QUALITY SCORECARD Monitoring the quality of your healthcare







- Slides: 39
QUALITY SCORECARD Monitoring the quality of your healthcare provided by Derbyshire Community Health Services (A Part of Derbyshire County PCT) in 2008/09 Click here to advance
Navigating this document Each slide contains navigation buttons in the bottom left corner: Click to go to the next page Click to go back to the previous page Click End show to exit the document Click highlighted text to go to the glossary page Click for more information on this indicator – this is optional Click to go back to the last page you viewed End show
What is this quality scorecard? Derbyshire County PCT (the PCT) is responsible for commissioning services that meet the needs of its population and provide value for money. One element of value is the quality of services it commissions. In order to assess this, each provider is required to provide the PCT with evidence that the services it provides are high quality. The PCT does this by setting and monitoring quality indicators, designed to look in more detail at areas of national or local importance (e. g. prevention of infection) and by covering a range of different service areas. The indicators are grouped into 4 domains: – Equitable services (designed to meet health needs at the right time and place) – Service user involvement (includes patient experience) – Safety and clinical effectiveness (safe clinical care based on best practice evidence) – Outcomes (what were the consequences of the care provided) End show
How are the scores calculated? Performance against the indicators was scored as follows: – Green – the provider can demonstrate that the indicator is being met with acceptable evidence. – Amber - the provider is working towards the indicator and is on track to meet it. – Red – the provider has not started working towards the indicator. In all instances, scoring decisions have been made by a Quality Management Group with joint representation from commissioner and provider and including a patient representative. End show
Important note on judging the scores Please read the following - do not skip forward yet! It is important to bear in mind that the expanding focus on quality measurement is a relatively new initiative in the NHS. Some aspects of performance have been measured nationally, for example waiting times for appointments, patient satisfaction with services etc. , but many areas have not been measured in any detailed or systematic way before, reflecting the need for quality to be promoted in all health outcome measurement tools. Formal evidence of quality has therefore been limited with systems to gather, collate and present evidence often scarcely resourced. In addition the Commissioner’s capability to identify and articulate useful measures of quality also required development. It should also be recognised that people, systems and processes required to manage quality measurement were also developing during this year and that much has been learnt along the way. Local evidence to provide assurance of meeting the quality indicators was, therefore, not always clear / available. This should not be interpreted as the service provider or the service itself being of a standard less than optimum but more as a result of a learning process. When judging the scorecard summaries it is therefore imperative to refer to the commentary for context to understand the baseline position and opportunity this presents for improvement rather than as a basis for dissatisfaction. The following pages provide summaries and more detail as to how Derbyshire Community Health Services scored. End show
Who to contact for more information For more information about anything in this report please contact either Chrissie Craske or Pete Pridmore as detailed below. Chrissie Craske, Head of Patient Experience and Quality, Directorate of Quality and Integrated Governance, Derbyshire Community Health Services, Toll Bar House, Derby Road, Ilkeston, Derbyshire, DE 7 5 FH chrissie. craske@derbyshirecountypct. nhs. uk Phone: Office 0115 931 6176 Mobile 07879 040743 Pete Pridmore Head of Clinical Quality – Commissioning, Clinical Quality Directorate, Derbyshire County PCT, St Mary's Court, Chesterfield S 41 7 TD pete. pridmore@derbyshirecountypct. nhs. uk Phone: Main Reception 01246 514100 Office 01246 514060 Mobile 07920 750804 End show
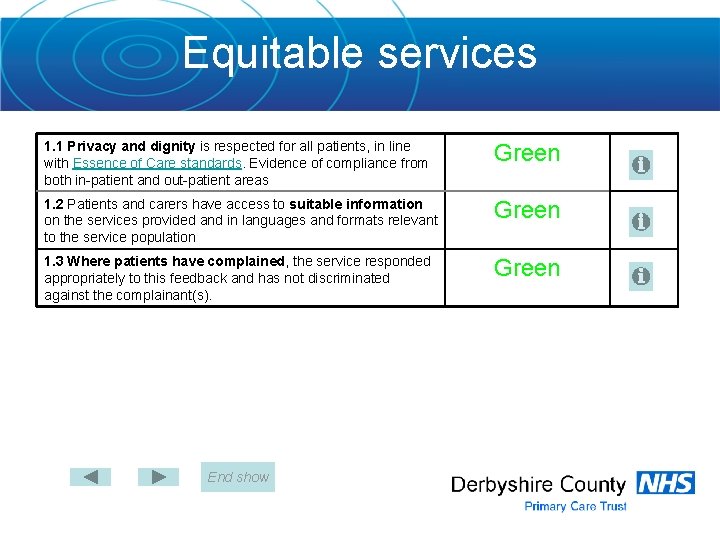
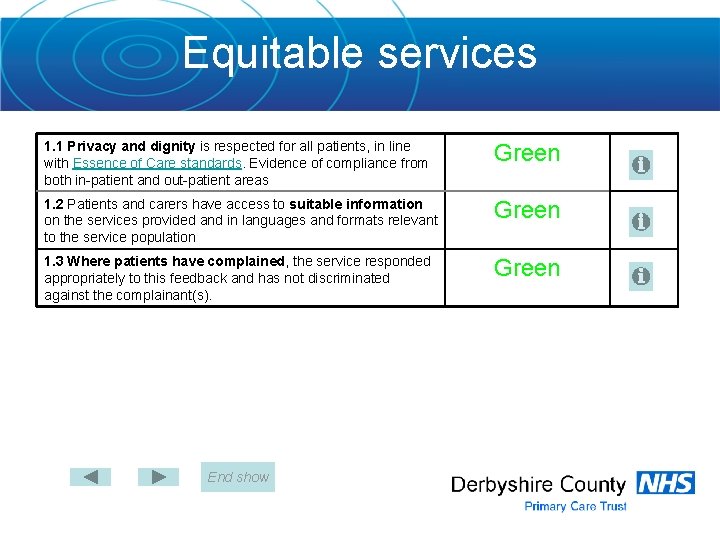
Equitable services 1. 1 Privacy and dignity is respected for all patients, in line with Essence of Care standards. Evidence of compliance from both in-patient and out-patient areas Green 1. 2 Patients and carers have access to suitable information on the services provided and in languages and formats relevant to the service population Green 1. 3 Where patients have complained, the service responded appropriately to this feedback and has not discriminated against the complainant(s). Green End show

Service user involvement 2. 1 Service user involvement: The provider will carry out patient surveys and/or focus groups/interviews to elicit feedback and opinions on services in order to effect change. Green 2. 2 Cleanliness of premises: The provider will carry out a survey to allow patients to feed back comments and opinions, and will act upon issues as appropriate. Green 2. 3 Consent: The provider must seek proper consent from all patients that takes into account Department of Health consent guidance and the Mental Capacity Act 2005. Amber End show

Clinical & cost-effectiveness 3. 1 All staff involved in delivering clinical care and treatment receive appropriate clinical supervision, taking into account national guidance from relevant professional bodies (70% of staff active participation). Amber 3. 2 Pressure ulcers: Clinical audit is undertaken to ensure best practice is followed or if not that action is taken to correct this. Specific audit of pressure ulcer management will be undertaken, auditing against NICE clinical guideline no. 29 Green 3. 3 Health care records: Content is audited for completeness (e. g. dated, timed, signed, allergies noted etc. ) on a regular basis and improvement demonstrated. Green End show

Clinical & cost-effectiveness 3. 4 Fractured neck of femur: For inpatients, evidence of Nutritional risk scoring must be carried out and action adhered to in 100% of patients Nutritional support in rehabilitation of patients with fractured neck of femur (100% of patients) Pressure ulcer prevention in patients with fractured neck of femur. (100% of patients) See note for more detail Falls assessment (100% of patients) 3. 5 Child protection Training on child protection is delivered to all staff and part of induction and mandatory training. End show Amber

Clinical & cost-effectiveness 3. 6 Children found to be overweight on height and weight measurement by PCT provided school nursing services will receive appropriate intervention (e. g. weight management in children and adolescents, Royal College of Paediatrics and National Obesity Forum) and will be signposted to appropriate services 3. 7 Healthcare-Associated infection 1: Appropriate action is taken to minimise the spread of healthcare associated infection. Glossary End show See note for more detail Green
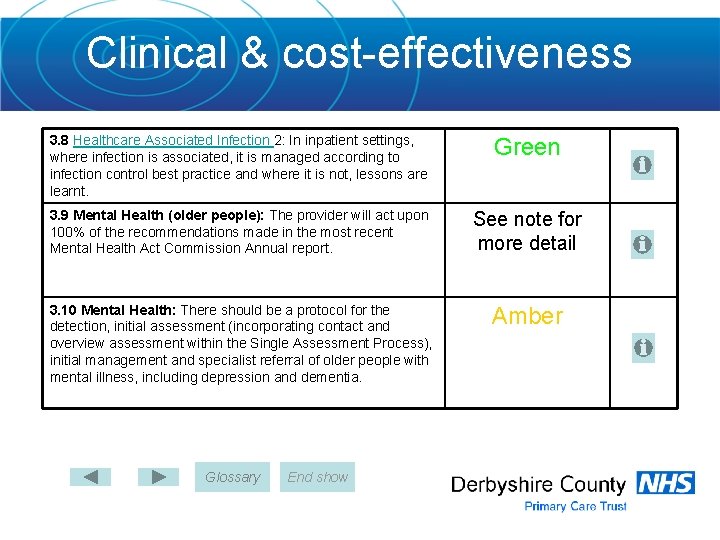
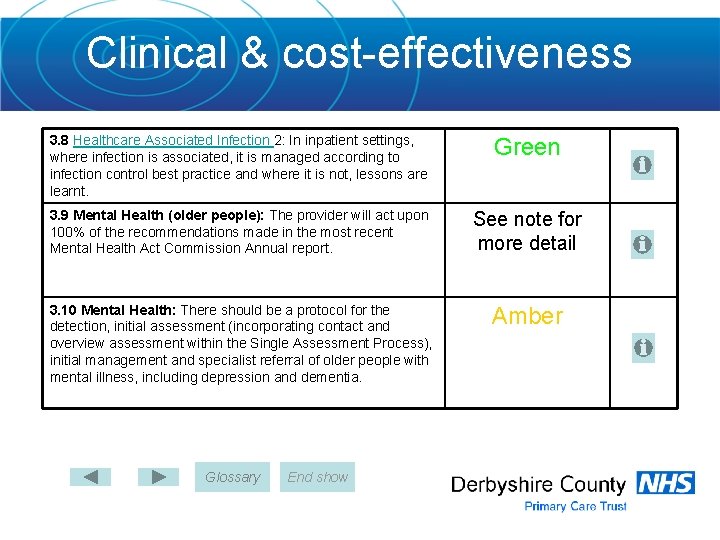
Clinical & cost-effectiveness 3. 8 Healthcare Associated Infection 2: In inpatient settings, where infection is associated, it is managed according to infection control best practice and where it is not, lessons are learnt. Green 3. 9 Mental Health (older people): The provider will act upon 100% of the recommendations made in the most recent Mental Health Act Commission Annual report. See note for more detail 3. 10 Mental Health: There should be a protocol for the detection, initial assessment (incorporating contact and overview assessment within the Single Assessment Process), initial management and specialist referral of older people with mental illness, including depression and dementia. Amber Glossary End show
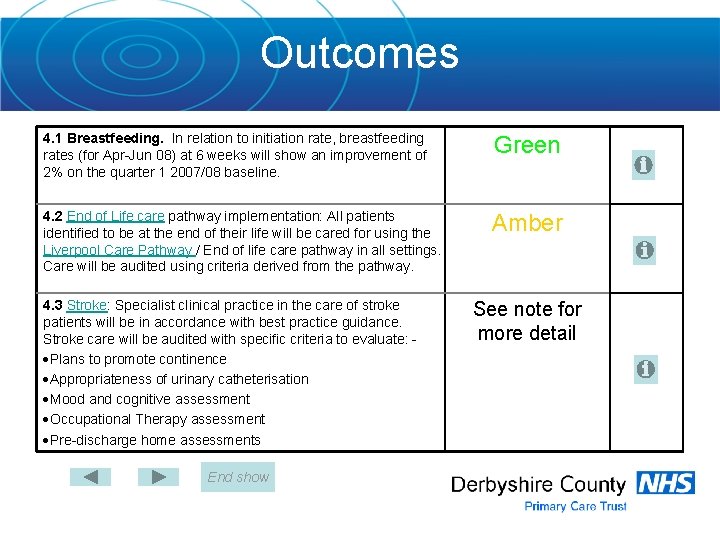
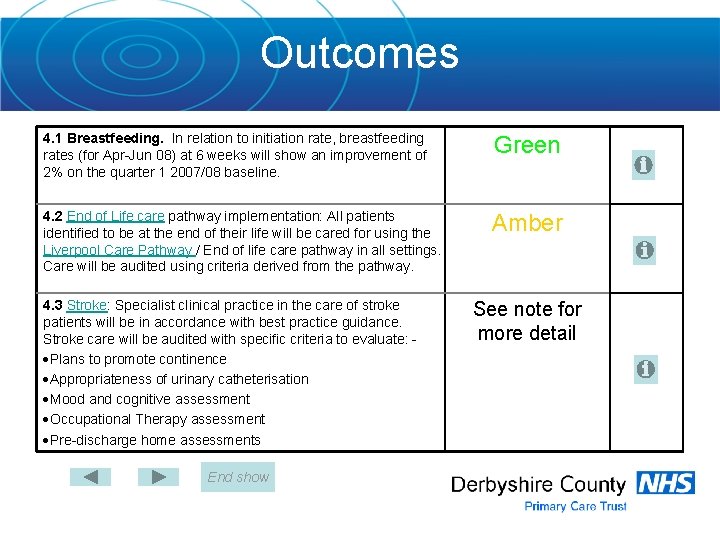
Outcomes 4. 1 Breastfeeding. In relation to initiation rate, breastfeeding rates (for Apr-Jun 08) at 6 weeks will show an improvement of 2% on the quarter 1 2007/08 baseline. Green 4. 2 End of Life care pathway implementation: All patients identified to be at the end of their life will be cared for using the Liverpool Care Pathway / End of life care pathway in all settings. Care will be audited using criteria derived from the pathway. Amber 4. 3 Stroke: Specialist clinical practice in the care of stroke patients will be in accordance with best practice guidance. Stroke care will be audited with specific criteria to evaluate: Plans to promote continence Appropriateness of urinary catheterisation Mood and cognitive assessment Occupational Therapy assessment Pre-discharge home assessments End show See note for more detail

Outcomes 4. 4 Day-case surgery: patient-reported outcomes (PROMs) will be measured using condition-specific tools. Other measures of quality to be measured as appropriate. This will be done for: Hernia repair Cataract extraction Osteotomy and internal fixation Primary excision arthroplasty of joint Varicose vein procedures 4. 5 Chronic back pain: outcomes of physiotherapy chronic back pain clinics will be monitored using a patient-reported outcome measure SF-36 before and after treatment. End show Green See note for more detail
Conclusion On balance the scorecard illustrates a successful first year in which much learning and development have taken place both from a provider and commissioning perspective. Provider scores against the indicators have shown a positive bias towards achievement or being well on track to achieve. In some instances it has proven difficult to develop meaningful evidence to score the indicators and as a consequence both parties have agreed that a score would be meaningless. Lessons have been learnt and revisions have been made for 2009/10. End show
Privacy and dignity is respected for all patients, in line with Essence of Care standards Essence of Care (Eo. C) benchmarking is a framework developed by the Department of Health working in partnership with service user representatives. The benchmark for privacy and dignity defines the standards nationally for treating patients with privacy and dignity. The community hospitals in DCHS have completed selfassessments against the Eo. C standards on privacy and dignity and have implemented action plans to improve care. Each year a Patient Environment Action Team (PEAT) audits the environment for privacy and dignity. Evidence shows that patients are treated with privacy and dignity both in-patient and out-patient areas. This is considered by the PCT to be an important indicator, therefore it will carry forward into next year.
Provision of information on services • The PCT Board declared compliance with the core standard (C 16) for provision of information on services in 2008/09, which received positive support by the Local Involvement Network (LINk). Information is published on the PCT website and various written formats. • In 2009/10 DCHS will seek to provide evidence of service user involvement in the design of information for their use and where required produce information in accessible formats.
Complaints • Complaints offer an opportunity to correct an immediate problem and frequently provide constructive ideas for improving services, culture and attitudes. • DCHS provided the PCT with evidence of quarterly complaints monitoring and the intention to report lessons learnt form complaints at the Annual General Meeting, which is open to the public. • This is considered by the PCT to be an important indicator, therefore it will carry forward into next year.
Service User Involvement • Service user involvement in the design, planning and evaluation of services will assist DCHS to ensure that services are meeting the needs and reasonable demands of service users. • DCHS is an active member of the PCT Public and Patient Involvement Steering Group and reports regularly on initiatives to involve service users. It is an active partner in a major consultation on services in Buxton and surrounding area. • A number of clinical teams have developed plans for further engagement with service users.
Patients will be given the opportunity to feed back comments and opinions on the cleanliness of premises • • It is well recognised that keeping premises clean is of vital importance to the control of infection as well as to the comfort and reassurance that this affords to people who have to use them. Patients and public are rightly concerned that the healthcare premises they use are clean. The PCT has sought assurance that premises are regularly inspected for cleanliness and that public/patient representatives are involved in the inspection process. This is achieved through visits by the Patient Environment Action Team (PEAT) and published reports on the findings of their inspection. DCHS achieved high scores for cleanliness in the PEAT inspection. Further to this DCHS sought the views of patients through Patient Experience Tracker devices designed to collect on the spot views from patients using local NHS premises. The results of this tool show that high levels of patient satisfaction are reported consistently. In 2009/10 DCHS has planned to audit patient views. This is considered by the PCT to be an important indicator, therefore it will carry forward into next year.
Consent • In order to give informed consent to any treatment staff must make all reasonable efforts to ensure that the person is fully informed of what the treatment involves and the risks and benefits associated with it. This is an integral part of involving people in their care and enables a person to make an informed decision about whether to accept or reject a proposed treatment. Consent applies to all aspects of care, not just complex (e. g. surgical) procedures. • DCHS revised their consent policy in February 2009 and looked for evidence of consent whilst completing a clinical records audit. It was established in this that further development of the audit tool was required to enable consent to be properly audited. • This is considered by the PCT to be an important indicator, therefore it will carry forward into next year.
All staff involved in delivering clinical care and treatment receive appropriate clinical supervision Clinical supervision is time set aside by staff to seek support, to learn and to improve the quality of their practice. This time is spent with a clinical supervisor of their choice. It is distinct and separate from management supervision. • A system was devised to find out how many staff have received clinical supervision but much of the required data is missing. It is not therefore possible to present a reliable figure on the proportion of staff receiving clinical supervision. • A more robust data collection system is planned for 2009/10 therefore this indicator will be carried over.
Pressure ulcers • • Pressure ulcers - also known as pressure sores, or bed sores - occur when the skin and underlying tissue becomes damaged. Pressure ulcers are a widespread, and often underestimated, health problem. For example, in the UK, it is estimated that between 4 -10% of all patients who are admitted to hospital, will develop at least one pressure ulcer. And, for elderly people with mobility problems, the figure can be as high as 70%. Even with the best possible medical and nursing care, pressure ulcers can be difficult to prevent in particularly vulnerable people. The NICE guideline on pressure ulcers sets out best practice for treatment, including risk assessment and appropriate equipment to be used. DCHS carried out an audit to establish a baseline to measure future improvement against. Action plans have been developed to respond to audit findings and the planned yearly audits will evaluate practice against this benchmark and best practice guidelines.
Healthcare records • Record keeping is an essential tool to assist staff to communicate and monitor the service-users in their care. Staff are bound to protect service-user information to preserve confidentiality. • Audit and reviews of record-keeping systems and practices can help to ensure that good care and confidentiality are maintained. DCHS have carried out audits of documentation in healthcare records in community hospital, and health visiting services. Work is in progress to audit community nursing records. • This is considered by the PCT to be an important indicator, therefore it will carry forward into next year.
Fractured neck of femur • • A guideline setting out best practice for management of patients with a fractured neck of femur was released by the Scottish Intercollegiate Guidelines Network (SIGN). A clinical audit to provide evidence of nutritional, pressure ulcer risk and falls assessment in DCHS patients recovering from a fractured hip was requested. All patients in DCHS community hospitals should be assessed for a number of risk assessments on admission. These include nutritional status, pressure ulcer risk and falls with compliance measured as part of the Healthcare Records audit. DCHS IT systems are unable however, to link these results to specific clinical conditions and this was not viewed of sufficient priority to explore further. It was agreed that this was not a workable measure of quality.

Child protection • • At least 75% of DCHS front line staff should have received awareness training in child protection to ensure that children potentially at risk of harm or neglect are recognised. Staff should also be aware to notify an appropriately trained professional (e. g. GP or Health Visitor) of these concerns. Assurance was given that all staff have had the opportunity to learn or access training but this was not able to be formally counted. All staff whose job role involves directly caring for children (e. g. Health Visitors and School Nurses) have been given more advanced training. This indicator has only been partially met for 2008/09. The system to record attendance at training is insufficiently robust, therefore DCHS are only able to provide evidence that 11% of front line staff have received awareness training. DCHS plan to provide evidence of robust systems for safeguarding children in 2009/10.
Obesity in children Every child measured is contributing to the national picture about how children are growing. The more children that participate, the clearer that picture will be. The information collected helps the PCT to plan and provide better health services for the children in our area. • The National Child Measurement Programme 08/09 set a target of 85% for the proportion of children who must have their height and weight measured. DCHS provided evidence of system for measuring the height and weight of children at reception to school and at year 6 and that achievement in 2007/08 was 85%. • Data for 2008/09 can not be provided until the end of school year. It was therefore agreed to waive the assessment of this indicator in this scorecard and defer reporting until October 2009.
Health Care Associated Infection 1 • Infection Prevention & Control in the DCHS is managed in accordance with the Health Care Associated Infection Selfassessment Tool, which provides an overall score of compliance with infection control systems and procedures. The score in 2007 was 73%. • At subsequent review in 2008/09 DCHS demonstrated a very notable 20% improvement in score to 93%.
Health Care Associated Infection 2 • DCHS has implemented the Code of Practice which includes (but is not limited to): – ongoing assessment of the risks associated with healthcareassociated infection – surveillance of healthcare-associated infections – Serious Untoward Incident and Root Cause Analysis trends and findings. • DCHS must report all MRSA bacteraemia cases and C. difficile deaths to the Strategic Health Authority. These must be investigated within 10 working days, with findings and action taken reported within 20 working days. All requirements have been met
Mental Health in older people • This indicator required that DCHS will act upon 100% of the recommendations made in the most recent Mental Health Act Commission (MHAC) Annual report. • In 2008/09 the MHAC did not visit DCHS and no report was made, therefore this indicator was no longer valid.

Mental Health This indicator has been reviewed and a revised indicator has been agreed for 2009/10.
Breastfeeding • • Breast milk gives babies all the nutrients they need for the first six months of life and helps protect them from infection and diseases. It also reduces mothers' chances of getting certain diseases later in life. The baseline for quarter 1 of 2007/08 was not available however quarter 1 of 2008/09 showed a breastfeeding rate of 41% at 6 weeks after birth. The threshold was for DCHS to show an improvement of 2% on this baseline rate over the year. DCHS achieved an average rate of 44% for 2008/09 with a peak of 47% in quarter 2, therefore the 2% improvement target across the year was met. Breastfeeding rates will continue to be monitored by a national programme in 2009/10. Additionally, DCHS will pursue the intent to achieve a certificate of commitment to the UNICEF ‘Baby Friendly’ initiative. This will ensure further support for breastfeeding.
End of life care • The Liverpool Care Pathway (LCP) lays down a guide for the management of patients at the end of their lives to ensure that they are not undergoing unnecessary tests and procedures and have their pain and other distressing symptoms managed. • Several areas in the south of the county have completed an audit of end of life care based on work with the LCP. The audit showed a high level of compliance with the pathway with some areas for improvement particularly where staff had not fully documented their care. • Areas in the north of the county work to an end of life care pathway based on the LCP but not entirely the same. No audit has been done on this pathway, however DCHS is working towards the use of a unified pathway in the near future and this indicator has been carried forward to 2009/10.
Stroke This indicator required further development and clarity Stroke care has therefore not been audited in 2008/09, it is however considered by both DCHS and PCT to be an important indicator and an amended indicator will used be in 2009/10
Day case surgery • • • In order that we can see the effect of a day case surgery operation, patients complete one PROMs survey before their operation, and complete a second after the operation. The results from the before and after are compared to give us an indication of how a patient’s life has changed as a result of the treatment. Whilst there is no guarantee that all patients will benefit from treatment, it is to be expected that overall many will. DCHS have made some progress in implementing the use of PROMs in order to evaluate the success of a number of surgical procedures. There is emerging data for cataract extraction and hernia repair, which is in the main showing positive outcomes. Data will also soon start to be collected for some other operations. DCHS has now joined the national program of PROMs monitoring for hernia and varicose vein operations and will continue to develop PROMs for cataract surgery and foot joint operations in 2009/10.
Chronic back pain: outcomes of physiotherapy chronic back pain clinics will be monitored using a patient-reported outcome measure SF-36 • DCHS have provided evidence of use of the Roland & Morris tool to measure the outcome of physiotherapy interventions. This tool was administered by therapist in conjunction with the patient and showed improvements in condition in 93% of patients’ following physiotherapy interventions. • A PROMs tool for chronic back pain was not implemented in 2008/09 as a result of ongoing discussions between DCHS and the PCT but is planned for implementation in 2009/10.
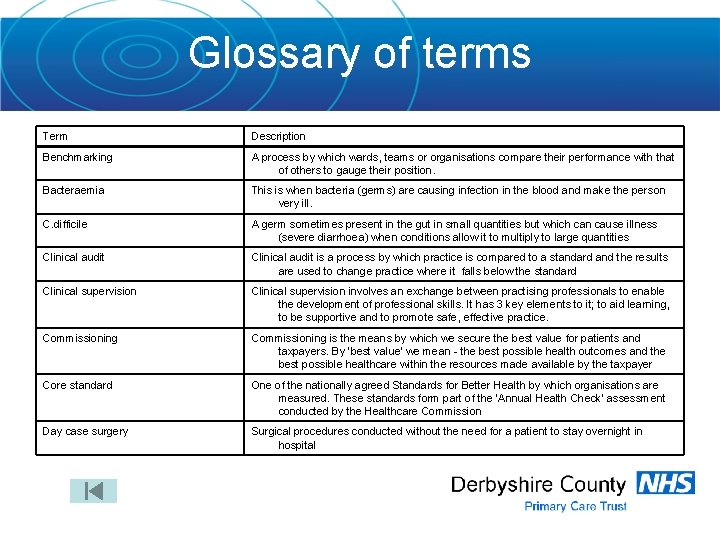
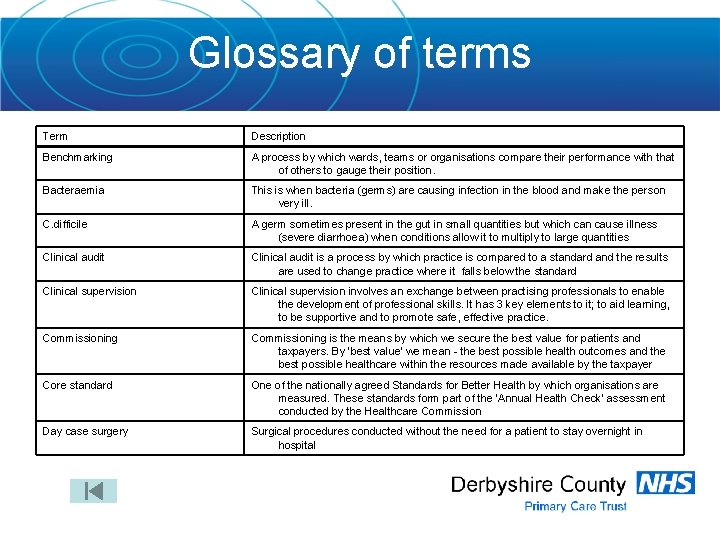
Glossary of terms Term Description Benchmarking A process by which wards, teams or organisations compare their performance with that of others to gauge their position. Bacteraemia This is when bacteria (germs) are causing infection in the blood and make the person very ill. C. difficile A germ sometimes present in the gut in small quantities but which can cause illness (severe diarrhoea) when conditions allow it to multiply to large quantities Clinical audit is a process by which practice is compared to a standard and the results are used to change practice where it falls below the standard Clinical supervision involves an exchange between practising professionals to enable the development of professional skills. It has 3 key elements to it; to aid learning, to be supportive and to promote safe, effective practice. Commissioning is the means by which we secure the best value for patients and taxpayers. By ‘best value’ we mean - the best possible health outcomes and the best possible healthcare within the resources made available by the taxpayer Core standard One of the nationally agreed Standards for Better Health by which organisations are measured. These standards form part of the ‘Annual Health Check’ assessment conducted by the Healthcare Commission Day case surgery Surgical procedures conducted without the need for a patient to stay overnight in hospital
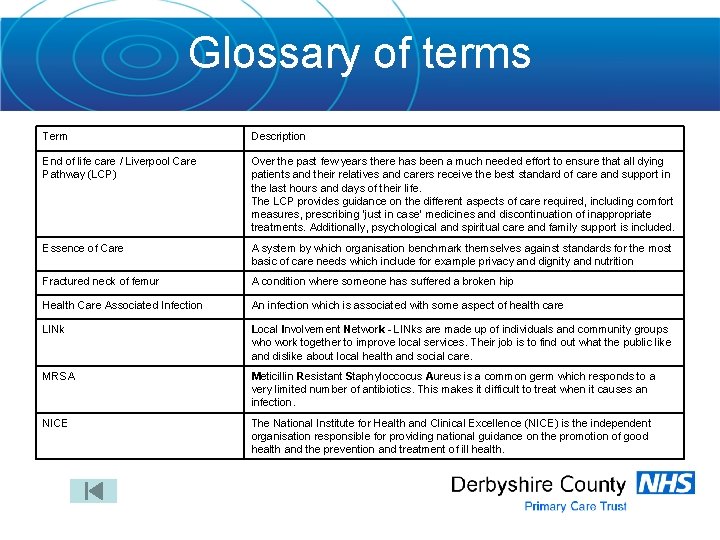
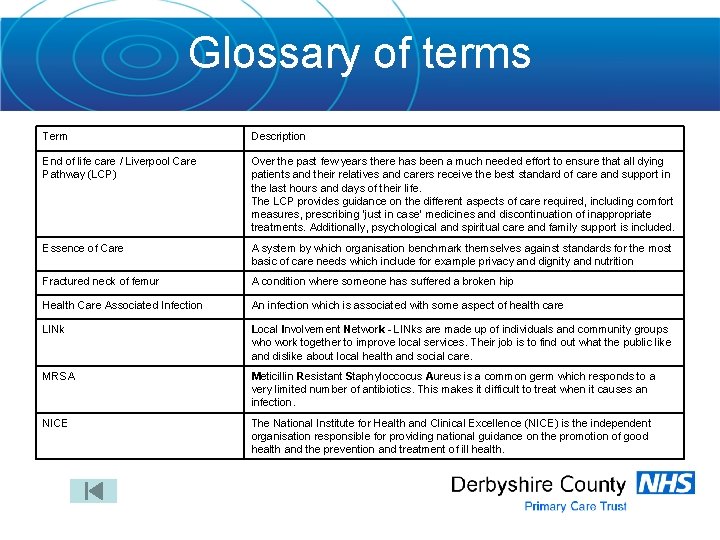
Glossary of terms Term Description End of life care / Liverpool Care Pathway (LCP) Over the past few years there has been a much needed effort to ensure that all dying patients and their relatives and carers receive the best standard of care and support in the last hours and days of their life. The LCP provides guidance on the different aspects of care required, including comfort measures, prescribing ‘just in case’ medicines and discontinuation of inappropriate treatments. Additionally, psychological and spiritual care and family support is included. Essence of Care A system by which organisation benchmark themselves against standards for the most basic of care needs which include for example privacy and dignity and nutrition Fractured neck of femur A condition where someone has suffered a broken hip Health Care Associated Infection An infection which is associated with some aspect of health care LINk Local Involvement Network - LINks are made up of individuals and community groups who work together to improve local services. Their job is to find out what the public like and dislike about local health and social care. MRSA Meticillin Resistant Staphyloccocus Aureus is a common germ which responds to a very limited number of antibiotics. This makes it difficult to treat when it causes an infection. NICE The National Institute for Health and Clinical Excellence (NICE) is the independent organisation responsible for providing national guidance on the promotion of good health and the prevention and treatment of ill health.
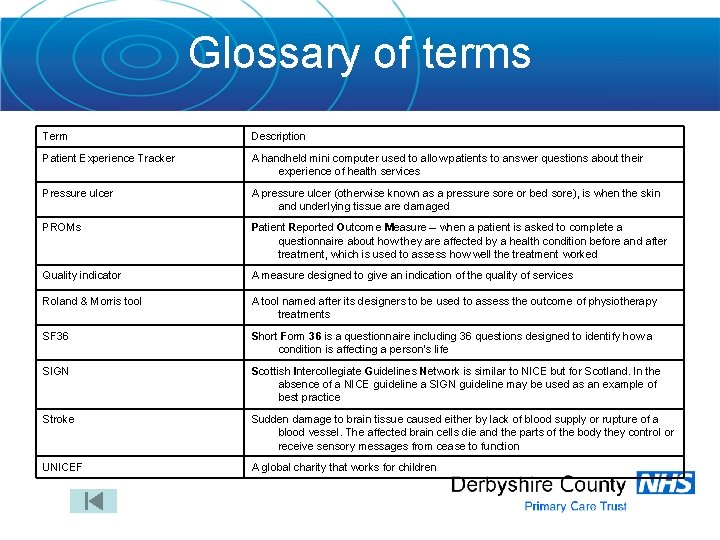
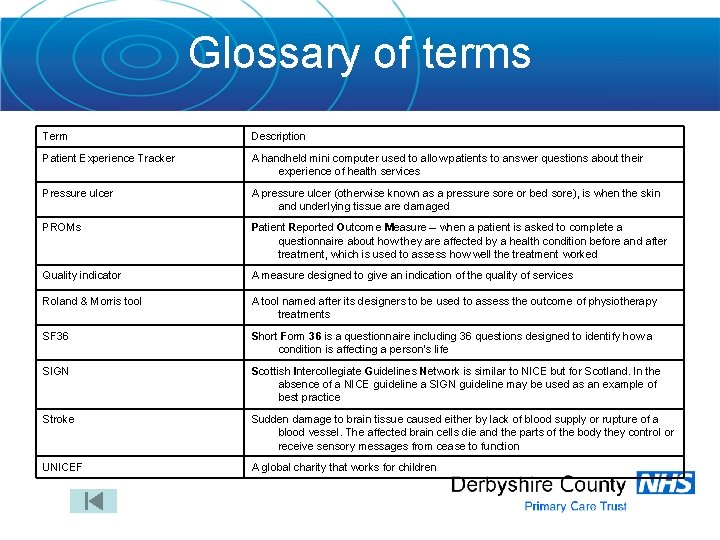
Glossary of terms Term Description Patient Experience Tracker A handheld mini computer used to allow patients to answer questions about their experience of health services Pressure ulcer A pressure ulcer (otherwise known as a pressure sore or bed sore), is when the skin and underlying tissue are damaged PROMs Patient Reported Outcome Measure – when a patient is asked to complete a questionnaire about how they are affected by a health condition before and after treatment, which is used to assess how well the treatment worked Quality indicator A measure designed to give an indication of the quality of services Roland & Morris tool A tool named after its designers to be used to assess the outcome of physiotherapy treatments SF 36 Short Form 36 is a questionnaire including 36 questions designed to identify how a condition is affecting a person’s life SIGN Scottish Intercollegiate Guidelines Network is similar to NICE but for Scotland. In the absence of a NICE guideline a SIGN guideline may be used as an example of best practice Stroke Sudden damage to brain tissue caused either by lack of blood supply or rupture of a blood vessel. The affected brain cells die and the parts of the body they control or receive sensory messages from cease to function UNICEF A global charity that works for children
 Quality monitoring scorecard
Quality monitoring scorecard Quality monitoring scorecard
Quality monitoring scorecard The hr scorecard
The hr scorecard Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Sports medicine definition
Sports medicine definition International society for quality in healthcare
International society for quality in healthcare Give us your hungry your tired your poor
Give us your hungry your tired your poor National water quality monitoring conference
National water quality monitoring conference National water quality monitoring council
National water quality monitoring council Dqmf
Dqmf Wigos data quality monitoring system
Wigos data quality monitoring system Real time data quality monitoring
Real time data quality monitoring Permanent power quality monitoring equipment
Permanent power quality monitoring equipment Nwqmc
Nwqmc National water quality monitoring conference
National water quality monitoring conference Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worms-breton
Tư thế worms-breton Hát lên người ơi alleluia
Hát lên người ơi alleluia Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân 101012 bằng
101012 bằng độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể