Migraine Headache A Patient Case Victoria Celetti WNE

![References 1. IHS Classification [Internet]. The International Headache Society. Oxford, UK. Blackwell Publishing. 2003 References 1. IHS Classification [Internet]. The International Headache Society. Oxford, UK. Blackwell Publishing. 2003](https://slidetodoc.com/presentation_image_h2/02842f3c8975556e8ea04ff40cd080a4/image-29.jpg)
- Slides: 29
Migraine Headache: A Patient Case Victoria Celetti WNE College of Pharmacy, Doctor of Pharmacy Candidate Class of 2016 Victoria. celetti@wne. edu
Learning Objectives • Using a patient case, determine what information is pertinent positive and pertinent negative in order to make a diagnosis • Understand the pathophysiology, signs and symptoms, and diagnosis of a given disease state using a patient case • Determine an appropriate treatment therapy using evidence based medicine • Determine if the initial therapy given to the patient was appropriately treated • Understand the impact of therapy given and what outcome it has on the patient
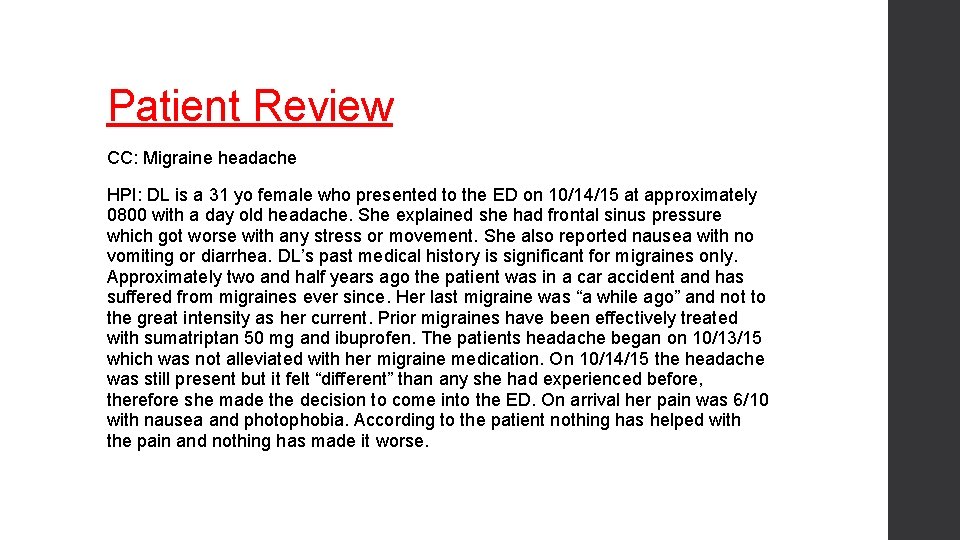
Patient Review CC: Migraine headache HPI: DL is a 31 yo female who presented to the ED on 10/14/15 at approximately 0800 with a day old headache. She explained she had frontal sinus pressure which got worse with any stress or movement. She also reported nausea with no vomiting or diarrhea. DL’s past medical history is significant for migraines only. Approximately two and half years ago the patient was in a car accident and has suffered from migraines ever since. Her last migraine was “a while ago” and not to the great intensity as her current. Prior migraines have been effectively treated with sumatriptan 50 mg and ibuprofen. The patients headache began on 10/13/15 which was not alleviated with her migraine medication. On 10/14/15 the headache was still present but it felt “different” than any she had experienced before, therefore she made the decision to come into the ED. On arrival her pain was 6/10 with nausea and photophobia. According to the patient nothing has helped with the pain and nothing has made it worse.
Patient Review PMH: migraine headaches FH: unknown SH: Full time student, mother to 17 month old, never a smoker, doesn’t use street drugs or alcohol Allergies: NKDA Home medications: Sumatriptan 50 mg: Take 1 tablet by mouth at the onset of headache. May repeat in 2 hours if necessary Multivitamin: take 1 tablet by mouth daily Prenatal vitamin: Take 1 tablet by mouth daily
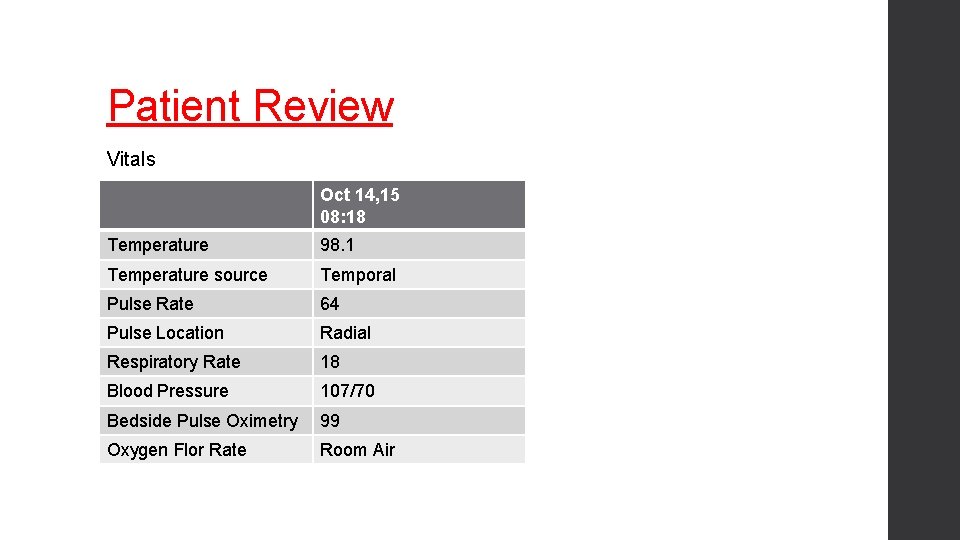
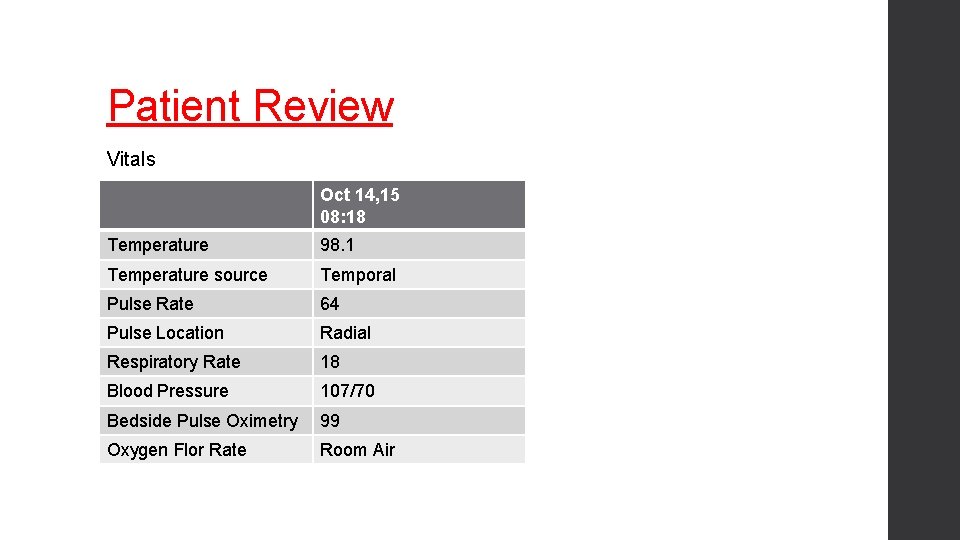
Patient Review Vitals Oct 14, 15 08: 18 Temperature 98. 1 Temperature source Temporal Pulse Rate 64 Pulse Location Radial Respiratory Rate 18 Blood Pressure 107/70 Bedside Pulse Oximetry 99 Oxygen Flor Rate Room Air
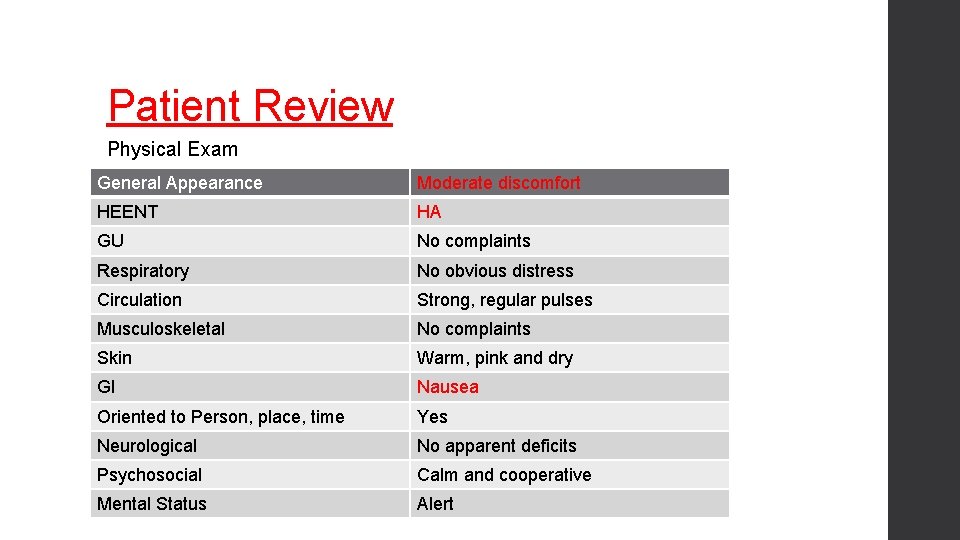
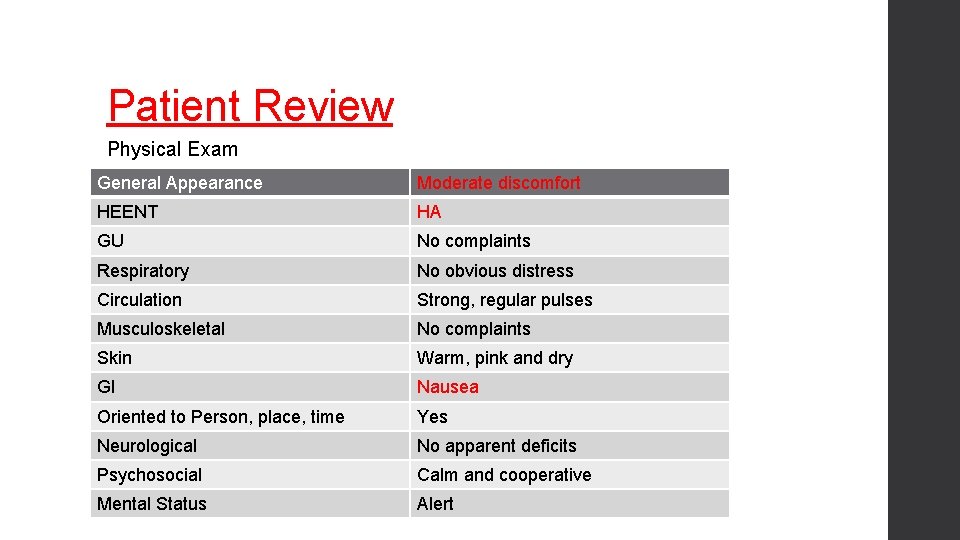
Patient Review Physical Exam General Appearance Moderate discomfort HEENT HA GU No complaints Respiratory No obvious distress Circulation Strong, regular pulses Musculoskeletal No complaints Skin Warm, pink and dry GI Nausea Oriented to Person, place, time Yes Neurological No apparent deficits Psychosocial Calm and cooperative Mental Status Alert
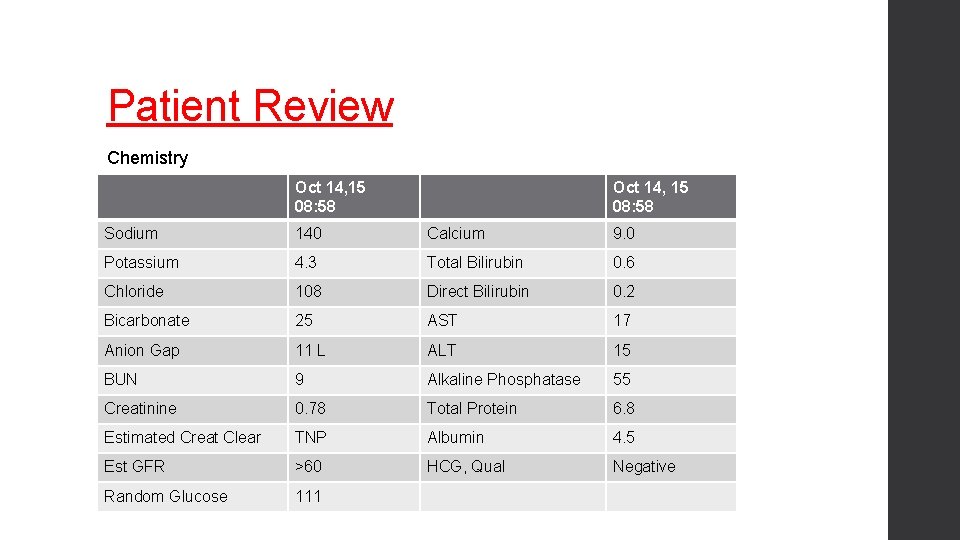
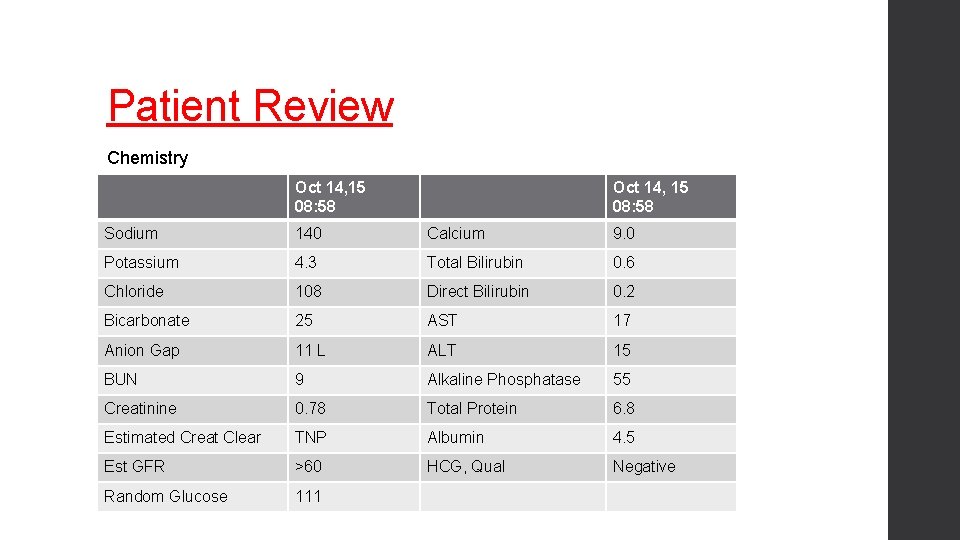
Patient Review Chemistry Oct 14, 15 08: 58 Sodium 140 Calcium 9. 0 Potassium 4. 3 Total Bilirubin 0. 6 Chloride 108 Direct Bilirubin 0. 2 Bicarbonate 25 AST 17 Anion Gap 11 L ALT 15 BUN 9 Alkaline Phosphatase 55 Creatinine 0. 78 Total Protein 6. 8 Estimated Creat Clear TNP Albumin 4. 5 Est GFR >60 HCG, Qual Negative Random Glucose 111
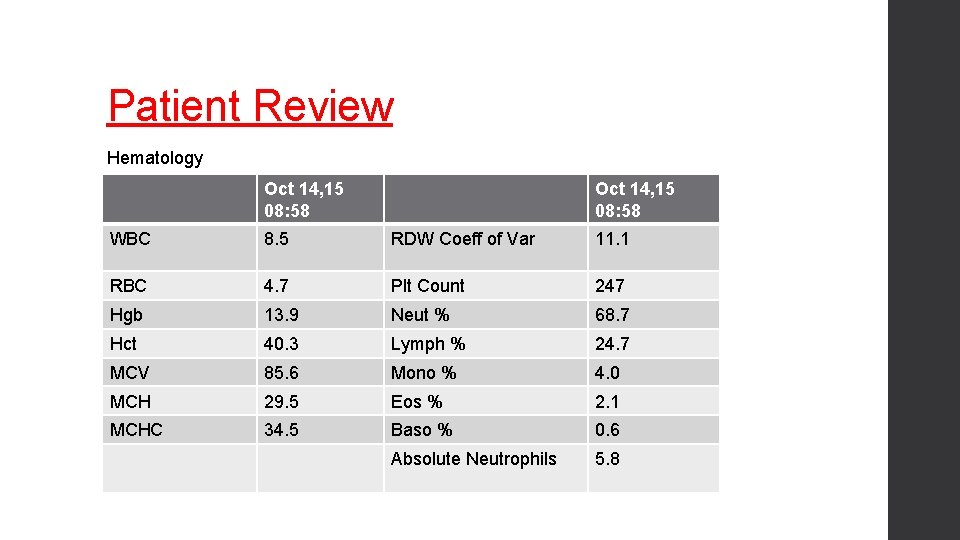
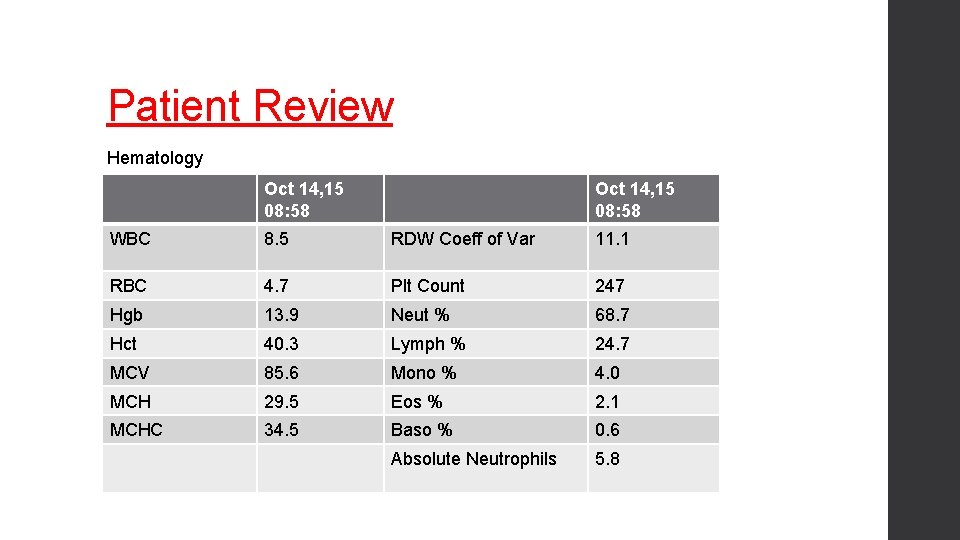
Patient Review Hematology Oct 14, 15 08: 58 WBC 8. 5 RDW Coeff of Var 11. 1 RBC 4. 7 Plt Count 247 Hgb 13. 9 Neut % 68. 7 Hct 40. 3 Lymph % 24. 7 MCV 85. 6 Mono % 4. 0 MCH 29. 5 Eos % 2. 1 MCHC 34. 5 Baso % 0. 6 Absolute Neutrophils 5. 8
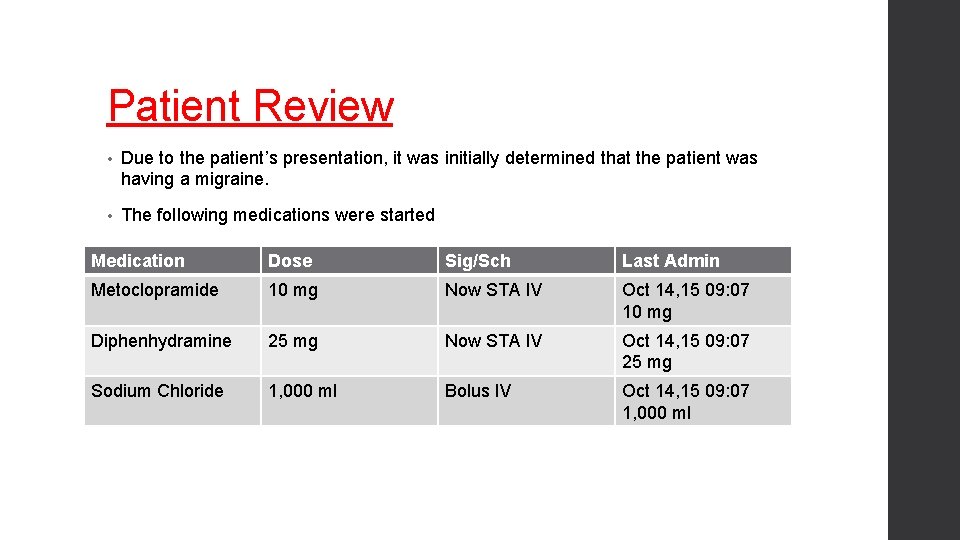
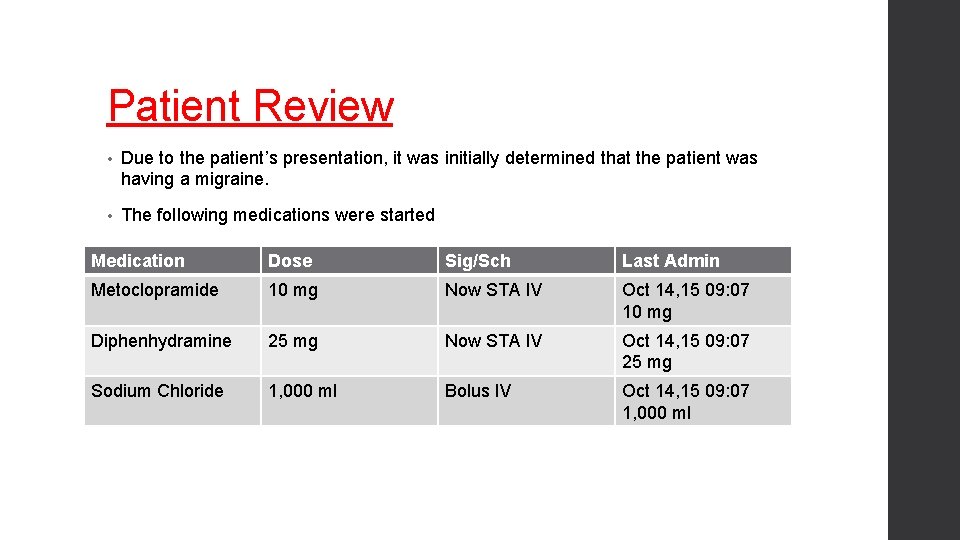
Patient Review • Due to the patient’s presentation, it was initially determined that the patient was having a migraine. • The following medications were started Medication Dose Sig/Sch Last Admin Metoclopramide 10 mg Now STA IV Oct 14, 15 09: 07 10 mg Diphenhydramine 25 mg Now STA IV Oct 14, 15 09: 07 25 mg Sodium Chloride 1, 000 ml Bolus IV Oct 14, 15 09: 07 1, 000 ml
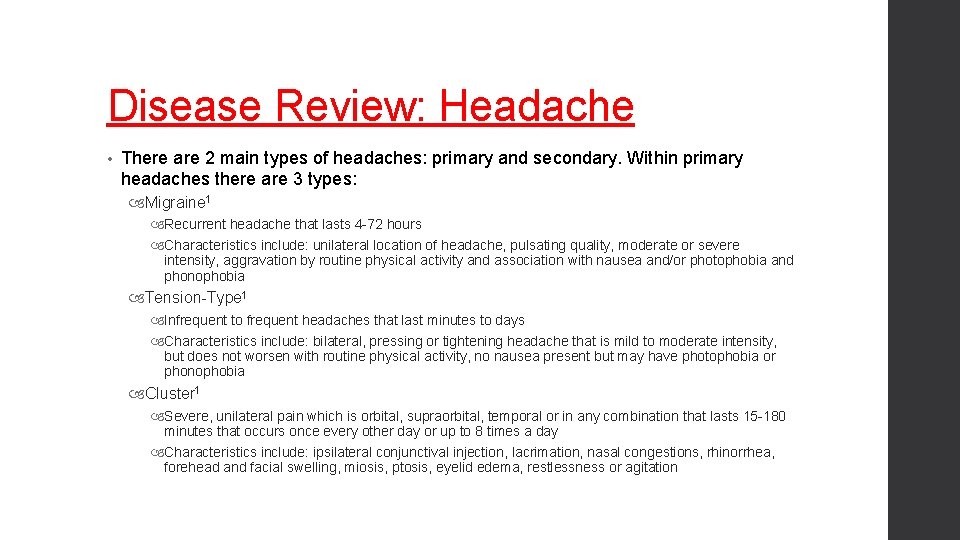
Disease Review: Headache • There are 2 main types of headaches: primary and secondary. Within primary headaches there are 3 types: Migraine 1 Recurrent headache that lasts 4 -72 hours Characteristics include: unilateral location of headache, pulsating quality, moderate or severe intensity, aggravation by routine physical activity and association with nausea and/or photophobia and phonophobia Tension-Type 1 Infrequent to frequent headaches that last minutes to days Characteristics include: bilateral, pressing or tightening headache that is mild to moderate intensity, but does not worsen with routine physical activity, no nausea present but may have photophobia or phonophobia Cluster 1 Severe, unilateral pain which is orbital, supraorbital, temporal or in any combination that lasts 15 -180 minutes that occurs once every other day or up to 8 times a day Characteristics include: ipsilateral conjunctival injection, lacrimation, nasal congestions, rhinorrhea, forehead and facial swelling, miosis, ptosis, eyelid edema, restlessness or agitation
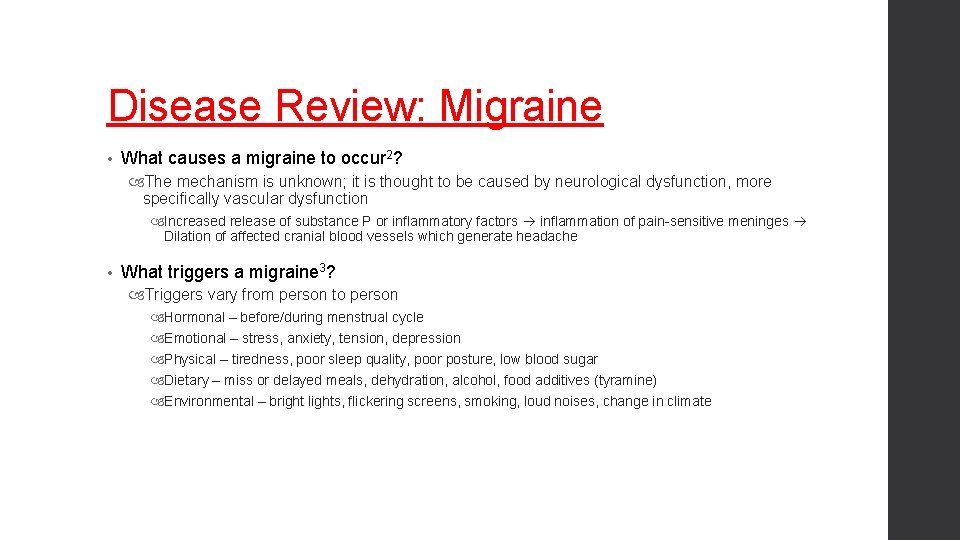
Disease Review: Migraine • What causes a migraine to occur 2? The mechanism is unknown; it is thought to be caused by neurological dysfunction, more specifically vascular dysfunction Increased release of substance P or inflammatory factors inflammation of pain-sensitive meninges Dilation of affected cranial blood vessels which generate headache • What triggers a migraine 3? Triggers vary from person to person Hormonal – before/during menstrual cycle Emotional – stress, anxiety, tension, depression Physical – tiredness, poor sleep quality, poor posture, low blood sugar Dietary – miss or delayed meals, dehydration, alcohol, food additives (tyramine) Environmental – bright lights, flickering screens, smoking, loud noises, change in climate
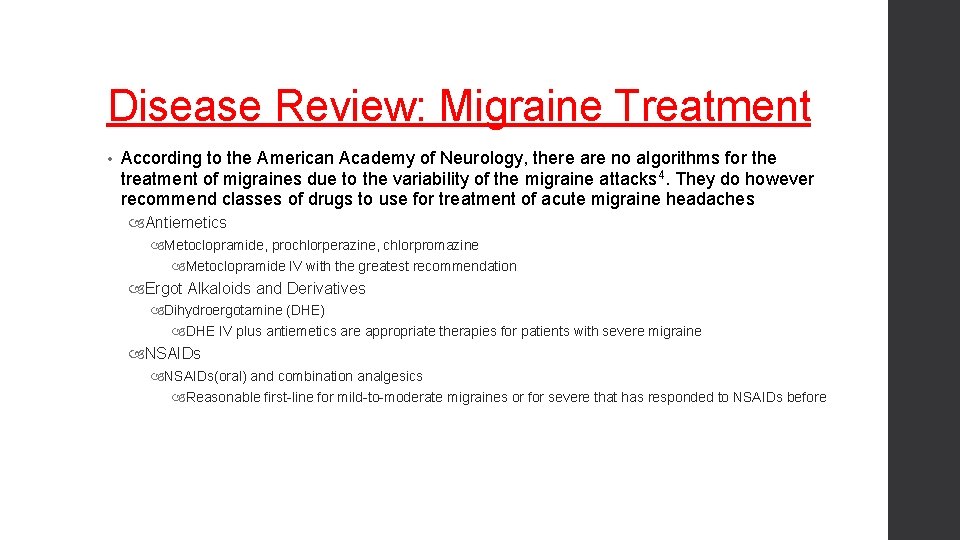
Disease Review: Migraine Treatment • According to the American Academy of Neurology, there are no algorithms for the treatment of migraines due to the variability of the migraine attacks 4. They do however recommend classes of drugs to use for treatment of acute migraine headaches Antiemetics Metoclopramide, prochlorperazine, chlorpromazine Metoclopramide IV with the greatest recommendation Ergot Alkaloids and Derivatives Dihydroergotamine (DHE) DHE IV plus antiemetics are appropriate therapies for patients with severe migraine NSAIDs(oral) and combination analgesics Reasonable first-line for mild-to-moderate migraines or for severe that has responded to NSAIDs before
Disease Review: Migraine Treatment • Opiates IM/IV May be considered for rescue therapy in a supervised setting for acute migraine • Triptans Naratriptan, rizatriptan, sumatriptan, zolmitriptan Triptans are effective and an appropriate treatment choice for moderate-to-severe migraine
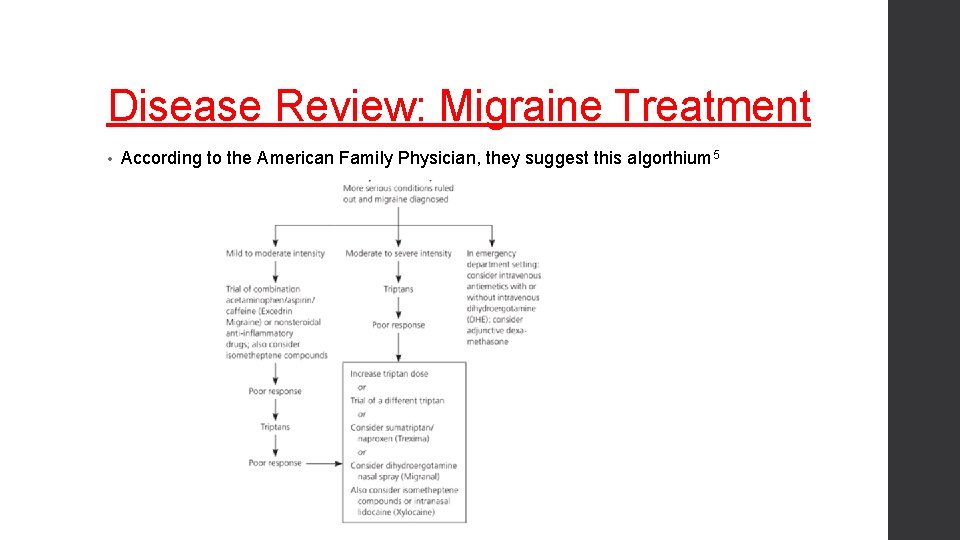
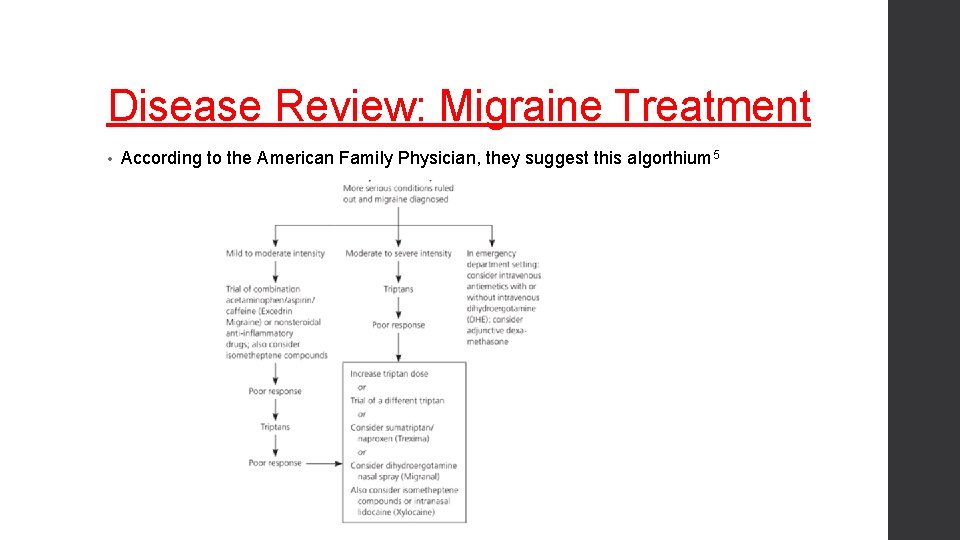
Disease Review: Migraine Treatment • According to the American Family Physician, they suggest this algorthium 5
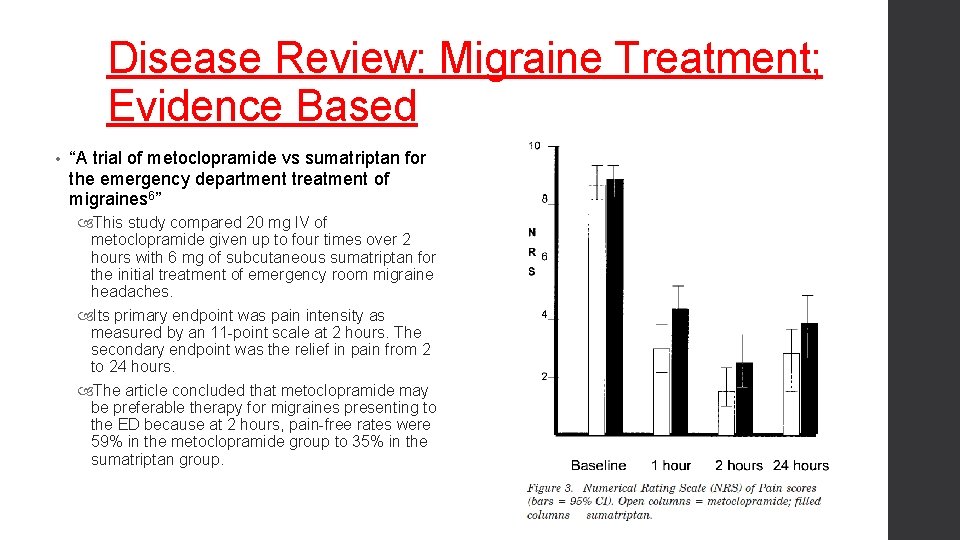
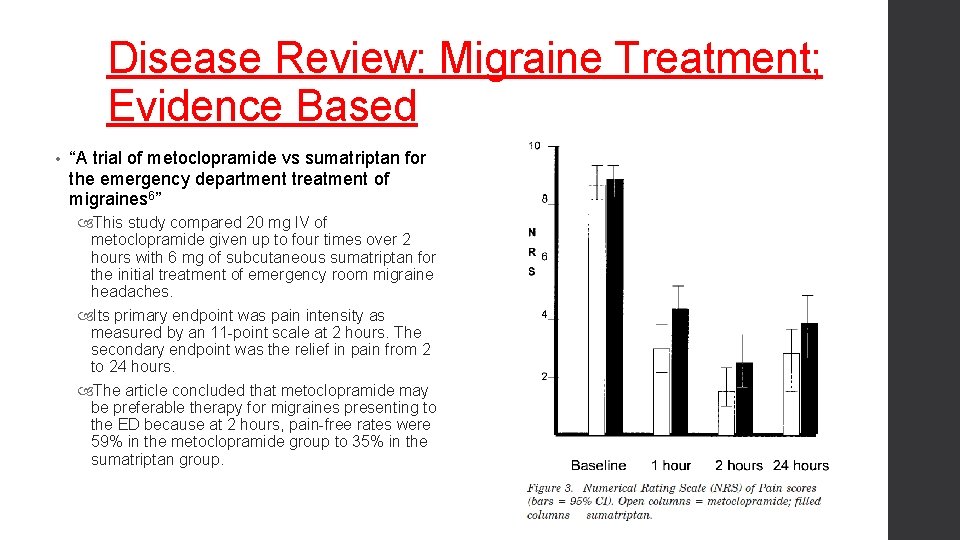
Disease Review: Migraine Treatment; Evidence Based • “A trial of metoclopramide vs sumatriptan for the emergency department treatment of migraines 6” This study compared 20 mg IV of metoclopramide given up to four times over 2 hours with 6 mg of subcutaneous sumatriptan for the initial treatment of emergency room migraine headaches. Its primary endpoint was pain intensity as measured by an 11 -point scale at 2 hours. The secondary endpoint was the relief in pain from 2 to 24 hours. The article concluded that metoclopramide may be preferable therapy for migraines presenting to the ED because at 2 hours, pain-free rates were 59% in the metoclopramide group to 35% in the sumatriptan group.
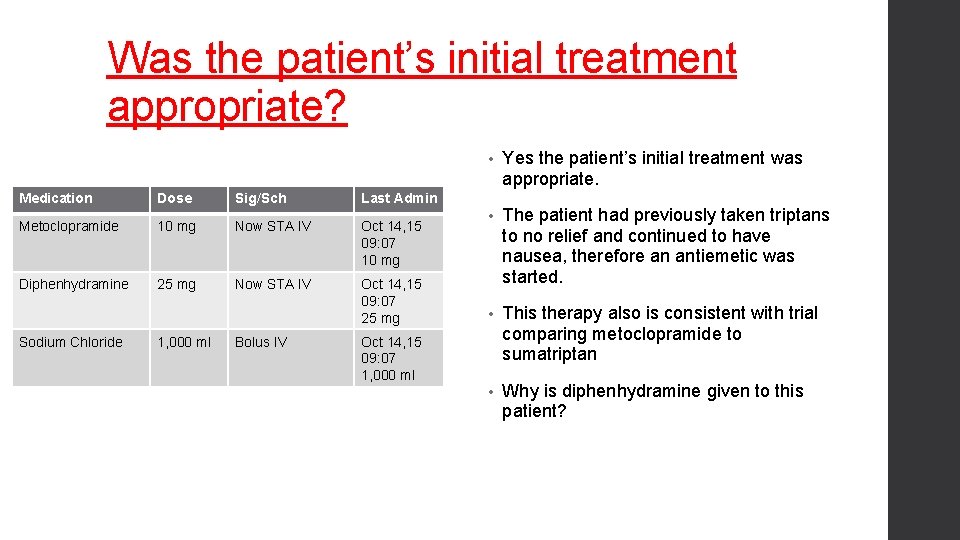
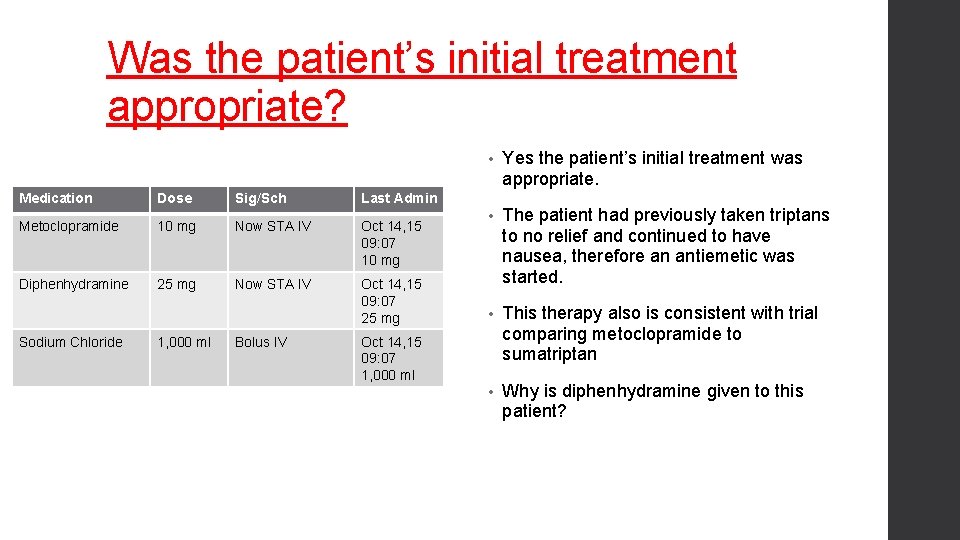
Was the patient’s initial treatment appropriate? Medication Dose Sig/Sch Last Admin Metoclopramide 10 mg Now STA IV Oct 14, 15 09: 07 10 mg Diphenhydramine 25 mg Now STA IV Oct 14, 15 09: 07 25 mg Sodium Chloride 1, 000 ml Bolus IV • Yes the patient’s initial treatment was appropriate. • The patient had previously taken triptans to no relief and continued to have nausea, therefore an antiemetic was started. • This therapy also is consistent with trial comparing metoclopramide to sumatriptan • Why is diphenhydramine given to this patient? Oct 14, 15 09: 07 1, 000 ml
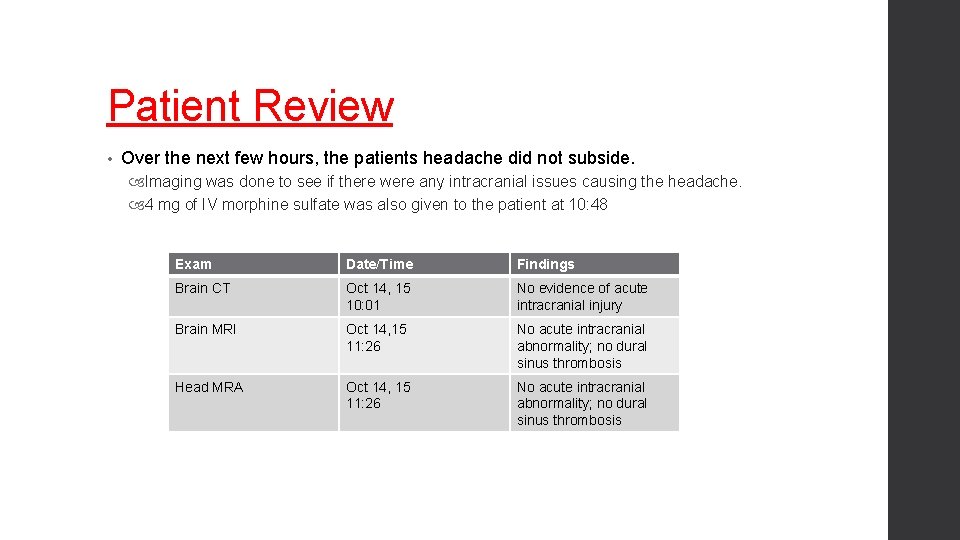
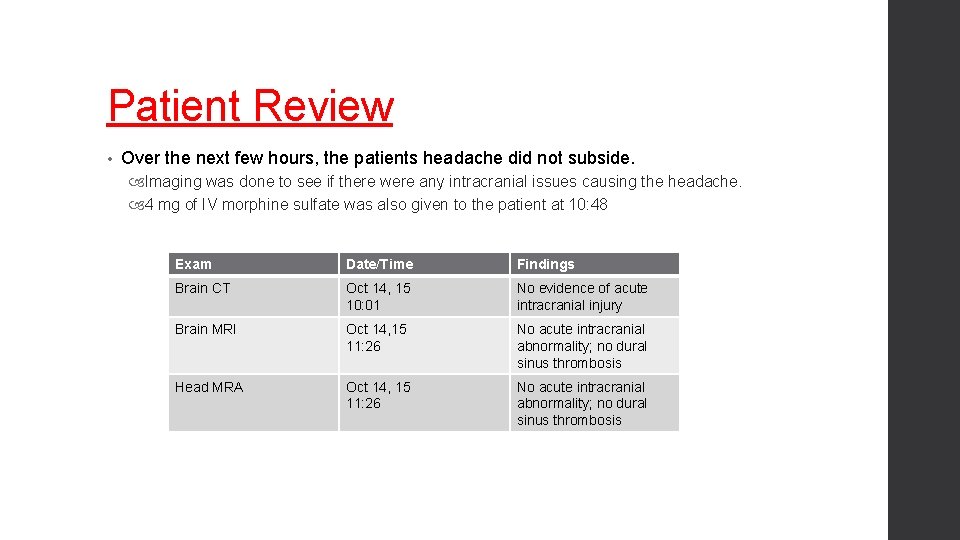
Patient Review • Over the next few hours, the patients headache did not subside. Imaging was done to see if there were any intracranial issues causing the headache. 4 mg of IV morphine sulfate was also given to the patient at 10: 48 Exam Date/Time Findings Brain CT Oct 14, 15 10: 01 No evidence of acute intracranial injury Brain MRI Oct 14, 15 11: 26 No acute intracranial abnormality; no dural sinus thrombosis Head MRA Oct 14, 15 11: 26 No acute intracranial abnormality; no dural sinus thrombosis
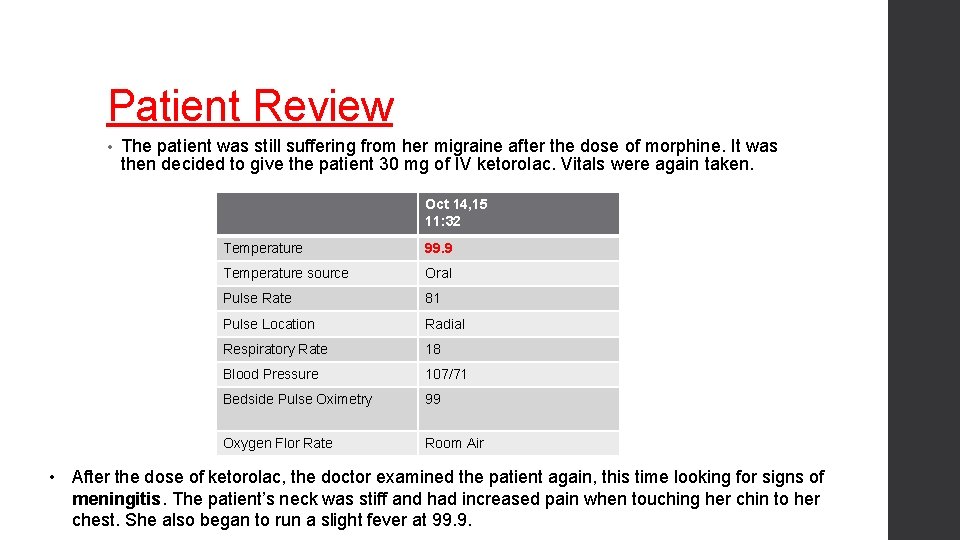
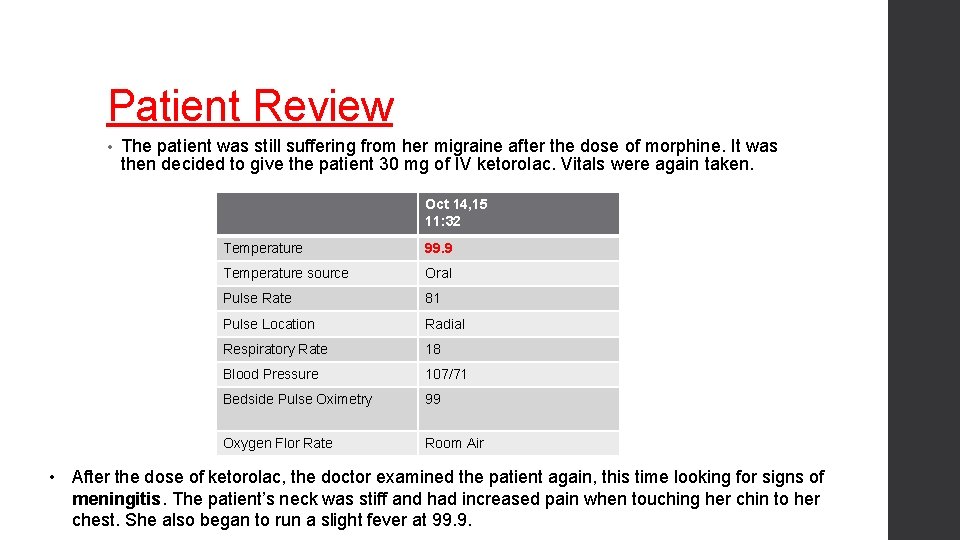
Patient Review • The patient was still suffering from her migraine after the dose of morphine. It was then decided to give the patient 30 mg of IV ketorolac. Vitals were again taken. Oct 14, 15 11: 32 Temperature 99. 9 Temperature source Oral Pulse Rate 81 Pulse Location Radial Respiratory Rate 18 Blood Pressure 107/71 Bedside Pulse Oximetry 99 Oxygen Flor Rate Room Air • After the dose of ketorolac, the doctor examined the patient again, this time looking for signs of meningitis. The patient’s neck was stiff and had increased pain when touching her chin to her chest. She also began to run a slight fever at 99. 9.
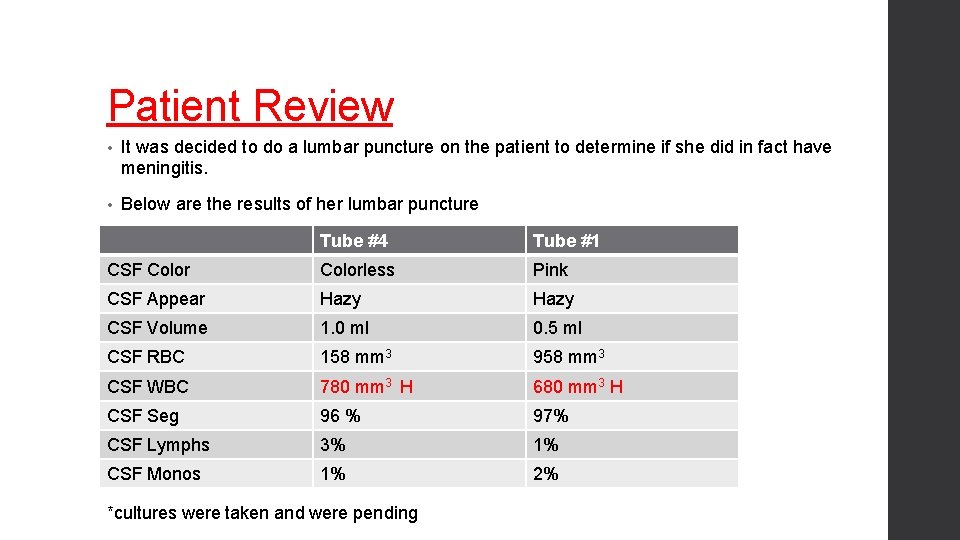
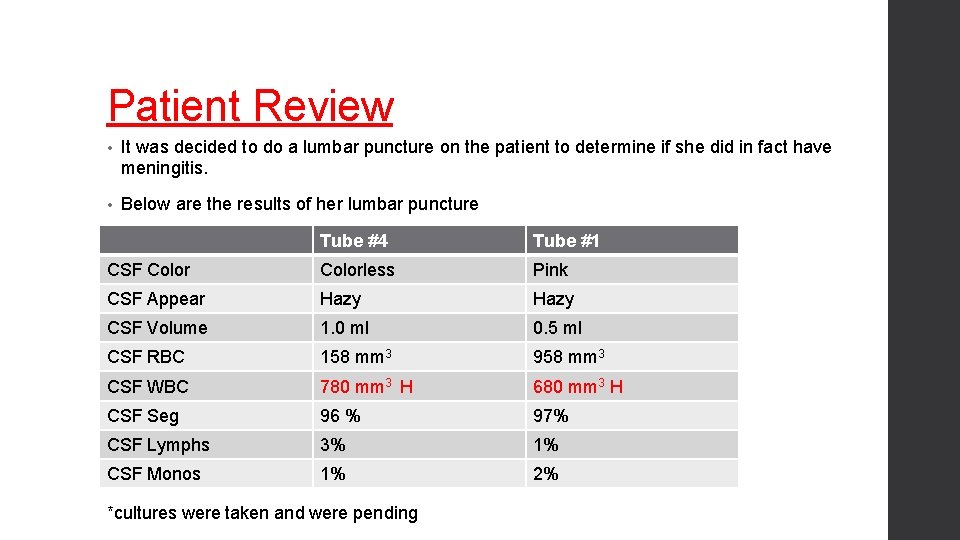
Patient Review • It was decided to do a lumbar puncture on the patient to determine if she did in fact have meningitis. • Below are the results of her lumbar puncture Tube #4 Tube #1 CSF Colorless Pink CSF Appear Hazy CSF Volume 1. 0 ml 0. 5 ml CSF RBC 158 mm 3 958 mm 3 CSF WBC 780 mm 3 H 680 mm 3 H CSF Seg 96 % 97% CSF Lymphs 3% 1% CSF Monos 1% 2% *cultures were taken and were pending
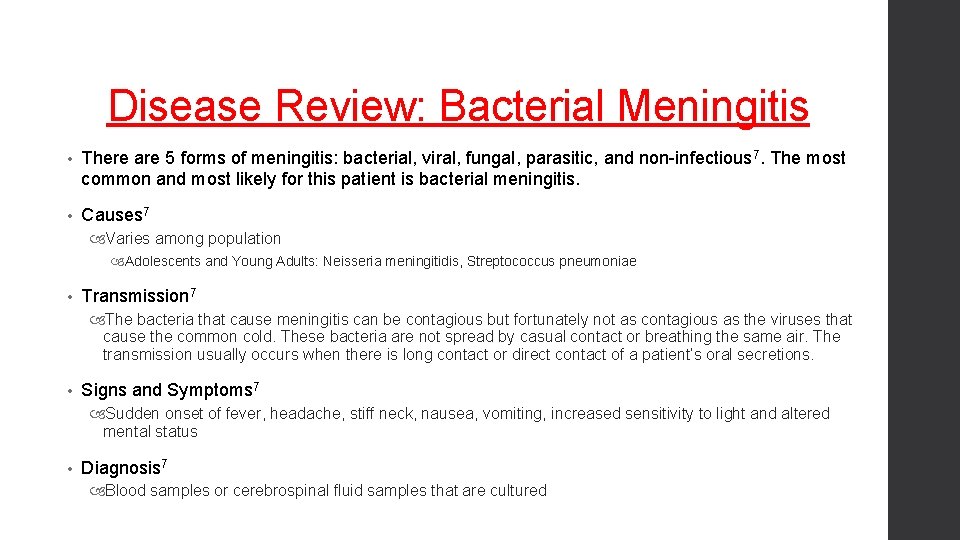
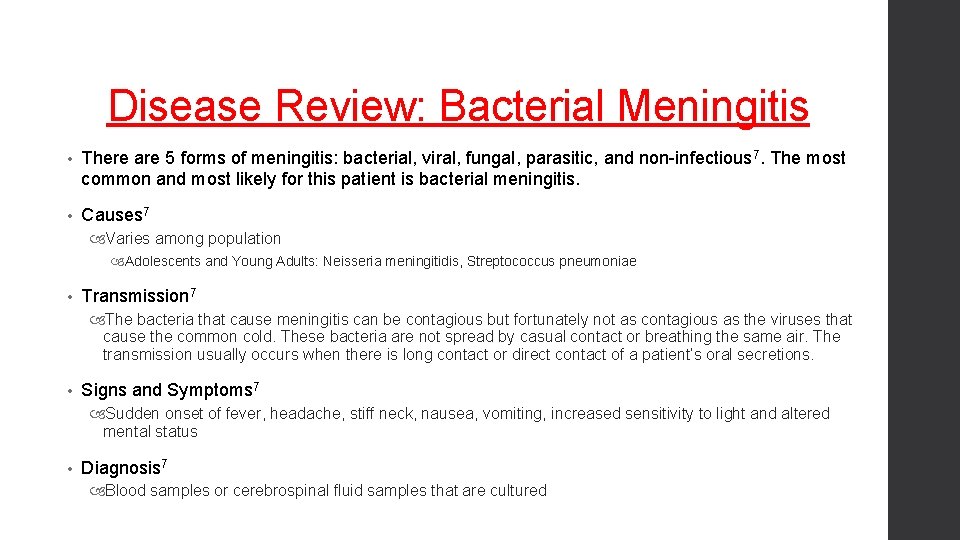
Disease Review: Bacterial Meningitis • There are 5 forms of meningitis: bacterial, viral, fungal, parasitic, and non-infectious 7. The most common and most likely for this patient is bacterial meningitis. • Causes 7 Varies among population Adolescents and Young Adults: Neisseria meningitidis, Streptococcus pneumoniae • Transmission 7 The bacteria that cause meningitis can be contagious but fortunately not as contagious as the viruses that cause the common cold. These bacteria are not spread by casual contact or breathing the same air. The transmission usually occurs when there is long contact or direct contact of a patient’s oral secretions. • Signs and Symptoms 7 Sudden onset of fever, headache, stiff neck, nausea, vomiting, increased sensitivity to light and altered mental status • Diagnosis 7 Blood samples or cerebrospinal fluid samples that are cultured
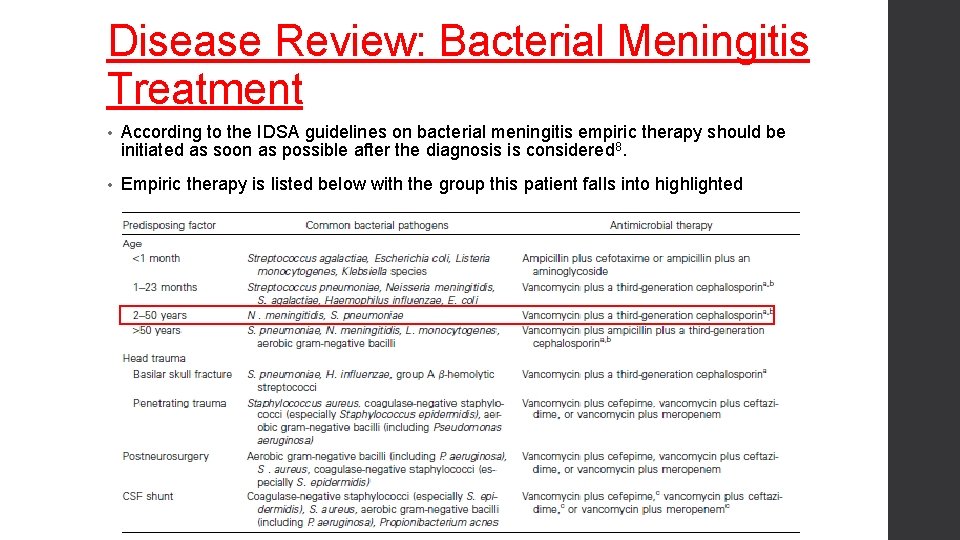
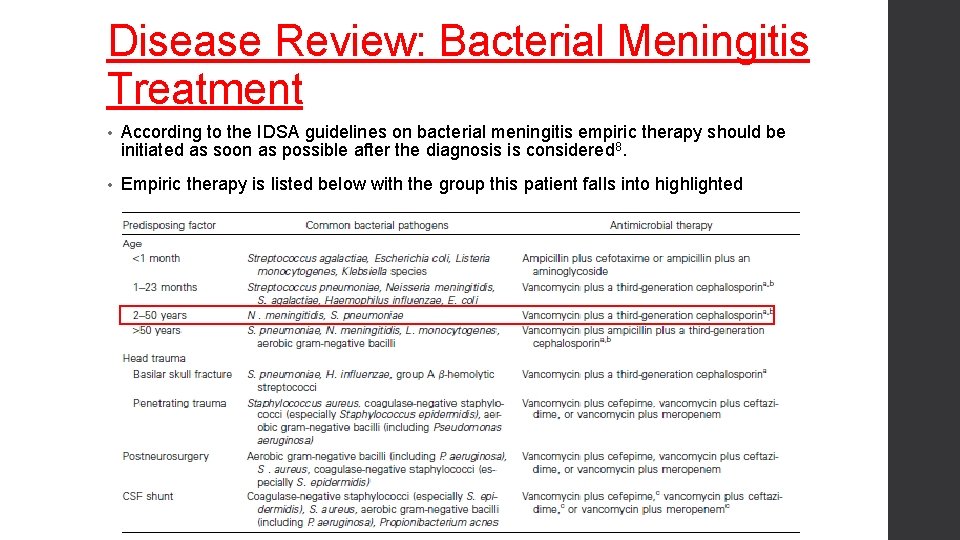
Disease Review: Bacterial Meningitis Treatment • According to the IDSA guidelines on bacterial meningitis empiric therapy should be initiated as soon as possible after the diagnosis is considered 8. • Empiric therapy is listed below with the group this patient falls into highlighted
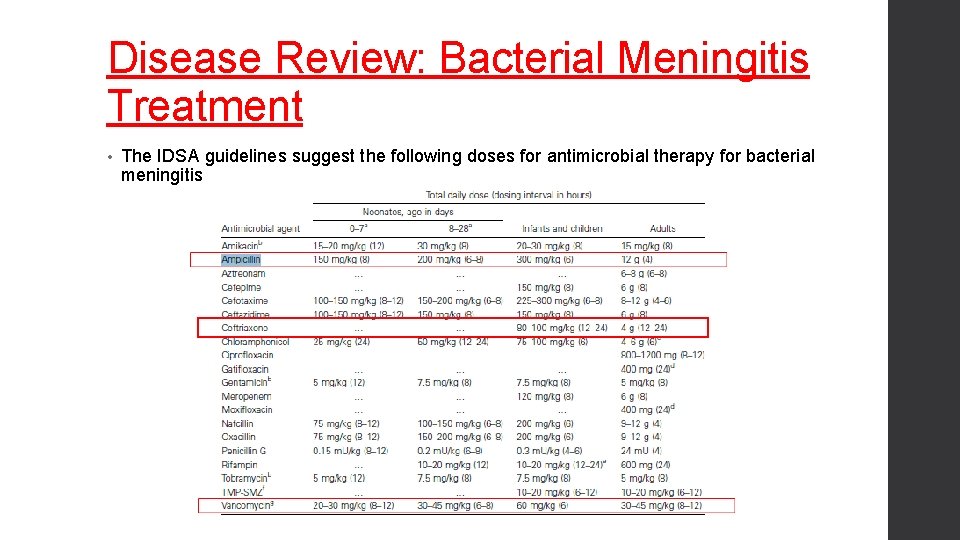
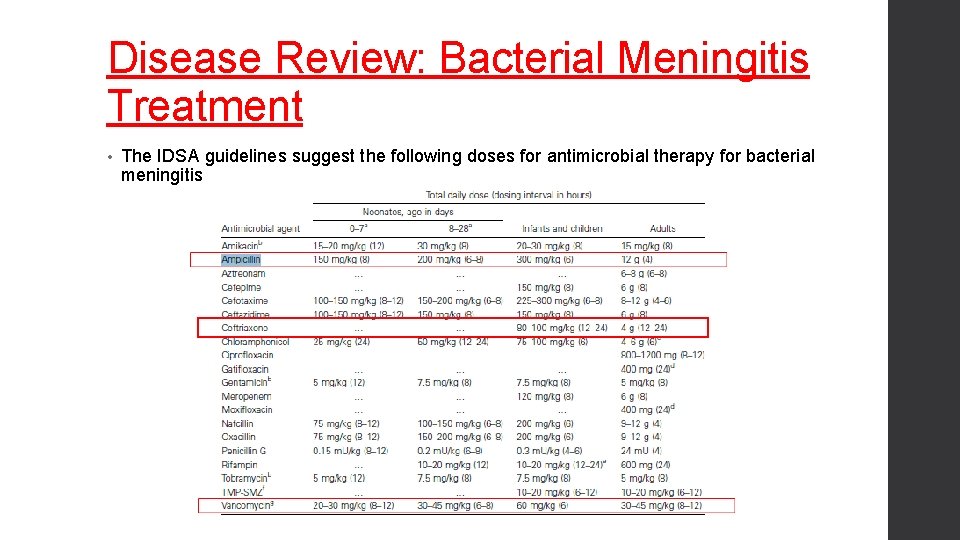
Disease Review: Bacterial Meningitis Treatment • The IDSA guidelines suggest the following doses for antimicrobial therapy for bacterial meningitis
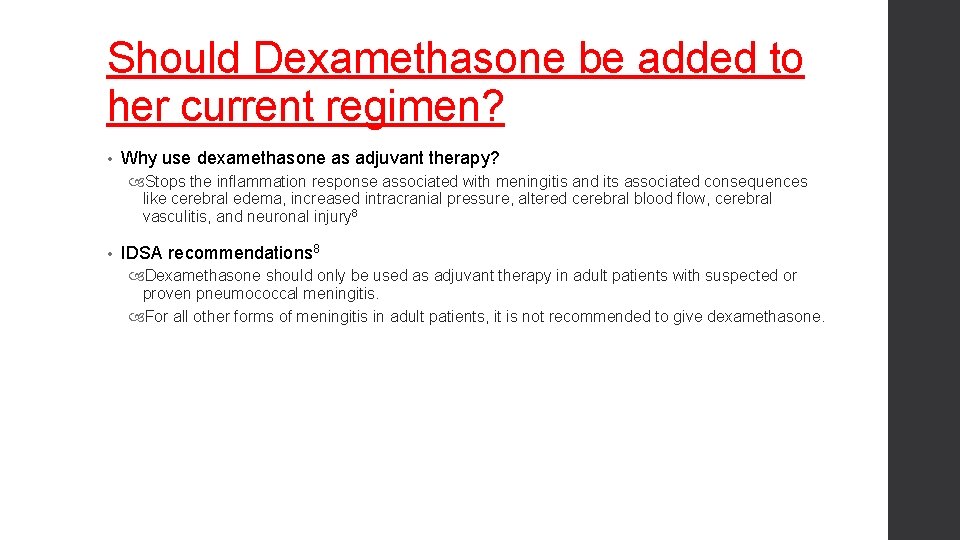
Should Dexamethasone be added to her current regimen? • Why use dexamethasone as adjuvant therapy? Stops the inflammation response associated with meningitis and its associated consequences like cerebral edema, increased intracranial pressure, altered cerebral blood flow, cerebral vasculitis, and neuronal injury 8 • IDSA recommendations 8 Dexamethasone should only be used as adjuvant therapy in adult patients with suspected or proven pneumococcal meningitis. For all other forms of meningitis in adult patients, it is not recommended to give dexamethasone.
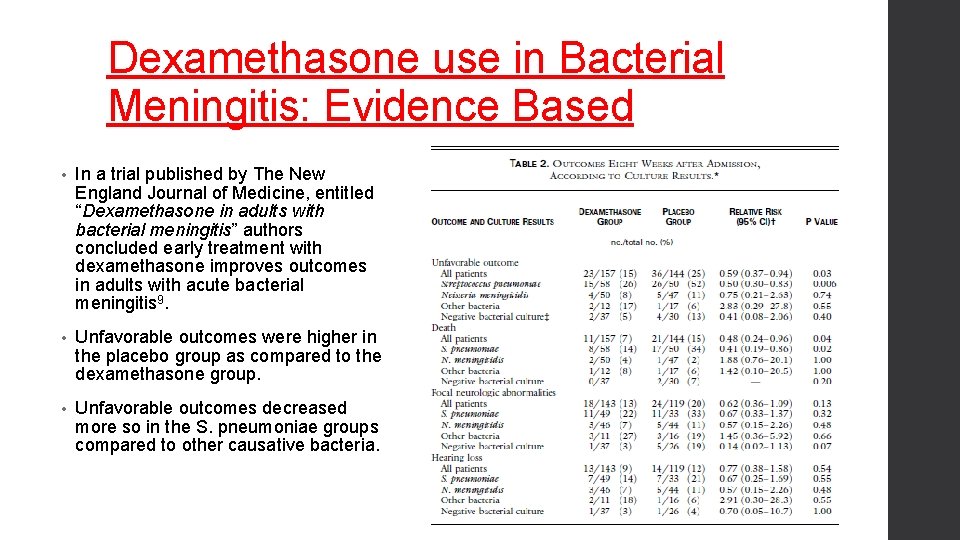
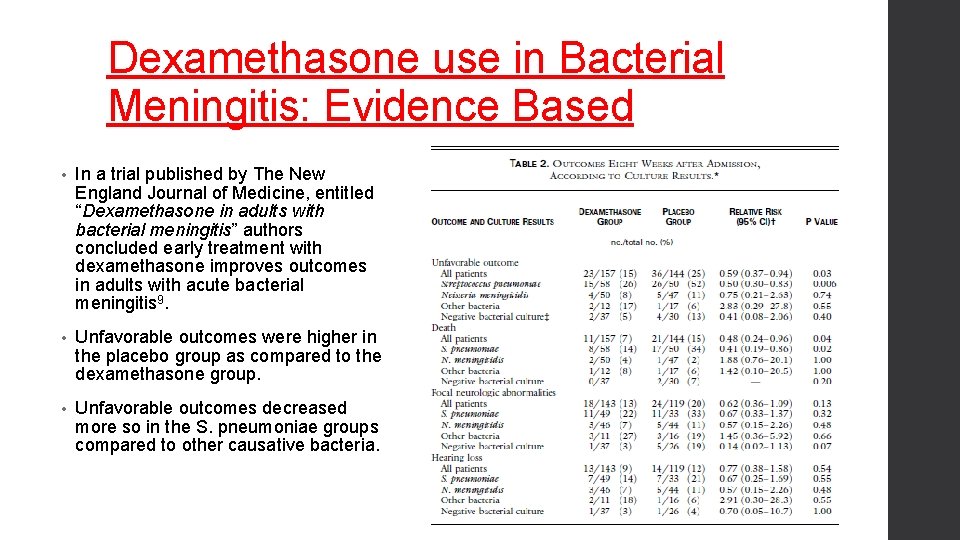
Dexamethasone use in Bacterial Meningitis: Evidence Based • In a trial published by The New England Journal of Medicine, entitled “Dexamethasone in adults with bacterial meningitis” authors concluded early treatment with dexamethasone improves outcomes in adults with acute bacterial meningitis 9. • Unfavorable outcomes were higher in the placebo group as compared to the dexamethasone group. • Unfavorable outcomes decreased more so in the S. pneumoniae groups compared to other causative bacteria.
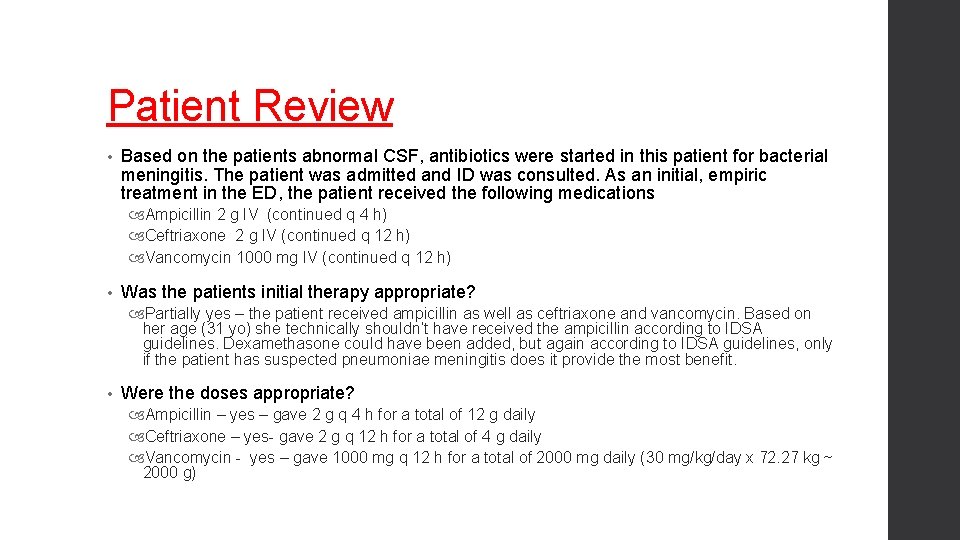
Patient Review • Based on the patients abnormal CSF, antibiotics were started in this patient for bacterial meningitis. The patient was admitted and ID was consulted. As an initial, empiric treatment in the ED, the patient received the following medications Ampicillin 2 g IV (continued q 4 h) Ceftriaxone 2 g IV (continued q 12 h) Vancomycin 1000 mg IV (continued q 12 h) • Was the patients initial therapy appropriate? Partially yes – the patient received ampicillin as well as ceftriaxone and vancomycin. Based on her age (31 yo) she technically shouldn’t have received the ampicillin according to IDSA guidelines. Dexamethasone could have been added, but again according to IDSA guidelines, only if the patient has suspected pneumoniae meningitis does it provide the most benefit. • Were the doses appropriate? Ampicillin – yes – gave 2 g q 4 h for a total of 12 g daily Ceftriaxone – yes- gave 2 g q 12 h for a total of 4 g daily Vancomycin - yes – gave 1000 mg q 12 h for a total of 2000 mg daily (30 mg/kg/day x 72. 27 kg ~ 2000 g)
Patient Outcome • The patient was admitted for further evaluation and follow up. • Cultures did come back with only 1 colony of Staphylococcus, determining the patient did not have bacterial meningitis, but did have some kind of atypical meningitis. • A cause is still unknown; it was speculated that the patient may have Lyme disease meningitis, therefore doxycycline was added to her regimen of antibiotics and ampicillin was taken away. Antibody assays came back relieving she did not have Lyme disease. • Next doctors questioned West Nile, labs came back negative. Doctors stopped vancomycin, ceftriaxone, and doxycycline, but started Augmentin 875/125 mg twice a day for 10 days for the small amount of staph detected in her CSF. The patient was discharged on Augmentin on Oct 16, 2015.
Counseling Points • What are some counseling points for Augmentin 10? • This drug may decrease the effectiveness of oral contraceptives- back up birth control is needed during antibiotic course and 7 days afterwards • This medication may cause an upset stomach such as nausea, vomiting or diarrhea • Augmentin should be taken at the start of a meal (should be taken with food)

Any Questions?
![References 1 IHS Classification Internet The International Headache Society Oxford UK Blackwell Publishing 2003 References 1. IHS Classification [Internet]. The International Headache Society. Oxford, UK. Blackwell Publishing. 2003](https://slidetodoc.com/presentation_image_h2/02842f3c8975556e8ea04ff40cd080a4/image-29.jpg)
References 1. IHS Classification [Internet]. The International Headache Society. Oxford, UK. Blackwell Publishing. 2003 -2005. Available from: http: //ihsclassification. org/en/02_klassifikation/ 2. Charles A, Brennan KC. The neurobiology of migraine. Handb Clin Neurol. 2010; 97: 99 -108. 3. Mayo Clinic [Internet]. Migraine-Causes. Minnesota, US. 2015 Feb. Available from: http: //www. mayoclinic. org/diseasesconditions/migraine-headache/basics/causes/con-20026358 4. Matchar DB, Young WB, Rosenberg JH, et al. Evidence-Based Guidelines for Migraine Headache in Primary Care Setting: Pharmacological Management of Acute Attacks. American Academy of Neurology. April 2000. 5. Gilmore B, Michael M. Treatment of Acute Migraine Headache. Am Fam Physician. 2011 Feb; 83(3): 271 -280. 6. Friedman BW, Corbo J, Lipton RB, et al. A trial of metoclopramide vs sumatriptan for the emergency department treatment of migraines. Neurology. 2005; 64: 463 -468 7. CDC [Internet]. Bacterial Meningitis. Atlanta, GA. 2014 April. Available from: http: //www. cdc. gov/meningitis/bacterial. html 8. Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice Guidelines for the Management of Bacterial Meningitis. IDSA. 2004 August. 39: 12671284. 9. De Gans J, Diederik V. Dexamethsone in Adults with Bacterial Meningitis. N Engl J Med. 2002 Nov 14; 347 (20): 1549 -1556 10. Augmentin. In: Lexi-Drugs [database on Internet]. Hudson (OH). 1975 -2015: Lexi-Comp, Inc; 2015 [cited 19 Oct 2015].
 Postdrome symptoms
Postdrome symptoms Centros alternativos de los 7 habitos
Centros alternativos de los 7 habitos Best case worst case average case
Best case worst case average case Marek giergiczny
Marek giergiczny Wne self service
Wne self service Marek giergiczny
Marek giergiczny Matuszczak wne
Matuszczak wne Self-service wne
Self-service wne Patient 2 patient
Patient 2 patient Osteopern
Osteopern Brepharitis
Brepharitis Past pointing test positive
Past pointing test positive Sunct
Sunct Headache chart
Headache chart Prodrome migraine
Prodrome migraine Syncope vs seizure
Syncope vs seizure Prodromen epilepsie
Prodromen epilepsie Aimovig storage
Aimovig storage Migraine avec aura définition
Migraine avec aura définition Pathophysiology of migraine
Pathophysiology of migraine Symptoms of true love
Symptoms of true love Migraine chocolate mnemonic
Migraine chocolate mnemonic Migraine
Migraine Ichd 3 vestibular migraine
Ichd 3 vestibular migraine Retinal migraine
Retinal migraine Dr abdul
Dr abdul New york headache center
New york headache center Benefits of gyan mudra
Benefits of gyan mudra Infosys sabbatical leave
Infosys sabbatical leave Right side headache
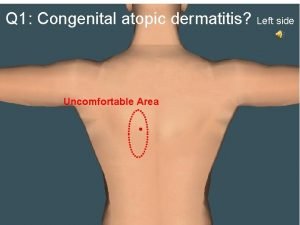
Right side headache