DRUG TREATMENT OF PSYCHOSIS Psychosis is a thought




![Antipsychotic/Neuroleptics [3 H]Haloperidol binding IC 50 (mol/L) Correlations between therapeutic potency and affinity for Antipsychotic/Neuroleptics [3 H]Haloperidol binding IC 50 (mol/L) Correlations between therapeutic potency and affinity for](https://slidetodoc.com/presentation_image_h2/2109267dbb72caa9c0794197f4fb5b25/image-31.jpg)
![Antipsychotic/Neuroleptics Piperazine Piperidine Effect Aliphatic [Drug dose] Antipsychotic/Neuroleptics Piperazine Piperidine Effect Aliphatic [Drug dose]](https://slidetodoc.com/presentation_image_h2/2109267dbb72caa9c0794197f4fb5b25/image-38.jpg)
![Antipsychotic/Neuroleptics Butyrophenone Phenothiazine Effect Thioxanthene [Drug dose] Antipsychotic/Neuroleptics Butyrophenone Phenothiazine Effect Thioxanthene [Drug dose]](https://slidetodoc.com/presentation_image_h2/2109267dbb72caa9c0794197f4fb5b25/image-41.jpg)

- Slides: 57
DRUG TREATMENT OF PSYCHOSIS
Psychosis is a thought disorder characterized by disturbances of reality and perception, impaired cognitive functioning, and inappropriate or diminished affect (mood). Psychosis denotes many mental disorders. Schizophrenia is a particular kind of psychosis characterized mainly by a clear sensorium but a marked thinking disturbance.
Psychosis-Producing Drugs 1) Levodopa 2) CNS stimulants a) Cocaine b) Amphetamines c) Khat, cathinone, methcathinone 3) Apomorphine 4) Phencyclidine
Schizophrenia • Pathogenesis is unknown. • Onset of schizophrenia is in the late teens early ‘ 20 s. • Genetic predisposition -- Familial incidence. • Multiple genes are involved. • Afflicts 1% of the population worldwide. • May or may not be present with anatomical changes.
Schizophrenia • A thought disorder. • The disorder is characterized by a divorcement from reality in the mind of the person (psychosis). • It may involve visual and auditory hallucinations, delusions, intense suspicion, feelings of persecution or control by external forces (paranoia), depersonalization, and there is attachment of excessive personal significance to daily events, called “ideas of reference”.
Schizophrenia Positive Symptoms. Hallucinations, delusions, paranoia, ideas of reference. Negative Symptoms. Apathy, social withdrawal, anhedonia, emotional blunting, cognitive deficits, extreme inattentiveness or lack of motivation to interact with the environment. These symptoms are progressive and non-responsive to medication.

Etiology of Schizophrenia Idiopathic Biological Correlates 1) Genetic Factors 2) Neurodevelopmental abnormalities. 3) Environmental stressors.
Etiology of Schizophrenia Characterized by several structural and functional abnormalities in the brains of schizophrenic patients: 1) Enlarge cerebral ventricles. 2) Atrophy of cortical layers. 3) Reduced volume of the basal ganglia.
Dopamine Theory of Schizophrenia Many lines of evidence point to the aberrant increased activity of the dopaminergic system as being critical in the symptomatology of schizophrenia. There is a greater occupancy of D 2 receptors by dopamine => greater dopaminergic stimulation
Dopamine Theory of Schizophrenia Dopamine Correlates: • Antipsychotics reduce dopamine synaptic activity. • These drugs produce Parkinson-like symptoms. • Drugs that increase DA in the limbic system cause psychosis. • Drugs that reduce DA in the limbic system (postsynaptic D 2 antagonists) reduce psychosis. • Increased DA receptor density (Post-mortem, PET). • Changes in amount of homovanillic acid (HVA), a DA metabolite, in plasma, urine, and CSF.
Pharmacodynamics Anatomic Correlates of Schizophrenia. . . Areas Associated with Mood and Thought Processes: Frontal cortex Amygdala Hippocampus Nucleus accumbens Limbic Cortex
Dopamine Theory of Schizophrenia Evidence against the Theory? • Antipsychotics are only partially effective in most (70%) and ineffective for some patients. • Phencyclidine, an NMDA receptor antagonist, produces more schizophrenia-like symptoms in nonschizophrenic subjects than DA agonists. • Atypical antipsychotics have low affinity for D 2 receptors. • Focus is broader now and research is geared to produce drugs with less extrapyramidal effects.
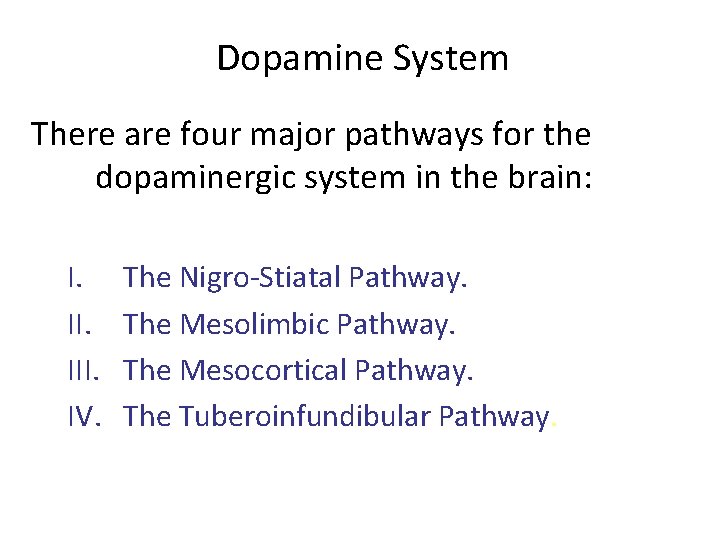
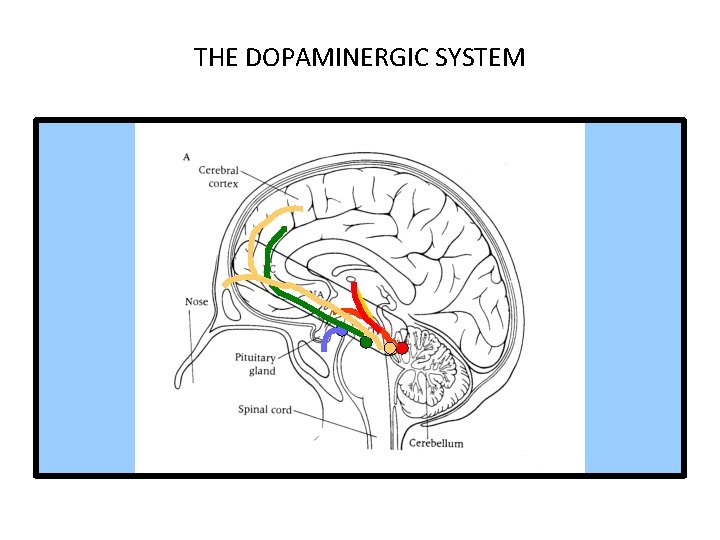
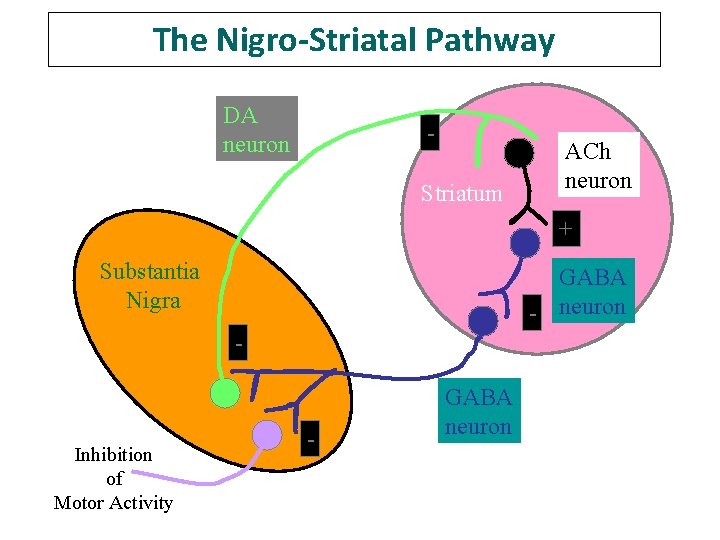
Dopamine System There are four major pathways for the dopaminergic system in the brain: I. III. IV. The Nigro-Stiatal Pathway. The Mesolimbic Pathway. The Mesocortical Pathway. The Tuberoinfundibular Pathway.
THE DOPAMINERGIC SYSTEM
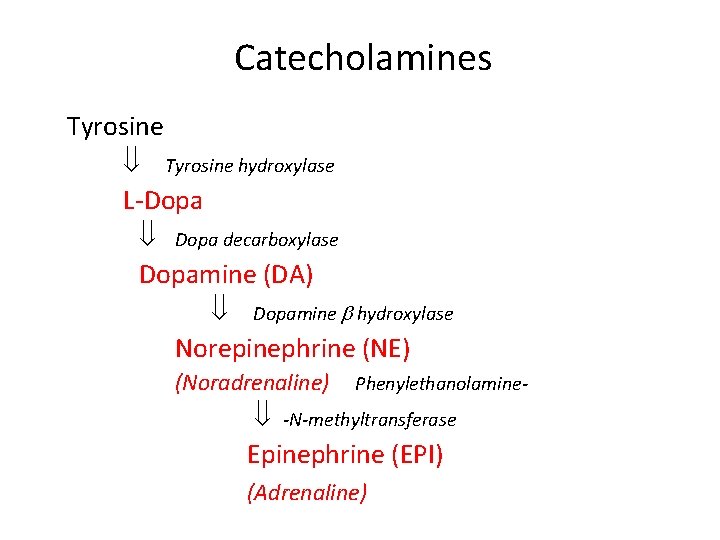
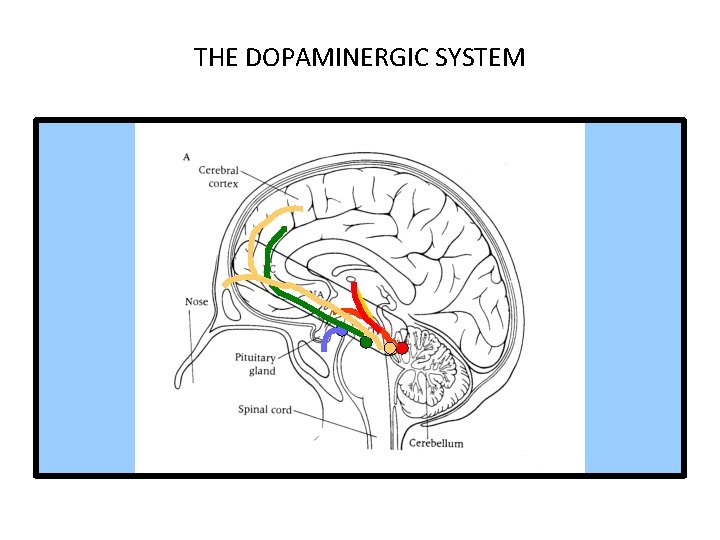
Catecholamines Tyrosine hydroxylase L-Dopa decarboxylase Dopamine (DA) Dopamine hydroxylase Norepinephrine (NE) (Noradrenaline) Phenylethanolamine- -N-methyltransferase Epinephrine (EPI) (Adrenaline)
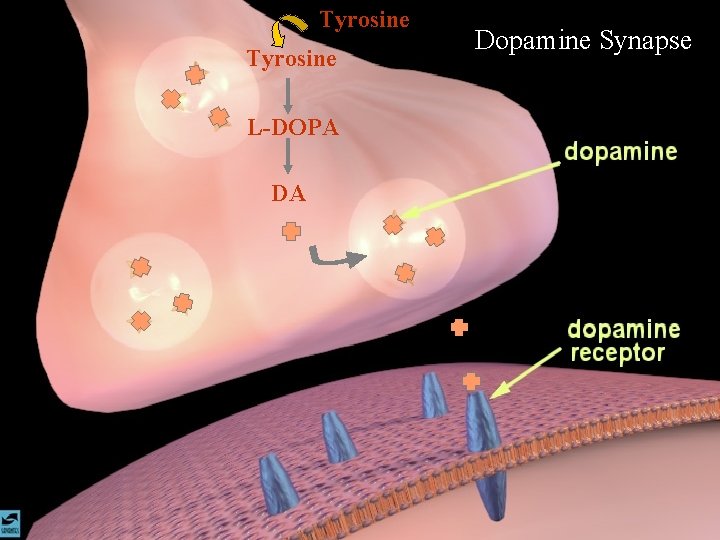
Tyrosine L-DOPA DA Dopamine Synapse
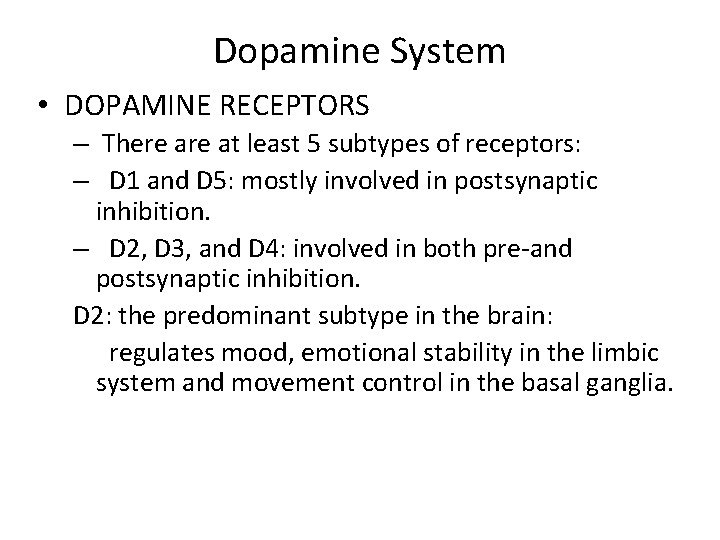
Dopamine System • DOPAMINE RECEPTORS – There at least 5 subtypes of receptors: – D 1 and D 5: mostly involved in postsynaptic inhibition. – D 2, D 3, and D 4: involved in both pre-and postsynaptic inhibition. D 2: the predominant subtype in the brain: regulates mood, emotional stability in the limbic system and movement control in the basal ganglia.


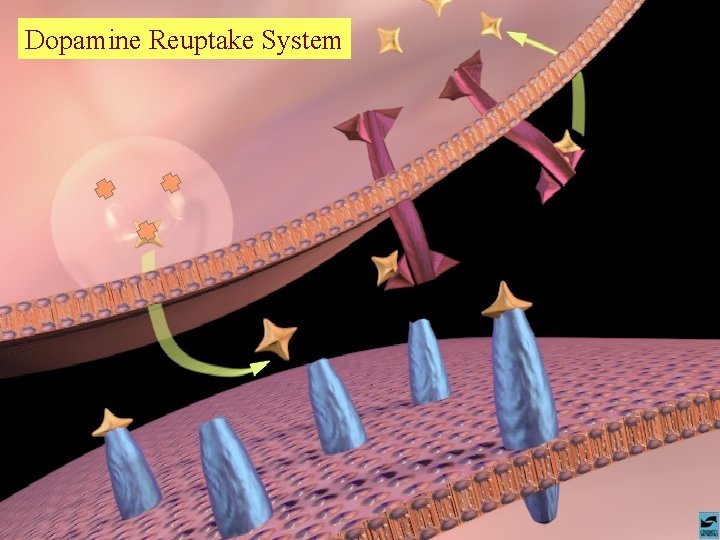
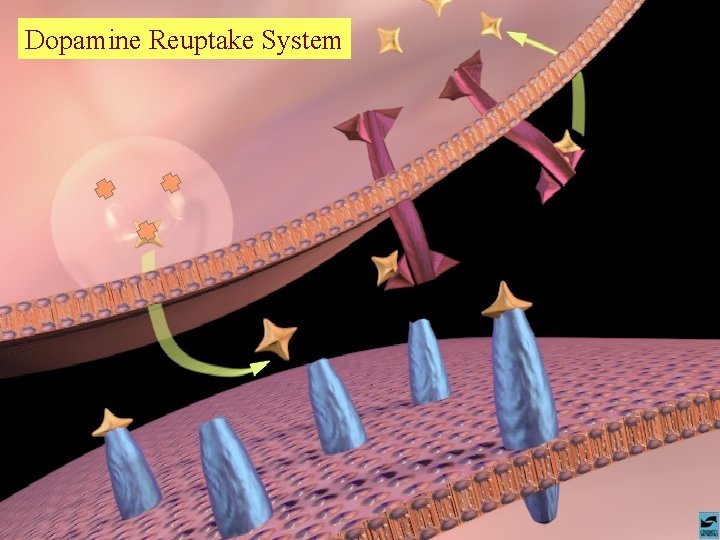
Dopamine Reuptake System

Antipsychotic treatments SCHIZOPHRENIA IS FOR LIFE There is no remission
Antipsychotic treatments Schizophrenia has been around perhaps, since the beginning of humankind, however, it was not until the last century that it was established as a separate entity amongst other mental disorders. Many treatments have been devised: v Hydrotherapy: “The pouring of cold water in a stream, from a height of at least four feet onto the forehead, is one of the most certain means of subsiding violent, maniacal excitement that we have ever seen tried”. . . wrote an anonymous physician in the early 1800’s.
Antipsychotic treatments v Lobotomies (Egaz Moniz). v In 1940’s Phenothiazenes were isolated and were used as pre-anesthetic medication, but quickly were adopted by psychiatrists to calm down their mental patients. v In 1955, chlorpromazine was developed as an antihistaminic agent by Rhône-Pauline Laboratories in France. In-patients at Mental Hospitals dropped by 1/3.
Antipsychotics treatment Antipsychotics/Neuroleptics • • Antipsychotics are the drugs currently used in the prevention of psychosis. They have also been termed neuroleptics, because they suppress motor activity and emotionality. ** These drugs are not a cure ** • Schizophrenics must be treated with medications indefinitely, in as much as the disease in lifelong and it is preferable to prevent the psychotic episodes than to treat them.
Antipsychotics/Neuroleptics Although the antipsychotic/neuroleptics are drugs used mainly in the treatment of schizophrenia, they are also used in the treatment of other psychoses associated with depression and manic -depressive illness, and psychosis associated with Alzheimer’s disease. These conditions are life-long and disabling.
Antipsychotics/Neuroleptics NON-compliance is the major reason for relapse.
Antipsychotic/Neuroleptics OLDER DRUGS Three major groups : 1) Phenothiazines 2) Thioxanthines 3) Butyrophenones
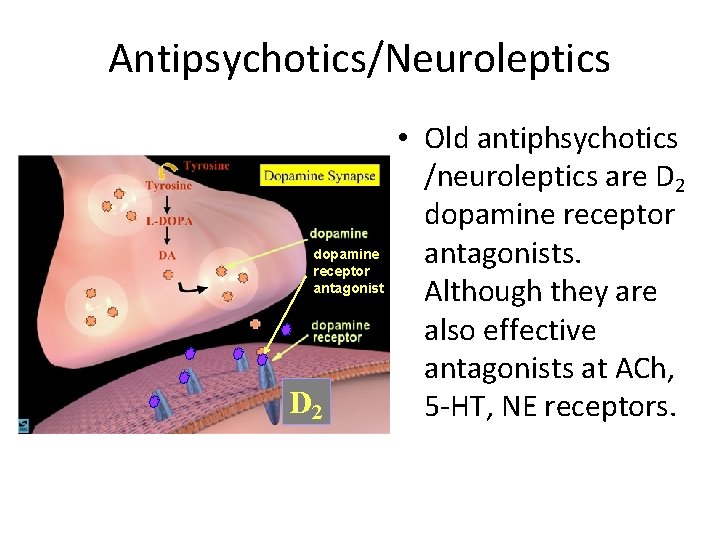
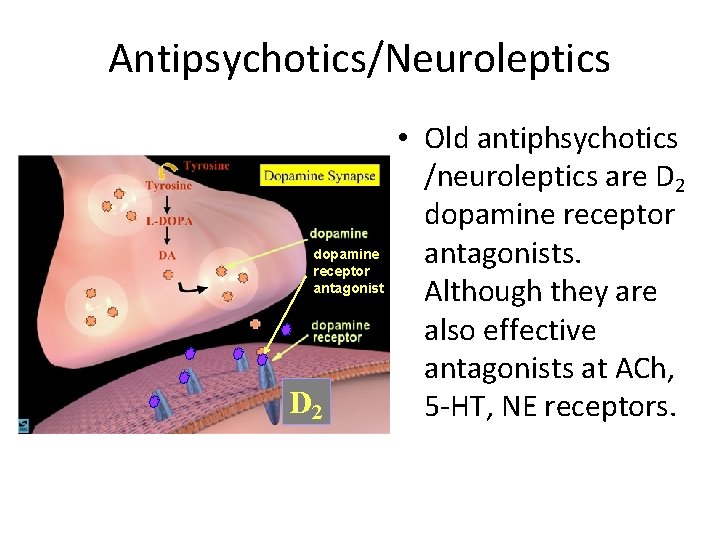
Antipsychotics/Neuroleptics dopamine receptor antagonist D 2 • Old antiphsychotics /neuroleptics are D 2 dopamine receptor antagonists. Although they are also effective antagonists at ACh, 5 -HT, NE receptors.
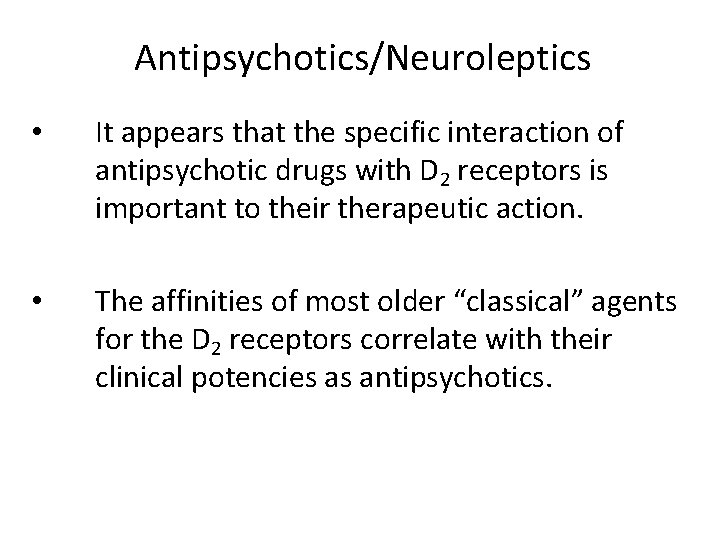
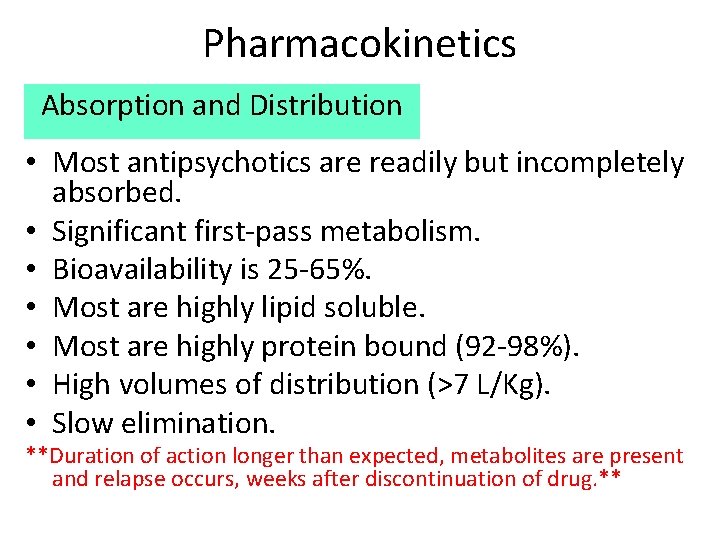
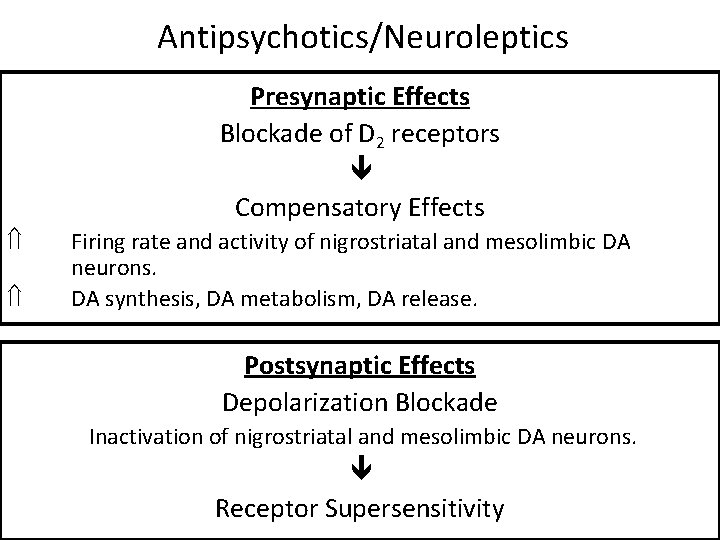
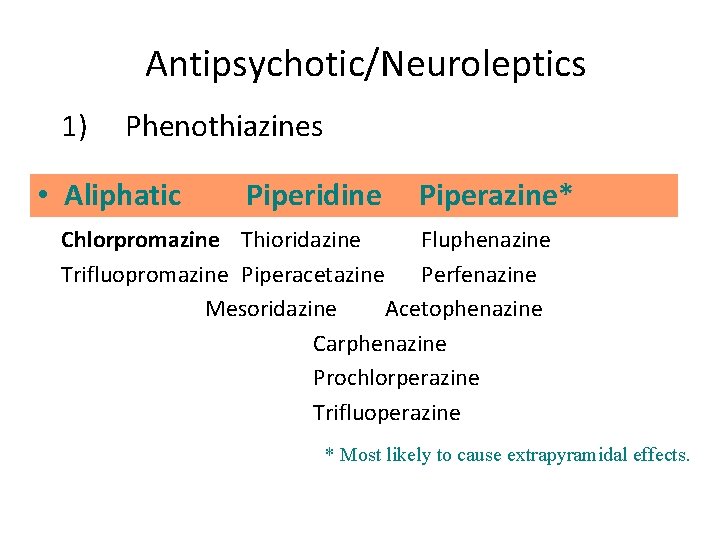
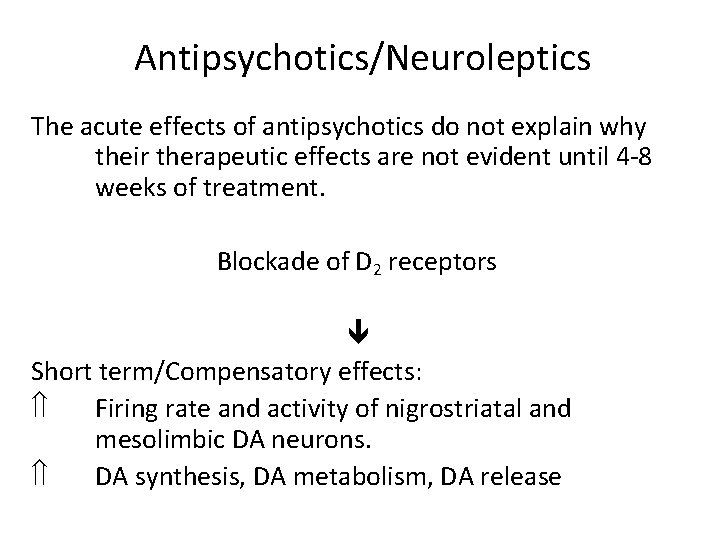
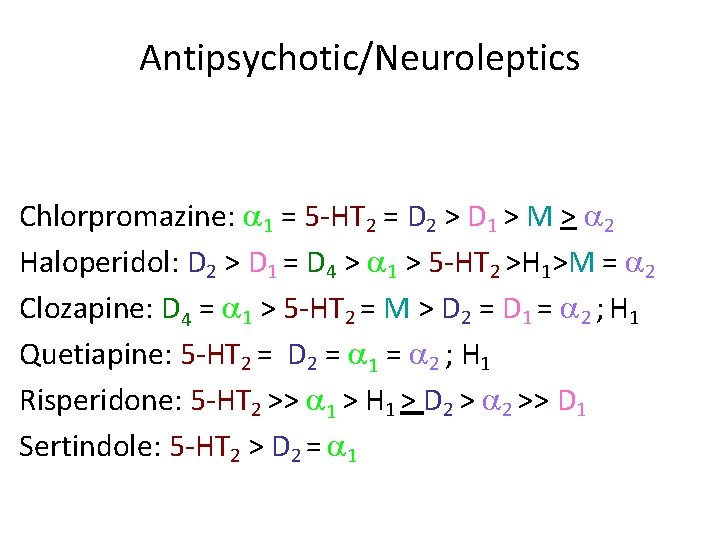
Antipsychotics/Neuroleptics • It appears that the specific interaction of antipsychotic drugs with D 2 receptors is important to their therapeutic action. • The affinities of most older “classical” agents for the D 2 receptors correlate with their clinical potencies as antipsychotics.
![AntipsychoticNeuroleptics 3 HHaloperidol binding IC 50 molL Correlations between therapeutic potency and affinity for Antipsychotic/Neuroleptics [3 H]Haloperidol binding IC 50 (mol/L) Correlations between therapeutic potency and affinity for](https://slidetodoc.com/presentation_image_h2/2109267dbb72caa9c0794197f4fb5b25/image-31.jpg)
Antipsychotic/Neuroleptics [3 H]Haloperidol binding IC 50 (mol/L) Correlations between therapeutic potency and affinity for binding D 2 receptors. promazine chlorpromazine thiothixene clozapine haloperidol spiroperidole Clinical dose of drug [mg d-1]
Antipsychotics/Neuroleptics • Both D 1 and D 2 receptors are found in high concentrations in the striatum and the nucleus accumbens. • Clozapine has a higher affinity for the D 4 receptors than for D 2. • Recently it has been found that most antipsychotic drugs may also bind D 3 receptors (therefore, they are non-selective).
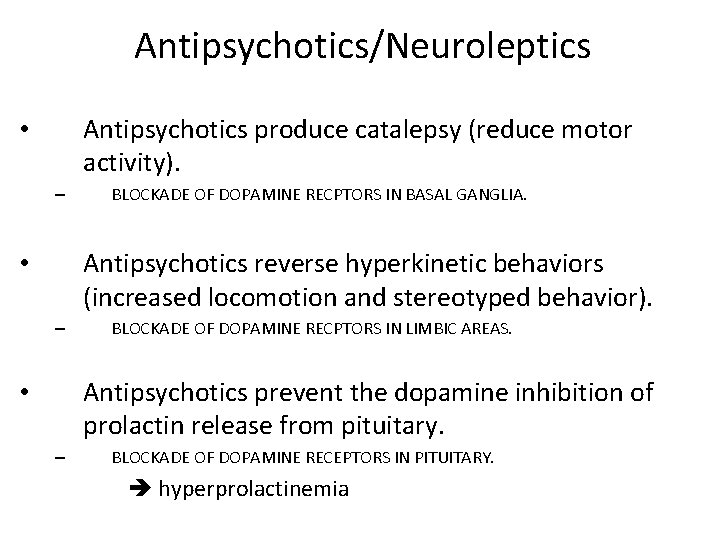
Antipsychotics/Neuroleptics Antipsychotics produce catalepsy (reduce motor activity). • – BLOCKADE OF DOPAMINE RECPTORS IN BASAL GANGLIA. Antipsychotics reverse hyperkinetic behaviors (increased locomotion and stereotyped behavior). • – BLOCKADE OF DOPAMINE RECPTORS IN LIMBIC AREAS. Antipsychotics prevent the dopamine inhibition of prolactin release from pituitary. • – BLOCKADE OF DOPAMINE RECEPTORS IN PITUITARY. hyperprolactinemia
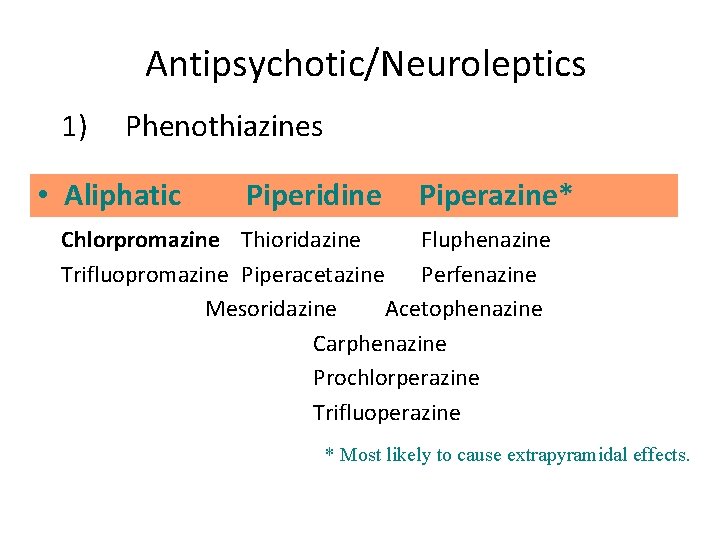
Pharmacokinetics Absorption and Distribution • Most antipsychotics are readily but incompletely absorbed. • Significant first-pass metabolism. • Bioavailability is 25 -65%. • Most are highly lipid soluble. • Most are highly protein bound (92 -98%). • High volumes of distribution (>7 L/Kg). • Slow elimination. **Duration of action longer than expected, metabolites are present and relapse occurs, weeks after discontinuation of drug. **
Pharmacokinetics Metabolism • Most antipsychotics are almost completely metabolized. • Most have active metabolites, although not important in therapeutic effect, with one exception. The metabolite of thioridazine, mesoridazine, is more potent than the parent compound accounts for most of therapeutic effect.
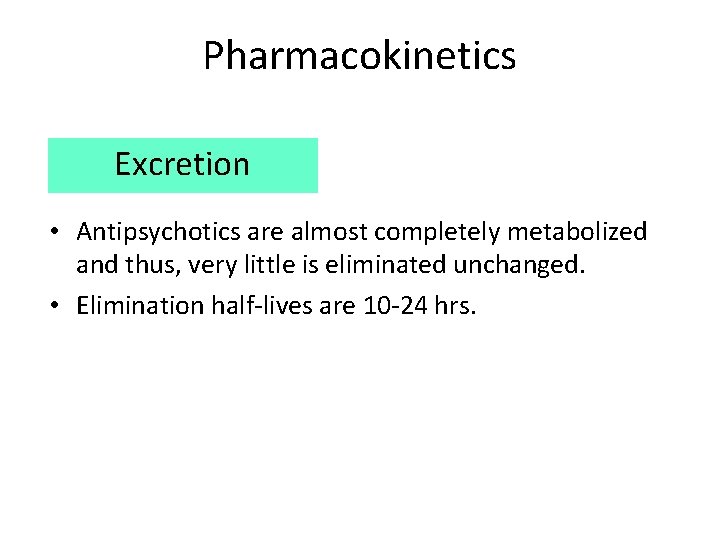
Pharmacokinetics Excretion • Antipsychotics are almost completely metabolized and thus, very little is eliminated unchanged. • Elimination half-lives are 10 -24 hrs.
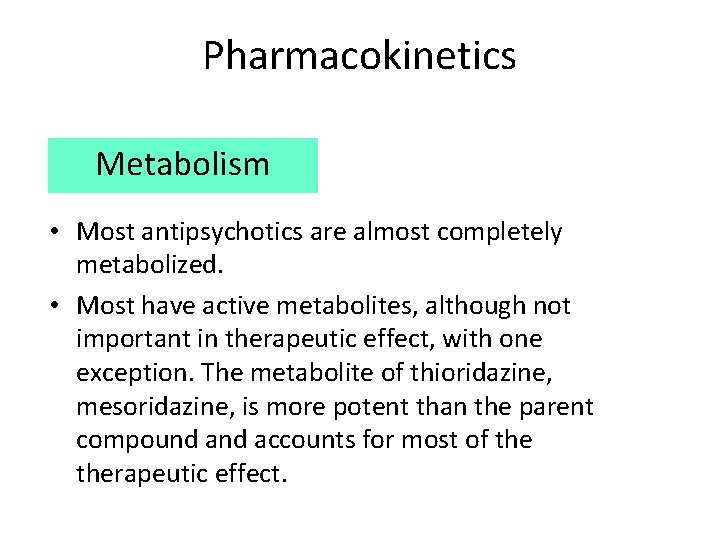
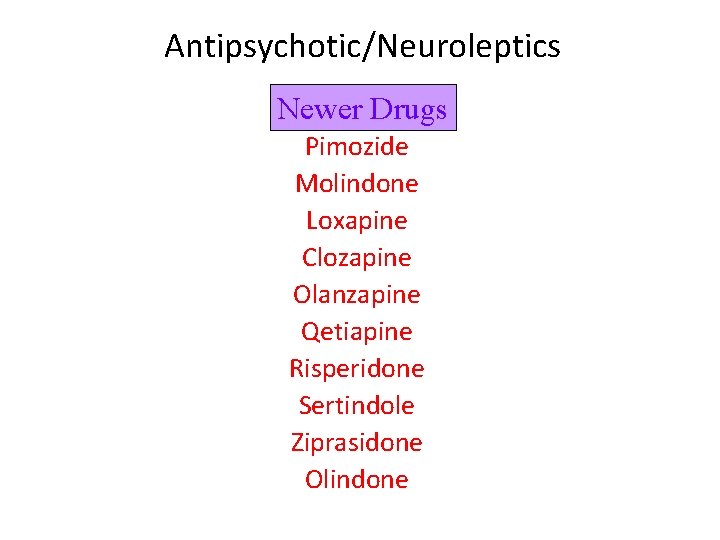
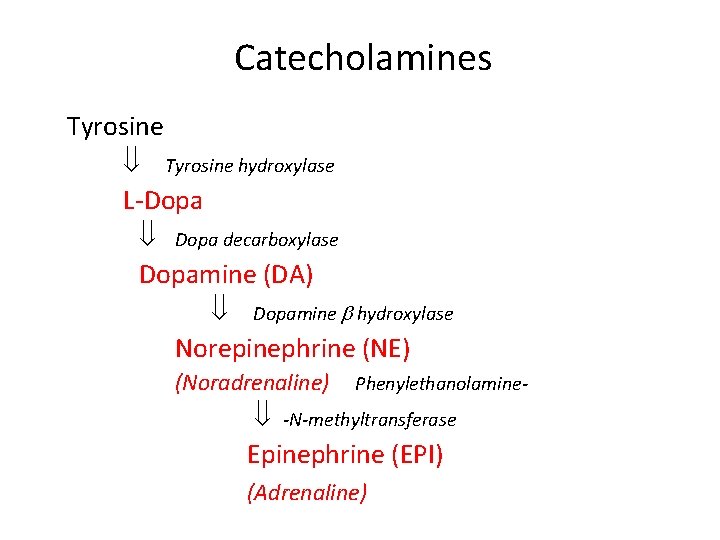
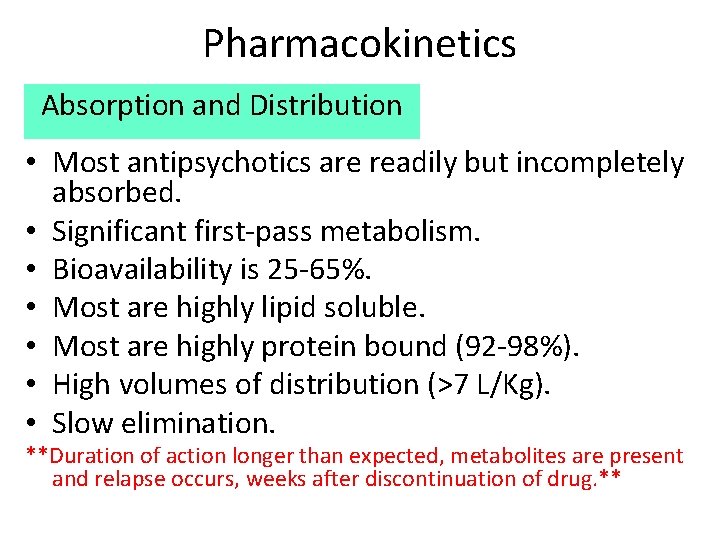
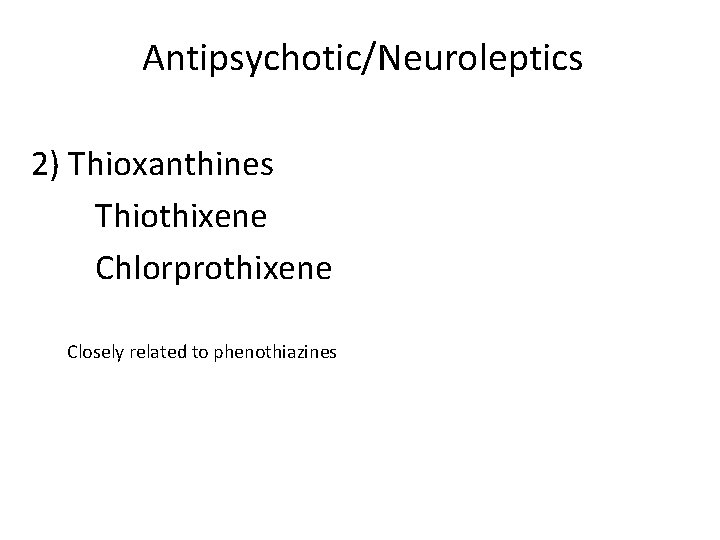
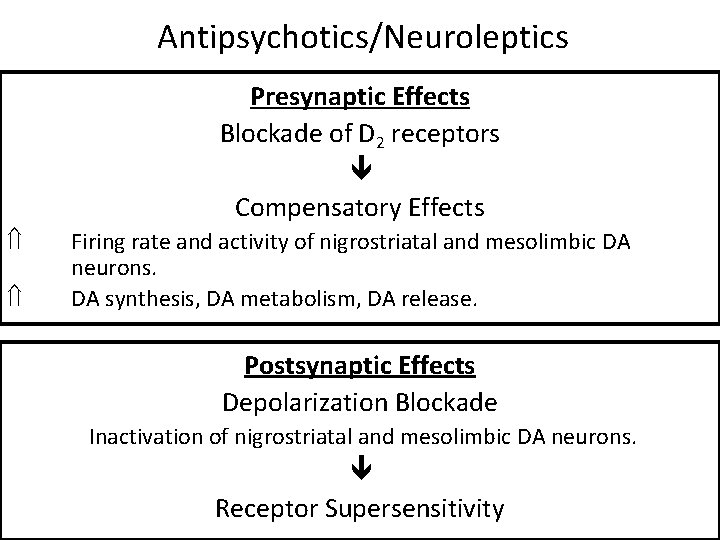
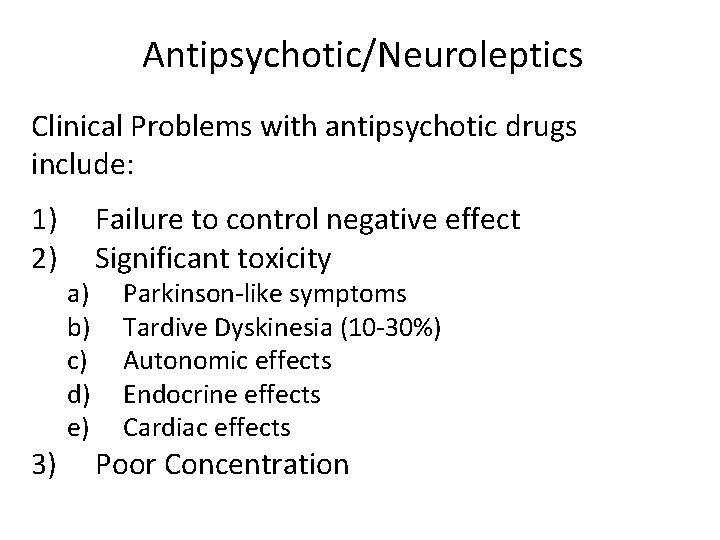
Antipsychotic/Neuroleptics 1) Phenothiazines • Aliphatic Piperidine Piperazine* Chlorpromazine Thioridazine Fluphenazine Trifluopromazine Piperacetazine Perfenazine Mesoridazine Acetophenazine Carphenazine Prochlorperazine Trifluoperazine * Most likely to cause extrapyramidal effects.
![AntipsychoticNeuroleptics Piperazine Piperidine Effect Aliphatic Drug dose Antipsychotic/Neuroleptics Piperazine Piperidine Effect Aliphatic [Drug dose]](https://slidetodoc.com/presentation_image_h2/2109267dbb72caa9c0794197f4fb5b25/image-38.jpg)
Antipsychotic/Neuroleptics Piperazine Piperidine Effect Aliphatic [Drug dose]
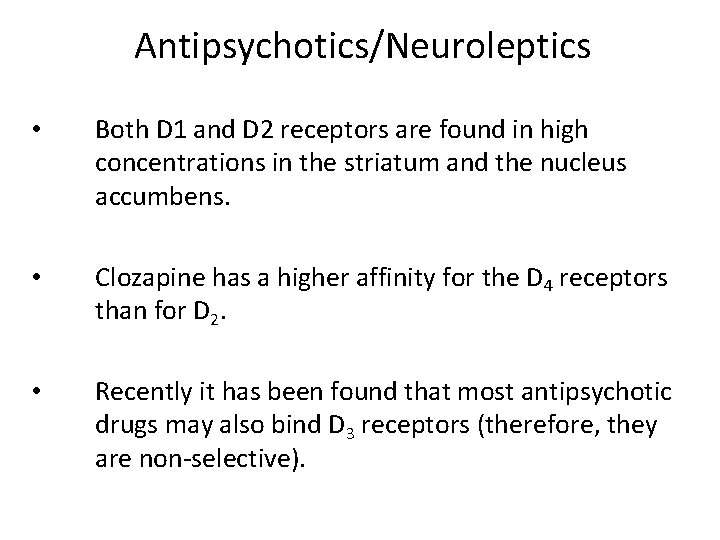
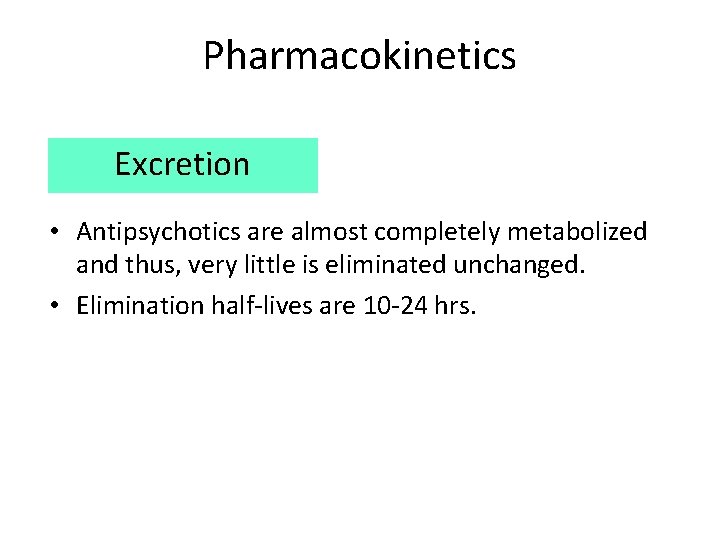
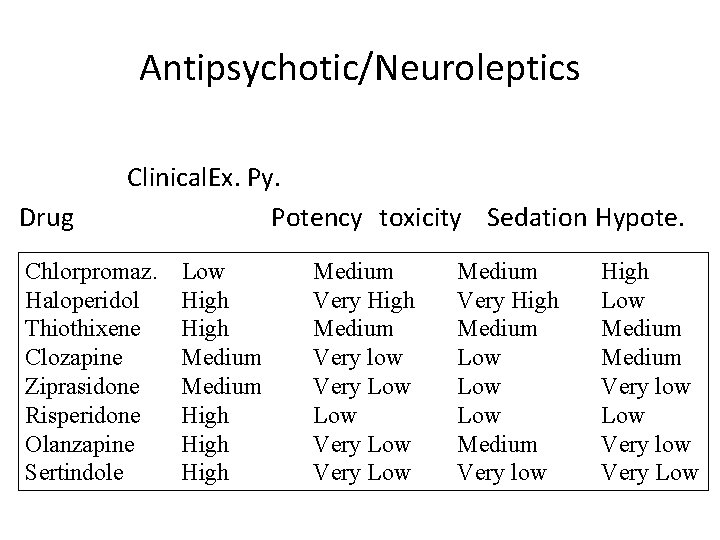
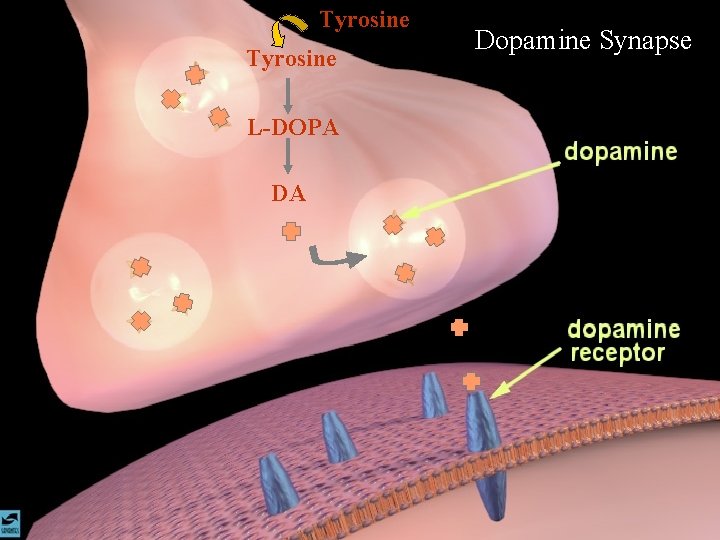
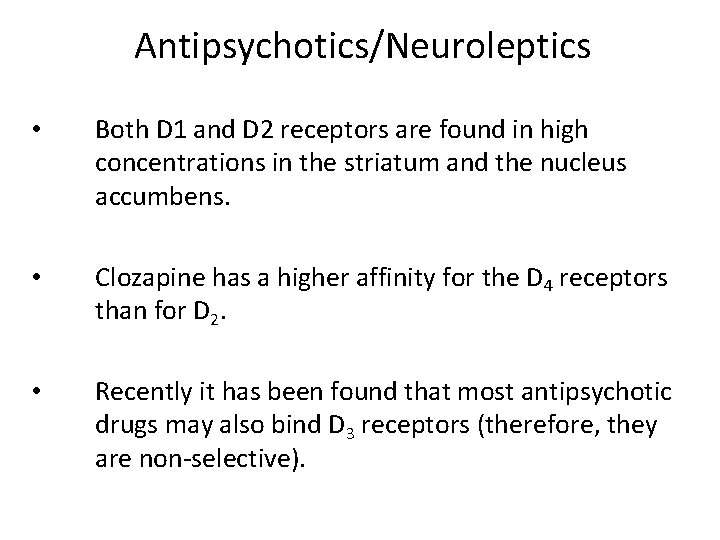
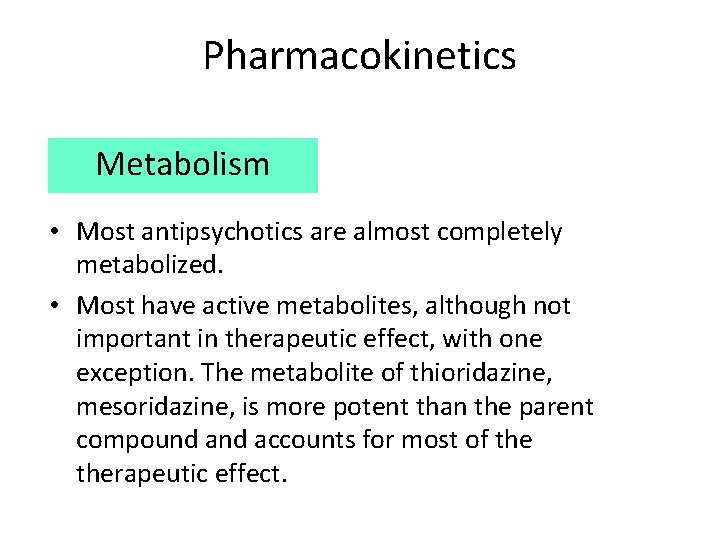
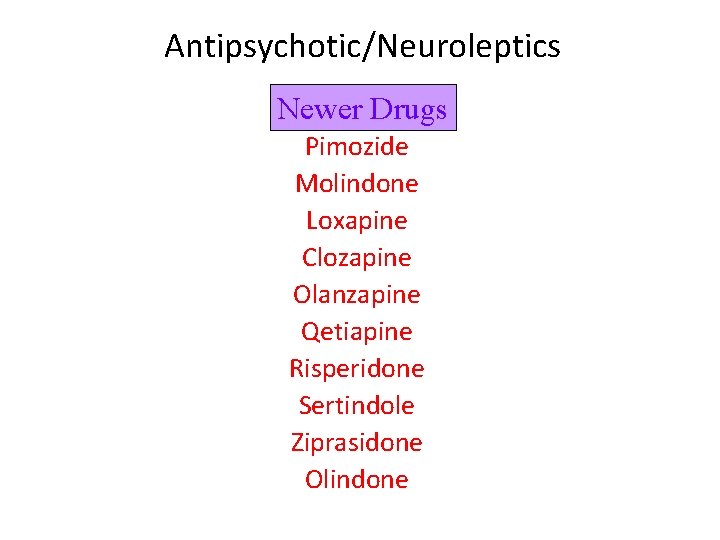
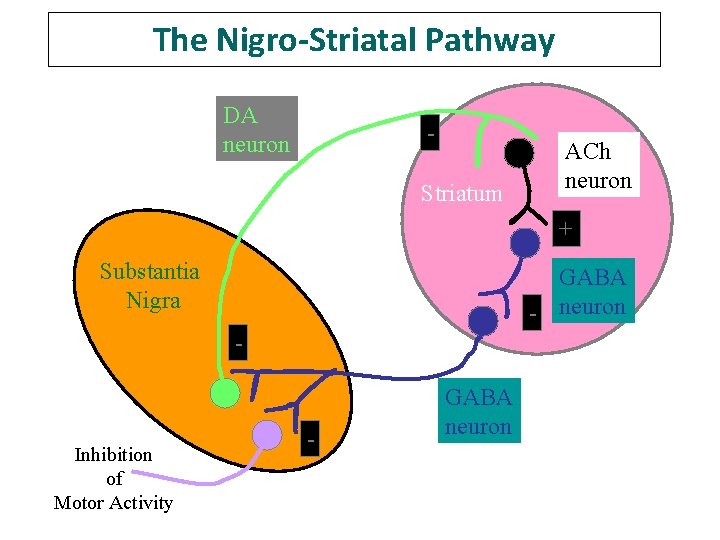
Antipsychotic/Neuroleptics 2) Thioxanthines Thiothixene Chlorprothixene Closely related to phenothiazines
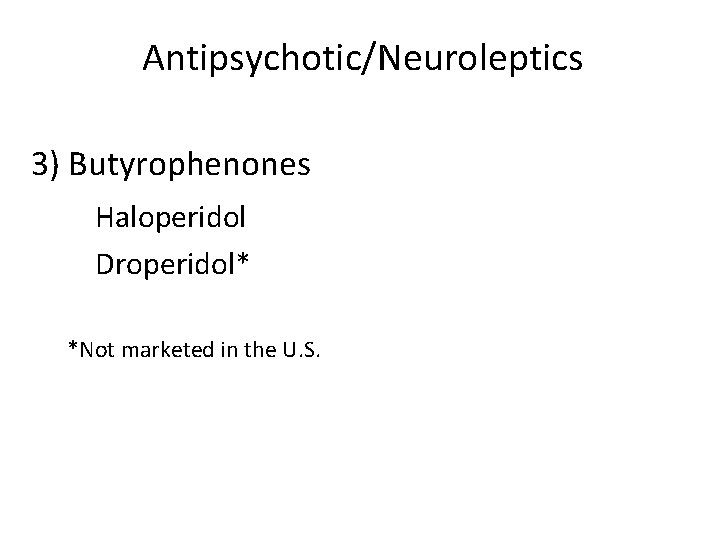
Antipsychotic/Neuroleptics 3) Butyrophenones Haloperidol Droperidol* *Not marketed in the U. S.
![AntipsychoticNeuroleptics Butyrophenone Phenothiazine Effect Thioxanthene Drug dose Antipsychotic/Neuroleptics Butyrophenone Phenothiazine Effect Thioxanthene [Drug dose]](https://slidetodoc.com/presentation_image_h2/2109267dbb72caa9c0794197f4fb5b25/image-41.jpg)
Antipsychotic/Neuroleptics Butyrophenone Phenothiazine Effect Thioxanthene [Drug dose]
Antipsychotics/Neuroleptics • Newer drugs have higher affinities for D 1, 5 HT or -AR receptors. • NE, GABA, Glycine and Glutamate have also been implicated in schizophrenia.
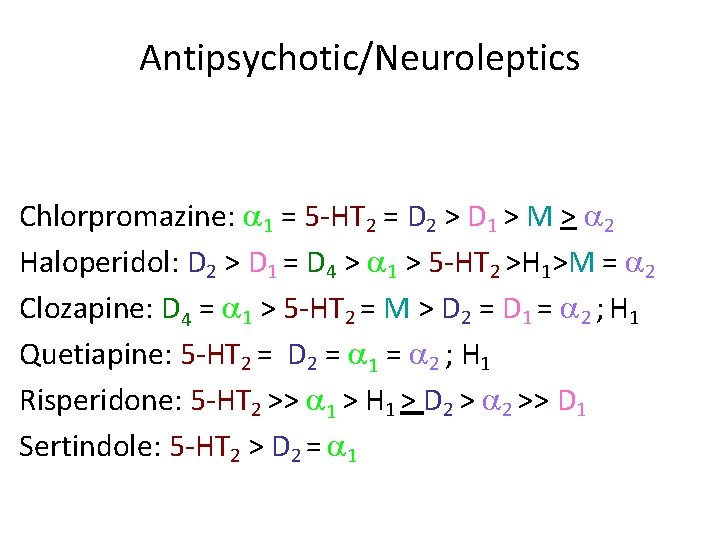
Antipsychotics/Neuroleptics The acute effects of antipsychotics do not explain why their therapeutic effects are not evident until 4 -8 weeks of treatment. Blockade of D 2 receptors Short term/Compensatory effects: Ý Firing rate and activity of nigrostriatal and mesolimbic DA neurons. Ý DA synthesis, DA metabolism, DA release
Antipsychotics/Neuroleptics Presynaptic Effects Blockade of D 2 receptors Compensatory Effects Ý Ý Firing rate and activity of nigrostriatal and mesolimbic DA neurons. DA synthesis, DA metabolism, DA release. Postsynaptic Effects Depolarization Blockade Inactivation of nigrostriatal and mesolimbic DA neurons. Receptor Supersensitivity
Antipsychotic/Neuroleptics Newer Drugs Pimozide Molindone Loxapine Clozapine Olanzapine Qetiapine Risperidone Sertindole Ziprasidone Olindone
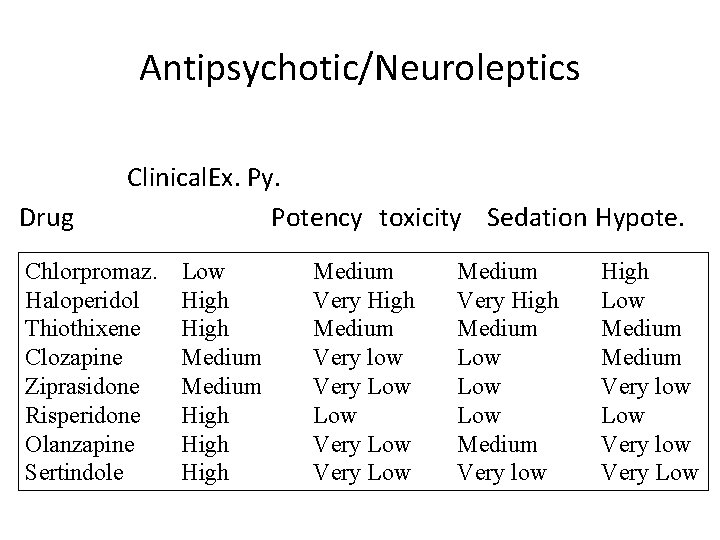
Antipsychotic/Neuroleptics Drug Clinical. Ex. Py. Potency toxicity Sedation Hypote. Chlorpromaz. Haloperidol Thiothixene Clozapine Ziprasidone Risperidone Olanzapine Sertindole Low High Medium High Medium Very low Very Low Medium Very High Medium Low Low Medium Very low High Low Medium Very low Low Very low Very Low
Antipsychotic/Neuroleptics Chlorpromazine: 1 = 5 -HT 2 = D 2 > D 1 > M > 2 Haloperidol: D 2 > D 1 = D 4 > 1 > 5 -HT 2 >H 1>M = 2 Clozapine: D 4 = 1 > 5 -HT 2 = M > D 2 = D 1 = 2 ; H 1 Quetiapine: 5 -HT 2 = D 2 = 1 = 2 ; H 1 Risperidone: 5 -HT 2 >> 1 > H 1 > D 2 >> D 1 Sertindole: 5 -HT 2 > D 2 = 1
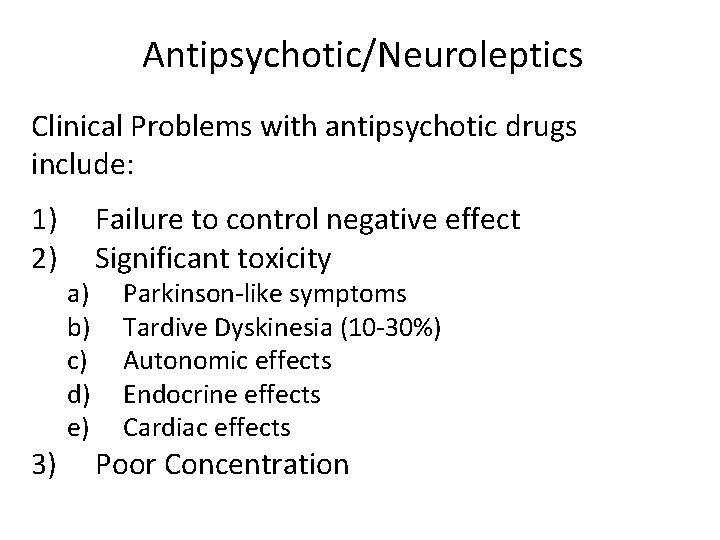
Antipsychotic/Neuroleptics Clinical Problems with antipsychotic drugs include: 1) 2) 3) a) b) c) d) e) Failure to control negative effect Significant toxicity Parkinson-like symptoms Tardive Dyskinesia (10 -30%) Autonomic effects Endocrine effects Cardiac effects Poor Concentration
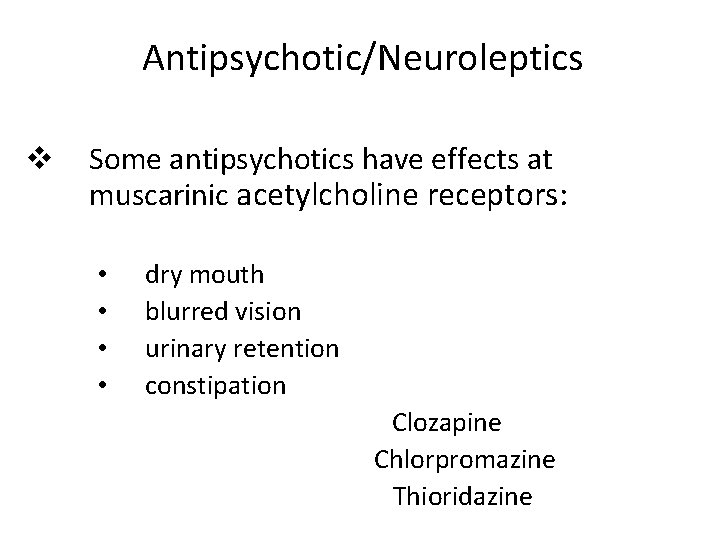
The Nigro-Striatal Pathway DA neuron Striatum ACh neuron + Substantia Nigra GABA - neuron - Inhibition of Motor Activity - GABA neuron
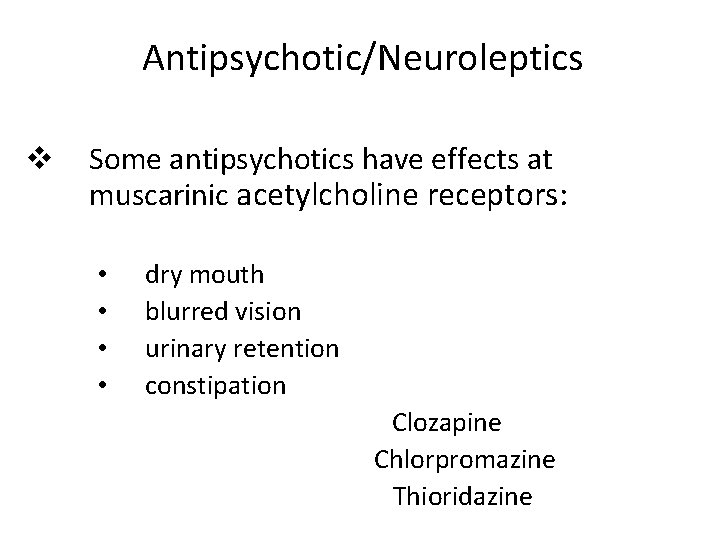
Antipsychotic/Neuroleptics v Some antipsychotics have effects at muscarinic acetylcholine receptors: • • dry mouth blurred vision urinary retention constipation Clozapine Chlorpromazine Thioridazine
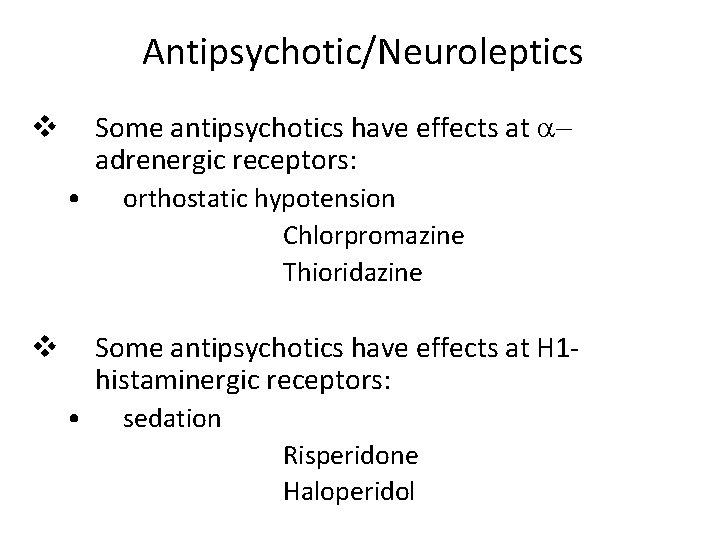
Antipsychotic/Neuroleptics Some antipsychotics have effects at adrenergic receptors: v • orthostatic hypotension Chlorpromazine Thioridazine Some antipsychotics have effects at H 1 histaminergic receptors: v • sedation Risperidone Haloperidol
Antipsychotic/Neuroleptics v Blockade of D 2 receptors in lactotrophs in breast increase prolactin concentration and may produce breast engorgement and galactorrhea.
Antipsychotic/Neuroleptics Neuroleptic Malignant Syndrome Is a rare but serious side effect of neuroleptic (antipsychotic) therapy that can be lethal. It can arise at any time in the course of treatment and shows no predilection for age, duration of treatment, antipsychotic medication, or dose.
Antipsychotic/Neuroleptics Neuroleptic Malignant Syndrome • • • Occurs in pts. hypersensitive to the Ex. Py. effects of antipsychotics. Due to excessively rapid blockade of postsynaptic dopamine receptors. The syndrome begins with marked muscle rigidity. If sweating is impaired, a fever may ensue. The stress leukocytosis and high fever associated with this syndrome may be mistaken for an infection. Autonomic instability with altered blood pressure and heart rate is another midbrain manifestation. Creatine kinase isozymes are usually elevated, reflecting muscle damage.
Antipsychotic/Neuroleptics Neuroleptic Malignant Syndrome Treatment Vigorous treatment with antiparkinsonian drugs is recommended as soon as possible. Muscle relaxants such as diazepam, dantrolene or bromocriptine may be helpful.
Antipsychotic/Neuroleptics Drug Interactions • • • Additive effects with sedatives. Additive effects with anticholinergics. Additive effects with antihistaminergics. Additive effects with -AR blocking drugs. Additive effects with drugs with quinidine-like action (thioridazine).

 Complete vs incomplete thinking
Complete vs incomplete thinking Methods of adulteration of crude drugs
Methods of adulteration of crude drugs Neurosurgery
Neurosurgery Organism
Organism Drug of choice for the treatment of extraluminal amebiasis
Drug of choice for the treatment of extraluminal amebiasis Cdtcc
Cdtcc Principles effective addiction treatment
Principles effective addiction treatment Autoscopic psychosis
Autoscopic psychosis Fahad alosaimi
Fahad alosaimi Dopamine hypothesis of schizophrenia ppt
Dopamine hypothesis of schizophrenia ppt Psychiatric disorders
Psychiatric disorders Psycosis
Psycosis Psychosis and ptsd
Psychosis and ptsd Postictal meaning
Postictal meaning Types of psychosis and neurosis
Types of psychosis and neurosis Functional psychosis
Functional psychosis First episode psychosis
First episode psychosis Difference between neurotic and psychotic
Difference between neurotic and psychotic Types of psychosis
Types of psychosis Psychosis vs neurosis
Psychosis vs neurosis What is forensic psychiatry
What is forensic psychiatry Infantile autism
Infantile autism First episode psychosis
First episode psychosis Mild psychosis
Mild psychosis Psychosis
Psychosis Neurosis vs psychosis
Neurosis vs psychosis Psychosis traduction
Psychosis traduction Dena schlosser baby picture
Dena schlosser baby picture History of macroeconomic thought
History of macroeconomic thought Cara fulton
Cara fulton Food for thought reading
Food for thought reading School of thoughts in criminology
School of thoughts in criminology Speech style
Speech style Postformal thought examples
Postformal thought examples Ucl desktop everywhere
Ucl desktop everywhere Quantitative school of management thought
Quantitative school of management thought Harry potter outline
Harry potter outline Jean piaget theory
Jean piaget theory Have you ever thought about questions
Have you ever thought about questions Abstract thought meaning
Abstract thought meaning The cat who thought she was a dog
The cat who thought she was a dog No second thought expulsion order
No second thought expulsion order Purity of thought
Purity of thought A long narrow coiled tube where digestion is completed
A long narrow coiled tube where digestion is completed Carat punctuation
Carat punctuation Operational thought
Operational thought Two key points
Two key points Recursive thought
Recursive thought Taylor shovel experiment
Taylor shovel experiment Labouvie-vief pragmatic thought
Labouvie-vief pragmatic thought Thought stopping
Thought stopping Automatic thoughts examples
Automatic thoughts examples The thirty-three thieves thought that they thrilled
The thirty-three thieves thought that they thrilled Mental status speech descriptors
Mental status speech descriptors Food for thought
Food for thought Einstein train thought experiment
Einstein train thought experiment Bring every thought into captivity
Bring every thought into captivity Thought thaught
Thought thaught