Introduction to PCMHI Functions CCC CM and How











- Slides: 51

Introduction to PC-MHI Functions: CCC, CM, and How they Work Together Katherine M. Dollar, Ph. D Sara Greenwood, MSW Johanna Klaus, Ph. D
Definitions* *Provided by Dr. Christopher Hunter from literature synthesis for shared definitions �Integrated Care is an overarching term conceptually defined as: A form of care where behavioral health and primary care providers interact in a systematic manner to meet the behavioral health and health needs of their patients. Or: “…Unifies care for physical and mental concerns” AHRQ 2008 Butler et al.
Introduction to Co-located, Collaborative Care Katherine M. Dollar, Ph. D August 2011 Based on material previously presented by Andrew Pomerantz, MD and Margaret Dundon, Ph. D

Co-location/Co-located Service A behavioral health provider working in a space that is embedded in (or in close proximity to ) a primary care clinic. Collaborative Care/Collaboration The interactions between primary care and behavioral health providers for the purpose of developing treatment plans, providing clinical services and coordinating care to meet the physical and behavioral health needs of patients.

Co-located Collaborative Care �A state of mind as much as a program �A platform for treatment, not a treatment �Many Dimensions
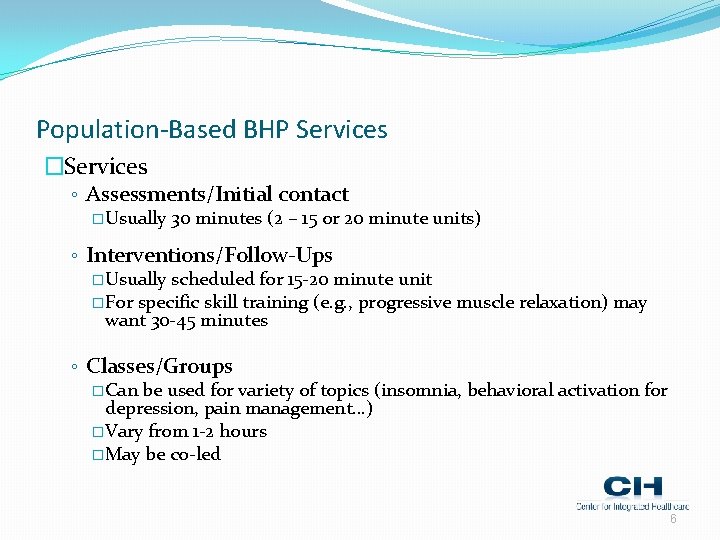
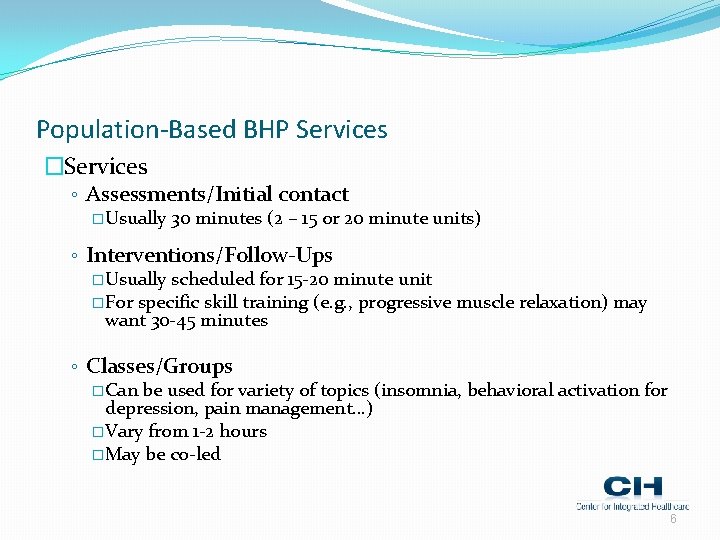
Population-Based BHP Services �Services ◦ Assessments/Initial contact � Usually 30 minutes (2 – 15 or 20 minute units) ◦ Interventions/Follow-Ups � Usually scheduled for 15 -20 minute unit � For specific skill training (e. g. , progressive muscle relaxation) may want 30 -45 minutes ◦ Classes/Groups � Can be used for variety of topics (insomnia, behavioral activation for depression, pain management…) � Vary from 1 -2 hours � May be co-led 6
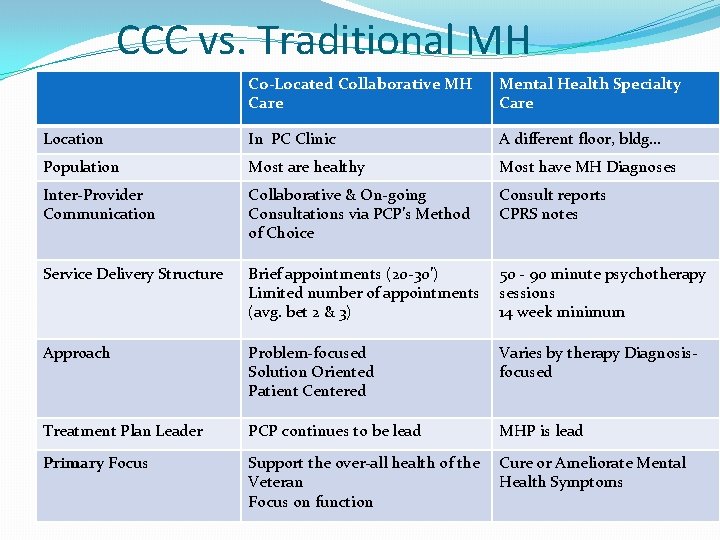
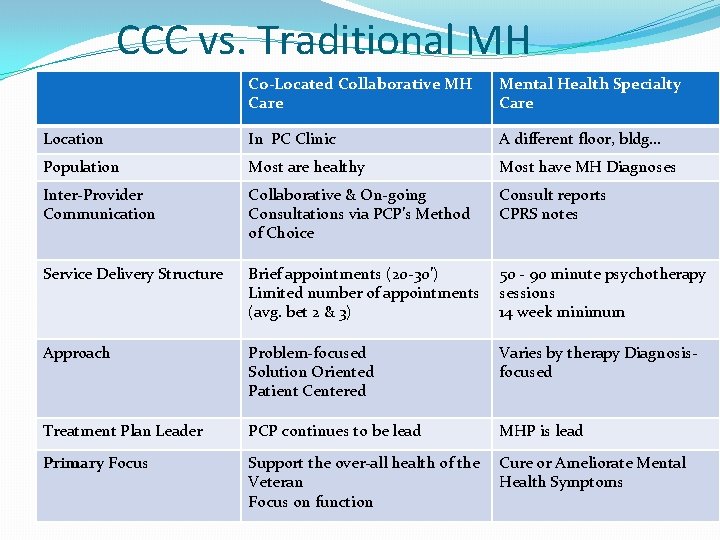
CCC vs. Traditional MH Co-Located Collaborative MH Care Mental Health Specialty Care Location In PC Clinic A different floor, bldg… Population Most are healthy Most have MH Diagnoses Inter-Provider Communication Collaborative & On-going Consultations via PCP’s Method of Choice Consult reports CPRS notes Service Delivery Structure Brief appointments (20 -30’) Limited number of appointments (avg. bet 2 & 3) 50 - 90 minute psychotherapy sessions 14 week minimum Approach Problem-focused Solution Oriented Patient Centered Varies by therapy Diagnosisfocused Treatment Plan Leader PCP continues to be lead MHP is lead Primary Focus Support the over-all health of the Veteran Focus on function Cure or Ameliorate Mental Health Symptoms
Population-Based Behavioral Health Care: CCC �Designed to have largest effect on population and maximal help to PC patients and providers: A little service for a lot of pts vs. traditional MH ◦ Co-location (embedded) �Advanced access (prn tx) and warm handoffs ◦ BHP may see 10 -15 pts a day (Visn 2 target: 8 -10) with limited follow-up (2 -3 visits on average) ◦ Collaboration- develop biopsychosocial treatment plan with PCP and other team members (pharmacist/social worker/dietitian/nurses…) 8
Staffing an integrated care program �Psychiatrist or APN �Behaviorist (Psychologist or LCSW) �Support Staff (some have separate clerks, some use PC clerks) �PACT: Teams and Teamlets 9
Scheduling �Open Access: from no scheduled appointments (WRJ) to limited schedule appointments or alternating scheduled and open �Minimizes wait times �Allows warm hand-offs and increases linkage success �Passes the endorsement of the PCP to the BHP 10
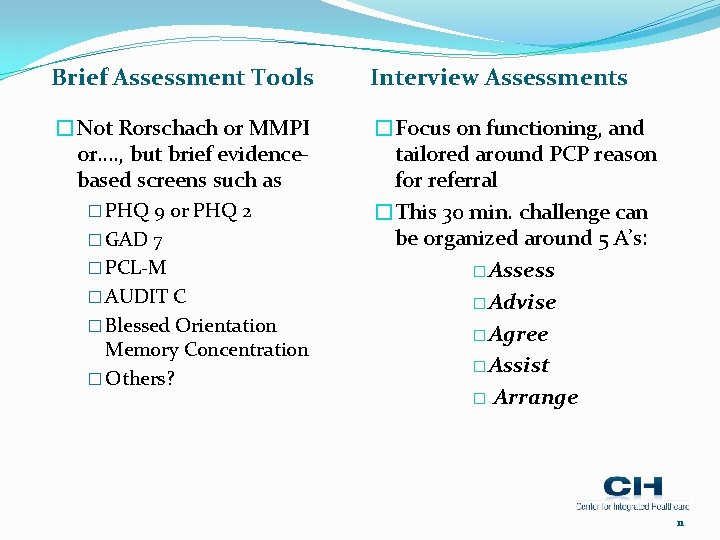
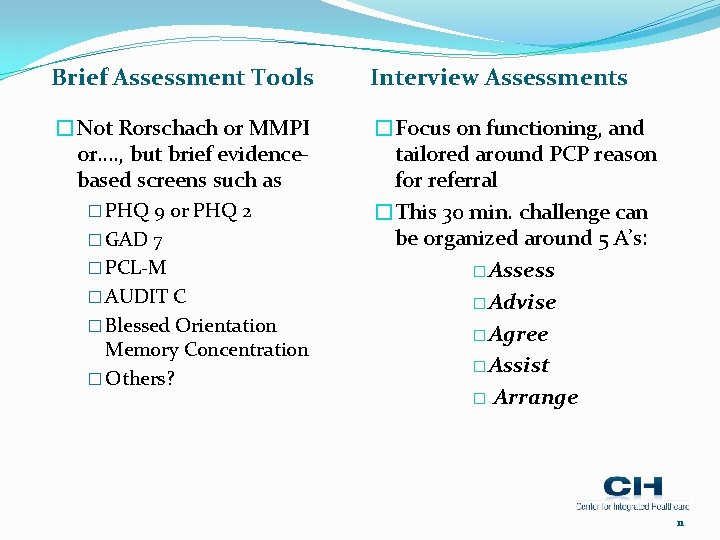
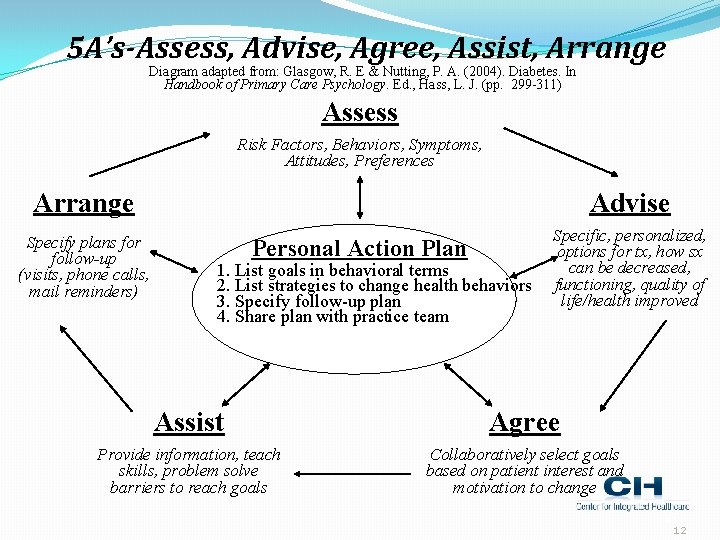
Brief Assessment Tools Interview Assessments �Not Rorschach or MMPI or…. , but brief evidencebased screens such as �Focus on functioning, and tailored around PCP reason for referral �This 30 min. challenge can be organized around 5 A’s: � Assess � Advise � Agree � Assist � Arrange � PHQ 9 or PHQ 2 � GAD 7 � PCL-M � AUDIT C � Blessed Orientation Memory Concentration � Others? 11
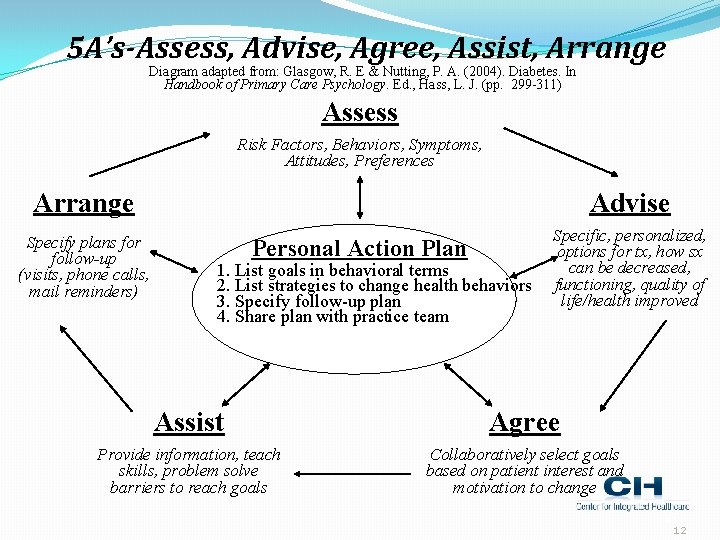
5 A’s-Assess, Advise, Agree, Assist, Arrange Diagram adapted from: Glasgow, R. E & Nutting, P. A. (2004). Diabetes. In Handbook of Primary Care Psychology. Ed. , Hass, L. J. (pp. 299 -311) Assess Risk Factors, Behaviors, Symptoms, Attitudes, Preferences Arrange Advise Specify plans for follow-up (visits, phone calls, mail reminders) Specific, personalized, options for tx, how sx can be decreased, functioning, quality of life/health improved Personal Action Plan 1. List goals in behavioral terms 2. List strategies to change health behaviors 3. Specify follow-up plan 4. Share plan with practice team Assist Agree Provide information, teach skills, problem solve barriers to reach goals Collaboratively select goals based on patient interest and motivation to change 12 12
Brief Interventions �Motivational Interviewing �Brief Interventions for SUDs �Problem Solving Therapy �Acceptance and Commitment Therapy �Psychiatric consultations with PCPs 13

CCC Domains of Competency �Domain 1: Clinical Practice �Domain 2: Practice Management �Domain 3: Consultation �Domain 4: Documentation �Domain 5: Teamwork �Domain 6: Administrative Skills 14
General Practice Management Skills �Teaching PCPs what BHPs can offer �Teaching PCPs how to do effective warm hand-offs �Teaching BHPs how to provide BRIEF, cogent summaries of impression and recommendations to PCP in 3 min. or less �Teaching patients self-management skills 15
Tips for Start-Up �This is a new approach to care for many, not a natural shift �PCPs have worked without the support thus far, and often do not know how to use it or understand how it is helpful �BHPs have to promote services and show success from interventions �Shift to seeing PCP as customer 16
Care Management Johanna Klaus, Ph. D
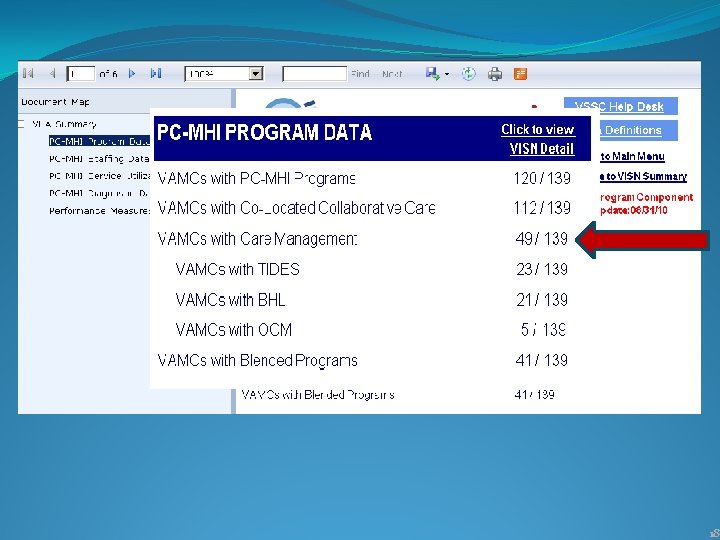
18
Care Management �Algorithm-based care that includes routine monitoring/assessment of patients focusing on �Psychoeducation; encourage self-management skills �Brief treatment including (but not limited to) medication �Adherence to medication, treatment plan �In consultation with the supervising clinician, provide relevant information to the PCP to allow collaboration for appropriate care decisions
Key Components of CM �Offer telephonic contact �Much appreciated by patients �Stepped Care Approach �Strong ties to mental health supervision �Initial decisions and prescribing in primary care �Assessment based �Tracking important �Emphasis on patient self-management support �Care manager – facilitates communication
Interventions: What can be done? �Watchful Waiting �Veteran’s preference �Medication monitoring �Brief interventions, eg. for alcohol misuse �Brief treatment: eg. problem-solving, behavioral activation �Refer to Specialty Mental Health
Why care management? �Supports Veteran-centered care – incorporates convenience and preference �Better symptom and functional outcomes �Greater adherence to treatment �Reduced mortality �Greater engagement in care
Current Evidence Base �Depression – very good evidence �Anxiety – evidence from a few studies �Substance Use �Alcohol - very good evidence for brief intervention �Prescription and non-prescription drugs – very few studies yet �Post Traumatic Stress Disorder and Chronic Pain – little evidence yet; studies in process
Large RCTs supporting Care Management �PROSPECT study: more patients treated for depression, decline in suicidal ideation, faster resolution of depressive symptoms �IMPACT study: faster decline in rates of suicidal ideation, more favorable course of depression in both degree and speed of symptom reduction
Role of the Care Manager �Assessment and triage �Decision support �Patient education and activation �Monitor adherence to treatment, treatment outcomes, and medication side effects �Follow-up with pts 6 -8 times over 6 months �Collaborate with mental health specialists �Support patient self-management �Referral management
Care Managers �Nurses and social workers most commonly, but others serve as care managers including psychologists �Content of contacts may differ depending on discipline – but includes active follow-up, measurement-based care, medication monitoring (when appropriate) and supporting patient selfmanagement
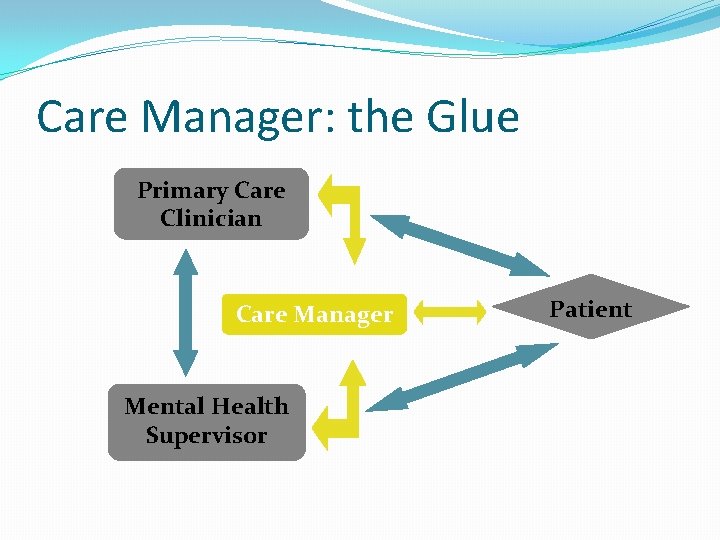
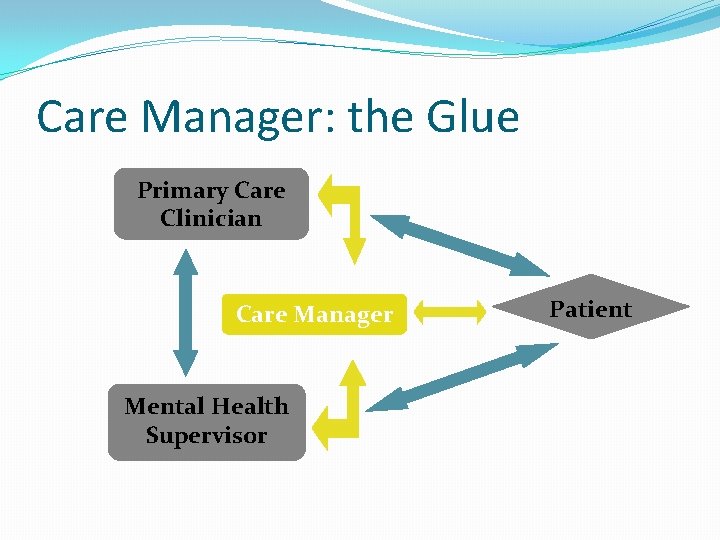
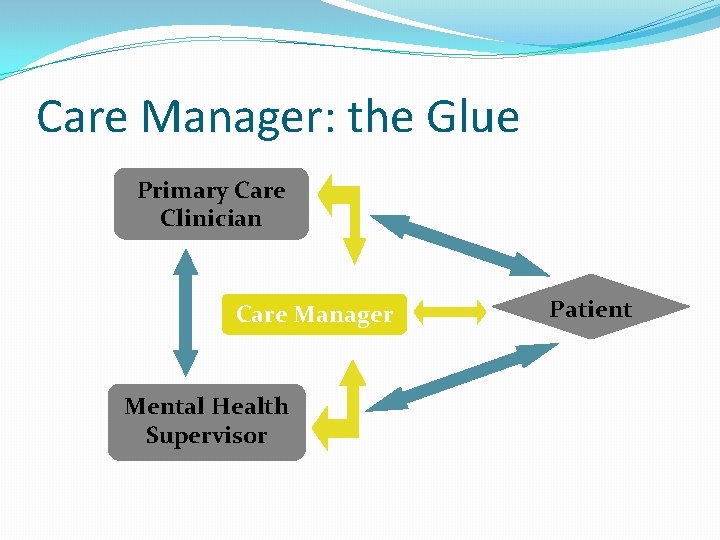
Care Manager: the Glue Primary Care Clinician Care Manager Mental Health Supervisor Patient
Care Manager Supervisor �Typically psychiatrist, sometimes a psychologist, preferably someone with integrated care clinical experience �Regular supervision, i. e. weekly �Encourage PC providers to prescribe; provide recommendations via care management supervision �Get to know PC providers; provide consultation
Case Example
Mr. Howell During his PCP visit , Mr. Howell, a 59 year old male with osteoarthritis, diabetes and hypertension told his PCP that in the past few weeks he had not been feeling very well. He tells his doctor, “I’m sleeping a lot more than usual—I don’t have to get up for work, but I really don’t feel like getting out of bed. I just don’t have any energy. ” He has gained 10 pounds since losing his job and reports his blood sugars are often in the 180 -240 range. His PHQ-2 is positive & AUDIT-C score is 1. He does not want to stay to talk someone because he wants to beat the traffic. How are patients identified? 30
Assessment �Goals of assessment: • Establish Veteran needs and preferences for treatment • Identify patients appropriate for care management services • Recognize patients who may benefit from higherintensity treatment �Provide "on-time, on-target" information to PCPs and collaboratively make appropriate care decisions �Assessment tools & triage options may vary by site 31
Mr. Howell • Contact Mr. Howell next day by the telephone • PHQ-9 score is 13 • He denies past or present suicidal ideation. • No history of mental health concerns; medical comorbidities include osteoarthritis, diabetes and hypertension • “Since I was laid off a few months ago from my manufacturing job, all I do is sit around the house. My mood is OK, but when I think about money and my financial future, it starts to really bother me; I feel like a failure to my family. ” • Stopped socializing with his friends and family members, notes that he especially misses visiting with his grandchildren. • Mr. Howell expresses hesitation in treatment for depression What do we learn from the assessment? 32

Decision Support � Treatment algorithms are a set of decision rules aimed at reducing variability in treatment and maximizing patients’ ability to achieve full remission. � The data gathered during the initial assessment help the care manager decide upon a treatment plan to suggest to the PCP. � Although care managers play a critical part in depression treatment, they do not make treatment decisions or prescribe medications. The patient’s PCP will make final decisions about prescribing medicines; the care manager’s input on diagnosis, co-morbidities and other treatment factors will help guide the provider’s choices. 33
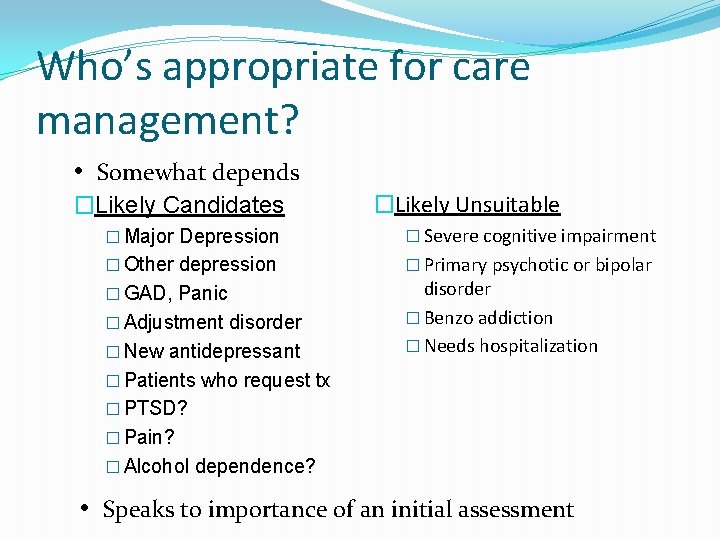
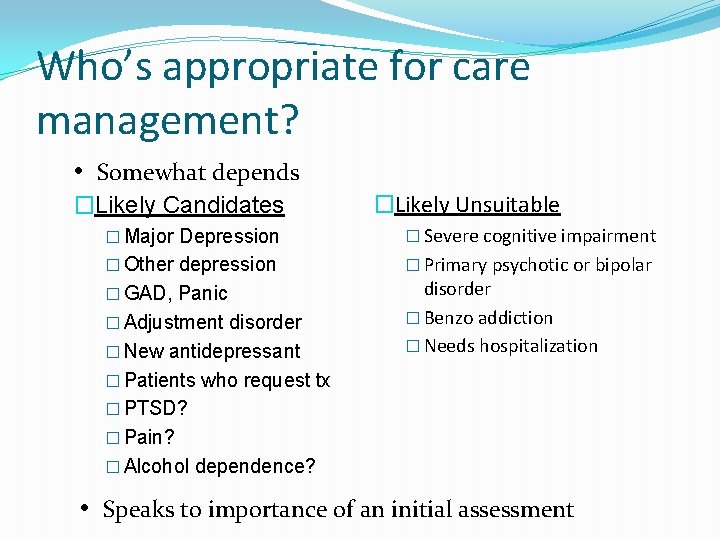
Who’s appropriate for care management? • Somewhat depends �Likely Candidates �Likely Unsuitable � Major Depression � Severe cognitive impairment � Other depression � Primary psychotic or bipolar � GAD, Panic � Adjustment disorder � New antidepressant disorder � Benzo addiction � Needs hospitalization � Patients who request tx � PTSD? � Pain? � Alcohol dependence? • Speaks to importance of an initial assessment
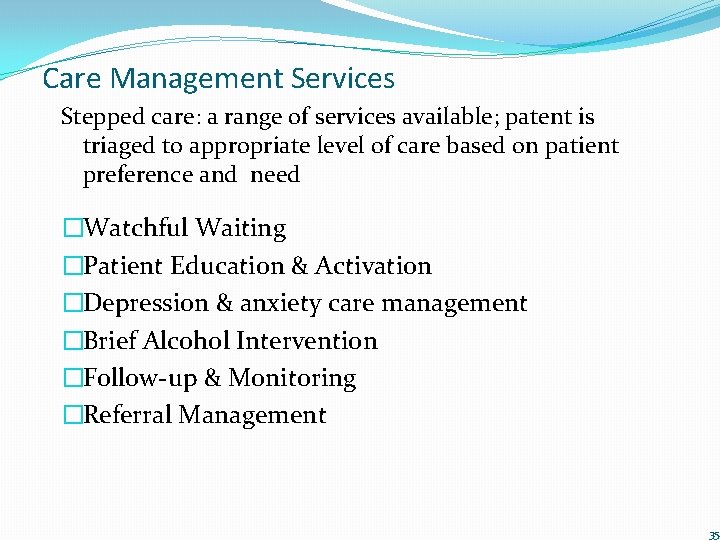
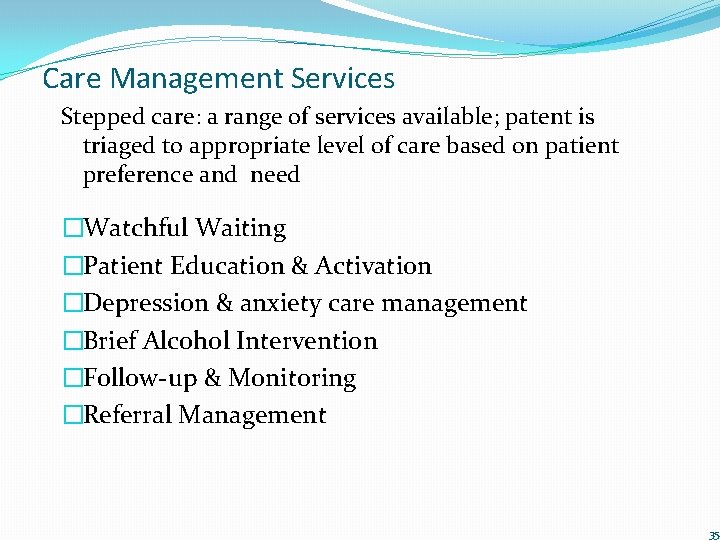
Care Management Services Stepped care: a range of services available; patent is triaged to appropriate level of care based on patient preference and need �Watchful Waiting �Patient Education & Activation �Depression & anxiety care management �Brief Alcohol Intervention �Follow-up & Monitoring �Referral Management 35
Mr. Howell What treatment plan recommendations would you make? 36

Mr. Howell After 5 weeks of monitoring and behavioral activation over the phone, Mr. Howell’s PHQ remains above 10. He is agreeable to trying an antidepressant. 37

Supervision �Care manager presents case to MH supervisor who recommends starting on a medication (Celexa 10 mg, increase to 20 mg after 1 week if tolerated). �Care manager follow-ups with PCP regarding recommendation �Care manager follows-up with Veteran and schedules contact for 1 week post medication start 38
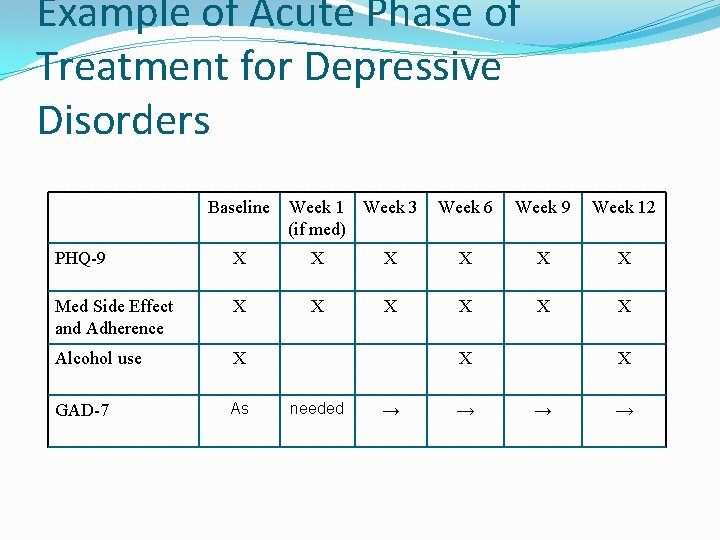
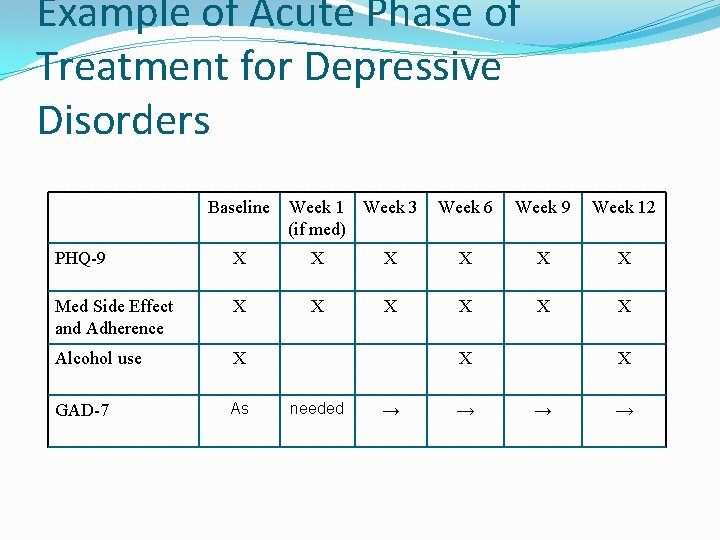
Example of Acute Phase of Treatment for Depressive Disorders Baseline Week 1 Week 3 (if med) Week 6 Week 9 Week 12 PHQ-9 X X X Med Side Effect and Adherence X X X Alcohol use X GAD-7 As X needed → → X → →
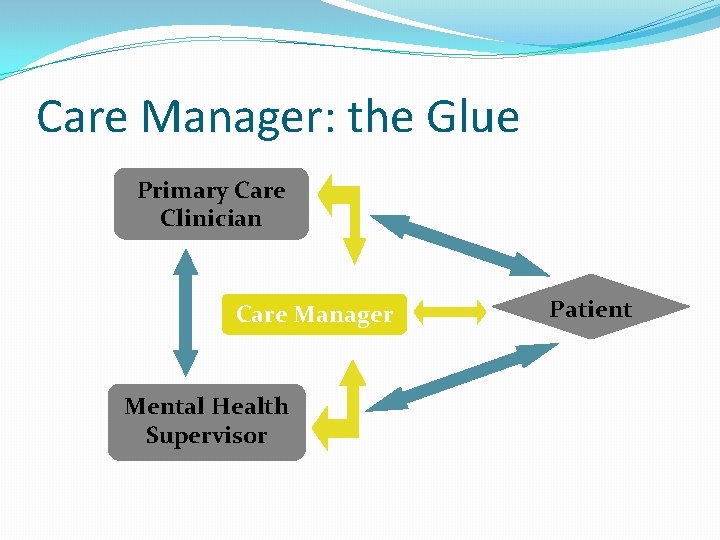
Care Manager: the Glue Primary Care Clinician Care Manager Mental Health Supervisor Patient
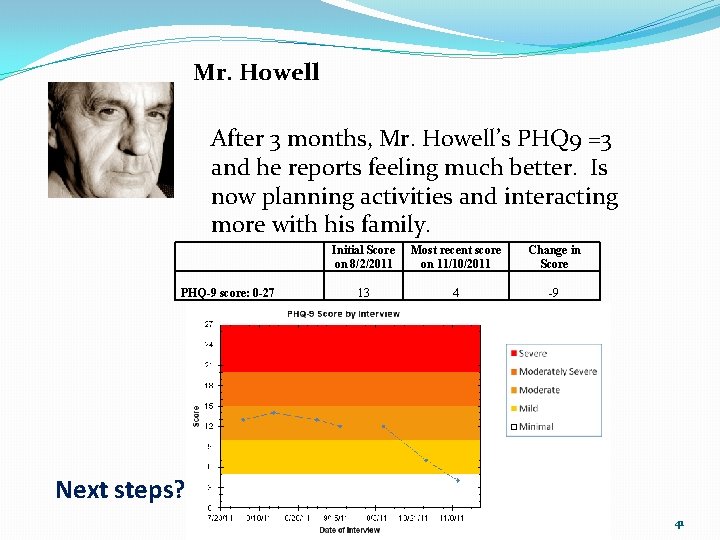
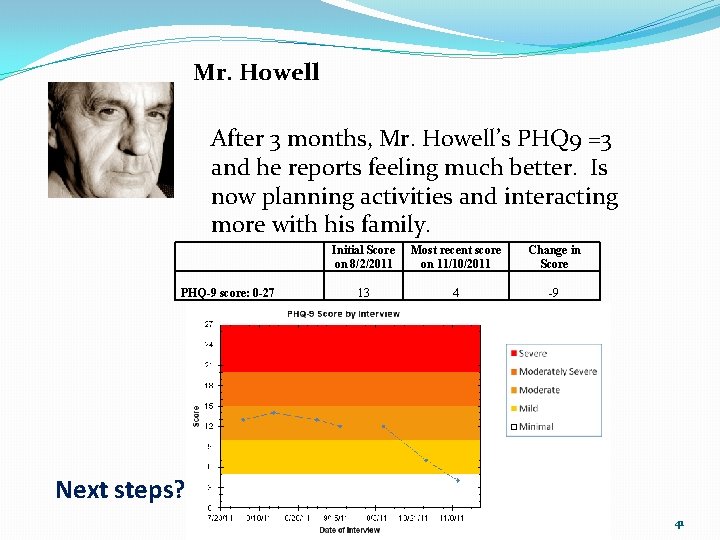
Mr. Howell After 3 months, Mr. Howell’s PHQ 9 =3 and he reports feeling much better. Is now planning activities and interacting more with his family. PHQ-9 score: 0 -27 Initial Score on 8/2/2011 Most recent score on 11/10/2011 Change in Score 13 4 -9 Next steps? 41
Maintenance and relapse prevention �Follow-up 1 time/month for next 2 months �Provide education on relapse prevention �Per supervision, provide PCP recommendation on medication discontinuation 42
Review Articles �Bower, P. , et al. (2006). British Journal of Psychiatry, 189, 484 – 493. �Gilbody, S. , et al. (2006). Arch Intern Med, 166(21), 2314 -21. �Williams, J. W. , et al. (2007). General Hospital Psychiatry, 29(2), 91 -116. �Roy-Byrne, et al. (2010) JAMA, 303(19): 1921 -1928

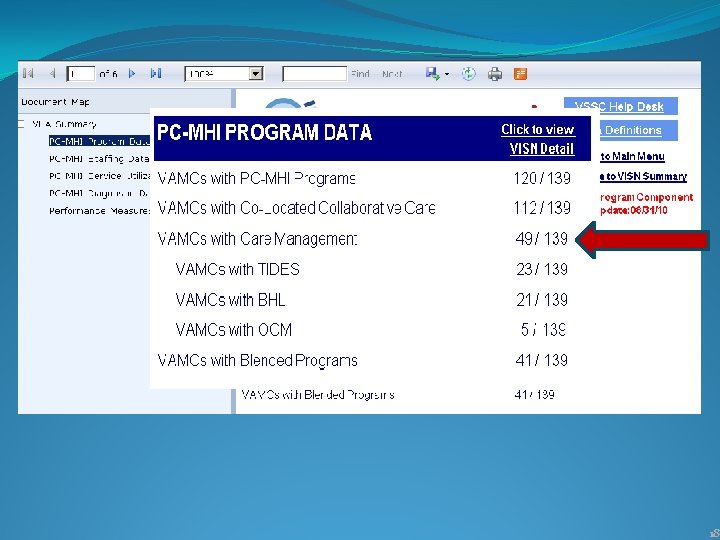
In case you have heard of these… Care Management Models in PC-MHI �Translating Initiatives for Depression into Effective Solutions (TIDES) • Evidence-based collaborative care model supporting depression management in the primary care setting • Has promoted improvements in treatment adherence for Veterans with depression in several VISNs �Behavioral Health Laboratory (BHL) • Evidence based clinical service supporting mental health and substance abuse management in the primary care setting • Associated with a significant increase in screening and identification of patients needing MH/SA services (Oslin, et. al. 2005) �Other evidence based strategies approved by the Office of Mental Health Services (ex. IMPACT) 44
Introduction to Blending Programs Sara Greenwood, MSW PC-MHI Education & Training Coordinator With acknowledgement to Mr. Lawrence Daily, LMSW, Network 16 Integrated Care Coordinator for his contribution to content development. 45
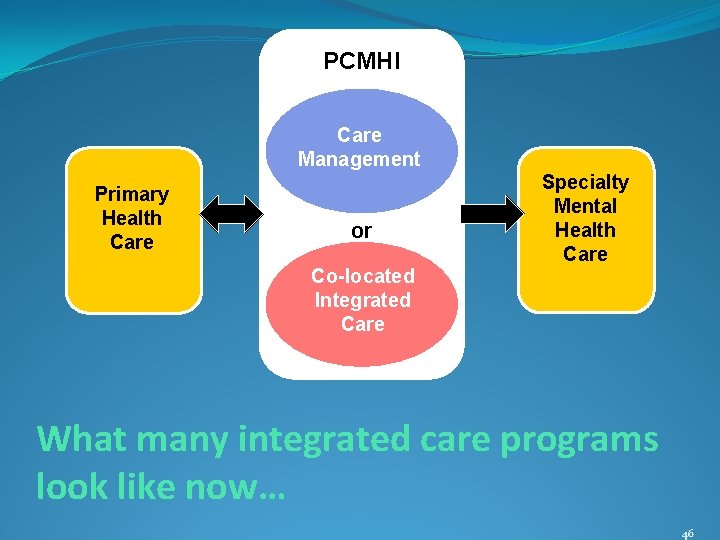
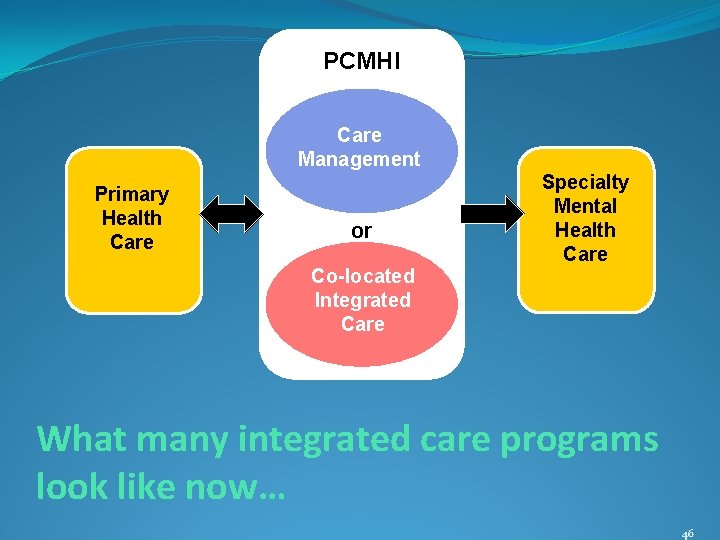
PCMHI Care Management Primary Health Care or Specialty Mental Health Care Co-located Integrated Care What many integrated care programs look like now… 46

47
Quickly divide into groups of 4 -6 & discuss the following questions [don’t forget to assign a note-taker!]: • What are the functions of colocated collaborative care? • What are the functions of care management? • What functions are similar? • How are the functions complementary? • What unique contributions do each provide? Small Group Pop Quiz! 48

PCMHI Care Management Primary Health Care BLENDED Co-located Integrated Care Specialty Mental Health Care A Well-functioning Blended Program Care managers & co-located collaborative care staff work as a team to provide services to Primary Care Providers and act as a liaison with specialty mental health care services. 49
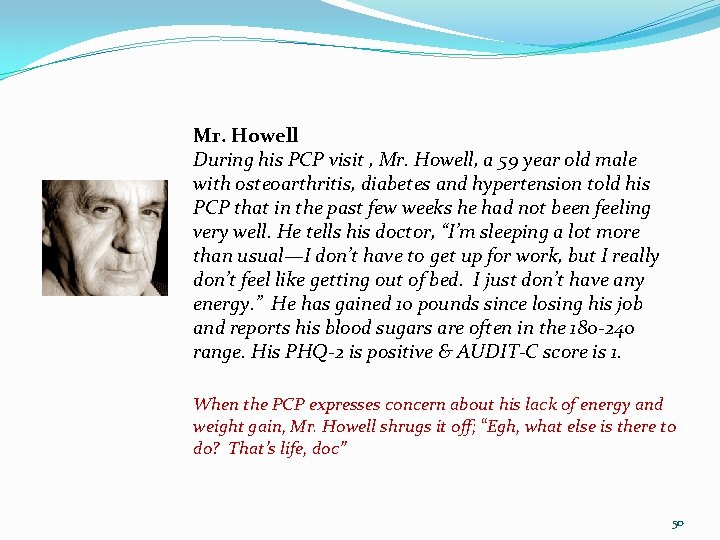
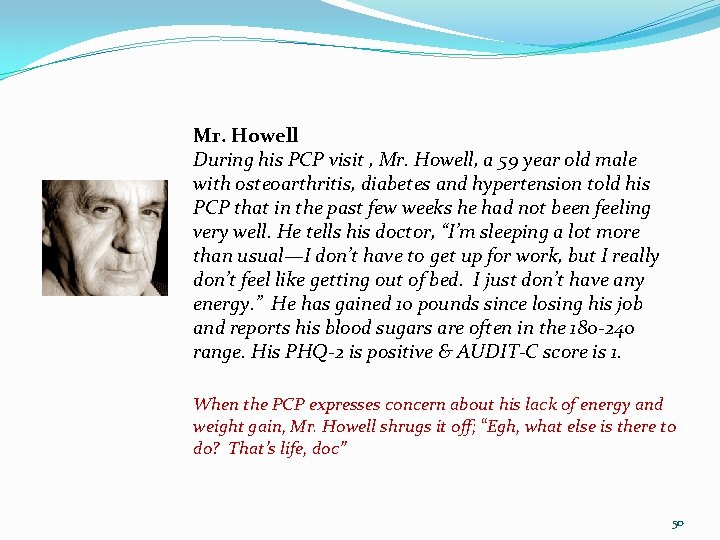
Mr. Howell During his PCP visit , Mr. Howell, a 59 year old male with osteoarthritis, diabetes and hypertension told his PCP that in the past few weeks he had not been feeling very well. He tells his doctor, “I’m sleeping a lot more than usual—I don’t have to get up for work, but I really don’t feel like getting out of bed. I just don’t have any energy. ” He has gained 10 pounds since losing his job and reports his blood sugars are often in the 180 -240 range. His PHQ-2 is positive & AUDIT-C score is 1. When the PCP expresses concern about his lack of energy and weight gain, Mr. Howell shrugs it off; “Egh, what else is there to do? That’s life, doc” 50

Mr. Howell During his PCP visit , Mr. Howell, a 59 year old male with osteoarthritis, diabetes and hypertension told his PCP that in the past few weeks he had not been feeling very well. He tells his doctor, “I’m sleeping a lot more than usual—I don’t have to get up for work, but I really don’t feel like getting out of bed. I just don’t have any energy. ” He has gained 10 pounds since losing his job and reports his blood sugars are often in the 180 -240 range. His PHQ-2 is positive & AUDIT-C score is 1. Toward the end of the appointment, Mr. Howell tears up. “I just sit around the house all day. ” “Not being able to play with my grandkids… my wife is working extra shifts to pay the bills, I just can’t handle it all. ” 51