Head and Neck Cancer The Role of the







- Slides: 57
Head and Neck Cancer: The Role of the SLP Pre and Post-Operatively Brian Martin, MS, CCC-SLP
Disclosures Brian Martin, MS, CCC-SLP is a salaried employee of The Medical University of South Carolina.
Learning Objectives: • • Gain broad knowledge of what head and neck cancer is Describe medical treatment options for head and neck cancer Understand common surgical procedures Understand basic pre-operative evaluation of the head and neck population by SLP Understand basic post-operative evaluation and treatment of the head and neck population by SLP Understand basic anatomy and physiology following total laryngectomy Understand the SLP’s role in care for laryngectomy patients
Overview of head and neck cancer
The basics: what is cancer? • Cancer starts when an abnormal group of cells begins to grow • • out of control Often occurs when abnormal cell growth overcomes the immune system’s ability to suppress it “Cancer” is not one disease - there are many different types which are typically classified by the type of tissue that the cancer originates, or location of “primary” site of cancer
Types of cancer There are hundreds of cancer types that are classified by the type of tissue where the cancer originates: • Carcinoma: originates in epithelial tissue • 80 -90% of all cancers fall into this category • Epithelial cells line and cover organs, are found in skin, and line internal “passageways” • Sarcoma: originates in connective tissue • Bones • Tendons • Cartilage • Myeloma: originates in plasma cells of bone marrow • Leukemia: originates in bone marrow itself • Lymphoma: originates in glands/nodes of lymphatic system
Head and neck cancer: incidence, prevalence • • • Incidence rate: around 20 per 100, 000 people Accounts for 3% of all cancers in the US Roughly 53, 000 Americans diagnosed each year Estimated 10, 800 Americans die each year from head and neck cancer Males are more likely to have head and neck cancer, statistics ranging from 2: 1 to 4: 1
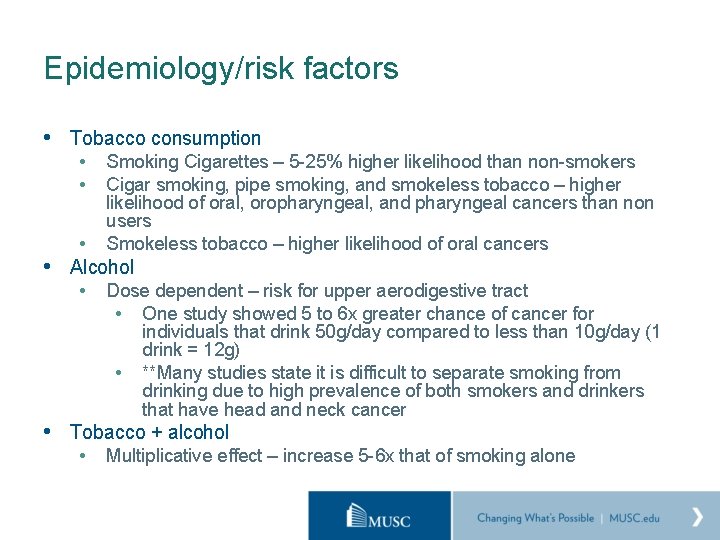
Epidemiology/risk factors • Tobacco consumption • • Smoking Cigarettes – 5 -25% higher likelihood than non-smokers Cigar smoking, pipe smoking, and smokeless tobacco – higher likelihood of oral, oropharyngeal, and pharyngeal cancers than non users Smokeless tobacco – higher likelihood of oral cancers • Alcohol • Dose dependent – risk for upper aerodigestive tract • One study showed 5 to 6 x greater chance of cancer for individuals that drink 50 g/day compared to less than 10 g/day (1 drink = 12 g) • **Many studies state it is difficult to separate smoking from drinking due to high prevalence of both smokers and drinkers that have head and neck cancer Tobacco + alcohol • Multiplicative effect – increase 5 -6 x that of smoking alone
Epidemiology/risk factors cont: • Human Papilloma Virus (HPV) • • Primarily p 16 genotype Younger population Non smokers BOT and Tonsillar cancers common
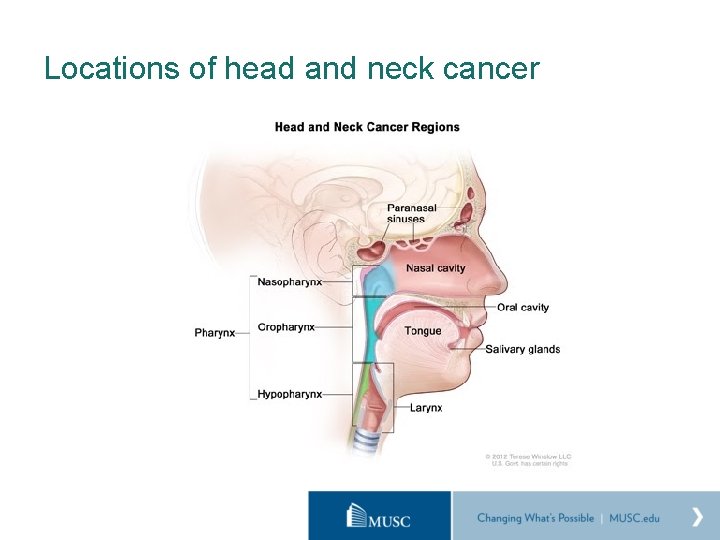
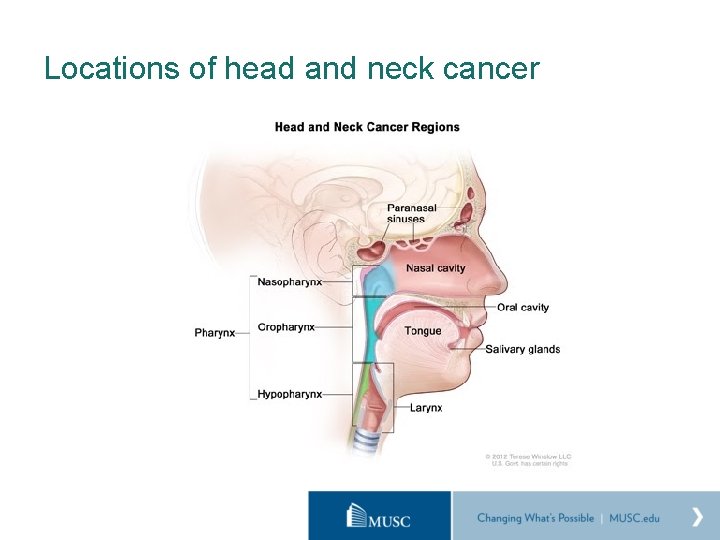
Locations of head and neck cancer
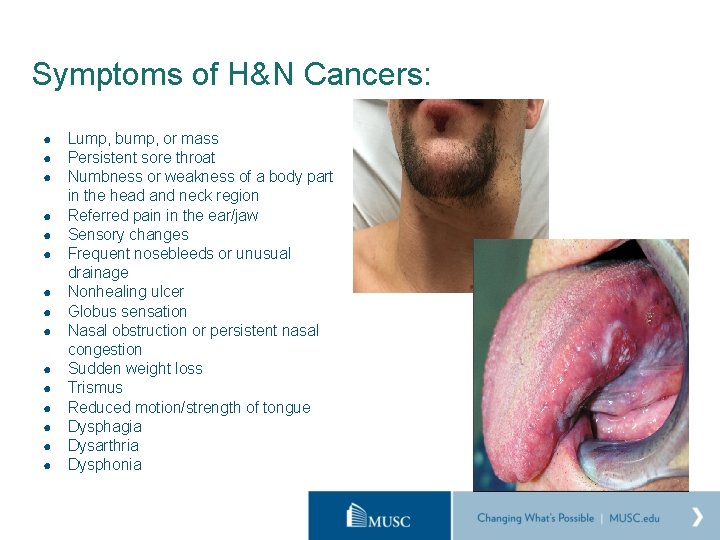
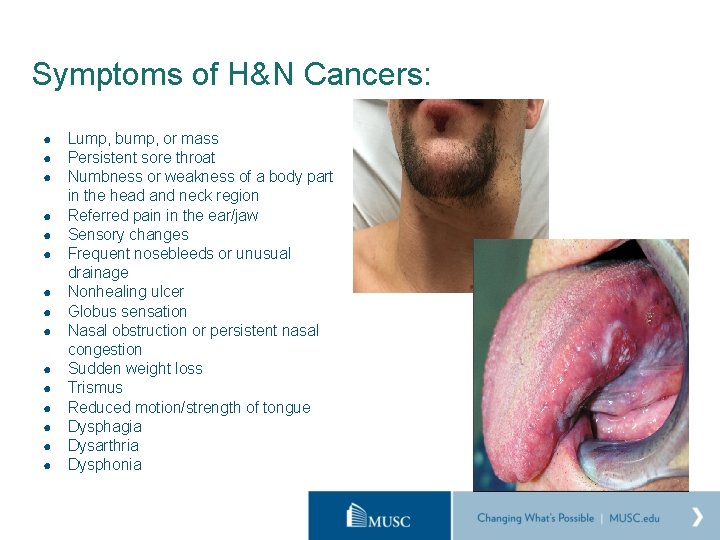
Symptoms of H&N Cancers: ● ● ● ● Lump, bump, or mass Persistent sore throat Numbness or weakness of a body part in the head and neck region Referred pain in the ear/jaw Sensory changes Frequent nosebleeds or unusual drainage Nonhealing ulcer Globus sensation Nasal obstruction or persistent nasal congestion Sudden weight loss Trismus Reduced motion/strength of tongue Dysphagia Dysarthria Dysphonia
TNM Staging T 4 N 2 M 0
TNM Staging T 4 N 2 M 0 • T refers to primary tumor • Number refers to size, and is location specific (i. e. T 4 in larynx may not be T 4 in lung)
TNM Staging T 4 N 2 M 0 • N refers to regional lymph nodes • Number indicates extent of involvement
TNM Staging T 4 N 2 M 0 • M refers to distant metastasis • 0 = no metastasis, 1 = distant metastasis
TNM Staging T 4 N 2 M 0 Stage IV • Multiple variables which are specific to type of cancer, location, size, nodal involvement, and metastasis leads to a roman numeral staging • Staging helps to determine what mode of medical intervention will be recommended
Medical intervention for head and neck cancer
Radiation • Provides small doses of radiation over a long period of time to • destroy cancer cells Dosage measured in grays (Gy) • 1 gy = absorption of 1 joule of energry per kilogram of matter • • Treatment typically once per day, 5 days a week 5 -7 weeks Each tx lasts about 10 minutes Definitive vs Adjuvant
Chemo • Typically given via IV • Targets most rapidly dividing cells • • Cancer cells Cells in GI tract Bone marrow Hair cells
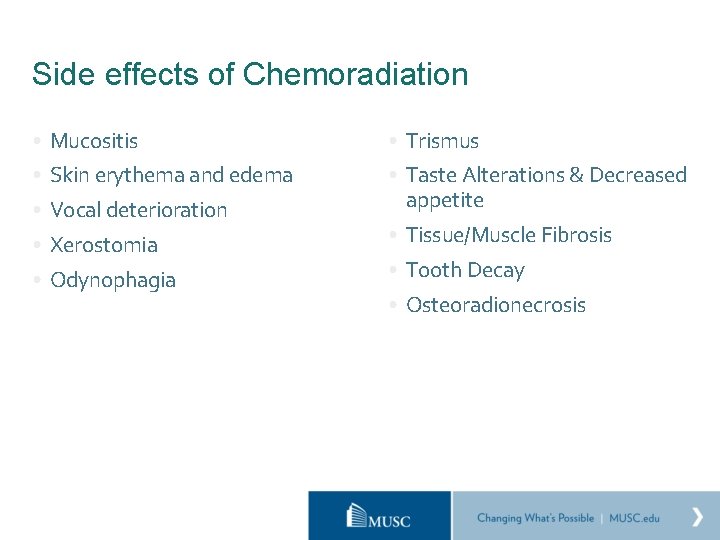
Side effects of Chemoradiation • Mucositis • Trismus • Skin erythema and edema • Taste Alterations & Decreased appetite • Vocal deterioration • Xerostomia • Odynophagia • Tissue/Muscle Fibrosis • Tooth Decay • Osteoradionecrosis
Surgical Intervention
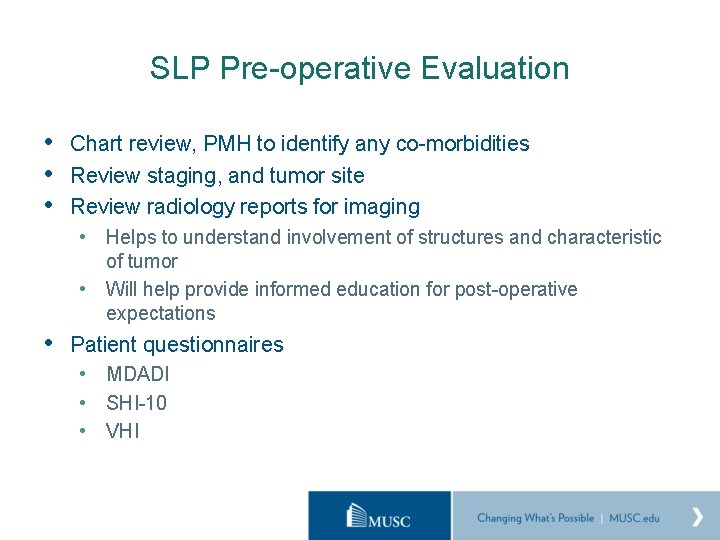
SLP Pre-operative Evaluation • Chart review, PMH to identify any co-morbidities • Review staging, and tumor site • Review radiology reports for imaging • Helps to understand involvement of structures and characteristic of tumor • Will help provide informed education for post-operative expectations • Patient questionnaires • MDADI • SHI-10 • VHI
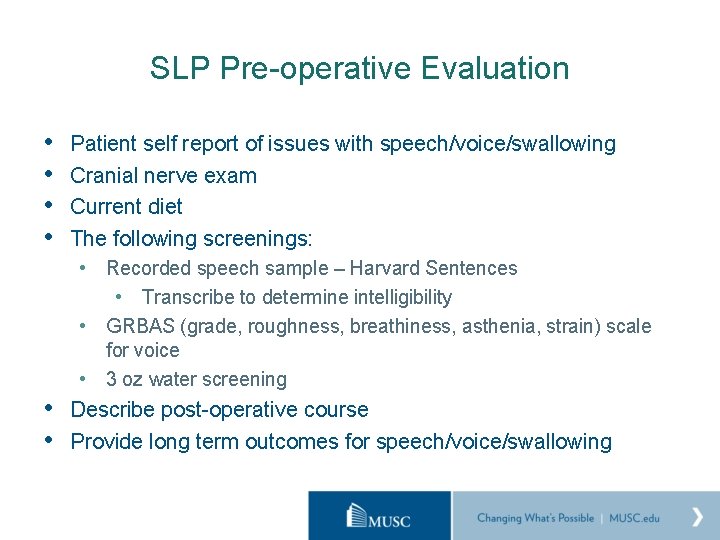
SLP Pre-operative Evaluation • • Patient self report of issues with speech/voice/swallowing Cranial nerve exam Current diet The following screenings: • Recorded speech sample – Harvard Sentences • Transcribe to determine intelligibility • GRBAS (grade, roughness, breathiness, asthenia, strain) scale for voice • 3 oz water screening • Describe post-operative course • Provide long term outcomes for speech/voice/swallowing
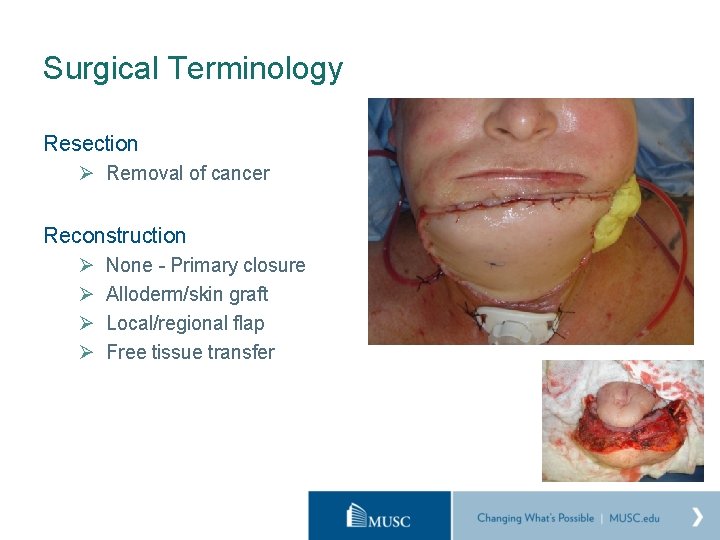
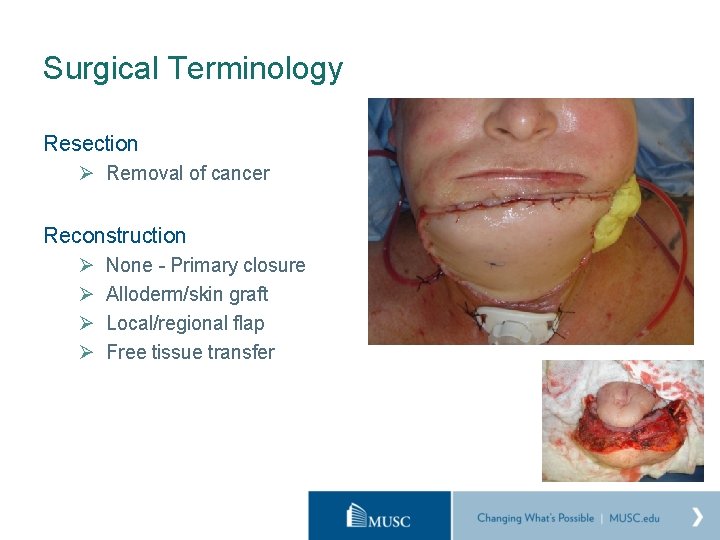
Surgical Terminology Resection Ø Removal of cancer Reconstruction Ø Ø None - Primary closure Alloderm/skin graft Local/regional flap Free tissue transfer

Terminology: Types of surgery Composite Resection › Removal of cancerous soft tissue and bone › Reconstructed with flaps which may be soft tissue only, or cutaneous/osteocutaneous Transoral Endoscopic Surgery › Surgical removal through the mouth (usually small tumors) › Helps preserve function/appearance Transoral Robotic Surgery (TORS) › Removal of oropharyngeal tumors through incisions in the mouth by using robotic technology › Bleed risk – advance from clear liquid, to full liquid, to puree and finally solids › Painful!!!
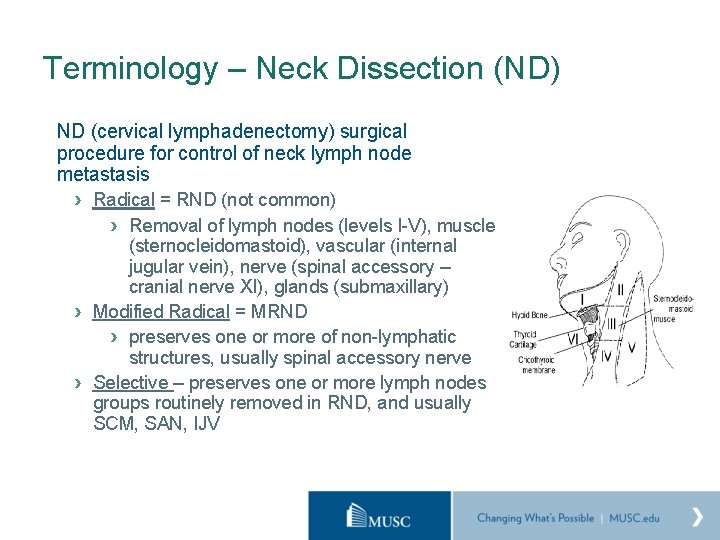
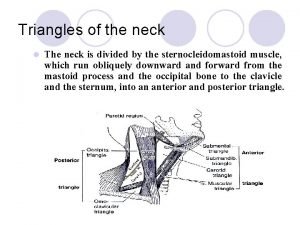
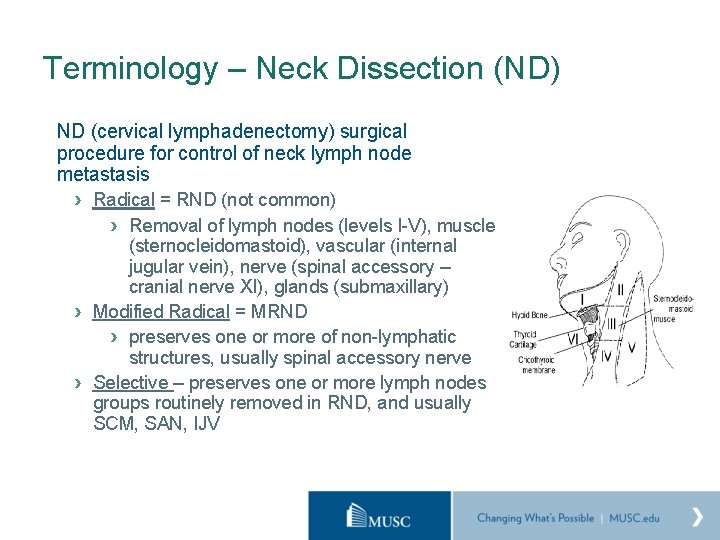
Terminology – Neck Dissection (ND) ND (cervical lymphadenectomy) surgical procedure for control of neck lymph node metastasis › Radical = RND (not common) › Removal of lymph nodes (levels I-V), muscle (sternocleidomastoid), vascular (internal jugular vein), nerve (spinal accessory – cranial nerve XI), glands (submaxillary) › Modified Radical = MRND › preserves one or more of non-lymphatic structures, usually spinal accessory nerve › Selective – preserves one or more lymph nodes groups routinely removed in RND, and usually SCM, SAN, IJV
Factors That Influence Outcomes Prior surgeries or prior radiation Co-morbidities › › History of neurologic involvement Respiratory status (COPD? ) Behavioral ETOH/drug use Psychologic involvement Size and location of Tumor Size/type of recon
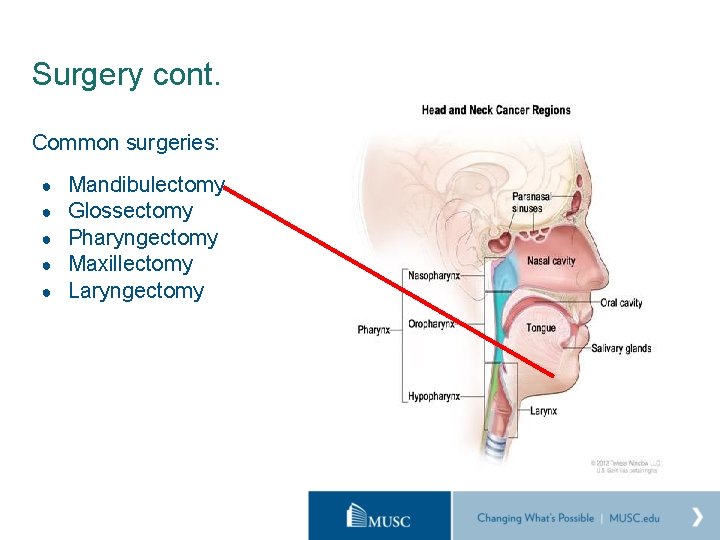
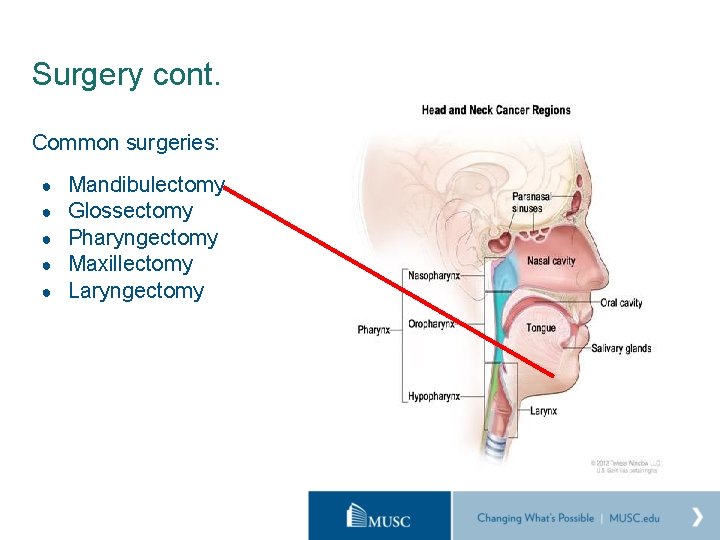
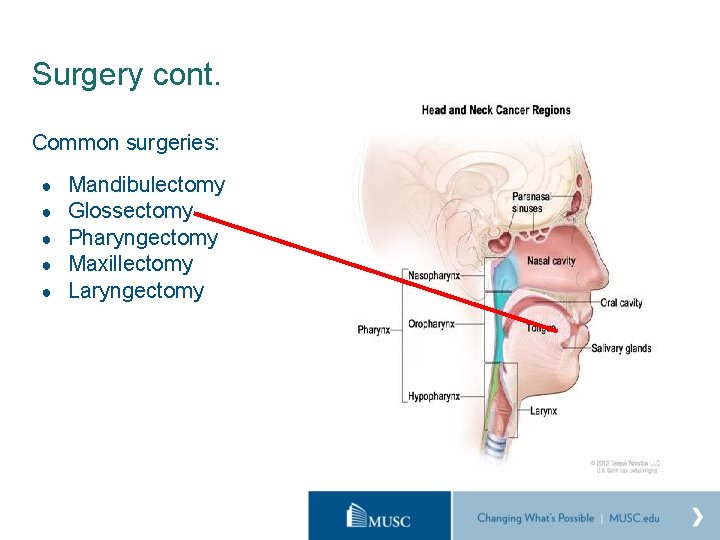
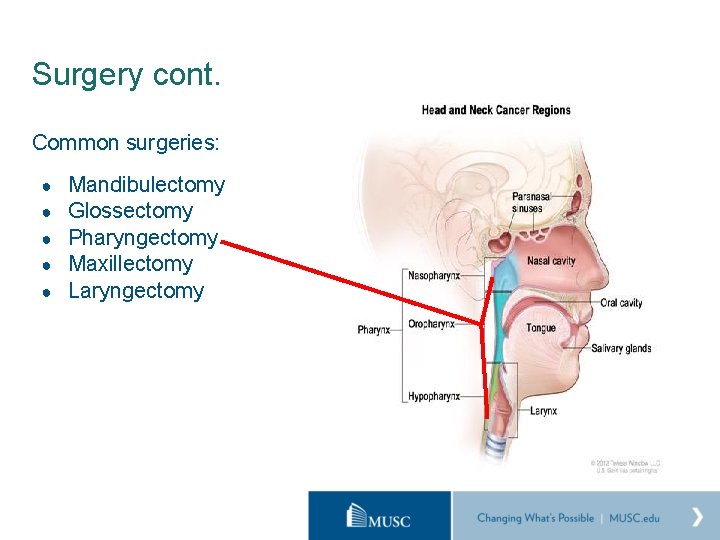
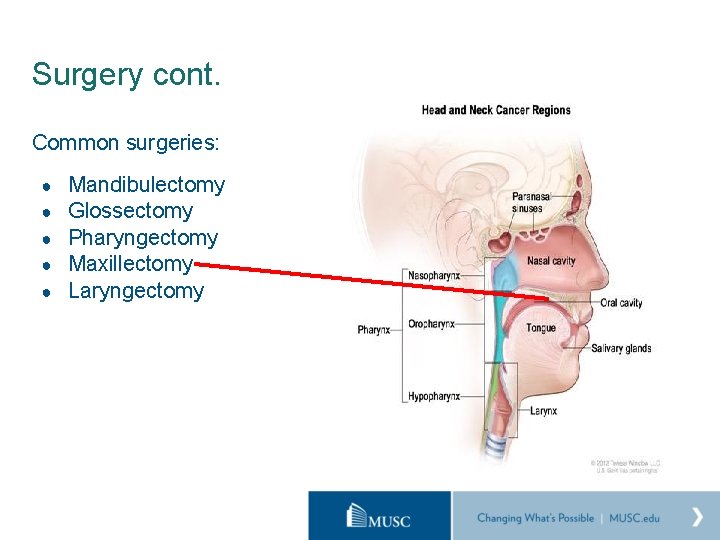
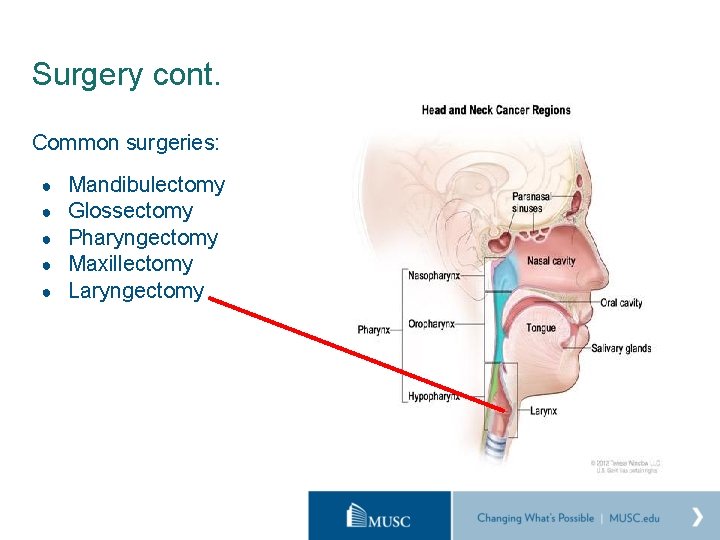
Surgery cont. Common surgeries: ● ● ● Mandibulectomy Glossectomy Pharyngectomy Maxillectomy Laryngectomy
Mandibulectomy Marginal Mandibulectomy – removal of a portion of the mandible, but not a whole section. ○ May only require local closure, alloderm graft, skin graft, locoregional flap ○ Typically good outcomes for speech/voice/swallowing unless involvement in tongue/FOM ○ May require temporary alternative means of nutrition until cleared to swallow by physician for healing purposes
Mandibulectomy Segmental Mandibulectomy – removal of entire section of mandible ○ Requires osteocutaneous flap and mandibular hardware to “fill the gap” and provide support ○ Poor speech initially – but improves somewhat with flap atrophy ○ Requires temporary alternative means of nutrition ■ MUSC - swallow study POD 5 or 1 -2 weeks after discharge ■ Oral swallow deficits due to displacement of oral tongue by flap ■ May require adaptive equipment to bypass oral stage

Composite mandibulectomy Removal of both bone and soft tissue (tongue, FOM, buccal cavity etc. ) ○ Worse speech/swallowing outcomes than marginal or segmental ○ May lead to life long deficits in speech and swallowing ○ Typically evaluated similarly to segmental mandibulectomy – POD 5 or 1 -2 weeks after discharge ○ Also may require adaptive equipment ○ If extensive FOM involvement, may result in pharyngeal deficits
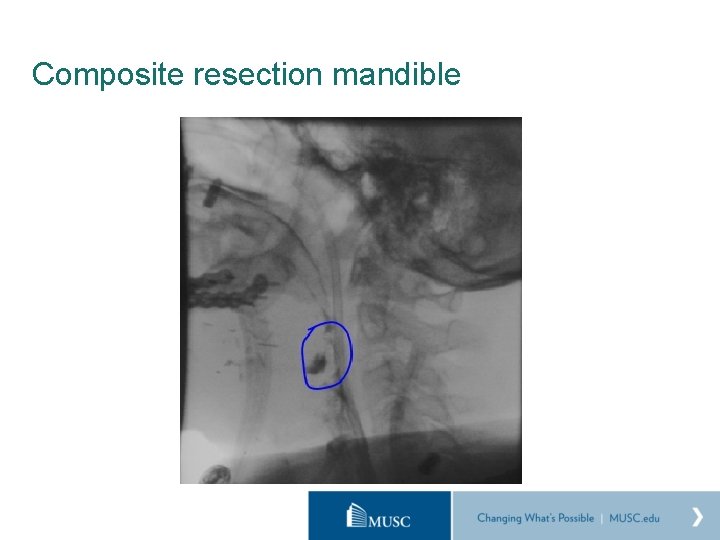
Composite resection mandible

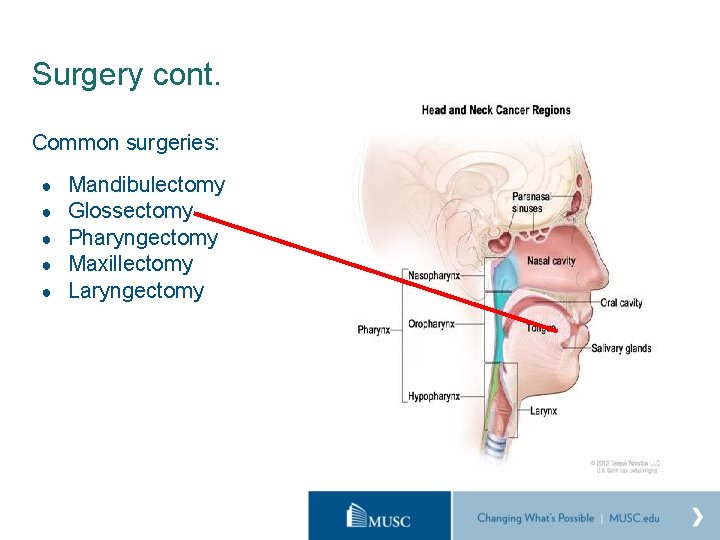
Surgery cont. Common surgeries: ● ● ● Mandibulectomy Glossectomy Pharyngectomy Maxillectomy Laryngectomy
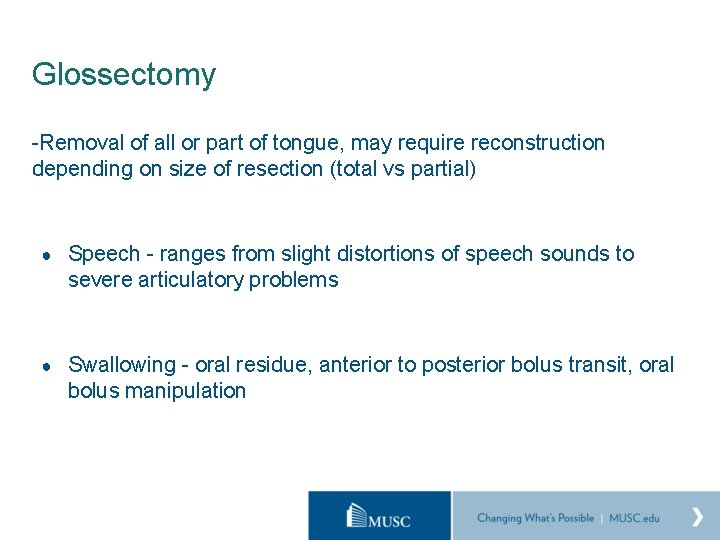
Glossectomy -Removal of all or part of tongue, may require reconstruction depending on size of resection (total vs partial) ● Speech - ranges from slight distortions of speech sounds to severe articulatory problems ● Swallowing - oral residue, anterior to posterior bolus transit, oral bolus manipulation


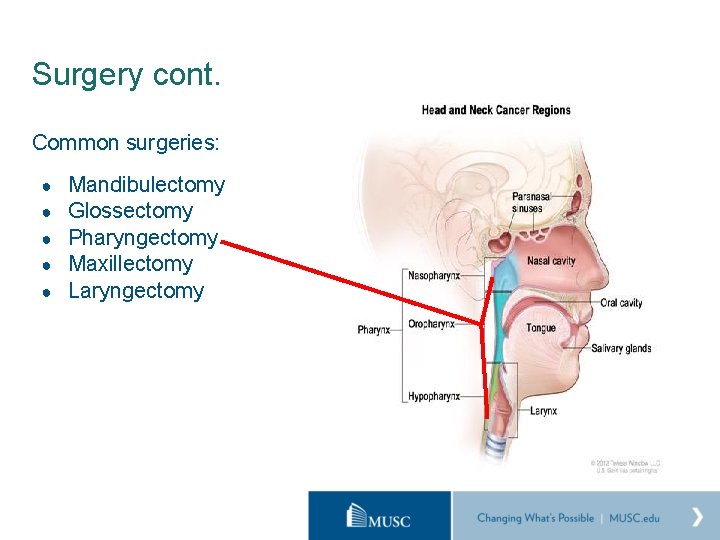
Surgery cont. Common surgeries: ● ● ● Mandibulectomy Glossectomy Pharyngectomy Maxillectomy Laryngectomy
Pharyngectomy Removal of a portion of pharynx often requiring reconstruction ● Swallowing - pharyngeal residue, interruption of pharyngeal peristalsis ● Changes in resonant vocal quality

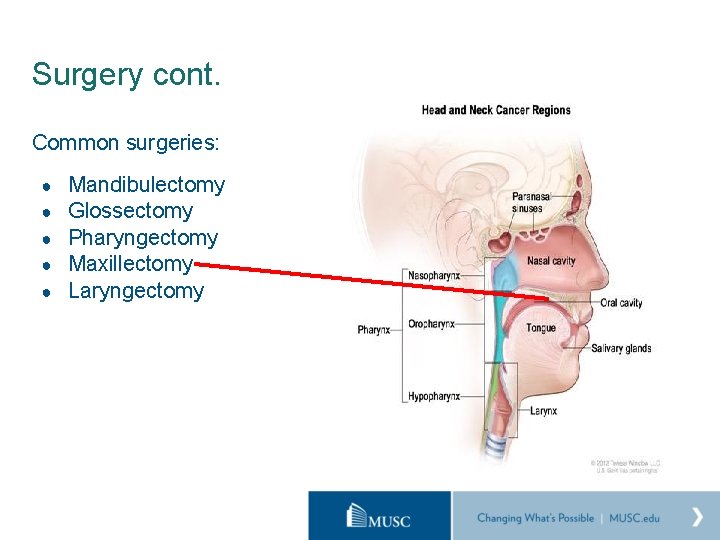
Surgery cont. Common surgeries: ● ● ● Mandibulectomy Glossectomy Pharyngectomy Maxillectomy Laryngectomy
Maxillectomy -Removal of all or part of maxilla (hard palate) requiring reconstruction or insertion of prosthetic device ● Speech - ranges from slight distortions of speech sounds to severe articulatory problems ● Swallowing - oral residue, anterior to posterior bolus transit, oral bolus manipulation, nasal regurgitation (obturator)
Dysphagia and Head and Neck Cancer Dysphagia in the head and neck cancer population post-treatment (including chemo, radiation and surgery) is as high as 50% according to some studies. • Functional outcomes are often related to: • Site of lesion • Stage of cancer • Treatment modality • Extent of resection • Type of reconstruction Organ preservation ≠ preserved function
Post-op treatment Treatment begins with discussion about expectations… • Is it realistic that patient return to a regular diet or is PO for pleasure/comfort more realistic? • Are they PEG dependent and likely to have it removed? • Compensatory strategies • • Postural changes can assist in anterior to posterior bolus movement, airway protection during swallow, or pharyngeal clearance of residue Compensatory strategies for speech • Adaptive equipment • Bypass oral phase • Syringe • Squeeze bottle • Glossectomy spoon • Exercise • • Swallow exercises Lingual strengthening and ROM • Biofeedback – FEES, s. EMG
Surgery cont. Common surgeries: ● ● ● Mandibulectomy Glossectomy Pharyngectomy Maxillectomy Laryngectomy
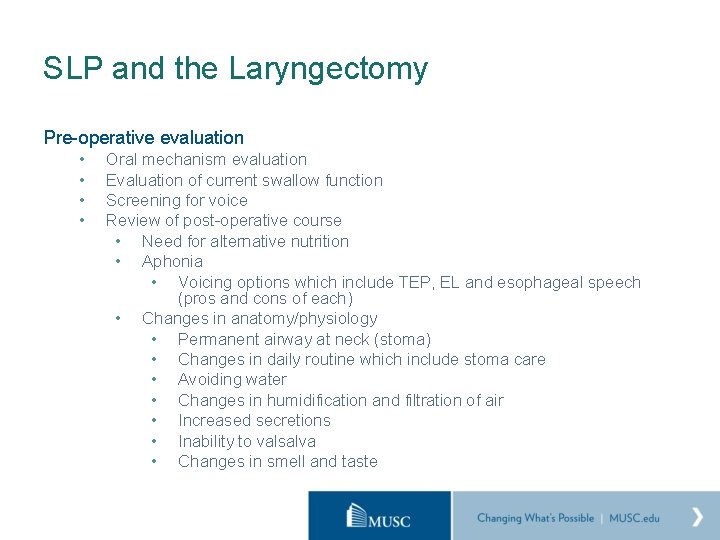
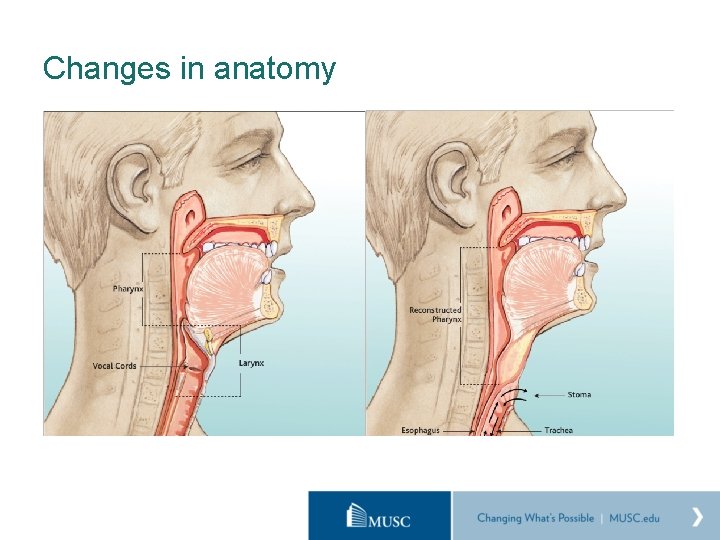
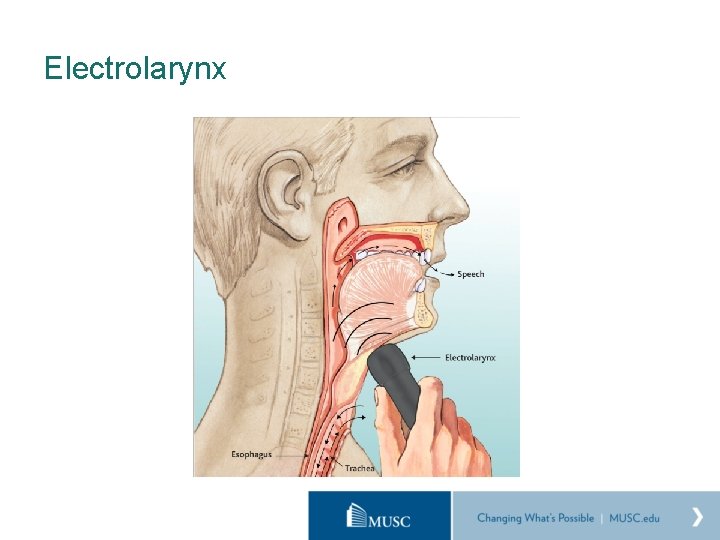
SLP and the Laryngectomy Pre-operative evaluation • • Oral mechanism evaluation Evaluation of current swallow function Screening for voice Review of post-operative course • Need for alternative nutrition • Aphonia • Voicing options which include TEP, EL and esophageal speech (pros and cons of each) • Changes in anatomy/physiology • Permanent airway at neck (stoma) • Changes in daily routine which include stoma care • Avoiding water • Changes in humidification and filtration of air • Increased secretions • Inability to valsalva • Changes in smell and taste
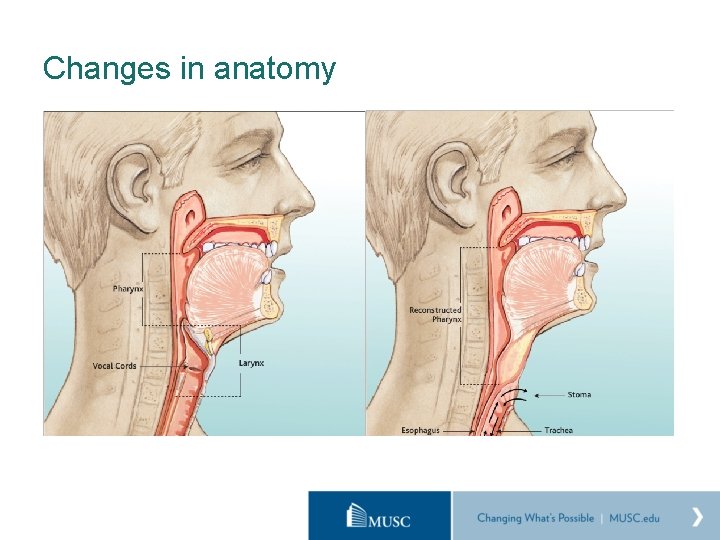
Changes in anatomy
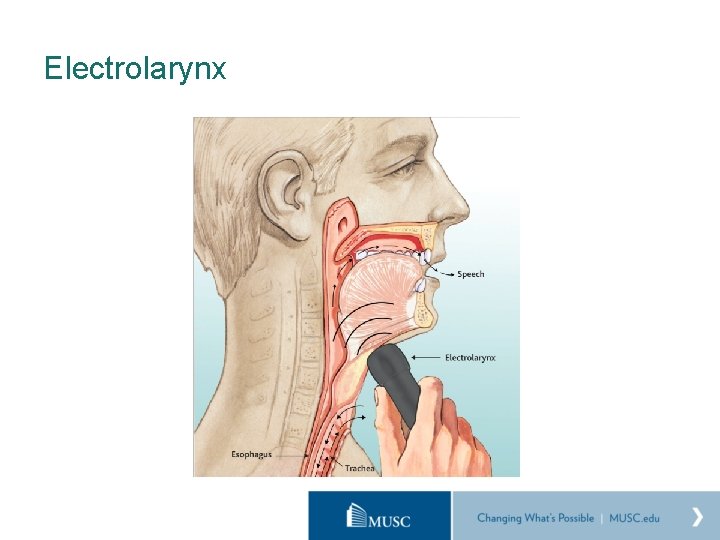
Electrolarynx
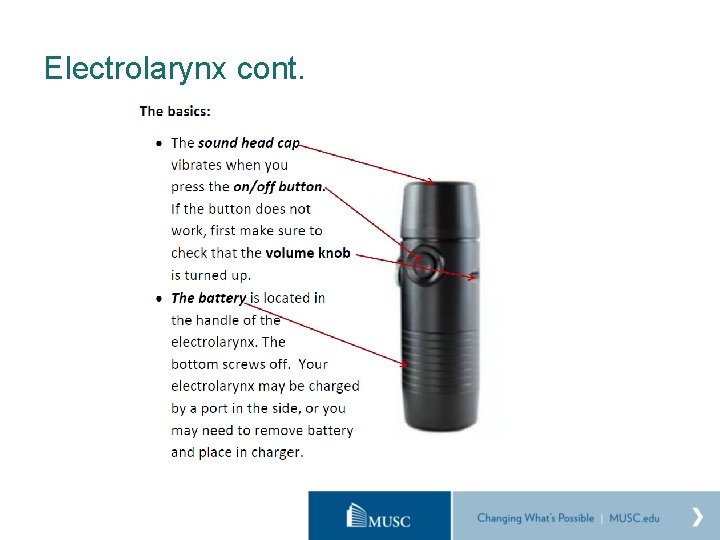
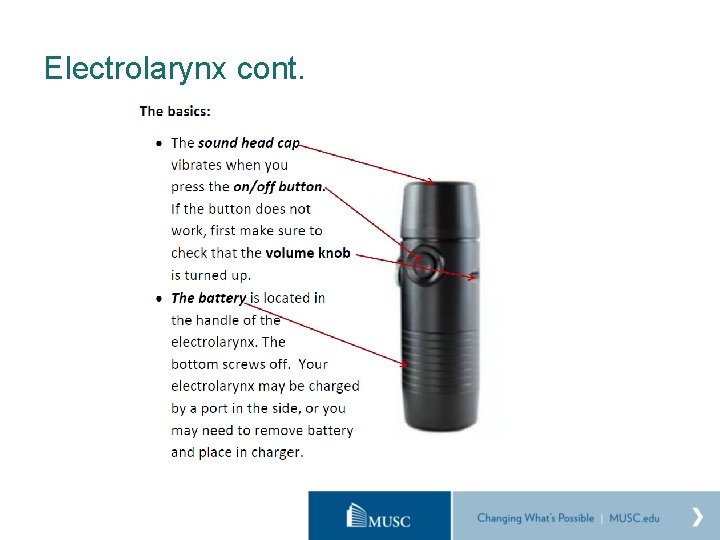
Electrolarynx cont.
Electrolarynx cont. Strategies to improve intelligibility • • Place oral wand in open space in mouth Press button, and immediately begin mouthing words Slow rate of speech Over articulation Exaggerate lip movement Release button as soon as speech is complete Practice! ** if using cutaneous instead of oral – find appropriate placement on neck/cheek/submentally and ensure sound cap is pressed completely against skin
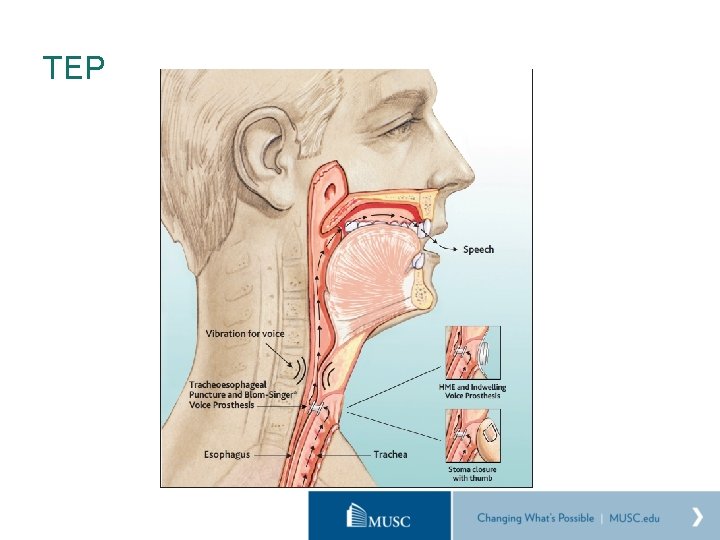
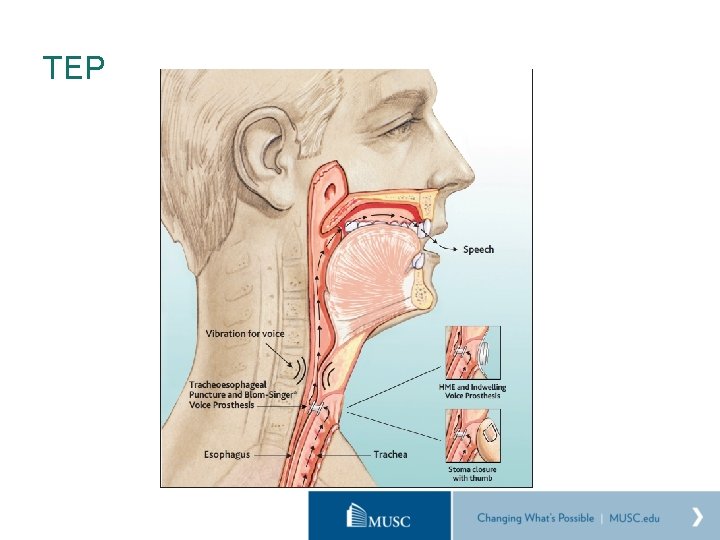
TEP

SLP’s role in TEP management • Voice prosthesis fails on average every 3 -6 months • When it fails, fluids leak through center • Occasionally, leaking will occur around prosthesis shaft (bigger • issue) Patients return to clinic for prosthesis change
References: • Lewin, Jan S. , Teng, Marita S. & Kotz, Tamara (2019). “Speech and swallowing rehabilitation of the patient with head and neck cancer. ” Up. To. Date last modified: April 2, 2019. • National Cancer Institute: PDQ® Laryngeal Cancer Treatment. Bethesda, MD: National Cancer Institute. Available at: https: //training. seer. cancer. gov/modules_reg_surv. html • Stenson, Kerstin M. (2020). “Epidemiology and risk factors for head and neck cancer. ” Up. To. Date last modified: January 21, 2020. • Bianchi, B, Ferri, A. , Copelli, C. , Poli, T. & Sesenna, E. (2008). “Free and locoregional flap associations in the reconstruction of extensive head and neck defects. ” International Journal of Oral and Maxillofacial Surgery, (37) 8, 723 -729. • “Head and neck cancers. ” Centers for Disease Control and Prevention. Last modified: May 29, 2018. Available at: https: //www. cdc. gov/cancer/headneck/index. htm • Husain, N. & Neyaz, A. (2017). “Human papillomavirus associated head and neck squamous cell carcinoma: Controversies and new concepts. ” J Oral Biol Craniofac Res, 7(3), 198 -205. • “Cancer Basics. ” American Cancer Society. Date last modified: December 8, 2015. Available at: https: //www. cancer. org/cancer-basics/what-is-cancer. html • Deschler DG, Moore MG, Smith RV, eds. “Quick Reference Guide to TNM Staging of Head and Neck Cancer and Neck Dissection Classi cation, 4 th ed. ” Alexandria, VA: American Academy of Otolaryngology–Head and Neck Surgery Foundation, 2014. • U. S. Cancer Statistics Working Group. U. S. Cancer Statistics Data Visualizations Tool, based on November 2018 submission data (1999 -2016): U. S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; www. cdc. gov/cancer/dataviz, June 2019.
Questions?
 Risk factors of head and neck cancer
Risk factors of head and neck cancer There once was a man from tennessee ukulele
There once was a man from tennessee ukulele Tnm 8 head and neck
Tnm 8 head and neck This is home ukulele
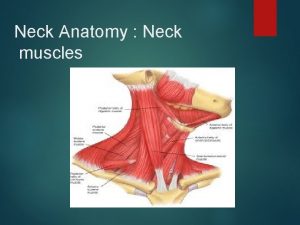
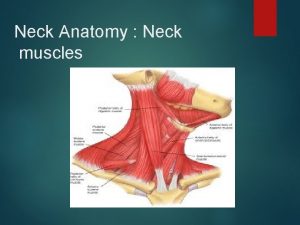
This is home ukulele Muscular system head and neck
Muscular system head and neck Zygomaticus minor
Zygomaticus minor Regional write up head face and neck
Regional write up head face and neck Eccomyosis
Eccomyosis What has a neck but no head
What has a neck but no head Difference between dividing head and indexing head
Difference between dividing head and indexing head Flood suction pump
Flood suction pump Web role in azure
Web role in azure The attacking firm goes head-to-head with its competitor.
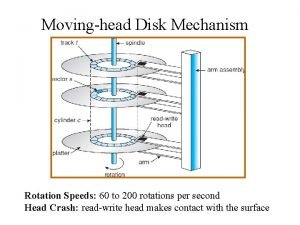
The attacking firm goes head-to-head with its competitor. Operation of moving head disk storage
Operation of moving head disk storage Parts of the neck
Parts of the neck Tonic syllable
Tonic syllable Biceps femoris innervation
Biceps femoris innervation Pre-head head tonic syllable tail
Pre-head head tonic syllable tail The head of moving head disk with 100 tracks
The head of moving head disk with 100 tracks Head nurse definition
Head nurse definition Rollendistanz krappmann beispiel
Rollendistanz krappmann beispiel Role conflict occurs when fulfilling the role expectations
Role conflict occurs when fulfilling the role expectations Rash on upper chest and back
Rash on upper chest and back Muscles of face and neck ppt
Muscles of face and neck ppt Neck bulge deepthroat
Neck bulge deepthroat Props in tinikling
Props in tinikling Hand of benediction nerve
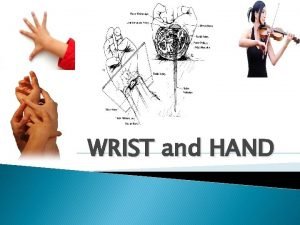
Hand of benediction nerve Boutonniere and swan neck deformity
Boutonniere and swan neck deformity Dr ayesha basharat
Dr ayesha basharat Boutonniere and swan neck deformity
Boutonniere and swan neck deformity Eular criteria
Eular criteria Dorsum of hand
Dorsum of hand Swan neck deformity
Swan neck deformity Foosh injury
Foosh injury Boutonniere and swan neck deformity
Boutonniere and swan neck deformity Objective examination of patient
Objective examination of patient Trigonum lumbale petiti
Trigonum lumbale petiti Causal organism of neck and bulb rot in garlic is _____
Causal organism of neck and bulb rot in garlic is _____ Chapter 24 the immune and lymphatic systems and cancer
Chapter 24 the immune and lymphatic systems and cancer What empties into the left subclavian vein
What empties into the left subclavian vein Frilled neck lizard adaptations
Frilled neck lizard adaptations Regional anatomical terms
Regional anatomical terms Triangles of neck
Triangles of neck Potential spaces
Potential spaces “the american embassy” by chimamanda ngozi adichie
“the american embassy” by chimamanda ngozi adichie Pylorus histology
Pylorus histology Neck righting reflex
Neck righting reflex Posterior triangle of neck
Posterior triangle of neck Dangerous space of neck
Dangerous space of neck Macfee incision
Macfee incision Potato tumor
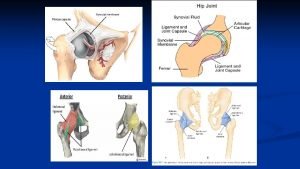
Potato tumor Iliac vessels anatomy
Iliac vessels anatomy Tonic labyrinthine reflex
Tonic labyrinthine reflex Lateral neck swelling
Lateral neck swelling Moro reflex absent
Moro reflex absent Scientific name for neck
Scientific name for neck Narrow neck which projects into the vagina inferiorly
Narrow neck which projects into the vagina inferiorly