Intravascular ultrasound IVUS to guide percutaneous coronary interventions
- Slides: 1
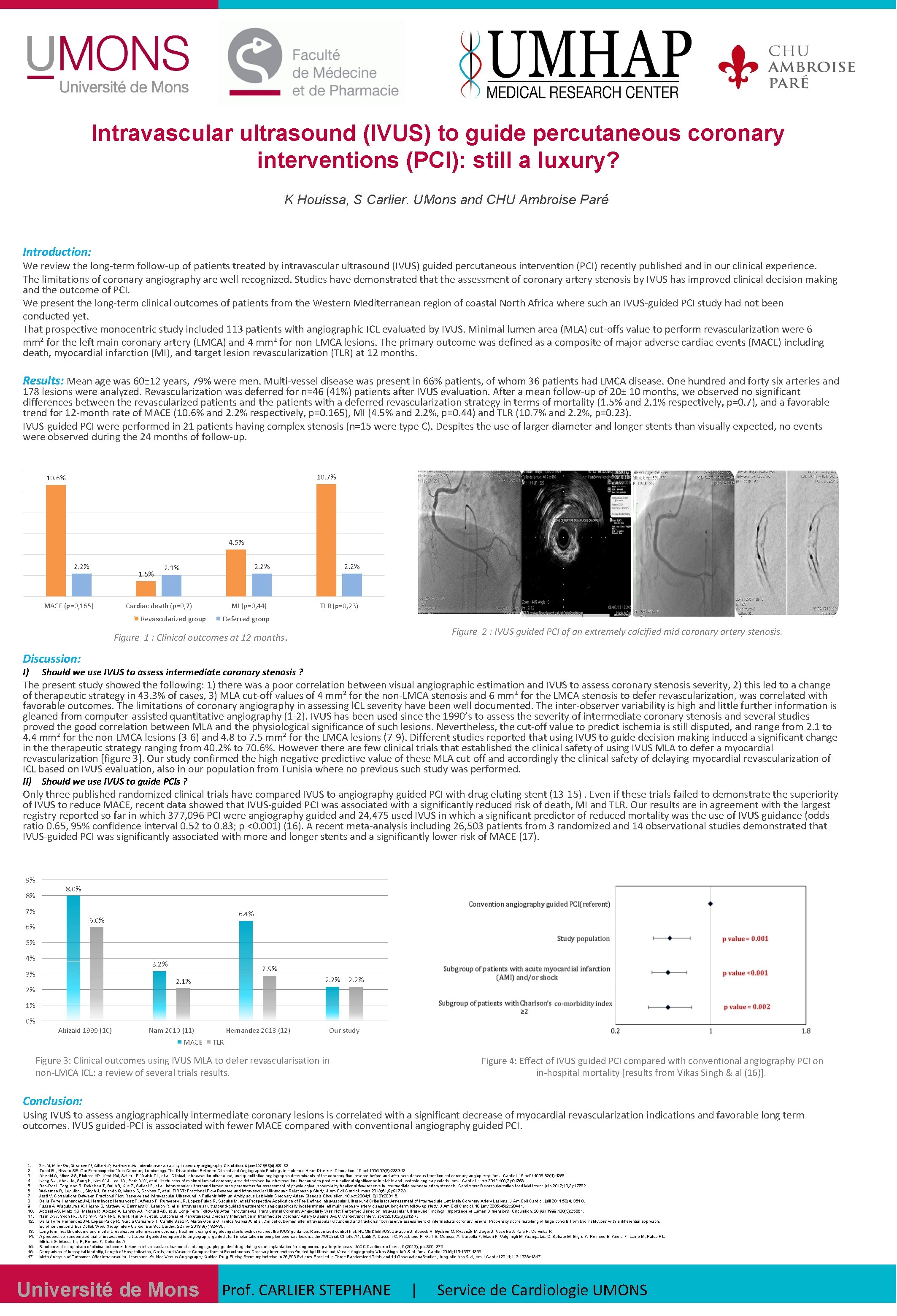
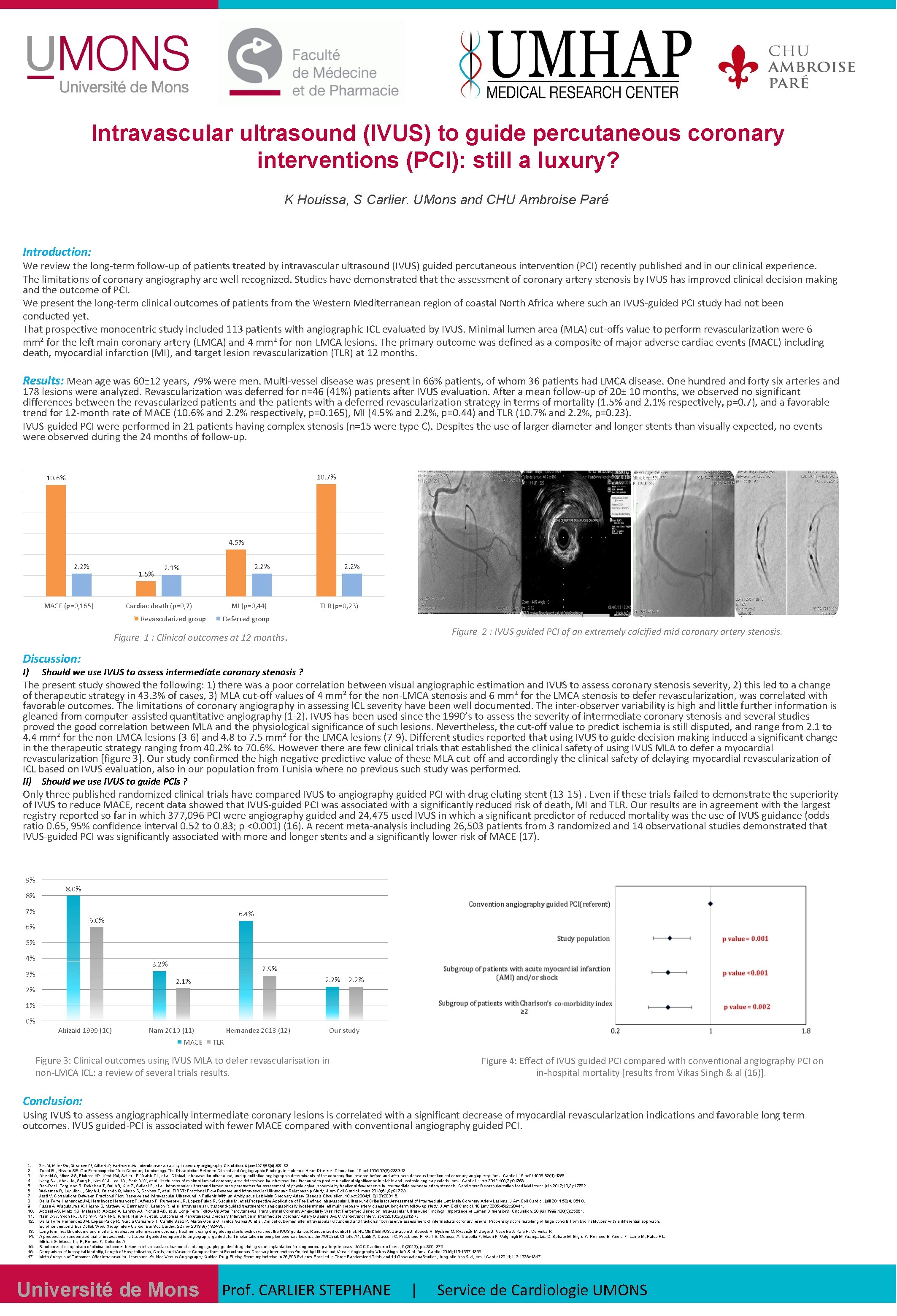
Intravascular ultrasound (IVUS) to guide percutaneous coronary interventions (PCI): still a luxury? K Houissa, S Carlier. UMons and CHU Ambroise Paré Introduction: We review the long-term follow-up of patients treated by intravascular ultrasound (IVUS) guided percutaneous intervention (PCI) recently published and in our clinical experience. The limitations of coronary angiography are well recognized. Studies have demonstrated that the assessment of coronary artery stenosis by IVUS has improved clinical decision making and the outcome of PCI. We present the long-term clinical outcomes of patients from the Western Mediterranean region of coastal North Africa where such an IVUS-guided PCI study had not been conducted yet. That prospective monocentric study included 113 patients with angiographic ICL evaluated by IVUS. Minimal lumen area (MLA) cut-offs value to perform revascularization were 6 mm² for the left main coronary artery (LMCA) and 4 mm² for non-LMCA lesions. The primary outcome was defined as a composite of major adverse cardiac events (MACE) including death, myocardial infarction (MI), and target lesion revascularization (TLR) at 12 months. Results: Mean age was 60± 12 years, 79% were men. Multi-vessel disease was present in 66% patients, of whom 36 patients had LMCA disease. One hundred and forty six arteries and 178 lesions were analyzed. Revascularization was deferred for n=46 (41%) patients after IVUS evaluation. After a mean follow-up of 20± 10 months, we observed no significant differences between the revascularized patients and the patients with a deferred revascularization strategy in terms of mortality (1. 5% and 2. 1% respectively, p=0. 7), and a favorable trend for 12 -month rate of MACE (10. 6% and 2. 2% respectively, p=0. 165), MI (4. 5% and 2. 2%, p=0. 44) and TLR (10. 7% and 2. 2%, p=0. 23). IVUS-guided PCI were performed in 21 patients having complex stenosis (n=15 were type C). Despites the use of larger diameter and longer stents than visually expected, no events were observed during the 24 months of follow-up. 10. 7% 10. 6% 4. 5% 2. 2% 1. 5% MACE (p=0, 165) 2. 2% 2. 1% Cardiac death (p=0, 7) Revascularized group MI (p=0, 44) 2. 2% TLR (p=0, 23) Deferred group Figure 2 : IVUS guided PCI of an extremely calcified mid coronary artery stenosis. Figure 1 : Clinical outcomes at 12 months. Discussion: I) Should we use IVUS to assess intermediate coronary stenosis ? The present study showed the following: 1) there was a poor correlation between visual angiographic estimation and IVUS to assess coronary stenosis severity, 2) this led to a change of therapeutic strategy in 43. 3% of cases, 3) MLA cut-off values of 4 mm² for the non-LMCA stenosis and 6 mm² for the LMCA stenosis to defer revascularization, was correlated with favorable outcomes. The limitations of coronary angiography in assessing l. CL severity have been well documented. The inter-observer variability is high and little further information is gleaned from computer-assisted quantitative angiography (1 -2). IVUS has been used since the 1990’s to assess the severity of intermediate coronary stenosis and several studies proved the good correlation between MLA and the physiological significance of such lesions. Nevertheless, the cut-off value to predict ischemia is still disputed, and range from 2. 1 to 4. 4 mm² for the non-LMCA lesions (3 -6) and 4. 8 to 7. 5 mm² for the LMCA lesions (7 -9). Different studies reported that using IVUS to guide decision making induced a significant change in therapeutic strategy ranging from 40. 2% to 70. 6%. However there are few clinical trials that established the clinical safety of using IVUS MLA to defer a myocardial revascularization [figure 3]. Our study confirmed the high negative predictive value of these MLA cut-off and accordingly the clinical safety of delaying myocardial revascularization of ICL based on IVUS evaluation, also in our population from Tunisia where no previous such study was performed. II) Should we use IVUS to guide PCIs ? Only three published randomized clinical trials have compared IVUS to angiography guided PCI with drug eluting stent (13 -15). Even if these trials failed to demonstrate the superiority of IVUS to reduce MACE, recent data showed that IVUS-guided PCI was associated with a significantly reduced risk of death, MI and TLR. Our results are in agreement with the largest registry reported so far in which 377, 096 PCI were angiography guided and 24, 475 used IVUS in which a significant predictor of reduced mortality was the use of IVUS guidance (odds ratio 0. 65, 95% confidence interval 0. 52 to 0. 83; p <0. 001) (16). A recent meta-analysis including 26, 503 patients from 3 randomized and 14 observational studies demonstrated that IVUS-guided PCI was significantly associated with more and longer stents and a significantly lower risk of MACE (17). 9% 8% 8. 0% 7% 6. 4% 6. 0% 6% 5% 4% 3. 2% 3% 2. 9% 2. 2% 2. 1% 2% 2. 2% 1% 0% Abizaid 1999 (10) Nam 2010 (11) MACE Hernandez 2013 (12) Our study TLR Figure 3: Clinical outcomes using IVUS MLA to defer revascularisation in non-LMCA ICL: a review of several trials results. Figure 4: Effect of IVUS guided PCI compared with conventional angiography PCI on in-hospital mortality [results from Vikas Singh & al (16)]. Conclusion: Using IVUS to assess angiographically intermediate coronary lesions is correlated with a significant decrease of myocardial revascularization indications and favorable long term outcomes. IVUS guided-PCI is associated with fewer MACE compared with conventional angiography guided PCI. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. Zir LM, Miller SW, Dinsmore RE, Gilbert JP, Harthorne JW. Interobserver variability in coronary angiography. Circulation. 4 janv 1976; 53(4): 627‑ 32 Topol EJ, Nissen SE. Our Preoccupation With Coronary Luminology The Dissociation Between Clinical and Angiographic Findings in Ischemic Heart Disease. Circulation. 15 oct 1995; 92(8): 2333‑ 42. Abizaid A, Mintz GS, Pichard AD, Kent KM, Satler LF, Walsh CL, et al. Clinical, intravascular ultrasound, and quantitative angiographic determinants of the coronary flow reserve before and after percutaneous transluminal coronary angioplasty. Am J Cardiol. 15 août 1998; 82(4): 423 ‑ 8. Kang S-J, Ahn J-M, Song H, Kim W-J, Lee J-Y, Park D-W, et al. Usefulness of minimal luminal coronary area determined by intravascular ultrasound to predict functional significance in stable and unstable angina pectoris. Am J Cardiol. 1 avr 2012; 109(7): 947 ‑ 53. Ben-Dor I, Torguson R, Deksissa T, Bui AB, Xue Z, Satler LF, et al. Intravascular ultrasound lumen area parameters for assessment of physiological ischemia by fractional flow reserve in intermediate coronary artery stenosis. Cardiovasc Revascularization Med Mol Interv. juin 2012; 13(3): 177 ‑ 82. Waksman R, Legutko J, Singh J, Orlando Q, Marso S, Schloss T, et al. FIRST: Fractional Flow Reserve and Intravascular Ultrasound Relationship Study. J Am Coll Cardiol. mars 2013; 61(9): 917‑ 23. Jasti V. Correlations Between Fractional Flow Reserve and Intravascular Ultrasound in Patients With an Ambiguous Left Main Coronary Artery Stenosis. Circulation. 18 oct 2004; 110(18): 2831‑ 6. De la Torre Hernandez JM, Hernández Hernandez F, Alfonso F, Rumoroso JR, Lopez-Palop R, Sadaba M, et al. Prospective Application of Pre-Defined Intravascular Ultrasound Criteria for Assessment of Intermediate Left Main Coronary Artery Lesions. J Am Coll Cardiol. juill 2011; 58(4): 351‑ 8. Fassa A, Wagatsuma K, Higano S, Mathew V, Barsness G, Lennon R, et al. Intravascular ultrasound-guided treatment for angiographically indeterminate left main coronary artery disease. A long-term follow-up study. J Am Coll Cardiol. 18 janv 2005; 45(2): 204 ‑ 11. Abizaid AS, Mintz GS, Mehran R, Abizaid A, Lansky AJ, Pichard AD, et al. Long-Term Follow-Up After Percutaneous Transluminal Coronary Angioplasty Was Not Performed Based on Intravascular Ultrasound Findings Importance of Lumen Dimensions. Circulation. 20 juill 1999; 100(3): 256 ‑ 61. Nam C-W, Yoon H-J, Cho Y-K, Park H-S, Kim H, Hur S-H, et al. Outcomes of Percutaneous Coronary Intervention in Intermediate Coronary Artery Disease. JACC Cardiovasc Interv. août 2010; 3(8): 812‑ 7. De la Torre Hernandez JM, Lopez-Palop R, Garcia Camarero T, Carrillo Saez P, Martin Gorria G, Frutos Garcia A, et al. Clinical outcomes after intravascular ultrasound and fractional flow reserve assessment of intermediate coronary lesions. Propensity score matching of large cohorts from two institutions with a differential approach. Euro. Intervention J Eur Collab Work Group Interv Cardiol Eur Soc Cardiol. 22 nov 2013; 9(7): 824‑ 30. Long-term health outcome and mortality evaluation after invasive coronary treatment using drug eluting stents with or without the IVUS guidance. Randomized control trial. HOME DESIVUS. Jakabcin J, Spacek R, Bystron M, Kvasnák M, Jager J, Veselka J, Kala P, Cervinka P. A prospective, randomized trial of intravascular-ultrasound guided compared to angiography guided stent implantation in complex coronary lesions: the AVIOtrial. Chieffo A 1, Latib A, Caussin C, Presbitero P, Galli S, Menozzi A, Varbella F, Mauri F, Valgimigli M, Arampatzis C, Sabate M, Erglis A, Reimers B, Airoldi F, Laine M, Palop RL, Mikhail G, Maccarthy P, Romeo F, Colombo A. Randomized comparison of clinical outcomes between intravascular ultrasound angiography-guided drug-eluting stent implantation for long coronary arterystenoses. JACC Cardiovasc Interv, 6 (2013), pp. 369– 376 Comparison of Inhospital Mortality, Length of Hospitalization, Costs, and Vascular Complications of Percutaneous Coronary Interventions Guided by Ultrasound Versus Angiography Vikas Singh, MD & al. Am J Cardiol 2015; 115: 1357 -1366. Meta-Analysis of Outcomes After Intravascular Ultrasound–Guided Versus Angiography-Guided Drug-Eluting Stent Implantation in 26, 503 Patients Enrolled in Three Randomized Trials and 14 Observational. Studies, Jung-Min Ahn & al, Am J Cardiol 2014; 113: 1338 e 1347. Université de Mons Prof. CARLIER STEPHANE | Service de Cardiologie UMONS