FRCR Clinical Radiology Lectures 1 Diagnostic Radiology Fluoroscopy
- Slides: 35
FRCR Clinical Radiology Lectures 1 Diagnostic Radiology Fluoroscopy and Fluorography Jenny Wilson Physicist
Objectives • To understand the basic physics of the production of X-rays • To describe basic measures of image quality • To state radiation quantities and understand the relationship between them • To understand the basic physics of image receptors
What should you know by the end? • Do you understand how X-rays are produced? • Do you understand what happens when X-rays pass through the patient and create an image? • What happens at the film or image receptor? Why do you get artefacts? • What factors affect image quality and patient dose?
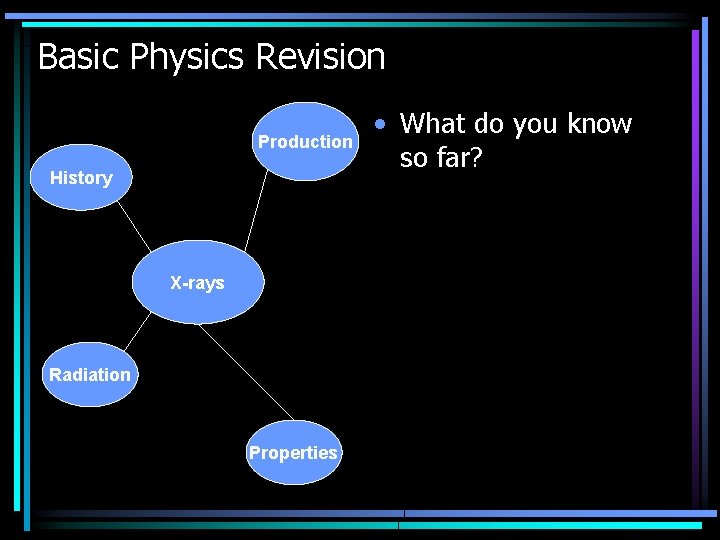
Basic Physics Revision Production History X-rays Radiation Properties • What do you know so far?
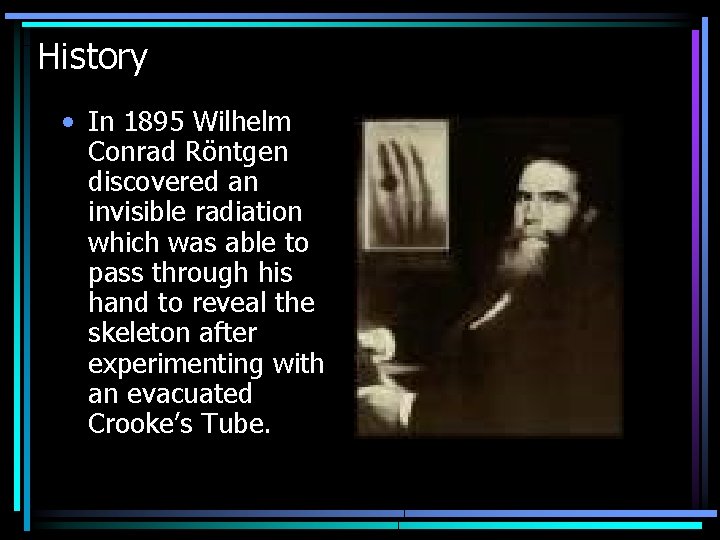
History • In 1895 Wilhelm Conrad Röntgen discovered an invisible radiation which was able to pass through his hand to reveal the skeleton after experimenting with an evacuated Crooke’s Tube.
History • He named the invisible radiation ‘X rays’ denoting their unknown origin • Within a year X-rays were being used for medical imaging • In 1901 Röntgen received the first Nobel Prize for his discovery
X-ray Radiation • • X-rays are electromagnetic radiation (as is light) Wave – Particle Duality Principle X-rays = X (ray) Photons
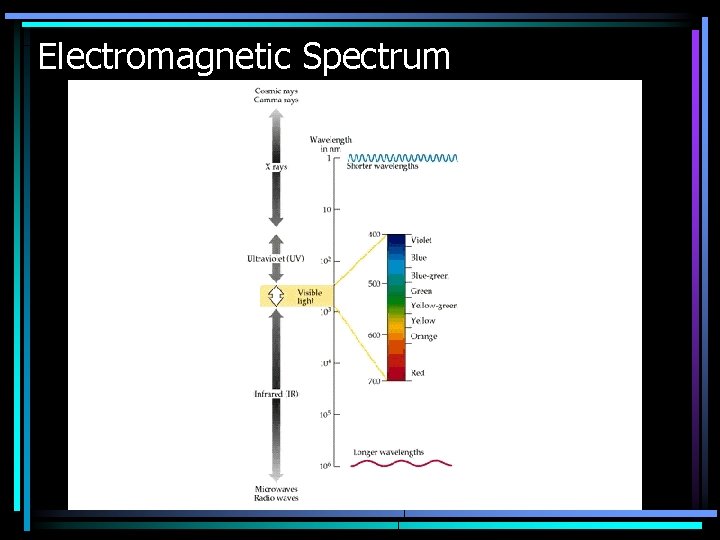
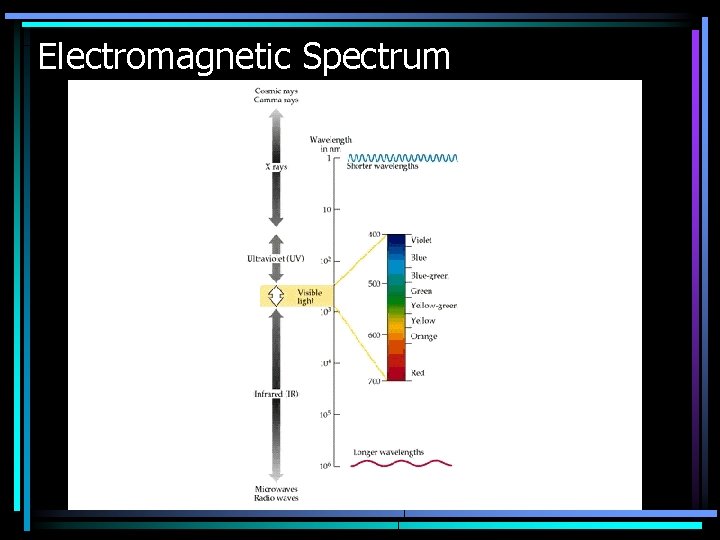
Electromagnetic Spectrum
X-ray Radiation • X-rays are a type of ionising radiation – they have enough energy to separate electrons from atomic nuclei • X-rays can pass through materials but are absorbed differently depending on the atomic number and thickness of the material. This is the basis of the X-ray image
X-ray Radiation • • Soft tissue is composed of ‘light’ elements such as H, C, N and O. Bones are composed of ‘heavier’ elements such as calcium. X-rays are attenuated more by the heavy elements so do not pass through to the film This property can be exploited by using a contrast agent made of very heavy elements, such as barium
Production of X-rays – 1 Basic Idea 1. Beam of electrons from heated –ve filament (i. e. a current) 2. Electrons directed towards a +ve target due to a potential (kilovoltage) difference 3. Electrons hit heavy metal target (Tungsten, Z=74) 4. X-rays are produced during interactions with the heavy metal nucleus
Production of X-rays – 2 Illustration
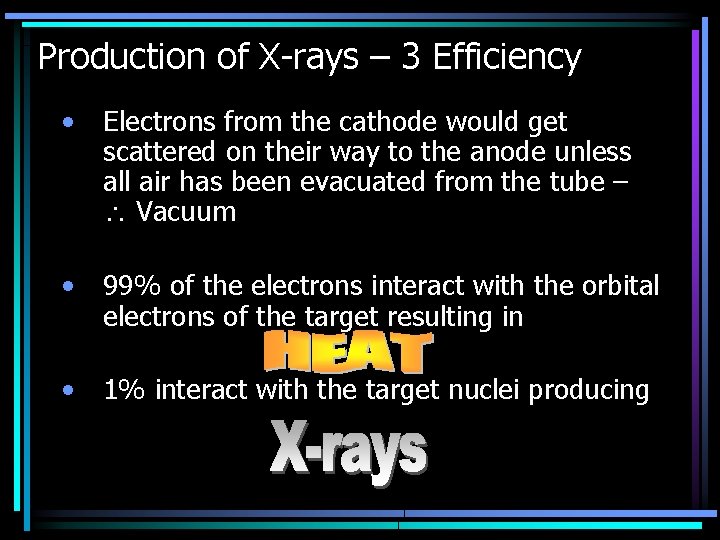
Production of X-rays – 3 Efficiency • Electrons from the cathode would get scattered on their way to the anode unless all air has been evacuated from the tube – Vacuum • 99% of the electrons interact with the orbital electrons of the target resulting in • 1% interact with the target nuclei producing
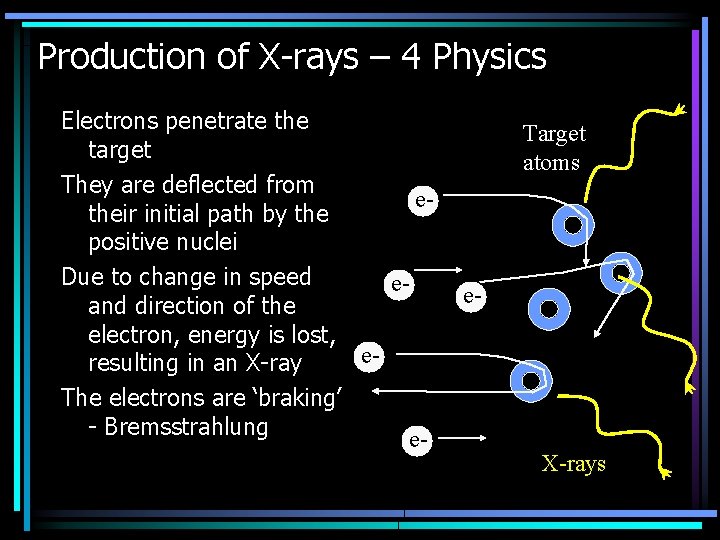
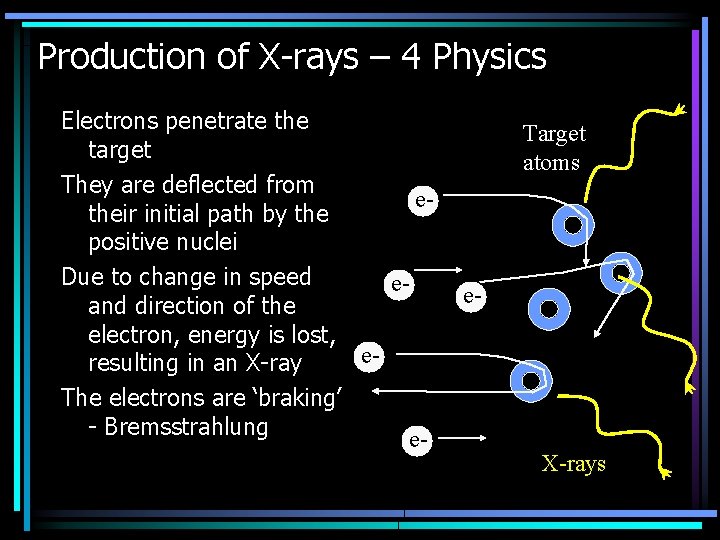
Production of X-rays – 4 Physics Electrons penetrate the target They are deflected from etheir initial path by the positive nuclei Due to change in speed eand direction of the electron, energy is lost, eresulting in an X-ray The electrons are ‘braking’ - Bremsstrahlung e- Target atoms e- X-rays
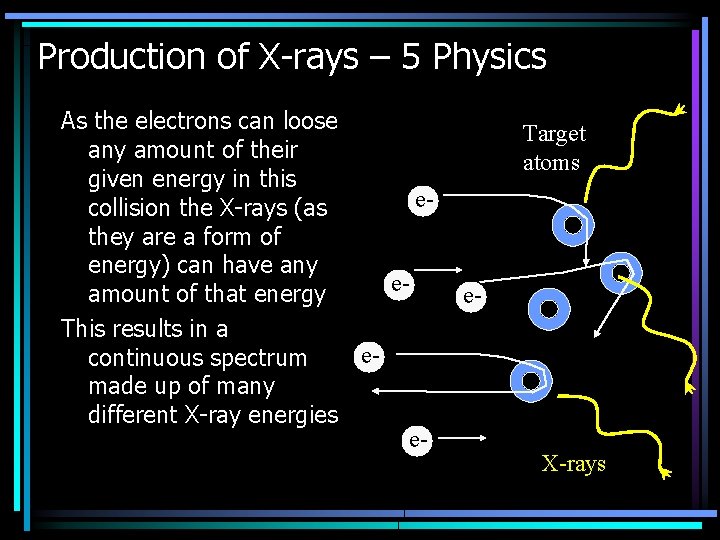
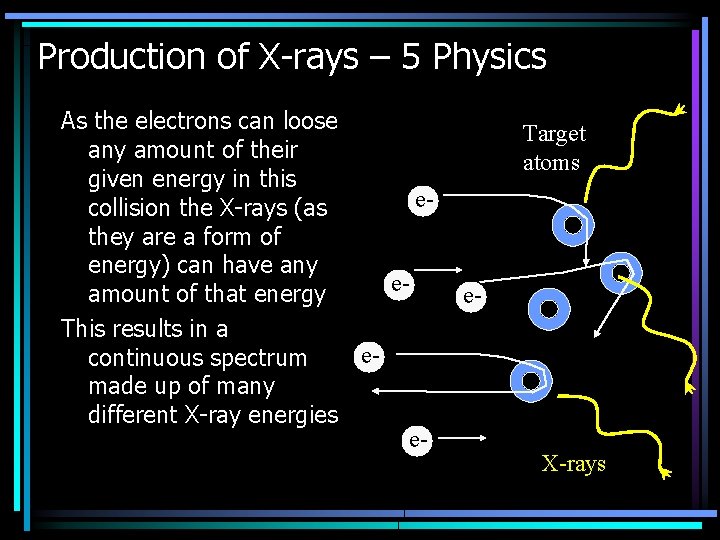
Production of X-rays – 5 Physics As the electrons can loose any amount of their given energy in this ecollision the X-rays (as they are a form of energy) can have any eamount of that energy This results in a econtinuous spectrum made up of many different X-ray energies e- Target atoms e- X-rays
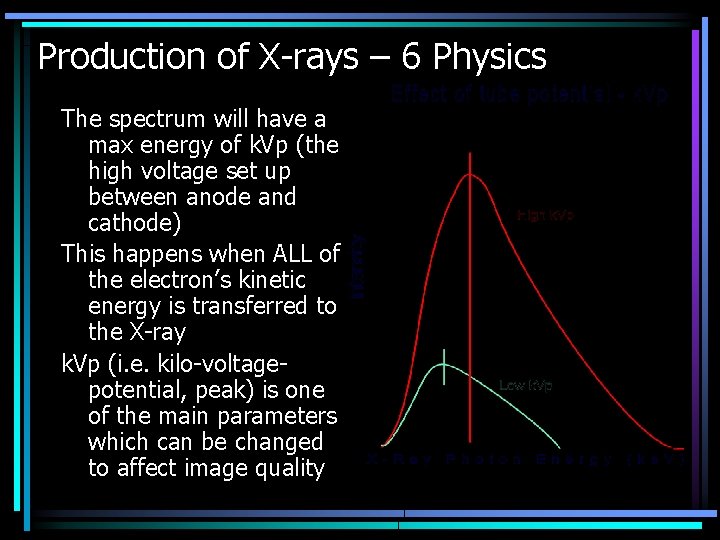
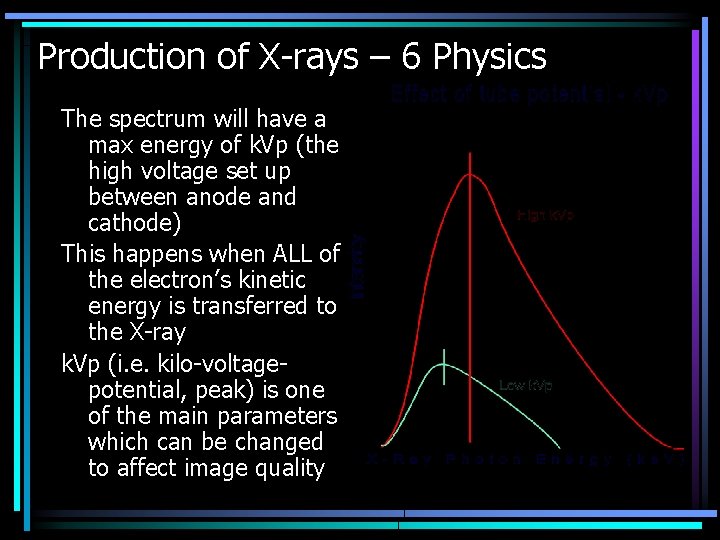
Production of X-rays – 6 Physics The spectrum will have a max energy of k. Vp (the high voltage set up between anode and cathode) This happens when ALL of the electron’s kinetic energy is transferred to the X-ray k. Vp (i. e. kilo-voltagepotential, peak) is one of the main parameters which can be changed to affect image quality
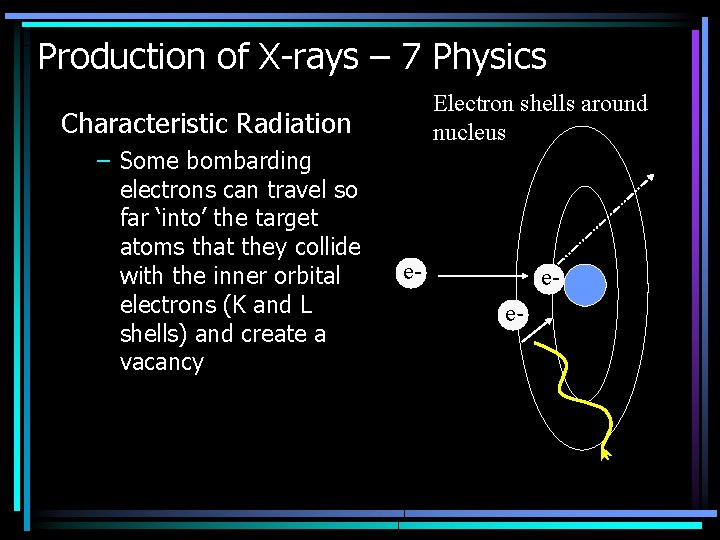
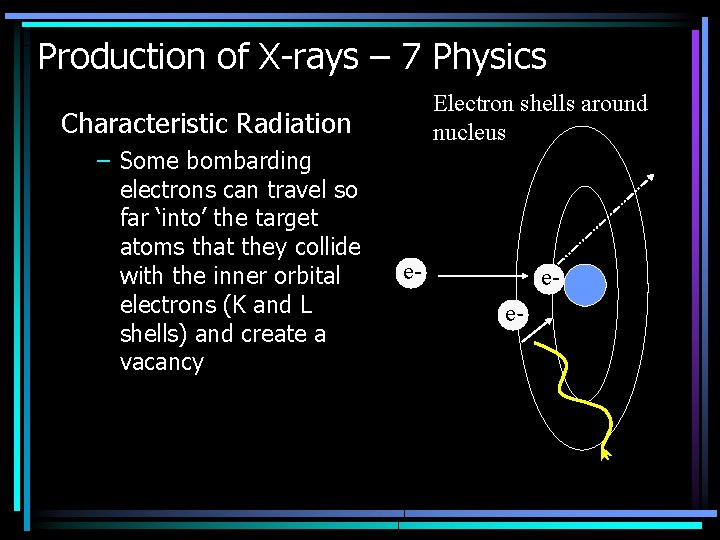
Production of X-rays – 7 Physics Electron shells around nucleus Characteristic Radiation – Some bombarding electrons can travel so far ‘into’ the target atoms that they collide with the inner orbital electrons (K and L shells) and create a vacancy e- ee-
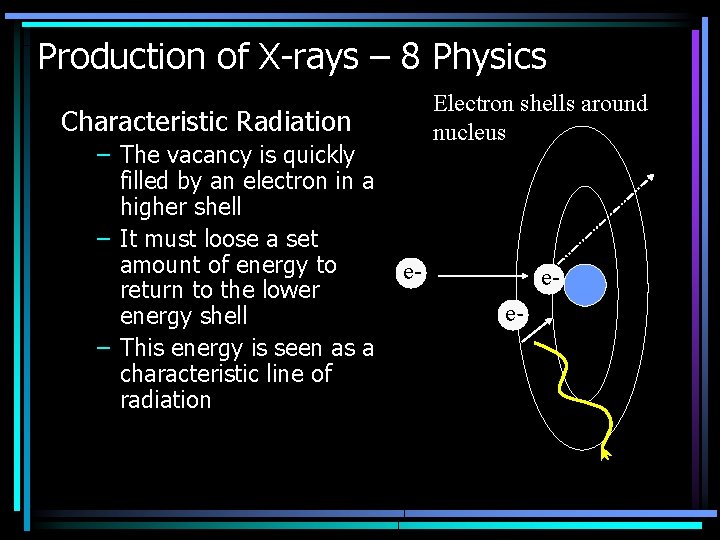
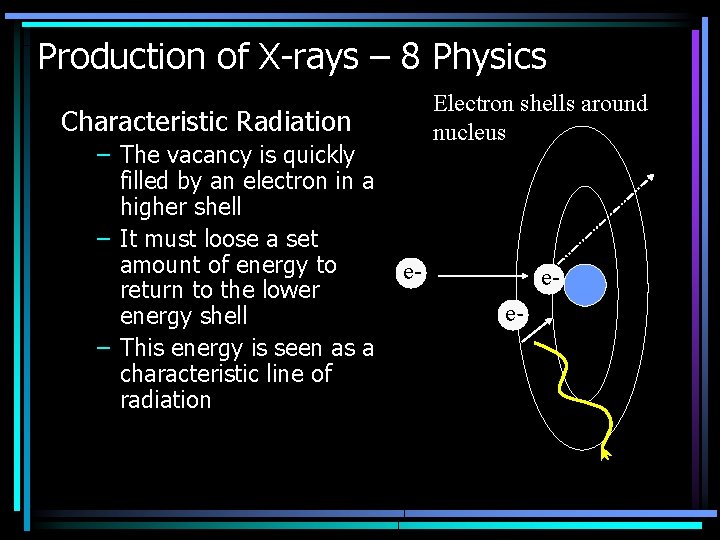
Production of X-rays – 8 Physics Electron shells around nucleus Characteristic Radiation – The vacancy is quickly filled by an electron in a higher shell – It must loose a set amount of energy to return to the lower energy shell – This energy is seen as a characteristic line of radiation e- ee-
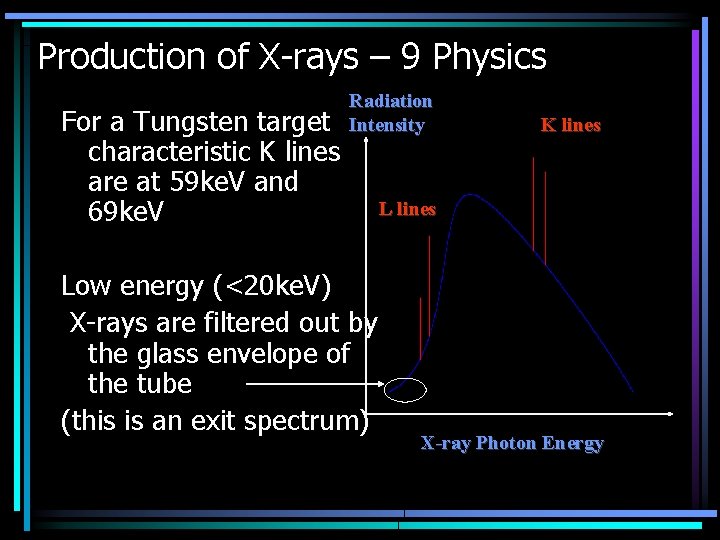
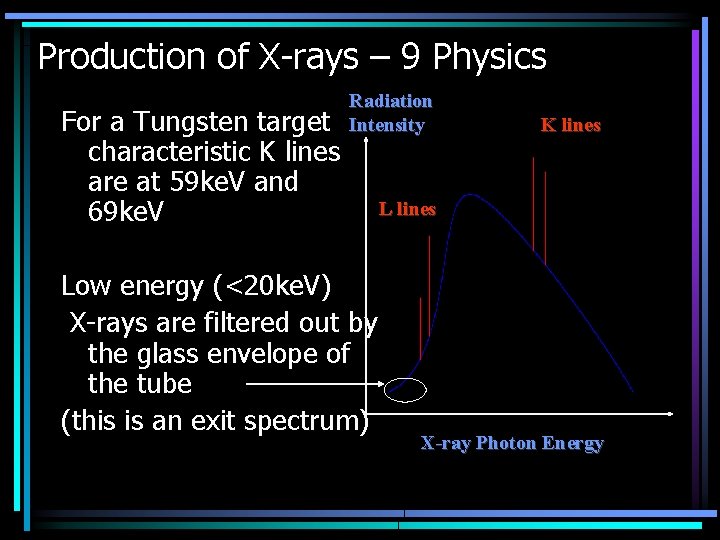
Production of X-rays – 9 Physics For a Tungsten target characteristic K lines are at 59 ke. V and 69 ke. V Radiation Intensity Low energy (<20 ke. V) X-rays are filtered out by the glass envelope of the tube (this is an exit spectrum) K lines L lines X-ray Photon Energy
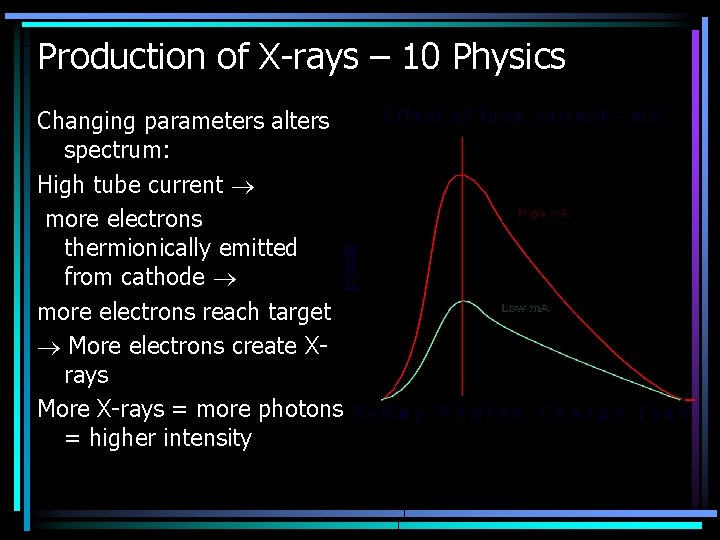
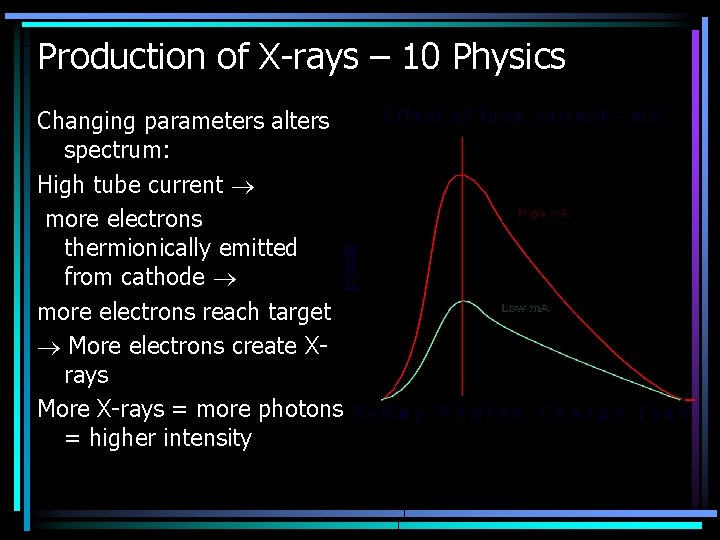
Production of X-rays – 10 Physics Changing parameters alters spectrum: High tube current more electrons thermionically emitted from cathode more electrons reach target More electrons create Xrays More X-rays = more photons = higher intensity
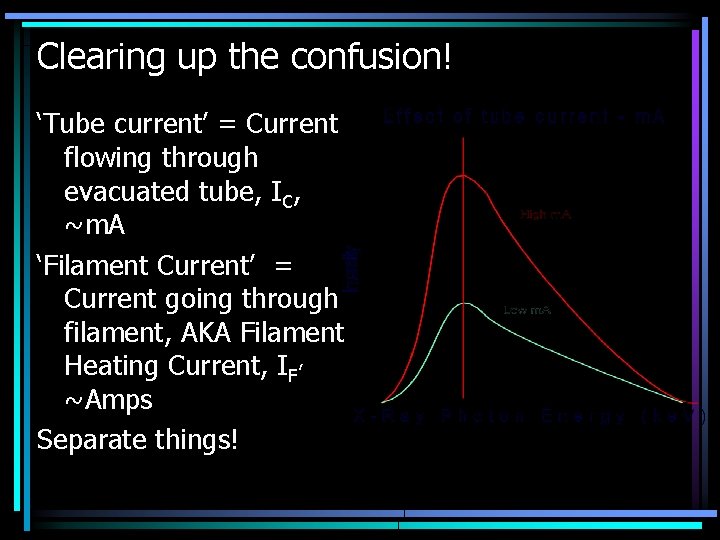
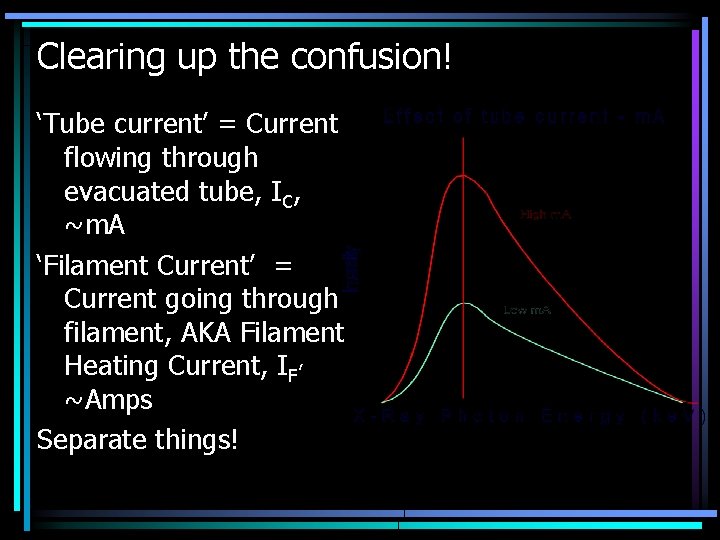
Clearing up the confusion! ‘Tube current’ = Current flowing through evacuated tube, IC, ~m. A ‘Filament Current’ = Current going through filament, AKA Filament Heating Current, IF, ~Amps Separate things!
Tube Current • Low current running inside glass envelope via travelling electrons (~milli-Amps) • Current flows through the vacuum • Tube voltage and Tube current obviously related (Ohms law) • As k. V increases, more electrons are pulled to the anode – this is the basis of a higher tube current occuring (more electrons, more charge per unit time)
Tube Current • If filament current is fixed, a set number of electrons are in the electron cloud per unit time. • In a perfect vaccum, once all these have passed to the anode the tube current will be at a constant maximum • But, always some spare electrons (space charge)! Slight rise in tube current as k. V increases and they are pulled towards the target
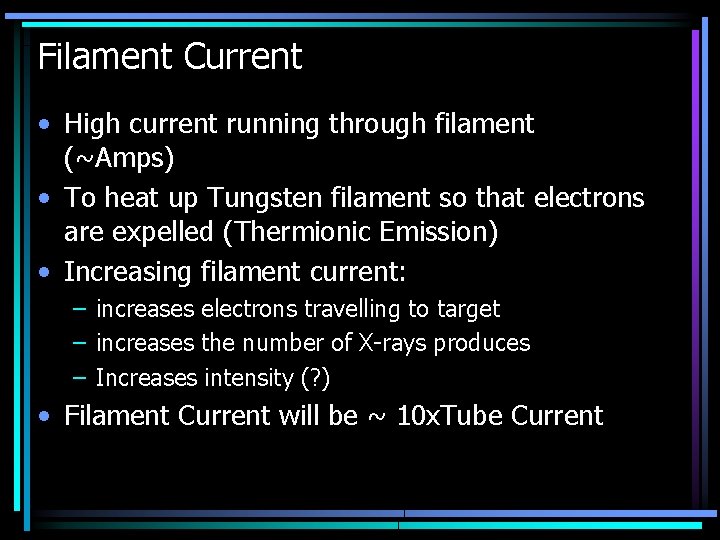
Filament Current • High current running through filament (~Amps) • To heat up Tungsten filament so that electrons are expelled (Thermionic Emission) • Increasing filament current: – increases electrons travelling to target – increases the number of X-rays produces – Increases intensity (? ) • Filament Current will be ~ 10 x. Tube Current
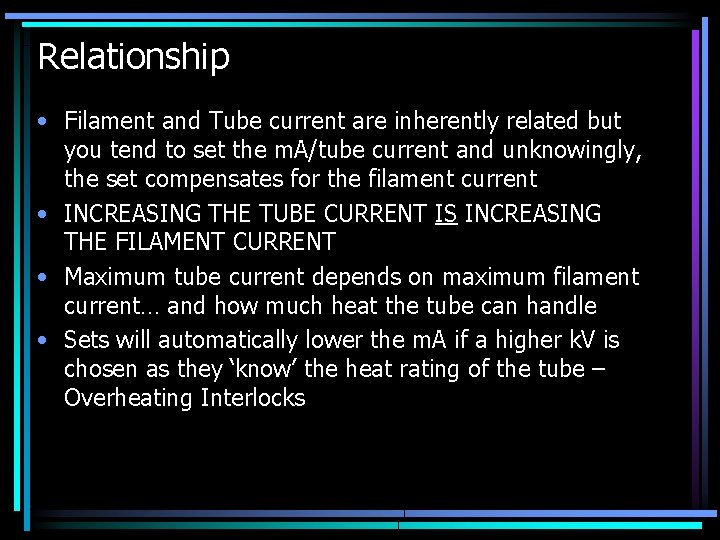
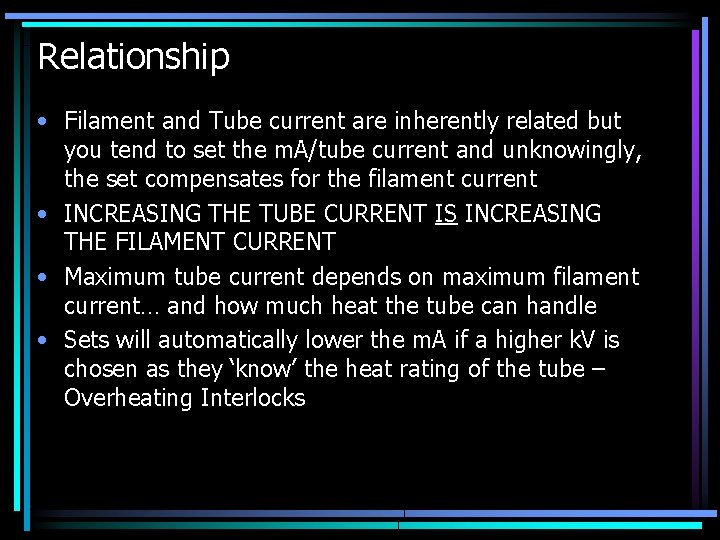
Relationship • Filament and Tube current are inherently related but you tend to set the m. A/tube current and unknowingly, the set compensates for the filament current • INCREASING THE TUBE CURRENT IS INCREASING THE FILAMENT CURRENT • Maximum tube current depends on maximum filament current… and how much heat the tube can handle • Sets will automatically lower the m. A if a higher k. V is chosen as they ‘know’ the heat rating of the tube – Overheating Interlocks
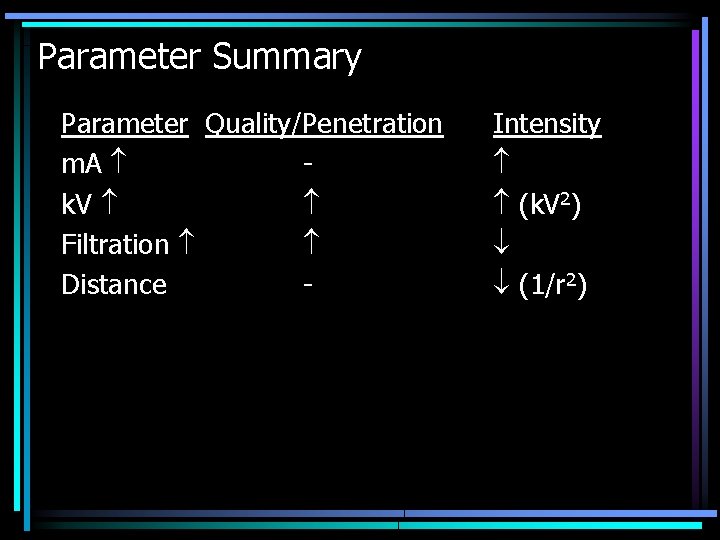
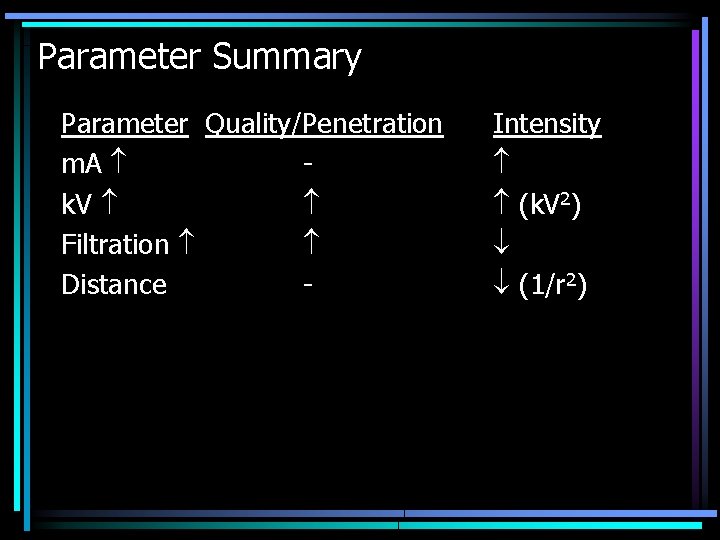
Parameter Summary Parameter Quality/Penetration m. A k. V Filtration Distance - Intensity (k. V 2) (1/r 2)
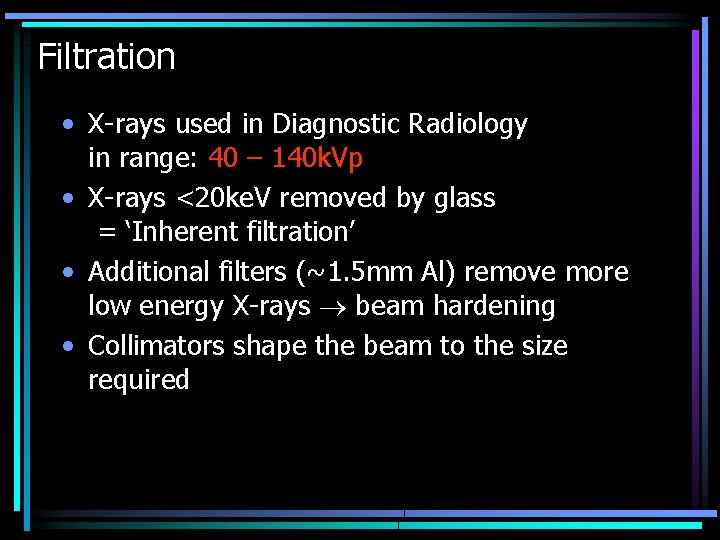
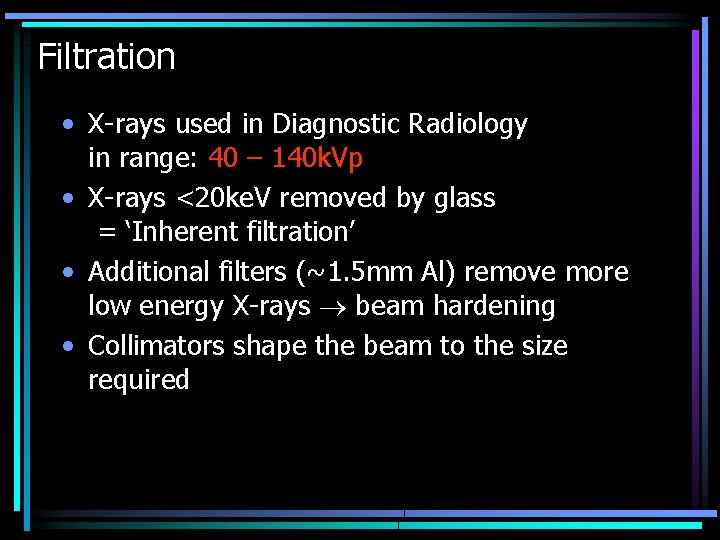
Filtration • X-rays used in Diagnostic Radiology in range: 40 – 140 k. Vp • X-rays <20 ke. V removed by glass = ‘Inherent filtration’ • Additional filters (~1. 5 mm Al) remove more low energy X-rays beam hardening • Collimators shape the beam to the size required
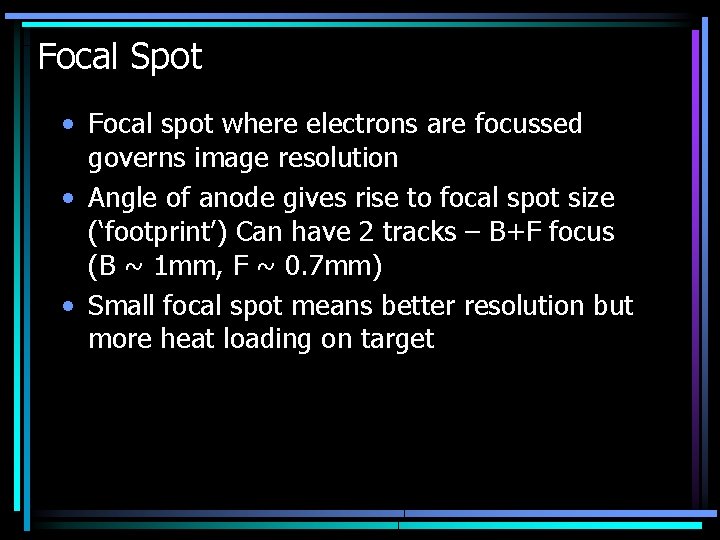
Focal Spot • Focal spot where electrons are focussed governs image resolution • Angle of anode gives rise to focal spot size (‘footprint’) Can have 2 tracks – B+F focus (B ~ 1 mm, F ~ 0. 7 mm) • Small focal spot means better resolution but more heat loading on target
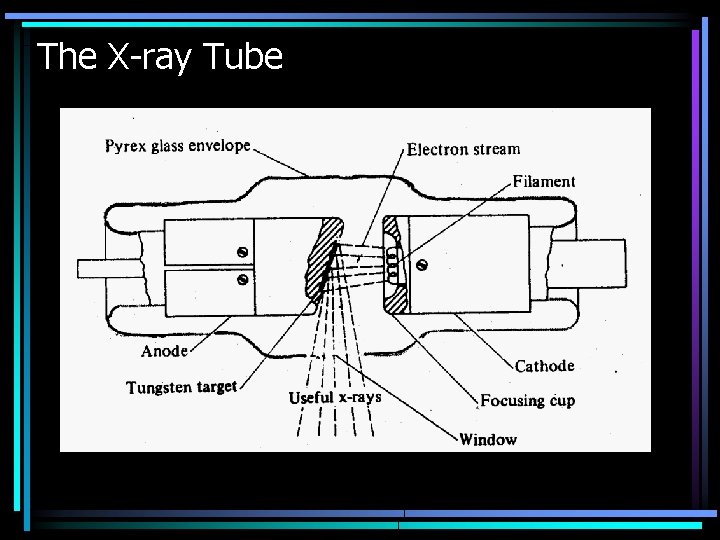
The X-ray Tube – Design 1 Diagnostic tubes must be designed with the following factors in mind: – Efficiency of X-ray production High Atomic Number (Z) Target, Vacuum and High k. V 2 to allow more electrons across – Efficiency of heat removal from the target (heat dissipation) Rotating anode (so electron beam doesn’t always hit the same spot) and air or oil circulation system to channel heat away
The X-ray Tube – Design 2 Diagnostic tubes must be designed with the following factors in mind: – Reliability in various different operating conditions Good engineering and design (expensive!) – Radiation Safety – isotropic irradiation Tube assembly contained in Lead Shielding
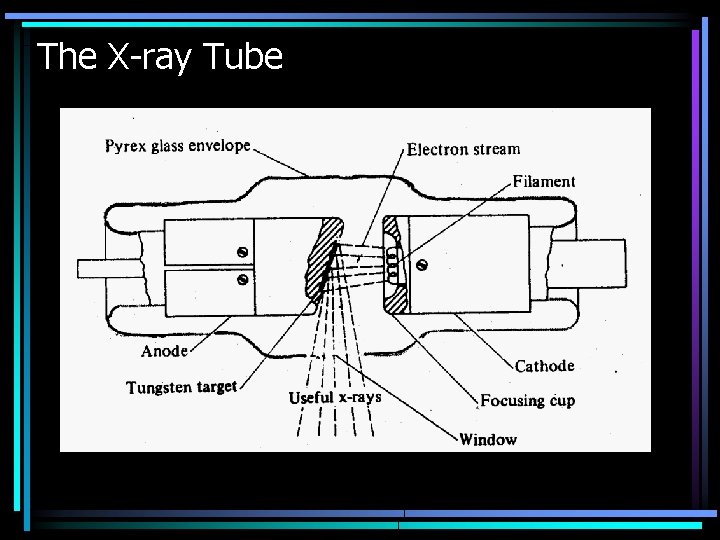
The X-ray Tube
Mammography
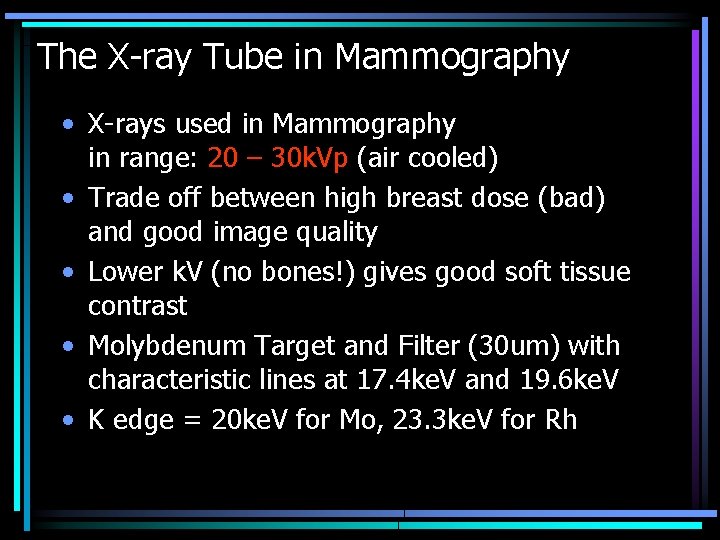
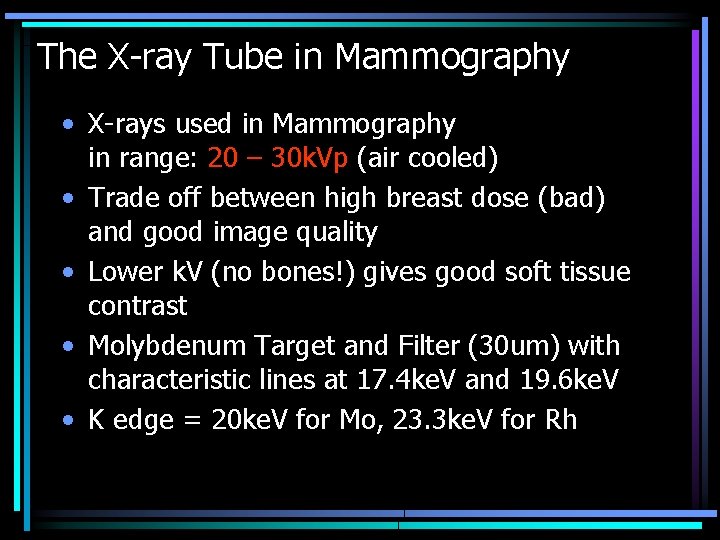
The X-ray Tube in Mammography • X-rays used in Mammography in range: 20 – 30 k. Vp (air cooled) • Trade off between high breast dose (bad) and good image quality • Lower k. V (no bones!) gives good soft tissue contrast • Molybdenum Target and Filter (30 um) with characteristic lines at 17. 4 ke. V and 19. 6 ke. V • K edge = 20 ke. V for Mo, 23. 3 ke. V for Rh
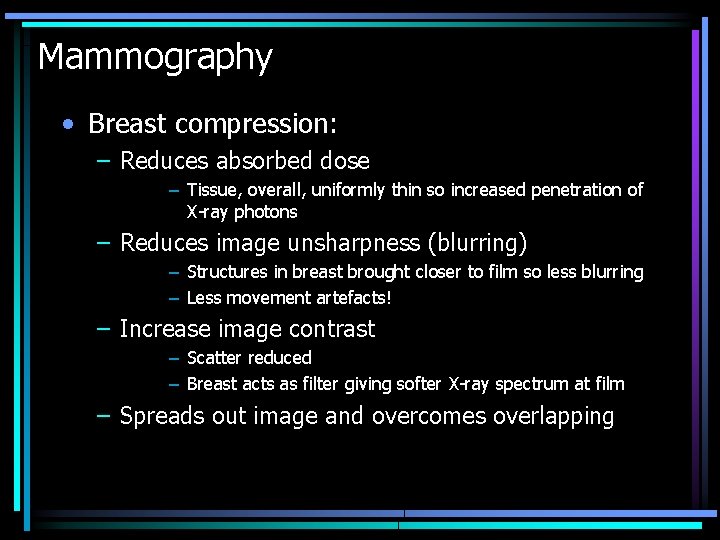
Mammography • Breast compression: – Reduces absorbed dose – Tissue, overall, uniformly thin so increased penetration of X-ray photons – Reduces image unsharpness (blurring) – Structures in breast brought closer to film so less blurring – Less movement artefacts! – Increase image contrast – Scatter reduced – Breast acts as filter giving softer X-ray spectrum at film – Spreads out image and overcomes overlapping
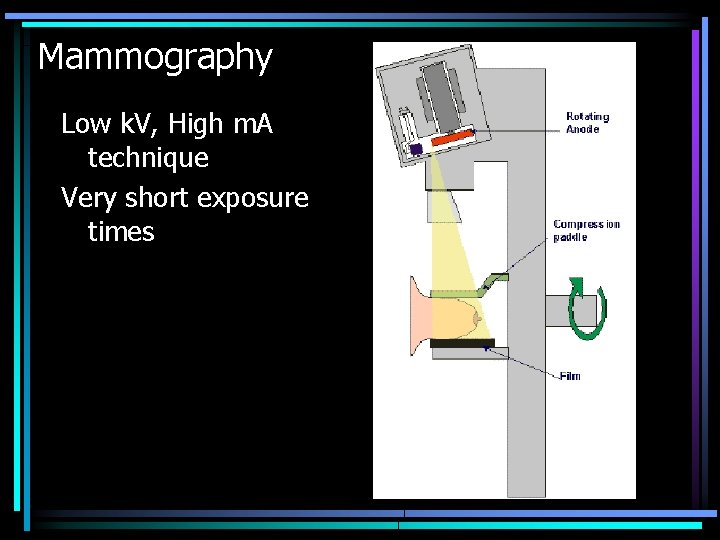
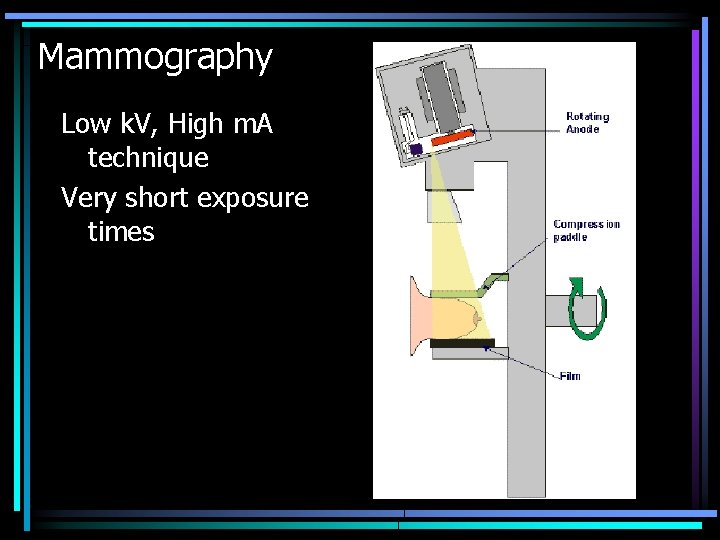
Mammography Low k. V, High m. A technique Very short exposure times
 Heel effect
Heel effect Frcr physics lectures
Frcr physics lectures Digital fluoroscopy vs conventional fluoroscopy
Digital fluoroscopy vs conventional fluoroscopy Cholecystolithiasis
Cholecystolithiasis Ivd clinical trial design
Ivd clinical trial design Diagnostic clinical landscape
Diagnostic clinical landscape Spot film device fluoroscopy
Spot film device fluoroscopy Carm fluoroscopy
Carm fluoroscopy Real time fluoroscopy
Real time fluoroscopy Bronchoscopy with fluoroscopy
Bronchoscopy with fluoroscopy Dr sohail lectures
Dr sohail lectures Anatomy lectures powerpoint
Anatomy lectures powerpoint Yelena bogdan md
Yelena bogdan md Trend lectures
Trend lectures Nuclear medicine lectures
Nuclear medicine lectures Introduction to recursion
Introduction to recursion Step wise project planning
Step wise project planning Pathology lectures for medical students
Pathology lectures for medical students Reinforcement learning lectures
Reinforcement learning lectures Medical hematology student lectures
Medical hematology student lectures C programming and numerical analysis an introduction
C programming and numerical analysis an introduction Digital logic design lectures
Digital logic design lectures Data mining lectures
Data mining lectures Power system lectures
Power system lectures Cern summer school lectures
Cern summer school lectures Utilities and energy lecture
Utilities and energy lecture Comsats virtual campus lectures
Comsats virtual campus lectures Theory of translation lectures
Theory of translation lectures Gpoint c++
Gpoint c++ Blood physiology guyton
Blood physiology guyton Cell and molecular biology lectures
Cell and molecular biology lectures Dr asim lectures
Dr asim lectures Rcog cpd
Rcog cpd Haematology lectures
Haematology lectures Kurose ross computer networking
Kurose ross computer networking Advanced medicinal chemistry
Advanced medicinal chemistry