CESAREAN Most common major surgical procedure in the















- Slides: 42
CESAREAN

Most common major surgical procedure in the UNITED STATES: 1/3 of births 70% Of cesarean deliveries in the UNITED STATES are primary cesareans; three common indication are: 1. Failure to progress during labor (35%) 2. Non_reasurring fetal status (24%) 3. Fetal malpresentation(19%)
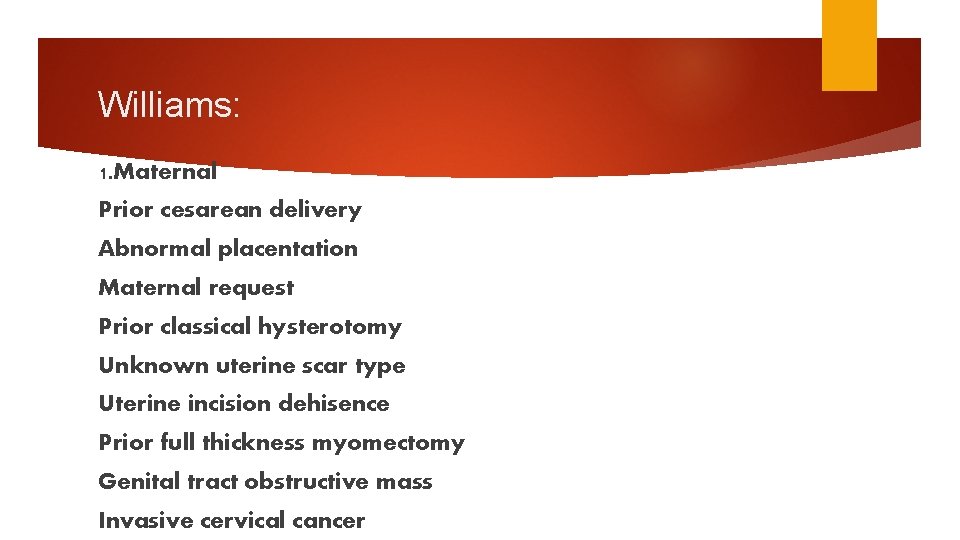
Williams: 1. Maternal Prior cesarean delivery Abnormal placentation Maternal request Prior classical hysterotomy Unknown uterine scar type Uterine incision dehisence Prior full thickness myomectomy Genital tract obstructive mass Invasive cervical cancer
Prmannet cercelage Prior pelvc reconstructive sugery Prior significan perineal trauma PELVIC DEFORMITY Hsv OR HIV infection CARDIAC OR PULMONARY DISease Cerebral aneurysm or arteriovenous mlformation perimortem cesarean delivery
Maternal Fetal Cephalopelvic Failed disproportion operative vaginal delivery Placenta previa or placental abruption
FETAL Non reasusuring fetal status Malpresentation Macrosomia Congenital anomaly Abnormal umbilical cord duppler study Thrombocytopenia Prior neonatal birth trauma
Preoperative Planned term cesarean delivery at 39 or 40 w of gestation Sedative may be given at bed time the night before surgery Solid food intake stopped at least 6 – 8 hours before surgery (uncomplicated patients moderate amount of clear liquid up to 2 hours before surgery) Admit the day of surgery Antacid is given shortly before the analgesia (Bicitra, 30 ml, orally in a single dose) Left lateral tilt Five minute tracing of fetus. Minimum fetal heart rate sound. Electrosurgical pad on the lateral thigh. Intra operative normothermia lowes wound infection rate
Preoperative Anesthesia consultation Baseline Hb (one month), blood type, antibody screen indirect coombs AB Prophylaxis: without AB 5 -20 Fold greater risk of infection compared with vaginal birth/Narrow sperctrum AB within 60 min before incision such as cefazolin or ampicillin Women<120 kg=CEFAZOLIN 2 gr (Williams 1 gr) WOMEN>=120 kg= CEFAZOLIN 3 gr Half life CEFAZOLIN>AMPICILLIN/Extra doses(excessive blood loss, duration of sugery >two half lives of thec drug CEFAZOLIN+AZITHRIMYCIN 500 mg IV=IN labor or ROM FOR AT LEAST 4 H ALLERGY: CLINDAMYCIN 900 mg+Gentamycin 5 mg/kg IV Thrombo phylaxy
Fetal presentation and placental location Bladder catheterization Hair removal Skin preparation Vaginal preparation
Skin incision Choice of incision — transverse skin incision: a better cosmetic appearance and possibly less postoperative pain and hernia formation. we rarely perform a vertical midline incision, we often select this approach when: The incision-to-delivery time is critical A transverse incision may not provide adequate exposure The patient has a bleeding diathesis and thus is at increased risk of subcutaneous or subfascial hematoma formation Patients with high infection risk Neurovascular structures (ilioinguinal and iliohypogastric nerves and superficial and inferior epigastric vessels) Obese patients
Transverse incision Pfannenstiel: common JOEL –Cohen Maylard incision (rectus andominies transected) (inferior epigastric arterie)
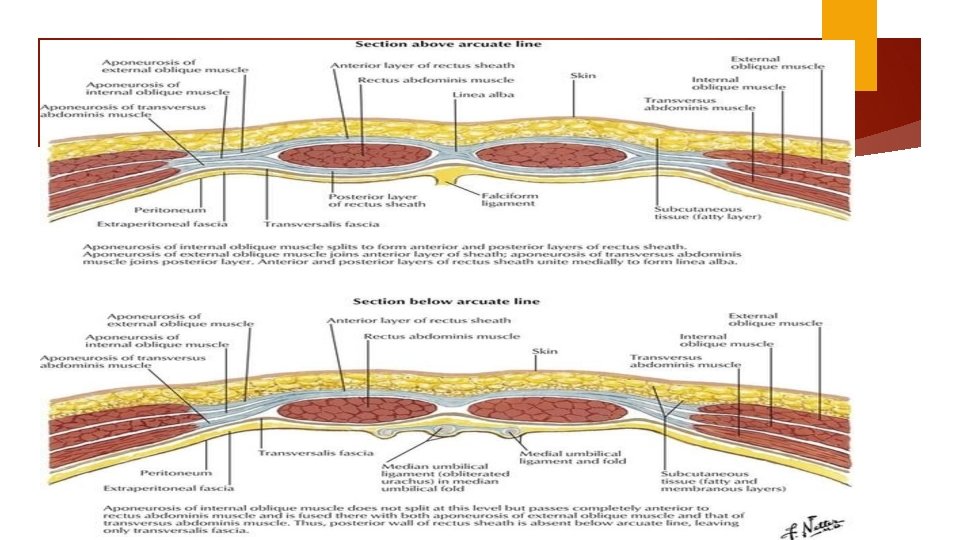
Pfannenstiel Level of pubic hair line (3 cm about superior border of symphysis pubis) 12 -15 cm Sharp dissection through the subcutaneous to the fascia (superficial epigastric vessel) Anterior abdominal fascial = aponeurosis external oblique muscle fused layer transverse abdominies + internal oblique Fascial separation cephalad 8 cm
vertical midline incision 2 to 3 cm above the superior margin of the symphysis 12 to 15 cm Sharp dissection through the subcutaneous layer Extended first superiorly then inferiorly Other stages are similar to Pfannenstiel
Subcutaneous tissue layer Fascial layer Rectus muscle layer Opening the peritoneum


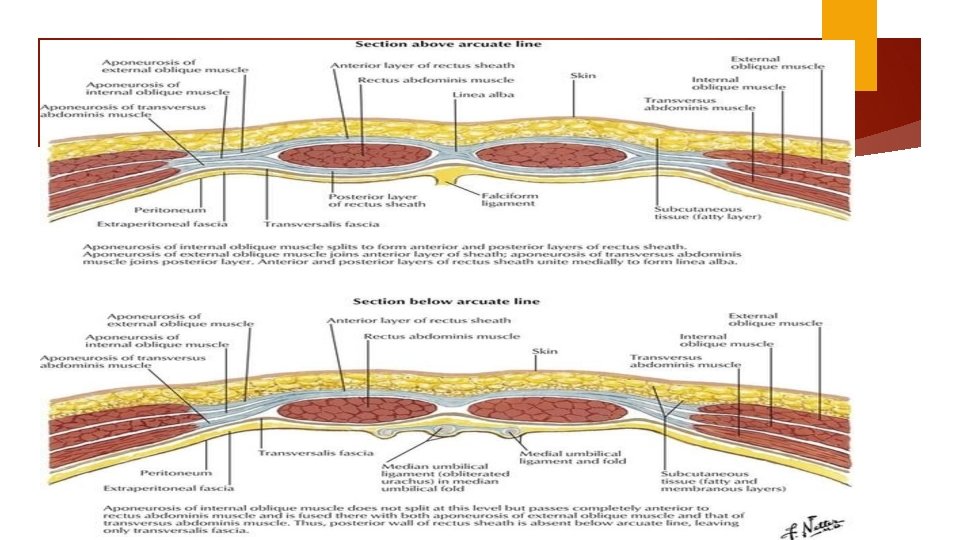

Hysterotomy Transverse incision Monro Kerr or Kerr incision Low uterine segment vertical (Kronig, De. Lee, or Cornell) classical incisions Fundal or posterior incision (placental accrete) The generally accepted indications for considering a vertical uterine incision are: ●Poorly developed lower uterine segment when more than normal intrauterine manipulation is anticipated (eg, extremely preterm breech presentation, back down transverse lie). ●Lower uterine segment pathology that precludes a transverse incision (eg, large leiomyoma, anterior placenta previa or accreta). ●Densely adherent bladder. ●Postmortem delivery. ●Delivery of a very large fetus (eg, anomalous, extreme macrosomia) when there is high risk of extension of a transverse incision into uterine vessels or a T or J extension may be required to extract the fetus.

Kerr Easier Less to repair incision-site bleeding Promote less bowel or omentum adherence to myometrial incision Less likely to rupture during subsequent pregnancy

Palpate Moist the fundus to identify uterine rotation sponge to pack protruding bowel Peritoneal Bladder edge is elevated and incised laterally flap shorter skin incision to delivery time
Uterine incision Digital palpation to find the physiological border between firmer upper segment and more flexible lower segment. Advanced 1 cervical dilation hysterotomy is higher to 2 cm Comparing blunt and sharp expansion: blunt associated with fewer unintended incision extension, shorter operative time and less blood loss.
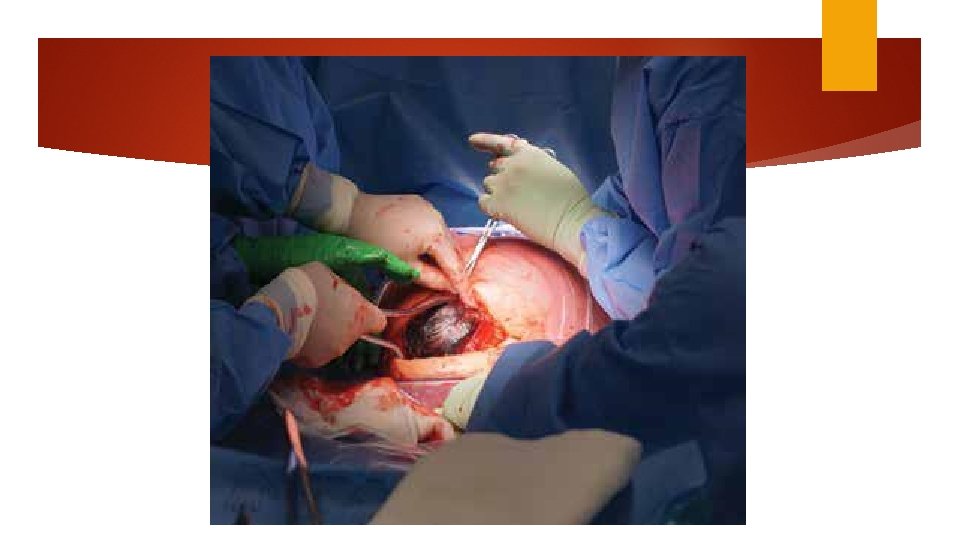
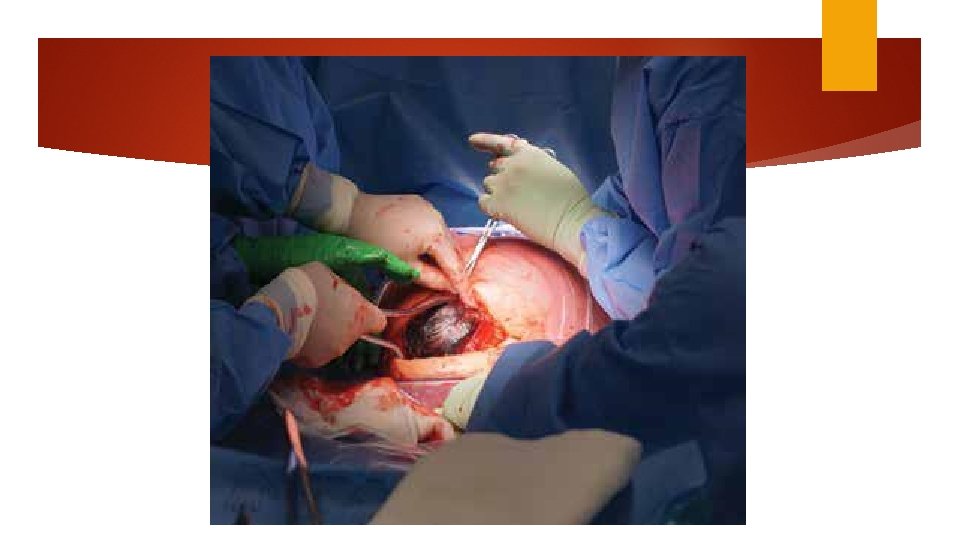
Delivery of the fetus Push (dislodge) Pull Fetal pillow Round head (difficult) Encircled umbilical cord

20 units of oxytocin per liter (10 ml/min) Delivery of the placenta
Uterine repair Uterus is lifted One or two layers of continues 0 no. 1 absorbable suture: chromic catgut / Vicryl Single layer is faster Individual bleeding site: figure of 8 or mattress
Scaring can be reduced by handling tissues delicately achieving hemostasis and minimizing tissue ischemia infection foreign body reaction No benefit to peritoneal closure No benefit of adhesion barrier
Abdominal closure Irrigation Muscle (greater intra operative nausea) approximated by 0 or no. 1 Chromic figure of 8 gut sucure. Overlying rectus fascia: continues nonlocking with delayed absorbable suture Subcutaneous Skin tissues if less than 2 cm thick need not be closed with 4 -0 delayed bsorbable
Joel-Cohen and Misgav ladach techniques Differ from Kerr by their initial incision and greater use of blunt dissection Joel-Cohen Technique: Straight 10 cm transverse skin incision 3 cm below the level of anterior superior iliac spine. Subcutaneous tissue is opened sharply. Misgav ladach technique defers in that peritoneum is interred bluntly Shorter operative time, less blood loss and post operative pain Difficult in women with adhesion or fibrosis








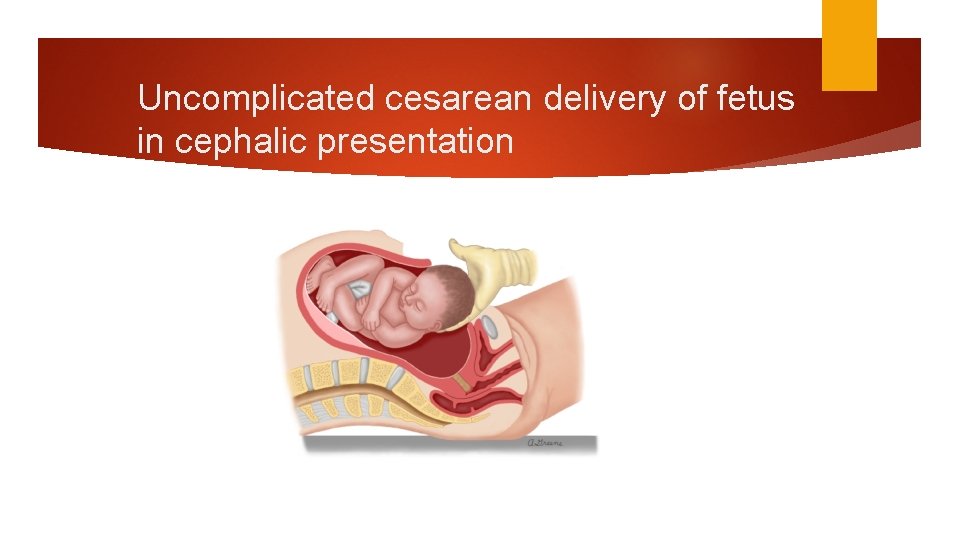
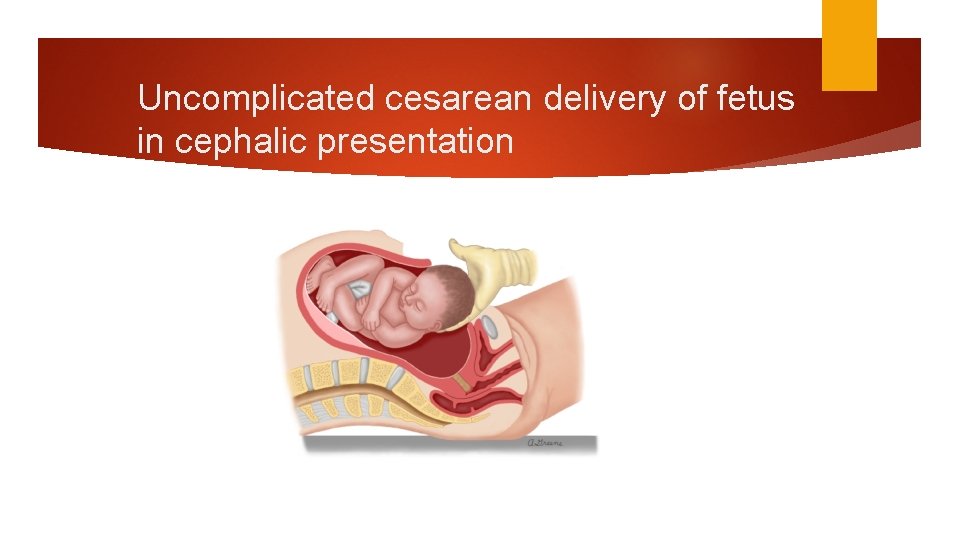
Uncomplicated cesarean delivery of fetus in cephalic presentation
UTERINE CLOSURE Exteriorizing the uterus
 Nursing diagnosis for lscs slideshare
Nursing diagnosis for lscs slideshare Baseball stitch classical cesarean
Baseball stitch classical cesarean Sindications
Sindications Cesarean hysterectomy steps
Cesarean hysterectomy steps Complications during c section
Complications during c section Cesarean julius caesar
Cesarean julius caesar Complications after cesarean section
Complications after cesarean section C section incision name
C section incision name Kode icd 10 fraktur clavicula
Kode icd 10 fraktur clavicula The healthcare common procedure coding system
The healthcare common procedure coding system Common factors of 48 and 60
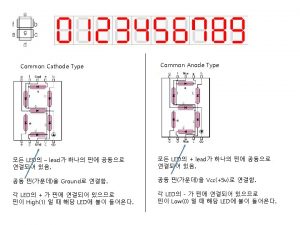
Common factors of 48 and 60 Common anode and common cathode
Common anode and common cathode Gcf of 48 56 and 72
Gcf of 48 56 and 72 What are the factors for 54
What are the factors for 54 Find the lcm of 16 24 36 and 54
Find the lcm of 16 24 36 and 54 Multiples of 9 and 21
Multiples of 9 and 21 Anterior posterior palatal strap indications
Anterior posterior palatal strap indications Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Glasgow thang điểm
Glasgow thang điểm Hát lên người ơi
Hát lên người ơi Môn thể thao bắt đầu bằng từ chạy
Môn thể thao bắt đầu bằng từ chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Phép trừ bù
Phép trừ bù Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V cc cc
V cc cc Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Tia chieu sa te
Tia chieu sa te