Falls Among Older Adults DATA prevalence risk factors


- Slides: 51
Falls Among Older Adults • DATA: prevalence, risk factors and costs • FEAR: Falls Self-Efficacy and Fear of Falling • INTERVENTIONS: Physical Therapy, Vision, Hearing, Medication Mgt, Home Safety / Environmental Safety, Education • RESOURCES –Education (Home safety/medication safety) –Balance/Exercise 1
FALLS – Prevalence/Consquences n n n Leading preventable cause of functional disability and mortality among older adults 1/3 of Community-Dwelling people over age 65 fall each year (Tinetti) yet less than half of those who fall discuss this with health care providers. (Stevens et al. , 2012) Falls are the leading cause of death due to injury for people 65 years and older (NCIPC 2002) n Mortality 12 months after a hip fracture ranges from 12 to 67%. 2
Falls Rates - chances of falling and serious injury increase with age n People age 75 and older who fall are four to five times more likely than those age 65 to 74 to be admitted to a long-term care facility for a year or longer. (Donald IP, Bulpitt CJ. The prognosis of falls in elderly people living at home. Age and Ageing 1999; 28: 121– 5; CDC website accessed Feb 2015) n Fall rate injuries for adults 85 and older is almost four times that for adults 65 to 74. (Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web–based Injury Statistics Query and Reporting System (WISQARS) 3
Fall Rates / Fatalities increasing 2012 vs people 2002 over 65 died n 2012: Nearly 24, 000 after a fall - almost double that # in 2002 (CDC http: //www. cdc. gov/homeandrecreationalsafety/falls/adultfalls. html ) n 2012: More than 2. 4 million people over 65 were treated in emergency departments for injuries from falls, an increase of 50% since 2002. 4
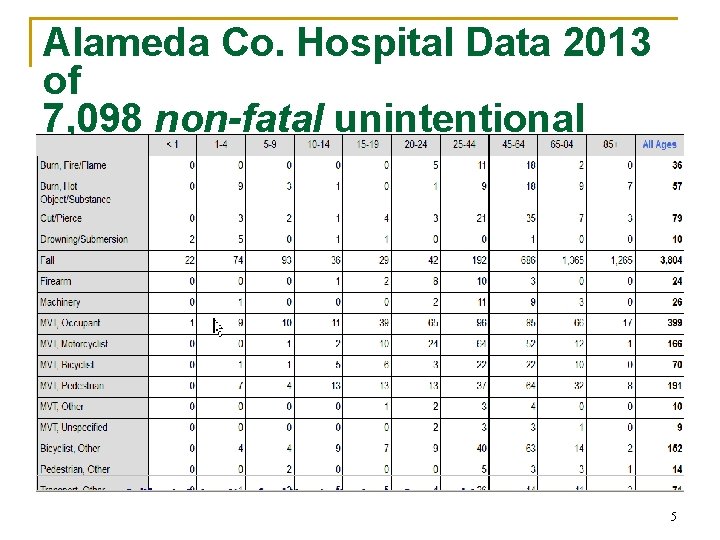
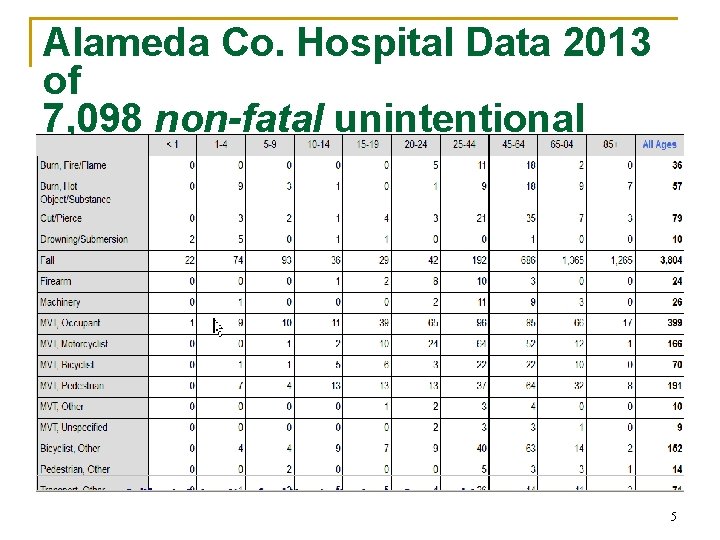
Alameda Co. Hospital Data 2013 of 7, 098 non-fatal unintentional injuries: ~ 40% from elders falling 5
Falls COSTS – Direct Medical n In 2012, the direct medical costs of falls, Costs n n adjusted for inflation, were $30 billion in 2009 Cost for inpatient and outpatient medical care for non-fatal falls: $19 billion 1997 study of people age 72 and older: fall-injury medical cost averaged $19, 440 (hospital, nursing home, emergency room, and home health care, but not doctors’ services) 6

Impact on individuals and families Detrimental impacts on quality of life are not included in cost analyses n Direct costs do not account for the long-term effects such as disability, dependence on others, lost time from work and household duties, and reduced quality of life as well as effect on family caregivers. n Economic systems: Elders who offered child care n Q of L: For those who survive, fewer than one-third of older adults who were hospitalized return to their pre-fall level of activity. 7
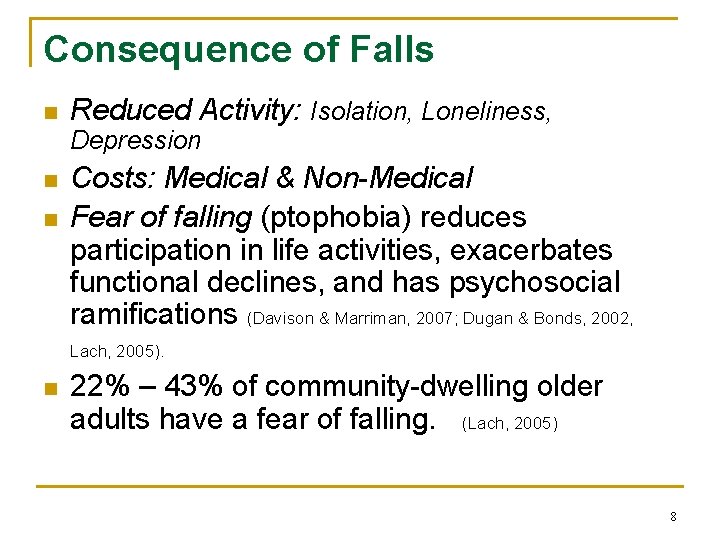
Consequence of Falls n Reduced Activity: Isolation, Loneliness, Depression n n Costs: Medical & Non-Medical Fear of falling (ptophobia) reduces participation in life activities, exacerbates functional declines, and has psychosocial ramifications (Davison & Marriman, 2007; Dugan & Bonds, 2002, Lach, 2005). n 22% – 43% of community-dwelling older adults have a fear of falling. (Lach, 2005) 8
Fear of Falling … Not a good feeling… inhibits activities can make things worse due to inactivity stiffness… less strength… balance gets worse …then falls risk is HIGHER 9
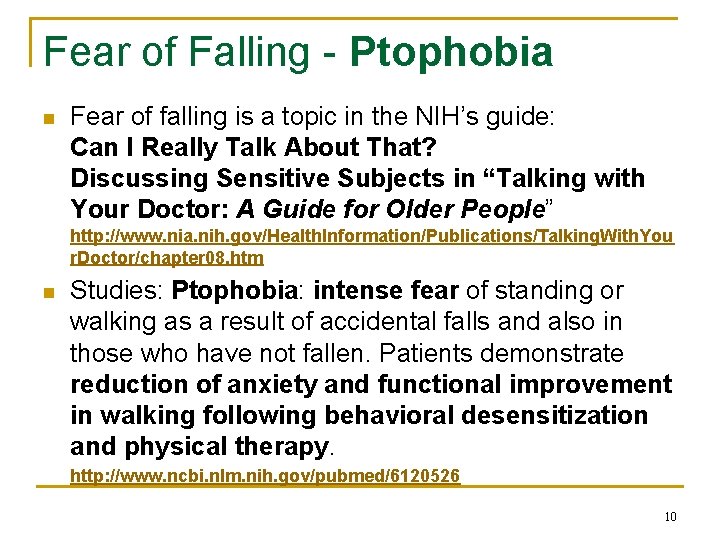
Fear of Falling - Ptophobia n Fear of falling is a topic in the NIH’s guide: Can I Really Talk About That? Discussing Sensitive Subjects in “Talking with Your Doctor: A Guide for Older People” http: //www. nia. nih. gov/Health. Information/Publications/Talking. With. You r. Doctor/chapter 08. htm n Studies: Ptophobia: intense fear of standing or walking as a result of accidental falls and also in those who have not fallen. Patients demonstrate reduction of anxiety and functional improvement in walking following behavioral desensitization and physical therapy. http: //www. ncbi. nlm. nih. gov/pubmed/6120526 10
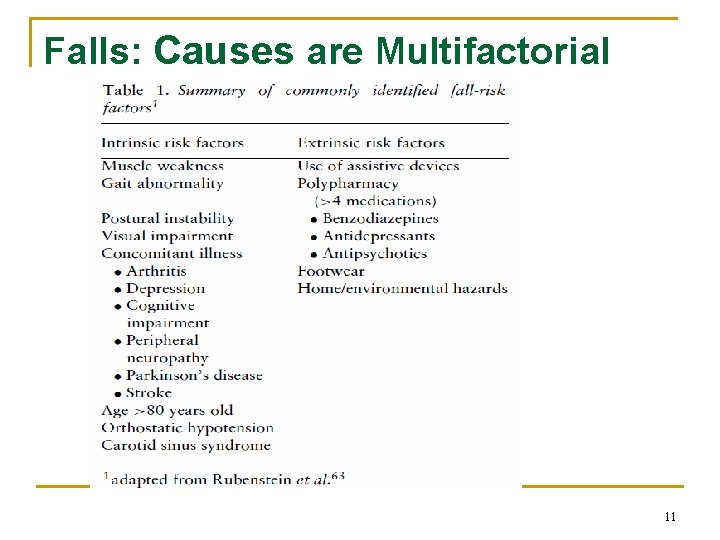
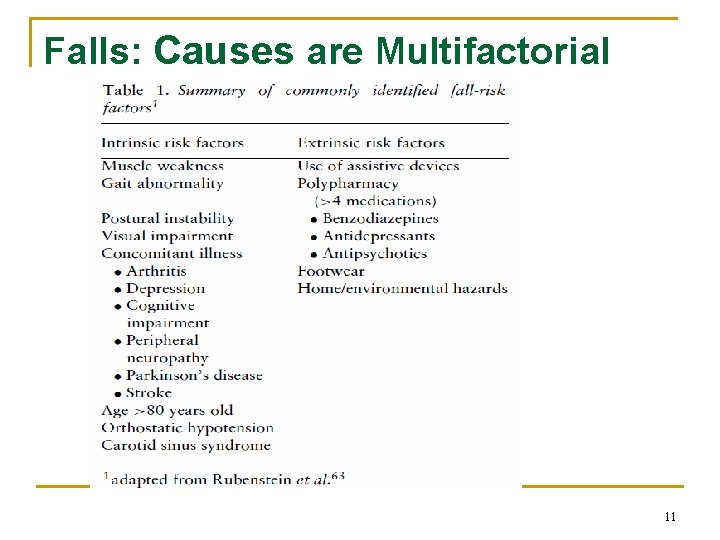
Falls: Causes are Multifactorial 11
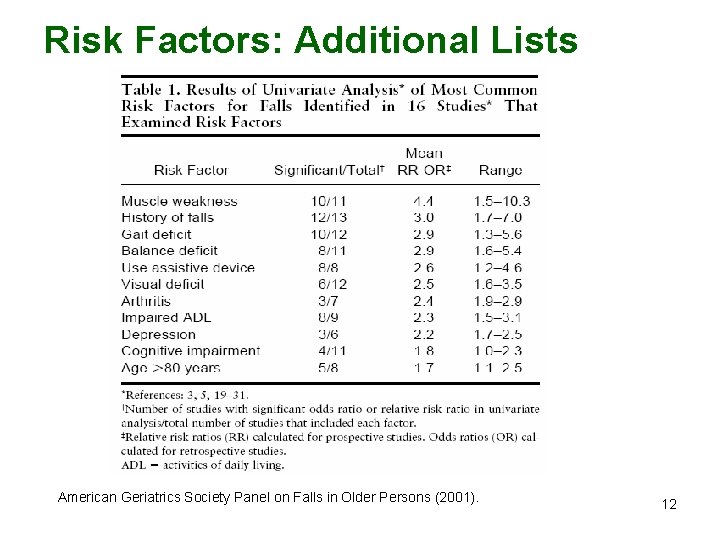
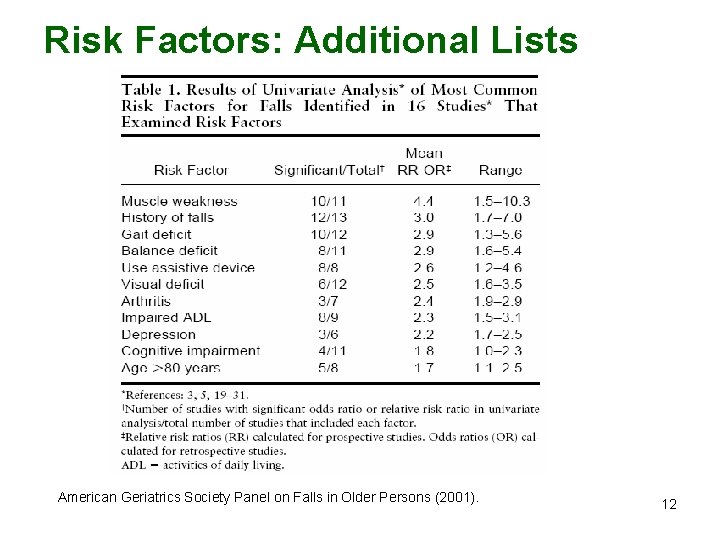
Risk Factors: Additional Lists American Geriatrics Society Panel on Falls in Older Persons (2001). 12
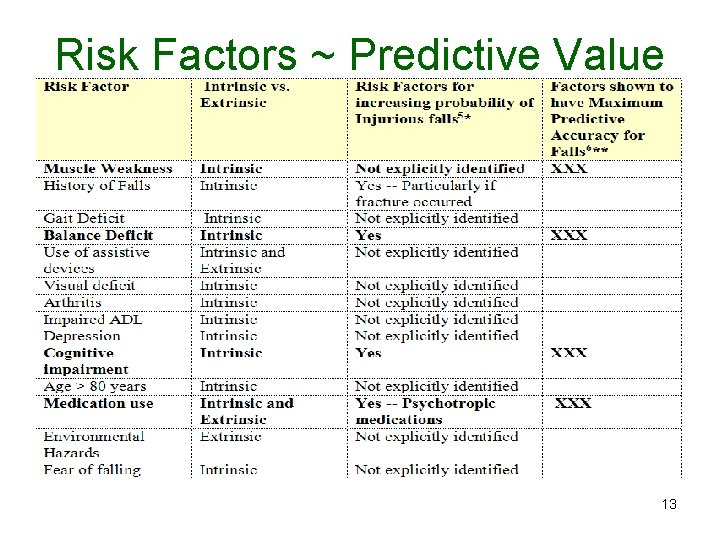
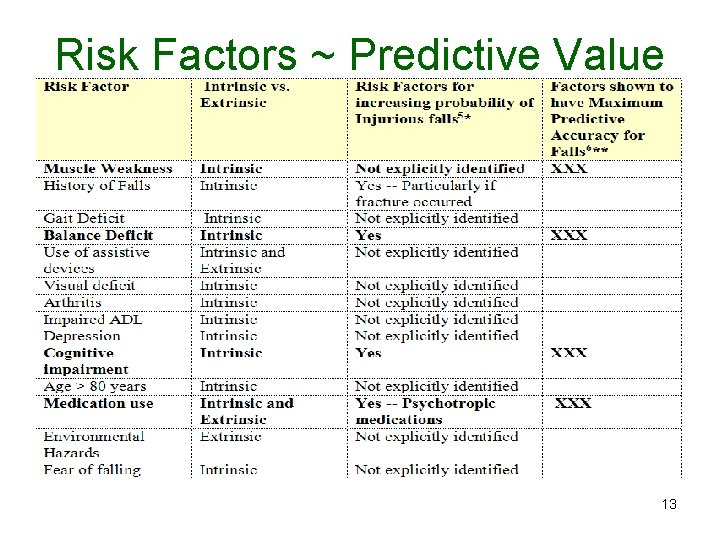
Risk Factors ~ Predictive Value 13
Balance Systems Nervous System Functions including • Vision and Hearing • Proprioception • Vestibular function • Orthostatic hypotension Fatigue “disturbs the functioning of the protective reactions and impairs perception, making them liable to injurious falls” (Koski, Luukinen, Laippala, & Kivelä, 1998). DECONDITIONING: impairs strength. This occurs RAPIDLY in older adults. 14
Neuropathies & Balance (Chemorelated –a topic where I work) n n Deep tendon reflexes are impaired unsteady gait loss of sensation vestibular and ocular changes (newer info) (Holley 2002; Paice, 2009; Wampler et al. , 2007) n CNS also affected (Weiss, 2008; Wolf 2008). n Age-related changes compounded by deficits incurred during treatments can persist for months and years posttreatment and sometimes is permanent (Holley, 2002; Galea, Wright & Barr 2003 Nielsen & Brandt, 2002; Weiss, 2008; Wilkes, 2007). 15
Not aware of balance / falls risk n n n People don’t recognize gradual changes Not discussed during medical visits RCFEs/Senior Centers offer programs to improve balance and fitness, yet people avoid (NY Times Nov 3, 2014) 16
• Exploratory study: Interviews to discern key words/phrases that might indicate balance problems. • Unexpected Result: Half of the referred patients denied a balance problem yet described ambulation difficulties normally attributed to balance deficits. 17
Recognize risks……. . n Balance changes slowly over time n Might not be aware of changes n Ability to get up from the floor – this also changes over time n Surgeries / Prior Falls: ‘Vicious cycle’: deconditioned / more likely to fall / greater fears / reduced self-efficacy 18
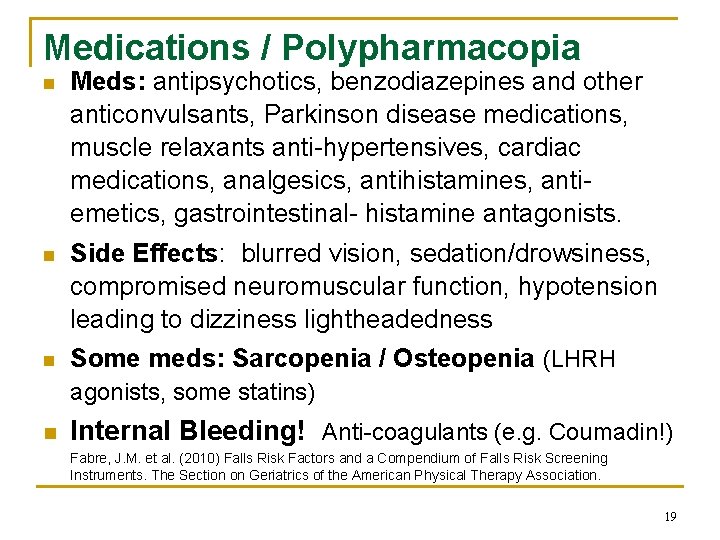
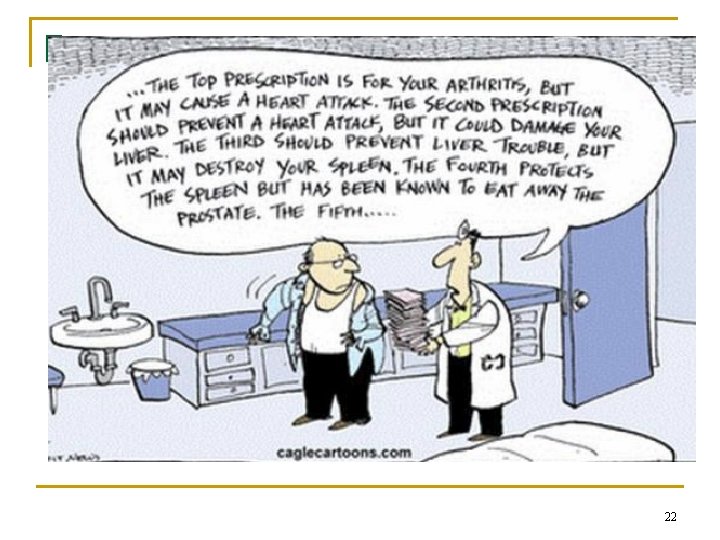
Medications / Polypharmacopia n Meds: antipsychotics, benzodiazepines and other anticonvulsants, Parkinson disease medications, muscle relaxants anti-hypertensives, cardiac medications, analgesics, antihistamines, antiemetics, gastrointestinal- histamine antagonists. n Side Effects: blurred vision, sedation/drowsiness, compromised neuromuscular function, hypotension leading to dizziness lightheadedness n Some meds: Sarcopenia / Osteopenia (LHRH agonists, some statins) n Internal Bleeding! Anti-coagulants (e. g. Coumadin!) Fabre, J. M. et al. (2010) Falls Risk Factors and a Compendium of Falls Risk Screening Instruments. The Section on Geriatrics of the American Physical Therapy Association. 19
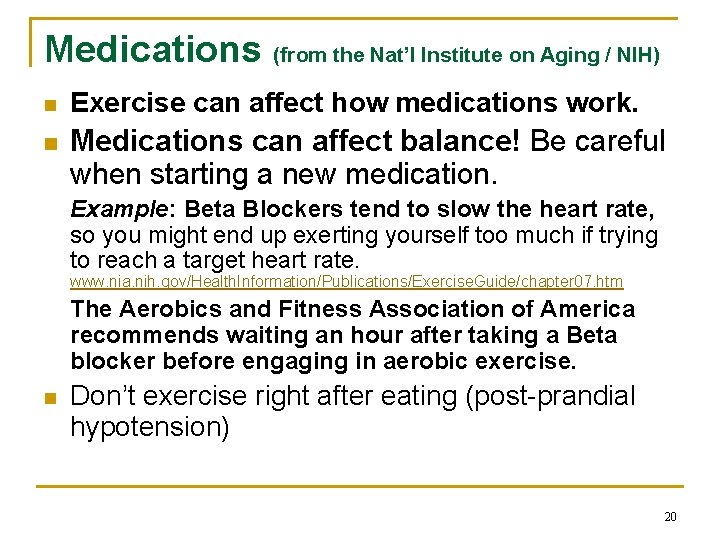
Medications (from the Nat’l Institute on Aging / NIH) n Exercise can affect how medications work. n Medications can affect balance! Be careful when starting a new medication. Example: Beta Blockers tend to slow the heart rate, so you might end up exerting yourself too much if trying to reach a target heart rate. www. nia. nih. gov/Health. Information/Publications/Exercise. Guide/chapter 07. htm The Aerobics and Fitness Association of America recommends waiting an hour after taking a Beta blocker before engaging in aerobic exercise. n Don’t exercise right after eating (post-prandial hypotension) 20
Medication Safety Links (from Alice K Hwe) n n n n www. pharmacyfoundation. org www. talkaboutrx. org www. bemedwise. org www. aarp. org/health/rx_drugs/usingmeds www. ascp. com/consumers/tips/index. cf www. fda. gov/medsinmyhome www. fda. gov/cder/consumerinfo/buy. Online. G uide_text. htm 21
Rx 22
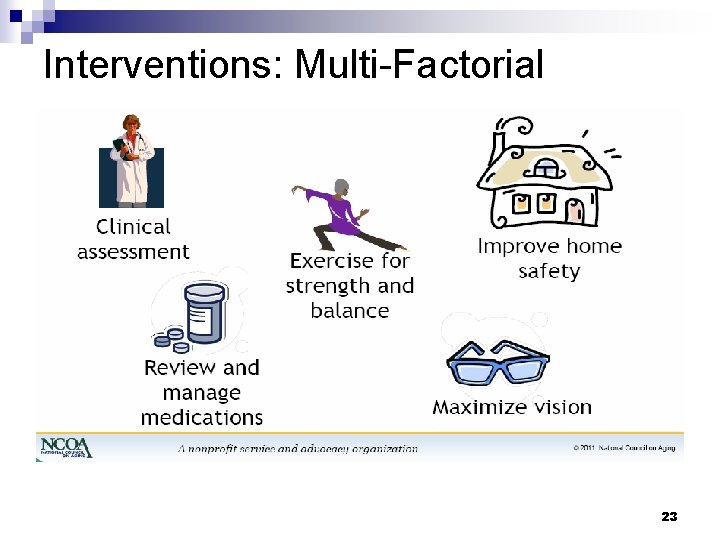
Interventions: Multi-Factorial 23
Raise Awareness / Assess n Assess periodically by a professional PT/OT, Doctor, Nurse, Exercise Physiologist/Kinesiologist, skilled trainer) Many tools: Berg, Tinetti, Timed Up & Go, Romberg, Fullerton etc n Open Dialogue: Ask about walking down stairs (need to use railing? ) or crossing curbs; Can you get up from the floor? (practical question!) 24
Studies consistently conclude n Multifactorial assessments and that n n individualized exercise/balance programs are the most successful, yielding decreased fall rates and decreased use of the medical system In group settings, adherence among exercise program participants is reinforced by the benefits of the social context, enhanced with peer-mentoring (music also helpful) Education and advice are useful only as an adjunct to a multifactorial program 25
Why doctors don’t assess n lack of evaluation time in primary care balance n settings (Dugan & Bonds, 2002) lack of awareness among health professionals of the multifactorial nature of falls and the need to assess for falls risks (Brown, Gottschalk, Van Ness, Fortinsky, & Tinetti, 2005; Tinetti et al. , 2008), n lack of program availability or accessibility (physical or financial) (Robertson, Devlin, Gardner, & Campbell 2001). 26
If falls were on the MD’s radar. . . Connecticut Collaboration for Falls Prevention (CCFP): education for health care providers raised awareness of risks and resources q Result: Emergency room admissions for falls declined in the 26 intervention zip codes versus the control zip codes Brown et al. (2005) Chou et al. , (2006) and Tinetti et al. , (2008) analyzed aspects of the interventions 27
Assess for Appropriate Interventions: Be Realistic per client’s Needs/Abilities n n Client Sets Functional Goals (to walk again w/o fear) Assist with resource lists (examples) q q q n Home Safety Services Referral to PT for eval Consult with MD re: issues related to medications Motivational Discussions: “Baby Steps” q q “Assignment” example: Put on shoes and jacket and walk outside for 2 minutes. Or just stand outside. Find “walking buddy” 28
Safety (short list ) n n n Remove Hazards from walking paths: wires/cords, low tables, clutter on floor Scatter Rugs! Bedspreads! Long skirts! Bathrobes! Pets (yes, pets causing falls has been measured…) Improve Lighting Grab Bars Remember: “Slippery when wet!” Storage of items used on a regular basis: eliminate using a step-stool to reach items (move things so you don’t have to reach up high or bend down and reach into a cabinet) 29
Safety n n n n Shoes (poor shoe design can contribute to risk) Walking aids are important …. However, make sure you use these devices safely. Have a physical therapist fit the walker or cane to you. “Some forms of vision loss increase risk of falling and injury. Have your eyes checked and update your eyeglasses” (NCOA 2011). Hearing can affect balance Fatigue! Poor Nutrition / Dehydration Alcohol; Medications (separately and in combination) 30
External Hazards n n n elevated tree root along a sidewalk, Problems with curb/sidewalk climbing on a ladder 31
Behavior Modification – Focus and Concentrate n n n Walk & Talk … sometimes not a good idea Concentrate while holding items and walking Stop climbing on chairs/step stools/ladders SLOWLY get out of bed / up from a chair IF TIRED: Be Extra Careful! ! Understand that you are changing … what you could easily do 10 years ago might not be safe today. 32
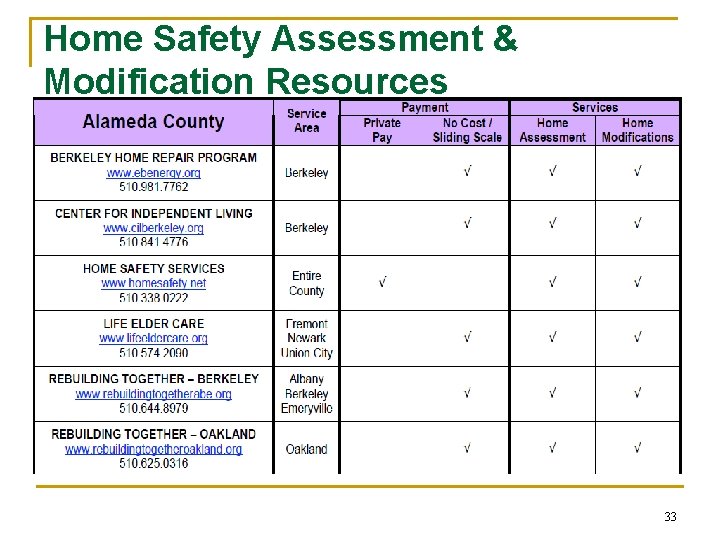
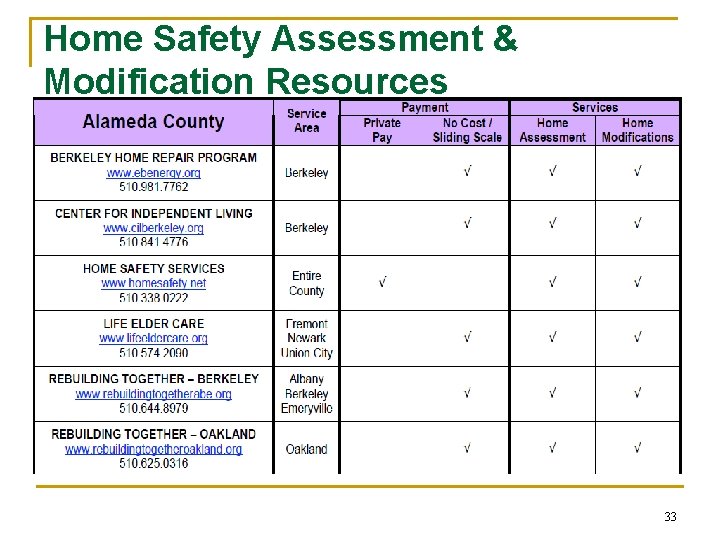
Home Safety Assessment & Modification Resources 33
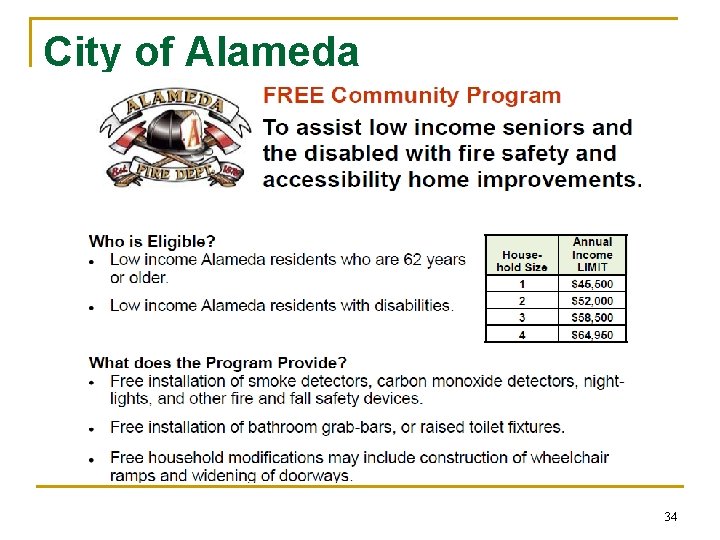
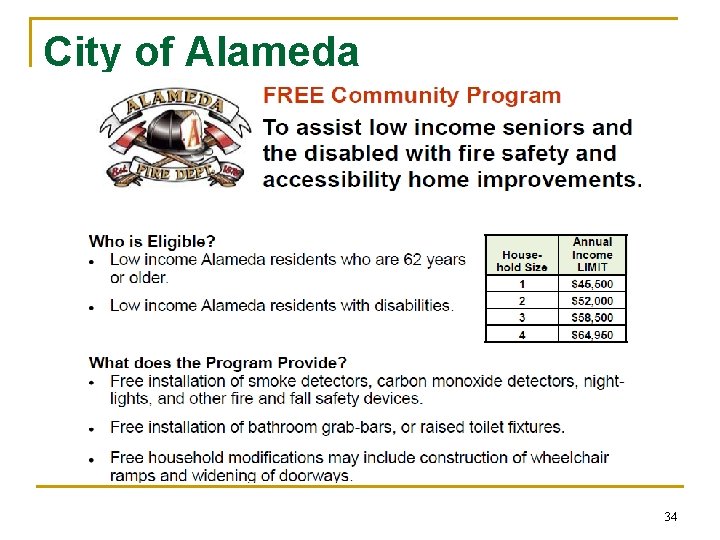
City of Alameda 34
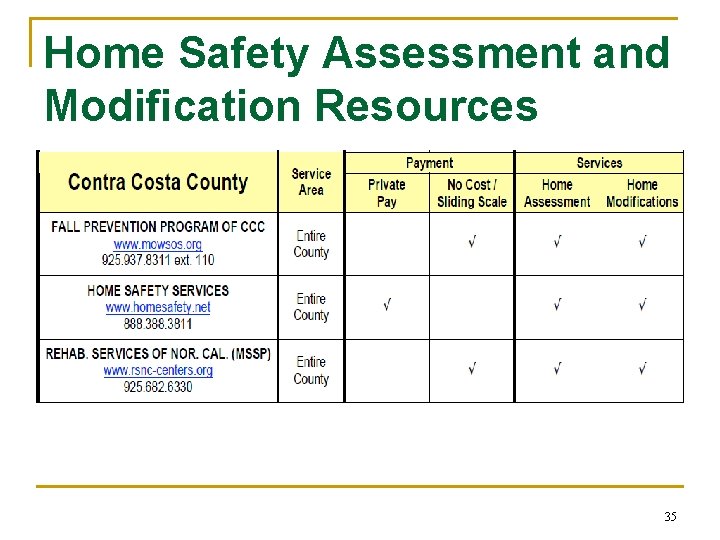
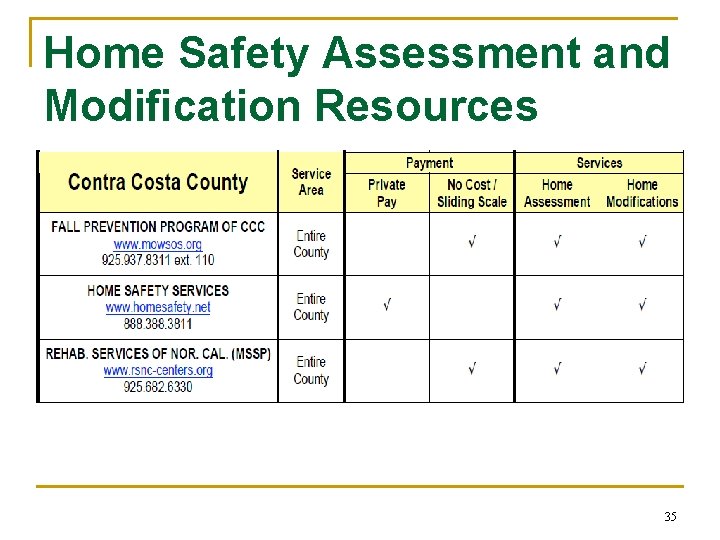
Home Safety Assessment and Modification Resources 35
High Tech n Residential Communities: Lights activated by motions (from bed to bathroom); Stair edges defined n “Magic Carpet” to assess for gait disturbances (TRIL centre in Ireland) http: //www. ict-ageing. eu/? page_id=1589 n Home Safety monitoring (in case of a fall) – passive alert systems for quicker response 36
Resources for Neuropathy The Pacific Chapter of The Neuropathy Association (PCNA). http: //www. pnhelp. org EMAIL: info@pnhelp. org PN Local Support Groups: organized by the PCNA Phone: (877) 622 -6298 Bev Anderson (main office of PCNA) Berkeley 3 rd Monday of the month 3 pm-4 pm; North Berkeley Senior Center / contact Kathleen Nagel (510) 653 -8625 37
Interventions And Successful Outcomes Multifactorial Assessments: include gait/strength analysis; medical review; home safety assess INTERVENTIONS n Physical Therapy n Individualized Exercise and Balance Training Group Exercise: Tai Chi has the best outcomes for improved balance and strength. Studies of Tai Chi as an intervention overwhelmingly find it reduces falls risks and actual rates of falls (Davison & Marinan, 2007; n 38
At any age Muscle Strength People in their 80 s and 90 s can acquire greater muscle strength, (although perhaps not muscle mass) with a strength program. (Campbell & Robertson, 2005 BMJ; Gillespie et al. , 2009, Cochrane; Lord, S. et al, 2003 JAGS; Robertson et al, 2001, BMJ) “While we do lose muscle as we age, exercise can partially restore strength and flexibility. It’s never too late to start an exercise program. ” © 2011. National Council on Aging 39
From the NCOA & NIH “Strength and balance exercises, managing your medications, having your vision checked and making your living environment safer are all steps you can take to prevent a fall. ” (Nat’l Council on Aging, Sept. 2011) “Balance exercises help prevent a common problem in older adults: falls. Falling is a major cause of broken hips and other injuries that often lead to disability and loss of independence. Some balance exercises build up your leg muscles; others require you to do simple activities like briefly standing on one leg. ” (NIA/NIH 2011) 40
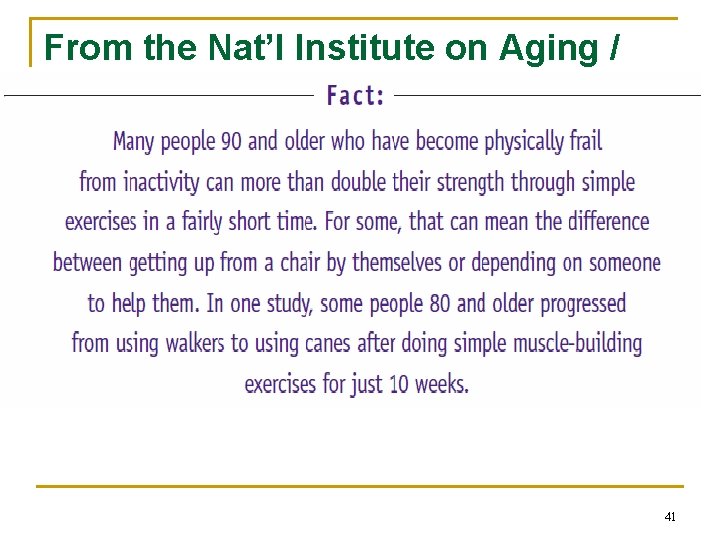
From the Nat’l Institute on Aging / NIH 41
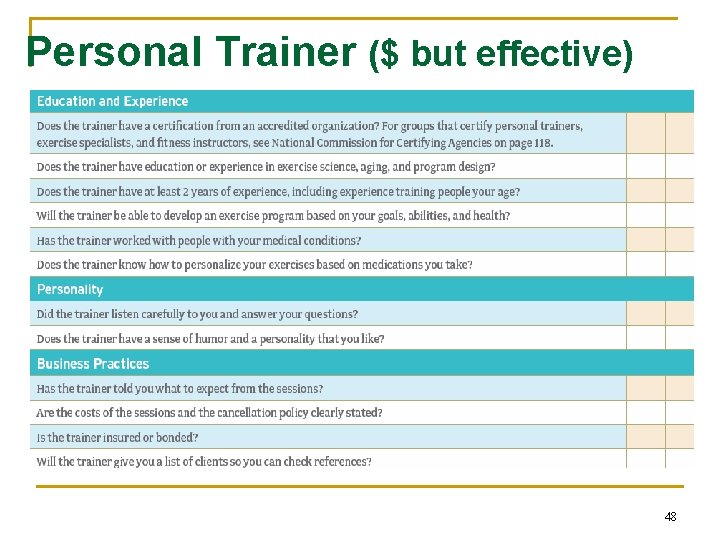
Resources – Referrals to Therapy All professionals need to “tune in” to the client’s concerns, needs, how to motivate n REFER to Physical Therapy for Evaluation q n Customized Program to address Deficits Personal Trainer skilled in older-adult needs (physiological and psychosocial) 42
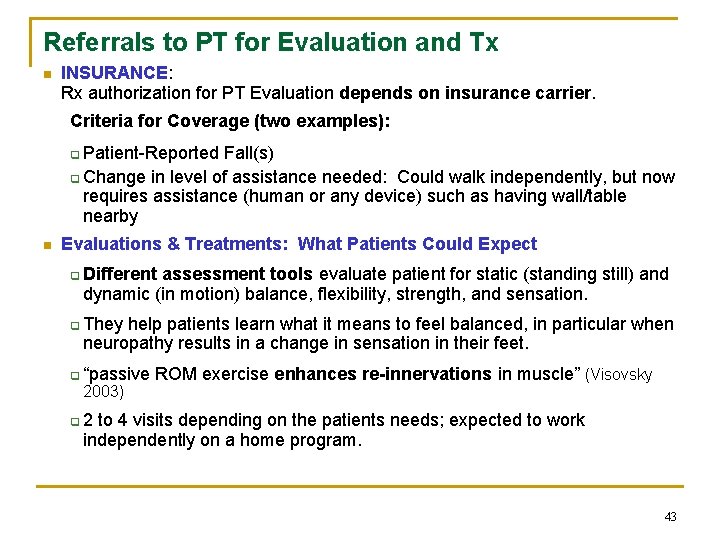
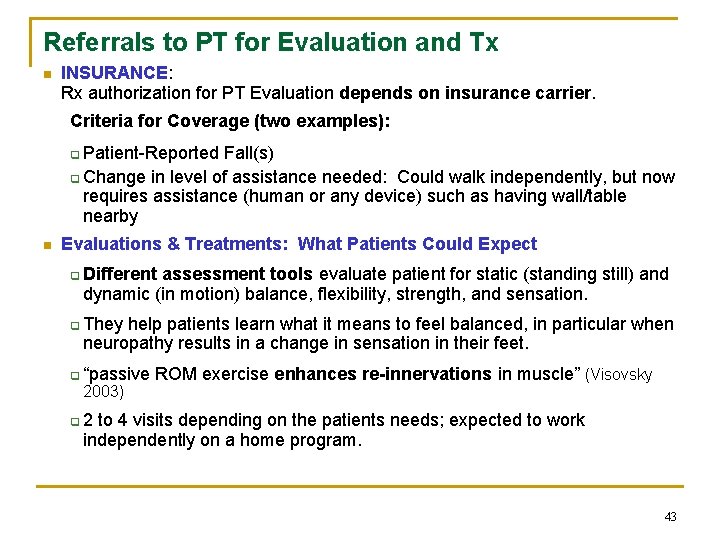
Referrals to PT for Evaluation and Tx n INSURANCE: Rx authorization for PT Evaluation depends on insurance carrier. Criteria for Coverage (two examples): q Patient-Reported Fall(s) q Change in level of assistance needed: Could walk independently, but now requires assistance (human or any device) such as having wall/table nearby n Evaluations & Treatments: What Patients Could Expect q Different assessment tools evaluate patient for static (standing still) and dynamic (in motion) balance, flexibility, strength, and sensation. q They help patients learn what it means to feel balanced, in particular when neuropathy results in a change in sensation in their feet. q “passive 2003) ROM exercise enhances re-innervations in muscle” (Visovsky q 2 to 4 visits depending on the patients needs; expected to work independently on a home program. 43
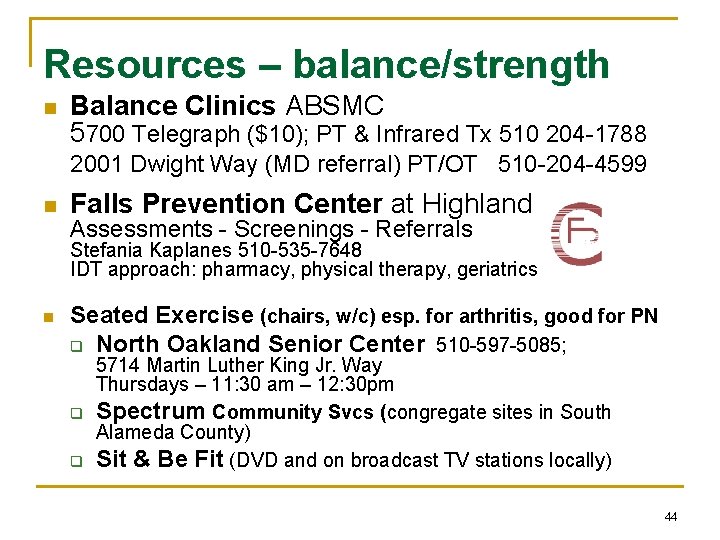
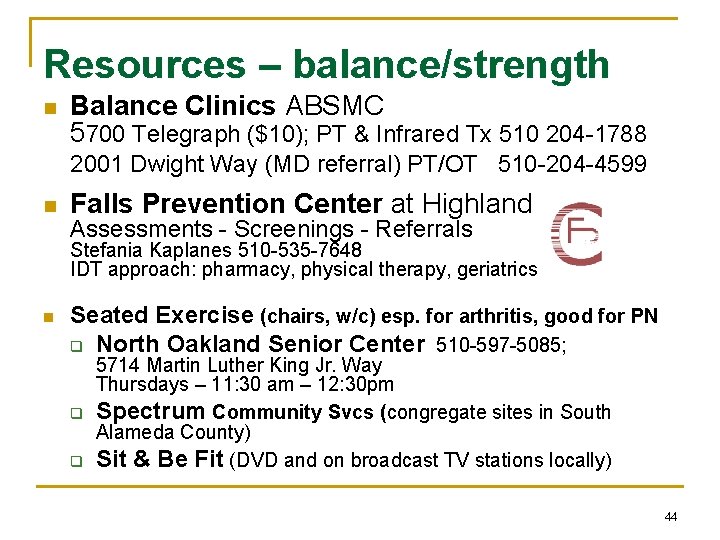
Resources – balance/strength n Balance Clinics ABSMC 5700 Telegraph ($10); PT & Infrared Tx 510 204 -1788 2001 Dwight Way (MD referral) PT/OT 510 -204 -4599 n Falls Prevention Center at Highland Assessments - Screenings - Referrals Stefania Kaplanes 510 -535 -7648 IDT approach: pharmacy, physical therapy, geriatrics n Seated Exercise (chairs, w/c) esp. for arthritis, good for PN q North Oakland Senior Center 510 -597 -5085; q q 5714 Martin Luther King Jr. Way Thursdays – 11: 30 am – 12: 30 pm Spectrum Community Svcs (congregate sites in South Alameda County) Sit & Be Fit (DVD and on broadcast TV stations locally) 44
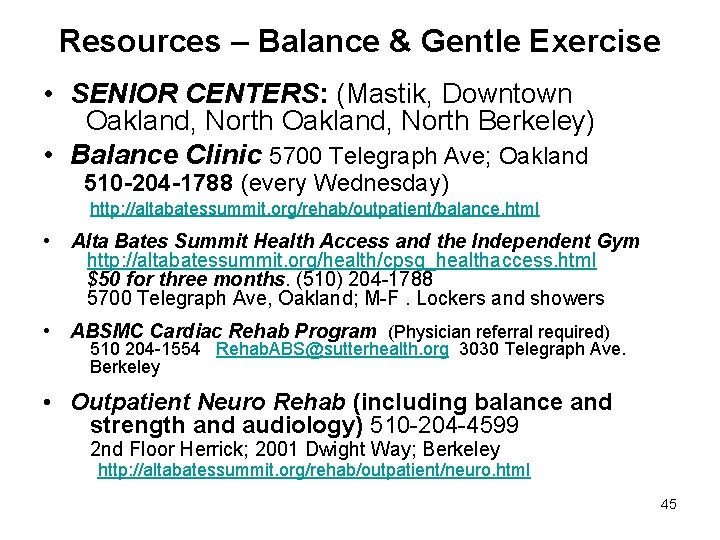
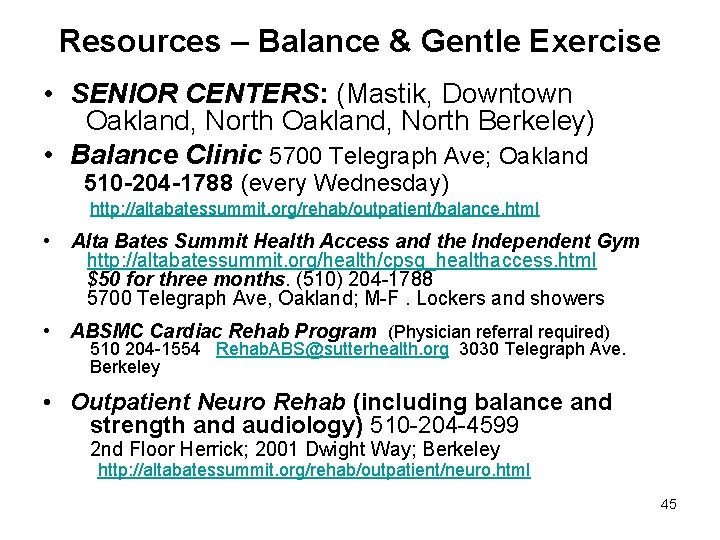
Resources – Balance & Gentle Exercise • SENIOR CENTERS: (Mastik, Downtown Oakland, North Berkeley) • Balance Clinic 5700 Telegraph Ave; Oakland 510 -204 -1788 (every Wednesday) http: //altabatessummit. org/rehab/outpatient/balance. html • Alta Bates Summit Health Access and the Independent Gym http: //altabatessummit. org/health/cpsg_healthaccess. html $50 for three months. (510) 204 -1788 5700 Telegraph Ave, Oakland; M-F. Lockers and showers • ABSMC Cardiac Rehab Program (Physician referral required) 510 204 -1554 Rehab. ABS@sutterhealth. org 3030 Telegraph Ave. Berkeley • Outpatient Neuro Rehab (including balance and strength and audiology) 510 -204 -4599 2 nd Floor Herrick; 2001 Dwight Way; Berkeley http: //altabatessummit. org/rehab/outpatient/neuro. html 45

Intervention Programs – ‘packaged’ • A Matter of Balance incorporates cognitive behavior therapy, setting realistic goals, making safety modifications to the home, and teaching exercises that increase strength and balance. Improved outcomes: reduced fear of falling and improved confidence in performing everyday tasks without fear of falling. • FIT & STRONG! For osteoarthritis teaches strength exercises and provides an educational component 46
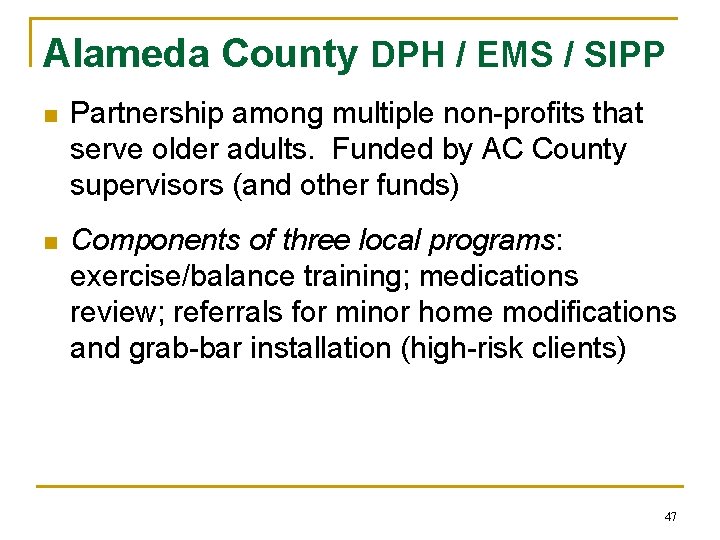
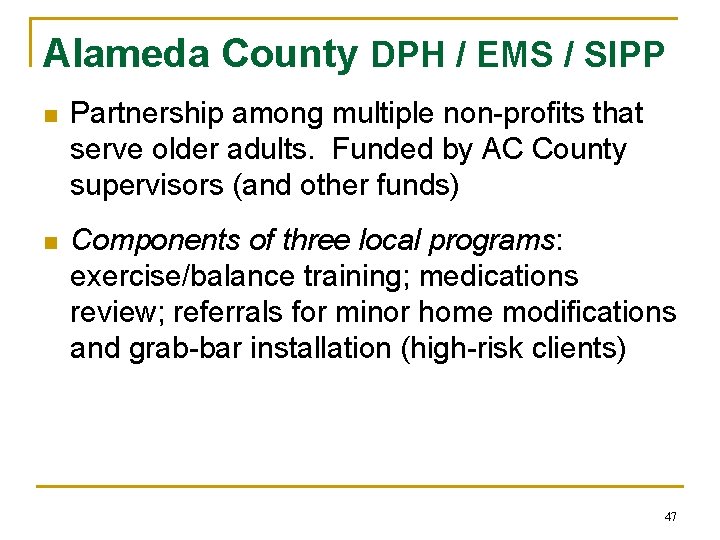
Alameda County DPH / EMS / SIPP n Partnership among multiple non-profits that serve older adults. Funded by AC County supervisors (and other funds) n Components of three local programs: exercise/balance training; medications review; referrals for minor home modifications and grab-bar installation (high-risk clients) 47
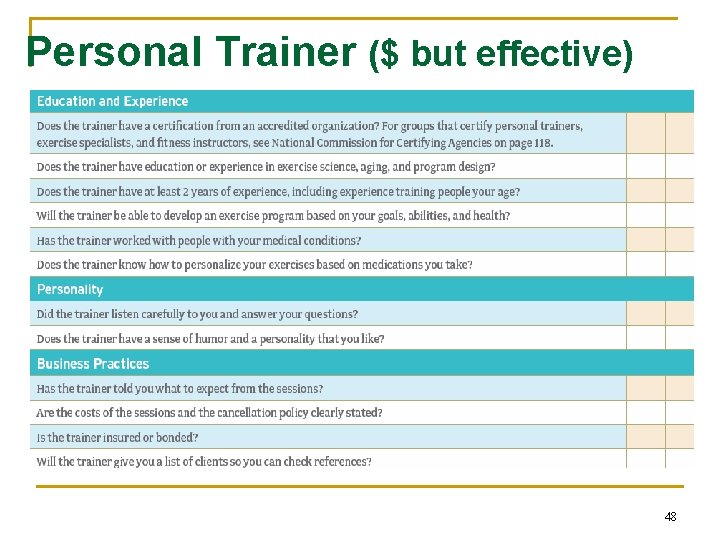
Personal Trainer ($ but effective) 48
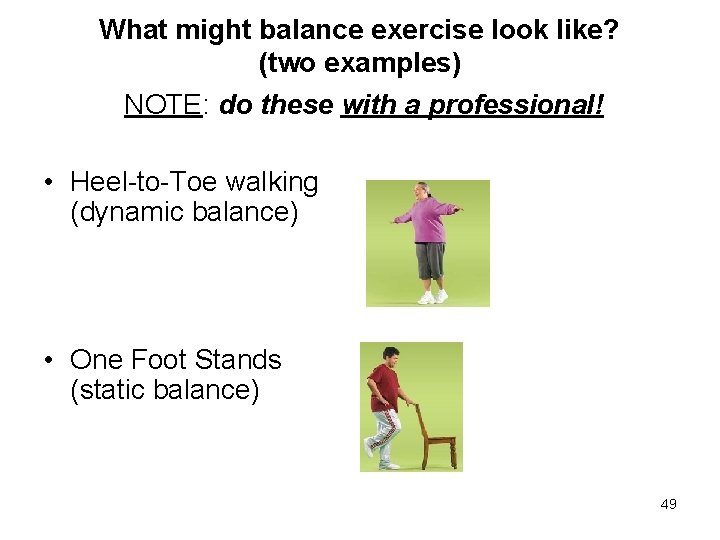
What might balance exercise look like? (two examples) NOTE: do these with a professional! • Heel-to-Toe walking (dynamic balance) • One Foot Stands (static balance) 49
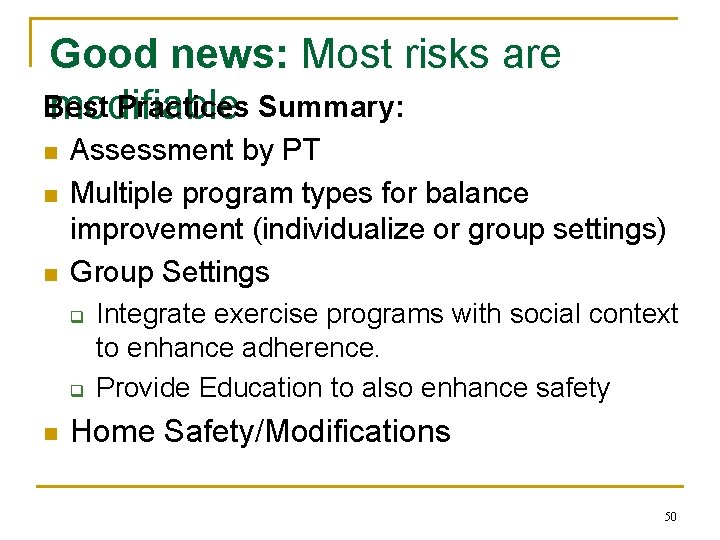
Good news: Most risks are Best Practices Summary: modifiable n n n Assessment by PT Multiple program types for balance improvement (individualize or group settings) Group Settings q q n Integrate exercise programs with social context to enhance adherence. Provide Education to also enhance safety Home Safety/Modifications 50
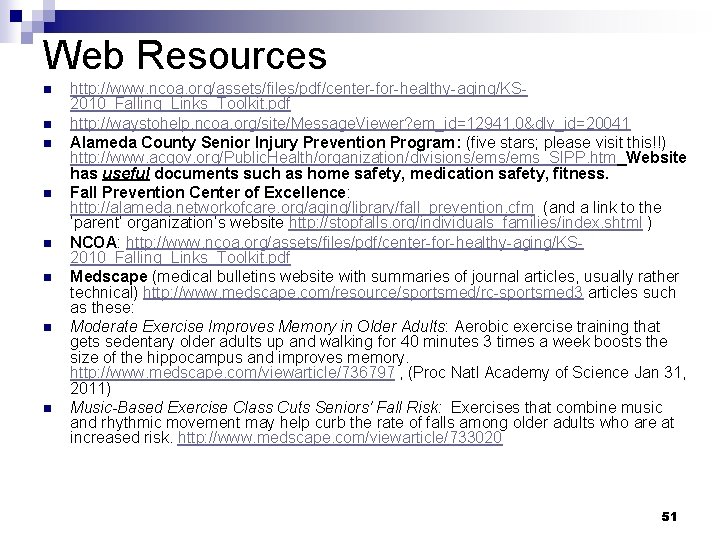
Web Resources n n n n http: //www. ncoa. org/assets/files/pdf/center-for-healthy-aging/KS 2010_Falling_Links_Toolkit. pdf http: //waystohelp. ncoa. org/site/Message. Viewer? em_id=12941. 0&dlv_id=20041 Alameda County Senior Injury Prevention Program: (five stars; please visit this!!) http: //www. acgov. org/Public. Health/organization/divisions/ems_SIPP. htm Website has useful documents such as home safety, medication safety, fitness. Fall Prevention Center of Excellence: http: //alameda. networkofcare. org/aging/library/fall_prevention. cfm (and a link to the ‘parent’ organization’s website http: //stopfalls. org/individuals_families/index. shtml ) NCOA: http: //www. ncoa. org/assets/files/pdf/center-for-healthy-aging/KS 2010_Falling_Links_Toolkit. pdf Medscape (medical bulletins website with summaries of journal articles, usually rather technical) http: //www. medscape. com/resource/sportsmed/rc-sportsmed 3 articles such as these: Moderate Exercise Improves Memory in Older Adults: Aerobic exercise training that gets sedentary older adults up and walking for 40 minutes 3 times a week boosts the size of the hippocampus and improves memory. http: //www. medscape. com/viewarticle/736797 , (Proc Natl Academy of Science Jan 31, 2011) Music-Based Exercise Class Cuts Seniors' Fall Risk: Exercises that combine music and rhythmic movement may help curb the rate of falls among older adults who are at increased risk. http: //www. medscape. com/viewarticle/733020 51
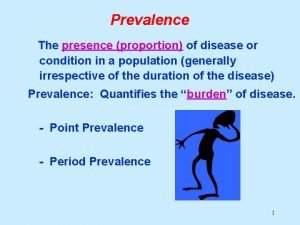
 Period prevalence vs point prevalence
Period prevalence vs point prevalence Period prevalence formula
Period prevalence formula Period prevalence vs point prevalence
Period prevalence vs point prevalence Period prevalence vs point prevalence
Period prevalence vs point prevalence Life is older older than the trees
Life is older older than the trees Mental health and older adults
Mental health and older adults Mental health and older adults
Mental health and older adults Altered cognition in older adults is commonly attributed to
Altered cognition in older adults is commonly attributed to Physical examination conclusion
Physical examination conclusion Renal
Renal Covids older adults
Covids older adults Older adults mental health
Older adults mental health Dynamic stretching for older adults
Dynamic stretching for older adults Credit risk market risk operational risk
Credit risk market risk operational risk Hester davis fall risk assessment scale
Hester davis fall risk assessment scale Falls risk assessment tool nsw
Falls risk assessment tool nsw Framp assessment
Framp assessment Falls clinic glasgow
Falls clinic glasgow What is a functional mobility assessment?
What is a functional mobility assessment? Put and take account
Put and take account Contoh soal rate epidemiologi
Contoh soal rate epidemiologi Point prevalence rate adalah
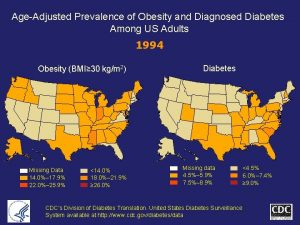
Point prevalence rate adalah Obesity prevalence europe
Obesity prevalence europe Prevalence ratio
Prevalence ratio Prevalensi adalah
Prevalensi adalah Prevalence of obesity
Prevalence of obesity Calculate prevalence rate
Calculate prevalence rate Prevalence calculation
Prevalence calculation Prevalence vs incidence
Prevalence vs incidence Ego syntonic vs dystonic
Ego syntonic vs dystonic Prevalence calculation
Prevalence calculation Prevalence vs incidence
Prevalence vs incidence Prevalence of schizophrenia
Prevalence of schizophrenia Prevalence ratio
Prevalence ratio Descriptive epidemiology
Descriptive epidemiology Prevalence ratio
Prevalence ratio Ocd prevalence
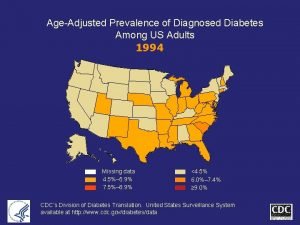
Ocd prevalence Age adjusted prevalence
Age adjusted prevalence Calculate relative risk
Calculate relative risk Who global estimates on prevalence of hearing loss 2020
Who global estimates on prevalence of hearing loss 2020 Who global estimates on prevalence of hearing loss 2020
Who global estimates on prevalence of hearing loss 2020 Adhd prevalence by country
Adhd prevalence by country Adhd prevalence by country
Adhd prevalence by country Contoh relative risk
Contoh relative risk Scleral lenses new holland
Scleral lenses new holland Prevalence
Prevalence Cvst prevalence
Cvst prevalence Prevalence
Prevalence Web accessibility for older users
Web accessibility for older users Taller and younger shorter and older
Taller and younger shorter and older Syncope in the older patient is
Syncope in the older patient is Synformal anticline
Synformal anticline