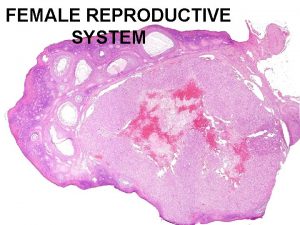
FEMALE REPRODUCTIVE SYSTEM Dr Ayisha Qureshi Assistant Professor



- Slides: 26
FEMALE REPRODUCTIVE SYSTEM Dr. Ayisha Qureshi Assistant Professor MBBS, Mphil
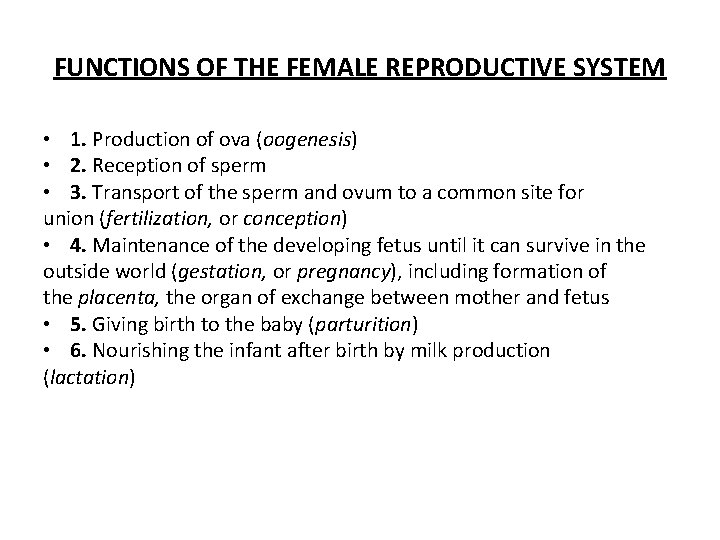
FUNCTIONS OF THE FEMALE REPRODUCTIVE SYSTEM • 1. Production of ova (oogenesis) • 2. Reception of sperm • 3. Transport of the sperm and ovum to a common site for union (fertilization, or conception) • 4. Maintenance of the developing fetus until it can survive in the outside world (gestation, or pregnancy), including formation of the placenta, the organ of exchange between mother and fetus • 5. Giving birth to the baby (parturition) • 6. Nourishing the infant after birth by milk production (lactation)
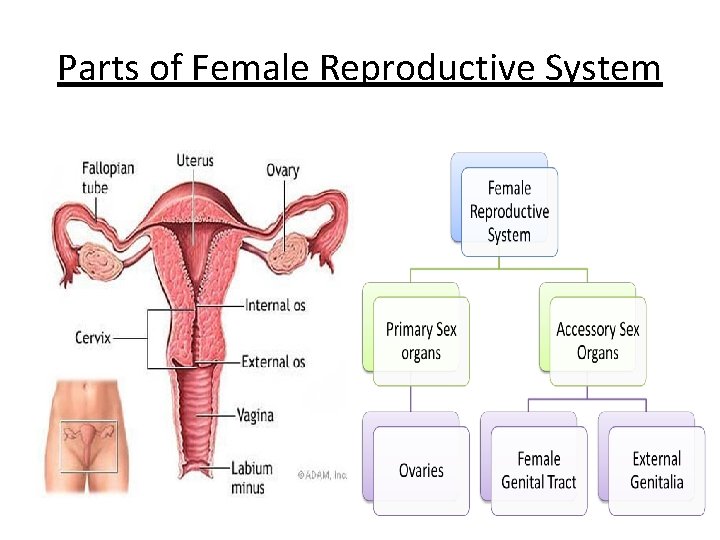
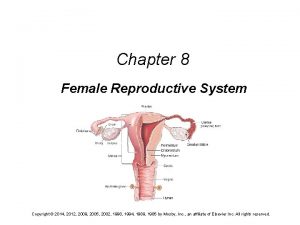
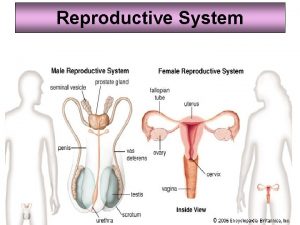
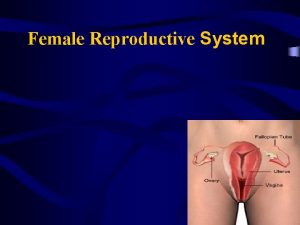
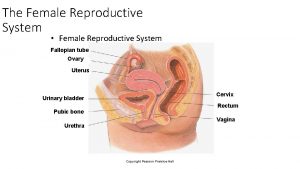
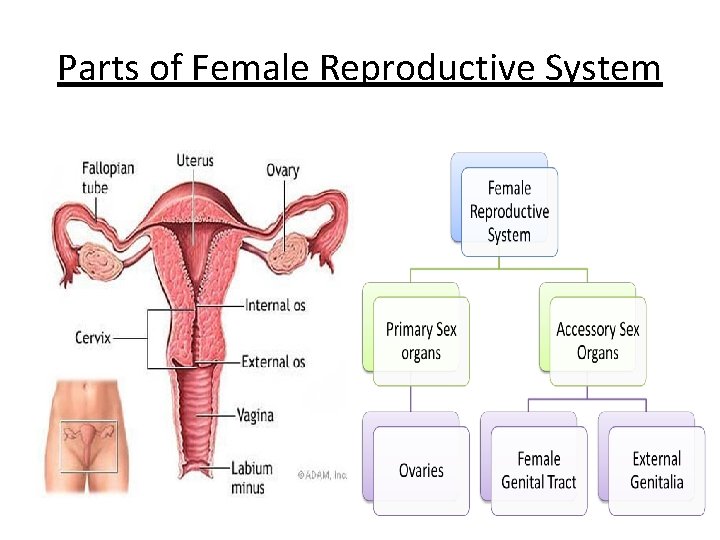
Parts of Female Reproductive System
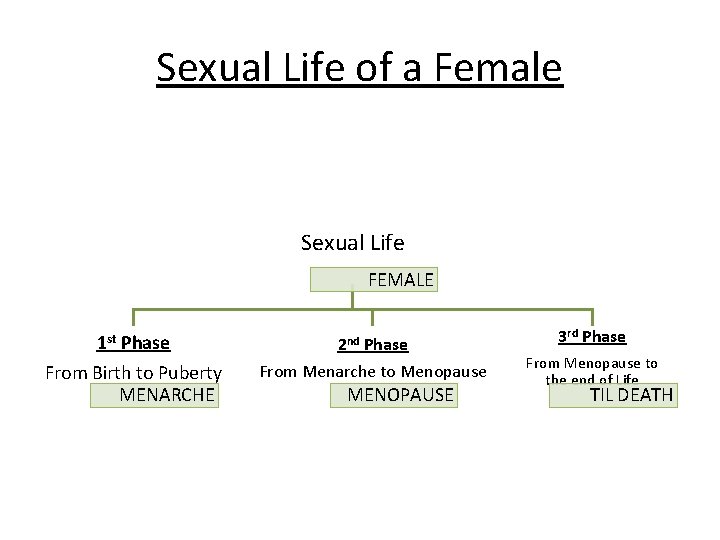
Sexual Life of a Female Sexual Life FEMALE 1 st Phase 2 nd Phase From Birth to Puberty MENARCHE From Menarche to Menopause MENOPAUSE 3 rd Phase From Menopause to the end of Life TIL DEATH
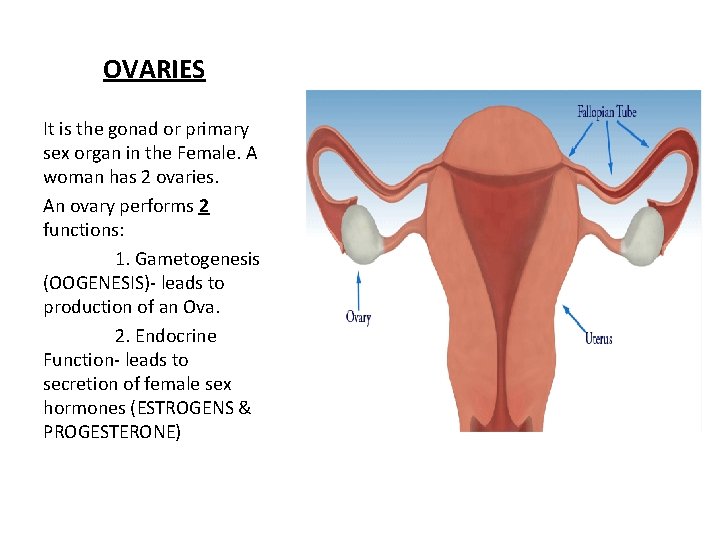
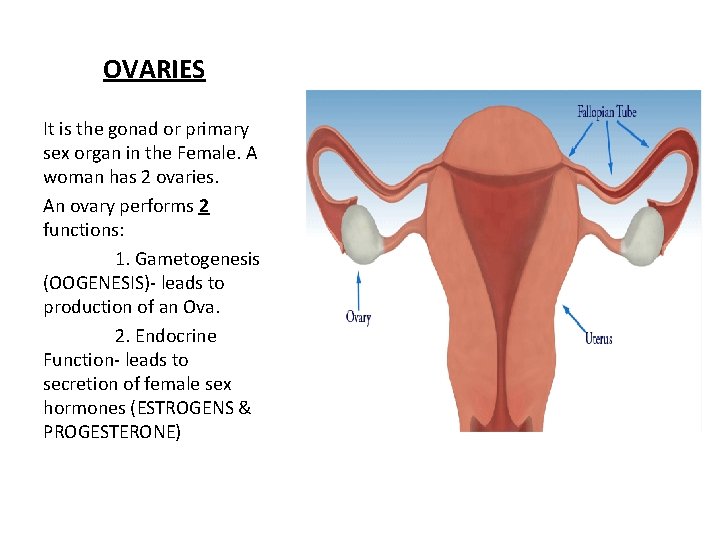
OVARIES It is the gonad or primary sex organ in the Female. A woman has 2 ovaries. An ovary performs 2 functions: 1. Gametogenesis (OOGENESIS)- leads to production of an Ova. 2. Endocrine Function- leads to secretion of female sex hormones (ESTROGENS & PROGESTERONE)
THE MENSTRUAL CYCLE
THE MENSTRUAL CYCLE • Definition: Menstrual cycle is defined as cyclic events that take place in a rhythmic fashion in a female. Menstrual cycle starts with Menarche which also marks the onset of puberty. Duration: usually 28 days (may vary b/w 20 & 40 days)
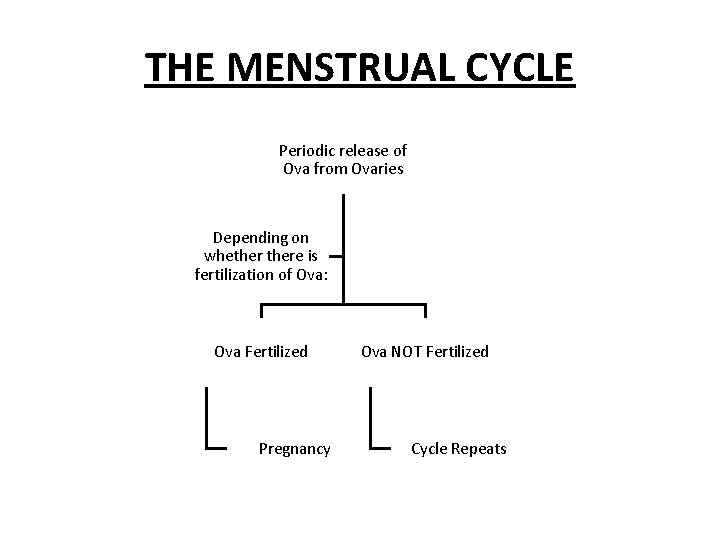
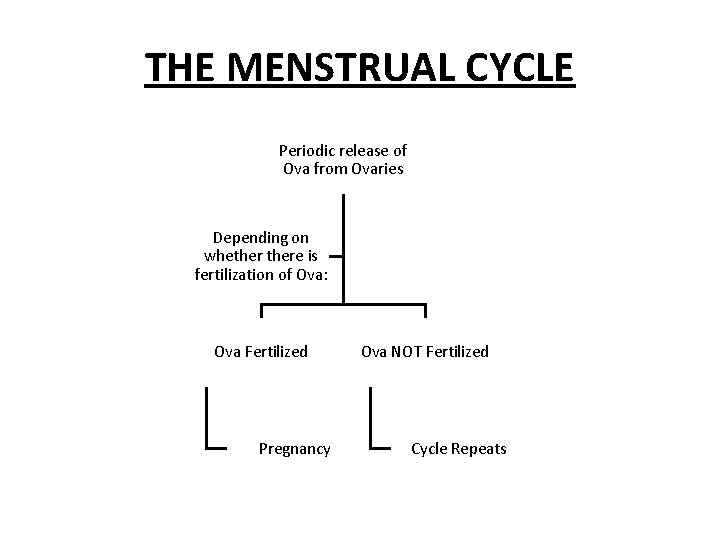
THE MENSTRUAL CYCLE Periodic release of Ova from Ovaries Depending on whethere is fertilization of Ova: Ova Fertilized Pregnancy Ova NOT Fertilized Cycle Repeats
CHANGES DURING MENSTRUAL CYCLE During each menstrual cycle, series of changes occur in the ovaries & the accessory sex organs. These changes are divided into 4 groups: 1. Ovarian Changes 2. Uterine Changes 3. Vaginal Changes 4. Changes in the Cervix
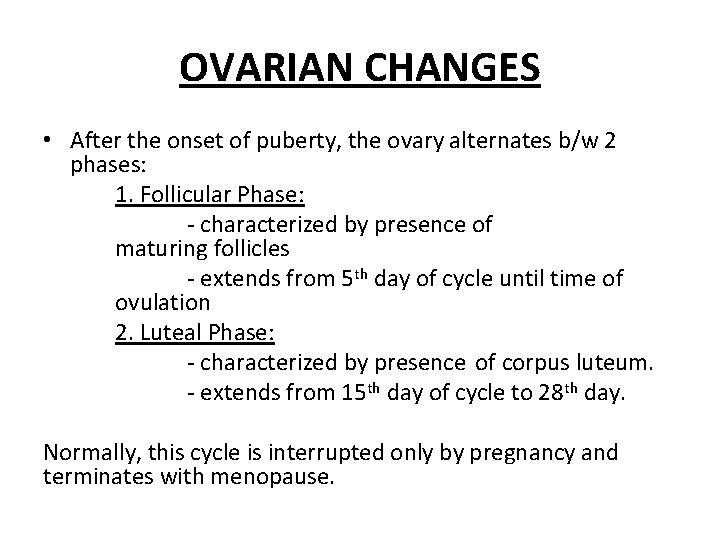
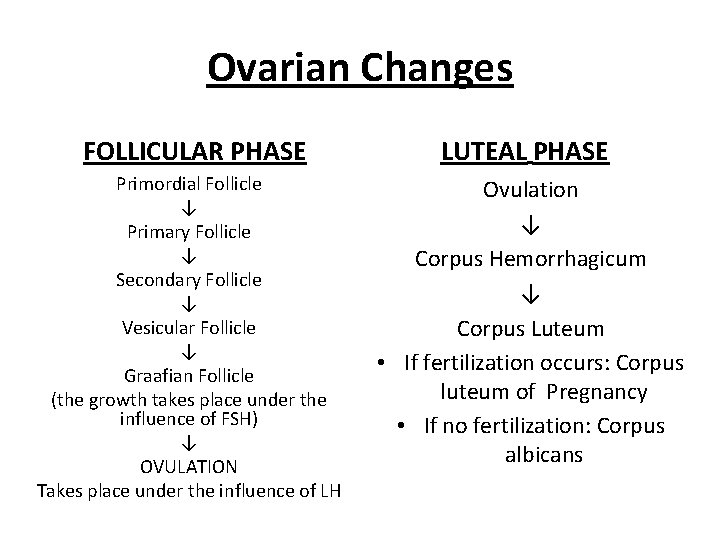
OVARIAN CHANGES • After the onset of puberty, the ovary alternates b/w 2 phases: 1. Follicular Phase: - characterized by presence of maturing follicles - extends from 5 th day of cycle until time of ovulation 2. Luteal Phase: - characterized by presence of corpus luteum. - extends from 15 th day of cycle to 28 th day. Normally, this cycle is interrupted only by pregnancy and terminates with menopause.
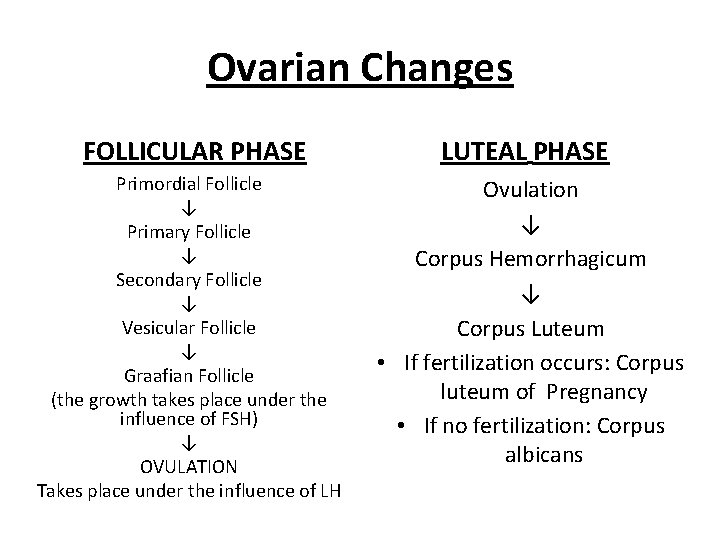
Ovarian Changes FOLLICULAR PHASE LUTEAL PHASE Primordial Follicle ↓ Primary Follicle ↓ Secondary Follicle ↓ Vesicular Follicle ↓ Graafian Follicle (the growth takes place under the influence of FSH) ↓ OVULATION Takes place under the influence of LH Ovulation ↓ Corpus Hemorrhagicum ↓ Corpus Luteum • If fertilization occurs: Corpus luteum of Pregnancy • If no fertilization: Corpus albicans

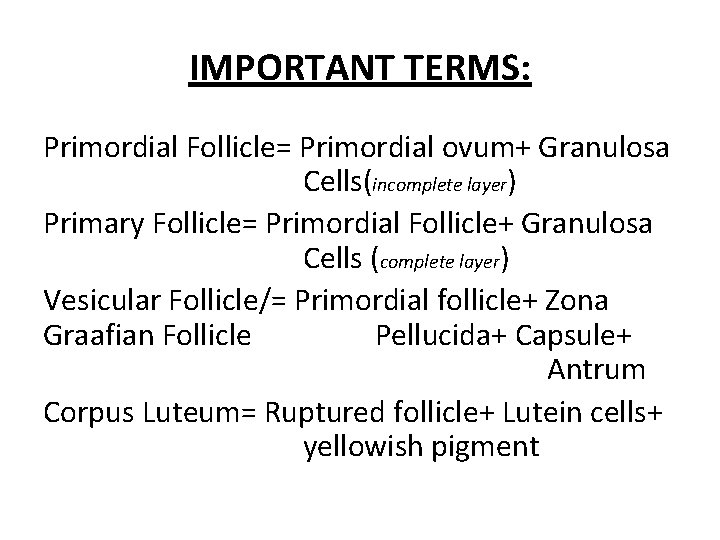
IMPORTANT TERMS: Primordial Follicle= Primordial ovum+ Granulosa Cells(incomplete layer) Primary Follicle= Primordial Follicle+ Granulosa Cells (complete layer) Vesicular Follicle/= Primordial follicle+ Zona Graafian Follicle Pellucida+ Capsule+ Antrum Corpus Luteum= Ruptured follicle+ Lutein cells+ yellowish pigment
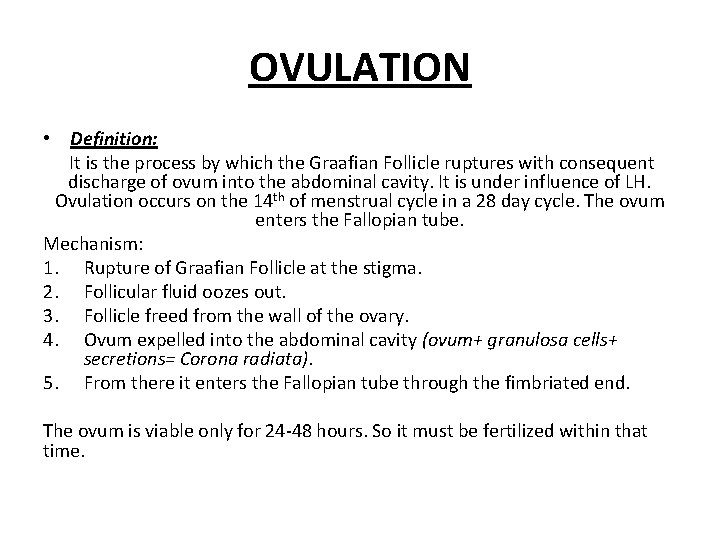
OVULATION • Definition: It is the process by which the Graafian Follicle ruptures with consequent discharge of ovum into the abdominal cavity. It is under influence of LH. Ovulation occurs on the 14 th of menstrual cycle in a 28 day cycle. The ovum enters the Fallopian tube. Mechanism: 1. Rupture of Graafian Follicle at the stigma. 2. Follicular fluid oozes out. 3. Follicle freed from the wall of the ovary. 4. Ovum expelled into the abdominal cavity (ovum+ granulosa cells+ secretions= Corona radiata). 5. From there it enters the Fallopian tube through the fimbriated end. The ovum is viable only for 24 -48 hours. So it must be fertilized within that time.
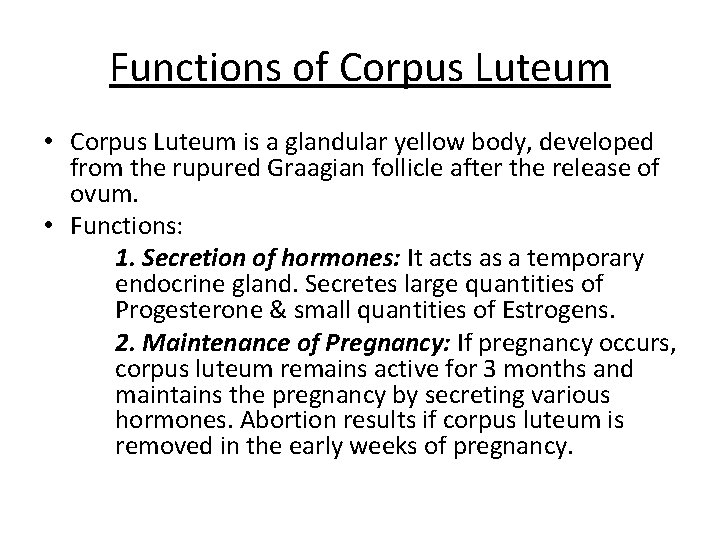
Functions of Corpus Luteum • Corpus Luteum is a glandular yellow body, developed from the rupured Graagian follicle after the release of ovum. • Functions: 1. Secretion of hormones: It acts as a temporary endocrine gland. Secretes large quantities of Progesterone & small quantities of Estrogens. 2. Maintenance of Pregnancy: If pregnancy occurs, corpus luteum remains active for 3 months and maintains the pregnancy by secreting various hormones. Abortion results if corpus luteum is removed in the early weeks of pregnancy.
UTERINE CHANGES • During each menstrual cycle, along with ovarian changes, uterine changes also occur: 1. Menstrual Phase 2. Proliferative Phase 3. Secretory Phase

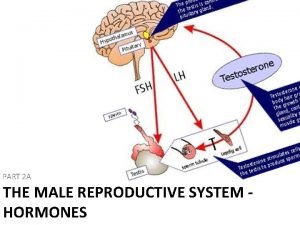
HORMONES & THEIR ROLE IN MENSTRUAL CYCLE • Hypothalamus: releases Gn. RH. • Anterior Pituitary: releases FSH & LH • Ovarian Hormones: Estrogens & Progesterone LH Surge: LH is important for ovulation. Ovulation will not occur if there is no LH surge even if large amounts of FSH are present. The need for large amounts of LH for Ovulation is known as Ovulatory Surge for LH surge.
APPLIED PHYSIOLOGY AMENORRHEA: Absence of menstruation HYPOMENORRHEA: Decreased menstrual bleeding. MENORRHAGIA: Excess menstrual bleeding. OLIGOMENORRHEA: Decreased frequency of menstrual bleeding. DYSMENORRHEA: Menstruation with pain.

FUNCTIONS OF ESTROGENS:
ESTROGENS • Source: Estrogens are secreted in large quantities by theca interna cells of the ovaries & to a small amount by the corpus luteum. • Chemistry: It is a steroid. • Different forms: β- estradiol, estrone, estriol • Half-life: 30 -60 minutes • Transport: mostly by albumin & to a lesser extent by globulin.
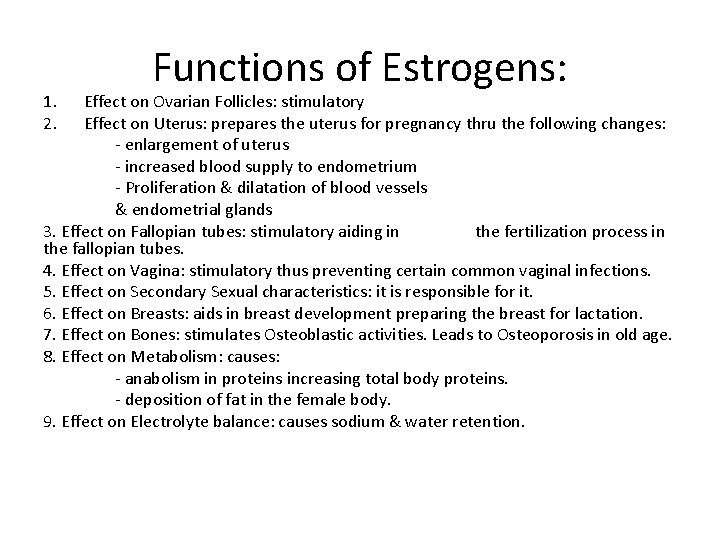
1. 2. Functions of Estrogens: Effect on Ovarian Follicles: stimulatory Effect on Uterus: prepares the uterus for pregnancy thru the following changes: - enlargement of uterus - increased blood supply to endometrium - Proliferation & dilatation of blood vessels & endometrial glands 3. Effect on Fallopian tubes: stimulatory aiding in the fertilization process in the fallopian tubes. 4. Effect on Vagina: stimulatory thus preventing certain common vaginal infections. 5. Effect on Secondary Sexual characteristics: it is responsible for it. 6. Effect on Breasts: aids in breast development preparing the breast for lactation. 7. Effect on Bones: stimulates Osteoblastic activities. Leads to Osteoporosis in old age. 8. Effect on Metabolism: causes: - anabolism in proteins increasing total body proteins. - deposition of fat in the female body. 9. Effect on Electrolyte balance: causes sodium & water retention.
PROGESTERONE:
Progesterone • Source: a small amount by theca interna cells of the ovaries & a larger amount by the corpus luteum. • Chemistry: steroid. • Half-life: 4 -5 minutes • Transport: albumin & globulin.
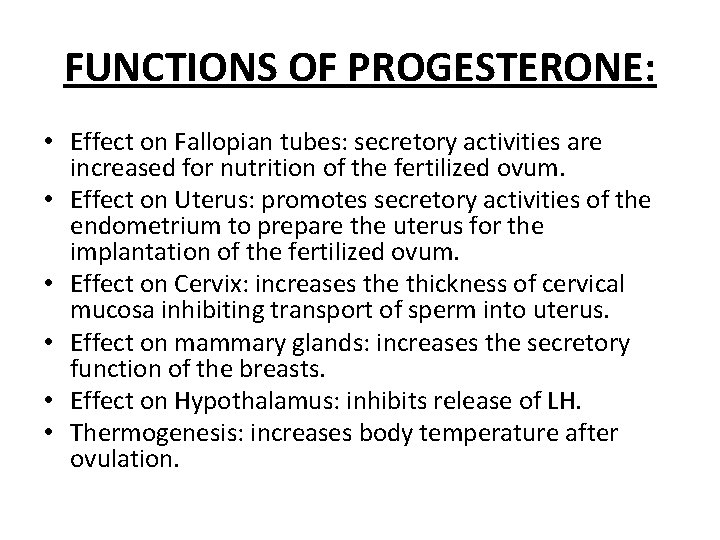
FUNCTIONS OF PROGESTERONE: • Effect on Fallopian tubes: secretory activities are increased for nutrition of the fertilized ovum. • Effect on Uterus: promotes secretory activities of the endometrium to prepare the uterus for the implantation of the fertilized ovum. • Effect on Cervix: increases the thickness of cervical mucosa inhibiting transport of sperm into uterus. • Effect on mammary glands: increases the secretory function of the breasts. • Effect on Hypothalamus: inhibits release of LH. • Thermogenesis: increases body temperature after ovulation.
 Ayisha ali
Ayisha ali Labeled female reproductive system
Labeled female reproductive system Male and female reproductive system
Male and female reproductive system Fetus reproductive system
Fetus reproductive system Female external reproductive system
Female external reproductive system Epilization
Epilization Male fallopian tube
Male fallopian tube Unit 5 lesson 3 the female reproductive system
Unit 5 lesson 3 the female reproductive system Ligaments of female reproductive system
Ligaments of female reproductive system Uterus function
Uterus function Pila reproduction
Pila reproduction Urogenital papilla fetal pig
Urogenital papilla fetal pig Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Female reproductive organs sagittal section
Female reproductive organs sagittal section Chapter 16 the reproductive system answer key
Chapter 16 the reproductive system answer key Female cow reproductive system
Female cow reproductive system Male reproductive system of cattle
Male reproductive system of cattle Differences between male and female reproductive organ
Differences between male and female reproductive organ Function of reproductive organs
Function of reproductive organs Male reproductive system
Male reproductive system Oogenesis
Oogenesis Fsh and lh in female reproductive system
Fsh and lh in female reproductive system Oogonium
Oogonium Lesson 3 the female reproductive system
Lesson 3 the female reproductive system Color of female reproductive system
Color of female reproductive system Female reproductive system bones
Female reproductive system bones Chapter 8 female reproductive system
Chapter 8 female reproductive system