Drug Overdose Prevention Program Training Module Illinois Department



- Slides: 28
Drug Overdose Prevention Program Training Module Illinois Department of Human Services Division of Alcoholism and Substance Abuse Dr. Seth Eisenberg, MD Rosie Gianforte, LCSW
TOPICS • • • Overview of the Heroin/Opiate Problem Identifying Opioid Overdoses How to Respond to an Overdose Use of Naloxone After Naloxone – Outreach Efforts/Treatment Referrals
Opioids • Opioids are a type of drugs in both legal (prescription medications such as oxycodone, hydrocodone, morphine, fentanyl) and illegal(heroin) forms. • Opioids are natural or synthetic substances that act on the brain • Opioids dull pain and relieve anxiety. • People may misuse opioids because they are in pain (physical and emotional) and opioids produce a relaxed feeling.
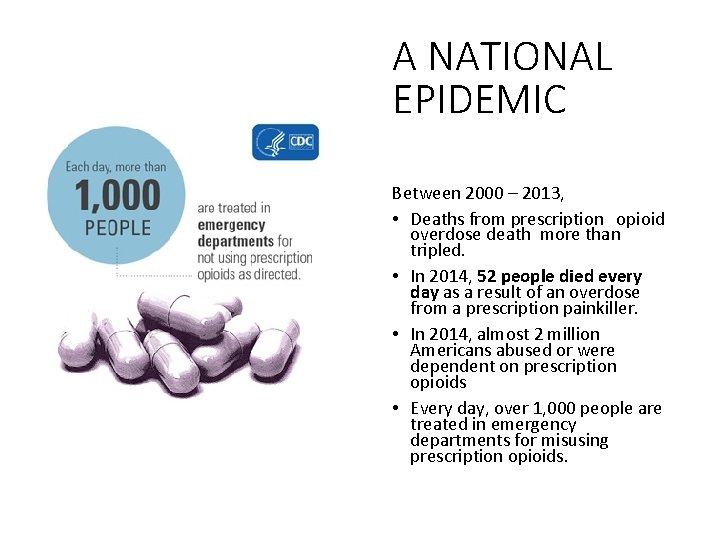
A NATIONAL EPIDEMIC Between 2000 – 2013, • Deaths from prescription opioid overdose death more than tripled. • In 2014, 52 people died every day as a result of an overdose from a prescription painkiller. • In 2014, almost 2 million Americans abused or were dependent on prescription opioids • Every day, over 1, 000 people are treated in emergency departments for misusing prescription opioids.
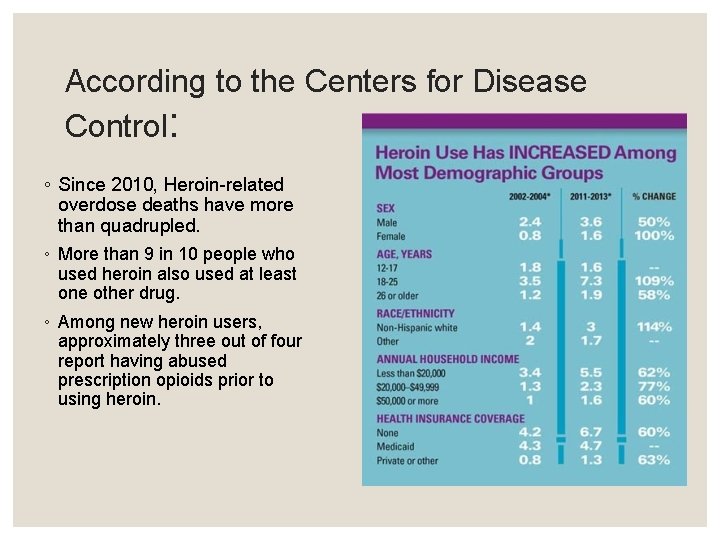
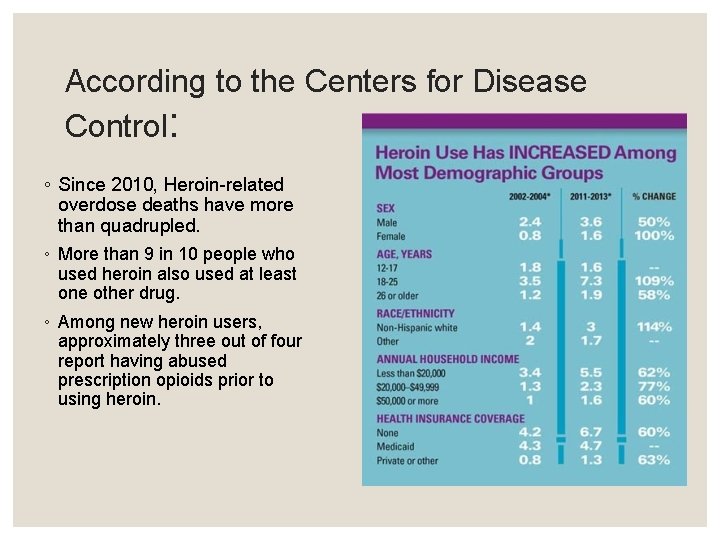
According to the Centers for Disease Control: ◦ Since 2010, Heroin-related overdose deaths have more than quadrupled. ◦ More than 9 in 10 people who used heroin also used at least one other drug. ◦ Among new heroin users, approximately three out of four report having abused prescription opioids prior to using heroin.
IN ILLINOIS – the Opiate crisis 2013 - 2015 ◦ Illinois was one of 14 states with the highest increases in overall drug overdose deaths between 2013 and 2014. ◦ Opioid drug overdoses killed 45% more people than homicides ◦ The Chicago Metropolitan area ranks first nationwide in emergency departmentions for heroin use. ◦ Cook County ranks first in the nation for percentage of arrestees testing positive for opiates. ◦ Illinois is one of 16 states in which more people die of dug overdose than car crashes. Source: Illinois Department of Public Health
Who is at risk of an overdose? ◦ Switching between prescriptions ◦ Mixing opioids with other prescriptions ◦ People with chronic medical conditions (HIV, cardiovascular or respiratory disease, mental illnesses) ◦ Recently released from incarceration and in-patient tx programs. ◦ Recently completing a mandatory opioid detoxification or having abstained from use for a period of time ◦ Discharge from emergency medical care after opioid intoxication
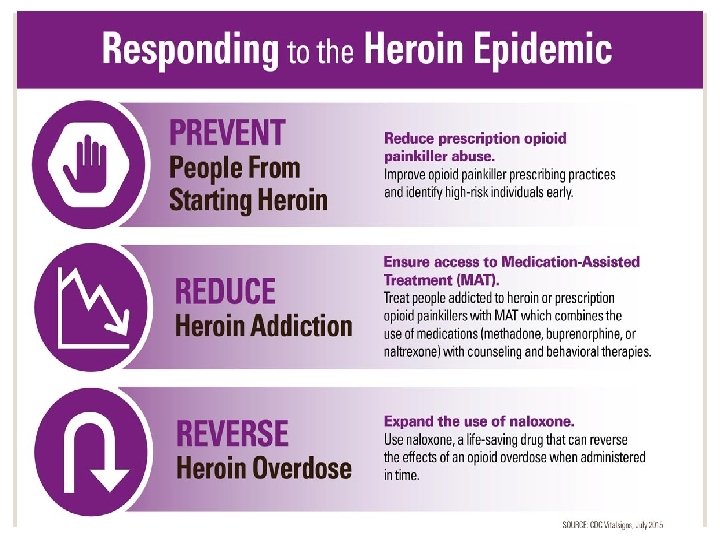
Strategies to prevent overdose death ◦ Talk to people and caregivers about ways to avoid an accidental overdose, especially at discharge: ◦ Do not adjust prescribed dosage, skip doses, or take any extra doses ◦ Do not mix with other dugs and/or alcohol (i. e. anti-anxiety drugs like benzodiazepines, antidepressants, or cocaine) ◦ Abstain from use of opioids unless prescribed, and attempt abstinence from heroin. ◦ Opioid Overdose Prevention Toolkit – 2014

Naloxone Facts • Onset of action is about 2 -3 minute • Duration of action is 30 -120 minutes depending on method of administration • It will not reverse an overdose caused by other drugs, only opioids • May be used in children and pregnant women • Naloxone should be stored in its original packaging, while avoiding light, at room temperature. Ø It can be left in the car glove box overnight, but not as a permanent storage option • Pay attention to the expiration date for any naloxone product. Most have an expiration date of about 12 -18 months. Ø Expired naloxone can still be administered if there is no other alternative available. However, it may not be as effective and a second dose may be required.
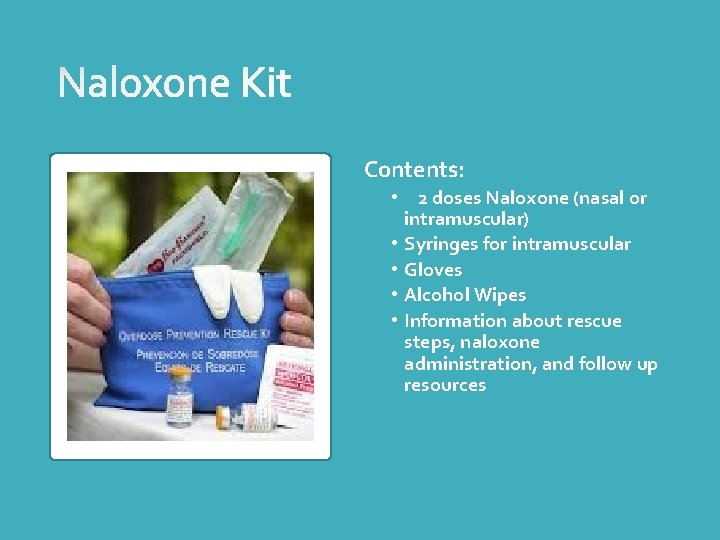
Contents: • 2 doses Naloxone (nasal or intramuscular) • Syringes for intramuscular • Gloves • Alcohol Wipes • Information about rescue steps, naloxone administration, and follow up resources
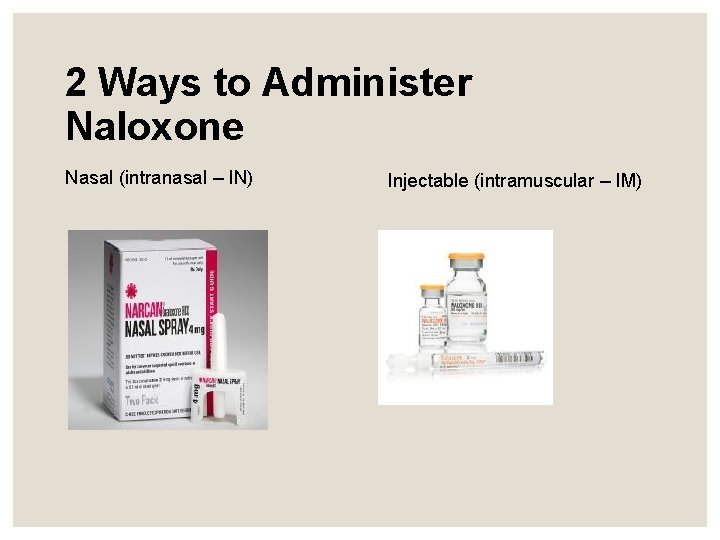
2 Ways to Administer Naloxone Nasal (intranasal – IN) Injectable (intramuscular – IM)
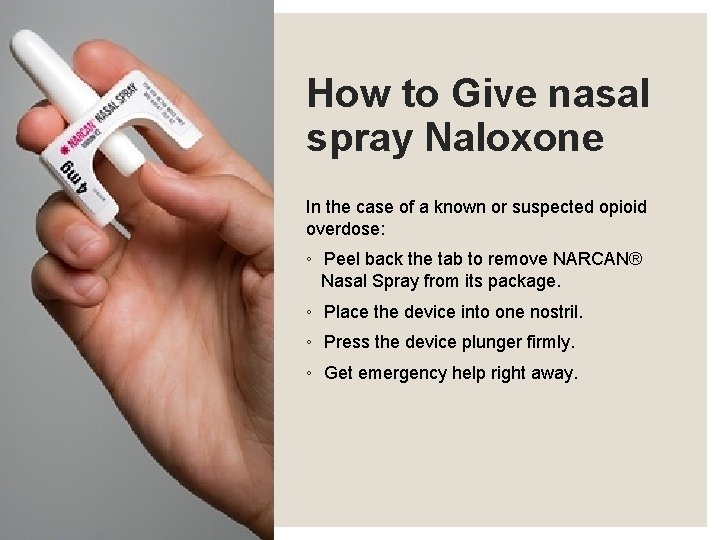
How to Give nasal spray Naloxone In the case of a known or suspected opioid overdose: ◦ Peel back the tab to remove NARCAN® Nasal Spray from its package. ◦ Place the device into one nostril. ◦ Press the device plunger firmly. ◦ Get emergency help right away.


Where to find Naloxone • Funded programs near you: Contact DHS/DASA DHS. DOPP. coordinator@illinois. gov • Ask your medical provider or pharmacy • Go to www. getnaloxonenow. org or www. naloxoneinfo. org • Ideally, naloxone should be available in these settings: • • Syringe Exchange Programs Jails Hospital Emergency Departments Free Clinics First Responders Friends and Family members Methadone, Suboxone and Other Treatment Programs
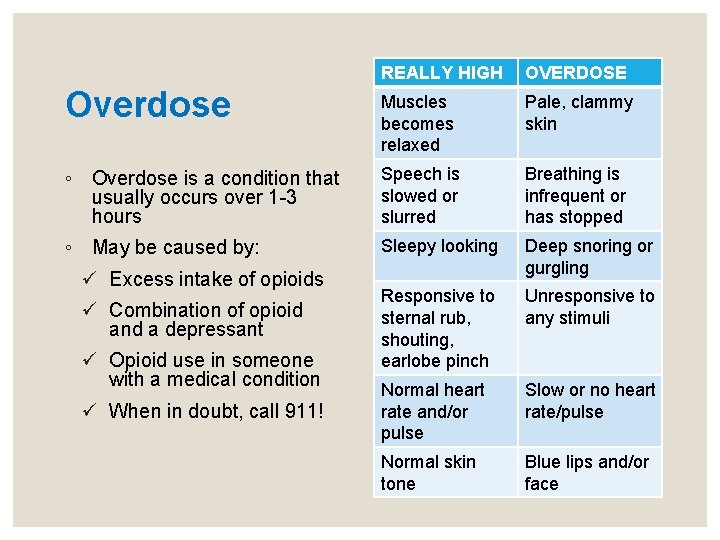
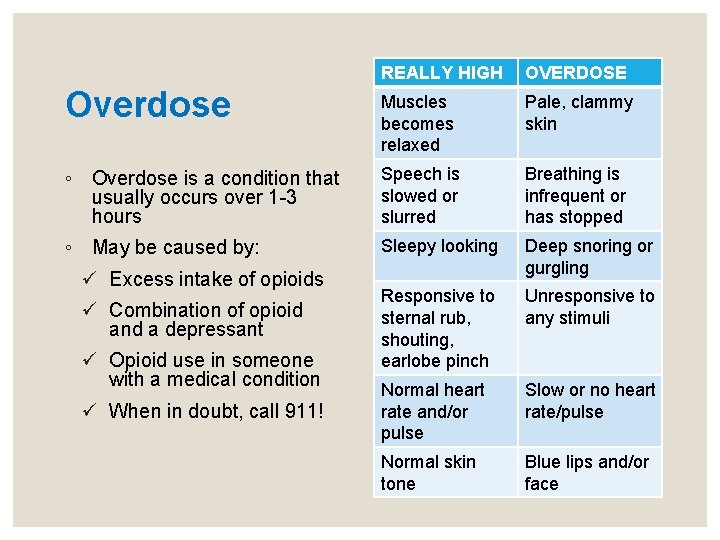
REALLY HIGH OVERDOSE Overdose Muscles becomes relaxed Pale, clammy skin ◦ Overdose is a condition that usually occurs over 1 -3 hours Speech is slowed or slurred Breathing is infrequent or has stopped ◦ May be caused by: Sleepy looking Deep snoring or gurgling Responsive to sternal rub, shouting, earlobe pinch Unresponsive to any stimuli Normal heart rate and/or pulse Slow or no heart rate/pulse Normal skin tone Blue lips and/or face ü Excess intake of opioids ü Combination of opioid and a depressant ü Opioid use in someone with a medical condition ü When in doubt, call 911!
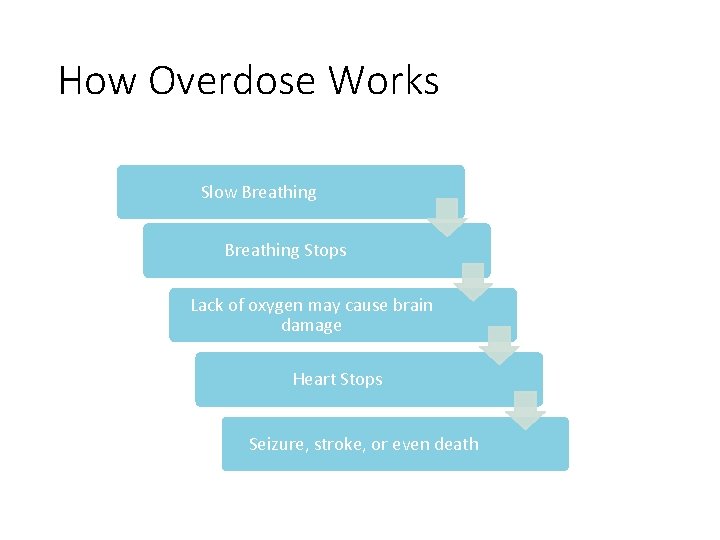
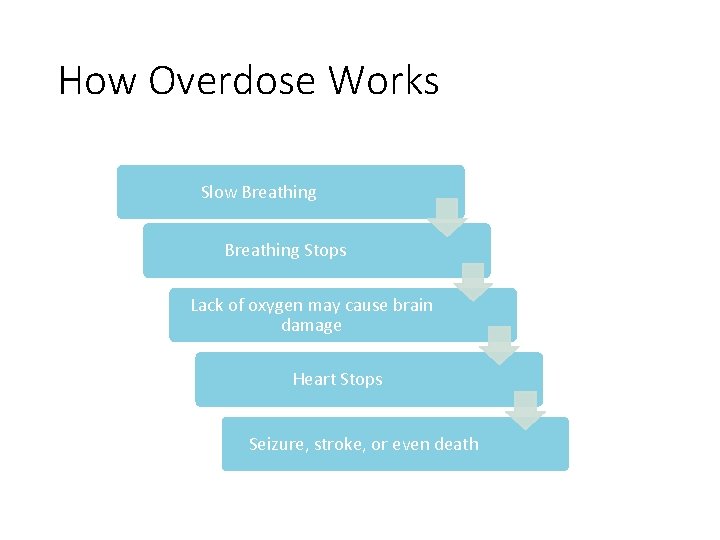
How Overdose Works Slow Breathing Stops Lack of oxygen may cause brain damage Heart Stops Seizure, stroke, or even death
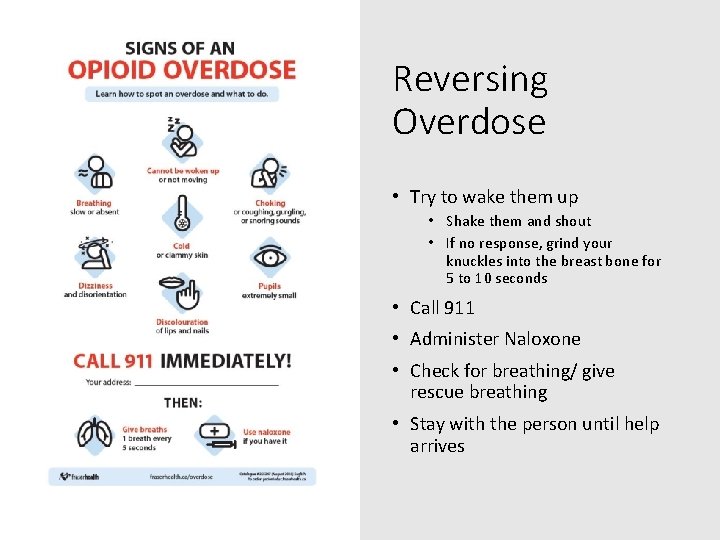
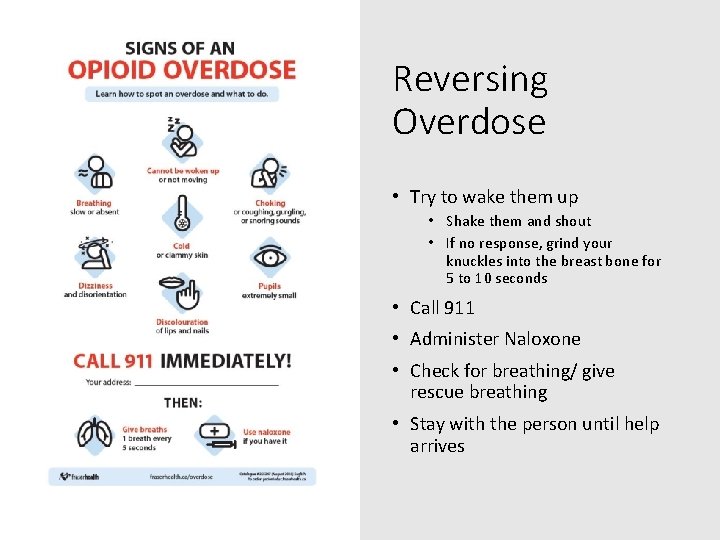
Reversing Overdose • Try to wake them up • Shake them and shout • If no response, grind your knuckles into the breast bone for 5 to 10 seconds • Call 911 • Administer Naloxone • Check for breathing/ give rescue breathing • Stay with the person until help arrives
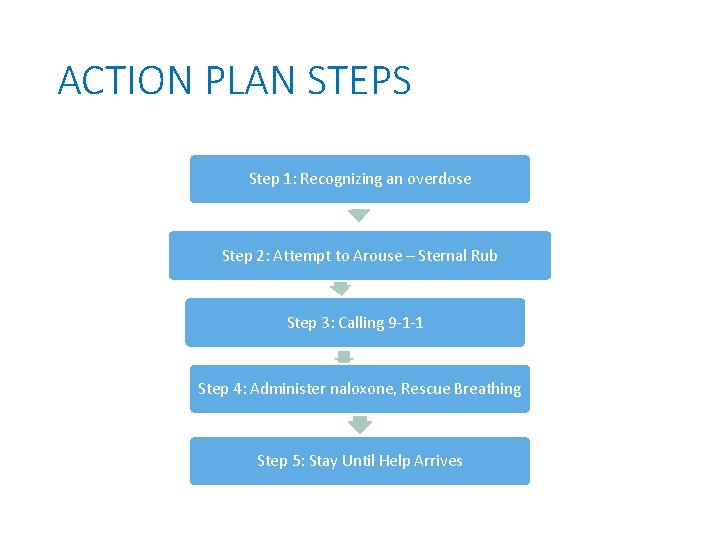
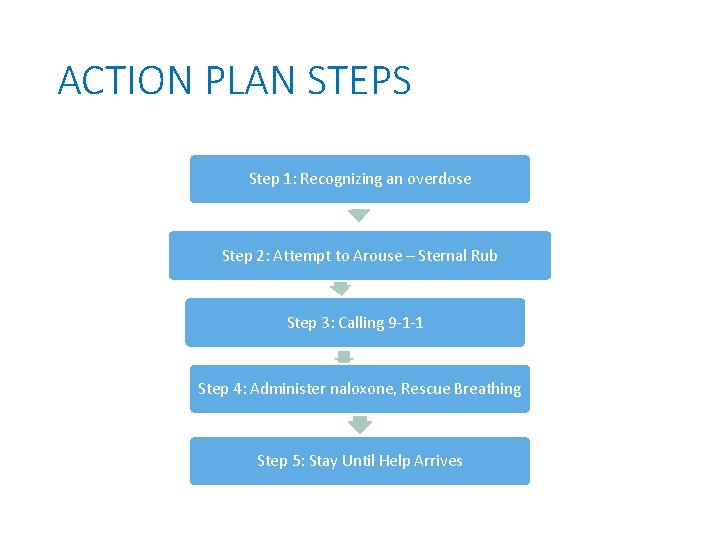
ACTION PLAN STEPS Step 1: Recognizing an overdose Step 2: Attempt to Arouse – Sternal Rub Step 3: Calling 9 -1 -1 Step 4: Administer naloxone, Rescue Breathing Step 5: Stay Until Help Arrives
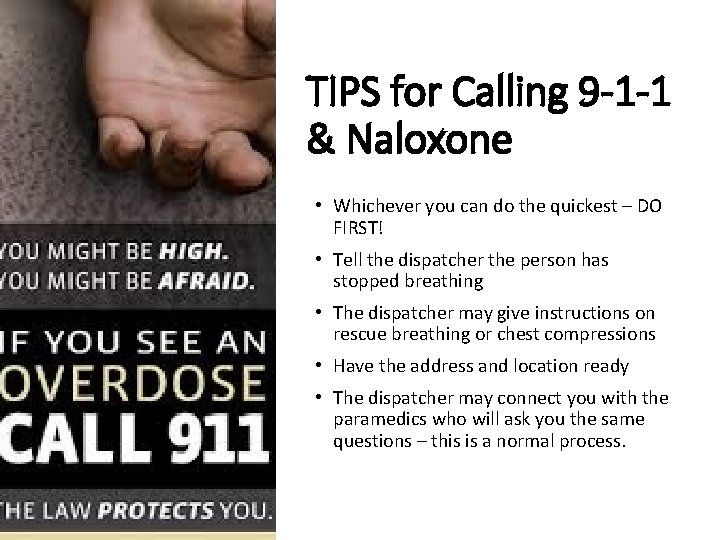
TIPS for Calling 9 -1 -1 & Naloxone • Whichever you can do the quickest – DO FIRST! • Tell the dispatcher the person has stopped breathing • The dispatcher may give instructions on rescue breathing or chest compressions • Have the address and location ready • The dispatcher may connect you with the paramedics who will ask you the same questions – this is a normal process.
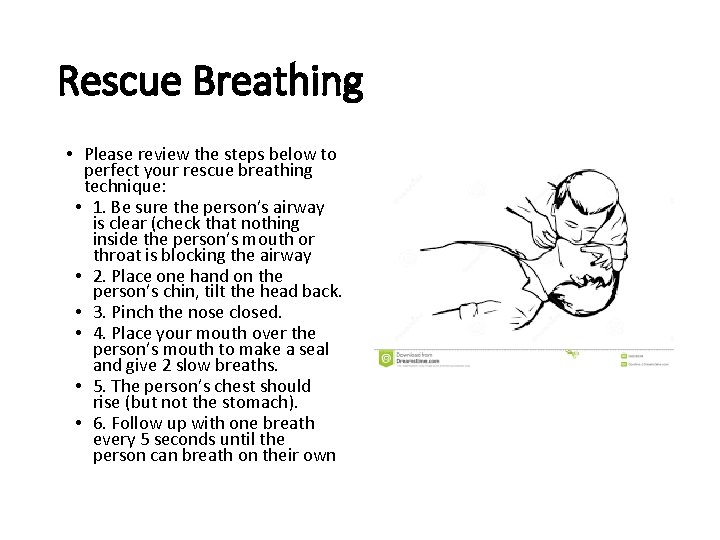
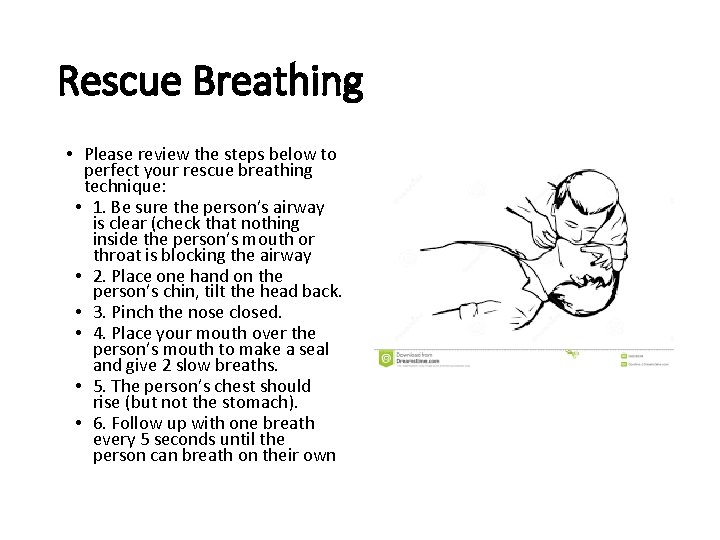
Rescue Breathing • Please review the steps below to perfect your rescue breathing technique: • 1. Be sure the person’s airway is clear (check that nothing inside the person’s mouth or throat is blocking the airway • 2. Place one hand on the person’s chin, tilt the head back. • 3. Pinch the nose closed. • 4. Place your mouth over the person’s mouth to make a seal and give 2 slow breaths. • 5. The person’s chest should rise (but not the stomach). • 6. Follow up with one breath every 5 seconds until the person can breath on their own
While you’re waiting for naloxone to kick in… • Start rescue breathing again until you see the person start to breathe on their own. • Wait 2 -3 minutes (longer if administering IN naloxone) to give the medication a chance to work. • If no response after 2 -3 minutes, give a second dose of naloxone and begin rescue breathing again. • If still no response, continue rescue breathing until paramedics arrive and let them take over. • Note: naloxone will only work if the individual has taken an opioid. If they overdosed on a non-opioid, naloxone will not have an effect on them.
What to expect after administration of naloxone… • Stay with the person for as long as you can or until help arrives • If the person is still unresponsive, make sure to lay them in the recovery position to prevent choking and wait for help. • If the person is responsive, they will be confused about what is happening and will probably not remember overdosing. • Explain what has happened • Comfort the person; withdrawal symptoms triggered by naloxone can feel unpleasant. • Some people may become agitated or combative and will need help remaining calm. • Don’t allow the person to take more opioids, as they can overdose again.
Summary – Do’s and Don’ts • DO support the person’s breathing by administering naloxone or performing rescue breathing • DO administer naloxone • DO put the person in the “recovery position” on the side, if the person is breathing independently • DO stay with the person and keep him/her warm • DON’T slap or try to forcefully stimulate the person • DON’T put the person into a cold bath or shower • DON’T inject the person with any substance • DON’T make the person vomit what he/she may have swallowed
Medicated Assisted Treatment (MAT) • After testing different treatments for over 25 years, M. A. T. was the one that showed the most success. • There are 3 forms: Methadone, Combination Buprenorphine/Naloxone, Vivitrol. They are all affective and the treatment center will decide which is best. • SAMSHA Treatment Locator: Convenient and Easy to use Behavioral Health and Substance Abuse Treatment locator: • https: //findtreatment. samhsa. go v/locator
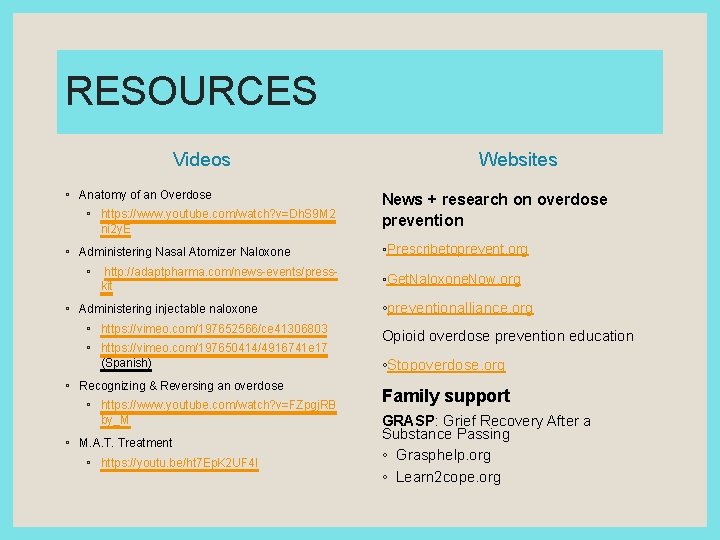
RESOURCES Videos ◦ Anatomy of an Overdose ◦ https: //www. youtube. com/watch? v=Dh. S 9 M 2 ni 2 y. E ◦ Administering Nasal Atomizer Naloxone ◦ http: //adaptpharma. com/news-events/presskit ◦ Administering injectable naloxone ◦ https: //vimeo. com/197652566/ce 41306803 ◦ https: //vimeo. com/197650414/4916741 e 17 (Spanish) ◦ Recognizing & Reversing an overdose ◦ https: //www. youtube. com/watch? v=FZpgj. RB by_M ◦ M. A. T. Treatment ◦ https: //youtu. be/ht 7 Ep. K 2 UF 4 I Websites News + research on overdose prevention ◦Prescribetoprevent. org ◦Get. Naloxone. Now. org ◦preventionalliance. org Opioid overdose prevention education ◦Stopoverdose. org Family support GRASP: Grief Recovery After a Substance Passing ◦ Grasphelp. org ◦ Learn 2 cope. org
Contact Information ◦ Drug Overdose Prevention Program email: ◦ DHS. DOPP. coordinator@illinois. gov ◦ Seth Eisenberg, M. D. ◦ Seth. Eisenberg@illinois. gov ◦ Rosie Gianforte ◦ Rosie. m. gianforte@illinois. gov ◦ 312 -814 -2136