Managing Adverse Events of Voluntary Medical Male Circumcision

- Slides: 41
Managing Adverse Events of Voluntary Medical Male Circumcision (VMMC) An orientation for non-VMMC providers
Audience for this session Health care providers who are not trained in VMMC but may see clients for VMMC-related issues, including providers at: • Sites where VMMC teams provide VMMC on outreach but leave before follow-up, or • Sites near VMMC service sites, where men with adverse events (AEs) may come, or • Any other site with no VMMC provider that may receive visits from male clients after a recent VMMC
Introduction • Male circumcision (MC) is the removal of the full foreskin covering the end of the penis so as to permanently expose the glans (or head of the penis) • MC is also known as Voluntary Medical Male Circumcision (VMMC) when it is offered to adult and adolescent males as part of an HIV prevention program.
Why we do VMMC: the benefits • Provides heterosexual men about 60% protection from acquiring HIV from a female partner • Provides partial protection against some other sexually transmitted infections (genital ulcers, human papillomavirus, genital herpes), and cancer of the penis • Because of this, protects female partners too (a man cannot transmit an infection he doesn’t have) • Reduces female partners' risk of cervical cancer • Helps with maintaining hygiene of the penis
When do clients present after VMMC? • Routine follow-up visits: usually on Days 2, 7 and sometimes 49 after surgical VMMC, or 2 or 7 days after device removal – may vary according to country guidelines • Should be scheduled and done by trained VMMC providers • Problem visits: any time after VMMC when an AE develops, mostly within 7 days, except for AEs related to premature resumption of sexual activity (before wound is healed), which often occur after 7 days • Should also be handled by VMMC providers, but client may present elsewhere
Why do VMMC-related AEs happen? • Many are preventable if client screening, VMMC procedures, and post-operative care instructions are done correctly • Some result from client failure to follow post-operative care instructions (for example, clean water not available or client resumes sex before healing) • Some will still happen no matter what providers or clients do
Objectives of this training: By the end of reviewing these slides you will be able to: • Describe the routine post-surgical care after VMMC • Recognize normal wound healing following VMMC (surgical and device) • Identify and classify common VMMC AEs following surgical and device circumcision • Provide appropriate basic AE care and follow-up • Recognize the AEs that require referral to a trained provider or to a higher level of care • Record and report AEs and follow-up care to the VMMC facility and the national reporting system
What should local providers be able to do when VMMC clients present? Note: Trained VMMC clinicians are the appropriate providers for routine and AE follow-up visits, and should routinely return to outreach sites to provide followup. But clients may visit non-VMMC providers if they are unable to return to the VMMC clinic due to logistical issues or other challenges. • For routine follow-up visits: • Recognize normal healing • Reinforce correct wound care and followup instructions • Recognize AEs Always have a contact name and phone number to access help from VMMC team • For follow-up visits with AEs • Make basic diagnosis • Provide care appropriate for site capacity • Determine whether referral to higher level of care i needed • If referral is not needed, determine when client should return for follow-up • At follow-up, determine whether AE is improving, and refer if not • Document diagnosis and management, and report t VMMC provider and/or to national AE system if tha is the policy
Accessing help from the VMMC team • Ensure you have at least 2 contact phone numbers for the nearby/visiting VMMC team • Know what the VMMC team’s plan is for clients who present at your site with emergencies and non-emergency AEs • Should include whether and how quickly they can provide transport when referral is needed, or make emergency visits • Should include what to do if no cell phone coverage • Know what instructions they give clients for adverse events • There must be a number given to clients to contact trained VMMC providers in case of questions, emergencies, or other AEs
Accessing help from the VMMC team (cont’d) • Always call with any concerns • Please notify the VMMC team of moderate and severe AEs, even if your site can handle them, so they can: • Learn about issues specific to your area, and make adjustments • Make arrangements for follow up as needed
Routine Scheduled Follow-up Visits: Recognizing Normal Healing

Recognizing normal healing Day 0 Day 7 Day 14 Day 28 Day 42 Dorsal Slit Surgical Procedure Forceps Guided Surgical Procedure Photos: FHI 360 and its partners on the Male Circumcision Consortium with support from the Bill & Melinda Gates Foundation 12
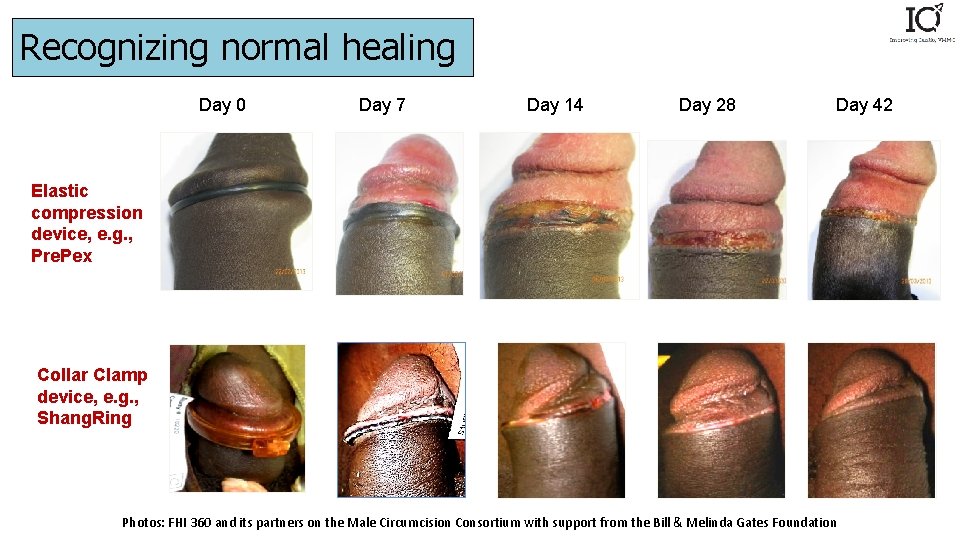
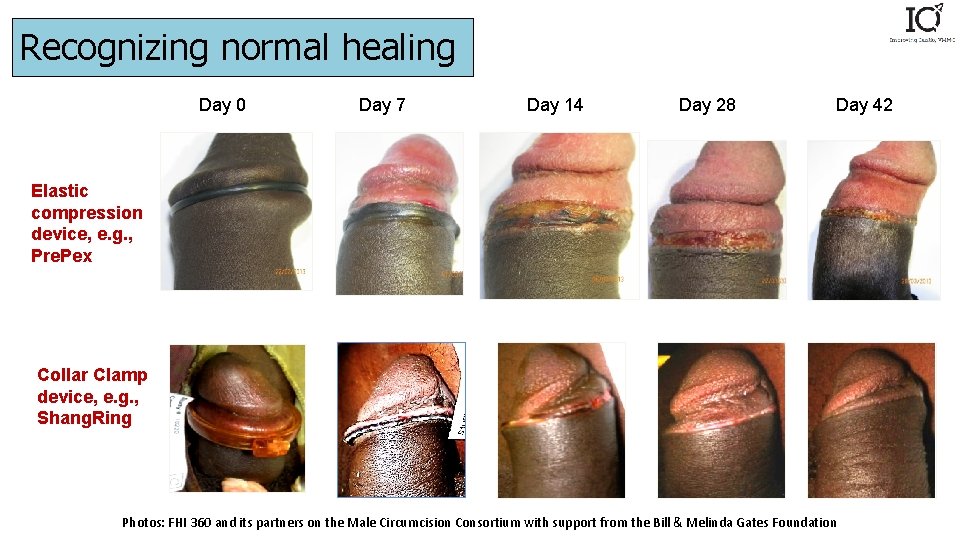
Recognizing normal healing Day 0 Day 7 Day 14 Day 28 Day 42 Elastic compression device, e. g. , Pre. Pex Collar Clamp device, e. g. , Shang. Ring Photos: FHI 360 and its partners on the Male Circumcision Consortium with support from the Bill & Melinda Gates Foundation 13
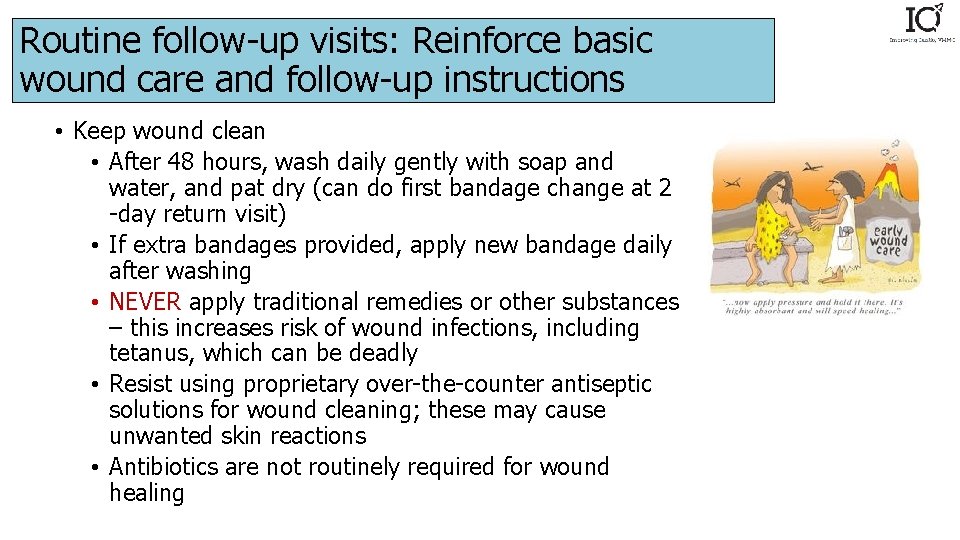
Routine follow-up visits: Reinforce basic wound care and follow-up instructions • Keep wound clean • After 48 hours, wash daily gently with soap and water, and pat dry (can do first bandage change at 2 -day return visit) • If extra bandages provided, apply new bandage daily after washing • NEVER apply traditional remedies or other substances – this increases risk of wound infections, including tetanus, which can be deadly • Resist using proprietary over-the-counter antiseptic solutions for wound cleaning; these may cause unwanted skin reactions • Antibiotics are not routinely required for wound healing
Routine follow-up visits: Reinforce basic wound care and follow-up instructions • Resuming sex before full healing can disrupt healing and put female partners at risk for HIV and sexually transmitted infections • Full healing: at least 6 weeks after surgery or device removal; longer if it does not appear fully healed by then • Review emergency contact information • Confirm next follow-up date (based on national follow-up schedule) • Inform client that if any problems develop prior to next scheduled visit, he should come in or call
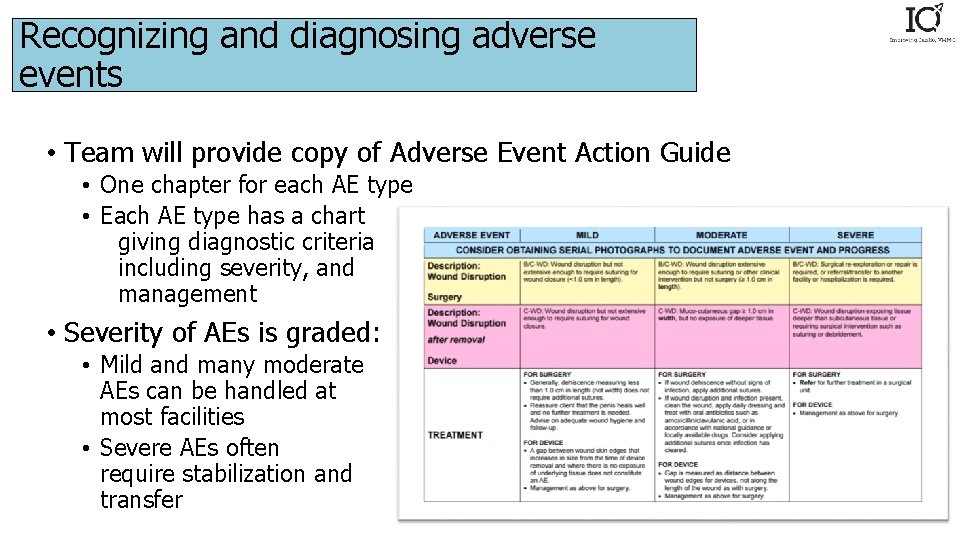
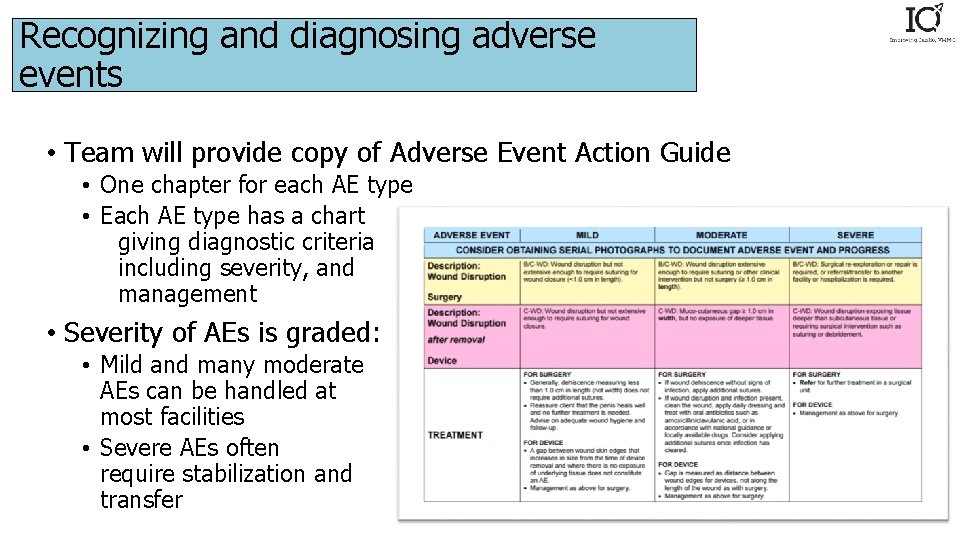
Recognizing and diagnosing adverse events • Team will provide copy of Adverse Event Action Guide • One chapter for each AE type • Each AE type has a chart giving diagnostic criteria including severity, and management • Severity of AEs is graded: • Mild and many moderate AEs can be handled at most facilities • Severe AEs often require stabilization and transfer
Recognizing and diagnosing adverse events • Most common postoperative AEs after surgical VMMC: bleeding, swelling/hematoma, wound infection • Most common complaints in Pre. Pex clients: painful urination, odor and/or pain several days after placement, discomfort due to psychological feeling of having an object over one’s penis • Device displacement is a less common but important event • Others include insufficient or excessive skin removal, trouble urinating, excess swelling, sexual complications • All AEs shown and discussed here can heal fully with correct treatment
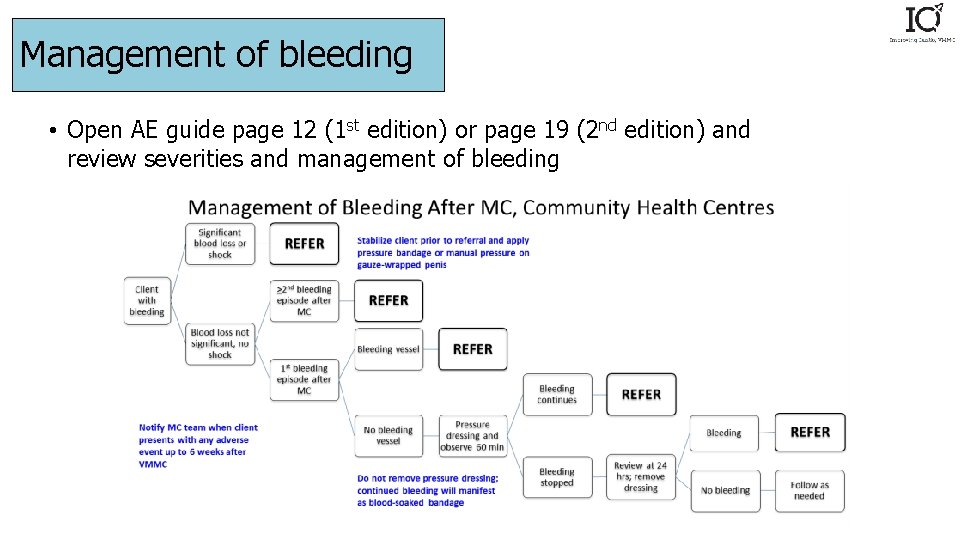
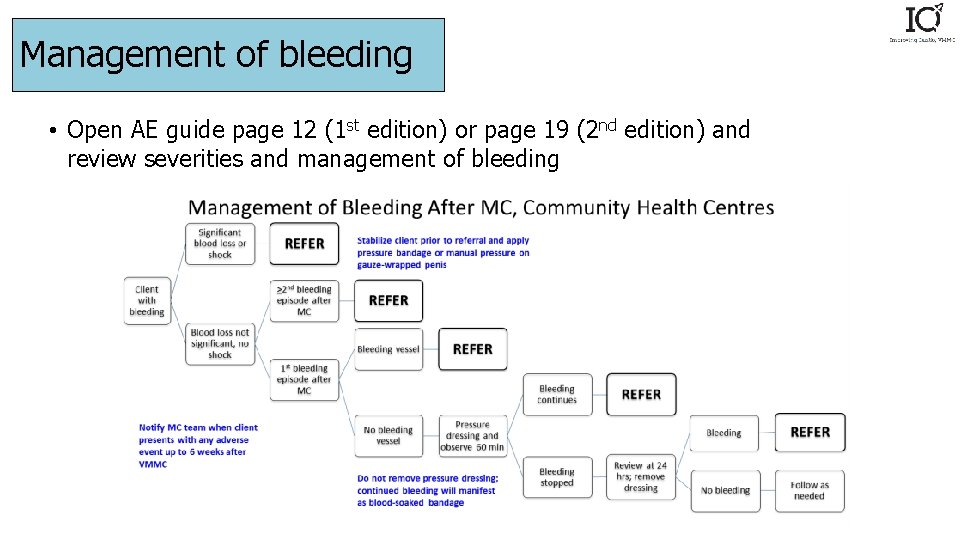
Management of bleeding • Open AE guide page 12 (1 st edition) or page 19 (2 nd edition) and review severities and management of bleeding
Management of bleeding • Any client presenting with bleeding should be asked about personal or family history of bleeding disorders, and any client admitting to such should be referred immediately after stabilization • Mild bleeding: can be handled at any facility using pressure • Moderate bleeding: can be handled by provider able to perform anesthetic injection and suturing • Severe bleeding: hold pressure, give IV fluids, and transfer if expertise in re-exploration surgery not available at site
Management of bleeding • For mild or moderate bleeding, patient should return for review by provider or VMMC team in 24 hours, and daily until clearly improving • ANY recurrent bleeding, i. e. , bleeding that starts again after resolving, without an obvious inciting event like injury or early resumption of sex should raise a concern for undiagnosed bleeding disorder and requires transfer • For men with mild bleeding disorders, VMMC may be first time they show symptoms
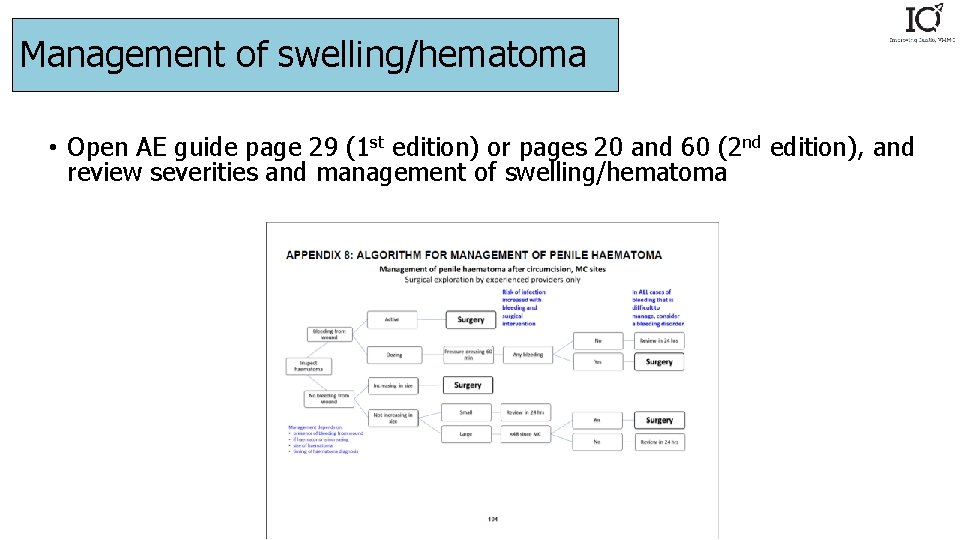
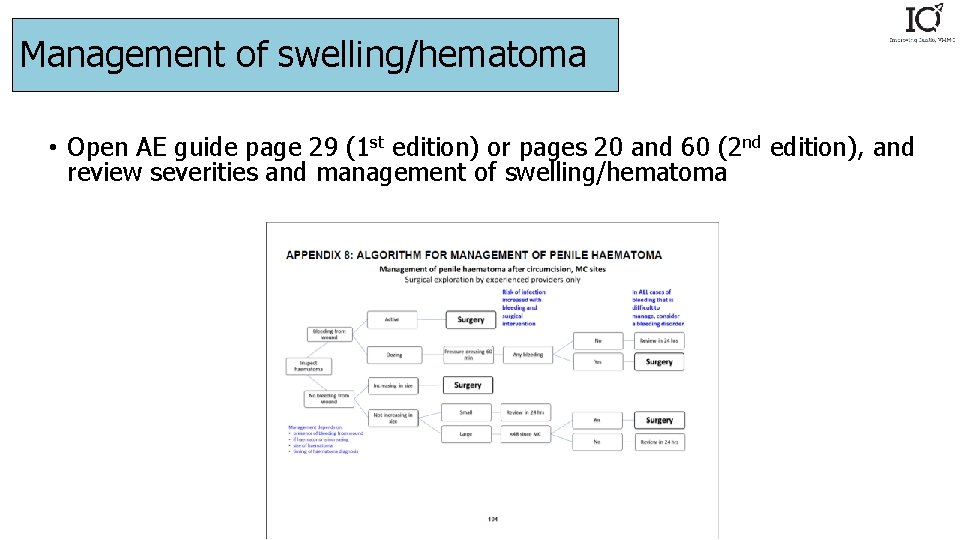
Management of swelling/hematoma • Open AE guide page 29 (1 st edition) or pages 20 and 60 (2 nd edition), and review severities and management of swelling/hematoma
Management of swelling/hematoma • Mild swelling: strap penis up against abdominal wall • Moderate swelling: same; examine for signs of infection (hematomas increase infection risk) • Severe: manage any bleeding; look for signs of infection or other causes of swelling, need surgical intervention • For severe hematoma, patient should return for review by provider or VMMC team in 24 hours and daily until clearly improving • Any hematoma that recurs or worsens raises concern for undiagnosed bleeding disorder, and requires transfer
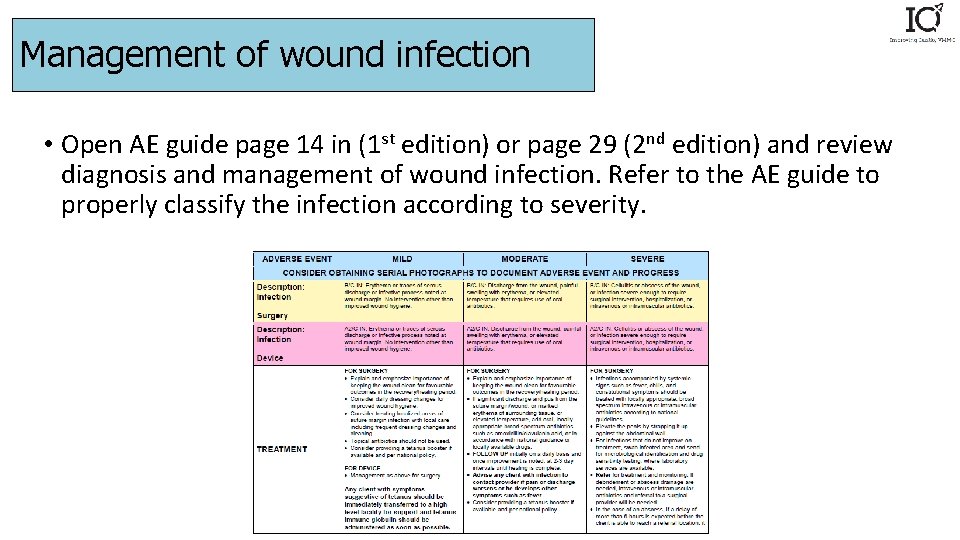
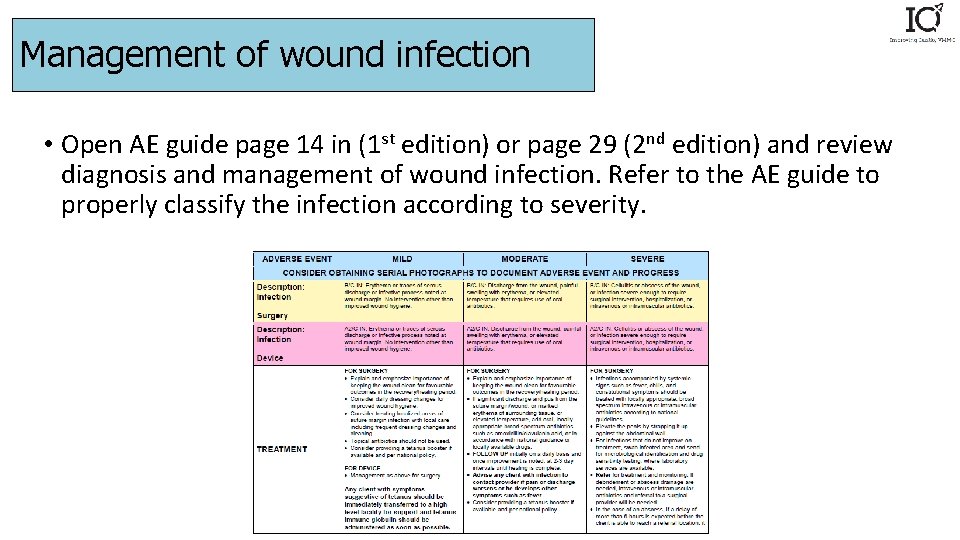
Management of wound infection • Open AE guide page 14 in (1 st edition) or page 29 (2 nd edition) and review diagnosis and management of wound infection. Refer to the AE guide to properly classify the infection according to severity.
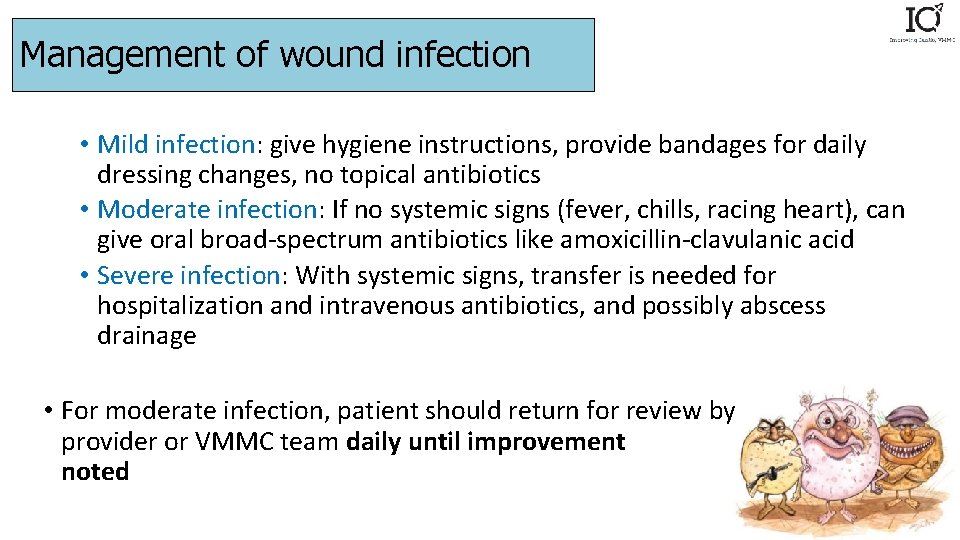
Management of wound infection • Mild infection: give hygiene instructions, provide bandages for daily dressing changes, no topical antibiotics • Moderate infection: If no systemic signs (fever, chills, racing heart), can give oral broad-spectrum antibiotics like amoxicillin-clavulanic acid • Severe infection: With systemic signs, transfer is needed for hospitalization and intravenous antibiotics, and possibly abscess drainage • For moderate infection, patient should return for review by provider or VMMC team daily until improvement noted
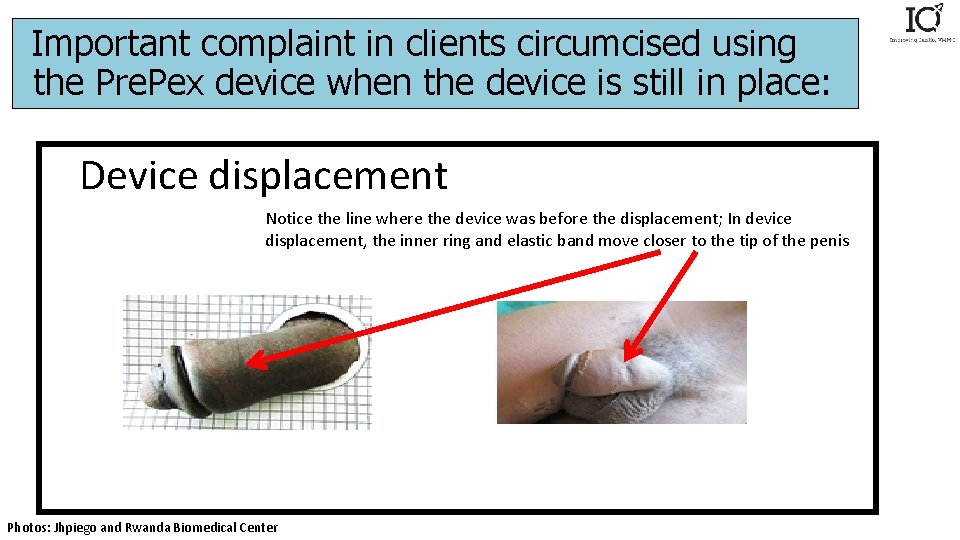
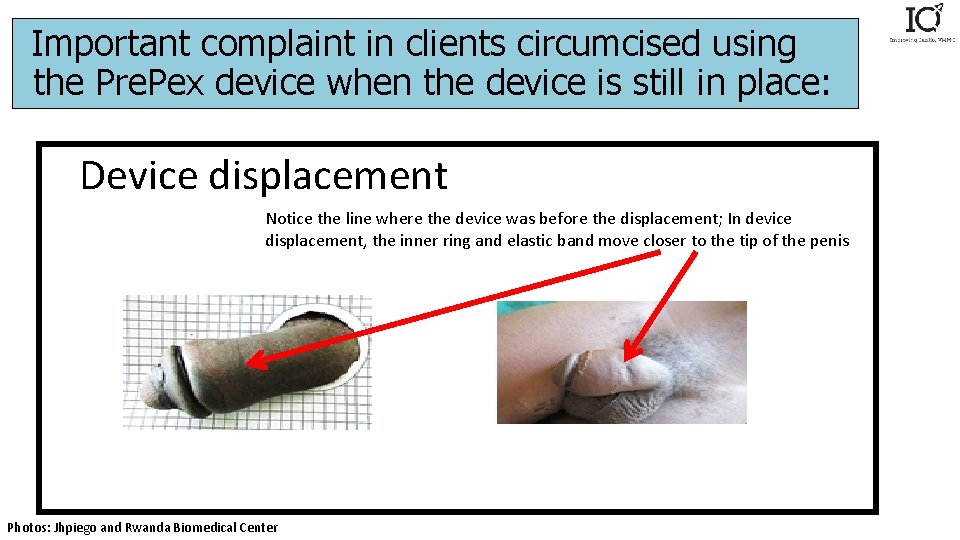
Important complaint in clients circumcised using the Pre. Pex device when the device is still in place: Device displacement Notice the line where the device was before the displacement; In device displacement, the inner ring and elastic band move closer to the tip of the penis Photos: Jhpiego and Rwanda Biomedical Center
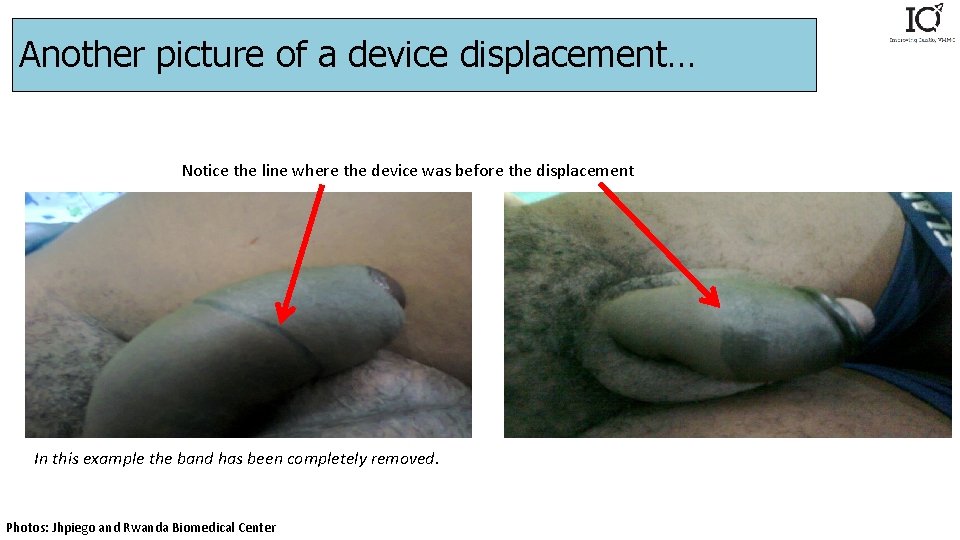
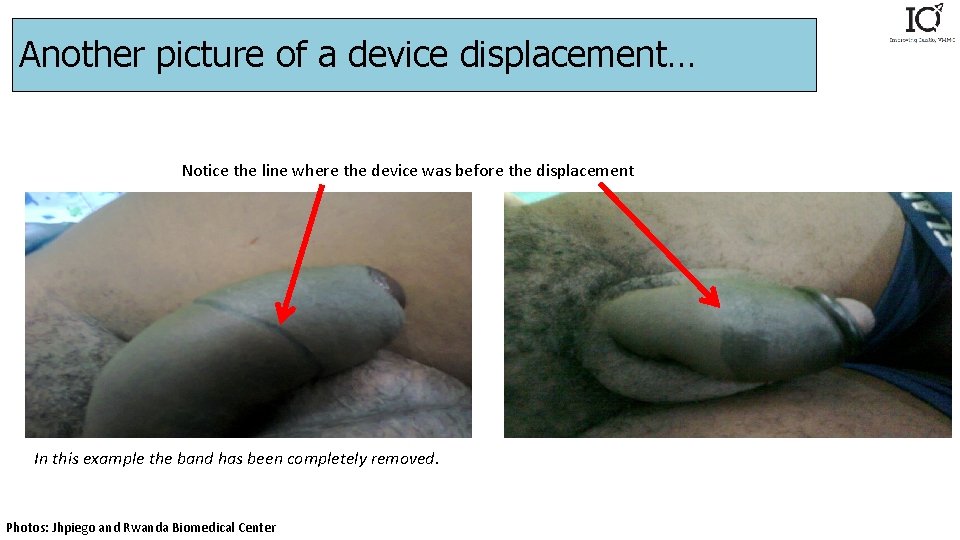
Another picture of a device displacement… Notice the line where the device was before the displacement In this example the band has been completely removed. Photos: Jhpiego and Rwanda Biomedical Center
Management of device displacement • Displaced or removed devices can only be safely replaced if done in the first few hours after placement, by a trained provider • After that, risk for swelling and infection rises, and foreskin tissue cannot survive; surgical VMMC needed • If VMMC-trained provider not present, a surgeon or a clinician with experience providing surgical circumcision may manage the client. Otherwise, the client ought to be referred to a site with providers trained in surgery in instances of altered anatomy (because of swelling), or referral hospital. • Here presenter should discuss VMMC team’s plan • Should include surgeon designated for referral
Management of other AEs with device in place • Contact VMMC team for help and to discuss • Odor and mild/moderate pain rarely need referral if area looks otherwise well; reassure client that odor is expected and rarely perceptible to others • Moderate/severe pain and other AEs may require removing device, but this typically requires urgent surgical VMMC and should first be discussed with the site where device was placed • Refer if not confident managing AE
Reporting • Report all cases of Adverse Events as per the national reporting policy • In your setting, is the site that diagnoses an AE responsible for reporting if it did not perform the procedure?
Summary • Know how to contact the VMMC team, what their emergency plans are, and what they tell clients to do in case of AEs • Call for help! • Most clients with common AEs need follow up in 24 hours, and sometimes daily afterward • Any bleeding, moderate or severe infection, or severe hematoma • See AE guide charts for details • If unsure, have patient return for an early review – this can save lives • VMMC may expose undiagnosed bleeding disorders • Any patient whose AE recurs or does not improve needs referral, even if mild • See AE guide for specific management guidance
Quiz
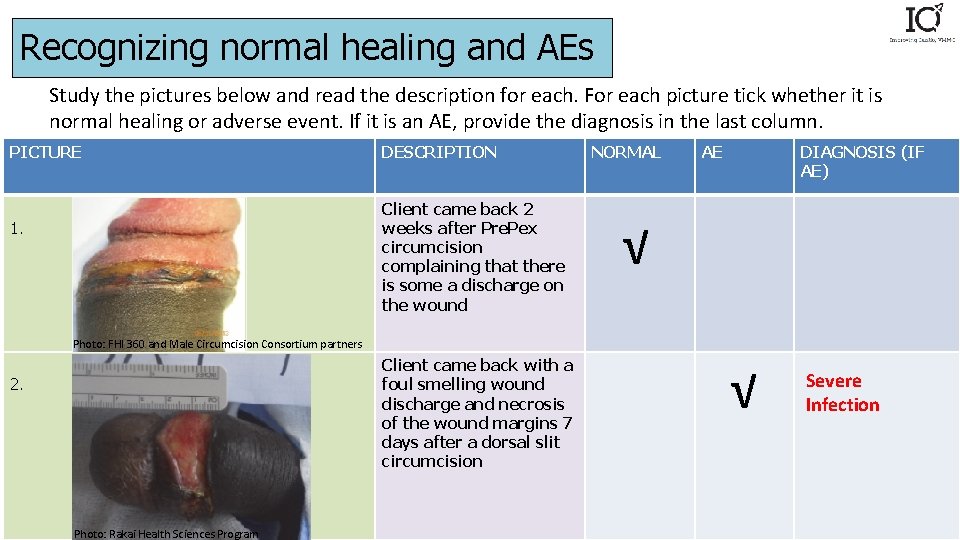
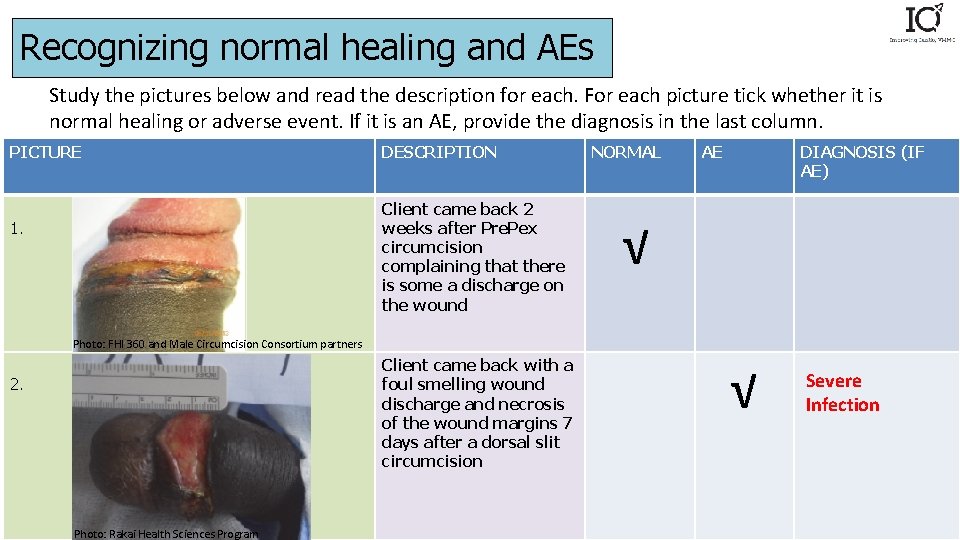
Recognizing normal healing and AEs Study the pictures below and read the description for each. For each picture tick whether it is normal healing or adverse event. If it is an AE, provide the diagnosis in the last column. PICTURE DESCRIPTION Client came back 2 weeks after Pre. Pex circumcision complaining that there is some a discharge on the wound 1. NORMAL AE DIAGNOSIS (IF AE) √ Photo: FHI 360 and Male Circumcision Consortium partners Client came back with a foul smelling wound discharge and necrosis of the wound margins 7 days after a dorsal slit circumcision 2. Photo: Rakai Health Sciences Program √ Severe Infection
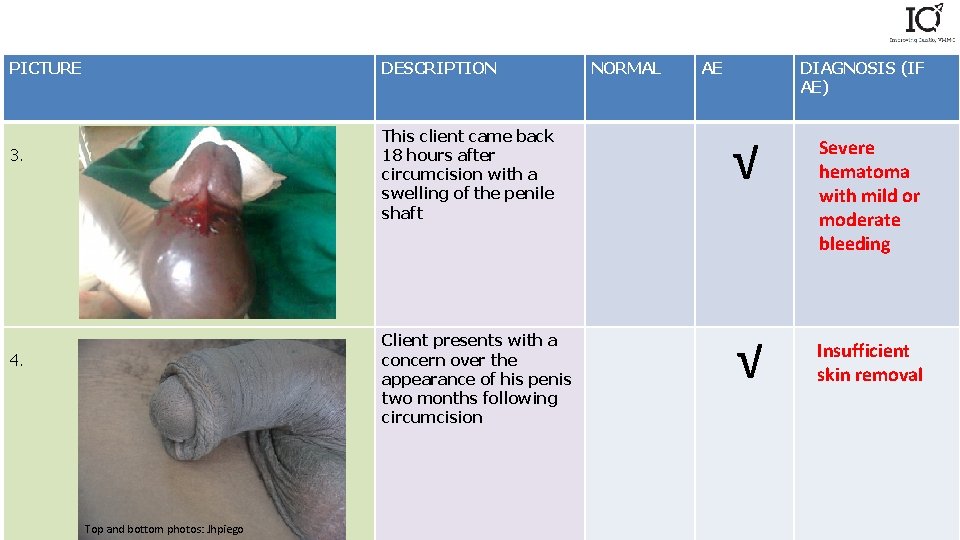
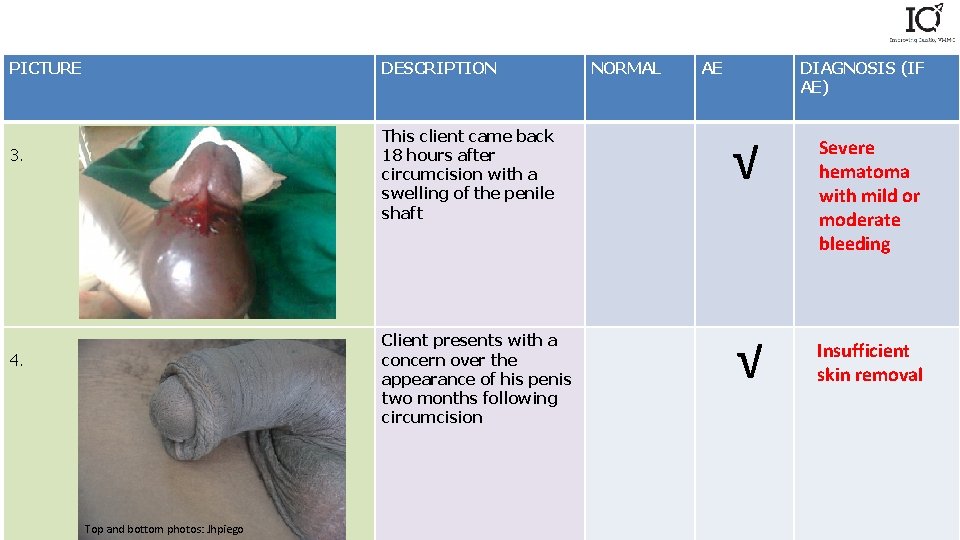
PICTURE DESCRIPTION 3. 4. Top and bottom photos: Jhpiego NORMAL AE DIAGNOSIS (IF AE) This client came back 18 hours after circumcision with a swelling of the penile shaft √ Client presents with a concern over the appearance of his penis two months following circumcision √ Severe hematoma with mild or moderate bleeding Insufficient skin removal
Case Studies
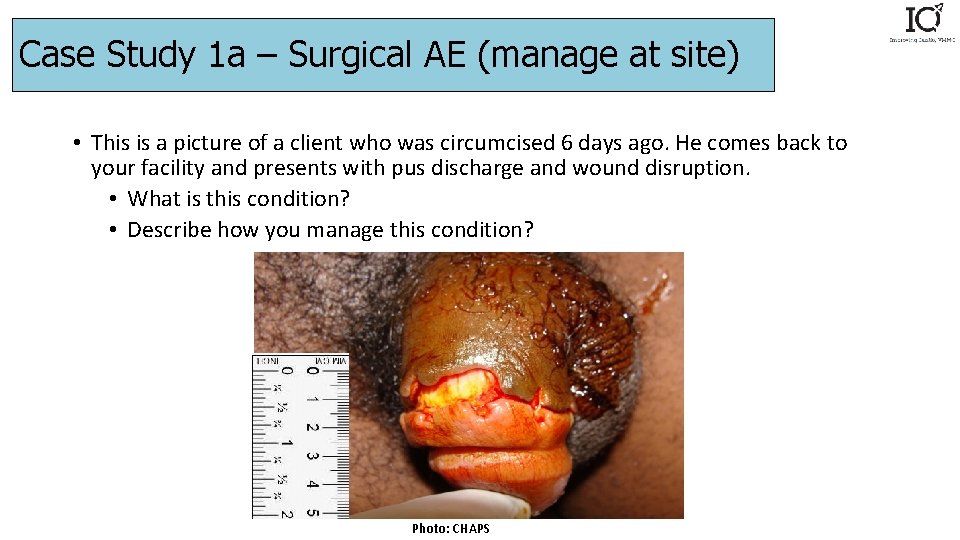
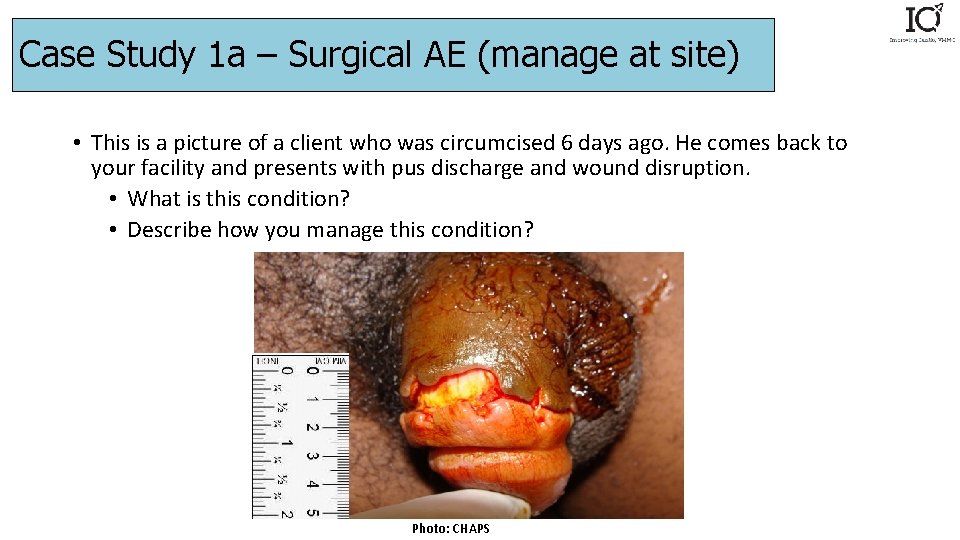
Case Study 1 a – Surgical AE (manage at site) • This is a picture of a client who was circumcised 6 days ago. He comes back to your facility and presents with pus discharge and wound disruption. • What is this condition? • Describe how you manage this condition? Photo: CHAPS
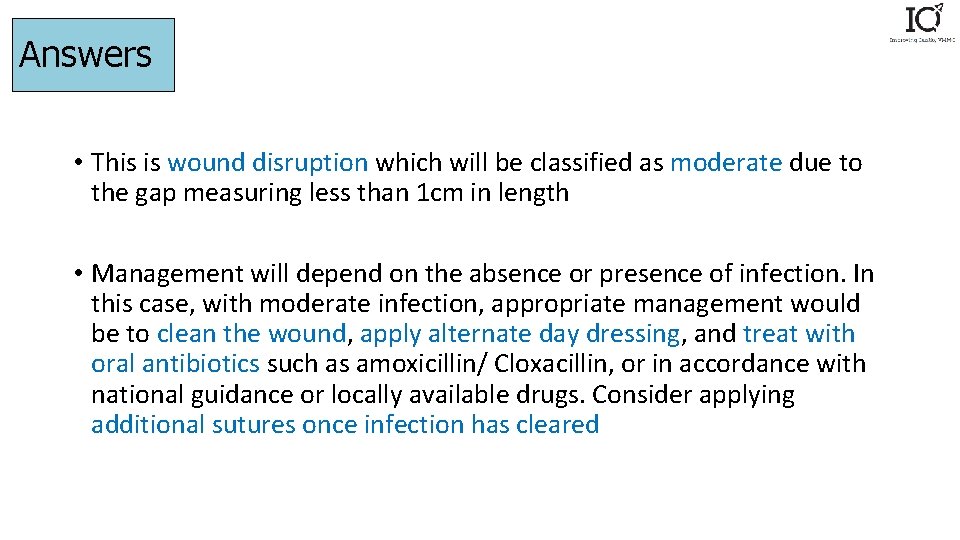
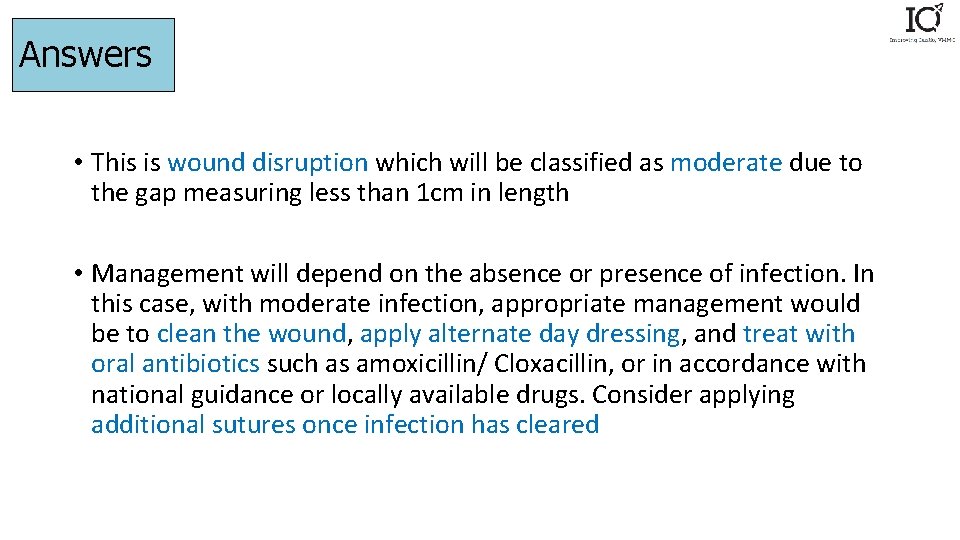
Answers • This is wound disruption which will be classified as moderate due to the gap measuring less than 1 cm in length • Management will depend on the absence or presence of infection. In this case, with moderate infection, appropriate management would be to clean the wound, apply alternate day dressing, and treat with oral antibiotics such as amoxicillin/ Cloxacillin, or in accordance with national guidance or locally available drugs. Consider applying additional sutures once infection has cleared
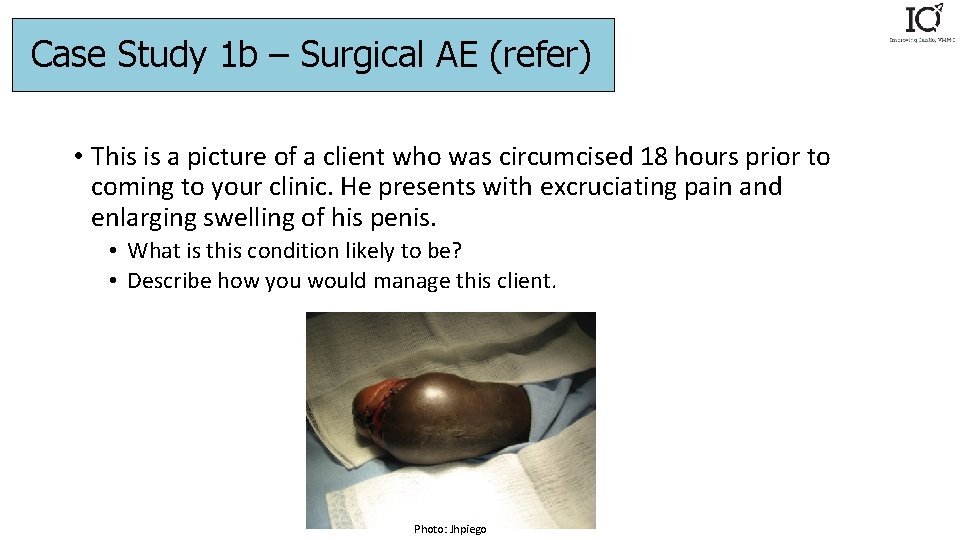
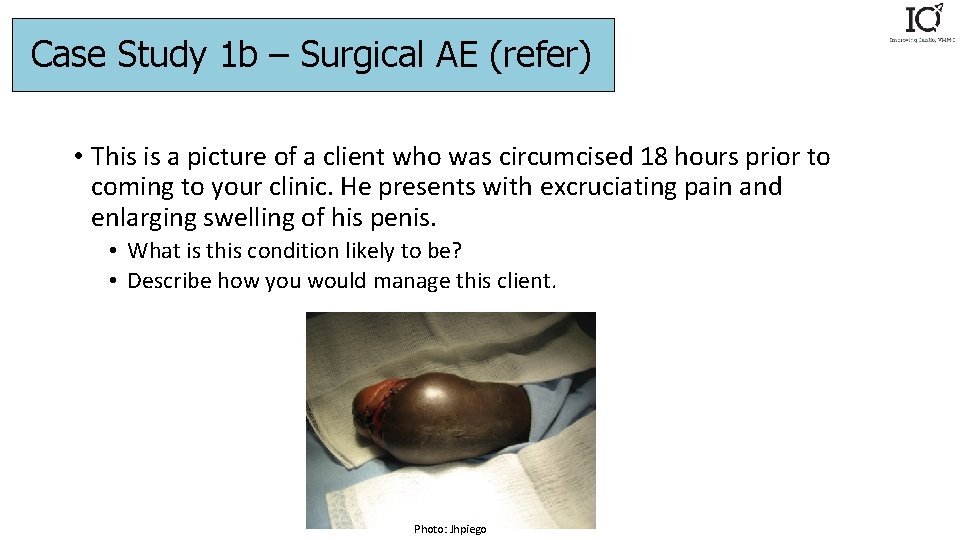
Case Study 1 b – Surgical AE (refer) • This is a picture of a client who was circumcised 18 hours prior to coming to your clinic. He presents with excruciating pain and enlarging swelling of his penis. • What is this condition likely to be? • Describe how you would manage this client. Photo: Jhpiego
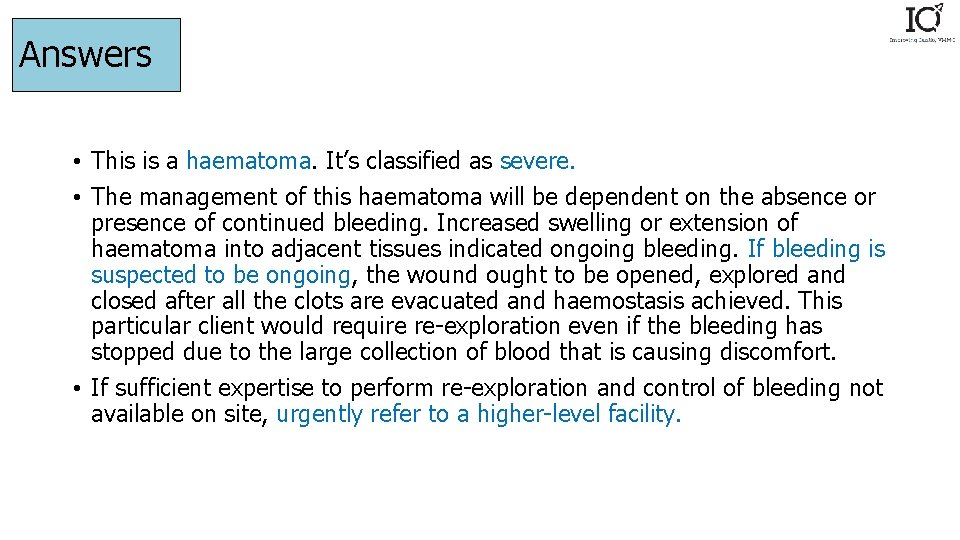
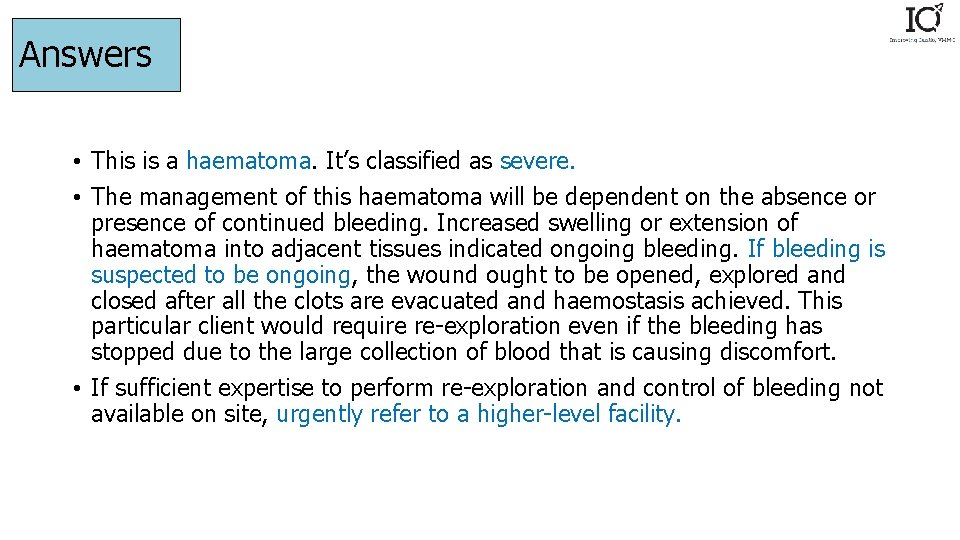
Answers • This is a haematoma. It’s classified as severe. • The management of this haematoma will be dependent on the absence or presence of continued bleeding. Increased swelling or extension of haematoma into adjacent tissues indicated ongoing bleeding. If bleeding is suspected to be ongoing, the wound ought to be opened, explored and closed after all the clots are evacuated and haemostasis achieved. This particular client would require re-exploration even if the bleeding has stopped due to the large collection of blood that is causing discomfort. • If sufficient expertise to perform re-exploration and control of bleeding not available on site, urgently refer to a higher-level facility.
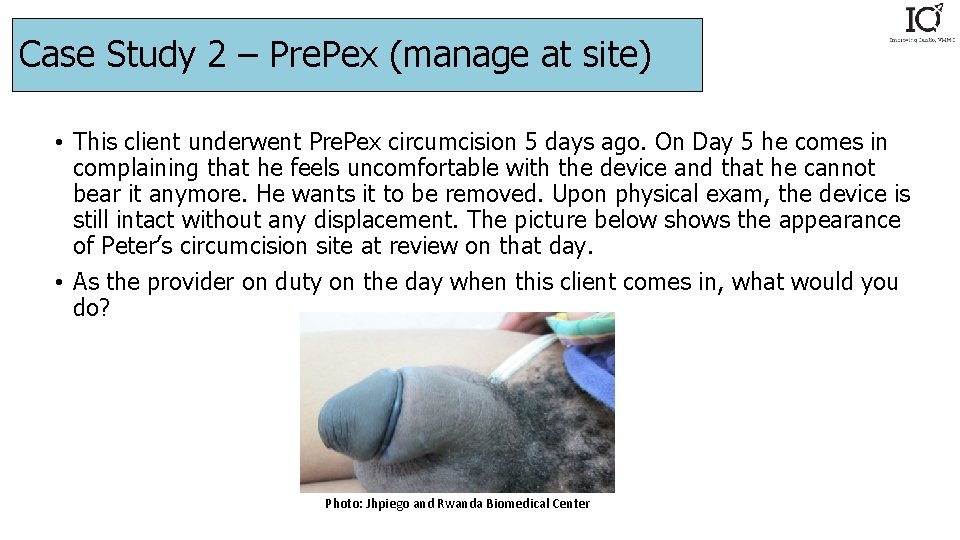
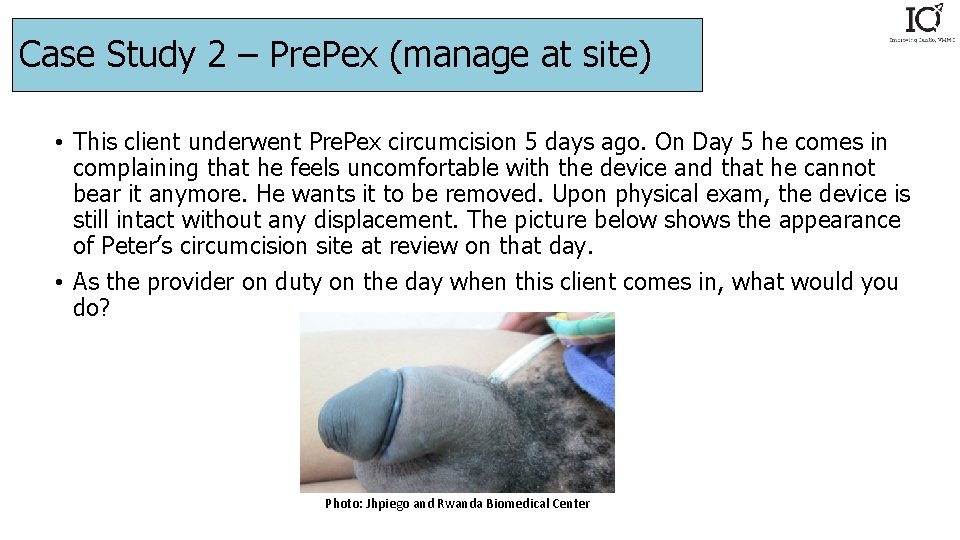
Case Study 2 – Pre. Pex (manage at site) • This client underwent Pre. Pex circumcision 5 days ago. On Day 5 he comes in complaining that he feels uncomfortable with the device and that he cannot bear it anymore. He wants it to be removed. Upon physical exam, the device is still intact without any displacement. The picture below shows the appearance of Peter’s circumcision site at review on that day. • As the provider on duty on the day when this client comes in, what would you do? Photo: Jhpiego and Rwanda Biomedical Center
Answers • Clients may come back wanting the device to be removed because of the discomfort and the change in the skin color. • Assure the client that what they are seeing is the normal process following the device placement. • Encourage client to wait for two more days for removal. • Refer client for removal if he insists
Thank you!
 Circumcised vs uncircumcised gentiles
Circumcised vs uncircumcised gentiles Male circumcision
Male circumcision Male circumcision
Male circumcision Male circumcision
Male circumcision Is an indirect voluntary act still voluntary?
Is an indirect voluntary act still voluntary? Adverse events following immunization (aefi) course answers
Adverse events following immunization (aefi) course answers Adverse events in hospital
Adverse events in hospital Ir adverse event
Ir adverse event Puerperal sepsis
Puerperal sepsis Circumcision
Circumcision Circumcised
Circumcised Heart pure meaning
Heart pure meaning Ptsd circumcision
Ptsd circumcision Disadvantages of circumcision
Disadvantages of circumcision Circumcision
Circumcision Circumcision
Circumcision Circumcision
Circumcision Circumcision
Circumcision Vaginaltoppen
Vaginaltoppen Mutually exclusive events vs not mutually exclusive events
Mutually exclusive events vs not mutually exclusive events Chapter 13 medical records management workbook answers
Chapter 13 medical records management workbook answers Adverse selection
Adverse selection Azalastyna
Azalastyna Overdriving headlights means
Overdriving headlights means Adverse selection
Adverse selection Adverse yaw
Adverse yaw Beta blockers moa
Beta blockers moa Adverse childhood experiences study
Adverse childhood experiences study Adverse treatment
Adverse treatment Adverse selektion
Adverse selektion Analgesic mechanism
Analgesic mechanism No adverse remarks meaning
No adverse remarks meaning What are adverse childhood experiences
What are adverse childhood experiences What is adverse selection
What is adverse selection Novartis adverse event reporting
Novartis adverse event reporting Adverse event adalah
Adverse event adalah Harley nadler
Harley nadler Tools to help solve adverse selection problems
Tools to help solve adverse selection problems Adverse selection
Adverse selection Unanticipated problem vs adverse event
Unanticipated problem vs adverse event Adverse yaw
Adverse yaw If you are driving under adverse conditions
If you are driving under adverse conditions