Ministar When and How Prof Alfredo R Galassi
- Slides: 44
Ministar: When and How Prof. Alfredo R Galassi MD, FACC, FESC, FSCAI Director of Cardiac Catheterization and Interventional Cardiology Unit Dept of Int Medicine and Systemic Disease Division of Cardiology, Cannizzaro Hospital, University of Catania, Italy
Alfredo R. Galassi, MD I have no real or apparent conflicts of interest to report.
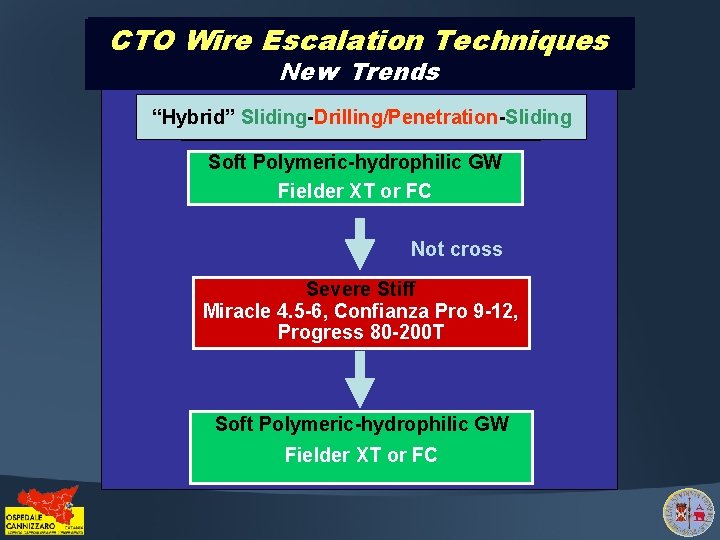
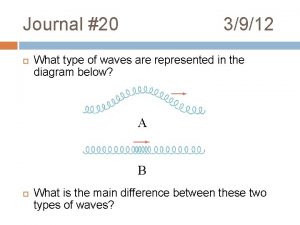
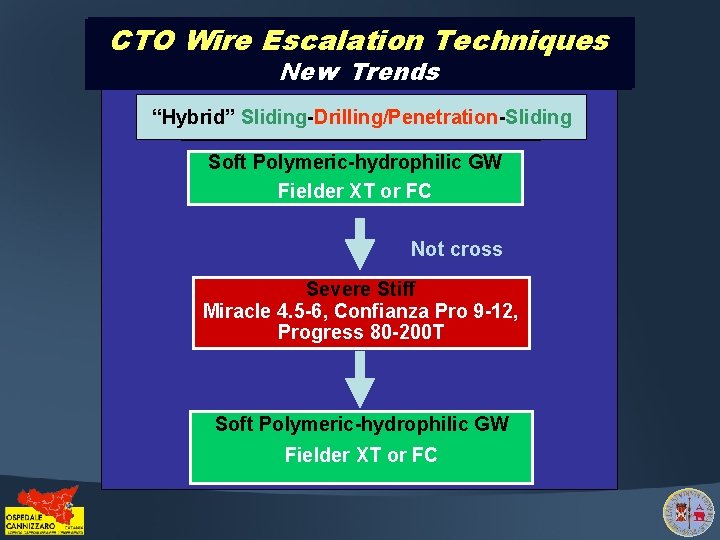
CTO Wire Escalation Techniques CTO Old Trends New Trends “Hybrid” Sliding-Drilling/Penetration-Sliding “Hybrid” Sliding-Drilling/Penetration Soft Polymeric-hydrophilic GW Fielder XT or FC Not cross Severe Moderate Stiff GW 0. 014” Miracle Confianza Pro 200 9 -12, Miracle 4. 5 -6, 3, Medium, Crossit Progress 80 -200 T Not cross Severe Stiff Soft Polymeric-hydrophilic GW Miracle 4. 5 -6, Confianza Pro 9 -12, Fielder XT or FC Progress 80 -200 T
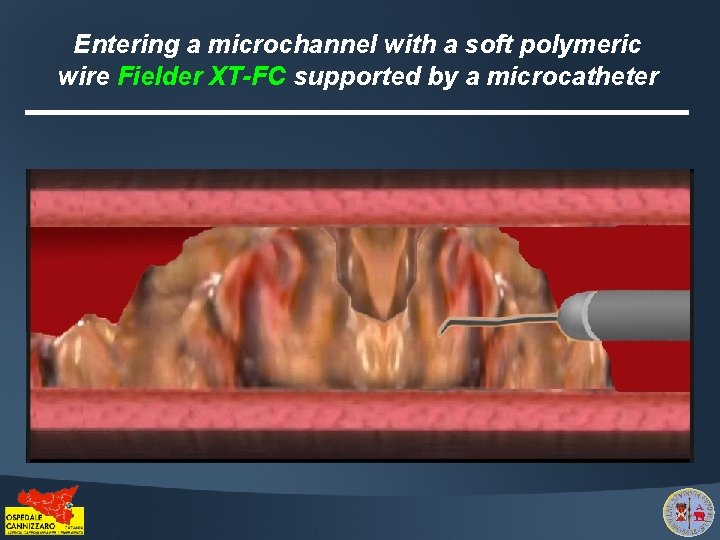
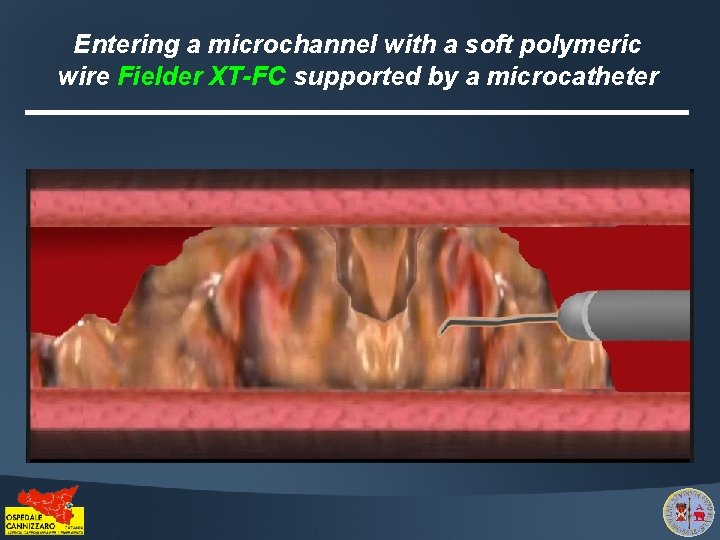
Entering a microchannel with a soft polymeric wire Fielder XT-FC supported by a microcatheter
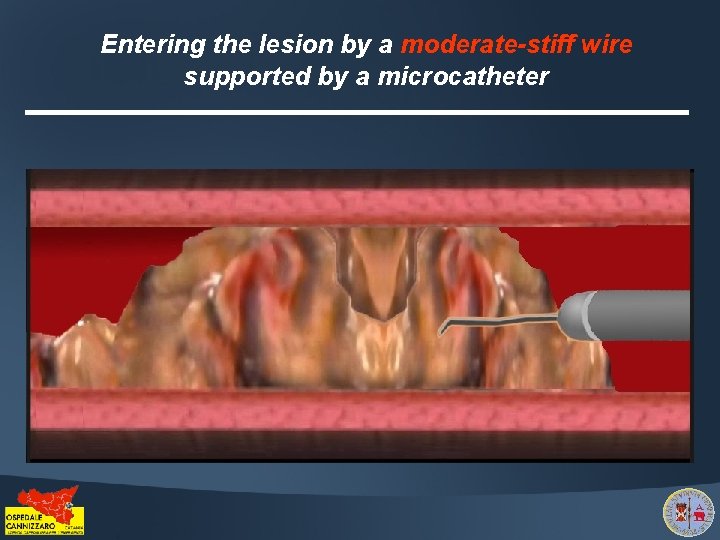
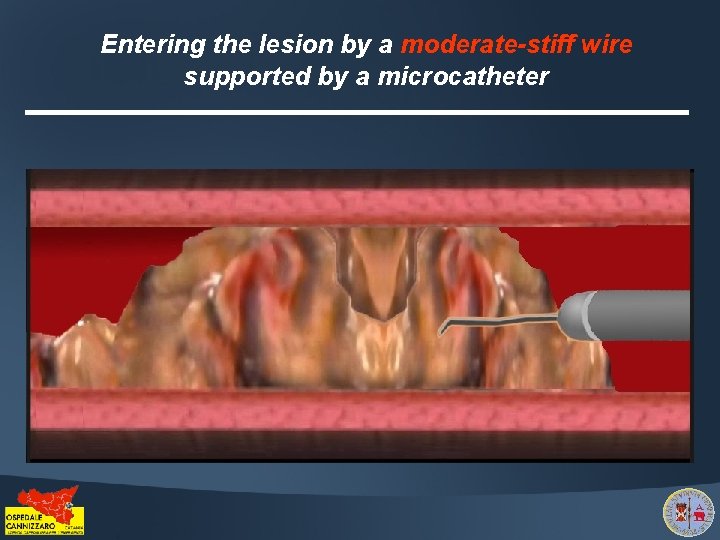
Entering the lesion by a moderate-stiff wire supported by a microcatheter
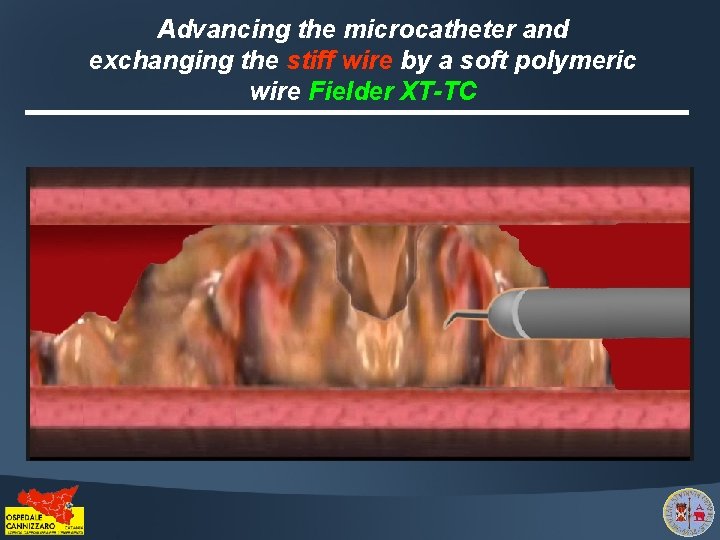
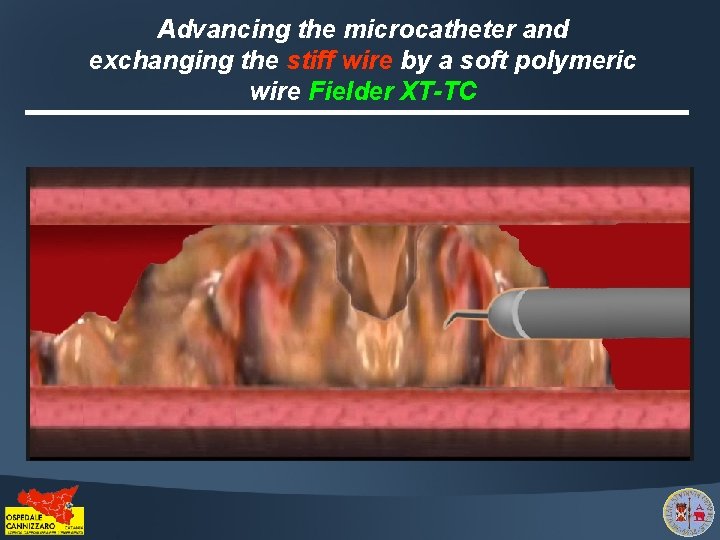
Advancing the microcatheter and exchanging the stiff wire by a soft polymeric wire Fielder XT-TC
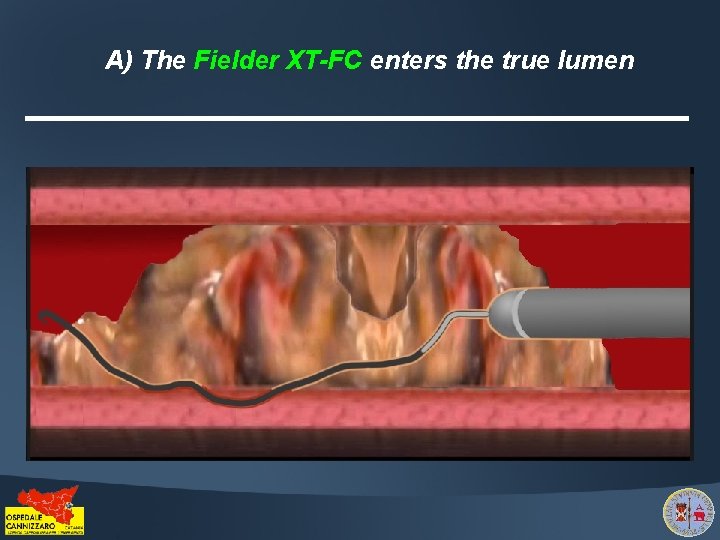
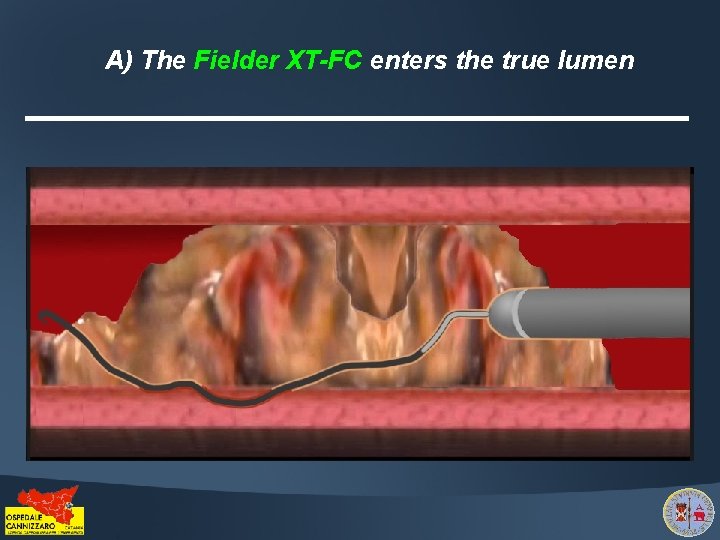
A) The Fielder XT-FC enters the true lumen
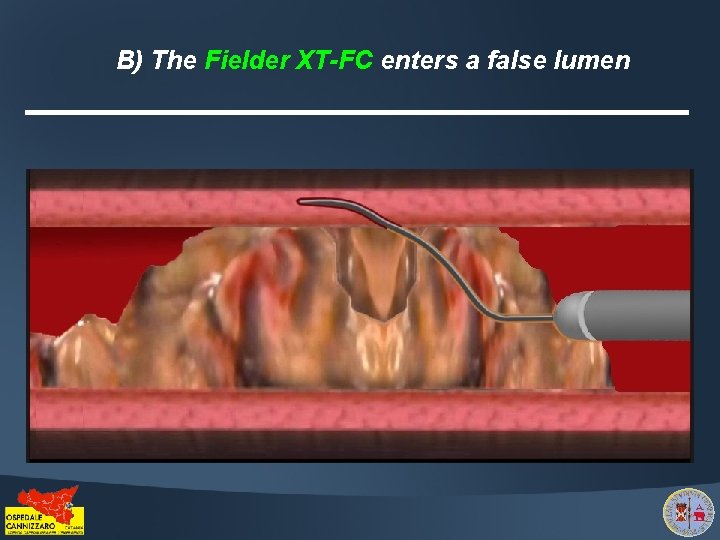
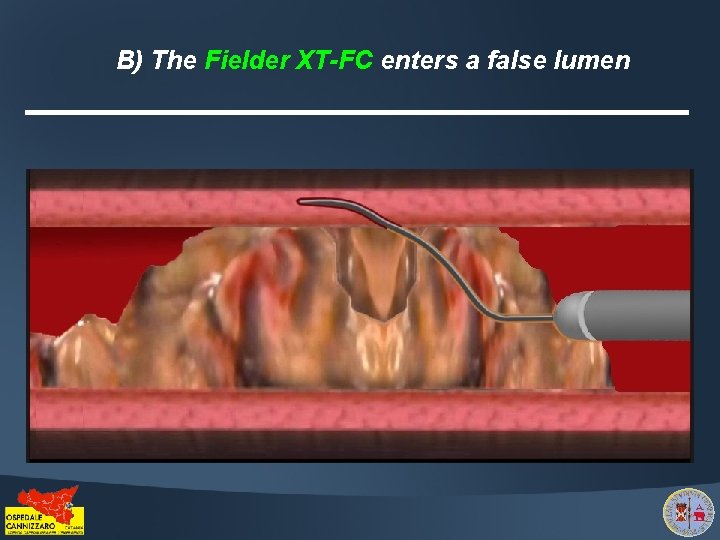
B) The Fielder XT-FC enters a false lumen
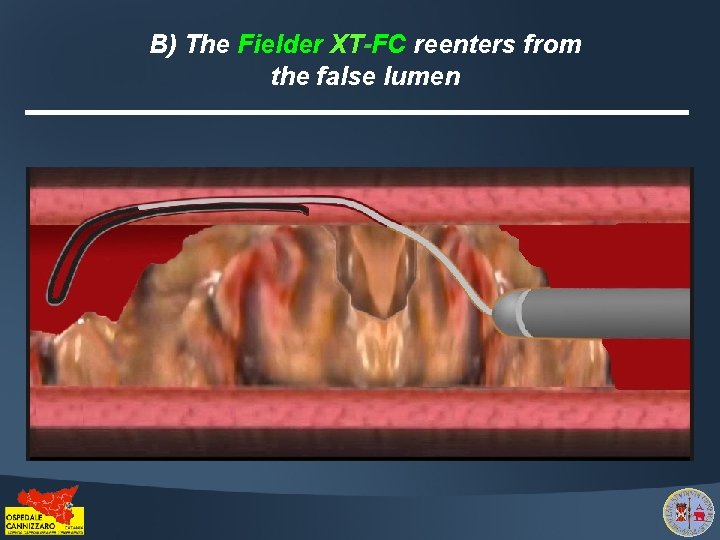
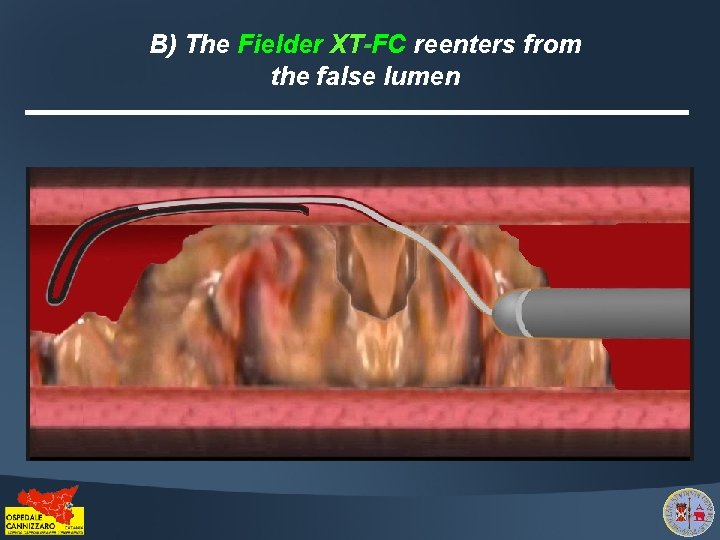
B) The Fielder XT-FC reenters from the false lumen
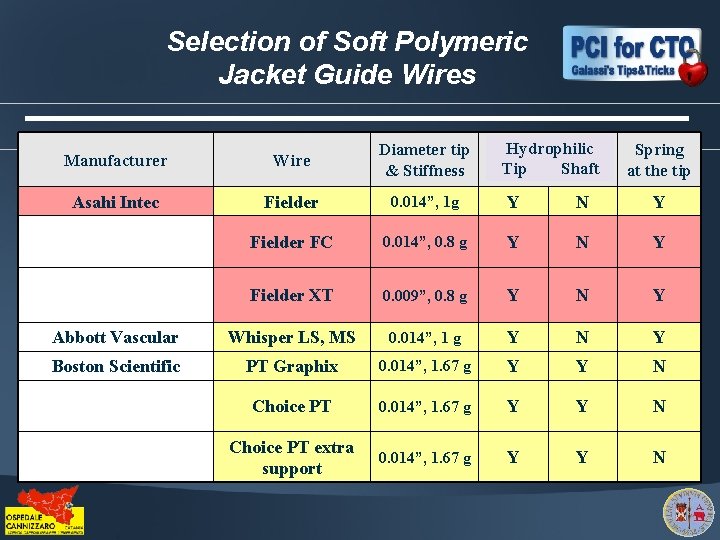
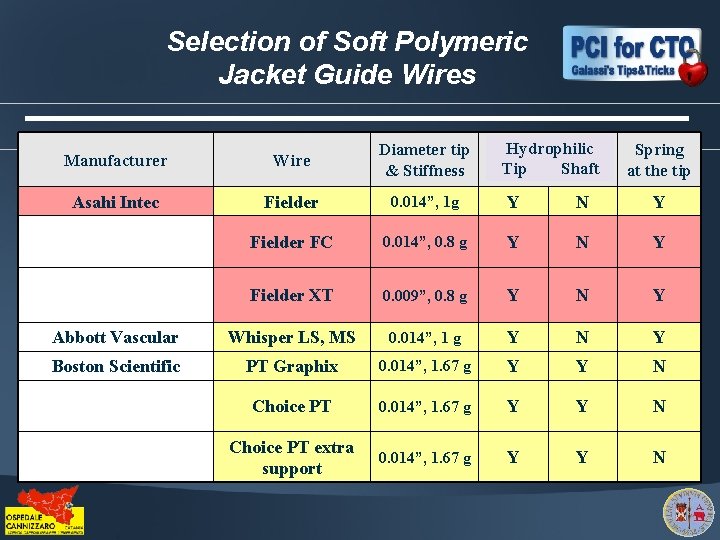
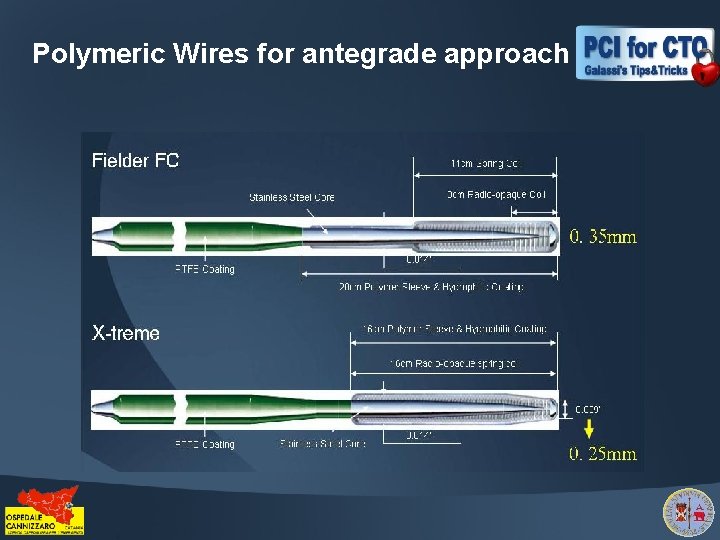
Selection of Soft Polymeric Jacket Guide Wires Hydrophilic Hydrophili c c shaft Tip Shaft tip Manufacturer Wire Diameter tip & Stiffness Spring at the tip Asahi Intec Fielder 0. 014”, 1 g Y N Y Fielder FC 0. 014”, 0. 8 g Y N Y Fielder XT 0. 009”, 0. 8 g Y N Y Abbott Vascular Whisper LS, MS 0. 014”, 1 g Y N Y Boston Scientific PT Graphix 0. 014”, 1. 67 g Y Y N Choice PT extra support 0. 014”, 1. 67 g Y Y N
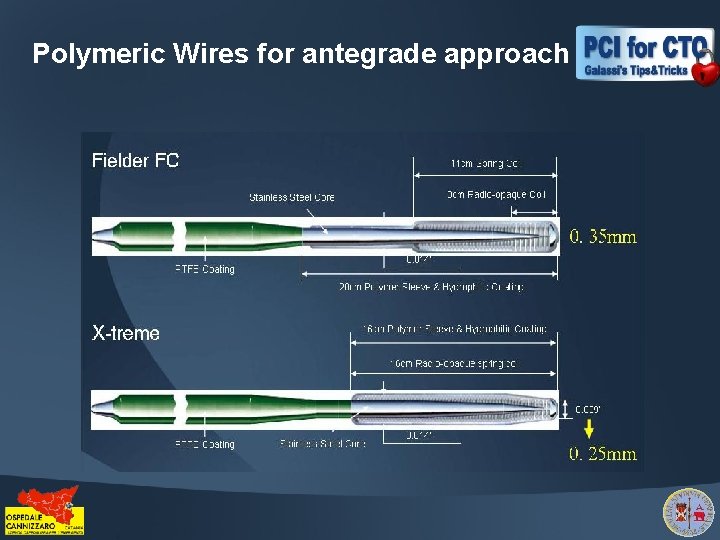
Polymeric Wires for antegrade approach
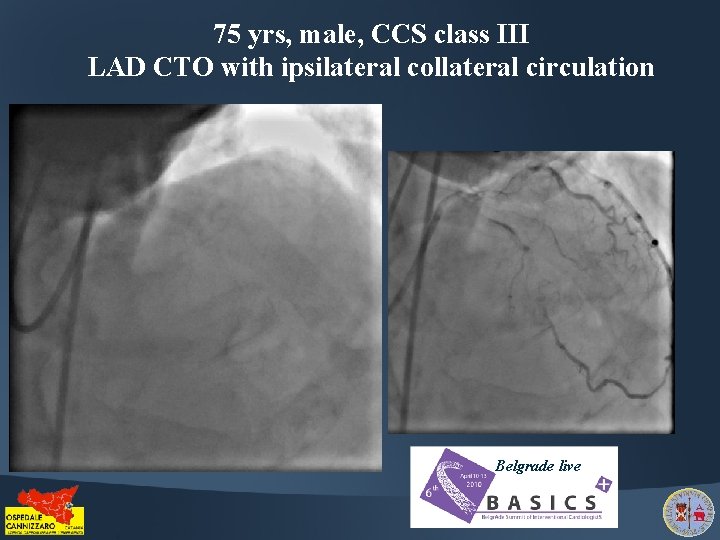
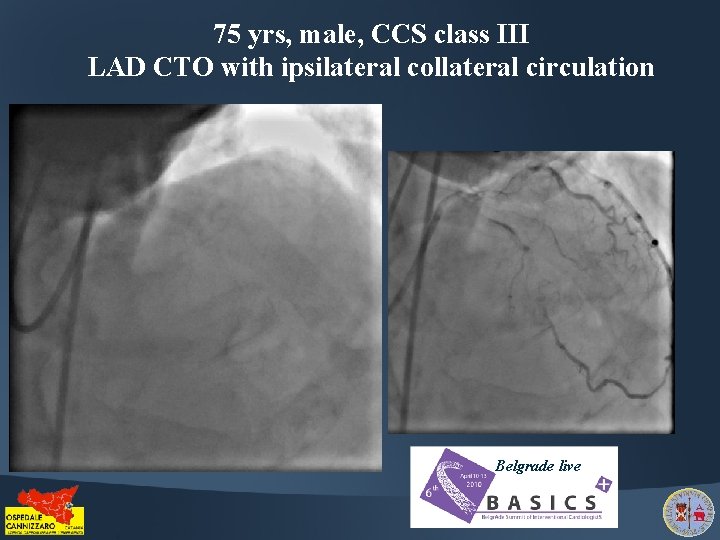
75 yrs, male, CCS class III LAD CTO with ipsilateral collateral circulation Belgrade live
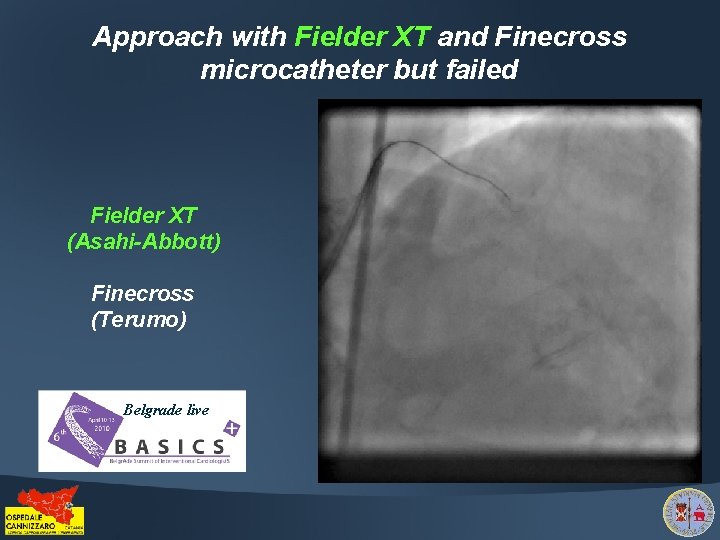
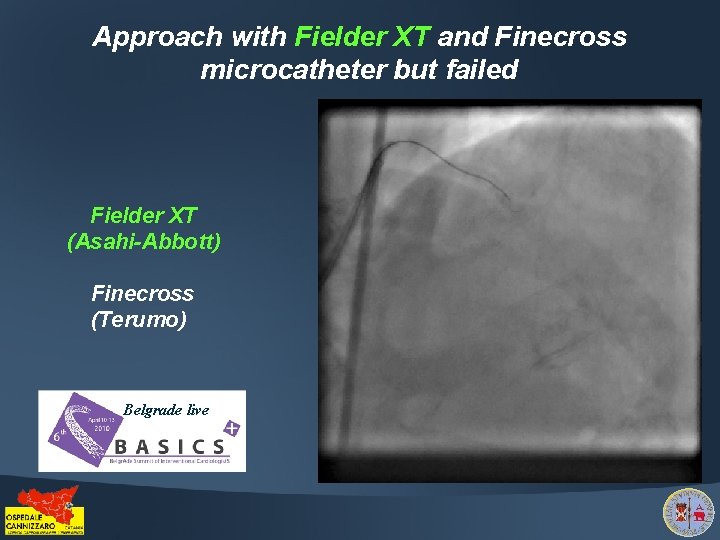
Approach with Fielder XT and Finecross microcatheter but failed Fielder XT (Asahi-Abbott) Finecross (Terumo) Belgrade live
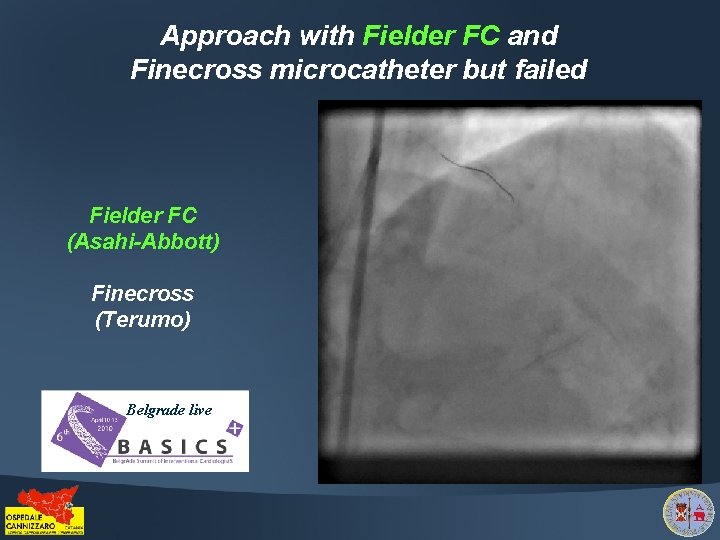
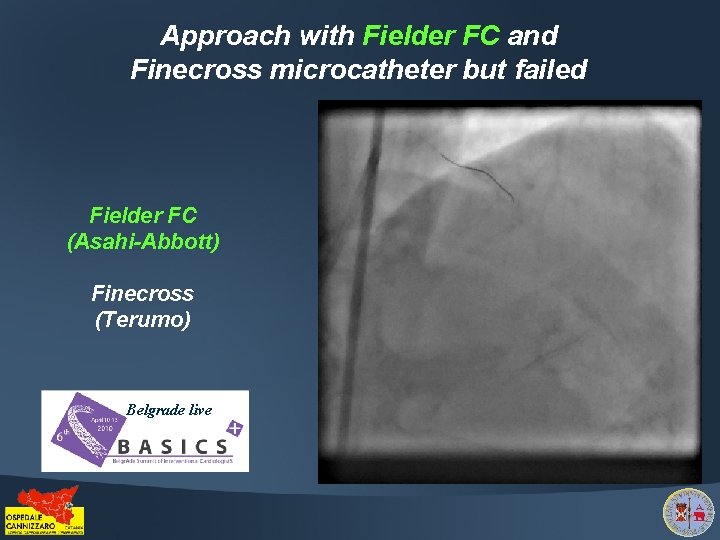
Approach with Fielder FC and Finecross microcatheter but failed Fielder FC (Asahi-Abbott) Finecross (Terumo) Belgrade live
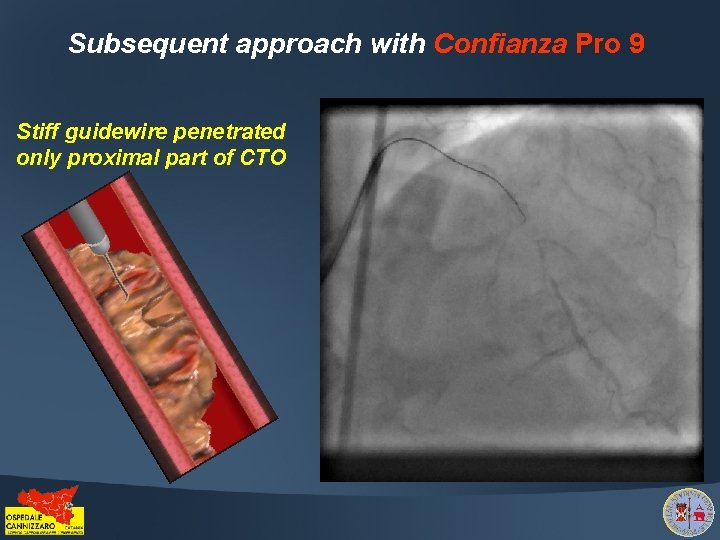
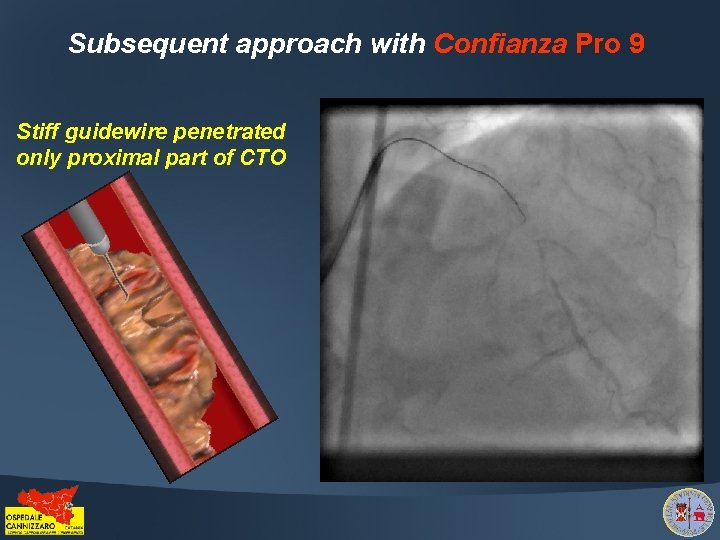
Subsequent approach with Confianza Pro 9 Stiff guidewire penetrated only proximal part of CTO
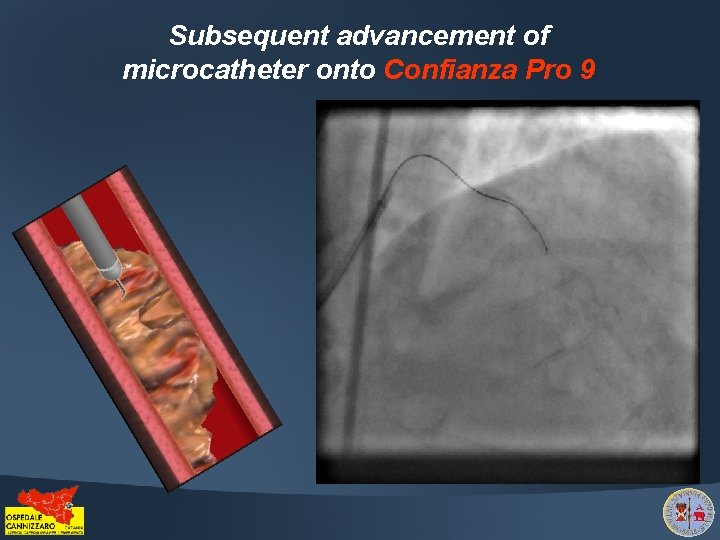
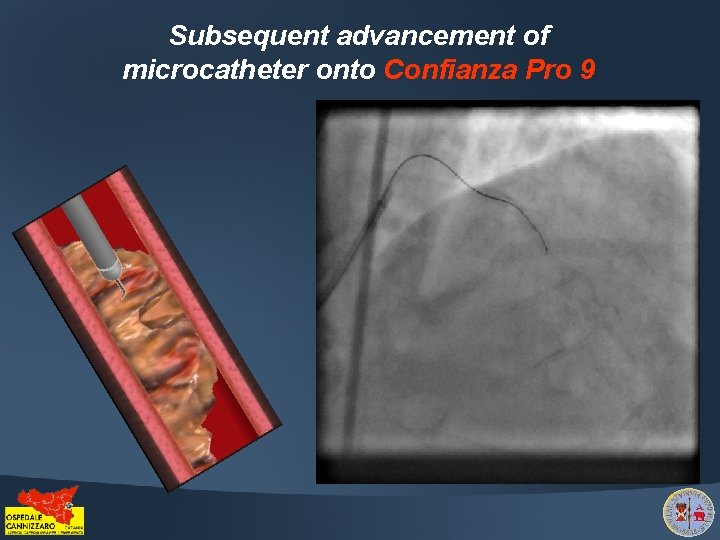
Subsequent advancement of microcatheter onto Confianza Pro 9
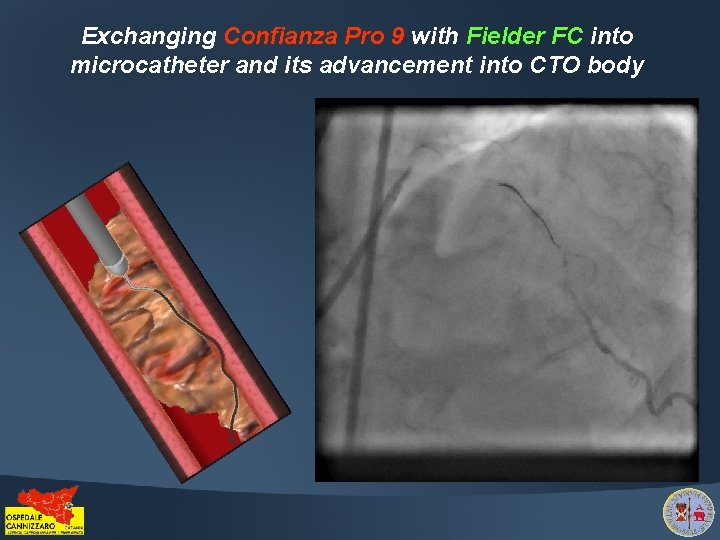
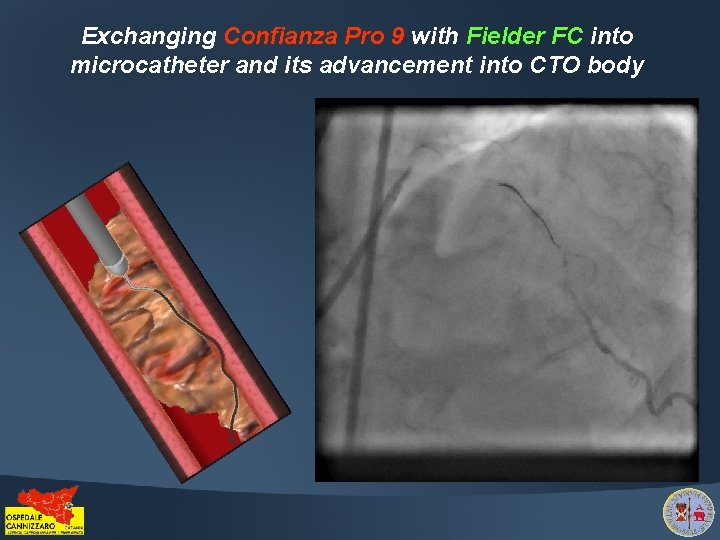
Exchanging Confianza Pro 9 with Fielder FC into microcatheter and its advancement into CTO body
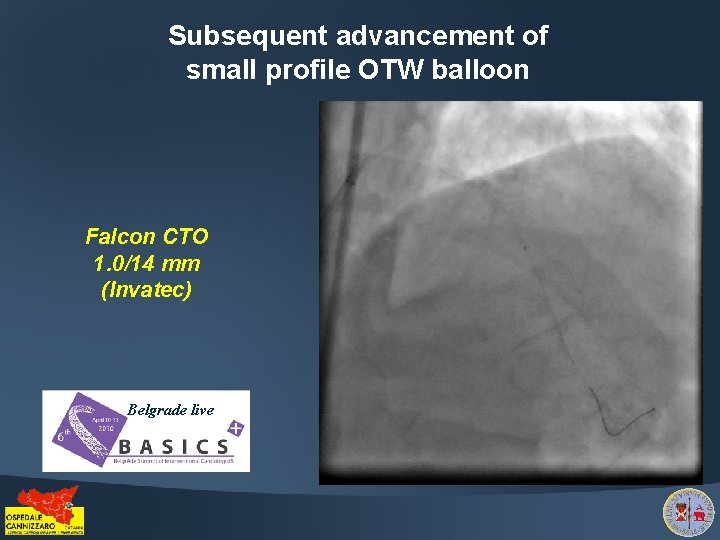
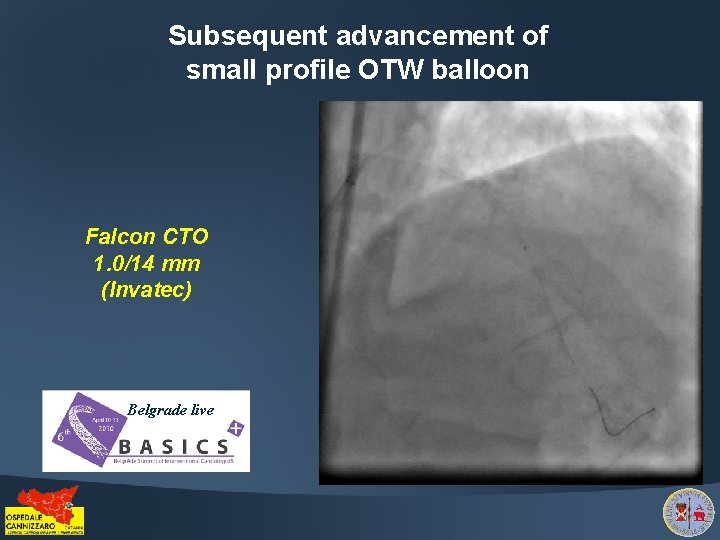
Subsequent advancement of small profile OTW balloon Falcon CTO 1. 0/14 mm (Invatec) Belgrade live
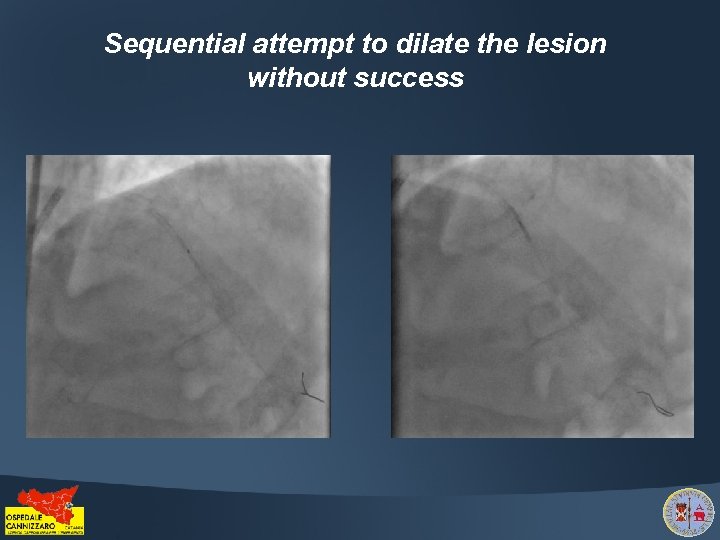
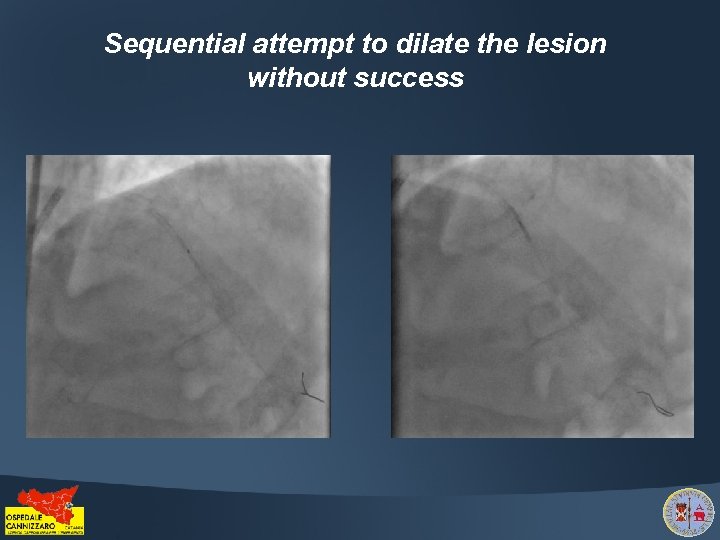
Sequential attempt to dilate the lesion without success
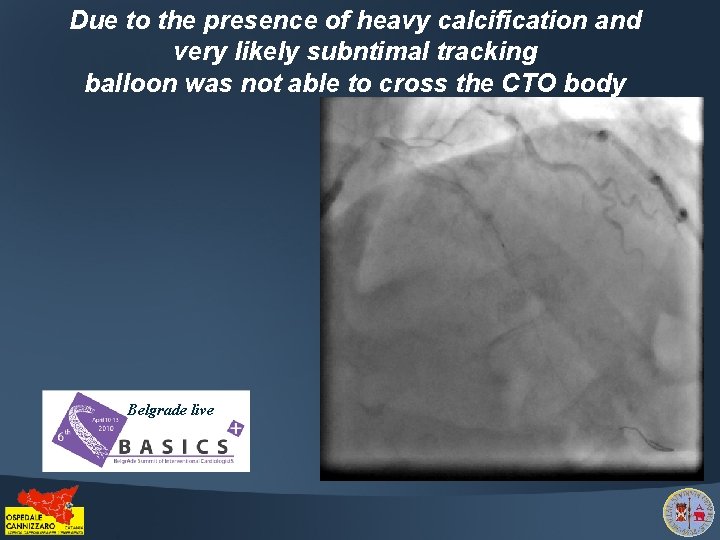
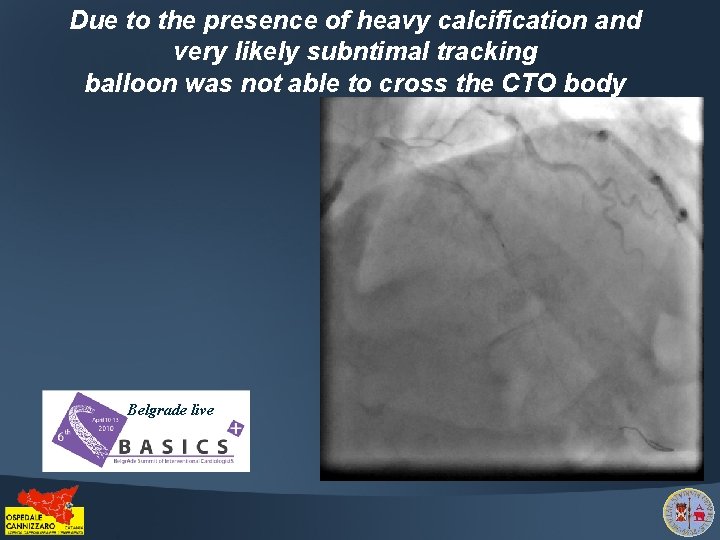
Due to the presence of heavy calcification and very likely subntimal tracking balloon was not able to cross the CTO body Belgrade live
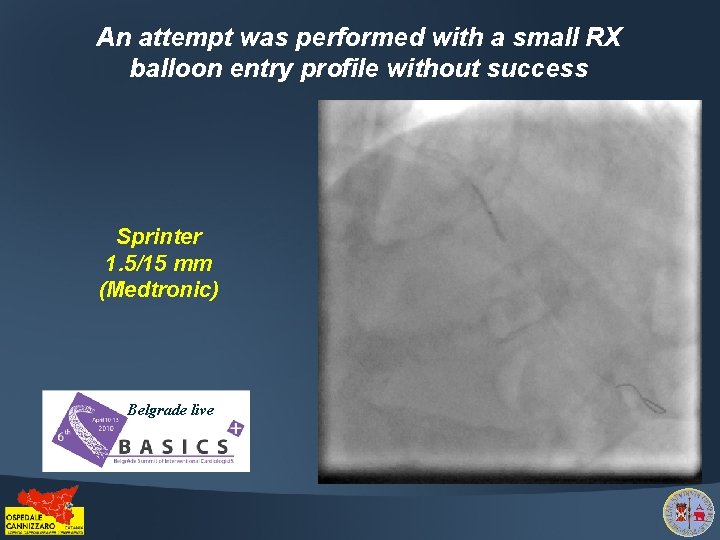
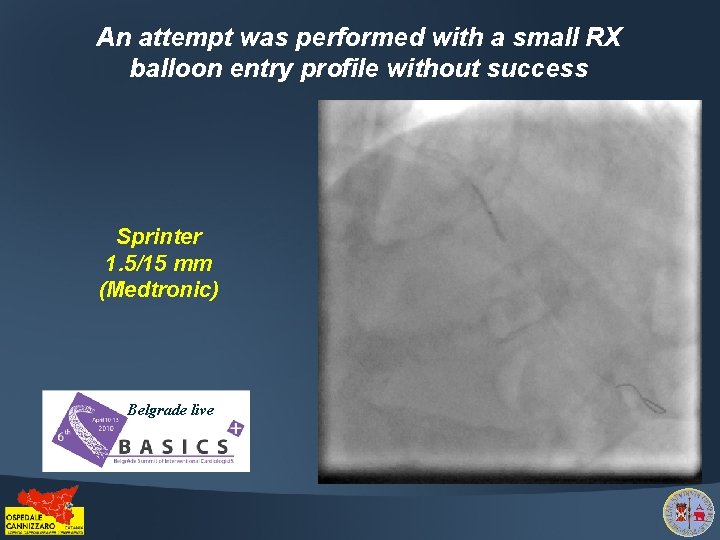
An attempt was performed with a small RX balloon entry profile without success Sprinter 1. 5/15 mm (Medtronic) Belgrade live
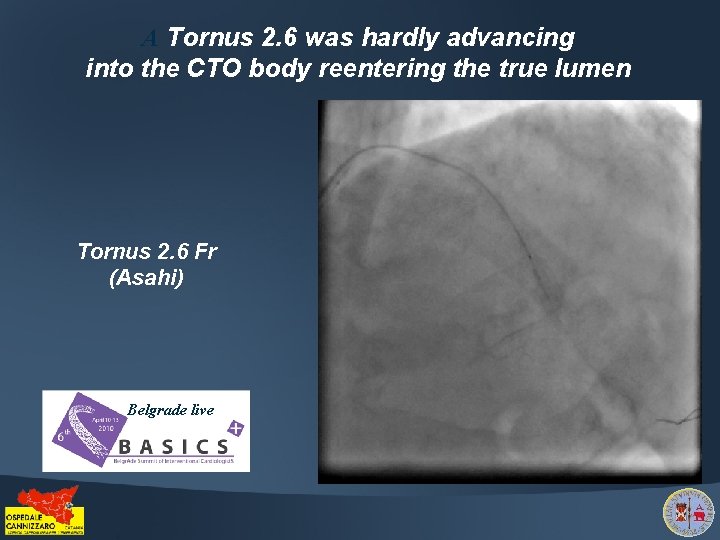
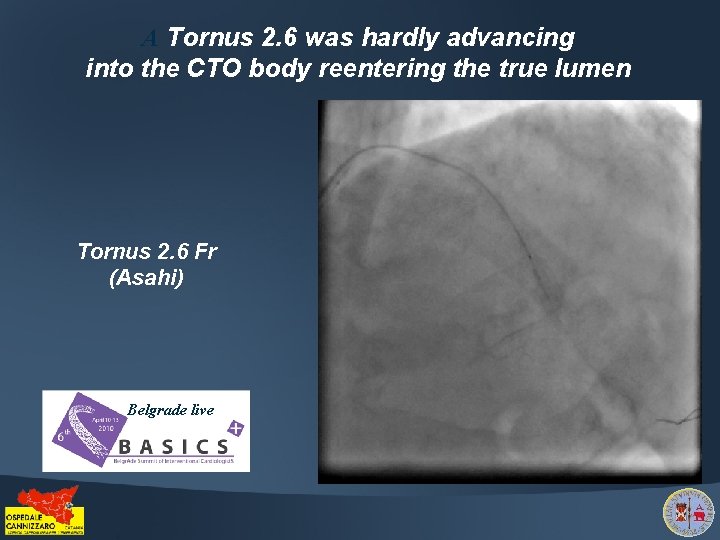
A Tornus 2. 6 was hardly advancing into the CTO body reentering the true lumen Tornus 2. 6 Fr (Asahi) Belgrade live
Finally the Tornus 2. 6 was able to advance into the CTO body Belgrade live
The Fielder FC guidewire was exchanged within Tornus with Prowater Flex (Asahi-Abbott) Belgrade live
Distal Tornus position was checked with ipsilateral collateral flow injection Prowater Flex (Asahi-Abbott) Belgrade live
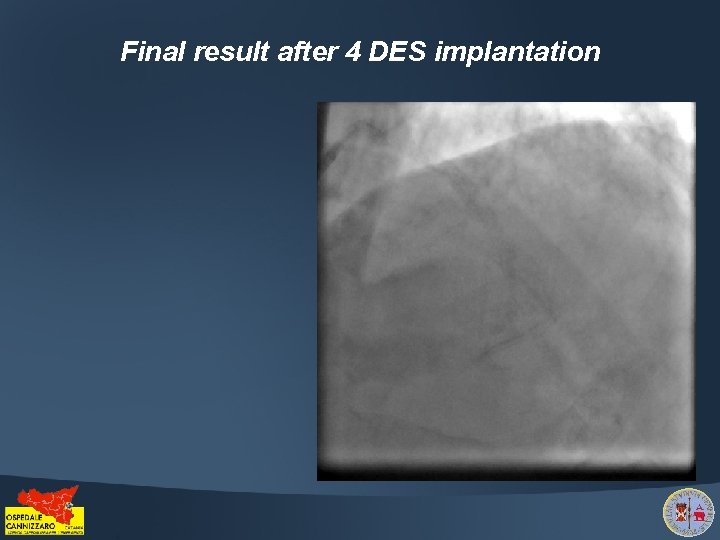
Final result after 4 DES implantation
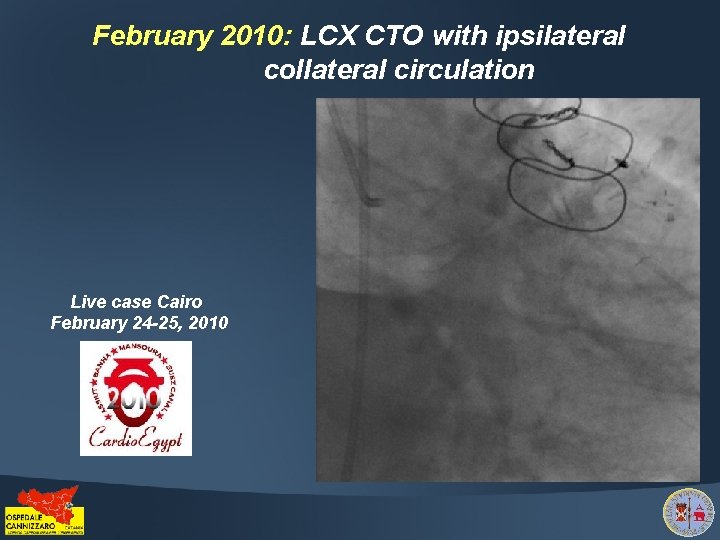
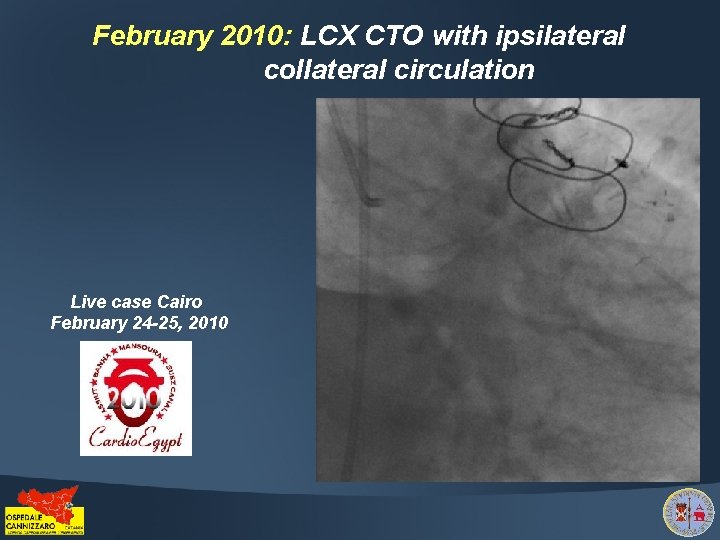
February 2010: LCX CTO with ipsilateral collateral circulation Live case Cairo February 24 -25, 2010
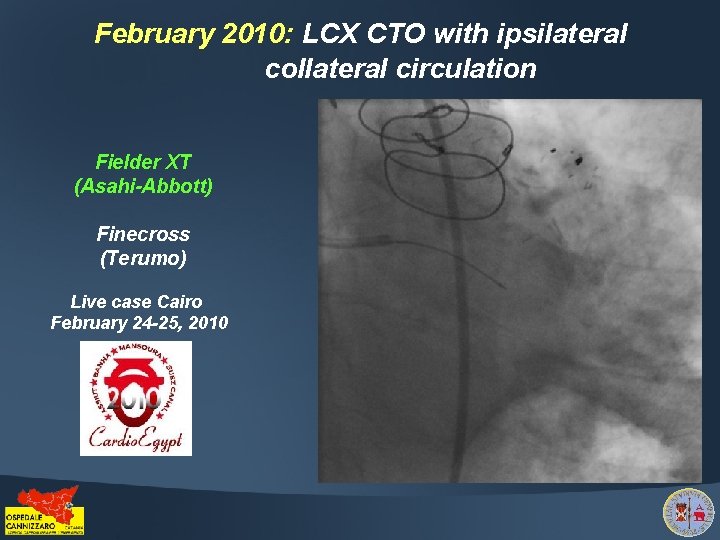
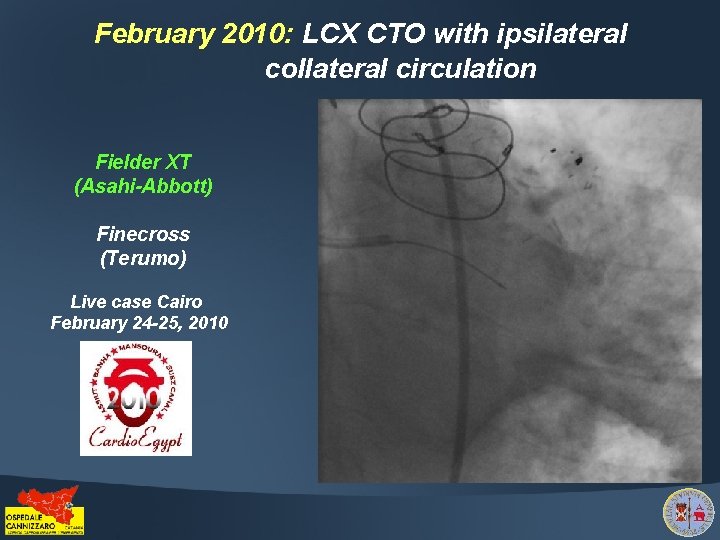
February 2010: LCX CTO with ipsilateral collateral circulation Fielder XT (Asahi-Abbott) Finecross (Terumo) Live case Cairo February 24 -25, 2010
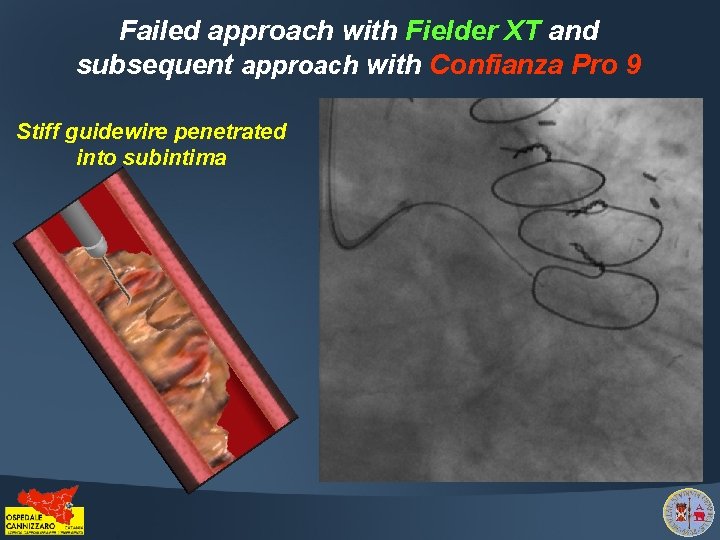
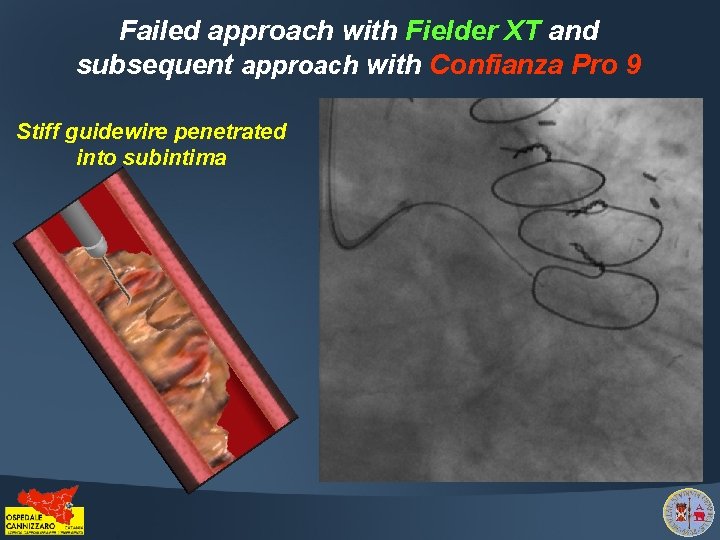
Failed approach with Fielder XT and subsequent approach with Confianza Pro 9 Stiff guidewire penetrated into subintima
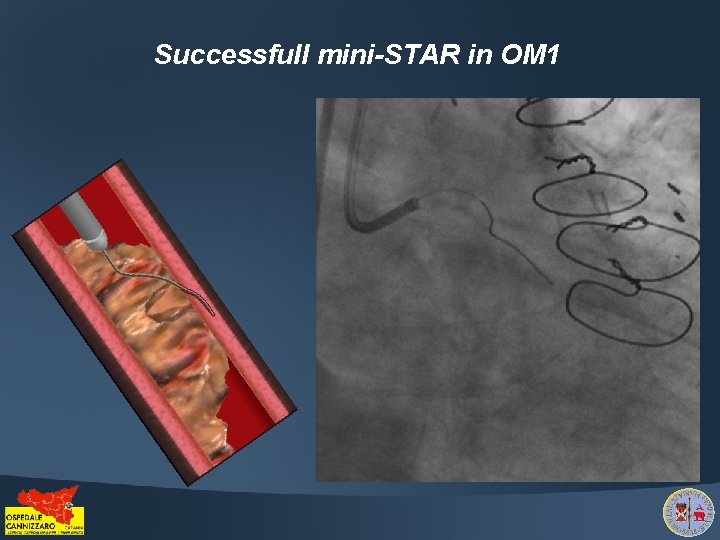
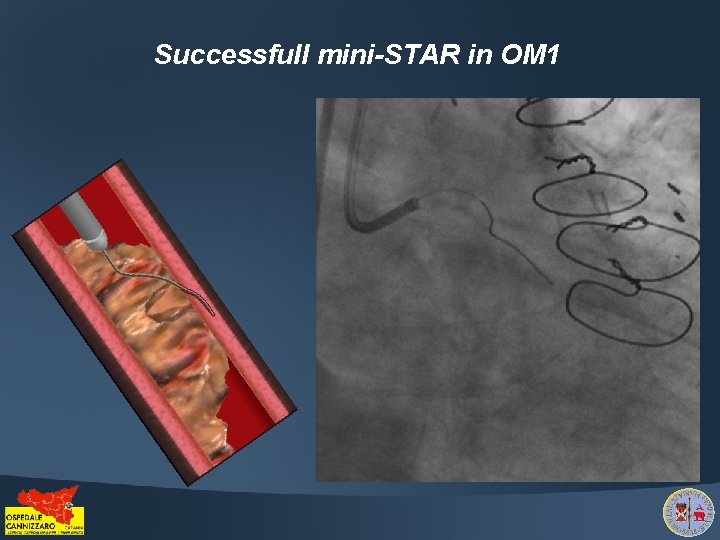
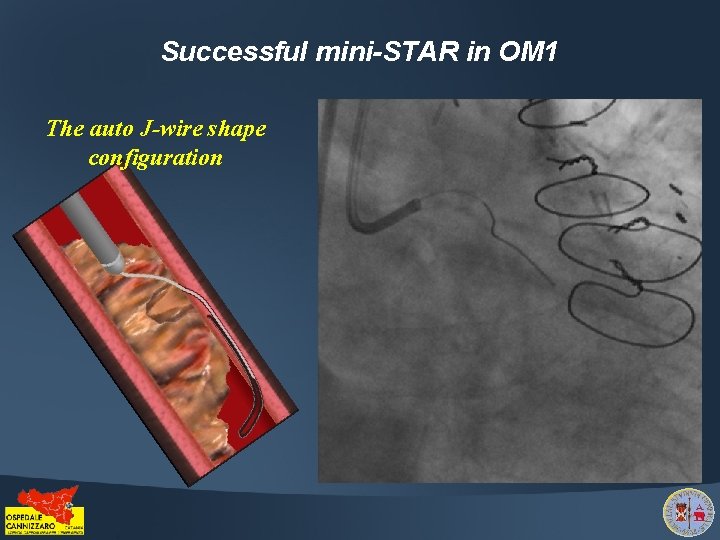
Successfull mini-STAR in OM 1
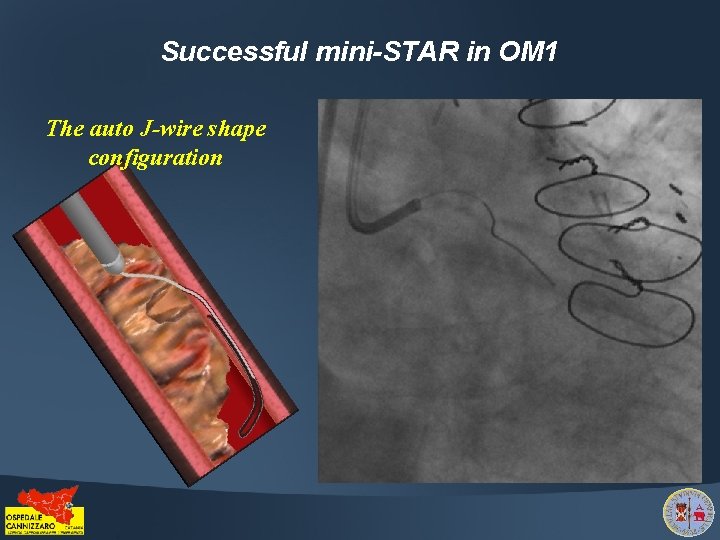
Successful mini-STAR in OM 1 The auto J-wire shape configuration
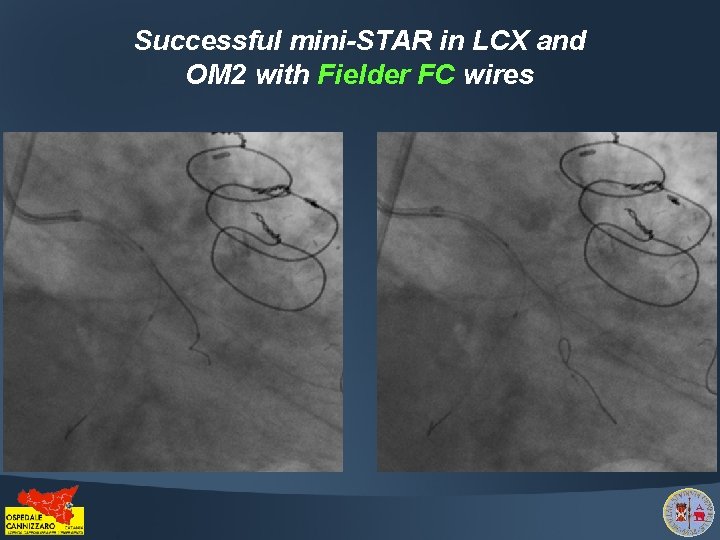
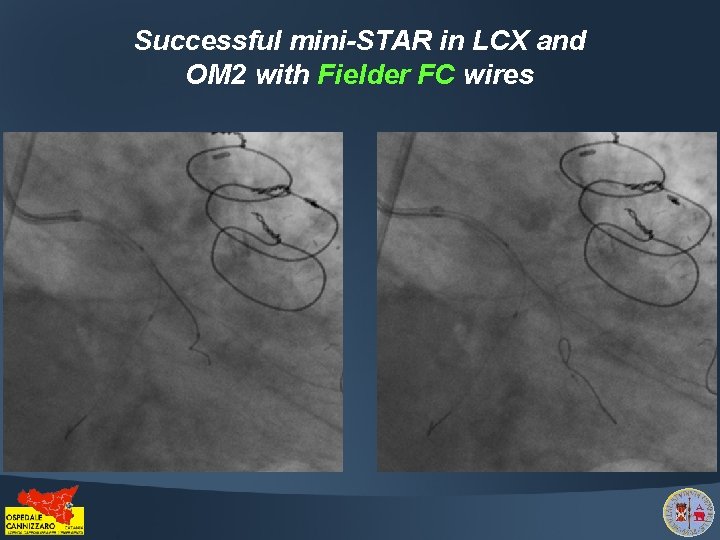
Successful mini-STAR in LCX and OM 2 with Fielder FC wires
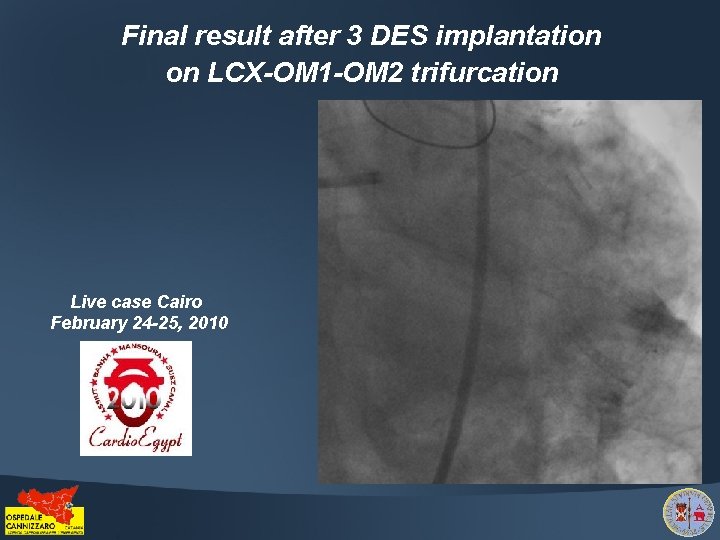
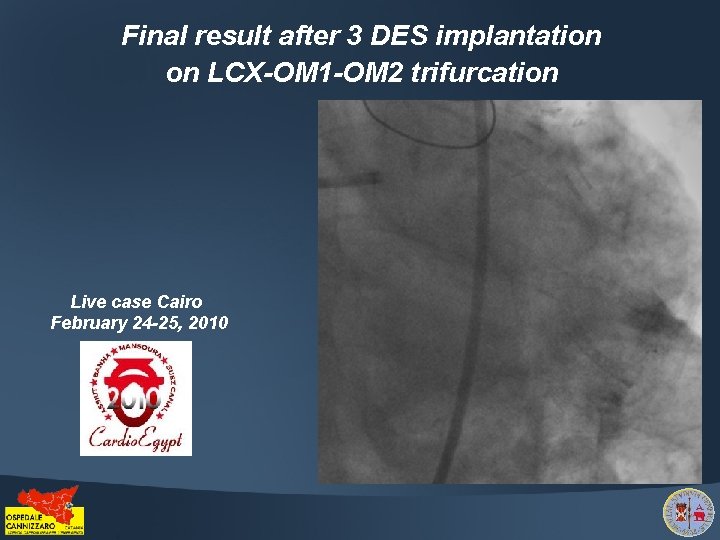
Final result after 3 DES implantation on LCX-OM 1 -OM 2 trifurcation Live case Cairo February 24 -25, 2010
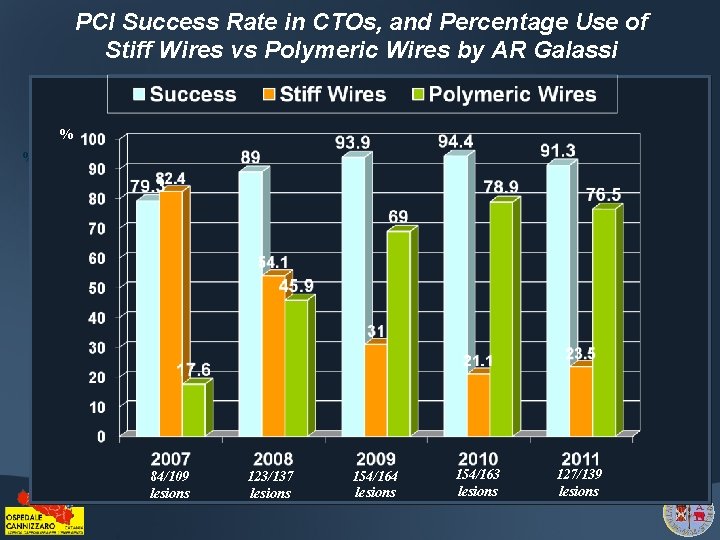
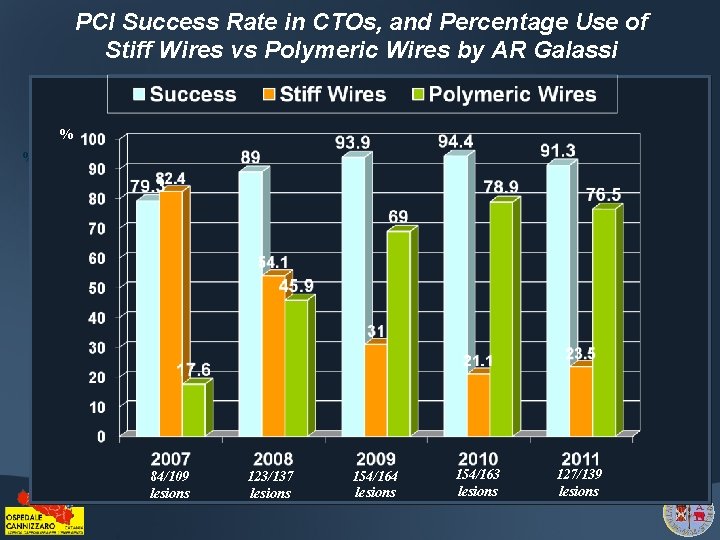
PCI Success Rate in CTOs, and Percentage Use of Stiff Wires vs Polymeric Wires by AR Galassi % % 84/109 lesions 123/137 lesions 154/164 lesions 154/163 lesions 127/139 lesions
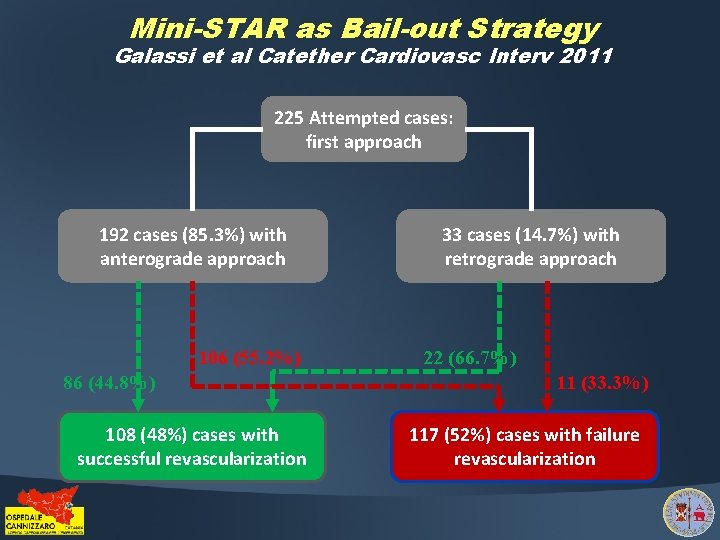
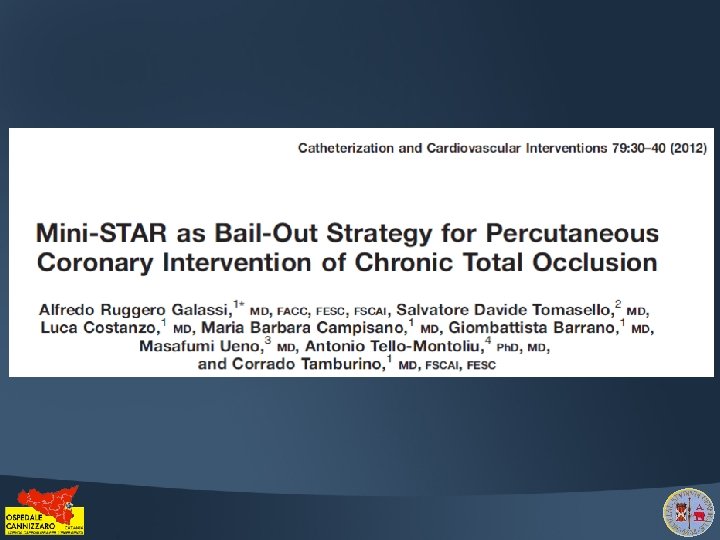
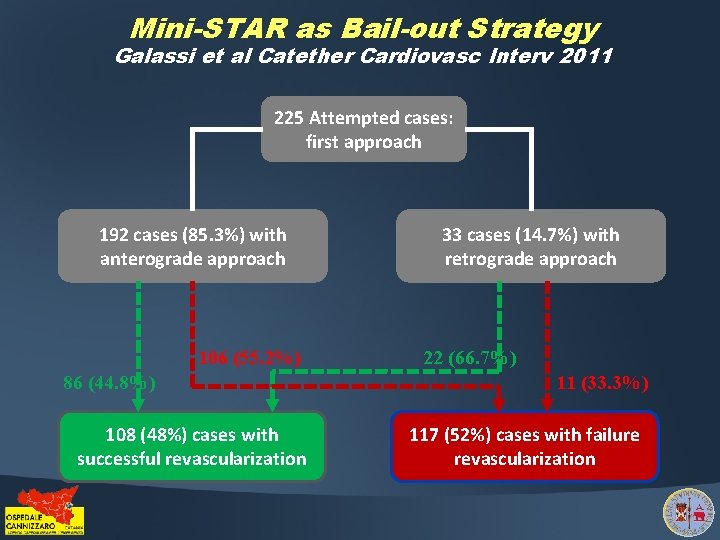
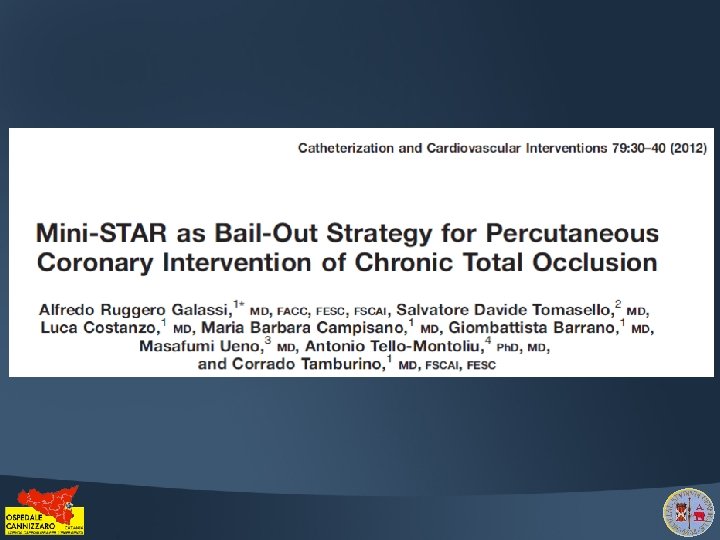
Mini-STAR as Bail-out Strategy Galassi et al Catether Cardiovasc Interv 2011 225 Attempted cases: first approach 192 cases (85. 3%) with anterograde approach 106 (55. 2%) 86 (44. 8%) 108 (48%) cases with successful revascularization 33 cases (14. 7%) with retrograde approach 22 (66. 7%) 11 (33. 3%) 117 (52%) cases with failure revascularization
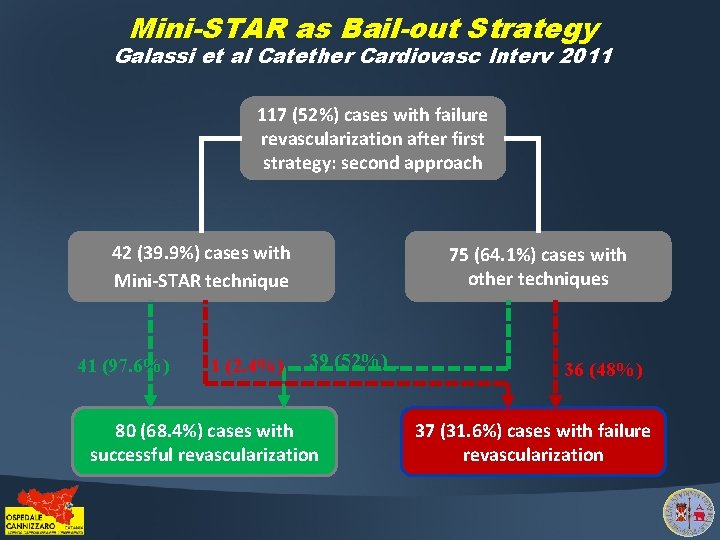
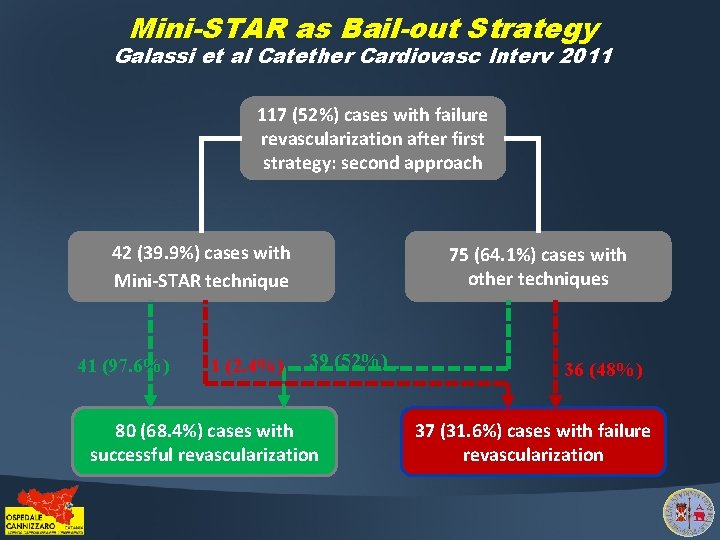
Mini-STAR as Bail-out Strategy Galassi et al Catether Cardiovasc Interv 2011 117 (52%) cases with failure revascularization after first strategy: second approach 42 (39. 9%) cases with Mini-STAR technique 41 (97. 6%) 1 (2. 4%) 75 (64. 1%) cases with other techniques 39 (52%) 80 (68. 4%) cases with successful revascularization 36 (48%) 37 (31. 6%) cases with failure revascularization
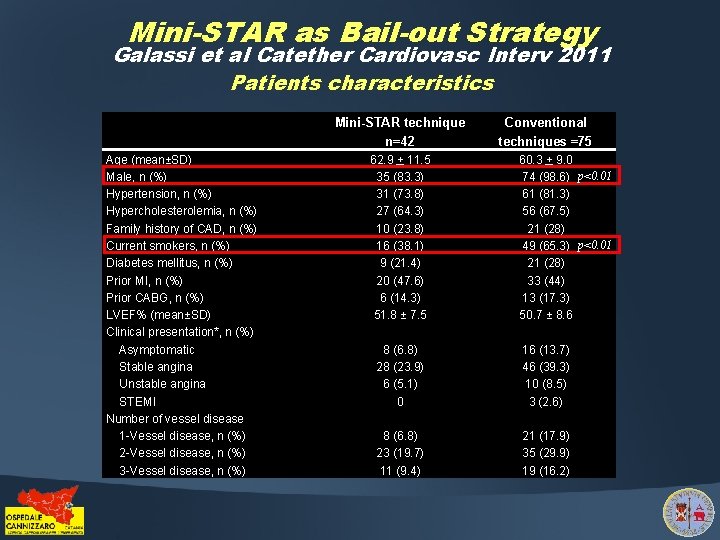
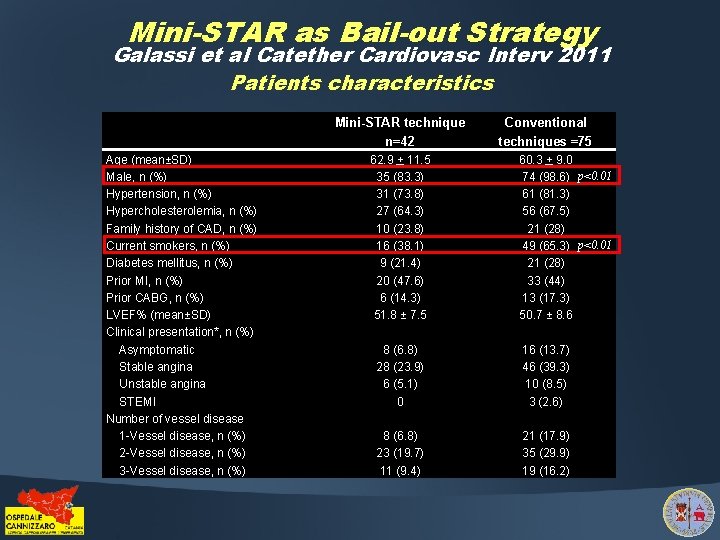
Mini-STAR as Bail-out Strategy Galassi et al Catether Cardiovasc Interv 2011 Patients characteristics Mini-STAR technique n=42 Age (mean±SD) Male, n (%) Hypertension, n (%) Hypercholesterolemia, n (%) Family history of CAD, n (%) Current smokers, n (%) Diabetes mellitus, n (%) Prior MI, n (%) Prior CABG, n (%) LVEF% (mean±SD) Clinical presentation*, n (%) Asymptomatic Stable angina Unstable angina STEMI Number of vessel disease 1 -Vessel disease, n (%) 2 -Vessel disease, n (%) 3 -Vessel disease, n (%) 62. 9 + 11. 5 35 (83. 3) 31 (73. 8) 27 (64. 3) 10 (23. 8) 16 (38. 1) 9 (21. 4) 20 (47. 6) 6 (14. 3) 51. 8 ± 7. 5 Conventional techniques =75 60. 3 + 9. 0 74 (98. 6) p<0. 01 61 (81. 3) 56 (67. 5) 21 (28) 49 (65. 3) p<0. 01 21 (28) 33 (44) 13 (17. 3) 50. 7 ± 8. 6 8 (6. 8) 28 (23. 9) 6 (5. 1) 0 16 (13. 7) 46 (39. 3) 10 (8. 5) 3 (2. 6) 8 (6. 8) 23 (19. 7) 11 (9. 4) 21 (17. 9) 35 (29. 9) 19 (16. 2)
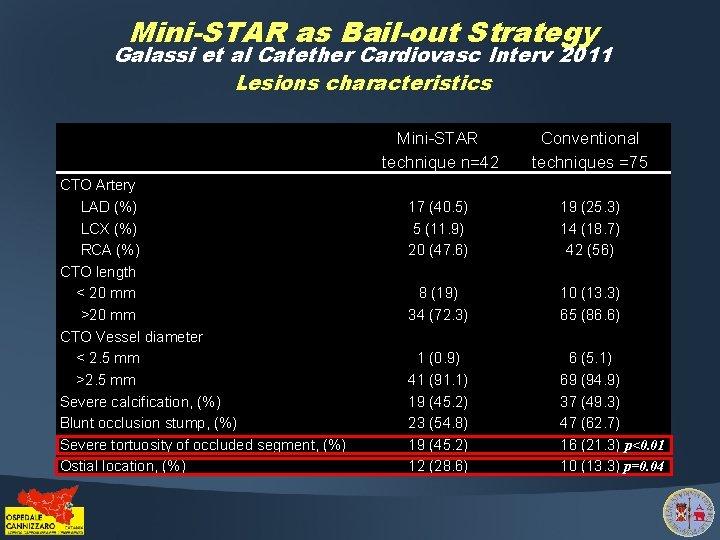
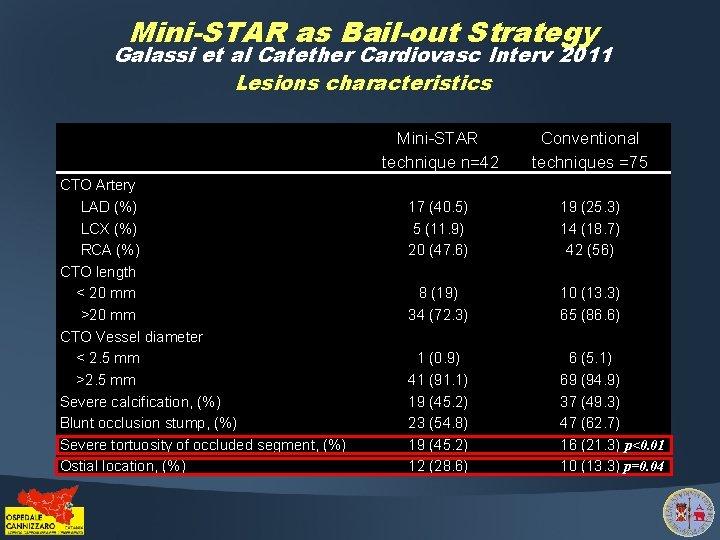
Mini-STAR as Bail-out Strategy Galassi et al Catether Cardiovasc Interv 2011 Lesions characteristics CTO Artery LAD (%) LCX (%) RCA (%) CTO length < 20 mm >20 mm CTO Vessel diameter < 2. 5 mm >2. 5 mm Severe calcification, (%) Blunt occlusion stump, (%) Severe tortuosity of occluded segment, (%) Ostial location, (%) Mini-STAR technique n=42 Conventional techniques =75 17 (40. 5) 5 (11. 9) 20 (47. 6) 19 (25. 3) 14 (18. 7) 42 (56) 8 (19) 34 (72. 3) 10 (13. 3) 65 (86. 6) 1 (0. 9) 41 (91. 1) 19 (45. 2) 23 (54. 8) 19 (45. 2) 12 (28. 6) 6 (5. 1) 69 (94. 9) 37 (49. 3) 47 (62. 7) 16 (21. 3) p<0. 01 10 (13. 3) p=0. 04
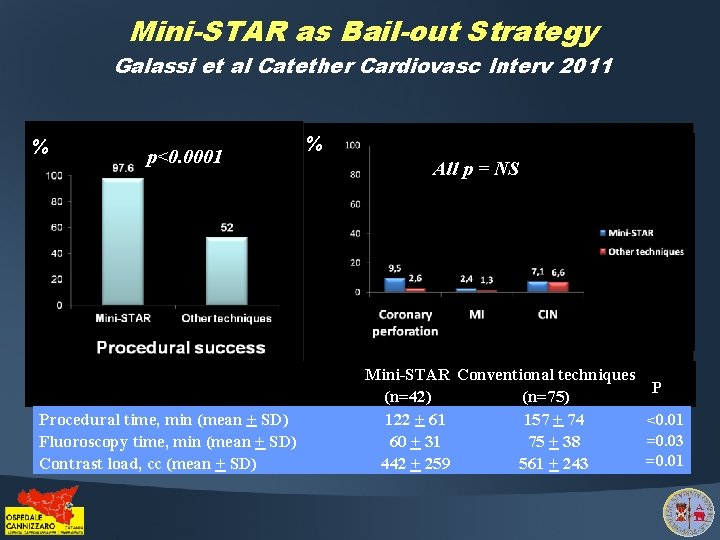
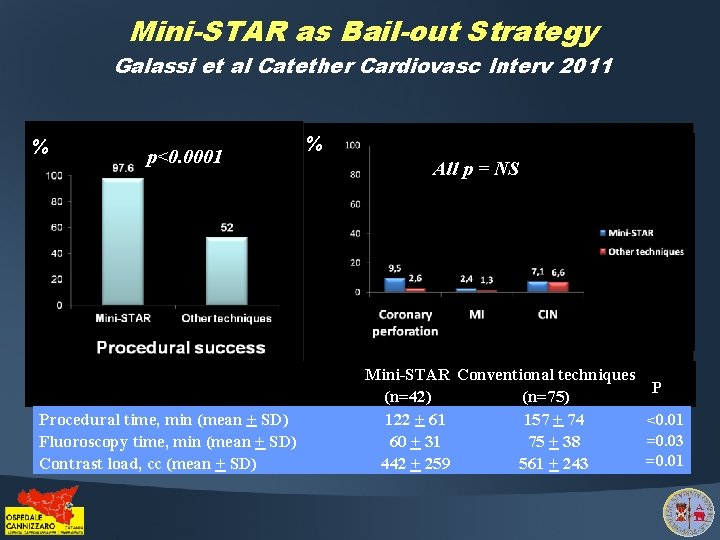
Mini-STAR as Bail-out Strategy Galassi et al Catether Cardiovasc Interv 2011 % p<0. 0001 Procedural time, min (mean + SD) Fluoroscopy time, min (mean + SD) Contrast load, cc (mean + SD) % All p = NS Mini-STAR Conventional techniques (n=42) (n=75) 122 + 61 157 + 74 60 + 31 75 + 38 442 + 259 561 + 243 P <0. 01 =0. 03 =0. 01
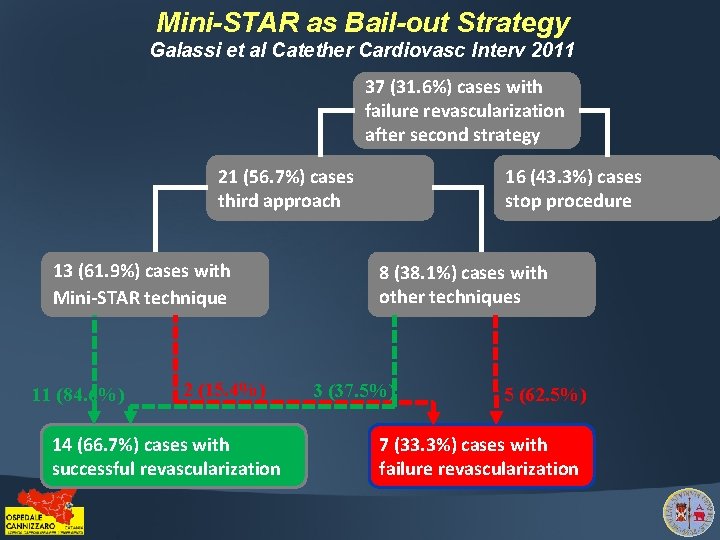
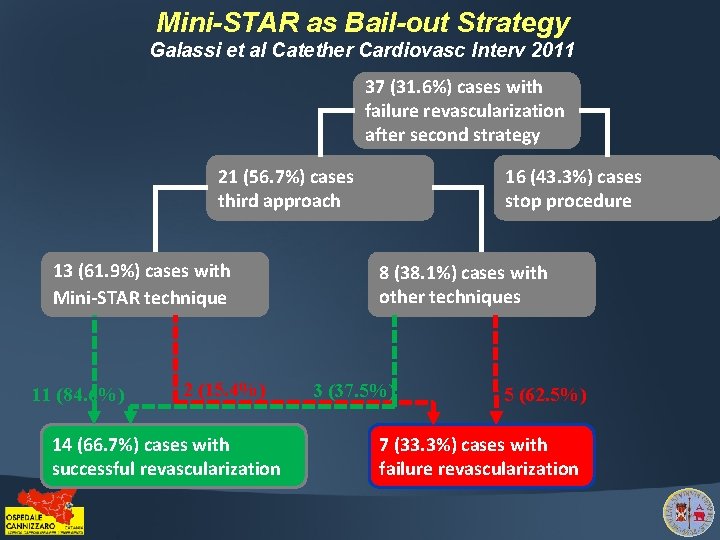
Mini-STAR as Bail-out Strategy Galassi et al Catether Cardiovasc Interv 2011 37 (31. 6%) cases with failure revascularization after second strategy 21 (56. 7%) cases third approach 13 (61. 9%) cases with Mini-STAR technique 11 (84. 6%) 2 (15. 4%) 14 (66. 7%) cases with successful revascularization 16 (43. 3%) cases stop procedure 8 (38. 1%) cases with other techniques 3 (37. 5%) 5 (62. 5%) 7 (33. 3%) cases with failure revascularization
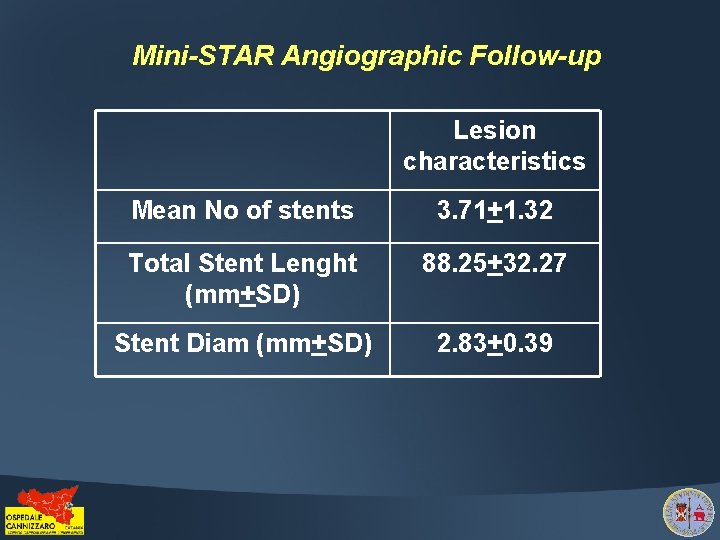
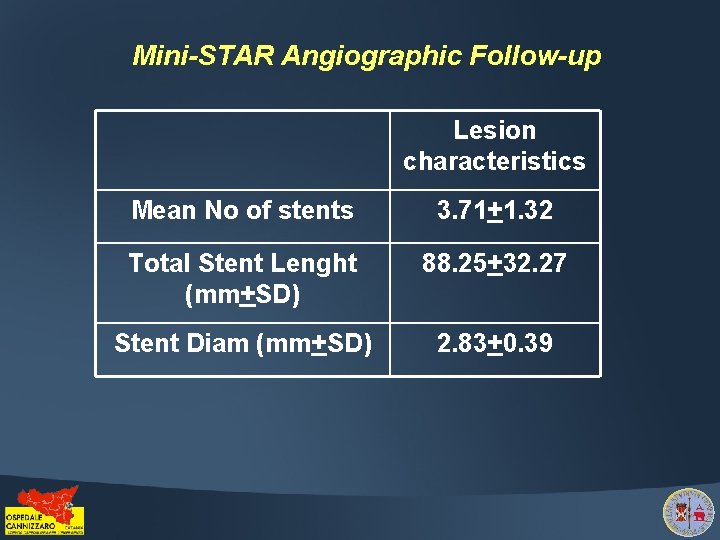
Mini-STAR Angiographic Follow-up Lesion characteristics Mean No of stents 3. 71+1. 32 Total Stent Lenght (mm+SD) 88. 25+32. 27 Stent Diam (mm+SD) 2. 83+0. 39
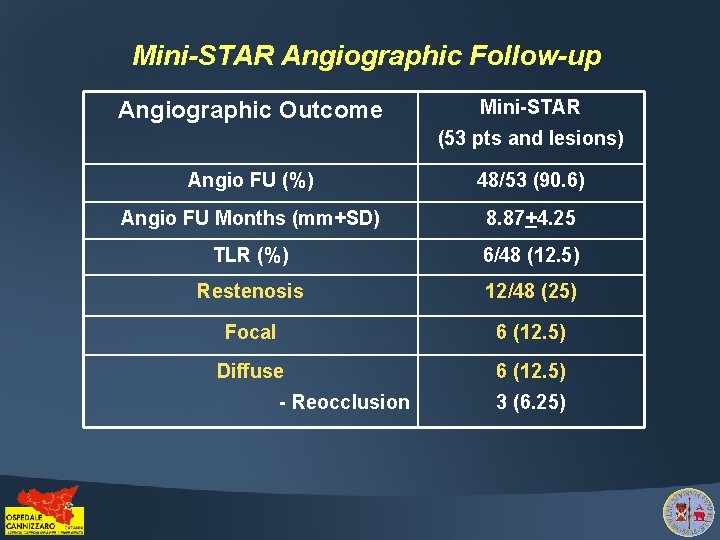
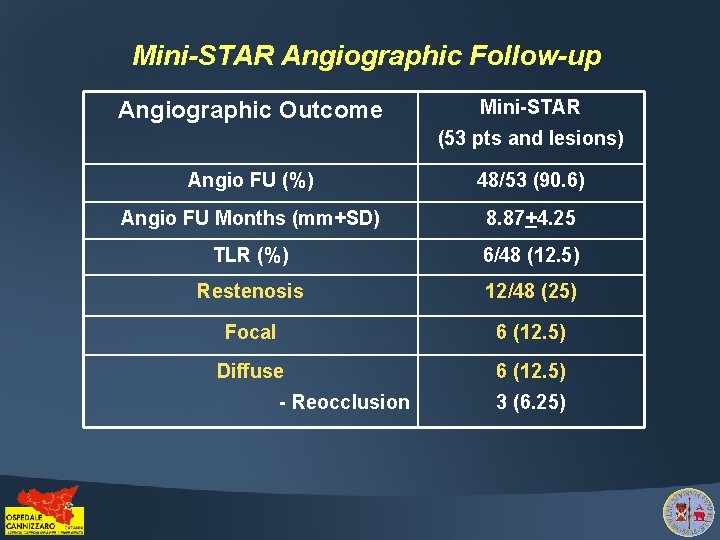
Mini-STAR Angiographic Follow-up Angiographic Outcome Mini-STAR (53 pts and lesions) Angio FU (%) 48/53 (90. 6) Angio FU Months (mm+SD) 8. 87+4. 25 TLR (%) 6/48 (12. 5) Restenosis 12/48 (25) Focal 6 (12. 5) Diffuse 6 (12. 5) - Reocclusion 3 (6. 25)
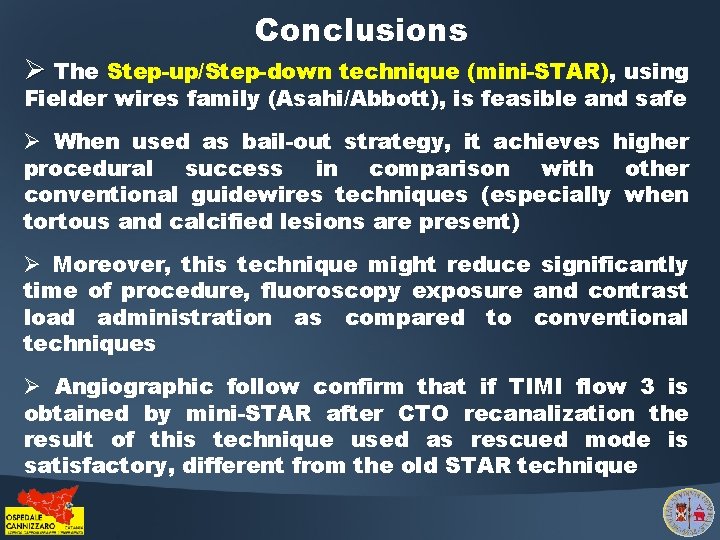
Conclusions Ø The Step-up/Step-down technique (mini-STAR), using Fielder wires family (Asahi/Abbott), is feasible and safe Ø When used as bail-out strategy, it achieves higher procedural success in comparison with other conventional guidewires techniques (especially when tortous and calcified lesions are present) Ø Moreover, this technique might reduce significantly time of procedure, fluoroscopy exposure and contrast load administration as compared to conventional techniques Ø Angiographic follow confirm that if TIMI flow 3 is obtained by mini-STAR after CTO recanalization the result of this technique used as rescued mode is satisfactory, different from the old STAR technique
 Pepe and alfredo are resting on an offshore raft
Pepe and alfredo are resting on an offshore raft Alfredo cristiano
Alfredo cristiano Anisomiopia
Anisomiopia Alfredo marcos
Alfredo marcos Reforma financiera de alfredo gonzález flores
Reforma financiera de alfredo gonzález flores Alfredo cuervo
Alfredo cuervo Alfredo capote
Alfredo capote Alfredo molina triana
Alfredo molina triana Alfredo cuervo barrero
Alfredo cuervo barrero Otg
Otg Alfredo cuervo barrero
Alfredo cuervo barrero Alfredo cuervo barrero
Alfredo cuervo barrero Alfredo ramos martinez
Alfredo ramos martinez What does jaars stand for
What does jaars stand for Alfredo arraut
Alfredo arraut Comic prohibido
Comic prohibido Usenet message alfredo
Usenet message alfredo Alfredo cuervo barrero
Alfredo cuervo barrero Alfredo cuervo barrero
Alfredo cuervo barrero Ies alfredo brañas
Ies alfredo brañas Iepgpe
Iepgpe Alfredo balena
Alfredo balena Alfredo embid
Alfredo embid Alfredo egydio setubal
Alfredo egydio setubal Alfredo chaparro muñoz
Alfredo chaparro muñoz Alfredo alberti
Alfredo alberti Alfredo carpineti
Alfredo carpineti 5 ejemplos de señales sonoras
5 ejemplos de señales sonoras Liquido cefalorraquideo funcion
Liquido cefalorraquideo funcion Alfredo rendon impi
Alfredo rendon impi Alfredo cuervo barrero
Alfredo cuervo barrero Incapaple
Incapaple Alfredo morel
Alfredo morel Alfredo embid
Alfredo embid Alfredo rendon impi
Alfredo rendon impi Alfredo ferrero costa
Alfredo ferrero costa Alfredo embid
Alfredo embid Alfredo marques gubern
Alfredo marques gubern Alfredo marques gubern
Alfredo marques gubern Caracter juridico
Caracter juridico Habitao
Habitao Triage extrahospitalario
Triage extrahospitalario Alfredo cuervo barrero
Alfredo cuervo barrero Alfredo dupasquier incidente
Alfredo dupasquier incidente Antonio alfredo ferreira loureiro
Antonio alfredo ferreira loureiro