RECOGNIZING AND RESPONDING TO SIGNS OF EMERGING PSYCHOSIS



- Slides: 43
RECOGNIZING AND RESPONDING TO SIGNS OF EMERGING PSYCHOSIS IN YOUNG PEOPLE JUVENILE COURT CLINICIAN’S CONFERENCE UMMS SOUTH STREET CAMPUS 4/27/2018 Michelle L. West, Ph. D. Megan Graham, LMHC mwest 3@bidmc. harvard. edu 617 -754 -1241 mgraham 1@bidmc. harvard. edu 617 -754 -1223 Center for Early Detection Assessment and Response to Risk (CEDAR) Clinic & Research Program Massachusetts Mental Health Center Beth Israel Deaconess Medical Center www. cedarclinic. org
AGENDA About early psychosis • Presenting symptoms, frequency, terminology, assessment tools • Clinical high risk (CHR) for psychosis vs. first episode psychosis (FEP) Our early psychosis programs • CEDAR • PREP® • Making referrals to us Questions/Discussion • Case examples – differential diagnosis
Early Psychosis Take Home Points 1. Psychosis is more common than people tend to think. 2. You can help youths at risk by recognizing early signs. 3. You can learn how to talk to young people and families about these experiences. 4. Early intervention is possible and can reduce suffering and disability.
1. PSYCHOSIS IS MORE COMMON THAN PEOPLE THINK IT IS.
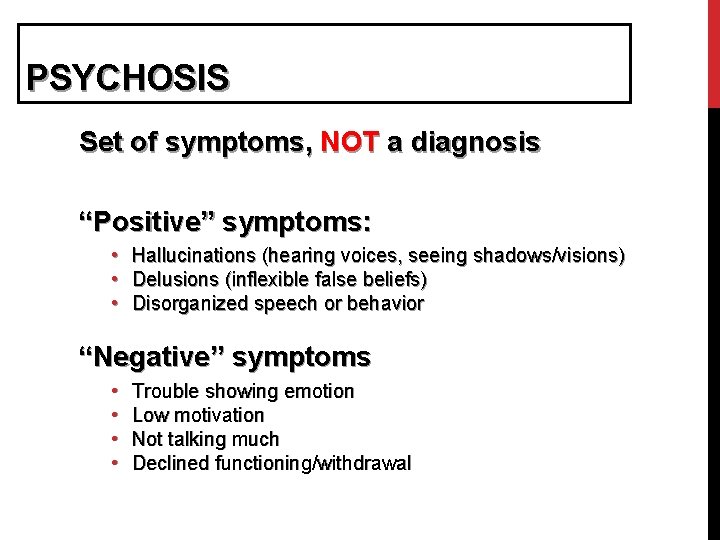
PSYCHOSIS Set of symptoms, NOT a diagnosis “Positive” symptoms: • Hallucinations (hearing voices, seeing shadows/visions) • Delusions (inflexible false beliefs) • Disorganized speech or behavior “Negative” symptoms • • Trouble showing emotion Low motivation Not talking much Declined functioning/withdrawal
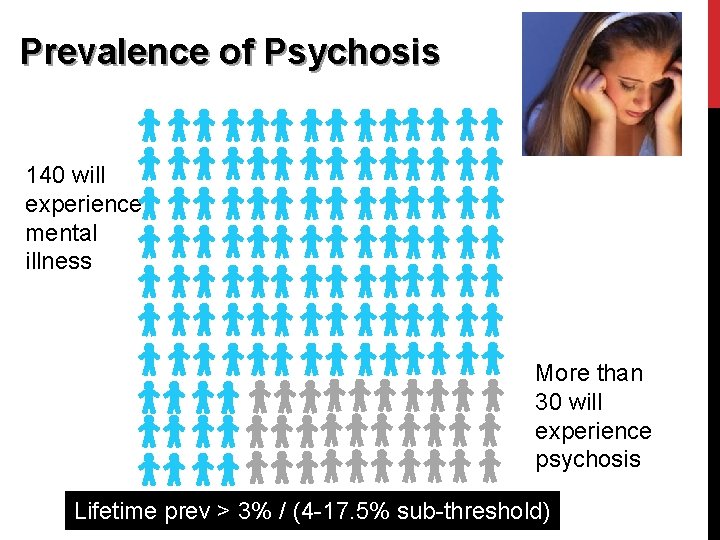
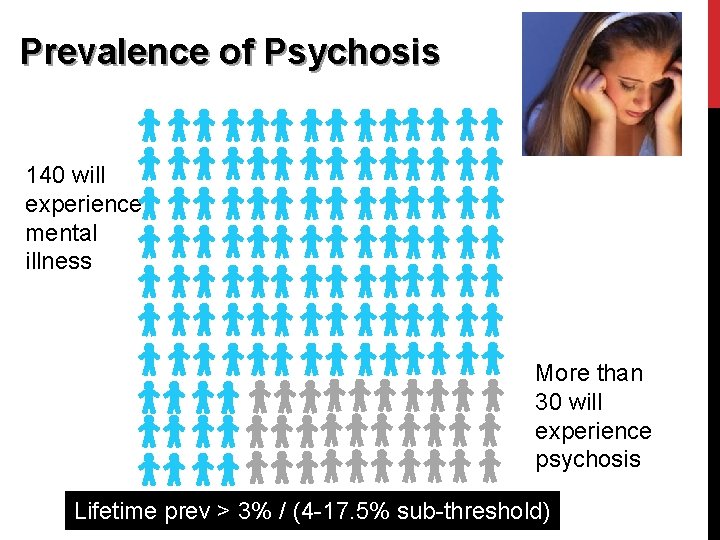
Prevalence of Psychosis Of 1000 College students 140 will experience mental illness More than 30 will experience psychosis Lifetime prev > 3% / (4 -17. 5% sub-threshold)
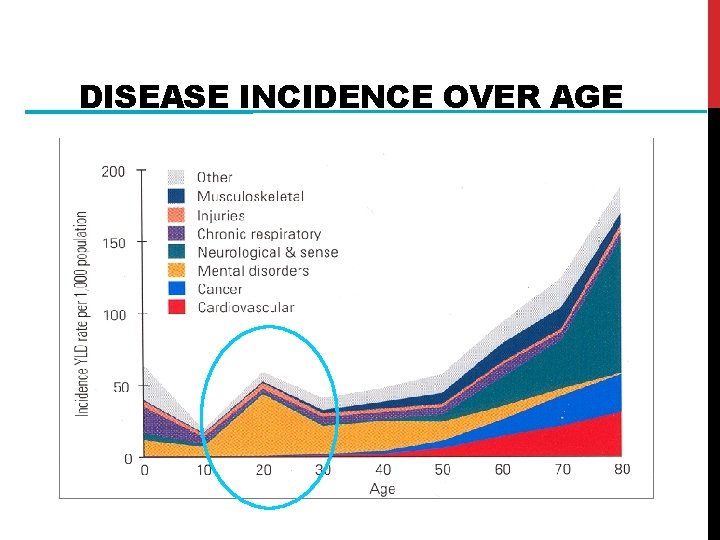
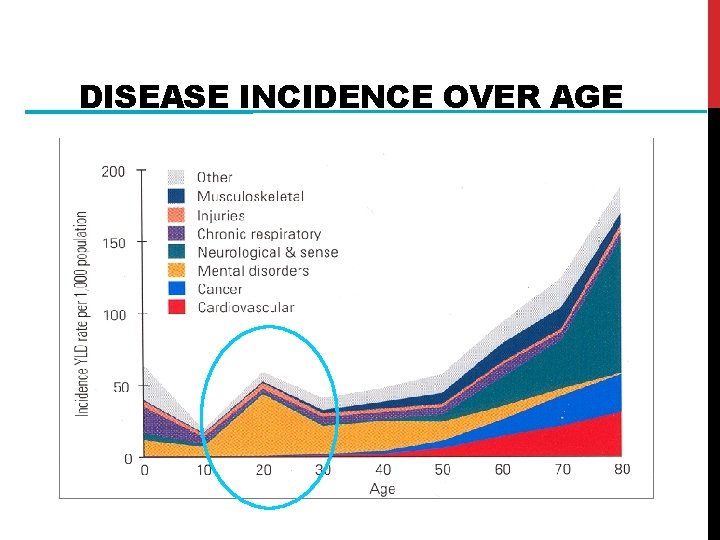
DISEASE INCIDENCE OVER AGE
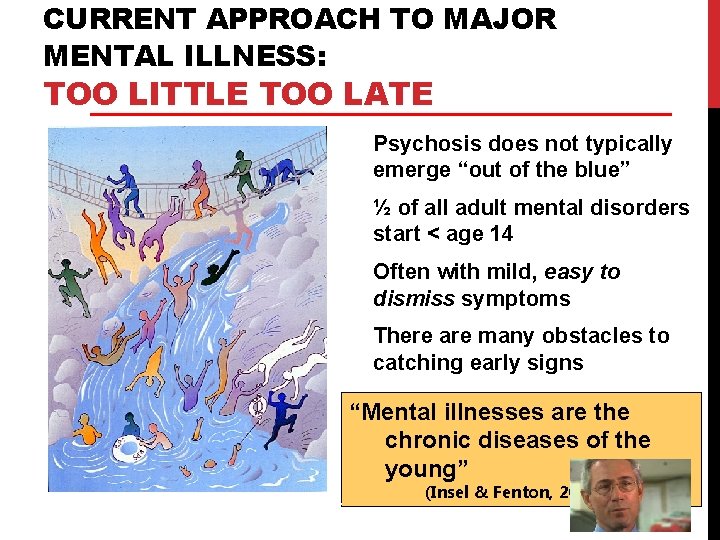
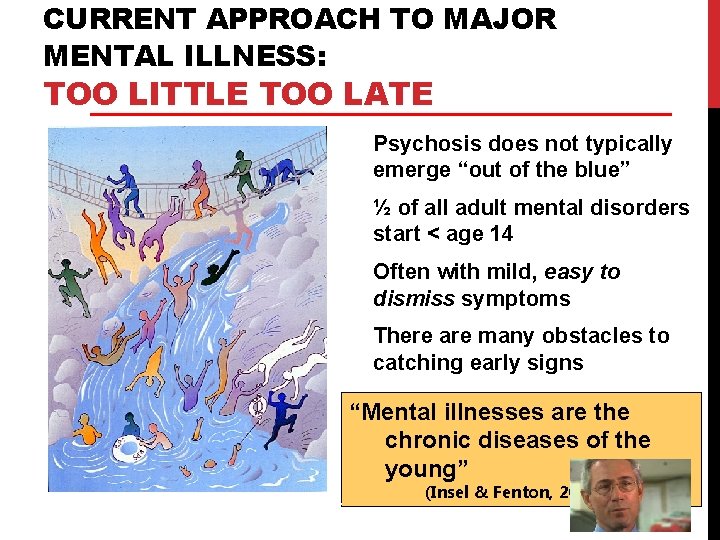
CURRENT APPROACH TO MAJOR MENTAL ILLNESS: TOO LITTLE TOO LATE Psychosis does not typically emerge “out of the blue” ½ of all adult mental disorders start < age 14 Often with mild, easy to dismiss symptoms There are many obstacles to catching early signs “Mental illnesses are the chronic diseases of the young” Courtesy of P Mc. Gorry (Insel & Fenton, 2005)
2. YOU CAN HELP STUDENTS AT RISK BY RECOGNIZING EARLY SIGNS.
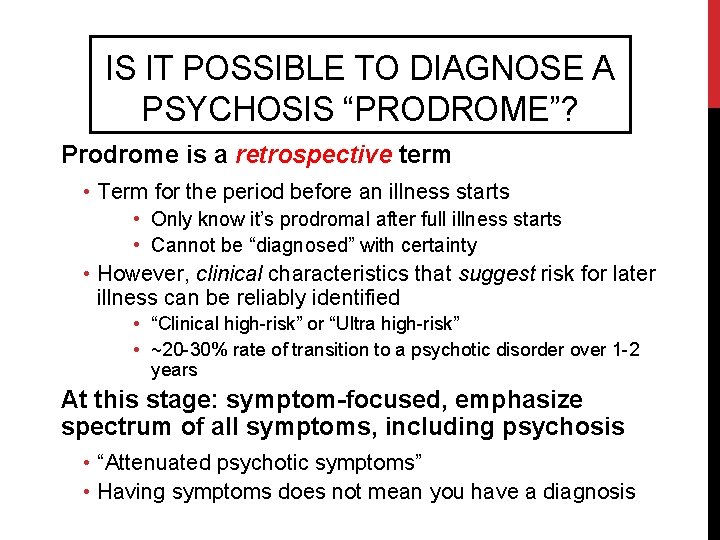
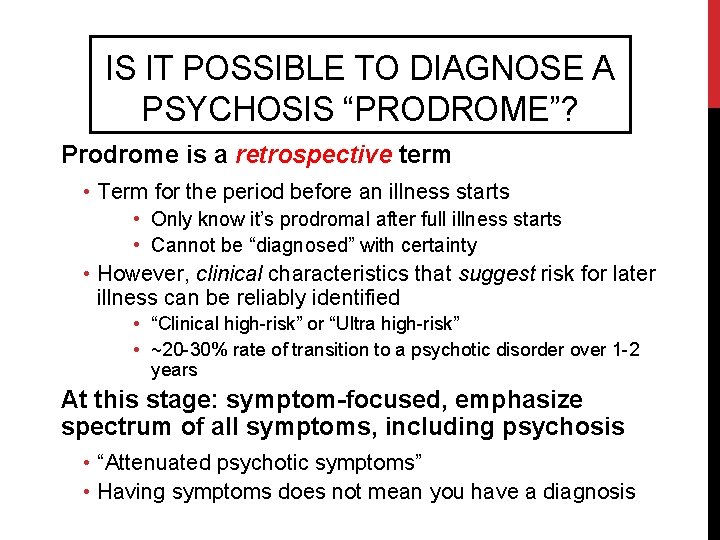
IS IT POSSIBLE TO DIAGNOSE A PSYCHOSIS “PRODROME”? Prodrome is a retrospective term • Term for the period before an illness starts • Only know it’s prodromal after full illness starts • Cannot be “diagnosed” with certainty • However, clinical characteristics that suggest risk for later illness can be reliably identified • “Clinical high-risk” or “Ultra high-risk” • ~20 -30% rate of transition to a psychotic disorder over 1 -2 years At this stage: symptom-focused, emphasize spectrum of all symptoms, including psychosis • “Attenuated psychotic symptoms” • Having symptoms does not mean you have a diagnosis
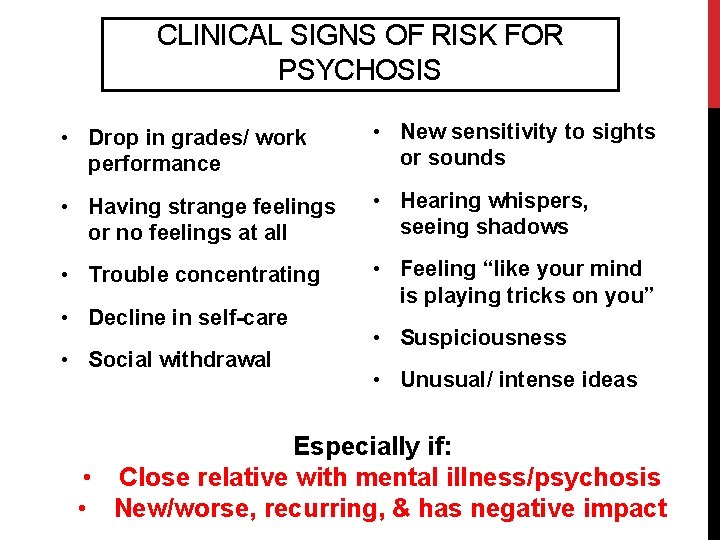
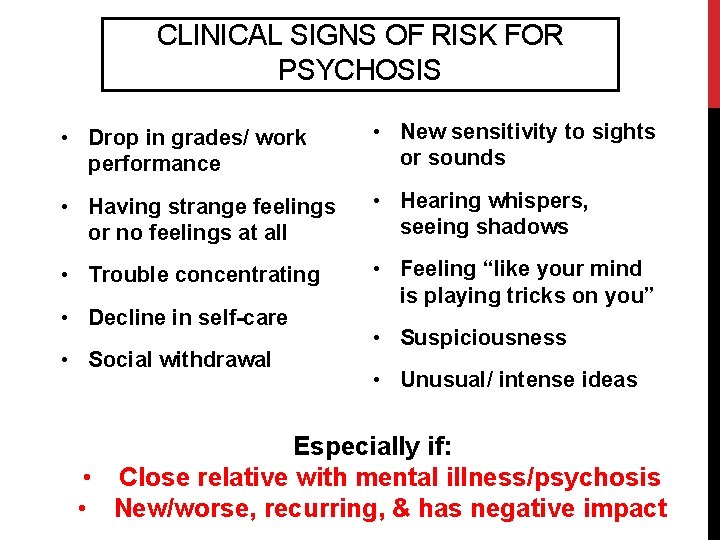
CLINICAL SIGNS OF RISK FOR PSYCHOSIS • Drop in grades/ work performance • New sensitivity to sights or sounds • Having strange feelings or no feelings at all • Hearing whispers, seeing shadows • Trouble concentrating • Feeling “like your mind is playing tricks on you” • Decline in self-care • Social withdrawal • Suspiciousness • Unusual/ intense ideas Especially if: • Close relative with mental illness/psychosis • New/worse, recurring, & has negative impact
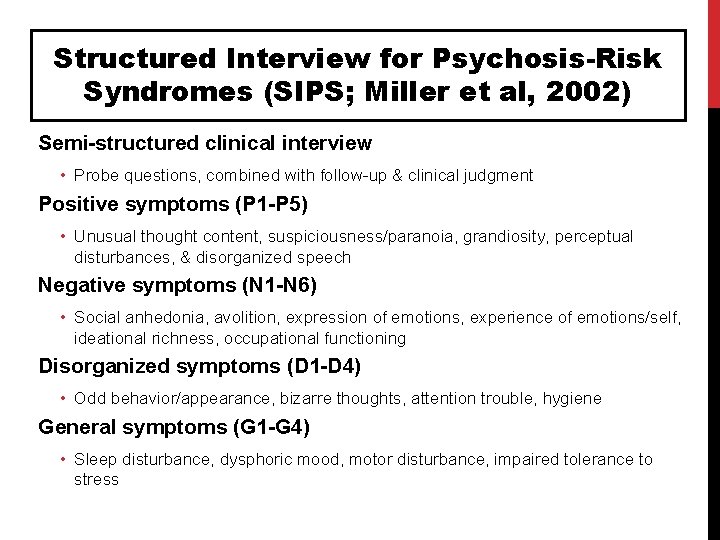
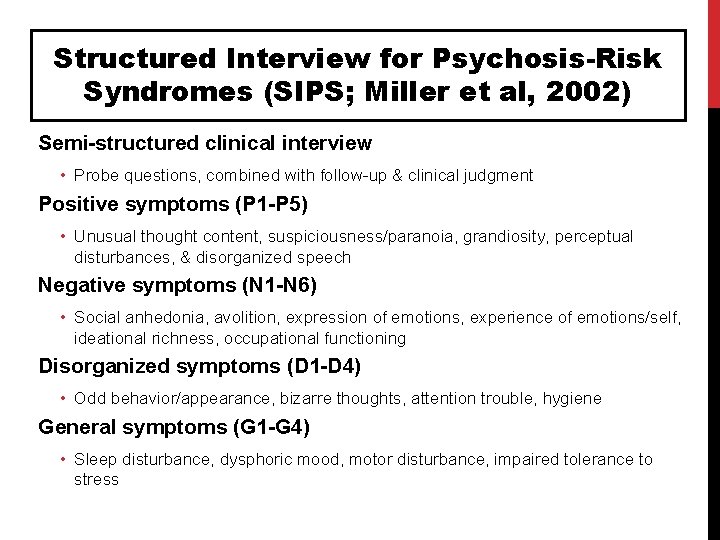
Structured Interview for Psychosis-Risk Syndromes (SIPS; Miller et al, 2002) Semi-structured clinical interview • Probe questions, combined with follow-up & clinical judgment Positive symptoms (P 1 -P 5) • Unusual thought content, suspiciousness/paranoia, grandiosity, perceptual disturbances, & disorganized speech Negative symptoms (N 1 -N 6) • Social anhedonia, avolition, expression of emotions, experience of emotions/self, ideational richness, occupational functioning Disorganized symptoms (D 1 -D 4) • Odd behavior/appearance, bizarre thoughts, attention trouble, hygiene General symptoms (G 1 -G 4) • Sleep disturbance, dysphoric mood, motor disturbance, impaired tolerance to stress
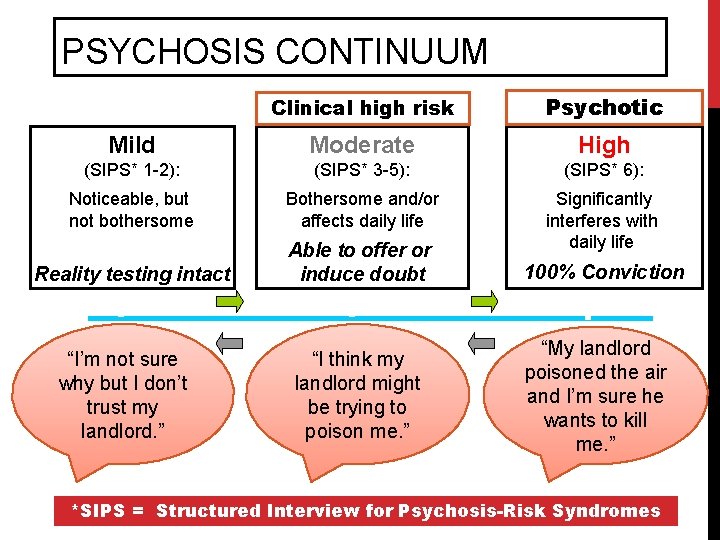
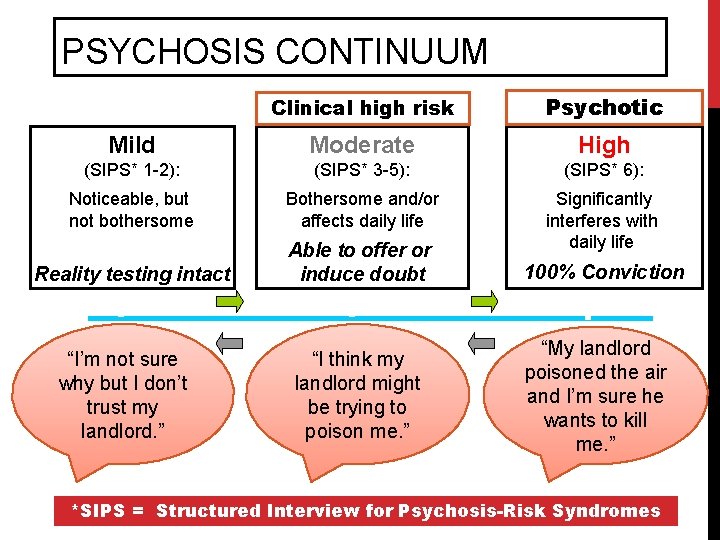
PSYCHOSIS CONTINUUM Clinical high risk Psychotic Mild Moderate High (SIPS* 1 -2): (SIPS* 3 -5): (SIPS* 6): Noticeable, but not bothersome Bothersome and/or affects daily life Reality testing intact Able to offer or induce doubt Significantly interferes with daily life 100% Conviction “I think my landlord might be trying to poison me. ” “My landlord poisoned the air and I’m sure he wants to kill me. ” “I’m not sure why but I don’t trust my landlord. ” *SIPS = Structured Interview for Psychosis-Risk Syndromes
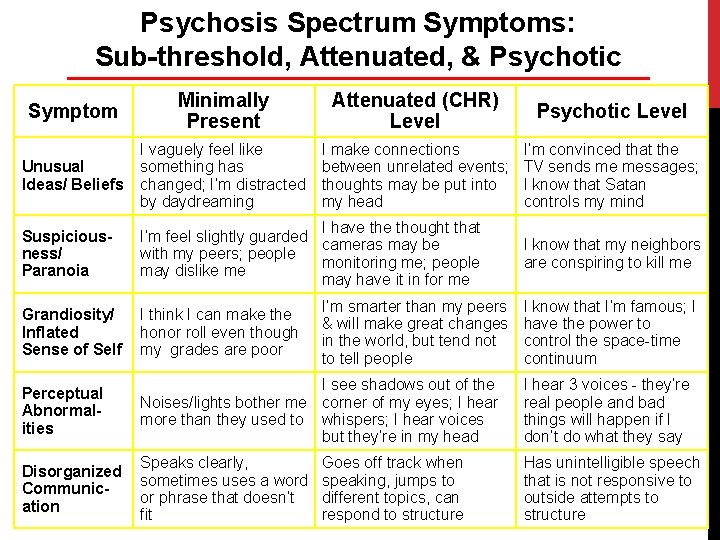
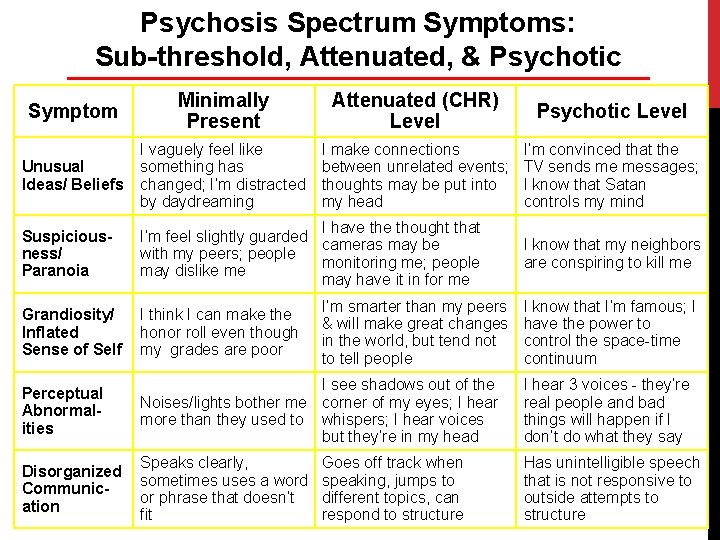
Psychosis Spectrum Symptoms: Sub-threshold, Attenuated, & Psychotic Symptom Minimally Present Attenuated (CHR) Level Psychotic Level Unusual Ideas/ Beliefs I vaguely feel like something has changed; I’m distracted by daydreaming I make connections between unrelated events; thoughts may be put into my head I’m convinced that the TV sends me messages; I know that Satan controls my mind Suspiciousness/ Paranoia I have thought that I’m feel slightly guarded cameras may be with my peers; people monitoring me; people may dislike me may have it in for me Grandiosity/ Inflated Sense of Self I think I can make the honor roll even though my grades are poor Perceptual Abnormalities I see shadows out of the Noises/lights bother me corner of my eyes; I hear more than they used to whispers; I hear voices but they’re in my head I hear 3 voices - they’re real people and bad things will happen if I don’t do what they say Disorganized Communication Speaks clearly, sometimes uses a word or phrase that doesn’t fit Has unintelligible speech that is not responsive to outside attempts to structure I’m smarter than my peers & will make great changes in the world, but tend not to tell people Goes off track when speaking, jumps to different topics, can respond to structure I know that my neighbors are conspiring to kill me I know that I’m famous; I have the power to control the space-time continuum
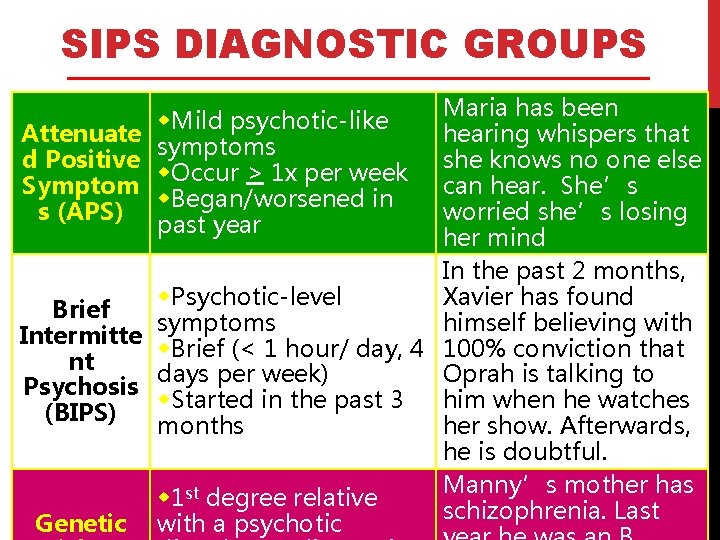
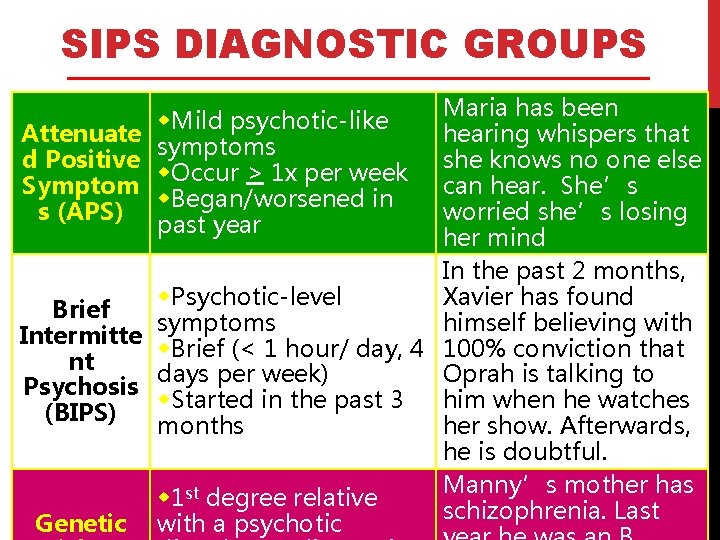
SIPS DIAGNOSTIC GROUPS Maria has been hearing whispers that she knows no one else can hear. She’s worried she’s losing her mind In the past 2 months, w. Psychotic-level Xavier has found Brief symptoms himself believing with Intermitte w. Brief (< 1 hour/ day, 4 100% conviction that nt days per week) Oprah is talking to Psychosis w. Started in the past 3 him when he watches (BIPS) months her show. Afterwards, he is doubtful. Manny’s mother has w 1 st degree relative schizophrenia. Last Genetic with a psychotic w. Mild psychotic-like Attenuate symptoms d Positive w. Occur > 1 x per week Symptom w. Began/worsened in s (APS) past year
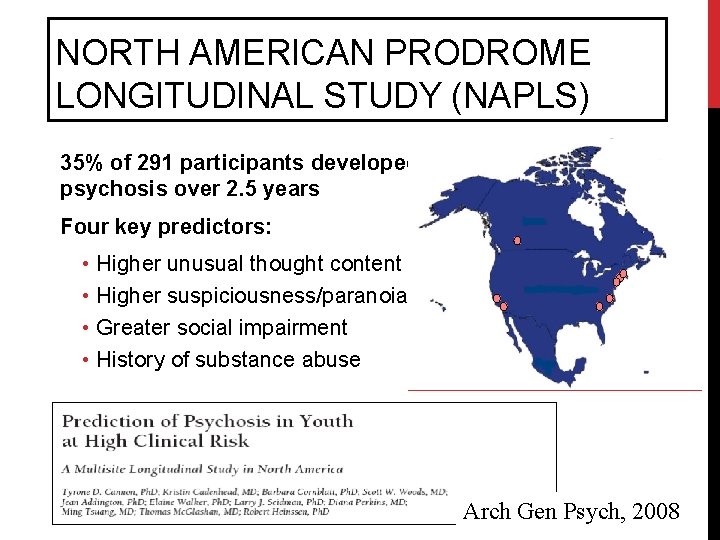
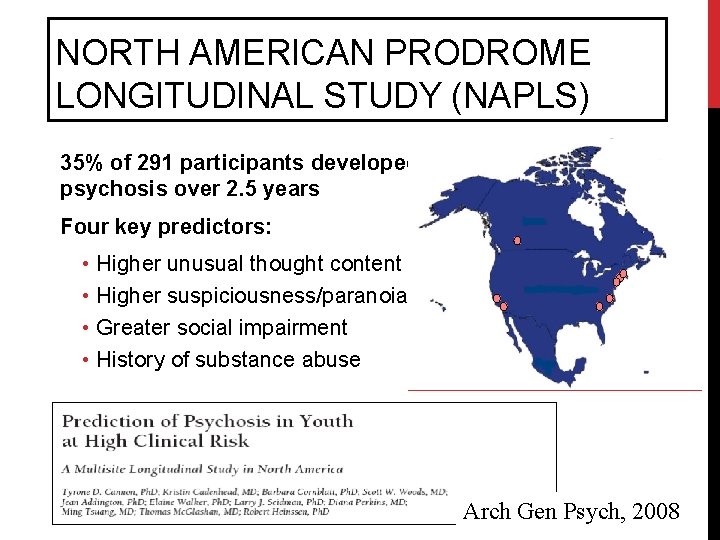
NORTH AMERICAN PRODROME LONGITUDINAL STUDY (NAPLS) 35% of 291 participants developed psychosis over 2. 5 years Four key predictors: • Higher unusual thought content • Higher suspiciousness/paranoia • Greater social impairment • History of substance abuse Arch Gen Psych, 2008
3. YOU CAN LEARN HOW TO TALK TO YOUNG PEOPLE AND FAMILIES ABOUT THESE EXPERIENCES.
CASE EXAMPLE Alicia is a 14 -year-old who enjoys art, riding horses, and spending time online. She’s always struggled to connect with peers. Alicia’s mom reports that she’s always been close to her family but that lately, Alicia expresses no interest in participating in family activities she used to enjoy. Alicia’s mom has also reported that Alicia has begun needing multiple prompts to complete activities of daily living; unprompted, she will go days without showering or changing her clothes. Over the past year, Alicia’s mom and teachers have noticed that she is spending more and more time on the Internet, and that she talks often about websites like Slender Man and Creepypasta. Alicia wrote a long, detailed story about being a character in Slender Man a few months ago, and thinks there’s a possibility that Slender Man’s world is actually the real world and that this world is fake.
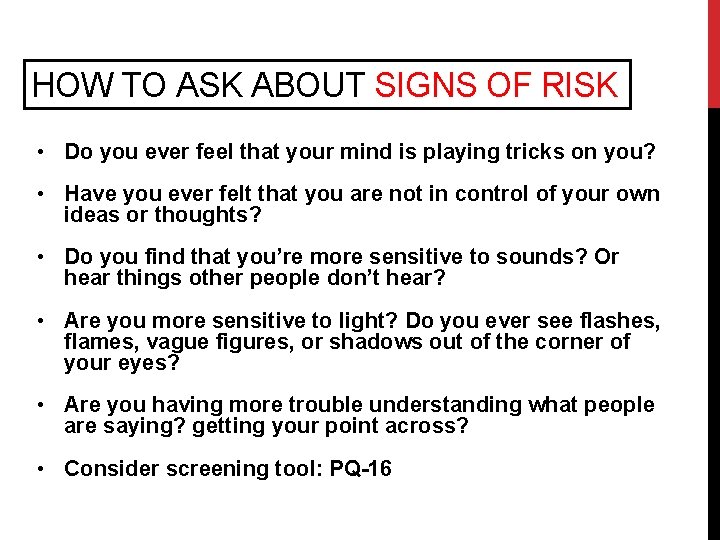
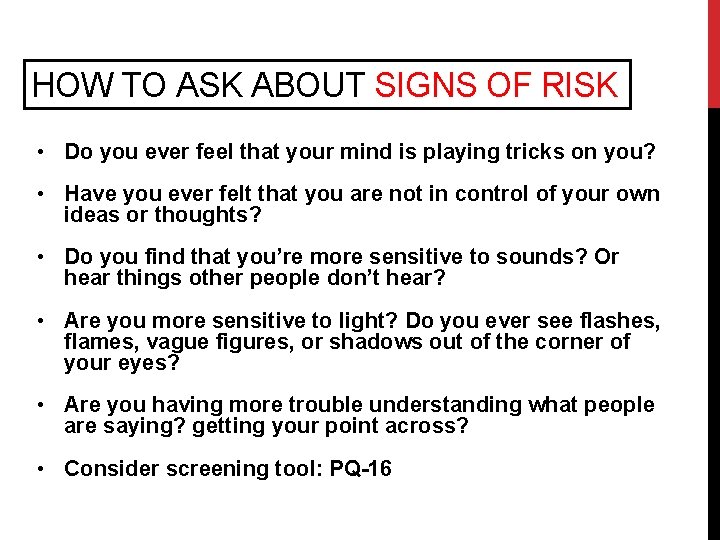
HOW TO ASK ABOUT SIGNS OF RISK • Do you ever feel that your mind is playing tricks on you? • Have you ever felt that you are not in control of your own ideas or thoughts? • Do you find that you’re more sensitive to sounds? Or hear things other people don’t hear? • Are you more sensitive to light? Do you ever see flashes, flames, vague figures, or shadows out of the corner of your eyes? • Are you having more trouble understanding what people are saying? getting your point across? • Consider screening tool: PQ-16
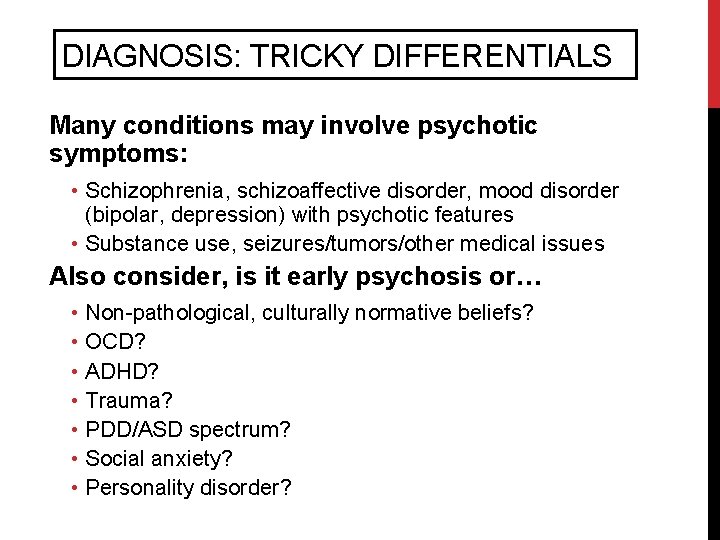
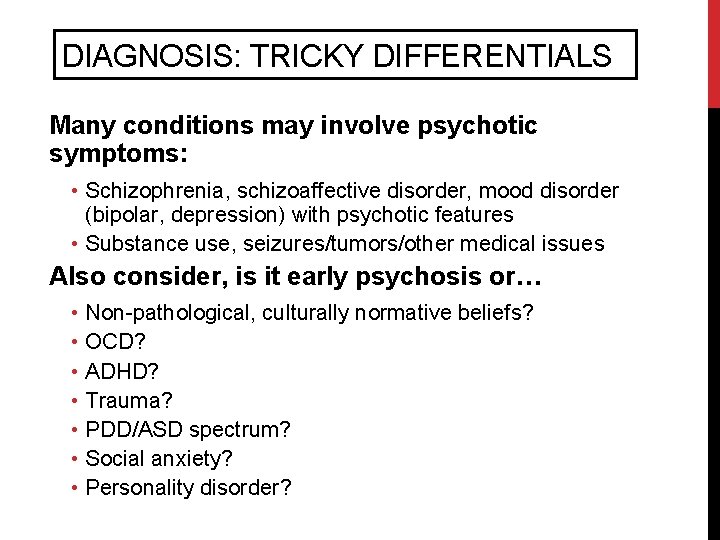
DIAGNOSIS: TRICKY DIFFERENTIALS Many conditions may involve psychotic symptoms: • Schizophrenia, schizoaffective disorder, mood disorder (bipolar, depression) with psychotic features • Substance use, seizures/tumors/other medical issues Also consider, is it early psychosis or… • Non-pathological, culturally normative beliefs? • OCD? • ADHD? • Trauma? • PDD/ASD spectrum? • Social anxiety? • Personality disorder?
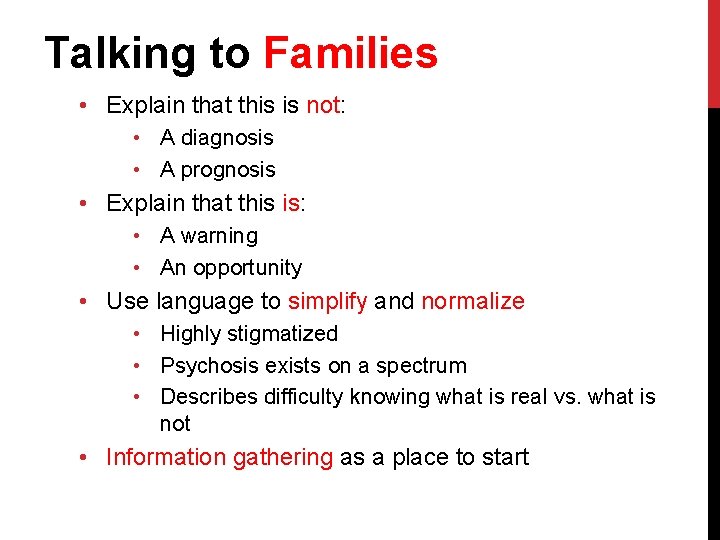
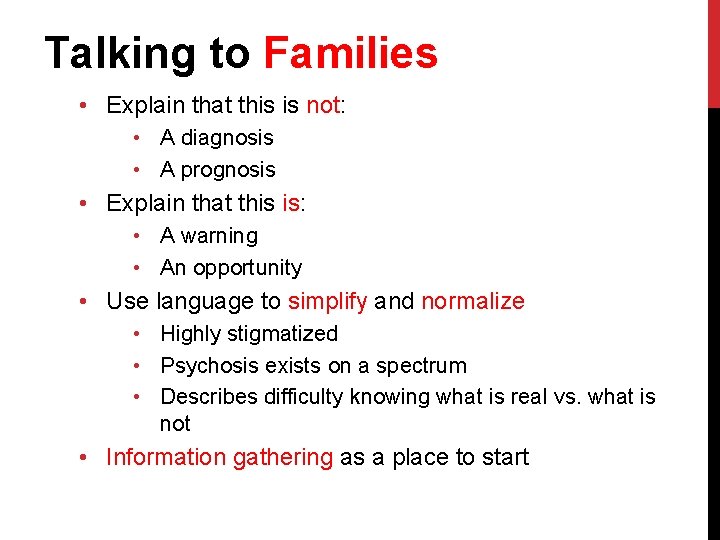
Talking to Families • Explain that this is not: • A diagnosis • A prognosis • Explain that this is: • A warning • An opportunity • Use language to simplify and normalize • Highly stigmatized • Psychosis exists on a spectrum • Describes difficulty knowing what is real vs. what is not • Information gathering as a place to start
4. EARLY INTERVENTION IS POSSIBLE AND CAN REDUCE SUFFERING AND DISABILITY.
CRITICAL PERIOD FOR INTERVENTION • Greatest deterioration first 2 years • Evidence of cognitive & brain deterioration in early stages of psychosis • Losses in social and role functioning • Early treatment can relieve suffering, prevent disability, and possibly prevent psychosis However, there are many obstacles to receiving specialized early psychosis treatment.

Alienation from medical system Stigma Lack of insight (client and/or family) Obstacles To Early Treatment Clinician reluctance/ lack of info
TREATMENT RESEARCH SO FAR Preliminary evidence for • • Cognitive behavioral therapy (CBT) Family education/support Omega 3 fatty acids Low dose antipsychotic medications Several Important Outcomes: Conversion to psychosis, positive/negative symptoms, social/role functioning, cognition Preti and Cella, 2010
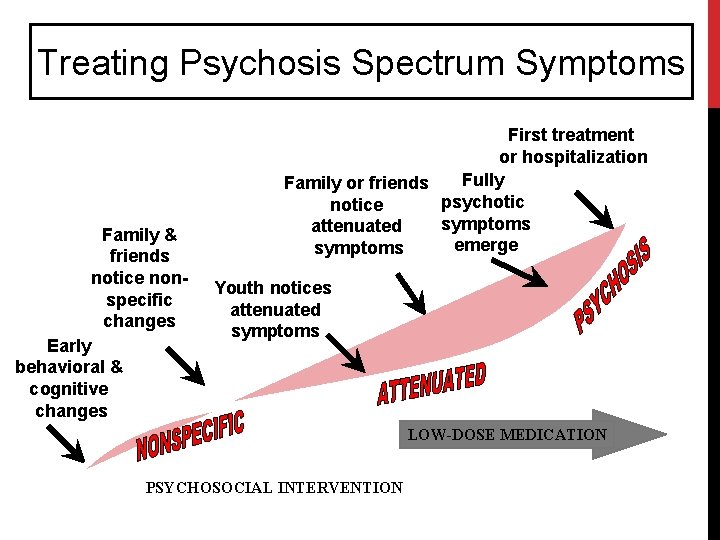
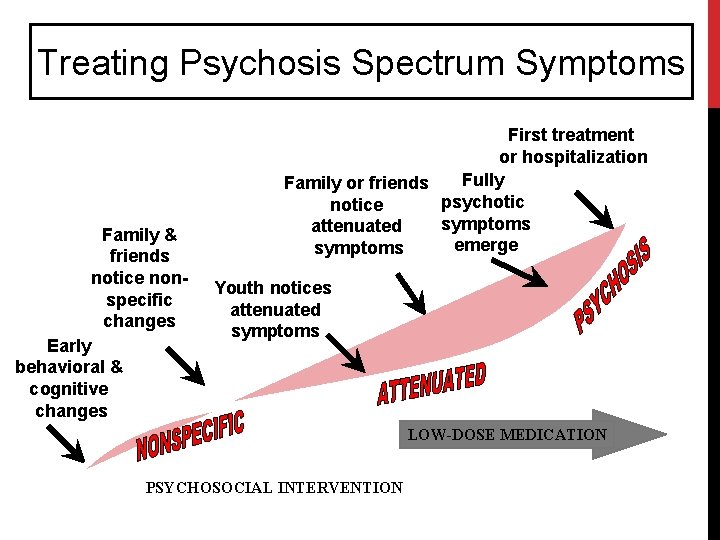
Treating Psychosis Spectrum Symptoms Family & friends notice nonspecific changes Early behavioral & cognitive changes First treatment or hospitalization Fully Family or friends psychotic notice symptoms attenuated emerge symptoms Youth notices attenuated symptoms MEDICATION LOW-DOSE MEDICATION PSYCHOSOCIAL INTERVENTION Adapted from Cornblatt et al
Our Early Psychosis Programs CEDAR CLINIC & RESEARCH PROGRAM PREP © PROGRAM

CEDAR CLINIC & RESEARCH PROGRAM CENTER FOR EARLY DETECTION, ASSESSMENT, & RESPONSE TO RISK www. cedarclinic. org
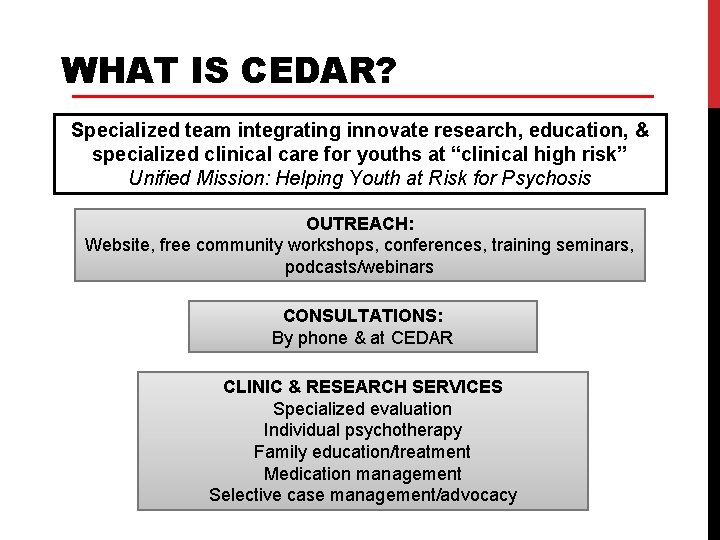
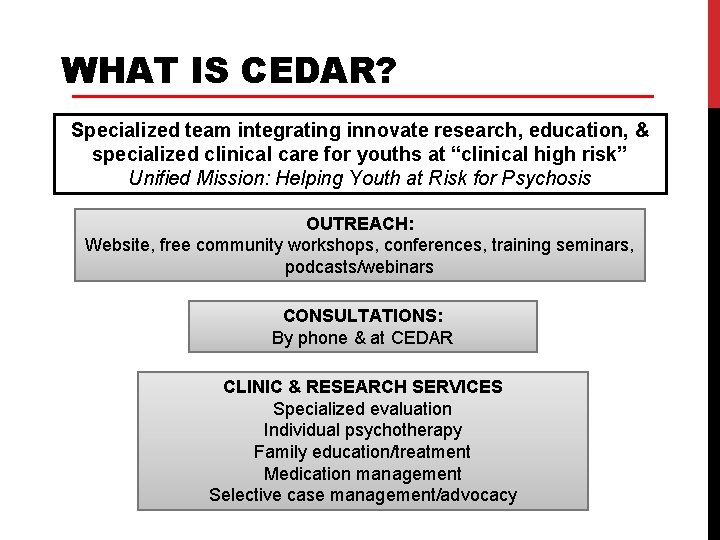
WHAT IS CEDAR? Specialized team integrating innovate research, education, & specialized clinical care for youths at “clinical high risk” Unified Mission: Helping Youth at Risk for Psychosis OUTREACH: Website, free community workshops, conferences, training seminars, podcasts/webinars CONSULTATIONS: By phone & at CEDAR CLINIC & RESEARCH SERVICES Specialized evaluation Individual psychotherapy Family education/treatment Medication management Selective case management/advocacy
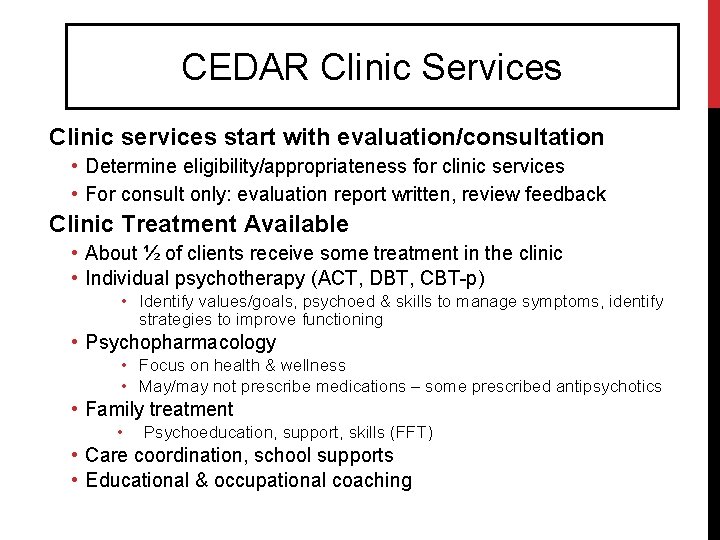
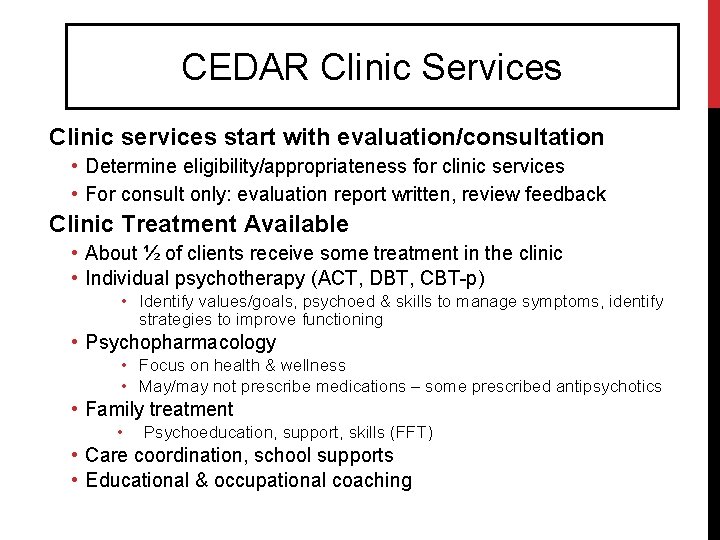
CEDAR Clinic Services Clinic services start with evaluation/consultation • Determine eligibility/appropriateness for clinic services • For consult only: evaluation report written, review feedback Clinic Treatment Available • About ½ of clients receive some treatment in the clinic • Individual psychotherapy (ACT, DBT, CBT-p) • Identify values/goals, psychoed & skills to manage symptoms, identify strategies to improve functioning • Psychopharmacology • Focus on health & wellness • May/may not prescribe medications – some prescribed antipsychotics • Family treatment • Psychoeducation, support, skills (FFT) • Care coordination, school supports • Educational & occupational coaching
© PREP PROGRAM PREVENTION & RECOVERY IN EARLY PSYCHOSIS
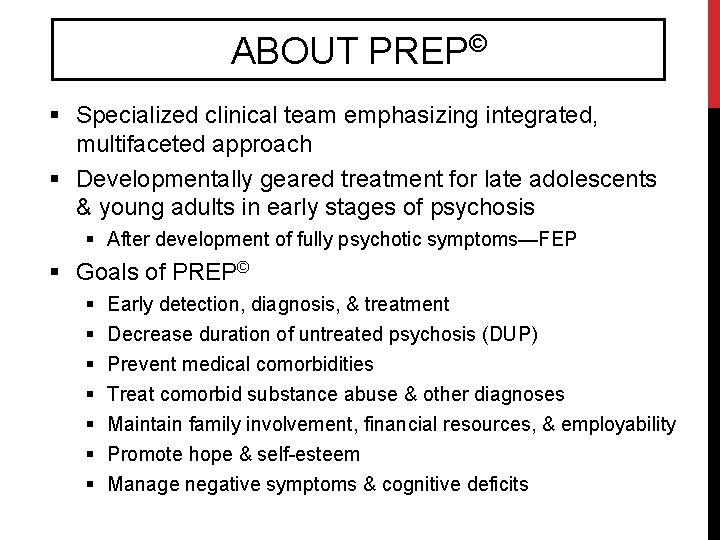
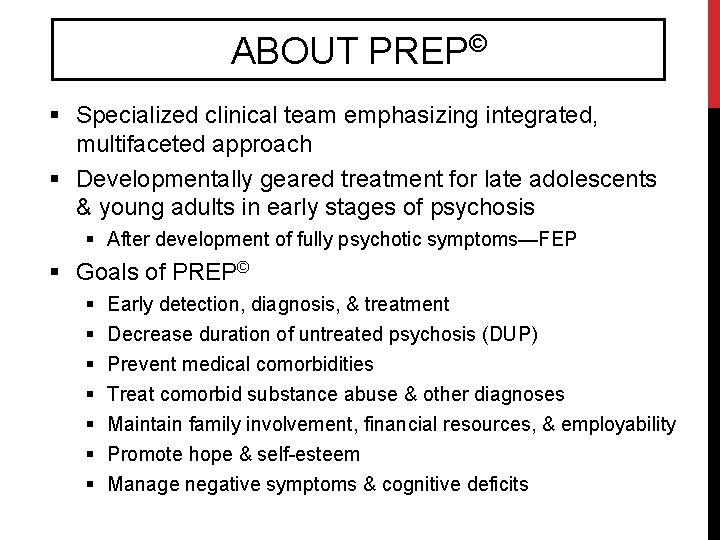
ABOUT PREP© § Specialized clinical team emphasizing integrated, multifaceted approach § Developmentally geared treatment for late adolescents & young adults in early stages of psychosis § After development of fully psychotic symptoms—FEP § Goals of PREP© § § § § Early detection, diagnosis, & treatment Decrease duration of untreated psychosis (DUP) Prevent medical comorbidities Treat comorbid substance abuse & other diagnoses Maintain family involvement, financial resources, & employability Promote hope & self-esteem Manage negative symptoms & cognitive deficits
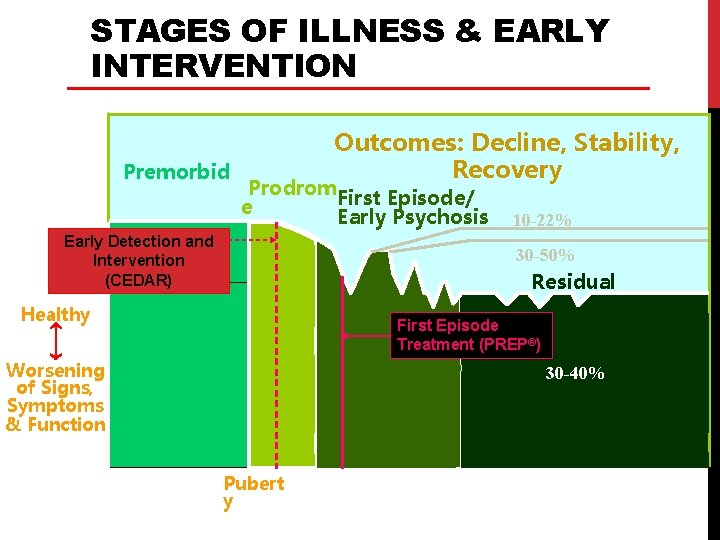
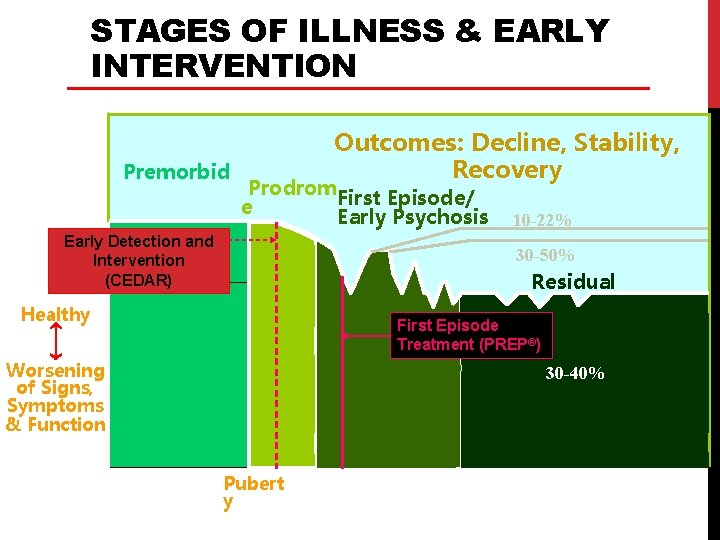
STAGES OF ILLNESS & EARLY INTERVENTION Premorbid Outcomes: Decline, Stability, Recovery Prodrom First Episode/ e Early Psychosis Early Detection 30 -50% and Intervention stable good (CEDAR) 10 -22% 30 -50% Residual Healthy First Episode Treatment (PREP®) Worsening of Signs, Symptoms & Function Gestation/Birth 10 30 -40% Pubert y Adapted from Lieberman et al. 20 30 Age in Years 40 50
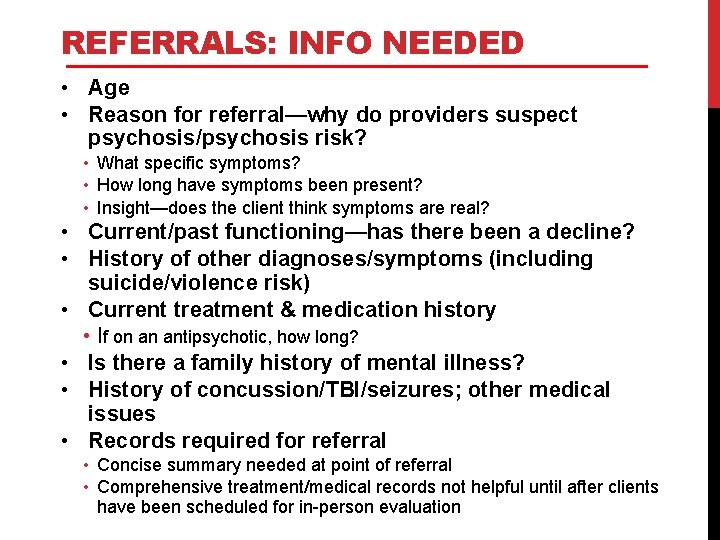
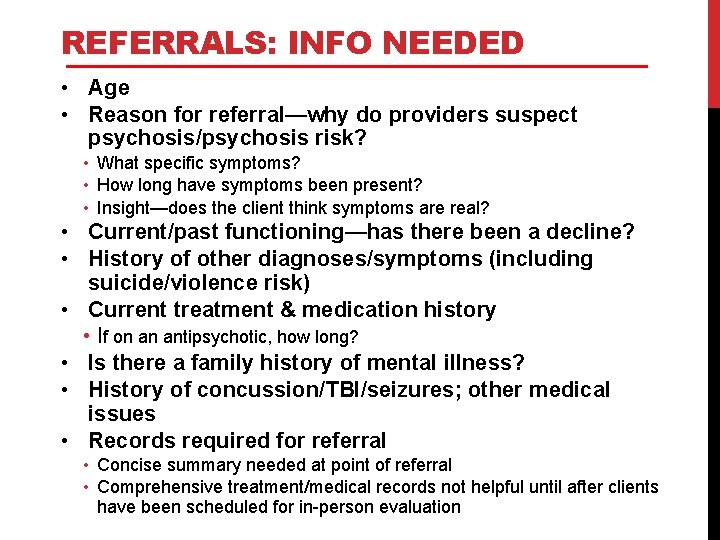
REFERRALS: INFO NEEDED • Age • Reason for referral—why do providers suspect psychosis/psychosis risk? • What specific symptoms? • How long have symptoms been present? • Insight—does the client think symptoms are real? • Current/past functioning—has there been a decline? • History of other diagnoses/symptoms (including suicide/violence risk) • Current treatment & medication history • If on an antipsychotic, how long? • Is there a family history of mental illness? • History of concussion/TBI/seizures; other medical issues • Records required for referral • Concise summary needed at point of referral • Comprehensive treatment/medical records not helpful until after clients have been scheduled for in-person evaluation
CASE EXAMPLES: DIFFERENTIAL DIAGNOSIS
Case Example: “Andy” 16 year-old White male 10 th grade student Referred by his DYS team Currently living at a residential program for DYS-involved boys Otherwise lives with mother & grandmother (father currently incarcerated) History of 2 arrests, both for assault-related charges Long-standing difficulties with attention in school, work completion Long-standing irritable mood & behavioral problems across contexts (e. g. , threats to harm self/others, aggressive behavior, rare self-injury) 1 minor head injury within the past year Past year: reported hearing whispers (1 x/week), ignores them Endorsed drinking alcohol, denied other substances Family history positive for mental health difficulties, including “anger problems” & substance use disorder (father)

CASE EXAMPLE: “COLIN” 21 year-old Hispanic man Self-referred Currently living with his mother; working part time History of marijuana and opiate use Reports feeling depressed, down on his luck, and unable to follow through on daily responsibilities/goals he’s set Has moved several times due to thoughts that he’s being watched Reports that God told him his previous apartment was dangerous Often gets off the T and changes direction of travel because he believes the CIA or the Feds are watching and following him Reports that he time travels and knows this because he leaves himself clues in different dimensions Reports that he doesn’t want people to “think he’s crazy”
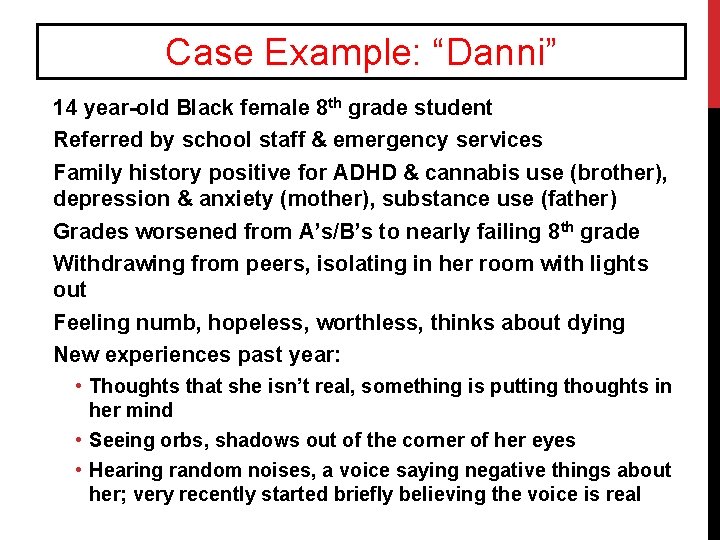
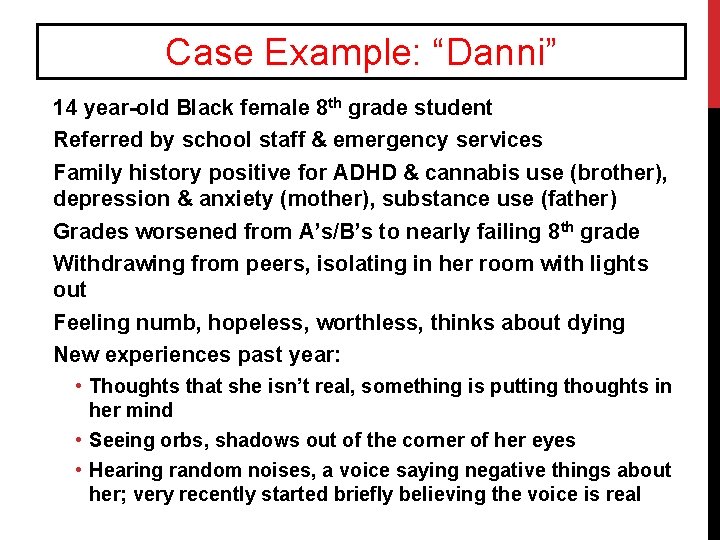
Case Example: “Danni” 14 year-old Black female 8 th grade student Referred by school staff & emergency services Family history positive for ADHD & cannabis use (brother), depression & anxiety (mother), substance use (father) Grades worsened from A’s/B’s to nearly failing 8 th grade Withdrawing from peers, isolating in her room with lights out Feeling numb, hopeless, worthless, thinks about dying New experiences past year: • Thoughts that she isn’t real, something is putting thoughts in her mind • Seeing orbs, shadows out of the corner of her eyes • Hearing random noises, a voice saying negative things about her; very recently started briefly believing the voice is real
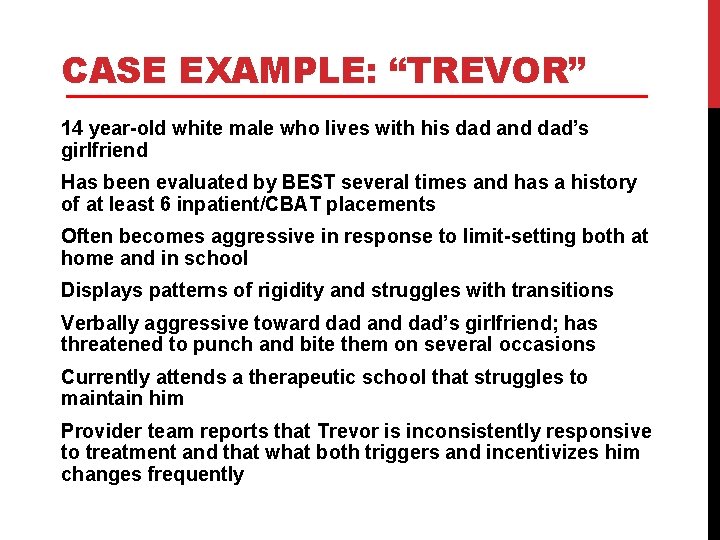
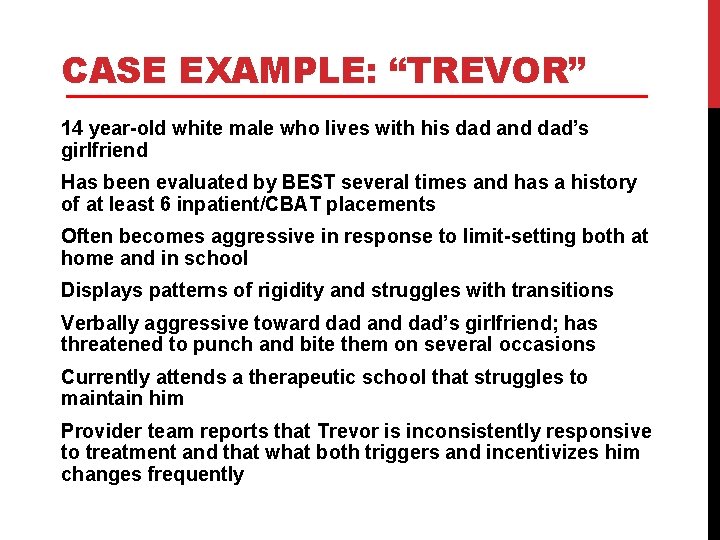
CASE EXAMPLE: “TREVOR” 14 year-old white male who lives with his dad and dad’s girlfriend Has been evaluated by BEST several times and has a history of at least 6 inpatient/CBAT placements Often becomes aggressive in response to limit-setting both at home and in school Displays patterns of rigidity and struggles with transitions Verbally aggressive toward dad and dad’s girlfriend; has threatened to punch and bite them on several occasions Currently attends a therapeutic school that struggles to maintain him Provider team reports that Trevor is inconsistently responsive to treatment and that what both triggers and incentivizes him changes frequently
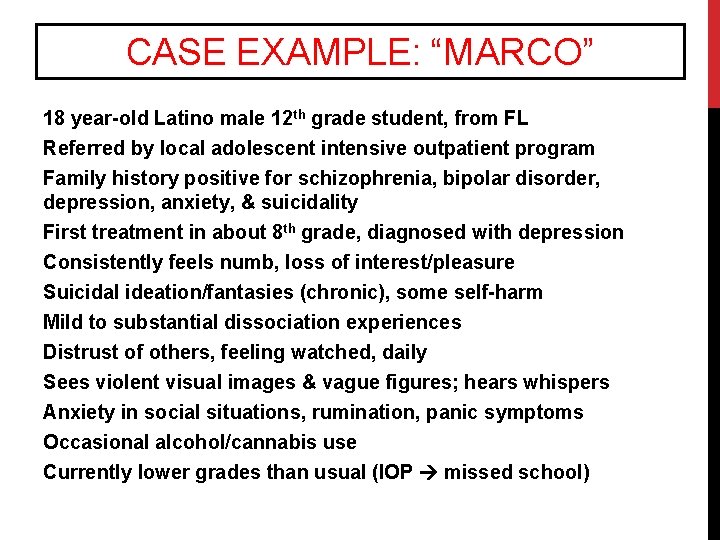
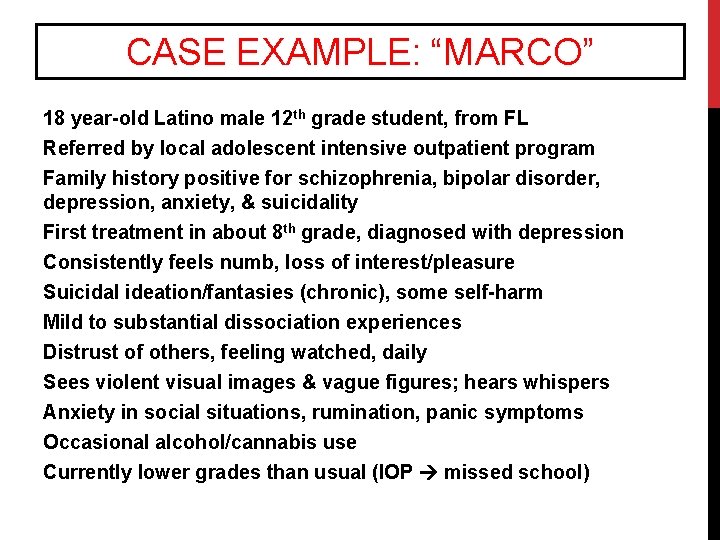
CASE EXAMPLE: “MARCO” 18 year-old Latino male 12 th grade student, from FL Referred by local adolescent intensive outpatient program Family history positive for schizophrenia, bipolar disorder, depression, anxiety, & suicidality First treatment in about 8 th grade, diagnosed with depression Consistently feels numb, loss of interest/pleasure Suicidal ideation/fantasies (chronic), some self-harm Mild to substantial dissociation experiences Distrust of others, feeling watched, daily Sees violent visual images & vague figures; hears whispers Anxiety in social situations, rumination, panic symptoms Occasional alcohol/cannabis use Currently lower grades than usual (IOP missed school)
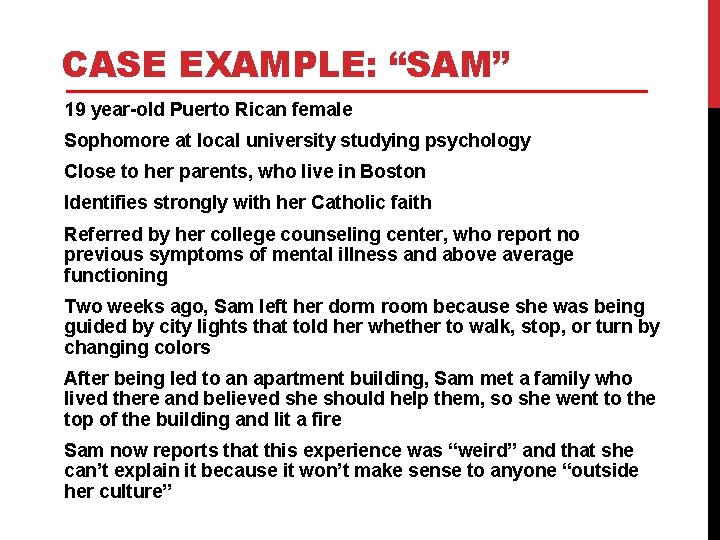
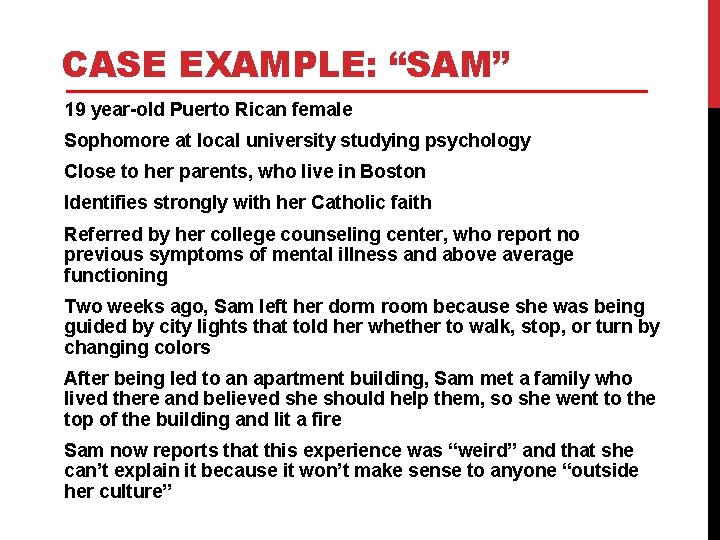
CASE EXAMPLE: “SAM” 19 year-old Puerto Rican female Sophomore at local university studying psychology Close to her parents, who live in Boston Identifies strongly with her Catholic faith Referred by her college counseling center, who report no previous symptoms of mental illness and above average functioning Two weeks ago, Sam left her dorm room because she was being guided by city lights that told her whether to walk, stop, or turn by changing colors After being led to an apartment building, Sam met a family who lived there and believed she should help them, so she went to the top of the building and lit a fire Sam now reports that this experience was “weird” and that she can’t explain it because it won’t make sense to anyone “outside her culture”
QUESTIONS?
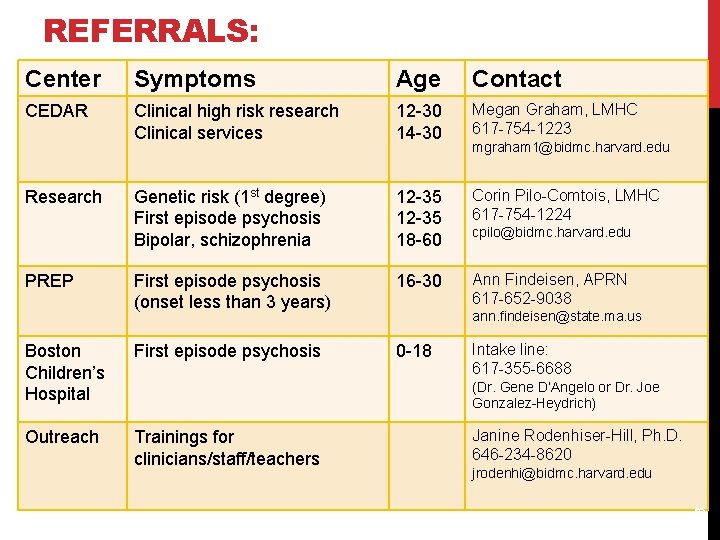
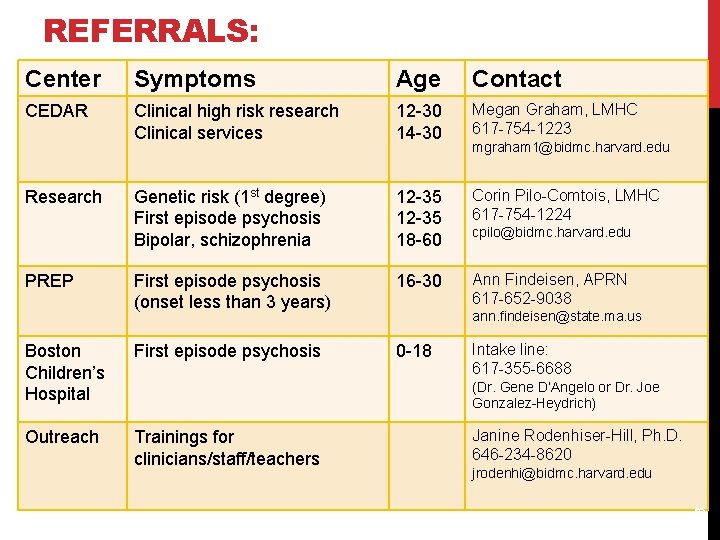
REFERRALS: Center Symptoms Age Contact CEDAR Clinical high risk research Clinical services 12 -30 14 -30 Megan Graham, LMHC 617 -754 -1223 Genetic risk (1 st degree) First episode psychosis Bipolar, schizophrenia 12 -35 18 -60 Corin Pilo-Comtois, LMHC 617 -754 -1224 First episode psychosis (onset less than 3 years) 16 -30 Ann Findeisen, APRN 617 -652 -9038 Boston Children’s Hospital First episode psychosis 0 -18 Outreach Trainings for clinicians/staff/teachers PREP cpilo@bidmc. harvard. edu ann. findeisen@state. ma. us Intake line: 617 -355 -6688 (Dr. Gene D’Angelo or Dr. Joe Gonzalez-Heydrich) Janine Rodenhiser-Hill, Ph. D. 646 -234 -8620 jrodenhi@bidmc. harvard. edu 43 Research mgraham 1@bidmc. harvard. edu
 Signs signs everywhere signs meaning
Signs signs everywhere signs meaning Psychosis and ptsd
Psychosis and ptsd Types of psychosis and neurosis
Types of psychosis and neurosis Mutilomania
Mutilomania Neurosis vs psychosis
Neurosis vs psychosis Difference between psychosis and neurosis
Difference between psychosis and neurosis Neurosis vs psychosis
Neurosis vs psychosis Difference between neurosis and psychosis
Difference between neurosis and psychosis Natural signs in semantics
Natural signs in semantics Types of psychosis
Types of psychosis Mild psychosis
Mild psychosis Culture bound syndrome examples
Culture bound syndrome examples Neurosis vs psychosis
Neurosis vs psychosis Dopamine hypothesis of schizophrenia ppt
Dopamine hypothesis of schizophrenia ppt First episode psychosis
First episode psychosis First episode psychosis
First episode psychosis Dena schlosser autopsy
Dena schlosser autopsy Postictal psychosis
Postictal psychosis How do you get schizophrenia
How do you get schizophrenia Functional psychosis
Functional psychosis Infantile autism
Infantile autism Jansen orfan
Jansen orfan What is psychosis
What is psychosis Railroad signs and meanings
Railroad signs and meanings The octagon shape is used exclusively for
The octagon shape is used exclusively for Harmful or useful
Harmful or useful Observing trends in entrepreneurship example
Observing trends in entrepreneurship example An opportunity has four essential qualities it is
An opportunity has four essential qualities it is Recognising opportunities
Recognising opportunities Recognizing and resolving abo discrepancies
Recognizing and resolving abo discrepancies Communicative stimulus-response tasks
Communicative stimulus-response tasks Recognizing opportunities and generating ideas
Recognizing opportunities and generating ideas Manipulated variable and responding variable graph
Manipulated variable and responding variable graph Manipulated variable and responding variable graph
Manipulated variable and responding variable graph Expression of congratulations
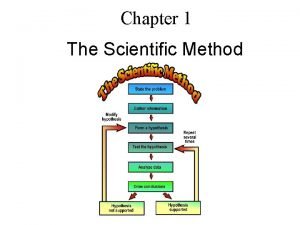
Expression of congratulations What is the fourth step of the scientific method
What is the fourth step of the scientific method Manipulated and responding variables examples
Manipulated and responding variables examples Making and responding to requests 2 bac
Making and responding to requests 2 bac These are techniques or activities that contribute directly
These are techniques or activities that contribute directly Recognizing opportunity
Recognizing opportunity Recognizing genre - argumentative text
Recognizing genre - argumentative text Developing possible alternative channel structures
Developing possible alternative channel structures Recognizing lab safety worksheet answer
Recognizing lab safety worksheet answer Chapter 3 recognizing opportunity
Chapter 3 recognizing opportunity