Creating an Integrated Mental Health Service Delivery Systems
- Slides: 39
Creating an Integrated Mental Health Service Delivery Systems for High-Needs Youth Jennifer F. Havens, MD Vice Chair for Public Psychiatry Department of Child and Adolescent Psychiatry NYU School of Medicine Director and Chief of Service Department of Child and Adolescent Psychiatry Bellevue Hospital Center
Conflict of Interest • Dr. Havens serves on the medical advisory board of Mindyra
Learning Objectives • Participants will understand challenges in the existing child mental health care system to effective care for high-needs youth • Participants will become familiar with models for effective emergency psychiatric care for youth • Participants will understand the importance of integrating trauma-informed care into inpatient treatment • Participants will understand the needs for adaptation in outpatient care for youth in highcomplexity families
Components of an Integrated Mental Health Service Delivery System • Effective psychiatric emergency services • Effective inpatient psychiatric services • Step-up and step-down intermediate level care • Outpatient services that can effectively address child acuity and family complexity
Youth at Higher Levels of Need in the Community • Movement to brief stabilization model of acute hospitalization • Much shorter lengths of stays • Youth discharged based on immediate risk • Whole system moving towards shorter intensive treatment periods (state hospitalization, residential treatment) • Move away from residential placement in Child Welfare and Juvenile Justice systems
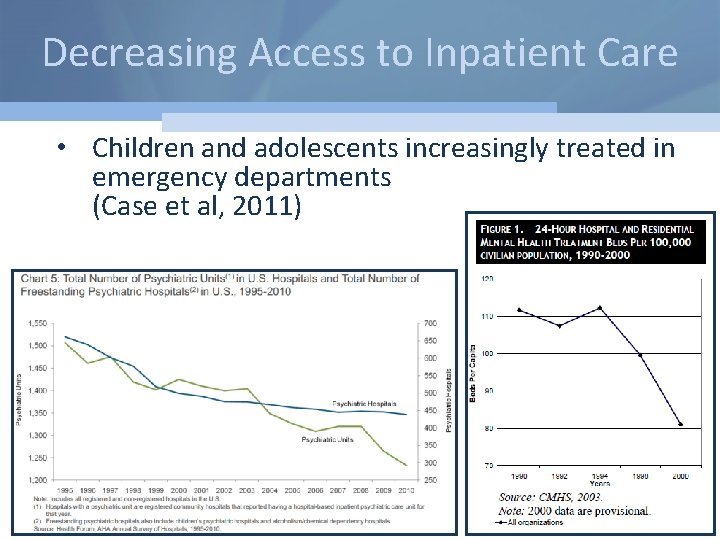
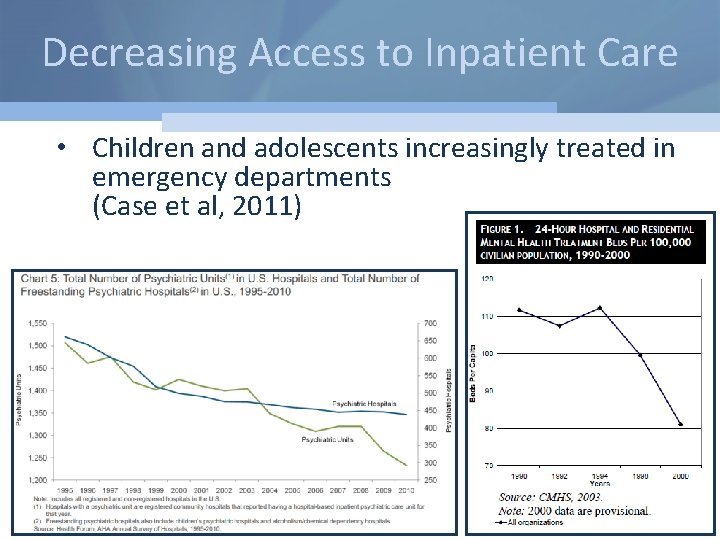
Decreasing Access to Inpatient Care • Children and adolescents increasingly treated in emergency departments (Case et al, 2011)
National Service Utilization by Children with Mental Health Conditions • Annual Report on Health Care for Children and Youth in the United States: National Estimates of Cost, Utilization and Expenditures for Children With Mental Health Conditions (Torio et al. , 2015) – Children ages 1 -17 – Sources: • AHRQ Healthcare Cost and Utilization Project National Inpatient Sample (2006 and 2011) • Nationwide Emergency Department Sample • Medical Expenditure Panel Survey (2006 and 2011)
National Findings: Inpatient Hospitalization • Increase in inpatient hospitalization between 2006 and 2011 – Significant increase for children ages 10 -14 and ages 5 -9 – Increase related to suicide and self-injury (103. 9%) • Mood disorders and ADHD most common principal diagnoses
National Findings: Emergency Department, Treat and Release • Significant increase treat and release visits between 2006 and 2011 (20. 9%) – Significant increase in every age group, especially children ages 1 -9 – Increase related to suicide and self-injury – Largest increase was for children in lowest income household • Mood disorders and ADHD most common principal diagnoses
Challenges to Effective Management of Psychiatric Emergencies • Increasing volume with little system adaptation • Youth treated in medical or adult psychiatry settings • ER evaluations limited to risk assessment only • Over-utilization of inpatient services
Characteristics of Emergency Mental Health Visits • More likely to be brought in by ambulance/police • Higher rates of admission and transfer • More likely to have repeat visits • Disproportionate increase among underinsured
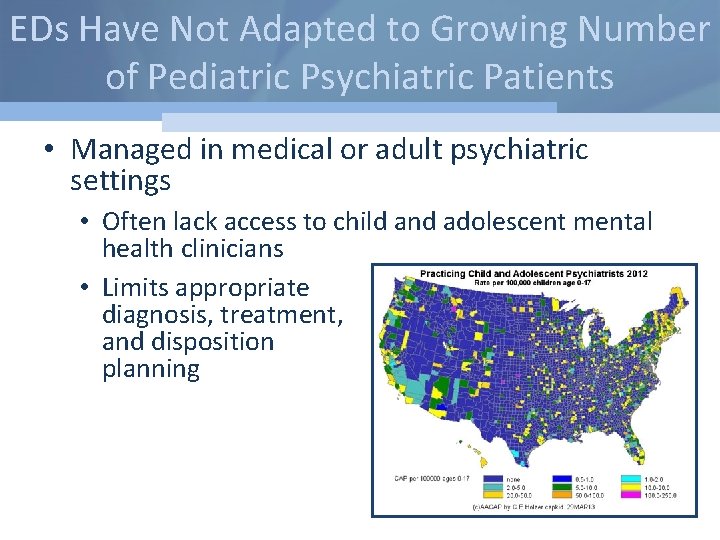
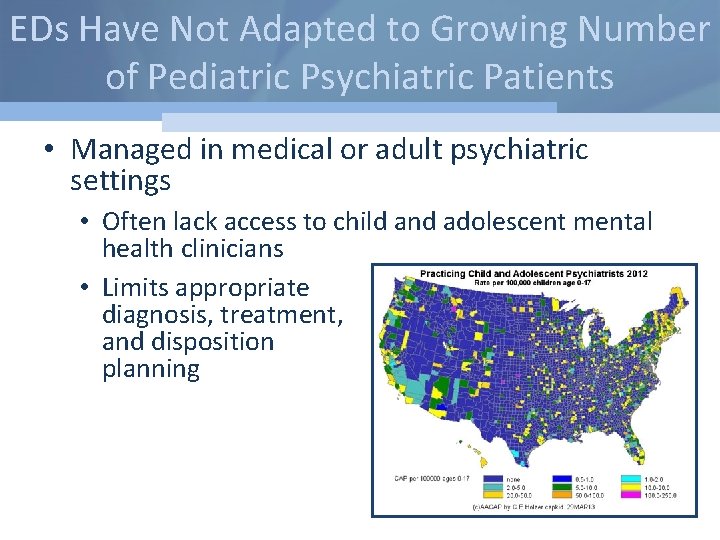
EDs Have Not Adapted to Growing Number of Pediatric Psychiatric Patients • Managed in medical or adult psychiatric settings • Often lack access to child and adolescent mental health clinicians • Limits appropriate diagnosis, treatment, and disposition planning
EDs Have Not Adapted to Growing Number of Pediatric Psychiatric Patients • Priority is triage patients out of emergency setting • When no inpatient beds available, children and adolescents “boarded” in ED for days or admitted to medical beds – Washington State recently ruled “boarding” in ED unconstitutional • Alienating and distressing experience for children and families
Pediatric Psychiatric Patients Have Significantly Longer ED Length of Stay • Psychiatric assessment requires more time than medical evaluation • Overutilization of inpatient care due to need for immediate treatment • Need for admission significantly increases length of stay – Admitted patients frequently require transfer because of lack of inpatient beds
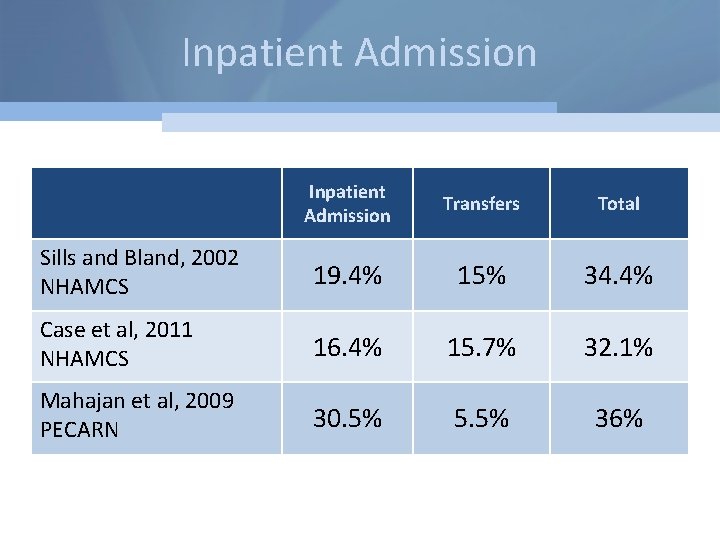
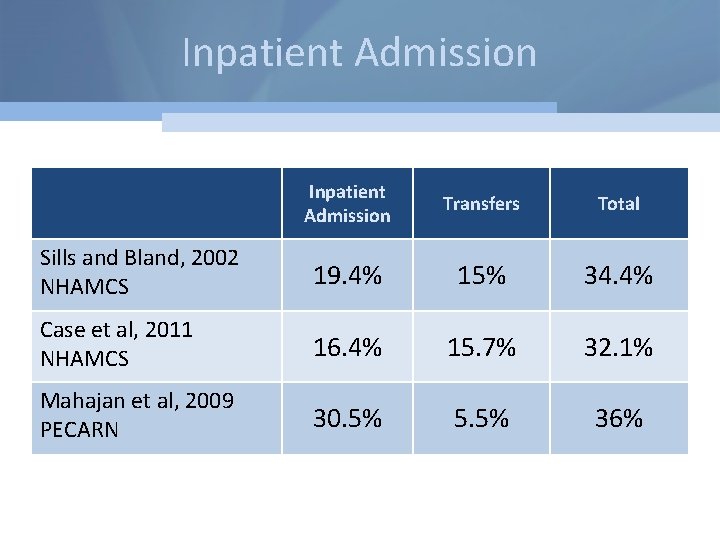
Inpatient Admission Transfers Total Sills and Bland, 2002 NHAMCS 19. 4% 15% 34. 4% Case et al, 2011 NHAMCS 16. 4% 15. 7% 32. 1% Mahajan et al, 2009 PECARN 30. 5% 5. 5% 36%
Underlying Reimbursement Issues • “ED Consultation” model associated with little to no revenue for psychiatry • Trainee-driven services in academic medical centers • Limited commercial insurance support for crisis intervention • Reliance on public or research dollars for program innovation
Enhanced Models of Pediatric Psychiatric Crisis Care • Community-Based – Home-based Crisis Intervention – Mobile Response Teams • Hospital-Based – Crisis Clinics • Emergency Department-Based – Dedicated Crisis Staff – Intervention and Follow-up • Blended Specialty Models
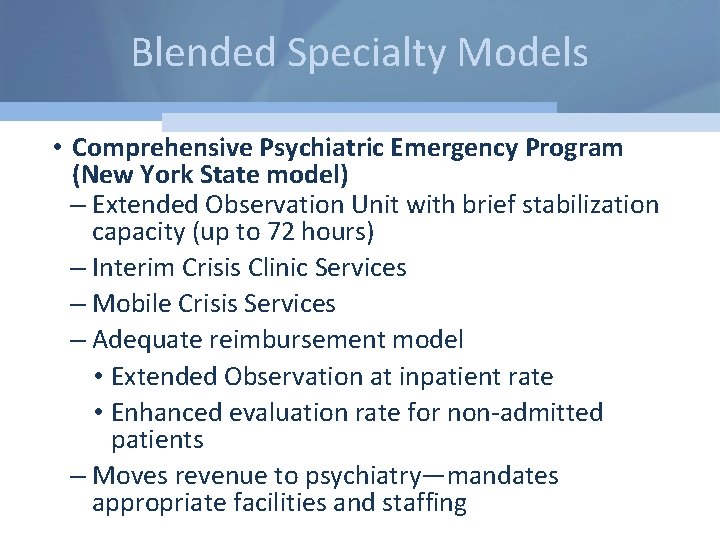
Blended Specialty Models • Comprehensive Psychiatric Emergency Program (New York State model) – Extended Observation Unit with brief stabilization capacity (up to 72 hours) – Interim Crisis Clinic Services – Mobile Crisis Services – Adequate reimbursement model • Extended Observation at inpatient rate • Enhanced evaluation rate for non-admitted patients – Moves revenue to psychiatry—mandates appropriate facilities and staffing
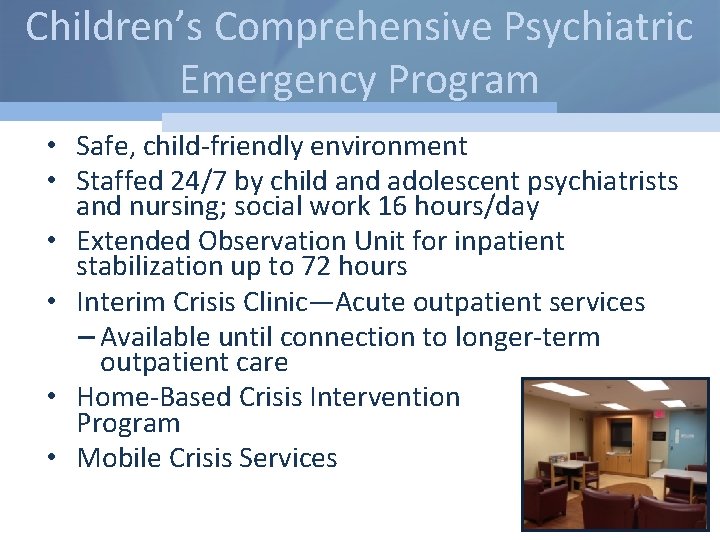
Children’s Comprehensive Psychiatric Emergency Program • Safe, child-friendly environment • Staffed 24/7 by child and adolescent psychiatrists and nursing; social work 16 hours/day • Extended Observation Unit for inpatient stabilization up to 72 hours • Interim Crisis Clinic—Acute outpatient services – Available until connection to longer-term outpatient care • Home-Based Crisis Intervention Program • Mobile Crisis Services
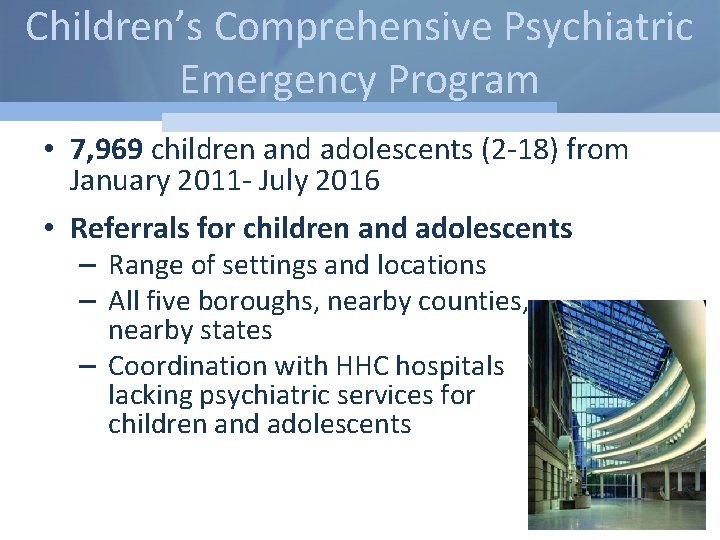
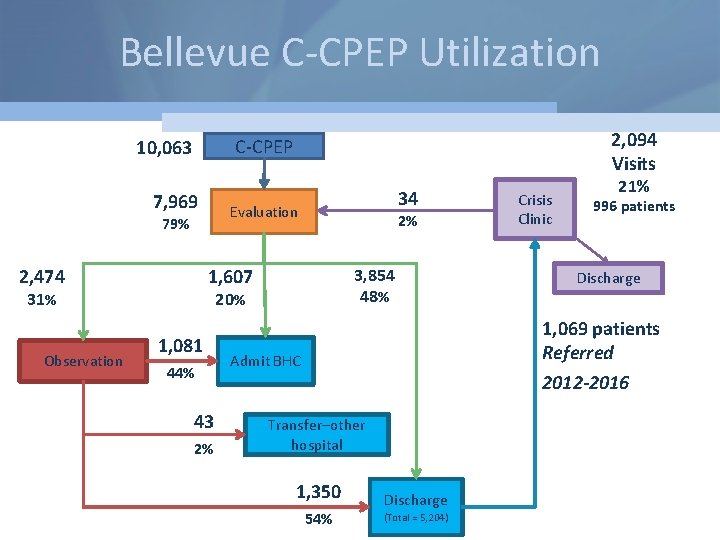
Children’s Comprehensive Psychiatric Emergency Program • 7, 969 children and adolescents (2 -18) from January 2011 - July 2016 • Referrals for children and adolescents – Range of settings and locations – All five boroughs, nearby counties, nearby states – Coordination with HHC hospitals lacking psychiatric services for children and adolescents
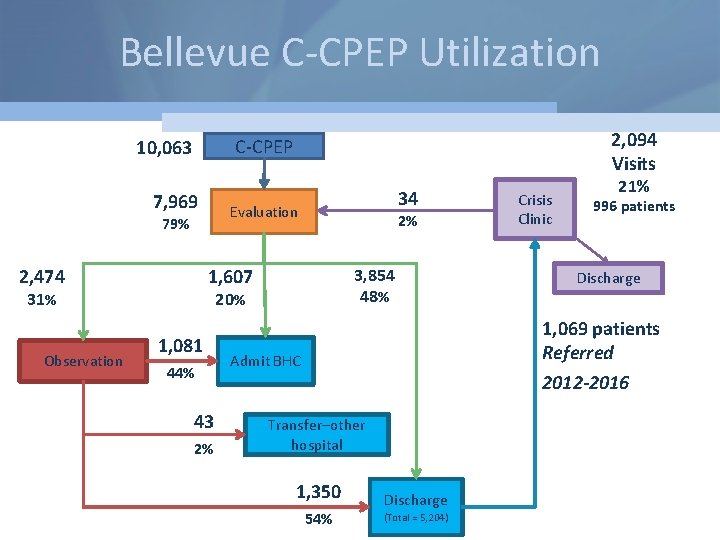
Bellevue C-CPEP Utilization 7, 969 2, 474 34 Evaluation 79% 2% 1, 607 31% Observation 2, 094 Visits C-CPEP 10, 063 3, 854 48% 20% 1, 081 44% 43 2% Crisis Clinic 21% 996 patients Discharge 1, 069 patients Referred 2012 -2016 Admit BHC Transfer–other hospital 1, 350 54% Discharge (Total = 5, 204)
Challenges to Effective Inpatient Treatment • Brief stabilization model of care – What can you really do in 4 -6 days - medicate and sedate and discharge • Diagnostic complexity associated with inappropriate treatment – Failure to identify trauma co-morbidities – Behavior guiding treatment not diagnosis • Lack of evidence-based acute programming models
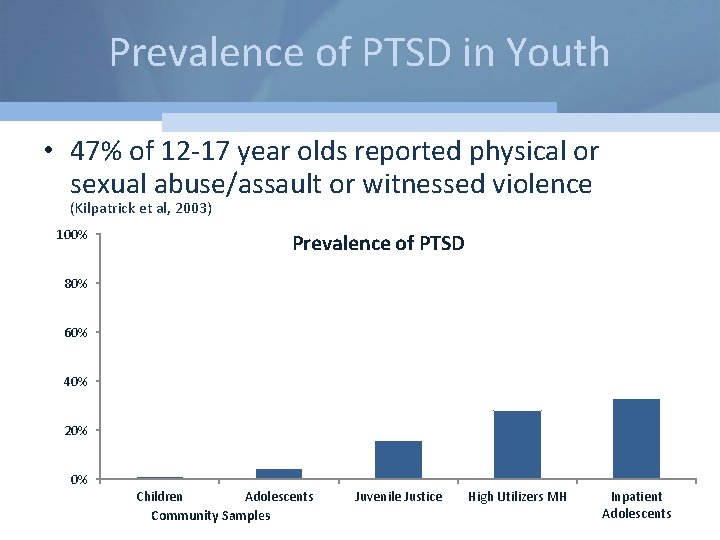
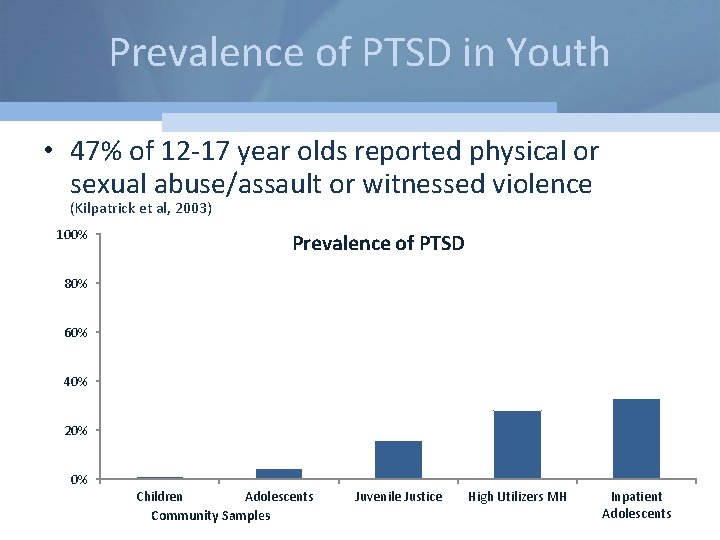
Prevalence of PTSD in Youth • 47% of 12 -17 year olds reported physical or sexual abuse/assault or witnessed violence (Kilpatrick et al, 2003) 100% Prevalence of PTSD 80% 60% 40% 20% 0% Children Adolescents Community Samples Juvenile Justice High Utilizers MH Inpatient Adolescents
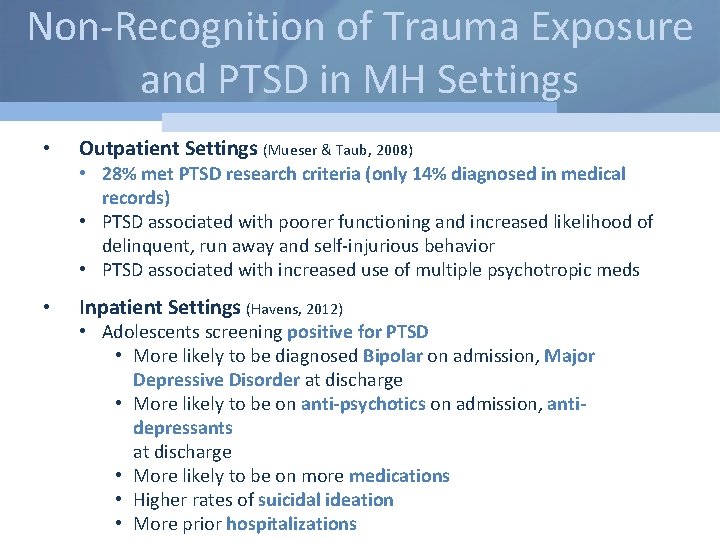
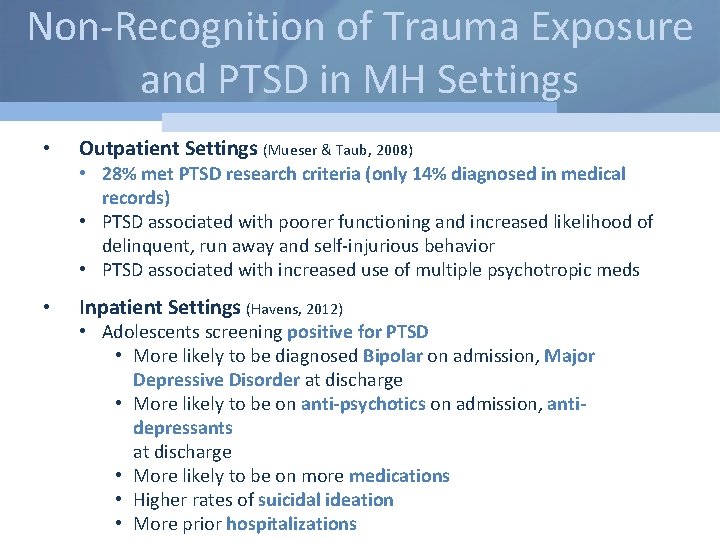
Non-Recognition of Trauma Exposure and PTSD in MH Settings • Outpatient Settings (Mueser & Taub, 2008) • 28% met PTSD research criteria (only 14% diagnosed in medical records) • PTSD associated with poorer functioning and increased likelihood of delinquent, run away and self-injurious behavior • PTSD associated with increased use of multiple psychotropic meds • Inpatient Settings (Havens, 2012) • Adolescents screening positive for PTSD • More likely to be diagnosed Bipolar on admission, Major Depressive Disorder at discharge • More likely to be on anti-psychotics on admission, antidepressants at discharge • More likely to be on more medications • Higher rates of suicidal ideation • More prior hospitalizations
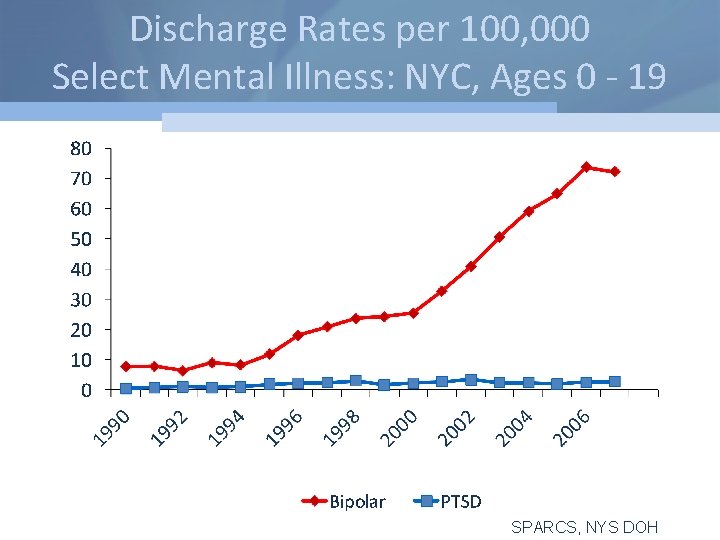
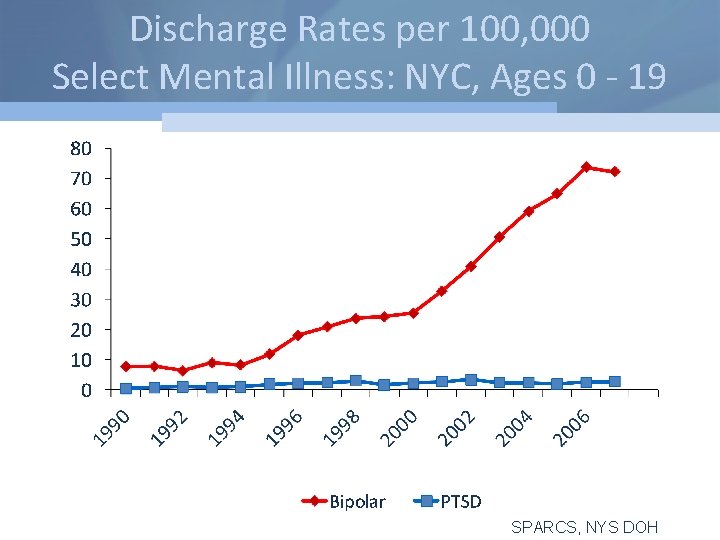
Discharge Rates per 100, 000 Select Mental Illness: NYC, Ages 0 - 19 SPARCS, NYS DOH
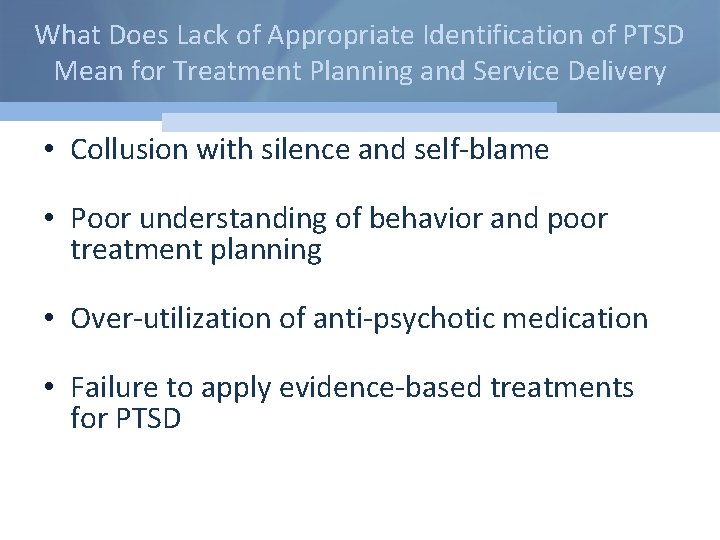
What Does Lack of Appropriate Identification of PTSD Mean for Treatment Planning and Service Delivery • Collusion with silence and self-blame • Poor understanding of behavior and poor treatment planning • Over-utilization of anti-psychotic medication • Failure to apply evidence-based treatments for PTSD
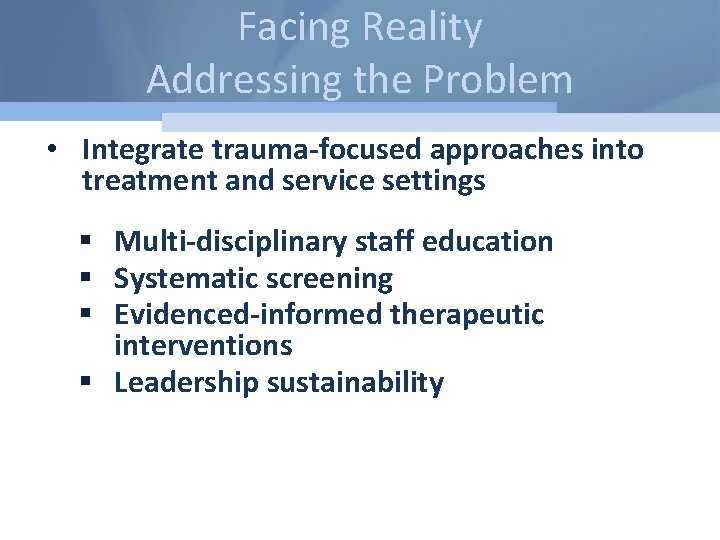
Facing Reality Addressing the Problem • Integrate trauma-focused approaches into treatment and service settings § Multi-disciplinary staff education § Systematic screening § Evidenced-informed therapeutic interventions § Leadership sustainability
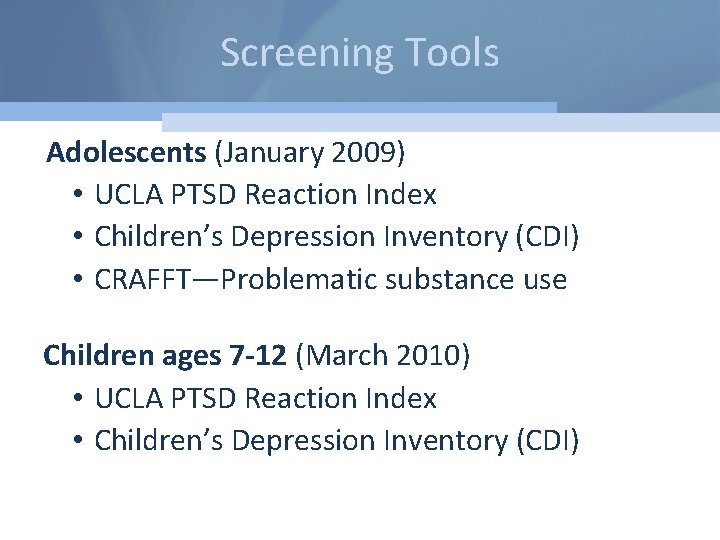
Screening Tools Adolescents (January 2009) • UCLA PTSD Reaction Index • Children’s Depression Inventory (CDI) • CRAFFT—Problematic substance use Children ages 7 -12 (March 2010) • UCLA PTSD Reaction Index • Children’s Depression Inventory (CDI)
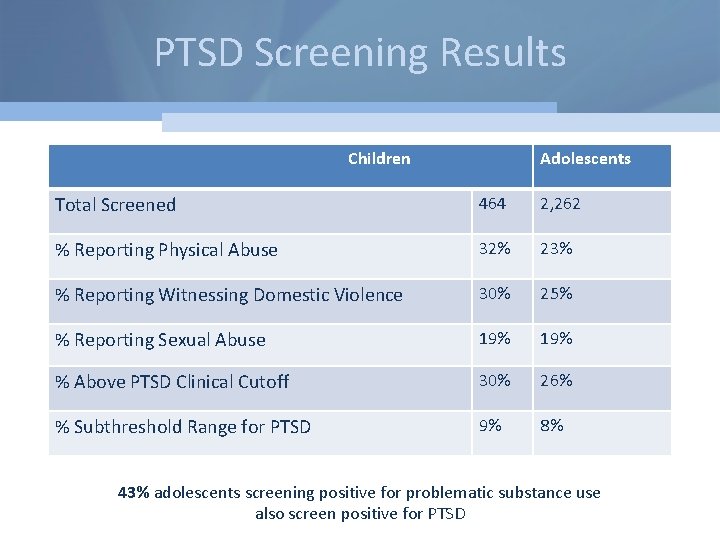
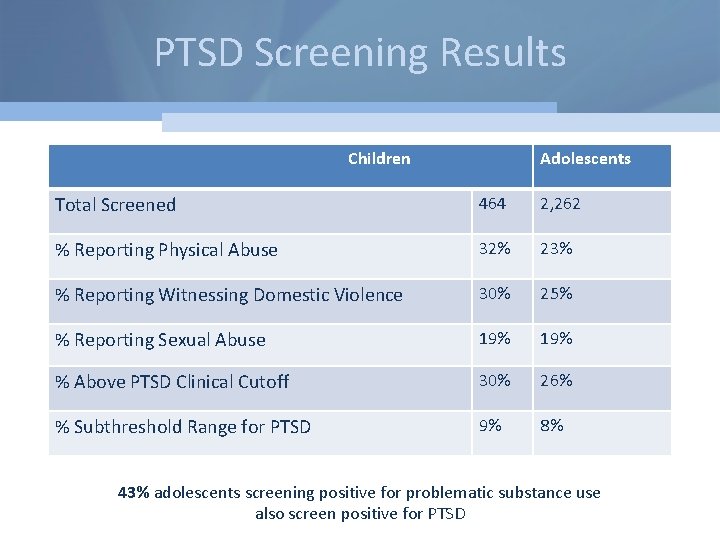
PTSD Screening Results Children Adolescents Total Screened 464 2, 262 % Reporting Physical Abuse 32% 23% % Reporting Witnessing Domestic Violence 30% 25% % Reporting Sexual Abuse 19% % Above PTSD Clinical Cutoff 30% 26% % Subthreshold Range for PTSD 9% 8% 43% adolescents screening positive for problematic substance use also screen positive for PTSD
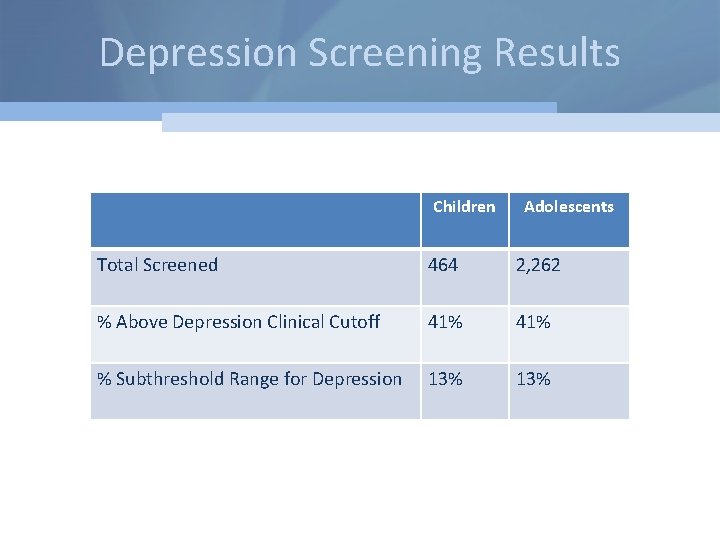
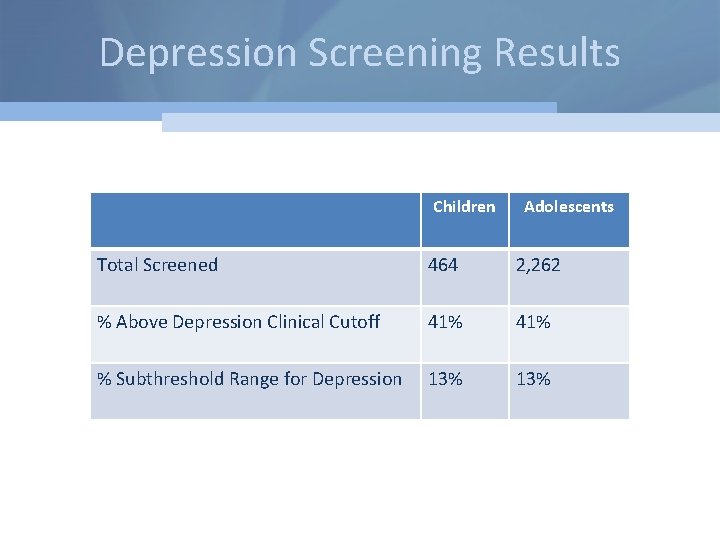
Depression Screening Results Children Adolescents Total Screened 464 2, 262 % Above Depression Clinical Cutoff 41% % Subthreshold Range for Depression 13%
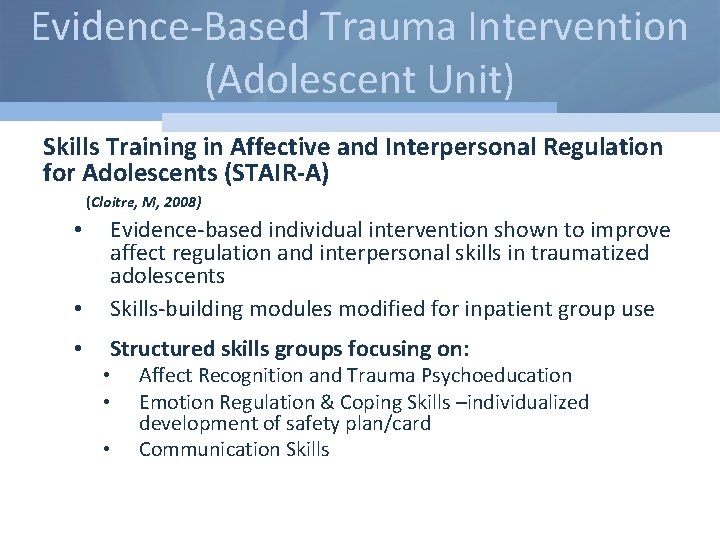
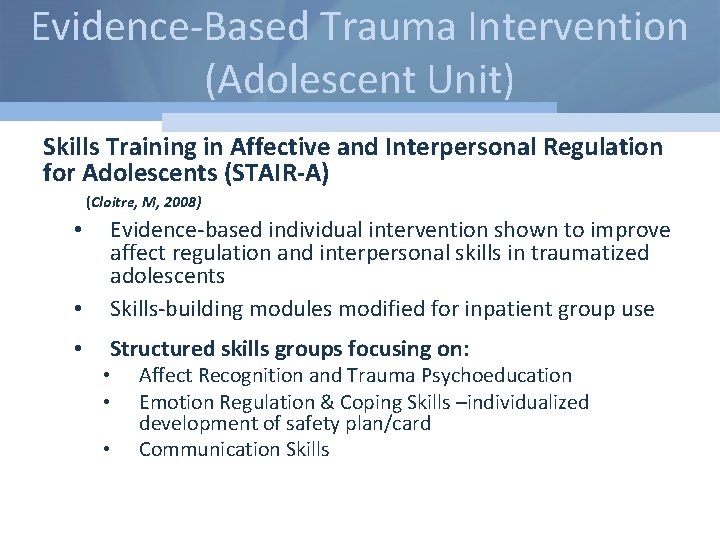
Evidence-Based Trauma Intervention (Adolescent Unit) Skills Training in Affective and Interpersonal Regulation for Adolescents (STAIR-A) (Cloitre, M, 2008) • Evidence-based individual intervention shown to improve affect regulation and interpersonal skills in traumatized adolescents Skills-building modules modified for inpatient group use • Structured skills groups focusing on: • • Affect Recognition and Trauma Psychoeducation Emotion Regulation & Coping Skills –individualized development of safety plan/card Communication Skills
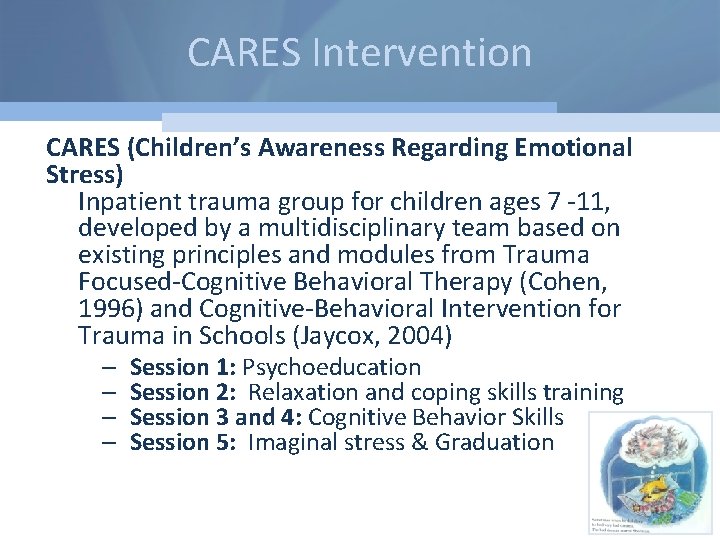
CARES Intervention CARES (Children’s Awareness Regarding Emotional Stress) Inpatient trauma group for children ages 7 -11, developed by a multidisciplinary team based on existing principles and modules from Trauma Focused-Cognitive Behavioral Therapy (Cohen, 1996) and Cognitive-Behavioral Intervention for Trauma in Schools (Jaycox, 2004) – – Session 1: Psychoeducation Session 2: Relaxation and coping skills training Session 3 and 4: Cognitive Behavior Skills Session 5: Imaginal stress & Graduation
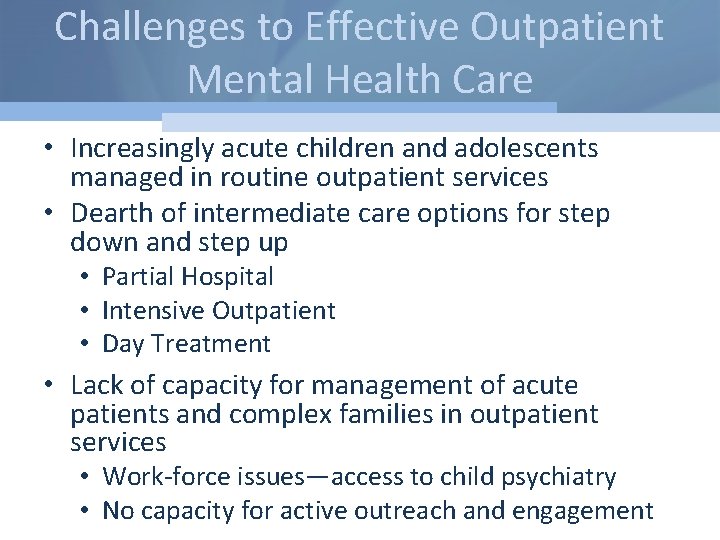
Challenges to Effective Outpatient Mental Health Care • Increasingly acute children and adolescents managed in routine outpatient services • Dearth of intermediate care options for step down and step up • Partial Hospital • Intensive Outpatient • Day Treatment • Lack of capacity for management of acute patients and complex families in outpatient services • Work-force issues—access to child psychiatry • No capacity for active outreach and engagement
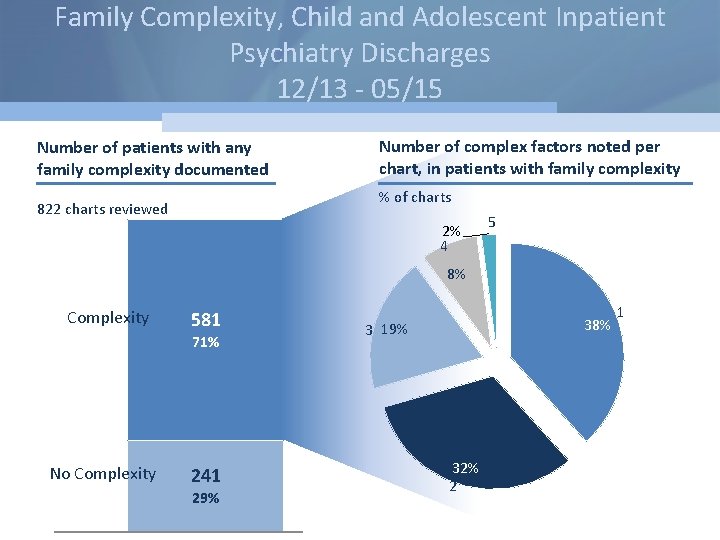
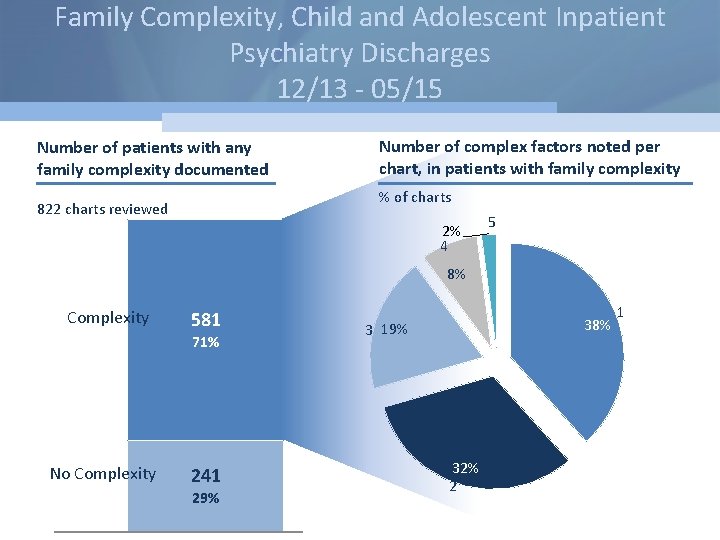
Family Complexity, Child and Adolescent Inpatient Psychiatry Discharges 12/13 - 05/15 Number of patients with any family complexity documented Number of complex factors noted per chart, in patients with family complexity % of charts 822 charts reviewed 2% 4 5 8% Complexity 581 71% No Complexity 241 29% 38% 3 19% 32% 2 263 79 1
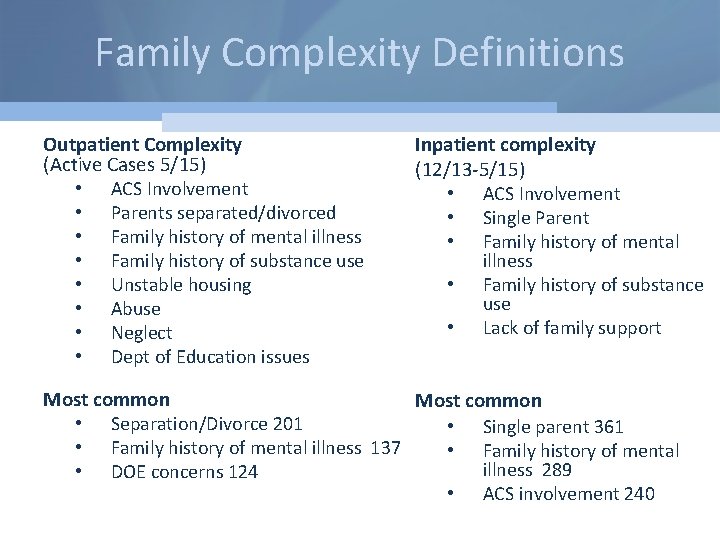
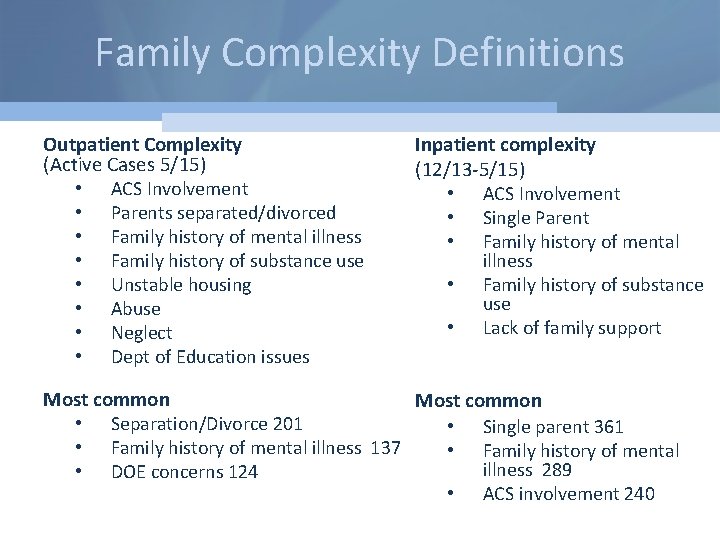
Family Complexity Definitions Outpatient Complexity (Active Cases 5/15) • ACS Involvement • Parents separated/divorced • Family history of mental illness • Family history of substance use • Unstable housing • Abuse • Neglect • Dept of Education issues Inpatient complexity (12/13 -5/15) • ACS Involvement • Single Parent • Family history of mental illness • Family history of substance use • Lack of family support Most common • Separation/Divorce 201 • Single parent 361 • Family history of mental illness 137 • Family history of mental illness 289 • DOE concerns 124 • ACS involvement 240
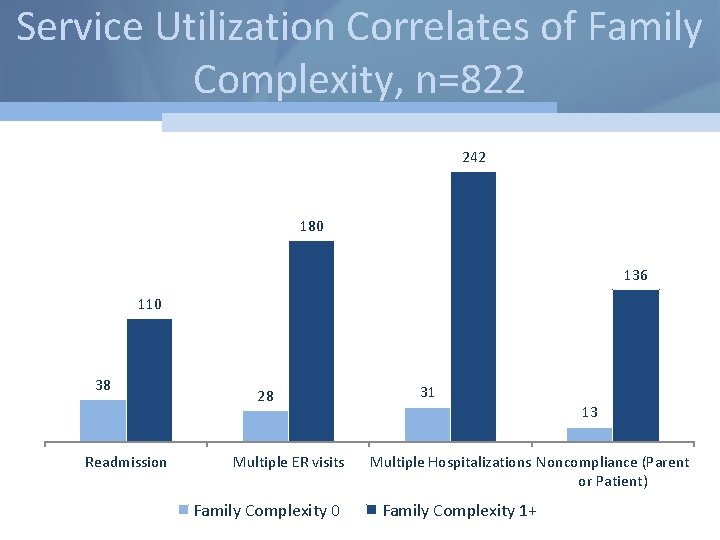
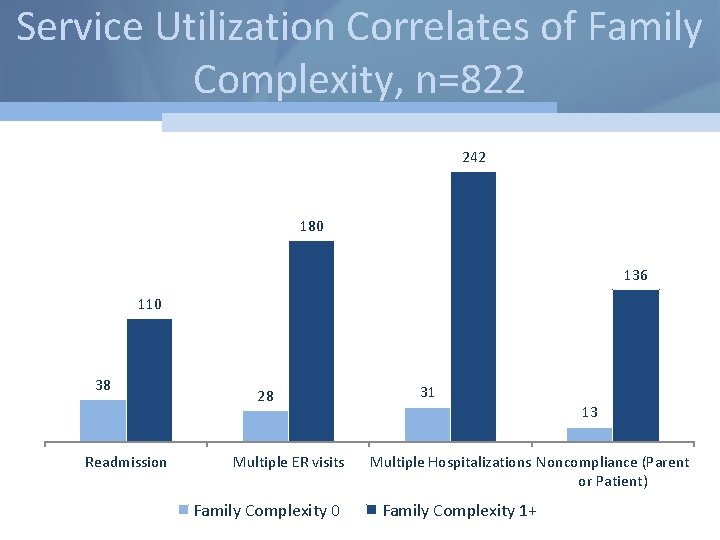
Service Utilization Correlates of Family Complexity, n=822 242 180 136 110 38 Readmission 28 Multiple ER visits Family Complexity 0 31 13 Multiple Hospitalizations Noncompliance (Parent or Patient) Family Complexity 1+
Adapting Clinic Models to Care for High Complexity Youth and Families • Outpatients clinics (and their payors) need to adapt to provide care to high complexity families – Evidenced Based Treatments (MST, FFT) – Family–Based Maintenance OPD treatment – Integrated Case Management
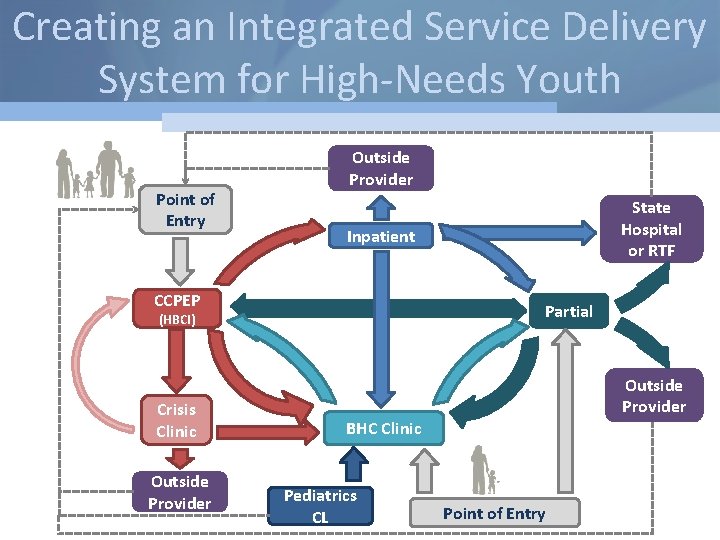
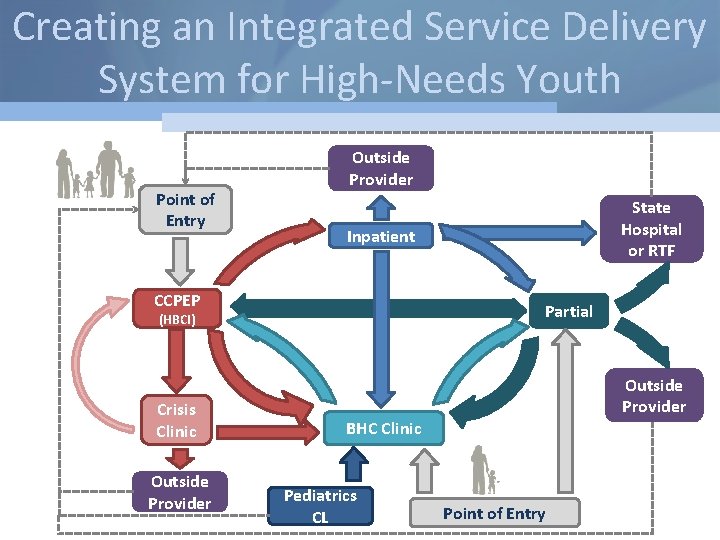
Creating an Integrated Service Delivery System for High-Needs Youth Point of Entry Outside Provider Inpatient CCPEP Partial (HBCI) Crisis Clinic Outside Provider State Hospital or RTF Outside Provider BHC Clinic Pediatrics CL Point of Entry
Conclusions • Every region needs a robust and comprehensive mental health care system for children and adolescents • Care systems and payors must incorporate effective care models for high complexity youth and families
 Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness Mental health jeopardy game
Mental health jeopardy game Social service delivery system
Social service delivery system Integrated delivery network definition
Integrated delivery network definition Objectives of delivery services
Objectives of delivery services Individual service plan
Individual service plan Federal public service workplace mental health strategy
Federal public service workplace mental health strategy Federal public service workplace mental health strategy
Federal public service workplace mental health strategy Integrated delivery system pros and cons
Integrated delivery system pros and cons Integrated care delivery system
Integrated care delivery system Ipd ppt
Ipd ppt First level service
First level service Integrated services delivery
Integrated services delivery Aia integrated project delivery
Aia integrated project delivery Website to access accenture delivery suite(ads)
Website to access accenture delivery suite(ads) Milkor
Milkor Vertical integration
Vertical integration Opacdr
Opacdr Integrated systems testing
Integrated systems testing Adams integrated systems
Adams integrated systems Damkt
Damkt Introduction to business process
Introduction to business process Mototrbo dispatch software
Mototrbo dispatch software Biov online kepri
Biov online kepri Ims integrated marketing systems
Ims integrated marketing systems Institute for software integrated systems
Institute for software integrated systems Whole systems integrated care
Whole systems integrated care Iaea gsr part 2
Iaea gsr part 2 What is integrated service management
What is integrated service management Integrated service digital network
Integrated service digital network Integrated service digital network
Integrated service digital network Apa itu isdn
Apa itu isdn Visn 20
Visn 20 Bury integrated pain service
Bury integrated pain service Bury integrated pain service
Bury integrated pain service Integrated service digital network
Integrated service digital network Integrated service management
Integrated service management Who traditional medicine strategy 2014–23
Who traditional medicine strategy 2014–23 Qi integrated health
Qi integrated health Types of health management information system
Types of health management information system