Greatest Hits Test 2 Selected slides to study
- Slides: 76
Greatest Hits Test 2 Selected slides to study for Test 2. If you print these out, please print them as handouts to conserve paper. (When you select print, select handouts. You can print up to 9 slides on a page). BIO 232 Fall 2017
The Heart as a Pump Stroke Volume Cardiac Output Cardiac Reserve
Stroke Volume End Diastolic Volume (EDV) End Systolic Volume (ESV)
Cardiac Output (CO) CO= HR x SV
Cardiac Reserve COMax - CORest = COReserve
Resting Heart Rate Decreases from Birth 140 -160 ♂ 64 -72 ♀ 72 -80
Tachycardia (100 or more beats/min) Bradycardia (60 or less beats/min) Miguel Indurain A Bradycardia Sufferer
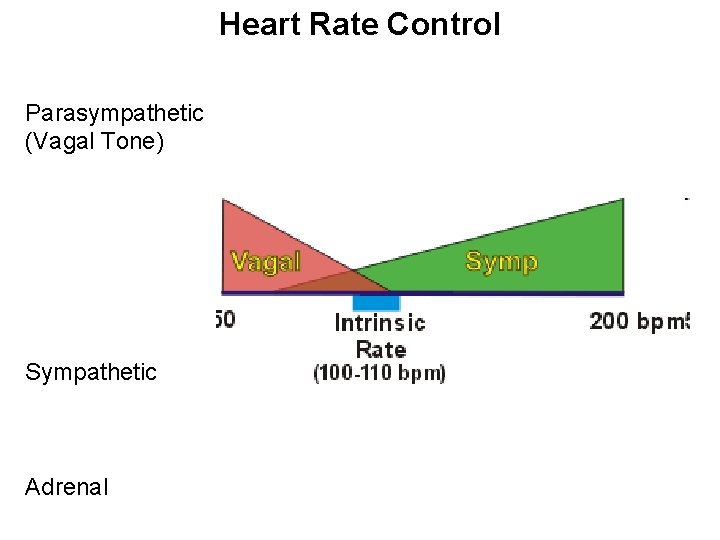
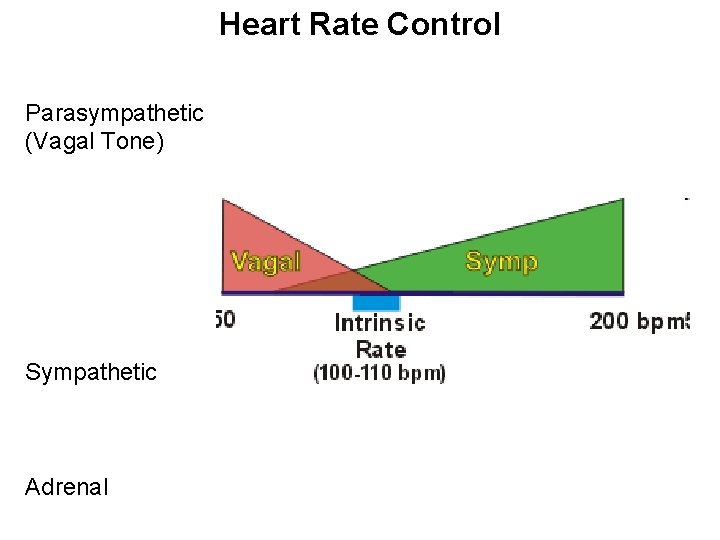
Heart Rate Control Parasympathetic (Vagal Tone) Sympathetic Adrenal
Factors that Alter EDV and ESV Preload Contractility Afterload
Preload: Heart “Stretchiness” Affects EDV Cardiac muscle stretches as heart fills
Frank-Starling Law of the Heart The volume of blood ejected from a ventricle during systole (contraction) depends on the volume present in the ventricle at the end of diastole (relaxation)
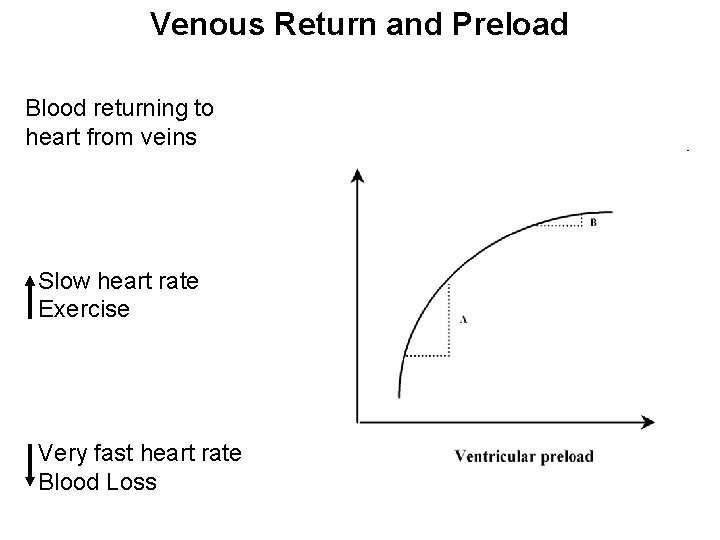
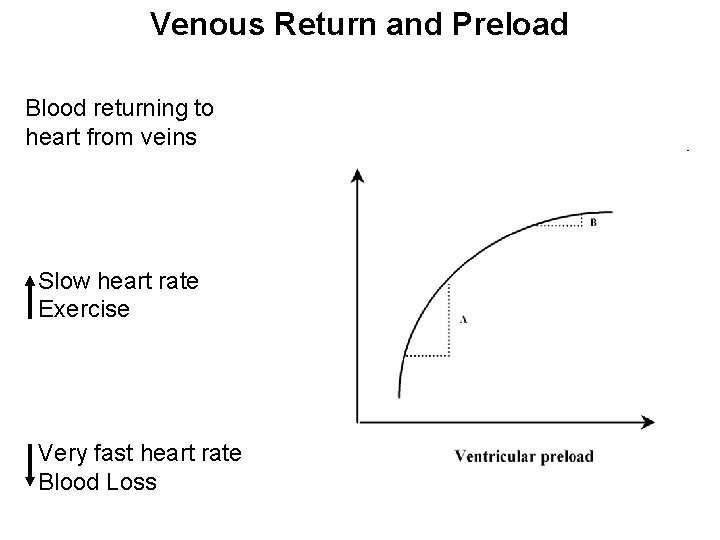
Venous Return and Preload Blood returning to heart from veins Slow heart rate Exercise Very fast heart rate Blood Loss
Contractility increases SV Contractile strength at a given muscle length More Ca++ Less Ca++
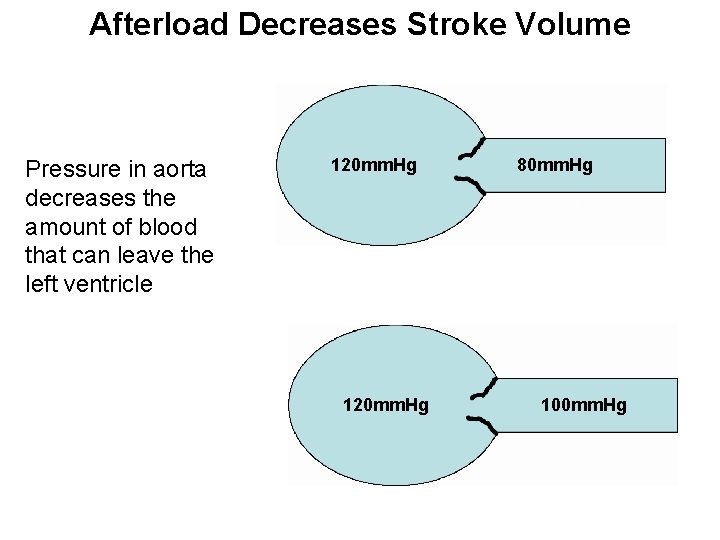
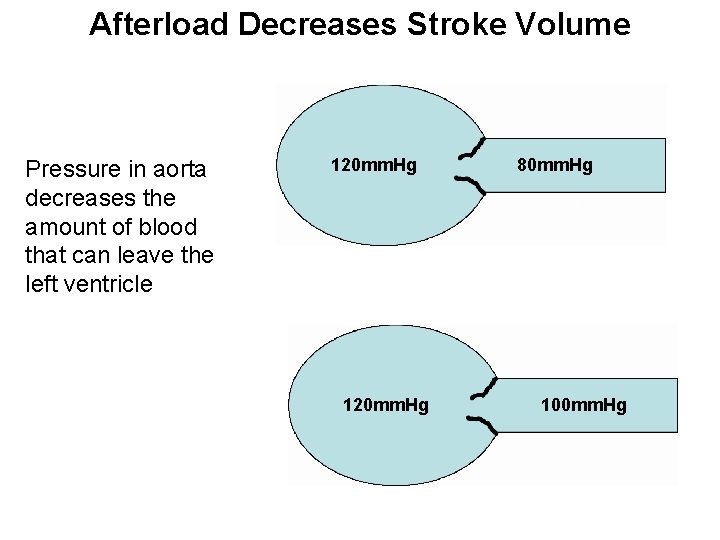
Afterload Decreases Stroke Volume Pressure in aorta decreases the amount of blood that can leave the left ventricle 120 mm. Hg 80 mm. Hg 100 mm. Hg
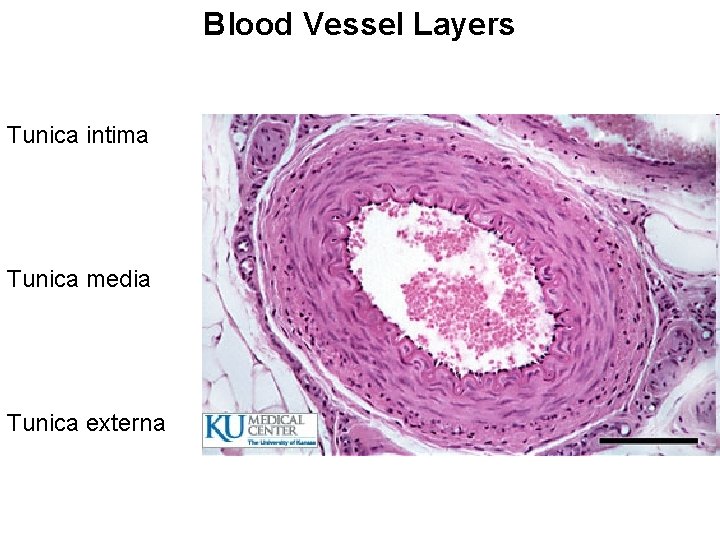
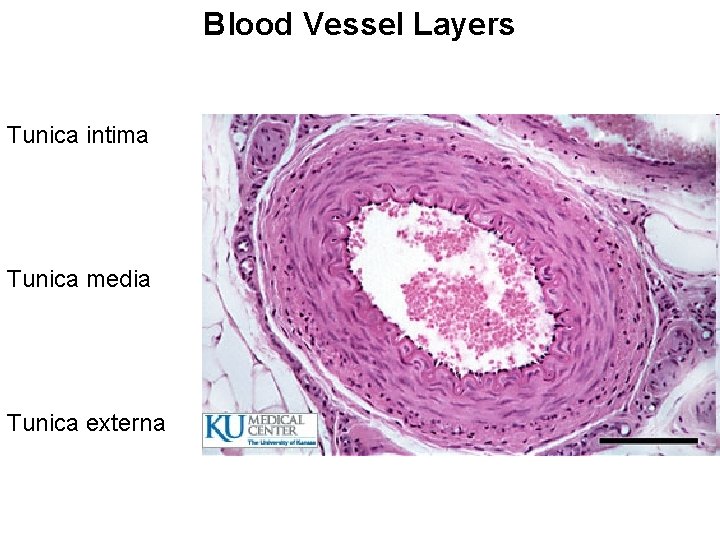
Blood Vessel Layers Tunica intima Tunica media Tunica externa
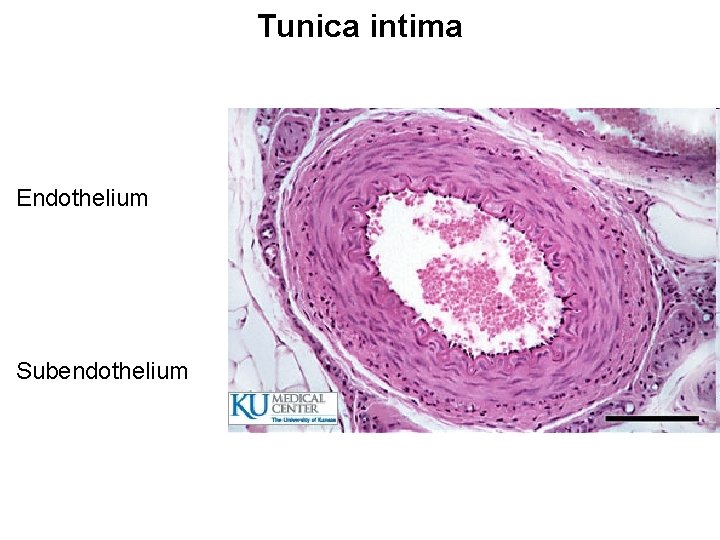
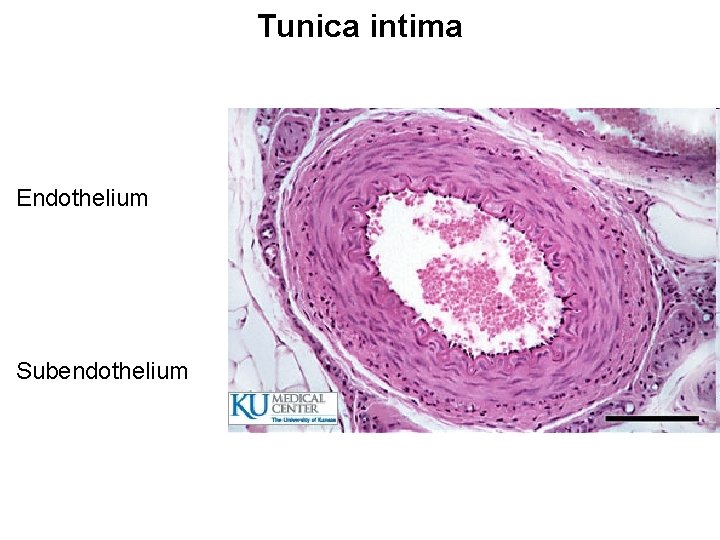
Tunica intima Endothelium Subendothelium
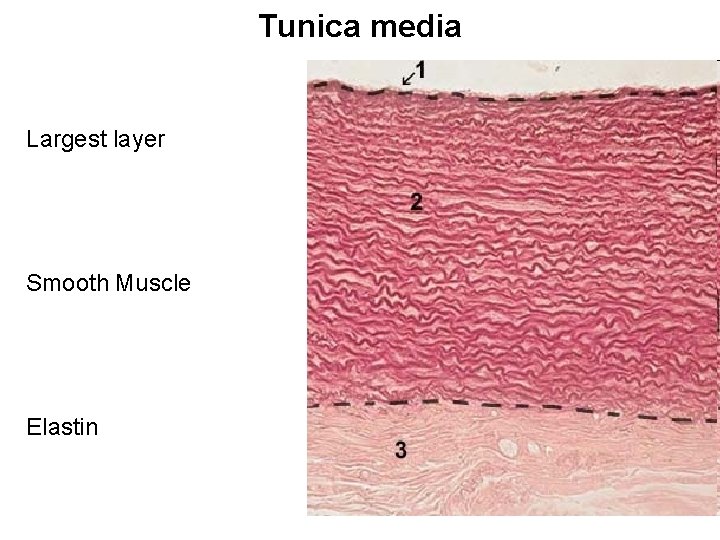
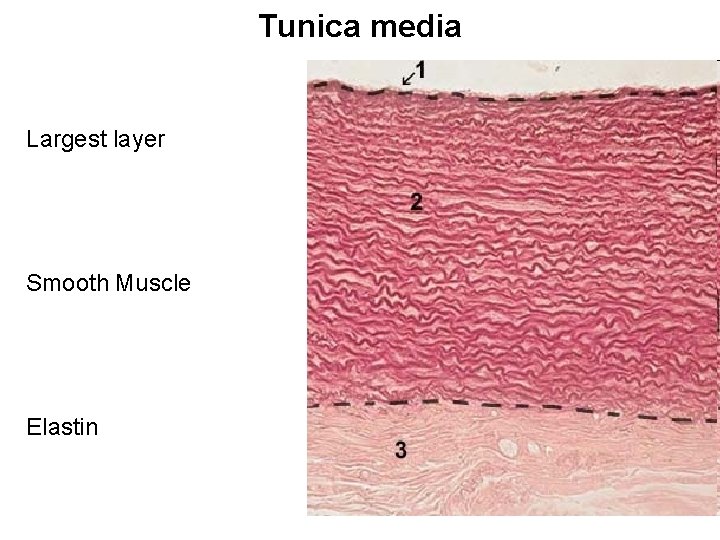
Tunica media Largest layer Smooth Muscle Elastin
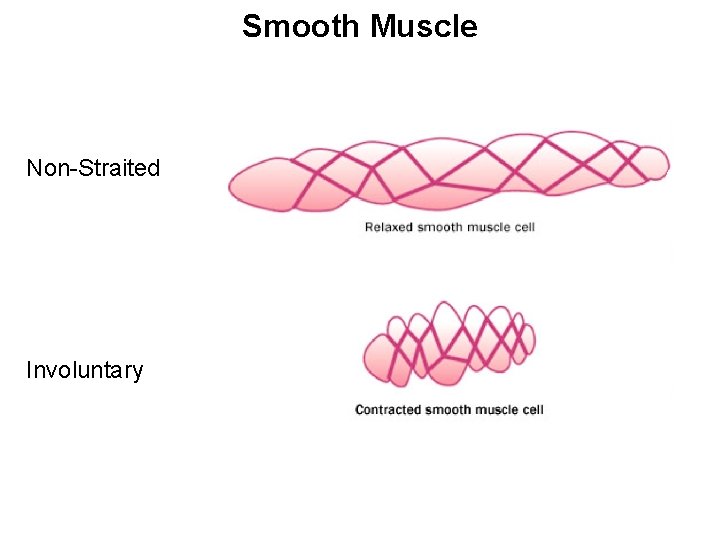
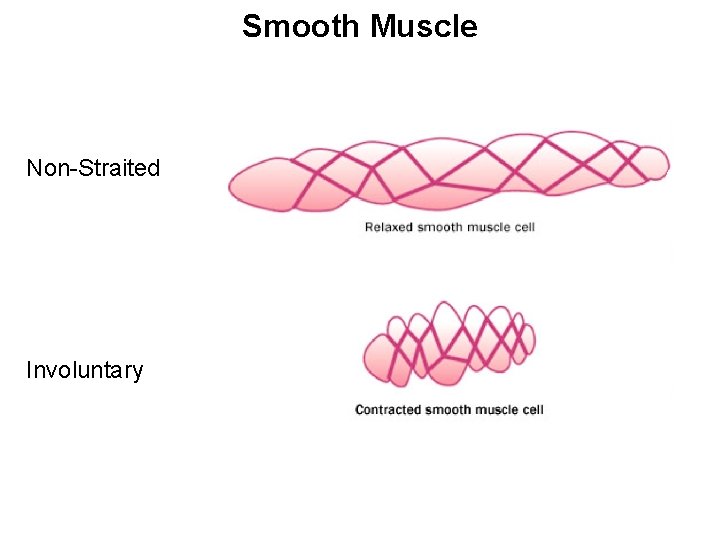
Smooth Muscle Non-Straited Involuntary
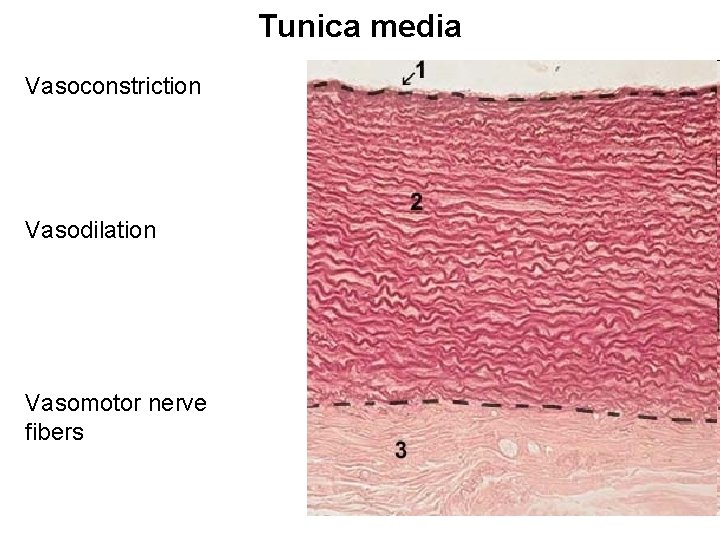
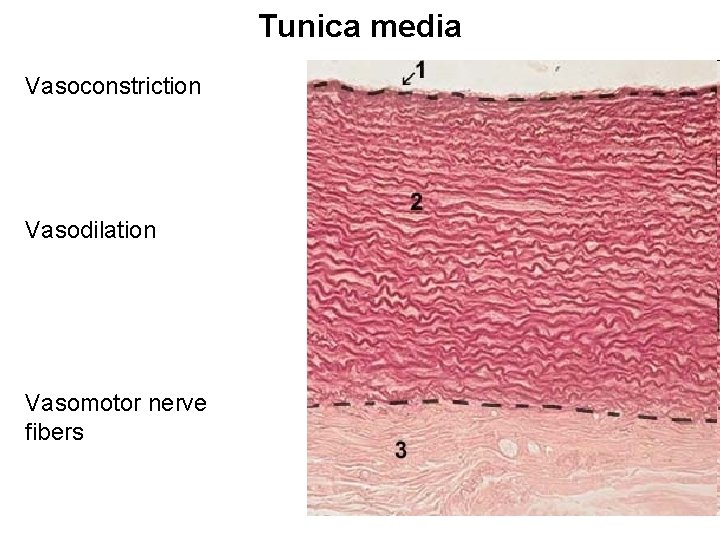
Tunica media Vasoconstriction Vasodilation Vasomotor nerve fibers
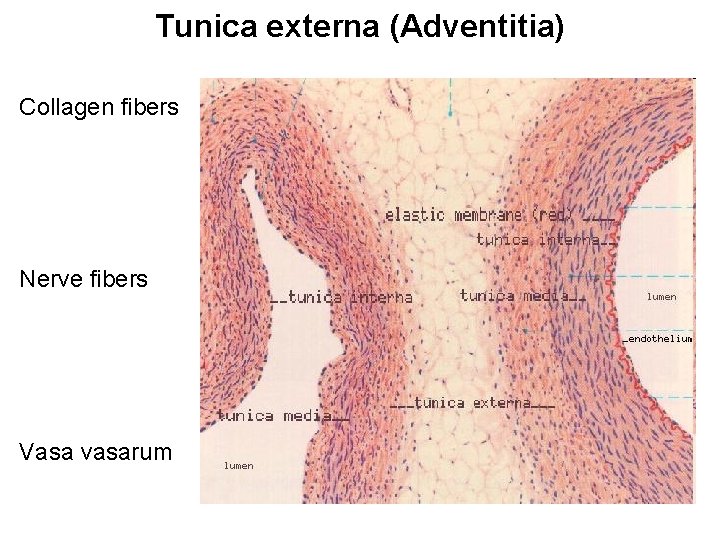
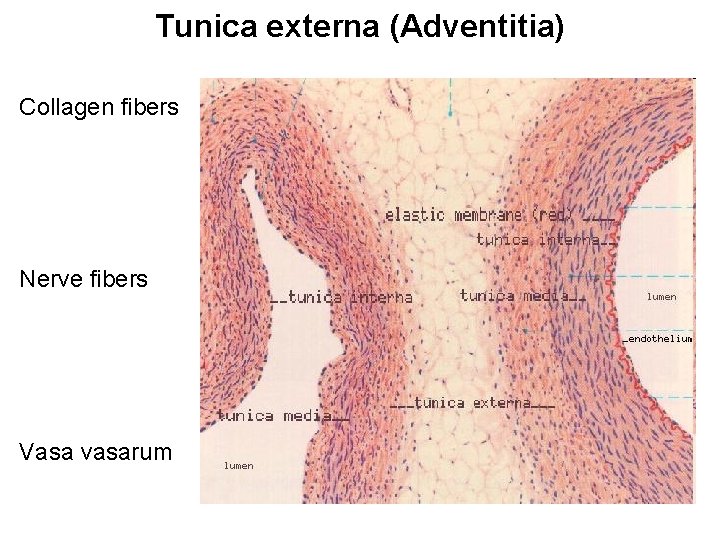
Tunica externa (Adventitia) Collagen fibers Nerve fibers Vasa vasarum
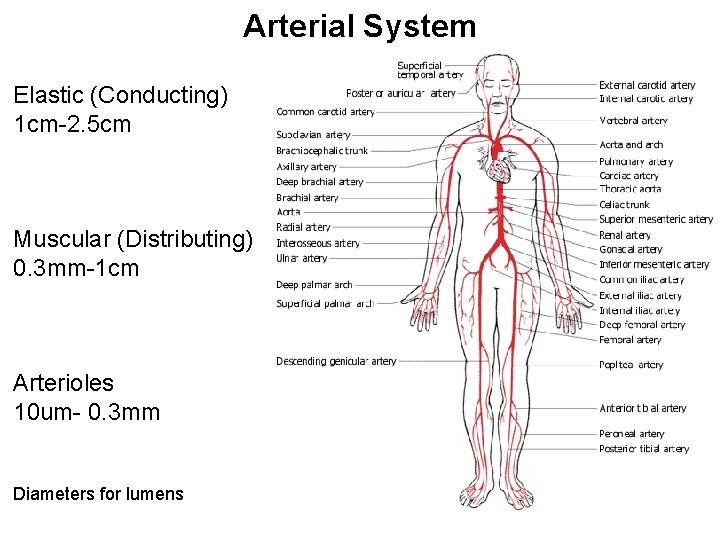
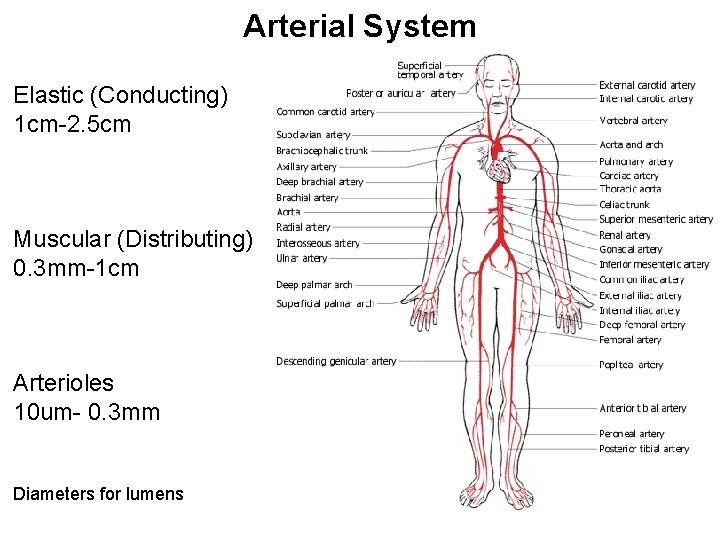
Arterial System Elastic (Conducting) 1 cm-2. 5 cm Muscular (Distributing) 0. 3 mm-1 cm Arterioles 10 um- 0. 3 mm Diameters for lumens
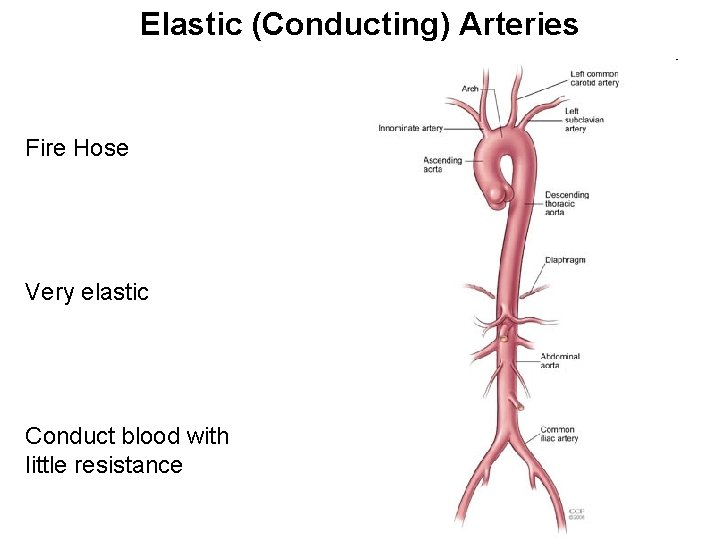
Elastic (Conducting) Arteries Fire Hose Very elastic Conduct blood with little resistance
Compliance/Distensibility Pressure waves Be able to describe the concept and why it is important. (Posted video may be helpful) Decreases pressure in smaller vessels
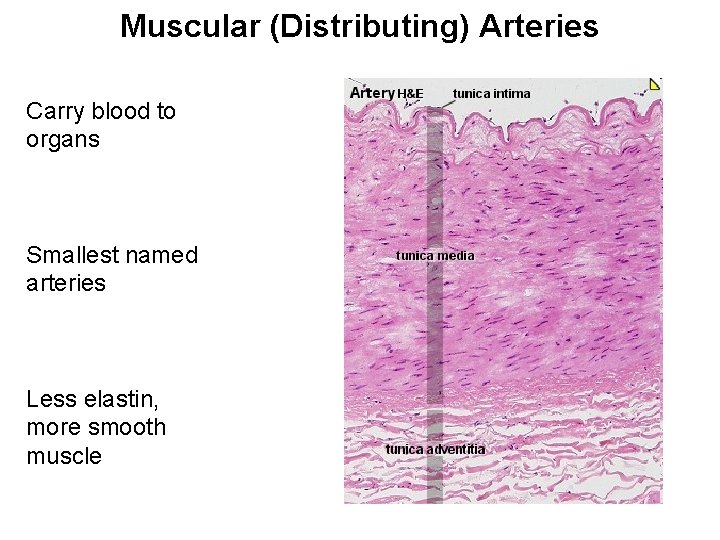
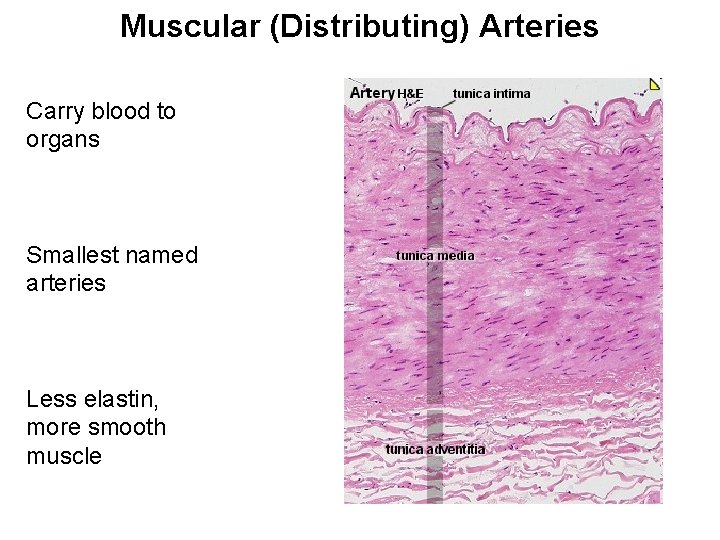
Muscular (Distributing) Arteries Carry blood to organs Smallest named arteries Less elastin, more smooth muscle
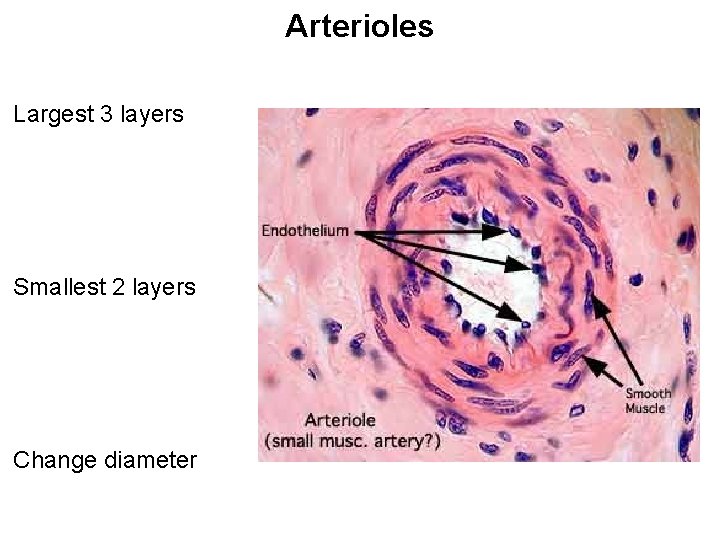
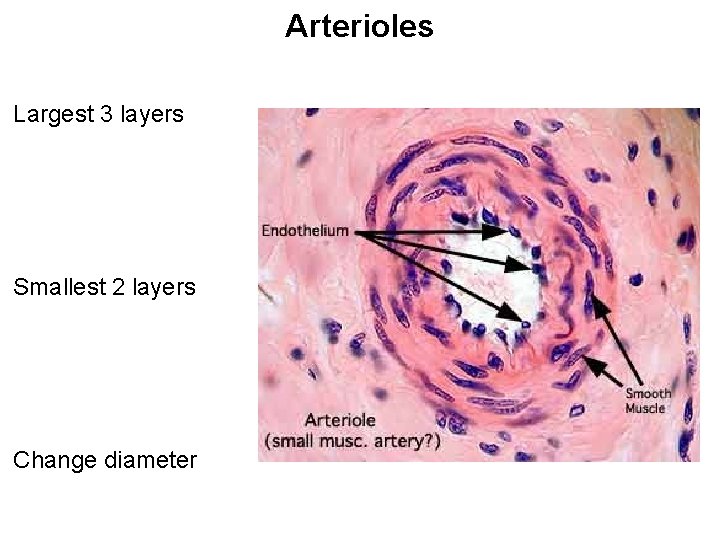
Arterioles Largest 3 layers Smallest 2 layers Change diameter
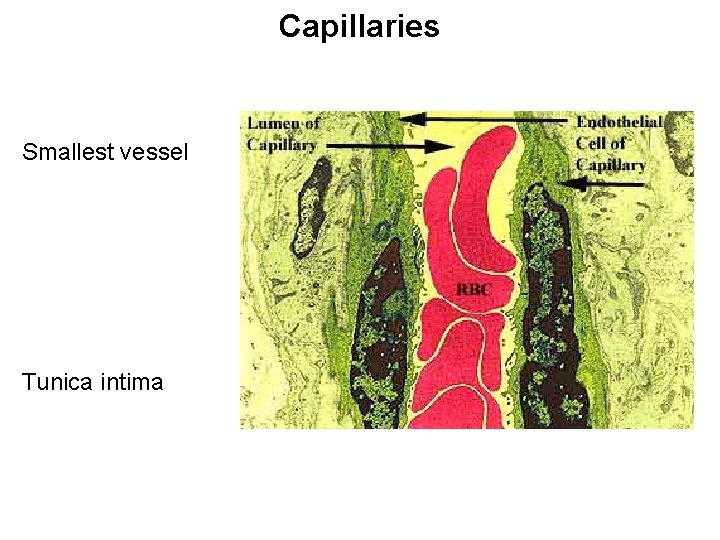
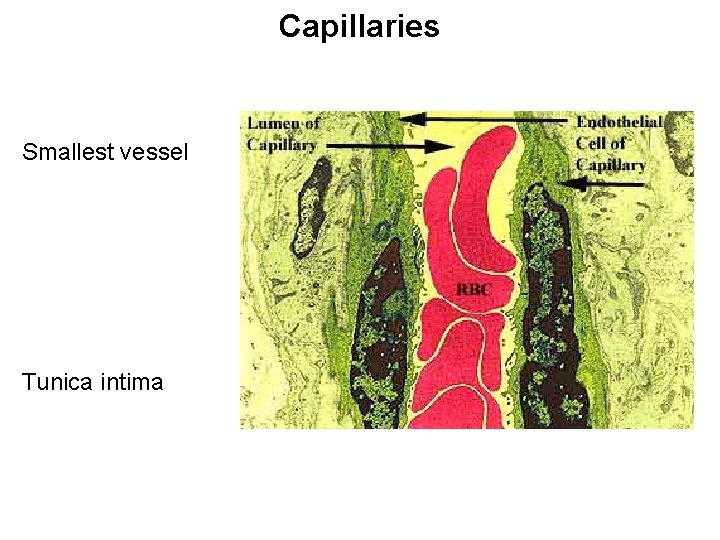
Capillaries Smallest vessel Tunica intima
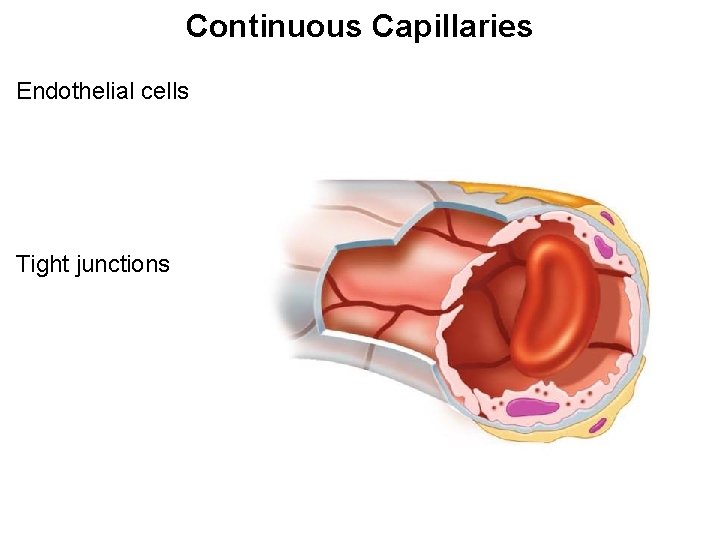
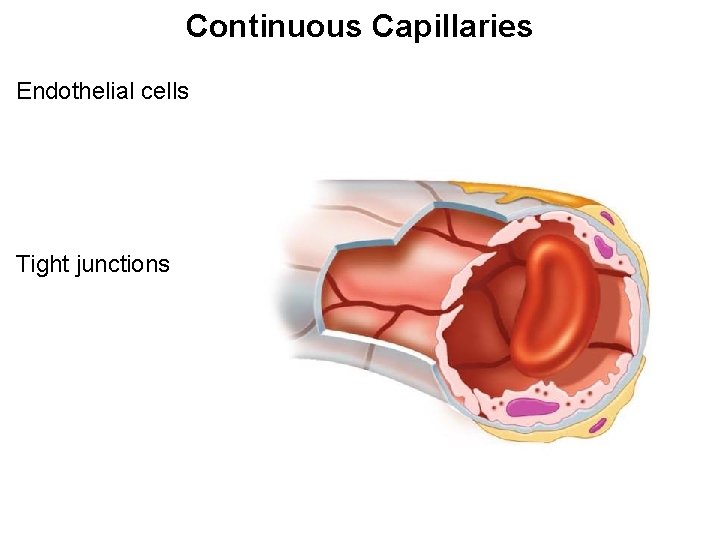
Continuous Capillaries Endothelial cells Tight junctions
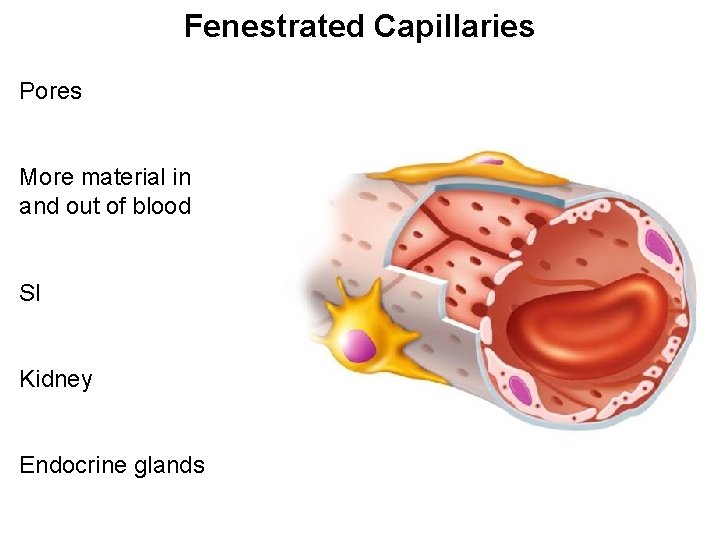
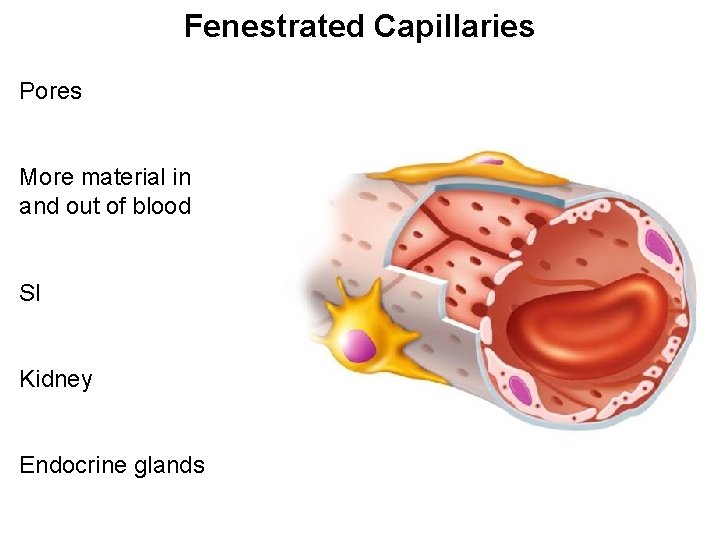
Fenestrated Capillaries Pores More material in and out of blood SI Kidney Endocrine glands
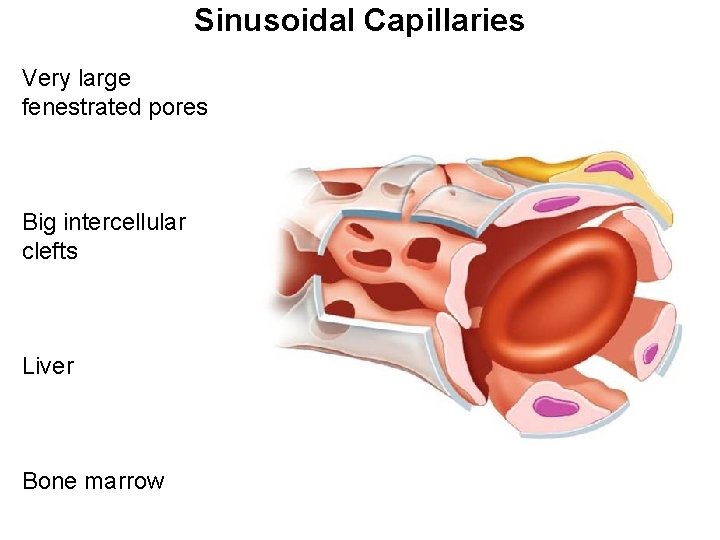
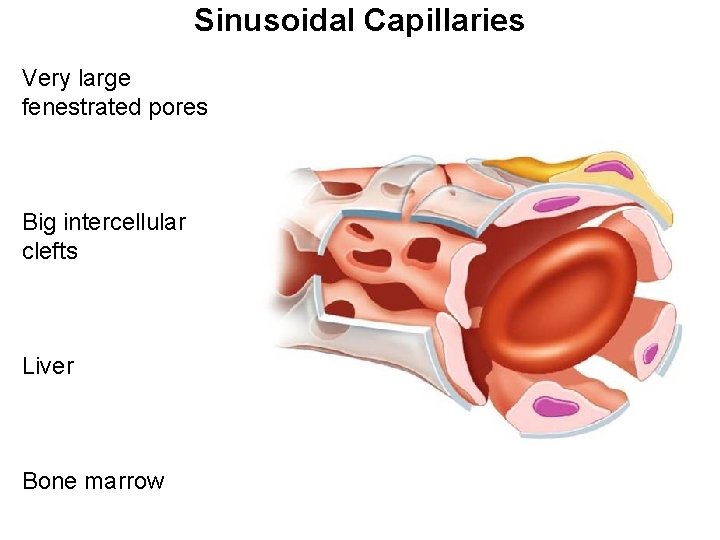
Sinusoidal Capillaries Very large fenestrated pores Big intercellular clefts Liver Bone marrow
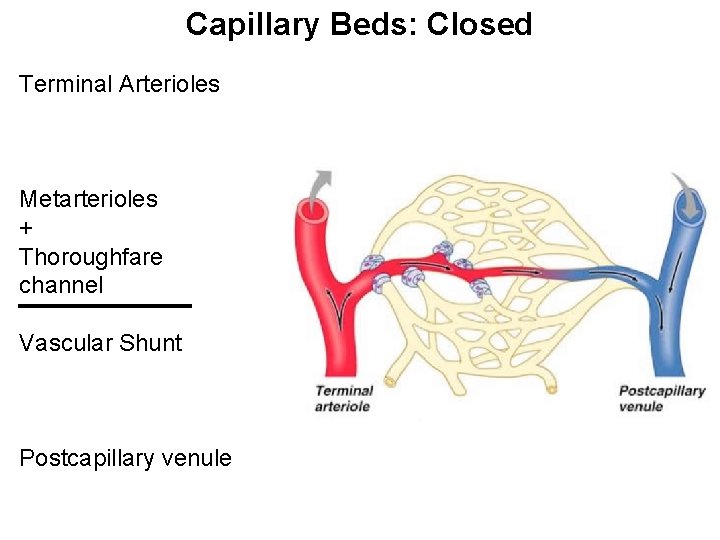
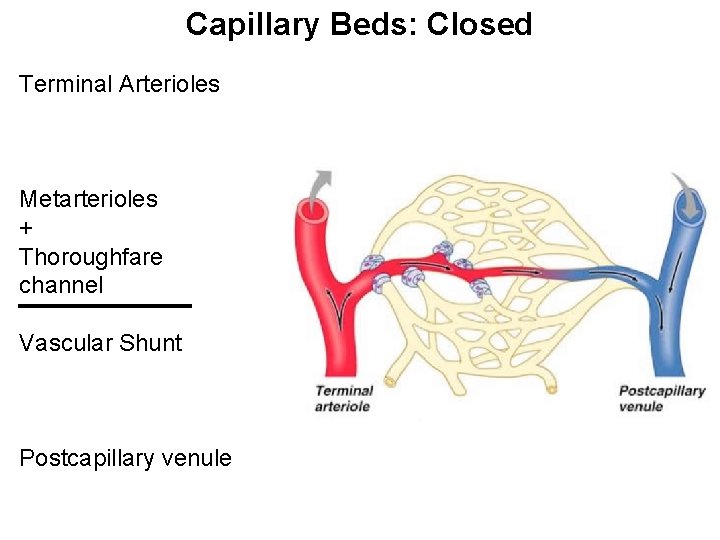
Capillary Beds: Closed Terminal Arterioles Metarterioles + Thoroughfare channel Vascular Shunt Postcapillary venule
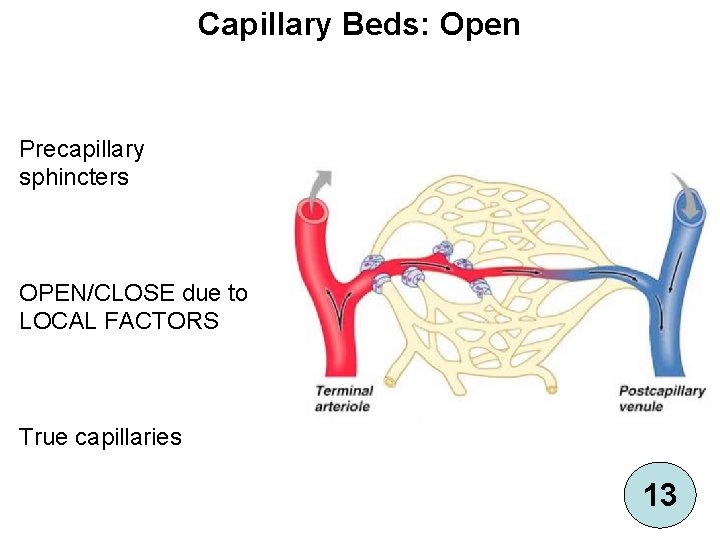
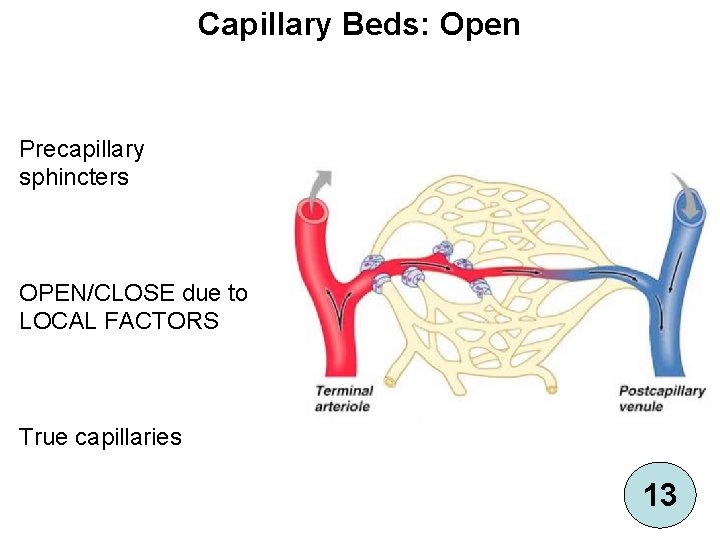
Capillary Beds: Open Precapillary sphincters OPEN/CLOSE due to LOCAL FACTORS True capillaries 13
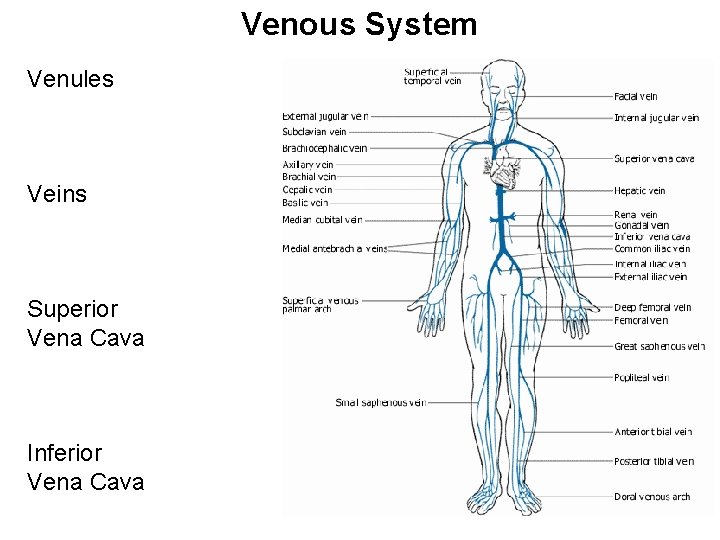
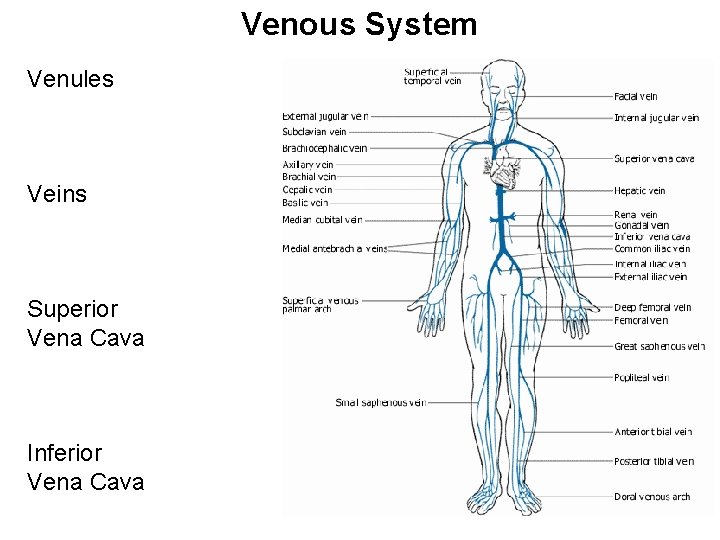
Venous System Venules Veins Superior Vena Cava Inferior Vena Cava
Systemic Venous System Large Lumen Thin walls Less smooth muscle Less elastin Holds ~65% of blood
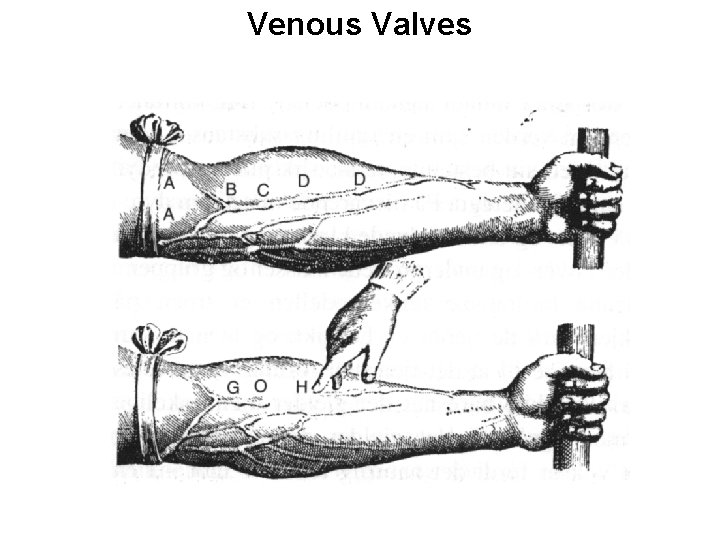
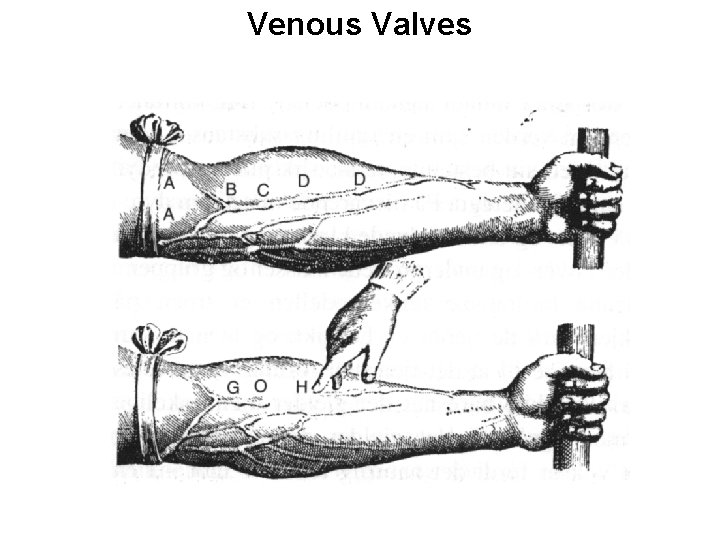
Venous Valves
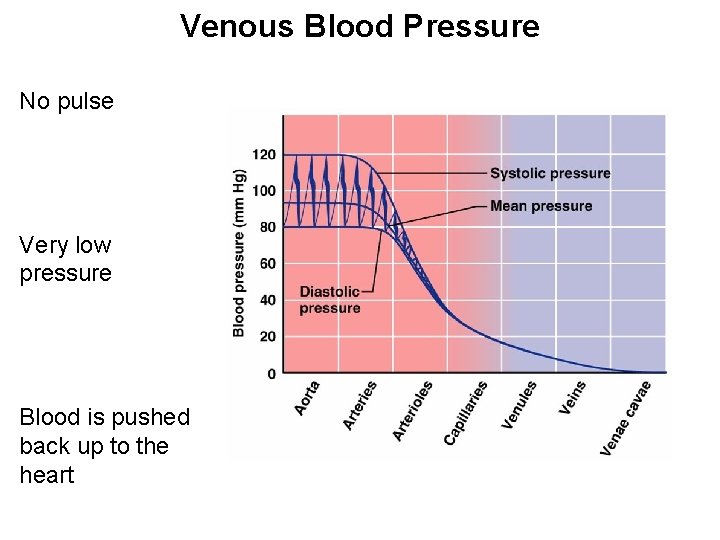
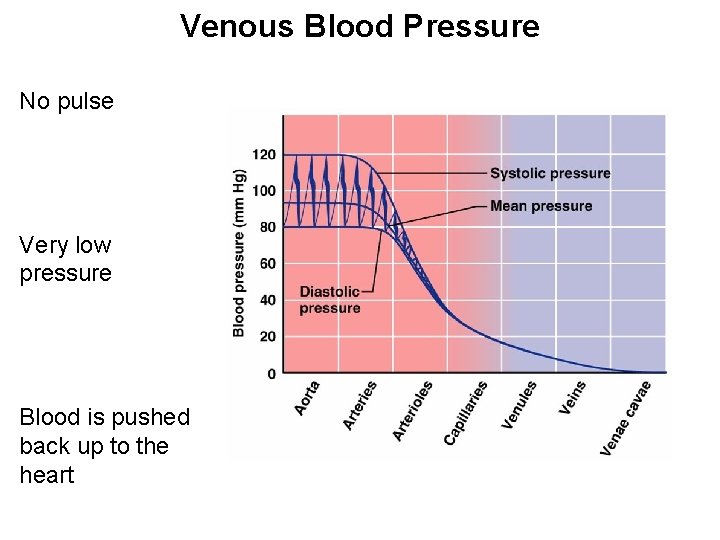
Venous Blood Pressure No pulse Very low pressure Blood is pushed back up to the heart
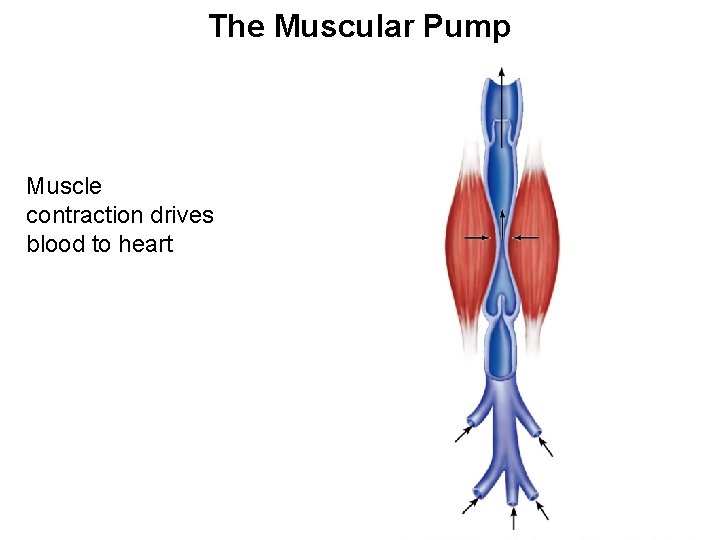
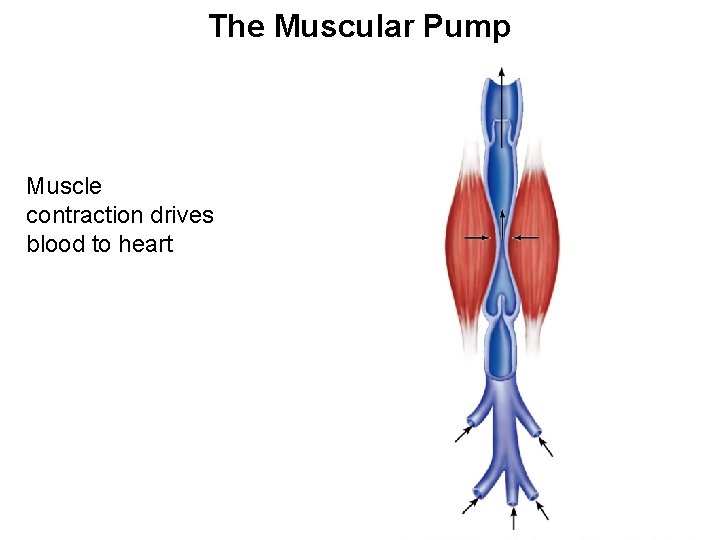
The Muscular Pump Muscle contraction drives blood to heart
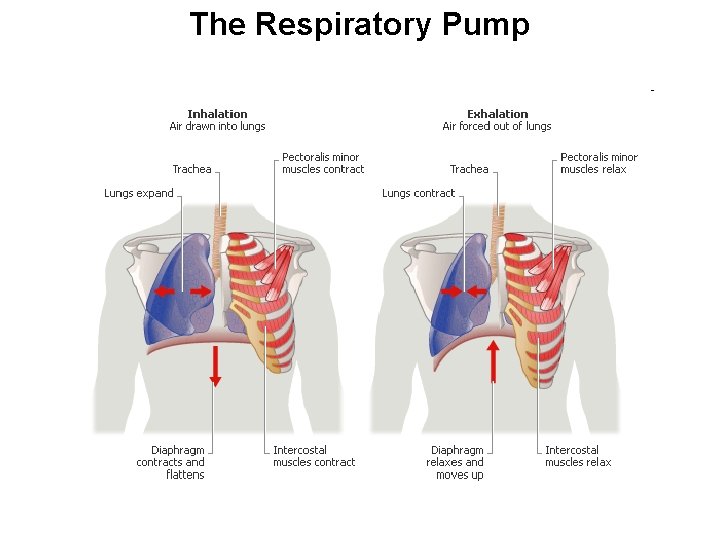
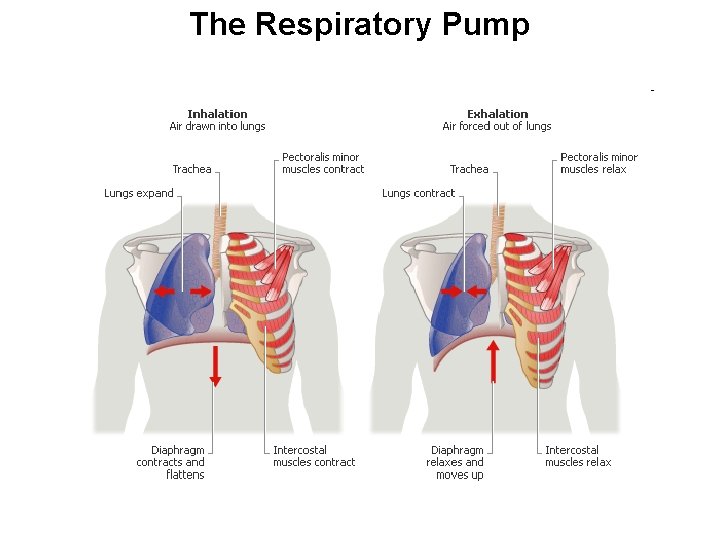
The Respiratory Pump
Flow Requires Pressure Differences Blood Flow Difference in Pressure
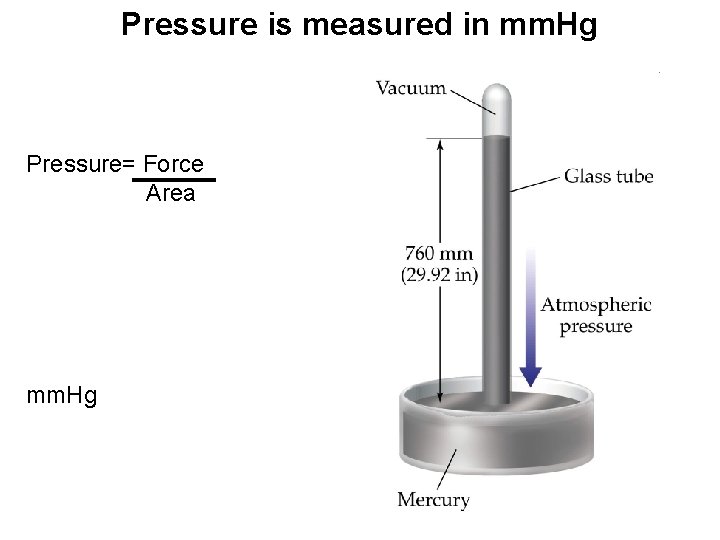
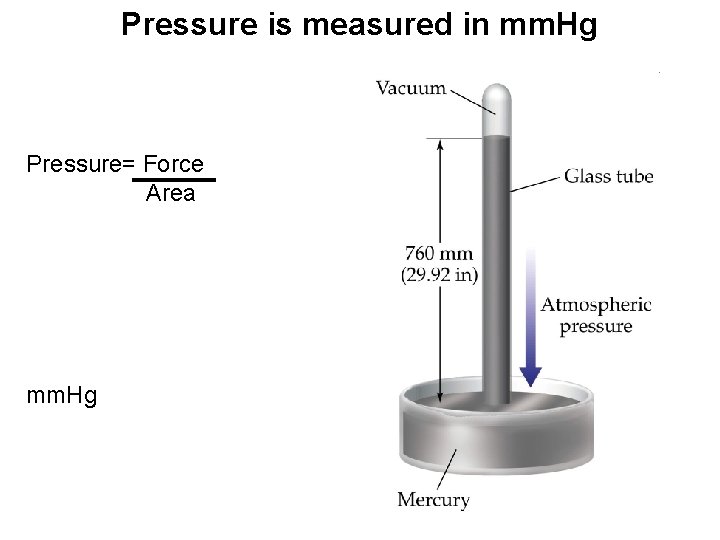
Pressure is measured in mm. Hg Pressure= Force Area mm. Hg
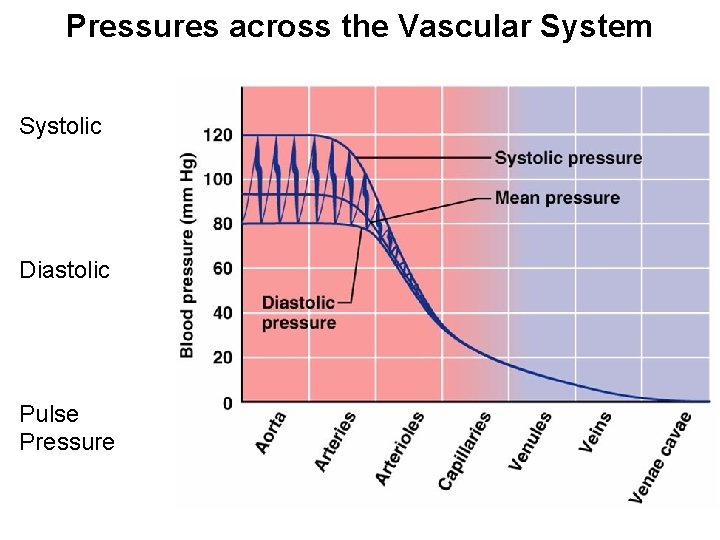
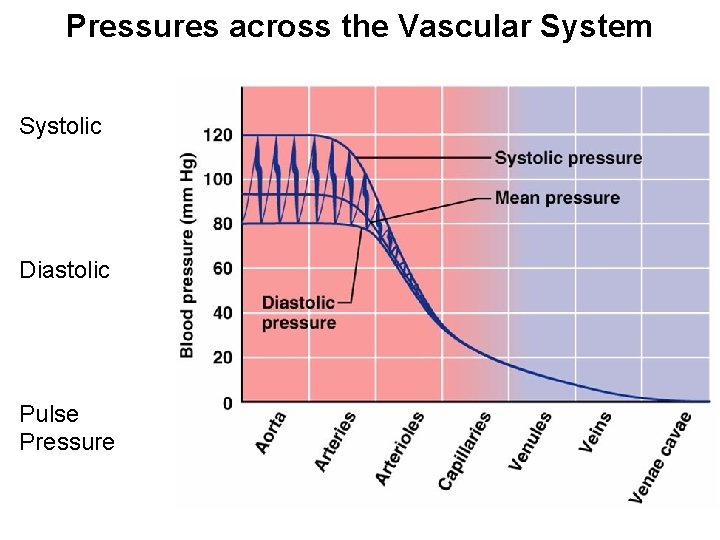
Pressures across the Vascular System Systolic Diastolic Pulse Pressure
Resistance Opposes Blood Flow Friction of blood moving through vessels Flow = ∆P R R is Peripheral Resistance (Systemic Circulation) (Will be printed on test)
One Equation to Rule them All (HR) (EDV-ESV) (R) = Δ P Difference in pressure between heart and capillary (Will be printed on test)
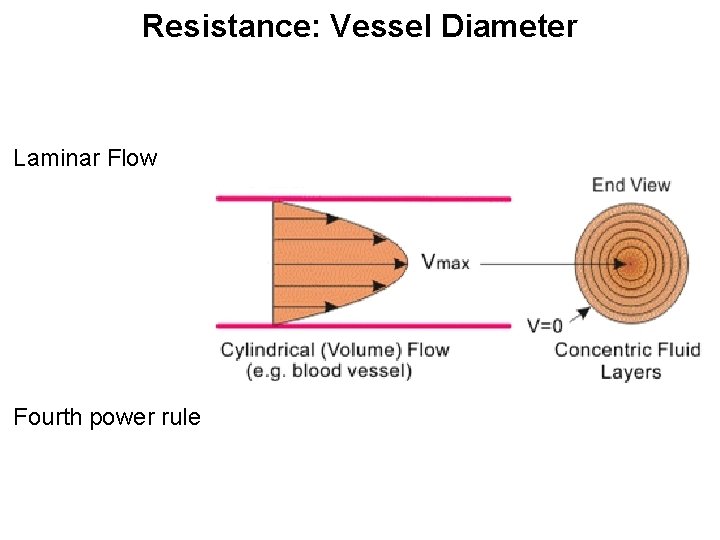
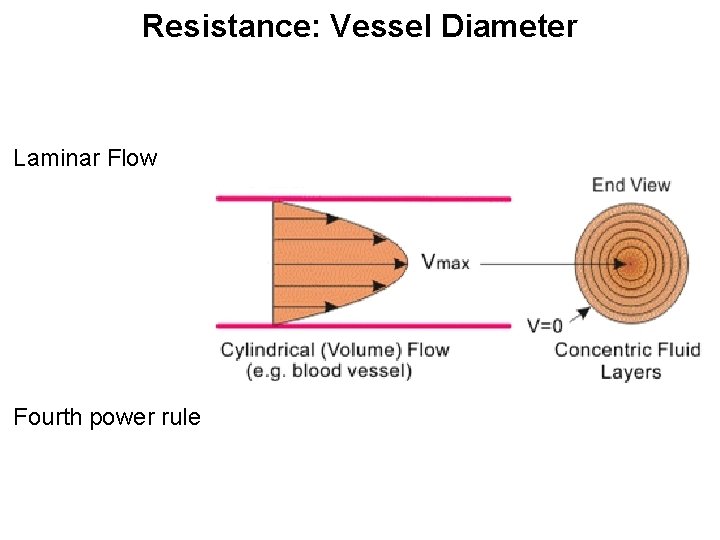
Resistance: Vessel Diameter Laminar Flow Fourth power rule
Resistance: Vessel Diameter Resistance low in conducting vessels Resistance in small arteries changes quickly
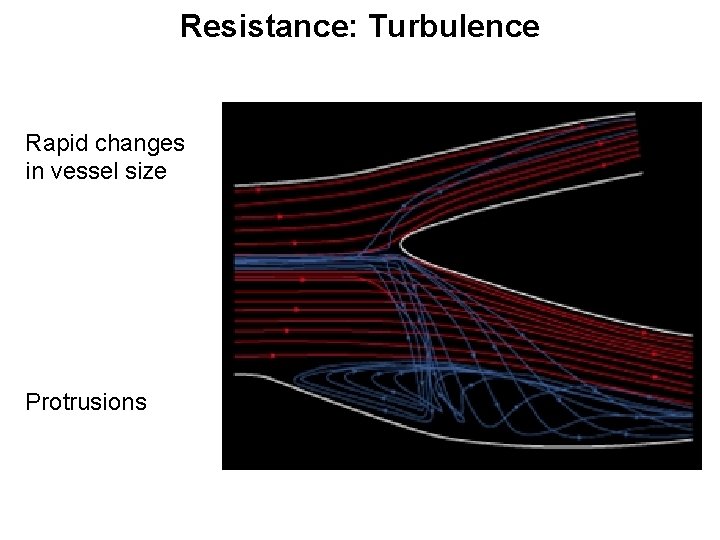
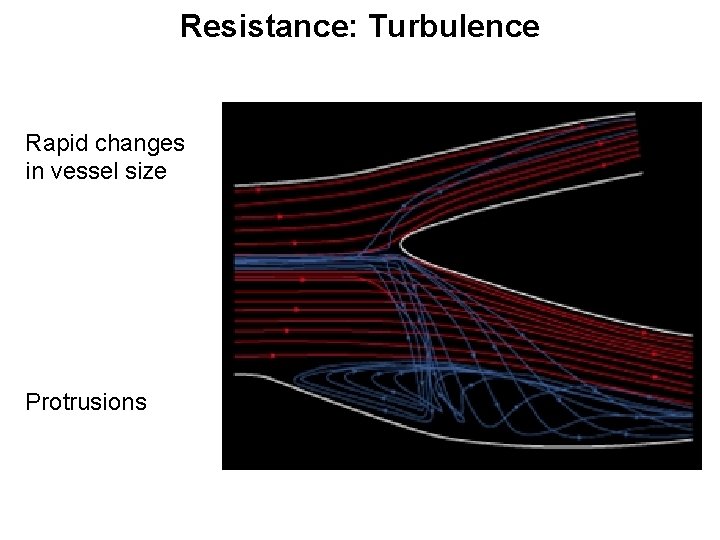
Resistance: Turbulence Rapid changes in vessel size Protrusions
Resistance: Viscosity Thickness of blood Polycythemia Anemia
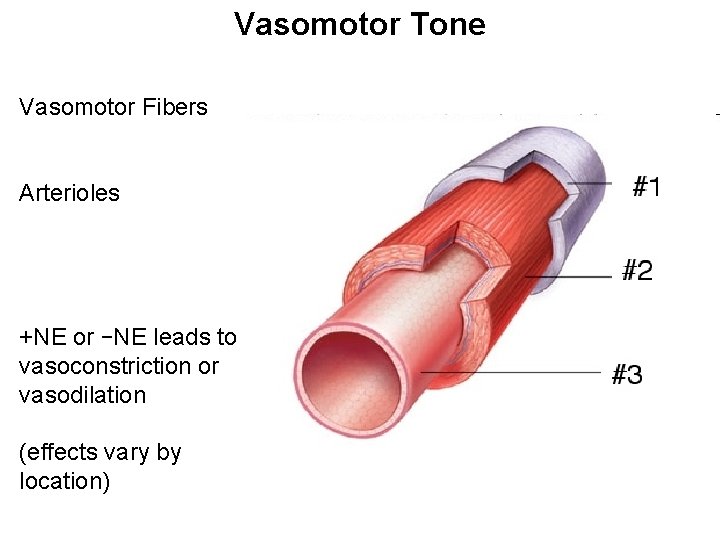
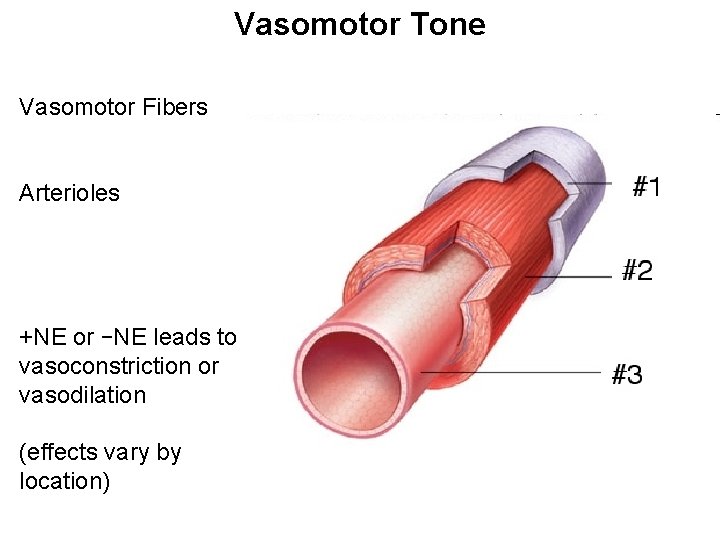
Vasomotor Tone Vasomotor Fibers Arterioles +NE or –NE leads to vasoconstriction or vasodilation (effects vary by location)
Short Term Hormonal Controls Norepinephrine and Epinephrine Atrial Natriuretic Peptide Angiotensin II
Norepinephrine and Epinephrine Vasodilation skeletal and cardiac muscle Vasoconstriction other organs CO
Atrial Natriuretic Peptide Myocardial cells of atria Vasodilation Decreases blood volume
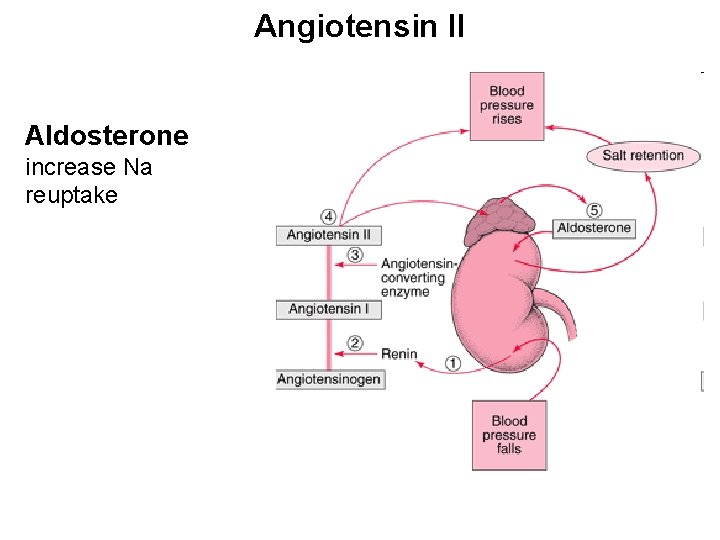
Angiotensin II Secreted by kidney if blood volume is low Vasoconstriction Increases Blood Volume
Long Term Control of Blood Pressure Blood Volume changes CO! More blood, more pressure Less blood, less pressure Renal
Direct Renal Mechanisms Less blood More H 2 O returned to blood More blood Less H 2 O returned to blood
A Very Brief Overview of Kidney Function Sodium follows water
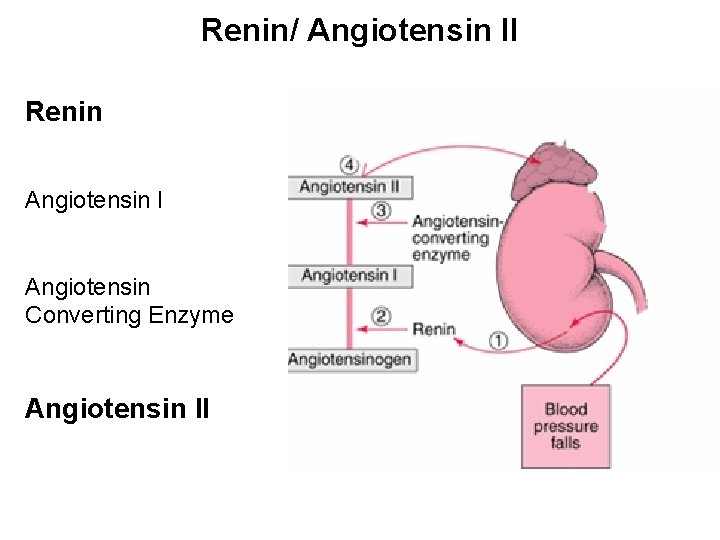
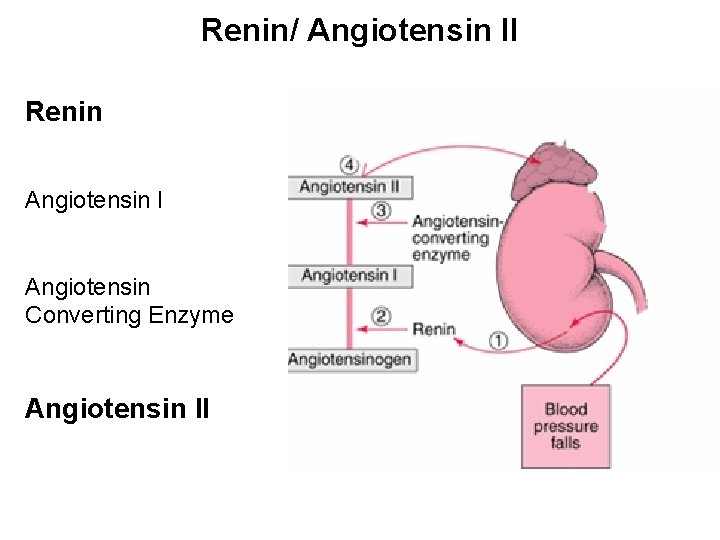
Renin/ Angiotensin II Renin Angiotensin I Angiotensin Converting Enzyme Angiotensin II
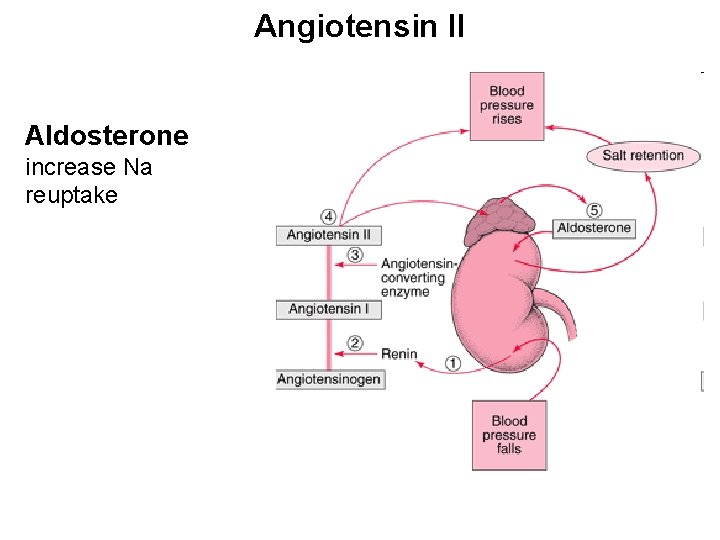
Angiotensin II Aldosterone increase Na reuptake
Atrial Natriuretic Peptide High Blood Pressure Blocks Aldosterone More Na and water leave as urine
Circulatory Shock Low blood pressure caused by unfilled vessels or abnormal circulation Hypovolemic Shock
Circulatory Shock Vascular Shock Anaphylactic Shock Septic Shock
Hypotension Low Blood Pressure Orthostatic Hypotension Chronic Hypotension
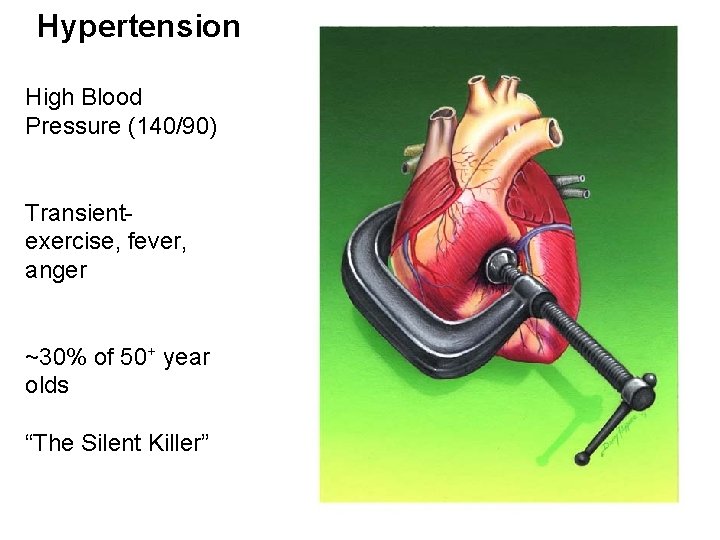
Hypertension High Blood Pressure (140/90) Transientexercise, fever, anger ~30% of 50+ year olds “The Silent Killer”
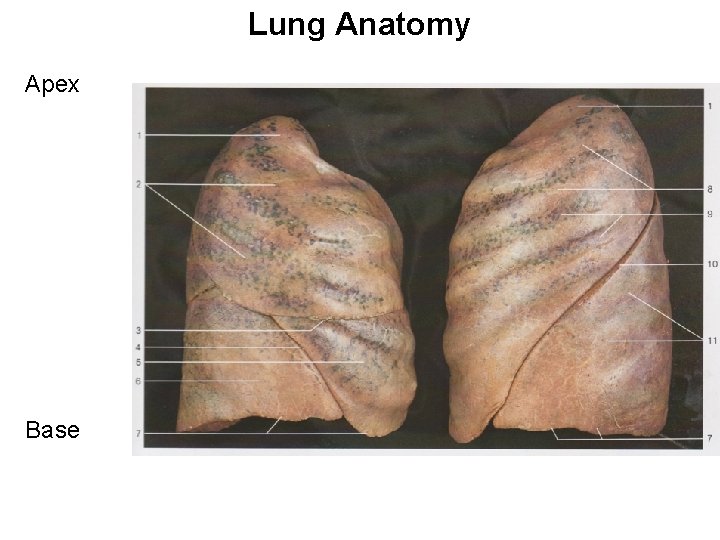
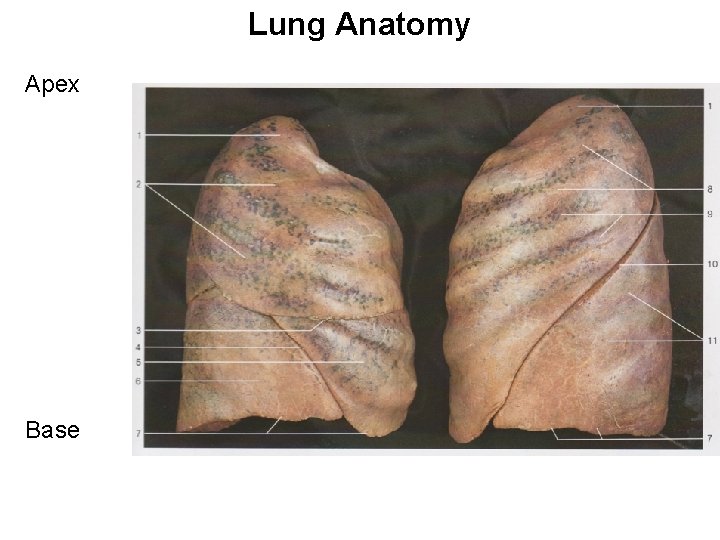
Lung Anatomy Apex Base
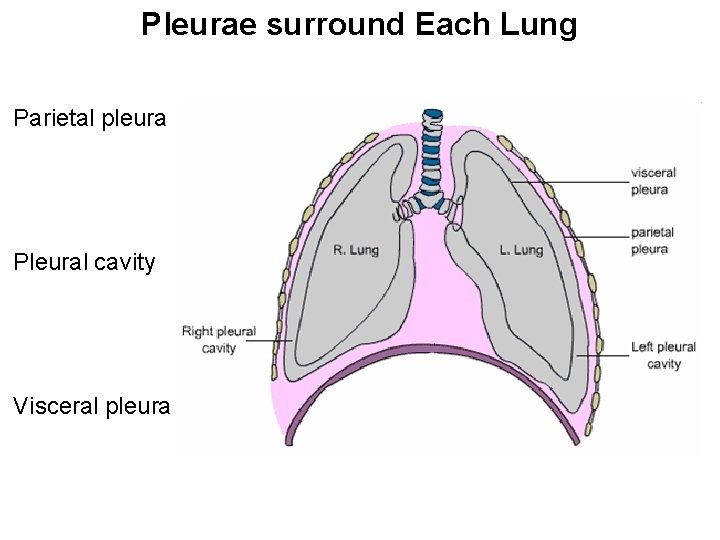
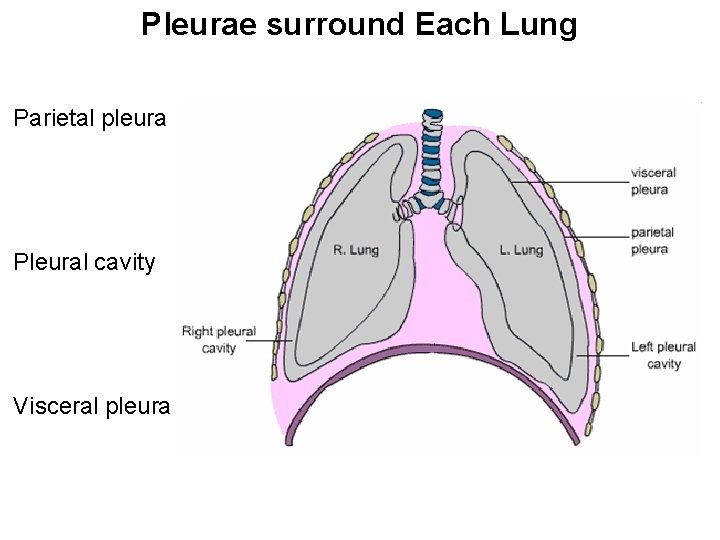
Pleurae surround Each Lung Parietal pleura Pleural cavity Visceral pleura
Pulmonary Ventilation Inspiration Expiration
Respiration Depends on Pressure and Flow Change in volume Change in pressure in lungs Change in air flow
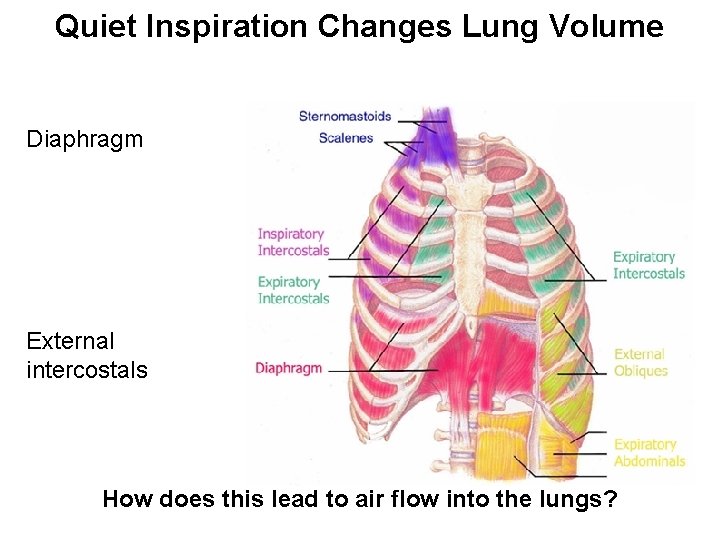
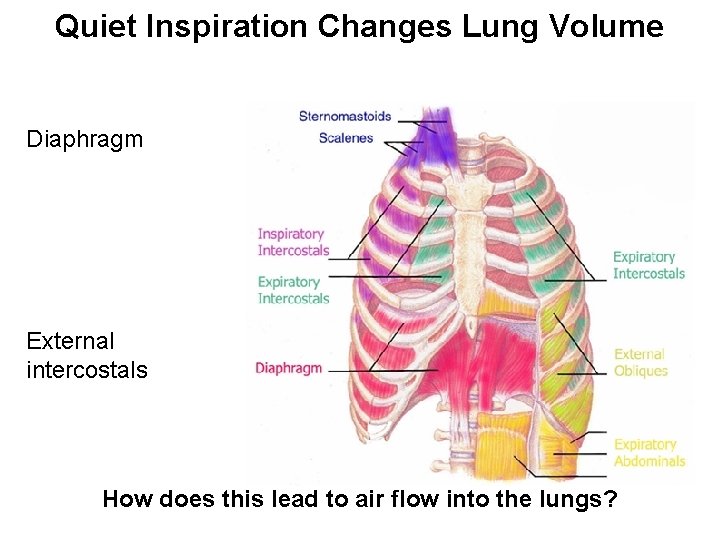
Quiet Inspiration Changes Lung Volume Diaphragm External intercostals How does this lead to air flow into the lungs?
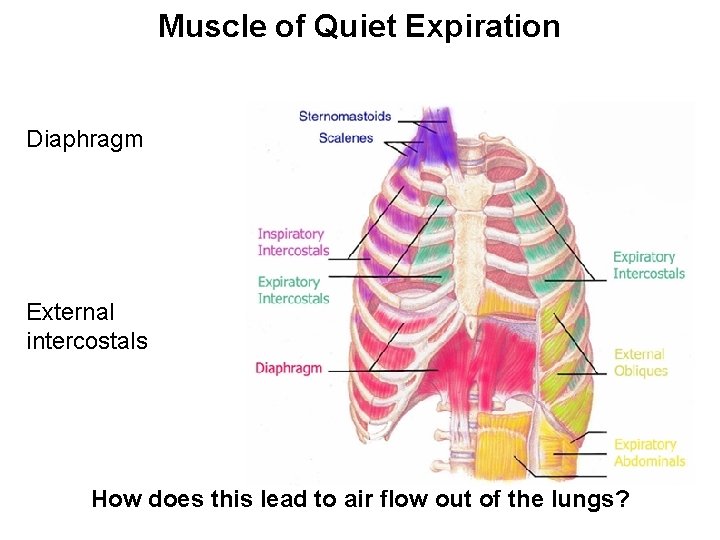
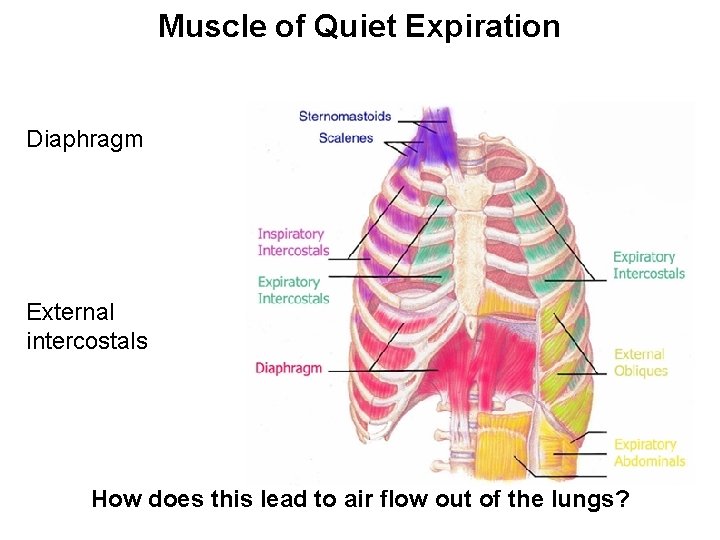
Muscle of Quiet Expiration Diaphragm External intercostals How does this lead to air flow out of the lungs?
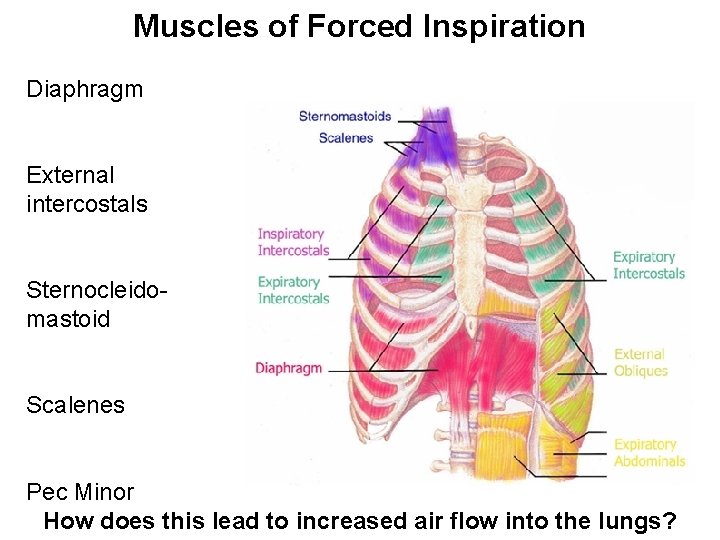
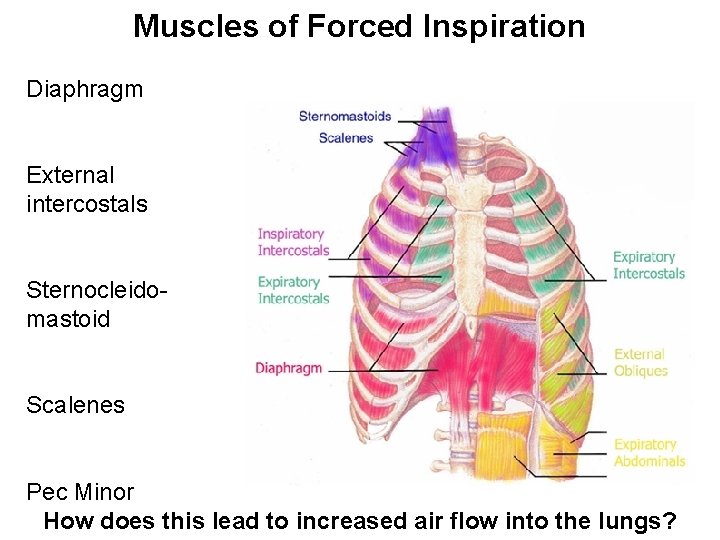
Muscles of Forced Inspiration Diaphragm External intercostals Sternocleidomastoid Scalenes Pec Minor How does this lead to increased air flow into the lungs?
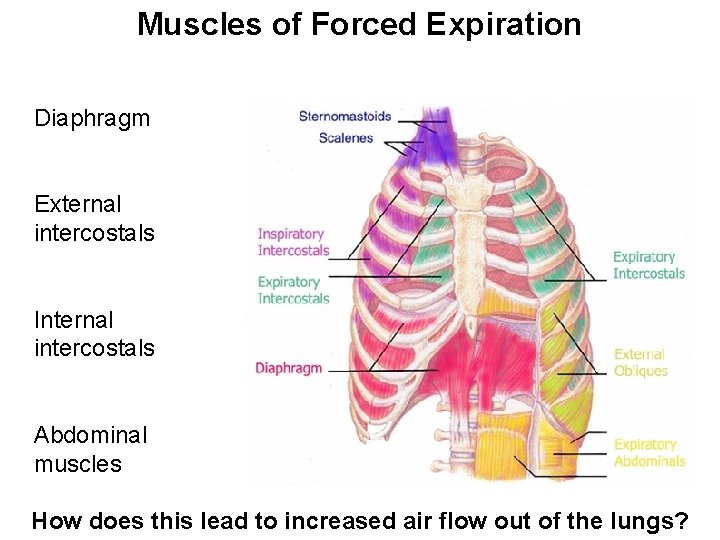
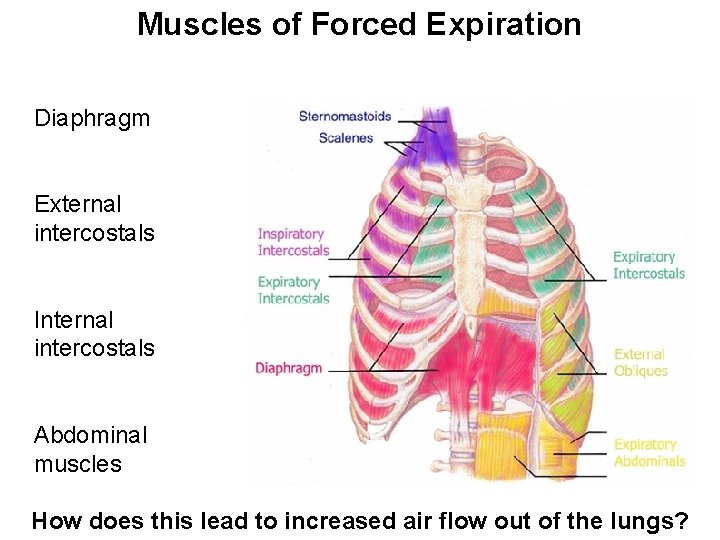
Muscles of Forced Expiration Diaphragm External intercostals Internal intercostals Abdominal muscles How does this lead to increased air flow out of the lungs?
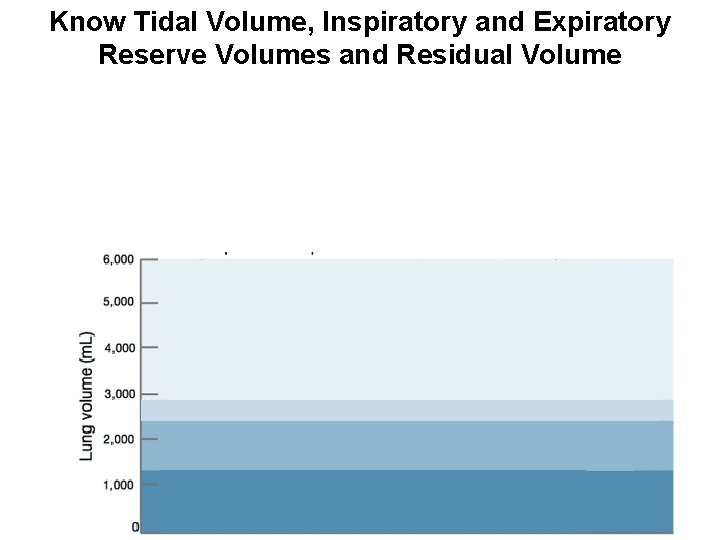
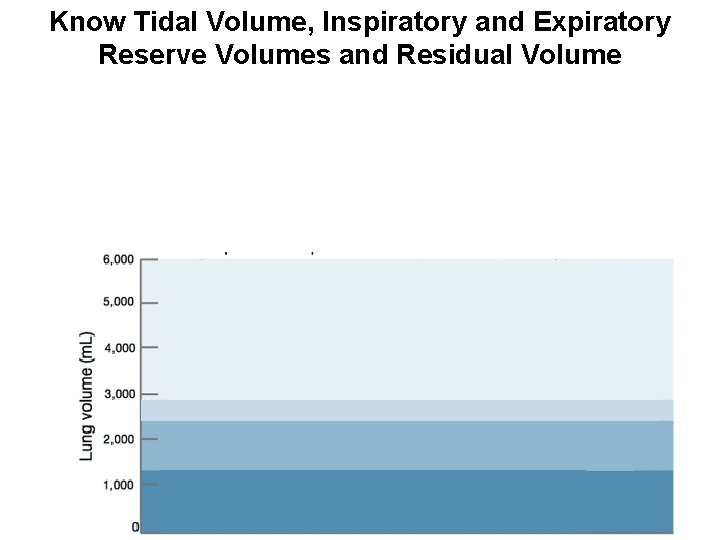
Know Tidal Volume, Inspiratory and Expiratory Reserve Volumes and Residual Volume
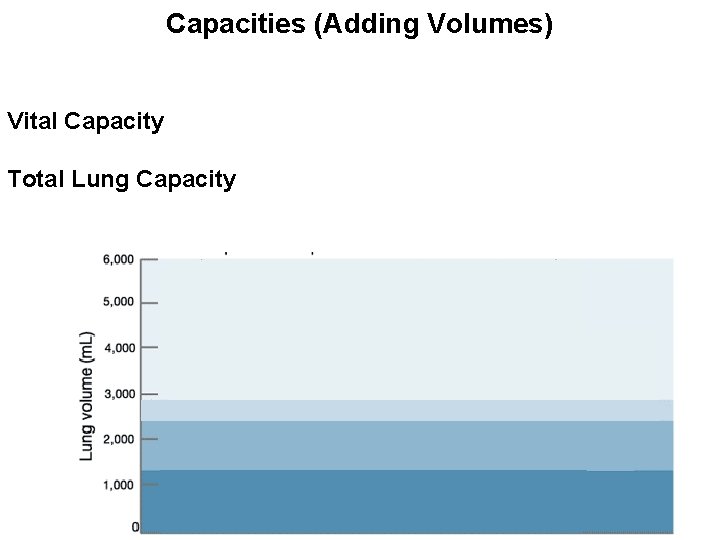
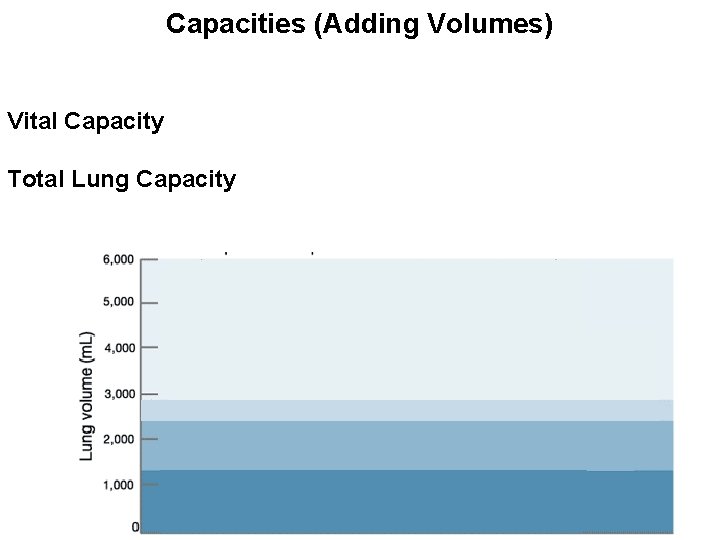
Capacities (Adding Volumes) Vital Capacity Total Lung Capacity
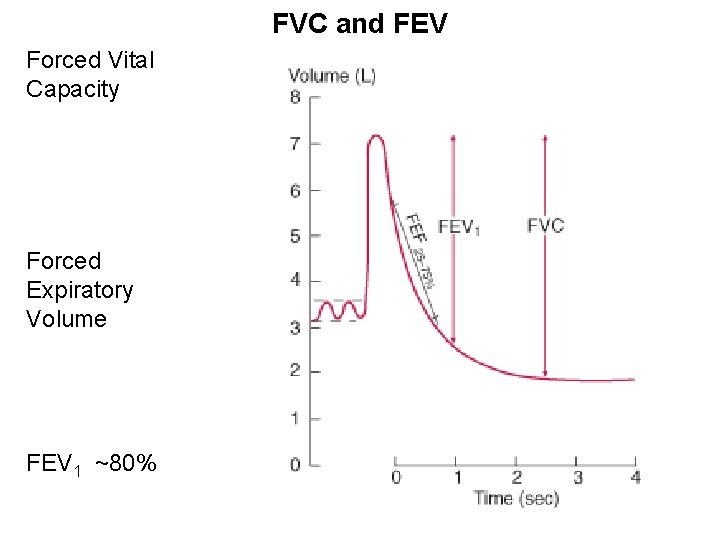
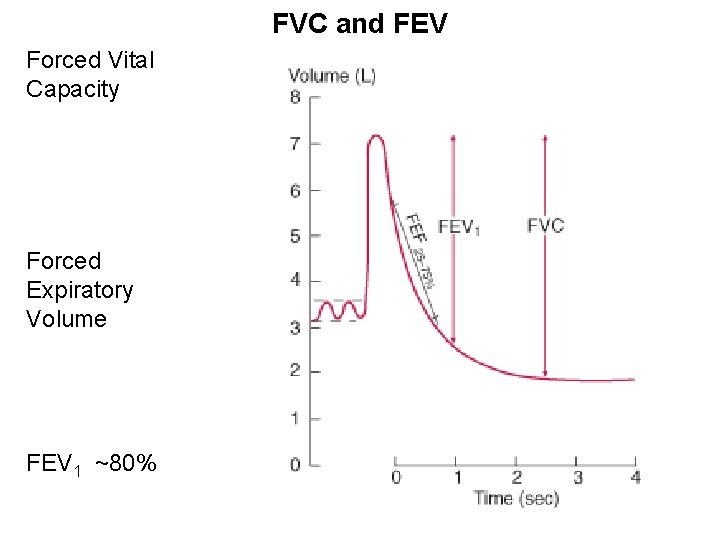
FVC and FEV Forced Vital Capacity Forced Expiratory Volume FEV 1 ~80%
FVC and FEV Obstructive Disorders Restrictive Disorders
Restrictive Disorders Reduction in lung capacities VLC, TLC, etc. Decrease in compliance “stretchiness” What would FVC and FEV look like?
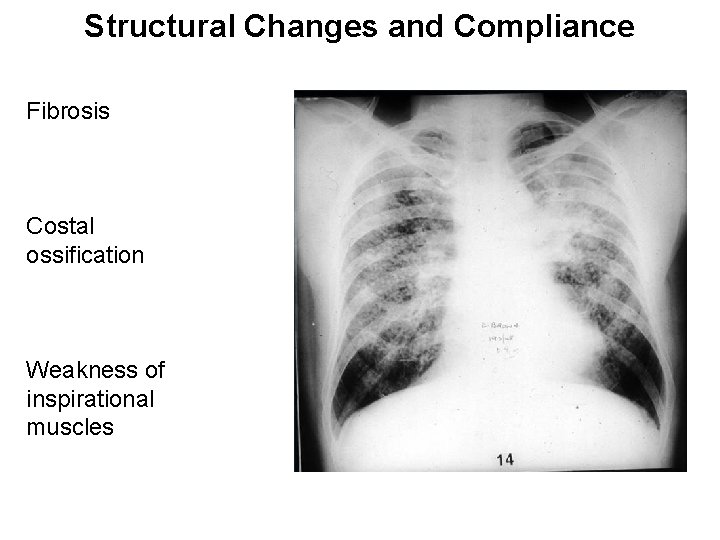
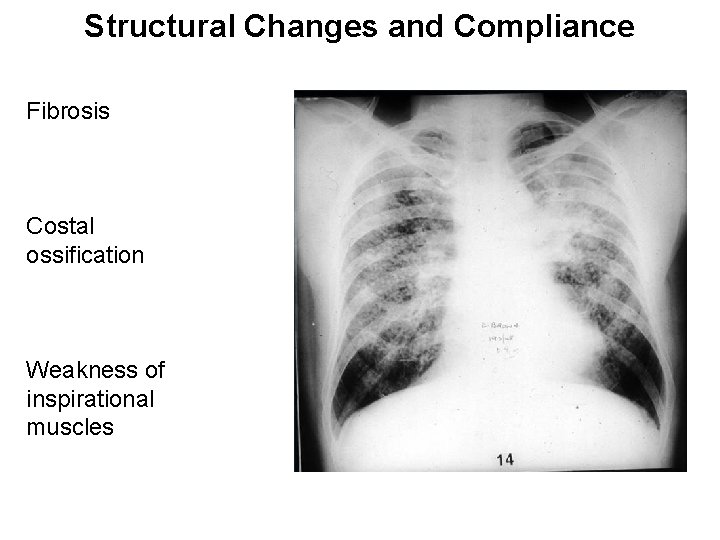
Structural Changes and Compliance Fibrosis Costal ossification Weakness of inspirational muscles
Obstructive Disorders Lung volume unchanged but air flow is restricted What would FVC and FEV look like? Minute ventilation