Surgical Asepsis and Assisting with Surgical Procedures Chapter



- Slides: 56
Surgical Asepsis and Assisting with Surgical Procedures Chapter 57 Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 1
Learning Objectives Define, spell, and pronounce the terms listed in the vocabulary. Apply critical thinking skills in performing patient assessment and care. Define the concepts of aseptic technique. Explain the differences among sanitization, disinfection, and sterilization. Summarize tips for improving autoclave techniques. Demonstrate how to wrap instrument packs for autoclave sterilization. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 2
Learning Objectives Explain the types and uses of sterilization indicators. Summarize the correct methods for loading, operating, and unloading an autoclave. Demonstrate how to operate an autoclave. Summarize common minor surgical procedures. Detail the medical assistant’s role in minor office surgery. Perform a skin prep for surgery. Perform a surgical hand scrub. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 3
Learning Objectives Outline the rules for setting up and maintaining a sterile field. Open a sterile pack to create a sterile field. Transfer sterile instruments and pour solutions into a sterile field. Apply sterile gloves without contamination. Demonstrate how to assist with a minor surgical procedure and suturing. Summarize postoperative instructions and care of wounds. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 4
Learning Objectives Demonstrate how to remove sutures and the technique of surgical staple removal. Explain the process of wound healing. Properly apply dressings and bandages to surgical sites. Conduct patient education in aseptic technique and surgical procedures. Discuss the legal and ethical concerns regarding surgical asepsis and infection control. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 5
Asepsis – freedom from infection or infectious material. Medical asepsis – destruction of organisms after they leave the body; prevent reinfection and cross-infection process of controlling pathogens Ø creates a clean environment but not a sterile one Ø Surgical asepsis – complete destruction of organisms on instruments or equipment that will enter the patient’s body Mandatory for any procedure that invades body tissues Ø Everything that comes in contact with the patient must be sterile Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 6
Sanitization Sanitization – cleansing process that decreases the number of microorganisms; removes debris such as blood and other body fluids; performed immediately after surgical procedure Wear thick utility gloves Rinse each instrument in cold, running water Clean sharp instruments at one time to avoid injury Open hinges and scrub serrations and ratchets Rinse instruments in hot water and check for proper working order Hand dry Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 7
Disinfection Disinfection – process of killing pathogenic organisms or of rendering them inactive Not always effective against spores and certain viruses Disinfectant chemicals may kill microbes within a short time but may be hard on instruments Some chemicals (Cidex) can kill all organisms but immersion time is 10 or more hours Follow manufacturer’s guidelines on how to properly use each product Typical facility has dirty and clean utility areas Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 8
Autoclave and PPE Sterilization procedures destroy all living organisms. Typically done with an autoclave. PPE procedures include: Heat-resistant autoclave gloves for loading and unloading. Ø Fluid-resistant gloves to prevent contact with contaminants. Ø Laboratory coat or impervious gown if needed to protect against splashes. Ø Face shield and/or goggles if there is a splash hazard. Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 9
Critical Thinking Application The office manager told Melissa she needs to review office policies and procedures on surgical supplies and sterilization methods. Why is this important before she starts performing sterilization procedures? What information in this manual would be most important to Melissa as she starts this new position? Why? Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 10
Autoclave: Procedure 57 -2 Uses steam under pressure to kill all microorganisms; pressure creates heat higher than the boiling point. Steam moisture must contact all surfaces for sterilization to occur. Recommended temperature in an autoclave is 121° to 123°C (250° to 255°F). Unwrapped items should take 20 minutes, small packs 30 minutes, large packs 40 minutes. At the end of the cycle open the door ¼ inch; allow pack to cool before removing from autoclave. Muslin packs have a shelf-life of 28 days; plastic wraps, 6 months. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 11
Autoclave Cycles Gravity or “fast exhaust” cycle—Used to sterilize stainless steel instruments; fills with steam and held at set temperature for set period of time; when cycle ends chamber rapidly returns to atmospheric pressure. Liquid or “slow exhaust” cycle—Used to prevent sterilized liquids from boiling; steam is exhausted slowly at end of cycle allowing liquids to cool. Prevacuum cycle—Used for porous materials; chamber is partially evacuated before introduction of steam for greater steam penetration. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 12

Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 13
Autoclave Errors Superheated steam—dries out before total moistening of pack. Wet steam—failing to preheat the autoclave, opening the door too wide at the end of the cycle, or overfilling the water reservoir causes condensation in the chamber. Residual air—without elimination of air, high temperature will not be reached. Refer to Table 57 -2. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 14
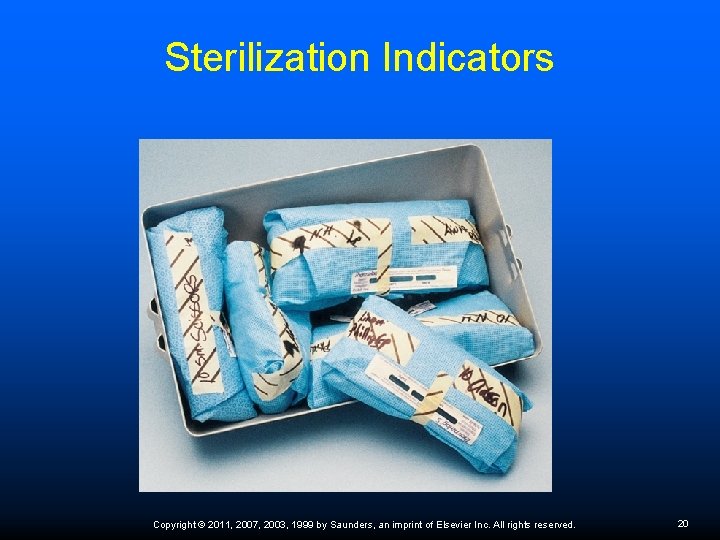
Wrapping Instrument Packs Inspect muslin wrappers before each use. Discard any wrappers with holes. Wrap all hinged instruments in the open position to allow full steam penetration of the joint. Place a gauze sponge around the tips of sharp instruments to prevent them from piercing the wrapping material. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 15
Wrapping Instrument Packs If a number of instruments are to be placed on a stainless steel tray for wrapping, place a double-folded towel on the tray before placing the instruments to protect them. With sterilizing bags, insert the jaws of the instruments first to ensure that the grasping end of the instrument can be reached easily when the bag is opened. Indicate on the wrapper what is in the pack; sterilization date; MA initials. Refer to Procedure 57 -1. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 16

Instrument Packs Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 17
Critical Thinking Application Melissa is processing instruments and trays when she notices that one of her co-workers never inspects a muslin wrapper before wrapping a pack. What is the significance of Melissa’s observation? How should she handle this situation? Why? Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 18
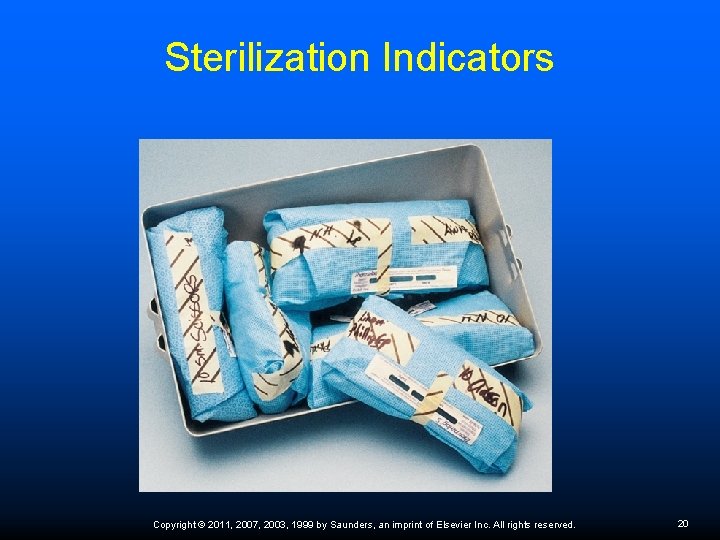
Sterilization Indicators Sterilization occurs only when steam reaches an optimal temperature for a designated length of time and has penetrated the center of the pack. Ø Autoclave tape—dye changes color when exposed to steam; merely indicates a high temperature was reached. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 19
Sterilization Indicators Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 20
Sterilization Indicators Indicator strips—contains temperature-sensitive dye that changes color when proper conditions are reached; should be loaded in the center of the largest pack. Ø Culture test—spore strip or tube that contains microbes that should be destroyed during the sterilization process. Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 21
Labels Indicate on the wrapper what is in the package, or label it with a code. This code should correspond to a list of instruments that is stored with the pack after sterilization. Label the contents with the date sterilized and your initials. Use a permanent marker, never a ballpoint pen. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 22
Loading the Autoclave Must be able to have circulation of steam and heat around all packs. Packs should be rested on their edges. Jars and bottles must be placed on their sides without lids. Perforated trays should be used for unwrapped instruments, with a towel under and over them to facilitate drying and prevent contamination when being removed from the autoclave. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 23
Unloading the Autoclave Allow the load to dry for at least 15 minutes. Dry, wrapped packs may be removed with clean, dry hands, but it is safer to wear heat-resistant gloves. Place the packs on a dry, dust-free surface. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 24
Unloading Guidelines Stand behind the door when opening it, to prevent accidental steam burns. Slowly open the door only a crack, allowing the items to cool for 15– 20 minutes before removing them. If for any reason the integrity of the sterilization process is in question, the load should be considered contaminated and reautoclaved. Reasons for concern include the following: Any load that fails to convert a sterilization indicator strip Ø Any loads processed after a biological test indicates that the autoclave is not working properly Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 25
Shelf-Life of Sterilized Packs Muslin and autoclave paper packs are considered sterile for up to 28 days from the date of sterilization. Polypropylene autoclave bags are sterile for up to 6 months from the sterilization date. Fabric wrappers must be inspected for holes and laundered after each use. Watch the expiration date. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 26
Critical Thinking Application Melissa discovers a number of packages of paper-wrapped sterile instruments that have no dates on them. The indicator tape shows that they have been autoclaved. What should she do with these packs? Why? Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 27
Surgical Procedures Suturing Cyst removal Incision and drainage of an abscess Collection of biopsies The medical assistant should be proficient at explaining each of these procedures to the patient, preparing the patient and the room, assisting the physician with the surgery, and applying a sterile dressing and bandage after the procedure is completed. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 28
Surgical Procedures Electrosurgery Laser surgery Microsurgery Endoscopic procedures Cryosurgery Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 29
Electrosurgery Grounding Pad Carefully inspect pad, cable, and skin before procedure. Place pad close to operative site. Pad must be tight against patient’s skin. Apply pad to fleshy area. Do not place pad over bony area, body hair, metal implants, or pacemaker. Carefully inspect pad site after procedure for discoloration. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 30
MA Role During Laser Surgery Observe the surgical field through safety goggles and protect the patient’s eyes Keep wet sponges ready Remove any flammable item from laser’s path Assist with suctioning of plume Sterile normal saline solution and syringe ready Anticipate needs for protective supplies, special equipment, or instruments Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 31
Assisting with Surgical Procedures Prepare the patient. Ø Answer all questions regarding the procedure. Provide preoperative instructions. Ø Ø Ø Have consent forms ready to sign. Give the patient the necessary preoperative instructions. Tell the patient to bring a relative or friend to drive him or her home after the surgery. Instruct the patient to leave jewelry and other valuables at home. Call the patient the day before the scheduled surgery to confirm any special instructions. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 32
Informed Consent Surgery cannot be legally performed without informed consent without risking an accusation of battery. The consent clearly limits what procedures can be done. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 33
Critical Thinking Application Melissa is preparing a patient for a breast biopsy. The consent form was previously signed and is in the chart. When Melissa is chatting with the patient while completing the final setup for the procedure, it becomes clear that the patient thinks she is having a “cyst removed” from her breast. What action should Melissa take, if any? What is the significance of what the patient said in this situation? Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 34
Assisting with a Surgical Procedure Position the patient Ø Expose the surgical site Skin preparation Ø Refer to Procedure 57 -3 Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 35
Preparation of the Room Refer to Table 57 -3 Sterile technique Everything that is sterile is white and everything that is not sterile is black. There is no gray! Ø Sterile surfaces must never come into contact with nonsterile surfaces. Ø Refer to Procedures 57 -4 to 57 -8 Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 36
Preparation for Surgery Sanitize your hands; gather all supplies. Escort patient into the room. Greet and converse with patient. Position patient on table. Sanitize your hands. Open first towel pack. Open skin preparation pack. Pour soap and antiseptic solutions. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 37
Preparation for Surgery Expose the site to be prepped. Glove and arrange preparation items within the sterile field. Place sterile towels at skin scrub boundaries using sterile technique. Prepare the patient’s skin. Discard skin preparation materials in appropriate containers. Discard gloves; wash your hands following the guidelines for a surgical hand scrub (Procedure 57 -4) if this procedure is part of the policy of the attending physician/facility. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 38
Preparation for Surgery Open table drape pack on Mayo stand to create sterile field. Open instrument pack (packs) and transfer instruments to sterile field. Add sterile syringe unit. Add sterile items as requested. Physician joins you and converses with the patient. Open the physician’s glove pack (the physician now puts on gloves). Open the patient drape pack (the physician now drapes the surgical site). Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 39
Preparation for Surgery Cleanse and hold up anesthesia vial for the physician to withdraw anesthesia with a sterile syringe (the physician will now administer the anesthesia). Repeat surgical hand wash; reglove with a new glove pack. Arrange sterile field instruments and other materials for safety and in sequence; check instrument condition. Open up the suture/needle pack per physician choice; load the first suture into the needle holder. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 40
Preparation for Surgery Place two gauze sponges at the site. Assist with the procedure. Check vital signs as instructed. Record and prepare specimens. Clean room and discard materials in biohazard waste containers. Chart the procedure on the medical record. Help the patient to prepare to leave the office. Sanitize, disinfect, and sterilize equipment. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 41
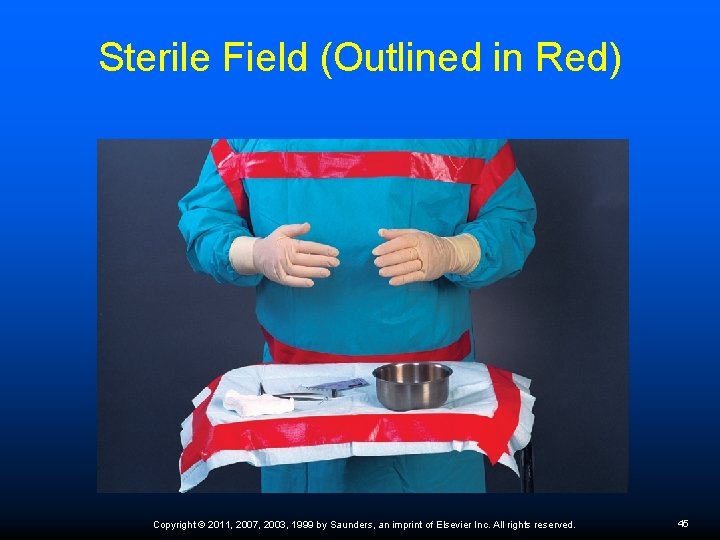
Sterile Field Talking should be kept to a minimum because air currents carry bacteria. Sterile team members should always face one another. Always keep the sterile field in your view. If you turn your back on a sterile field or lose sight of it, it is considered contaminated. Nonsterile persons or items should never cross over the sterile field. Tables are sterile only at table level; anything that falls below the edge of the Mayo tray is considered contaminated. A 1 -inch border surrounding the tray is considered contaminated, so anything placed on the tray within that 1 -inch border is contaminated. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 42
Sterile Field Consider a sterile barrier contaminated if it has been wet, cut, or torn. Packages placed on a clean surface are contaminated on the outside, but the inside of the sterilized package may be used as a sterile field. Keep sterile gloved hands above waist level at all times; do not let hands drop below the waist. Never remove then replace any item in the field (such as using sterile forceps to cleanse a wound), or the field will be contaminated. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 43
Sterile Field The inside of a sterile package remains sterile if the package is peeled open properly; it should be opened the entire way, then the contents tossed onto the field without crossing over the sterile area. If a sterile package falls to the floor, it must be discarded NOTE: If you are in doubt about the sterility of anything, consider it contaminated. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 44
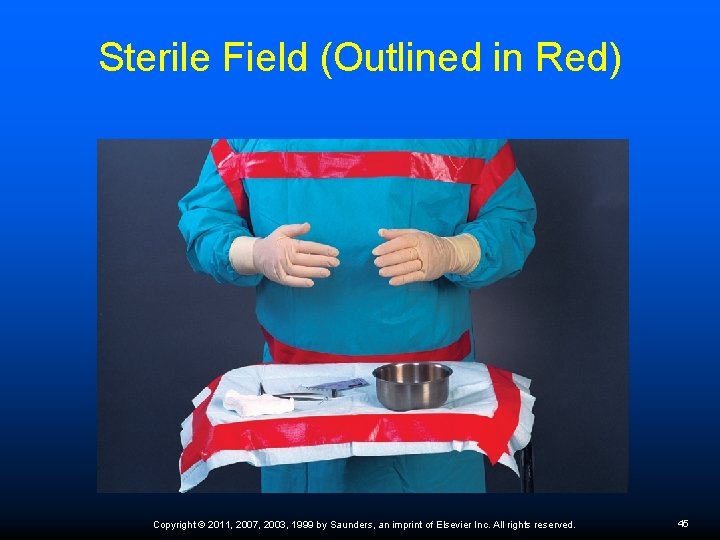
Sterile Field (Outlined in Red) Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 45
Assisting the Physician during Surgery Passing instruments Specimen collection Completing the surgical procedure – Procedures 57 -9 through 57 -11 Postoperative responsibilities Wear disposable gloves until all contaminated materials are properly removed and handled. Ø Place disposable equipment and supplies in biohazard waste cans and/or sharps containers. Ø The room should be checked for any blood spills or other contamination and cleaned appropriately. Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 46
Critical Thinking Application While passing the scalpel to the surgeon when assisting with an I&D, Melissa feels the blade “slice” through her glove. She quickly and secretly looks at it and notices a “very tiny” nick in her glove. Because this is a “dirty” procedure, she decides to say nothing and continues assisting with the procedure. Is her reasoning sound here? What is the best approach to handling this situation? Why? Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 47
Stages of Wound Healing Lag phase – blood vessels contract to control hemorrhage, platelets form a network, fibrin is released, and clotting begins; macrophages clear away bacteria and dead tissue; in 1 to 4 days fibrin threads contract and pull wound edges together under the scab. Proliferation phase – the wound healing and new growth period lasts 5 to 20 days; tissues repair themselves, new cells form, and the wound continues to contract and seal. Remodeling phase – shallow wounds contract in the first two stages but large wounds require the cellular activity of the third phase to build a bridge of new tissue that closes the wound; collagen provides strength and forms scar tissue. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 48
Classifications of Wound Repair The clean, surgical wound that has been sutured closed and heals quickly without much scarring does so by first intention. Tissues that are severely damaged, purposely kept open, or fail to close are said to heal by granulation (healing from the bottom of the wound outward), which is called second intention Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 49
Influences on Healing Process Young, healthy, and adequate nutrition promote healing Protection and rest of injured area Destruction or reinjury during second phase can delay healing and increase scarring Presence of infection or debris in wound Necrotic tissue must be removed. Removal of debris is called debridement, which may occur naturally or be performed surgically Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 50
Advantages to Open Wound Healing It allows air to freely circulate around the wound. The wound is not irritated or rubbed by a dressing. The wound stays dry, which inhibits bacterial growth, reducing the chance of infection. Sutures stay dry and hold together better. Any preexisting infection remains localized and is not spread by the dressing or bandage. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 51
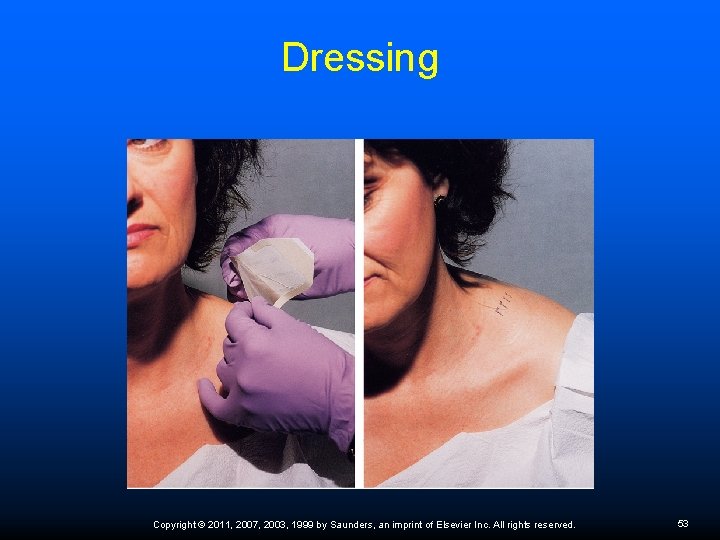
Dressing Sterile covering placed over a wound Protects the wound from injury and contamination Maintains constant pressure to minimize bleeding and swelling Holds the wound edges together Absorbs drainage and secretions Small, clean lacerations may be closed with Steri-Strips Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 52
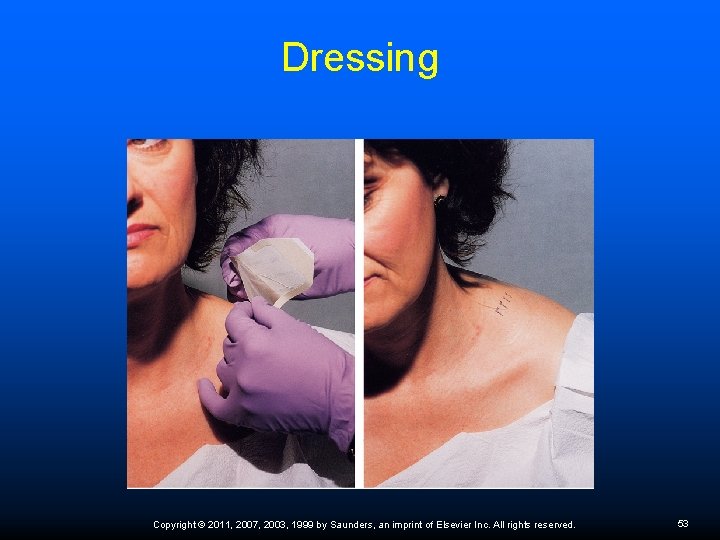
Dressing Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 53
Bandages Hold dressings in place Help maintain even pressure, support the affected part, and protect wound from injury and contamination Gauze, cloth, or elastic cloth rolls Refer to Procedure 57 -13 Bandages that are too loose fall off and those that are too tight may compromise circulation and further harm the patient Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 54

Bandages Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 55
Patient Education about surgical procedures uses information sheets or pamphlets given to the patient before surgery, conversations with the patient about the procedure, and information sheets to prevent and minimize complications. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 56