Developing an ACO Measure Set for Maine Michael
![Measure sets significantly ranged in size [max] 108 measures [avg] 29 measures [min] 3 Measure sets significantly ranged in size [max] 108 measures [avg] 29 measures [min] 3](https://slidetodoc.com/presentation_image_h/0b2372a5385e776d5c36b30452ec29fc/image-8.jpg)
- Slides: 42
Developing an ACO Measure Set for Maine Michael Bailit December 10, 2013
Agenda: 1. National Measures Landscape: Buying Value Analysis 2. Measure Selection Processes in Other States 3. Key Policy Decisions in Measure Selection 4. Potential Next Steps for Maine’s Measure Selection Process 2
The Buying Value study § Buying Value… – is a private purchaser-led project to accelerate adoption of value purchasing in the private sector; – believe that selection of appropriate performance measures is fundamental to the success of a value -based payment system, and – convened a payer and purchaser group to promote measure alignment among private and public purchasers, health plans, providers, and state and federal officials. 3
Why is lack of alignment problematic? § The measure misalignment creates what is experienced as “measure chaos” for providers subject to multiple measure sets, with related accountability expectations and sometimes financial implications. § Mixed signals from the market make it difficult for providers to focus their quality improvement efforts and lead them to tune out some payers and some measures. 4
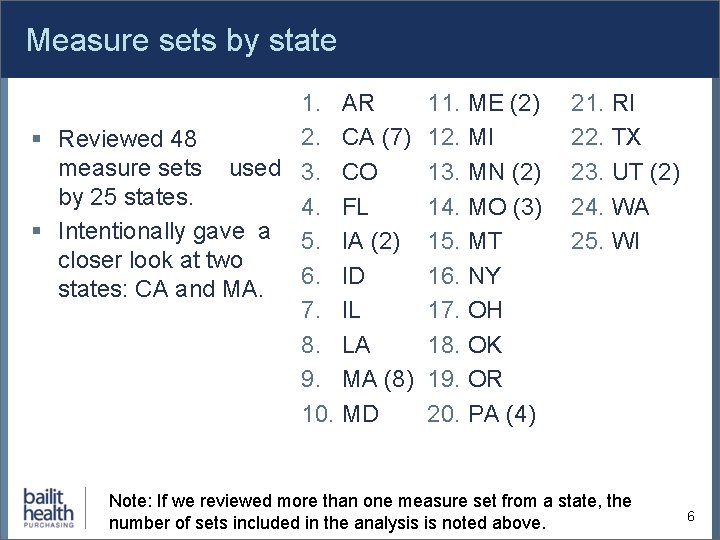
Background on the Buying Value analysis § As part of its effort to promote measure alignment, Buying Value commissioned a recent report from Bailit studying the alignment of state-level measure sets. § To complete this analysis, Bailit gathered 48 measure sets used for different program types, and designed for different purposes, across 25 different states and three regional collaboratives. – Program type examples: ACO, PCMH, Medicaid managed care plan, exchange – Program purpose examples: reporting, payment, reporting and payment, multi-payer alignment 5
Measure sets by state 1. AR 2. CA (7) § Reviewed 48 measure sets used 3. CO by 25 states. 4. FL § Intentionally gave a 5. IA (2) closer look at two 6. ID states: CA and MA. 7. IL 8. LA 9. MA (8) 10. MD 11. ME (2) 12. MI 13. MN (2) 14. MO (3) 15. MT 16. NY 17. OH 18. OK 19. OR 20. PA (4) 21. RI 22. TX 23. UT (2) 24. WA 25. WI Note: If we reviewed more than one measure set from a state, the number of sets included in the analysis is noted above. 6
Analysis included two measure sets from Maine § Systems Core Measure Set obtained from the Maine Health Management Coalition § Measure set used in Maine’s multi-payer PCMH pilot 7
![Measure sets significantly ranged in size max 108 measures avg 29 measures min 3 Measure sets significantly ranged in size [max] 108 measures [avg] 29 measures [min] 3](https://slidetodoc.com/presentation_image_h/0b2372a5385e776d5c36b30452ec29fc/image-8.jpg)
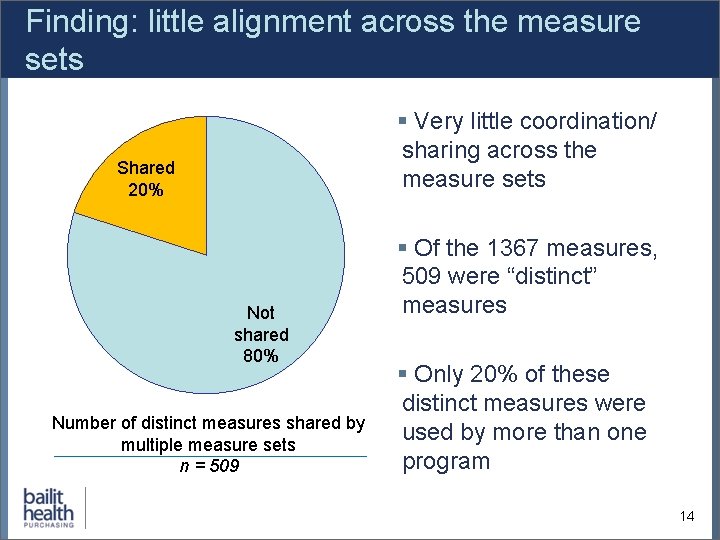
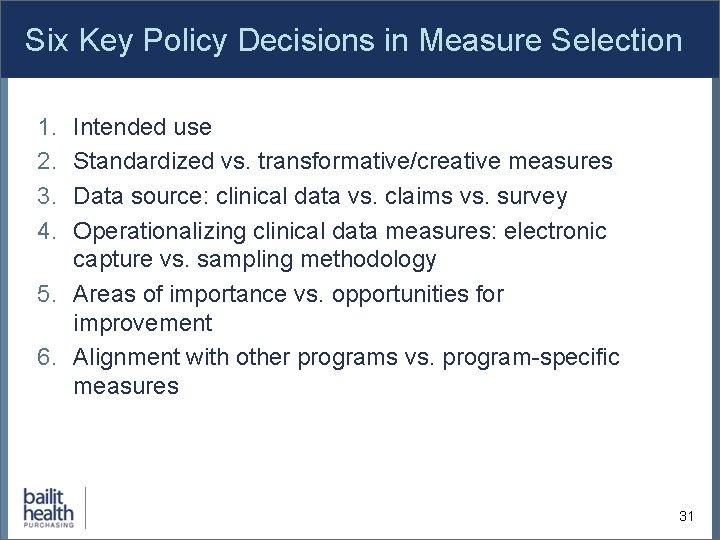
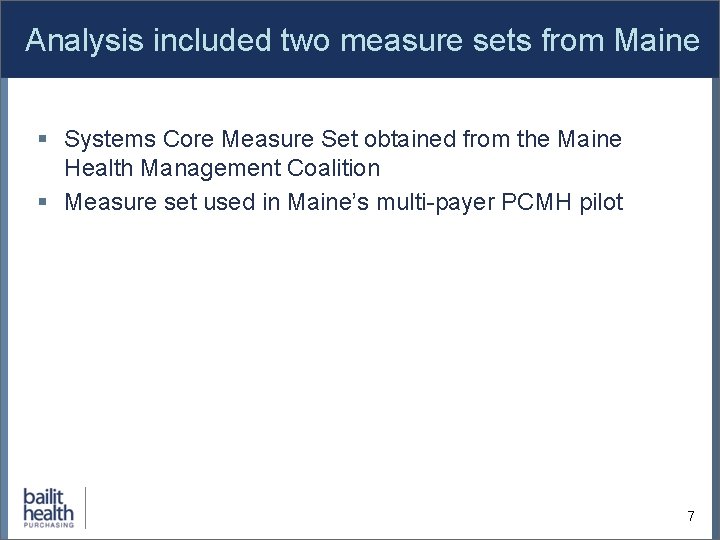
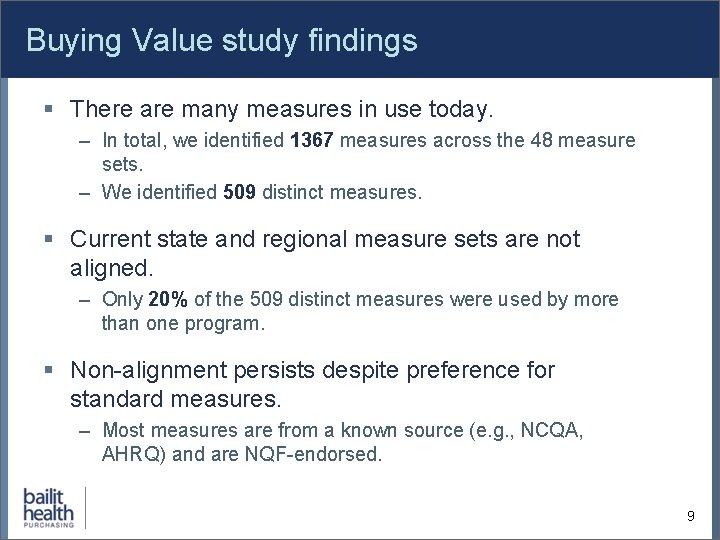
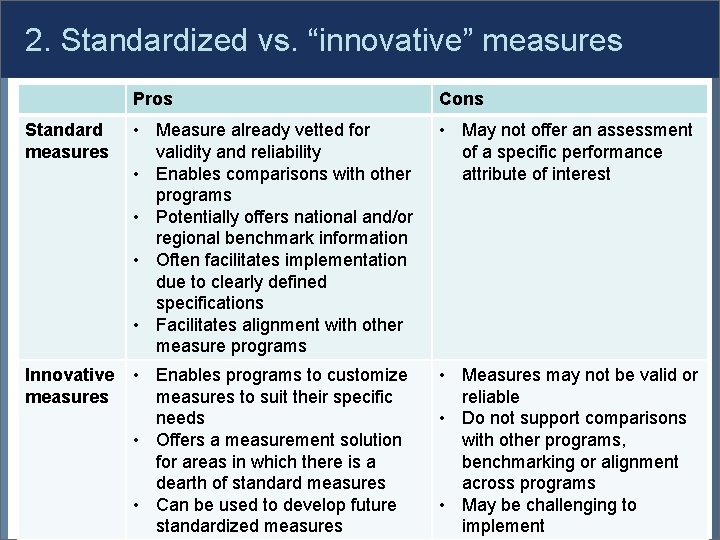
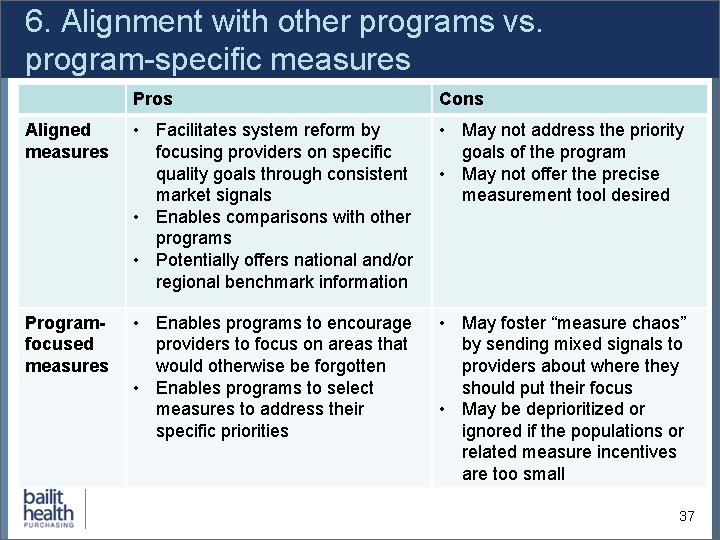
Measure sets significantly ranged in size [max] 108 measures [avg] 29 measures [min] 3 measures Note: This is counting the measures as NQF counts them (or if the measure was not NQF-endorsed, as the program counted them). 8
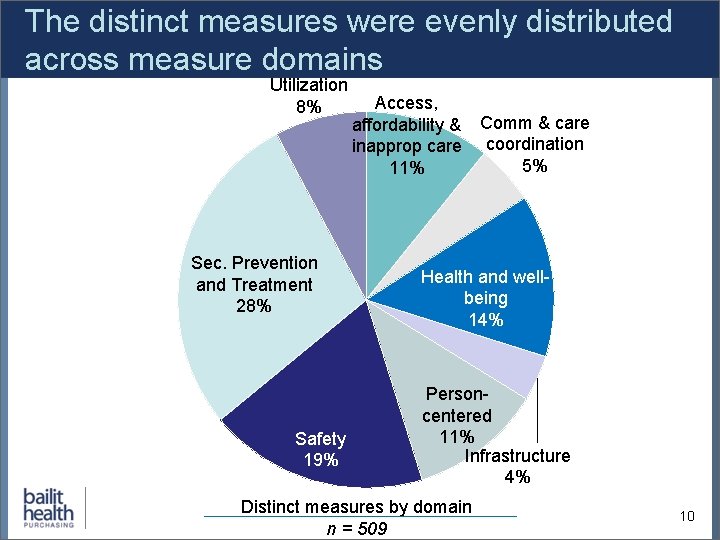
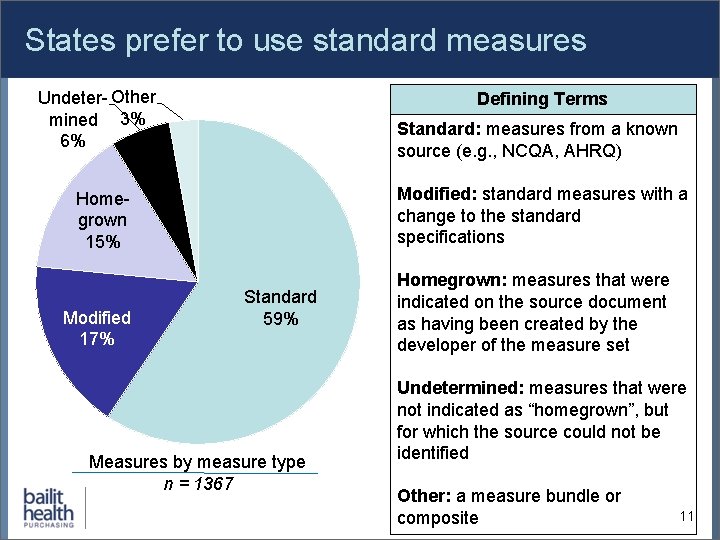
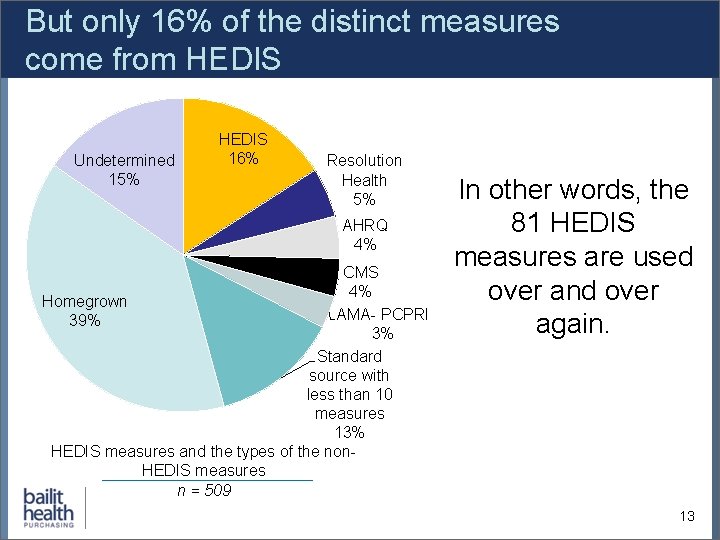
Buying Value study findings § There are many measures in use today. – In total, we identified 1367 measures across the 48 measure sets. – We identified 509 distinct measures. § Current state and regional measure sets are not aligned. – Only 20% of the 509 distinct measures were used by more than one program. § Non-alignment persists despite preference for standard measures. – Most measures are from a known source (e. g. , NCQA, AHRQ) and are NQF-endorsed. 9
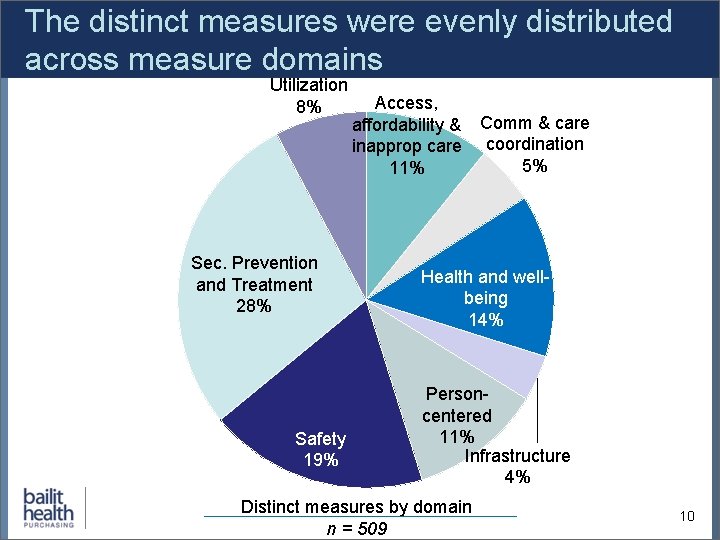
The distinct measures were evenly distributed across measure domains Utilization 8% Sec. Prevention and Treatment 28% Safety 19% Access, affordability & inapprop care 11% Comm & care coordination 5% Health and wellbeing 14% Personcentered 11% Infrastructure 4% Distinct measures by domain n = 509 10
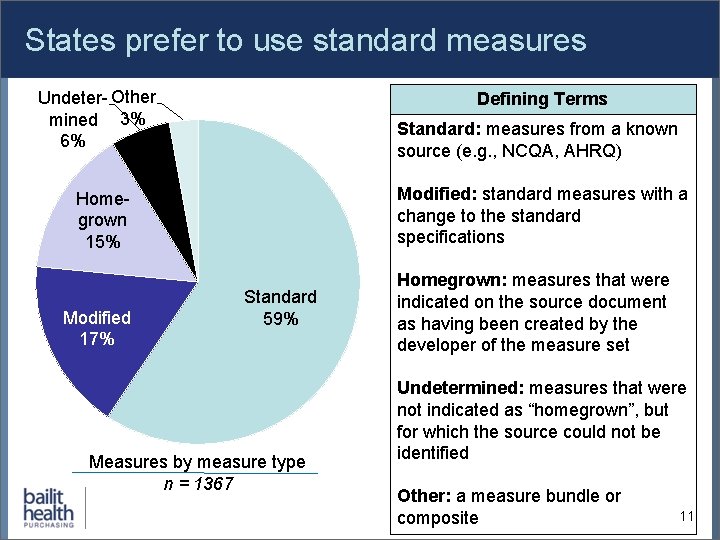
States prefer to use standard measures Undeter- Other mined 3% 6% Defining Terms Standard: measures from a known source (e. g. , NCQA, AHRQ) Modified: standard measures with a change to the standard specifications Homegrown 15% Modified 17% Standard 59% Measures by measure type n = 1367 Homegrown: measures that were indicated on the source document as having been created by the developer of the measure set Undetermined: measures that were not indicated as “homegrown”, but for which the source could not be identified Other: a measure bundle or composite 11
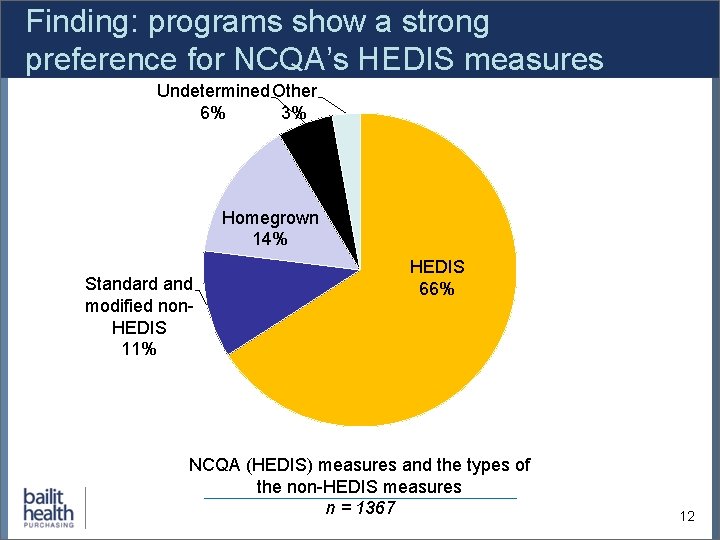
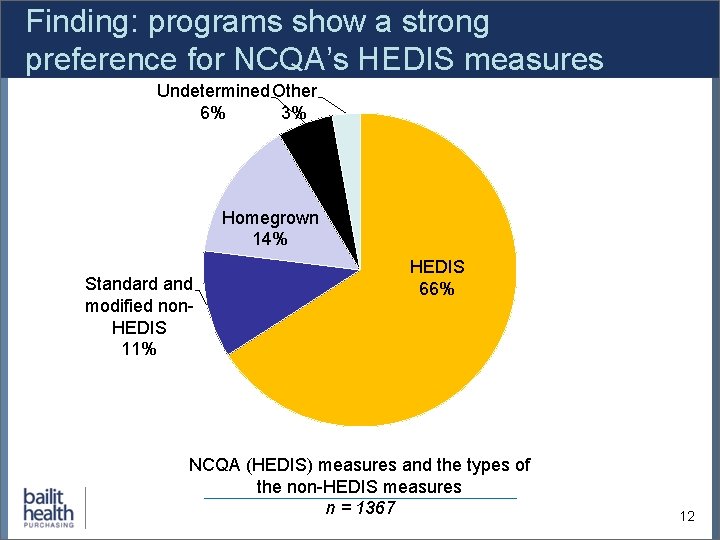
Finding: programs show a strong preference for NCQA’s HEDIS measures Undetermined Other 6% 3% Homegrown 14% Standard and modified non. HEDIS 11% HEDIS 66% NCQA (HEDIS) measures and the types of the non-HEDIS measures n = 1367 12
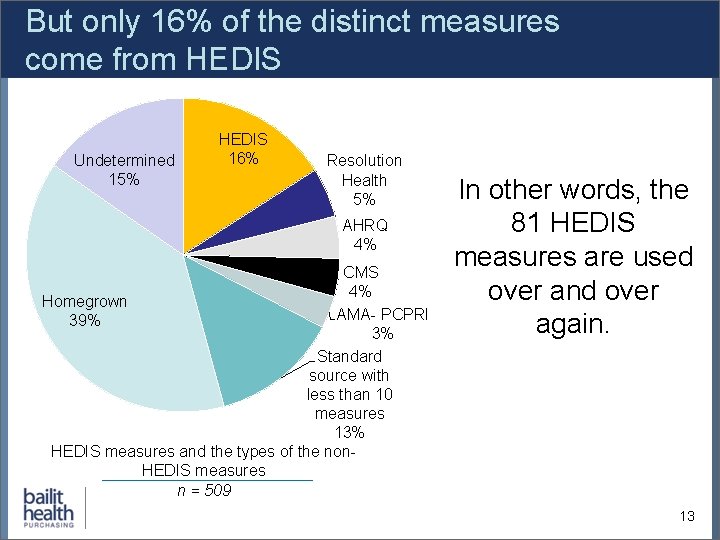
But only 16% of the distinct measures come from HEDIS Undetermined 15% HEDIS 16% Resolution Health 5% AHRQ 4% CMS 4% Homegrown AMA- PCPRI 39% 3% Standard source with less than 10 measures 13% HEDIS measures and the types of the non. HEDIS measures n = 509 In other words, the 81 HEDIS measures are used over and over again. 13
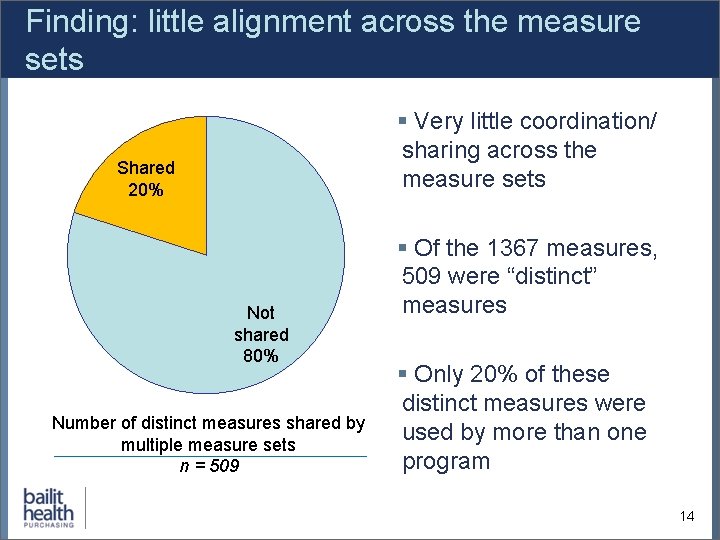
Finding: little alignment across the measure sets § Very little coordination/ sharing across the measure sets Shared 20% Not shared 80% Number of distinct measures shared by multiple measure sets n = 509 § Of the 1367 measures, 509 were “distinct” measures § Only 20% of these distinct measures were used by more than one program 14
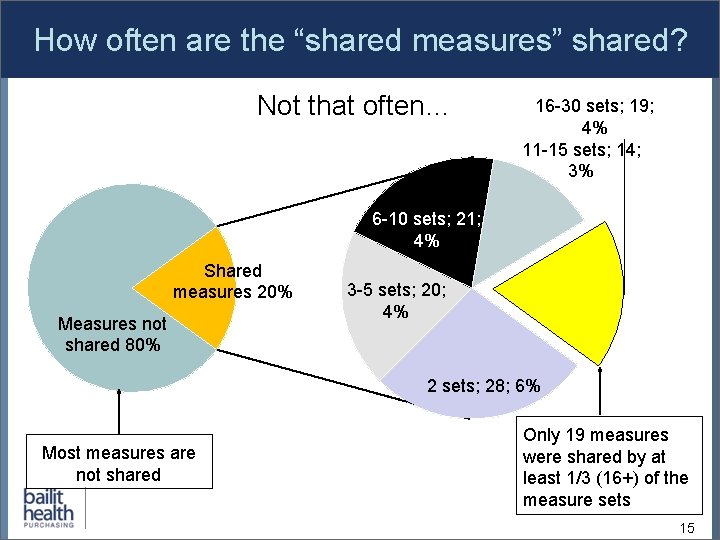
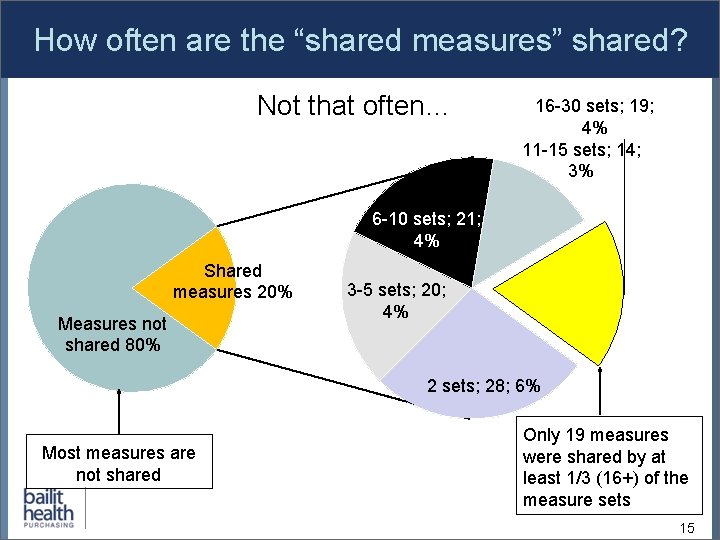
How often are the “shared measures” shared? Not that often… 16 -30 sets; 19; 4% 11 -15 sets; 14; 3% 6 -10 sets; 21; 4% Shared measures 20% Measures not shared 80% 3 -5 sets; 20; 4% 2 sets; 28; 6% Most measures are not shared Only 19 measures were shared by at least 1/3 (16+) of the measure sets 15
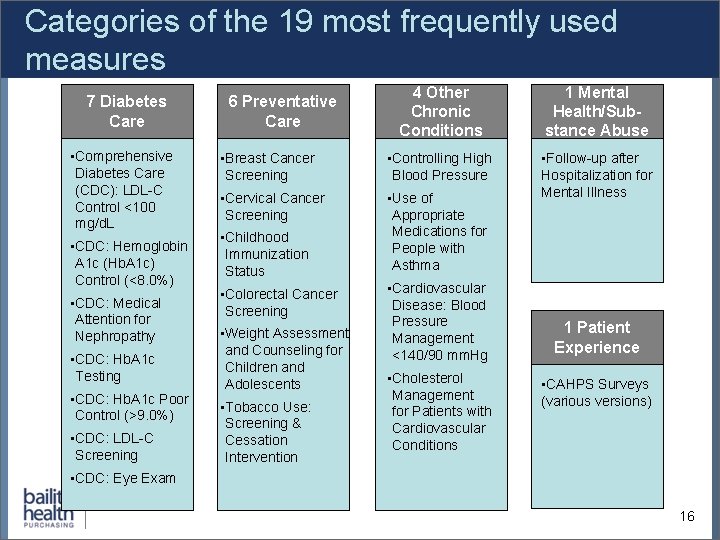
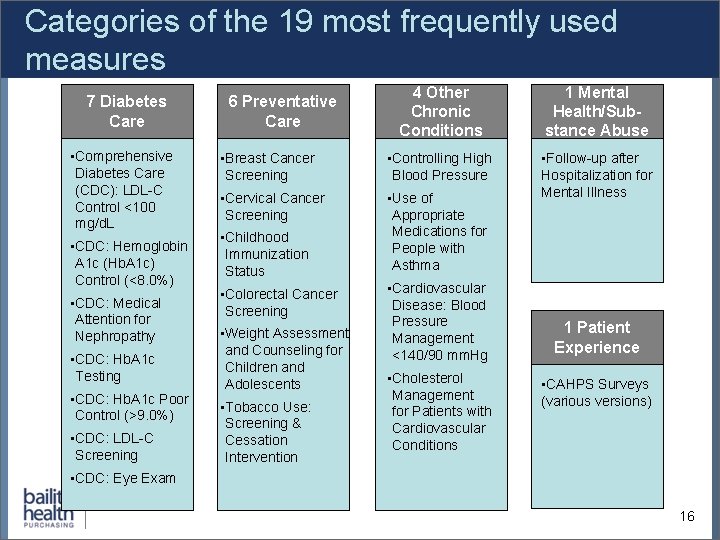
Categories of the 19 most frequently used measures 7 Diabetes Care • Comprehensive Diabetes Care (CDC): LDL-C Control <100 mg/d. L • CDC: Hemoglobin A 1 c (Hb. A 1 c) Control (<8. 0%) • CDC: Medical Attention for Nephropathy • CDC: Hb. A 1 c Testing • CDC: Hb. A 1 c Poor Control (>9. 0%) • CDC: LDL-C Screening 4 Other Chronic Conditions 1 Mental Health/Substance Abuse • Breast Cancer Screening • Controlling High Blood Pressure • Cervical Cancer Screening • Use of Appropriate Medications for People with Asthma • Follow-up after Hospitalization for Mental Illness 6 Preventative Care • Childhood Immunization Status • Colorectal Cancer Screening • Weight Assessment and Counseling for Children and Adolescents • Tobacco Use: Screening & Cessation Intervention • Cardiovascular Disease: Blood Pressure Management <140/90 mm. Hg • Cholesterol Management for Patients with Cardiovascular Conditions 1 Patient Experience • CAHPS Surveys (various versions) • CDC: Eye Exam 16
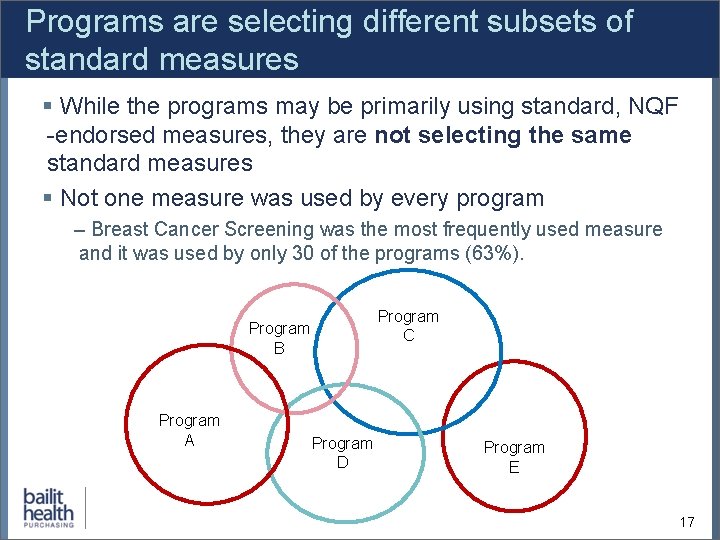
Programs are selecting different subsets of standard measures § While the programs may be primarily using standard, NQF -endorsed measures, they are not selecting the same standard measures § Not one measure was used by every program – Breast Cancer Screening was the most frequently used measure and it was used by only 30 of the programs (63%). Program C Program B Program A Program D Program E 17
State measure set variation Regardless of how we cut the data - by program type, program purpose, domain, and within CA and MA - the programs were not aligned. 18
Conclusions from the Buying Value study 1. Measures sets appear to be developed independently without an eye towards alignment with other sets. 2. The diversity in available measures allows states and regions interested in creating measure sets to select measures that they believe best meet their local needs. 3. Even the few who seek to create alignment struggle due to a paucity of tools to facilitate such alignment. 4. Alignment with other programs won’t happen by chance; it must be a goal that is considered throughout the measure set development process. 19
Agenda: 1. National Measures Landscape/ Buying Value Analysis 2. Measure Selection Processes in Other States 3. Key Policy Decisions in Measure Selection 4. Potential Next Steps for Maine’s Measure Selection Process 20
Measure selection in other states § Bailit has supported multiple states and regions through a measure selection process. § On the next slides we will draw from four of those experiences: – – Colorado Oregon Pennsylvania (AF 4 Q South Central Pennsylvania) Vermont § The slides that follow will provide a brief overview of the different approaches to measure selection and discuss how the factors influenced the unique outcomes. 21
Case Example #1: Colorado Medicaid § Status: Measure set in development § Purpose: Key performance indicator measure set for Regional Care Collaborative Organizations (RCCOs) within the Medicaid program § Type of process: Informal internal deliberation, to be followed by external stakeholder vetting § Stakeholders involved: State Medicaid agency staff, thus far 22
Case Example #1: Colorado Medicaid § Key criteria for measure selection: – Distribution across target populations and within domains of interest – Alignment with other state programs – Feasibility § Unique interests: – Coordination of care measures – Social determinants of health measures – Inclusion of “creative” non-standardized measures 23
Case Example #2: Oregon Medicaid § Status: Two largely overlapping measure sets implemented 1 -1 -13: CMS waiver accountability and CCO incentive pool § Purpose: Incentive measure set for Coordinated Care Organizations (CCOs) required by CMS as a part of its Medicaid section 1115 waiver § Type of process: Formal, state-staffed committee process § Stakeholders involved: Legislatively-mandated physician advisory committee. CCO representatives and health services researchers. 24
Case Example #2: Oregon Medicaid § Key criteria for measure selection: – Representative of the array of services provided and beneficiaries served by the CCOs – Measures must be valid and reliable – Reliance on national measure sets whenever possible § Unique interests: – “Transformative” potential – State-specific opportunities for improvement relative to national benchmarks 25
Case Example #3: AF 4 Q South Central Pennsylvania § Status: Completed but not implemented § Purpose: Multi-payer aligned commercial measure set for PCMHs in the region § Type of process: Formal committee process managed by AF 4 Q staff and key stakeholders § Stakeholders involved: One leading payer and one leading hospital system, with intermittent involvement of other local health plans, hospital systems and employers 26
Case Example #3: AF 4 Q South Central Pennsylvania § Key criteria for measure selection: – Distribution across domains of interest – Alignment with federal measure sets – Feasibility § Unique interests: – Alignment with pre-existing stakeholder-developed measure sets – Relevance for patient-centered medical homes 27
Case Example #4: Vermont multi-payer ACO § Status of Project: Completed and slated to be implemented 1 -1 -14 § Purpose: Measure set for coordinated Medicaid and commercial insurer ACO pilot program § Type of process: Formal, state-staffed committee process § Stakeholders involved: Potential ACOs, payers (commercial and Medicaid), consumer advocates, provider associations, quality improvement organization 28
Case Example #4: Vermont multi-payer ACO § Key criteria for measure selection: – Representative of the array of services provided and beneficiaries – NQF-endorsed measures that have relevant benchmarks whenever possible § Unique interests: – Alignment with Medicare Shared Savings Program – Alignment with HEDIS – State-specific opportunities for improvement relative to national benchmarks – Use of systems measures, utilization measures and pending measures 29
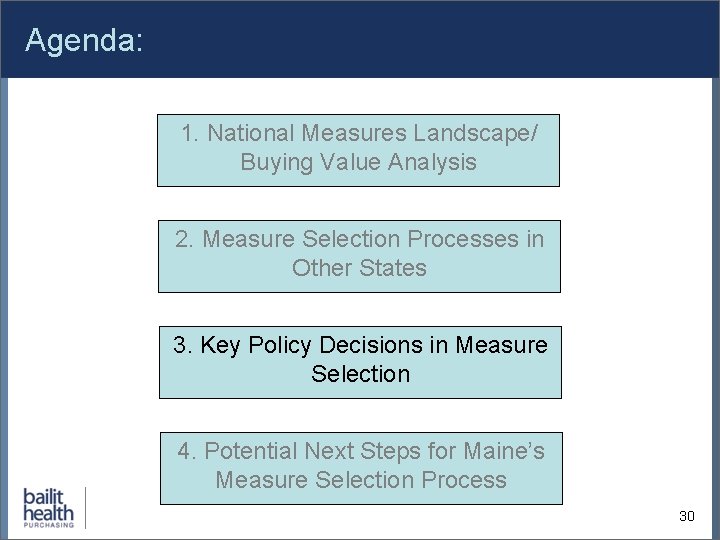
Agenda: 1. National Measures Landscape/ Buying Value Analysis 2. Measure Selection Processes in Other States 3. Key Policy Decisions in Measure Selection 4. Potential Next Steps for Maine’s Measure Selection Process 30
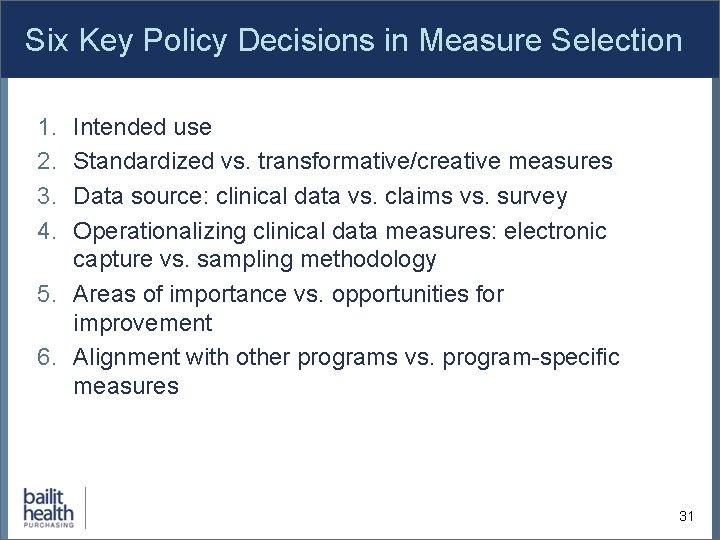
Six Key Policy Decisions in Measure Selection 1. 2. 3. 4. Intended use Standardized vs. transformative/creative measures Data source: clinical data vs. claims vs. survey Operationalizing clinical data measures: electronic capture vs. sampling methodology 5. Areas of importance vs. opportunities for improvement 6. Alignment with other programs vs. program-specific measures 31
1. Intended use § Measures can be used for multiple purposes. The first question to ask when forming a measure set is “measurement to what end”? § Measures may be more appropriate for some uses and not others at a particular point in time. § Some potential measure uses: – Assessing performance relative to goals and expectations – Qualifying and/or modifying payment – Observing states and trends 32
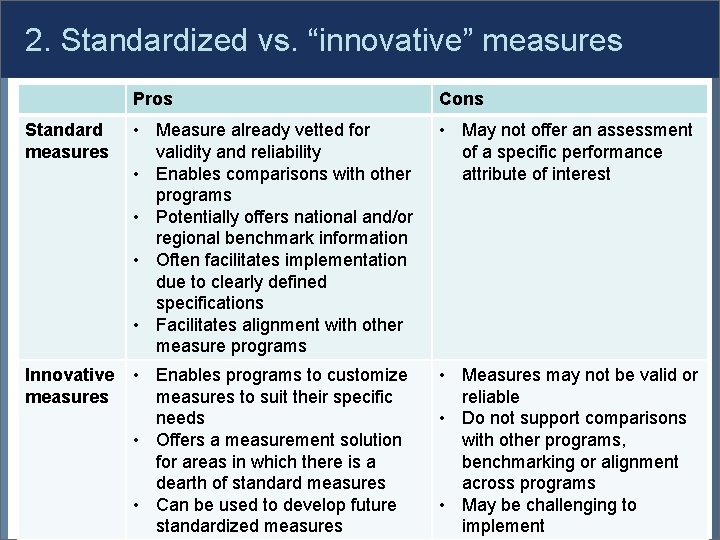
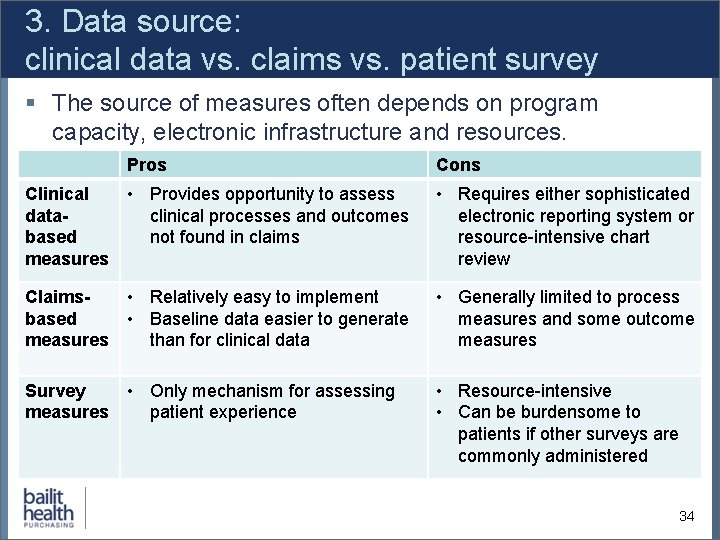
2. Standardized vs. “innovative” measures Pros Cons Standard measures • Measure already vetted for validity and reliability • Enables comparisons with other programs • Potentially offers national and/or regional benchmark information • Often facilitates implementation due to clearly defined specifications • Facilitates alignment with other measure programs • May not offer an assessment of a specific performance attribute of interest Innovative measures • Enables programs to customize measures to suit their specific needs • Offers a measurement solution for areas in which there is a dearth of standard measures • Can be used to develop future standardized measures • Measures may not be valid or reliable • Do not support comparisons with other programs, benchmarking or alignment across programs • May be challenging to 33 implement
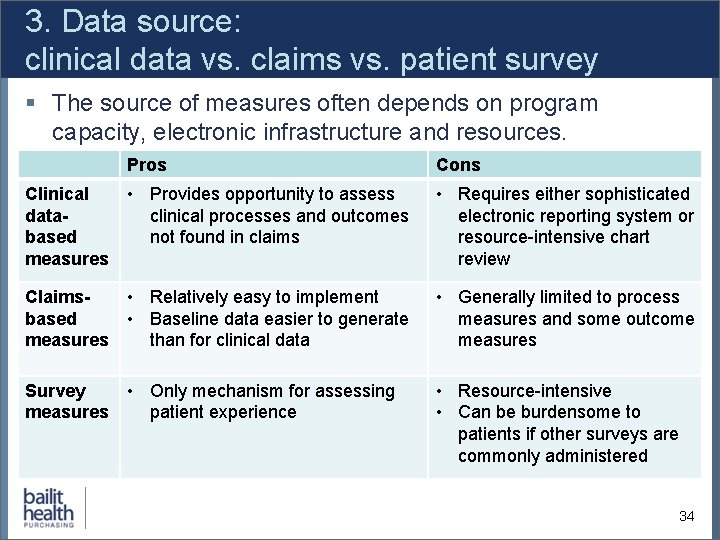
3. Data source: clinical data vs. claims vs. patient survey § The source of measures often depends on program capacity, electronic infrastructure and resources. Pros Cons Clinical • Provides opportunity to assess dataclinical processes and outcomes based not found in claims measures • Requires either sophisticated electronic reporting system or resource-intensive chart review Claims • Relatively easy to implement based • Baseline data easier to generate measures than for clinical data • Generally limited to process measures and some outcome measures Survey • Only mechanism for assessing measures patient experience • Resource-intensive • Can be burdensome to patients if other surveys are commonly administered 34
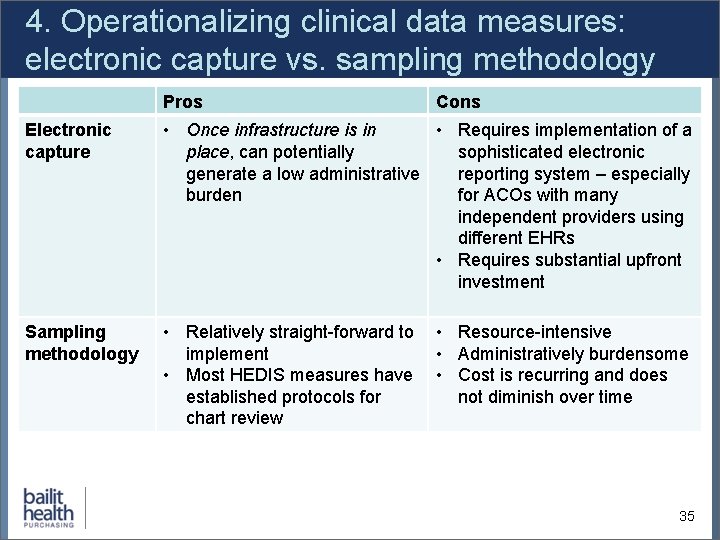
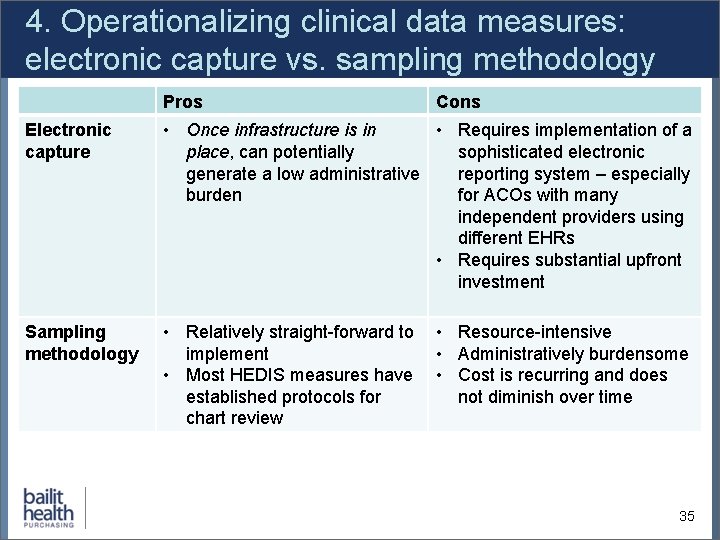
4. Operationalizing clinical data measures: electronic capture vs. sampling methodology Pros Cons Electronic capture • Once infrastructure is in • Requires implementation of a place, can potentially sophisticated electronic generate a low administrative reporting system – especially burden for ACOs with many independent providers using different EHRs • Requires substantial upfront investment Sampling methodology • Relatively straight-forward to implement • Most HEDIS measures have established protocols for chart review • Resource-intensive • Administratively burdensome • Cost is recurring and does not diminish over time 35
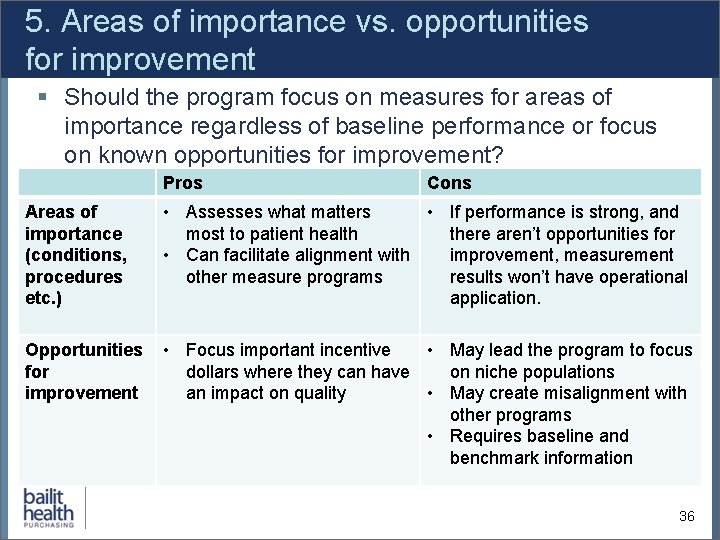
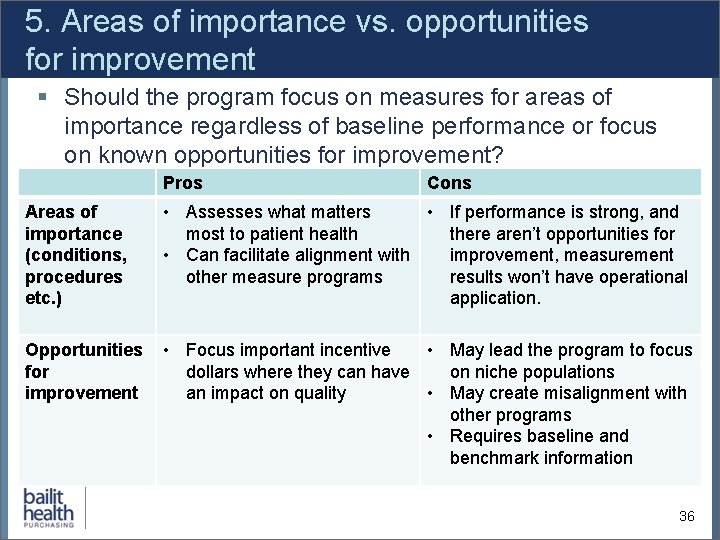
5. Areas of importance vs. opportunities for improvement § Should the program focus on measures for areas of importance regardless of baseline performance or focus on known opportunities for improvement? Pros Cons Areas of importance (conditions, procedures etc. ) • Assesses what matters • If performance is strong, and most to patient health there aren’t opportunities for • Can facilitate alignment with improvement, measurement other measure programs results won’t have operational application. Opportunities for improvement • Focus important incentive • May lead the program to focus dollars where they can have on niche populations an impact on quality • May create misalignment with other programs • Requires baseline and benchmark information 36
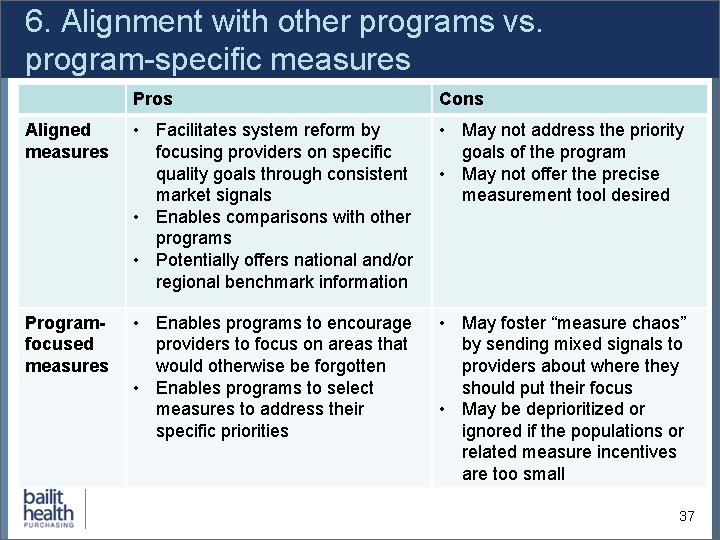
6. Alignment with other programs vs. program-specific measures Pros Cons Aligned measures • Facilitates system reform by focusing providers on specific quality goals through consistent market signals • Enables comparisons with other programs • Potentially offers national and/or regional benchmark information • May not address the priority goals of the program • May not offer the precise measurement tool desired Programfocused measures • Enables programs to encourage providers to focus on areas that would otherwise be forgotten • Enables programs to select measures to address their specific priorities • May foster “measure chaos” by sending mixed signals to providers about where they should put their focus • May be deprioritized or ignored if the populations or related measure incentives are too small 37
Agenda: 1. National Measures Landscape/ Buying Value Analysis 2. Measure Selection Processes in Other States 3. Key Policy Decisions in Measure Selection 4. Potential Next Steps for Maine’s Measure Selection Process 38
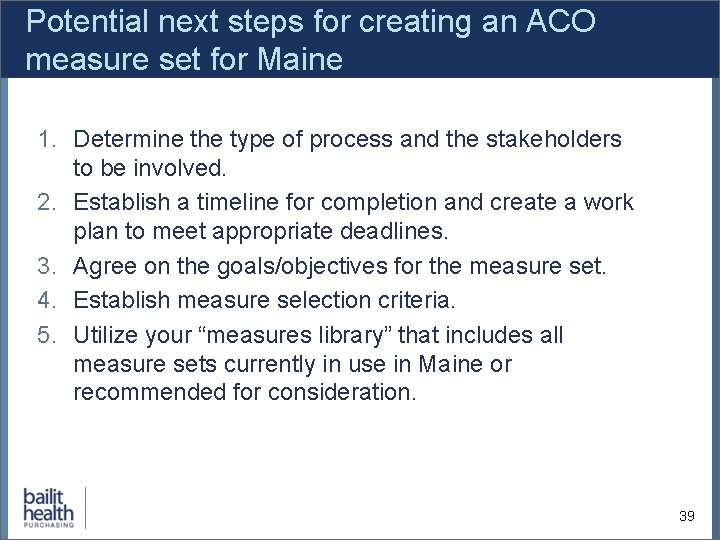
Potential next steps for creating an ACO measure set for Maine 1. Determine the type of process and the stakeholders to be involved. 2. Establish a timeline for completion and create a work plan to meet appropriate deadlines. 3. Agree on the goals/objectives for the measure set. 4. Establish measure selection criteria. 5. Utilize your “measures library” that includes all measure sets currently in use in Maine or recommended for consideration. 39
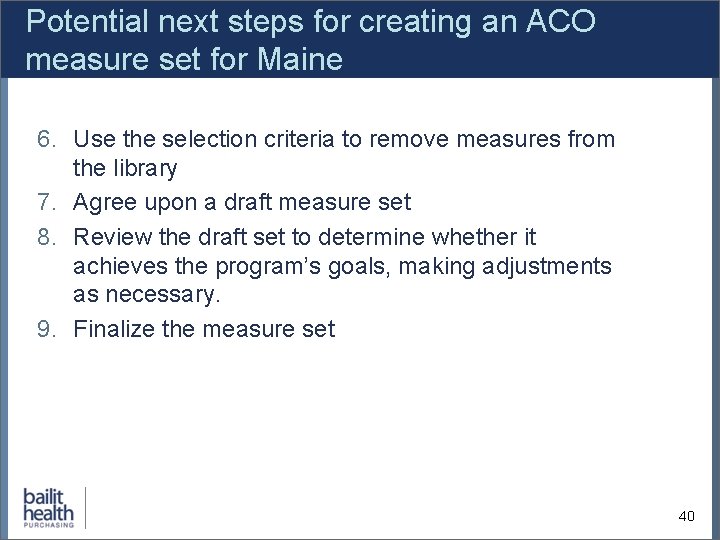
Potential next steps for creating an ACO measure set for Maine 6. Use the selection criteria to remove measures from the library 7. Agree upon a draft measure set 8. Review the draft set to determine whether it achieves the program’s goals, making adjustments as necessary. 9. Finalize the measure set 40
Final considerations § Reaching agreement on a core measure set takes considerable time and effort – many facilitated meetings, staff work to prepare for each meeting and a willingness to compromise. § Measure sets are not static. They need to be reviewed each year and modified based on implementation experience, changing clinical standards, changing priorities, and (hopefully) improved performance. 41
Contact information Michael Bailit, MBA • • mbailit@bailithealth. com 781 -453 -1166