Falls and Fall Prevention Prevalence of Falls in








- Slides: 33

Falls and Fall Prevention
Prevalence of Falls in Older Adults § 33% of older adults fall each year § Falls are the leading cause of fatal and nonfatal injuries § Falls rates increase with age
Falls Prevalence (continued) § Every 15 seconds, an older adult is treated in an ER for fall-related injuries § Every 29 minutes, an older adult dies from a fall
Non-fatal Fall Injuries § Major cause of serious injury § Most common cause of hospital admission § 1. 6 million older adults are treated in EDs § Fall injury rates 72% higher for women than men § More women are hospitalized for injuries than men
Fall-related Fracture Injuries § Most prevalent of all fall injuries § Related to osteoporosis § Over 95% of hip fractures are caused by falls • Hip fracture leads to hospital admission • 20% of people with hip fracture die within 1 year • Survivors experience significant disability
Costs of Falls § Total cost of all fall injuries for older adults = $28. 3 BILLION per year • Average health care cost for fall injury = $19, 440 § 2020 estimate is $54. 9 BILLION § Costs driven by hospitalization due to fractures • Hip fractures most costly

Other “Costs” Related to Falls § Disability § Functional limitations § Decreased productivity § Reduced quality of life • Fear of falling
Risk Factors for Falls § Personal • Age • Functional status • Chronic conditions § Environmental • Fall and tripping hazards
Can Fall Risk Be Reduced? § Non-modifiable risk § Modifiable risk
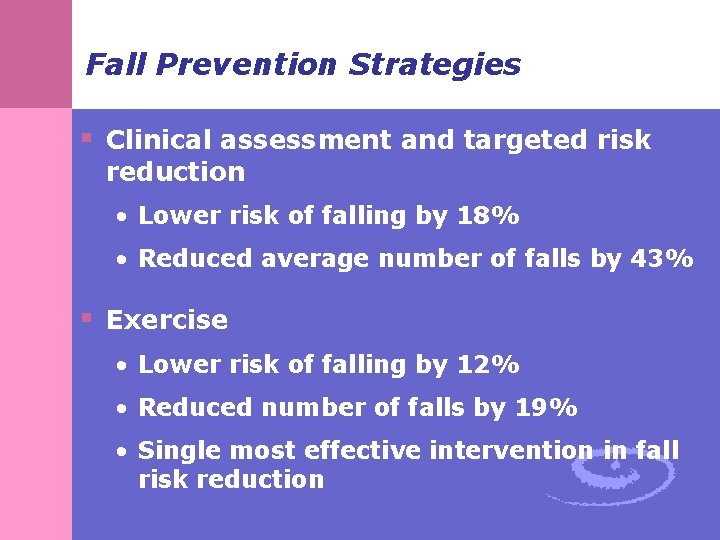
Fall Prevention Strategies § Clinical assessment and targeted risk reduction • Lower risk of falling by 18% • Reduced average number of falls by 43% § Exercise • Lower risk of falling by 12% • Reduced number of falls by 19% • Single most effective intervention in fall risk reduction

More Fall Prevention Strategies § Medication management § Home modifications • Home safety assessment • Remove fall and tripping hazards § Hip protectors § Multi-component strategies

Falls Injury Prevention Model Points of Intervention Continuum
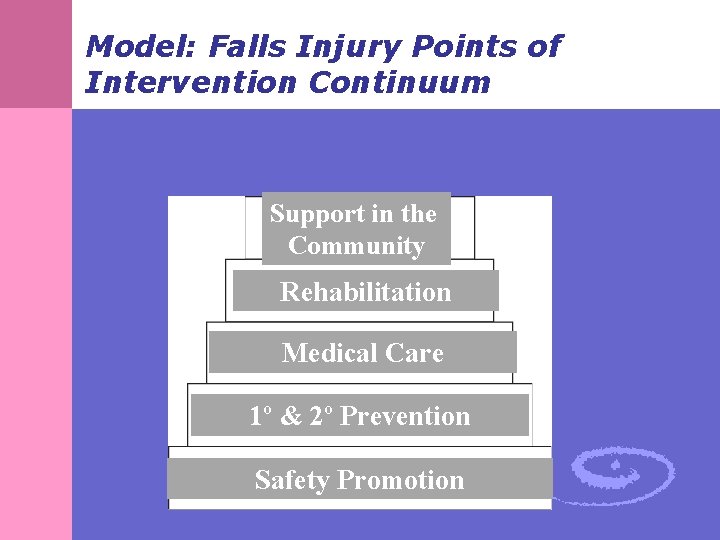
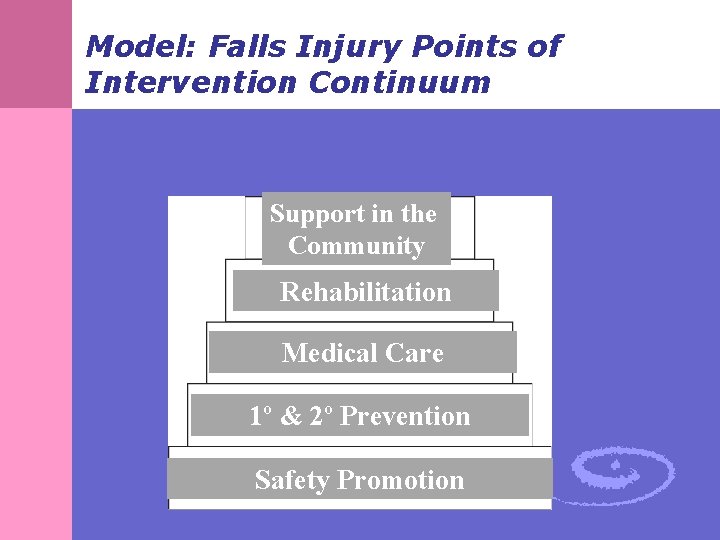
Model: Falls Injury Points of Intervention Continuum Support in the Community Rehabilitation Medical Care 1º & 2º Prevention Safety Promotion
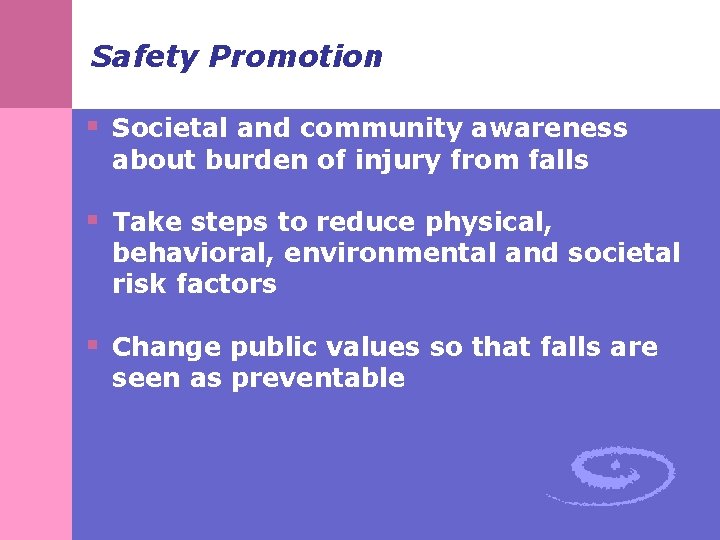
Safety Promotion § Societal and community awareness about burden of injury from falls § Take steps to reduce physical, behavioral, environmental and societal risk factors § Change public values so that falls are seen as preventable

Primary Prevention § Focus on preventing the first fall § Includes: • Risk identification and modification • Treatment of medical illnesses • Home safety/environmental modifications • Physical activity to promote strength and balance
Secondary Prevention § Aims to minimize the injury or complications once a fall occurs § Prevent future falls § Examples: • Improving bone health to prevent fractures • Personal alarm system for help • Hip protectors • Teaching older person how to get up from fall
Emergency, Primary & Acute Medical Care § Goal: reduction in future morbidity and mortality and improvement of outcomes following a fall § Includes: • Emergency response and transport • Treatment by physicians • Referral for surgery & rehabilitation • Correction of factors leading to the fall
Tertiary Prevention: Rehabilitation § Aim is to maximize the level of functioning after a fall and prevent future falls § Activities to prevent long-term complications and disability after a fall § Address gait and balance issues, focus on strengthening lower body muscles

Support in the Community § Post fall injury, appropriate home and medical support to enable and promote independence § Examples: • Community-based fall prevention program • Community-based exercise program • Home care services

Fall Prevention Programs
Step by Step Falls Prevention Program § Goals: • Enhance knowledge about falls and preventive behavior • Embed falls prevention into senior centers and enhance relationships between centers and providers § Focus: Physical activity and behavior modification § Target: Community-dwelling older adults § Located in Senior centers and facilitated by senior center staff
Step by Step Program Activities § Falls risk assessment § “Passbook” with tips on falls prevention § Balance exercises § Emphasized “appropriate” exercise level • Program was ongoing
A Matter of Balance § A Matter of Balance acknowledges the risk of falling but emphasizes practical coping strategies to reduce this fear, including: § Promoting a view of falls and fear of falling as controllable § Setting realistic goals for increasing activity § Changing the environment to reduce fall risk factors § Promoting exercise to increase strength and balance
MOB Program Goal § The program’s goal is to reduce fear of falling, stop the fear of falling cycle, and increase activity levels among community-dwelling older adults.
MOB Program Rationale § Studies indicate that up to half of community dwelling older adults experience fear of falling and that many respond to this concern by curtailing activity § A majority of falls occur during routine activities § Falls usually are not caused by just one issue § A large portion of falls are preventable § Being inactive results in loss of muscle strength and balance

MOB Program Focus § Fear of falling can actually contribute to falling § Participants learn to view falls and fear of falling as controllable and set realistic goals for increasing activity § Participants find ways to change the environment and learn simple exercises to increase strength and balance § The group format provides an opportunity for people with a common problem to learn from each other
MOB Program Components § Group discussion § Cognitive § Skill building restructuring— learning to shift from negative to positive § Assertiveness § Thinking patterns § Problem-solving training § Exercise training § Sharing practical solutions or thinking about something in a different way.
MOB Program Logistics § Length/Timeframe of program: eight twohour classes § Recommended class size: 10 -12 participants (minimum of 8, maximum of 14 ) § Target population: people who are 60 or older, ambulatory, able to problem-solve, concerned about falls and interested in improving flexibility, balance, and strength
MOB Desired Outcomes § View falls and fear of falling as controllable § Set realistic goals for increasing activity § Change participants’ environment to reduce fall risk factors § Increase strength and balance through exercise
MOB Measurement Tools § Survey (given during the first class) with questions regarding falls management, exercise levels, and background information § Last class survey; repeat of questions regarding falls management and exercise levels § Last class evaluation with questions concerning comfort in talking about fear of falling, changes made to environment, comfort in increasing activity levels, plans to increase activity levels, and background information.
MOB Results § 97% of participants are more comfortable talking about fear of falling § 97% feel comfortable increasing activity § 99% plan to continue exercising § 98% would recommend MOB (Healy, Mc. Mahon, & Haynes, 2006)
 Primary prevention secondary prevention tertiary prevention
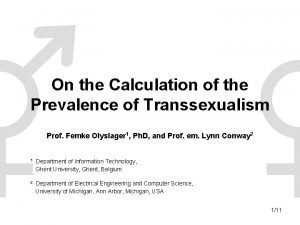
Primary prevention secondary prevention tertiary prevention Period prevalence vs point prevalence
Period prevalence vs point prevalence Defination of incidence
Defination of incidence Period prevalence vs point prevalence
Period prevalence vs point prevalence Period prevalence vs point prevalence
Period prevalence vs point prevalence National guidance on falls prevention scotland
National guidance on falls prevention scotland Fall prevention quiz
Fall prevention quiz 5 ps of fall prevention
5 ps of fall prevention Examples of smart goals for fall prevention
Examples of smart goals for fall prevention Chapter 14 fall prevention
Chapter 14 fall prevention S-p-l-a-t-t fall prevention
S-p-l-a-t-t fall prevention Fall prevention interventions
Fall prevention interventions Mullinure hospital armagh
Mullinure hospital armagh Fall prevention interventions
Fall prevention interventions Fall prevention interventions
Fall prevention interventions Fall prevention occupational therapy
Fall prevention occupational therapy How to calculate prevalence
How to calculate prevalence How to calculate incidence rate example
How to calculate incidence rate example Cara menghitung secondary attack rate
Cara menghitung secondary attack rate Epidemiologi adalah
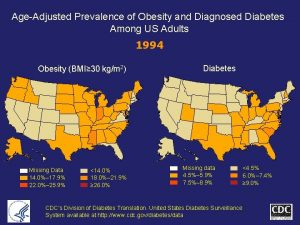
Epidemiologi adalah Obesity prevalence europe
Obesity prevalence europe Prevalence ratio
Prevalence ratio Prevalensi adalah
Prevalensi adalah Prevalence of obesity
Prevalence of obesity Calculate prevalence rate
Calculate prevalence rate Prevalence calculation
Prevalence calculation Incidence vs prevalence
Incidence vs prevalence Ocd vs anxiety
Ocd vs anxiety Epirates
Epirates Prevalence of schizophrenia
Prevalence of schizophrenia Prevalence ratio
Prevalence ratio Calculate prevalence rate
Calculate prevalence rate Ocd prevalence
Ocd prevalence Age adjusted prevalence
Age adjusted prevalence