Course Natural History and Prognosis Schizophrenia Course of















- Slides: 79

Course, Natural History and Prognosis Schizophrenia
Course of Schizophrenia
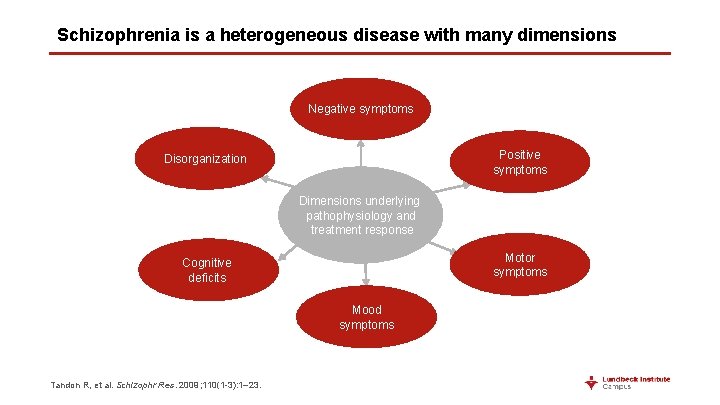
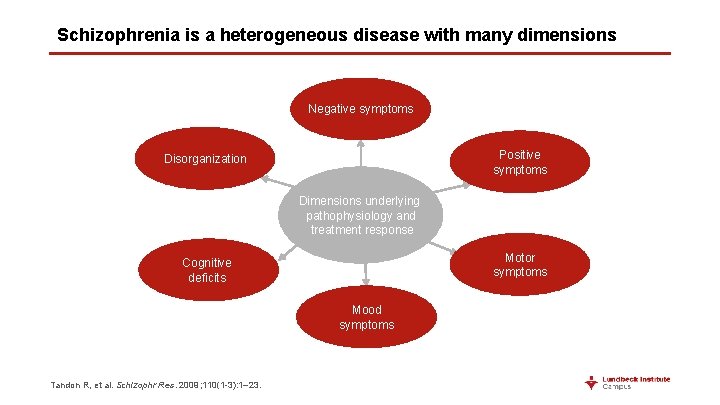
Schizophrenia is a heterogeneous disease with many dimensions Negative symptoms Positive symptoms Disorganization Dimensions underlying pathophysiology and treatment response Motor symptoms Cognitive deficits Mood symptoms Tandon R, et al. Schizophr Res. 2009; 110(1 -3): 1– 23.
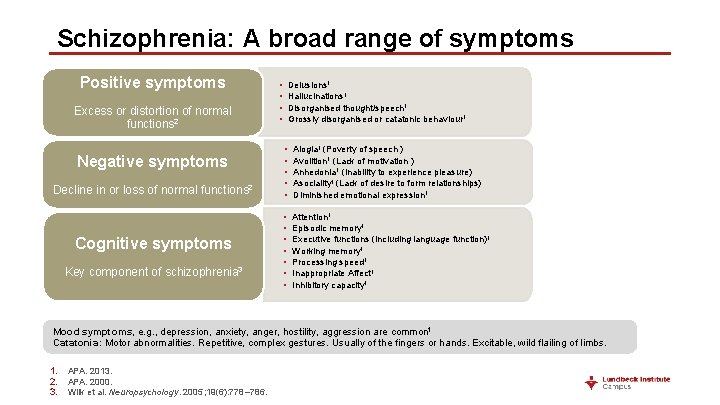
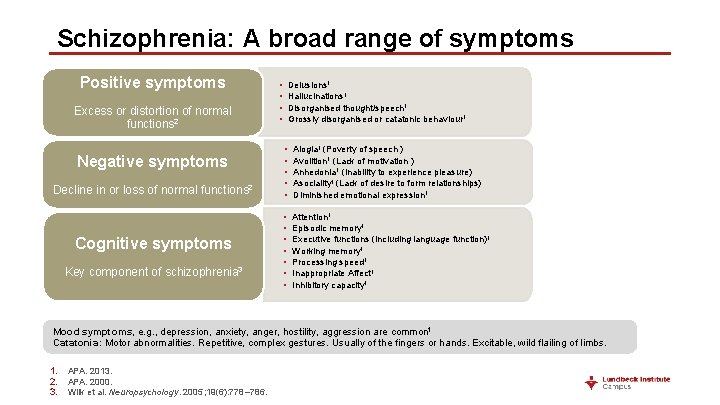
Schizophrenia: A broad range of symptoms Positive symptoms Excess or distortion of normal functions 2 Negative symptoms Decline in or loss of normal functions 2 Cognitive symptoms Key component of schizophrenia 3 • • Delusions 1 Hallucinations 1 Disorganised thought/speech 1 Grossly disorganised or catatonic behaviour 1 • • • Alogia 1 (Poverty of speech ) Avolition 1 (Lack of motivation ) Anhedonia 1 (Inability to experience pleasure) Asociality 1 (Lack of desire to form relationships) Diminished emotional expression 1 • • Attention 1 Episodic memory 1 Executive functions (including language function)1 Working memory 1 Processing speed 1 Inappropriate Affect 1 Inhibitory capacity 1 Mood symptoms, e. g. , depression, anxiety, anger, hostility, aggression are common 1 Catatonia: Motor abnormalities. Repetitive, complex gestures. Usually of the fingers or hands. Excitable, wild flailing of limbs. 1. 2. 3. APA. 2013. APA. 2000. Wilk et al. Neuropsychology. 2005; 19(6): 778– 786.
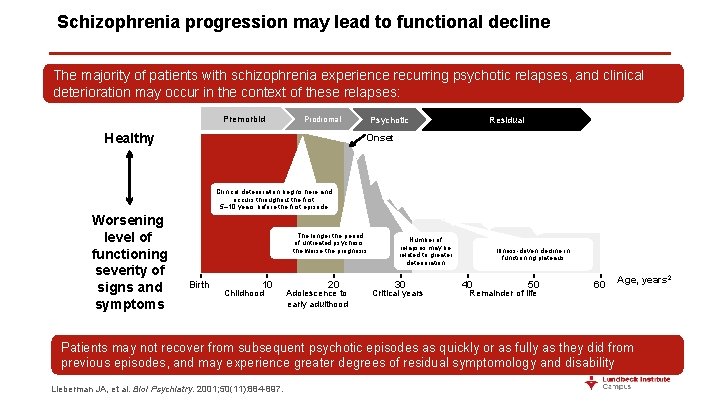
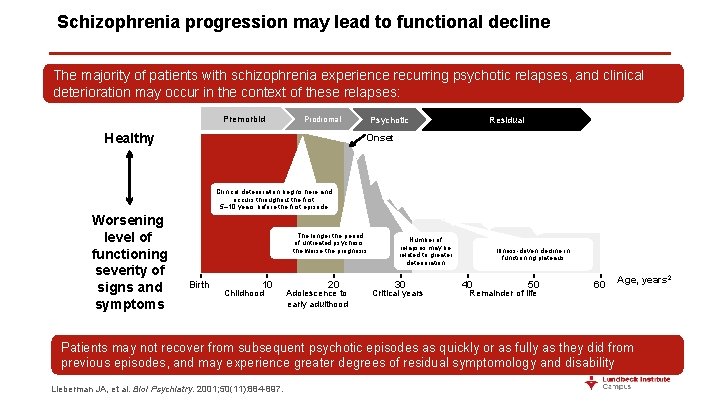
Schizophrenia progression may lead to functional decline The majority of patients with schizophrenia experience recurring psychotic relapses, and clinical deterioration may occur in the context of these relapses: Premorbid Psychotic Prodromal Healthy Residual Onset Clinical deterioration begins here and occurs throughout the first 5– 10 years before the first episode Worsening level of functioning severity of signs and symptoms The longer the period of untreated psychosis, the worse the prognosis Birth 10 Childhood 20 Adolescence to early adulthood Number of relapses may be related to greater deterioration 30 Critical years Illness-driven decline in functioning plateaus 40 50 Remainder of life 60 Age, years 2 Patients may not recover from subsequent psychotic episodes as quickly or as fully as they did from previous episodes, and may experience greater degrees of residual symptomology and disability Lieberman JA, et al. Biol Psychiatry. 2001; 50(11): 884 -897.
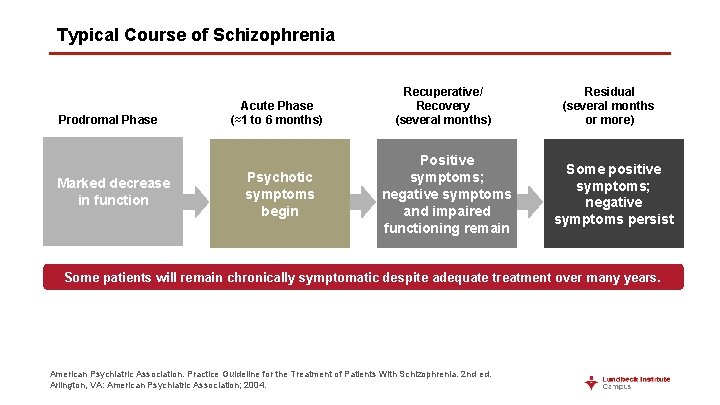
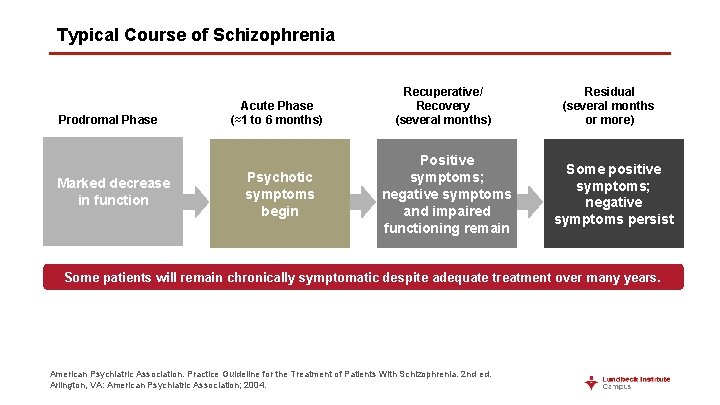
Typical Course of Schizophrenia Prodromal Phase Marked decrease in function Acute Phase (≈1 to 6 months) Psychotic symptoms begin Recuperative/ Recovery (several months) Positive symptoms; negative symptoms and impaired functioning remain Residual (several months or more) Some positive symptoms; negative symptoms persist Some patients will remain chronically symptomatic despite adequate treatment over many years. American Psychiatric Association. Practice Guideline for the Treatment of Patients With Schizophrenia. 2 nd ed. Arlington, VA: American Psychiatric Association; 2004.
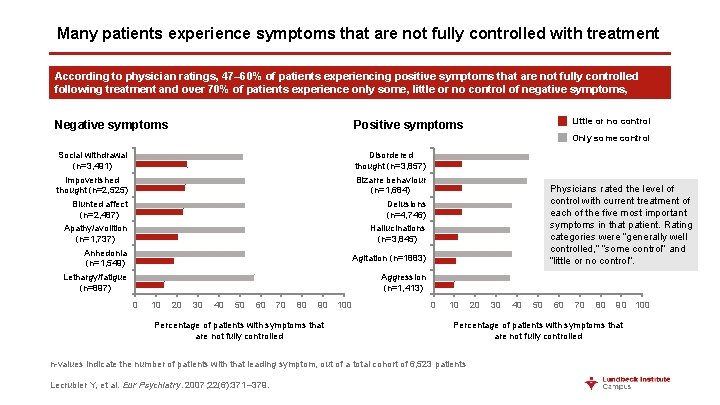
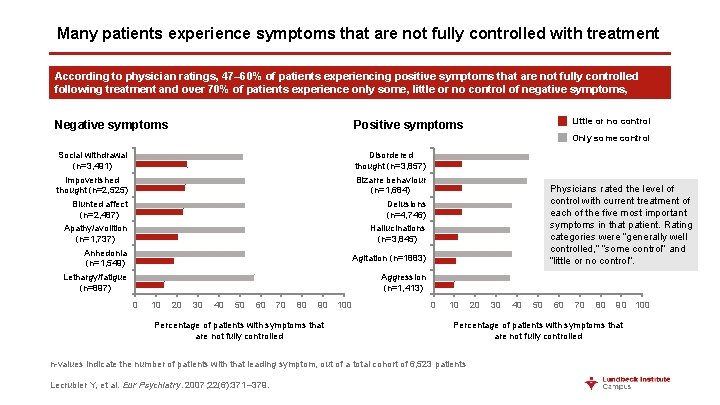
Many patients experience symptoms that are not fully controlled with treatment According to physician ratings, 47– 60% of patients experiencing positive symptoms that are not fully controlled following treatment and over 70% of patients experience only some, little or no control of negative symptoms, Negative symptoms Little or no control Positive symptoms Only some control Disordered thought (n=3, 857) Bizarre behaviour (n=1, 684) Delusions (n=4, 746) Hallucinations (n=3, 845) Social withdrawal (n=3, 491) Impoverished thought (n=2, 525) Blunted affect (n=2, 487) Apathy/avolition (n=1, 737) Anhedonia (n=1, 549) Lethargy/fatigue (n=897) Physicians rated the level of control with current treatment of each of the five most important symptoms in that patient. Rating categories were “generally well controlled, ” “some control” and “little or no control”. Agitation (n=1883) Aggression (n=1, 413) 0 10 20 30 40 50 60 70 80 90 100 Percentage of patients with symptoms that are not fully controlled 0 10 30 40 50 60 70 80 90 100 Percentage of patients with symptoms that are not fully controlled n-values indicate the number of patients with that leading symptom, out of a total cohort of 6, 523 patients Lecrubier Y, et al. Eur Psychiatry. 2007; 22(6): 371– 379. 20
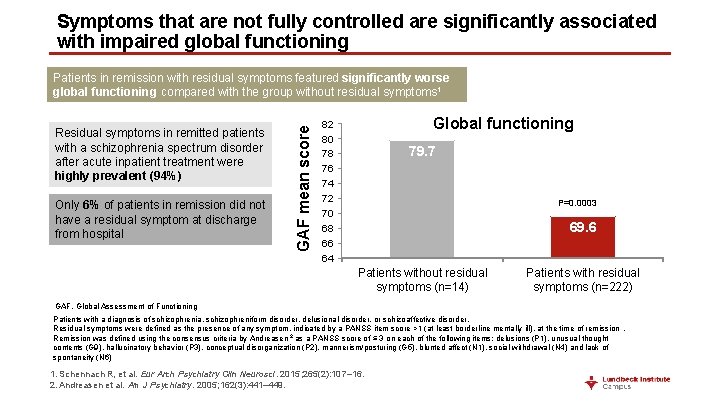
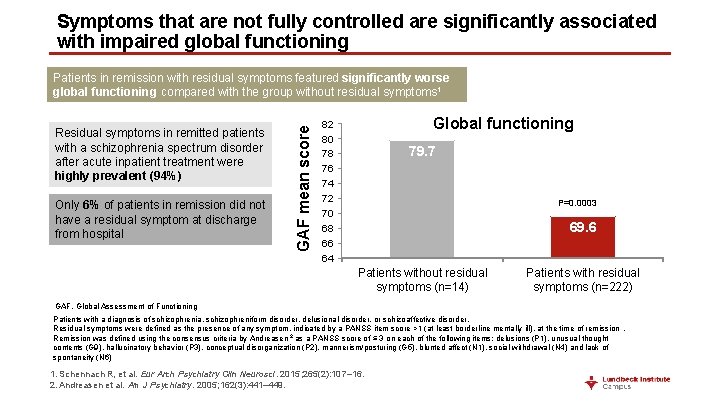
Symptoms that are not fully controlled are significantly associated with impaired global functioning Residual symptoms in remitted patients with a schizophrenia spectrum disorder after acute inpatient treatment were highly prevalent (94%) Only 6% of patients in remission did not have a residual symptom at discharge from hospital GAF mean score Patients in remission with residual symptoms featured significantly worse global functioning compared with the group without residual symptoms 1 Global functioning 82 80 78 76 74 72 70 68 66 64 79. 7 P=0. 0003 69. 6 Patients without residual symptoms (n=14) Patients with residual symptoms (n=222) GAF, Global Assessment of Functioning Patients with a diagnosis of schizophrenia, schizophreniform disorder, delusional disorder, or schizoaffective disorder. Residual symptoms were defined as the presence of any symptom, indicated by a PANSS item score >1 (at least borderline mentally ill), at the time of remission. Remission was defined using the consensus criteria by Andreasen 2 as a PANSS score of ≤ 3 on each of the following items: delusions (P 1), unusual thought contents (G 9), hallucinatory behavior (P 3), conceptual disorganization (P 2), mannerism/posturing (G 5), blunted affect (N 1), social withdrawal (N 4) and lack of spontaneity (N 6) 1. Schennach R, et al. Eur Arch Psychiatry Clin Neurosci. 2015; 265(2): 107– 16. 2. Andreasen et al. Am J Psychiatry. 2005; 162(3): 441– 449.

Disorganization, a common residual symptom, 1 is associated with impaired community functioning ilit R Se es lf- po ca re ns ib un m om C ci So on N 0 y io n ic at ta c al -tu c rb on ul en re co l s ta To Correlation (r) with Life Skills Profile Dimension t ce Disorganization is a reliable predictor of several aspects of community functioning: 2 -0. 07 -0. 1 -0. 2 -0. 3 -0. 4 -0. 25 -0. 31 -0. 37 * ** -0. 5 * p<0. 05. **p<0. 01. Scales were scored so that higher scores indicated better community functioning. Disorganization was defined using the PANSS P 2 item (conceptual disorganization). Schennach R, et al. Eur Arch Psychiatry Clin Neurosci. 2015; 265(2): 107– 16. Norman RM, et al. Am J Psychiatry. 1999; 156(3): 400– 5. -0. 37 ** -0. 47 ***
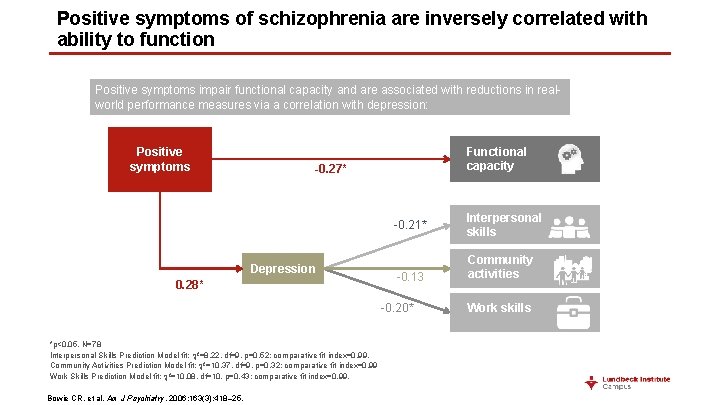
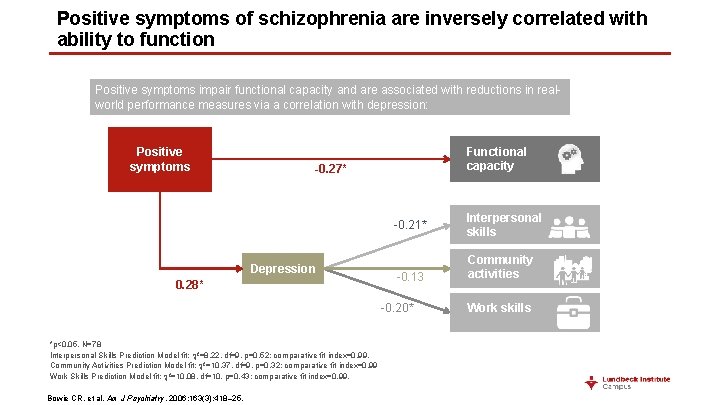
Positive symptoms of schizophrenia are inversely correlated with ability to function Positive symptoms impair functional capacity and are associated with reductions in realworld performance measures via a correlation with depression: Positive symptoms Functional capacity -0. 27* -0. 21* Depression 0. 28* -0. 13 -0. 20* *p<0. 05. N=78 Interpersonal Skills Prediction Model fit: ²=8. 22, df=9, p=0. 52; comparative fit index=0. 99. Community Activities Prediction Model fit: ²=10. 37, df=9, p=0. 32; comparative fit index=0. 99 Work Skills Prediction Model fit: ²=10. 08, df=10, p=0. 43; comparative fit index=0. 99. Bowie CR, et al. Am J Psychiatry. 2006; 163(3): 418– 25. Interpersonal skills Community activities Work skills
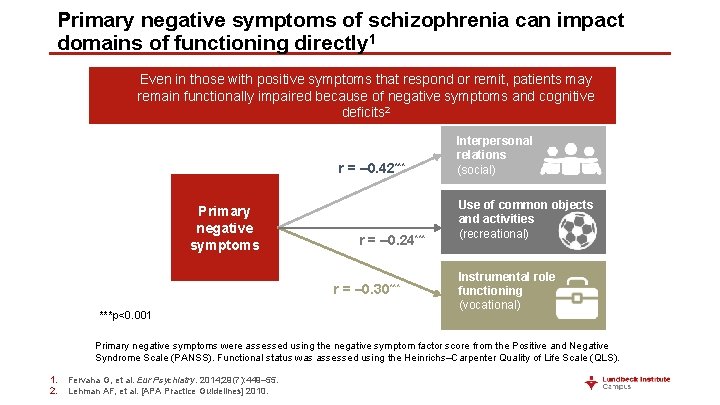
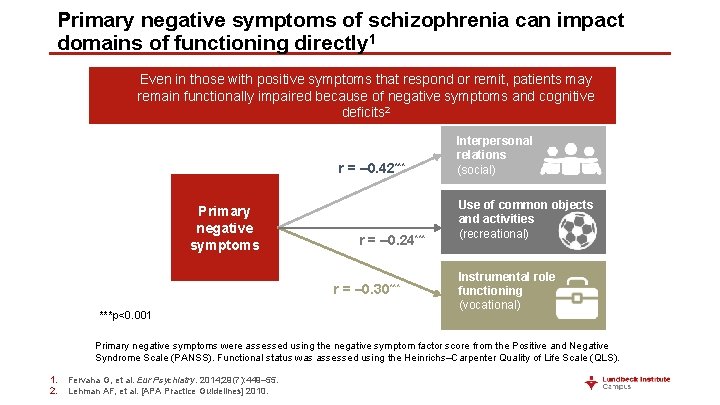
Primary negative symptoms of schizophrenia can impact domains of functioning directly 1 Even in those with positive symptoms that respond or remit, patients may remain functionally impaired because of negative symptoms and cognitive deficits 2 r = – 0. 42*** Primary negative symptoms r = – 0. 24*** r = – 0. 30*** ***p<0. 001 Interpersonal relations (social) Use of common objects and activities (recreational) Instrumental role functioning (vocational) Primary negative symptoms were assessed using the negative symptom factor score from the Positive and Negative Syndrome Scale (PANSS). Functional status was assessed using the Heinrichs–Carpenter Quality of Life Scale (QLS). 1. 2. Fervaha G, et al. Eur Psychiatry. 2014; 29(7): 449– 55. Lehman AF, et al. [APA Practice Guidelines] 2010.
Take home points • Functioning is complex and multifactorial, and a variety of factors contribute to functional impairment in patients with schizophrenia • Symptoms that are not fully controlled are significantly associated with impaired global functioning • Current treatment guidelines include optimizing functioning and quality of life as important treatment goals

Prognosis 13
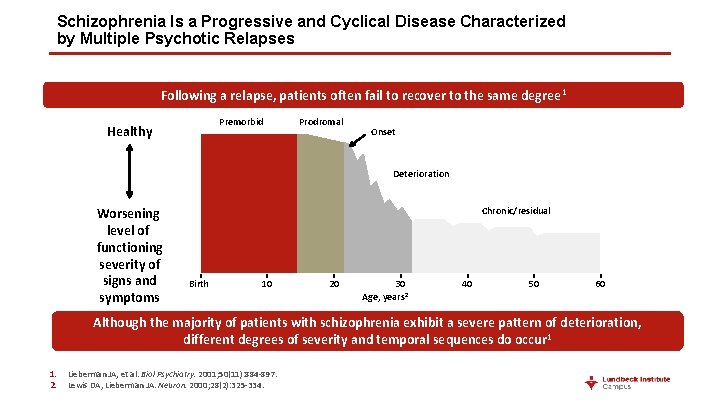
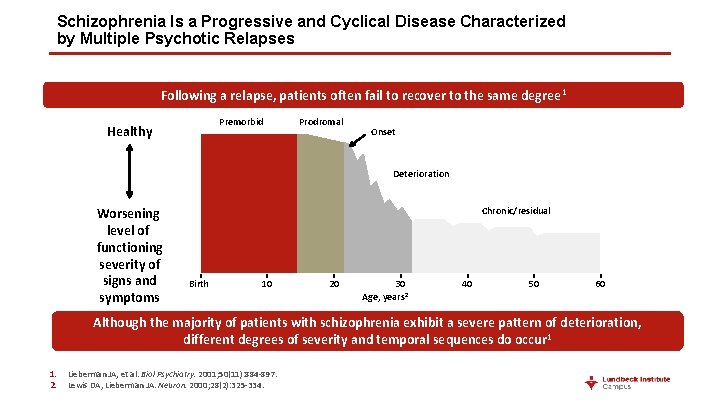
Schizophrenia Is a Progressive and Cyclical Disease Characterized by Multiple Psychotic Relapses Following a relapse, patients often fail to recover to the same degree 1 Premorbid Healthy Prodromal Onset Deterioration Worsening level of functioning severity of signs and symptoms Chronic/residual Birth 10 20 30 Age, years 2 40 50 60 Although the majority of patients with schizophrenia exhibit a severe pattern of deterioration, different degrees of severity and temporal sequences do occur 1 1. 2. Lieberman JA, et al. Biol Psychiatry. 2001; 50(11): 884 -897. Lewis DA, Lieberman JA. Neuron. 2000; 28(2): 325 -334.
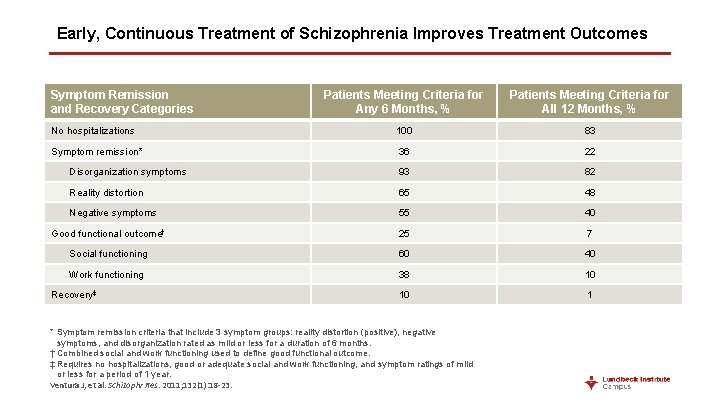
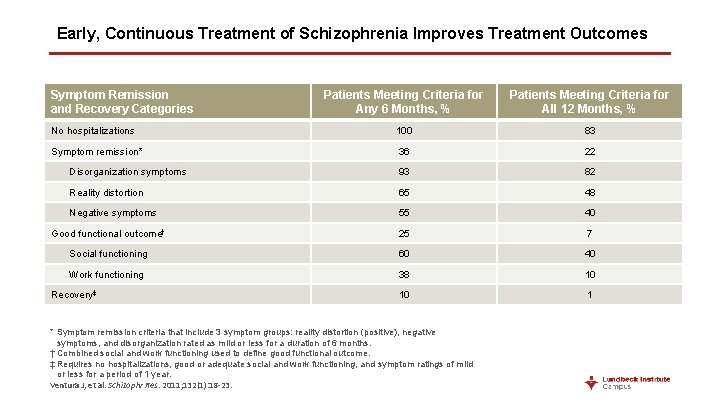
Early, Continuous Treatment of Schizophrenia Improves Treatment Outcomes Symptom Remission and Recovery Categories Patients Meeting Criteria for Any 6 Months, % Patients Meeting Criteria for All 12 Months, % No hospitalizations 100 83 Symptom remission* 36 22 Disorganization symptoms 93 82 Reality distortion 65 48 Negative symptoms 55 40 Good functional outcome† 25 7 Social functioning 60 40 Work functioning 38 10 10 1 Recovery‡ * Symptom remission criteria that include 3 symptom groups: reality distortion (positive), negative symptoms, and disorganization rated as mild or less for a duration of 6 months. † Combined social and work functioning used to define good functional outcome. ‡ Requires no hospitalizations, good or adequate social and work functioning, and symptom ratings of mild or less for a period of 1 year. Ventura J, et al. Schizophr Res. 2011; 132(1): 18 -23.
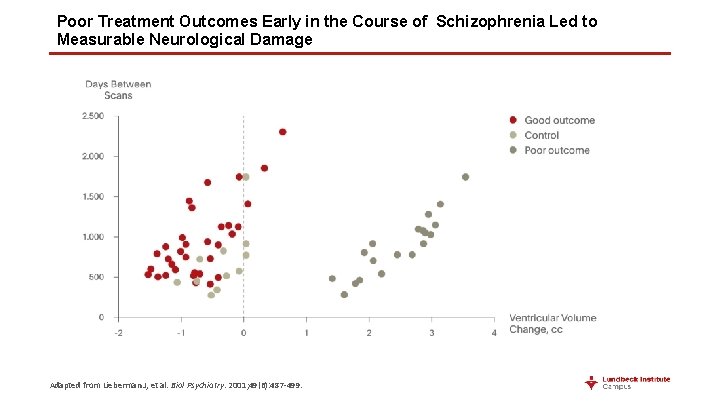
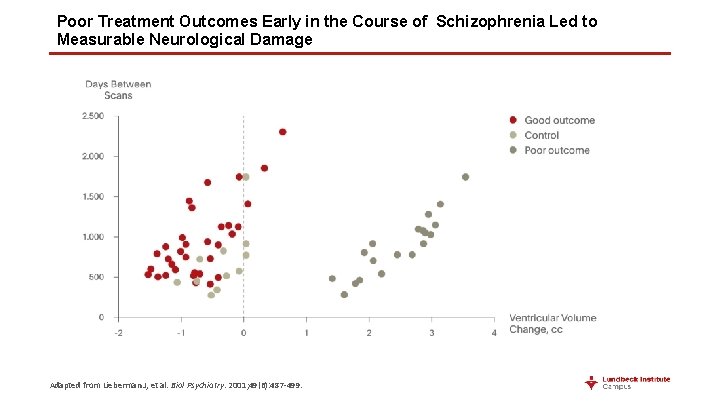
Poor Treatment Outcomes Early in the Course of Schizophrenia Led to Measurable Neurological Damage Adapted from Lieberman J, et al. Biol Psychiatry. 2001; 49(6): 487 -499.
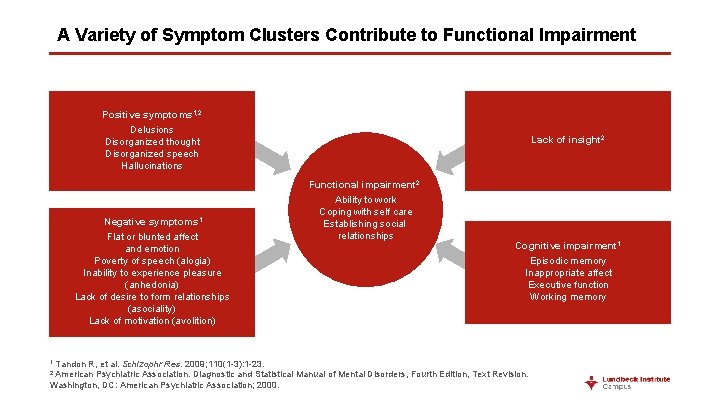
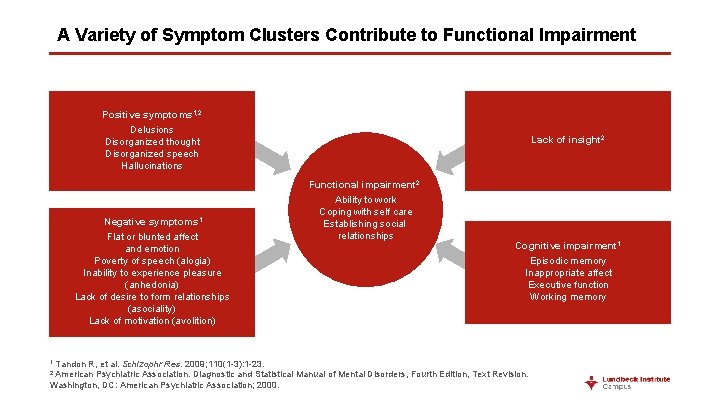
A Variety of Symptom Clusters Contribute to Functional Impairment Positive symptoms 1, 2 Delusions Disorganized thought Disorganized speech Hallucinations Lack of insight 2 Functional impairment 2 Negative symptoms 1 Flat or blunted affect and emotion Poverty of speech (alogia) Inability to experience pleasure (anhedonia) Lack of desire to form relationships (asociality) Lack of motivation (avolition) 1 Tandon R, et al. Schizophr Ability to work Coping with self care Establishing social relationships Cognitive impairment 1 Episodic memory Inappropriate affect Executive function Working memory Res. 2009; 110(1 -3): 1 -23. 2 American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000.
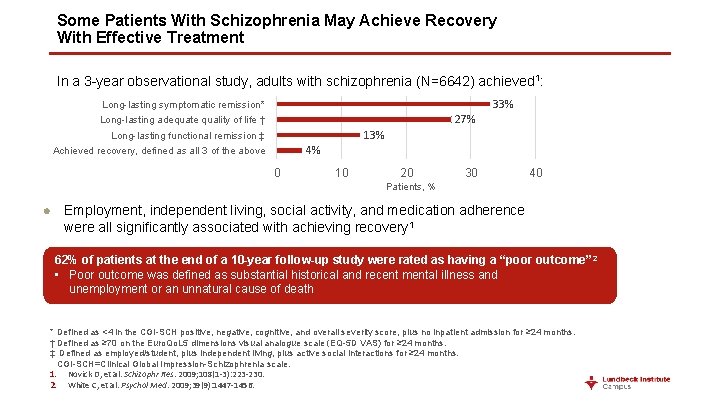
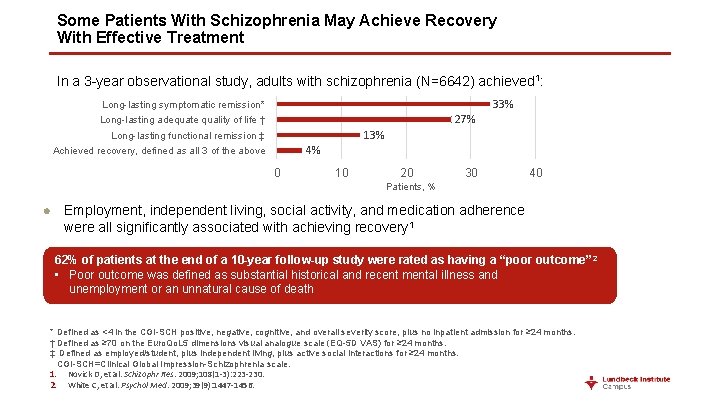
Some Patients With Schizophrenia May Achieve Recovery With Effective Treatment In a 3 -year observational study, adults with schizophrenia (N=6642) achieved 1: 33% Long-lasting symptomatic remission* 27% Long-lasting adequate quality of life † 13% Long-lasting functional remission ‡ 4% Achieved recovery, defined as all 3 of the above 0 10 20 30 40 Patients, % Employment, independent living, social activity, and medication adherence were all significantly associated with achieving recovery 1 62% of patients at the end of a 10 -year follow-up study were rated as having a “poor outcome” 2 • Poor outcome was defined as substantial historical and recent mental illness and unemployment or an unnatural cause of death * Defined as <4 in the CGI-SCH positive, negative, cognitive, and overall severity score, plus no inpatient admission for ≥ 24 months. † Defined as ≥ 70 on the Euro. Qo. L 5 dimensions visual analogue scale (EQ-5 D VAS) for ≥ 24 months. ‡ Defined as employed/student, plus independent living, plus active social interactions for ≥ 24 months. CGI-SCH=Clinical Global Impression-Schizophrenia scale. 1. Novick D, et al. Schizophr Res. 2009; 108(1 -3): 223 -230. 2. White C, et al. Psychol Med. 2009; 39(9): 1447 -1456.
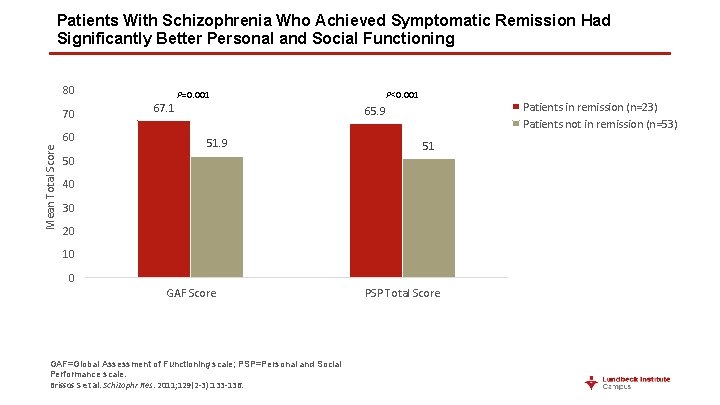
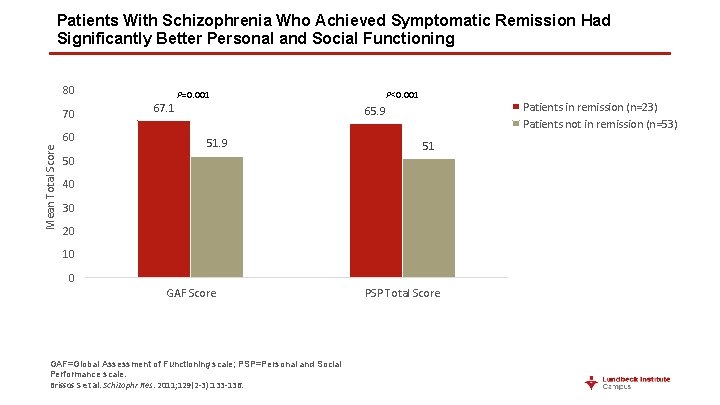
Patients With Schizophrenia Who Achieved Symptomatic Remission Had Significantly Better Personal and Social Functioning 80 70 Mean Total Score 60 67. 1 P=0. 001 P<0. 001 Patients in remission (n=23) Patients not in remission (n=53) 65. 9 51 50 40 30 20 10 0 GAF Score GAF=Global Assessment of Functioning scale; PSP=Personal and Social Performance scale. Brissos S et al. Schizophr Res. 2011; 129(2 -3): 133 -136. PSP Total Score
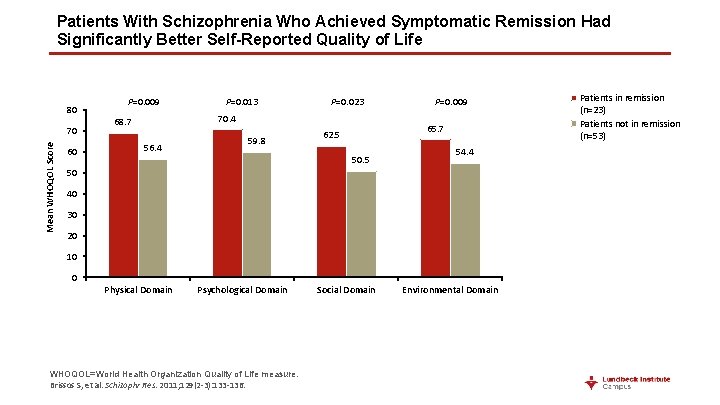
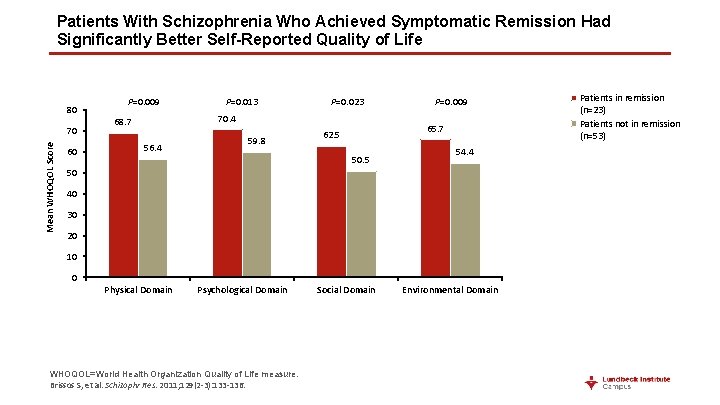
Patients With Schizophrenia Who Achieved Symptomatic Remission Had Significantly Better Self-Reported Quality of Life 80 Mean WHOQOL Score 70 60 P=0. 009 P=0. 013 P=0. 023 70. 4 68. 7 56. 4 59. 8 P=0. 009 65. 7 62. 5 50. 5 54. 4 50 40 30 20 10 0 Physical Domain Psychological Domain WHOQOL=World Health Organization Quality of Life measure. Brissos S, et al. Schizophr Res. 2011; 129(2 -3): 133 -136. Social Domain Environmental Domain Patients in remission (n=23) Patients not in remission (n=53)

Symptomatic Remission in Schizophrenia Led to Significantly Better Insight and Fewer Depressive Symptoms Patients in remission (n=23) Patients not in remission (n=53) P=0. 003 Mean PANSS™ Item G 12 Score (Insight) 3. 0 2. 5 2. 0 1. 5 1. 0 2. 0 3. 0 Mean PANSS™ Item G 6 Score (Depression) 3. 5 0 PANSS™=Positive and Negative Syndrome Scale; a trademark of Multi-Health Systems, Inc. Brissos S, et al. Schizophr Res. 2011; 129(2 -3): 133 -136. Patients in remission (n=23) Patients not in remission (n=53) 2. 5 P=0. 013 2. 0 1. 5 1. 0 0. 5 0 1. 0
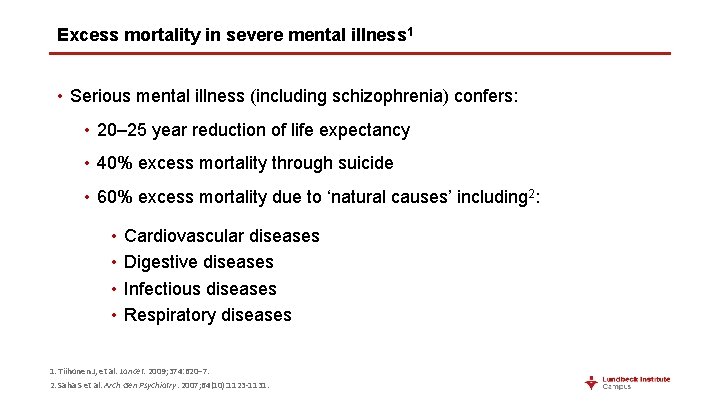
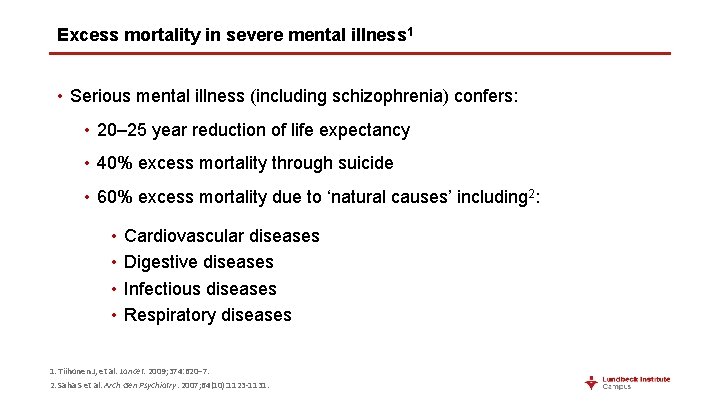
Excess mortality in severe mental illness 1 • Serious mental illness (including schizophrenia) confers: • 20– 25 year reduction of life expectancy • 40% excess mortality through suicide • 60% excess mortality due to ‘natural causes’ including 2: • • Cardiovascular diseases Digestive diseases Infectious diseases Respiratory diseases 1. Tiihonen J, et al. Lancet. 2009; 374: 620– 7. 2. Saha S et al. Arch Gen Psychiatry. 2007; 64(10): 1123 -1131.
Relapse
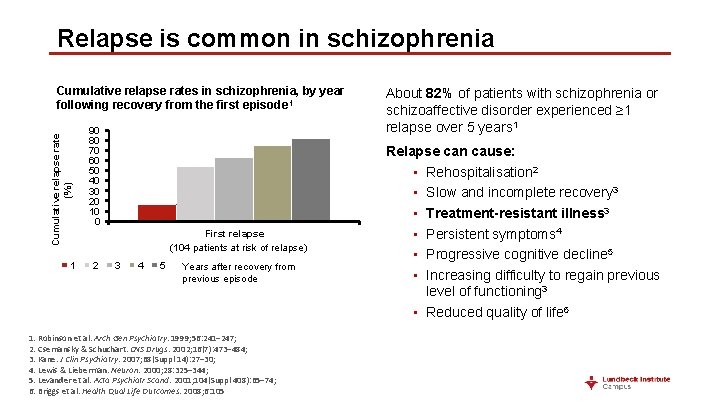
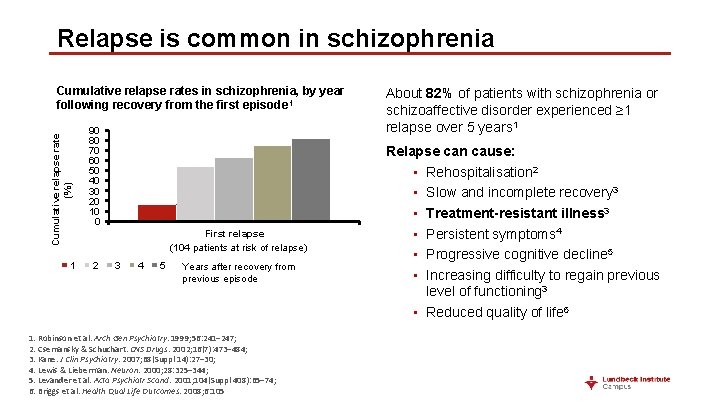
Relapse is common in schizophrenia Cumulative relapse rate (%) Cumulative relapse rates in schizophrenia, by year following recovery from the first episode 1 1 90 80 70 60 50 40 30 20 10 0 First relapse (104 patients at risk of relapse) 2 3 4 5 Years after recovery from previous episode 1. Robinson et al. Arch Gen Psychiatry. 1999; 56: 241– 247; 2. Csernansky & Schuchart. CNS Drugs. 2002; 16(7): 473– 484; 3. Kane. J Clin Psychiatry. 2007; 68(Suppl 14): 27– 30; 4. Lewis & Lieberman. Neuron. 2000; 28: 325– 344; 5. Levander et al. Acta Psychiatr Scand. 2001; 104(Suppl 408): 65– 74; 6. Briggs et al. Health Qual Life Outcomes. 2008; 6: 105 About 82% of patients with schizophrenia or schizoaffective disorder experienced ≥ 1 relapse over 5 years 1 Relapse can cause: • Rehospitalisation 2 • Slow and incomplete recovery 3 • Treatment-resistant illness 3 • Persistent symptoms 4 • Progressive cognitive decline 5 • Increasing difficulty to regain previous level of functioning 3 • Reduced quality of life 6
Multiple factors increase the risk of relapse • The risk of relapse following treatment for first-episode psychosis was significantly increased by: 1, 2 • Non-adherence to medication • Treatment resistance • Persistent substance use • Carers’ criticism • Poorer pre-morbid adjustment Improving medication adherence, and relapse prevention, are key components of the management of schizophrenia 1, 3 Findings from a systematic review and meta-analysis of 29 longitudinal studies 1, 2 1. Emsley et al. BMC Psychiatry 2013; 13: 50; 2. Alvarez-Jimenez et al. Schizophr Res 2012; 139(1– 3): 116– 128; 3. Kane. J Clin Psychiatry 2007; 68(Suppl 14): 27– 30
Relapses, characterized by acute psychotic exacerbation, can have a negative impact on psychosocial functioning In addition to the risk of self-harm and harm to others, relapse may have serious psychosocial implications: Cause distress to patients and families Jeopardize friendships and relationships Disrupt education or employment Diminish personal autonomy Contribute to stigma Add to the economic burden of treating schizophrenia x Emsley R, et al. Schizophr Res. 2013; 148(1– 3): 117– 121.
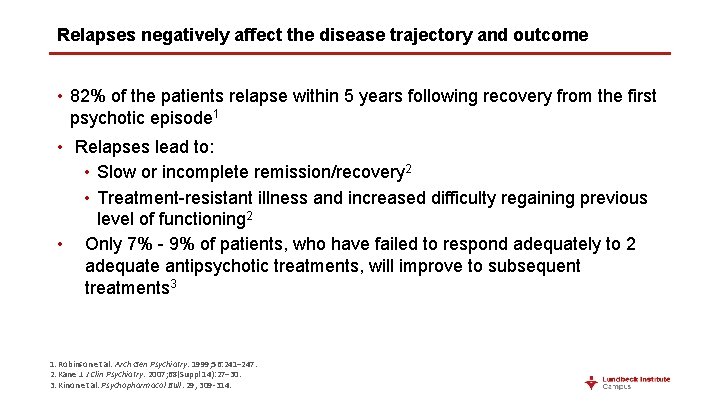
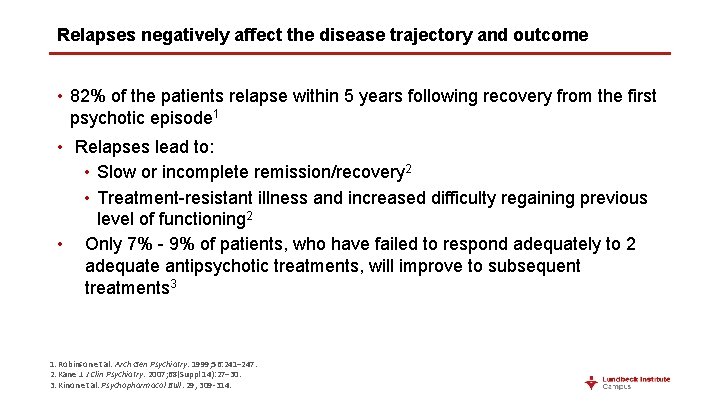
Relapses negatively affect the disease trajectory and outcome • 82% of the patients relapse within 5 years following recovery from the first psychotic episode 1 • Relapses lead to: • Slow or incomplete remission/recovery 2 • Treatment-resistant illness and increased difficulty regaining previous level of functioning 2 • Only 7% - 9% of patients, who have failed to respond adequately to 2 adequate antipsychotic treatments, will improve to subsequent treatments 3 1. Robinson et al. Arch Gen Psychiatry. 1999; 56: 241– 247. 2. Kane J. J Clin Psychiatry. 2007; 68(Suppl 14): 27– 30. 3. Kinon et al. Psychopharmacol Bull. 29, 309 -314.
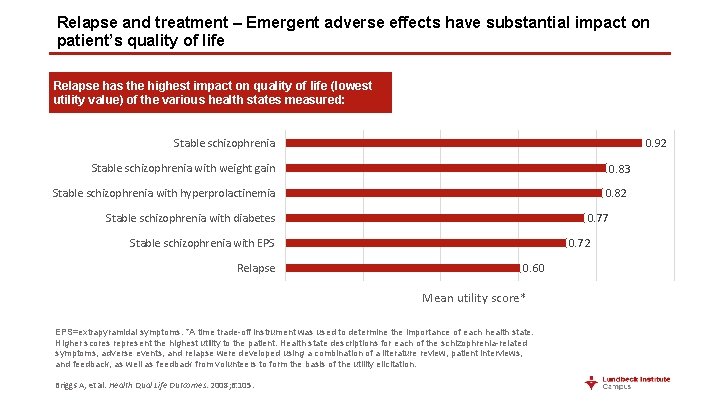
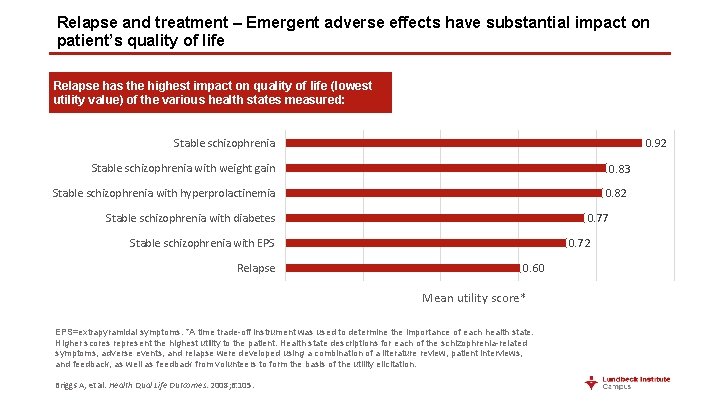
Relapse and treatment – Emergent adverse effects have substantial impact on patient’s quality of life Relapse has the highest impact on quality of life (lowest utility value) of the various health states measured: 0. 92 Stable schizophrenia with weight gain 0. 83 0. 82 Stable schizophrenia with hyperprolactinemia 0. 77 Stable schizophrenia with diabetes 0. 72 Stable schizophrenia with EPS Relapse 0. 60 Mean utility score* EPS=extrapyramidal symptoms. *A time trade-off instrument was used to determine the importance of each health state. Higher scores represent the highest utility to the patient. Health state descriptions for each of the schizophrenia-related symptoms, adverse events, and relapse were developed using a combination of a literature review, patient interviews, and feedback, as well as feedback from volunteers to form the basis of the utility elicitation. Briggs A, et al. Health Qual Life Outcomes. 2008; 6: 105.
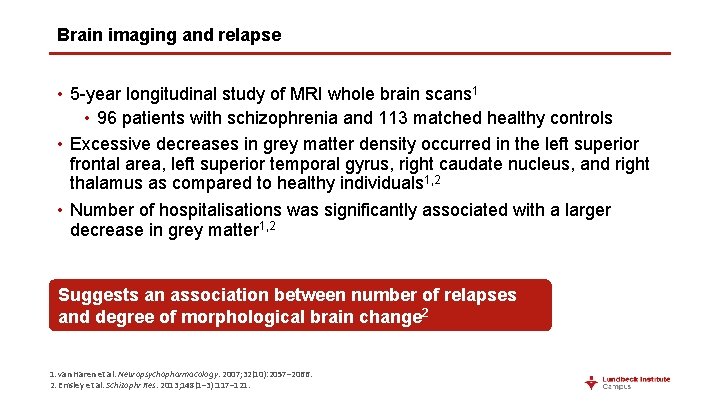
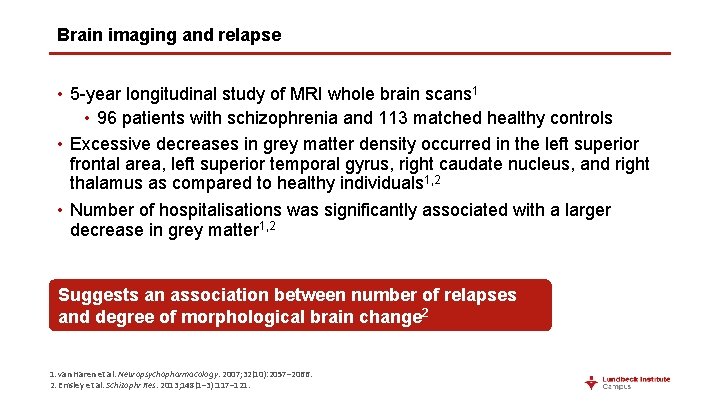
Brain imaging and relapse • 5 -year longitudinal study of MRI whole brain scans 1 • 96 patients with schizophrenia and 113 matched healthy controls • Excessive decreases in grey matter density occurred in the left superior frontal area, left superior temporal gyrus, right caudate nucleus, and right thalamus as compared to healthy individuals 1, 2 • Number of hospitalisations was significantly associated with a larger decrease in grey matter 1, 2 Suggests an association between number of relapses and degree of morphological brain change 2 1. van Haren et al. Neuropsychopharmacology. 2007; 32(10): 2057– 2066. 2. Emsley et al. Schizophr Res. 2013; 148(1– 3): 117– 121.

Days to remission after each relapse 140 130 Days to remission 120 100 76. 5 80 60 47 40 20 0 First Lieberman J, et al. J Clin Psychiatry. 1996; 57: 5– 9. Second Third
Impact of Relapse on Patients With Schizophrenia
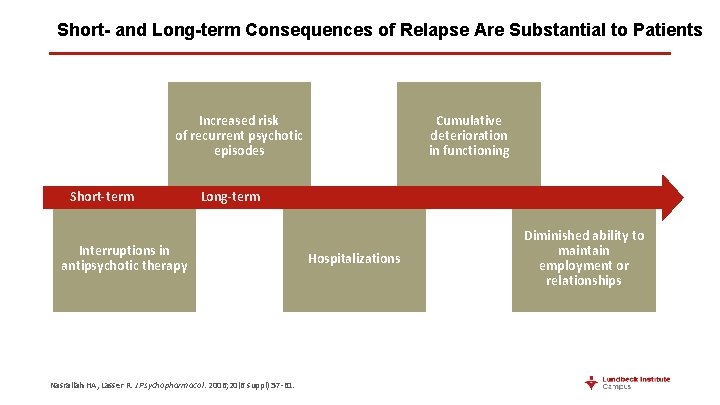
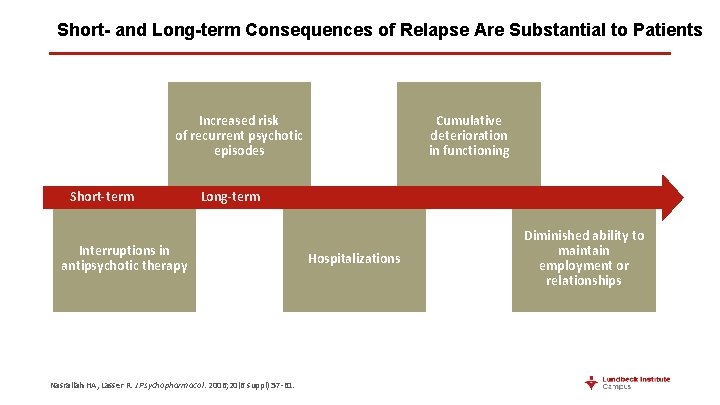
Short- and Long-term Consequences of Relapse Are Substantial to Patients Increased risk of recurrent psychotic episodes Short-term Cumulative deterioration in functioning Long-term Interruptions in antipsychotic therapy Nasrallah HA, Lasser R. J Psychopharmacol. 2006; 20(6 suppl): 57 -61. Hospitalizations Diminished ability to maintain employment or relationships
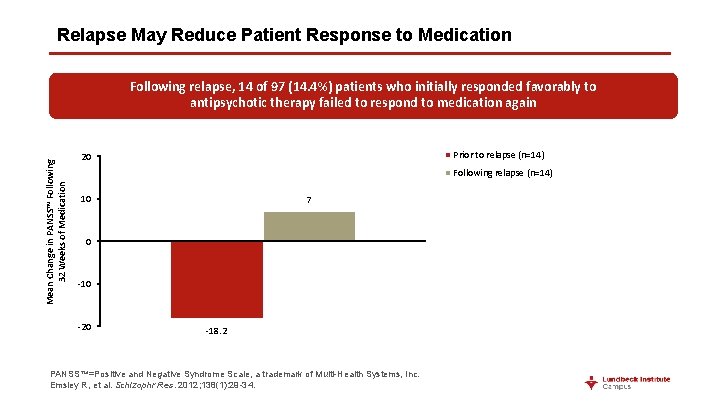
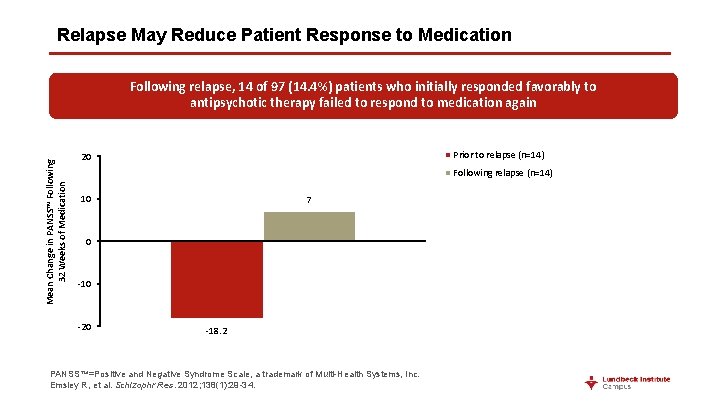
Relapse May Reduce Patient Response to Medication Mean Change in PANSS™ Following 32 Weeks of Medication Following relapse, 14 of 97 (14. 4%) patients who initially responded favorably to antipsychotic therapy failed to respond to medication again Prior to relapse (n=14) 20 Following relapse (n=14) 10 7 0 -10 -20 -18. 2 PANSS™=Positive and Negative Syndrome Scale, a trademark of Multi-Health Systems, Inc. Emsley R, et al. Schizophr Res. 2012; 138(1): 29 -34.
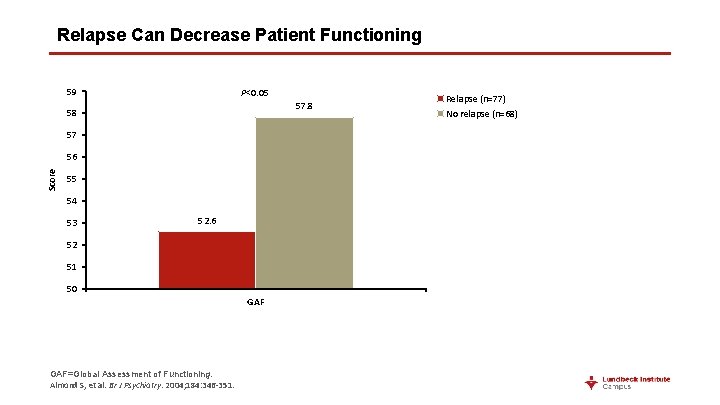
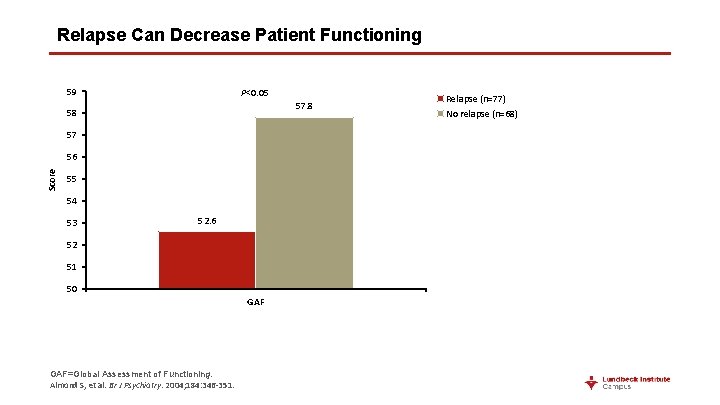
Relapse Can Decrease Patient Functioning 59 P<0. 05 57. 8 58 57 Score 56 55 54 53 52. 6 52 51 50 GAF=Global Assessment of Functioning. Almond S, et al. Br J Psychiatry. 2004; 184: 346 -351. Relapse (n=77) No relapse (n=68)

Impact of Early Intervention for Patients With Schizophrenia
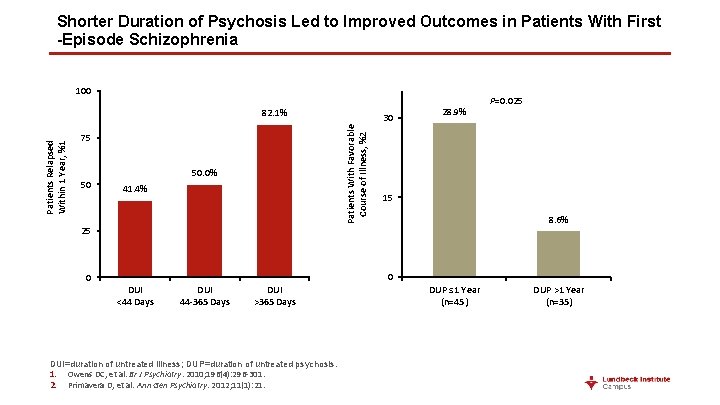
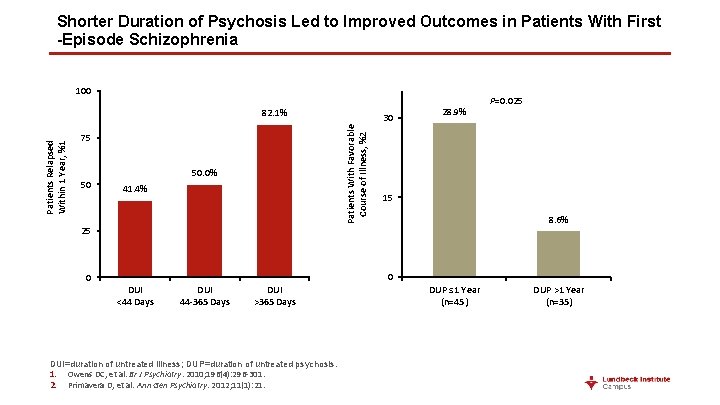
Shorter Duration of Psychosis Led to Improved Outcomes in Patients With First -Episode Schizophrenia 100 75 50 30 Patients With Favorable Course of Illness, %2 Patients Relapsed Within 1 Year, %1 82. 1% 50. 0% 41. 4% 28. 9% P=0. 025 15 8. 6% 25 0 0 DUI <44 Days DUI 44 -365 Days DUI >365 Days DUI=duration of untreated illness; DUP=duration of untreated psychosis. 1. Owens DC, et al. Br J Psychiatry. 2010; 196(4): 296 -301. 2. Primavera D, et al. Ann Gen Psychiatry. 2012; 11(1): 21. DUP ≤ 1 Year (n=45) DUP >1 Year (n=35)
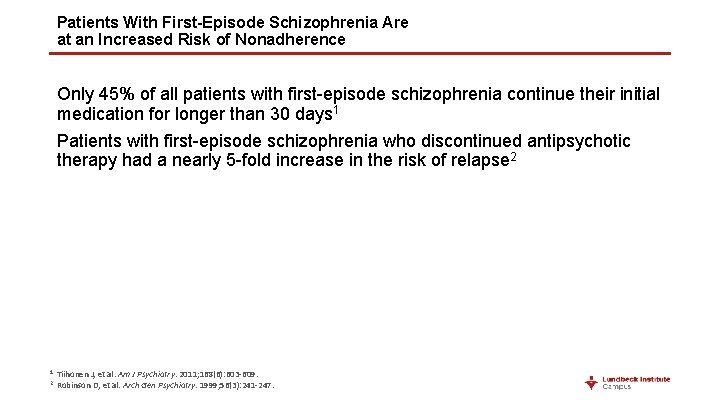
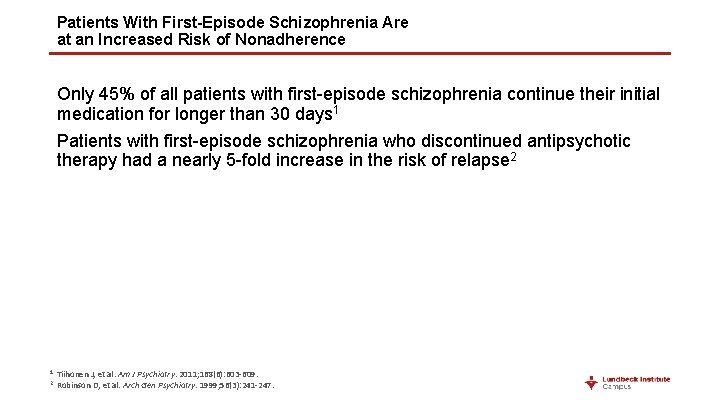
Patients With First-Episode Schizophrenia Are at an Increased Risk of Nonadherence Only 45% of all patients with first-episode schizophrenia continue their initial medication for longer than 30 days 1 Patients with first-episode schizophrenia who discontinued antipsychotic therapy had a nearly 5 -fold increase in the risk of relapse 2 1 2 Tiihonen J, et al. Am J Psychiatry. 2011; 168(6): 603 -609. Robinson D, et al. Arch Gen Psychiatry. 1999; 56(3): 241 -247.

Continuous Maintenance Treatment Led to Decreased Deterioration in Symptoms During the Second Year Following Diagnosis * Increase from baseline in the sum of PANSS™ positive and negative scores ≥ 25% or ≥ 10 points (if baseline value ≤ 40) or a CGI-C score ≥ 6. CGI-C=Clinical Global Impression-Change scale; PANSS™=Positive and Negative Syndrome Scale, a trademark of Multi-Health Systems, Inc. ; Gaebel W, et al. J Clin Psychiatry. 2011; 72(2): 205 -218.
Supportive Relationships Can Improve Long-term Adherence and Reduce Relapse Risk in Patients With Schizophrenia
Family Involvement and Better Patient Insight May Improve Patient Adherence • Patients with early-episode schizophrenia who were significantly more adherent 6 months after hospital discharge: • Were more aware of their illness and need for medication • Had more positive perceptions of doctor–patient trust in therapeutic alliance • Had better perceived family involvement in treatment and had more positive family attitudes toward medication • Had more positive attitudes toward medication Baloush-Kleinman V et al. Schizophr Res. 2011; 130(1 -3): 176 -181.
Instrumental Family Support* Predicts Higher Medication Usage in Patients With Schizophrenia • A logistic regression analysis was conducted to assess if family factors, including the independent dimensions of expressed emotion (EE) and family support variables, would predict usage of psychiatric medications • Higher levels of instrumental family support were associated with greater likelihood of medication usage • Only family instrumental support significantly predicted medication usage (odds ratio = 4. 8, P=0. 05) * Instrumental support was operationalized as the total number of statements that illustrated family caregiver ‘‘task-oriented’’ assistance, such as completion of errands; e. g. , ‘‘I helped him fill out an employment application. ’’ Ramírez García JI, et al. Soc Psychiatry Psychiatr Epidemiol. 2006; 41(8): 624 -631.
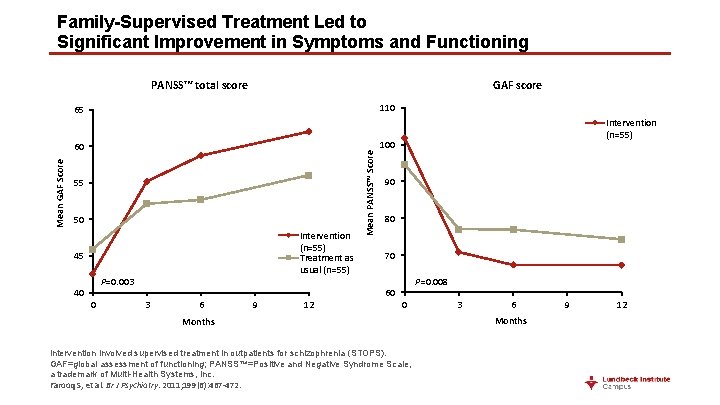
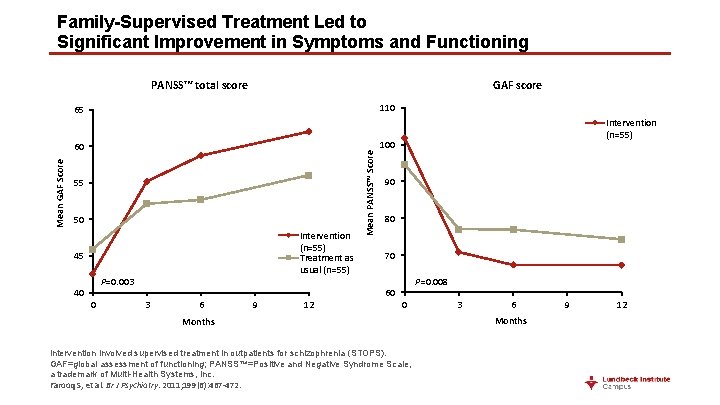
Family-Supervised Treatment Led to Significant Improvement in Symptoms and Functioning PANSS™ total score GAF score 110 Mean GAF Score 60 55 50 Intervention (n=55) Treatment as usual (n=55) 45 P=0. 003 40 0 Mean PANSS™ Score 65 Intervention (n=55) 100 90 80 70 P=0. 008 60 3 6 9 12 0 Months Intervention involved supervised treatment in outpatients for schizophrenia (STOPS). GAF=global assessment of functioning; PANSS™=Positive and Negative Syndrome Scale, a trademark of Multi-Health Systems, Inc. Farooq S, et al. Br J Psychiatry. 2011; 199(6): 467 -472. 3 6 Months 9 12
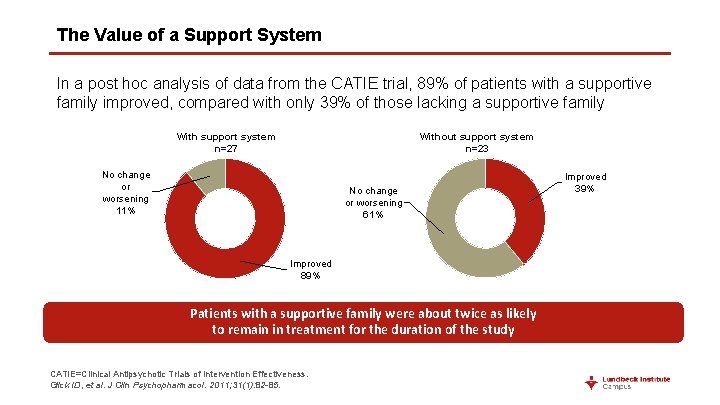
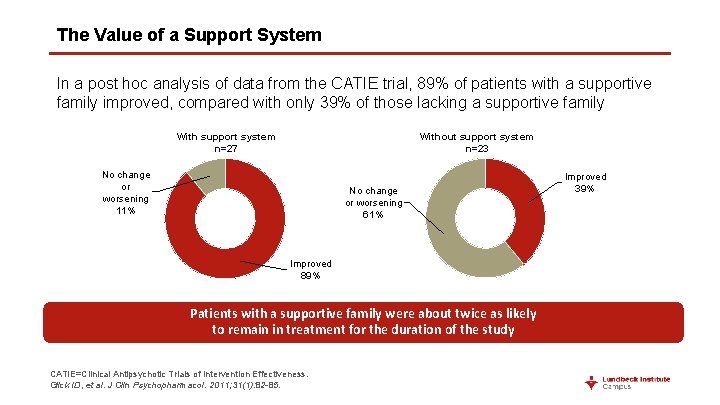
The Value of a Support System In a post hoc analysis of data from the CATIE trial, 89% of patients with a supportive family improved, compared with only 39% of those lacking a supportive family With support system n=27 Without support system n=23 No change or worsening 11% No change or worsening 61% Improved 89% Patients with a supportive family were about twice as likely to remain in treatment for the duration of the study CATIE=Clinical Antipsychotic Trials of Intervention Effectiveness. Glick ID, et al. J Clin Psychopharmacol. 2011; 31(1): 82 -85. Improved 39%
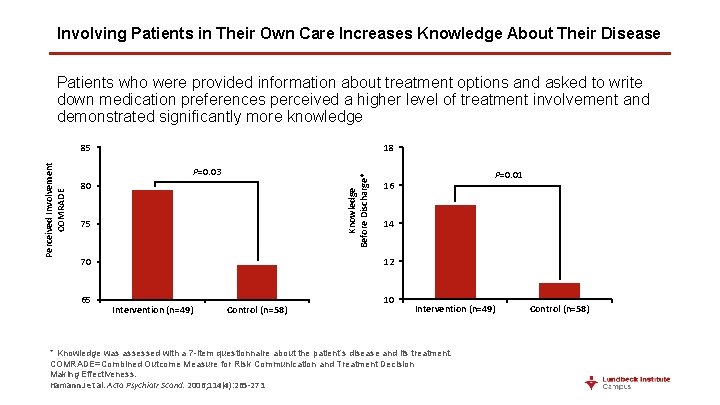
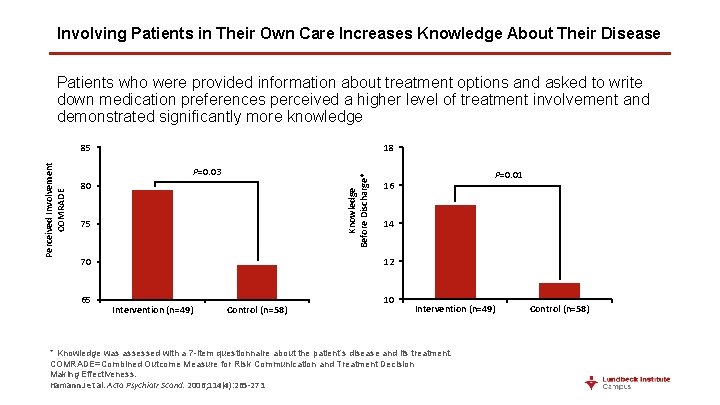
Involving Patients in Their Own Care Increases Knowledge About Their Disease Patients who were provided information about treatment options and asked to write down medication preferences perceived a higher level of treatment involvement and demonstrated significantly more knowledge 18 P=0. 03 Knowledge Before Discharge* Perceived Involvement COMRADE 85 80 75 14 12 70 65 P=0. 01 16 Intervention (n=49) Control (n=58) 10 Intervention (n=49) * Knowledge was assessed with a 7 -item questionnaire about the patient’s disease and its treatment. COMRADE=Combined Outcome Measure for Risk Communication and Treatment Decision Making Effectiveness. Hamann J et al. Acta Psychiatr Scand. 2006; 114(4): 265 -273. Control (n=58)

Simple Techniques Improve the Communication Between Patients and Clinicians 1. 5 300 250 Mean Number of Clinician Statements of Empathy Mean Number of Patient Statements Contributing to Dialogue P<0. 05 200 150 100 50 P<0. 03 1 0. 5 0 0 Intervention (n=24) Control (n=26) Steinwachs DM et al. Psychiatr Serv. 2011; 62(11): 1296 -1302. Intervention (n=24) Control (n=26)
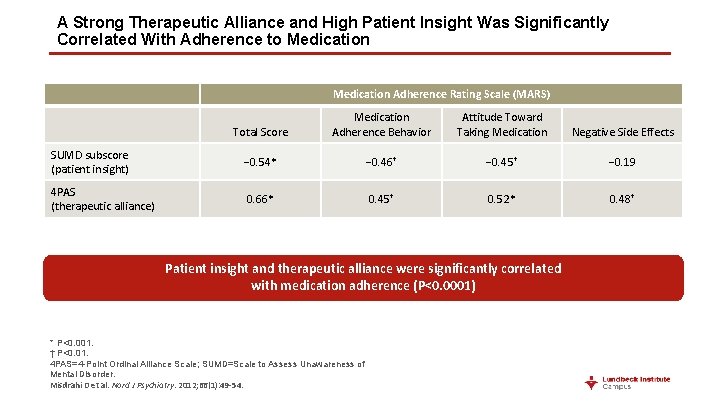
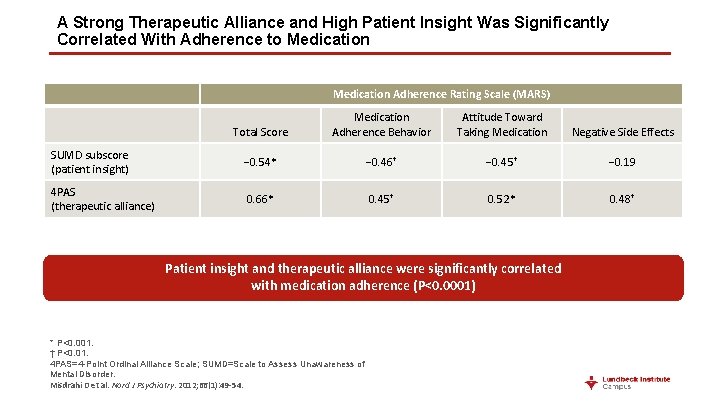
A Strong Therapeutic Alliance and High Patient Insight Was Significantly Correlated With Adherence to Medication Adherence Rating Scale (MARS) Total Score Medication Adherence Behavior Attitude Toward Taking Medication Negative Side Effects SUMD subscore (patient insight) − 0. 54* − 0. 46† − 0. 45† − 0. 19 4 PAS (therapeutic alliance) 0. 66* 0. 45† 0. 52* 0. 48† Patient insight and therapeutic alliance were significantly correlated with medication adherence (P<0. 0001) * P<0. 001. † P<0. 01. 4 PAS=4 -Point Ordinal Alliance Scale; SUMD=Scale to Assess Unawareness of Mental Disorder. Misdrahi D et al. Nord J Psychiatry. 2012; 66(1): 49 -54.
High Prevalence of Nonadherence to Medication Among Patients With Schizophrenia
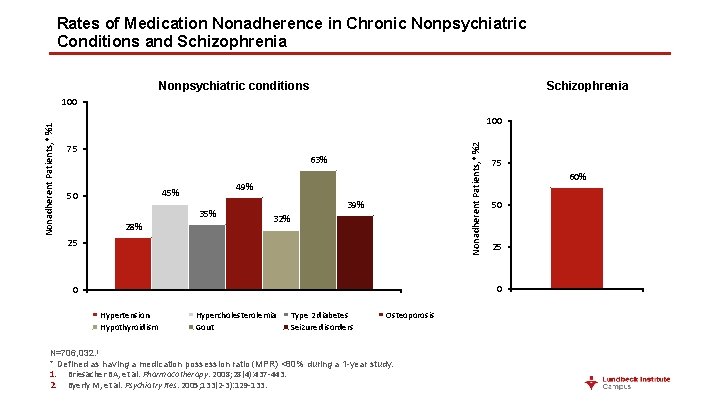
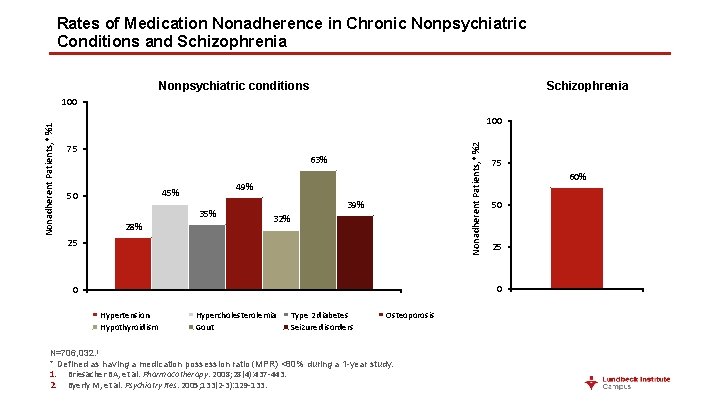
Rates of Medication Nonadherence in Chronic Nonpsychiatric Conditions and Schizophrenia Nonpsychiatric conditions Schizophrenia 100 75 Nonadherent Patients, * %2 Nonadherent Patients, * %1 100 63% 49% 45% 50 35% 28% 39% 32% 25 75 60% 50 25 0 0 Hypertension Hypothyroidism Hypercholesterolemia Gout Type 2 diabetes Seizure disorders Osteoporosis N=706, 032. 1 * Defined as having a medication possession ratio (MPR) <80% during a 1 -year study. 1. Briesacher BA, et al. Pharmacotherapy. 2008; 28(4): 437 -443. 2. Byerly M, et al. Psychiatry Res. 2005; 133(2 -3): 129 -133.

Few Patients With Schizophrenia Take Their Medication as Prescribed 24% Nonadherent 41% Partially adherent Excess fillers 16% Adherent 19% MPR=medication possession ratio. Gilmer TP et al. Am J Psychiatry. 2004; 161(4): 692 -699.

Clinicians Overestimated Patient Adherence to Medication 100 90 80 70 60 50 40 30 20 10 0 Nonadherent Adherent 84% Patients, % Adherent 52% ≤ 6 ≤ 5 0% 0% ≤ 4 ≤ 3 ≤ 2 ≤ 1 Clinician Rating Scale Score (Measure of Adherence) MEMS=medication event monitoring system. Byerly M et al. Psychiatry Res. 2005; 133(2 -3): 129 -133. 100 90 80 70 60 50 40 30 20 10 0 Nonadherent 72% 60% 48% 20% <90% <80% <70% <50% 12% <30% Actual Daily Adherence Based on MEMS 4% <10%
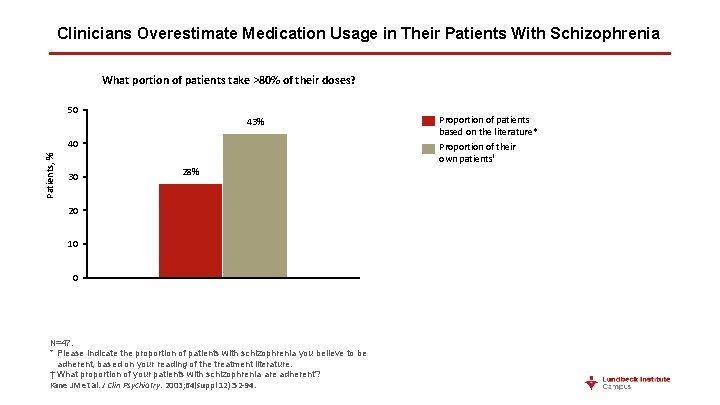
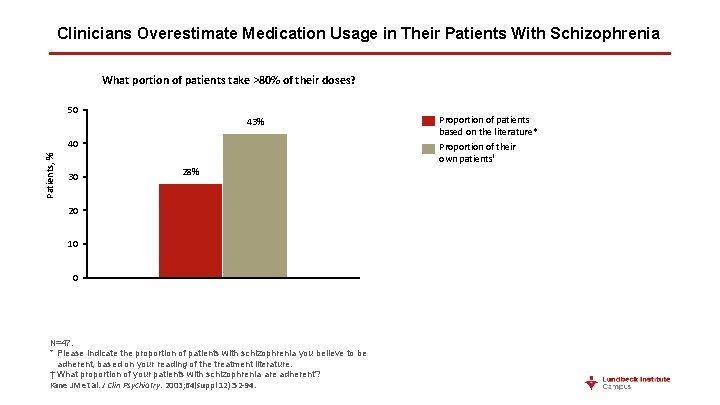
Clinicians Overestimate Medication Usage in Their Patients With Schizophrenia What portion of patients take >80% of their doses? 50 43% Patients, % 40 30 28% 20 10 0 N=47. * Please indicate the proportion of patients with schizophrenia you believe to be adherent, based on your reading of the treatment literature. † What proportion of your patients with schizophrenia are adherent? Kane JM et al. J Clin Psychiatry. 2003; 64(suppl 12): 52 -94. Proportion of patients based on the literature* Proportion of their own patients†
Risk Factors for Nonadherence in Patients With Schizophrenia
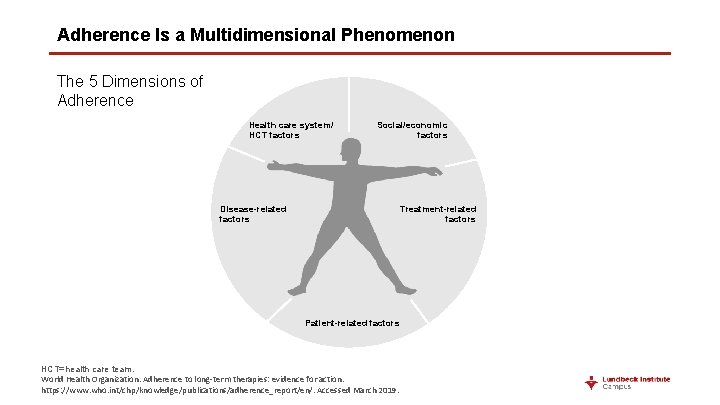
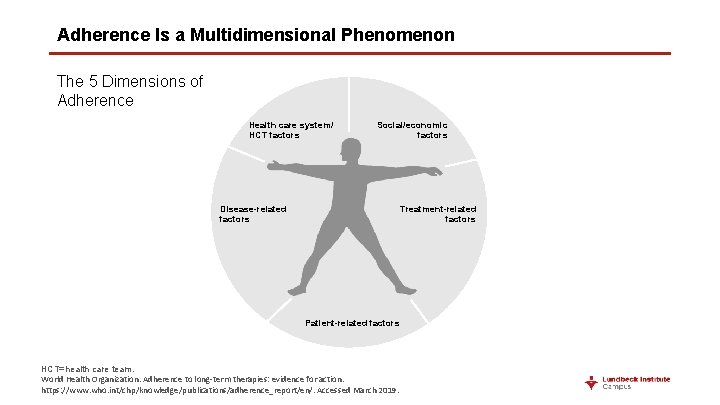
Adherence Is a Multidimensional Phenomenon The 5 Dimensions of Adherence Health care system/ HCT factors Social/economic factors Disease-related factors Treatment-related factors Patient-related factors HCT=health care team. World Health Organization. Adherence to long-term therapies: evidence for action. https: //www. who. int/chp/knowledge/publications/adherence_report/en/. Accessed March 2019.
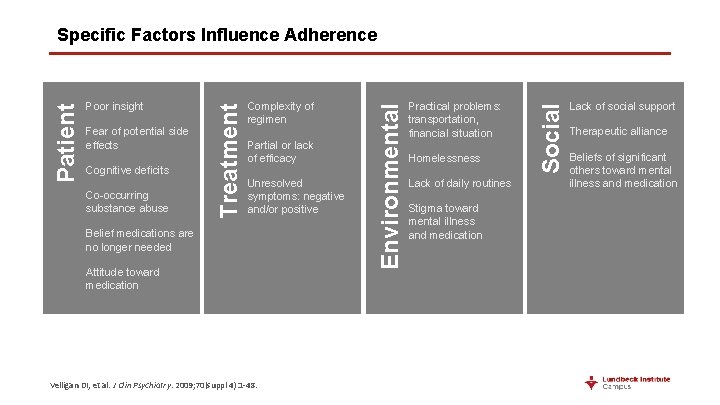
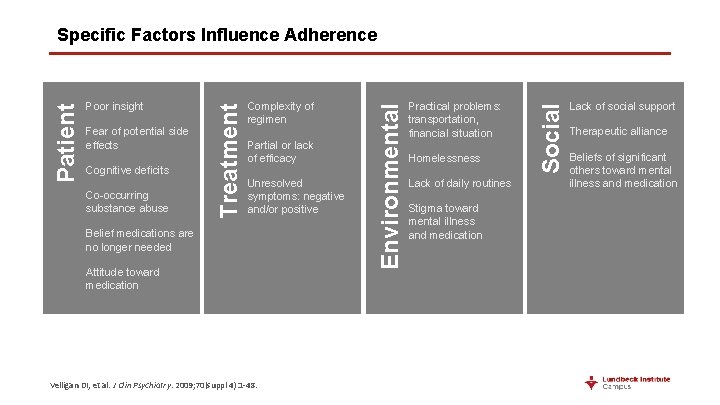
Cognitive deficits Co-occurring substance abuse Partial or lack of efficacy Unresolved symptoms: negative and/or positive Belief medications are no longer needed Attitude toward medication Velligan DI, et al. J Clin Psychiatry. 2009; 70(suppl 4): 1 -48. Practical problems: transportation, financial situation Homelessness Lack of daily routines Stigma toward mental illness and medication Social Fear of potential side effects Complexity of regimen Environmental Poor insight Treatment Patient Specific Factors Influence Adherence Lack of social support Therapeutic alliance Beliefs of significant others toward mental illness and medication
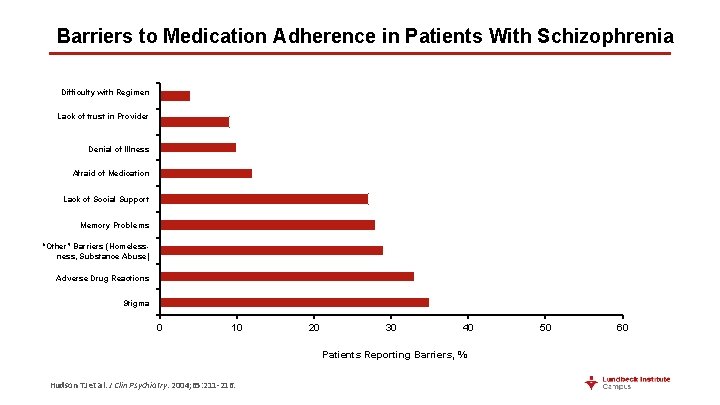
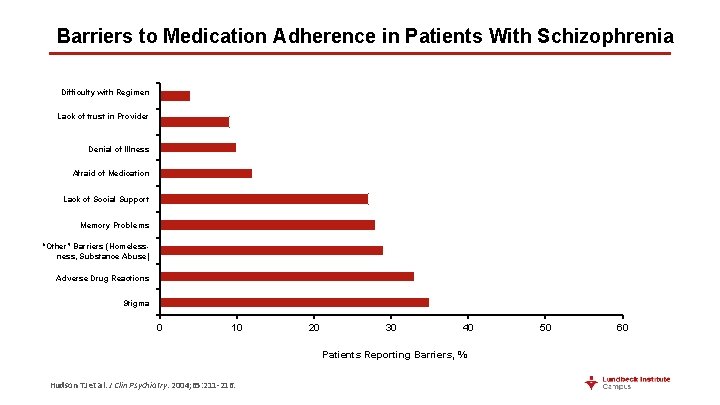
Barriers to Medication Adherence in Patients With Schizophrenia Difficulty with Regimen Lack of trust in Provider Denial of Illness Afraid of Medication Lack of Social Support Memory Problems “Other” Barriers (Homelessness, Substance Abuse) Adverse Drug Reactions Stigma 0 10 20 30 40 Patients Reporting Barriers, % Hudson TJ et al. J Clin Psychiatry. 2004; 65: 211 -216. 50 60
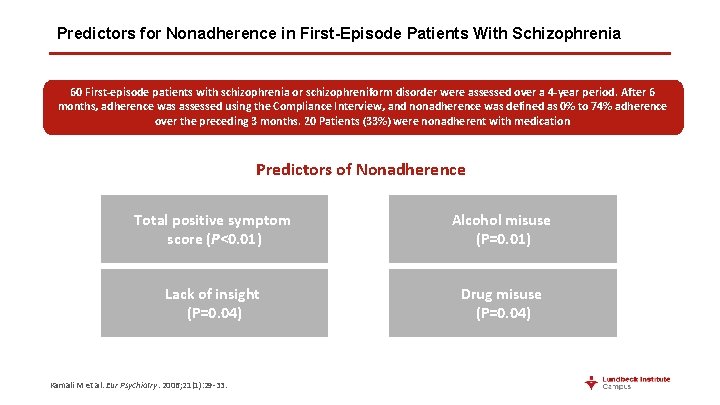
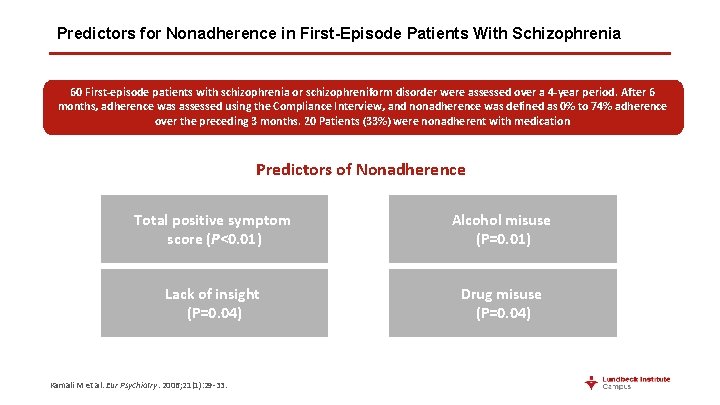
Predictors for Nonadherence in First-Episode Patients With Schizophrenia 60 First-episode patients with schizophrenia or schizophreniform disorder were assessed over a 4 -year period. After 6 months, adherence was assessed using the Compliance Interview, and nonadherence was defined as 0% to 74% adherence over the preceding 3 months. 20 Patients (33%) were nonadherent with medication Predictors of Nonadherence Total positive symptom score (P<0. 01) Alcohol misuse (P=0. 01) Lack of insight (P=0. 04) Drug misuse (P=0. 04) Kamali M et al. Eur Psychiatry. 2006; 21(1): 29 -33.
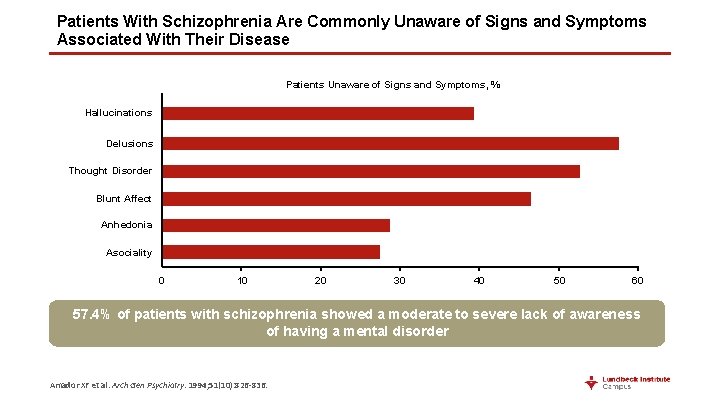
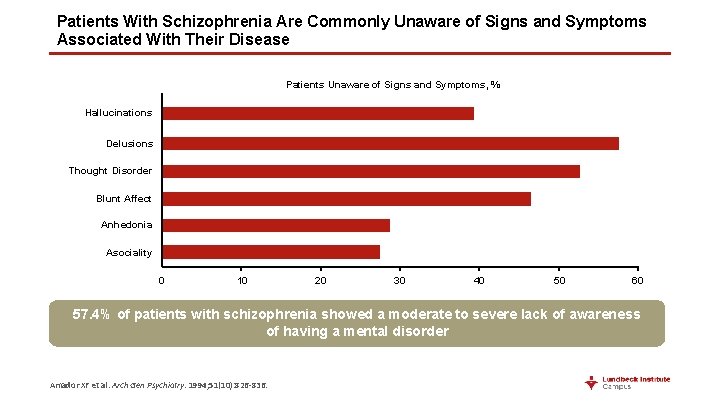
Patients With Schizophrenia Are Commonly Unaware of Signs and Symptoms Associated With Their Disease Patients Unaware of Signs and Symptoms, % Hallucinations Delusions Thought Disorder Blunt Affect Anhedonia Asociality 0 10 20 30 40 50 60 57. 4% of patients with schizophrenia showed a moderate to severe lack of awareness of having a mental disorder Amador XF et al. Arch Gen Psychiatry. 1994; 51(10): 826 -836.
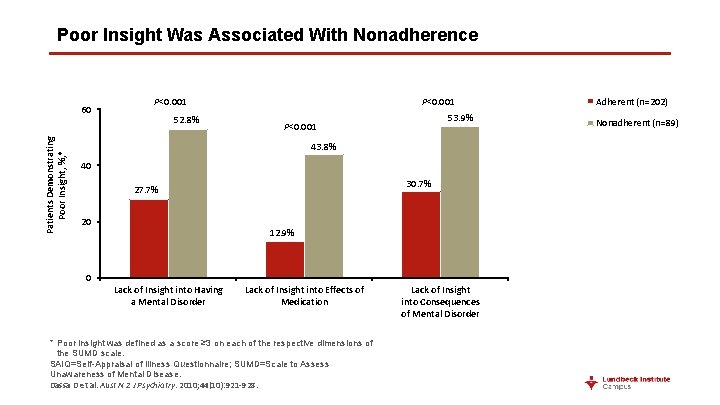
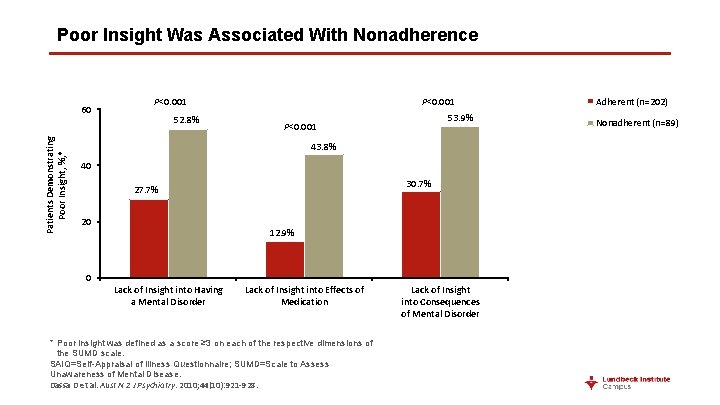
Poor Insight Was Associated With Nonadherence Patients Demonstrating Poor Insight, %, * 60 P<0. 001 52. 8% P<0. 001 53. 9% P<0. 001 43. 8% 40 30. 7% 27. 7% 20 12. 9% 0 Lack of Insight into Having a Mental Disorder Lack of Insight into Effects of Medication * Poor insight was defined as a score ≥ 3 on each of the respective dimensions of the SUMD scale. SAIQ=Self-Appraisal of Illness Questionnaire; SUMD=Scale to Assess Unawareness of Mental Disease. Dassa D et al. Aust N Z J Psychiatry. 2010; 44(10): 921 -928. Lack of Insight into Consequences of Mental Disorder Adherent (n=202) Nonadherent (n=89)
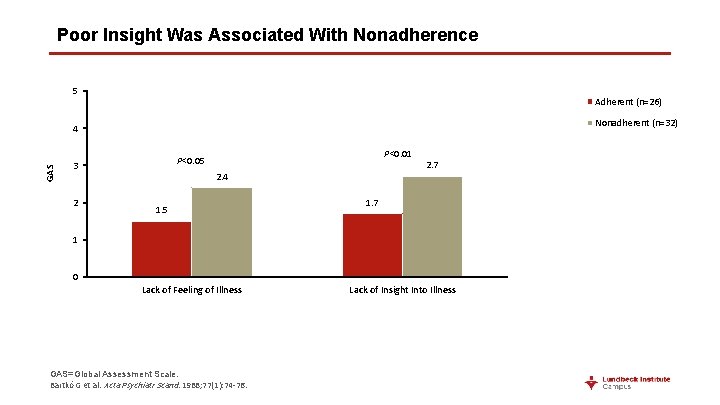
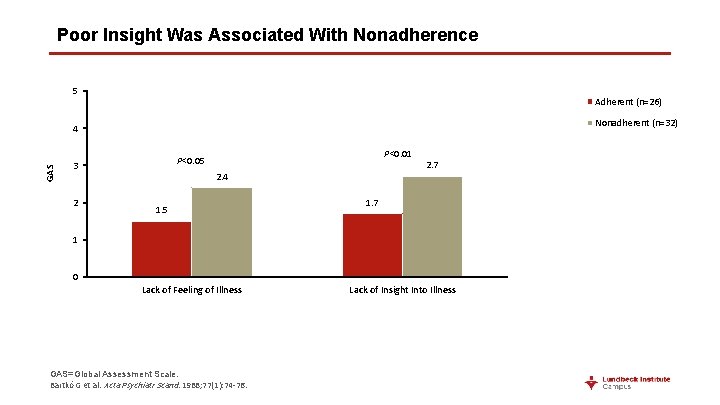
Poor Insight Was Associated With Nonadherence 5 Adherent (n=26) Nonadherent (n=32) GAS 4 2 P<0. 01 P<0. 05 3 2. 4 1. 5 2. 7 1 0 Lack of Feeling of Illness GAS=Global Assessment Scale. Bartkó G et al. Acta Psychiatr Scand. 1988; 77(1): 74 -76. Lack of Insight Into Illness
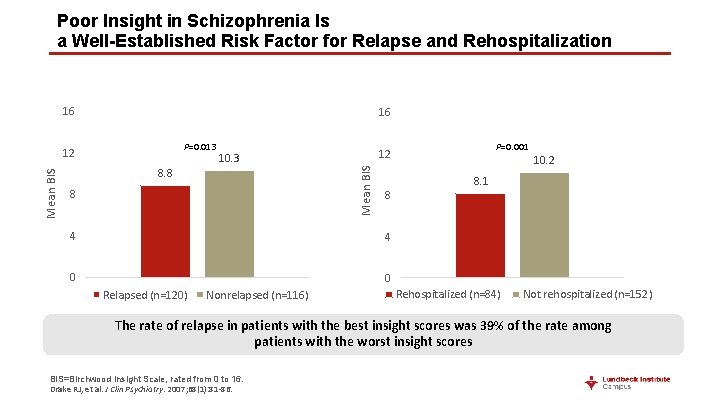
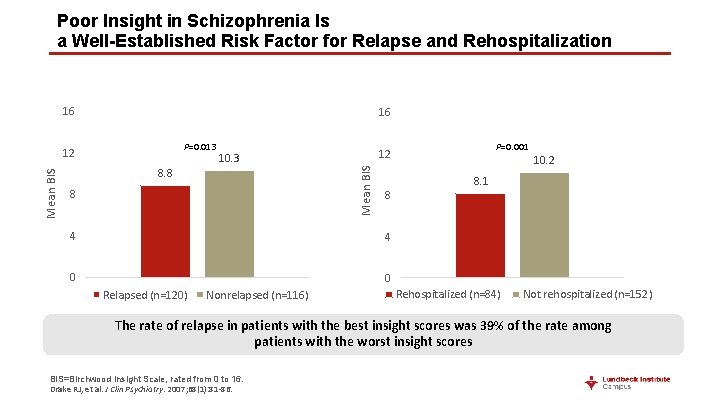
Poor Insight in Schizophrenia Is a Well-Established Risk Factor for Relapse and Rehospitalization 16 16 Mean BIS 10. 3 8. 8 8 8 4 4 0 0 Relapsed (n=120) Nonrelapsed (n=116) P=0. 001 12 Mean BIS P=0. 013 12 10. 2 8. 1 Rehospitalized (n=84) Not rehospitalized (n=152) The rate of relapse in patients with the best insight scores was 39% of the rate among patients with the worst insight scores BIS=Birchwood Insight Scale, rated from 0 to 16. Drake RJ, et al. J Clin Psychiatry. 2007; 68(1): 81 -86.
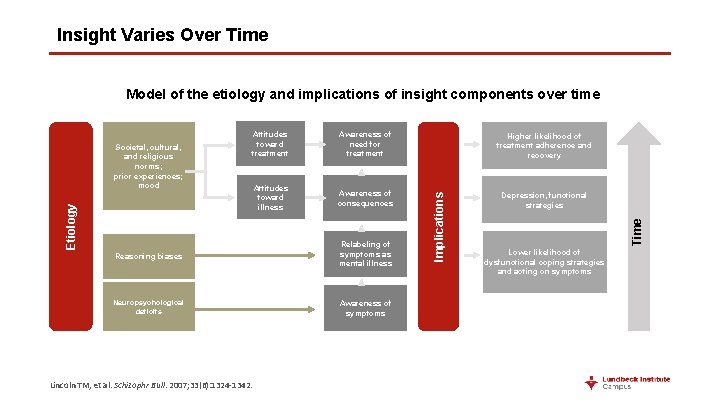
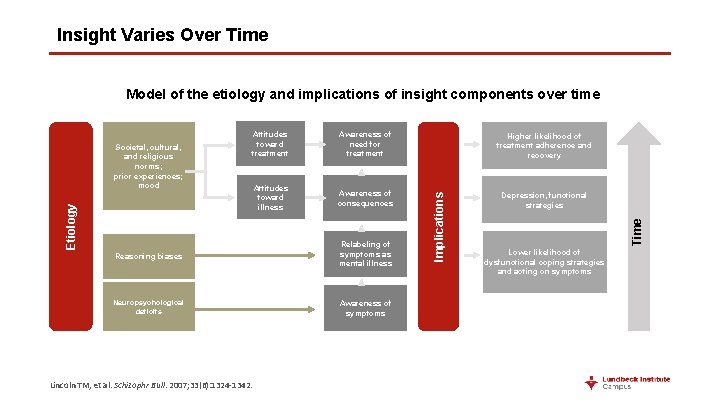
Insight Varies Over Time Model of the etiology and implications of insight components over time Higher likelihood of treatment adherence and recovery Attitudes toward illness Awareness of consequences Depression, functional strategies Reasoning biases Relabeling of symptoms as mental illness Neuropsychological deficits Awareness of symptoms Lincoln TM, et al. Schizophr Bull. 2007; 33(6): 1324 -1342. Time Awareness of need for treatment Implications Attitudes toward treatment Etiology Societal, cultural, and religious norms; prior experiences; mood Lower likelihood of dysfunctional coping strategies and acting on symptoms

Consequences of Nonadherence to Antipsychotics in Patients With Schizophrenia
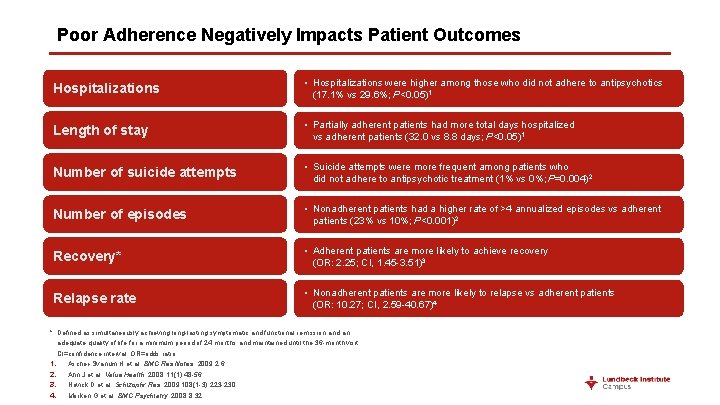
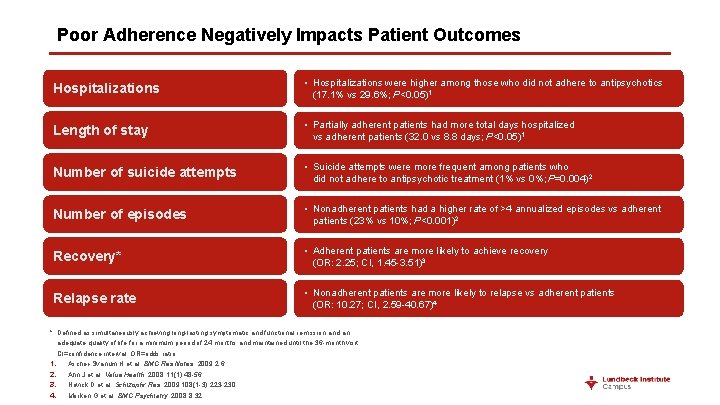
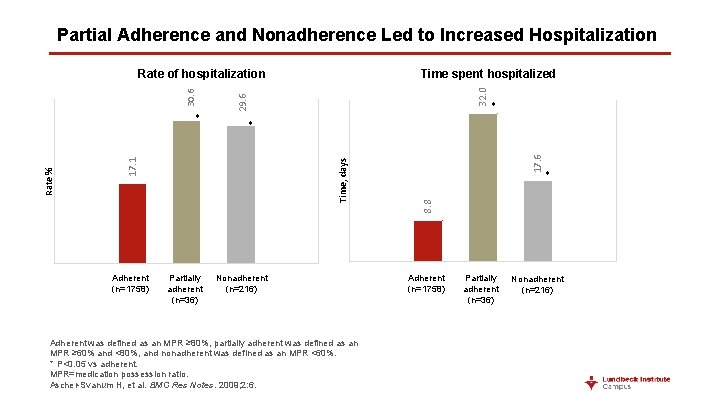
Poor Adherence Negatively Impacts Patient Outcomes Hospitalizations • Hospitalizations were higher among those who did not adhere to antipsychotics (17. 1% vs 29. 6%; P<0. 05)1 Length of stay • Partially adherent patients had more total days hospitalized vs adherent patients (32. 0 vs 8. 8 days; P<0. 05)1 Number of suicide attempts • Suicide attempts were more frequent among patients who did not adhere to antipsychotic treatment (1% vs 0%; P=0. 004)2 Number of episodes • Nonadherent patients had a higher rate of >4 annualized episodes vs adherent patients (23% vs 10%; P<0. 001)2 Recovery* • Adherent patients are more likely to achieve recovery (OR: 2. 25; CI, 1. 45 -3. 51)3 Relapse rate • Nonadherent patients are more likely to relapse vs adherent patients (OR: 10. 27; CI, 2. 59 -40. 67)4 * Defined as simultaneously achieving long-lasting symptomatic and functional remission and an adequate quality of life for a minimum period of 24 months and maintained until the 36 -month visit. CI=confidence interval; OR=odds ratio. 1. Ascher-Svanum H et al. BMC Res Notes. 2009; 2: 6. 2. Ahn J et al. Value Health. 2008; 11(1): 48 -56. 3. Novick D et al. Schizophr Res. 2009; 108(1 -3): 223 -230. 4. Morken G et al. BMC Psychiatry. 2008; 8: 32.

Nonadherent Patients With First-Episode Psychosis Were More Likely to Relapse 1. 0 Adherence (n=92) Nonadherence (n=48) Fraction Survival (Patients Not Relapsed) 0. 8 0. 6 0. 4 0. 2 0. 0 0 12 24 Months Caseiro O, et al. J Psychiatr Res. 2012; 46(8): 1099 -1105. 36

Nonadherence Predicts Relapse in Patients With Recent-Onset Schizophrenia Proportion Not Relapsed 1. 0 0. 9 Adherent (n=65) 0. 8 Nonadherent* (n=35) 0. 7 0. 6 0. 5 0. 4 0. 3 0. 2 0 31 151 271 Days in Study 391 511 Missing as little as 25% of the prescribed dosage over a period of ≥ 2 weeks significantly raised the risk of psychotic symptom return * Nonadherence was defined as adherence with <50% of the prescribed medication dose for at least 2 weeks. All sources of information were considered in categorizing medication adherence. Typically, patient self-report and clinician judgments were available at each rating point, pill counts were available every 1– 2 weeks, and plasma levels were assayed every 4 weeks. Subotnik KL et al. Am J Psychiatry. 2011; 168(3): 286– 292.
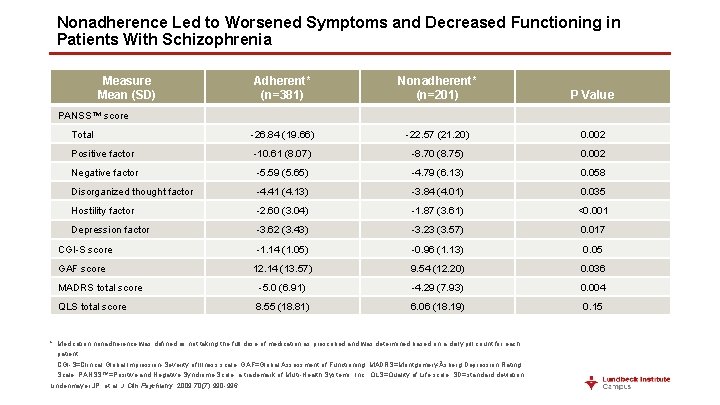
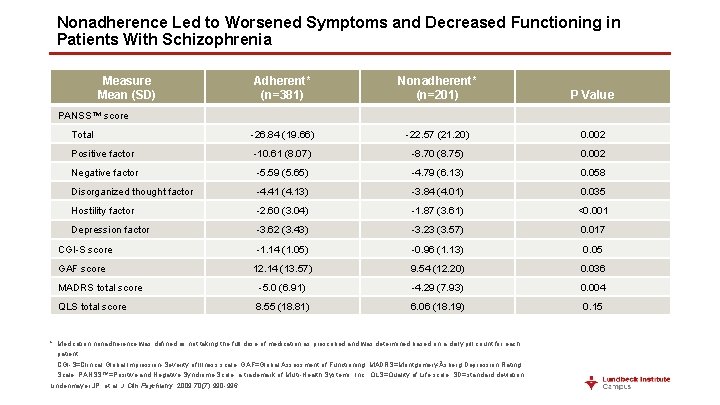
Nonadherence Led to Worsened Symptoms and Decreased Functioning in Patients With Schizophrenia Measure Mean (SD) Adherent* (n=381) Nonadherent* (n=201) P Value Total -26. 84 (19. 66) -22. 57 (21. 20) 0. 002 Positive factor -10. 61 (8. 07) -8. 70 (8. 75) 0. 002 Negative factor -5. 59 (5. 65) -4. 79 (6. 13) 0. 058 Disorganized thought factor -4. 41 (4. 13) -3. 84 (4. 01) 0. 035 Hostility factor -2. 60 (3. 04) -1. 87 (3. 61) <0. 001 Depression factor -3. 62 (3. 43) -3. 23 (3. 57) 0. 017 -1. 14 (1. 05) -0. 96 (1. 13) 0. 05 12. 14 (13. 57) 9. 54 (12. 20) 0. 036 -5. 0 (6. 91) -4. 29 (7. 93) 0. 004 8. 55 (18. 81) 6. 06 (18. 19) 0. 15 PANSS™ score CGI-S score GAF score MADRS total score QLS total score * Medication nonadherence was defined as not taking the full dose of medication as prescribed and was determined based on a daily pill count for each patient. CGI-S=Clinical Global Impression-Severity of Illness scale; GAF=Global Assessment of Functioning; MADRS=Montgomery-Åsberg Depression Rating Scale; PANSS™=Positive and Negative Syndrome Scale, a trademark of Multi-Health Systems, Inc. ; QLS=Quality of Life scale; SD=standard deviation. Lindenmayer JP, et al. J Clin Psychiatry. 2009; 70(7): 990 -996.

Nonadherence to Antipsychotics and Relapse Are Associated With a High Health Care Burden Annual health care costs are 2 to 3 times higher for patients who have had a recent relapse 1, 2 Adherence to antipsychotic therapy could save a Medicaid system $106 million in inpatient costs 3 Loss of neuroleptic efficacy accounted for ~60% of hospitalization costs, while nonadherence was predicted to account for ~40%4 1. 2. 3. 4. Hong J, et al. Prog Neuropsychopharmacol Biol Psychiatry. 2009; 33(5): 835 -841. Ascher-Svanum H, et al. BMC Psychiatry. 2010; 10: 2. Marcus SC, Olfson M. Schizophr Bull. 2008; 34(1): 173 -180. Weiden PJ, Olfson M. Schizophr Bull. 1995; 21(3): 419 -249.
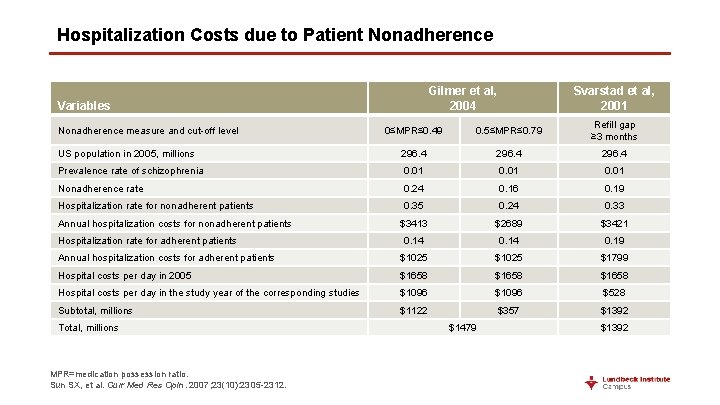
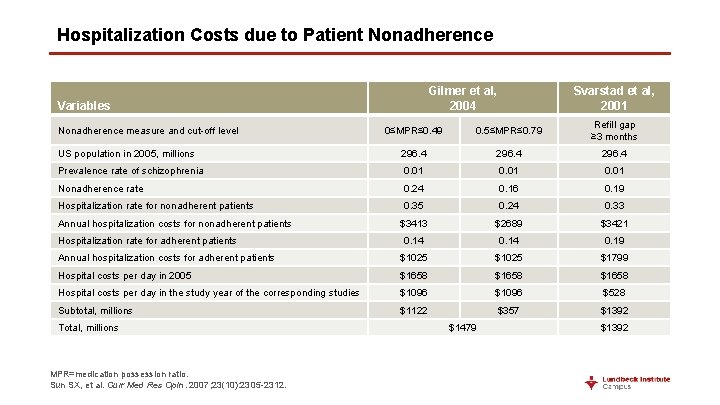
Hospitalization Costs due to Patient Nonadherence Gilmer et al, 2004 Variables Svarstad et al, 2001 0≤MPR≤ 0. 49 0. 5≤MPR≤ 0. 79 Refill gap ≥ 3 months US population in 2005, millions 296. 4 Prevalence rate of schizophrenia 0. 01 Nonadherence rate 0. 24 0. 16 0. 19 Hospitalization rate for nonadherent patients 0. 35 0. 24 0. 33 $3413 $2689 $3421 0. 14 0. 19 Annual hospitalization costs for adherent patients $1025 $1799 Hospital costs per day in 2005 $1658 Hospital costs per day in the study year of the corresponding studies $1096 $528 Subtotal, millions $1122 $357 $1392 Nonadherence measure and cut-off level Annual hospitalization costs for nonadherent patients Hospitalization rate for adherent patients Total, millions MPR=medication possession ratio. Sun SX, et al. Curr Med Res Opin. 2007; 23(10): 2305 -2312. $1479 $1392
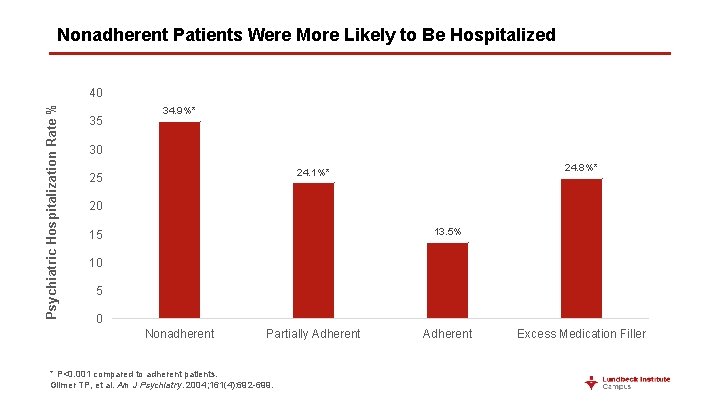
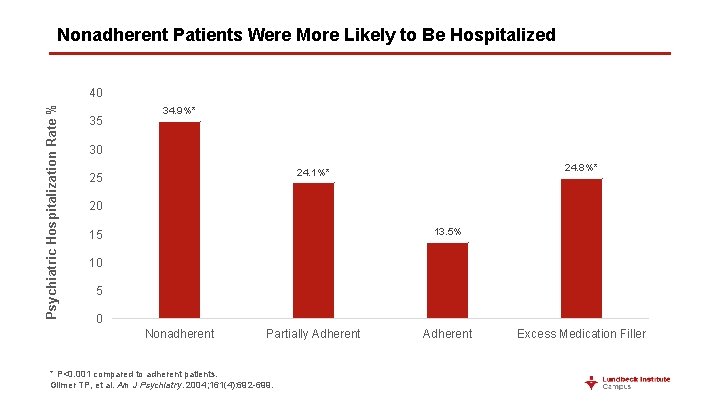
Nonadherent Patients Were More Likely to Be Hospitalized Psychiatric Hospitalization Rate % 40 35 34. 9%* 30 24. 8%* 24. 1%* 25 20 13. 5% 15 10 5 0 Nonadherent Partially Adherent * P<0. 001 compared to adherent patients. Gilmer TP, et al. Am J Psychiatry. 2004; 161(4): 692 -699. Adherent Excess Medication Filler
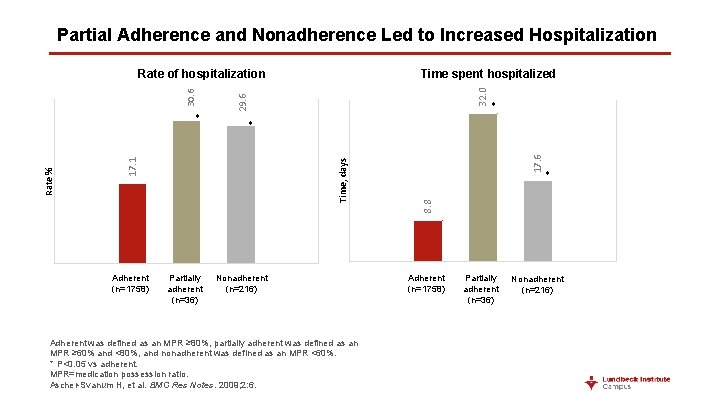
Partial Adherence and Nonadherence Led to Increased Hospitalization Adherent (n=1758) 32. 0 Nonadherent (n=216) Adherent was defined as an MPR ≥ 80%, partially adherent was defined as an MPR ≥ 60% and <80%, and nonadherent was defined as an MPR <60%. * P<0. 05 vs adherent. MPR=medication possession ratio. Ascher-Svanum H, et al. BMC Res Notes. 2009; 2: 6. 17. 6 * 8. 8 Time, days Partially adherent (n=36) * * 17. 1 Rate % * Time spent hospitalized 29. 6 30. 6 Rate of hospitalization Adherent (n=1758) Partially adherent (n=36) Nonadherent (n=216)

Nonadherent Patients Were More Likely to Be Hospitalized 25 22% P<0. 001 Patients Hospitalized, % 20 14% 15 10 5 0 Nonadherent was defined as an MPR <70%. MPR=medication possession ratio. Weiden PJ, et al. Psychiatr Serv. 2004; 55(8): 886 -891. Adherent
Treatment Resistant Schizophrenia
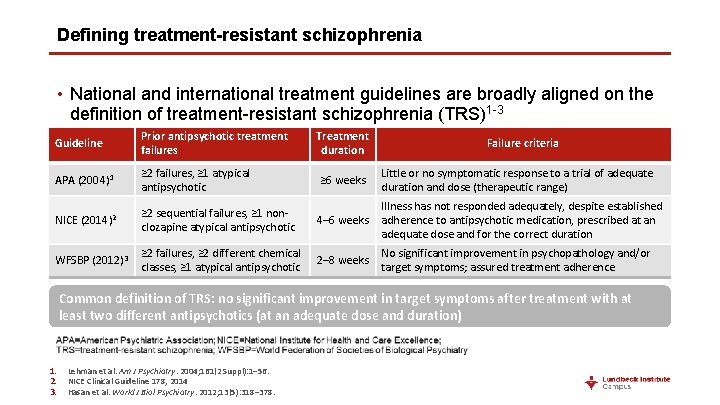
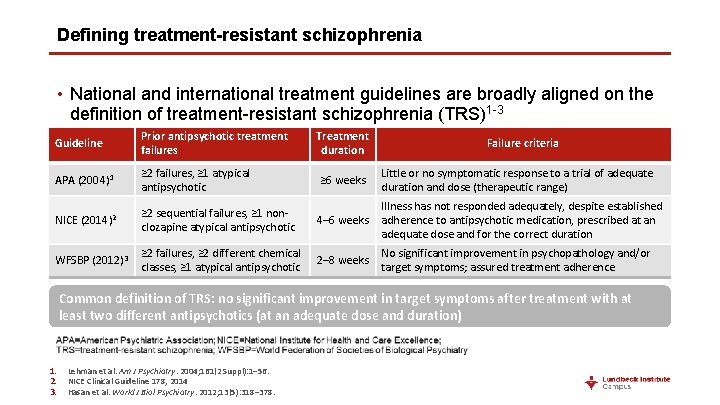
Defining treatment-resistant schizophrenia • National and international treatment guidelines are broadly aligned on the definition of treatment-resistant schizophrenia (TRS)1 -3 Guideline Prior antipsychotic treatment failures Treatment duration APA (2004) 1 ≥ 2 failures, ≥ 1 atypical antipsychotic ≥ 6 weeks Little or no symptomatic response to a trial of adequate duration and dose (therapeutic range) ≥ 2 sequential failures, ≥ 1 nonclozapine atypical antipsychotic 4– 6 weeks Illness has not responded adequately, despite established adherence to antipsychotic medication, prescribed at an adequate dose and for the correct duration ≥ 2 failures, ≥ 2 different chemical classes, ≥ 1 atypical antipsychotic 2– 8 weeks No significant improvement in psychopathology and/or target symptoms; assured treatment adherence NICE (2014)2 WFSBP (2012)3 Failure criteria Common definition of TRS: no significant improvement in target symptoms after treatment with at least two different antipsychotics (at an adequate dose and duration) 1. 2. 3. Lehman et al. Am J Psychiatry. 2004; 161(2 Suppl): 1– 56. NICE Clinical Guideline 178, 2014 Hasan et al. World J Biol Psychiatry. 2012; 13(5): 318– 378.
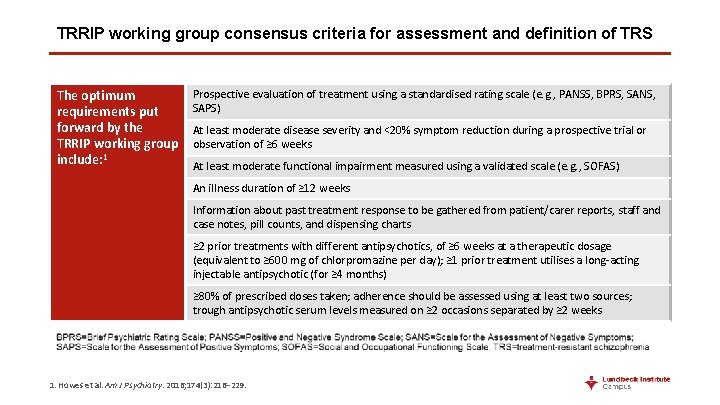
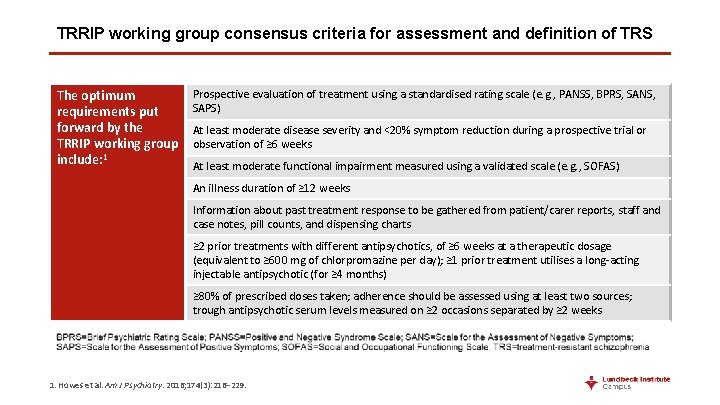
TRRIP working group consensus criteria for assessment and definition of TRS The optimum requirements put forward by the TRRIP working group include: 1 Prospective evaluation of treatment using a standardised rating scale (e. g. , PANSS, BPRS, SANS, SAPS) At least moderate disease severity and <20% symptom reduction during a prospective trial or observation of ≥ 6 weeks At least moderate functional impairment measured using a validated scale (e. g. , SOFAS) An illness duration of ≥ 12 weeks Information about past treatment response to be gathered from patient/carer reports, staff and case notes, pill counts, and dispensing charts ≥ 2 prior treatments with different antipsychotics, of ≥ 6 weeks at a therapeutic dosage (equivalent to ≥ 600 mg of chlorpromazine per day); ≥ 1 prior treatment utilises a long-acting injectable antipsychotic (for ≥ 4 months) ≥ 80% of prescribed doses taken; adherence should be assessed using at least two sources; trough antipsychotic serum levels measured on ≥ 2 occasions separated by ≥ 2 weeks 1. Howes et al. Am J Psychiatry. 2016; 174(3): 216– 229.
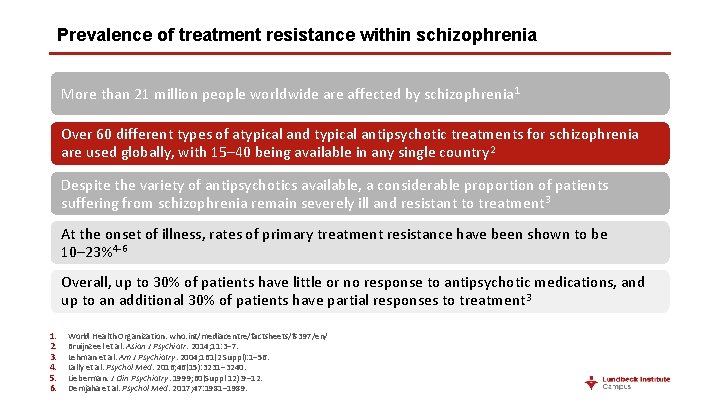
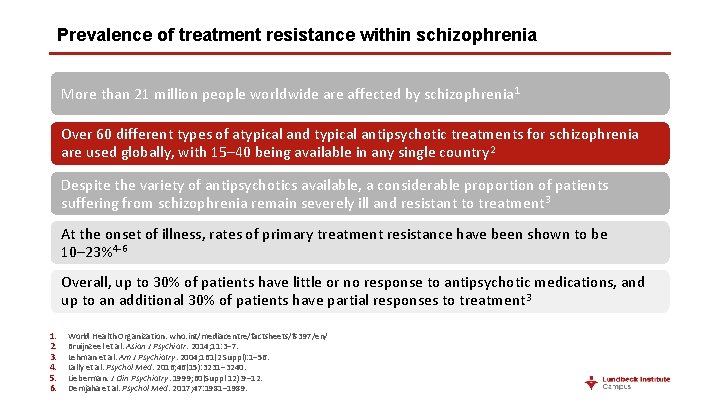
Prevalence of treatment resistance within schizophrenia More than 21 million people worldwide are affected by schizophrenia 1 Over 60 different types of atypical and typical antipsychotic treatments for schizophrenia are used globally, with 15– 40 being available in any single country 2 Despite the variety of antipsychotics available, a considerable proportion of patients suffering from schizophrenia remain severely ill and resistant to treatment 3 At the onset of illness, rates of primary treatment resistance have been shown to be 10– 23%4 -6 Overall, up to 30% of patients have little or no response to antipsychotic medications, and up to an additional 30% of patients have partial responses to treatment 3 1. 2. 3. 4. 5. 6. World Health Organization. who. int/mediacentre/factsheets/fs 397/en/ Bruijnzeel et al. Asian J Psychiatr. 2014; 11: 3– 7. Lehman et al. Am J Psychiatry. 2004; 161(2 Suppl): 1– 56. Lally et al. Psychol Med. 2016; 46(15): 3231– 3240. Lieberman. J Clin Psychiatry. 1999; 60(Suppl 12): 9– 12. Demjaha et al. Psychol Med. 2017; 47: 1981– 1989.
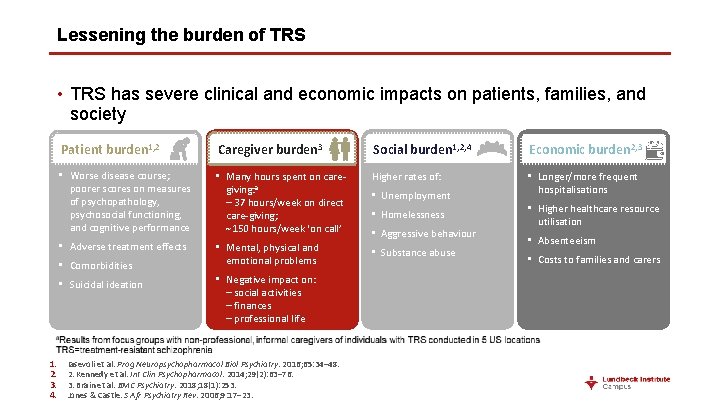
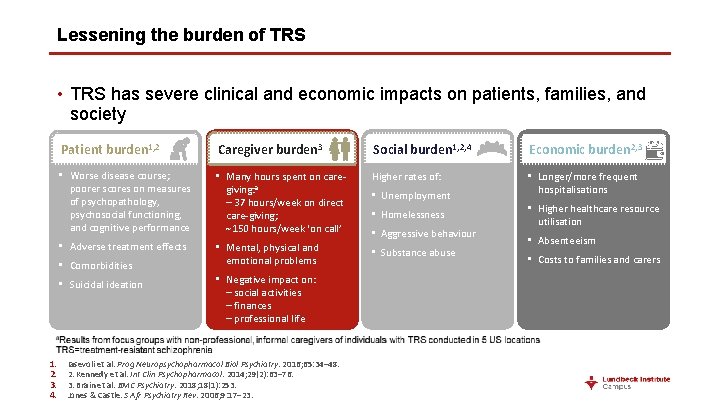
Lessening the burden of TRS • TRS has severe clinical and economic impacts on patients, families, and society Patient burden 1, 2 Caregiver burden 3 Social burden 1, 2, 4 Economic burden 2, 3 • Worse disease course; poorer scores on measures of psychopathology, psychosocial functioning, and cognitive performance • Many hours spent on caregiving: a – 37 hours/week on direct care-giving; 150 hours/week ‘on call’ Higher rates of: • Longer/more frequent hospitalisations • Adverse treatment effects • Mental, physical and emotional problems • Substance abuse • Comorbidities • Suicidal ideation 1. 2. 3. 4. • Negative impact on: – social activities – finances – professional life Iasevoli et al. Prog Neuropsychopharmacol Biol Psychiatry. 2016; 65: 34– 48. 2. Kennedy et al. Int Clin Psychopharmacol. 2014; 29(2): 63– 76. 3. Brain et al. BMC Psychiatry. 2018; 18(1): 253. Jones & Castle. S Afr Psychiatry Rev. 2006; 9: 17– 23. • Unemployment • Homelessness • Aggressive behaviour • Higher healthcare resource utilisation • Absenteeism • Costs to families and carers
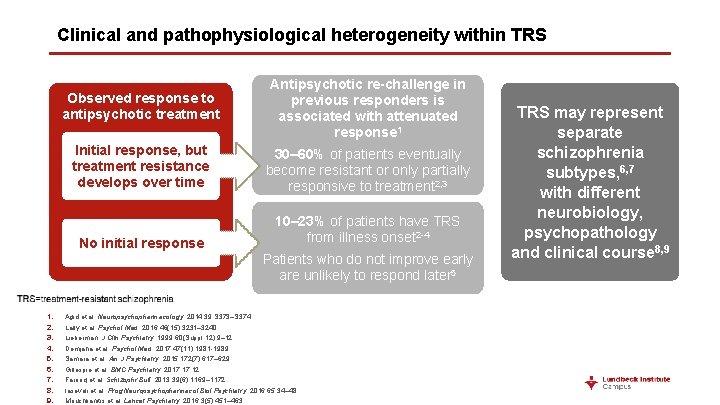
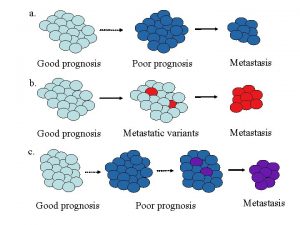
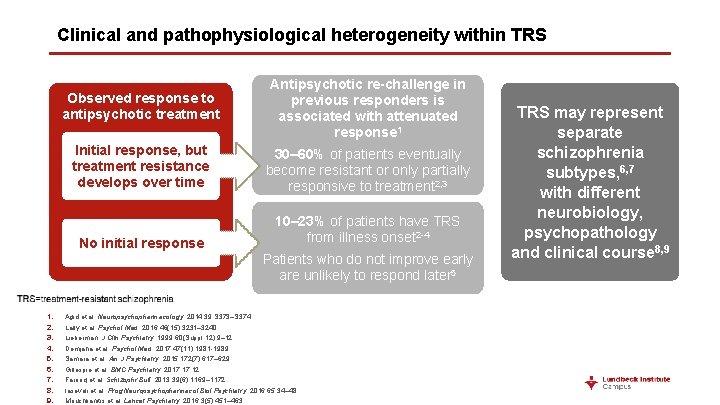
Clinical and pathophysiological heterogeneity within TRS Observed response to antipsychotic treatment Antipsychotic re-challenge in previous responders is associated with attenuated response 1 Initial response, but treatment resistance develops over time 30– 60% of patients eventually become resistant or only partially responsive to treatment 2, 3 No initial response 10– 23% of patients have TRS from illness onset 2 -4 Patients who do not improve early are unlikely to respond later 5 1. 2. 3. 4. 5. 6. 7. 8. 9. Agid et al. Neuropsychopharmacology. 2014; 39: S 373–S 374. Lally et al. Psychol Med. 2016; 46(15): 3231– 3240. Lieberman. J Clin Psychiatry. 1999; 60(Suppl 12): 9– 12. Demjaha et al. Psychol Med. 2017; 47(11): 1981 -1989. Samara et al. Am J Psychiatry. 2015; 172(7): 617– 629. Gillespie et al. BMC Psychiatry. 2017; 17: 12. Farooq et al. Schizophr Bull. 2013; 39(6): 1169– 1172. Iasevoli et al. Prog Neuropsychopharmacol Biol Psychiatry. 2016; 65: 34– 48. Mouchlianitis et al. Lancet Psychiatry. 2016; 3(5): 451– 463. TRS may represent separate schizophrenia subtypes, 6, 7 with different neurobiology, psychopathology and clinical course 8, 9
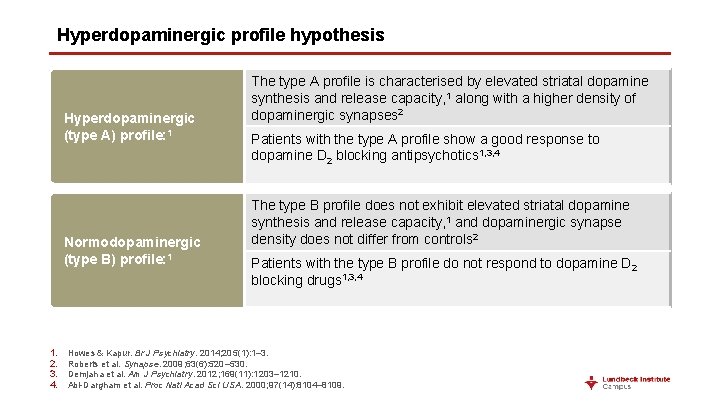
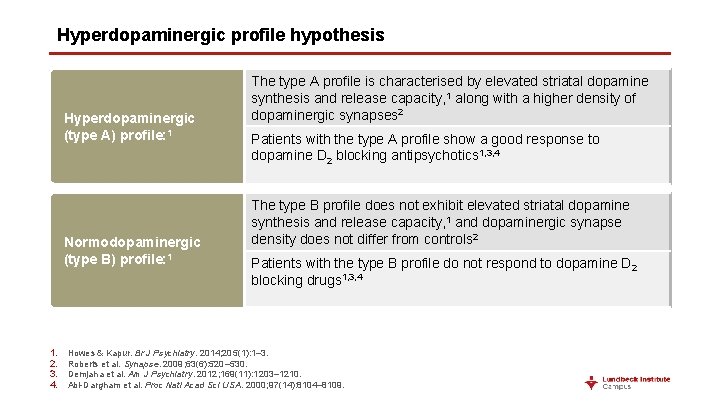
Hyperdopaminergic profile hypothesis Hyperdopaminergic (type A) profile: 1 Normodopaminergic (type B) profile: 1 1. 2. 3. 4. The type A profile is characterised by elevated striatal dopamine synthesis and release capacity, 1 along with a higher density of dopaminergic synapses 2 Patients with the type A profile show a good response to dopamine D 2 blocking antipsychotics 1, 3, 4 The type B profile does not exhibit elevated striatal dopamine synthesis and release capacity, 1 and dopaminergic synapse density does not differ from controls 2 Patients with the type B profile do not respond to dopamine D 2 blocking drugs 1, 3, 4 Howes & Kapur. Br J Psychiatry. 2014; 205(1): 1– 3. Roberts et al. Synapse. 2009; 63(6): 520– 530. Demjaha et al. Am J Psychiatry. 2012; 169(11): 1203– 1210. Abi-Dargham et al. Proc Natl Acad Sci USA. 2000; 97(14): 8104– 8109.
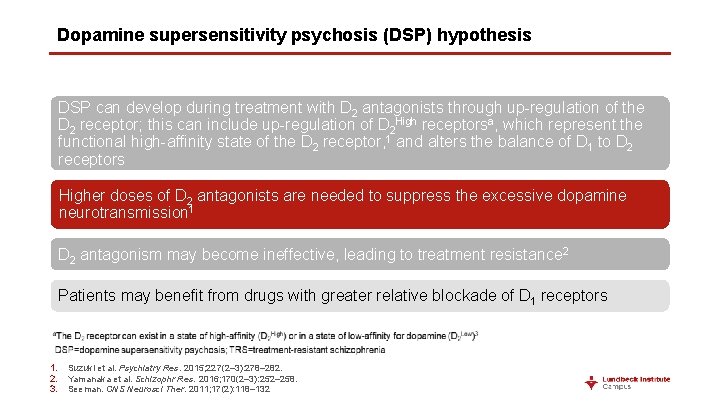
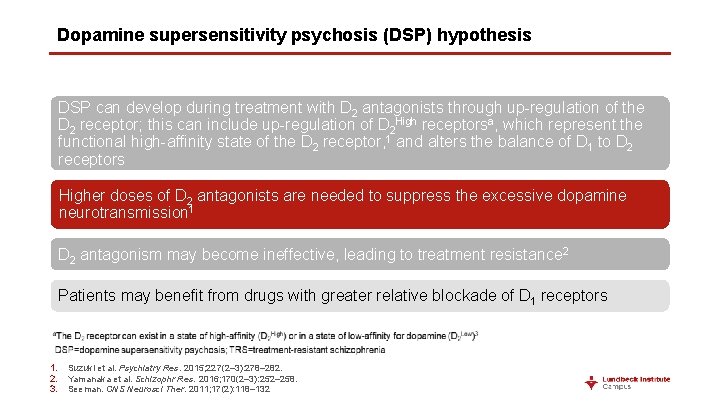
Dopamine supersensitivity psychosis (DSP) hypothesis DSP can develop during treatment with D 2 antagonists through up-regulation of the D 2 receptor; this can include up-regulation of D 2 High receptorsa, which represent the functional high-affinity state of the D 2 receptor, 1 and alters the balance of D 1 to D 2 receptors Higher doses of D 2 antagonists are needed to suppress the excessive dopamine neurotransmission 1 D 2 antagonism may become ineffective, leading to treatment resistance 2 Patients may benefit from drugs with greater relative blockade of D 1 receptors 1. 2. 3. Suzuki et al. Psychiatry Res. 2015; 227(2– 3): 278– 282. Yamanaka et al. Schizophr Res. 2016; 170(2– 3): 252– 258. Seeman. CNS Neurosci Ther. 2011; 17(2): 118– 132
 Schizophrenia crash course
Schizophrenia crash course Orleans hanna algebra prognosis test
Orleans hanna algebra prognosis test Conocimiento anticipado de alguna cosa
Conocimiento anticipado de alguna cosa Ich score prognosis
Ich score prognosis Perinatolgy
Perinatolgy Autism prognosis
Autism prognosis Autism prognosis
Autism prognosis Autism prognosis
Autism prognosis Kanners syndrome
Kanners syndrome Global developmental delay symptoms
Global developmental delay symptoms Static-99
Static-99 What is prognosis
What is prognosis Prognosis
Prognosis Child-pugh score prognosis
Child-pugh score prognosis Cholangitis prognosis
Cholangitis prognosis Good prognosis
Good prognosis Prognosis of cystic fibrosis
Prognosis of cystic fibrosis Pyloric adenoma
Pyloric adenoma Good prognosis
Good prognosis Natural capital and natural income
Natural capital and natural income Chapter 31 schizophrenia and other psychoses
Chapter 31 schizophrenia and other psychoses Natural history and spectrum of disease
Natural history and spectrum of disease Course number and title
Course number and title Natural hazards vs natural disasters
Natural hazards vs natural disasters Ap world history course and exam description
Ap world history course and exam description Mse example
Mse example Brief psychotic disorder
Brief psychotic disorder Signs of schizophrenia in children
Signs of schizophrenia in children Humanistic approach to schizophrenia
Humanistic approach to schizophrenia Schizoaffective disorder
Schizoaffective disorder First-line treatment for schizophrenia
First-line treatment for schizophrenia Bleuler 4a
Bleuler 4a Schizophrenia's literal translation means...
Schizophrenia's literal translation means... Types of delusions
Types of delusions Thesis statement about schizophrenia
Thesis statement about schizophrenia Residual schizophrenia
Residual schizophrenia Hebephrenic schizophrenia
Hebephrenic schizophrenia Disorganized schizophrenia
Disorganized schizophrenia Schizophrenia disorganized behavior
Schizophrenia disorganized behavior Example of loose associations in schizophrenia
Example of loose associations in schizophrenia Thought insertion
Thought insertion Phases of schizophrenia
Phases of schizophrenia Double bind
Double bind Negative explanatory style
Negative explanatory style Conclusion of schizophrenia
Conclusion of schizophrenia Associative looseness
Associative looseness Loose associations
Loose associations Motivational interviewing schizophrenia
Motivational interviewing schizophrenia Schizophrenia def
Schizophrenia def Module 68 schizophrenia
Module 68 schizophrenia Prevalence of schizophrenia
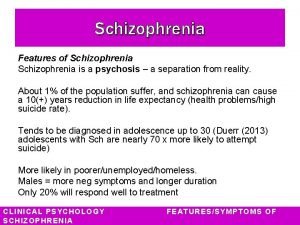
Prevalence of schizophrenia Dr tachere
Dr tachere Reality testing worksheet schizophrenia
Reality testing worksheet schizophrenia Cognitive explanations of schizophrenia
Cognitive explanations of schizophrenia Example of loose associations in schizophrenia
Example of loose associations in schizophrenia Schizophrenia def
Schizophrenia def First-line treatment for schizophrenia
First-line treatment for schizophrenia Timmy turner age
Timmy turner age Undifferentiated schizophrenia
Undifferentiated schizophrenia Schizophrenia def
Schizophrenia def Chapter 12 schizophrenia spectrum disorders
Chapter 12 schizophrenia spectrum disorders Catatonic schizophrenia
Catatonic schizophrenia Nigrostriatal pathway
Nigrostriatal pathway Dopamine hypothesis of schizophrenia ppt
Dopamine hypothesis of schizophrenia ppt What is schizophrenia
What is schizophrenia What causes schizophrenia
What causes schizophrenia Avolition definition schizophrenia
Avolition definition schizophrenia Schizophrenia
Schizophrenia Biological explanations of schizophrenia
Biological explanations of schizophrenia Genes schizophrenia
Genes schizophrenia Symptoms of schizophrenia
Symptoms of schizophrenia Sirs 2021
Sirs 2021 Example epic
Example epic Catatonic schizophrenia
Catatonic schizophrenia Schizo
Schizo Schizophrenia unfolding case study answers
Schizophrenia unfolding case study answers Schizophrenia
Schizophrenia Statistics of schizophrenia
Statistics of schizophrenia Schizophrenia
Schizophrenia Alya alghamdi
Alya alghamdi