CVA Scenario 79 yearold woman arrives at the
- Slides: 33
CVA
Scenario • 79 -year-old woman, arrives at the emergency room with expressive aphasia, left facial droop, left-sided hemiparesis, and mild dysphagia • husband states that when she awoke that morning at 0600, she stayed in bed, complaining of a mild headache over the right temple and feeling slightly weak • He went and got coffee, then thinking it was unusual for her to have those complaints, went back to check on her. He found she was having some trouble saying words and had developed a leftsided facial droop. • When he helped her up from the bedside, he noticed weakness in her left hand leg and brought her to the emergency department.
Past Medical History • • Paroxysmal atrial fibrillation Hypertension-well controlled Hyperlipidemia Recent cardiac stress test had normal findings
Medications • • • Flecainide (Tambocor) 100 mg BID Hormone replacement therapy Amlodipine 5 mg qd Aspirin 81 mg daily Simvastatin 20 mg qhs Lisinopril 10 mg qd
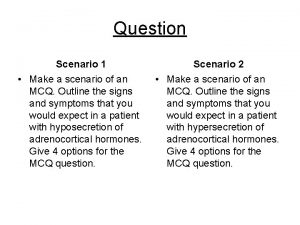
Question • The ED physician suspects a CVA • What role do diagnostic tests play in evaluating this patient for a suspected CVA?
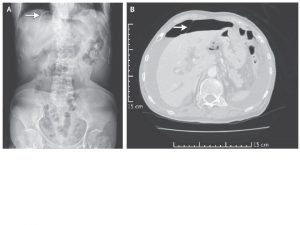
Answer • Noncontrast computed tomography (CT) scan is the primary test used to diagnose a stroke. CT can differentiate between ischemic and hemorrhagic stroke. • The CT scan should be obtained within 25 minutes and read within 45 minutes of arrival at the emergency department. • If the stroke is ischemic and is less than 3 hours old, the CT will appear normal because the brain structure with or without blood flow appears the same in a noncontrast CT scan.
Question • What other diagnostic test might be ordered at this time (not of the brain)?
Answer • Pt has a history of PAF; an electrocardiogram (ECG) will be necessary to evaluate rhythm status. • An echocardiogram would be helpful for evaluating the possibility of thrombi in the atria or ventricle. • A carotid ultrasound is used to identify any atherosclerotic plaques.
Question • Which factor in this patient’s history is the most likely contributor to her having experienced a CVA?
Answer • There is overwhelming evidence linking PAF to increased stroke risk. • Studies have shown that patients with PAF should be on chronic anticoagulation.
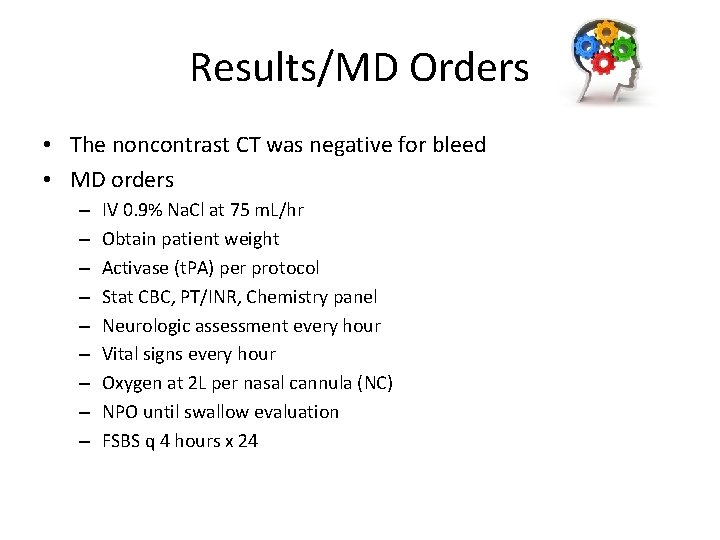
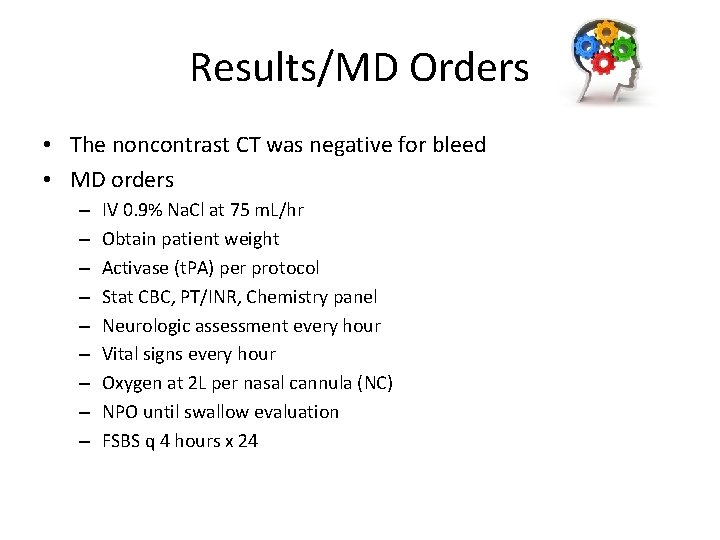
Results/MD Orders • The noncontrast CT was negative for bleed • MD orders – – – – – IV 0. 9% Na. Cl at 75 m. L/hr Obtain patient weight Activase (t. PA) per protocol Stat CBC, PT/INR, Chemistry panel Neurologic assessment every hour Vital signs every hour Oxygen at 2 L per nasal cannula (NC) NPO until swallow evaluation FSBS q 4 hours x 24
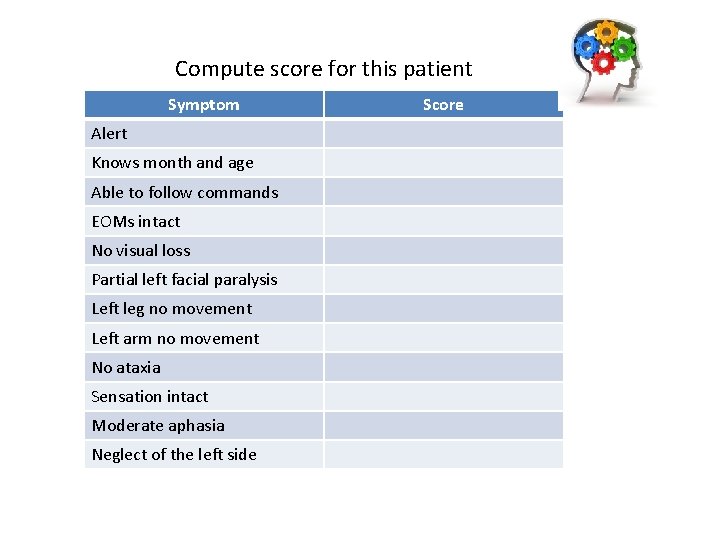
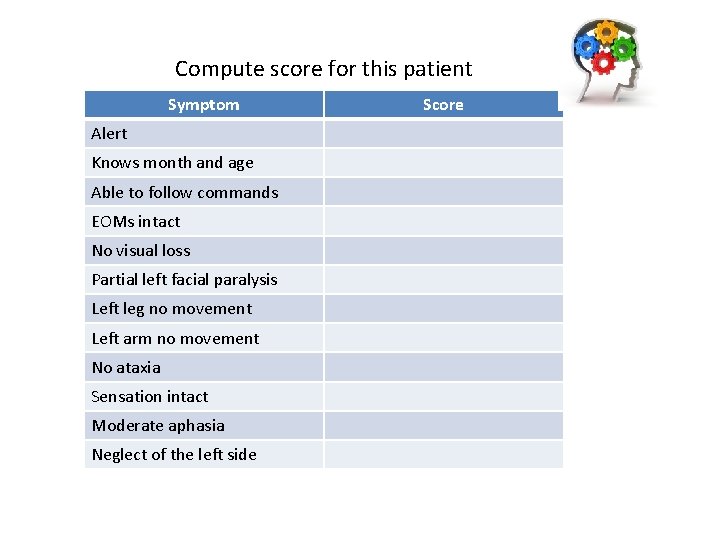
Compute score for this patient Symptom Alert Knows month and age Able to follow commands EOMs intact No visual loss Partial left facial paralysis Left leg no movement Left arm no movement No ataxia Sensation intact Moderate aphasia Neglect of the left side Score
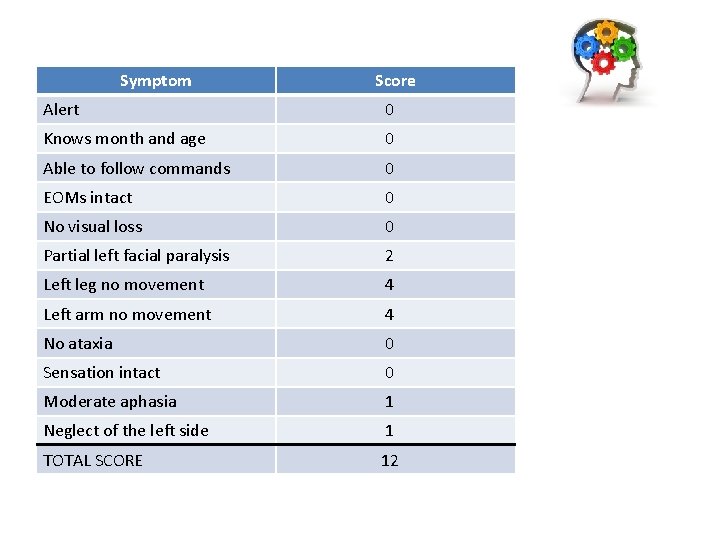
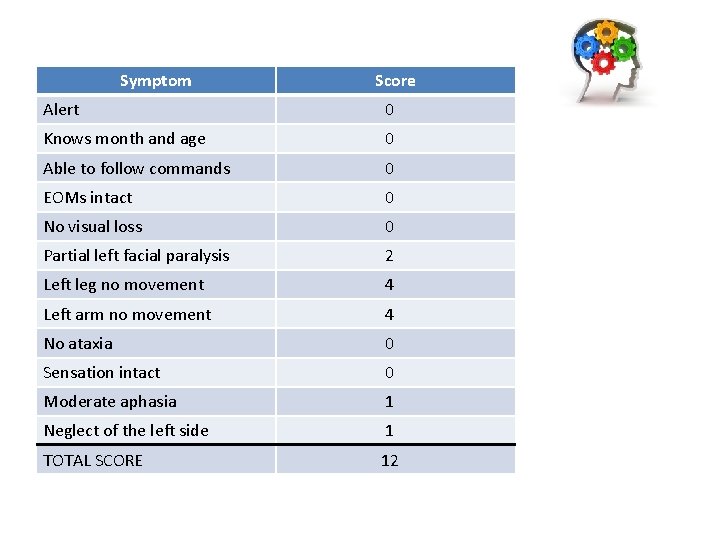
Symptom Score Alert 0 Knows month and age 0 Able to follow commands 0 EOMs intact 0 No visual loss 0 Partial left facial paralysis 2 Left leg no movement 4 Left arm no movement 4 No ataxia 0 Sensation intact 0 Moderate aphasia 1 Neglect of the left side 1 TOTAL SCORE 12
What level of CVA did she have? • She scored a 12, which places her stroke in the “moderate” stroke category
Contraindications for beginning fibrinolytic therapy include which of the following? Select all that apply. a. Currently on Coumadin with an INR of 2. 4 b. Major surgery in the last 14 days c. Systolic BP of 150 d. Platelet count of less than 100, 000 e. Blood glucose of less than 50 mg/d. L f. History of myocardial infarction 1 year ago g. Improving neurologic status
Answers • a, b, d, e, f, g • For a patient to qualify for fibrinolytic therapy, the neurologic signs should not be clearing spontaneously. • There should be no history of head trauma, myocardial infarction, or prior stroke in the past 3 months or major surgery in past 14 days. • The patient's platelet count must be greater than 100, 000 and the blood glucose level greater than 50 mg/d. L (2. 7 mmol). • The systolic BP needs to be less than 185 and the diastolic BP less than 110. • The patient should not be taking an oral anticoagulant; if so, the INR must be less than 1. 7
Question • What are your responsibilities during the administration of Activase (t. PA)?
Answer • During the infusion, you need to perform a neurologic check, assess vital signs, and inspect the infusion site for bleeding every 15 minutes for the first hour, every 30 minutes for the next 2 hours, and then hourly for 24 hours. • Place her on an ECG monitor. Initiate bleeding precautions. • If the drug is infusing peripherally in the unaffected arm, have her keep the extremity still and straight.
Case Progression • The patient is admitted to the neurology unit • The following day an MRI reveals a small CVA in the right hemisphere • She is placed on flecainide, amlodipine, clopidogrel, aspirin, simvastatin, and lisinopril
Question • If her deficits are temporary, how long might it take before they completely reverse?
Answer • Maximum resolution of mild deficits usually takes 6 months to 1 year.
Question During the first 24 hours after receipt of Activase, the primary concern is controlling the patient’s a) Cardiac rhythm b) BP c) Glucose level d) Oxygen saturation
Answer • Although all parameters must be monitored and controlled, the BP is the most vital. • A number of patients experience post-CVA HTN. • BP may need to be lowered to reduce the risk of hemorrhage and worsening cerebral edema. • However, overly aggressive lowering of the BP may compromise cerebral blood flow in the area surrounding the infarct resulting in stroke extension.
Question While assessing her, you note the following findings. Which one is unrelated to the CVA? a) Headache b) Lethargy c) Lumbar pain d) Blurred vision
Answer • Lumbar pain is not a neurologic symptom associated with a CVA. • The exact signs and symptoms of a stroke are dependent on the type of stroke and the location of the injury. • Although motor deficits are the more common symptoms of a CVA, a decreased level of consciousness, headache, and blurred vision are commonly occurring manifestations that are noted in many patients, regardless of the location or type of stroke.
Question Why was this patient placed on clopidogrel (Plavix) post-CVA?
Answer • Clopidogrel plus aspirin is currently recommended to prevent platelet aggregation and thereby prevent CVA and secondary CVA
Question Because this patient had a thrombolytic infusion, how many hours should you wait before beginning administration of any anticoagulant or antiplatelet medications?
Answer • 24 hours
Question Is there any benefit from continuing simvastatin (Zocor) after her CVA?
Answer • statins, have been shown to dramatically reduce the incidence of first and second CVAs. • It is believed that statins stabilize the endothelial wall and prevent plaque ruptures.
Question As you walk into the nurses’ station, the charge nurse is coordinating the swallowing evaluation, including a modified barium swallow study and referral for a speech-language pathologist. Give the rationale for these orders
Answer • Because symptoms of probable dysphagia were noted on the initial examination, a modified barium swallow study is done to show food is taken into the mouth, chewed, propelled to the posterior pharynx, and swallowed. • The SLP makes the diagnosis of dysphagia, recommends the safest position of the head for eating, and recommends the optimal food texture and liquid consistency to prevent aspiration.
 A woman travels in a lift. the mass of the woman is 50 kg
A woman travels in a lift. the mass of the woman is 50 kg Alex tickles his brother by stroking adjacent
Alex tickles his brother by stroking adjacent Once upon a time there lived a woman who had two daughters
Once upon a time there lived a woman who had two daughters Sensation vs perception
Sensation vs perception Who is the priest in oedipus
Who is the priest in oedipus Neil thisse is a loyalist answers
Neil thisse is a loyalist answers When command is transferred the process should include
When command is transferred the process should include What goes up but never comes down
What goes up but never comes down Cva vs tia
Cva vs tia Cva rwa
Cva rwa Left hemiparesis
Left hemiparesis Bilateral cva
Bilateral cva Libra nms
Libra nms Pisanje cva
Pisanje cva Cva complications
Cva complications Cva
Cva Dullness to percussion
Dullness to percussion Citas apa itesm
Citas apa itesm Cva
Cva Primer cv-a
Primer cv-a Cva tenderness
Cva tenderness Dwanghuilen na cva
Dwanghuilen na cva Cva paris nanterre edt
Cva paris nanterre edt Periodontal treatment of medically compromised patients
Periodontal treatment of medically compromised patients Cva tenderness
Cva tenderness Snijegović
Snijegović Costovertebral angle tenderness
Costovertebral angle tenderness đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Tư thế worm breton là gì
Tư thế worm breton là gì Bổ thể
Bổ thể ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi