Surgical Procedures Devashish J Anjaria Surgical Fundamentals August





















- Slides: 62
Surgical Procedures Devashish J. Anjaria Surgical Fundamentals August 11, 2006

Case Presentation • 25 year old male presents s/p single stab wound to the left chest. He clearly smells of alcohol and is lethargic – responding only to painful stimuli. Field vitals are P 150, BP 80/palp, Resp 35. • What’s the plan? ?

ABC’s
Airway • Secure airway = cuffed tube in the trachea – Endotracheal • Orotracheal • Nasotracheal – Surgical airway • Cricothyroidotomy • Tracheostomy
Indications • Inability to oxygenate – Pa. O 2/Fi. O 2 < 200 • Inability to ventilate – Respiratory rate > 30 or < 5 – PCO 2 > 60 • Inability to protect airway – GCS ≤ 8
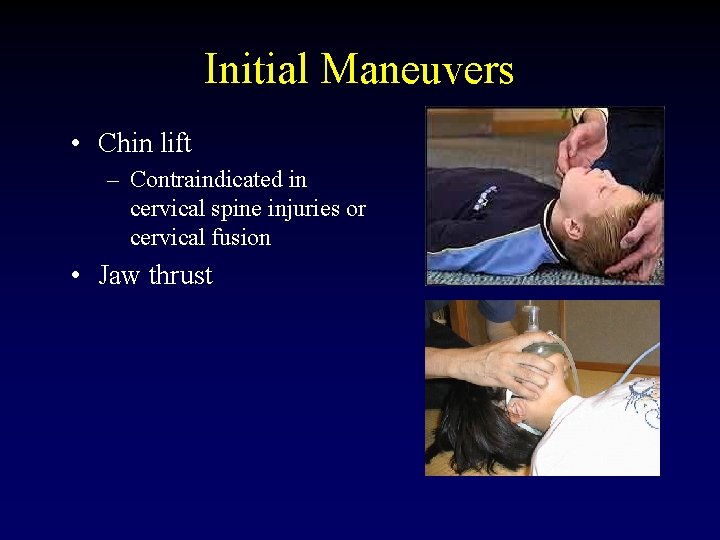
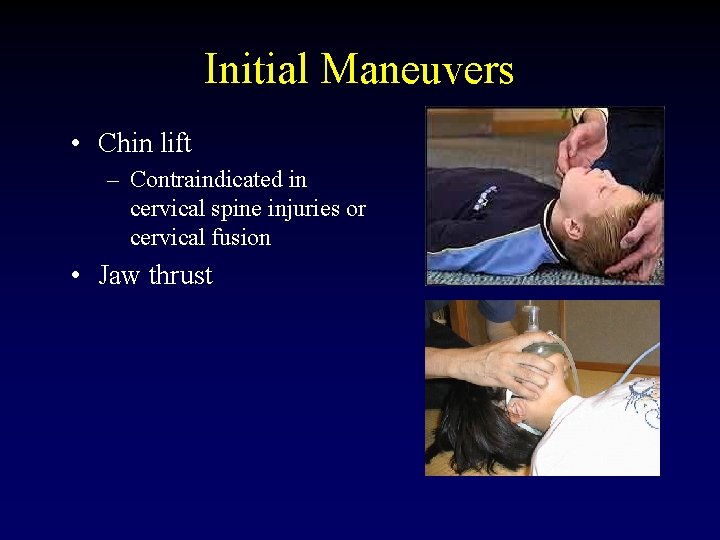
Initial Maneuvers • Chin lift – Contraindicated in cervical spine injuries or cervical fusion • Jaw thrust
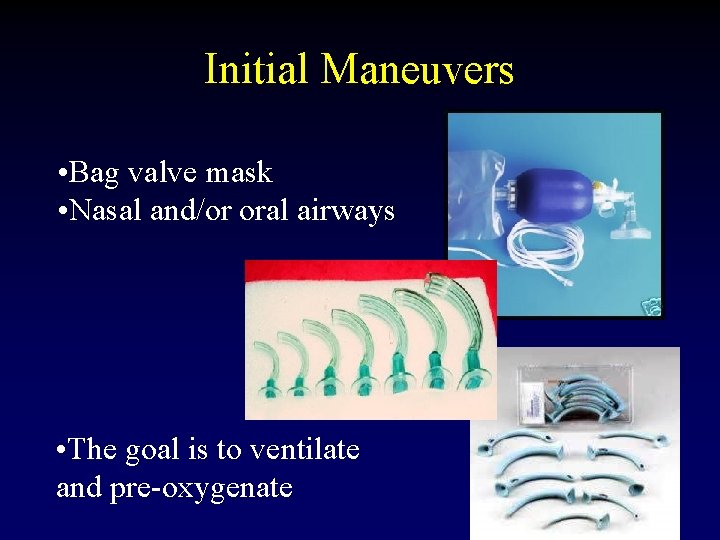
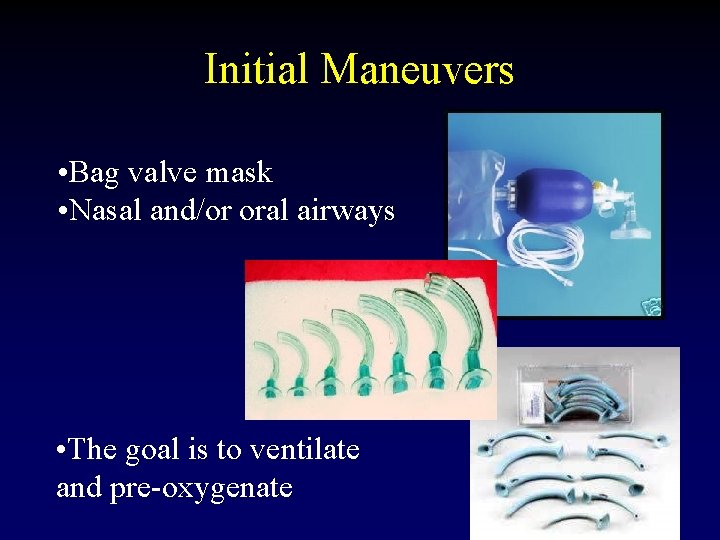
Initial Maneuvers • Bag valve mask • Nasal and/or oral airways • The goal is to ventilate and pre-oxygenate
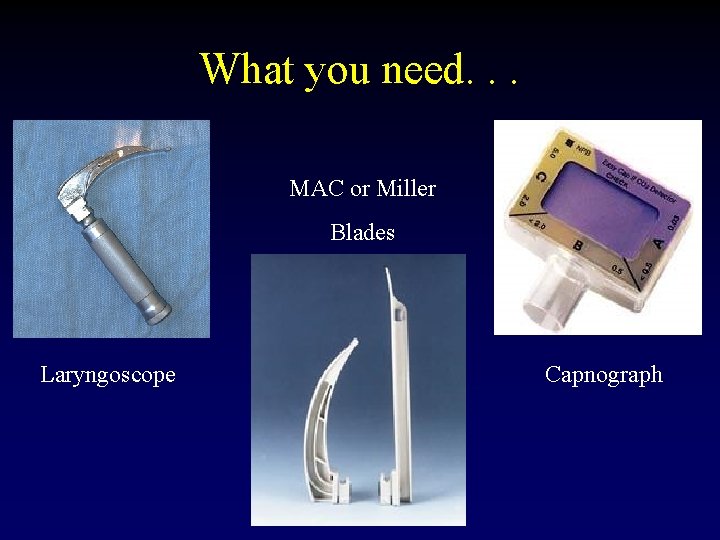
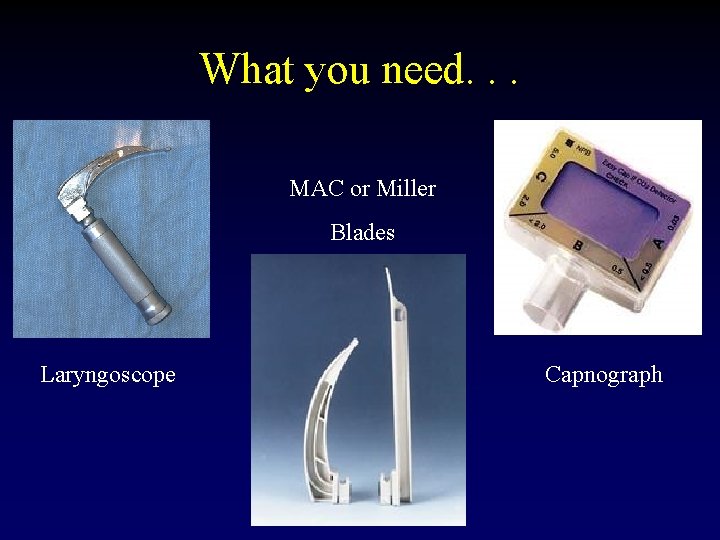
What you need. . . MAC or Miller Blades Laryngoscope Capnograph
What you need. . . • • • Working suction 10 cc syringe (to inflate the balloon) Medications – to premedicate, if applicable Tape or twill Stylet Pulse ox monitoring
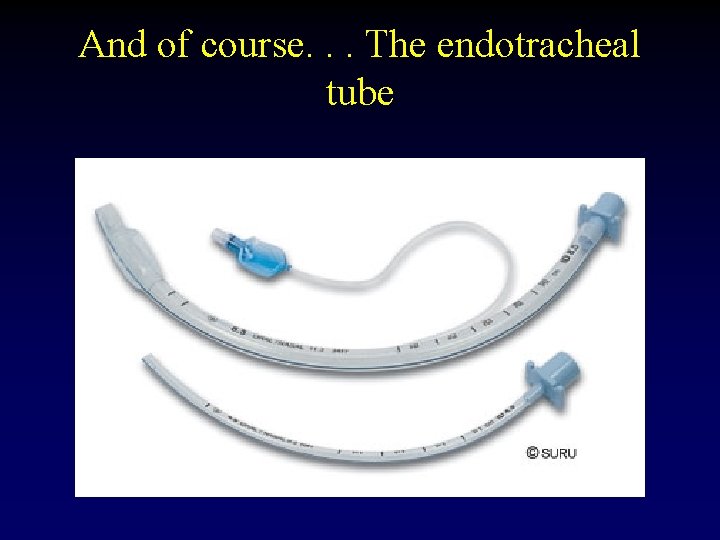
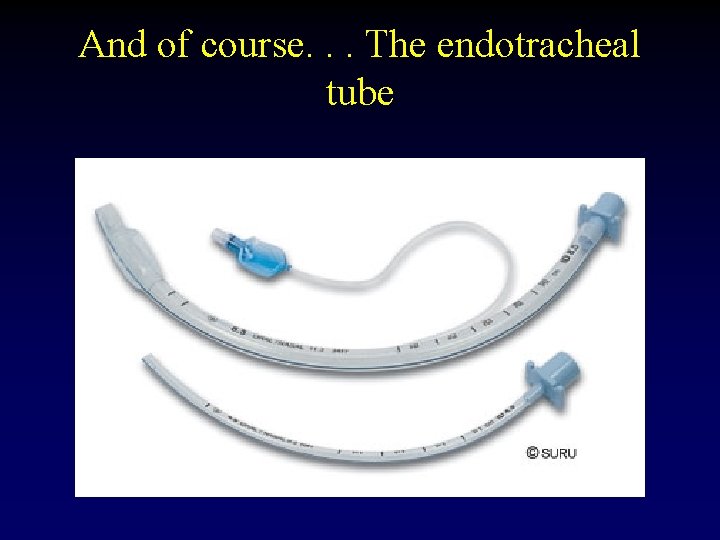
And of course. . . The endotracheal tube
Nasotracheal Intubation • Prerequisites – Awake spontaneously breathing patient • Contraindications – Facial fractures – Basilar skull fracture – Apnea – Coagulopathy – Pregnancy

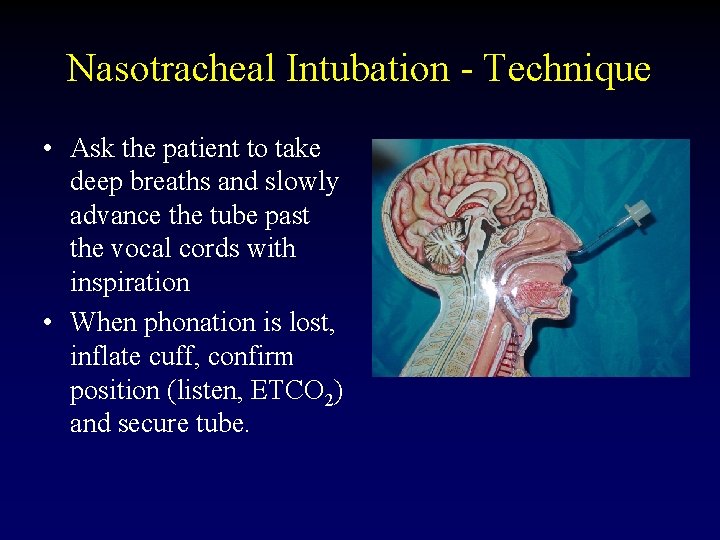
Nasotracheal Intubation - Technique • Pick an endotracheal tube 1 size smaller than the largest nasal airway which fits. • Thoroughly lubricate the endotracheal tube • Anesthetize the nares (if possible) with lidocaine jelly or cetacaine spray • Gently advance the tube until fogging is encountered and/or air moves through tube.
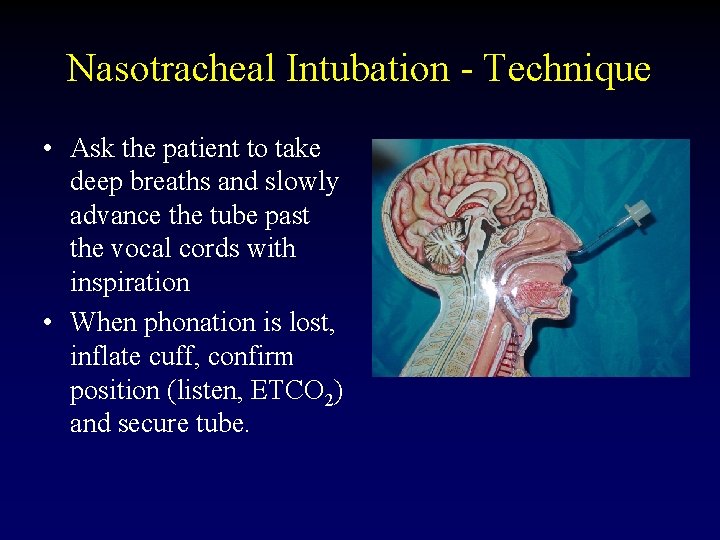
Nasotracheal Intubation - Technique • Ask the patient to take deep breaths and slowly advance the tube past the vocal cords with inspiration • When phonation is lost, inflate cuff, confirm position (listen, ETCO 2) and secure tube.
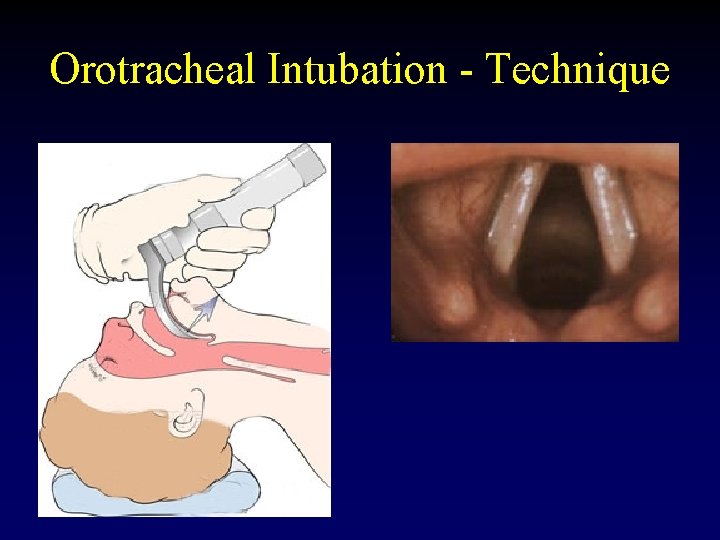
Orotracheal Intubation - Technique • • Stabilize cervical spine if necessary Have somebody apply cricoid pressure Open mouth and separate teeth with right hand Hold laryngoscope in left hand insert in right side of mouth, pushing the tongue to the left. • Vertical traction is applied to lift the epiglottis and visualize the vocal cords
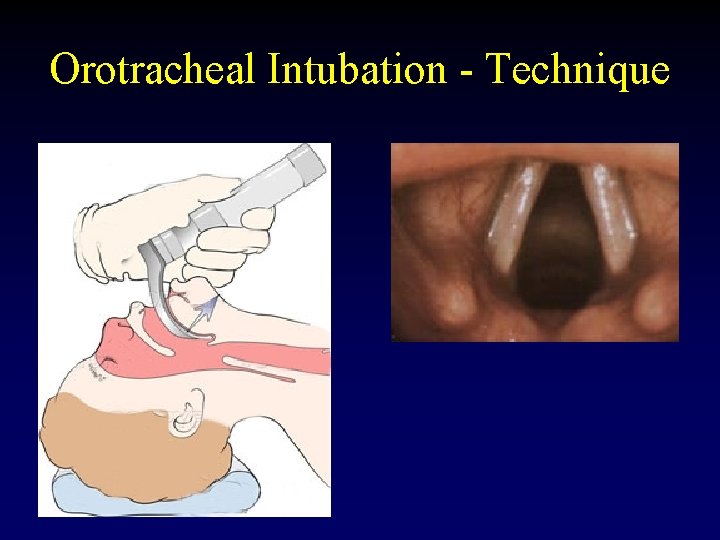
Orotracheal Intubation - Technique
Orotracheal Intubation - Technique • The endotracheal tube is inserted through the cords and the cuff is inflated. • Tube position is confirmed – Auscultation/Chest excursion – Capnography – CXR • Tube is secured

Sedatives and Neuromuscular Blockers • Induction agents – Thiopental 4 – 6 mg/kg – Etomidate 0. 3 mg/kg – Ketamine 1 – 3 mg/kg • Neuromuscular blocking agents – Succinylcholine 1. 0 mg/kg – Vecuronium 0. 3 mg/kg for intubating • Sedatives – Midazolam 0. 05 – 0. 15 mg/kg – Propofol
Intubating Pearls • If the patient is an elective or semi-elective intubation – pre-oxygenate with 100% O 2 for at least 5 minutes. This can allow up to 10 minutes to intubate without desaturation. • If intubating without a pulse oximeter, hold your breath while attempting intubation, if you need to breath so does the patient – bag ventilate. • ETCO 2 requires cardiac output and therefore may not be reliable if intubating during a cardiac arrest – if none detected, confirm with physical exam.
Case Presentation • Neuromuscular blockade was administered however you are not able to intubate the patient. • Despite bagging, the patient is desaturating and now becoming bradycardic. • Now what? ? ?
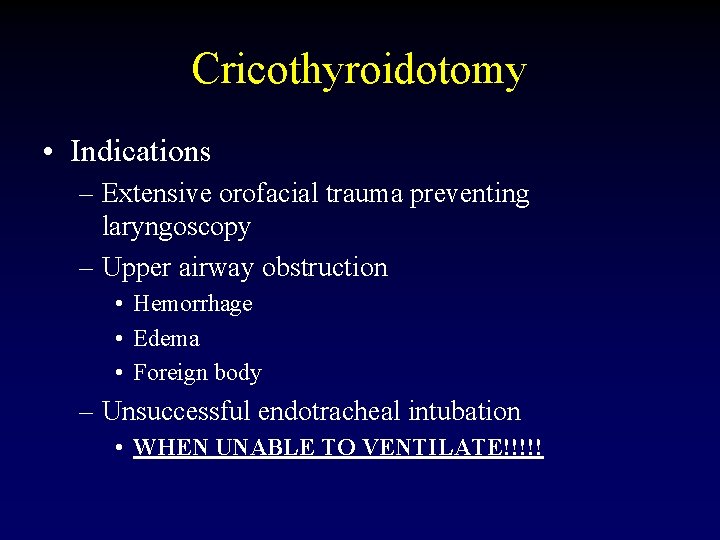
Cricothyroidotomy • Indications – Extensive orofacial trauma preventing laryngoscopy – Upper airway obstruction • Hemorrhage • Edema • Foreign body – Unsuccessful endotracheal intubation • WHEN UNABLE TO VENTILATE!!!!!
Cricothyroidotomy • Contraindications – Children under age 12 • Needle cricothyroidotomy is preferred to prevent damage to the cricoid cartilage.

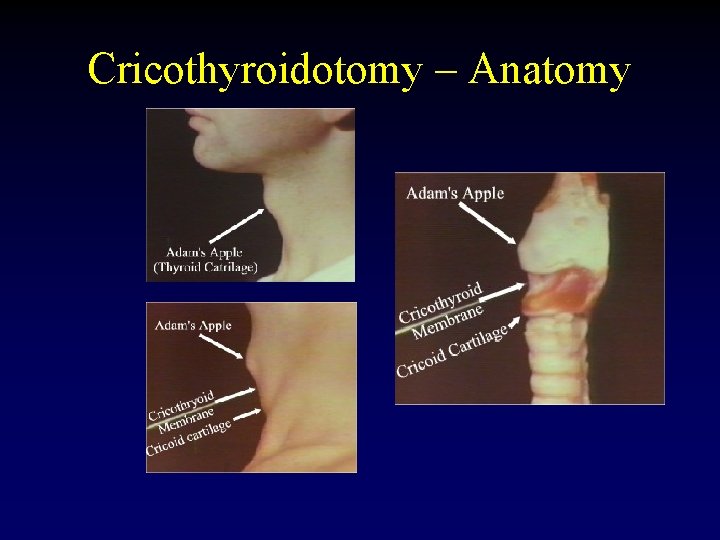
Cricothyroidotomy – Anatomy
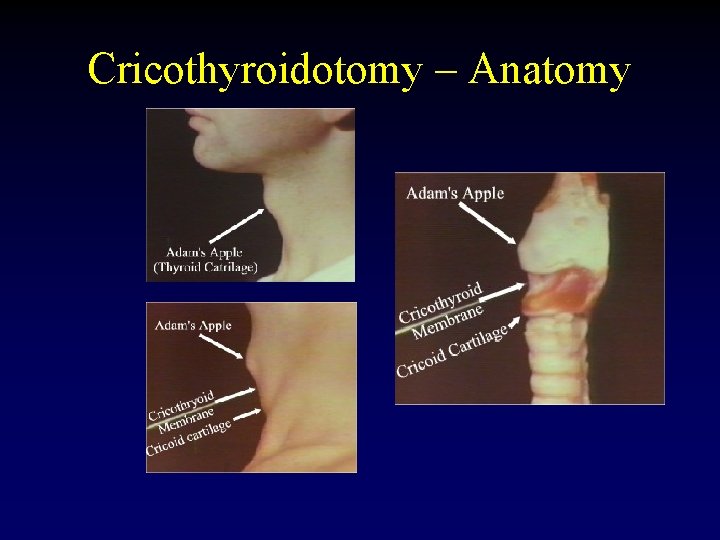
Cricothyroidotomy – Anatomy

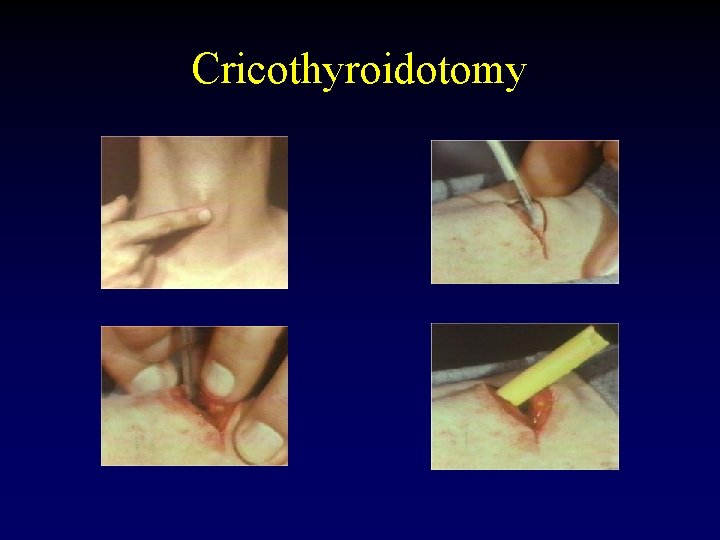
Cricothyroidotomy • Prep the neck • Palpate the cricothyroid membrane below the thyroid cartilage in the midline • Stabilize thyroid cartilage frimly with one hand make a transverse incision 2 cm in length down to and incising the cricothyroid membrane.
Cricothyroidotomy • Insert either a tracheal spreader or the back end of the scalpel handle and gently dialate • Insert a tube (tracheostomy, endotrachial, BIC pen? ) • Confirm ventilation • Suture tube to secure • Obtain hemostasis if necessary
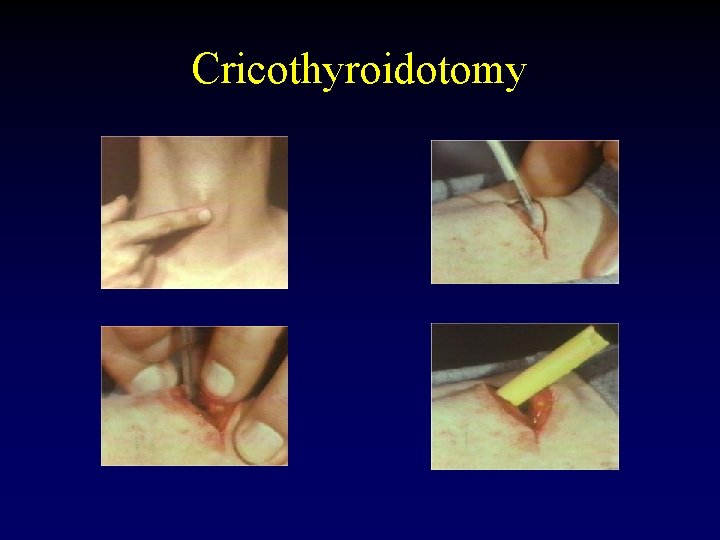
Cricothyroidotomy

Case Presentation • As you are screaming “a knife, my kingdom for a knife, ” your colleague successfully intubates with return of end-tidal CO 2. • The chest is auscultated with good breath sounds heard on the right, and no breath sounds on the left. • Now what?
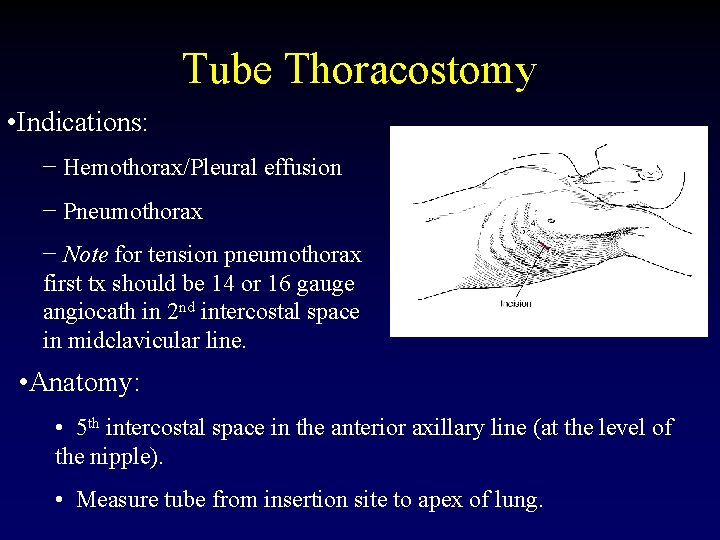
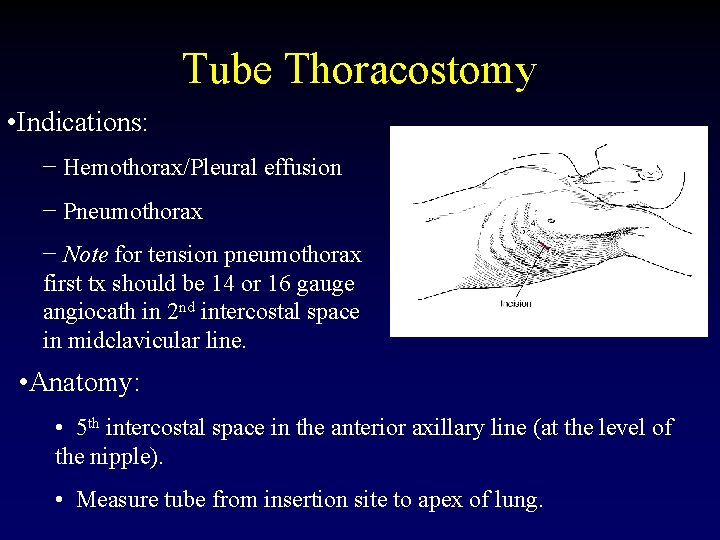
Tube Thoracostomy • Indications: − Hemothorax/Pleural effusion − Pneumothorax − Note for tension pneumothorax first tx should be 14 or 16 gauge angiocath in 2 nd intercostal space in midclavicular line. • Anatomy: • 5 th intercostal space in the anterior axillary line (at the level of the nipple). • Measure tube from insertion site to apex of lung.

Tube Thoracostomy • What you need. . . – Chest tube – Pleuravac – Sterile drapes, gloves and gown – Instruments – scalpel and Kelly clamp – Heavy silk suture – Gauze and silk tape for dressing

Tube Thoracostomy • Procedure: − Prep and drape hemothorax − Infiltrate skin, subcutaneous tissue and pleura with 1% lidocaine – – 1. 5 -2 cm incision directly over the 6 th rib down to the rib With a blunt clamp, dissect over the superior edge of the rib. Bluntly pierce the pleura with the clamp and spread the track. Be prepared for a rush of blood, fluid and/or air.
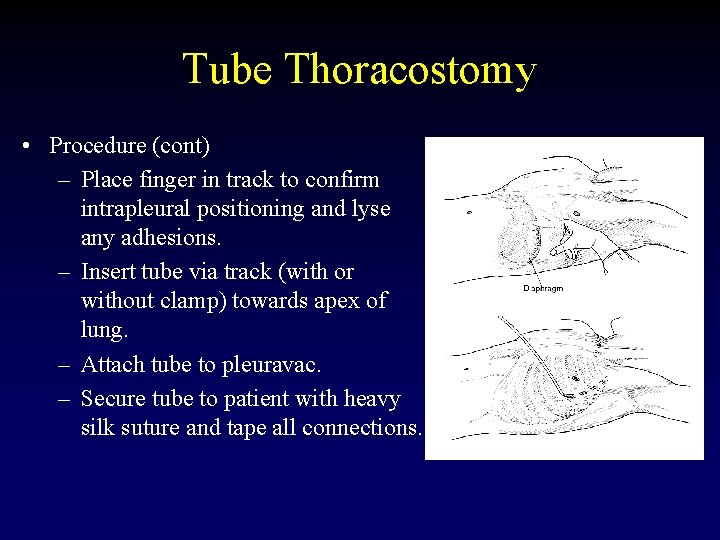
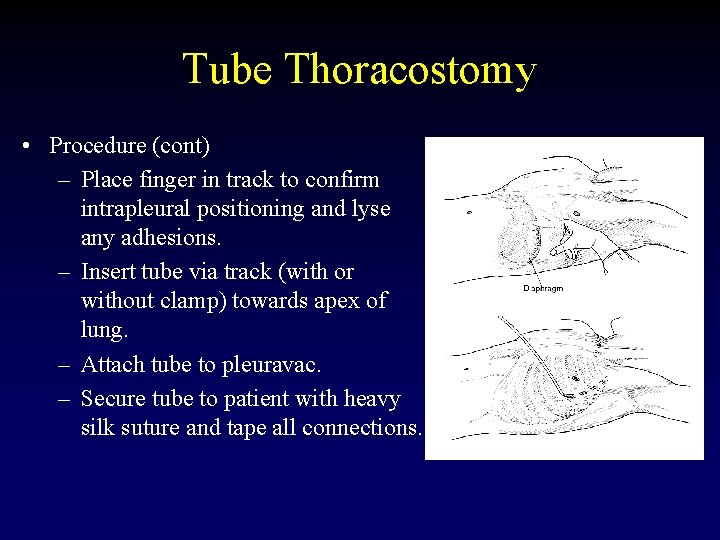
Tube Thoracostomy • Procedure (cont) – Place finger in track to confirm intrapleural positioning and lyse any adhesions. – Insert tube via track (with or without clamp) towards apex of lung. – Attach tube to pleuravac. – Secure tube to patient with heavy silk suture and tape all connections.

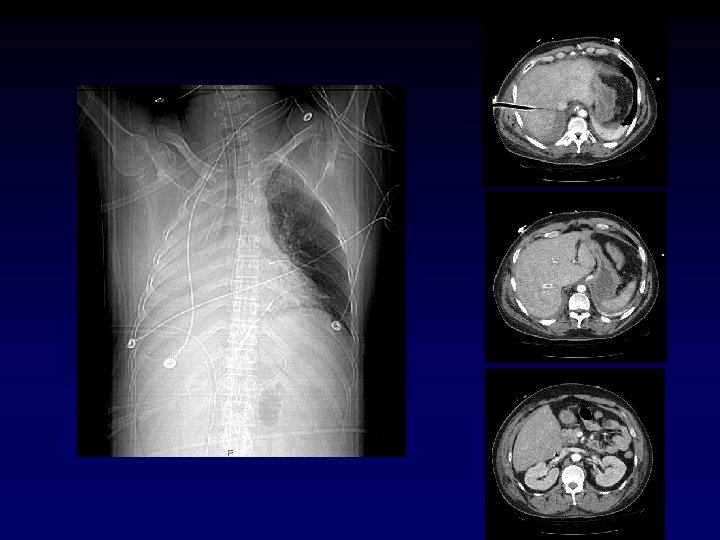
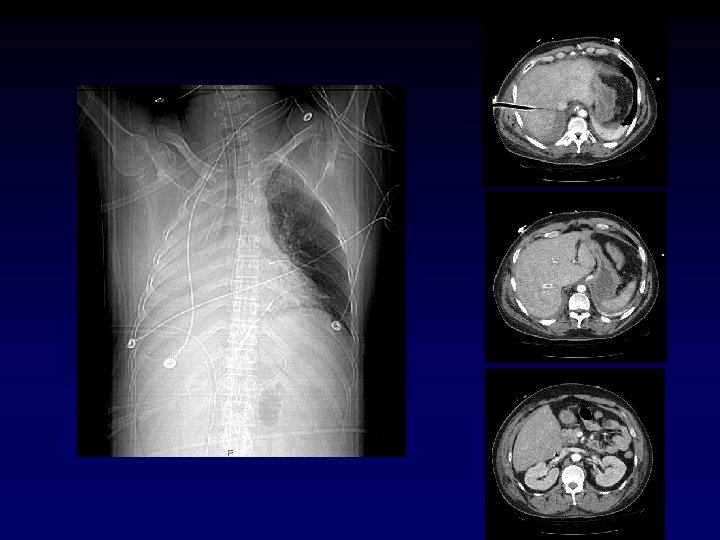
Warning! • History of chest tubes, thoracotomies or inflammatory pulmonary pathology. – Assume adhesions between the lung and the chest wall. – The chest tube insertion cause a lung laceration. • Be very careful how low you are, you can easily place an abdominal tube if you are not careful.

Case Presentation • Now that the chest tube is draining the hemopneumothorax, the patient’s pressure drops to 60/palp • Help? • The patient has bilateral track marks from history of IVDA.
Central Venous Access • Indications – CVP monitoring – TPN – Long-term infusion of drugs – Inotropic agents – Hemodialysis – Poor peripheral access

Central Venous Access • Vein sites – Femoral – Subclavian – Internal jugular • Contraindications – Vein thrombosis – Coagulopathy or thrombocytopenia

Central Venous Access • What you need – – – Central line kit/tray Sterile gloves and gown Mask and hat Sterile drapes Sterile flush – 10 cc syringe per port – Lidocaine – Betadine – Silk suture
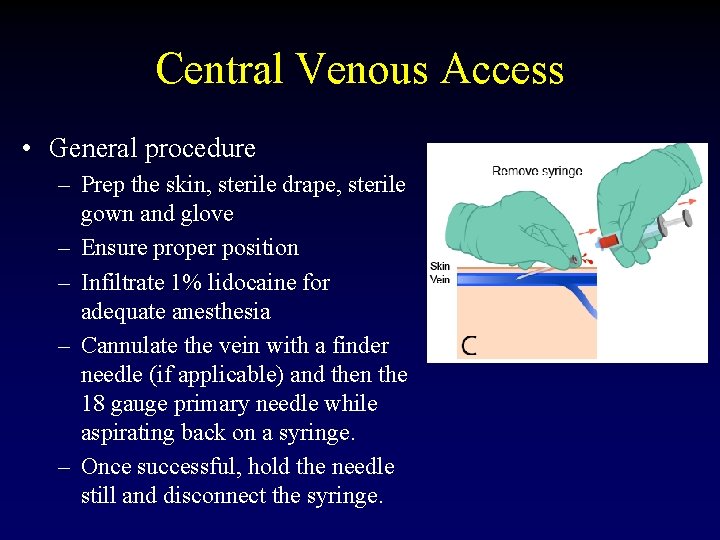
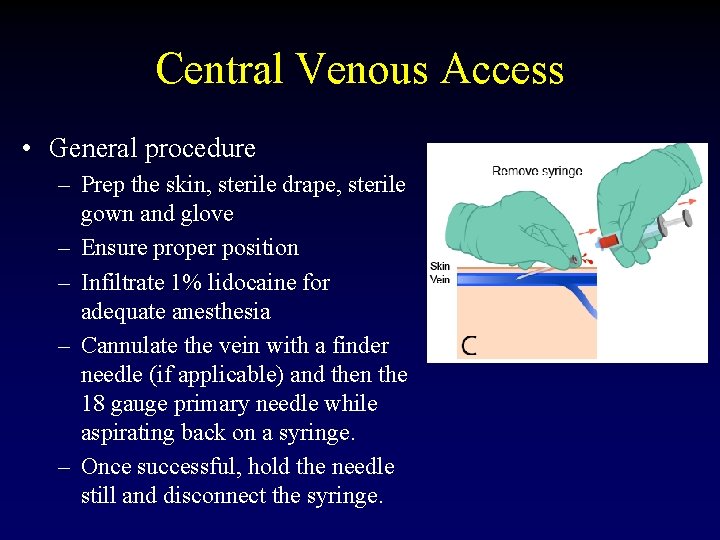
Central Venous Access • General procedure – Prep the skin, sterile drape, sterile gown and glove – Ensure proper position – Infiltrate 1% lidocaine for adequate anesthesia – Cannulate the vein with a finder needle (if applicable) and then the 18 gauge primary needle while aspirating back on a syringe. – Once successful, hold the needle still and disconnect the syringe.

Central Venous Access • General procedure (cont. ) – Ensure that back bleeding from needle is venous – Feed J wire into vein while holding needle still – Remove needle, leaving wire in place – Make a skin incision over the needle – Use the dilator over the wire to dilate the skin and subcutaneous tissues – Remove the dilator and feed the venous catheter over the wire.
Central Venous Access • General procedure (cont. ) – Place the catheter to the appropriate length and remove the wire. – Aspirate and flush all ports to confirm placement – Suture the line into place – Apply sterile dressing – CXR for jugular or subclavian attempts. – During the entire procedure – NEVER LOSE CONTROL OF THE WIRE
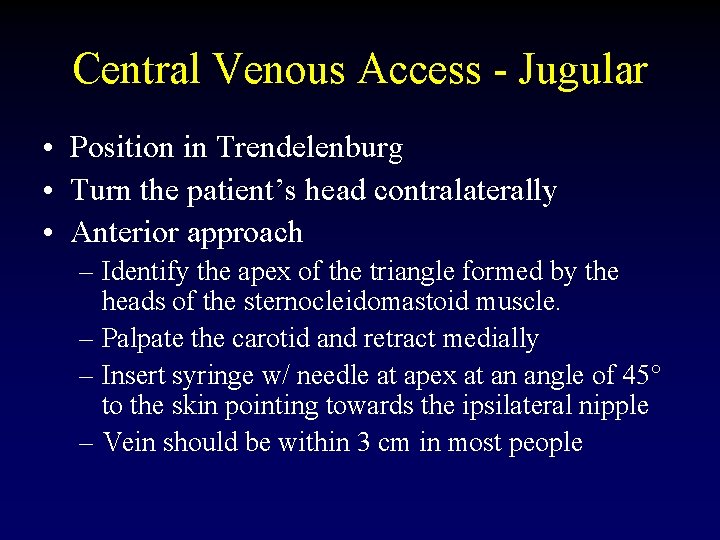
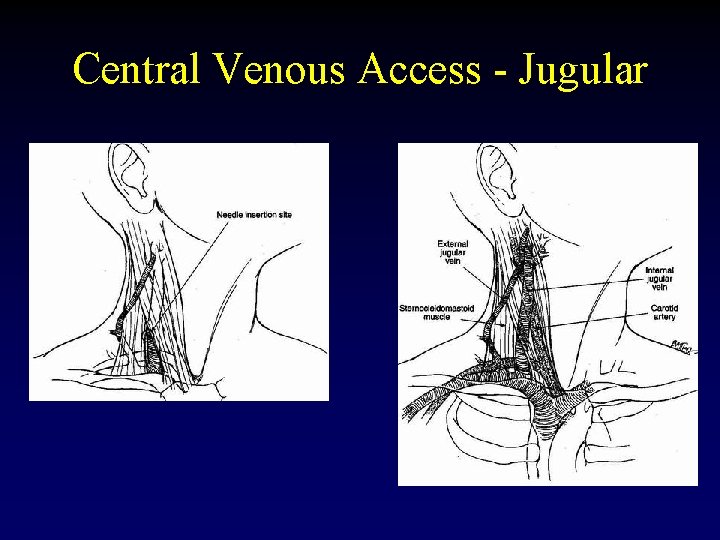
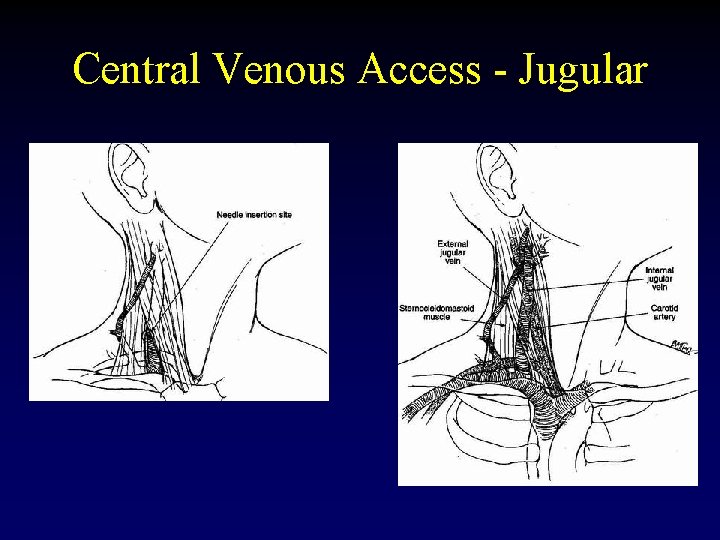
Central Venous Access - Jugular • Position in Trendelenburg • Turn the patient’s head contralaterally • Anterior approach – Identify the apex of the triangle formed by the heads of the sternocleidomastoid muscle. – Palpate the carotid and retract medially – Insert syringe w/ needle at apex at an angle of 45° to the skin pointing towards the ipsilateral nipple – Vein should be within 3 cm in most people
Central Venous Access - Jugular

Central Venous Access - Jugular • Posterior approach – Identify the lateral border of the SCM where the ext. jugular crosses (about 4 -5 cm above the clavicle) – Insert a needle anteriorly and inferiorly pointing to the sternal notch – The vein should be encountered within 3 cm in most individuals.
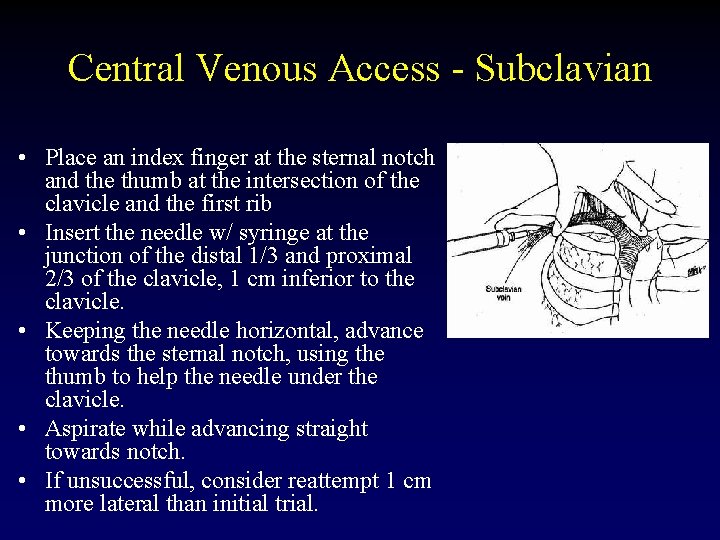
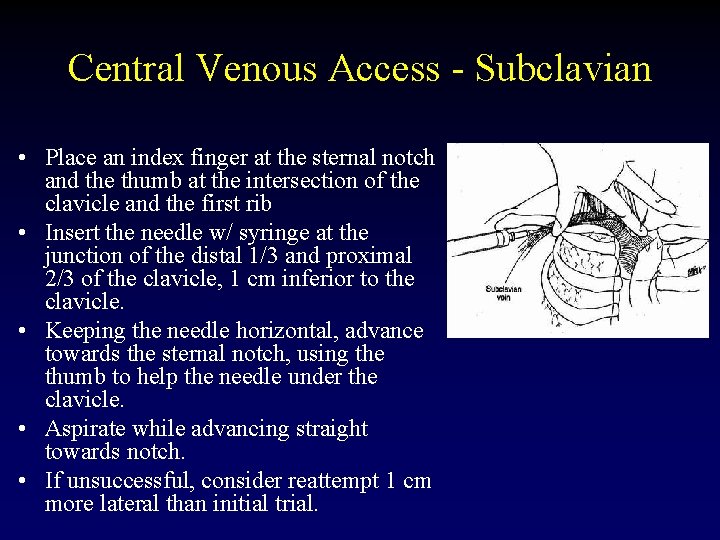
Central Venous Access - Subclavian • Place an index finger at the sternal notch and the thumb at the intersection of the clavicle and the first rib • Insert the needle w/ syringe at the junction of the distal 1/3 and proximal 2/3 of the clavicle, 1 cm inferior to the clavicle. • Keeping the needle horizontal, advance towards the sternal notch, using the thumb to help the needle under the clavicle. • Aspirate while advancing straight towards notch. • If unsuccessful, consider reattempt 1 cm more lateral than initial trial.

Central Venous Access - Femoral • Palpate the femoral artery – Midpoint between ant. sup. iliac spine and pubic symphysis • Femoral vein is immediately medial to the artery. • Insert needle medial and parallel to the pulse at 45° to the skin. • The vein should be encountered within < 6 cm.
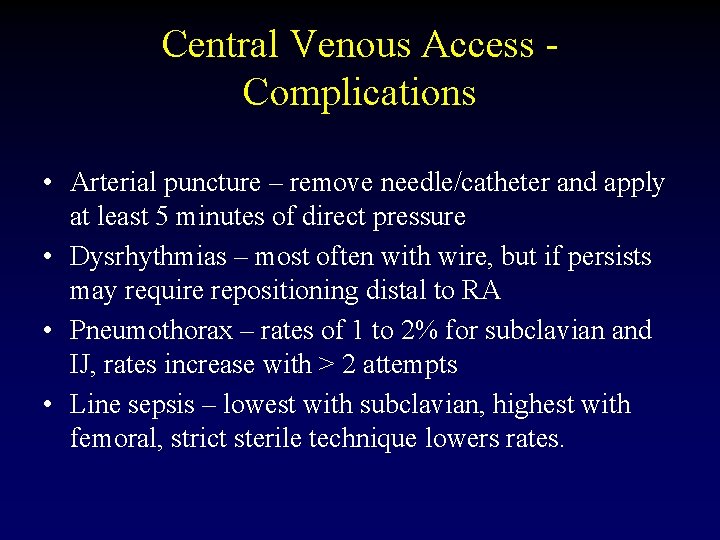
Central Venous Access Complications • Arterial puncture – remove needle/catheter and apply at least 5 minutes of direct pressure • Dysrhythmias – most often with wire, but if persists may require repositioning distal to RA • Pneumothorax – rates of 1 to 2% for subclavian and IJ, rates increase with > 2 attempts • Line sepsis – lowest with subclavian, highest with femoral, strict sterile technique lowers rates.

Case Presentation • Now with a femoral cordis in place, the patient receives 2 liters of LR with an improvement in vitals. He has 800 cc of blood drained from his left chest. • Is he adequately resuscitated? Over? Under?
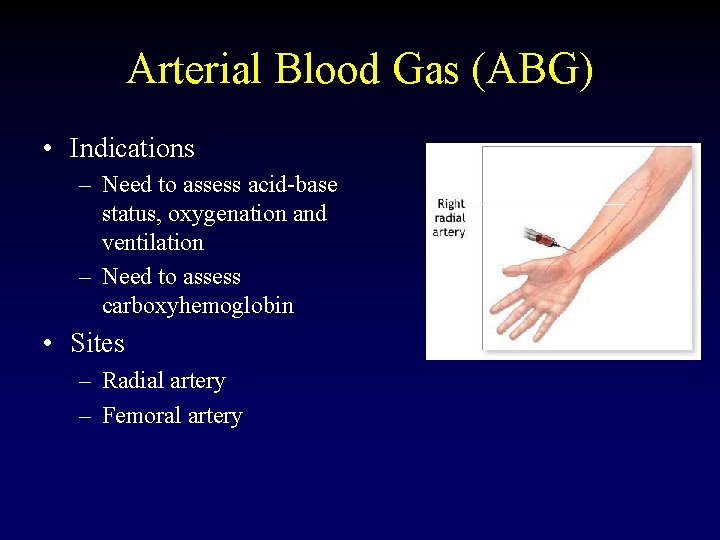
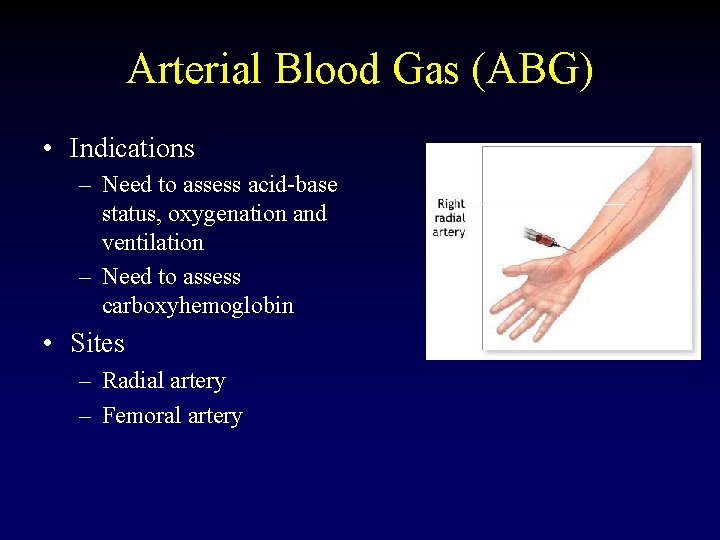
Arterial Blood Gas (ABG) • Indications – Need to assess acid-base status, oxygenation and ventilation – Need to assess carboxyhemoglobin • Sites – Radial artery – Femoral artery
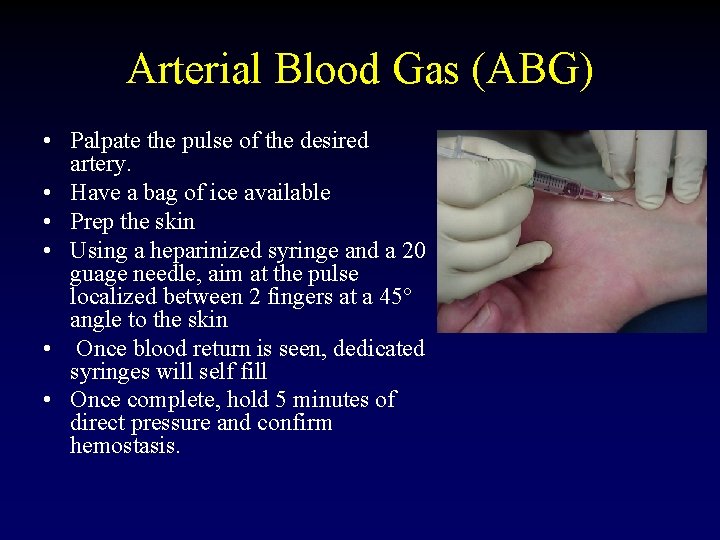
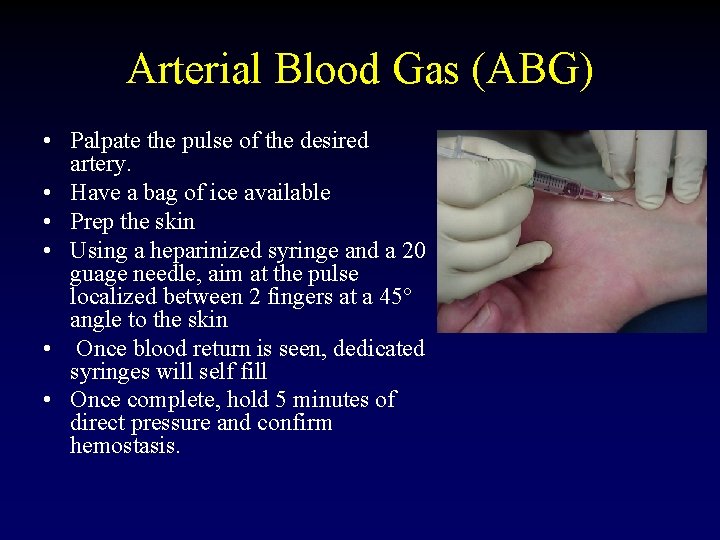
Arterial Blood Gas (ABG) • Palpate the pulse of the desired artery. • Have a bag of ice available • Prep the skin • Using a heparinized syringe and a 20 guage needle, aim at the pulse localized between 2 fingers at a 45° angle to the skin • Once blood return is seen, dedicated syringes will self fill • Once complete, hold 5 minutes of direct pressure and confirm hemostasis.

Case Presentation • As the respiratory therapist is suctioning the patient’s mouth, he starts vomiting rice and beans mixed with beer. • He does not appear to have aspirated, but his stomach is not empty yet. . .
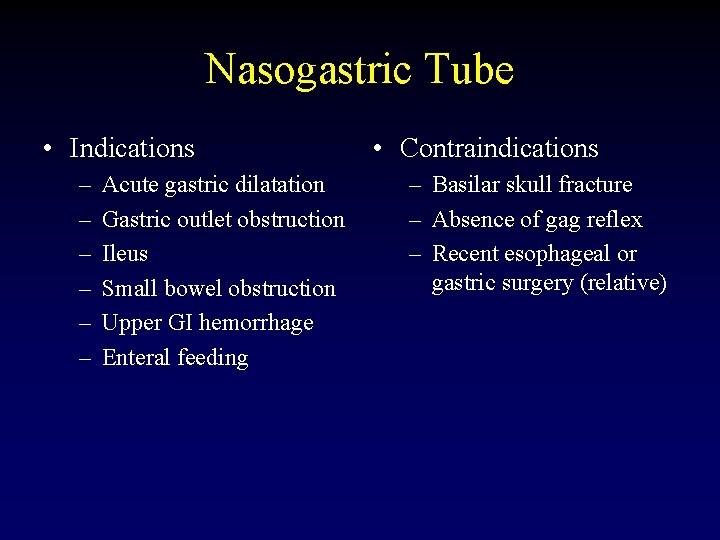
Nasogastric Tube • Indications – – – Acute gastric dilatation Gastric outlet obstruction Ileus Small bowel obstruction Upper GI hemorrhage Enteral feeding • Contraindications – Basilar skull fracture – Absence of gag reflex – Recent esophageal or gastric surgery (relative)

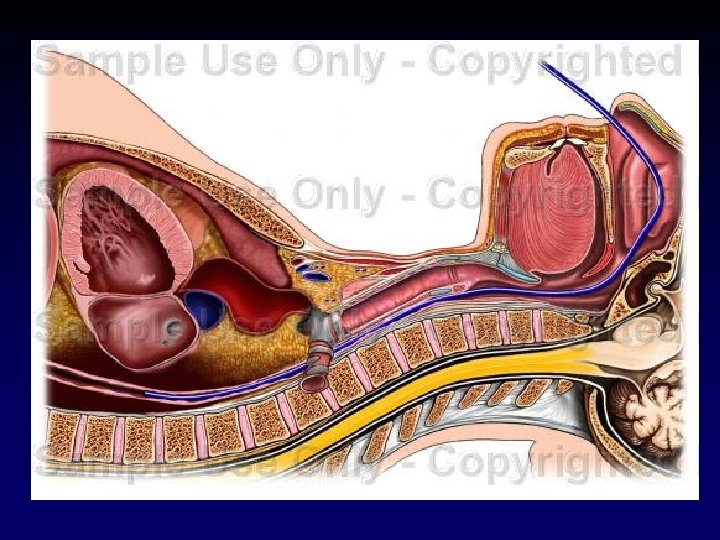
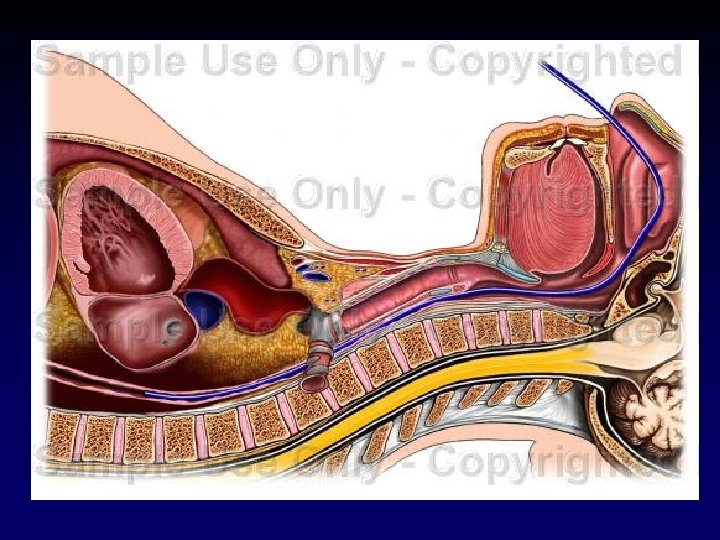
Nasogastric Tube • Measure tube from nose to earlobe to anterior abdomen so that proximal hole is distal to xiphoid. • Lubricate the tube • Have the patient flex their neck
Nasogastric Tube • Slowly insert the tube straight posteriorly from the nares. • Advance the tube into the pharynx aiming posteriorly, asking the patient to swallow if possible. • Once the tube has been inserted to desired length, inject air into the tube and auscultate over the stomach for placement.

Nasogastric Tube • Secure the tube with tape to the nose. Be sure not to secure it to the forehead/upward as this can cause alar necrosis. • If the tube is to be used for feeding, placement should be confirmed by xray.
Conclusions • Knowledge about simple surgical procedures can be lifesaving – however pure knowledge is not a substitute for repeated practice. • Take every opportunity to practice these procedures with senior and/or attending supervision under controlled circumstances.

 Devashish anjaria
Devashish anjaria Devashish anjaria
Devashish anjaria Devashish paul
Devashish paul Analysis of fences by august wilson
Analysis of fences by august wilson S3xt trade
S3xt trade Light in august summary
Light in august summary August kekulé
August kekulé August shi
August shi 30th august 2005
30th august 2005 Napoleon bonaparte was born on 15 august
Napoleon bonaparte was born on 15 august Central place theory hexagon
Central place theory hexagon Toomas nipernaadi kokkuvõte
Toomas nipernaadi kokkuvõte Anka neretvanka analiza
Anka neretvanka analiza Berlin weather august
Berlin weather august August safety topics
August safety topics Do que miranda, amiga de via, chamava august?
Do que miranda, amiga de via, chamava august? Diexi slides
Diexi slides August stern
August stern Fences character map
Fences character map Dr lorraine johnstone
Dr lorraine johnstone Full moon august 2011
Full moon august 2011 August strindberg faderen analyse
August strindberg faderen analyse Diane august
Diane august Kaugnayan sa kaligirang pangkasaysayan
Kaugnayan sa kaligirang pangkasaysayan Teori big bang
Teori big bang Povjestice postolar i vrag
Povjestice postolar i vrag What happened on august 23 1939
What happened on august 23 1939 6 months before august 31
6 months before august 31 Mirjam nilsson contoso
Mirjam nilsson contoso Strindbergs fruar
Strindbergs fruar August prima porta
August prima porta August alsina testimony album zip download
August alsina testimony album zip download Percobaan august weismann
Percobaan august weismann 2003 august 25
2003 august 25 Julie august
Julie august Disyembre 30 1896 pangyayari
Disyembre 30 1896 pangyayari August safety
August safety August 26 2010
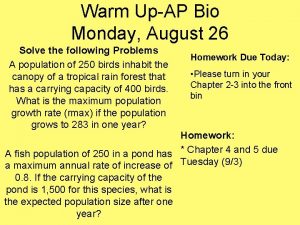
August 26 2010 August lec 250
August lec 250 August hlond przepowiednie
August hlond przepowiednie Gottfried august bürger lenore
Gottfried august bürger lenore August leyweg 4
August leyweg 4 August name pronunciation
August name pronunciation August šenoa povjestice
August šenoa povjestice August 29, 1958
August 29, 1958 Medicina upap
Medicina upap August bergqvist
August bergqvist August 27 2002
August 27 2002 Longest rivers in china
Longest rivers in china Micro computer services began operations on august 1
Micro computer services began operations on august 1 It was late summer 26 august 1910
It was late summer 26 august 1910 Propaganda techniques testimonial
Propaganda techniques testimonial Madonna born
Madonna born August wilson
August wilson August alsina testimony album download zip
August alsina testimony album download zip Dr ralph ferraro
Dr ralph ferraro Cnn 10 august 31
Cnn 10 august 31 Fences themes
Fences themes August strindberg giftas
August strindberg giftas August kiss
August kiss August 21, 2017 plus 1260 days
August 21, 2017 plus 1260 days Moric august benovsky dennik
Moric august benovsky dennik March april june july august
March april june july august