Histopathologic Validation of the Intravascular Ultrasound Diagnosis of







- Slides: 22

Histopathologic Validation of the Intravascular Ultrasound Diagnosis of Calcified Coronary Artery Nodules Akiko Maehara, MD Cardiovascular Research Foundation/Columbia University Medical Center, New York

Akiko Maehara, MD § Contracted Research/Grant Support: § Boston Scientific Corporation § Honoraria: § Volcano Therapeutics, Inc.
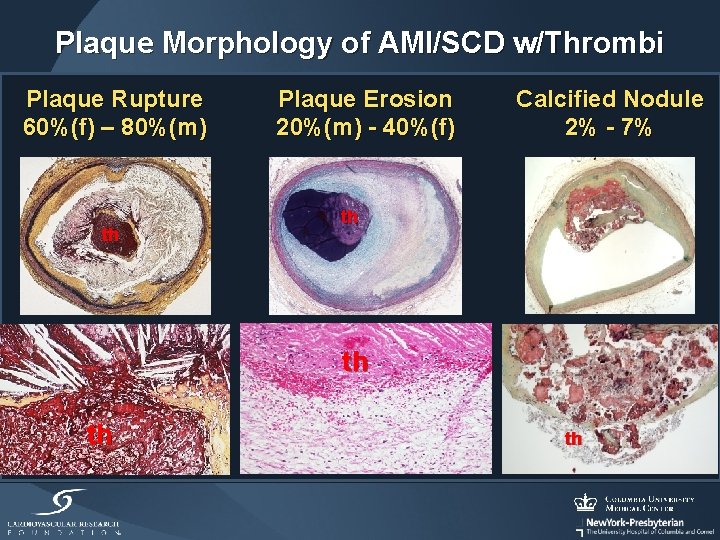
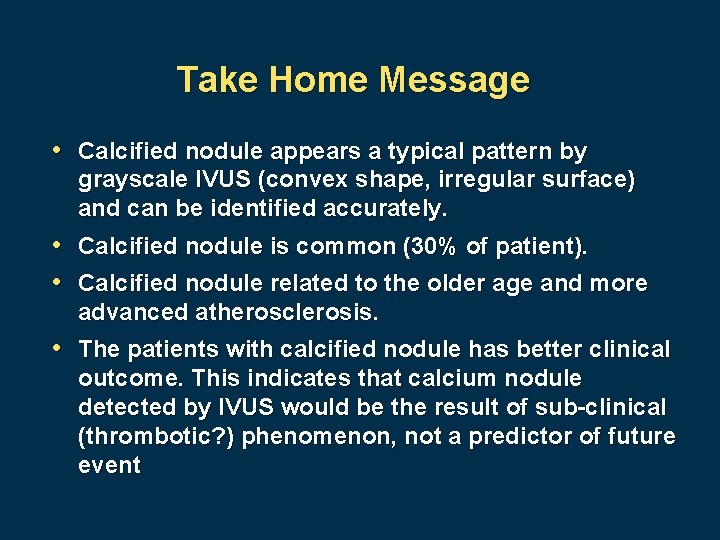
Plaque Morphology of AMI/SCD w/Thrombi Plaque Rupture 60%(f) – 80%(m) th Plaque Erosion 20%(m) - 40%(f) Calcified Nodule 2% - 7% th th
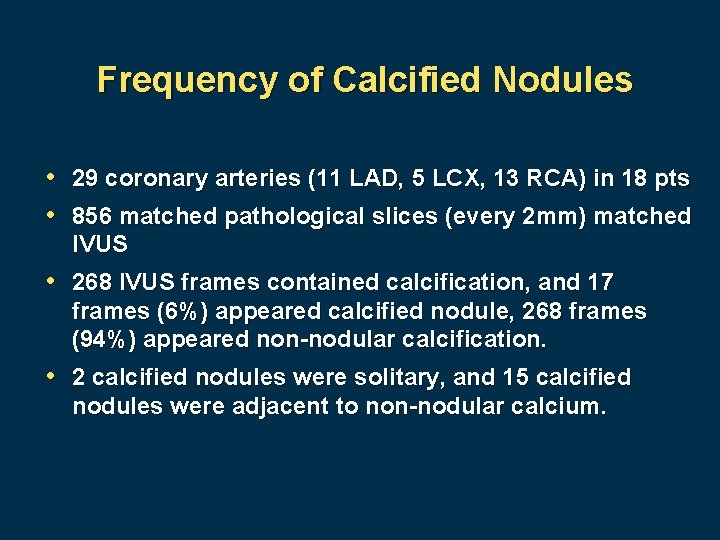
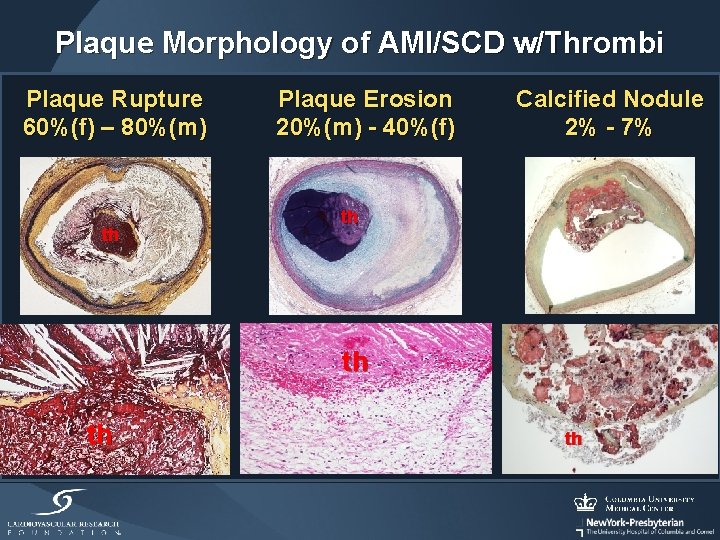
Frequency of Calcified Nodules • 29 coronary arteries (11 LAD, 5 LCX, 13 RCA) in 18 pts • 856 matched pathological slices (every 2 mm) matched IVUS • 268 IVUS frames contained calcification, and 17 frames (6%) appeared calcified nodule, 268 frames (94%) appeared non-nodular calcification. • 2 calcified nodules were solitary, and 15 calcified nodules were adjacent to non-nodular calcium.
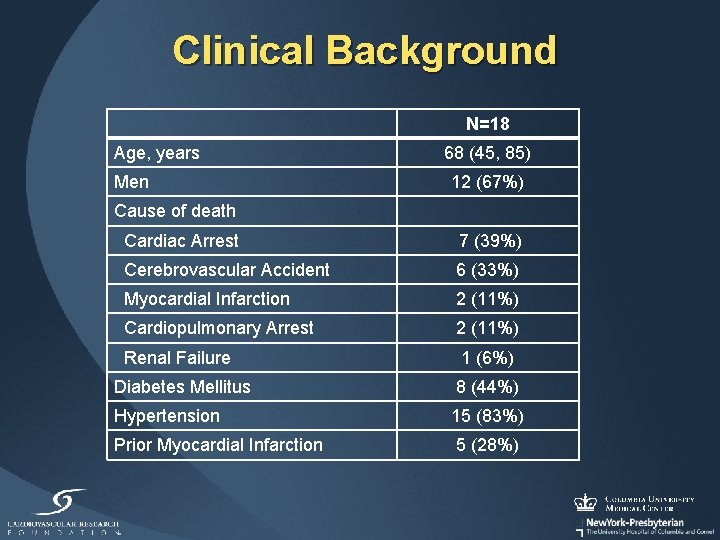
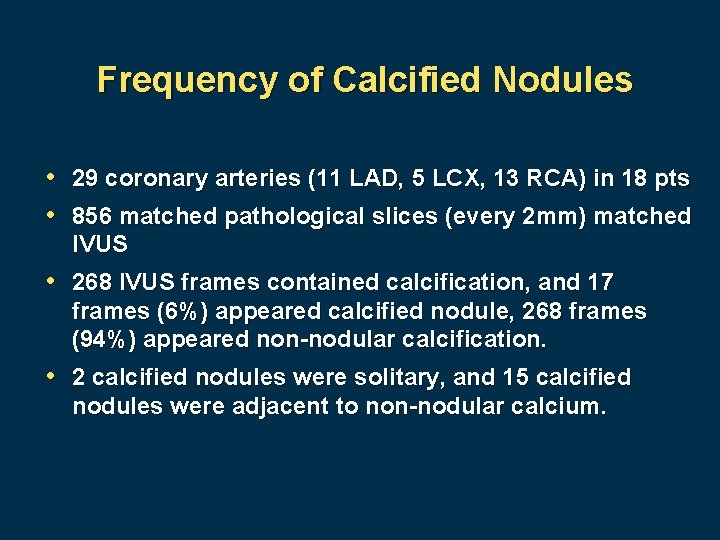
Clinical Background N=18 Age, years Men 68 (45, 85) 12 (67%) Cause of death Cardiac Arrest 7 (39%) Cerebrovascular Accident 6 (33%) Myocardial Infarction 2 (11%) Cardiopulmonary Arrest 2 (11%) Renal Failure 1 (6%) Diabetes Mellitus 8 (44%) Hypertension 15 (83%) Prior Myocardial Infarction 5 (28%)
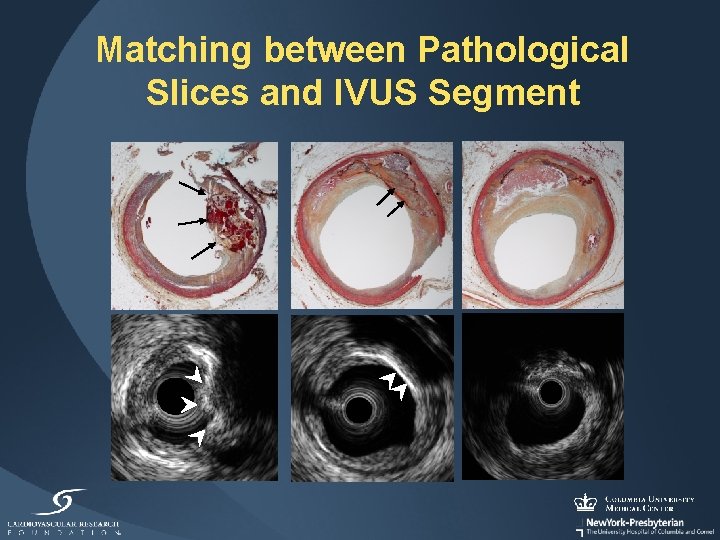
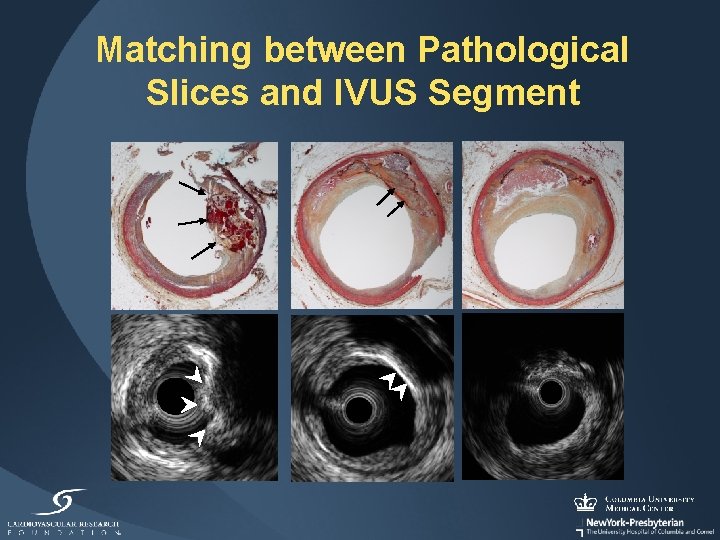
Matching between Pathological Slices and IVUS Segment

IVUS Case Example A B Proximal D C A B D C 1 mm
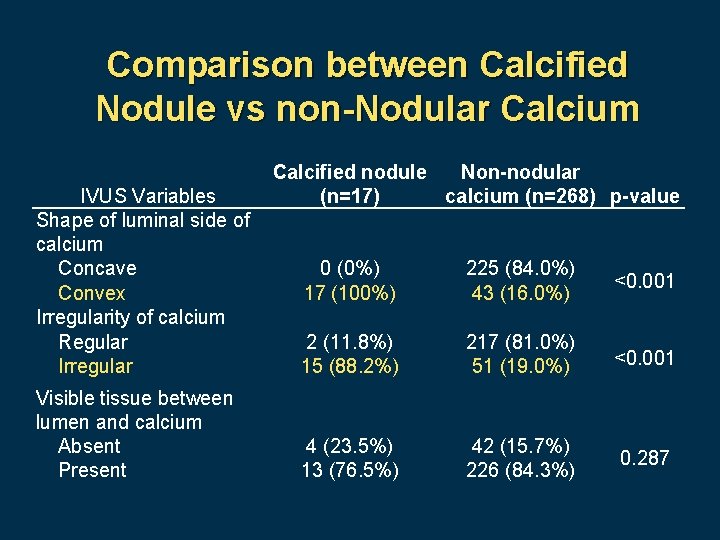
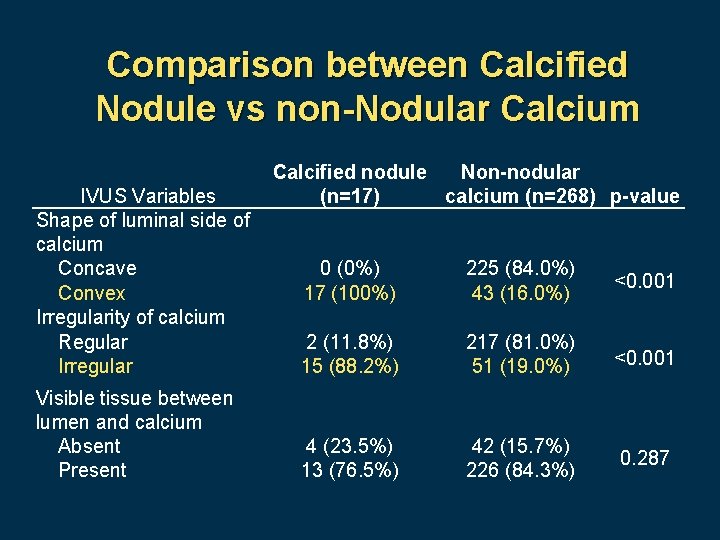
Comparison between Calcified Nodule vs non-Nodular Calcium IVUS Variables Shape of luminal side of calcium Concave Convex Irregularity of calcium Regular Irregular Visible tissue between lumen and calcium Absent Present Calcified nodule Non-nodular (n=17) calcium (n=268) p-value 0 (0%) 17 (100%) 225 (84. 0%) 43 (16. 0%) <0. 001 2 (11. 8%) 15 (88. 2%) 217 (81. 0%) 51 (19. 0%) <0. 001 4 (23. 5%) 13 (76. 5%) 42 (15. 7%) 226 (84. 3%) 0. 287
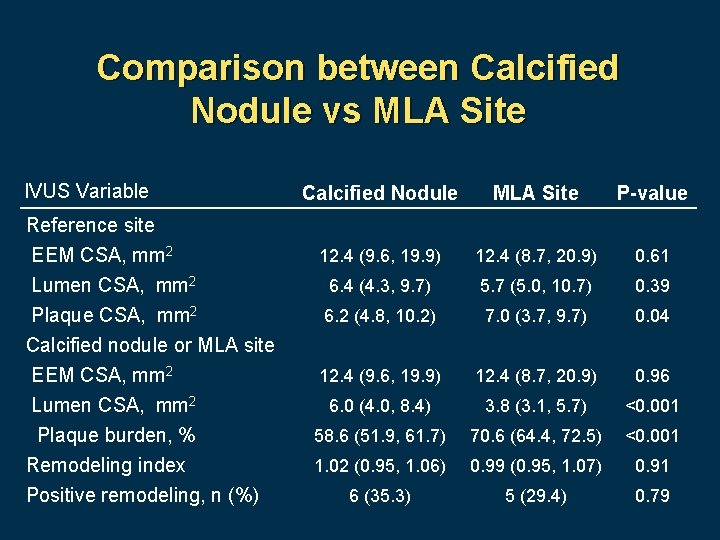
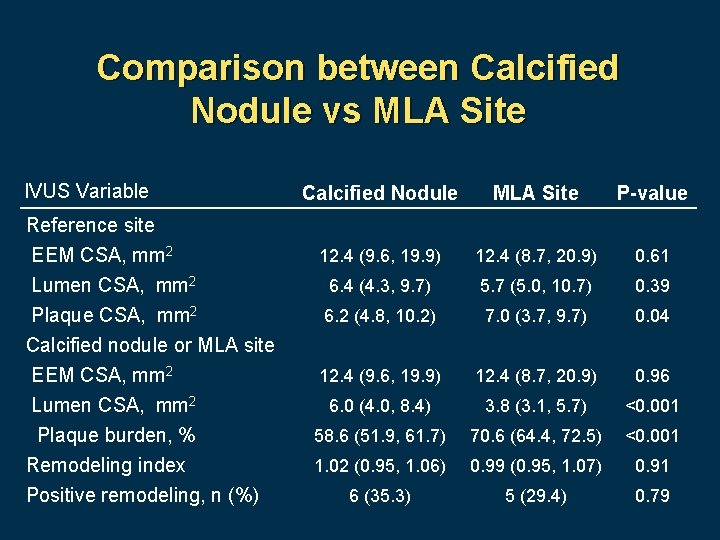
Comparison between Calcified Nodule vs MLA Site IVUS Variable Reference site EEM CSA, mm 2 Lumen CSA, mm 2 Plaque CSA, mm 2 Calcified nodule or MLA site EEM CSA, mm 2 Lumen CSA, mm 2 Plaque burden, % Remodeling index Positive remodeling, n (%) Calcified Nodule MLA Site P-value 12. 4 (9. 6, 19. 9) 12. 4 (8. 7, 20. 9) 0. 61 6. 4 (4. 3, 9. 7) 5. 7 (5. 0, 10. 7) 0. 39 6. 2 (4. 8, 10. 2) 7. 0 (3. 7, 9. 7) 0. 04 12. 4 (9. 6, 19. 9) 12. 4 (8. 7, 20. 9) 0. 96 6. 0 (4. 0, 8. 4) 3. 8 (3. 1, 5. 7) <0. 001 58. 6 (51. 9, 61. 7) 70. 6 (64. 4, 72. 5) <0. 001 1. 02 (0. 95, 1. 06) 0. 99 (0. 95, 1. 07) 0. 91 6 (35. 3) 5 (29. 4) 0. 79
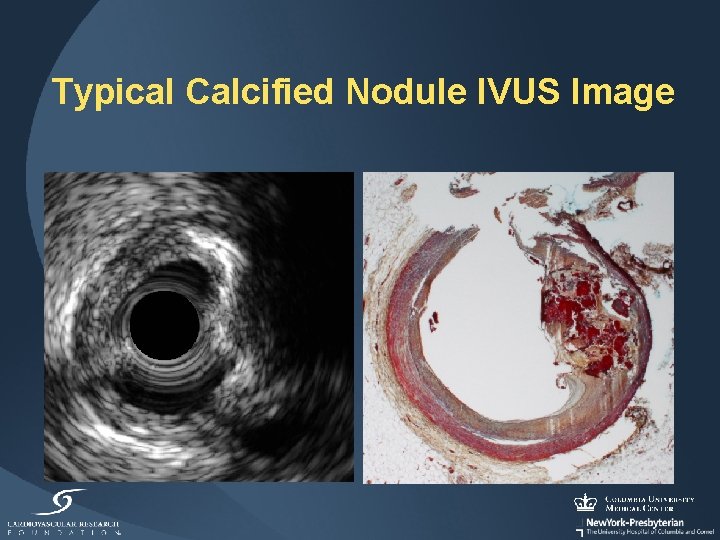
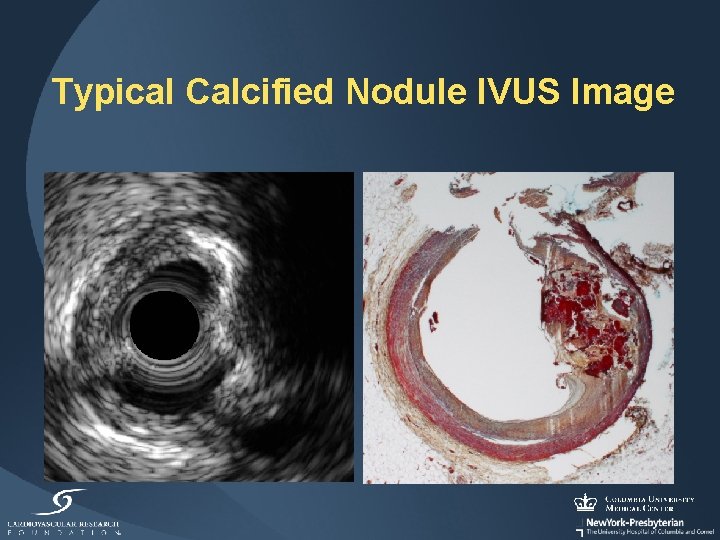
Typical Calcified Nodule IVUS Image

The PROSPECT Trial 700 pts with ACS UA (with ECGΔ) or NSTEMI or STEMI >24º undergoing PCI of 1 or 2 major coronary arteries at up to 40 sites in the U. S. and Europe Metabolic S. • Waist circum • Fast lipids • Fast glu • Hgb. A 1 C • Fast insulin • Creatinine PCI of culprit lesion(s) Successful and uncomplicated Formally enrolled PI: Gregg W. Stone Sponsor: Abbott Vascular; Partner: Volcano Biomarkers • Hs CRP • IL-6 • s. CD 40 L • MPO • TNFα • MMP 9 • Lp-PLA 2 • others

Virtual histology lesion classification Lesions are classified into 5 main types 1. Fibrotic 2. Fibrocalcific 3. Pathological intimal thickening (PIT) 4. Thick cap fibroatheroma (Th. CFA) 5. VH-thin cap fibroatheroma (VH-TCFA)

Frequency of calcified nodules • Among 623 patients with 1573 vessels imaged and qualified for analysis, a total of 314 calcified nodules were detected in 250 arteries in 185 patients. • Thus, the prevalence of at least one calcified nodule was 16% per artery (250 of 1573) and 30% per patient (185 of 623). • Two or more calcified nodules were detected in 48 coronary arteries (3%) in 76 patients (12%).
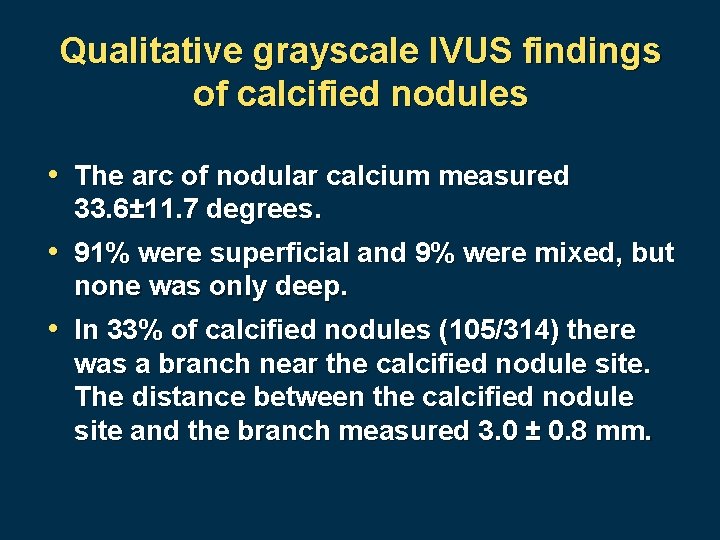
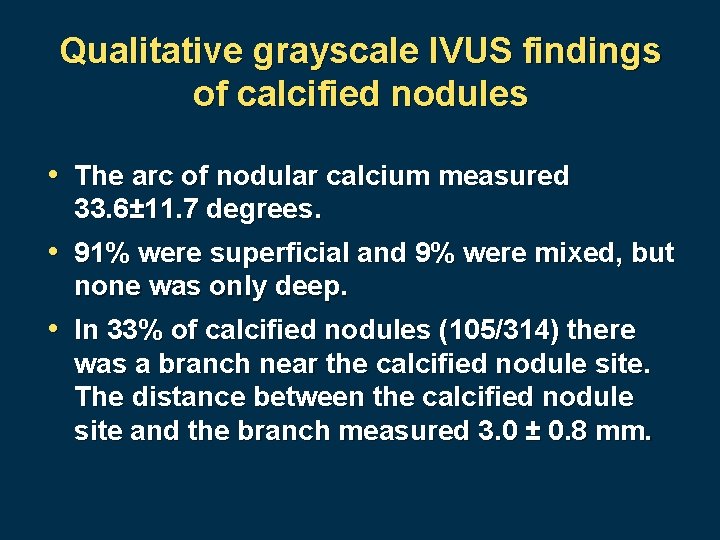
Qualitative grayscale IVUS findings of calcified nodules • The arc of nodular calcium measured 33. 6± 11. 7 degrees. • 91% were superficial and 9% were mixed, but none was only deep. • In 33% of calcified nodules (105/314) there was a branch near the calcified nodule site. The distance between the calcified nodule site and the branch measured 3. 0 ± 0. 8 mm.
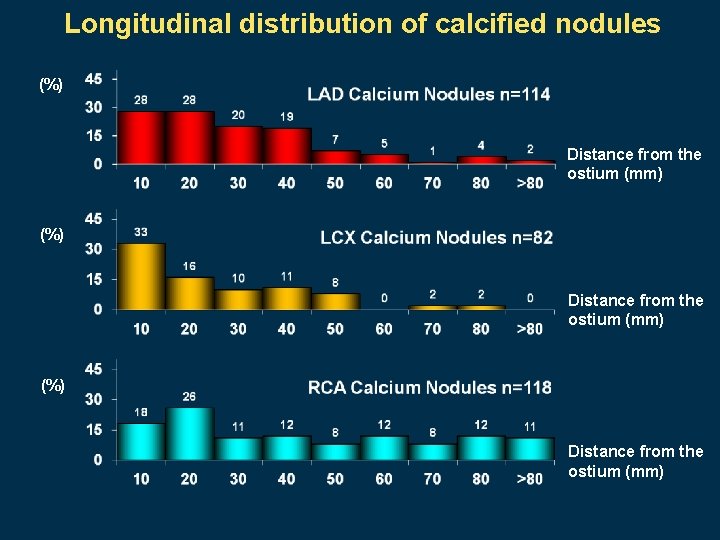
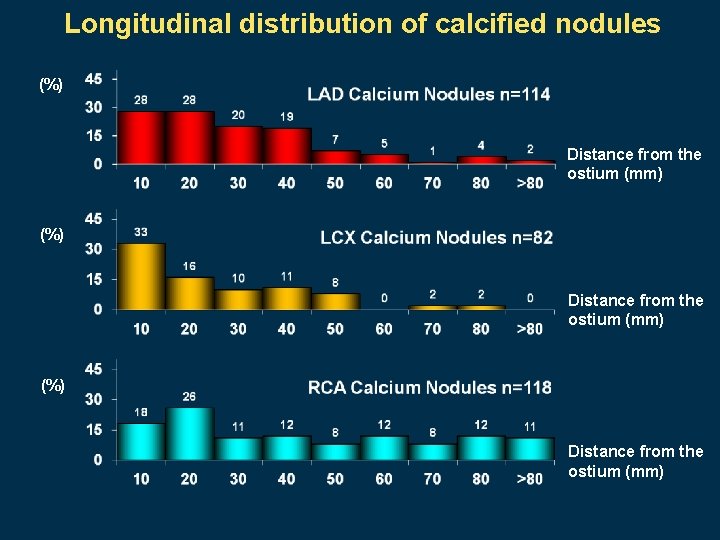
Longitudinal distribution of calcified nodules (%) Distance from the ostium (mm)
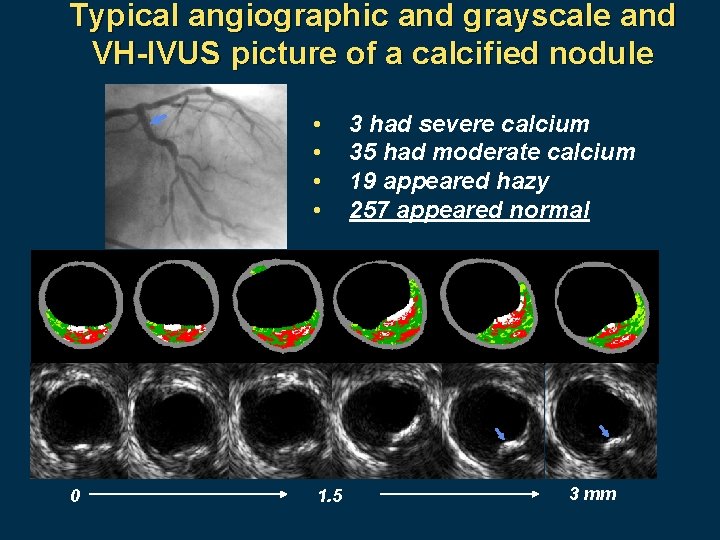
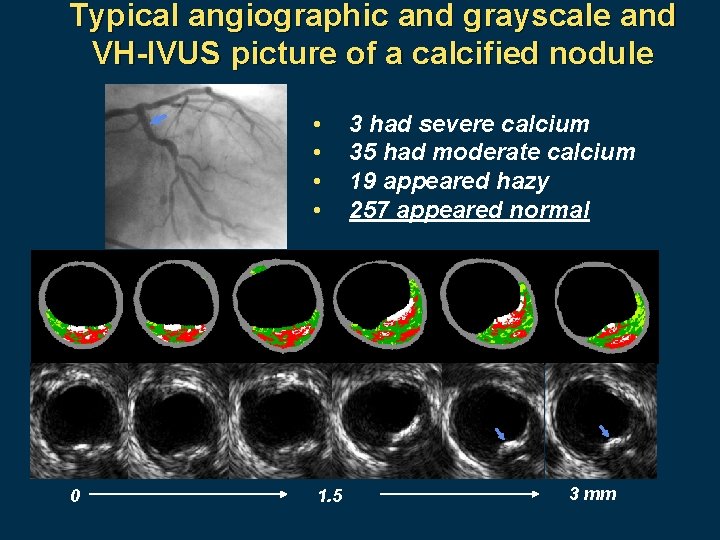
Typical angiographic and grayscale and VH-IVUS picture of a calcified nodule • • 0 1. 5 3 had severe calcium 35 had moderate calcium 19 appeared hazy 257 appeared normal 3 mm

Clinical characteristics of patients with and without calcified nodules Calcified nodule No calcified nodule 185 438 Age, yrs 61. 1 [53. 2, 69. 1] 57. 0 [49. 2, 66. 0] 0. 0003 Male gender 80. 0% (148/185) 75. 8% (332/438) 0. 25 %STEMI >24 hrs 31. 4% (58/185) 29. 5% (129/438) DM 17. 3% (32/185) 16. 7% (73/436) 0. 64 0. 87 Prior PCI 13. 5% (25/185) 8. 9% (39/437) 0. 09 HDL, mg/d. L 38. 8 [37. 0, 51. 0] 38. 6 [33. 0, 45. 0] 0. 02 4. 0 [3. 3, 5. 0] 4. 5 [3. 8, 5. 5] 0. 002 Number of patients TC/HDL-C ratio Patient level analysis P Value
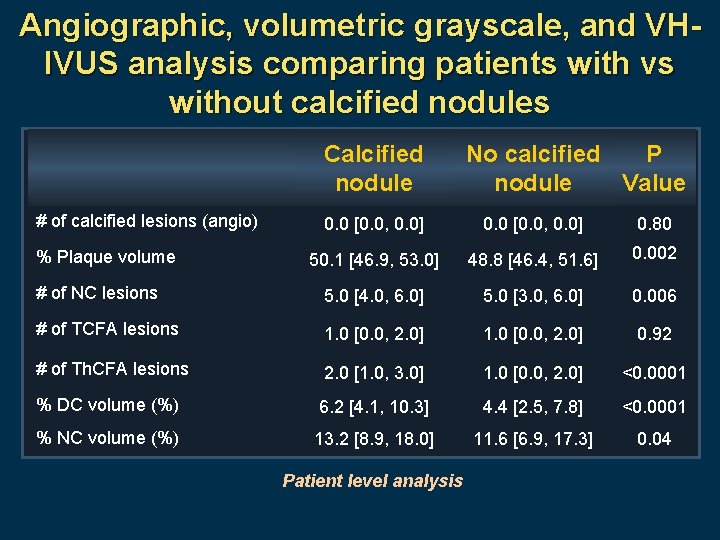
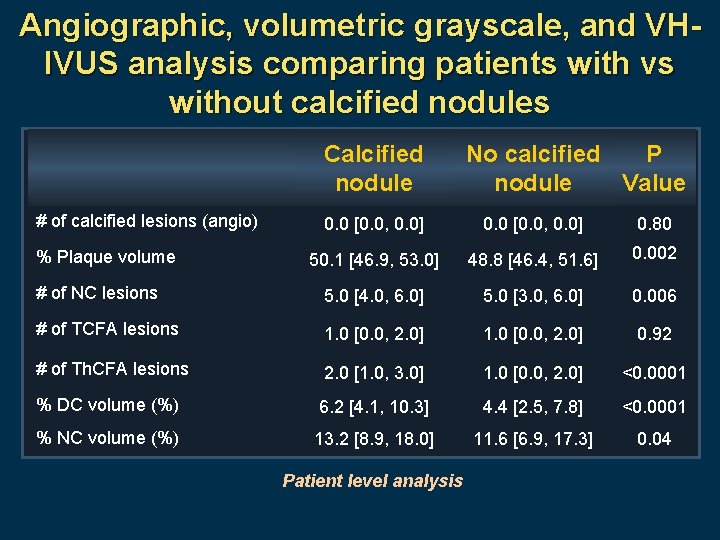
Angiographic, volumetric grayscale, and VHIVUS analysis comparing patients with vs without calcified nodules Calcified nodule # of calcified lesions (angio) No calcified P nodule Value 0. 0 [0. 0, 0. 0] 0. 80 50. 1 [46. 9, 53. 0] 48. 8 [46. 4, 51. 6] 0. 002 # of NC lesions 5. 0 [4. 0, 6. 0] 5. 0 [3. 0, 6. 0] 0. 006 # of TCFA lesions 1. 0 [0. 0, 2. 0] 0. 92 # of Th. CFA lesions 2. 0 [1. 0, 3. 0] 1. 0 [0. 0, 2. 0] <0. 0001 % DC volume (%) 6. 2 [4. 1, 10. 3] 4. 4 [2. 5, 7. 8] <0. 0001 % NC volume (%) 13. 2 [8. 9, 18. 0] 11. 6 [6. 9, 17. 3] 0. 04 % Plaque volume Patient level analysis
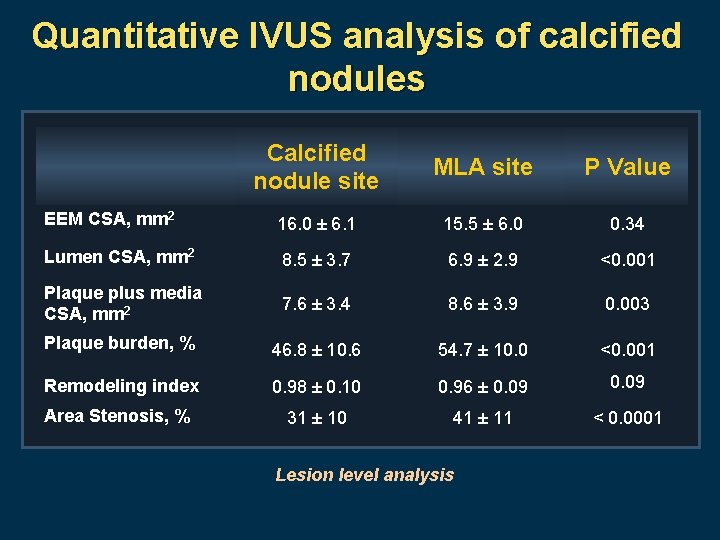
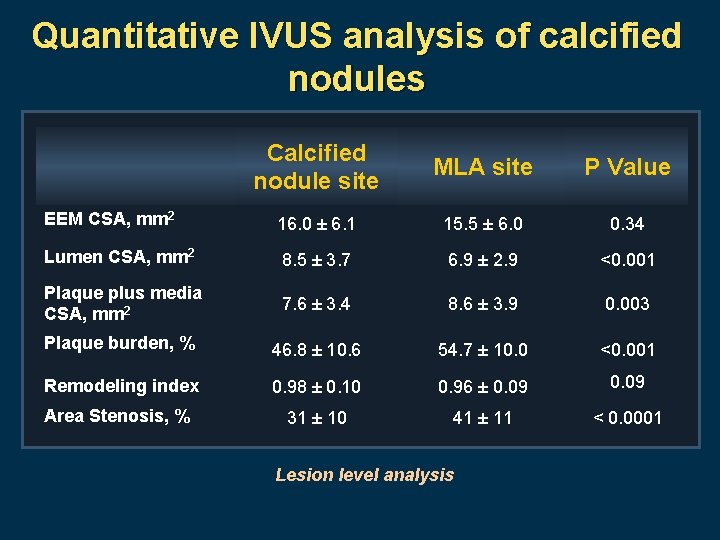
Quantitative IVUS analysis of calcified nodules Calcified nodule site MLA site P Value EEM CSA, mm 2 16. 0 ± 6. 1 15. 5 ± 6. 0 0. 34 Lumen CSA, mm 2 8. 5 ± 3. 7 6. 9 ± 2. 9 <0. 001 Plaque plus media CSA, mm 2 7. 6 ± 3. 4 8. 6 ± 3. 9 0. 003 Plaque burden, % 46. 8 ± 10. 6 54. 7 ± 10. 0 <0. 001 Remodeling index 0. 98 ± 0. 10 0. 96 ± 0. 09 Area Stenosis, % 31 ± 10 41 ± 11 < 0. 0001 Lesion level analysis
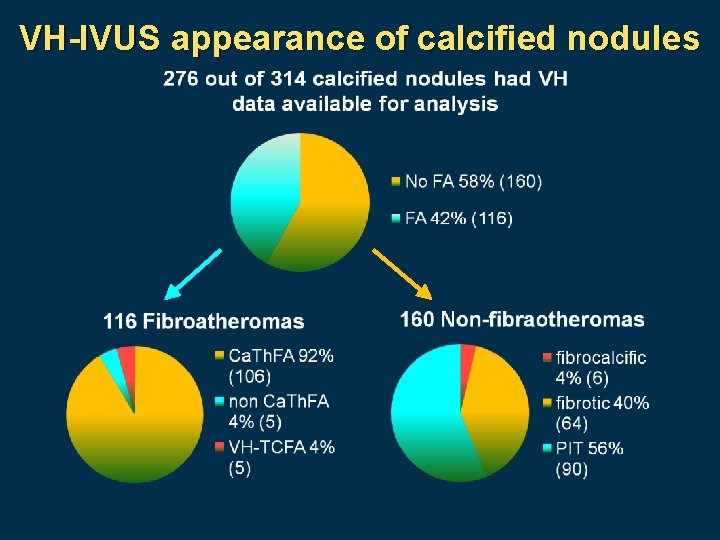
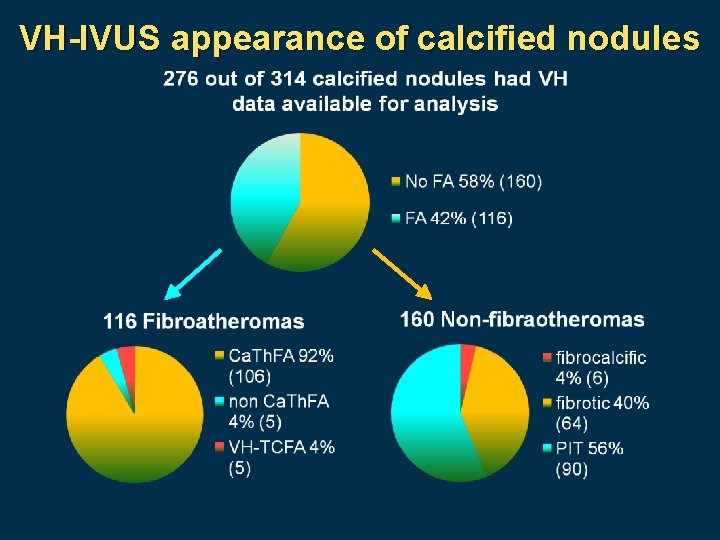
VH-IVUS appearance of calcified nodules
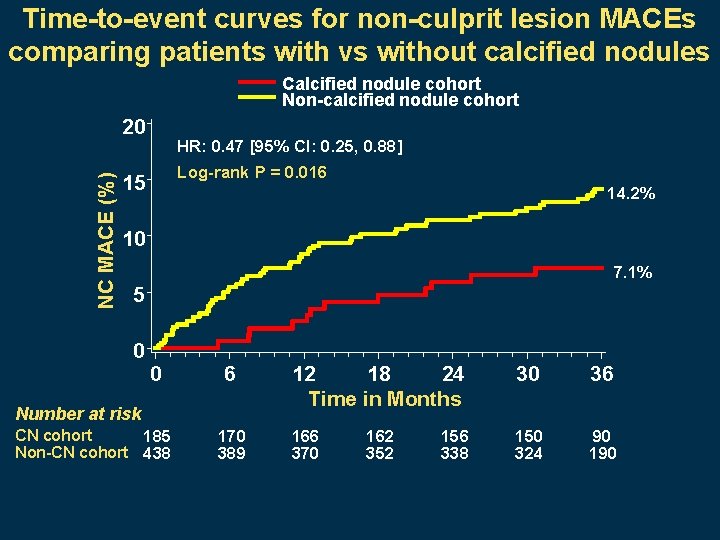
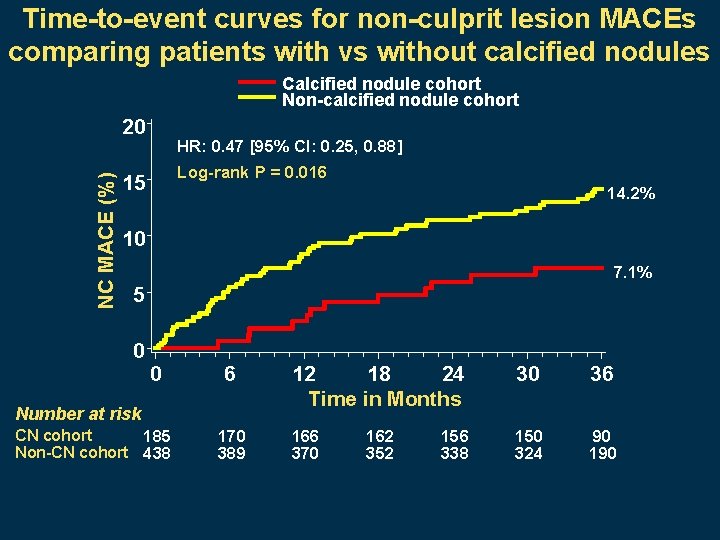
Time-to-event curves for non-culprit lesion MACEs comparing patients with vs without calcified nodules Calcified nodule cohort Non-calcified nodule cohort NC MACE (%) 20 HR: 0. 47 [95% CI: 0. 25, 0. 88] Log-rank P = 0. 016 15 14. 2% 10 7. 1% 5 0 0 6 Number at risk CN cohort 185 Non-CN cohort 438 170 389 12 18 24 Time in Months 30 36 166 370 150 324 90 162 352 156 338
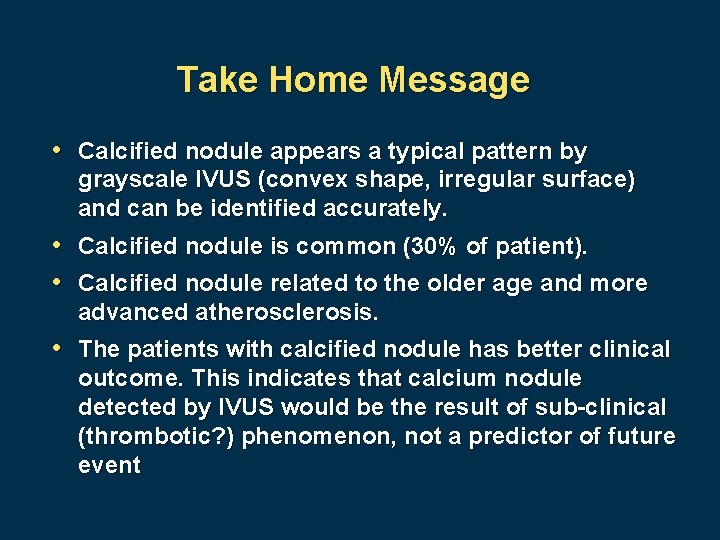
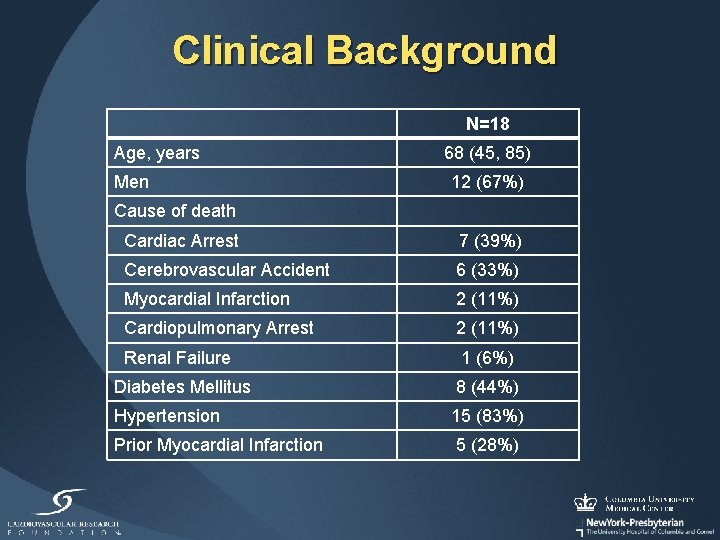
Take Home Message • Calcified nodule appears a typical pattern by grayscale IVUS (convex shape, irregular surface) and can be identified accurately. • Calcified nodule is common (30% of patient). • Calcified nodule related to the older age and more advanced atherosclerosis. • The patients with calcified nodule has better clinical outcome. This indicates that calcium nodule detected by IVUS would be the result of sub-clinical (thrombotic? ) phenomenon, not a predictor of future event
 Intravascular ultrasound
Intravascular ultrasound Intravascular ultrasound
Intravascular ultrasound Score de ferriman
Score de ferriman Liquido intravascular
Liquido intravascular Hus dic
Hus dic Disseminated intravascular coagulation pathophysiology
Disseminated intravascular coagulation pathophysiology Hipernatremia clasificacion
Hipernatremia clasificacion Farmacodin
Farmacodin Disforese
Disforese Liquido intersticial y liquido intravascular
Liquido intersticial y liquido intravascular Intravascular hemolytic anemia
Intravascular hemolytic anemia Liquido intravascular
Liquido intravascular The nursing process
The nursing process Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Nursing diagnosis three parts
Nursing diagnosis three parts Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis How to do self breast examination for cancer
How to do self breast examination for cancer Ultrasound
Ultrasound Pelvic ultrasound
Pelvic ultrasound Walden ultrasound
Walden ultrasound Neurointerventional ultrasound
Neurointerventional ultrasound Ultrasound time gain compensation
Ultrasound time gain compensation