Introduction 1 UPPP is the most common surgical

- Slides: 22
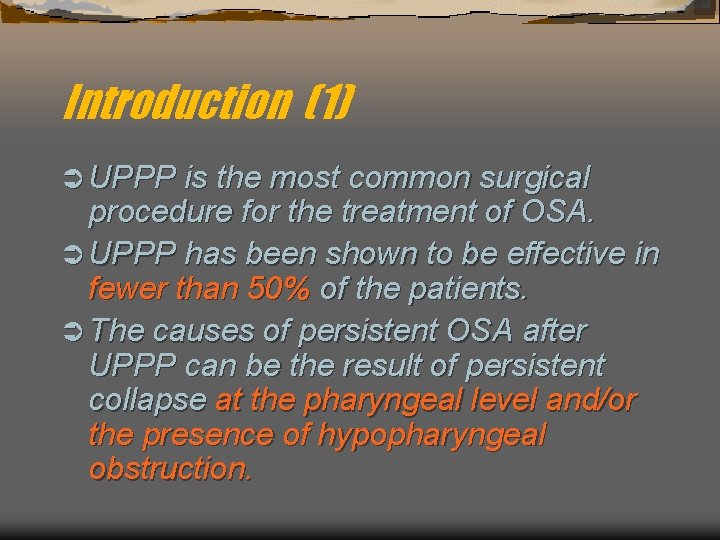
Introduction (1) Ü UPPP is the most common surgical procedure for the treatment of OSA. Ü UPPP has been shown to be effective in fewer than 50% of the patients. Ü The causes of persistent OSA after UPPP can be the result of persistent collapse at the pharyngeal level and/or the presence of hypopharyngeal obstruction.
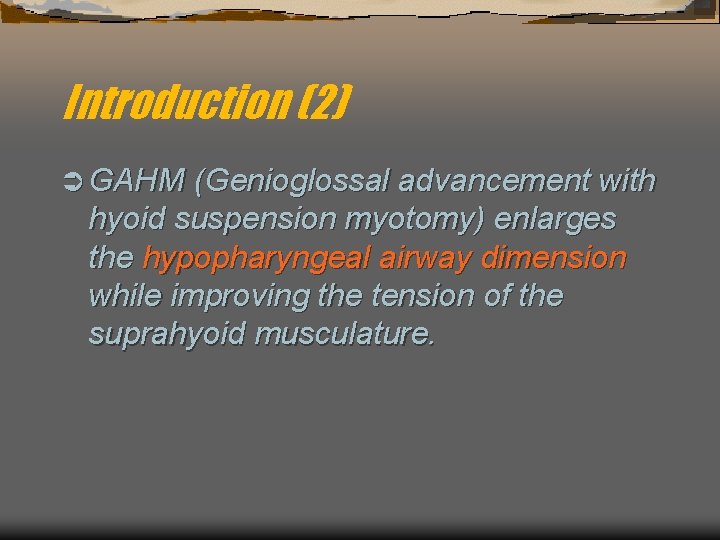
Introduction (2) Ü GAHM (Genioglossal advancement with hyoid suspension myotomy) enlarges the hypopharyngeal airway dimension while improving the tension of the suprahyoid musculature.
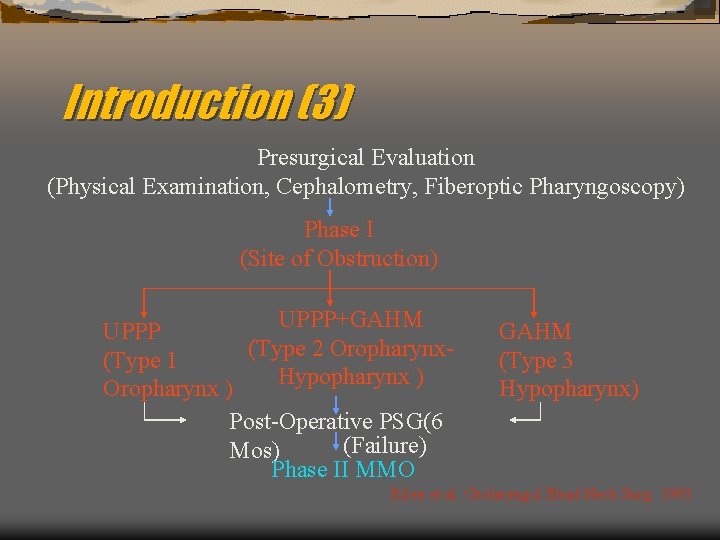
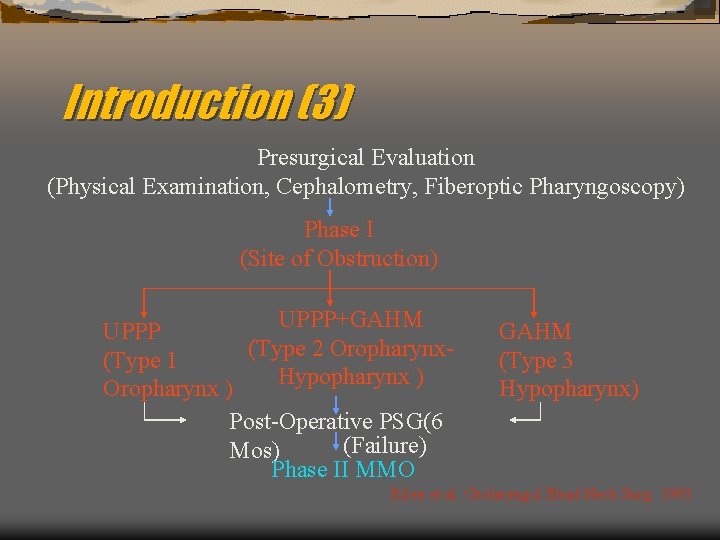
Introduction (3) Presurgical Evaluation (Physical Examination, Cephalometry, Fiberoptic Pharyngoscopy) Phase I (Site of Obstruction) UPPP+GAHM UPPP (Type 2 Oropharynx(Type 1 Hypopharynx ) Oropharynx ) Post-Operative PSG(6 (Failure) Mos) Phase II MMO GAHM (Type 3 Hypopharynx) Riley et al. Otolaryngol Head Neck Surg. 1993
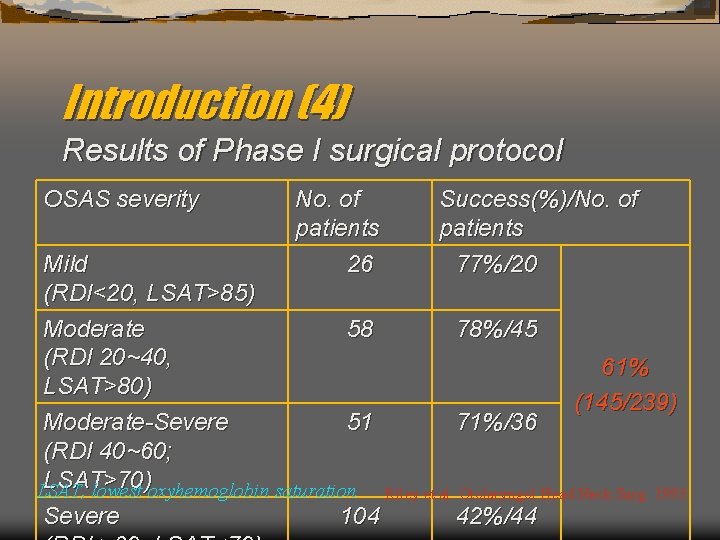
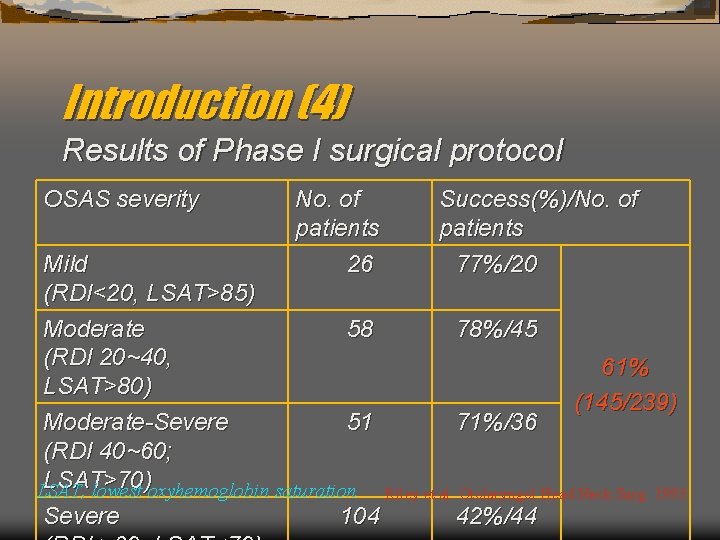
Introduction (4) Results of Phase I surgical protocol OSAS severity No. of patients 26 Success(%)/No. of patients 77%/20 Mild (RDI<20, LSAT>85) Moderate 58 78%/45 (RDI 20~40, 61% LSAT>80) (145/239) Moderate-Severe 51 71%/36 (RDI 40~60; LSAT>70) LSAT, lowest oxyhemoglobin saturation Riley et al. Otolaryngol Head Neck Surg. 1993 Severe 104 42%/44
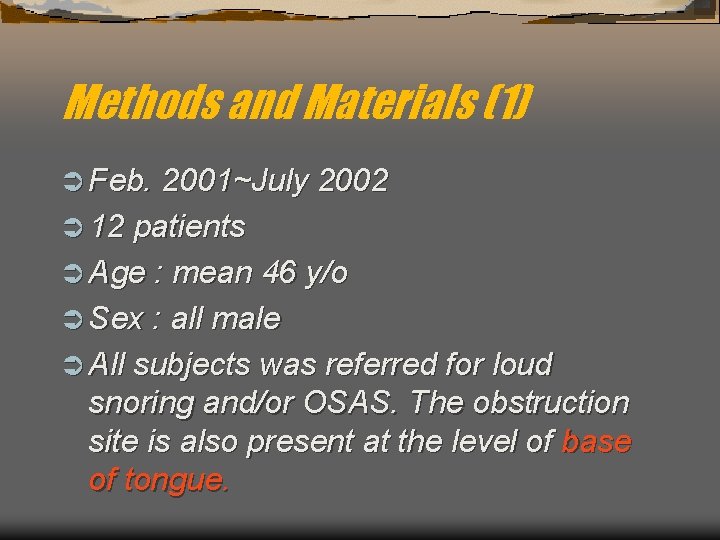
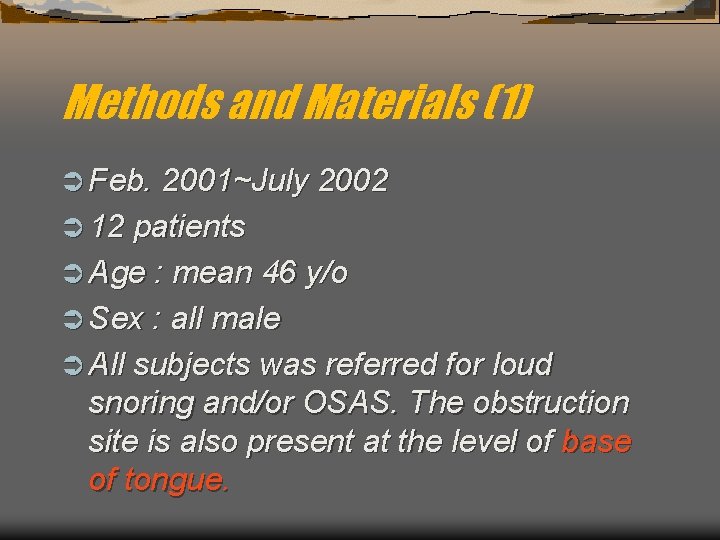
Methods and Materials (1) Ü Feb. 2001~July 2002 Ü 12 patients Ü Age : mean 46 y/o Ü Sex : all male Ü All subjects was referred for loud snoring and/or OSAS. The obstruction site is also present at the level of base of tongue.
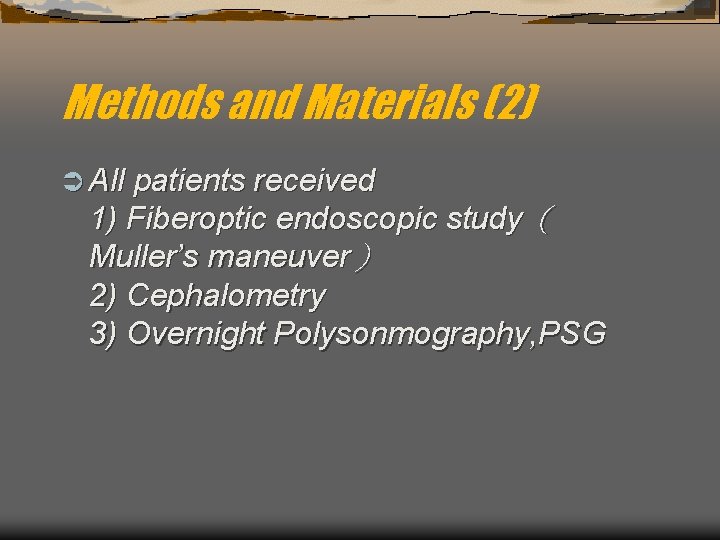
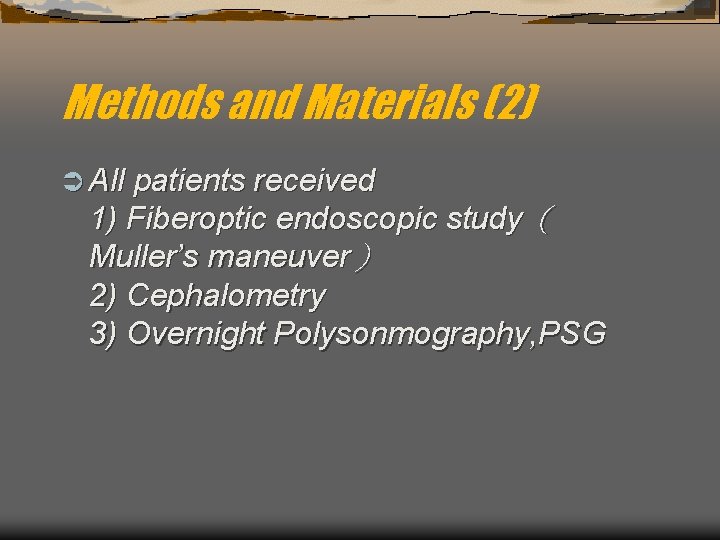
Methods and Materials (2) Ü All patients received 1) Fiberoptic endoscopic study( Muller’s maneuver) 2) Cephalometry 3) Overnight Polysonmography, PSG

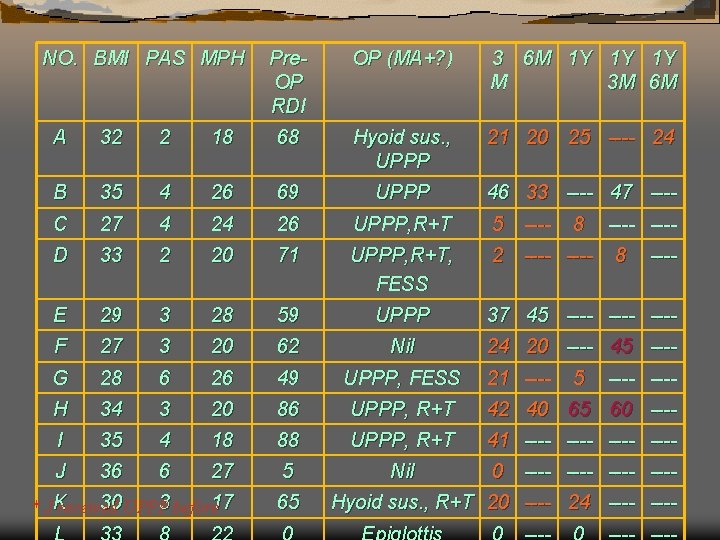
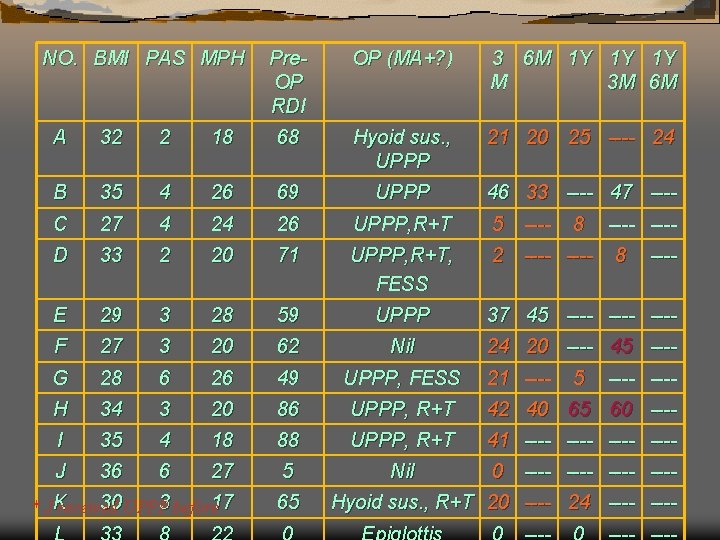
NO. BMI PAS MPH Pre. OP RDI OP (Genioglossal Advancement + ? ) A 32 2 18 68 Hyoid suspension, UPPP B 35 4 26 69 UPPP C 27 4 24 26 UPPP, R+T D 33 2 20 71 UPPP, R+T, FESS E 29 3 28 59 UPPP F 27 3 20 62 Nil G 28 6 26 49 UPPP, FESS H 34 3 20 86 UPPP, R+T I 35 4 18 88 UPPP, R+T J 36 6 27 5 Nil K 30 3 17 65 Hyoid suspension, R+T 22 0 Epiglottis reduction * J received UPPP L 33 before 8
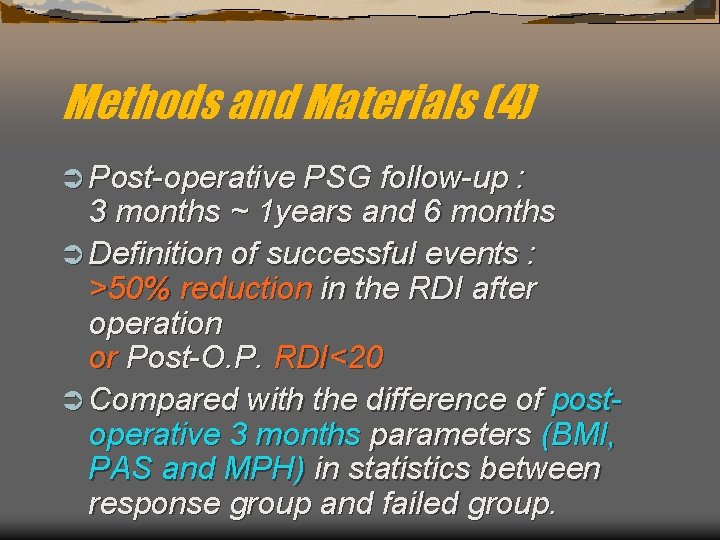
Methods and Materials (4) Ü Post-operative PSG follow-up : 3 months ~ 1 years and 6 months Ü Definition of successful events : >50% reduction in the RDI after operation or Post-O. P. RDI<20 Ü Compared with the difference of postoperative 3 months parameters (BMI, PAS and MPH) in statistics between response group and failed group.
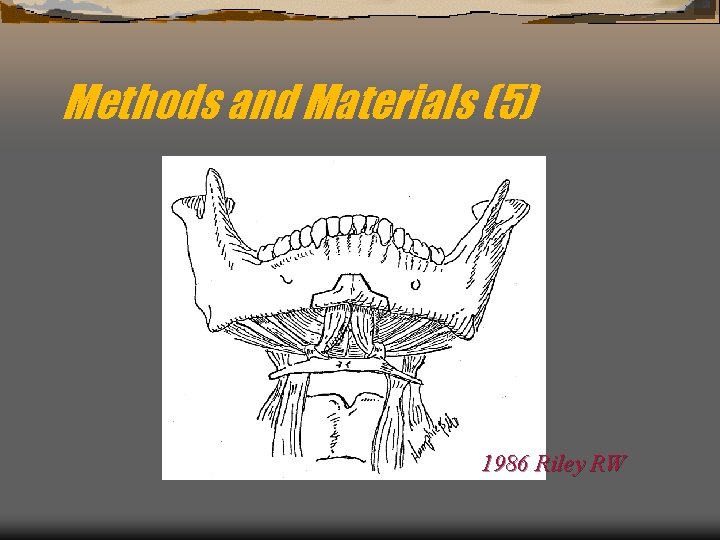
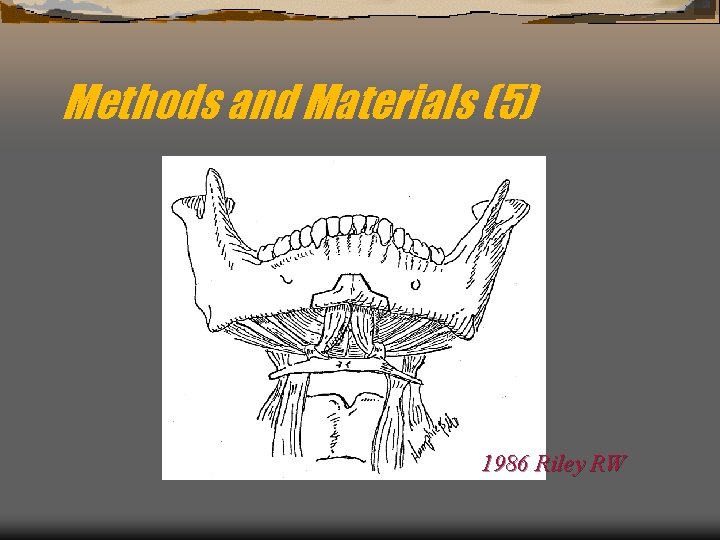
Methods and Materials (5) 1986 Riley RW
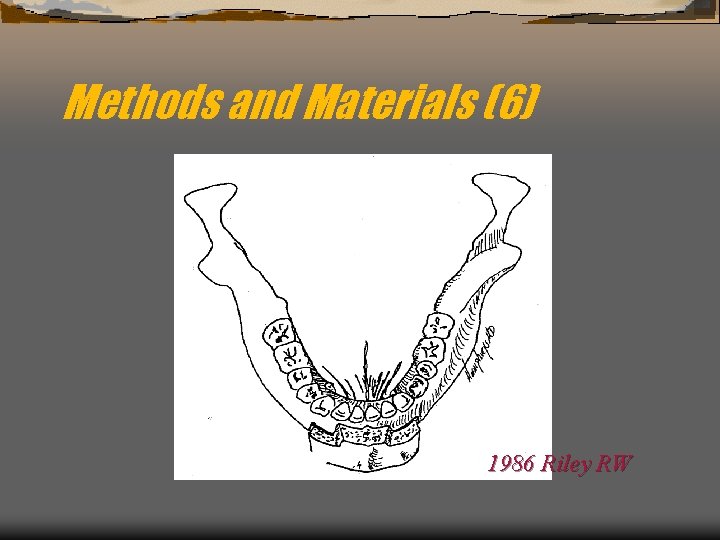
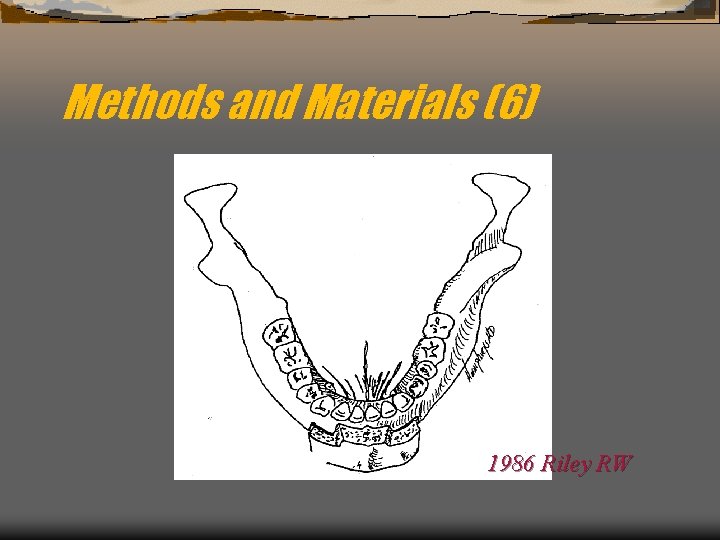
Methods and Materials (6) 1986 Riley RW
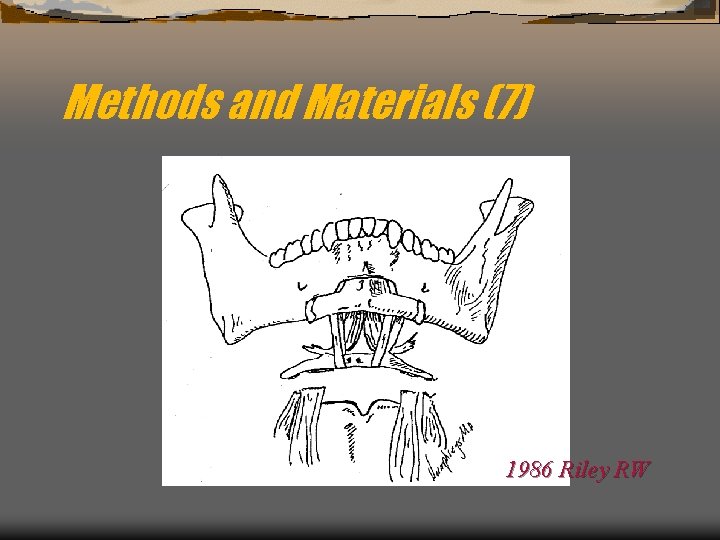
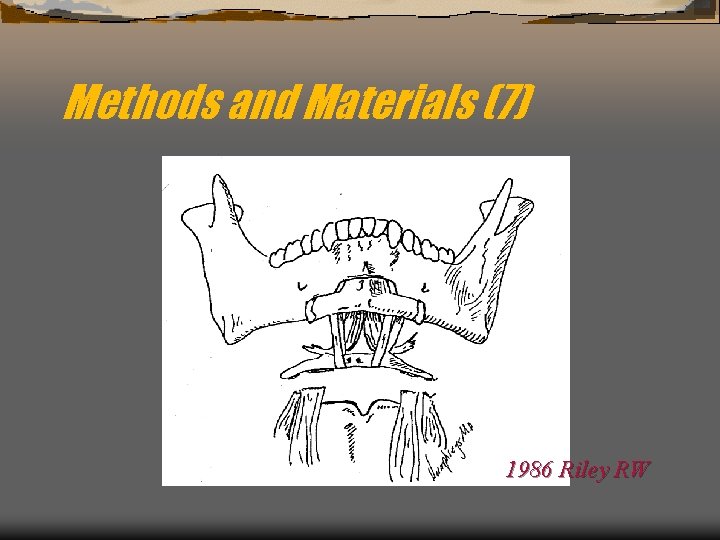
Methods and Materials (7) 1986 Riley RW
NO. BMI PAS MPH Pre. OP RDI OP (MA+? ) 3 6 M 1 Y 1 Y 1 Y M 3 M 6 M A 32 2 18 68 Hyoid sus. , UPPP 21 20 25 ---- 24 B 35 4 26 69 UPPP 46 33 ---- 47 ---- C 27 4 24 26 UPPP, R+T 5 ---- D 33 2 20 71 UPPP, R+T, FESS 2 ---- E 29 3 28 59 UPPP 37 45 ---- F 27 3 20 62 Nil 24 20 ---- 45 ---- G 28 6 26 49 UPPP, FESS H 34 3 20 86 UPPP, R+T 42 40 65 60 ---- I 35 4 18 88 UPPP, R+T 41 ---- J 36 6 27 5 Nil 0 ---- 30 UPPP 3 before 17 * JK received 65 21 ---- 8 5 ---- ---8 ---- Hyoid sus. , R+T 20 ---- 24 ----
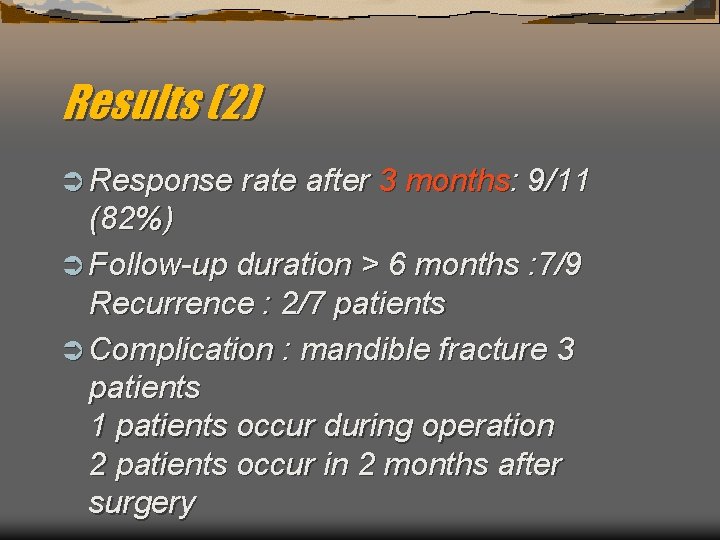
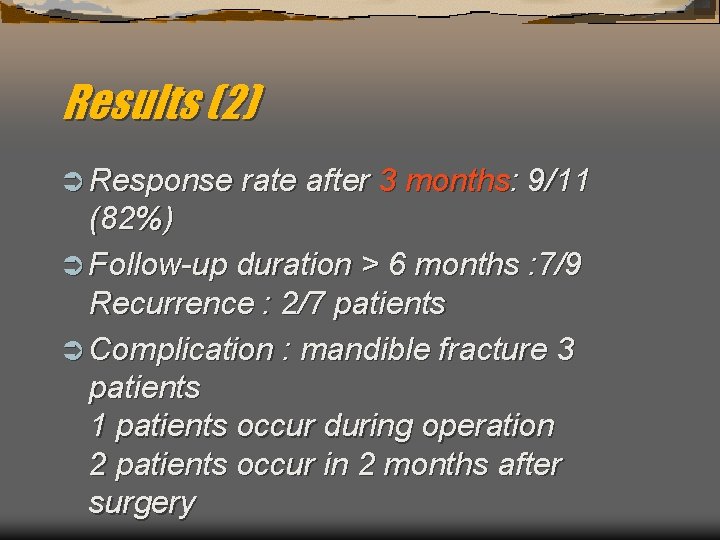
Results (2) Ü Response rate after 3 months: 9/11 (82%) Ü Follow-up duration > 6 months : 7/9 Recurrence : 2/7 patients Ü Complication : mandible fracture 3 patients 1 patients occur during operation 2 patients occur in 2 months after surgery
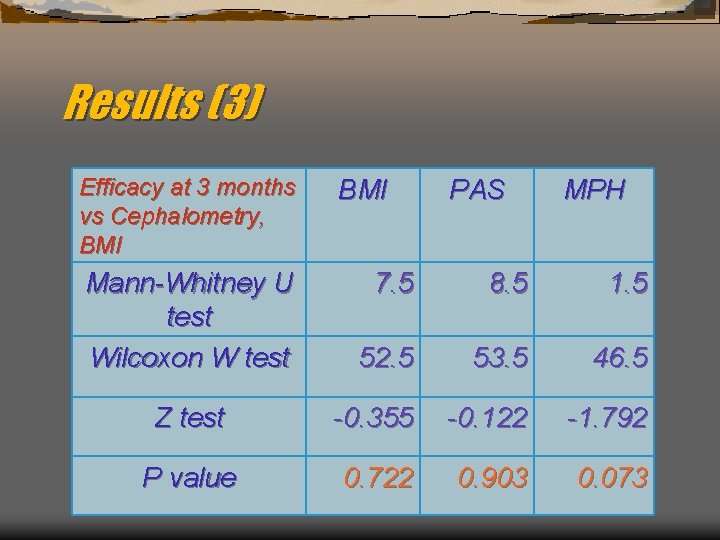
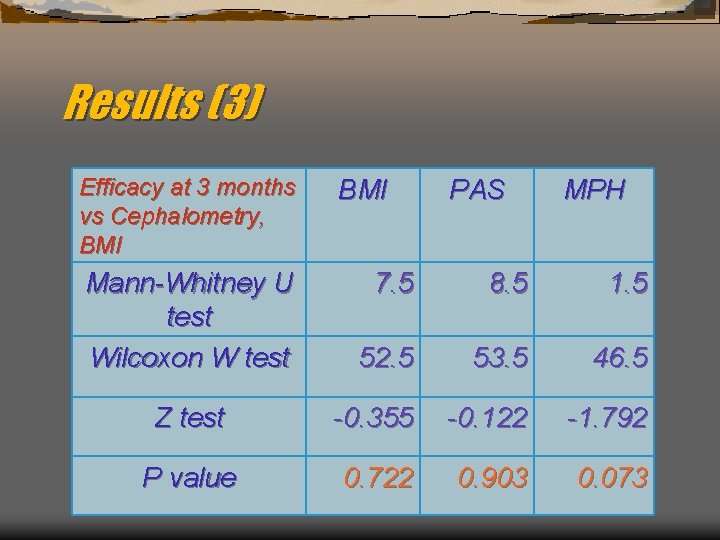
Results (3) Efficacy at 3 months vs Cephalometry, BMI Mann-Whitney U test Wilcoxon W test BMI PAS MPH 7. 5 8. 5 1. 5 52. 5 53. 5 46. 5 Z test -0. 355 -0. 122 -1. 792 P value 0. 722 0. 903 0. 073
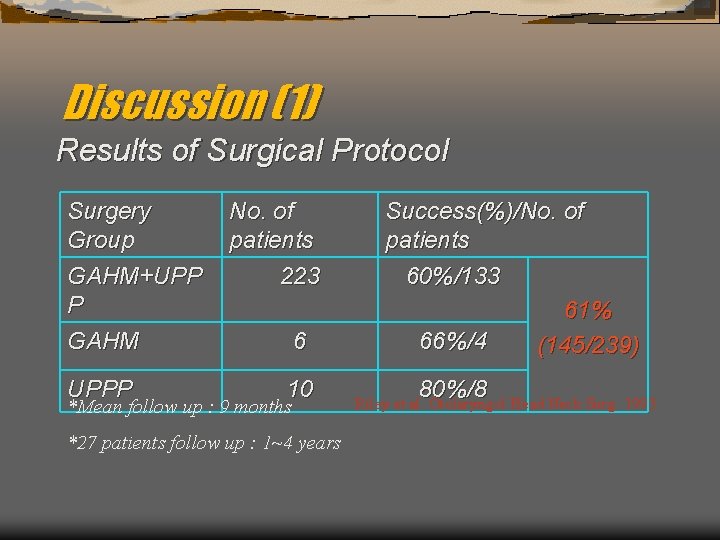
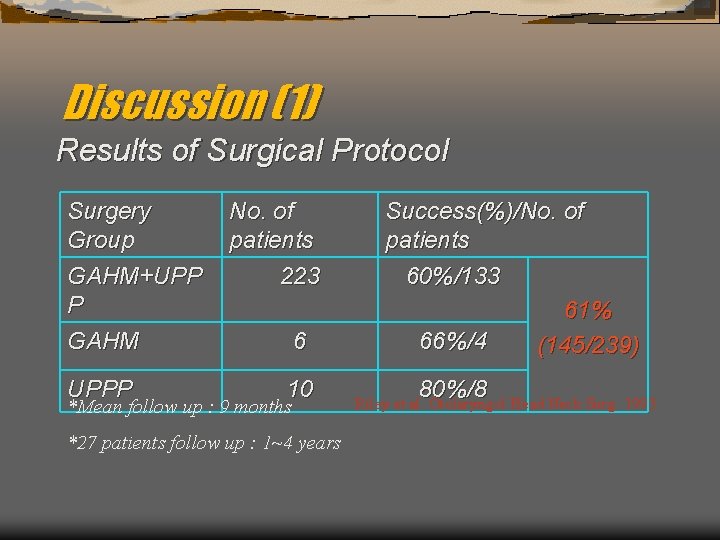
Discussion (1) Results of Surgical Protocol Surgery Group GAHM+UPP P GAHM UPPP No. of patients 223 6 10 *Mean follow up : 9 months *27 patients follow up : 1~4 years Success(%)/No. of patients 60%/133 61% 66%/4 (145/239) 80%/8 Riley et al. Otolaryngol Head Neck Surg. 1993
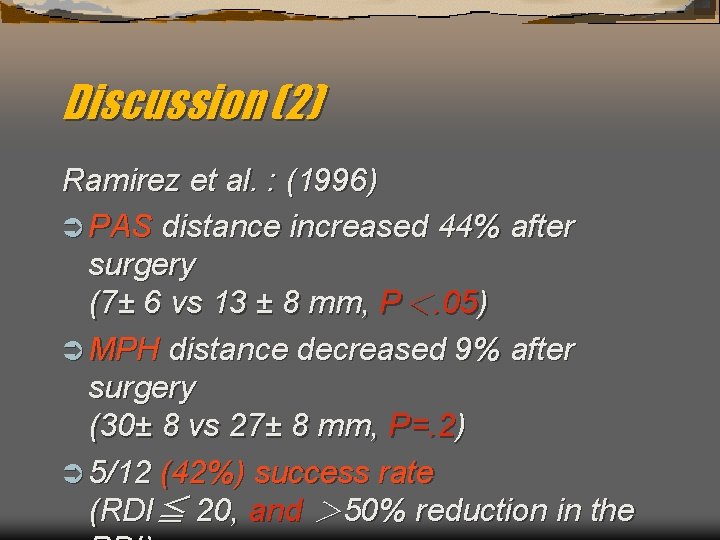
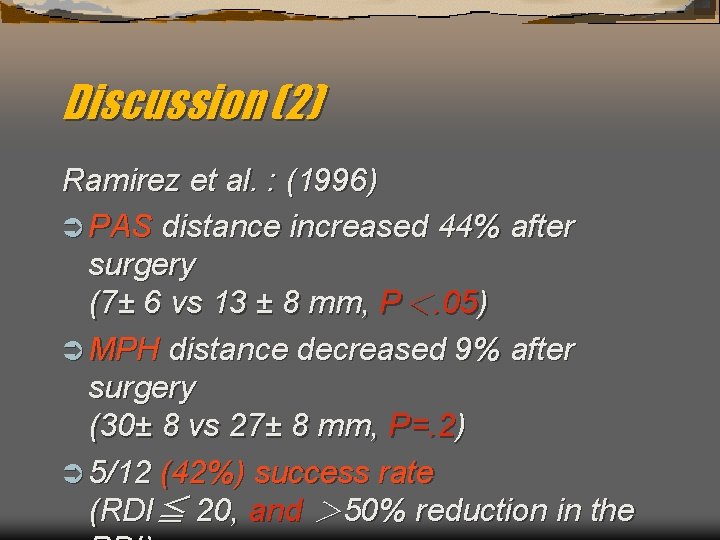
Discussion (2) Ramirez et al. : (1996) Ü PAS distance increased 44% after surgery (7± 6 vs 13 ± 8 mm, P<. 05) Ü MPH distance decreased 9% after surgery (30± 8 vs 27± 8 mm, P=. 2) Ü 5/12 (42%) success rate (RDI≦ 20, and > 50% reduction in the
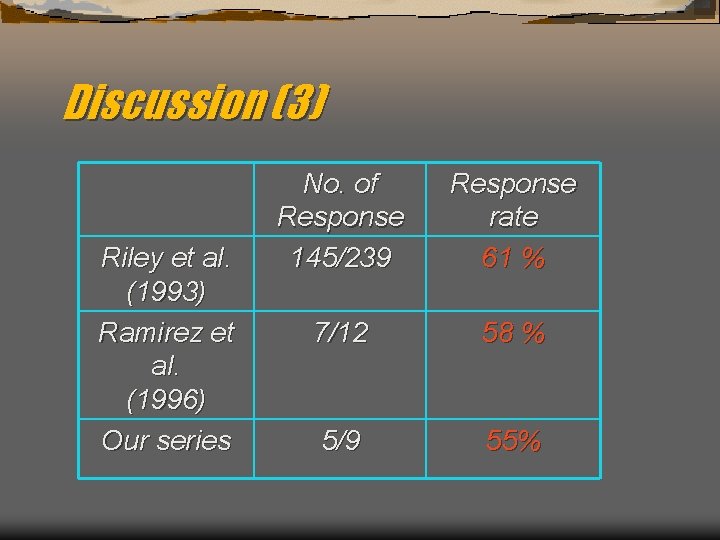
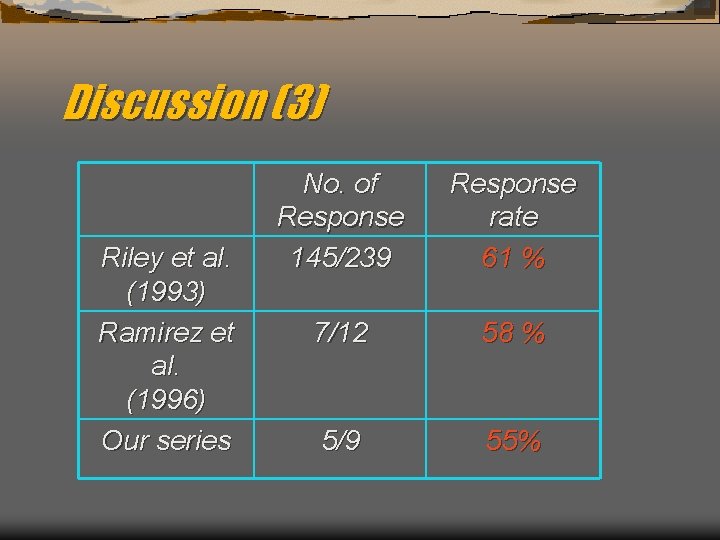
Discussion (3) Riley et al. (1993) Ramirez et al. (1996) Our series No. of Response 145/239 Response rate 61 % 7/12 58 % 5/9 55%
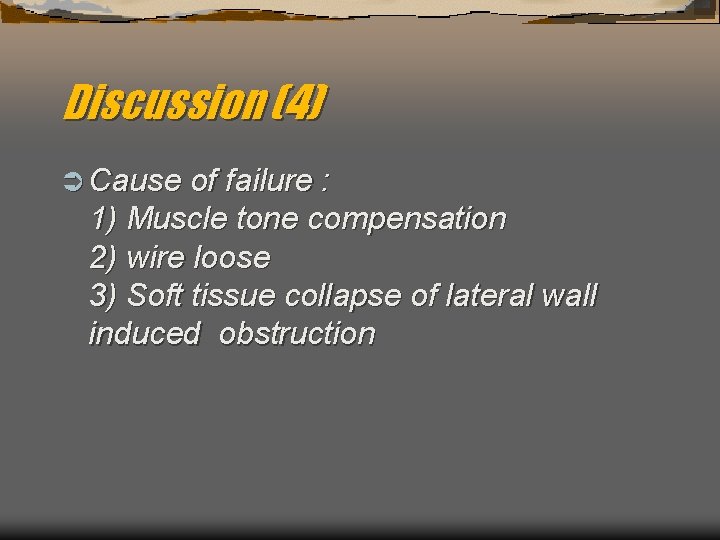
Discussion (4) Ü Cause of failure : 1) Muscle tone compensation 2) wire loose 3) Soft tissue collapse of lateral wall induced obstruction
Discussion (5) Ü It is difficult to evaluate the efficacy of the surgery in the patients with multiple level obstruction who had multiple level surgery in the present study.
Discussion (6) Ü Higher response rate (61~85%) is reported in other series. It may be because of the difference of the race or the distance of advancement. Ü Cause of failure noted in 3 months after surgery? The poor predictive value of lateral cephalometry soft-tissue measurements may reflect the finding that pharyngeal
Conclusion Ü The genioglossal advancement with UPPP can be used in patients who have obstruction at the palate and base-oftongue areas. Ü Better evaluation for better prognosis.
 Control network
Control network Gcf 54 and 27
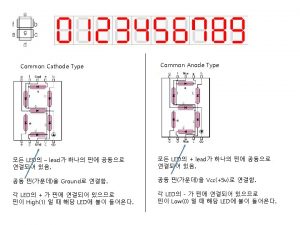
Gcf 54 and 27 Common anode and common cathode
Common anode and common cathode Factor tree for 56
Factor tree for 56 Factors of 54
Factors of 54 Factors of 60 and 48
Factors of 60 and 48 Multiples of 9 and 21
Multiples of 9 and 21 Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Chúa yêu trần thế
Chúa yêu trần thế Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới