Diagnosis and management of preschool wheeze Sejal Saglani







- Slides: 74
Diagnosis and management of preschool wheeze Sejal Saglani Professor of Paediatric Respiratory Medicine Imperial College London
Outline • Focus on children aged 1 -5 years – NOT bronchiolitis • Diagnosis of wheeze • Features that are unusual and suggest alternative or associated diagnoses – When is it troublesome wheeze that needs investigation? – When should preschool wheezers be referred to tertiary care? • Management of acute episode of wheeze • Maintenance therapy to prevent episodes – Novel approaches to phenotyping – Inflammation – Infection
Is it wheeze? • • • Open-ended questions Ask where noise is coming from Ask parents to mimic noise Listen when child acutely symptomatic Ask parents to record noise Use of a symptoms video
• • • What is this sound? 1. wheeze 2. upper respiratory noise 3. stridor 4. rattle
• • • What is this sound? 1. wheeze 2. upper respiratory noise 3. stridor 4. rattle



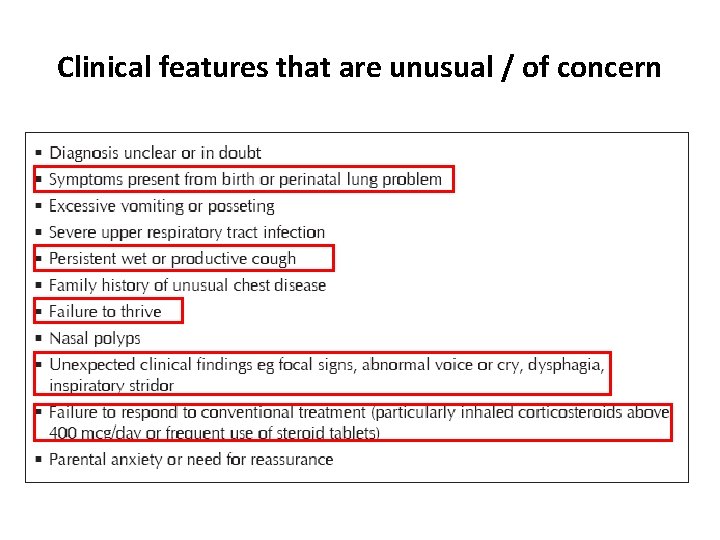
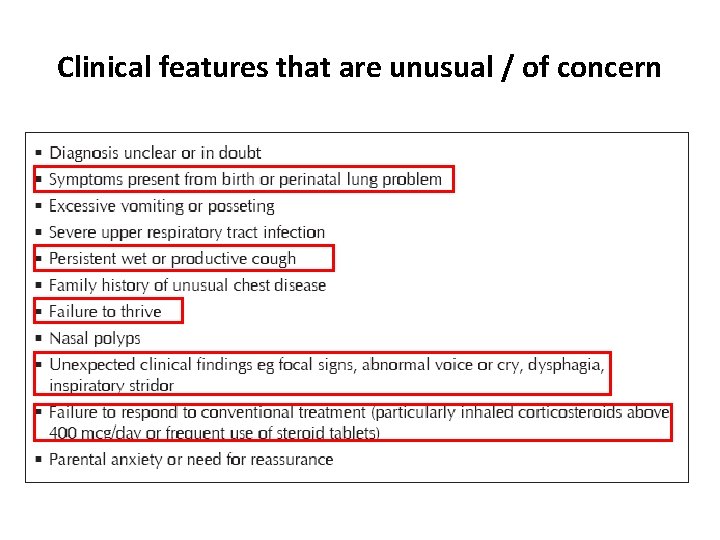
Clinical features that are unusual / of concern
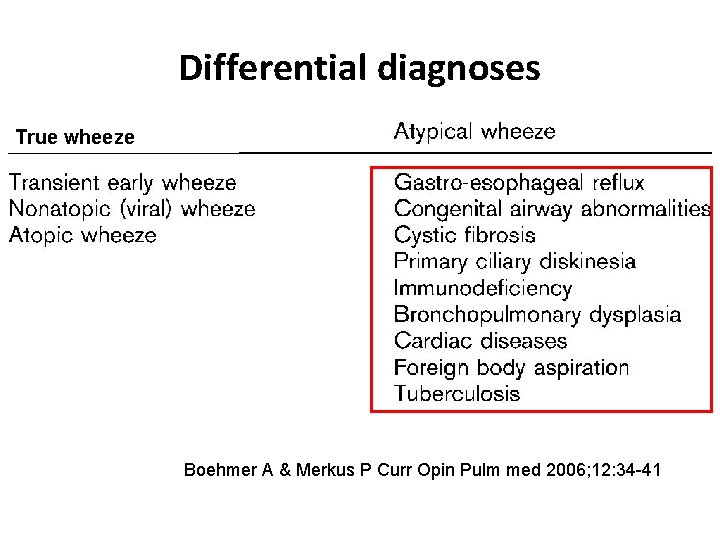
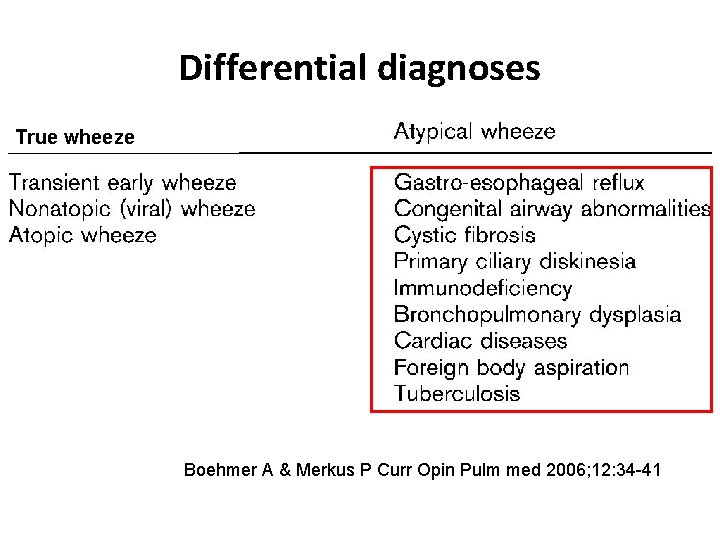
Differential diagnoses True wheeze Boehmer A & Merkus P Curr Opin Pulm med 2006; 12: 34 -41
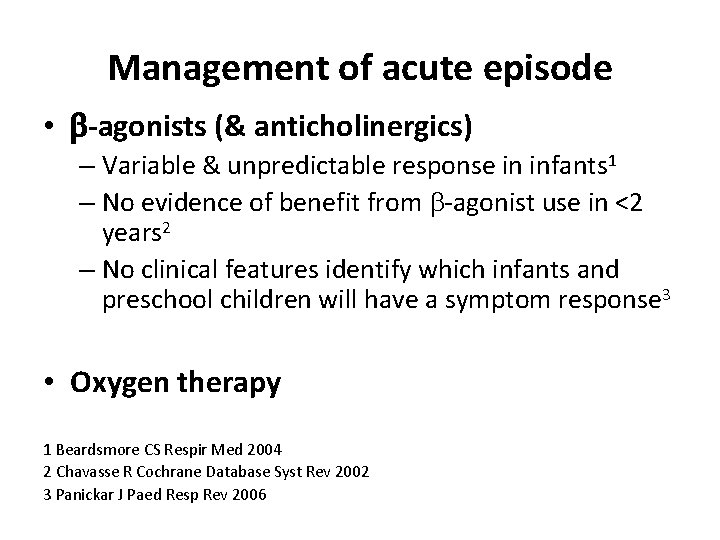
Management of acute episode • b-agonists (& anticholinergics) – Variable & unpredictable response in infants 1 – No evidence of benefit from b-agonist use in <2 years 2 – No clinical features identify which infants and preschool children will have a symptom response 3 • Oxygen therapy 1 Beardsmore CS Respir Med 2004 2 Chavasse R Cochrane Database Syst Rev 2002 3 Panickar J Paed Resp Rev 2006
IV Mg. SO 4 in acute preschool viral wheeze? • RDBPCT, 6 months – 4 years (n=61) • Acute wheeze associated with viral infection • Persistent severe wheeze after initial inhaled salbutamol therapy • Randomised to bolus Mg. SO 4 or saline • Exclusion: asthma symptoms between acute episodes, maintenance ICS • Primary outcome: respiratory distress assessment instrument (RDAI) score Pruikkonen H Eur Respir J 2018; 51: pii: 1701579
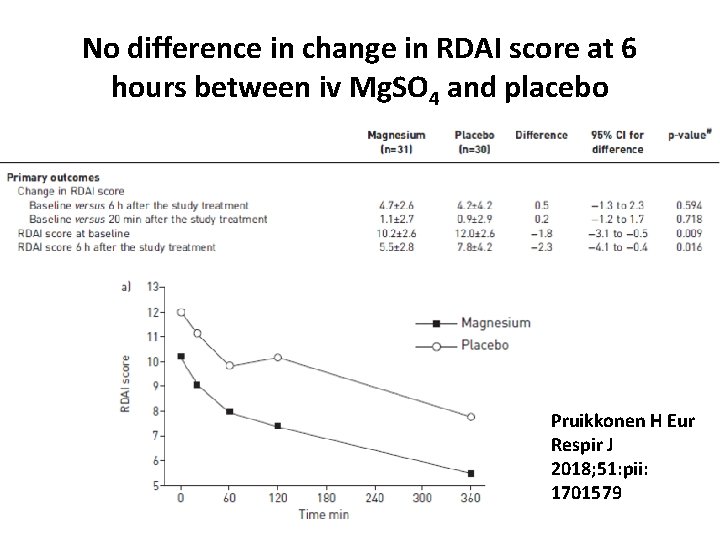
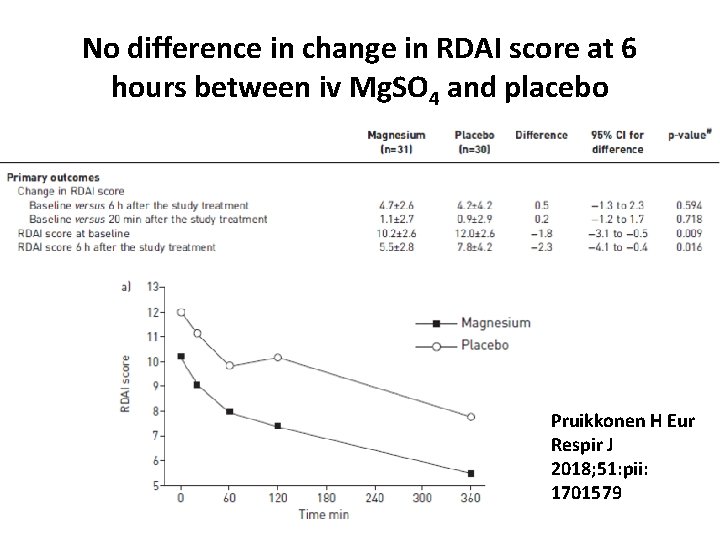
No difference in change in RDAI score at 6 hours between iv Mg. SO 4 and placebo Pruikkonen H Eur Respir J 2018; 51: pii: 1701579
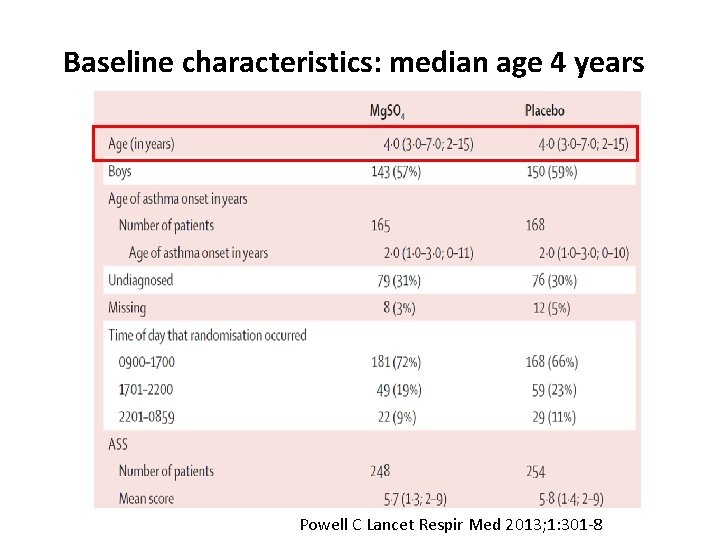
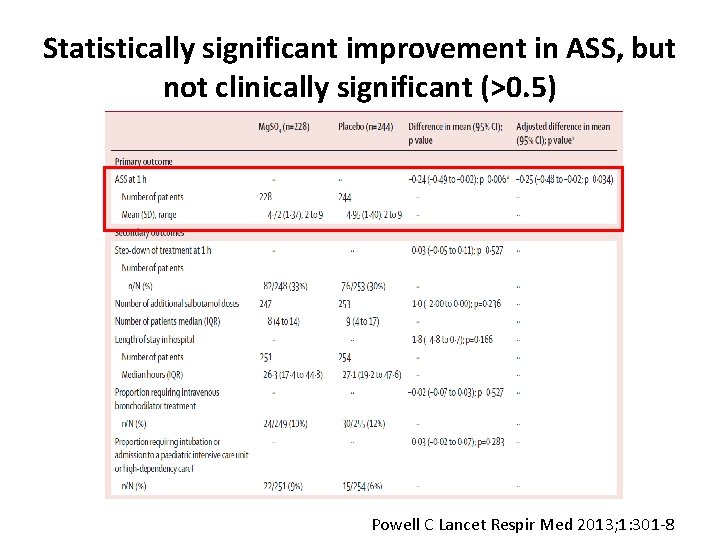
Efficacy of nebulised Mg. SO 4 for acute asthma? MAGNETIC Trial • Multi-centre RDBPT • Neb salbutamol + ipratropium + Mg. SO 4 or placebo • 508 children age 2 -16 years • Primary outcome: change in Yung Asthma Severity Score at 60 mins Powell C Lancet Respir Med 2013; 1: 301 -8
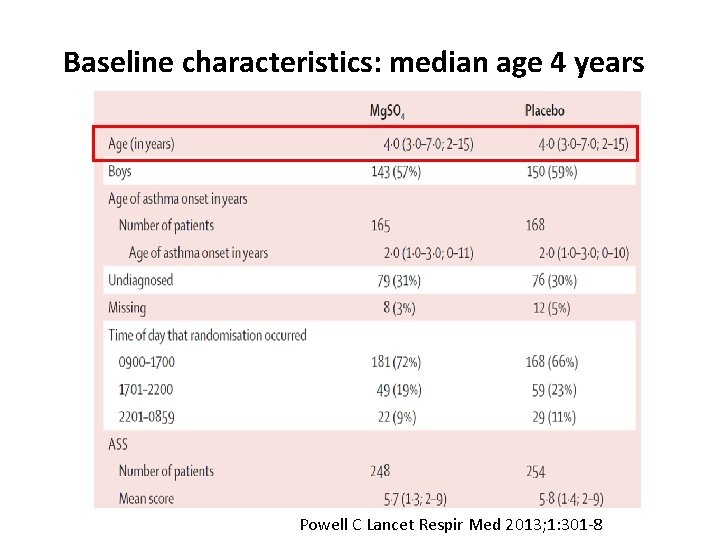
Baseline characteristics: median age 4 years Powell C Lancet Respir Med 2013; 1: 301 -8
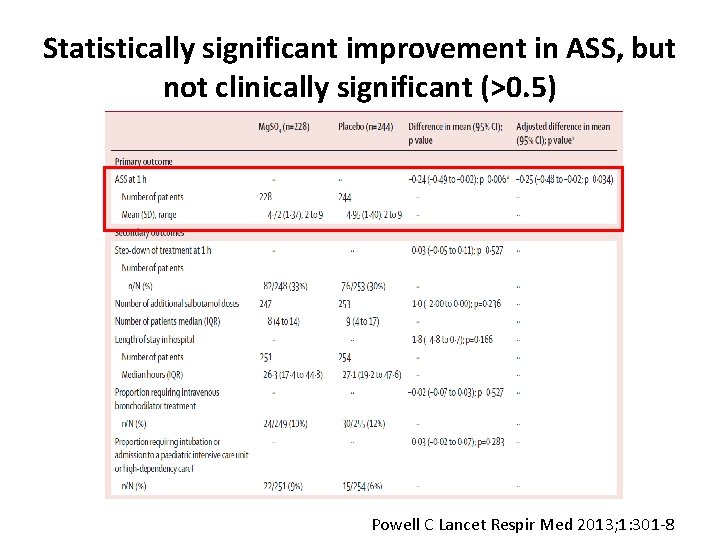
Statistically significant improvement in ASS, but not clinically significant (>0. 5) Powell C Lancet Respir Med 2013; 1: 301 -8
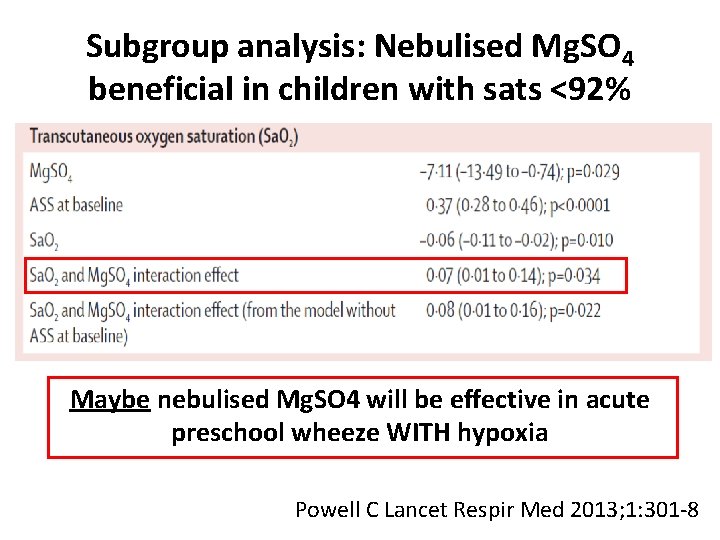
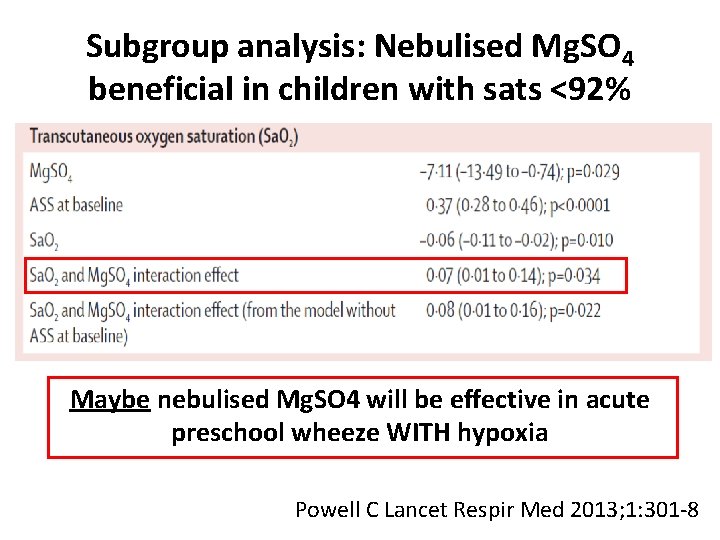
Subgroup analysis: Nebulised Mg. SO 4 beneficial in children with sats <92% Maybe nebulised Mg. SO 4 will be effective in acute preschool wheeze WITH hypoxia Powell C Lancet Respir Med 2013; 1: 301 -8
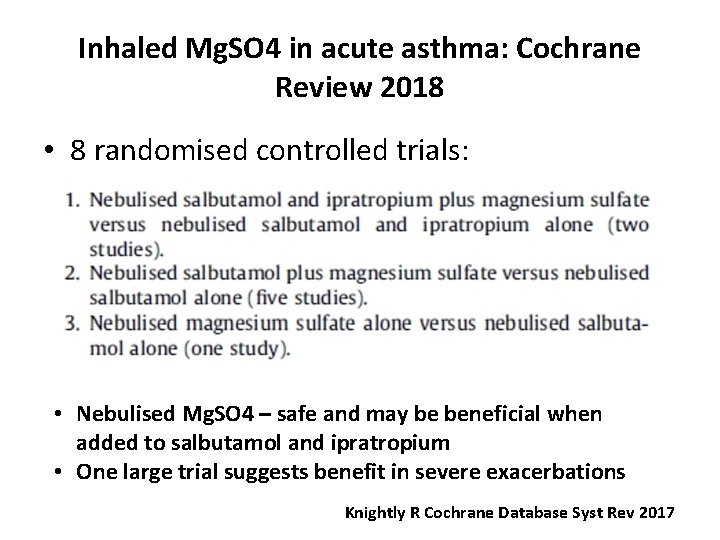
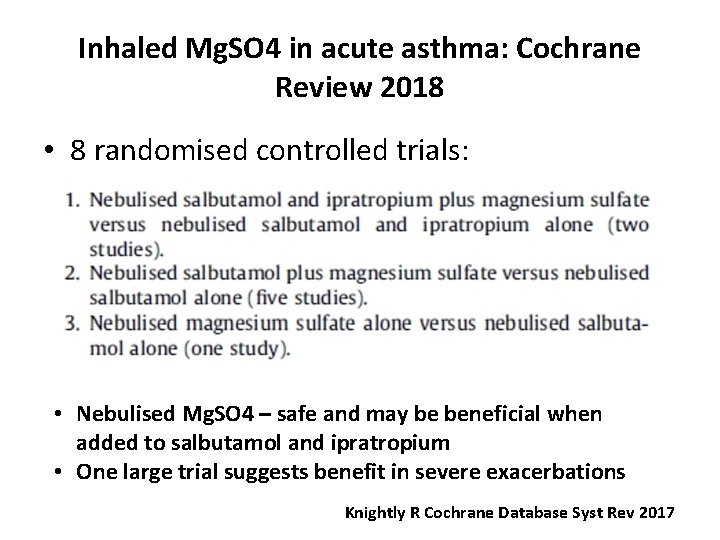
Inhaled Mg. SO 4 in acute asthma: Cochrane Review 2018 • 8 randomised controlled trials: • Nebulised Mg. SO 4 – safe and may be beneficial when added to salbutamol and ipratropium • One large trial suggests benefit in severe exacerbations Knightly R Cochrane Database Syst Rev 2017
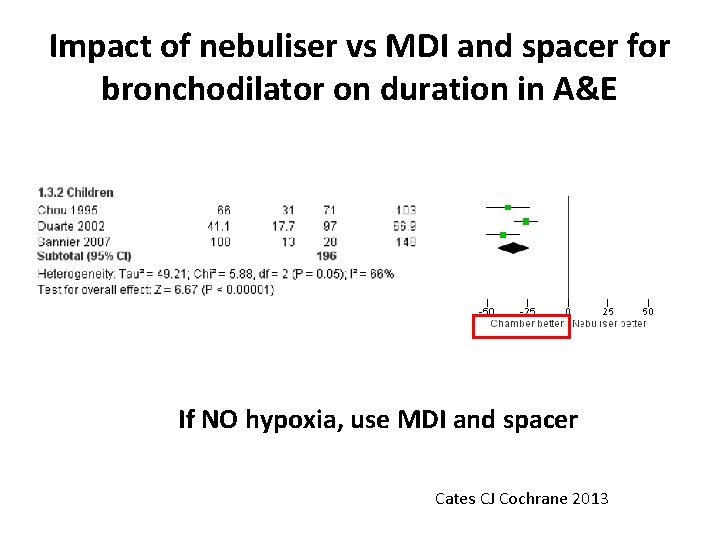
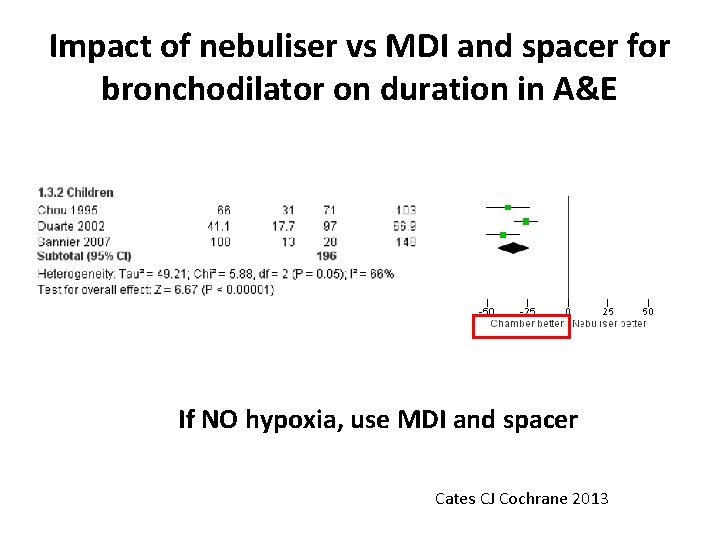
Impact of nebuliser vs MDI and spacer for bronchodilator on duration in A&E If NO hypoxia, use MDI and spacer Cates CJ Cochrane 2013

Management of acute preschool wheeze attack: Role of oral steroids
Question • Would you use a short course of systemic steroids for a preschool aged child (1 -5 years) presenting with an acute attack of wheeze? • 1. Yes • 2. No
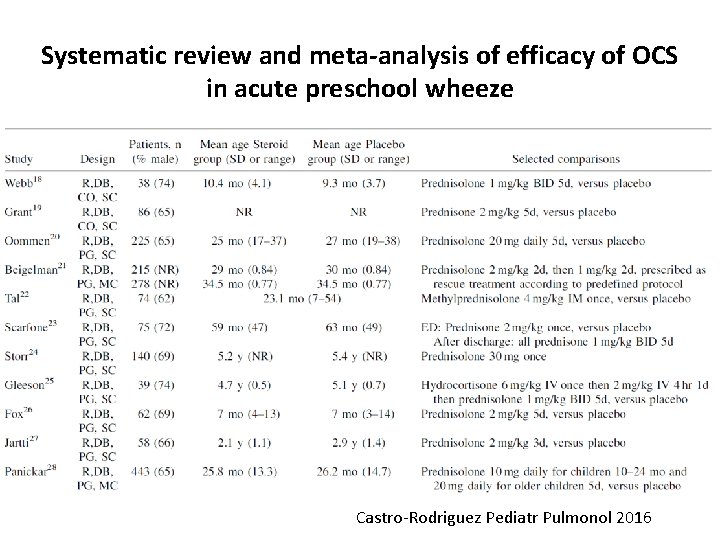
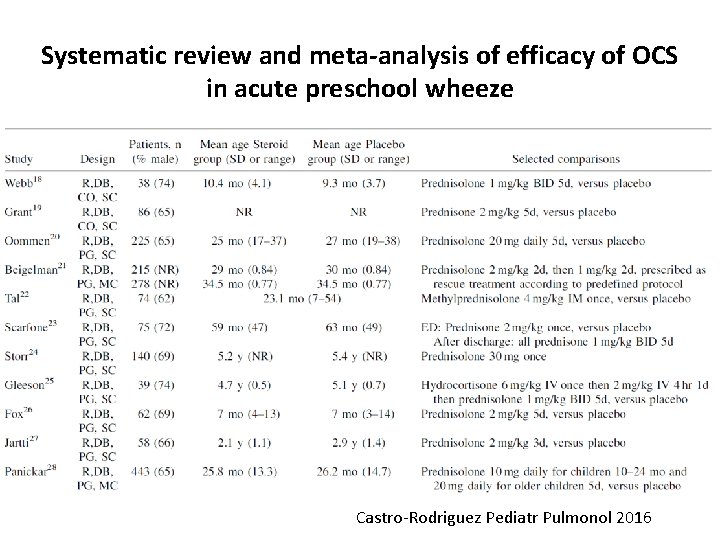
Systematic review and meta-analysis of efficacy of OCS in acute preschool wheeze Castro-Rodriguez Pediatr Pulmonol 2016
Criteria for inclusion • • • Placebo controlled trials Oral steroids Children < 6 years Recurrent wheeze / asthma of any severity No distinction of clinical phenotypes Outcomes: hospitalisation, length of stay, unscheduled visits, need for additional OCS Castro-Rodriguez Pediatr Pulmonol 2016
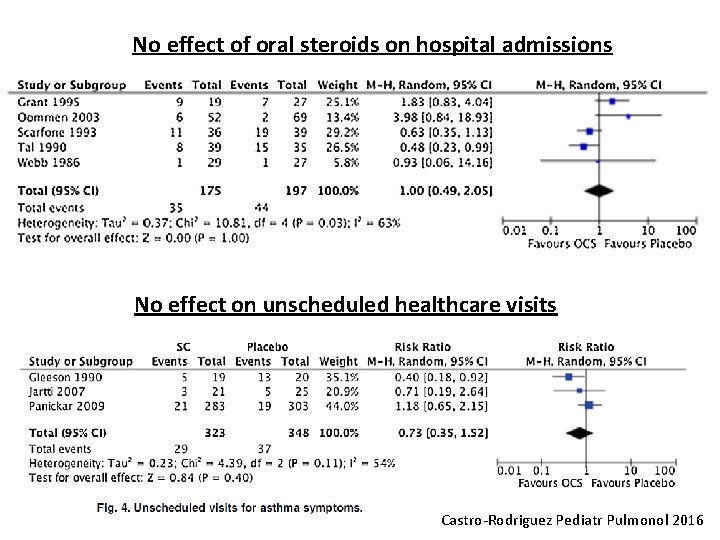
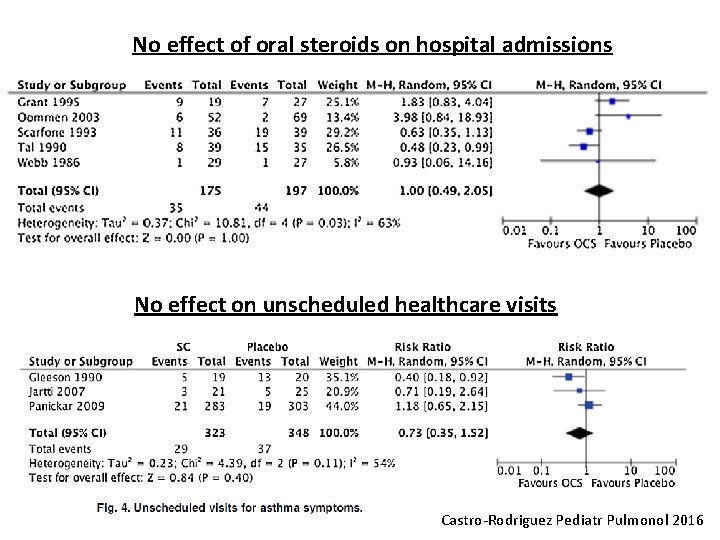
No effect of oral steroids on hospital admissions No effect on unscheduled healthcare visits Castro-Rodriguez Pediatr Pulmonol 2016
Lancet Respir Med 2018; 6: 97 -106
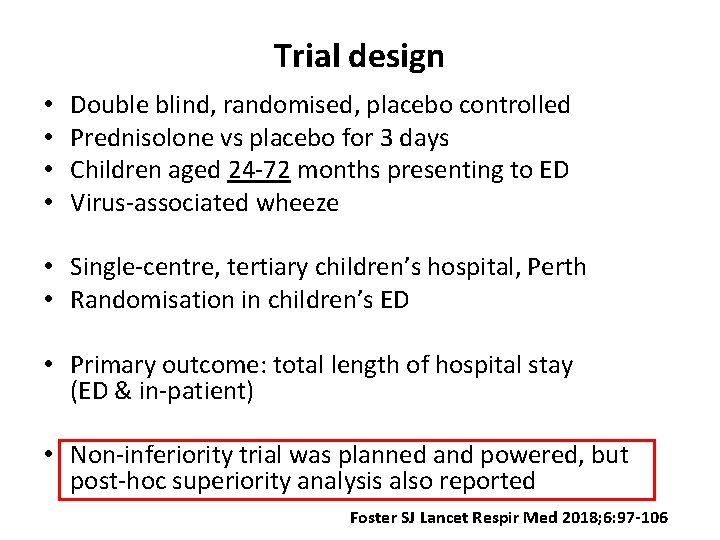
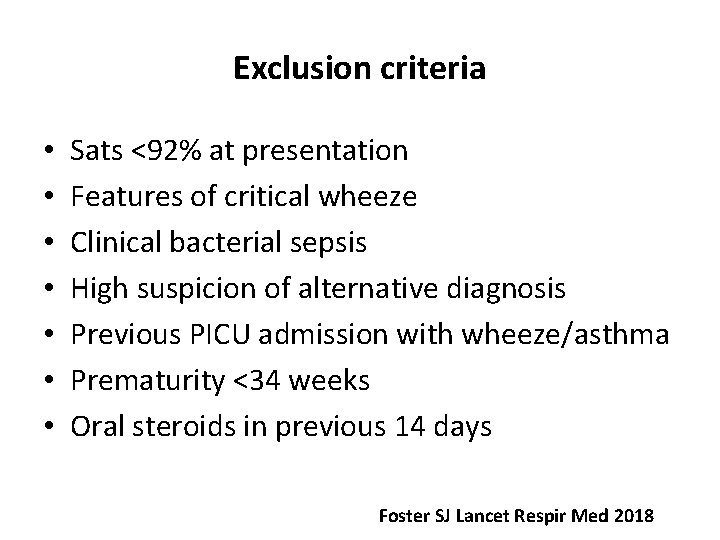
Trial design • • Double blind, randomised, placebo controlled Prednisolone vs placebo for 3 days Children aged 24 -72 months presenting to ED Virus-associated wheeze • Single-centre, tertiary children’s hospital, Perth • Randomisation in children’s ED • Primary outcome: total length of hospital stay (ED & in-patient) • Non-inferiority trial was planned and powered, but post-hoc superiority analysis also reported Foster SJ Lancet Respir Med 2018; 6: 97 -106
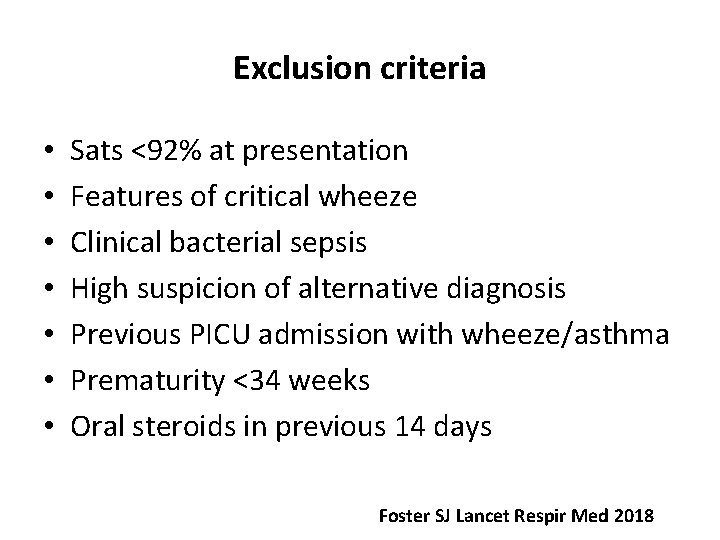
Exclusion criteria • • Sats <92% at presentation Features of critical wheeze Clinical bacterial sepsis High suspicion of alternative diagnosis Previous PICU admission with wheeze/asthma Prematurity <34 weeks Oral steroids in previous 14 days Foster SJ Lancet Respir Med 2018

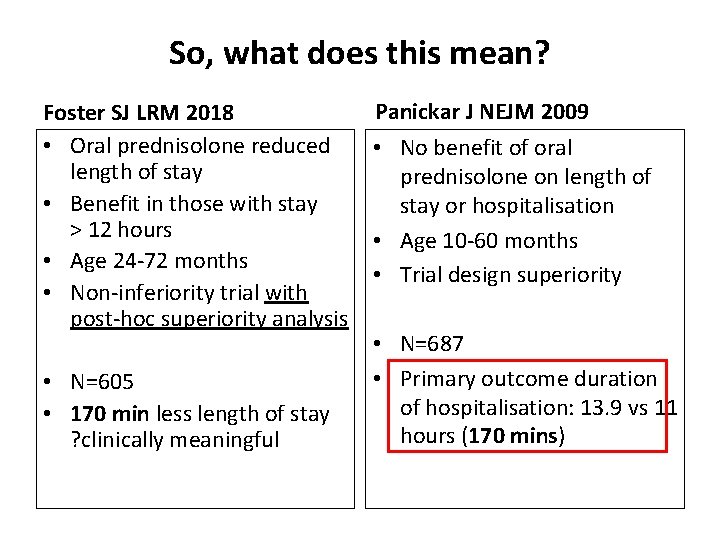
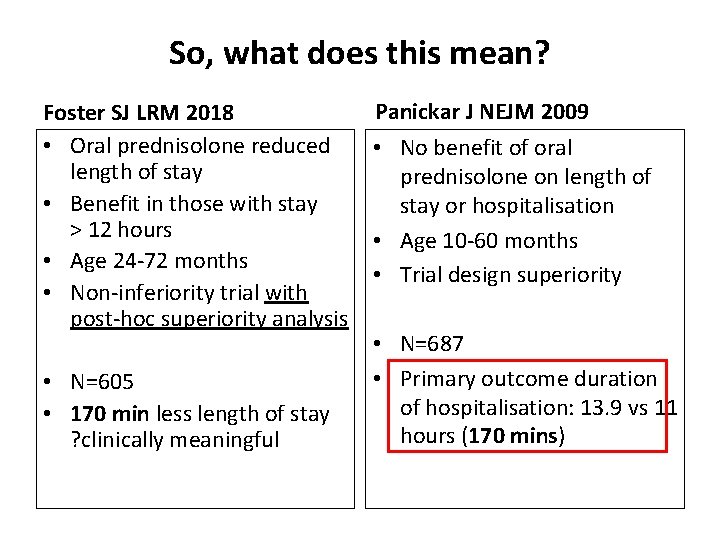
So, what does this mean? Foster SJ LRM 2018 • Oral prednisolone reduced length of stay • Benefit in those with stay > 12 hours • Age 24 -72 months • Non-inferiority trial with post-hoc superiority analysis • N=605 • 170 min less length of stay ? clinically meaningful Panickar J NEJM 2009 • No benefit of oral prednisolone on length of stay or hospitalisation • Age 10 -60 months • Trial design superiority • N=687 • Primary outcome duration of hospitalisation: 13. 9 vs 11 hours (170 mins)
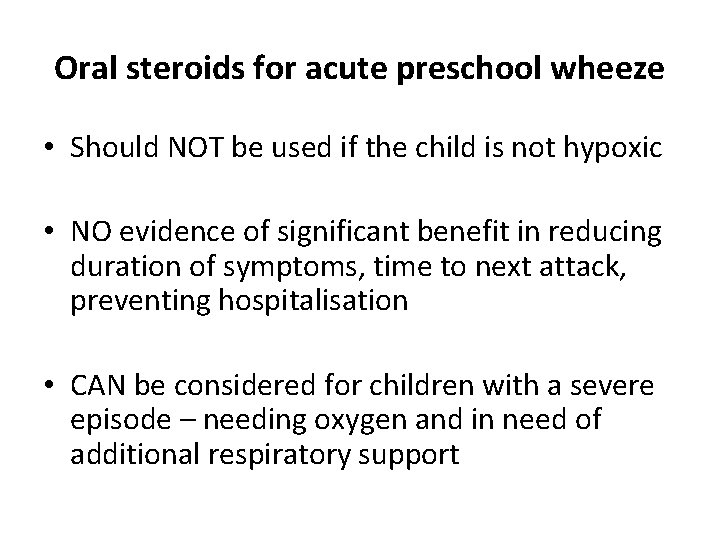
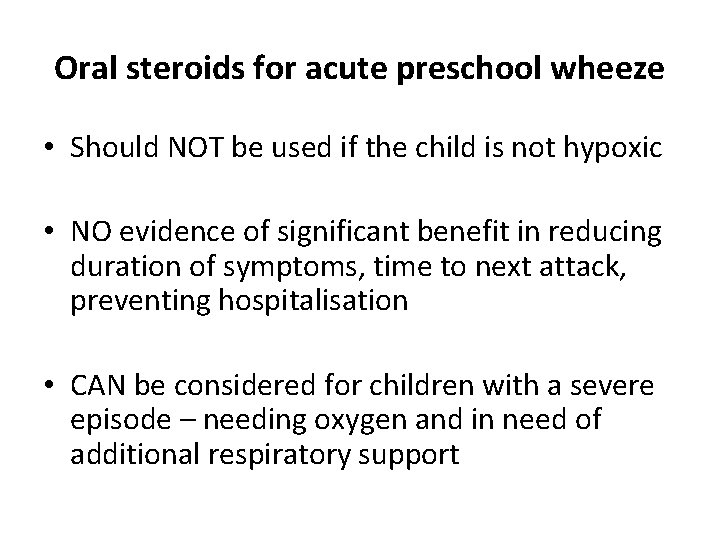
Oral steroids for acute preschool wheeze • Should NOT be used if the child is not hypoxic • NO evidence of significant benefit in reducing duration of symptoms, time to next attack, preventing hospitalisation • CAN be considered for children with a severe episode – needing oxygen and in need of additional respiratory support
Montelukast for acute preschool wheeze attacks?
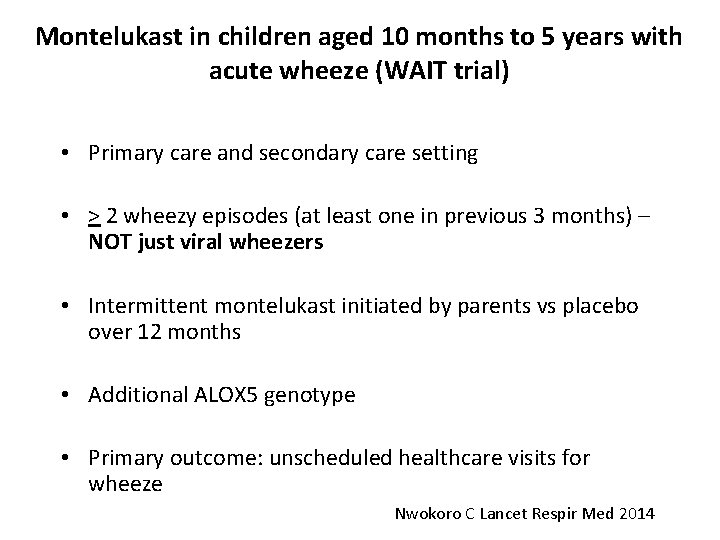
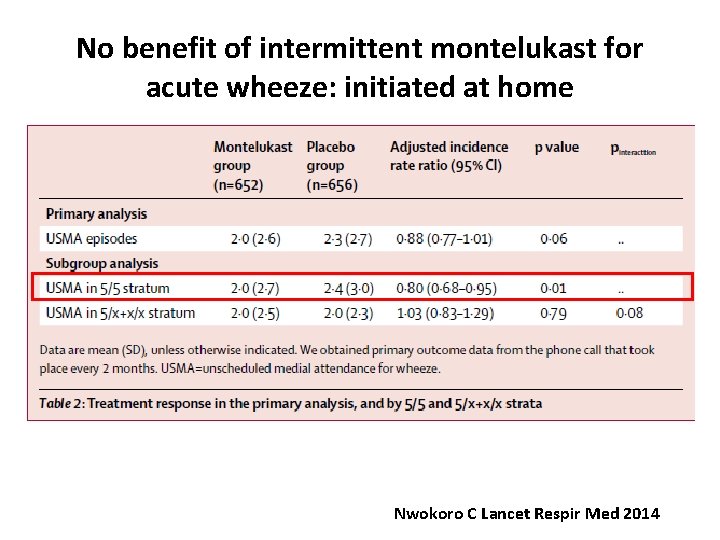
Montelukast in children aged 10 months to 5 years with acute wheeze (WAIT trial) • Primary care and secondary care setting • > 2 wheezy episodes (at least one in previous 3 months) – NOT just viral wheezers • Intermittent montelukast initiated by parents vs placebo over 12 months • Additional ALOX 5 genotype • Primary outcome: unscheduled healthcare visits for wheeze Nwokoro C Lancet Respir Med 2014
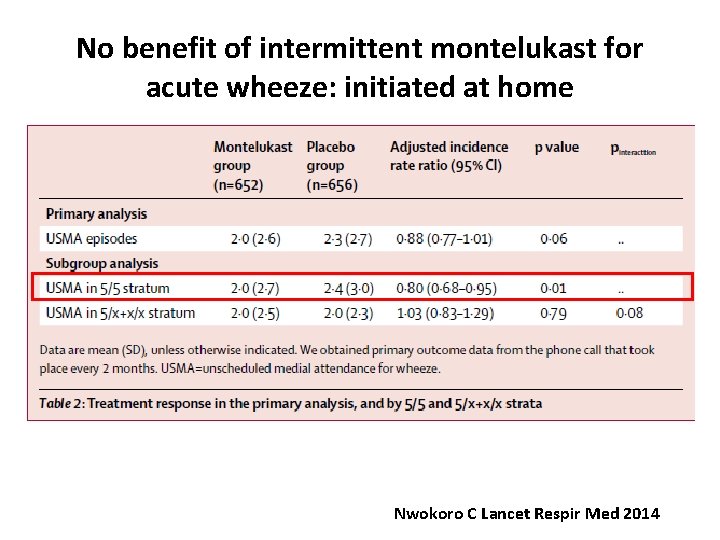
No benefit of intermittent montelukast for acute wheeze: initiated at home Nwokoro C Lancet Respir Med 2014
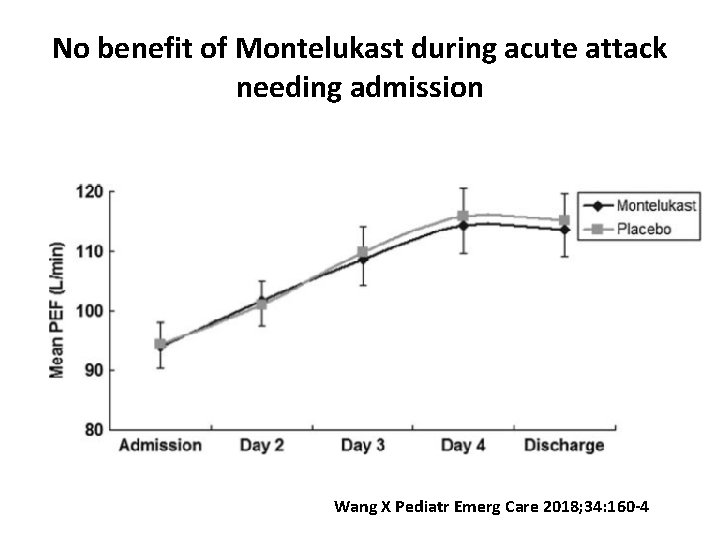
Montelukast initiated in hospital for preschool wheeze • Age 2 -5 years • Children with acute asthma needing emergency attendance / hospitalisation • RDBPCT n=120 • Exclusion: on ICS/LABA for previous 4 weeks, unable to perform spirometry • Primary outcome: change in PEFR and FEV 1 Wang X Pediatr Emerg Care 2018; 34: 160 -4
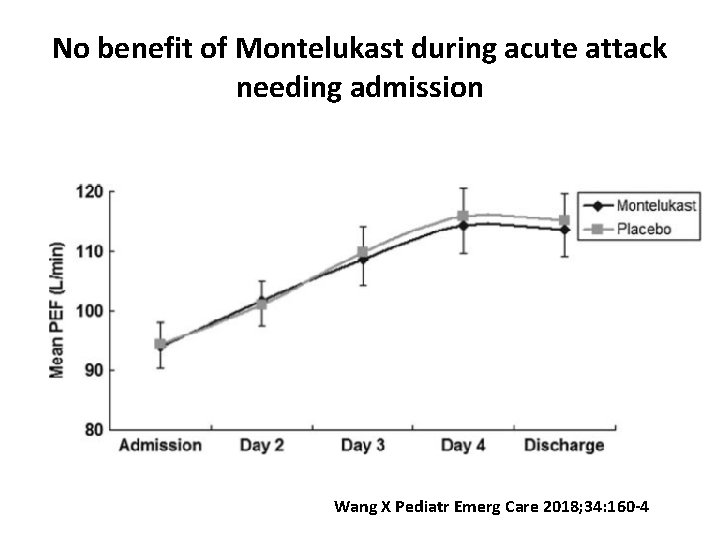
No benefit of Montelukast during acute attack needing admission Wang X Pediatr Emerg Care 2018; 34: 160 -4
Management of acute preschool wheeze attack: Role of antibiotics?
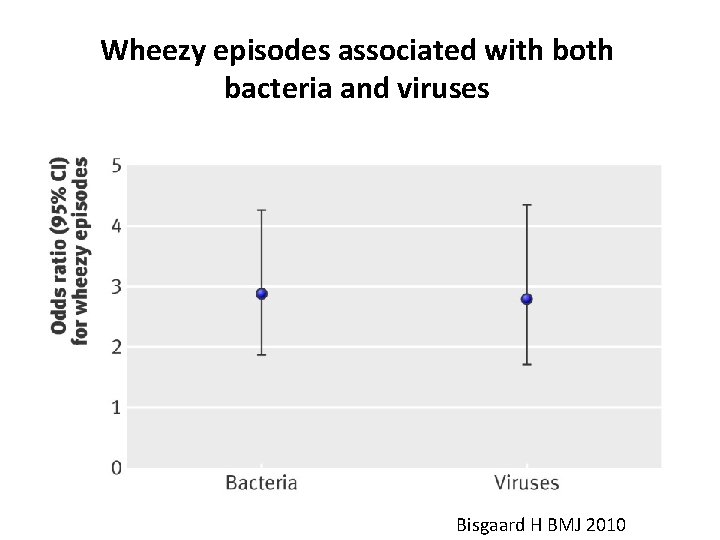
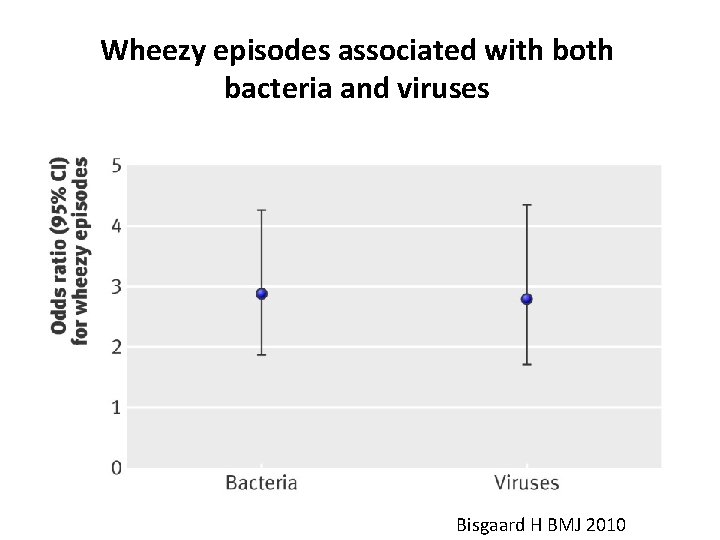
Wheezy episodes associated with both bacteria and viruses Bisgaard H BMJ 2010
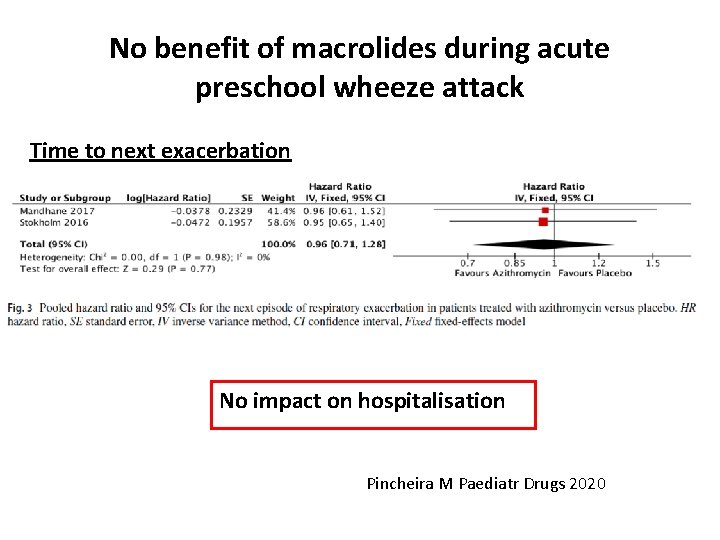
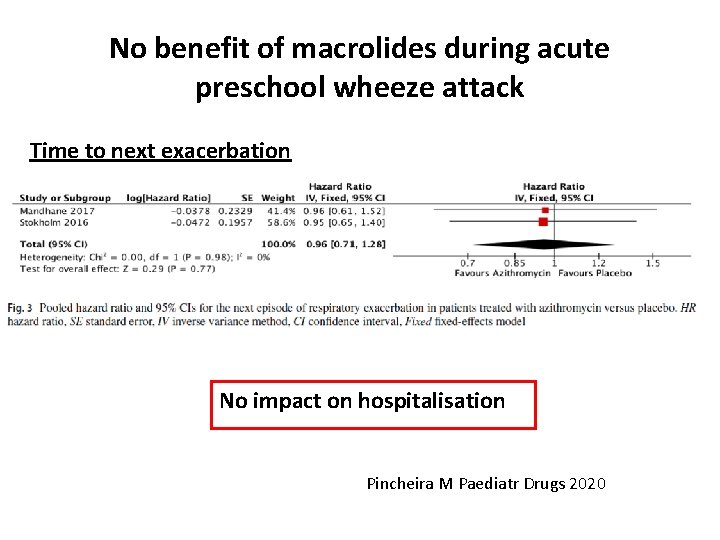
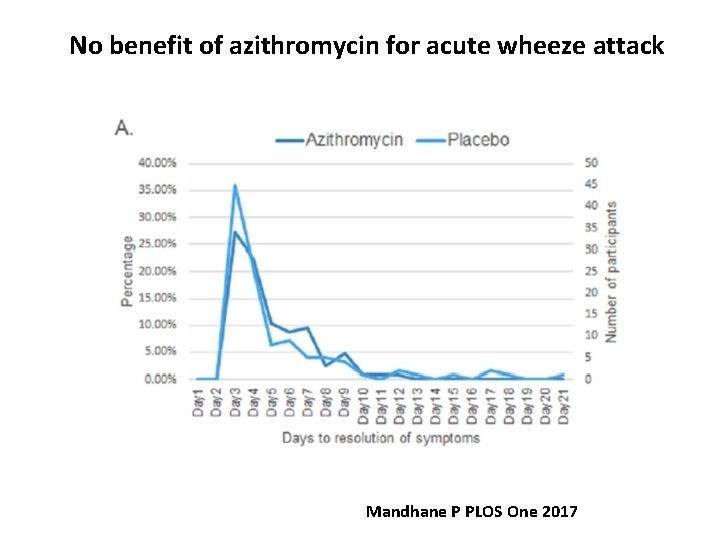
No benefit of macrolides during acute preschool wheeze attack Time to next exacerbation No impact on hospitalisation Pincheira M Paediatr Drugs 2020
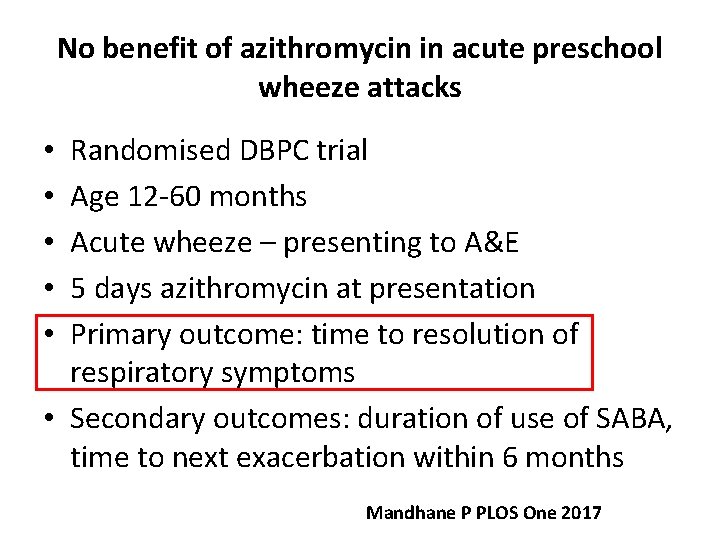
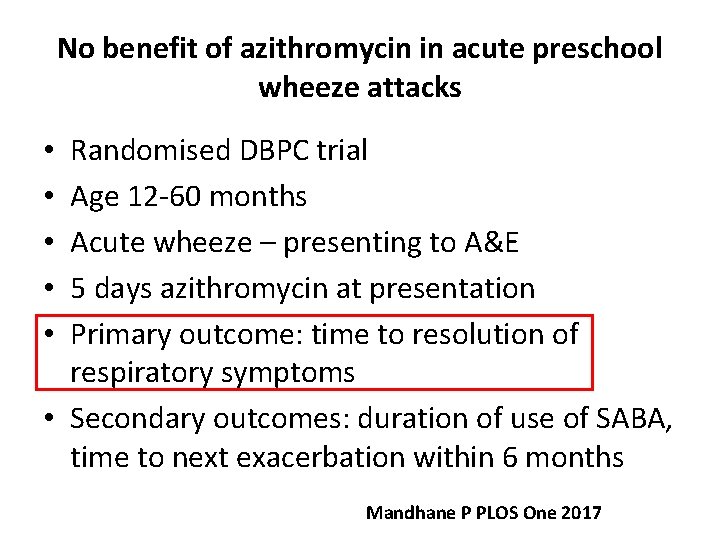
No benefit of azithromycin in acute preschool wheeze attacks Randomised DBPC trial Age 12 -60 months Acute wheeze – presenting to A&E 5 days azithromycin at presentation Primary outcome: time to resolution of respiratory symptoms • Secondary outcomes: duration of use of SABA, time to next exacerbation within 6 months • • • Mandhane P PLOS One 2017
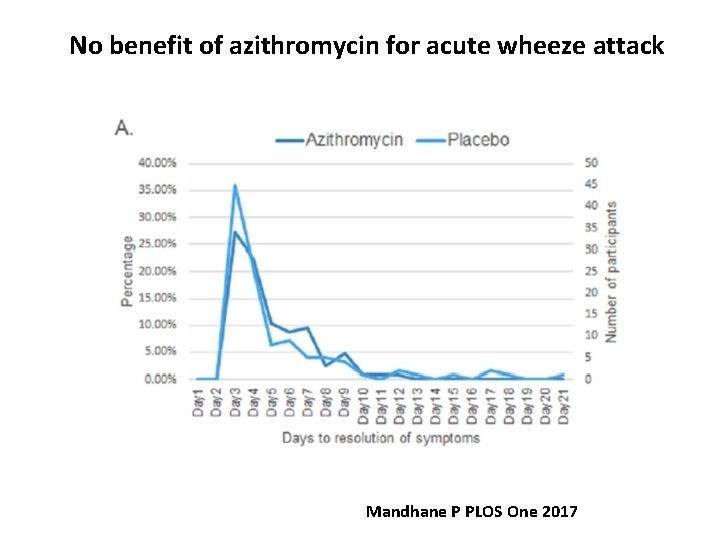
No benefit of azithromycin for acute wheeze attack Mandhane P PLOS One 2017
Case 1 – Acute severe wheeze • 2 year old male • Onset of coryzal symptoms and subsequent difficulty in breathing • What are the key points in the history and initial assessment / examination?
Observations • • • First episode, No atopy, Normal saturations, Obvious wheeze, RR=35/min
What would you do? • • • 1. prescribe oral steroids 2. prescribe azithromycin 3. prescribe SABA with mdi and spacer? 4. all of the above 5. none of the above
Deterioration • Was sent home with salbutamol inhaler mdi and spacer • Returned 12 hours later, no response despite 10 puffs 2 hours ago • RR=45/min, sats 92% in air, wheeze bilaterally
• What next? – Give oral steroids? – Give a macrolide? – Continue with bronchodilators as needed • What advice would you give at discharge? – Needs a review in 48 hours – Offer an outpatient follow-up appointment • Would you start maintenance therapy? – Yes – No
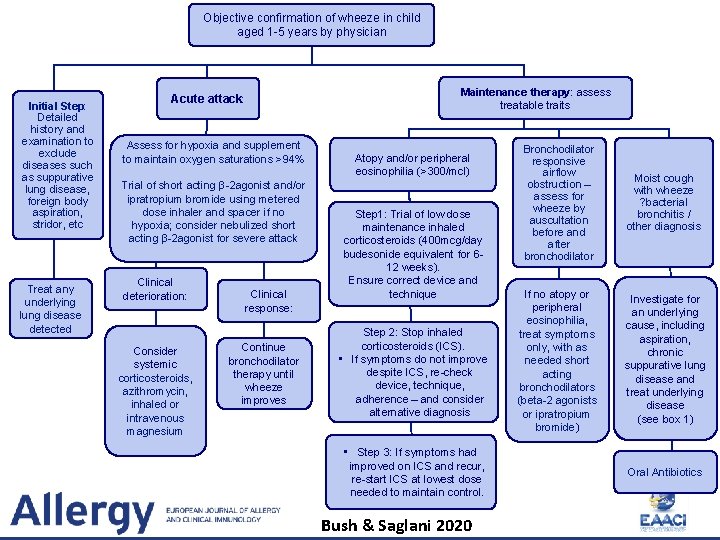
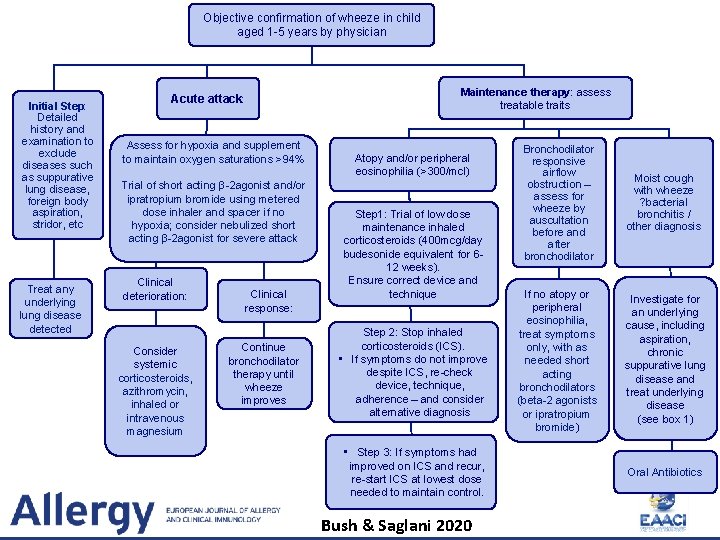
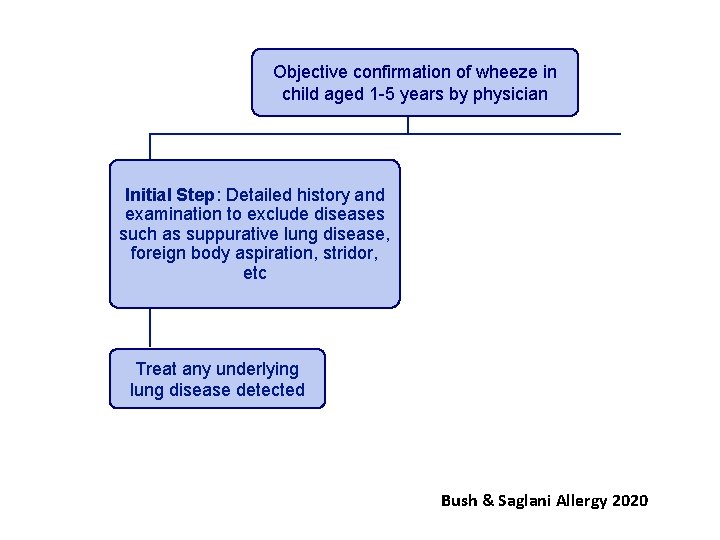
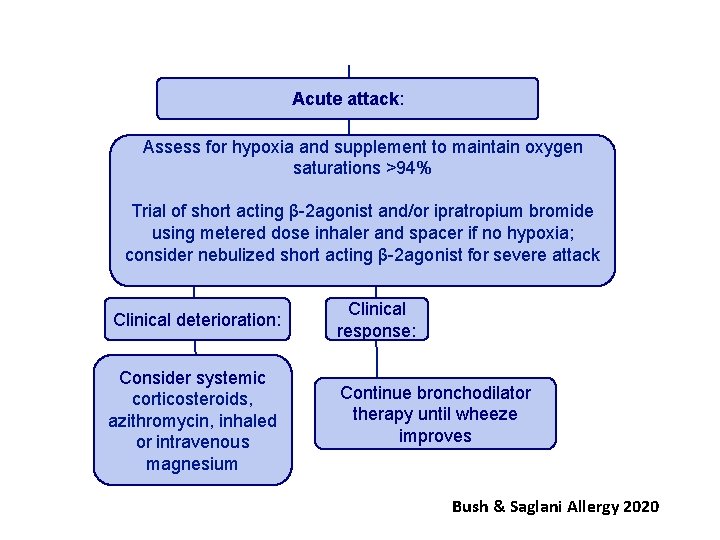
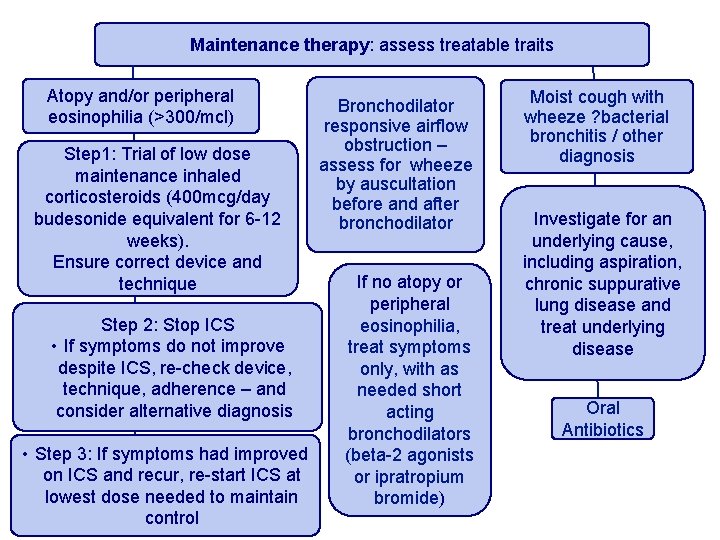
Objective confirmation of wheeze in child aged 1 -5 years by physician Initial Step: Detailed history and examination to exclude diseases such as suppurative lung disease, foreign body aspiration, stridor, etc Treat any underlying lung disease detected Acute attack: Assess for hypoxia and supplement to maintain oxygen saturations >94% Trial of short acting β-2 agonist and/or ipratropium bromide using metered dose inhaler and spacer if no hypoxia; consider nebulized short acting β-2 agonist for severe attack Clinical deterioration: Consider systemic corticosteroids, azithromycin, inhaled or intravenous magnesium Clinical response: Continue bronchodilator therapy until wheeze improves Maintenance therapy: assess treatable traits Atopy and/or peripheral eosinophilia (>300/mcl) Step 1: Trial of low dose maintenance inhaled corticosteroids (400 mcg/day budesonide equivalent for 612 weeks). Ensure correct device and technique Step 2: Stop inhaled corticosteroids (ICS). • If symptoms do not improve despite ICS, re-check device, technique, adherence – and consider alternative diagnosis • Step 3: If symptoms had improved on ICS and recur, re-start ICS at lowest dose needed to maintain control. Bush & Saglani 2020 Bronchodilator responsive airflow obstruction – assess for wheeze by auscultation before and after bronchodilator Moist cough with wheeze ? bacterial bronchitis / other diagnosis If no atopy or peripheral eosinophilia, treat symptoms only, with as needed short acting bronchodilators (beta-2 agonists or ipratropium bromide) Investigate for an underlying cause, including aspiration, chronic suppurative lung disease and treat underlying disease (see box 1) Oral Antibiotics
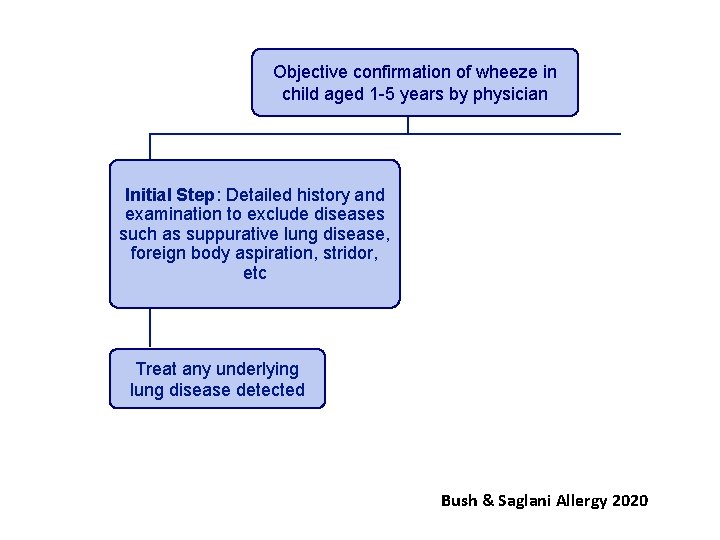
Objective confirmation of wheeze in child aged 1 -5 years by physician Initial Step: Detailed history and examination to exclude diseases such as suppurative lung disease, foreign body aspiration, stridor, etc Treat any underlying lung disease detected Bush & Saglani Allergy 2020
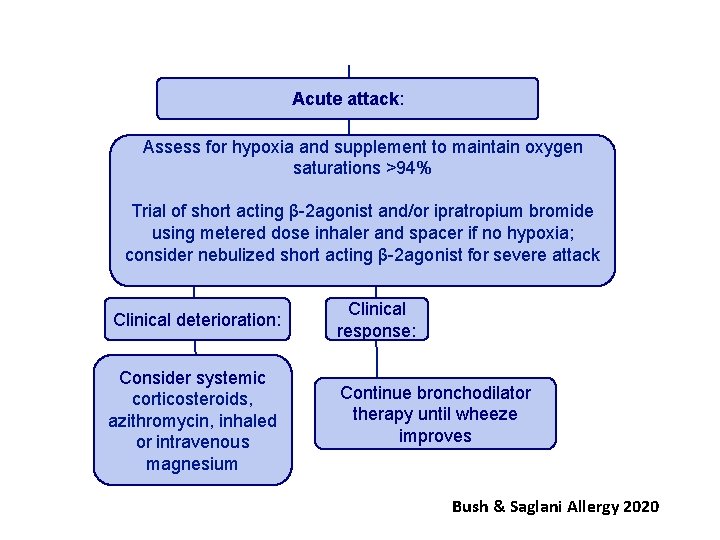
Acute attack: Assess for hypoxia and supplement to maintain oxygen saturations >94% Trial of short acting β-2 agonist and/or ipratropium bromide using metered dose inhaler and spacer if no hypoxia; consider nebulized short acting β-2 agonist for severe attack Clinical deterioration: Clinical response: Consider systemic corticosteroids, azithromycin, inhaled or intravenous magnesium Continue bronchodilator therapy until wheeze improves Bush & Saglani Allergy 2020
Role of maintenance therapy: To prevent episodes of preschool wheeze and control symptoms
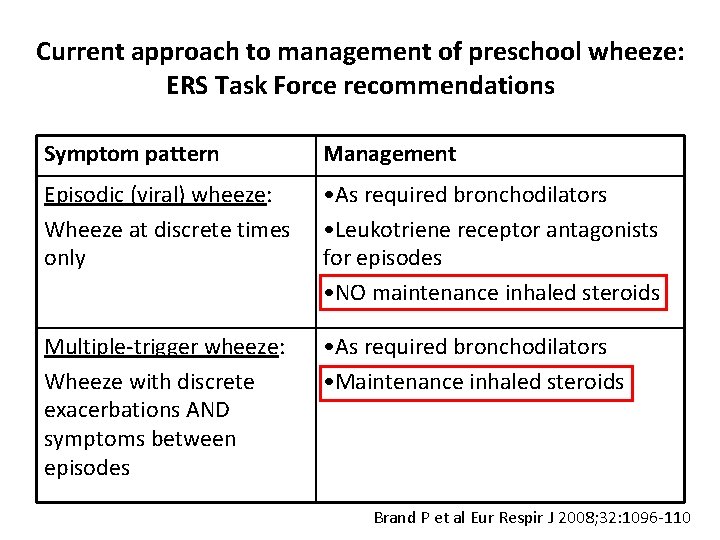
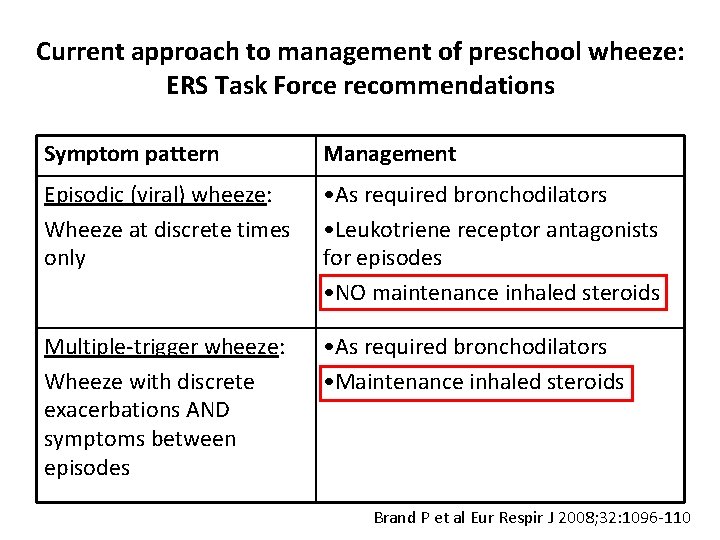
Current approach to management of preschool wheeze: ERS Task Force recommendations Symptom pattern Management Episodic (viral) wheeze: Wheeze at discrete times only • As required bronchodilators • Leukotriene receptor antagonists for episodes • NO maintenance inhaled steroids Multiple-trigger wheeze: Wheeze with discrete exacerbations AND symptoms between episodes • As required bronchodilators • Maintenance inhaled steroids Brand P et al Eur Respir J 2008; 32: 1096 -110
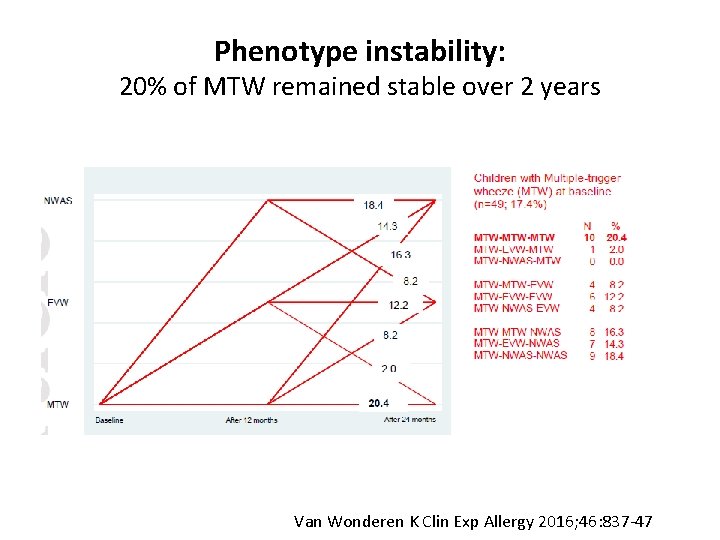
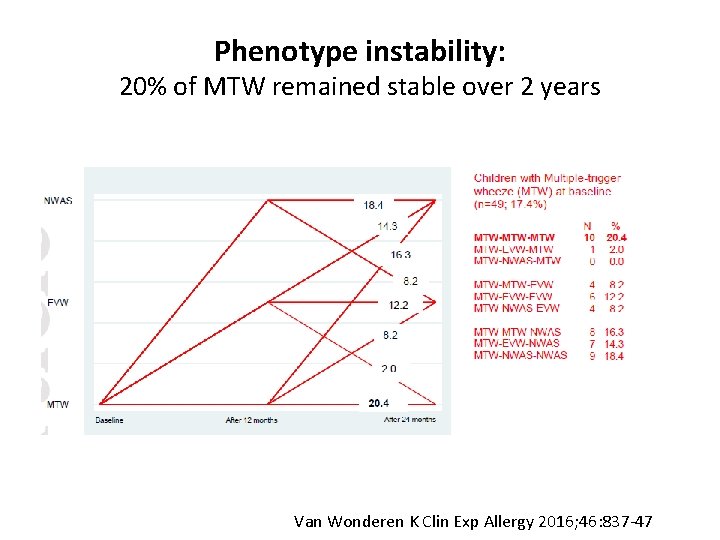
Phenotype instability: 20% of MTW remained stable over 2 years Van Wonderen K Clin Exp Allergy 2016; 46: 837 -47
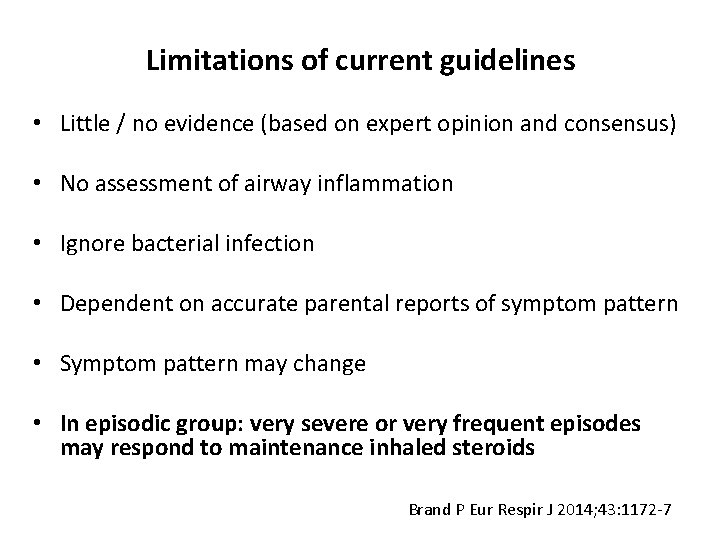
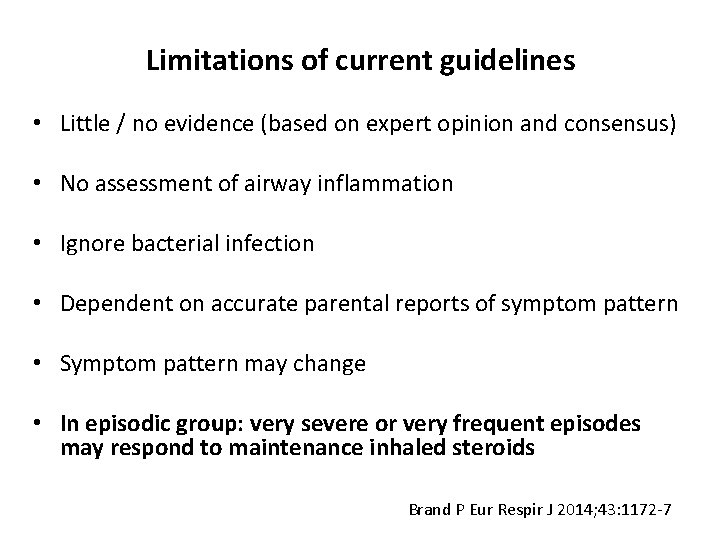
Limitations of current guidelines • Little / no evidence (based on expert opinion and consensus) • No assessment of airway inflammation • Ignore bacterial infection • Dependent on accurate parental reports of symptom pattern • Symptom pattern may change • In episodic group: very severe or very frequent episodes may respond to maintenance inhaled steroids Brand P Eur Respir J 2014; 43: 1172 -7
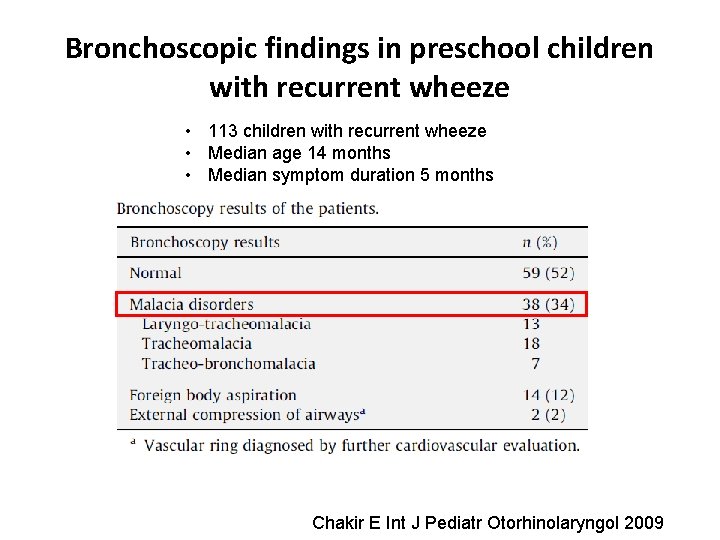
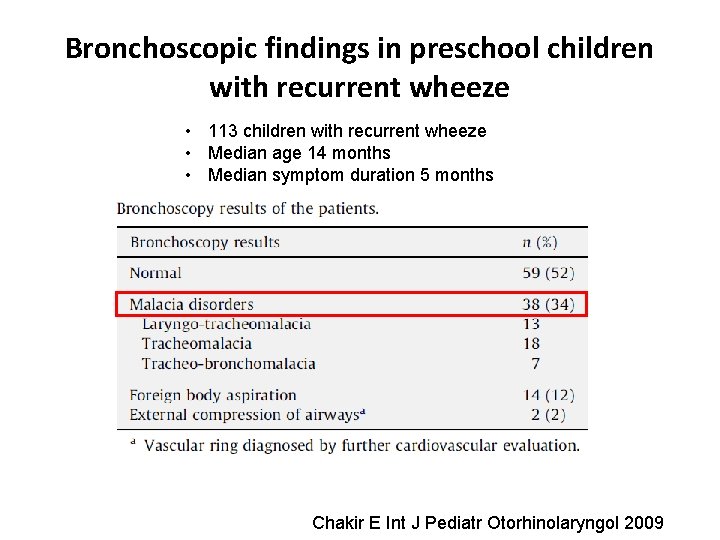
Bronchoscopic findings in preschool children with recurrent wheeze • 113 children with recurrent wheeze • Median age 14 months • Median symptom duration 5 months Chakir E Int J Pediatr Otorhinolaryngol 2009

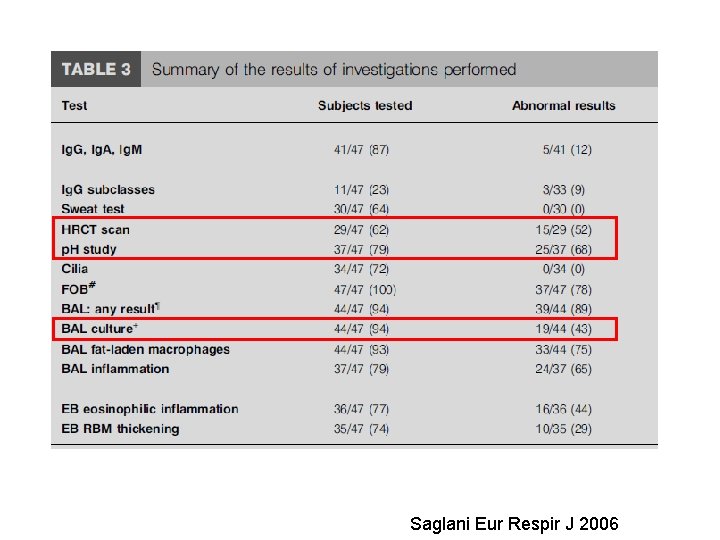
Brompton experience Saglani Eur Respir J 2006
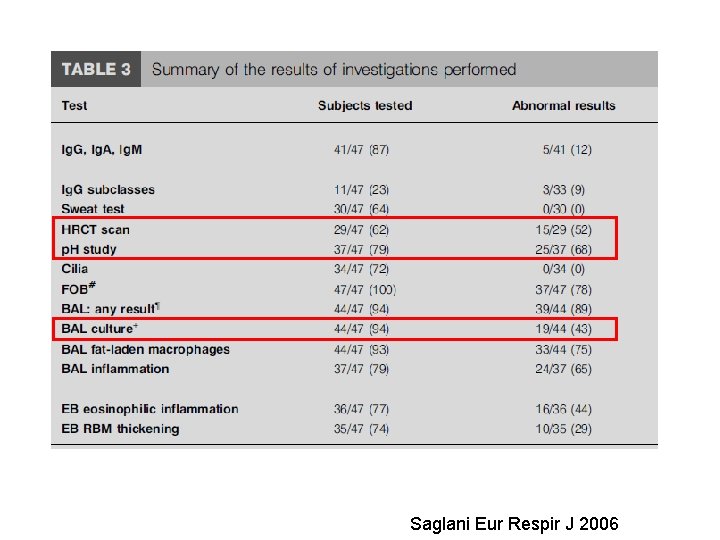
Saglani Eur Respir J 2006
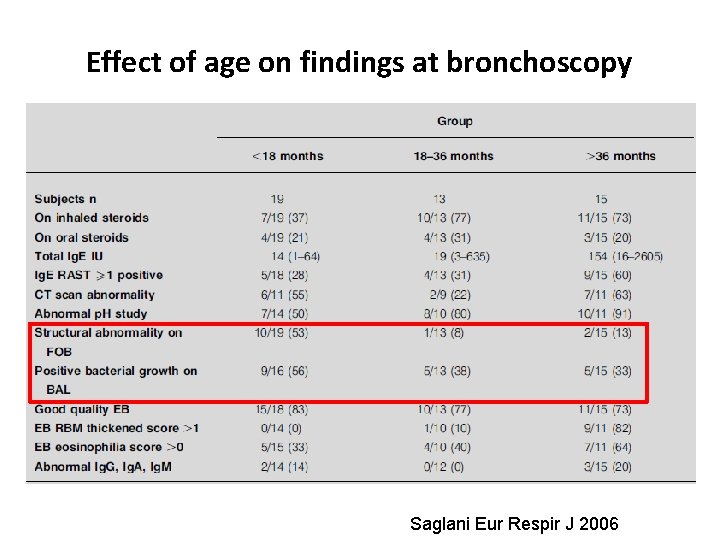
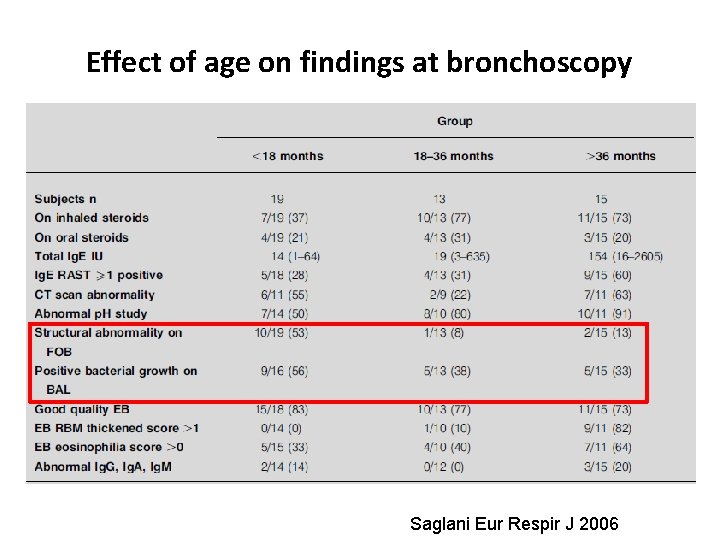
Effect of age on findings at bronchoscopy Saglani Eur Respir J 2006
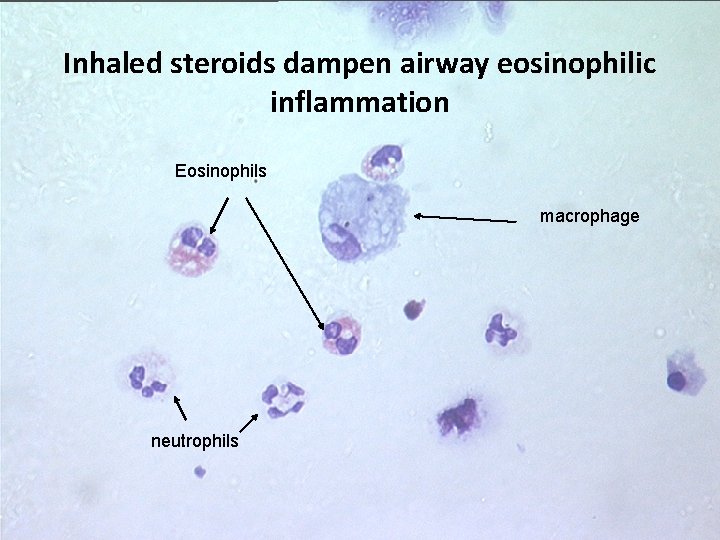
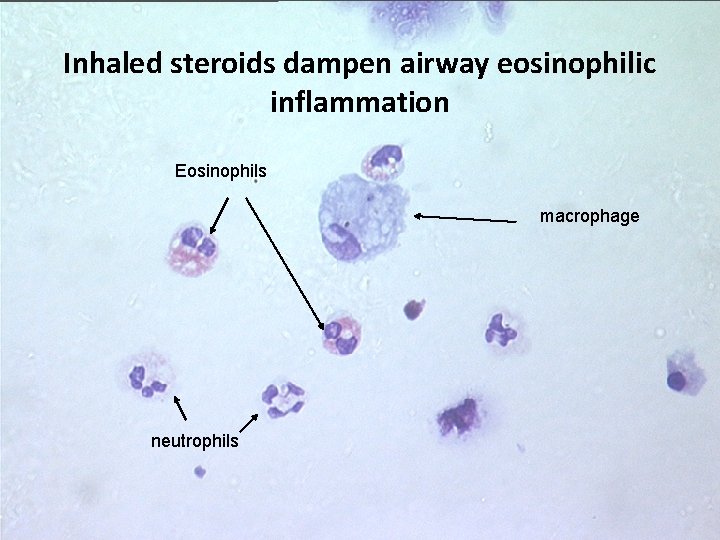
Inhaled steroids dampen airway eosinophilic inflammation Eosinophils macrophage neutrophils
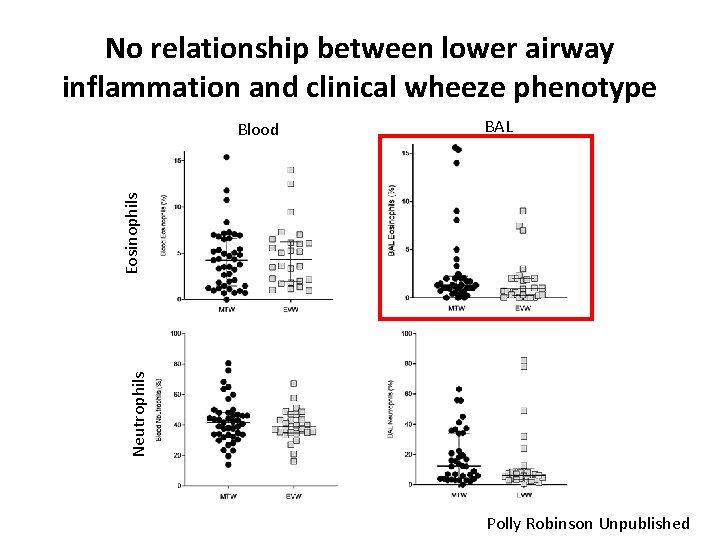
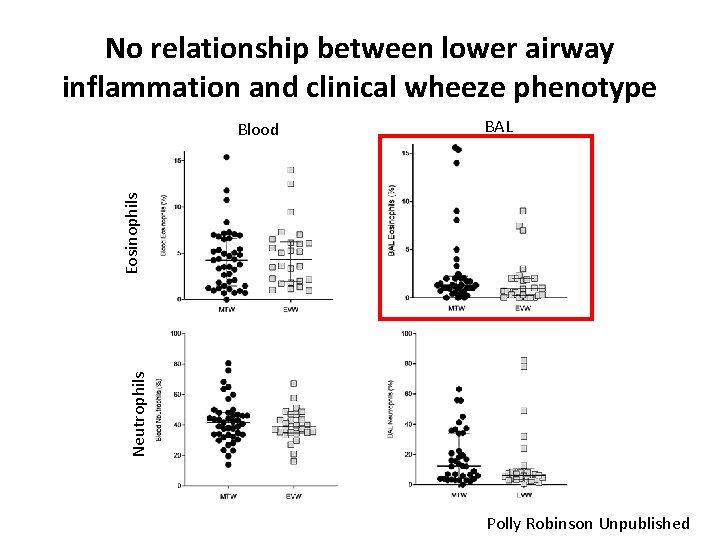
No relationship between lower airway inflammation and clinical wheeze phenotype BAL Neutrophils Eosinophils Blood Polly Robinson Unpublished
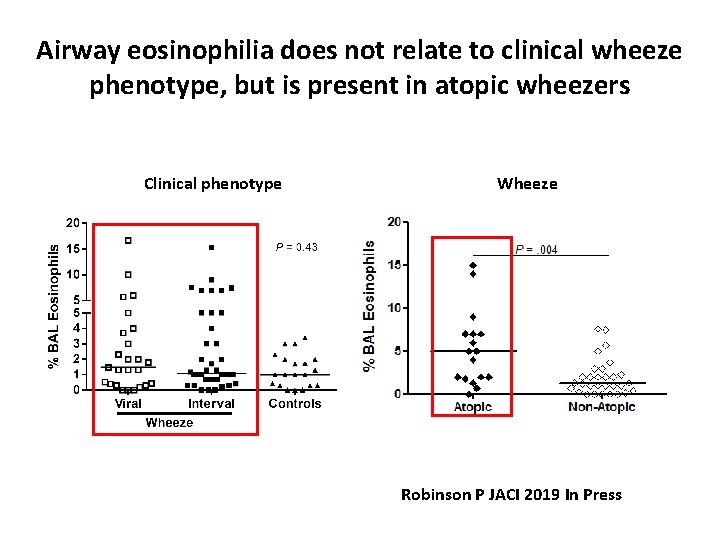
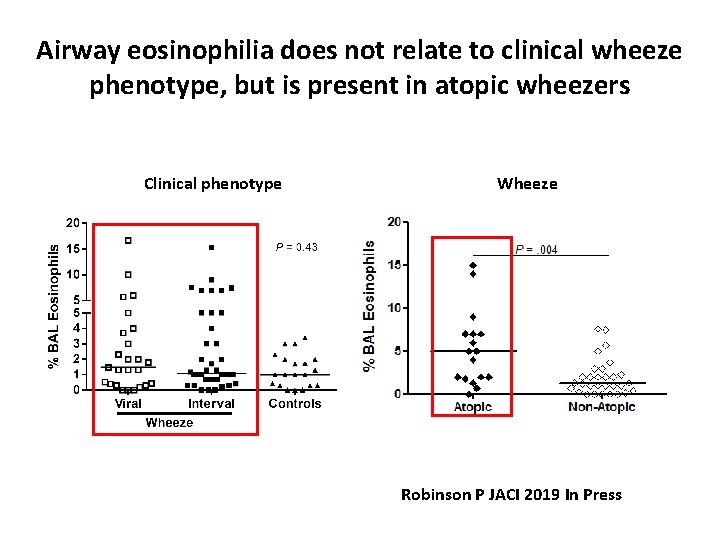
Airway eosinophilia does not relate to clinical wheeze phenotype, but is present in atopic wheezers Clinical phenotype Wheeze Robinson P JACI 2019 In Press
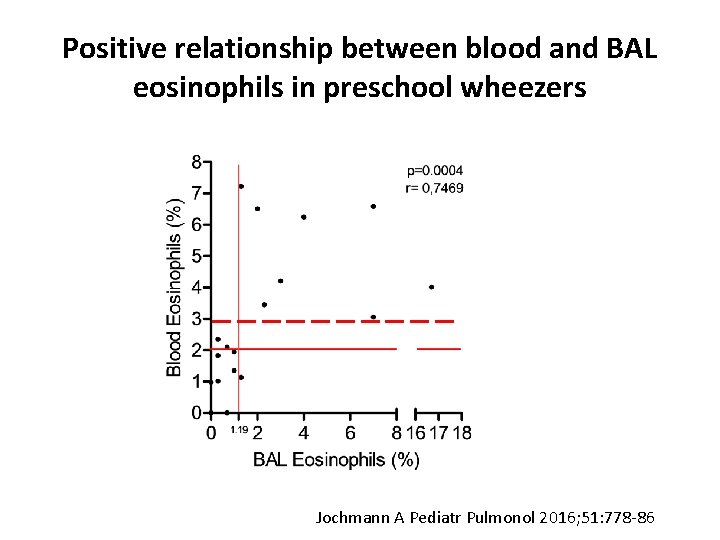
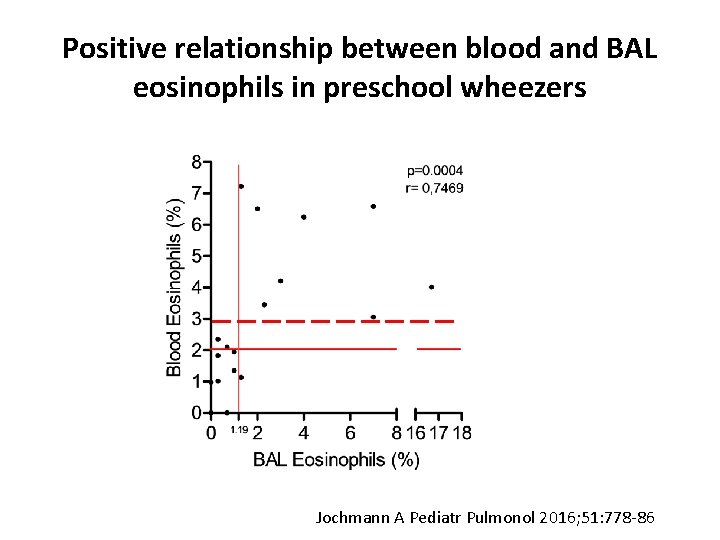
Positive relationship between blood and BAL eosinophils in preschool wheezers Jochmann A Pediatr Pulmonol 2016; 51: 778 -86
Objective biomarker based approach to prevent preschool wheeze attacks
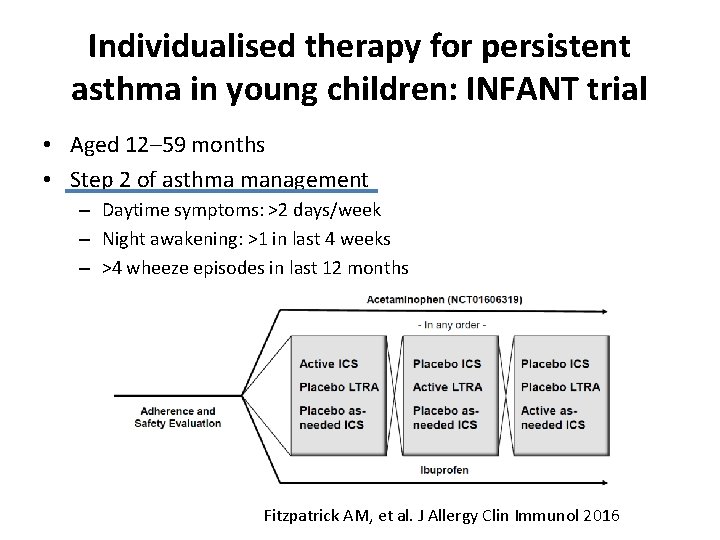
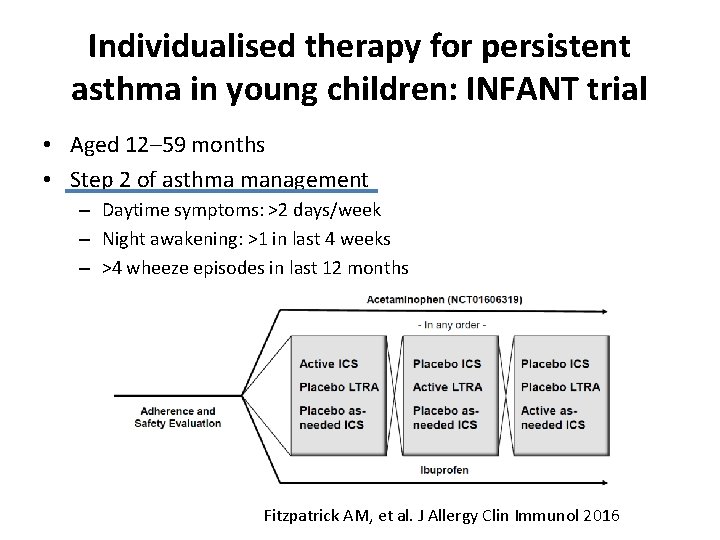
Individualised therapy for persistent asthma in young children: INFANT trial • Aged 12– 59 months • Step 2 of asthma management – Daytime symptoms: >2 days/week – Night awakening: >1 in last 4 weeks – >4 wheeze episodes in last 12 months Fitzpatrick AM, et al. J Allergy Clin Immunol 2016
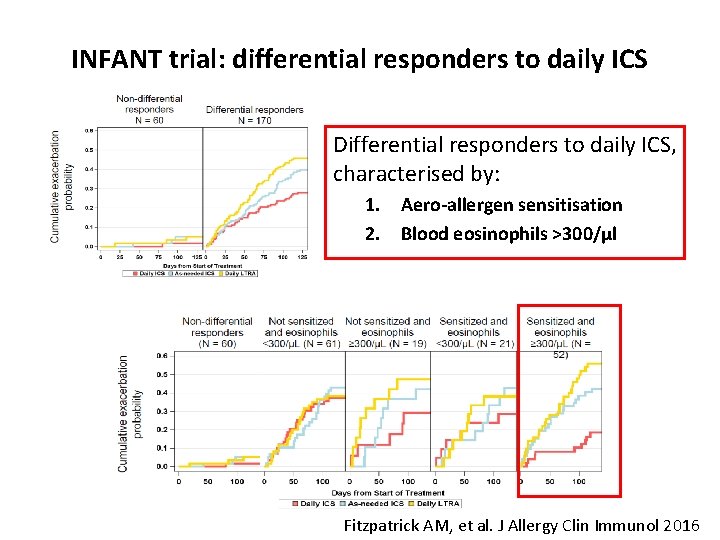
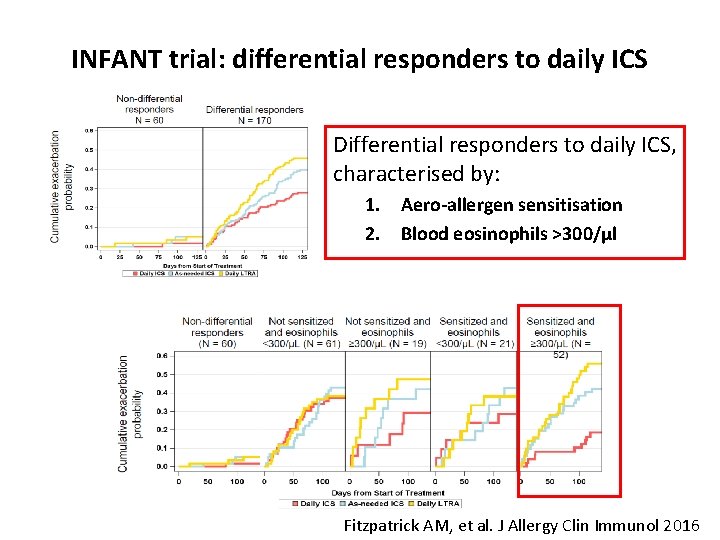
INFANT trial: differential responders to daily ICS Differential responders to daily ICS, characterised by: 1. Aero-allergen sensitisation 2. Blood eosinophils >300/µl Fitzpatrick AM, et al. J Allergy Clin Immunol 2016
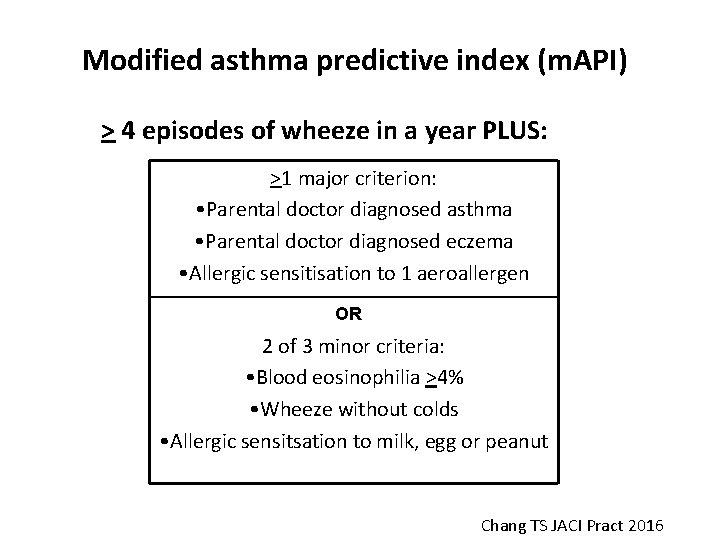
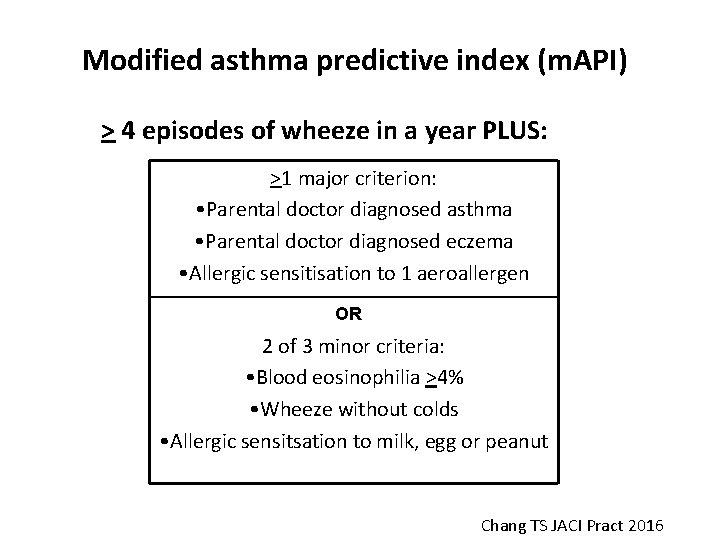
Modified asthma predictive index (m. API) > 4 episodes of wheeze in a year PLUS: >1 major criterion: • Parental doctor diagnosed asthma • Parental doctor diagnosed eczema • Allergic sensitisation to 1 aeroallergen OR 2 of 3 minor criteria: • Blood eosinophilia >4% • Wheeze without colds • Allergic sensitsation to milk, egg or peanut Chang TS JACI Pract 2016
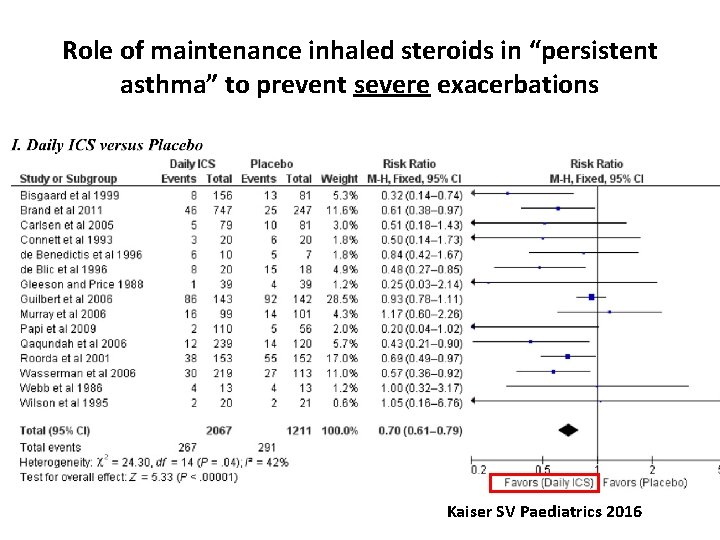
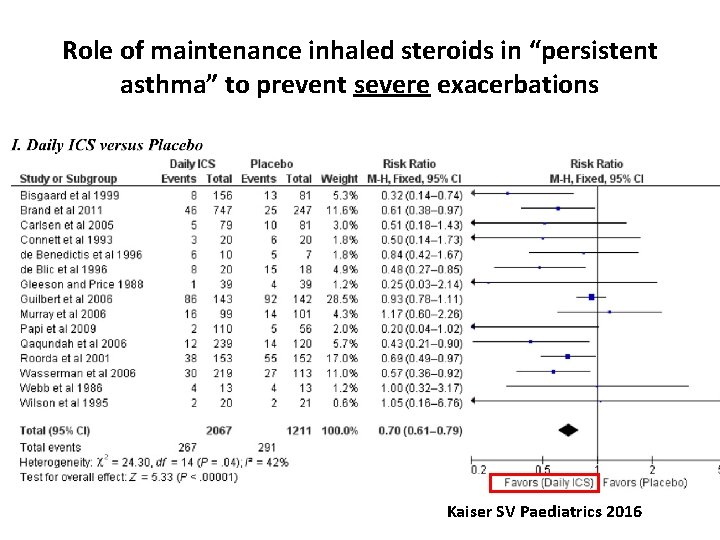
Role of maintenance inhaled steroids in “persistent asthma” to prevent severe exacerbations Kaiser SV Paediatrics 2016
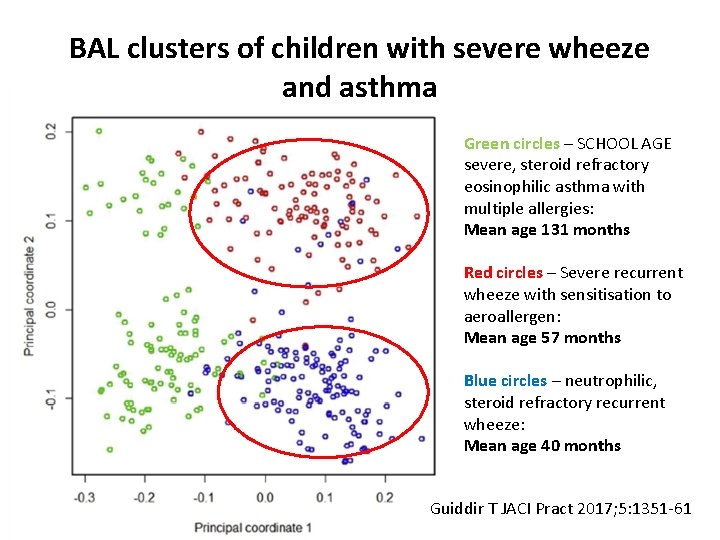
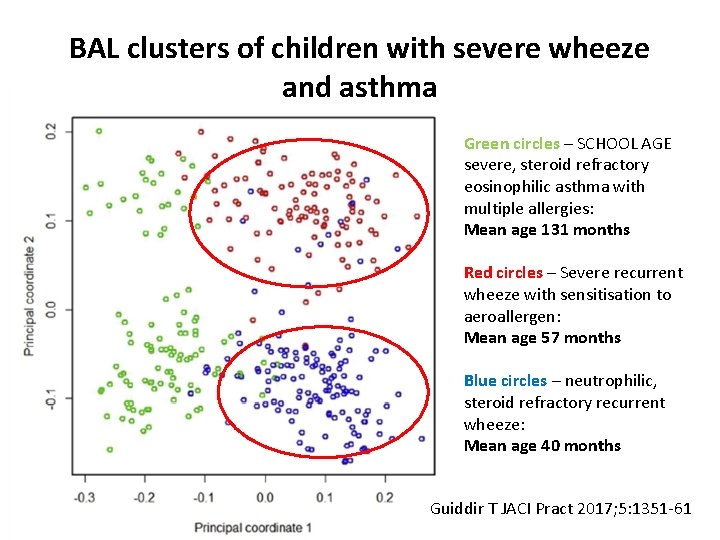
BAL clusters of children with severe wheeze and asthma Green circles – SCHOOL AGE severe, steroid refractory eosinophilic asthma with multiple allergies: Mean age 131 months Red circles – Severe recurrent wheeze with sensitisation to aeroallergen: Mean age 57 months Blue circles – neutrophilic, steroid refractory recurrent wheeze: Mean age 40 months Guiddir T JACI Pract 2017; 5: 1351 -61
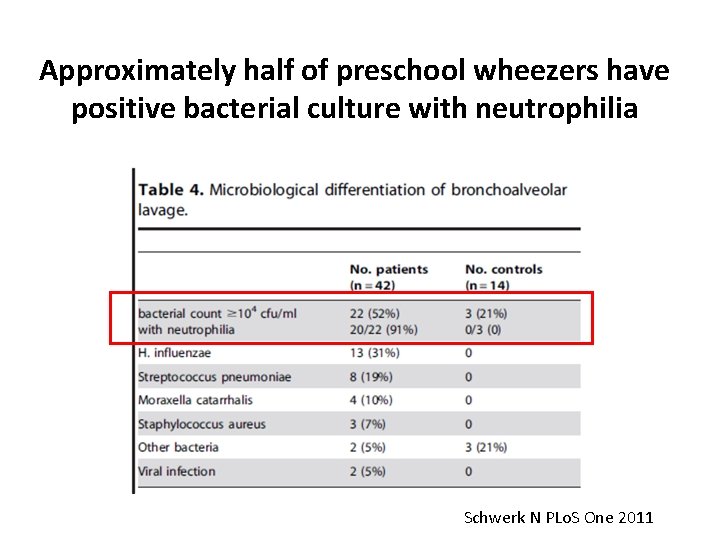
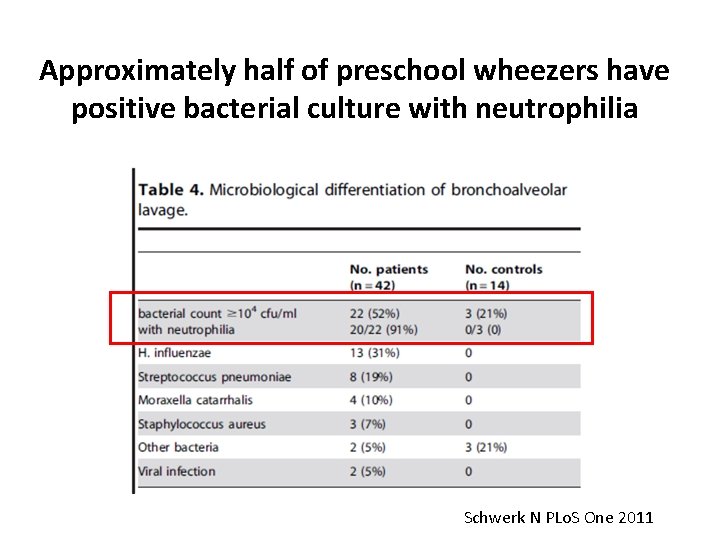
Approximately half of preschool wheezers have positive bacterial culture with neutrophilia Schwerk N PLo. S One 2011
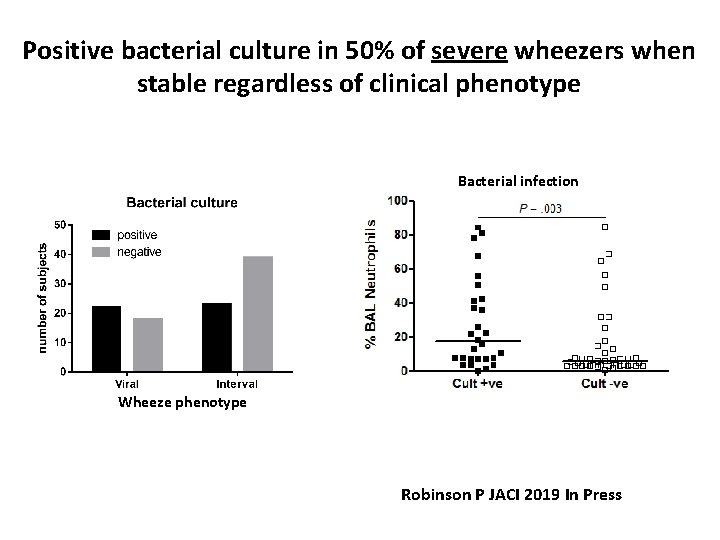
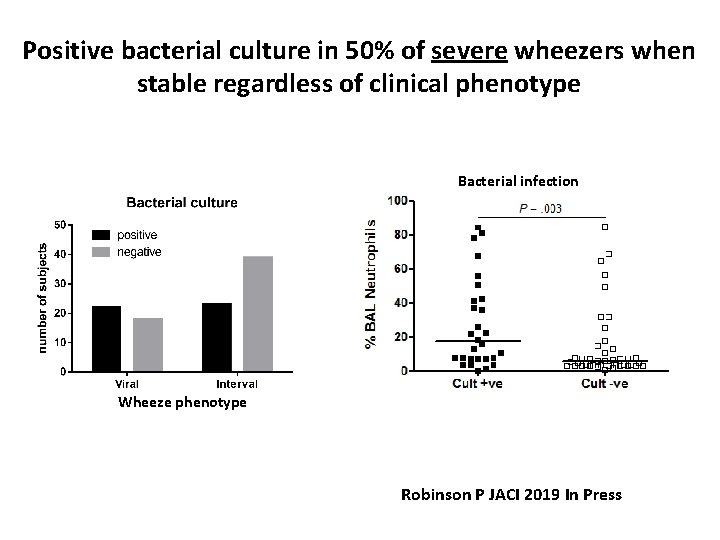
Positive bacterial culture in 50% of severe wheezers when stable regardless of clinical phenotype Bacterial infection Wheeze phenotype Robinson P JACI 2019 In Press
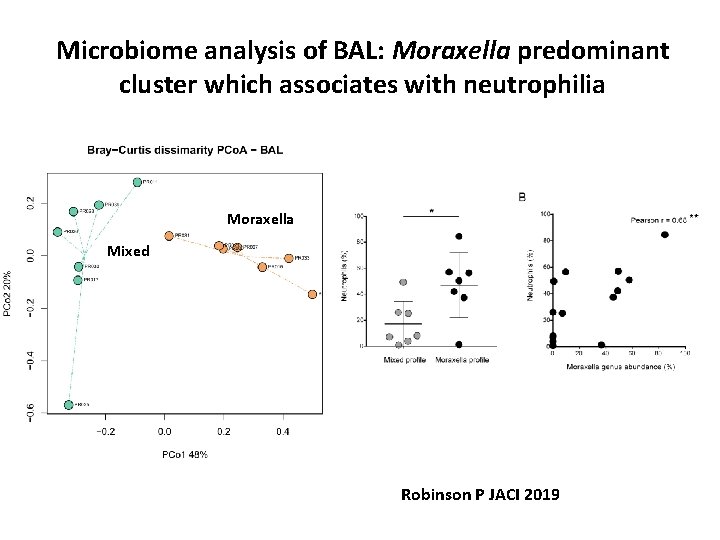
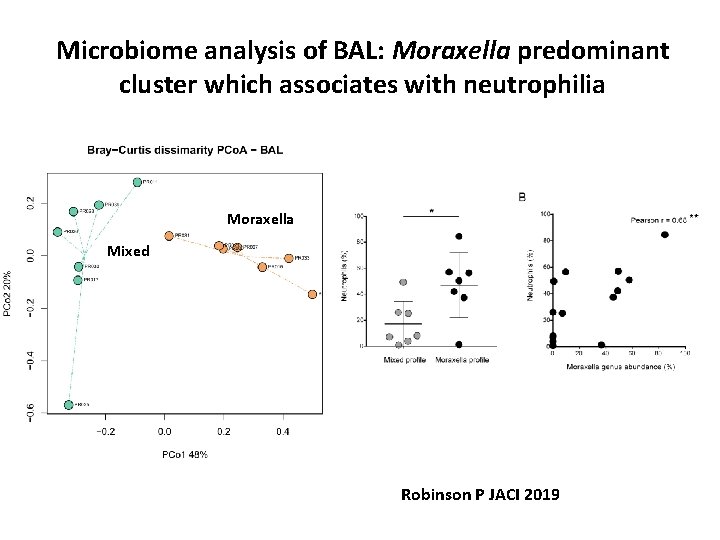
Microbiome analysis of BAL: Moraxella predominant cluster which associates with neutrophilia Moraxella Mixed Robinson P JACI 2019
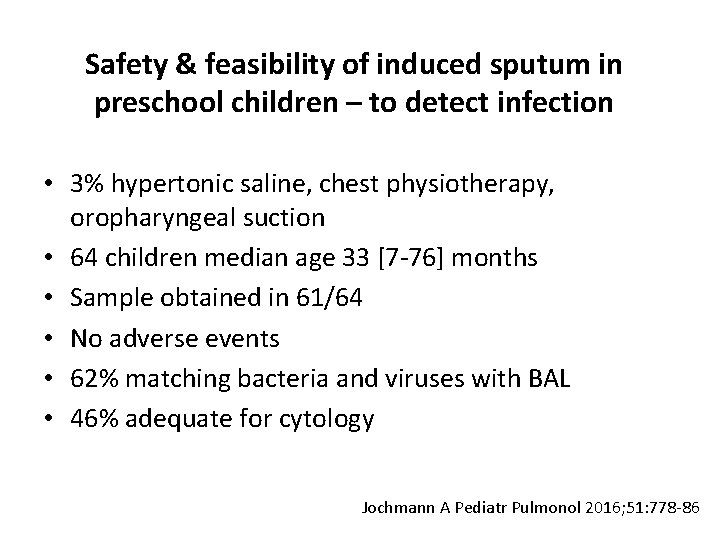
Safety & feasibility of induced sputum in preschool children – to detect infection • 3% hypertonic saline, chest physiotherapy, oropharyngeal suction • 64 children median age 33 [7 -76] months • Sample obtained in 61/64 • No adverse events • 62% matching bacteria and viruses with BAL • 46% adequate for cytology Jochmann A Pediatr Pulmonol 2016; 51: 778 -86
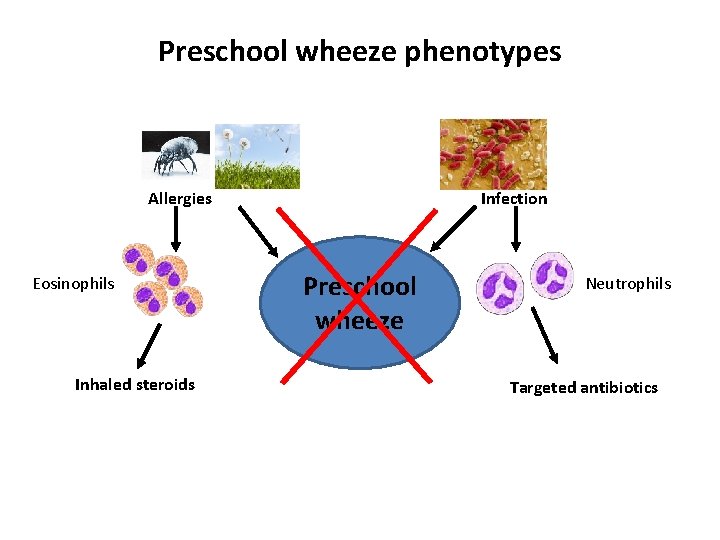
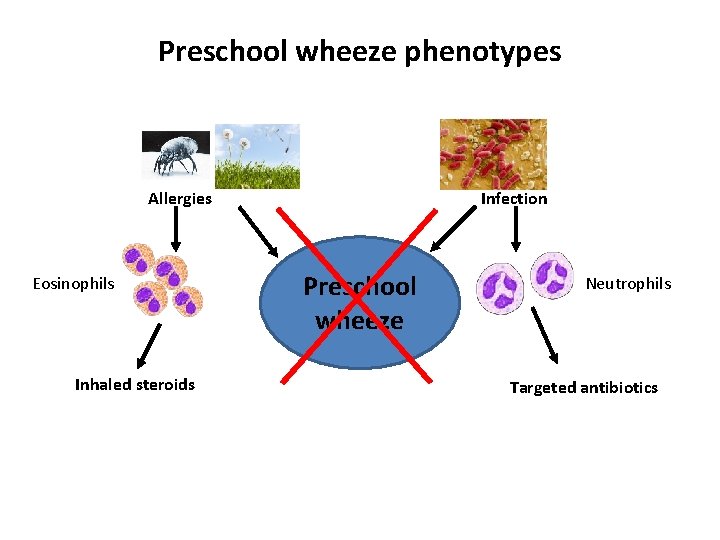
Preschool wheeze phenotypes Allergies Eosinophils Inhaled steroids Infection Preschool wheeze Neutrophils Targeted antibiotics
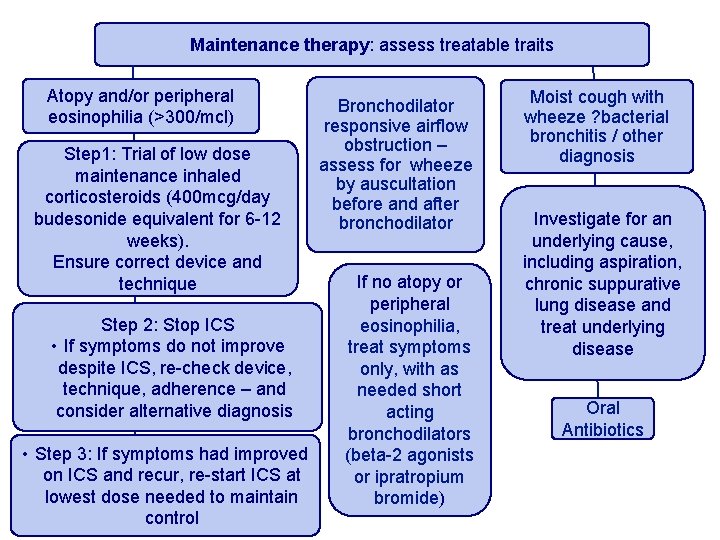
Maintenance therapy: assess treatable traits Atopy and/or peripheral eosinophilia (>300/mcl) Step 1: Trial of low dose maintenance inhaled corticosteroids (400 mcg/day budesonide equivalent for 6 -12 weeks). Ensure correct device and technique Step 2: Stop ICS • If symptoms do not improve despite ICS, re-check device, technique, adherence – and consider alternative diagnosis • Step 3: If symptoms had improved on ICS and recur, re-start ICS at lowest dose needed to maintain control Bronchodilator responsive airflow obstruction – assess for wheeze by auscultation before and after bronchodilator If no atopy or peripheral eosinophilia, treat symptoms only, with as needed short acting bronchodilators (beta-2 agonists or ipratropium bromide) Moist cough with wheeze ? bacterial bronchitis / other diagnosis Investigate for an underlying cause, including aspiration, chronic suppurative lung disease and treat underlying disease Oral Antibiotics

Acknowledgements Inflammation, Repair & Development • • Clare Lloyd Polly Robinson Lisa Gregory Simone Walker Royal Brompton Hospital • • Andy Bush Louise Fleming James Cook Yvonne Bingham Pippa Hall Angela Jamalzadeh Sammy Ndlovu-Dawika
 Clara solomon nyu
Clara solomon nyu Viral induced wheeze vs asthma
Viral induced wheeze vs asthma Bronchovesicular breath sounds
Bronchovesicular breath sounds What is nursing process
What is nursing process Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Second phase of nursing process
Second phase of nursing process Types of nursing diagnoses
Types of nursing diagnoses Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Saguaro infant care and preschool
Saguaro infant care and preschool Type 1 diabetes in adults diagnosis and management
Type 1 diabetes in adults diagnosis and management The webinar will begin shortly
The webinar will begin shortly Preschool foundations volume 1
Preschool foundations volume 1 Ukraine preschool
Ukraine preschool Preschool moral development
Preschool moral development Expulsion
Expulsion Kyrene school schedule
Kyrene school schedule Iqpps standards
Iqpps standards Scripted stories for preschool
Scripted stories for preschool Clouds etiwanda school district
Clouds etiwanda school district Drdp 2015 preschool fundamental view
Drdp 2015 preschool fundamental view Preschool fluency activities
Preschool fluency activities Ca preschool foundations
Ca preschool foundations Preschool learning foundations volume 1
Preschool learning foundations volume 1 Bus stop preschool
Bus stop preschool Preschool learning foundations volume 3
Preschool learning foundations volume 3 Preschool learning foundations social emotional
Preschool learning foundations social emotional Preschool learning foundations
Preschool learning foundations Paducah head start preschool
Paducah head start preschool Objective vs outcome
Objective vs outcome Hippy home instruction for parents of preschool youngsters
Hippy home instruction for parents of preschool youngsters Preschool learning foundations math
Preschool learning foundations math Early childhood screening rochester mn
Early childhood screening rochester mn Clovis unified school district preschool
Clovis unified school district preschool Blended family
Blended family Stages of writing preschool
Stages of writing preschool Panorama heights preschool
Panorama heights preschool Hollingworth preschool
Hollingworth preschool Kyrene school district preschool
Kyrene school district preschool Kyrene cerritos
Kyrene cerritos Iqpps standards
Iqpps standards Preschool room arrangement
Preschool room arrangement Modbury south preschool
Modbury south preschool Es prefix
Es prefix Preschool learning foundations
Preschool learning foundations Magical thinking preschool
Magical thinking preschool Kyrene mirada
Kyrene mirada Jack in the box
Jack in the box Documentation boards for preschool
Documentation boards for preschool Egalia preschool sweden
Egalia preschool sweden Drdp measures at a glance
Drdp measures at a glance Preschool westlake
Preschool westlake Virginia preschool initiative income guidelines 2020
Virginia preschool initiative income guidelines 2020 June preschool newsletter
June preschool newsletter A special place preschool
A special place preschool Preschool learning foundations math
Preschool learning foundations math Preschool infrastructure
Preschool infrastructure Celc lutheran
Celc lutheran Reggio emilia italy preschool
Reggio emilia italy preschool Preschool hemet
Preschool hemet Etiwanda clouds
Etiwanda clouds The mind is a fire to be kindled
The mind is a fire to be kindled Hbpc preschool
Hbpc preschool Pyramid levels of management
Pyramid levels of management Management pyramid
Management pyramid Basic concepts of management
Basic concepts of management Charting identification chapter 28
Charting identification chapter 28 Wright tongue position classification
Wright tongue position classification Endodontic diagnosis and treatment planning
Endodontic diagnosis and treatment planning Chapter 81 brake system technology answers key
Chapter 81 brake system technology answers key Electronic suspension system
Electronic suspension system Chapter 42 gasoline injection diagnosis and repair
Chapter 42 gasoline injection diagnosis and repair Chapter 28 oral diagnosis and treatment planning
Chapter 28 oral diagnosis and treatment planning Automotive technology sixth edition
Automotive technology sixth edition Nursing diagnosis for community health
Nursing diagnosis for community health Brake system diagnosis
Brake system diagnosis