FACT VERSUS FICTION CURRENT OPINION ON THE EARLY
- Slides: 56
FACT VERSUS FICTION. . . CURRENT OPINION ON THE EARLY DIAGNOSIS OF CEREBRAL PALSY Robyn Smith Department of Physiotherapy UFS 2012
Defining Cerebral Palsy (CP) �Always been challenge to define �Older definitions only focussed on the motor component �Not comprehensive and inclusive enough
DEFINING CEREBRAL PALSY (CP) Cerebral Palsy (CP) Cerebral Motor Disturbance (CMD)
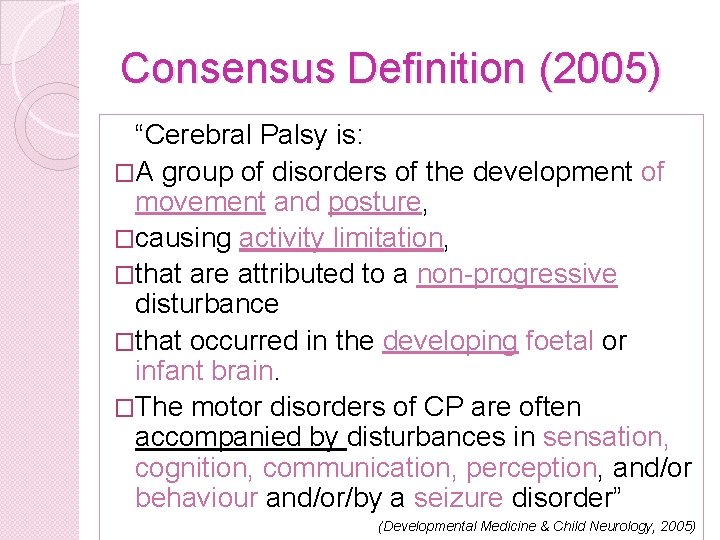
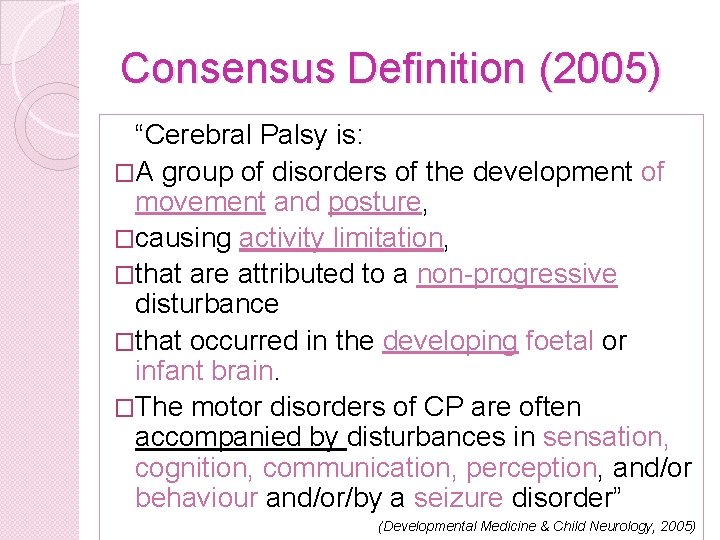
Consensus Definition (2005) “Cerebral Palsy is: �A group of disorders of the development of movement and posture, �causing activity limitation, �that are attributed to a non-progressive disturbance �that occurred in the developing foetal or infant brain. �The motor disorders of CP are often accompanied by disturbances in sensation, cognition, communication, perception, and/or behaviour and/or/by a seizure disorder” (Developmental Medicine & Child Neurology, 2005)
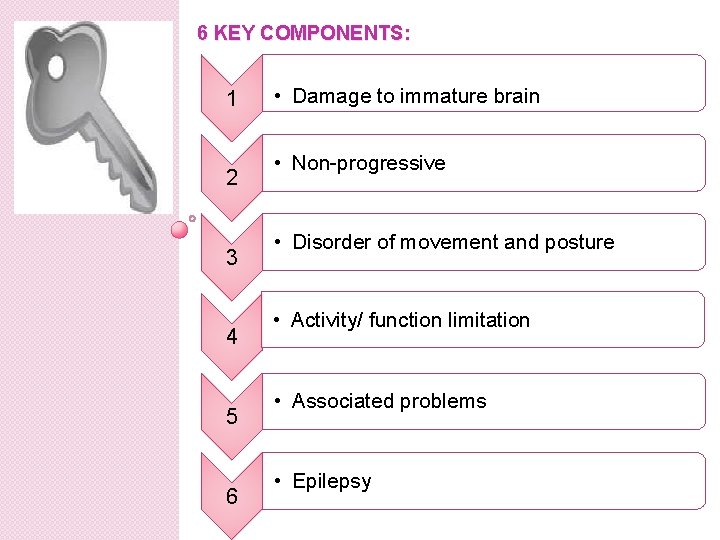
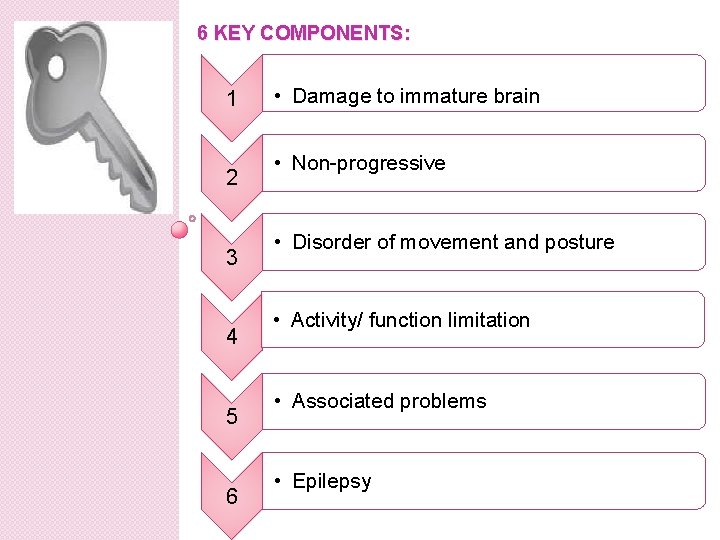
6 KEY COMPONENTS: 1 2 3 4 5 6 • Damage to immature brain • Non-progressive • Disorder of movement and posture • Activity/ function limitation • Associated problems • Epilepsy
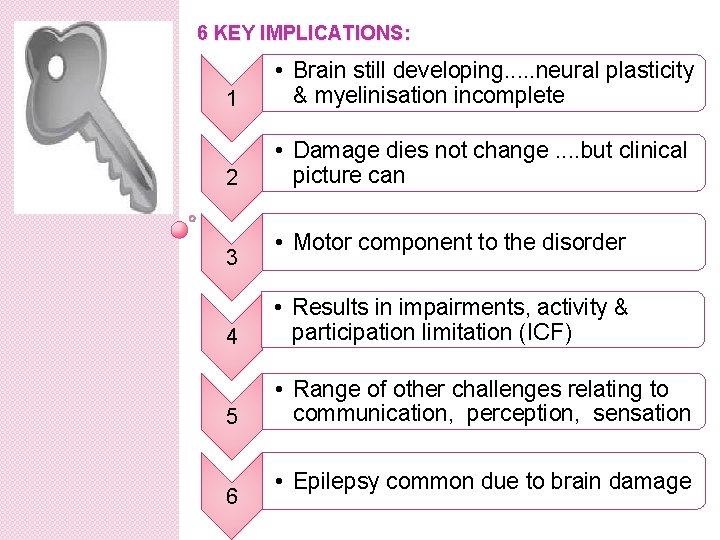
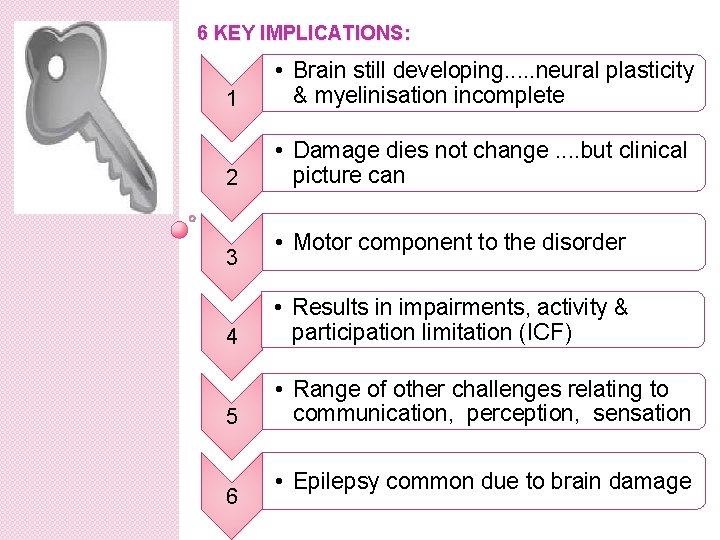
6 KEY IMPLICATIONS: 1 • Brain still developing. . . neural plasticity & myelinisation incomplete 2 • Damage dies not change. . but clinical picture can 3 • Motor component to the disorder 4 • Results in impairments, activity & participation limitation (ICF) 5 • Range of other challenges relating to communication, perception, sensation 6 • Epilepsy common due to brain damage
Incidence of CP � Statistical data varies from country to country � Incidence: 2 -4/1000 live births (Styer-Acevado , 2008) � Contravening expectations, the incidence has remained unchanged even in 1 st world countries � Newest study in US showing an increased incidence in cerebral palsy amongst premature infants (Science Daily, February: 2010) � Medical advances in neonatal intensive care has resulted in a decrease in neonatal mortality, and smaller infants are surviving longer
Incidence of CP �UNFORTUNATELY , this is creating a whole new population of children at risk of marked central nervous system dysfunction
So when does the brain insult occur causing CP? � 85% congenital in nature “Perinatal causes” in-utero, during or shortly after birth process � 15% postnatal due to e. g. TBI, anoxia, near drowning, meningitis
PERINATAL RISK FACTORS FOR CP
Prenatal risk factors �Anoxia – due conditions placenta or umbilicus �Rh and ABO incompatibility – severe anaemia in newborn �Maternal infections �Metabolic disorders e. g. DM, hyperthyroidism �Genetic factors
Prenatal risk factors �Substance addiction of mother e. g. alcohol, cocaine, nicotene �Toxin ingestion �Certain medications �Multiple births e. g. twins and triplets �PET in mother �Cerebral hemorrhaging in foetus due sepsis, middle cerebral artery infarct in foetus
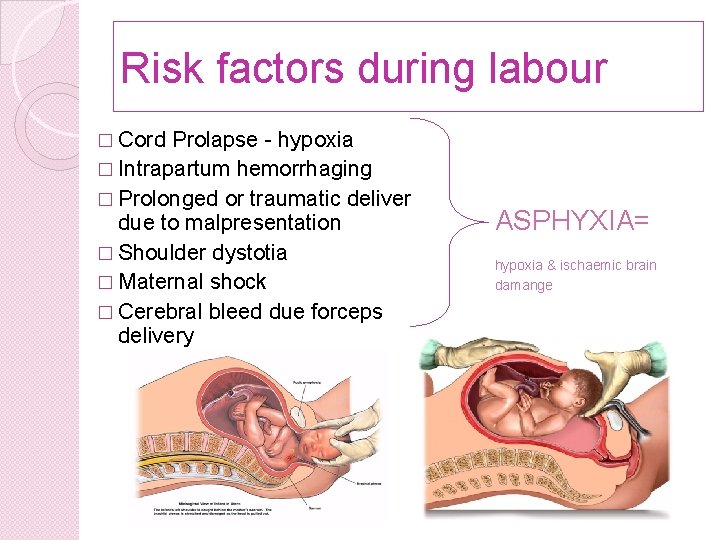
Risk factors during labour � Cord Prolapse - hypoxia � Intrapartum hemorrhaging � Prolonged or traumatic deliver due to malpresentation � Shoulder dystotia � Maternal shock � Cerebral bleed due forceps delivery ASPHYXIA= hypoxia & ischaemic brain damange
Risk factors at birth �Prematurity (30 -43% become CP’s) �ELBW/ VLBW (40% and 18% chance severe disability respectively) �IUGR
Risks during neonatal period � Seizures � Sepsis � HIE � Uncontrolled hypoglycaemia � Untreated severe jaundice (kernicterus) � Neonatal stroke
THE CHALLENGE OF DIAGNOSING CEREBRAL PALSY
Is there is something wrong with my child? � Clinicians often feel like they are treading on eggshells!!!! � Parents want definitive answers that are often not easy to provide � CP notoriously difficult to formally diagnose within the first 12 months of life � Unless child is severely affected � Often difficult to address parents fears and concerns in a satisfactory manner
Why is it so difficult to provide clear cut answers to parents of infants at risk ? ? ?
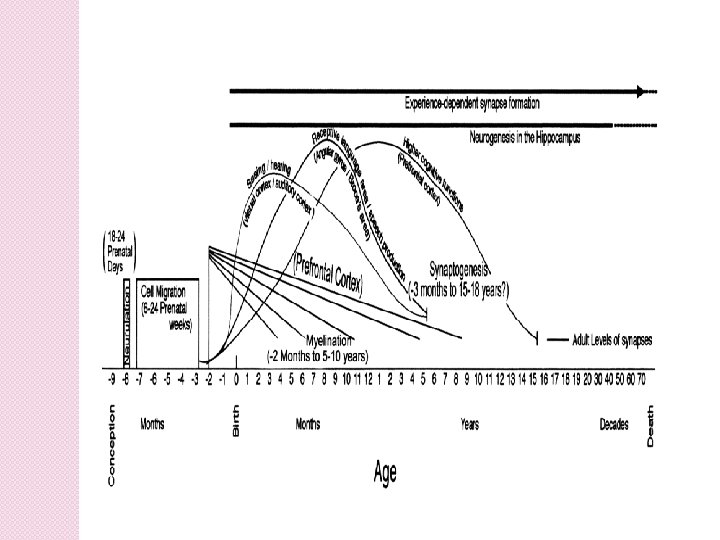
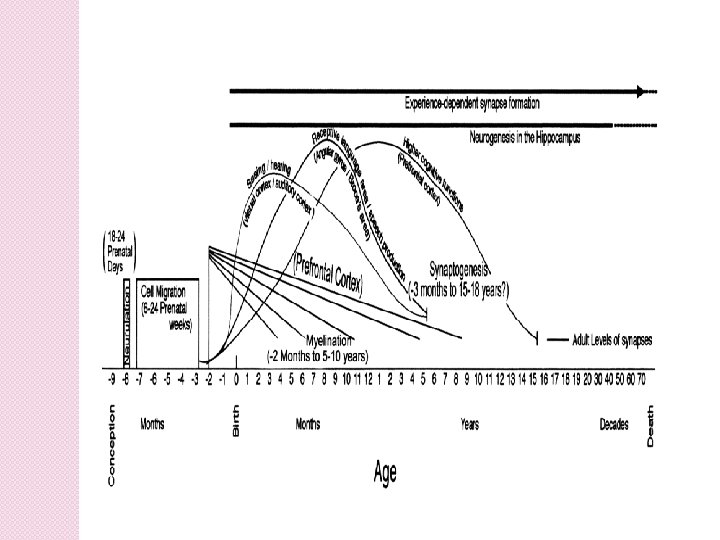
Immature Brain : A continuously changing system The human brain is a extremely complex and dynamic, constantly changing system � A substantial part of the brain’s development occurs in utero. This includes neuronal proliferation, migration and differentiation � Differentiation and neuronal pruning are prolific in the first months of life after birth The first eighteen months of the normal child’s life is the most significant period of significant and rapid development
Immature Brain : A continuously changing system � Myelinisation is most significant during the 1 st year of life, but is only completed around the age of 30 years of age � Shaping of the nervous system by extrinsic and intrinsic factors e. g. stimulation, exposure, opportunity to practice, internal motivation and personality plays an important role � Brain is in a constant process of remodelling and evolution during childhood Even though neurons themselves do not regenerate, neural plasticity during childhood may have a marked impact on clinical outcome of children with cerebral damage
Concept of neural plasticity � Adaptability and plasticity of the infantile brain � Neuronal circuitry of brain reorganises itself, new synapses form to compensate for areas of damage. � Practice and repetition important here. � Plasticity and opportunity for change is greatest in young children Thus the value of early intervention programmes
HOW DOES ONE THEN OBJECTIVELY GO ABOUT MAKING A DIAGNOSIS OF CEREBRAL PALSY IN AN INFANT ? ? ? ?
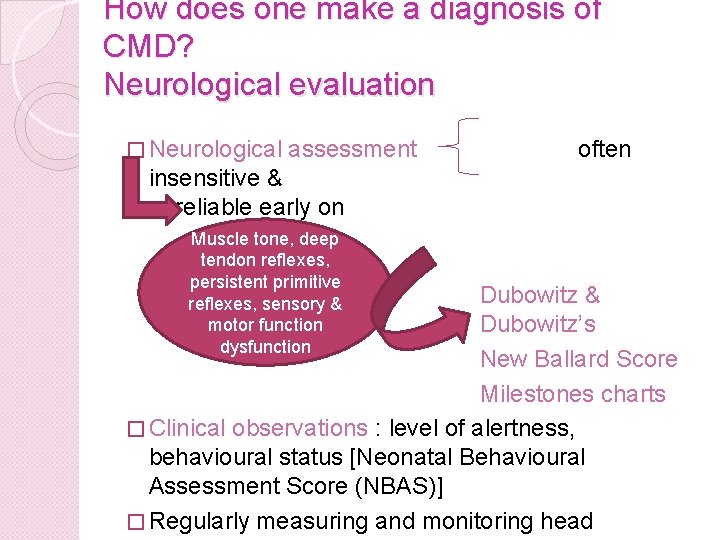
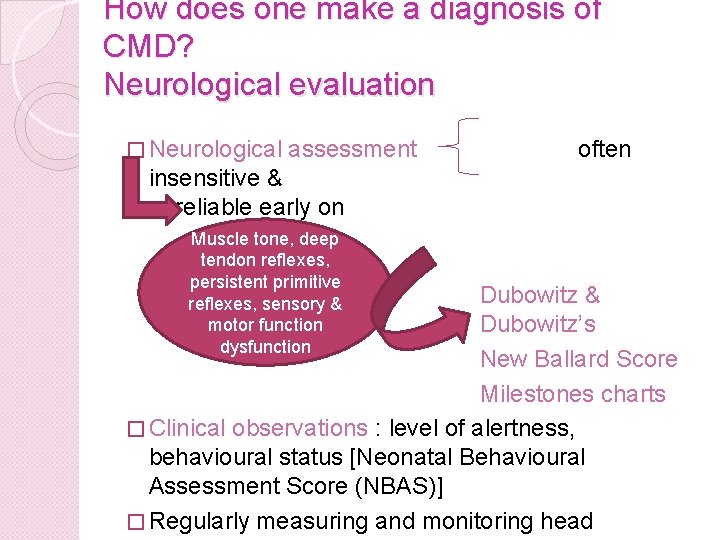
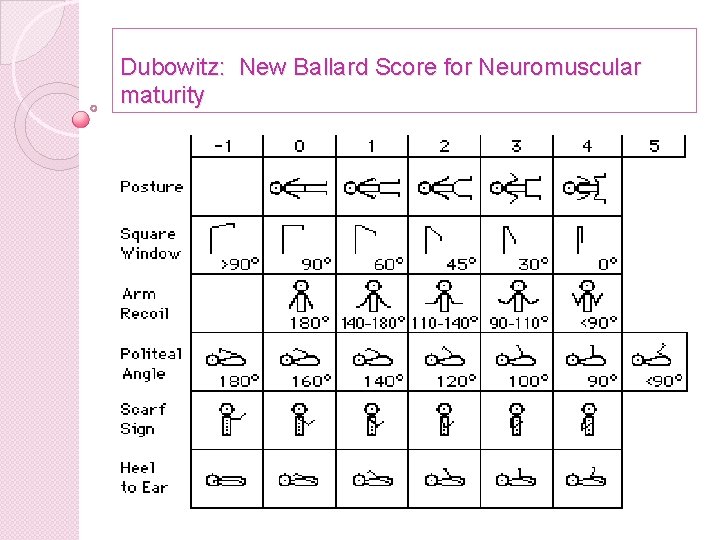
How does one make a diagnosis of CMD? Neurological evaluation � Neurological assessment often insensitive & unreliable early on Muscle tone, deep tendon reflexes, persistent primitive reflexes, sensory & motor function dysfunction Dubowitz & Dubowitz’s New Ballard Score Milestones charts � Clinical observations : level of alertness, behavioural status [Neonatal Behavioural Assessment Score (NBAS)] � Regularly measuring and monitoring head
Challenges of neurological assessment in infants. . . � � � � Accurate execution of neurological testing often complicated Predicting outcome in young infants based on a neurological assessment is often very difficult Primitive reflexes not always integrated yet Children with transient signs often incorrectly diagnosed Tonal changes & presentation of asymmetry often only visible from approximately 6/12 Children who initially appear asymptomatic and clinical signs only appear later Developmental delay and “late bloomers” ? Where do they fall LOT OF FALSE POSITVE RESULTS SOME FALSE NEGATIVE RESULTS Misdiagnosis or incorrect diagnosis have huge implications on a family!!!!
Neurological evaluation �Clinical neurological evaluation still widely used as a tool in the diagnosis of neurological dysfunction and cannot be discarded �Performing a comprehensive neurological evaluation in a premature infant often not possible due to their fragile state and health challenges. �The predictive value of results from neurological assessment is far poorer in premature vs. term and older infants.
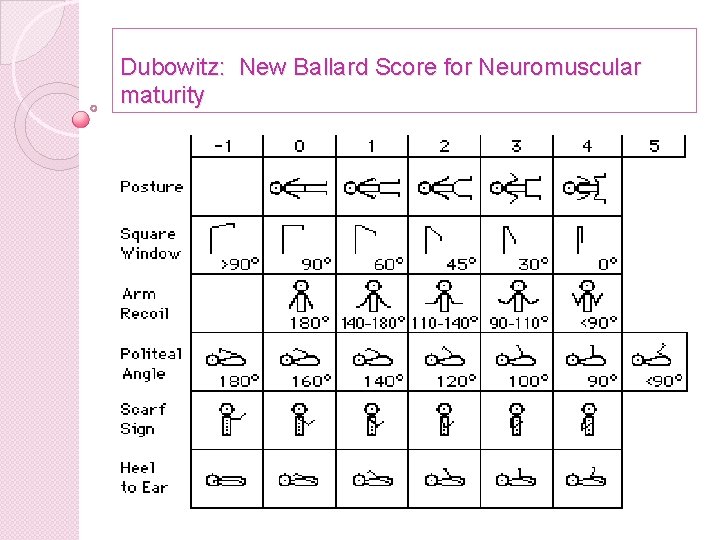
Dubowitz: New Ballard Score for Neuromuscular maturity
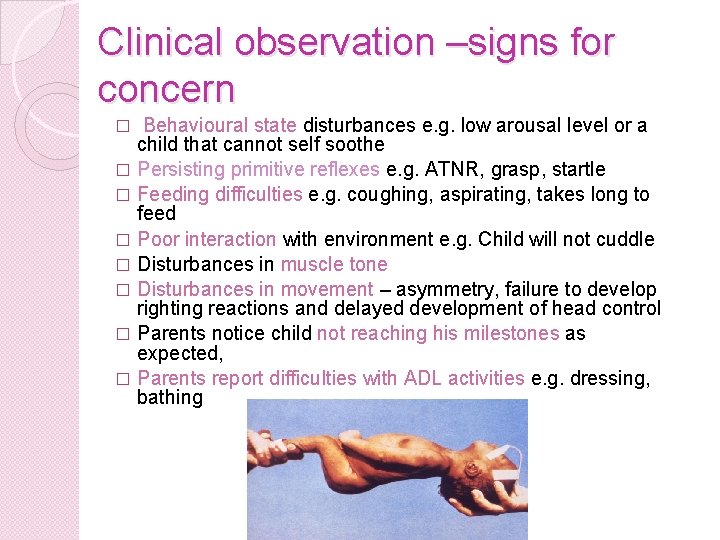
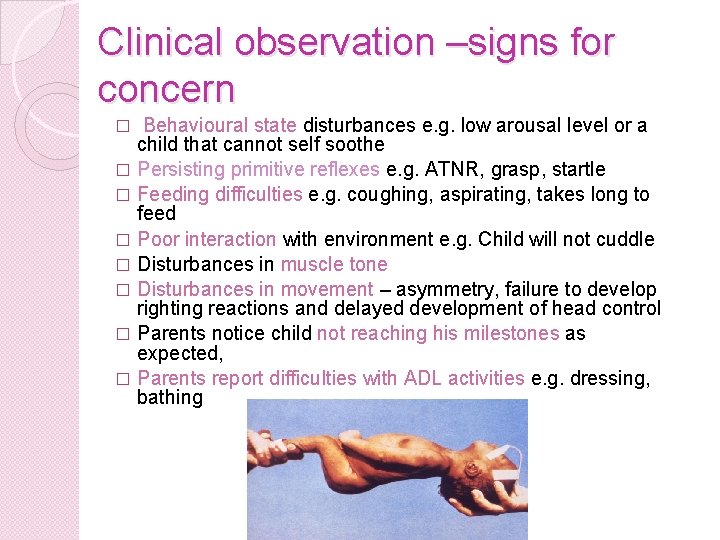
Clinical observation –signs for concern Behavioural state disturbances e. g. low arousal level or a child that cannot self soothe � Persisting primitive reflexes e. g. ATNR, grasp, startle � Feeding difficulties e. g. coughing, aspirating, takes long to feed � Poor interaction with environment e. g. Child will not cuddle � Disturbances in muscle tone � Disturbances in movement – asymmetry, failure to develop righting reactions and delayed development of head control � Parents notice child not reaching his milestones as expected, � Parents report difficulties with ADL activities e. g. dressing, bathing �
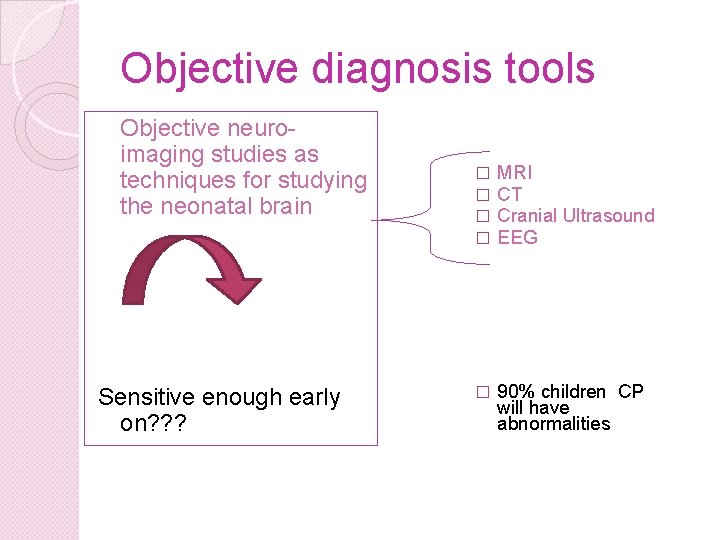
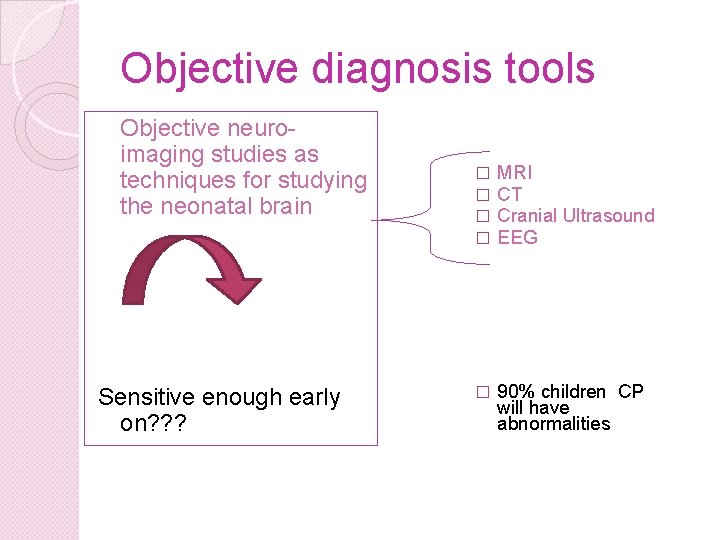
Objective diagnosis tools Objective neuroimaging studies as techniques for studying the neonatal brain � � MRI CT Cranial Ultrasound EEG � 90% children CP will have abnormalities Sensitive enough early on? ? ?
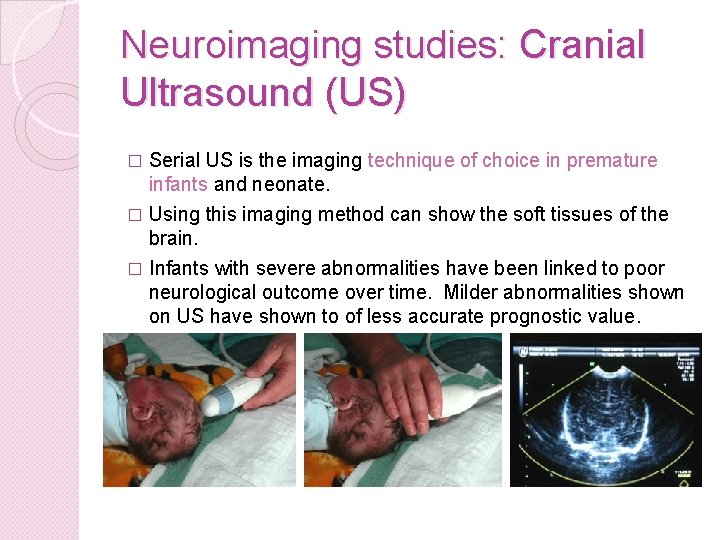
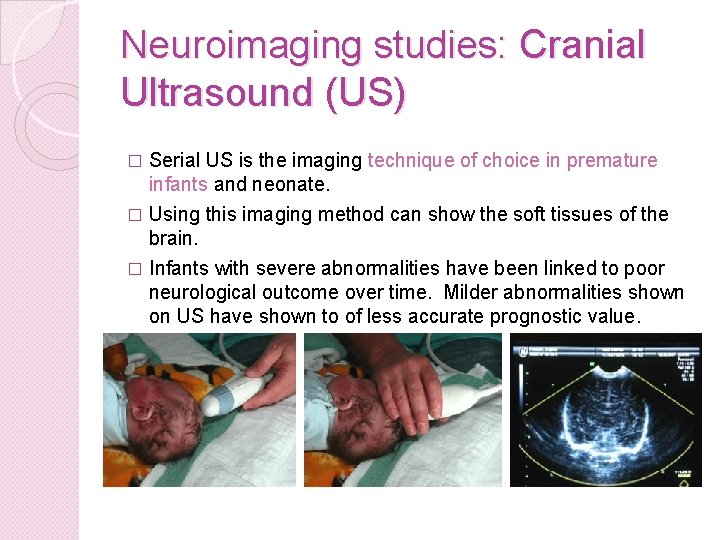
Neuroimaging studies: Cranial Ultrasound (US) Serial US is the imaging technique of choice in premature infants and neonate. � Using this imaging method can show the soft tissues of the brain. � Infants with severe abnormalities have been linked to poor neurological outcome over time. Milder abnormalities shown on US have shown to of less accurate prognostic value. �
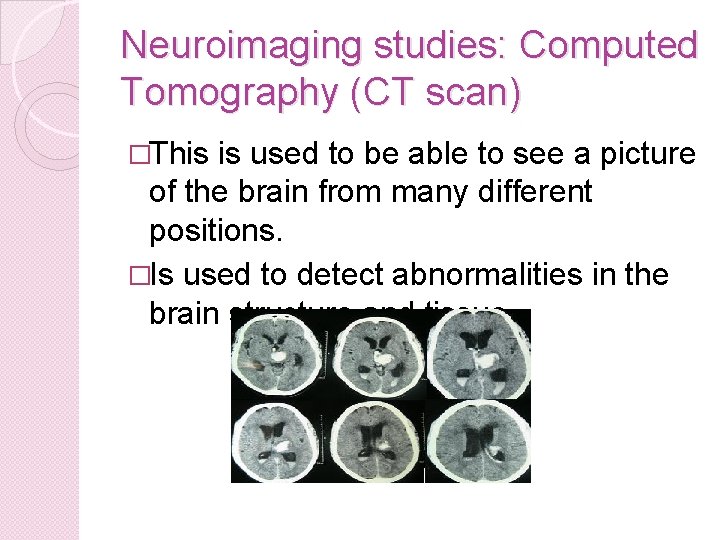
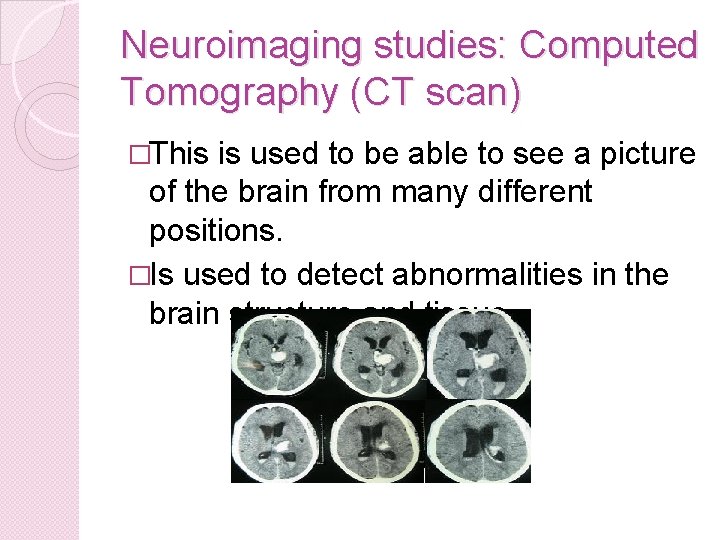
Neuroimaging studies: Computed Tomography (CT scan) �This is used to be able to see a picture of the brain from many different positions. �Is used to detect abnormalities in the brain structure and tissue.
Neuroimaging studies: Magnetic Resonance Imaging (MRI) � The use of magnets and radio waves to allow a more detail image of the brain. � In children with neurological dysfunction one will look out for areas of brain atrophy indicating under development of the brain
Neuroimaging studies: Electroencephalogram (EEG) � Is used to measure electrical activity in the brain and is performed on babies that have had seizures
total dependence of neuroimaging to diagnose early brain dysfunction in ill and premature infants
Other clinical investigations If neuroimaging studies do not show any atypical findings the following may be considered : � Metabolic studies metabolic causes are however rare (0 -4% of all cases). � Genetic studies � Muscle biopsy to rule out conditions e. g. muscular dystrophy, SMA surgical procedure where an incision approximately 3 inches long is made, and a small section of muscle is removed. Usually they remove the muscle from the upper thigh. The biopsy is used to check for degeneration of muscle tissue. � Neurophysiological tests electroencephalogram and somatosensory evoked potentials
Prechtl’s method of qualitative assessment of spontaneous movements of the infant ? ? The way forward in the early diagnosis of CP
Prechtl’s method of neuromotor assessment � Heinz Prechtl pioneer in field of early neurological development � Realised that self generated motility early in development played an important role in survival and adaptation � These spontaneous general movements (GM) are present from the foetal period until approximately 58 weeks post- conception (4 months). � Prechtl discovered that the quality of these spontaneous general movements accurately reflected the condition of the nervous system in the foetus and young infant � Change in the type of GM strongly related to gestational age � Also affected by endogenous maturation process of the CNS important � To some limited degree, postnatal experience � This method is used in the early detection of brain
How are the images generated? Serial video imaging of infant over time using a portable video � camera set up on a tripod (direct overhead or lateral view of the infant) � GM are also affected by the behavioural state of the child – best state to view GM is the active, awake state or sleeping state in the prem. � If there is too much crying or fussing the video session should be postponed � Infant positioned in supine with the head end of the crib elevated at 30 o � The child is to be clothed in a diaper or short clothing and the crib must be free of restricting devices that may negatively impact on the infants freedom of movement � Duration of the video recording between 10 -20 minutes � Done weekly up until 58 weeks post-conception age (4 months)
How is the video material then Interpreted? �Interpretation of the images is based on the “gestalt perception” of the observer. �Based on pattern recognition when viewing static or moving images of GM �Intuitively guided �Inter-observer reliability is extremely high, from studies done it is reported to be between 89 -93%
Normal optimal General Movements (GM) � Neuronal network generates signals to the muscles in the absence of sensory input – central pattern generator(CPG) � Series of gross motor movements of variable amplitude, force, intensity and speed � These complex movements involve all body parts including the limbs, trunk and head � Lasts few seconds to a few minutes � Observed during the awake and sleep states of the infant � GM are of the first movements the foetus develops � GM show age specific characteristics
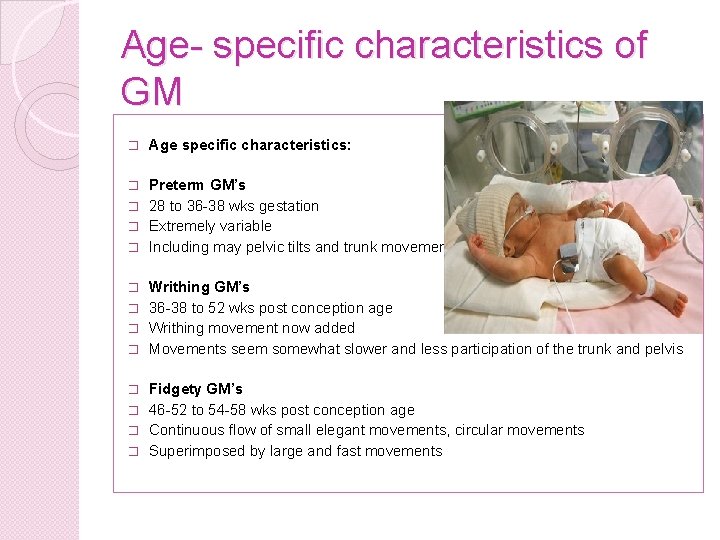
Age- specific characteristics of GM � Age specific characteristics: Preterm GM’s � 28 to 36 -38 wks gestation � Extremely variable � Including may pelvic tilts and trunk movements � Writhing GM’s � 36 -38 to 52 wks post conception age � Writhing movement now added � Movements seem somewhat slower and less participation of the trunk and pelvis � Fidgety GM’s � 46 -52 to 54 -58 wks post conception age � Continuous flow of small elegant movements, circular movements � Superimposed by large and fast movements �
Normal optimal General movements (GM) �Complexity and variation of the movements are key �Constant variation of flexion/extension, abduction/adduction and IR/ER limbs �Fluent �Gradual beginning & end �Over time the infant continuously produces new movement patterns � 10 - 20% infants
Sub-optimal general Movements (GM) �Sufficient variability �Not fluent �Most infants
Abnormal General Movements (GM) �Loss of the complexity, variability and fluency of GM happens when the CNS is impaired �Stereotypical movements hallmark of early brain dysfunction �The transition periods between the various types of GM are important markers
Abnormal General Movements (GM) Then described as being: �Poor repertoire –sterotyped, monotonous movements �Cramped synchronous GM- movements appear rigid, lack smooth and fluent character. Limb and trunk muscles contract simultaneously. Strongly associated with later hypertonicity and dyskinetic types of CP �Chaotic movements –appear abrupt, large amplitude
Clinical significance of abnormal GM � PVL, IVH, HIE, IUGR and hyperbilirubinaemia can give rise to abnormal GM’s � Quality of GM’s can be influenced by severe illness and sedation, but these abnormalities may be transient (why series of images over time is important) � GM considered mildly abnormal if periods of atypical movements interspersed with normal GM – long term predictive value less accurately predicted � Neurological evaluation often insensitive in fragile premature infants. GM are of far higher predicative value in these infants. � Better correlation between the neurological evaluation and the assessment of GM improves with increasing age
Clinical significance of abnormal GM � Predictive value highest at the stage of transition to fidgety movements (46 -58 wks postconception) � Infant who do not develop fidgety or show abnormal fidgety movement at an extremely high risk of developing CP � Specificity and sensitivity estimated to be 95% � Infants who develop abnormal GM, who do not develop CMD develop some other developmental disorder. � No studies to date have been done where infants with mildly abnormal GM have been followed up until school going age where perceptual & learning and scholastic difficulties often first present � Mildly abnormal GM associated with ADHD and
Normal evolution of GM �At 15/52 GM start to decline �Infant starts to develop other patterns of spontaneous movement �Development then of postural control �Followed by typical sensory-motor development �Then observer focus more on the observation of volitional active movement ? ? ? Employ similar observational methods here
Conclusion. . . �Highly specific and valid objective measure for indentifying early neurological dysfunction �Persistently abnormal GM especially relating to repertoire and cramped synchronous movements show a high predictive value of poor neurological outcome over time
Advantages of the qualitative method of assessment of spontaneous movements � � � � Non-invasive Low cost Easy to learn to execute Non time-consuming Ideal for serial observation/assessment over time. The value of developmental profiles over time is extremely valuable in predicting long term outcome in preterm, term and post-term infants. More reliable than neurological examination and neuroimaging techniques early on and especially in premature infants Enables early rehabilitation and intervention and family support allowing the child to reach his full potential Suggested to be of the greatest clinical value when used in combination with neurological assessment and neuroimaging techniques in predicting early neurological dysfunction
Limitations of this assessment method. . . . � Cannot be used in infants who have severely depressed neurological status e. g. children with acute severe HIE (often comatose) or children on CNS suppressing medication (sedation) � Cannot completely replace a comprehensive neurological system including assessment of auditory, visual and sensory sub-systems � Method cannot be used in infants that are mechanically ventilated due to restrictive apparatus � Video series may need to be interrupted id the child’s condition deteriorates � Training expensive � Local expertise in the execution of the technique limited, which makes skill transfer in the profession a challenge
So how is this relevant to us as physiotherapists? As PT’s working in NICU and in early intervention care with this at risk population we needs to be multi-skilled as these infants more often than not have multi-system involved. Unfortunately cannot just focus’ on basic neurodevelopmental care programmes, chest PT or even the odd baby massage. If working in a NICU one has to be knowledgeable regarding neurodevelopment as we have a critical role to play in initial neurodevelopmental screening , assessment and implementation of early neurodevelopmental therapy intervention programmes to ensure the best possible functional outcome for these children and their families
NEED TO BE COME MORE AWARE OF ADVANCES IN OUTR FILEDS, AND BECOME MORE OPEN TO TRYING DIFFERENT EVIDENCE BASED ASSESSMENT AND INTERVENTION APPROACHES IN THE MANAGEMENT OF OUR PATIENTS
Training ? ? ? �Physicians and physiotherapists working in the NICU and field of infant neurology �Europe �R 10 000 for a 4 day course �Credentialing needed to execute the technique in an official capacity
References � � � � Dubowitz gestational age assessment. 2010. retrieved on 01 March 2010 Available online at : http: //neopraxis. org/Dubowitz_gestational_age_assessment. htm Hadders-Alga, M. 2004. General movements: a window for early identification of children at high risk for developmental disorders journal of Paediatrics August 2004: S 12 -S 18 Bax, M. Goldstein, M, Rosenbaum, P, Leviton, A & Paneth, N. 2005. Proposed definition of Cerebral palsy 2005. Developmental Medicine & Child Neurology 2005, 47: 571 -576 Garcia, J. M. , Gherpelli, J. L. D. 7 Leone, C. R. 2004. The role of spontaneous general movements in the neurological outcome of cerbral lesions in preterm infants. Journal de Pediatrica 80(4): 296 -304 Cioni, G. , Pretchlib, H, Paoliclli F. P. B. , Einspielerb, C. , Federica, M. & Roversi, C. 1997. Which better predicts later outcome in fullterm infant: quality of general movements or neurological examination. Early human development 50; 1: 71 -75 Nel, M. 2009. Prechtl’s qualitative method of assessment of spontaneous movements. NDT early intervention course (unpublished) Smith, R. 2010. Aetiology and Classification of CP. Lecture presentation UFS (unpublished) � Styer-Acevado, J. 2008. The infant and child with cerebral palsy in Pediatric Physical Therapy. Lippincott, Williams & Wilkins. Baltimore. Pp 179 -186
 Example of facts
Example of facts Evolution fact fiction or opinion
Evolution fact fiction or opinion Element of fiction and non fiction
Element of fiction and non fiction Contemporary realism literature
Contemporary realism literature Fiction
Fiction It is genre of speculative fiction dealing with imaginative
It is genre of speculative fiction dealing with imaginative Jeopardy fact and opinion
Jeopardy fact and opinion Choose about fact x opinion, in this same order:
Choose about fact x opinion, in this same order: Example of fact
Example of fact Read the sentences and decide if they are
Read the sentences and decide if they are A bowling ball has three holes in it fact or opinion
A bowling ball has three holes in it fact or opinion Family fact and opinion
Family fact and opinion Fact or opinion activity
Fact or opinion activity Are there fewer panda bears than grizzly bears
Are there fewer panda bears than grizzly bears Fact or opinion
Fact or opinion Below under difference
Below under difference Facts about school
Facts about school Fact and opinion about pizza
Fact and opinion about pizza Fact or opinion
Fact or opinion Can you make them behave king george fact and opinion
Can you make them behave king george fact and opinion Fact or opinion
Fact or opinion Fact and opinion jeopardy 4th grade
Fact and opinion jeopardy 4th grade A fact statement
A fact statement News fact and opinion newspaper articles
News fact and opinion newspaper articles Fact or opinion
Fact or opinion Argument vs opinion
Argument vs opinion Fact or opinion
Fact or opinion Thanksgiving fact or opinion
Thanksgiving fact or opinion Oranges contain both calcium and vitamin c. fact or opinion
Oranges contain both calcium and vitamin c. fact or opinion Private opinion becomes public opinion when
Private opinion becomes public opinion when Diffusion current density
Diffusion current density Energy band diagram of pnp transistor
Energy band diagram of pnp transistor The jfet always operates with
The jfet always operates with The shielded metal arc welding machines voltage output
The shielded metal arc welding machines voltage output Line current and phase current
Line current and phase current Balanced delta-delta connection
Balanced delta-delta connection Y connected generator
Y connected generator Touch current vs leakage current
Touch current vs leakage current Drift current and diffusion current
Drift current and diffusion current Infineon
Infineon Line vs phase voltage
Line vs phase voltage Mesh current method with current source
Mesh current method with current source Drift current and diffusion current in semiconductor
Drift current and diffusion current in semiconductor Early cpr and early defibrillation can: *
Early cpr and early defibrillation can: * Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Cái miệng xinh xinh thế chỉ nói điều hay thôi
Cái miệng xinh xinh thế chỉ nói điều hay thôi Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là V cc cc
V cc cc 101012 bằng
101012 bằng Thể thơ truyền thống
Thể thơ truyền thống Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia