging-contingent upon provisions for minimum due process • Second Part • Created the National Practitioner Data Bank • Compiles action taken by health care entities to terminate, reduce, suspend, or limit physicians’ privileges for longer than 30 days for clinical incompetence and/or professional misconduct • State licensing boards and professional societies report adverse actions • Malpractice payments and settlements must be reported • It is the “duty” of the hospital to query the data bank as part of evaluating applications for initial appointment and reappointment
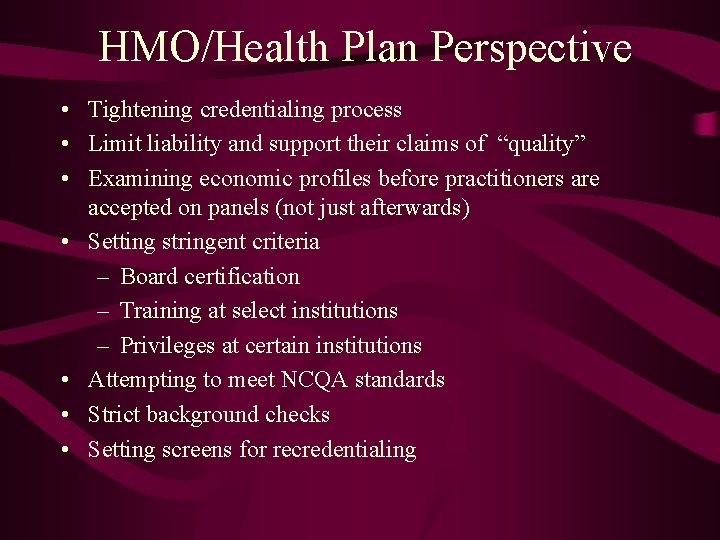
HMO/Health Plan Perspective • Tightening credentialing process • Limit liability and support their claims of “quality” • Examining economic profiles before practitioners are accepted on panels (not just afterwards) • Setting stringent criteria – Board certification – Training at select institutions – Privileges at certain institutions • Attempting to meet NCQA standards • Strict background checks • Setting screens for recredentialing
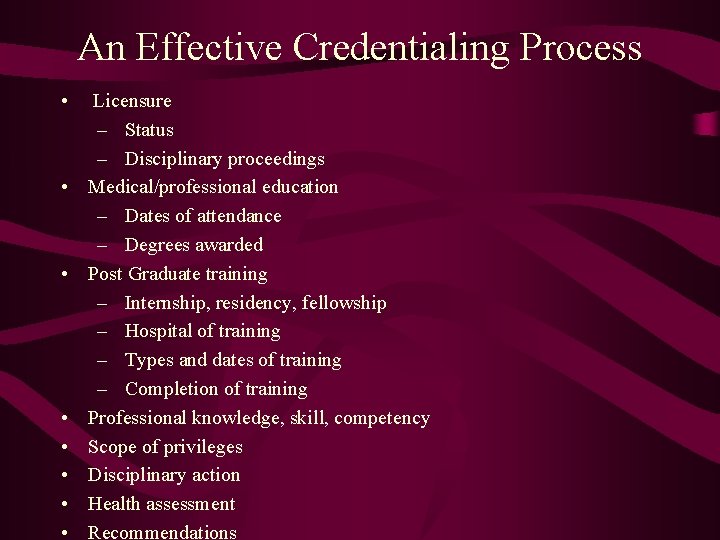
An Effective Credentialing Process • • Licensure – Status – Disciplinary proceedings Medical/professional education – Dates of attendance – Degrees awarded Post Graduate training – Internship, residency, fellowship – Hospital of training – Types and dates of training – Completion of training Professional knowledge, skill, competency Scope of privileges Disciplinary action Health assessment Recommendations
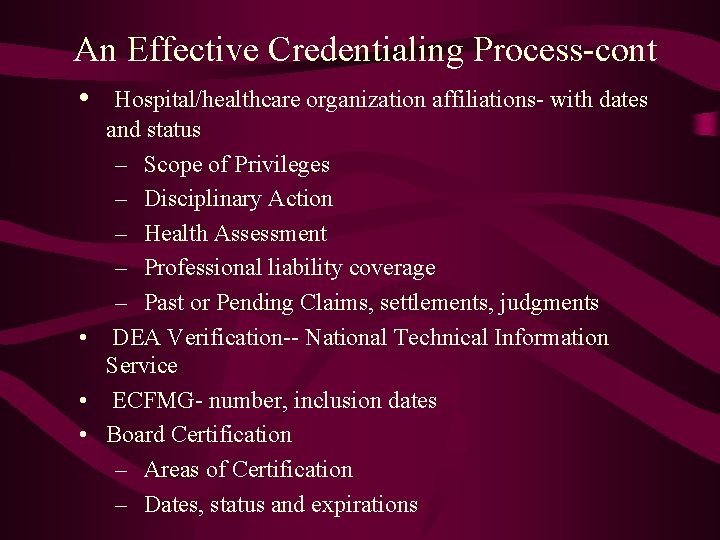
An Effective Credentialing Process-cont • Hospital/healthcare organization affiliations- with dates and status – Scope of Privileges – Disciplinary Action – Health Assessment – Professional liability coverage – Past or Pending Claims, settlements, judgments • DEA Verification-- National Technical Information Service • ECFMG- number, inclusion dates • Board Certification – Areas of Certification – Dates, status and expirations
An Effective Credentialing Process-cont • • • Federation of State Medical Boards- Disciplinary action search Faculty appointment – Dates affiliated and current status – Disciplinary actions – Health status – Recommendations Professional peer references – Relationship of reference – Professional knowledge/skills/attitude – Competency – Disciplinary Action – Health status AMA Profile National Practitioner Data Bank Entries Interview with applicants
An Effective Credentialing Process-cont • • • Site visit/chart review Gaps in history Frequent changes from state to state Changes in specialty Contradictory information Frequent changes in malpractice carrier Application that gathers all necessary information – Hospital requirements – Managed care organization requirements Setting screens Reappointment process comparable to initial appointment
Economic Credentialing • Includes: – Setting financial and economic criteria for admission to medical staff or for specific privileges – Use of financial and utilization data in whole or in part to make decisions about reappointment and continuation of specific privileges – Granting exclusive contract to provide clinical services
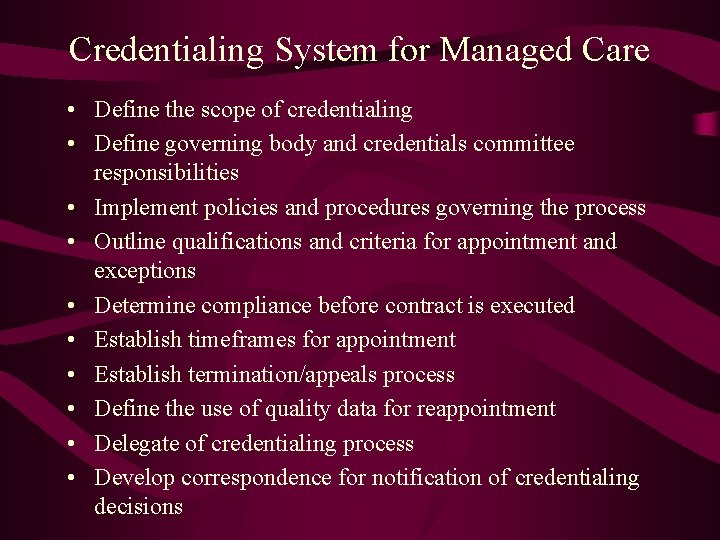
Credentialing System for Managed Care • Define the scope of credentialing • Define governing body and credentials committee responsibilities • Implement policies and procedures governing the process • Outline qualifications and criteria for appointment and exceptions • Determine compliance before contract is executed • Establish timeframes for appointment • Establish termination/appeals process • Define the use of quality data for reappointment • Delegate of credentialing process • Develop correspondence for notification of credentialing decisions
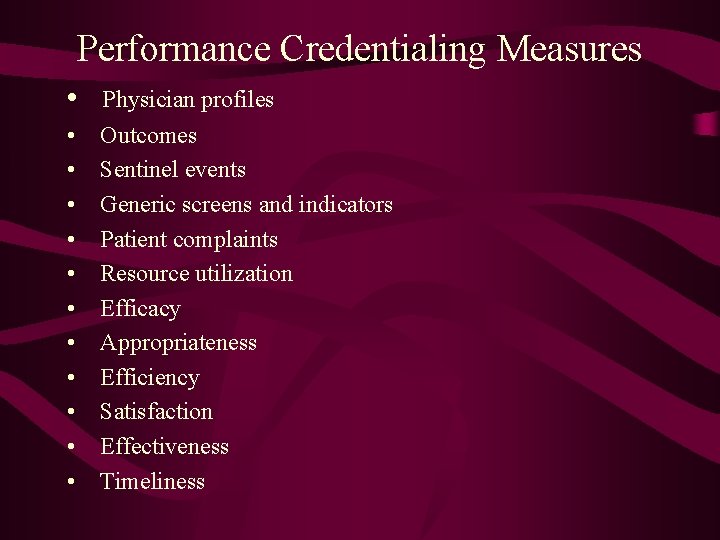
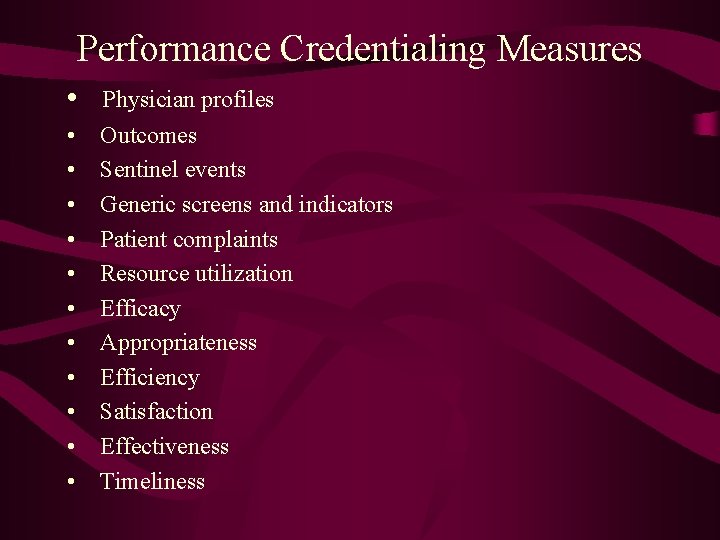
Performance Credentialing Measures • Physician profiles • • • Outcomes Sentinel events Generic screens and indicators Patient complaints Resource utilization Efficacy Appropriateness Efficiency Satisfaction Effectiveness Timeliness
 Stronge leader effectiveness performance evaluation model
Stronge leader effectiveness performance evaluation model National association of patent practitioners
National association of patent practitioners Assurance framework template
Assurance framework template Theatre practitioner meaning
Theatre practitioner meaning Grade r progress report
Grade r progress report Software engineering a practitioners approach
Software engineering a practitioners approach Association of independent insolvency practitioners
Association of independent insolvency practitioners Kimber dita for practitioners volume 1 (epub|pdf|mobi)
Kimber dita for practitioners volume 1 (epub|pdf|mobi) Tax practitioners association indore
Tax practitioners association indore Curbside management practitioners guide
Curbside management practitioners guide Unregistered health practitioners
Unregistered health practitioners Social business practitioners
Social business practitioners Australian college of nurse practitioners
Australian college of nurse practitioners Perform quality assurance
Perform quality assurance Pmp quality management
Pmp quality management Pmbok quality assurance vs quality control
Pmbok quality assurance vs quality control Ana quality assurance model
Ana quality assurance model Quality improvement vs quality assurance
Quality improvement vs quality assurance Quality assurance concepts
Quality assurance concepts Quality gurus
Quality gurus Crosby quality is free
Crosby quality is free Old quality vs new quality
Old quality vs new quality Quality monitoring scorecard
Quality monitoring scorecard Quality monitoring scorecard
Quality monitoring scorecard National water quality monitoring conference
National water quality monitoring conference National water quality monitoring council
National water quality monitoring council Data quality monitoring framework
Data quality monitoring framework Wigos data quality monitoring system
Wigos data quality monitoring system Real time data quality monitoring
Real time data quality monitoring Permanent power quality monitoring equipment
Permanent power quality monitoring equipment Nwqmc conference
Nwqmc conference National water quality monitoring conference
National water quality monitoring conference Highmarl true performance quality measures
Highmarl true performance quality measures High quality performance
High quality performance York university moodle
York university moodle Performance monitoring and coaching form
Performance monitoring and coaching form