Fall Prevention Standard 10 Preventing Falls and Harm


- Slides: 31
Fall Prevention (Standard 10: Preventing Falls and Harm from Falls) 2017
Session Plan Fall Prevention At the end of this session you will be able to: • Locate the fall prevention policy • Define a fall • State fall risk factors • State how & when to complete a patient falls risk assessment • State how to complete the Falls Risk Assessment & Falls Prevention Plan (MR 10) • State what to do after a patient falls Page 2
Introduction ‘Falls are a significant cause of harm to older people. The rate, intensity and cost of falls identify them as a national safety and quality issue’. The aim of fall prevention programs is to reduce the number of falls, and the harm caused by falls, experienced by people in hospital care. St Vincent’s Private Hospital Melbourne (SVPHM) has implemented policies, procedures and resources to decrease patient falls and harm from falls. (Australian Commission on Safety and Quality in Health Care (ACSQHC). Preventing Falls and Harm From Falls in Older People: Best Practice Guidelines for Australian Hospitals 2009) Page 3

Falls data • Every year approx 30% Australians > 65 years old, fall o 10% of these falls lead to injury Pointer S, Harrison J and Bradley C (2003). National Injury Prevention Plan Priorities for 2004 and Beyond: discussion paper, Australian Institute of Health and Welfare, Canberra • In 2002, death rate from falls (all settings) ranged from: o 18 deaths per 100, 000 people (aged 65‑ 84 years) o 81 deaths per 100, 000 people (aged 85 years and older) Australian Bureau of Statistics (ABS) The Health of Older People, Australia (2004) http: //www. abs. gov. au Page 4

National Standards In 2013 the Australian Commission on Safety and Quality in Health Care (ACSQHC) introduced the National Safety and Quality Health Service (NSQHS) Standards. Guidelines were produced to address patient fall prevention. Page 5
Fall definition Various definitions of a fall have been developed. St Vincent’s Private Hospital Melbourne (SVPHM) has adopted the World Health Organisation (WHO) definition of a fall: ‘. . . inadvertently coming to rest on the ground, floor or other lower level, excluding intentional change in position, to rest on furniture, wall or other objects’. Fall examples: • standing then falling back onto bed or chair • trip or stumble then fall onto floor • limb falls off operating table • standing in bathroom then fall back onto toilet • patient has a vasovagal episode and falls World Health Organisation, WHO Global Report on Falls Prevention in Older Age, Geneva, 2007, p Page 6
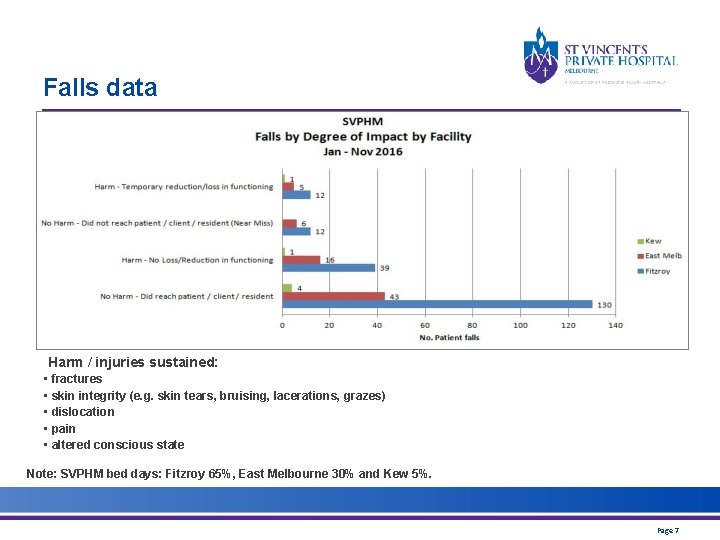
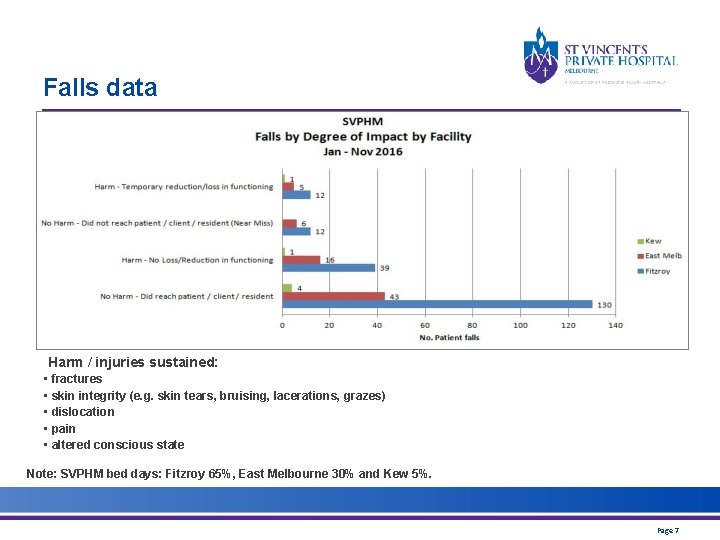
Falls data Harm / injuries sustained: • fractures • skin integrity (e. g. skin tears, bruising, lacerations, grazes) • dislocation • pain • altered conscious state Note: SVPHM bed days: Fitzroy 65%, East Melbourne 30% and Kew 5%. Page 7
When do most falls occur? Falls occur at any hour of the day or night however: most falls occur between 09: 00 – 12: 00 This is the period when patients require: • assistance with personal hygiene & toileting • pre-operative preparation • post surgery care • discharge. Page 8
Policy SVPHM has revised and published the following policy: • Falls Prevention, Minimising Harm from Falls and Post Fall Management Policy SVPHM ‘Policy and Protocols’ are accessed via the intranet. Page 9
Risk Assessment SVPHM Falls Risk Assessment & Falls Prevention Plan (FRA&FPP) (MR 10) is based on Australian and international guidelines. The aim is: • to identify each patient’s individual falls risk factors • to implement falls prevention strategies - against each identified risk factor • to keep all falls related documentation together • nurses guide referral to the multidisciplinary team (as required) o including allied health, pharmacy & discharge planning • to comply with Standard 10: Preventing Falls & Harm from Falls. Page 10
Risk Assessment Note: Scores & ratings are not used: individual risk factors are addressed. One risk factor: patient is ‘at risk of falling’. Five risk factors: patient is ‘at risk of falling’. Clinical handover: • Select ‘Falls’ under Risk on IBA handover sheet. • Ensure falls risk factors and fall prevention strategies are included in handover according to: o Clinical Handover Policy § ‘i. SHARED’ Page 11
Falls Risk Assessment & Prevention Plan • Patients must be assessed: o on admission (section A) o every day (early on day shift) (section B) o after any change in condition (i. e. post op) & environment (section B) o after a fall (sections C & B, Risk. Man) • Assess individual risk factors • Implement fall & harm prevention strategies • Communicate with patient / carer Page 12
Falls Risk Assessment Use Clinical Judgement • Assessment categories: o o o o falls history mobility cognition and behaviour continence dizziness and loss of consciousness medications vision risk of injury from falling • Complete assessment with the patient and/or carer Page 13
Falls Prevention Plan Fall prevention strategies: ALL patients • Orientate patient to room, bathroom, ward & call bell • Ensure call bell, visual aids, phone & mobility aids are within reach • Ensure bed brakes are employed at all times • Position over-bed table on the most appropriate side of bed • Position IV pole & other devices on the most appropriate side of bed • Clear room of unnecessary obstacles • Advise patient about appropriate safe footwear • Use bed rails only when appropriate • Set bed and chair at appropriate height o patient’s feet flat on the ground & hips slightly higher than their knees • Consider placement of patient in ward Page 14
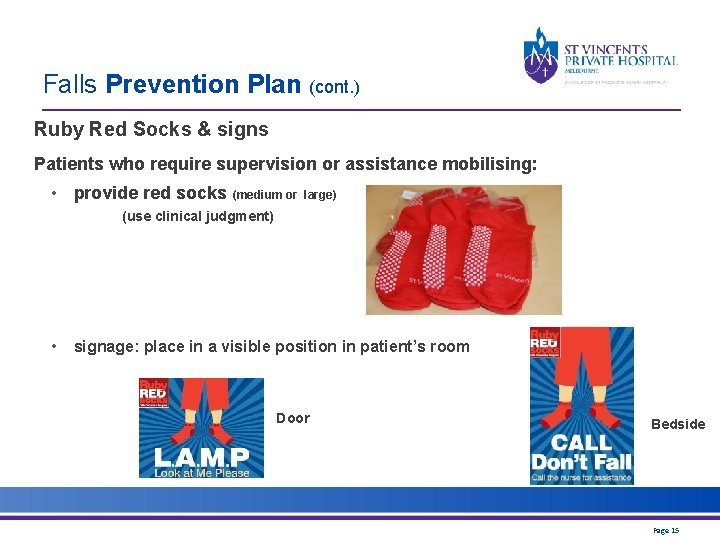
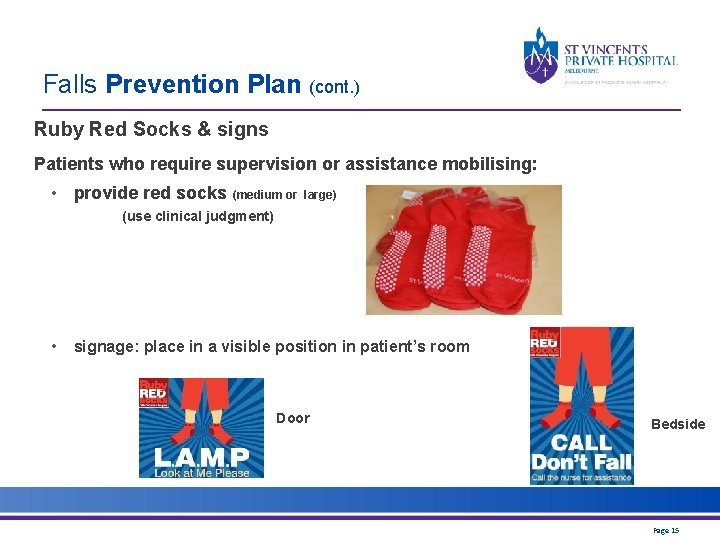
Falls Prevention Plan (cont. ) Ruby Red Socks & signs Patients who require supervision or assistance mobilising: • provide red socks (medium or large) (use clinical judgment) • signage: place in a visible position in patient’s room Door Bedside Page 15
Falls Prevention Plan (cont. ) Use Clinical Judgement Strategies: address specific risk factors If a fall risk factor is identified as being present, then the corresponding fall prevention strategies are implemented. e. g. Does the patient use a mobility aid? YES Select & implement appropriate fall prevention strategies: • Refer to physiotherapist • Supervise mobility & transfers • Provide Ruby Red Socks • Attach signs: Call Don’t Fall & Look at Me Please • Set bed & chair at an appropriate height • Set up room & bathroom with aids & equipment as required • Advise patient to ask for help when mobilising Page 16
Falls Prevention Plan (cont. ) Use Clinical Judgement Additional fall prevention strategies Consider the following strategies in complex patients or patients with multiple risk factors: • • bed/chair alarm low bed constant one on one supervision last option: chemical or mechanical restraint (medical approval required) o refer to Restraint of Patient (Adult) Policy: o strict monitoring and documentation requirements. Page 17
Falls risk assessment example: A 75 y/o patient was admitted with a medical condition. FALLS RISK ASSESSMENT: • history of falling in the past 12 months • currently uses mobility aids • incontinent of urine FALL PREVENTION STRATEGIES: • supervise mobility and transfers • refer for an assessment by a physiotherapist • display fall prevention signs • provide Ruby Red Socks (use clinical judgement) • educate patient regarding falls risk: request patient calls staff for assistance • MSU • toileting regime • continence aids Page 18
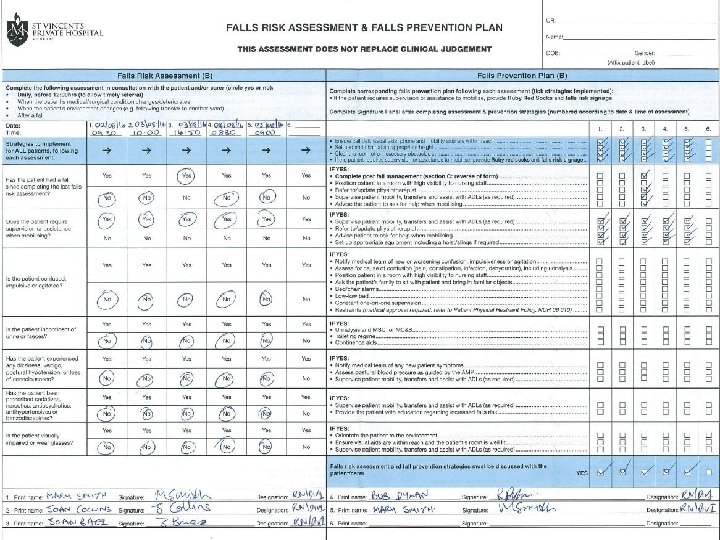
Falls Risk Assessment & Falls Prevention Plan (MR 10) The MR 10 form was revised and updated in July 2016 based on: • form audit results • staff survey results What has changed on the form (MR 10): • Date and time have been added to Risk Assessment columns. • Risk Assessment, Prevention Plan & Signature Panel are all linked by number. o e. g. Column ‘ 1’ Risk Assessment (including date & time) is associated with column ‘ 1’ in Prevention Plan and ‘ 1’ on Signature panel. • Strategies for ALL patients & discussion with patient/carer sections are highlighted. • Post Fall Management (section C): most items are mandatory. Page 19
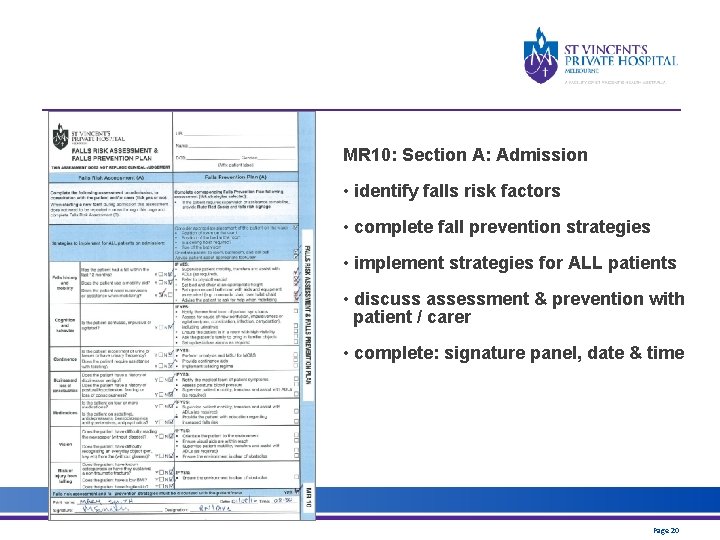
MR 10: Section A: Admission • identify falls risk factors • complete fall prevention strategies • implement strategies for ALL patients • discuss assessment & prevention with patient / carer • complete: signature panel, date & time Page 20
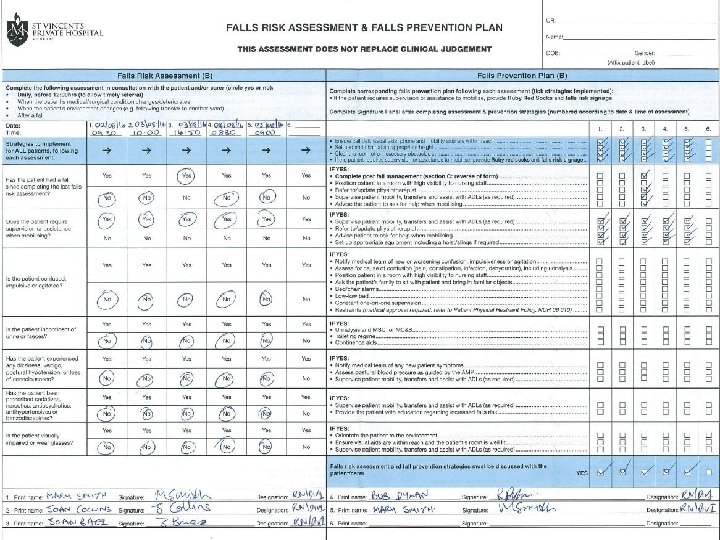
Falls Risk Assessment & Falls Prevention Plan (MR 10): Section B: Assessments • Date & time • Implement ‘strategies for ALL patients’ • Identify fall risk factors • Complete & implement fall prevention strategies • Discuss assessment & prevention with patient/carer • Complete signature panel Refer to next slide Page 21
Page 22
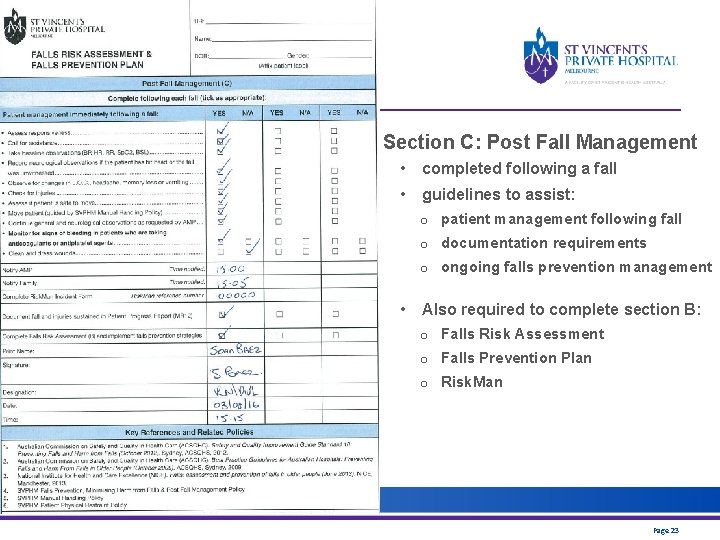
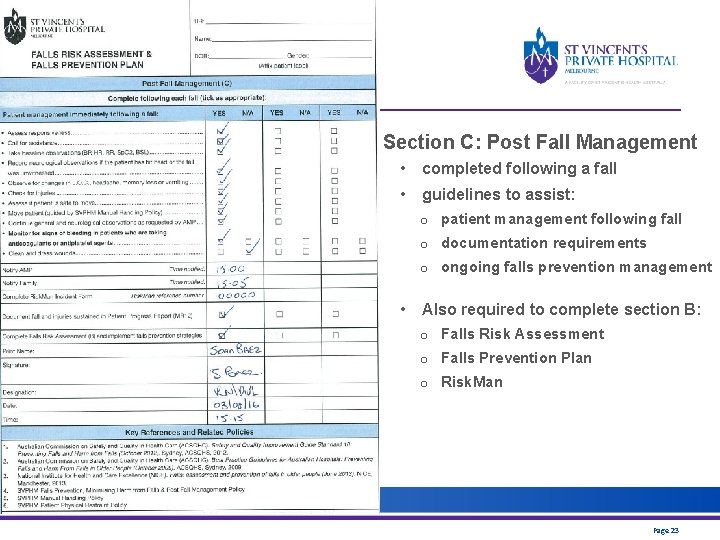
Section C: Post Fall Management • completed following a fall • guidelines to assist: o patient management following fall o documentation requirements o ongoing falls prevention management • Also required to complete section B: o Falls Risk Assessment o Falls Prevention Plan o Risk. Man Page 23
Post fall management: example A patient falls while walking to the bathroom unassisted: • Assess responsiveness • Call for help • Apply first aid • Take baseline observations of vital signs and neurological observations • Check for injuries • Assess if the patient is safe to move • Move the patient (using correct manual handling techniques) • Notify AMP • Notify family / next of kin • Complete Post Fall Management: section C of FRA&FPP (MR 10) • Complete section B of FRA&FPP (MR 10): revise fall prevention strategies • Complete a Risk. Man incident report & document incident in the patient’s medical record • Continue observations as required/requested Page 24
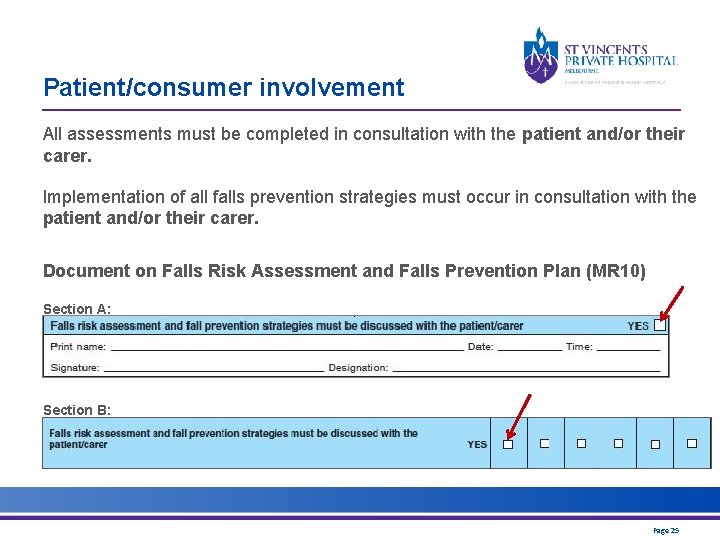
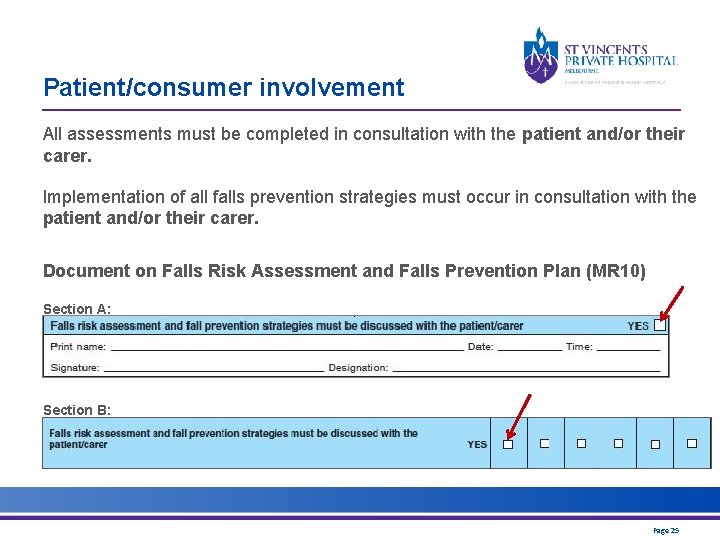
Patient/consumer involvement All assessments must be completed in consultation with the patient and/or their carer. Implementation of all falls prevention strategies must occur in consultation with the patient and/or their carer. Document on Falls Risk Assessment and Falls Prevention Plan (MR 10) Section A: Section B: Page 25
Falls with Harm A Risk. Man incident report is completed when a patient falls. Select: • Classification = Fall If a skin tear, laceration, graze or bruise is sustained, ALSO select: • Skin Tear or Wound (as appropriate) o document treatment including name/type of dressing applied (if applicable) Page 26
Prevent patient falls in theatre Between Jan 2013 - Nov 2015, 63% of patient falls in theatre (all facilities) involved a patient’s limb falling off the operating table OR a patient falling off the operating table (includes near miss falls). Patient limbs falling off the operating table sits within the WHO fall definition: ‘. . . inadvertently coming to rest on the ground, floor or other lower level, excluding intentional change in position to rest on furniture, wall or other objects’. Ensure: • communication between multidisciplinary teams regarding patient positioning • bed and operating table brakes are engaged prior to any transfer • patients are safely secured to the operating table by positioning, attaching arm boards or straps (as required). Page 27
Bed rails should only be used to reduce the risk of a patient accidentally slipping, sliding, falling or rolling out of a bed. Bed rails used for this purpose are not a form of restraint. Decisions about bed rail use are a balance between competing risks. Bed rails should NOT usually be used: • if the patient is agile enough, and confused enough, to climb over them. Bed rails should be used: • if the patient is being transported on their bed; • in areas where patients are recovering from anaesthetic or sedation and are under constant observation. Staff should use their professional judgement to consider the risks and benefits of bed rail use for individual patients. Discuss patient preferences and safety requirements with patients and their families and document these discussions. Page 28
Falls Reporting All patient falls are reported to managers, clinicians and family. Patient fall data & rate reports are distributed to NUMs & DONs monthly. Falls with serious HARM are reported internally to SVPHM: • Directors of Nursing/General Managers • CEO • NUM completes Fall Investigation Report • Fall Prevention Committee discuss fall Falls with serious HARM are reported to: • St Vincent’s Health Australia (SVHA) Private Hospital Division: o Director Clinical Governance Falls with serious HARM include: o CEO fall with fracture • SVHA legal team fall with closed head injury Page 29
Summary Revised Falls Risk Assessment and Falls Prevention Plan: • Assessments: o on admission o daily (early on day shift) o after environment change (e. g. ward change) o after condition change (e. g. post surgery) o after a fall • Assess patient’s falls risk factors • Implement fall and harm prevention strategies } include patient &/or carer • Post fall assessment is entered on the same form • One fall risk factor = falls risk (ensure handover/IBA) Page 30
References • Australian Commission on Safety and Quality in Health Care (ACSQHC). Preventing Falls & Harm From Falls in Older People Best Practice Guidelines for Australian Hospitals, 2009 • Australian Commission on Safety and Quality in Health Care (ACSQHC). Safety and Quality Improvement Guide Standard 10: Preventing Falls and Harm from Falls. Sydney. 2012. • King Edward Memorial Hospital (KEMH). Clinical Guidelines: 2. 12 Falls Prevention at King Edward Memorial Hospital. Perth Western Australia. September 2010 • Myer, C. An exploration of the translation of falls prevention knowledge for community-dwelling people living with dementia. Falls Prevention Summit, Brisbane, May 2013 • National Institute for Care and Excellence (NICE). Falls: assessment and prevention of falls in older people. NICE clinical guideline 161. UK. Issued: June 2013. Page 31