Falls In Patient and Community Falls Pathway Prevention











- Slides: 26

Falls In Patient and Community Falls Pathway Prevention / Risk Reduction and Management Policy Training NTW (0)40 March 2018

Outcomes By the end of the session you will be able to: • Outline the significance of falls for the patient and the Trust • Identify risk factors associated with falls • Describe multi-factorial assessment/interventions and your responsibilities in relation to falls assessment and management • Have awareness and understanding of In Patient and Community Fall Pathways which includes other providers/agencies.
Introduction The aim of the policy/pathway is to provide clinicians with a strategy to: • Have awareness of assessment required for identified risk factors • Target multi-disciplinary or multi agency interventions • Influence a reduction in falls rates
Definition A fall is defined as an event whereby An individual comes to rest on the ground or other lower level with or without the loss of consciousness. ( Rubinstein 1986 )

Background and Significance • Falls are among the most common and serious problems facing the older population. • Falling is associated with considerable mortality, mobility, reduced functioning, anxiety, depression, social isolation and loss of confidence. • Incident rates of falls in hospitals are almost 3 times the rate for the community. • Falls comprise of a quarter of all types of patient safety incidents reported from mental health units. (NPSA 2007). • Reducing falls has become a national agenda for both in patient and community linking with Safety Thermometer. • NICE guideline CG 161: Falls: assessment and prevention of falls in older people June 2013

NICE Guidelines 2013 • Falls and fall-related injuries are a common and serious problem for older people. People aged 65 and older have the highest risk of falling, with 30% of people older than 65 and 50% of people older than 80 falling at least once a year. • The human cost of falling includes distress, pain, injury, loss of confidence, loss of independence and mortality. Falling also affects the family members and carers of people who fall. Falls are estimated to cost the NHS more than £ 2. 3 billion per year. Therefore falling has an impact on quality of life, health and healthcare costs. • People aged 50 to 64 who are admitted to hospital and are judged by a clinician to be at higher risk of falling because of an underlying condition are also covered by the guideline recommendations about assessing and preventing falls in older people during a hospital stay.
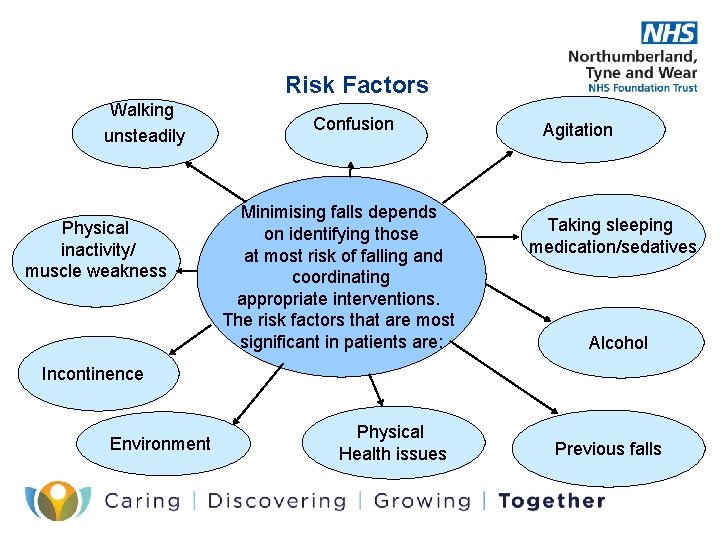
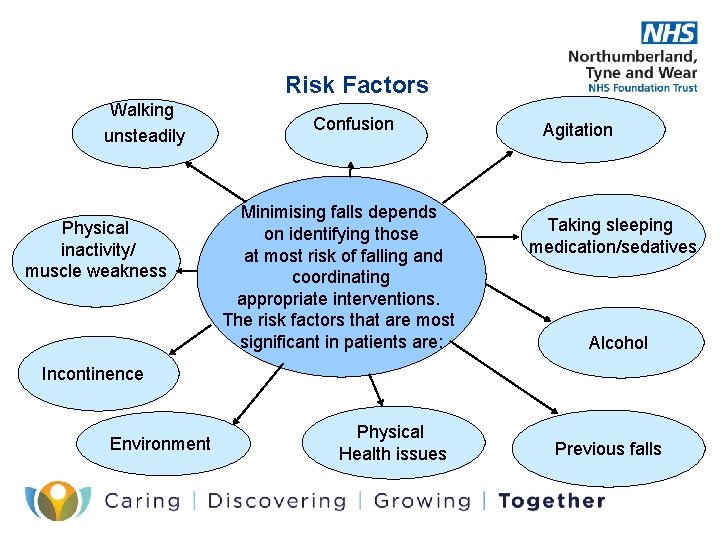
Risk Factors Walking unsteadily Physical inactivity/ muscle weakness Confusion Minimising falls depends on identifying those at most risk of falling and coordinating appropriate interventions. The risk factors that are most significant in patients are: Agitation Taking sleeping medication/sedatives Alcohol Incontinence Environment Physical Health issues Previous falls

Impact of Falls • Psychological Effects- Even falls where no physical injury occurs can lead to worry and distress for patients, their families and staff. • Prolonged Hospital Stays- The pain and discomfort from even minor injuries can delay patients recovery and extend their length of stay • Loss of independence- limb fractures can have a profound effect on patients ability to maintain or regain independence • Secondary Complications- In frail older patients this can happen ie if someone has a pelvic fracture their mobility is reduced and they are then at greater risk of DVT or pressure ulcer • Low Survival Rates- If a patient fractures a hip while already ill in hospital there is a 3 in 10 chance they will not survive and only 1 in 10 chance of getting back to their previous level of independence
Falls Assessment • NTW Falls assessment tool is a rapid method of assessing a patients likelihood of falling and the things which are most likely to be contributing factors. • This is located within core assessment. • Consists of factors including types of falls people have experienced, medication, medical history, sensory communication and physical health • Each factor generates a score which identifies the level of need. • Scores provide guidance to the level of need and interventions required however this DOES NOT preclude clinical judgement. • Once the patients needs have been identified it is necessary to implement any referrals to other professionals and service providers. • For in patient areas a care plan aimed at modifying the risk factors should be devised by members of the MDT. • For community services care planning should focus on sign posting to relevant internal and external services and supplying service user/carer information leaflets

Falls Assessment Tool



Community Clinicians Responsibilities • On initial assessment obtain the patients history/risk of falls via FACE and or narrative risk assessment. • Complete falls assessment tool if indicated. • Sign post to relevant internal and or external services/professionals. • Care planning will usually entail completion of onward referral and leaflet advice as evidenced by tick boxes on Falls Assessment tool, supplemented by inclusion in initial care plan as part of the initial assessment. • This should be done with a collaborative approach including patient, relative and MDT. • In complex circumstances specific care planning should still be undertaken in consultation with / where no other Primary Care Professional is involved
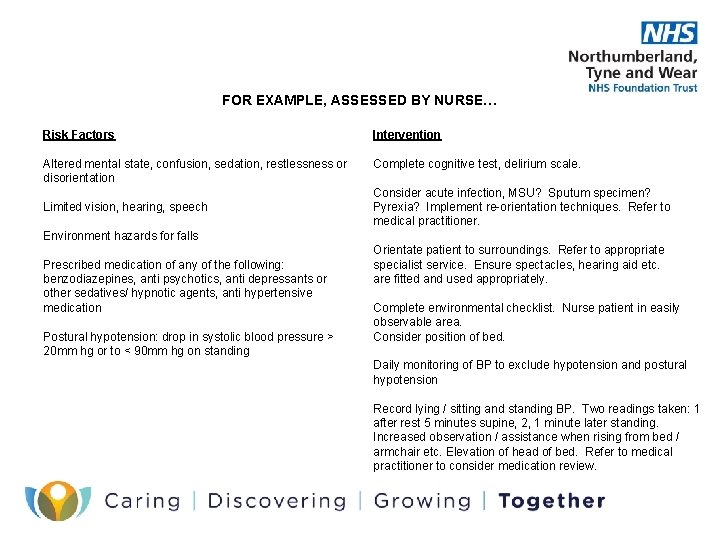
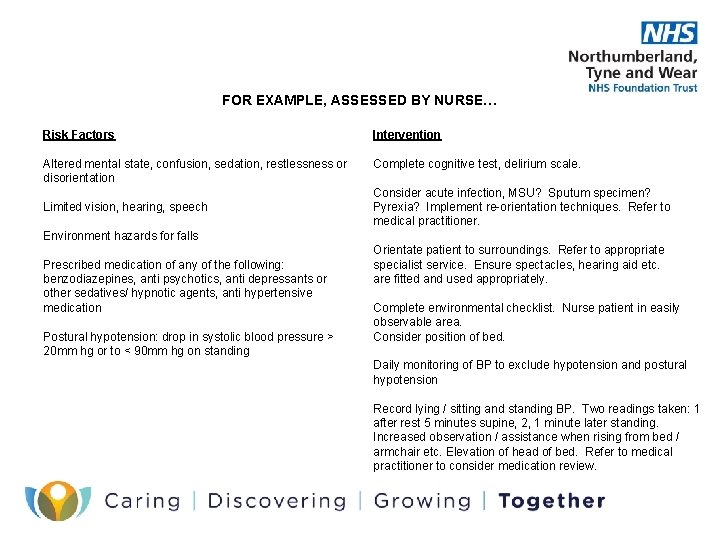
FOR EXAMPLE, ASSESSED BY NURSE… Risk Factors Intervention Altered mental state, confusion, sedation, restlessness or disorientation Complete cognitive test, delirium scale. Limited vision, hearing, speech Consider acute infection, MSU? Sputum specimen? Pyrexia? Implement re-orientation techniques. Refer to medical practitioner. Environment hazards for falls Prescribed medication of any of the following: benzodiazepines, anti psychotics, anti depressants or other sedatives/ hypnotic agents, anti hypertensive medication Postural hypotension: drop in systolic blood pressure > 20 mm hg or to < 90 mm hg on standing Orientate patient to surroundings. Refer to appropriate specialist service. Ensure spectacles, hearing aid etc. are fitted and used appropriately. Complete environmental checklist. Nurse patient in easily observable area. Consider position of bed. Daily monitoring of BP to exclude hypotension and postural hypotension Record lying / sitting and standing BP. Two readings taken: 1 after rest 5 minutes supine, 2, 1 minute later standing. Increased observation / assistance when rising from bed / armchair etc. Elevation of head of bed. Refer to medical practitioner to consider medication review.
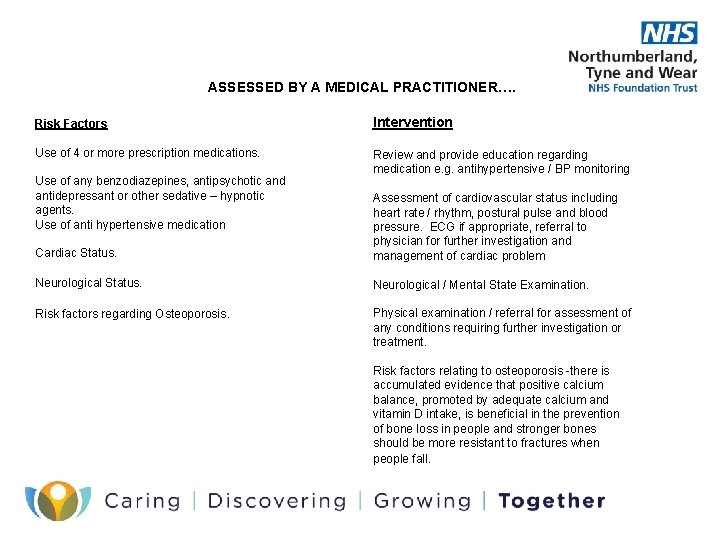
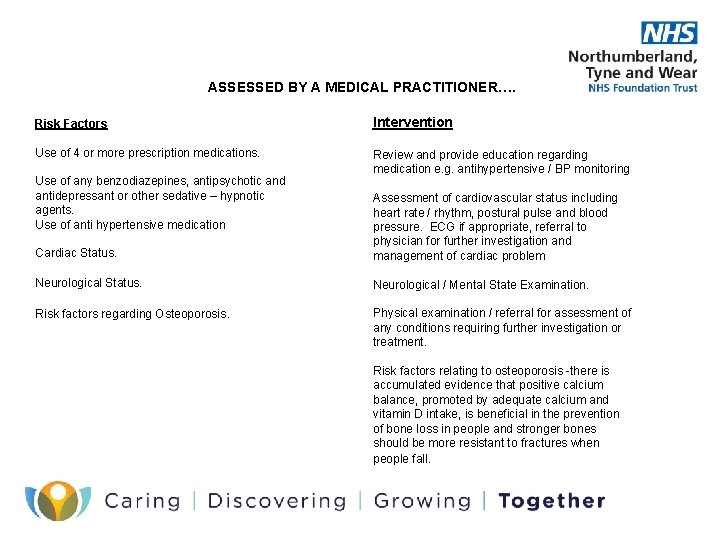
ASSESSED BY A MEDICAL PRACTITIONER…. Risk Factors Intervention Use of 4 or more prescription medications. Review and provide education regarding medication e. g. antihypertensive / BP monitoring Use of any benzodiazepines, antipsychotic and antidepressant or other sedative – hypnotic agents. Use of anti hypertensive medication Cardiac Status. Assessment of cardiovascular status including heart rate / rhythm, postural pulse and blood pressure. ECG if appropriate, referral to physician for further investigation and management of cardiac problem Neurological Status. Neurological / Mental State Examination. Risk factors regarding Osteoporosis. Physical examination / referral for assessment of any conditions requiring further investigation or treatment. Risk factors relating to osteoporosis -there is accumulated evidence that positive calcium balance, promoted by adequate calcium and vitamin D intake, is beneficial in the prevention of bone loss in people and stronger bones should be more resistant to fractures when people fall.
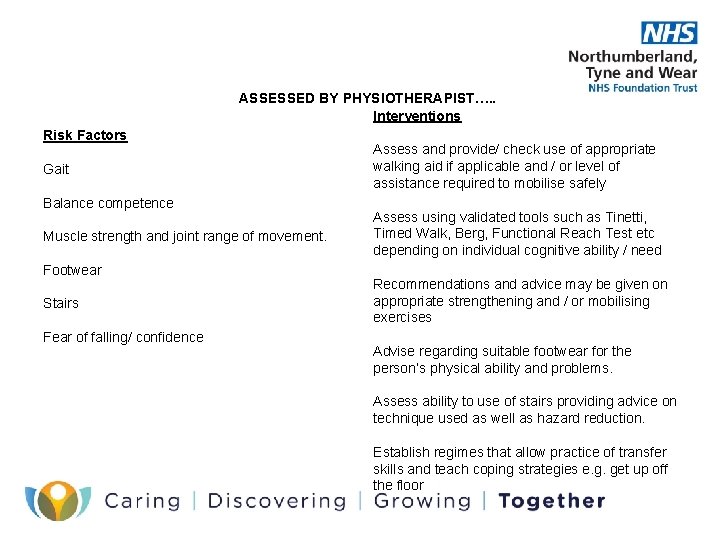
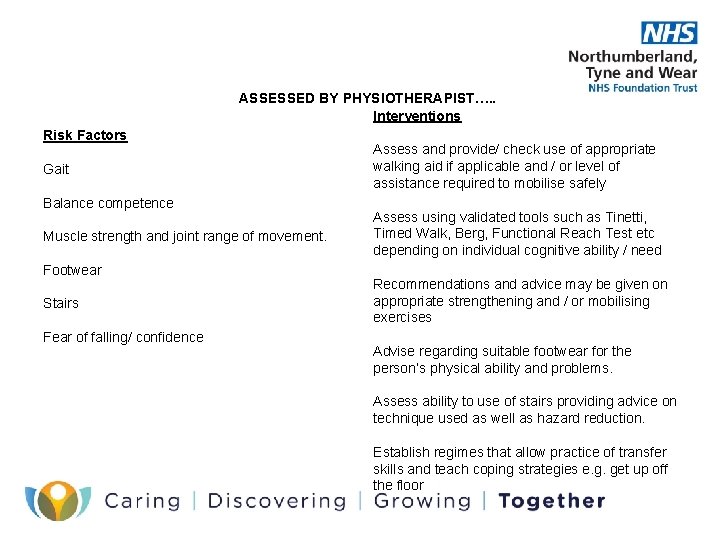
ASSESSED BY PHYSIOTHERAPIST…. . Interventions Risk Factors Gait Balance competence Muscle strength and joint range of movement. Footwear Stairs Fear of falling/ confidence Assess and provide/ check use of appropriate walking aid if applicable and / or level of assistance required to mobilise safely Assess using validated tools such as Tinetti, Timed Walk, Berg, Functional Reach Test etc depending on individual cognitive ability / need Recommendations and advice may be given on appropriate strengthening and / or mobilising exercises Advise regarding suitable footwear for the person’s physical ability and problems. Assess ability to use of stairs providing advice on technique used as well as hazard reduction. Establish regimes that allow practice of transfer skills and teach coping strategies e. g. get up off the floor
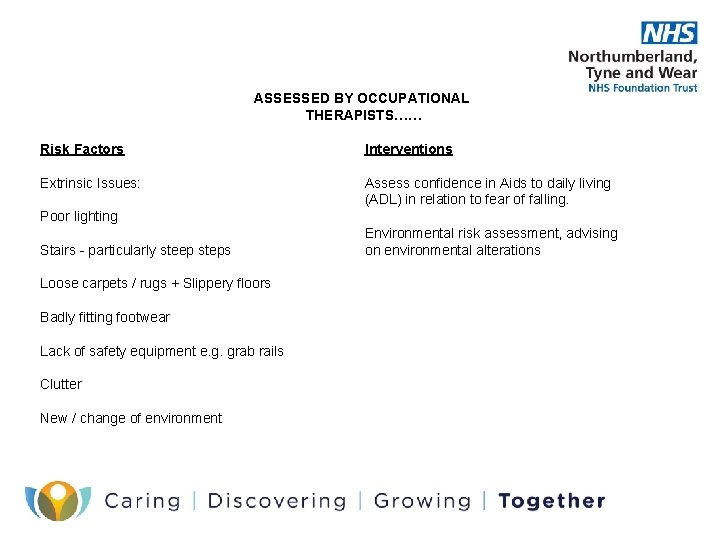
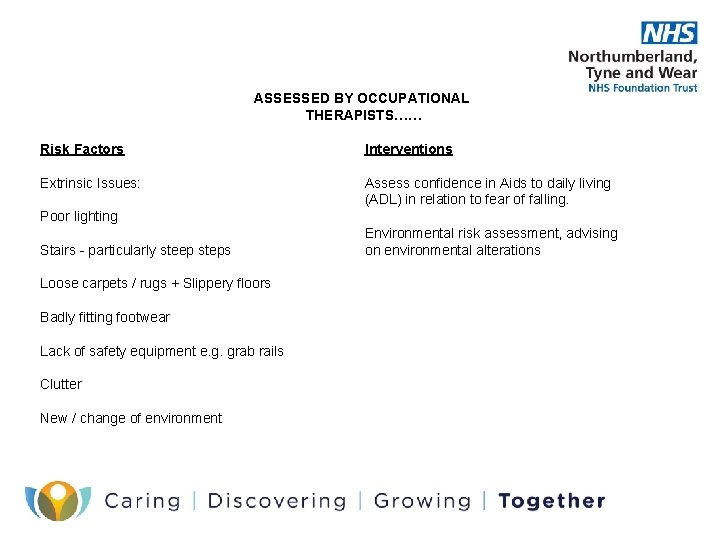
ASSESSED BY OCCUPATIONAL THERAPISTS…… Risk Factors Interventions Extrinsic Issues: Assess confidence in Aids to daily living (ADL) in relation to fear of falling. Poor lighting Stairs - particularly steep steps Loose carpets / rugs + Slippery floors Badly fitting footwear Lack of safety equipment e. g. grab rails Clutter New / change of environment Environmental risk assessment, advising on environmental alterations
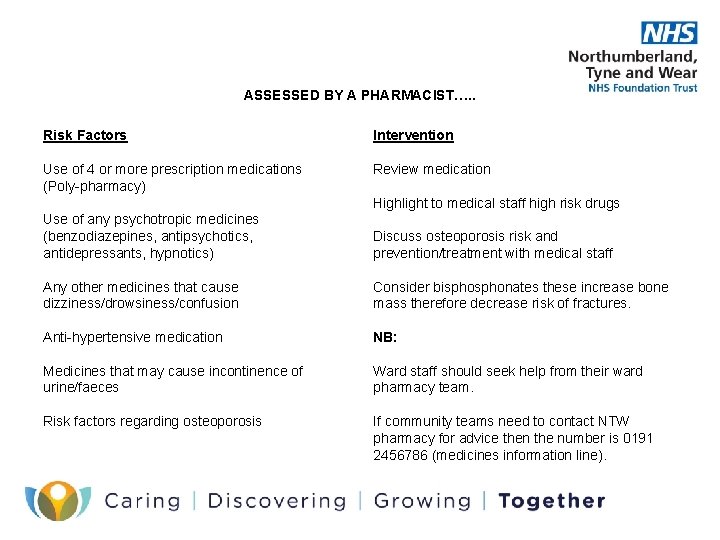
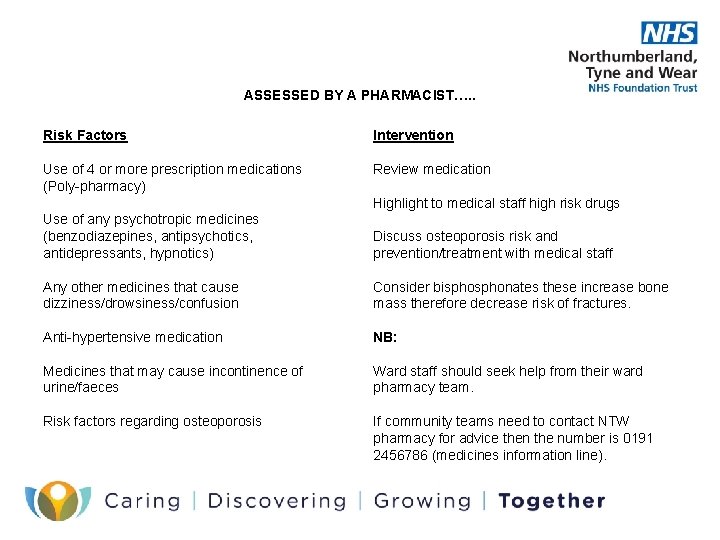
ASSESSED BY A PHARMACIST…. . Risk Factors Intervention Use of 4 or more prescription medications (Poly-pharmacy) Review medication Highlight to medical staff high risk drugs Use of any psychotropic medicines (benzodiazepines, antipsychotics, antidepressants, hypnotics) Discuss osteoporosis risk and prevention/treatment with medical staff Any other medicines that cause dizziness/drowsiness/confusion Consider bisphonates these increase bone mass therefore decrease risk of fractures. Anti-hypertensive medication NB: Medicines that may cause incontinence of urine/faeces Ward staff should seek help from their ward pharmacy team. Risk factors regarding osteoporosis If community teams need to contact NTW pharmacy for advice then the number is 0191 2456786 (medicines information line).
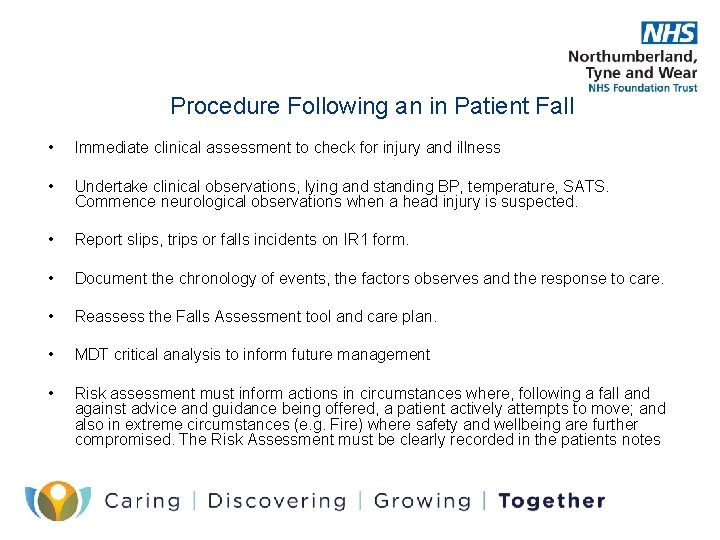
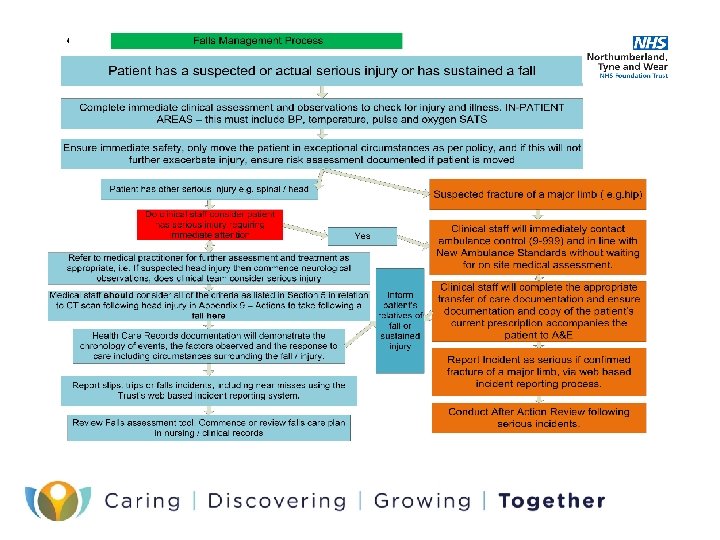
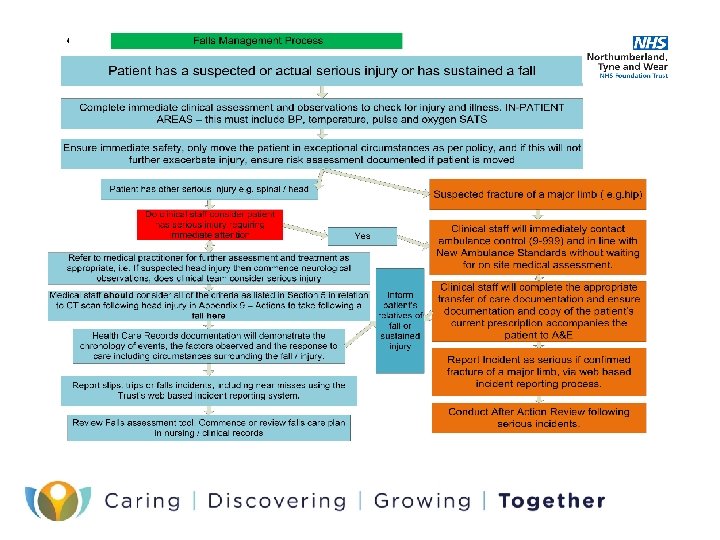
Procedure Following an in Patient Fall • Immediate clinical assessment to check for injury and illness • Undertake clinical observations, lying and standing BP, temperature, SATS. Commence neurological observations when a head injury is suspected. • Report slips, trips or falls incidents on IR 1 form. • Document the chronology of events, the factors observes and the response to care. • Reassess the Falls Assessment tool and care plan. • MDT critical analysis to inform future management • Risk assessment must inform actions in circumstances where, following a fall and against advice and guidance being offered, a patient actively attempts to move; and also in extreme circumstances (e. g. Fire) where safety and wellbeing are further compromised. The Risk Assessment must be clearly recorded in the patients notes
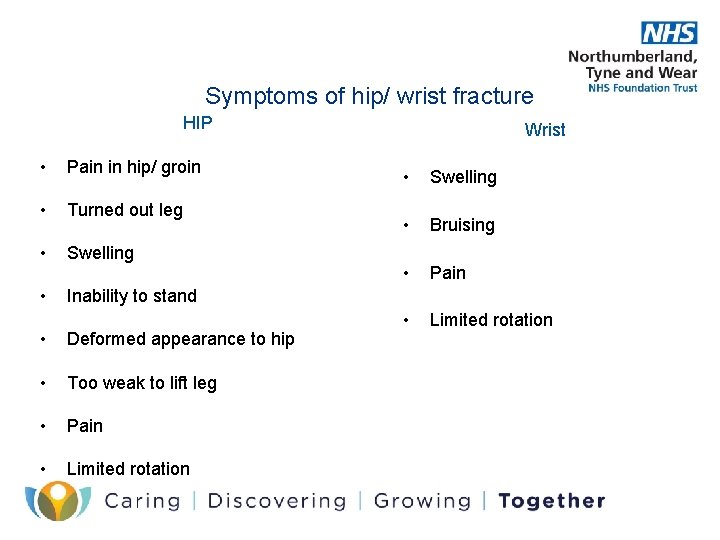
Symptoms of hip/ wrist fracture HIP • Pain in hip/ groin • Turned out leg • Swelling • Inability to stand • Deformed appearance to hip • Too weak to lift leg • Pain • Limited rotation Wrist • Swelling • Bruising • Pain • Limited rotation

Suspected fracture of a major limb e. g. Hip/ Wrist • Immediately contact ambulance control request an ambulance (9 -999) in line with New Ambulance Standards, without waiting for on site medical assessment. (Ward staff to remind ambulance control we are not an acute hospital care provider) • Complete appropriate transfer of care documentation and copy of patients current prescription. • Inform patient safety dept quoting the web based incident number and indicate SUI. After Action Review for falls resulting in a fracture of neck of femur will be carried out as Serious and Untoward incident)

Equipment available for falls prevention Hip protectors: Most hip fractures (60 -90%) are related to a trauma to the hip and they can have an important role in the prevention of fractures when used in conjunction with multi factorial assessment and interventions. Some individuals may not be suitable to wear hip protectors. Those with high risk or with existing pressure ulcers should not wear protectors. NICE concluded that at present there is insufficient evidence that hip protectors are effective in preventing fractures but they have identified some benefits to those people in extended care settings including hospitals. For people with a very high fracture risk a device which reduces the impact force of a fall on the vulnerable hip joint must be beneficial Beds. Low profile beds are available to hire with appropriate crash mat via Medical. Device. ADM@ntw. nhs. uk or Infection prevention control. Can be arranged by on call IPC nurse out of hours Bed rails: PGN available re the assessment and use of bed rails
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention National and local guidance on falls prevention
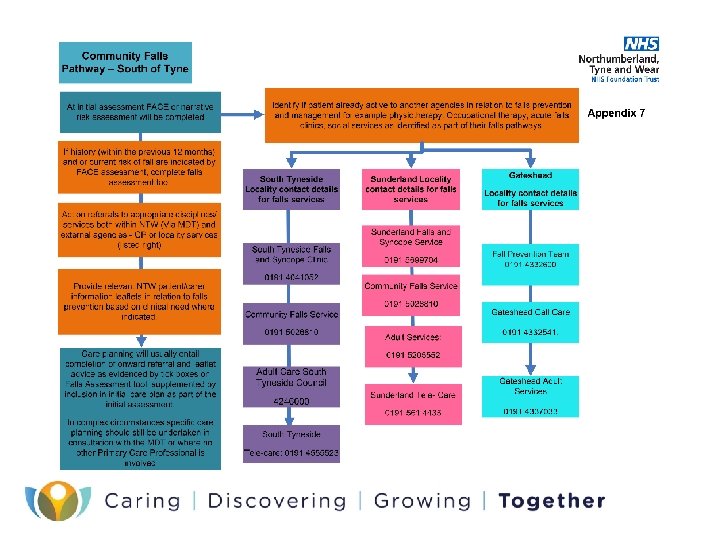
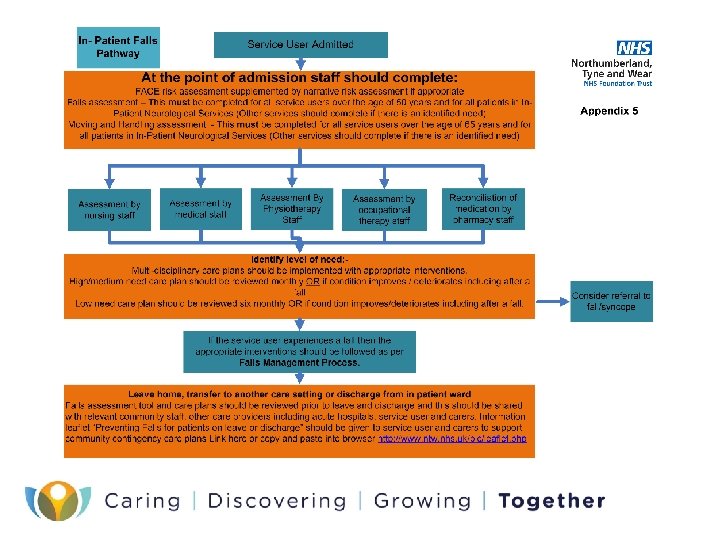
National and local guidance on falls prevention Falls pathway
Falls pathway 18 week patient pathway
18 week patient pathway Pico question for falls and hourly rounding
Pico question for falls and hourly rounding Patient 2 patient
Patient 2 patient Community action cycle
Community action cycle Gluconeogenesis of amino acids
Gluconeogenesis of amino acids Spill prevention control and countermeasure plan template
Spill prevention control and countermeasure plan template Prevention and combating of corrupt activities act summary
Prevention and combating of corrupt activities act summary Colorado jprs
Colorado jprs Injuries first aid
Injuries first aid Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Accident prevention signs and tags
Accident prevention signs and tags Accident prevention sign and symbols
Accident prevention sign and symbols Industrial safety signs and symbols ppt
Industrial safety signs and symbols ppt Osha needlestick protocol
Osha needlestick protocol Leavel dan clark
Leavel dan clark European centre for disease prevention and control
European centre for disease prevention and control Deadlock prevention avoidance and detection
Deadlock prevention avoidance and detection Health promotion and levels of disease prevention
Health promotion and levels of disease prevention Policy on harassment prevention and resolution
Policy on harassment prevention and resolution Deadlock detection prevention and avoidance
Deadlock detection prevention and avoidance Osha subpart f
Osha subpart f Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention