Marc Riedl MD MS Professor of Medicine Clinical


- Slides: 49


Marc Riedl, MD, MS Professor of Medicine Clinical Director, US HAEA Angioedema Center Division of Rheumatology, Allergy & Immunology University of California, San Diego
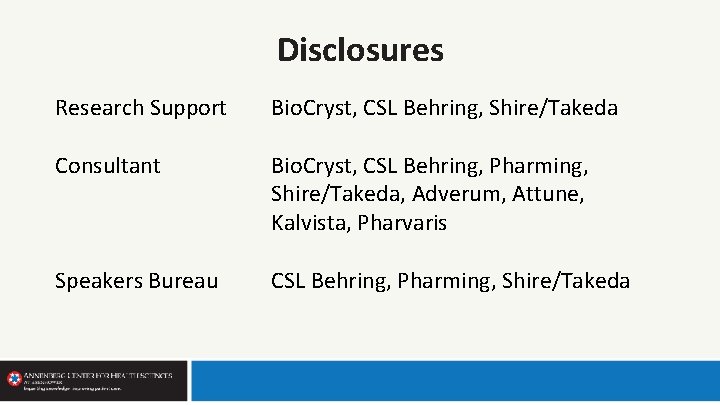
Disclosures Research Support Bio. Cryst, CSL Behring, Shire/Takeda Consultant Bio. Cryst, CSL Behring, Pharming, Shire/Takeda, Adverum, Attune, Kalvista, Pharvaris Speakers Bureau CSL Behring, Pharming, Shire/Takeda
Learning Objectives • Describe signs and symptoms that are suggestive of hereditary angioedema (HAE) • Identify laboratory findings that differentiate HAE from other forms of angioedema • Compare and contrast pharmacologic strategies for the prophylactic treatment of HAE • Individualize treatment plans for preventing HAE in order to best provide guideline-recommended care
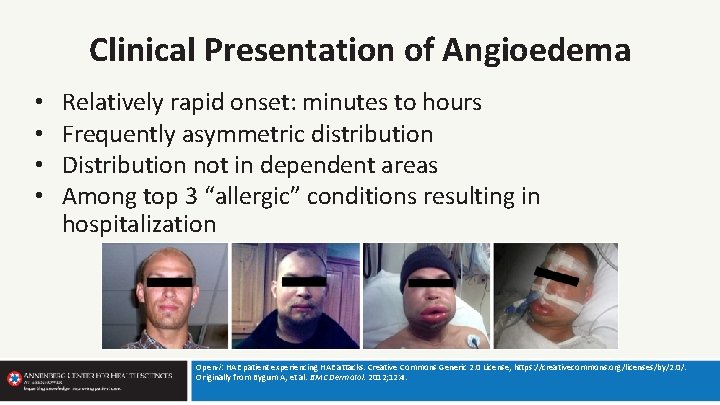
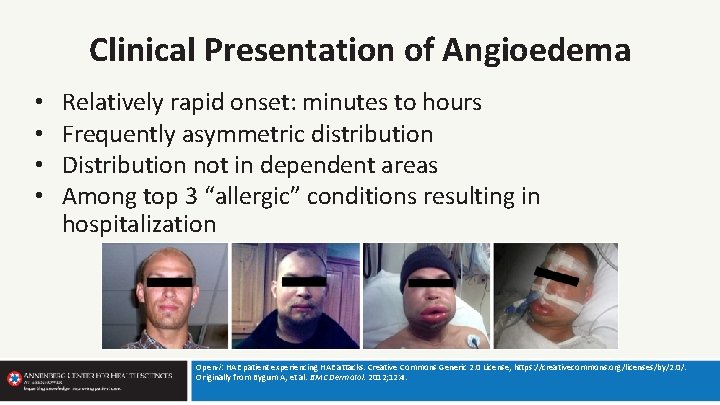
Clinical Presentation of Angioedema • • Relatively rapid onset: minutes to hours Frequently asymmetric distribution Distribution not in dependent areas Among top 3 “allergic” conditions resulting in hospitalization Open-i: HAE patient experiencing HAE attacks. Creative Commons Generic 2. 0 License, https: //creativecommons. org/licenses/by/2. 0/. Originally from Bygum A, et al. BMC Dermatol. 2012; 12: 4.
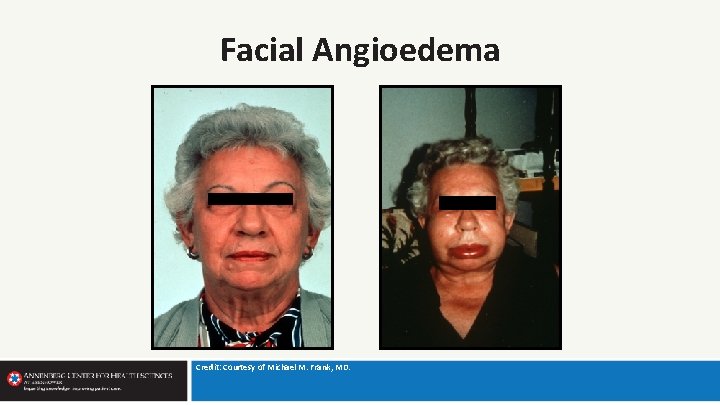
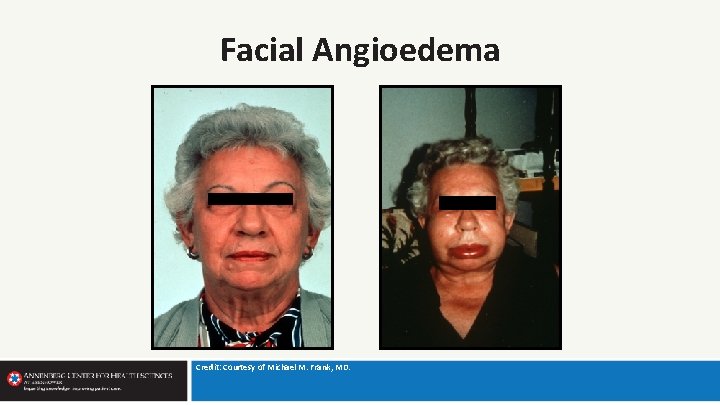
Facial Angioedema Credit: Courtesy of Michael M. Frank, MD.
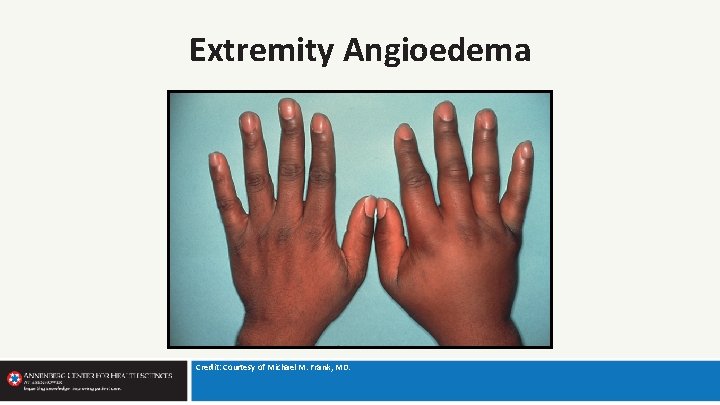
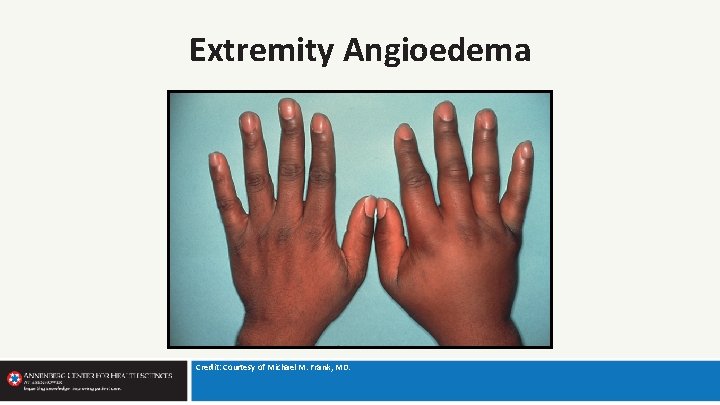
Extremity Angioedema Credit: Courtesy of Michael M. Frank, MD.
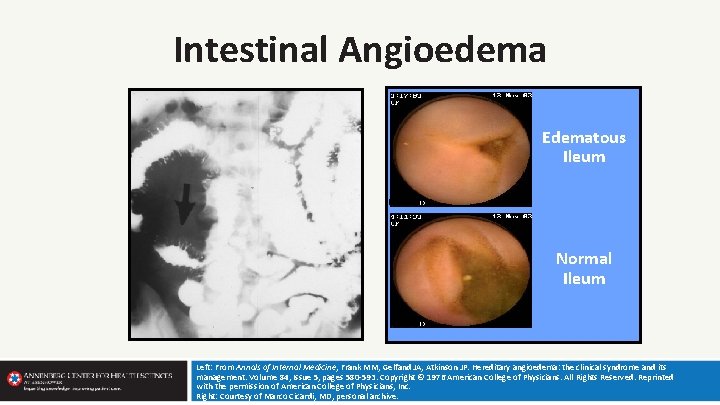
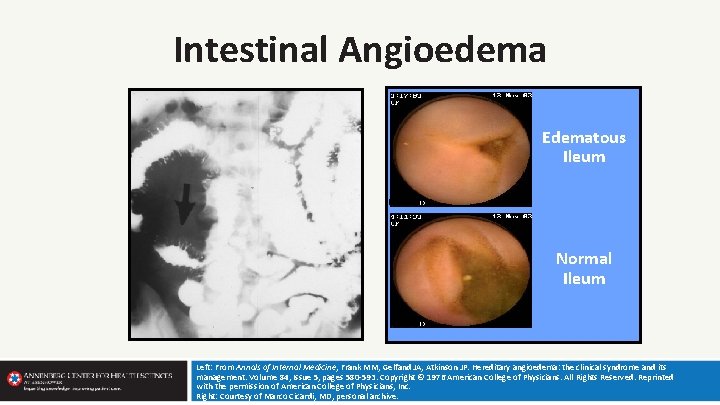
Intestinal Angioedema Edematous Ileum Normal Ileum Left: From Annals of Internal Medicine, Frank MM, Gelfand JA, Atkinson JP. Hereditary angioedema: the clinical syndrome and its management. Volume 84, Issue 5, pages 580 -593. Copyright © 1976 American College of Physicians. All Rights Reserved. Reprinted with the permission of American College of Physicians, Inc. Right: Courtesy of Marco Cicardi, MD, personal archive.
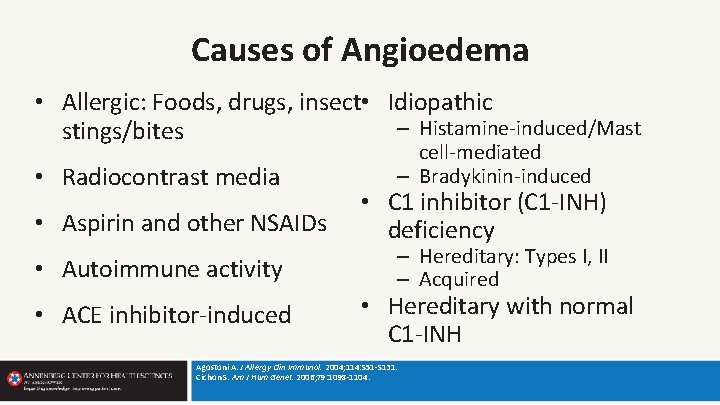
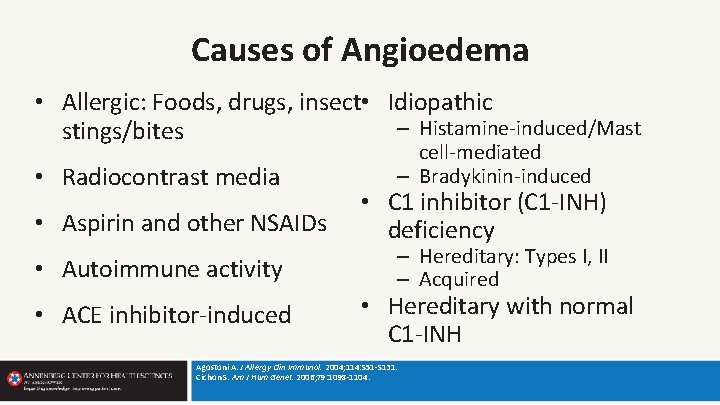
Causes of Angioedema • Allergic: Foods, drugs, insect • Idiopathic – Histamine-induced/Mast stings/bites • Radiocontrast media • Aspirin and other NSAIDs • Autoimmune activity • ACE inhibitor-induced cell-mediated – Bradykinin-induced • C 1 inhibitor (C 1 -INH) deficiency – Hereditary: Types I, II – Acquired • Hereditary with normal C 1 -INH Agostoni A. J Allergy Clin Immunol. 2004; 114: S 51 -S 131. Cichon S. Am J Hum Genet. 2006; 79: 1098 -1104.
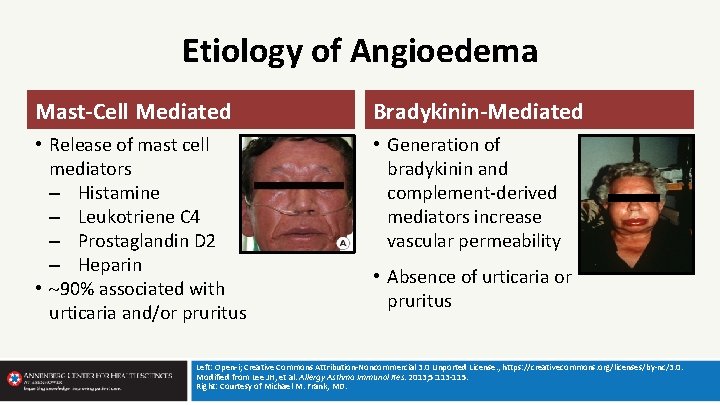
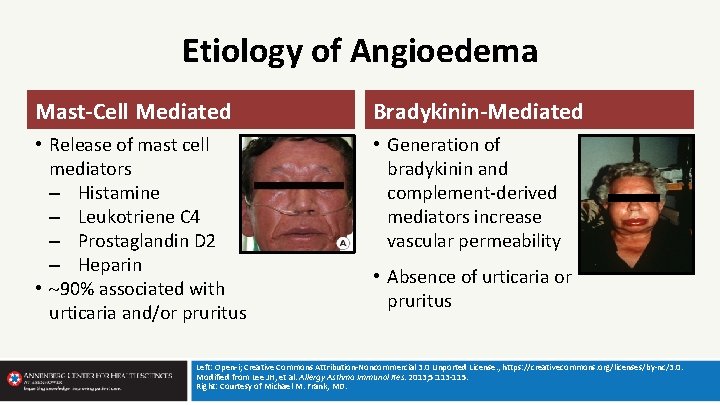
Etiology of Angioedema Mast-Cell Mediated Bradykinin-Mediated • Release of mast cell mediators – Histamine – Leukotriene C 4 – Prostaglandin D 2 – Heparin • 90% associated with urticaria and/or pruritus • Generation of bradykinin and complement-derived mediators increase vascular permeability • Absence of urticaria or pruritus Left: Open-i; Creative Commons Attribution-Noncommercial 3. 0 Unported License. , https: //creativecommons. org/licenses/by-nc/3. 0. Modified from Lee JH, et al. Allergy Asthma Immunol Res. 2013; 5: 113 -115. Right: Courtesy of Michael M. Frank, MD.
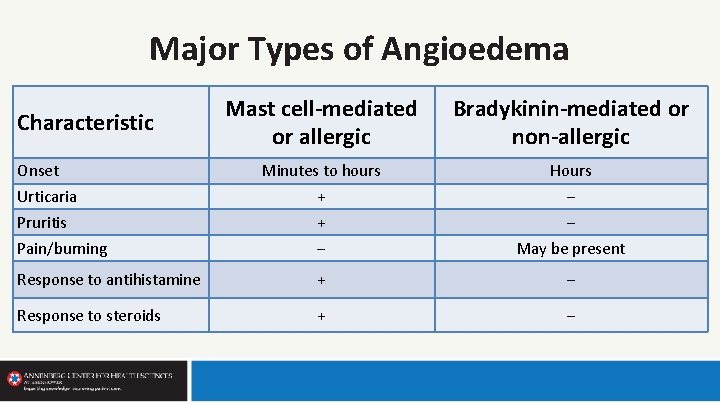
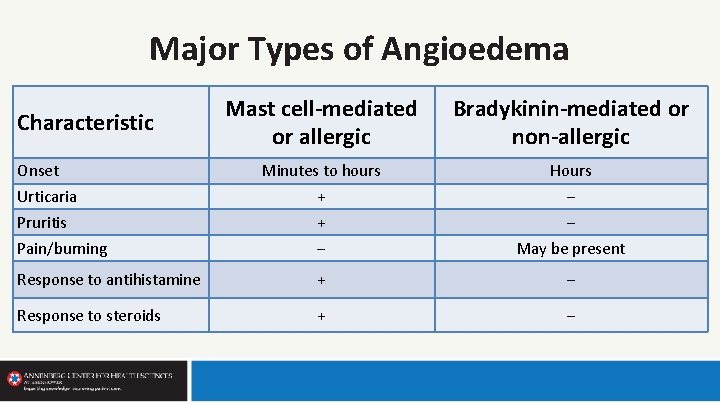
Major Types of Angioedema Mast cell-mediated or allergic Bradykinin-mediated or non-allergic Minutes to hours Hours Urticaria + ‒ Pruritis + ‒ Pain/burning ‒ May be present Response to antihistamine + ‒ Response to steroids + ‒ Characteristic Onset
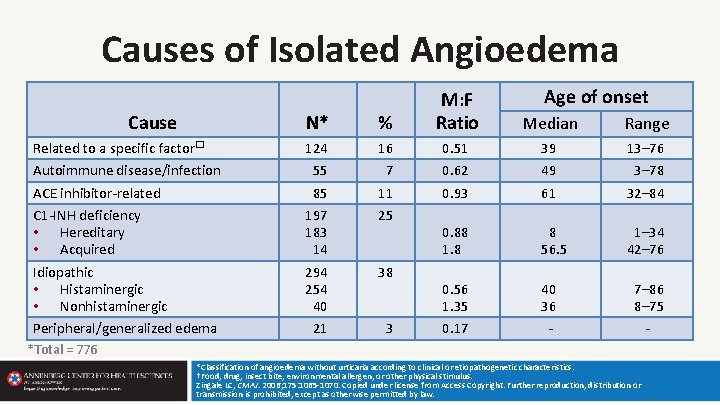
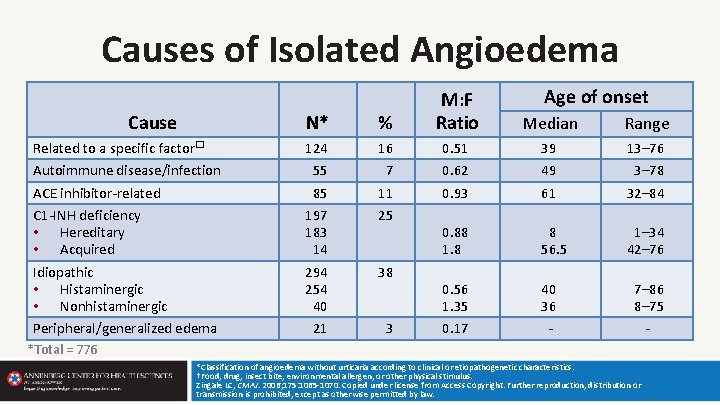
Causes of Isolated Angioedema Cause N* % Related to a specific factor� Autoimmune disease/infection ACE inhibitor-related C 1 -INH deficiency • Hereditary • Acquired Idiopathic • Histaminergic • Nonhistaminergic 124 55 85 197 183 14 294 254 40 16 7 11 25 Peripheral/generalized edema 21 3 38 Age of onset M: F Ratio Median Range 0. 51 0. 62 0. 93 39 49 61 13– 76 3– 78 32– 84 0. 88 1. 8 8 56. 5 1– 34 42– 76 0. 56 1. 35 40 36 7– 86 8– 75 0. 17 - - *Total = 776 *Classification of angioedema without urticaria according to clinical or etiopathogenetic characteristics. †Food, drug, insect bite, environmental allergen, or other physical stimulus. Zingale LC, CMAJ. 2006; 175: 1065 -1070. Copied under license from Access Copyright. Further reproduction, distribution or transmission is prohibited, except as otherwise permitted by law.
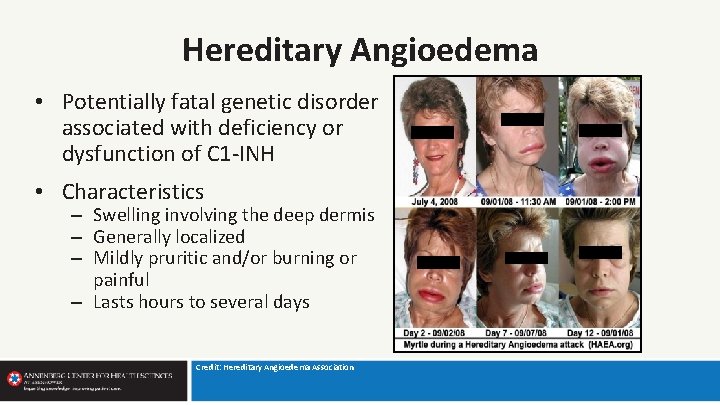
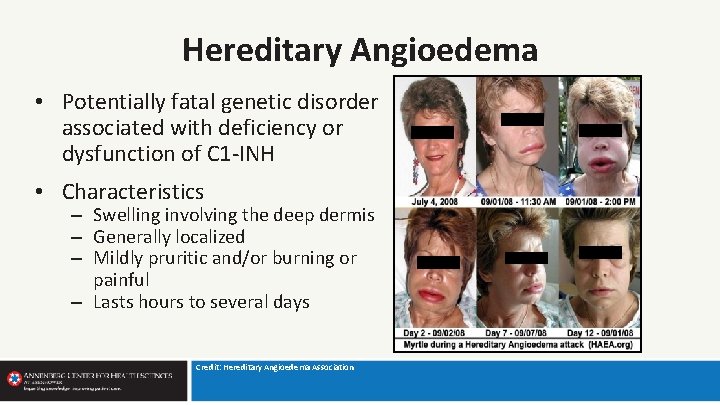
Hereditary Angioedema • Potentially fatal genetic disorder associated with deficiency or dysfunction of C 1 -INH • Characteristics – Swelling involving the deep dermis – Generally localized – Mildly pruritic and/or burning or painful – Lasts hours to several days Credit: Hereditary Angioedema Association
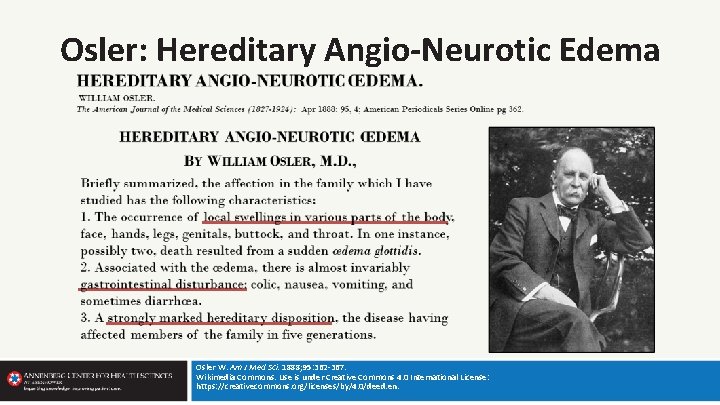
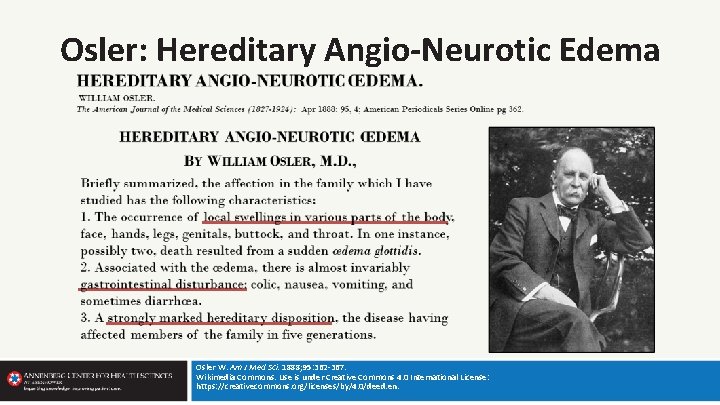
Osler: Hereditary Angio-Neurotic Edema Osler W. Am J Med Sci. 1888; 95: 362 -367. Wikimedia Commons. Use is under Creative Commons 4. 0 International License: https: //creativecommons. org/licenses/by/4. 0/deed. en.
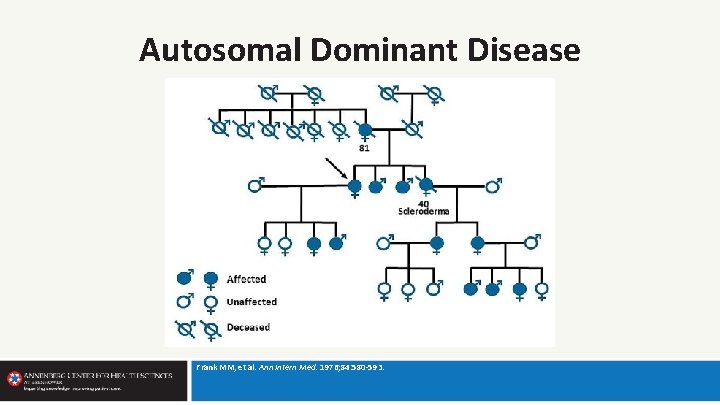
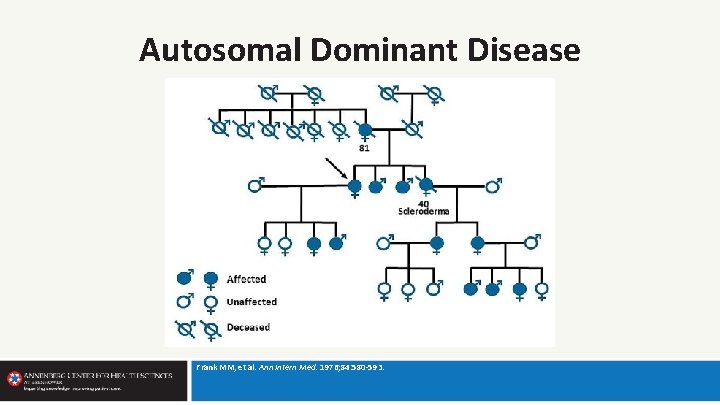
Autosomal Dominant Disease Frank MM, et al. Ann Intern Med. 1976; 84: 580 -593.
Deficiency of C 1 Esterase Inhibition Donaldson VH, et al. Am J Med. 1963; 35: 37 -44.
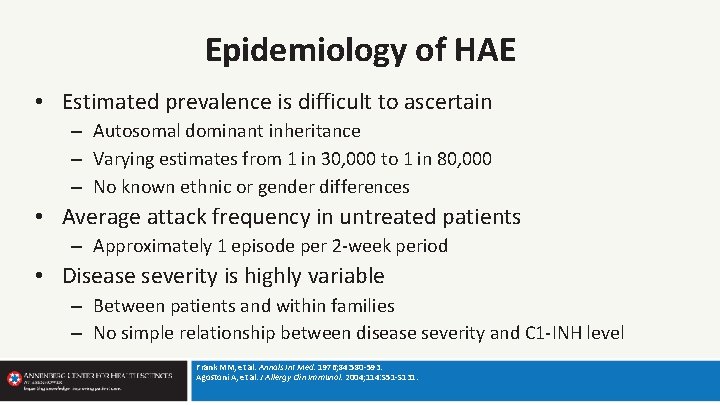
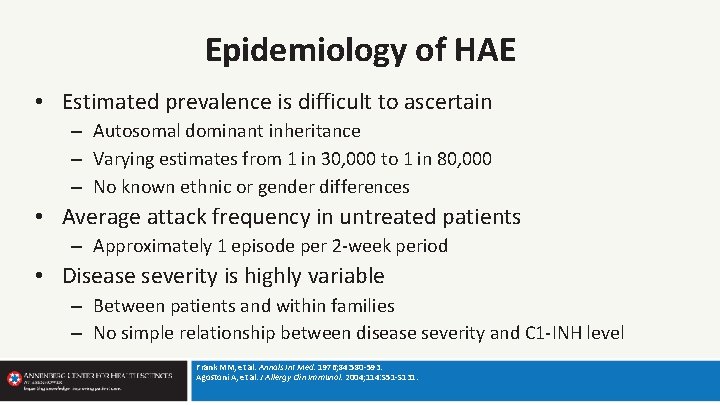
Epidemiology of HAE • Estimated prevalence is difficult to ascertain – Autosomal dominant inheritance – Varying estimates from 1 in 30, 000 to 1 in 80, 000 – No known ethnic or gender differences • Average attack frequency in untreated patients – Approximately 1 episode per 2 -week period • Disease severity is highly variable – Between patients and within families – No simple relationship between disease severity and C 1 -INH level Frank MM, et al. Annals Int Med. 1976; 84: 580 -593. Agostoni A, et al. J Allergy Clin Immunol. 2004; 114: S 51 -S 131.
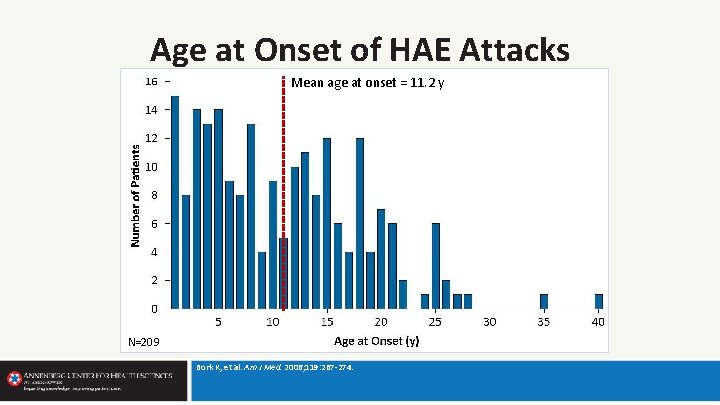
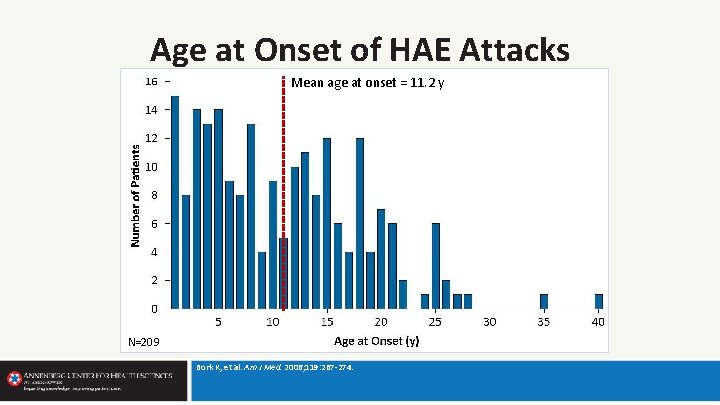
Age at Onset of HAE Attacks Mean age at onset = 11. 2 y N=209 Bork K, et al. Am J Med. 2006; 119: 267 -274.
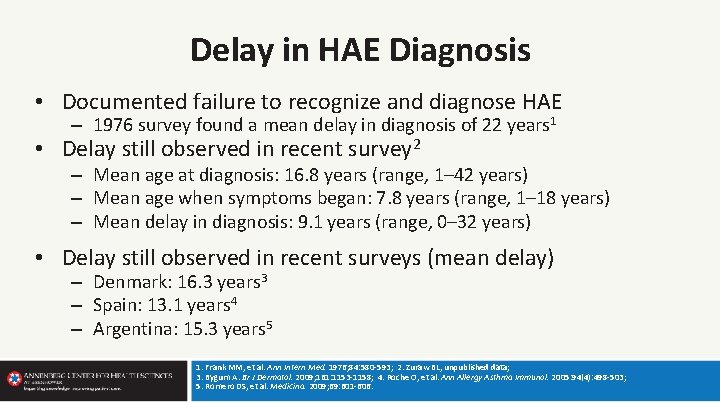
Delay in HAE Diagnosis • Documented failure to recognize and diagnose HAE – 1976 survey found a mean delay in diagnosis of 22 years 1 • Delay still observed in recent survey 2 – Mean age at diagnosis: 16. 8 years (range, 1– 42 years) – Mean age when symptoms began: 7. 8 years (range, 1– 18 years) – Mean delay in diagnosis: 9. 1 years (range, 0– 32 years) • Delay still observed in recent surveys (mean delay) – Denmark: 16. 3 years 3 – Spain: 13. 1 years 4 – Argentina: 15. 3 years 5 1. Frank MM, et al. Ann Intern Med. 1976; 84: 580 -593; 2. Zuraw BL, unpublished data; 3. Bygum A. Br J Dermatol. 2009; 161: 1153 -1158; 4. Roche O, et al. Ann Allergy Asthma Immunol. 2005: 94(4): 498 -503; 5. Romero DS, et al. Medicina. 2009; 69: 601 -606.
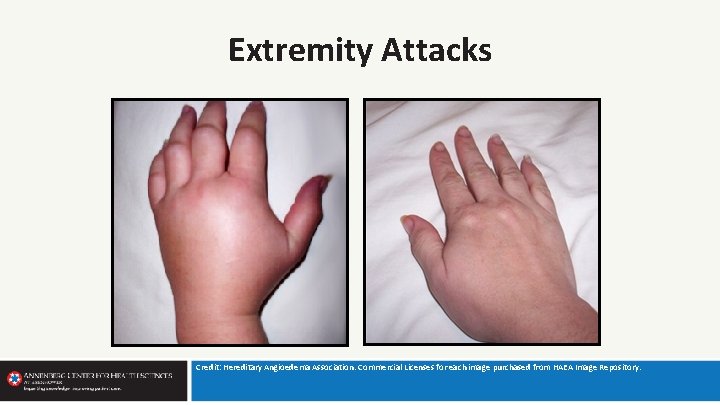
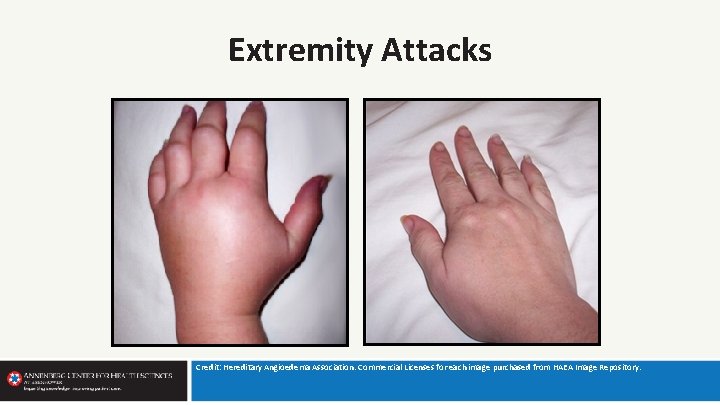
Extremity Attacks Credit: Hereditary Angioedema Association. Commercial Licenses for each image purchased from HAEA Image Repository.
Abdominal Attacks • Occur in 93% of patients with HAE • Mild to severe intractable pain • Vomiting common; constipation/diarrhea may occur • Intestinal obstruction • Fluid loss may lead to hypovolemic shock • Protuberant abdomen, tenderness and rebound possible • Symptoms mimic surgical emergencies, resulting in misdiagnosis and unnecessary surgery Frank MM, et al. Ann Intern Med. 1976; 84: 580 -593. Agostoni A, et al. J Allergy Clin Immunol. 2004: 114: S 51 -S 131. Frank MM. Immunol Allergy Clin N Am. 2006; 26: 653 -668. Agostoni A, Cicardi M. Medicine. 1992; 71: 206 -215.
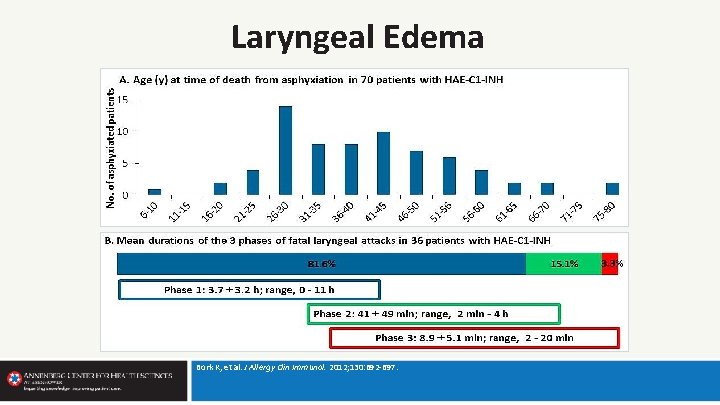
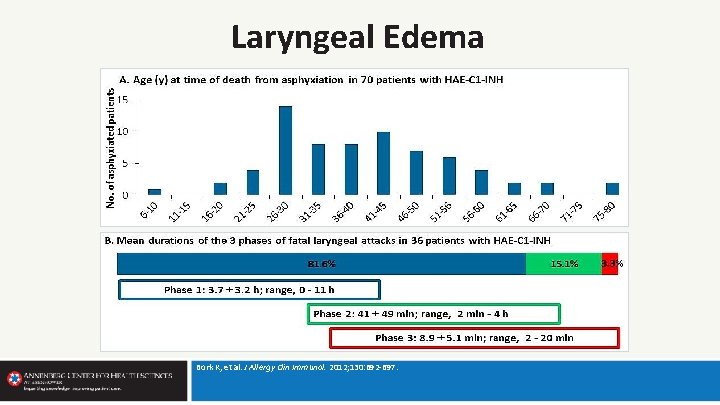
Laryngeal Edema Bork K, et al. J Allergy Clin Immunol. 2012; 130: 692 -697.
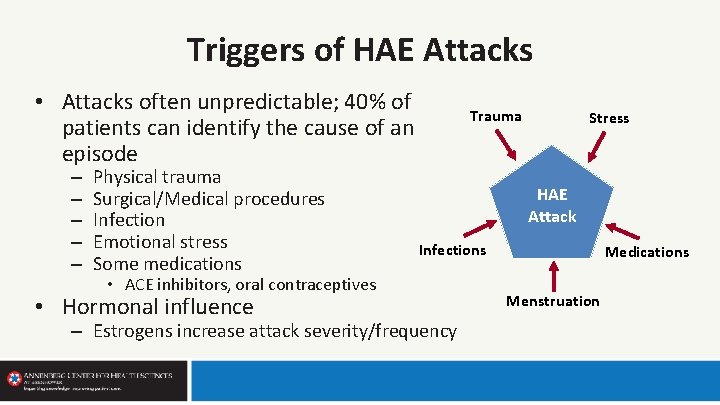
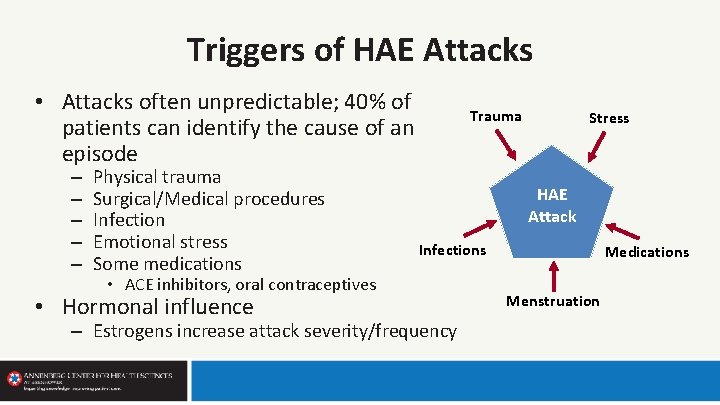
Triggers of HAE Attacks • Attacks often unpredictable; 40% of patients can identify the cause of an episode – – – Physical trauma Surgical/Medical procedures Infection Emotional stress Some medications Trauma HAE Attack Infections • ACE inhibitors, oral contraceptives • Hormonal influence Stress – Estrogens increase attack severity/frequency Medications Menstruation
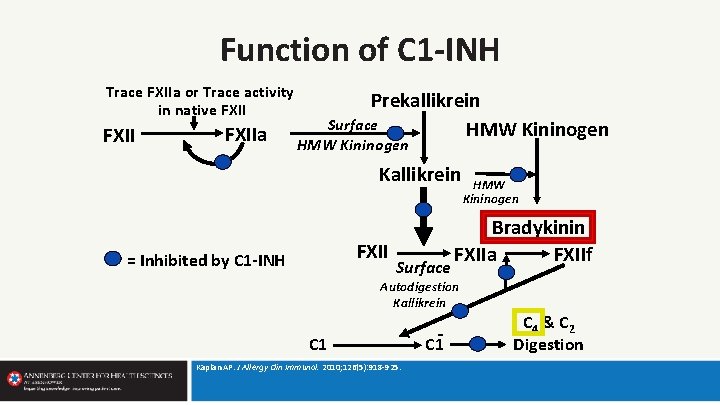
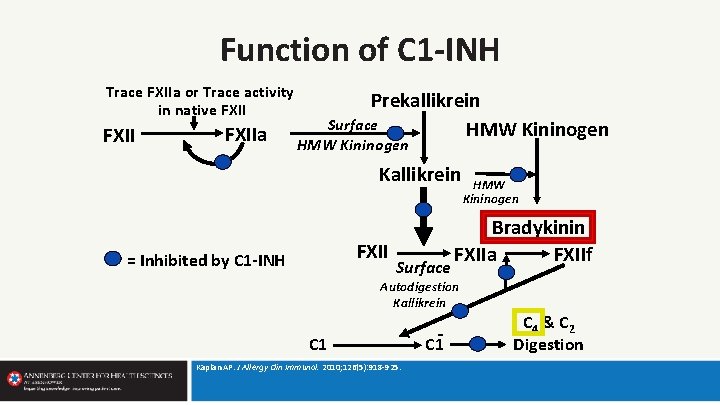
Function of C 1 -INH Trace FXIIa or Trace activity in native FXIIa Prekallikrein Surface HMW Kininogen Kallikrein FXII = Inhibited by C 1 -INH Surface Bradykinin FXIIa FXIIf Autodigestion Kallikrein C 1 Kaplan AP. J Allergy Clin Immunol. 2010; 126(5): 918 -925. C 1 HMW Kininogen C 4 & C 2 Digestion
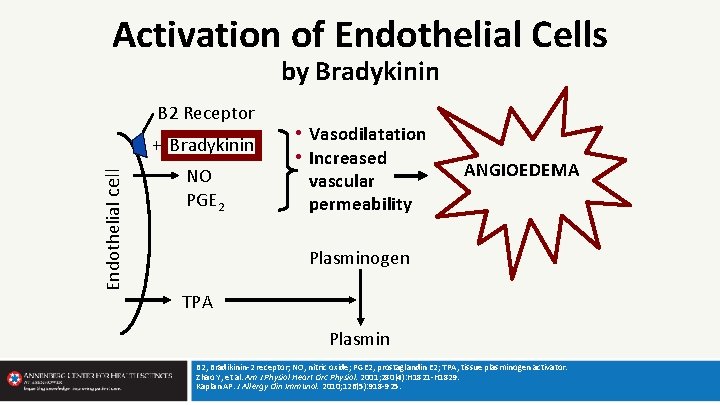
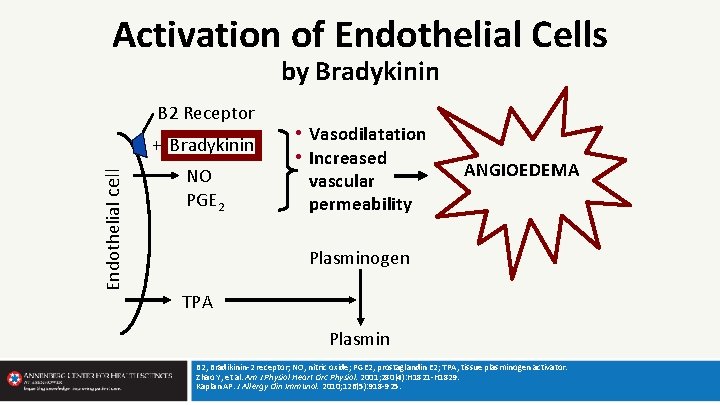
Activation of Endothelial Cells by Bradykinin B 2 Receptor Endothelial cell + Bradykinin NO PGE 2 • Vasodilatation • Increased vascular permeability ANGIOEDEMA Plasminogen TPA Plasmin B 2, Bradikinin-2 receptor; NO, nitric oxide; PGE 2, prostaglandin E 2; TPA, tissue plasminogen activator. Zhao Y, et al. Am J Physiol Heart Circ Physiol. 2001; 280(4): H 1821 -H 1829. Kaplan AP. J Allergy Clin Immunol. 2010; 126(5): 918 -925.
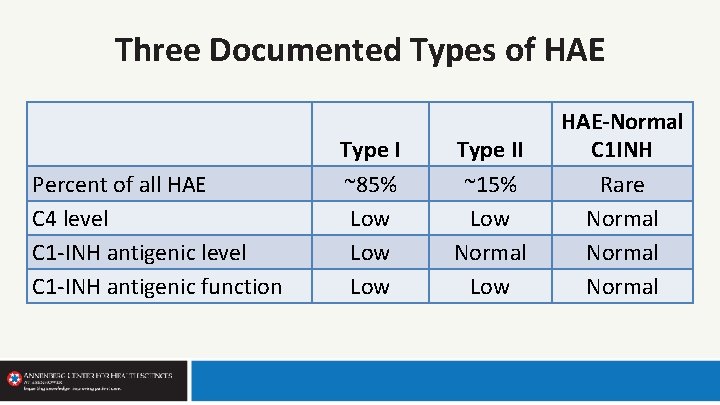
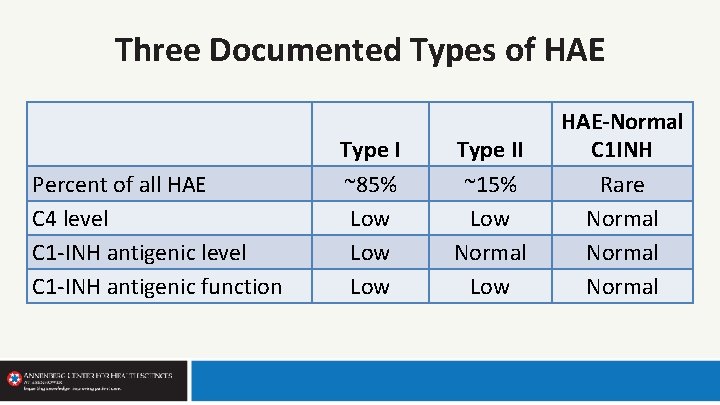
Three Documented Types of HAE Percent of all HAE C 4 level C 1 -INH antigenic function Type I ~85% Low Low Type II ~15% Low Normal Low HAE-Normal C 1 INH Rare Normal
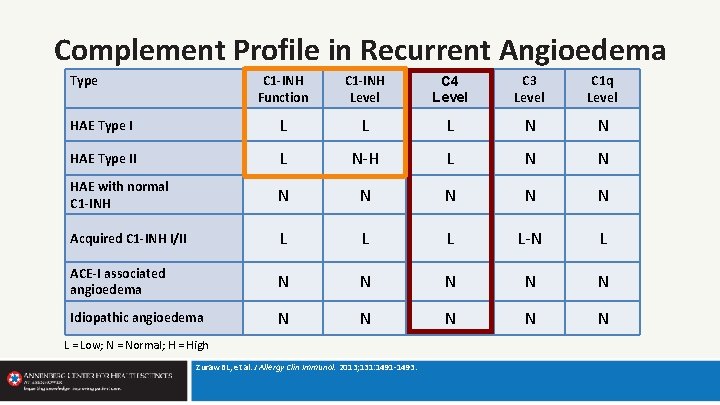
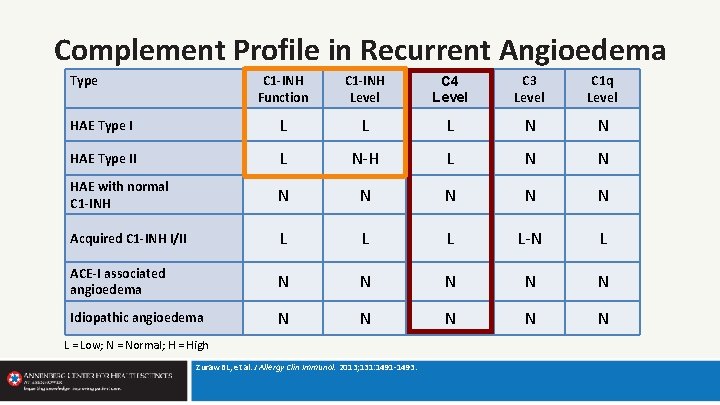
Complement Profile in Recurrent Angioedema Type C 1 -INH Function C 1 -INH Level C 4 Level C 3 Level C 1 q Level HAE Type I L L L N N HAE Type II L N-H L N N HAE with normal C 1 -INH N N N Acquired C 1 -INH I/II L L-N L ACE-I associated angioedema N N N Idiopathic angioedema N N N L = Low; N = Normal; H = High Zuraw BL, et al. J Allergy Clin Immunol. 2013; 131: 1491 -1493.
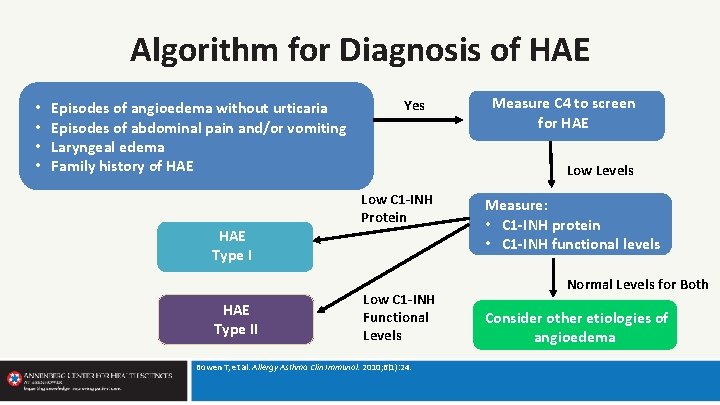
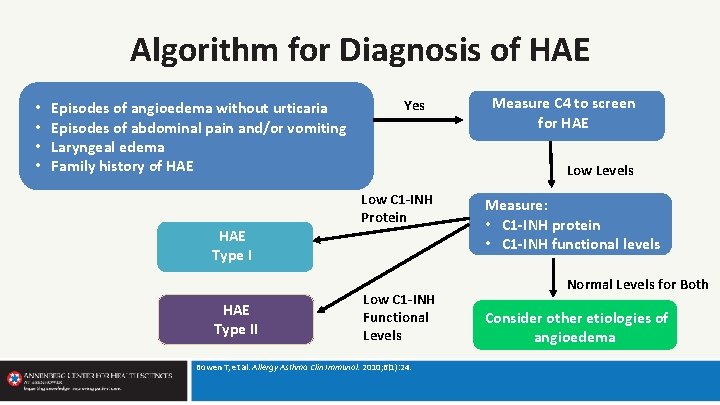
Algorithm for Diagnosis of HAE • • Episodes of angioedema without urticaria Episodes of abdominal pain and/or vomiting Laryngeal edema Family history of HAE Type II Yes Measure C 4 to screen for HAE Low Levels Low C 1 -INH Protein Low C 1 -INH Functional Levels Bowen T, et al. Allergy Asthma Clin Immunol. 2010; 6(1): 24. Measure: • C 1 -INH protein • C 1 -INH functional levels Normal Levels for Both Consider other etiologies of angioedema
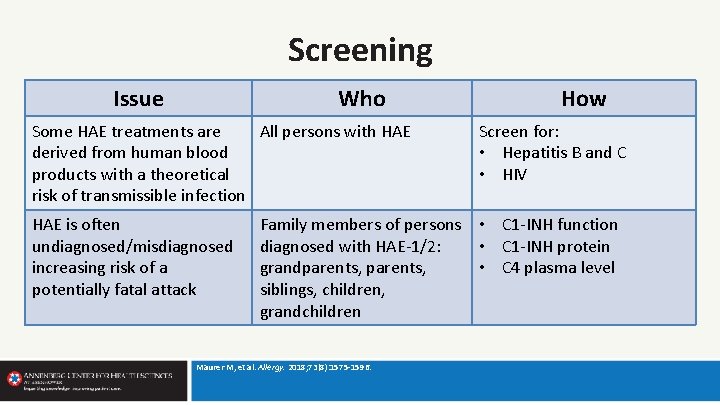
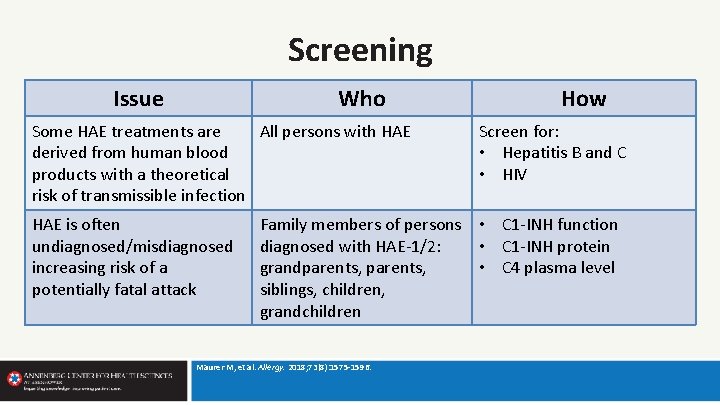
Screening Issue Who Some HAE treatments are All persons with HAE derived from human blood products with a theoretical risk of transmissible infection HAE is often undiagnosed/misdiagnosed increasing risk of a potentially fatal attack How Screen for: • Hepatitis B and C • HIV Family members of persons • C 1 -INH function diagnosed with HAE-1/2: • C 1 -INH protein grandparents, • C 4 plasma level siblings, children, grandchildren Maurer M, et al. Allergy. 2018; 73(8): 1575 -1596.
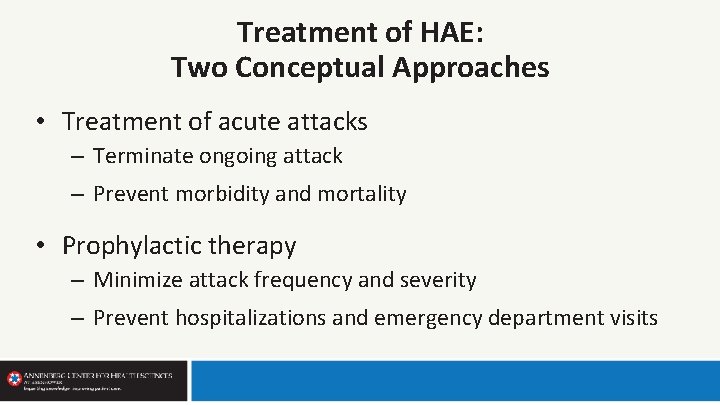
Treatment of HAE: Two Conceptual Approaches • Treatment of acute attacks – Terminate ongoing attack – Prevent morbidity and mortality • Prophylactic therapy – Minimize attack frequency and severity – Prevent hospitalizations and emergency department visits
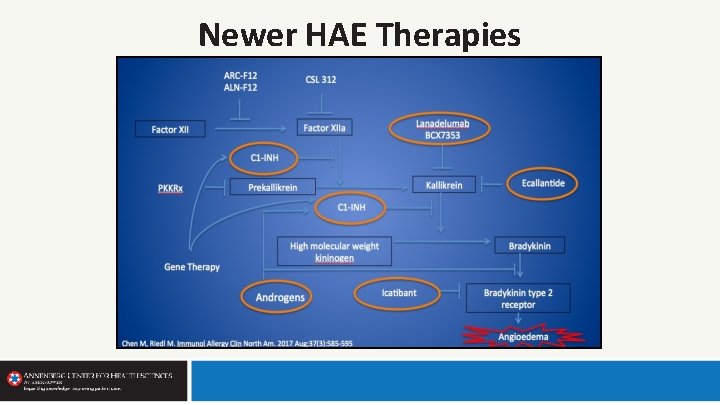
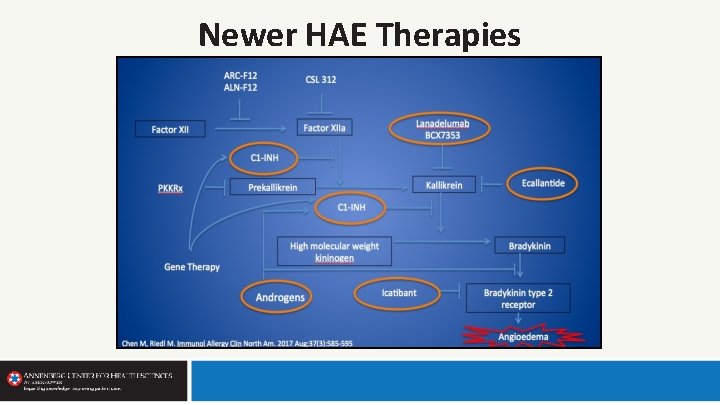
Newer HAE Therapies
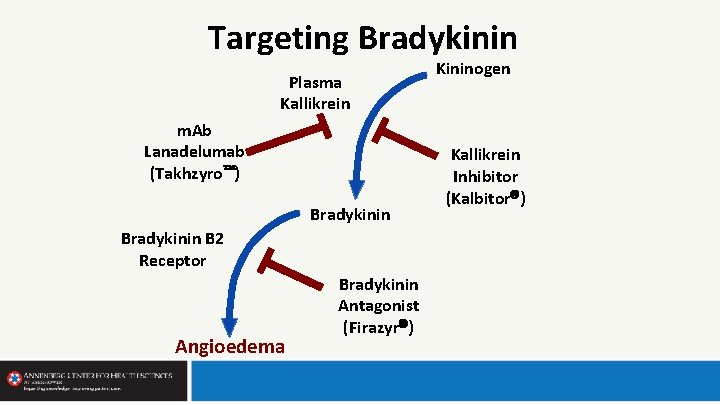
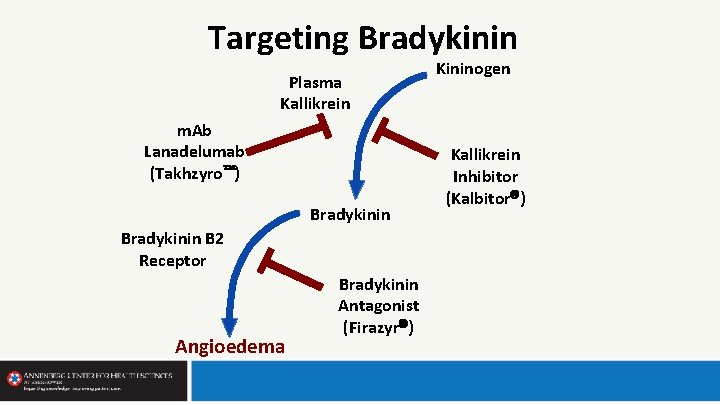
Targeting Bradykinin Plasma Kallikrein m. Ab Lanadelumab (Takhzyro ) Bradykinin B 2 Receptor Angioedema Bradykinin Antagonist (Firazyr ) Kininogen Kallikrein Inhibitor (Kalbitor )
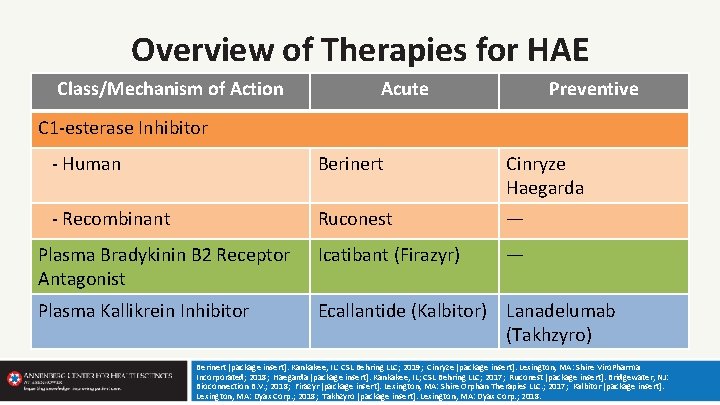
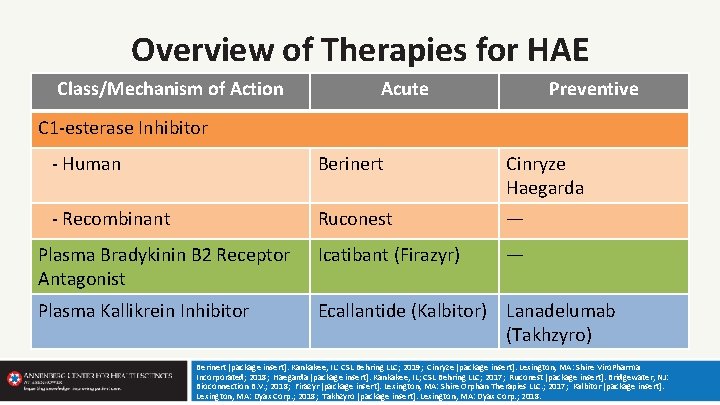
Overview of Therapies for HAE Class/Mechanism of Action Acute Preventive C 1 -esterase Inhibitor - Human Berinert Cinryze Haegarda - Recombinant Ruconest — Plasma Bradykinin B 2 Receptor Antagonist Icatibant (Firazyr) — Plasma Kallikrein Inhibitor Ecallantide (Kalbitor) Lanadelumab (Takhzyro) Berinert [package insert]. Kankakee, IL: CSL Behring LLC; 2019; Cinryze [package insert]. Lexington, MA: Shire Viro. Pharma Incorporated; 2018; Haegarda [package insert]. Kankakee, IL; CSL Behring LLC; 2017; Ruconest [package insert]. Bridgewater, NJ: Bioconnection B. V. ; 2018; Firazyr [package insert]. Lexington, MA: Shire Orphan Therapies LLC. ; 2017; Kalbitor [package insert]. Lexington, MA: Dyax Corp. ; 2018; Takhzyro [package insert]. Lexington, MA: Dyax Corp. ; 2018.
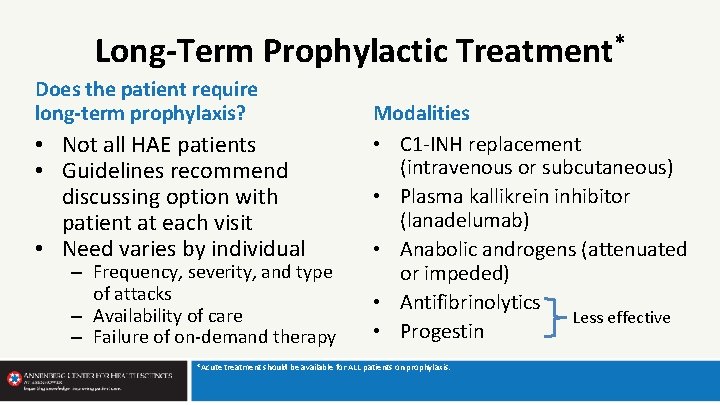
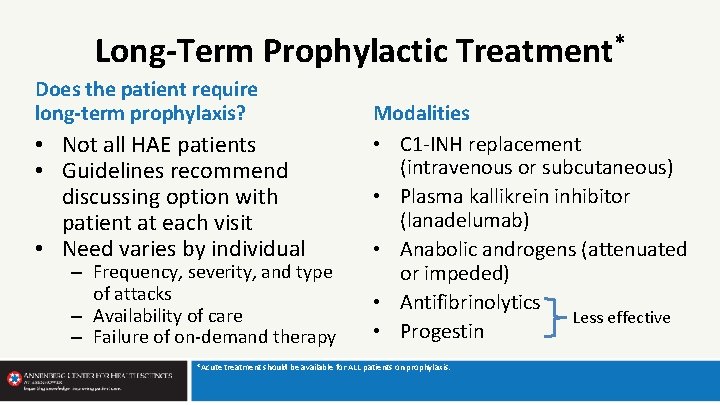
Long-Term Prophylactic Treatment* Does the patient require long-term prophylaxis? • Not all HAE patients • Guidelines recommend discussing option with patient at each visit • Need varies by individual – Frequency, severity, and type of attacks – Availability of care – Failure of on-demand therapy Modalities • C 1 -INH replacement (intravenous or subcutaneous) • Plasma kallikrein inhibitor (lanadelumab) • Anabolic androgens (attenuated or impeded) • Antifibrinolytics Less effective • Progestin *Acute treatment should be available for ALL patients on prophylaxis.
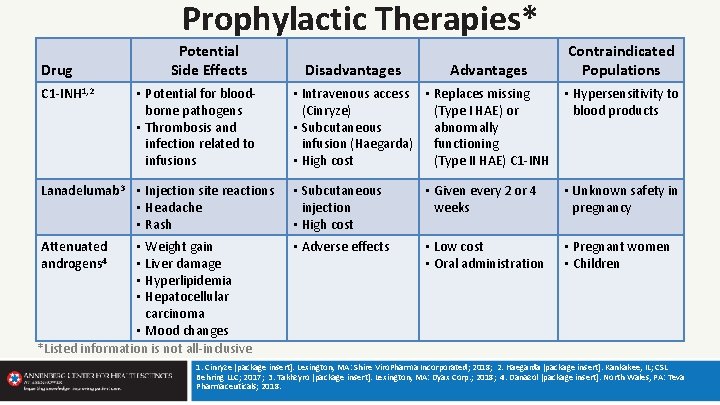
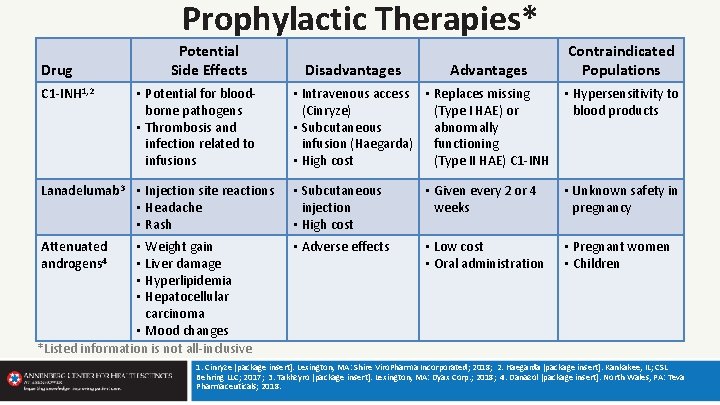
Prophylactic Therapies* Drug C 1 -INH 1, 2 Potential Side Effects • Potential for bloodborne pathogens • Thrombosis and infection related to infusions Disadvantages Advantages Contraindicated Populations • Intravenous access • Replaces missing • Hypersensitivity to (Cinryze) (Type I HAE) or blood products • Subcutaneous abnormally infusion (Haegarda) functioning • High cost (Type II HAE) C 1 -INH Lanadelumab 3 • Injection site reactions • Headache • Rash • Subcutaneous injection • High cost • Given every 2 or 4 weeks • Unknown safety in pregnancy Attenuated androgens 4 • Adverse effects • Low cost • Oral administration • Pregnant women • Children • Weight gain • Liver damage • Hyperlipidemia • Hepatocellular carcinoma • Mood changes *Listed information is not all-inclusive 1. Cinryze [package insert]. Lexington, MA: Shire Viro. Pharma Incorporated; 2018; 2. Haegarda [package insert]. Kankakee, IL; CSL Behring LLC; 2017; 3. Takhzyro [package insert]. Lexington, MA: Dyax Corp. ; 2018; 4. Danazol [package insert]. North Wales, PA: Teva Pharmaceuticals; 2018.
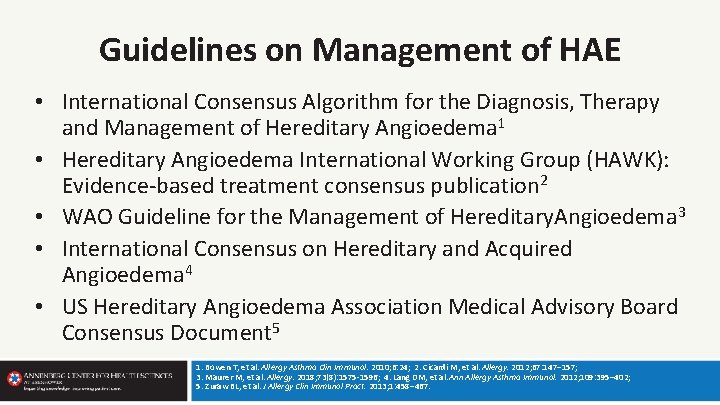
Guidelines on Management of HAE • International Consensus Algorithm for the Diagnosis, Therapy and Management of Hereditary Angioedema 1 • Hereditary Angioedema International Working Group (HAWK): Evidence-based treatment consensus publication 2 • WAO Guideline for the Management of Hereditary. Angioedema 3 • International Consensus on Hereditary and Acquired Angioedema 4 • US Hereditary Angioedema Association Medical Advisory Board Consensus Document 5 1. Bowen T, et al. Allergy Asthma Clin Immunol. 2010; 6: 24; 2. Cicardi M, et al. Allergy. 2012; 67: 147– 157; 3. Maurer M, et al. Allergy. 2018; 73(8): 1575 -1596; 4. Lang DM, et al. Ann Allergy Asthma Immunol. 2012; 109: 395– 402; 5. Zuraw BL, et al. J Allergy Clin Immunol Pract. 2013; 1: 458– 467.
HAE Guidelines • Consensus documents – Efforts to move from expert opinion to evidence-based recommendations • High-quality evidence lacking in some areas • Provide guidance for management, not rigorous rules or protocols
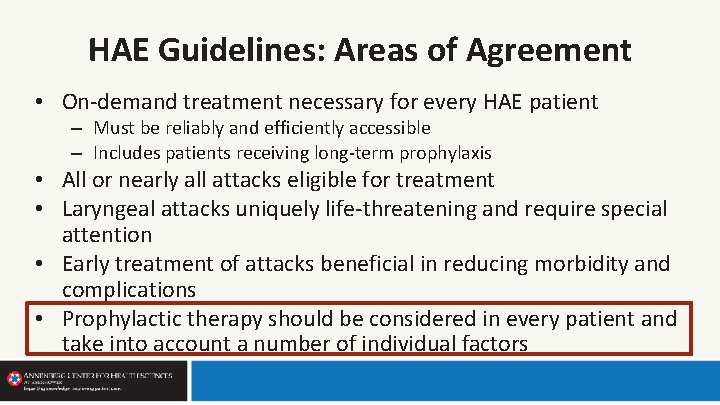
HAE Guidelines: Areas of Agreement • On-demand treatment necessary for every HAE patient – Must be reliably and efficiently accessible – Includes patients receiving long-term prophylaxis • All or nearly all attacks eligible for treatment • Laryngeal attacks uniquely life-threatening and require special attention • Early treatment of attacks beneficial in reducing morbidity and complications • Prophylactic therapy should be considered in every patient and take into account a number of individual factors
HAE Guidelines: Areas of Agreement • On-demand treatment necessary for every HAE patient – Must be reliably and efficiently accessible – Includes patients receiving long-term prophylaxis • All or nearly all attacks eligible for treatment • Laryngeal attacks uniquely life-threatening and require special attention • Early treatment of attacks beneficial in reducing morbidity and complications • Prophylactic therapy should be considered in every patient and take into account a number of individual factors
HAE Guidelines: Areas Lacking Clarity • Specific indications for prophylaxis
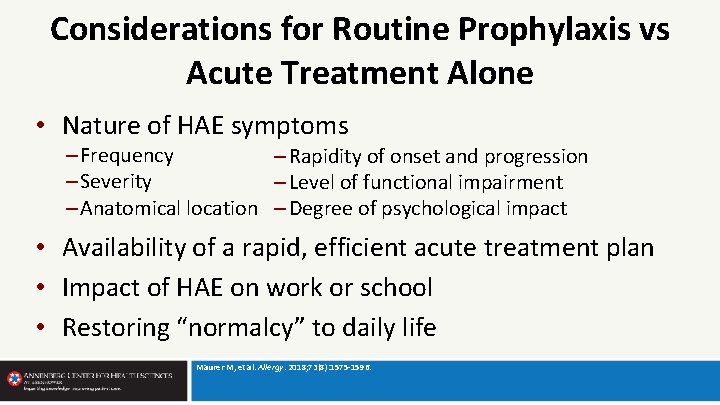
Considerations for Routine Prophylaxis vs Acute Treatment Alone • Nature of HAE symptoms – Frequency – Rapidity of onset and progression – Severity – Level of functional impairment – Anatomical location – Degree of psychological impact • Availability of a rapid, efficient acute treatment plan • Impact of HAE on work or school • Restoring “normalcy” to daily life Maurer M, et al. Allergy. 2018; 73(8): 1575 -1596.
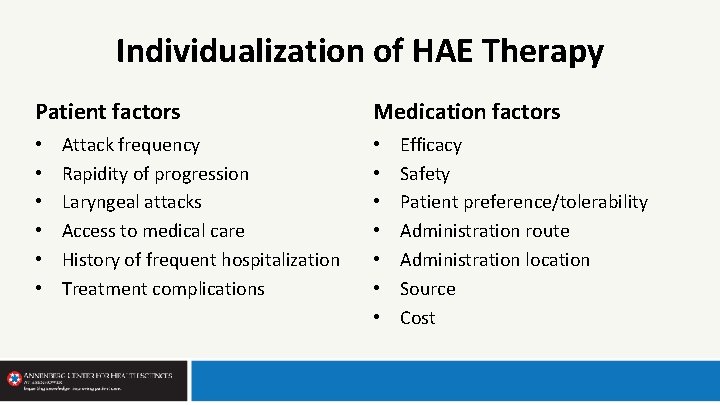
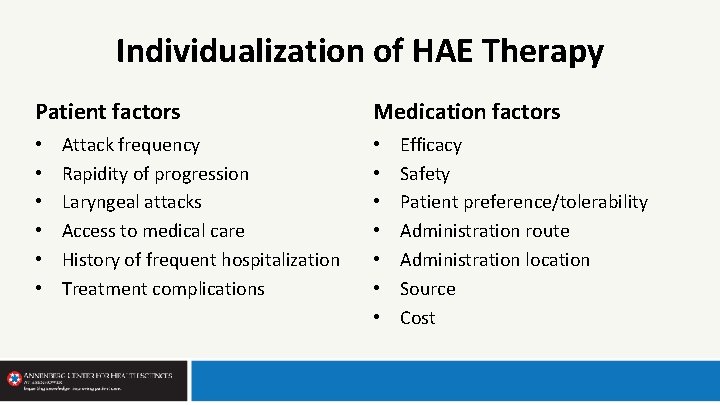
Individualization of HAE Therapy Patient factors • • • Attack frequency Rapidity of progression Laryngeal attacks Access to medical care History of frequent hospitalization Treatment complications Medication factors • • Efficacy Safety Patient preference/tolerability Administration route Administration location Source Cost
Components of a Comprehensive Treatment Plan: Essentials of Modern HAE Therapy 1. Acute treatment plan for every patient 2. Routine prophylaxis for some patients 3. Logistics of treatment plan a. Recommendation for involvement of HAE specialist when possible 4. Monitoring for efficacy and side effects
Creating a Comprehensive Treatment Plan for Hereditary Angioedema • Evaluation/diagnosis • Optimization of management plans • Collaboration with local MDs and specialists • Telemedicine presence Riedl MA. Immunol Allergy Clin North Am. 2013; 33(4): 471 -485.
Benefits of Involving an HAE Specialist • National referral centers or networks • Collaborative care with local physicians • Optimal patient education regarding condition and treatment options • Iterative process to adjust/adapt treatment plan over time
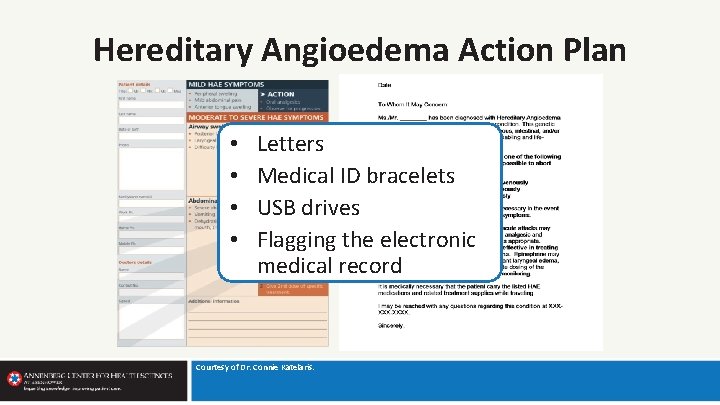
Hereditary Angioedema Action Plan • • Letters Medical ID bracelets USB drives Flagging the electronic medical record Courtesy of Dr. Connie Katelaris.
Monitoring for Efficacy and Side Effects • Known and unknown risks of medications – – – Androgens Plasma products Long-term safety of monoclonal antibody Local and systemic treatment reactions IV access issues • Individual patient variability in response to therapies • HAE is a complex, highly variable, chronic condition – Benefits of periodic monitoring
Special Populations Children – Prevent infections vaccinations – Avoid estrogen-containing contraceptives progesterone-only (HAE-1/2) – Educate patient, family, caregivers, educators Pregnant women – Pregnancy can mitigate, aggravate, or have no effect vigilant care and selection of medications with favorable safety profile Maurer M, et al. Allergy. 2018; 73(8): 1575 -1596.
Summary • Key to diagnosis of HAE is a high index of suspicion • Diagnosis of C 1 -INH deficiency (HAE Type I and II) requires laboratory confirmation • All HAE patients should have an effective plan in place for on-demand treatment of acute attacks • Prophylactic treatment beneficial in selected patients based on individual factors • Treatment plans including self-administered medication improve patient quality of life
 Alexander riedl
Alexander riedl Promotion from associate professor to professor
Promotion from associate professor to professor Marc ophalvens
Marc ophalvens Marc hyden
Marc hyden Des exemples d'objets communicants
Des exemples d'objets communicants Estereobat
Estereobat Marc sylvie
Marc sylvie Marc koninckx
Marc koninckx Capacidades intersubjetivas y mentalistas
Capacidades intersubjetivas y mentalistas Marc to bibframe
Marc to bibframe Harvard university track and field
Harvard university track and field Jean-marc perreault
Jean-marc perreault Leontien ruttenberg
Leontien ruttenberg Marc bieri
Marc bieri Ivo saliger das urteil des paris
Ivo saliger das urteil des paris Adamo e la piccola eva paul klee
Adamo e la piccola eva paul klee Marc desmet sj
Marc desmet sj Marc breault eyes
Marc breault eyes Scegs meetinstrument
Scegs meetinstrument Savant genome browser
Savant genome browser Marc todesco
Marc todesco Prire
Prire Itard
Itard Marc aurele gladiator
Marc aurele gladiator Marc andreu guerao
Marc andreu guerao Marc van kreveld
Marc van kreveld Marc van der meer
Marc van der meer Cantique des cantiques chagall
Cantique des cantiques chagall Marc mosko
Marc mosko Marc stamminger
Marc stamminger Qt division
Qt division Portfoli
Portfoli Marc bachand
Marc bachand Marc 21 tutorial
Marc 21 tutorial Marc sagrista garcia
Marc sagrista garcia Blue rider pictures
Blue rider pictures Marc levoy
Marc levoy Marc scarborough
Marc scarborough Canca
Canca Marc tag 300
Marc tag 300 Catedu.es/arasaac
Catedu.es/arasaac Marc steinberg onr
Marc steinberg onr Marc xml
Marc xml Marc guenot
Marc guenot Multilingualism meaning
Multilingualism meaning Marc format
Marc format Marc ancrenaz
Marc ancrenaz Marc d hauser
Marc d hauser Self – marc quinn, 1991
Self – marc quinn, 1991 Marc leobet
Marc leobet