Immunology 101 4 Leonard H Sigal MD lensigalgmail


- Slides: 29
Immunology 101. 4 Leonard H Sigal, MD lensigal@gmail. com

Introduction to Immunology. 4 01 02 03 04 “DIAGNOSTIC” TESTS OFTEN AREN’T ANTI-NUCLEAR ANTIBODIES (ANA) AND RHEUMATOID FACTOR ERYTHROCYTE SEDIMENTATION RATE (ESR; SED RATE) AND CREACTIVE PROTEIN (CRP) ANTIBODY TESTING FOR LYME DISEASE
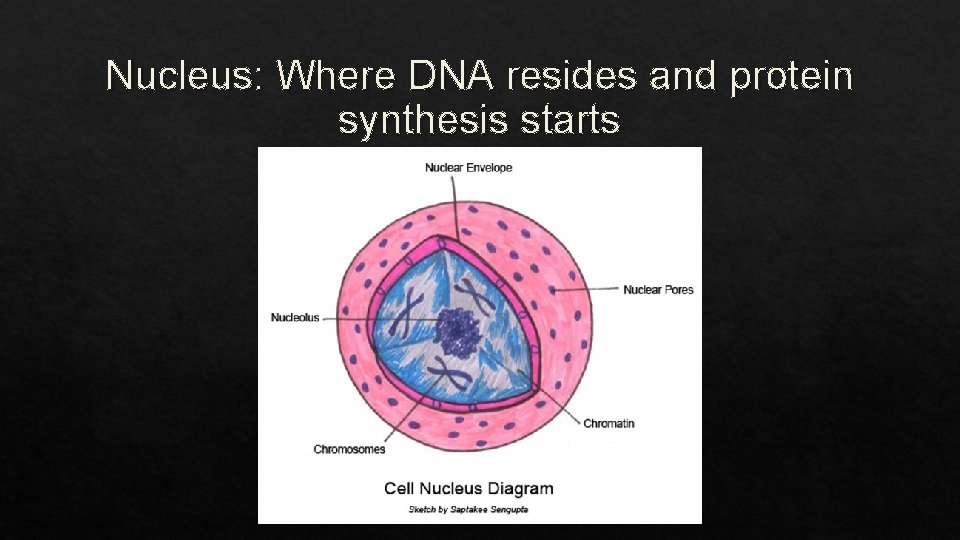
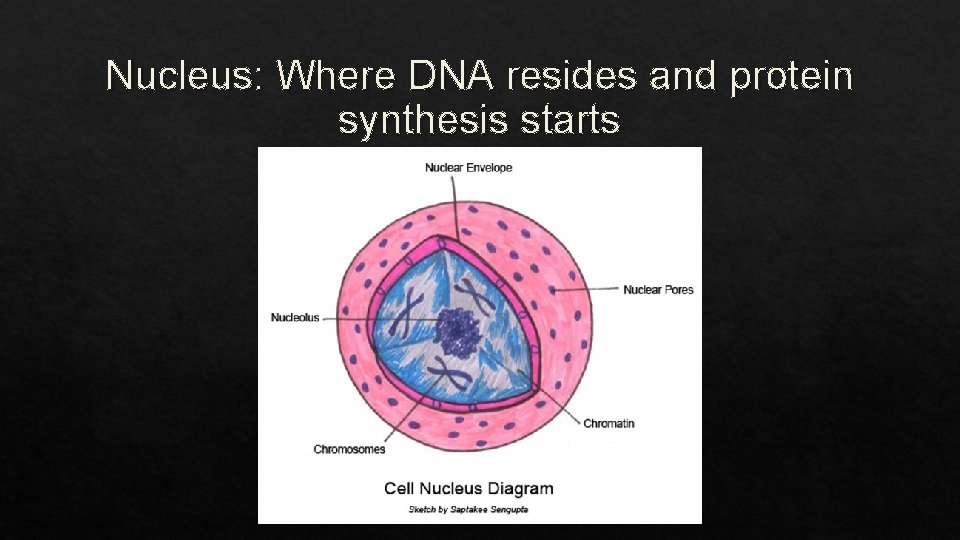
Nucleus: Where DNA resides and protein synthesis starts
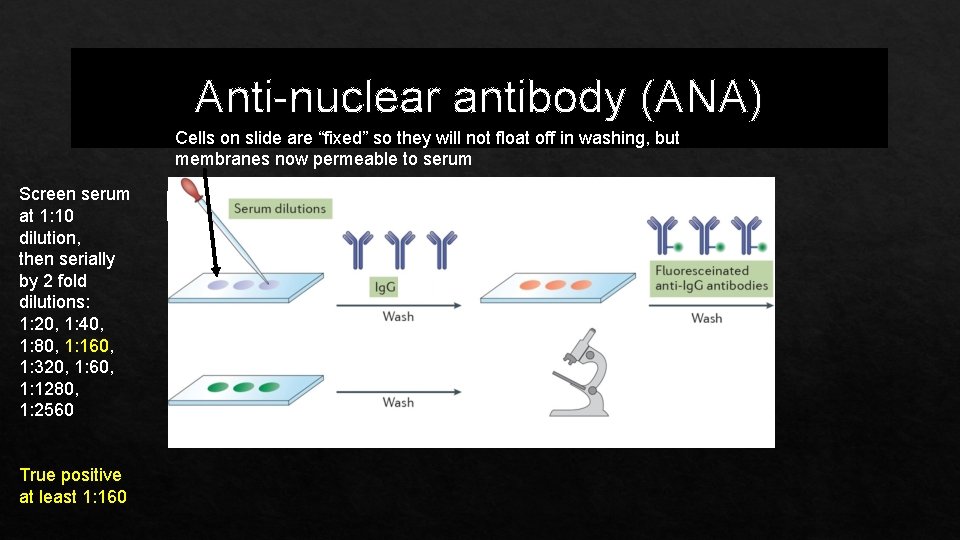
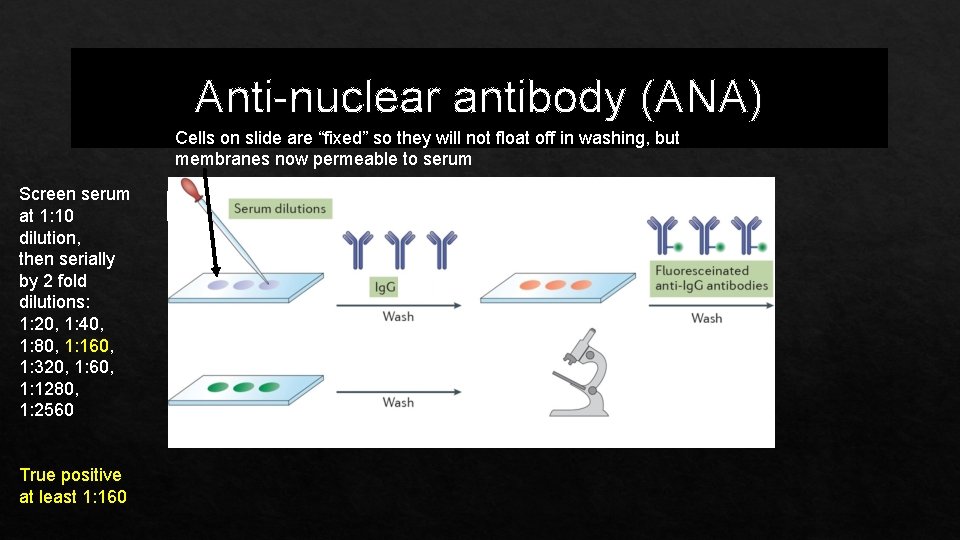
Anti-nuclear antibody (ANA) Cells on slide are “fixed” so they will not float off in washing, but membranes now permeable to serum Screen serum at 1: 10 dilution, then serially by 2 fold dilutions: 1: 20, 1: 40, 1: 80, 1: 160, 1: 320, 1: 60, 1: 1280, 1: 2560 True positive at least 1: 160
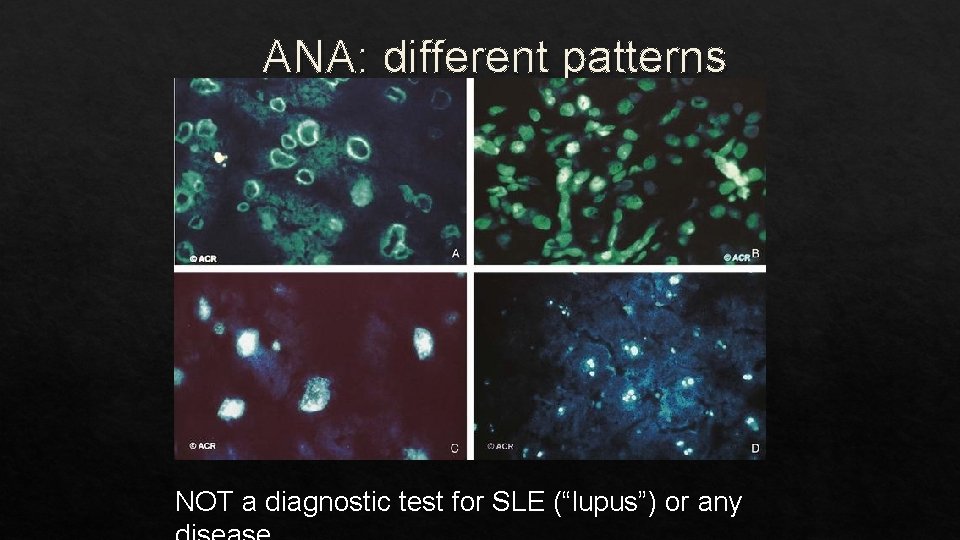
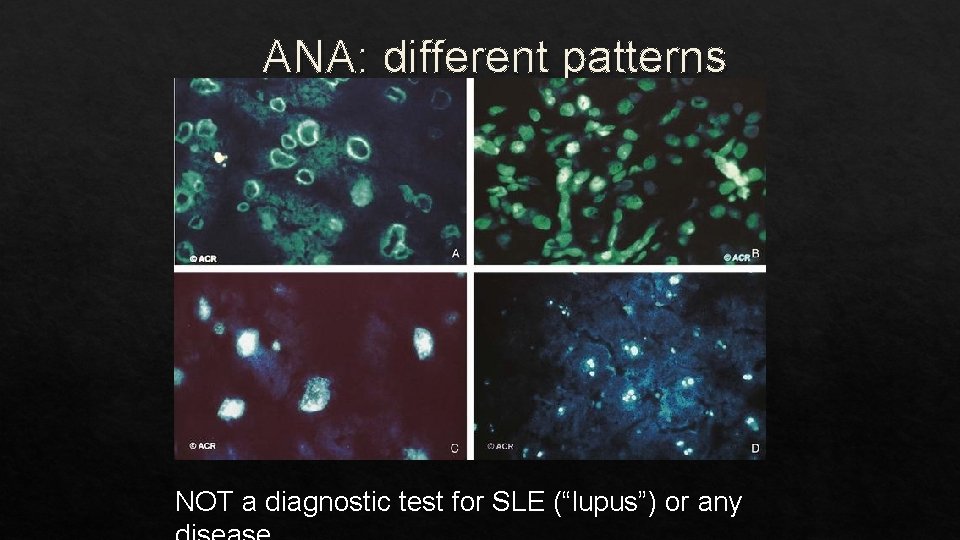
ANA: different patterns NOT a diagnostic test for SLE (“lupus”) or any
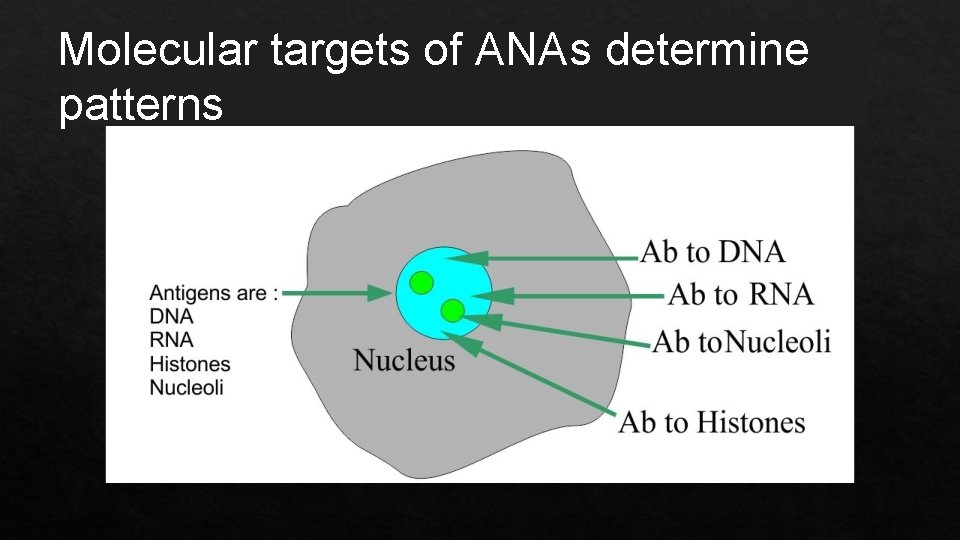
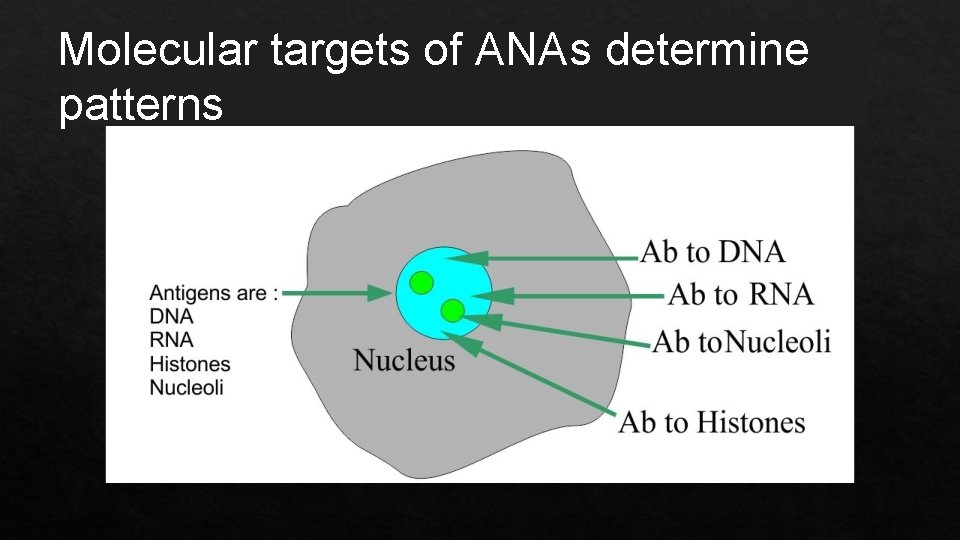
Molecular targets of ANAs determine patterns

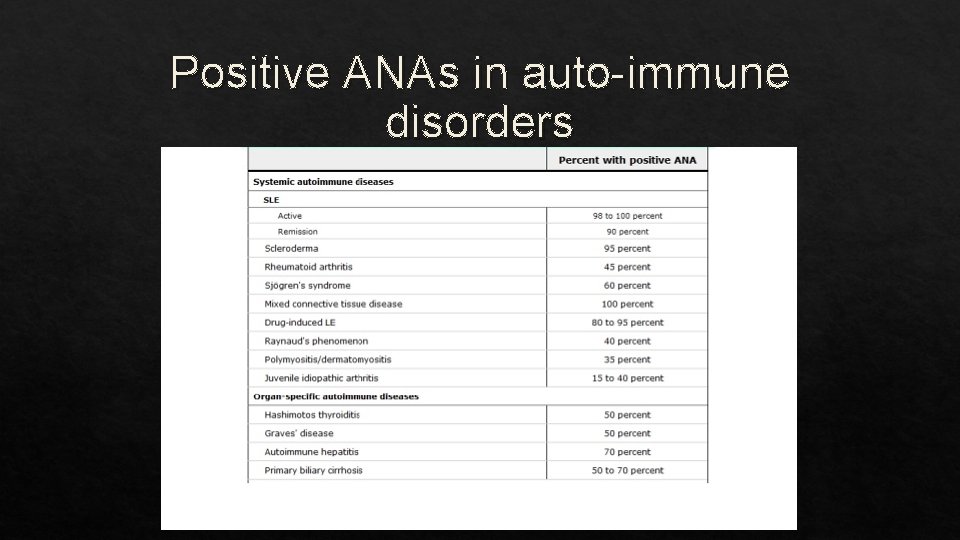
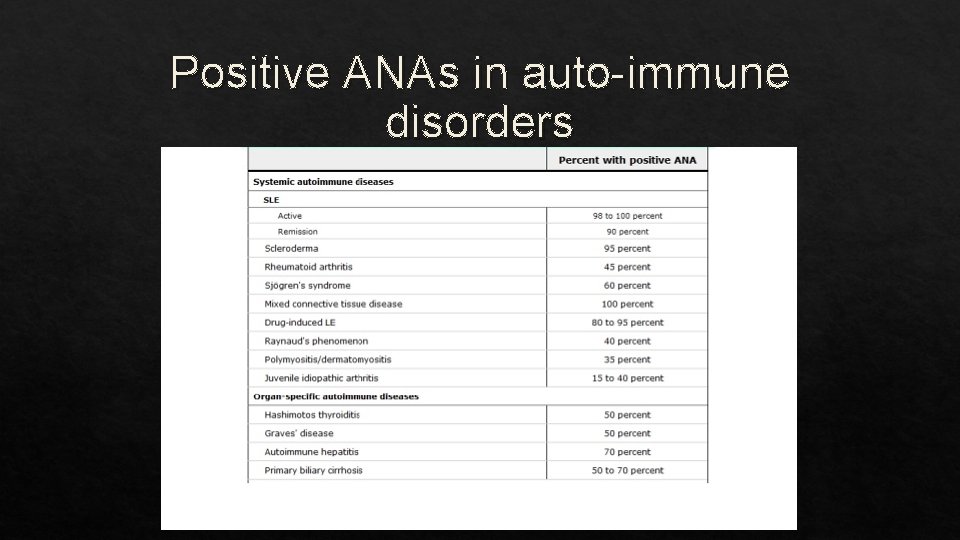
Positive ANAs in auto-immune disorders
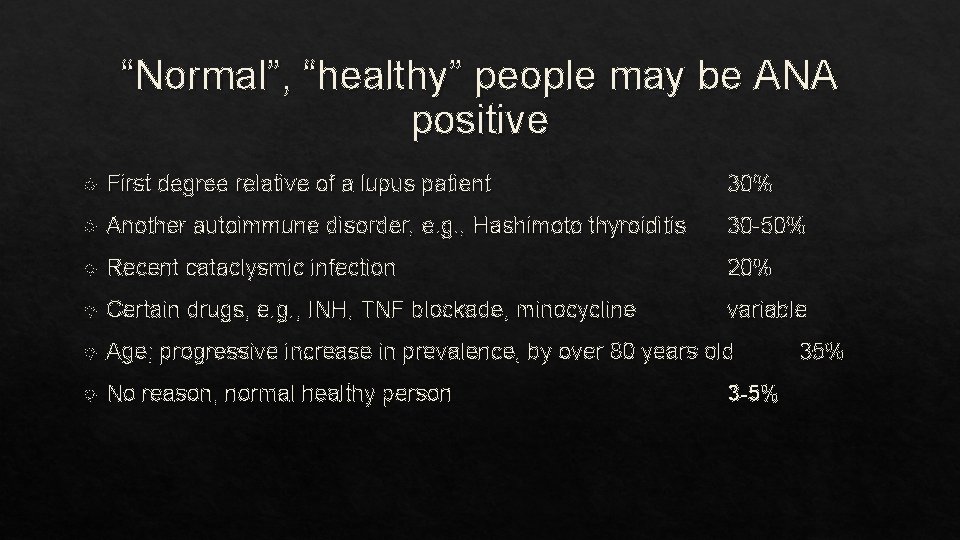
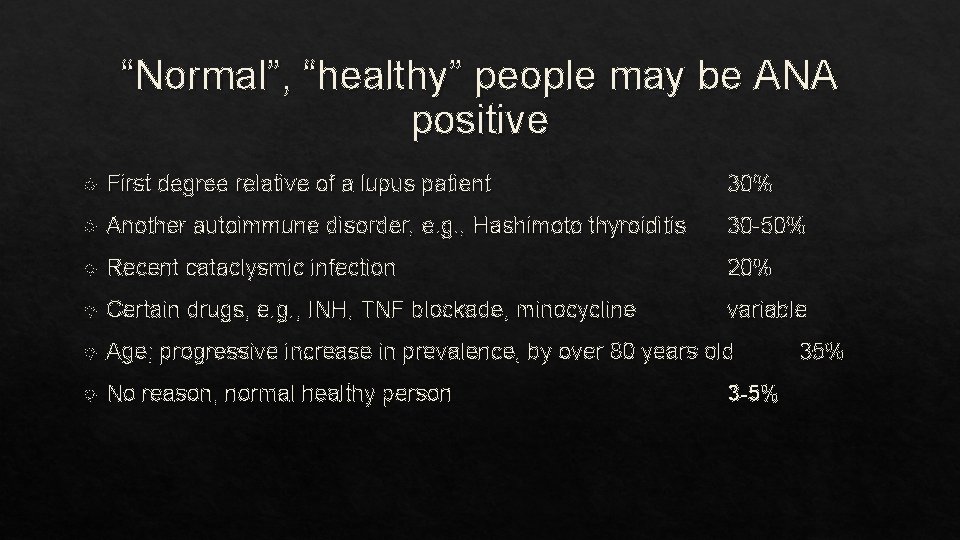
“Normal”, “healthy” people may be ANA positive First degree relative of a lupus patient 30% Another autoimmune disorder, e. g. , Hashimoto thyroiditis 30 -50% Recent cataclysmic infection 20% Certain drugs, e. g. , INH, TNF blockade, minocycline variable Age; progressive increase in prevalence, by over 80 years old No reason, normal healthy person 3 -5% 35%
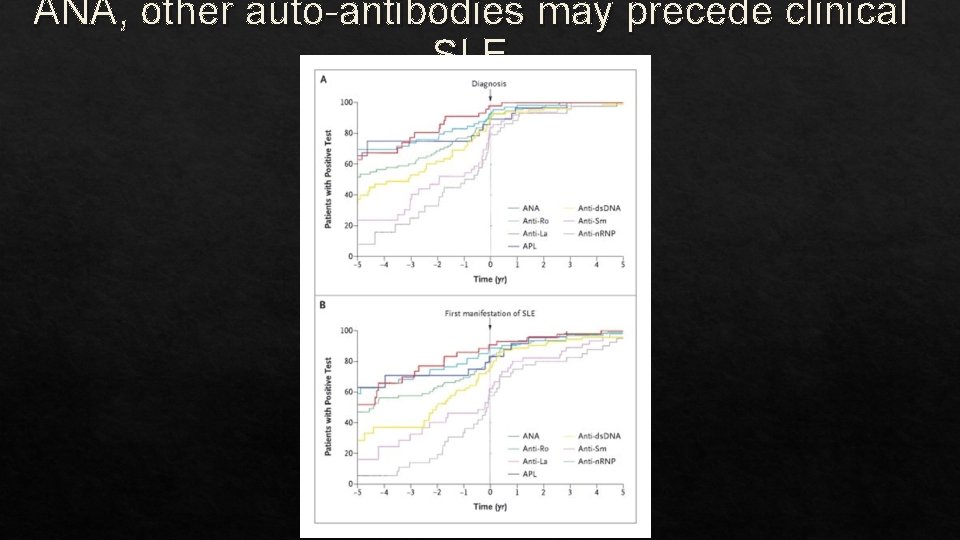
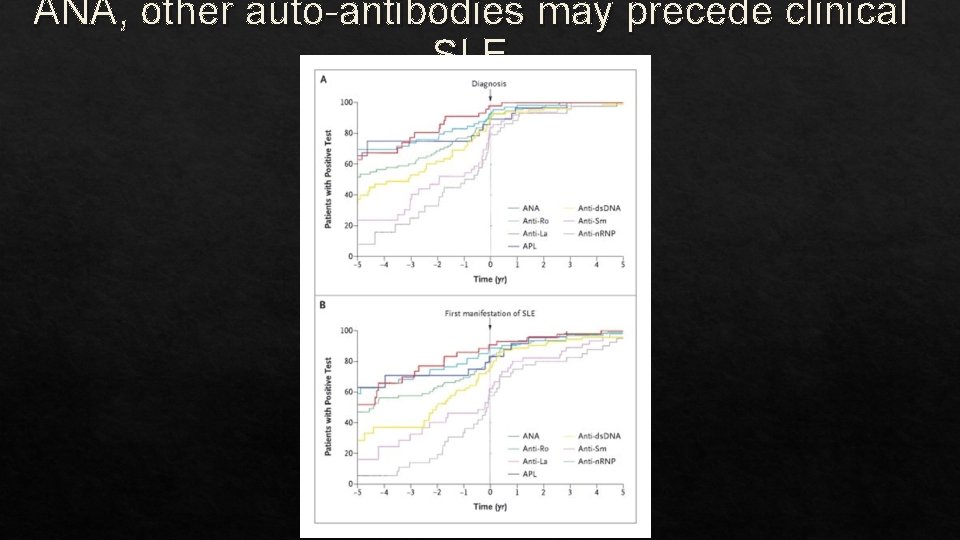
ANA, other auto-antibodies may precede clinical SLE
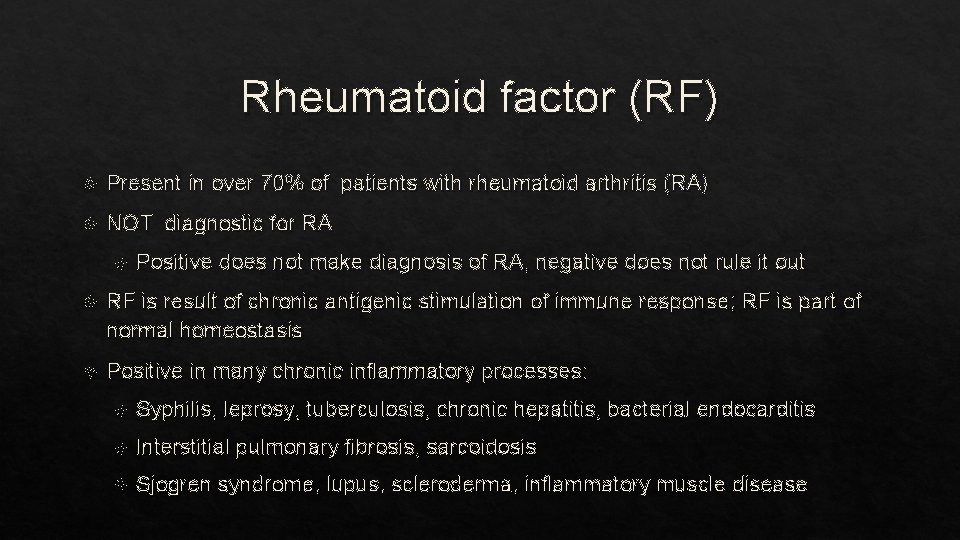
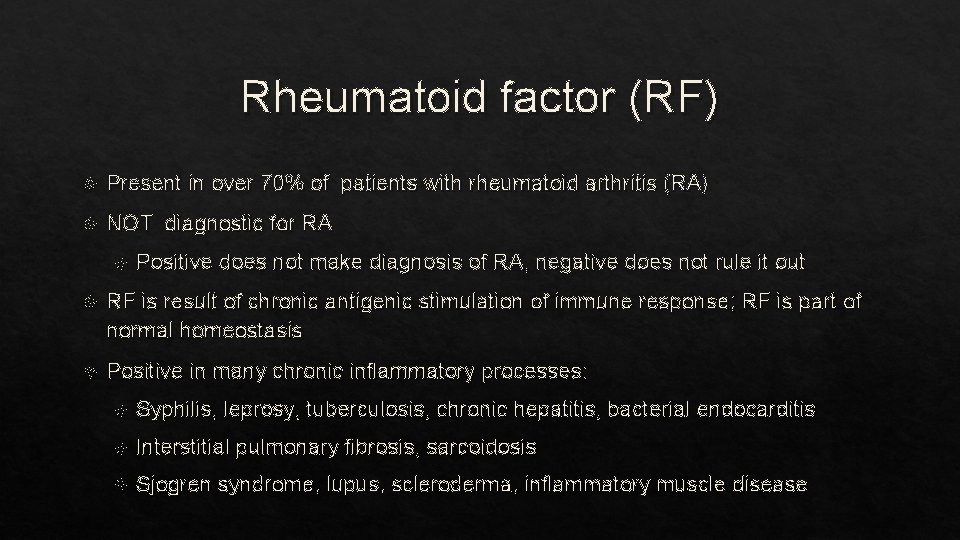
Rheumatoid factor (RF) Present in over 70% of patients with rheumatoid arthritis (RA) NOT diagnostic for RA Positive does not make diagnosis of RA, negative does not rule it out RF is result of chronic antigenic stimulation of immune response; RF is part of normal homeostasis Positive in many chronic inflammatory processes: Syphilis, leprosy, tuberculosis, chronic hepatitis, bacterial endocarditis Interstitial pulmonary fibrosis, sarcoidosis Sjogren syndrome, lupus, scleroderma, inflammatory muscle disease
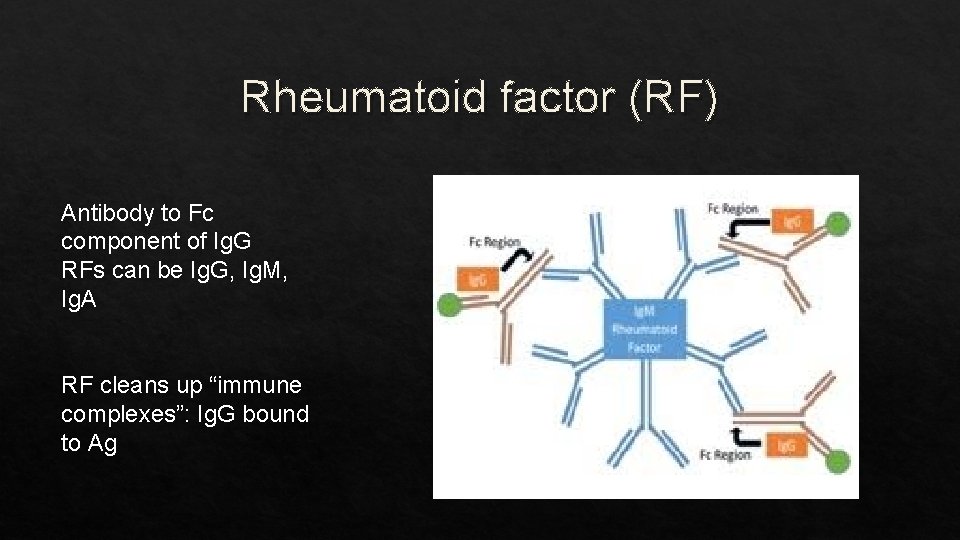
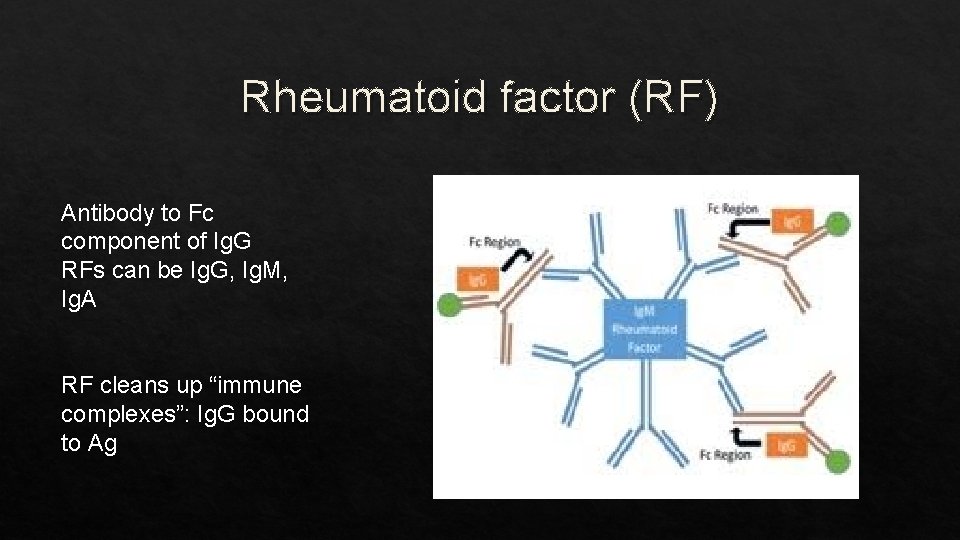
Rheumatoid factor (RF) Antibody to Fc component of Ig. G RFs can be Ig. G, Ig. M, Ig. A RF cleans up “immune complexes”: Ig. G bound to Ag
Anti-CCP antibody (ACPA) Ab to Cyclic Citrullinated Protein (CCP) Amino acid arginine in normal proteins can be modified to citrulline in stressed and dying cells, in certain physiological processes Citrulline not one of the 20 standard amino acid building blocks of protein; thus, something “non-self” target of an immune response ACPA found in 70% of RA patients, but VERY specific for RA (more than RF)
So, ANA, RF and anti-CCP are helpful, but… None is diagnostic If historical/clinical scenario is suggestive, positive test helps make diagnosis If scenario is NOT suggestive, negative test helps rule-out diagnosis History and physical exam are FAR more important in making diagnosis Now, on to non-specific tests suggesting inflammation is present
Non-specific markers of inflammation
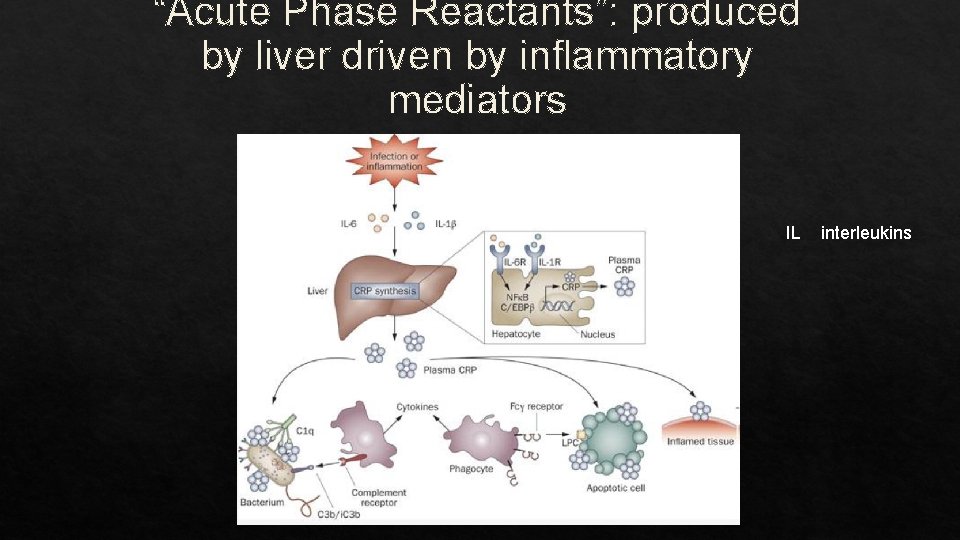
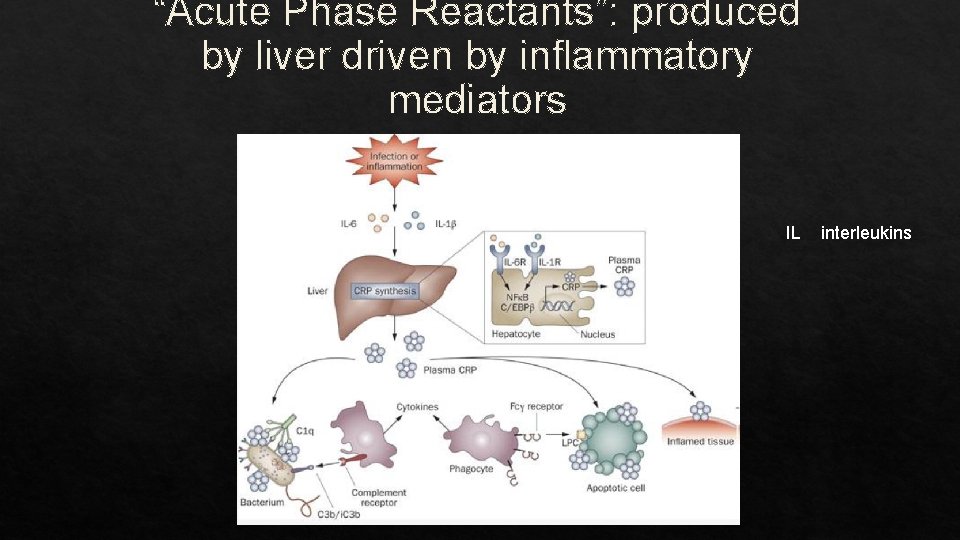
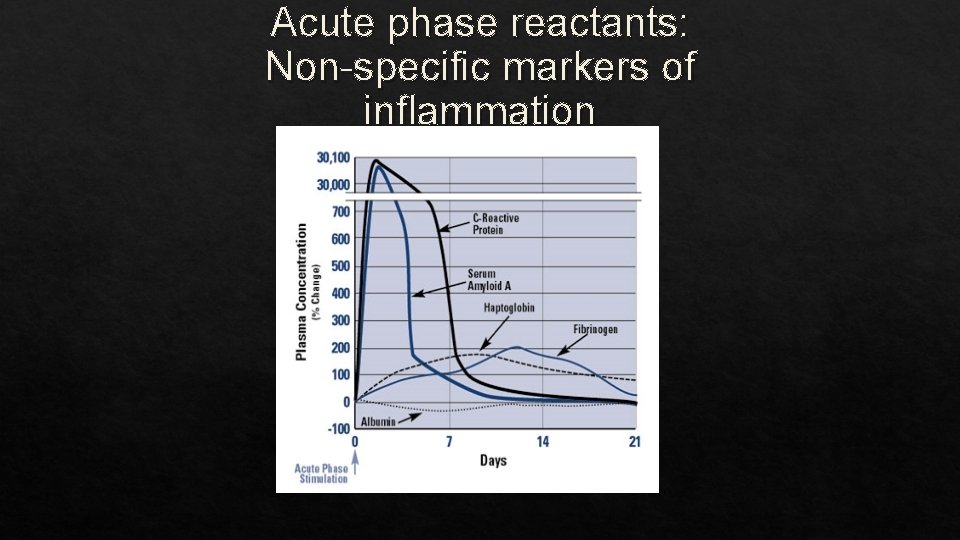
“Acute Phase Reactants”: produced by liver driven by inflammatory mediators IL interleukins
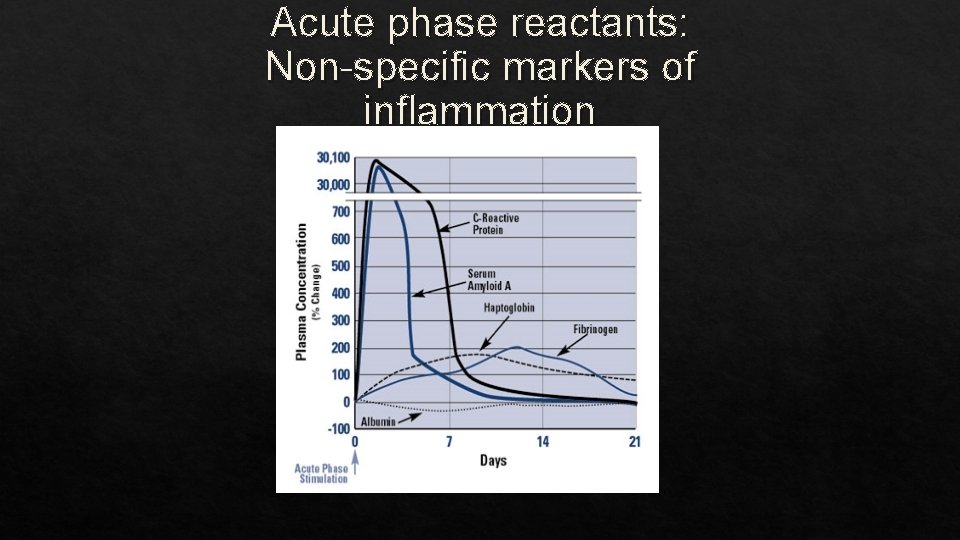
Acute phase reactants: Non-specific markers of inflammation
C-Reactive Protein (CRP) CRP is a “pentraxin”, a pentamer of 115 k. Da subunits penta (5) + ragos (berries) Discovered 1930: serum factor binding C polysaccharide of Pneumococcus Produced by liver cells, also by macrophages & adipocytes Role: bind inner leaflet of cell membrane on necrotic cells activate complement; may clear nuclear debris of dead/dying cells
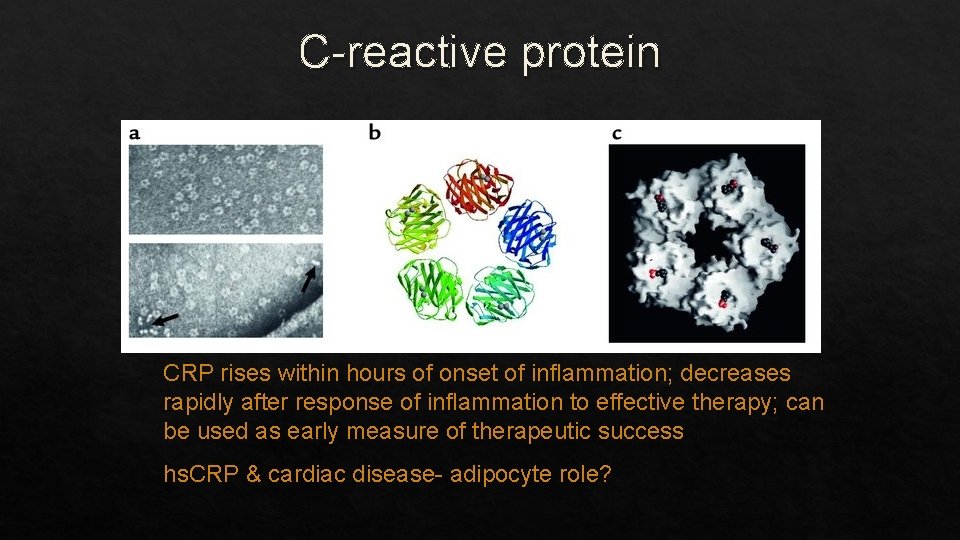
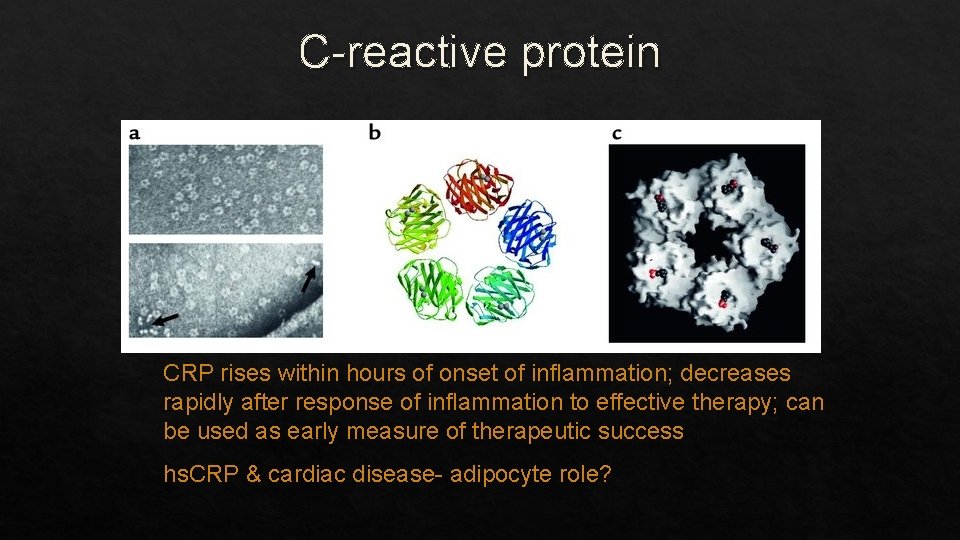
C-reactive protein CRP rises within hours of onset of inflammation; decreases rapidly after response of inflammation to effective therapy; can be used as early measure of therapeutic success hs. CRP & cardiac disease- adipocyte role?
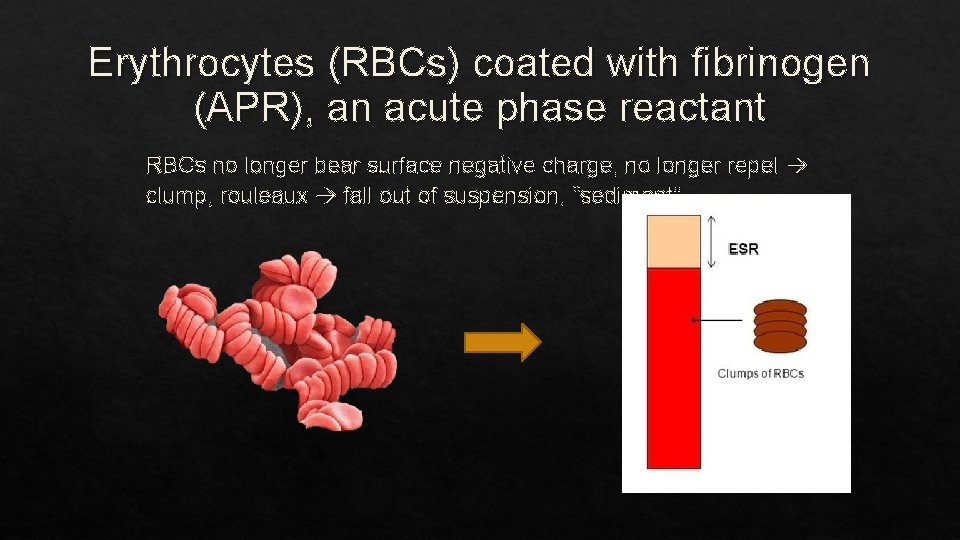
Erythrocyte sedimentation rate- “Sed rate”; ESR RBCs: negative surface charge repel each other Fibrinogen, an acute phase reactant, has a positive charge, coats RBCs, neutralizing their charge Neutral RBC clump, form stacks “rouleaux” and fall out of suspension (“sediment”) Measure rate at top of RBC containing plasma sediments in 1 hr. Rises 1 -3 days after onset of inflammation, after CRP
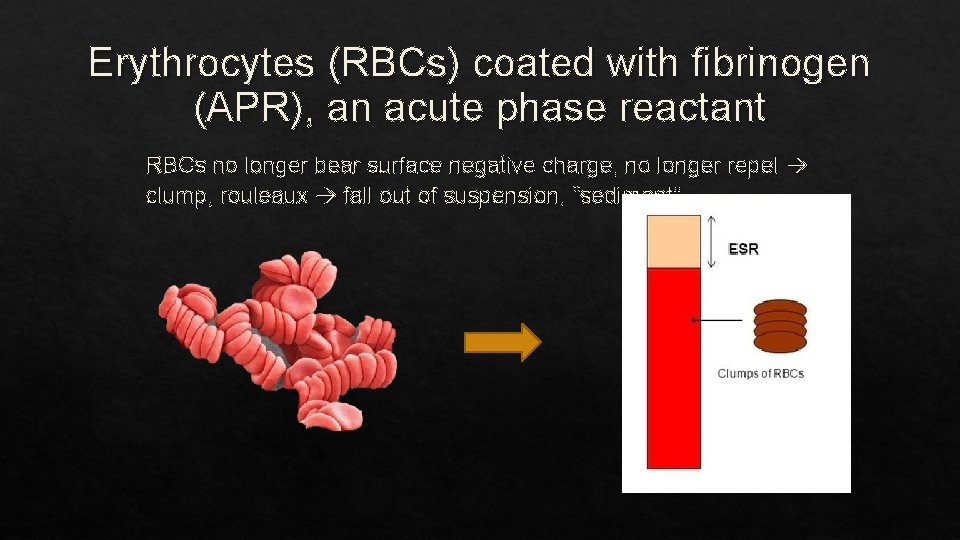
Erythrocytes (RBCs) coated with fibrinogen (APR), an acute phase reactant RBCs no longer bear surface negative charge, no longer repel clump, rouleaux fall out of suspension, “sediment”
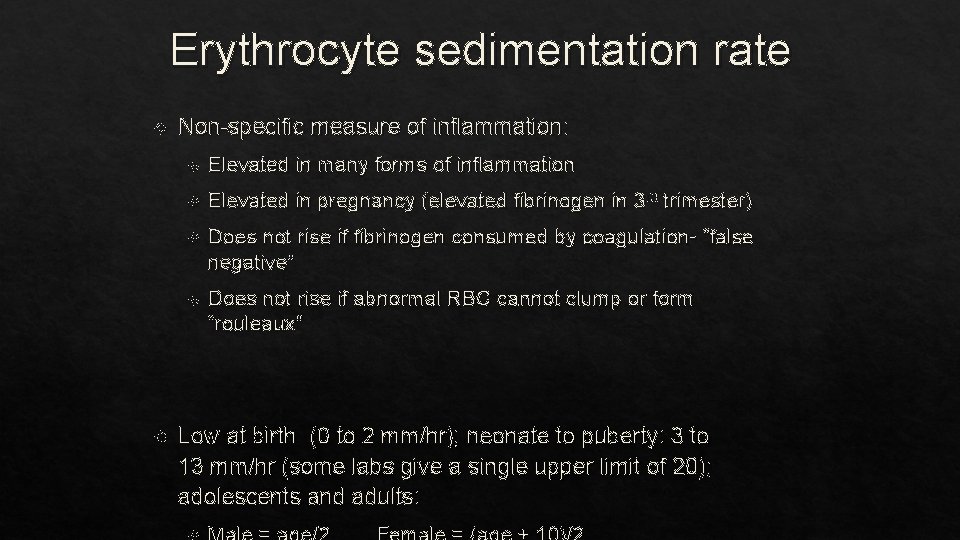
Erythrocyte sedimentation rate Non-specific measure of inflammation: Elevated in many forms of inflammation Elevated in pregnancy (elevated fibrinogen in 3 rd trimester) Does not rise if fibrinogen consumed by coagulation- “false negative” Does not rise if abnormal RBC cannot clump or form “rouleaux” Low at birth (0 to 2 mm/hr); neonate to puberty: 3 to 13 mm/hr (some labs give a single upper limit of 20); adolescents and adults:
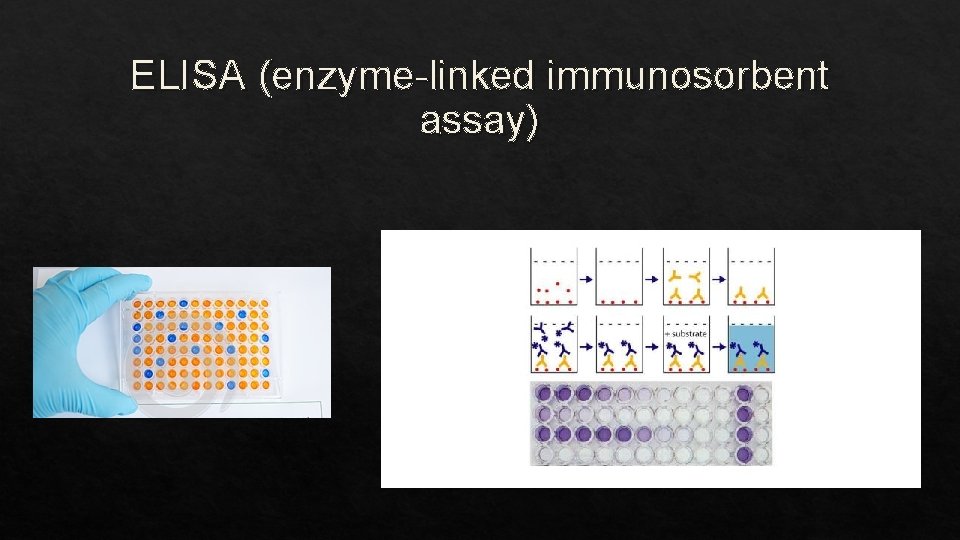
Lyme disease Can measure antibodies specific for Borrelia burgdorferi (and for Anaplasma phagocytophila and for Babesia microti); can also see the latter on blood smear Testing is done in two stage First is ELISA (enzyme-linked immunosorbent assay) followed by Western blot (aka: “immunoblot”)
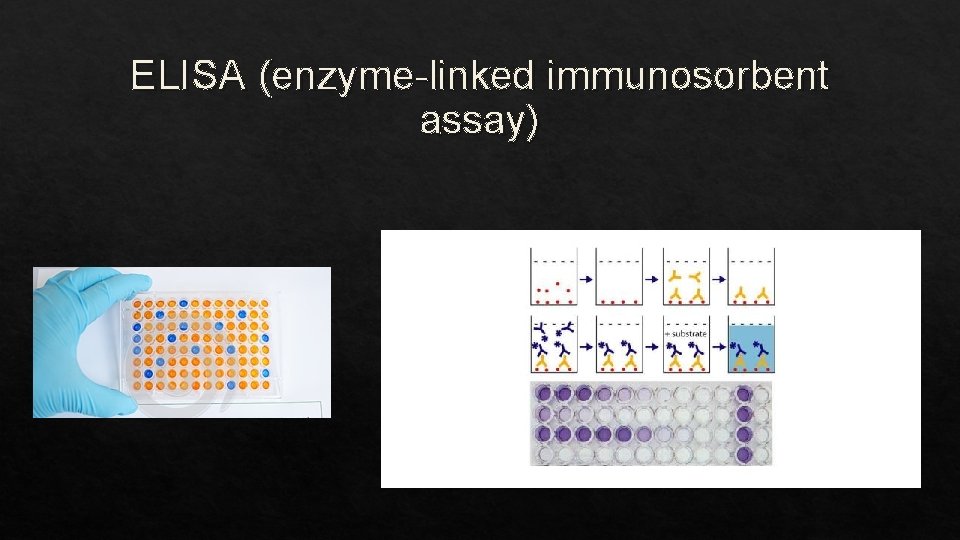
ELISA (enzyme-linked immunosorbent assay)
ELISA Easy to do in large numbers Can be automated Can give “false-positives” Need something more specific
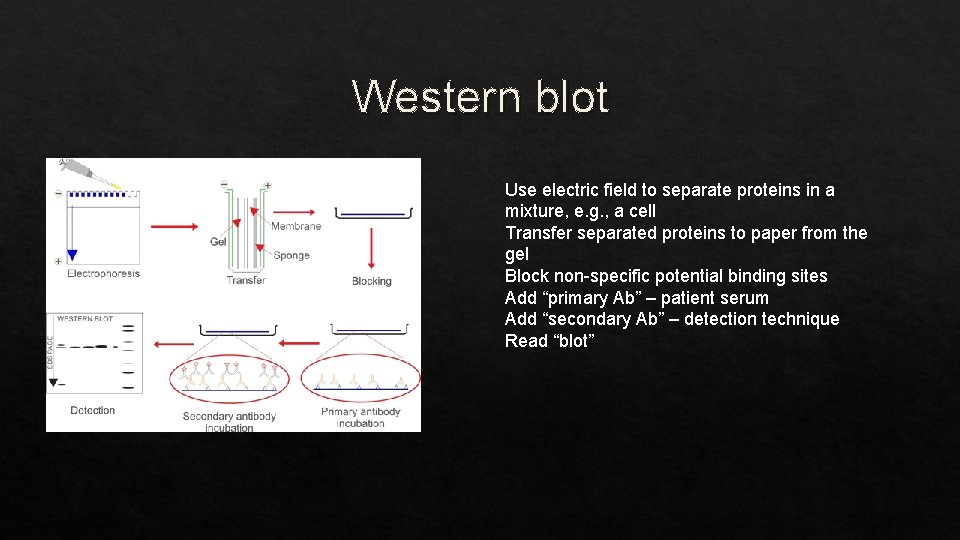
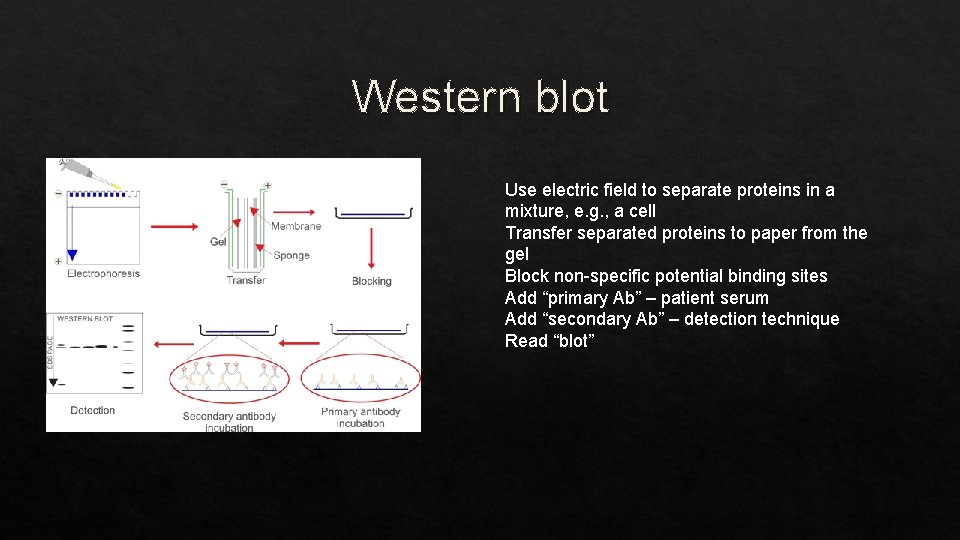
Western blot Use electric field to separate proteins in a mixture, e. g. , a cell Transfer separated proteins to paper from the gel Block non-specific potential binding sites Add “primary Ab” – patient serum Add “secondary Ab” – detection technique Read “blot”
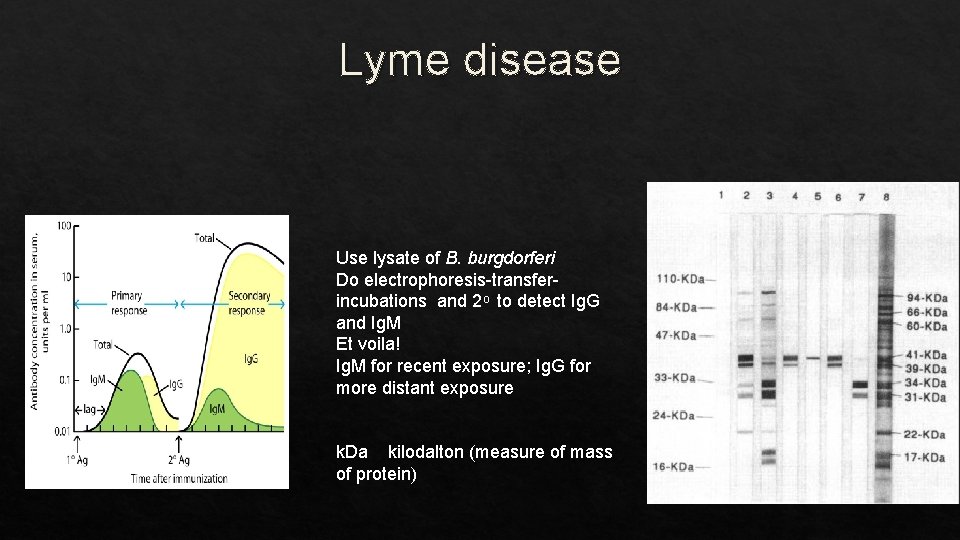
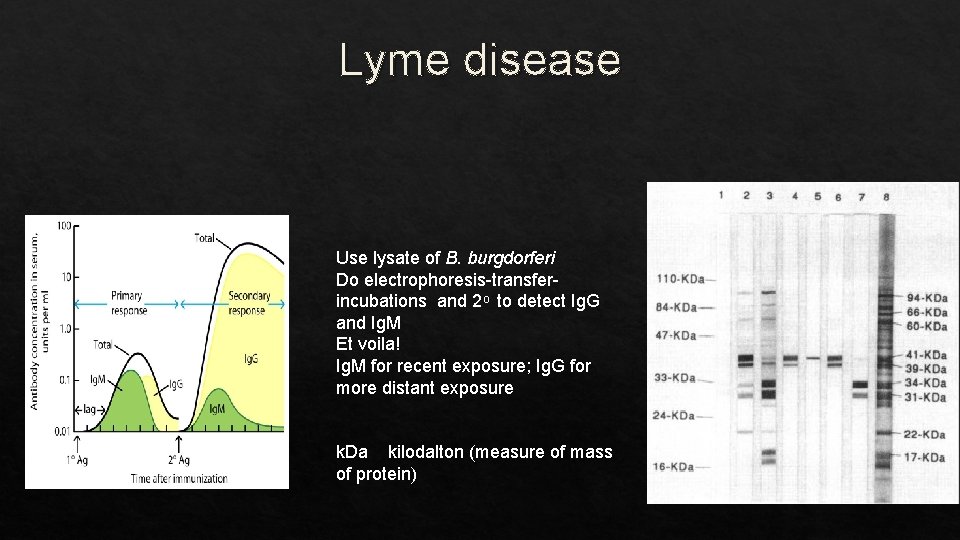
Lyme disease Use lysate of B. burgdorferi Do electrophoresis-transferincubations and 2 to detect Ig. G and Ig. M Et voila! Ig. M for recent exposure; Ig. G for more distant exposure k. Da kilodalton (measure of mass of protein)
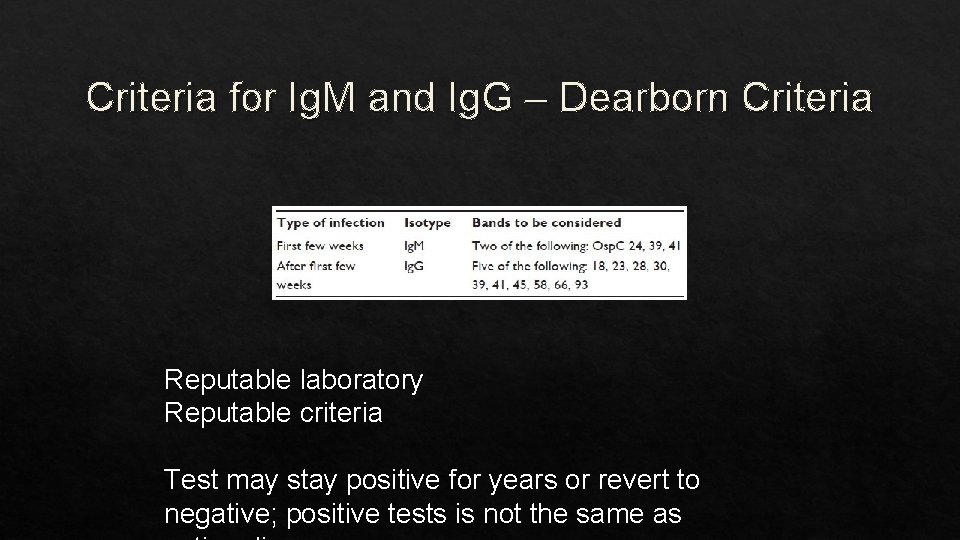
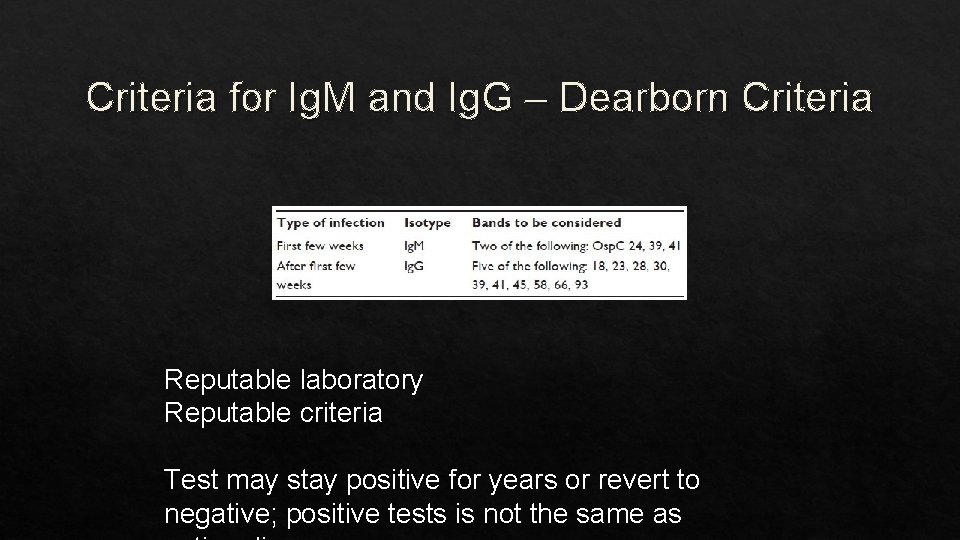
Criteria for Ig. M and Ig. G – Dearborn Criteria Reputable laboratory Reputable criteria Test may stay positive for years or revert to negative; positive tests is not the same as
Thank you for your attention Leonard H Sigal, MD Next session: lensigal@gmail. com
 Aaron tavel
Aaron tavel Sigal hillel
Sigal hillel Nature reviews immunology
Nature reviews immunology Assisting in microbiology and immunology
Assisting in microbiology and immunology Cellular and molecular immunology
Cellular and molecular immunology Fea course
Fea course Pals immunology
Pals immunology Abbas basic immunology
Abbas basic immunology Fraunhofer institute for cell therapy and immunology
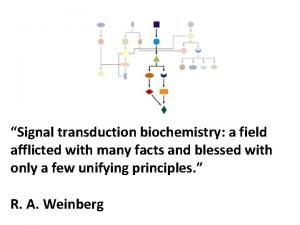
Fraunhofer institute for cell therapy and immunology Molecular immunology ppt
Molecular immunology ppt Nature reviews immunology
Nature reviews immunology Sle criteria 2020
Sle criteria 2020 Guangde tu
Guangde tu Kuby immunology
Kuby immunology Diploma in immunology
Diploma in immunology History of immunology
History of immunology Avidity in immunology
Avidity in immunology Nature reviews immunology
Nature reviews immunology Trends in education
Trends in education Braverman reproductive immunology
Braverman reproductive immunology American academy of allergy asthma and immunology 2018
American academy of allergy asthma and immunology 2018 Tumor immunology
Tumor immunology Pcams immunology
Pcams immunology Lattice formation antigen antibody reaction
Lattice formation antigen antibody reaction Nature reviews immunology
Nature reviews immunology Journal of experimental medicine
Journal of experimental medicine Nature reviews immunology
Nature reviews immunology Cells
Cells Server medical art
Server medical art Leonard web design
Leonard web design