Integrated Services Programme Emerging Service Delivery Model Health




![ORGANISATION DESIGN CHALLENGES § ISA Model for Statutory/Non-statutory § Co-Leadership model [Operations/Clinical/Nursing] § How ORGANISATION DESIGN CHALLENGES § ISA Model for Statutory/Non-statutory § Co-Leadership model [Operations/Clinical/Nursing] § How](https://slidetodoc.com/presentation_image_h2/7b7f365cfe0a43c04cd1c6d340bae2f9/image-26.jpg)
- Slides: 28

Integrated Services Programme Emerging Service Delivery Model Health Management Institute Presentation
AGENDA § Case for change § Integrated Services Programme § Where to from here
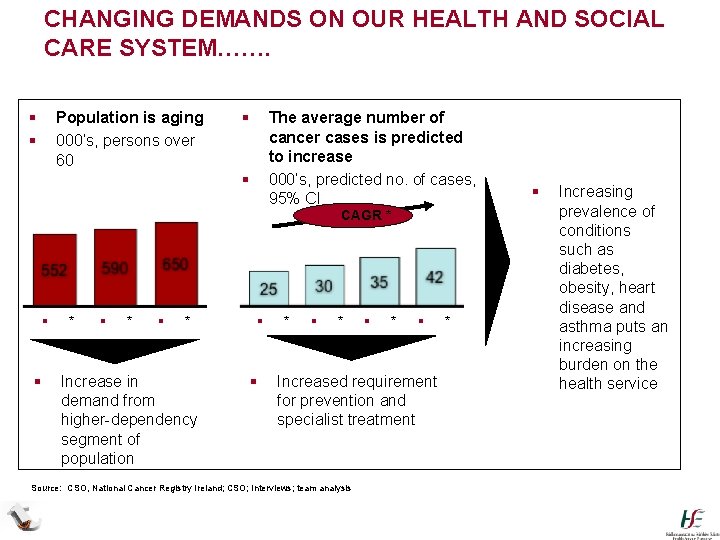
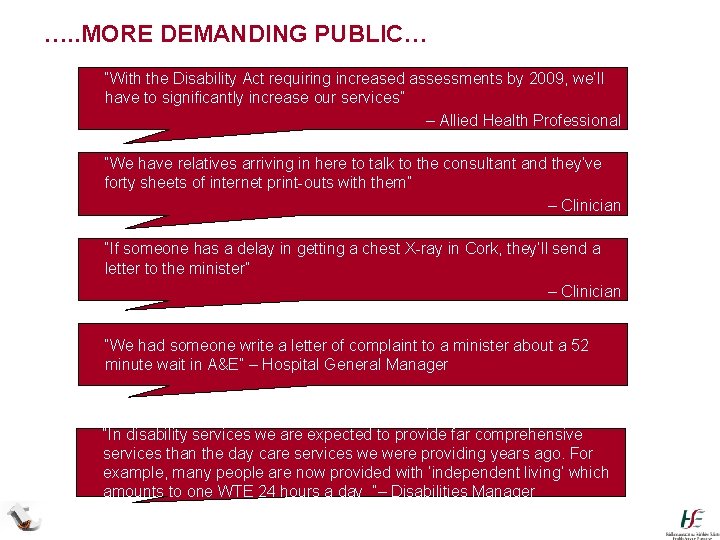
CHANGING DEMANDS ON OUR HEALTH AND SOCIAL CARE SYSTEM……. § § Population is aging 000’s, persons over 60 § The average number of cancer cases is predicted to increase 000’s, predicted no. of cases, 95% CI § § § * § * Increase in demand from higher-dependency segment of population § § * § CAGR * § * § Increased requirement for prevention and specialist treatment Source: CSO, National Cancer Registry Ireland; CSO; Interviews; team analysis * § Increasing prevalence of conditions such as diabetes, obesity, heart disease and asthma puts an increasing burden on the health service
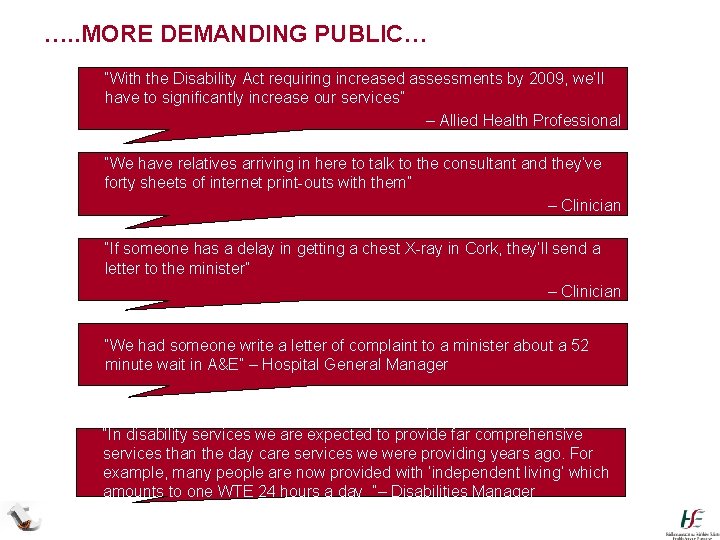
…. . MORE DEMANDING PUBLIC… § “With the Disability Act requiring increased assessments by 2009, we’ll have to significantly increase our services” § – Allied Health Professional § “We have relatives arriving in here to talk to the consultant and they’ve forty sheets of internet print-outs with them” § – Clinician § “If someone has a delay in getting a chest X-ray in Cork, they’ll send a letter to the minister” § – Clinician § “We had someone write a letter of complaint to a minister about a 52 minute wait in A&E” – Hospital General Manager § “In disability services we are expected to provide far comprehensive services than the day care services we were providing years ago. For example, many people are now provided with ‘independent living’ which amounts to one WTE 24 hours a day ”– Disabilities Manager
…IN A DIFFICULT INTERNAL AND EXTERNAL ENVIRONMENT § Serious economic challenges for country and for our services § Need to ensure our services are safe § Ensuring services are sustainable § Focusing on our patients rather than organisations § Continuous change § Dealing with increasingly complex population health needs § Recognised need to bring decision making closer to the front line and to empower the people delivering services on the ground

CASE FOR CHANGE HSE Corporate Plan 2008 -2011 sets out a clear vision for implementing an Integrated health and social model for Ireland. Why are we making these changes? § § § To drive and support safe, quality care for patients and clients. To bring decision making close to where services are delivered. To allow clinicians to shape and assure the services they work in. To get the best health outcomes for the money spent. To plan and organise around what we know people need and what we know works to give the best results. § To organise to meet increasingly complex patient and client needs § To remove barriers to integrated care.
WHAT SHOULD THIS MEAN FOR PATIENTS & CLIENTS § Services will be more accessible locally, centred around the patient, rather than centred around an institution § Shift towards prevention and better self care rather than a focus on acute care and treatment § Improved patient outcomes § Right balance between inpatient, day case and community based care § More efficient use of resources and more transparent accountability * As per the HSE Corporate Plan 2008
WHAT SHOULD THIS MEAN FOR STAFF § § § § Work across boundaries Extended hours New roles will develop Flexibility as needs emerge Multidisciplinary team working Manager/Clinician collaboration Technology

Integrated Services Programme
INTEGRATED SERVICES PROGRAMME § Established end 2008 following Mc. Kinsey review § Initial focus was to define service delivery model and get agreement on direction § Purpose is to re-organise services towards an integrated model of care § Building on existing strategies/direction
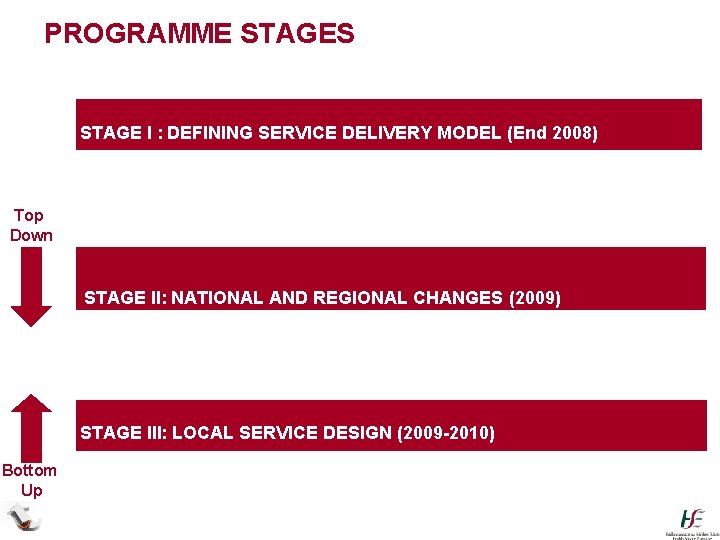
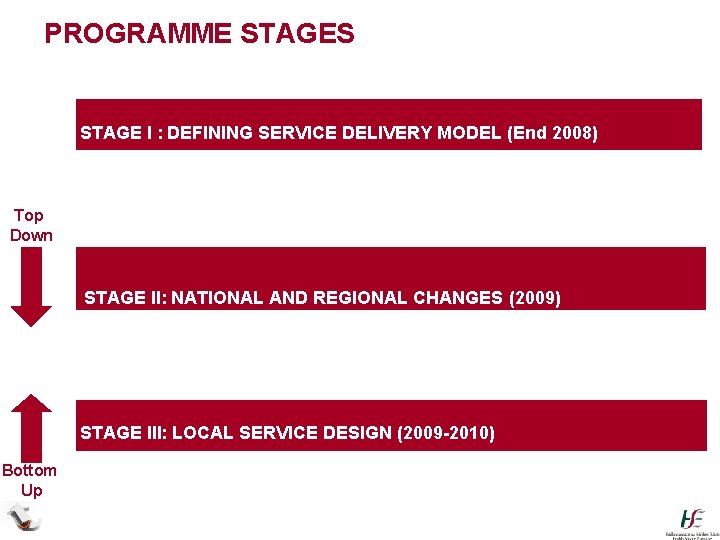
PROGRAMME STAGES STAGE I : DEFINING SERVICE DELIVERY MODEL (End 2008) Top Down STAGE II: NATIONAL AND REGIONAL CHANGES (2009) STAGE III: LOCAL SERVICE DESIGN (2009 -2010) Bottom Up
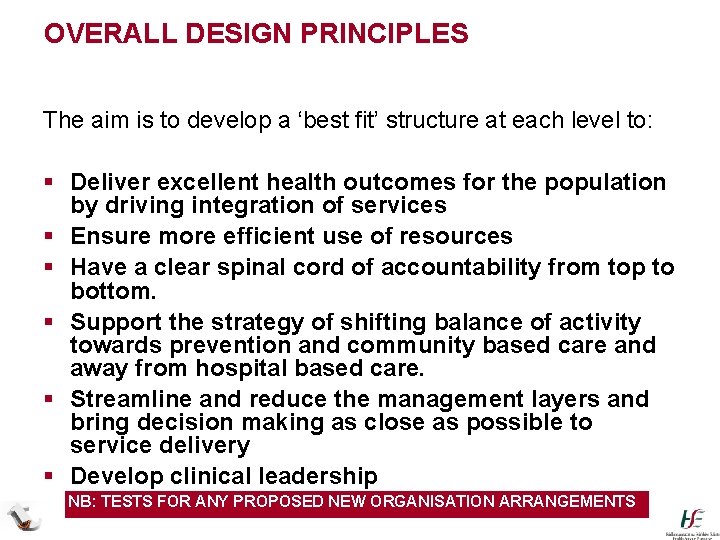
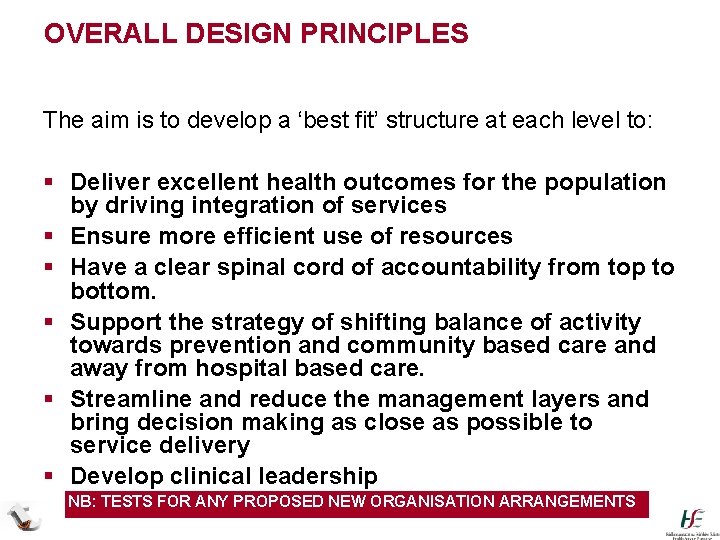
OVERALL DESIGN PRINCIPLES The aim is to develop a ‘best fit’ structure at each level to: § Deliver excellent health outcomes for the population by driving integration of services § Ensure more efficient use of resources § Have a clear spinal cord of accountability from top to bottom. § Support the strategy of shifting balance of activity towards prevention and community based care and away from hospital based care. § Streamline and reduce the management layers and bring decision making as close as possible to service delivery § Develop clinical leadership NB: TESTS FOR ANY PROPOSED NEW ORGANISATION ARRANGEMENTS
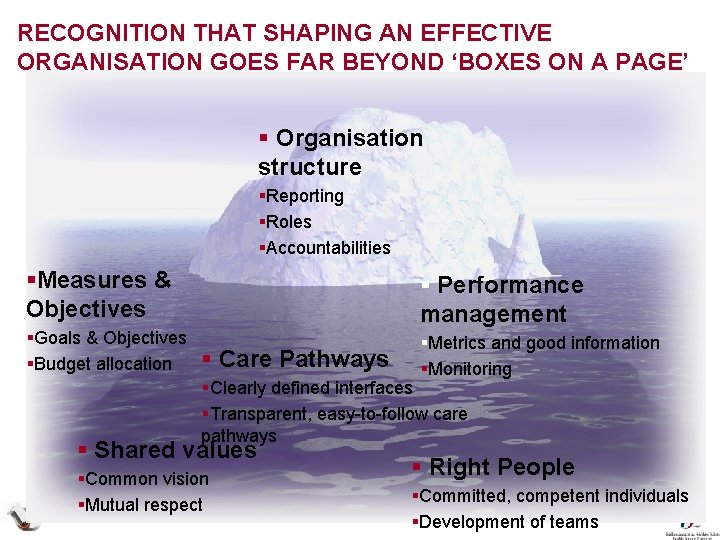
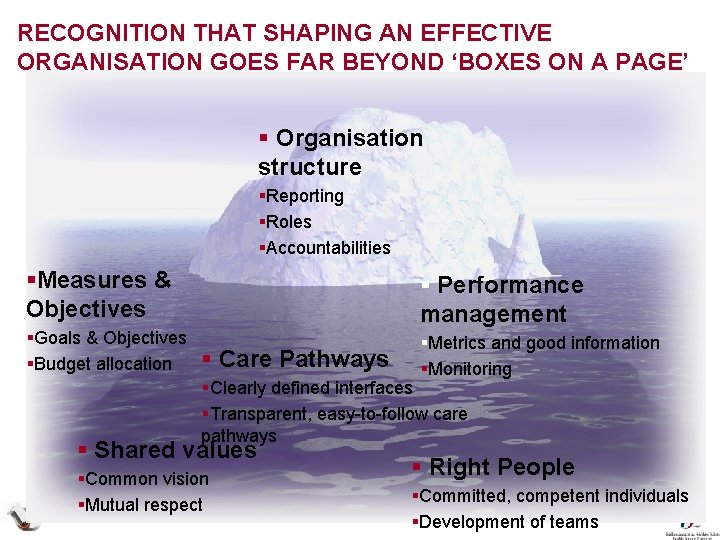
RECOGNITION THAT SHAPING AN EFFECTIVE ORGANISATION GOES FAR BEYOND ‘BOXES ON A PAGE’ § Organisation structure §Reporting §Roles §Accountabilities §Measures & Objectives § Performance management §Goals & Objectives §Budget allocation §Metrics and good information §Monitoring § Care Pathways §Clearly defined interfaces §Transparent, easy-to-follow care pathways § Shared values §Common vision §Mutual respect § Right People §Committed, competent individuals §Development of teams
Service Delivery Model
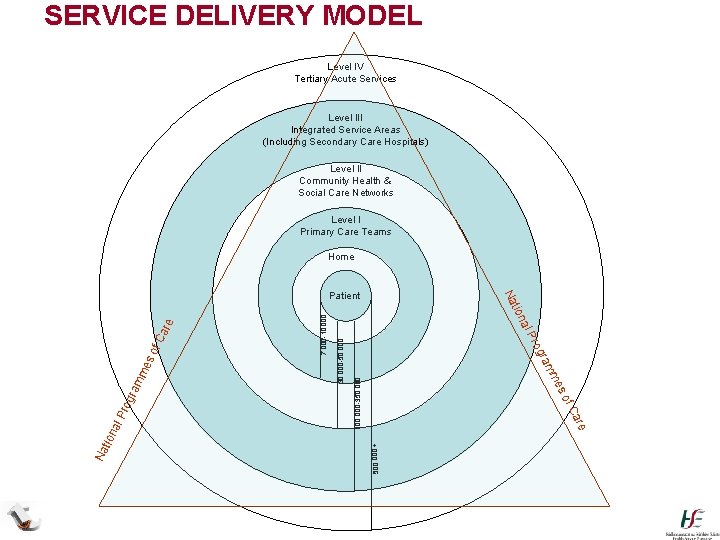
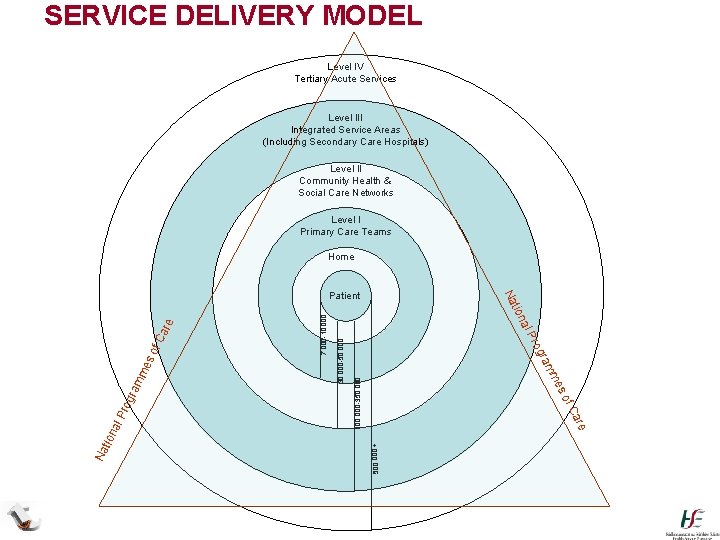
SERVICE DELIVERY MODEL Level IV Tertiary Acute Services Level III Integrated Service Areas (Including Secondary Care Hospitals) Level II Community Health & Social Care Networks Level I Primary Care Teams Home 100, 000 -350, 000 500, 000 + 30, 000 -50, 000 7, 000 -10, 000 f. C are so me ram rog al P are f. C so tion me ram rog Na l. P na tio Na Patient
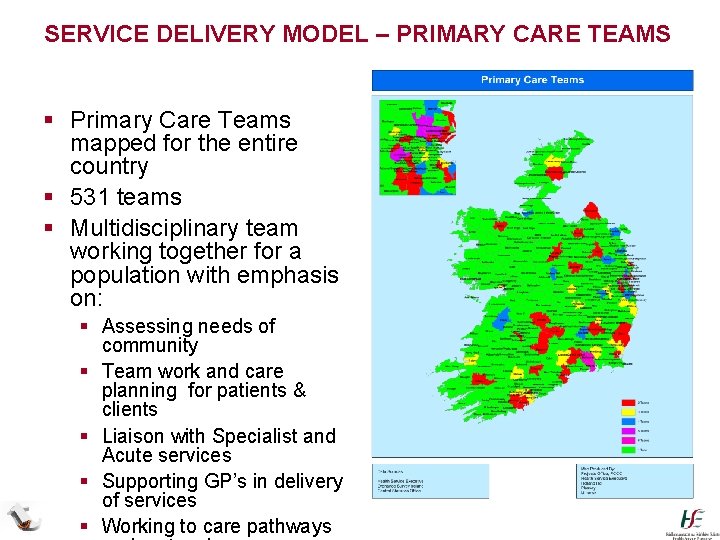
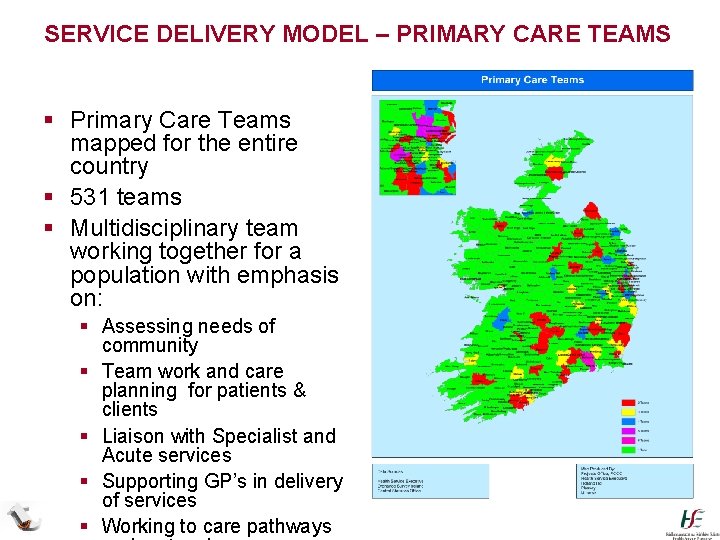
SERVICE DELIVERY MODEL – PRIMARY CARE TEAMS § Primary Care Teams mapped for the entire country § 531 teams § Multidisciplinary team working together for a population with emphasis on: § Assessing needs of community § Team work and care planning for patients & clients § Liaison with Specialist and Acute services § Supporting GP’s in delivery of services § Working to care pathways
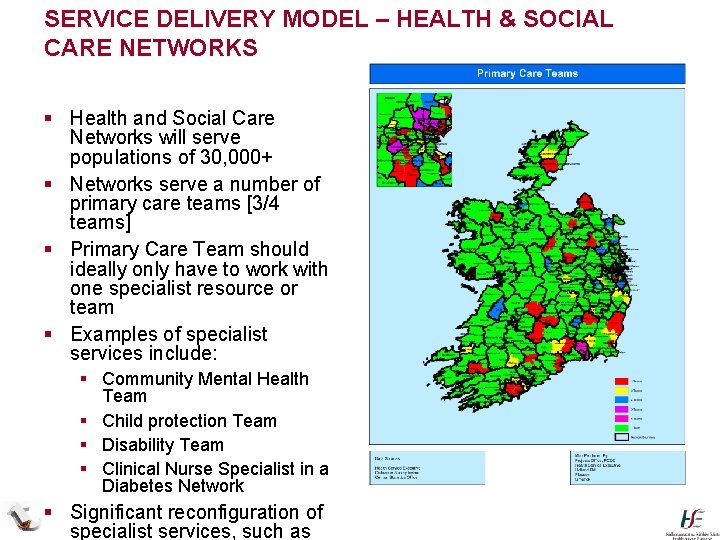
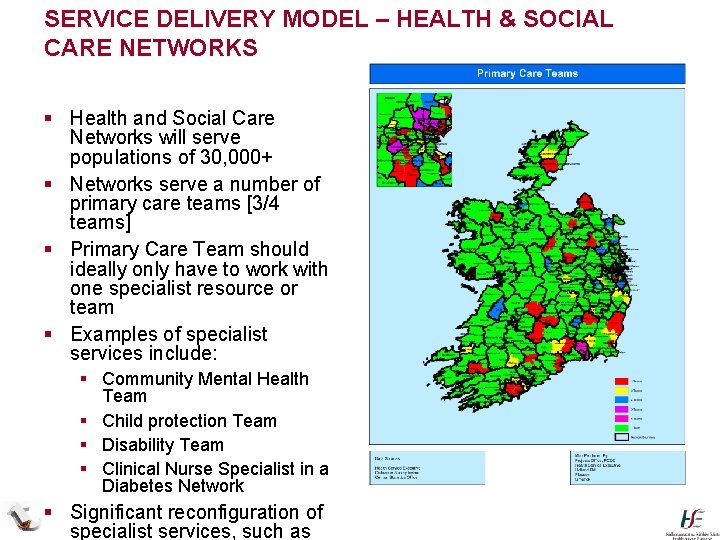
SERVICE DELIVERY MODEL – HEALTH & SOCIAL CARE NETWORKS § Health and Social Care Networks will serve populations of 30, 000+ § Networks serve a number of primary care teams [3/4 teams] § Primary Care Team should ideally only have to work with one specialist resource or team § Examples of specialist services include: § Community Mental Health Team § Child protection Team § Disability Team § Clinical Nurse Specialist in a Diabetes Network § Significant reconfiguration of specialist services, such as
SERVICE DELIVERY MODEL – ISA/SPECIALIST SERVICES § Specialised Community Care services (e. g. Mental Health) § Agreed strategy is maximum delivery to these groups through Primary Care with some specialist services delivered at Health and Social Care network and ISA level § National AND Care Groups responsible for setting direction and detailed model § Specialised Acute Care Services § Acute care services provided for larger populations § Programmes of Care and Hospital Reconfiguration programmes will define what is delivered where
INTEGRATED SERVICE AREAS § Policy objective is to transfer non-complex acute service to local hospitals and/or PCTs § To support concept PCTs and related secondary care Acute hospitals should have co-terminous populations § Geographical entity to be known as an Integrated Service Area (ISA); will contain hospital or no. of hospitals that provide for the secondary care needs for that population § Also considers other factors such as ambulance catchment areas, local authority boundaries and local community considerations
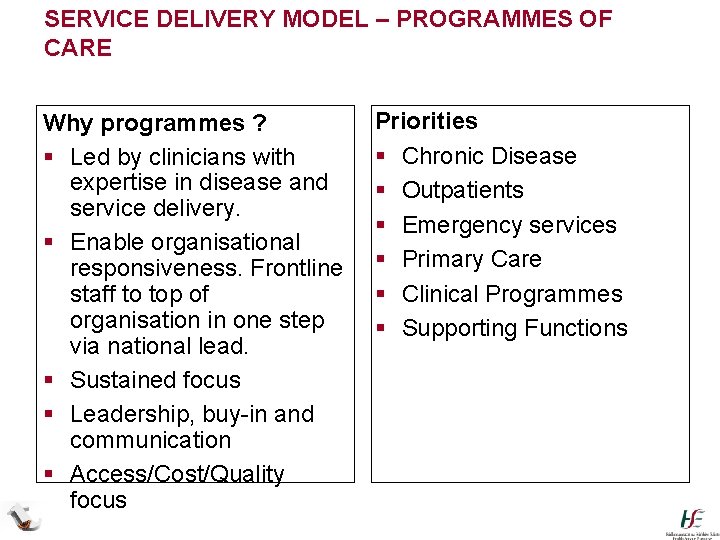
SERVICE DELIVERY MODEL – PROGRAMMES OF CARE Why programmes ? § Led by clinicians with expertise in disease and service delivery. § Enable organisational responsiveness. Frontline staff to top of organisation in one step via national lead. § Sustained focus § Leadership, buy-in and communication § Access/Cost/Quality focus Priorities § Chronic Disease § Outpatients § Emergency services § Primary Care § Clinical Programmes § Supporting Functions

Organisation Structure
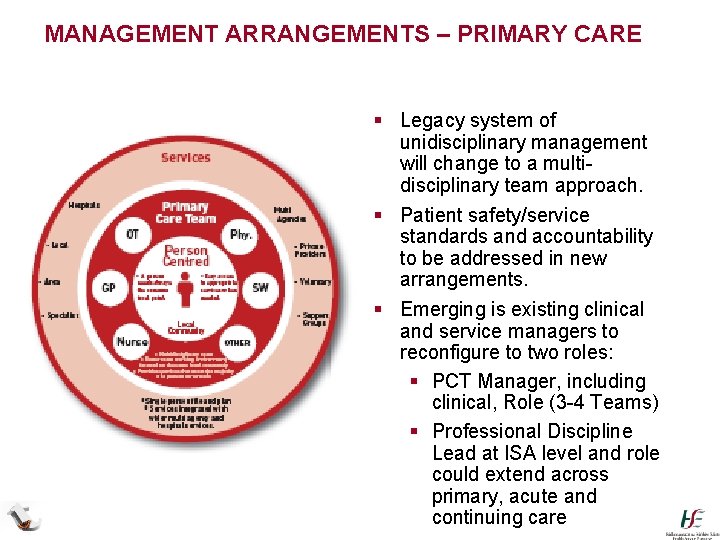
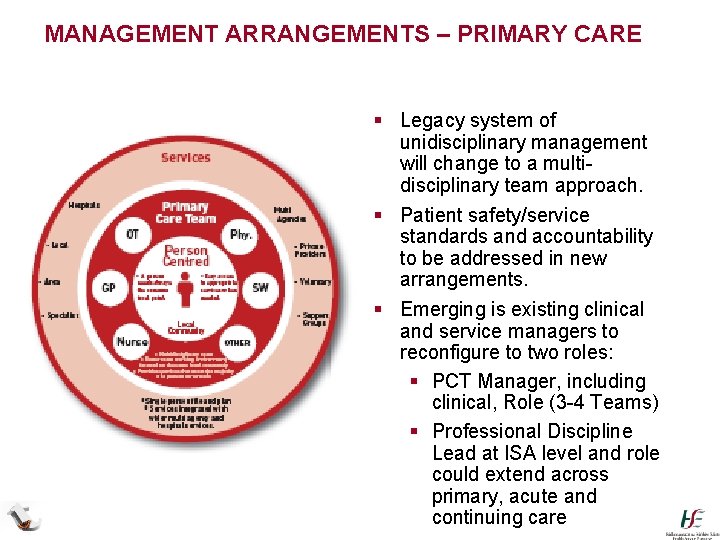
MANAGEMENT ARRANGEMENTS – PRIMARY CARE § Legacy system of unidisciplinary management will change to a multidisciplinary team approach. § Patient safety/service standards and accountability to be addressed in new arrangements. § Emerging is existing clinical and service managers to reconfigure to two roles: § PCT Manager, including clinical, Role (3 -4 Teams) § Professional Discipline Lead at ISA level and role could extend across primary, acute and continuing care
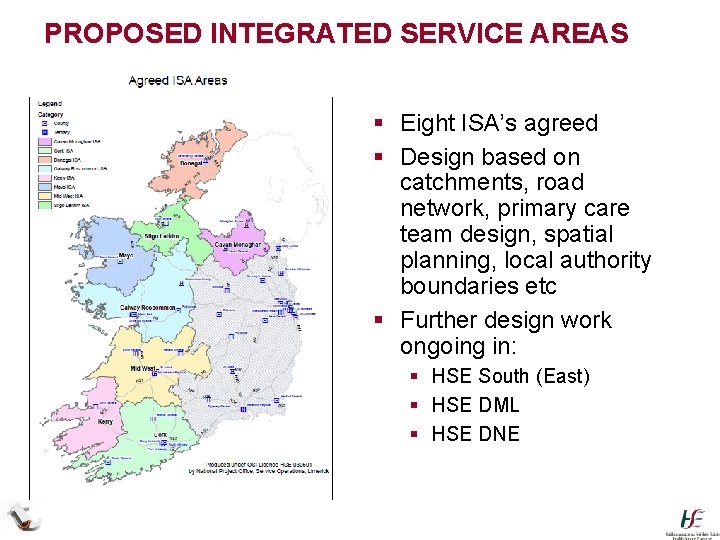
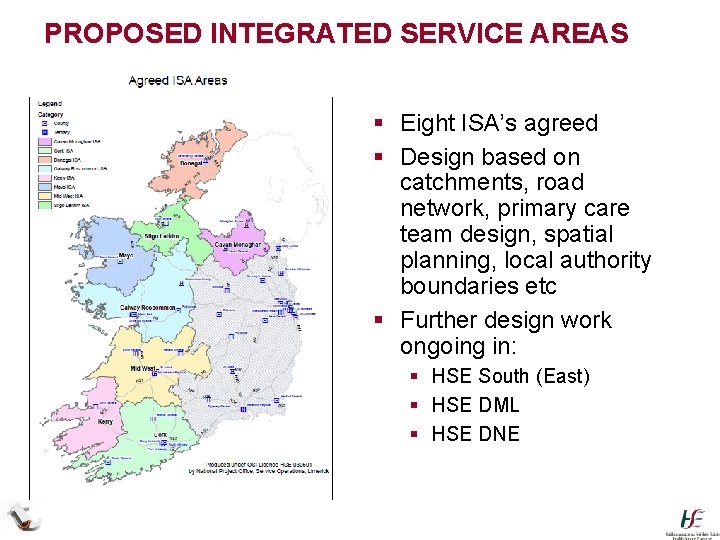
PROPOSED INTEGRATED SERVICE AREAS /Leitrim § Eight ISA’s agreed § Design based on catchments, road network, primary care team design, spatial planning, local authority boundaries etc § Further design work ongoing in: § HSE South (East) § HSE DML § HSE DNE
PROGRESS MADE § Stage I – Corporate restructuring complete § Stage II – Regions established § Regional Directors in place § Further work required to implement § Stage III § ISA catchments being scoped § Service Delivery Model defined and discussions commenced with trade unions – paused § Programmes of Care defined and teams being established § Performance Management Process being developed
![ORGANISATION DESIGN CHALLENGES ISA Model for StatutoryNonstatutory CoLeadership model OperationsClinicalNursing How ORGANISATION DESIGN CHALLENGES § ISA Model for Statutory/Non-statutory § Co-Leadership model [Operations/Clinical/Nursing] § How](https://slidetodoc.com/presentation_image_h2/7b7f365cfe0a43c04cd1c6d340bae2f9/image-26.jpg)
ORGANISATION DESIGN CHALLENGES § ISA Model for Statutory/Non-statutory § Co-Leadership model [Operations/Clinical/Nursing] § How should Clinical Director role develop? § Currently one per hospital § Agreement to move to Clinical Directorates across hospitals – eg Medicine, Women and Children, Peri. Operative § Requirement for a similar role in Primary Care? § How do we ensure quality and safety of non medical services, such as Children and Family services ? § Role for Nursing and AHPs across areas ? § Management and Professional development
NEXT STEPS § ISA Design & Rollout § Complete design for remaining Integrated Service Areas § Implement interim arrangements in HSE West § Develop model for areas with large non-statutory providers § Approval of ISA Management Team structure § Service Delivery Model § Develop and rollout Clinical Directors § Implement primary care model § Implement changes identified in other services such as Childcare and Mental Health § Develop Care Pathways § Develop Performance Management System Change Process
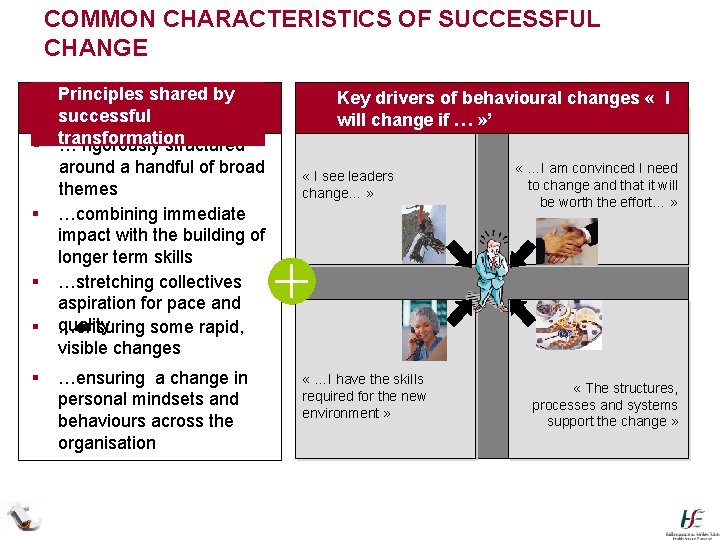
COMMON CHARACTERISTICS OF SUCCESSFUL CHANGE § Principles shared by successful § transformation … rigorously structured around a handful of broad themes § …combining immediate impact with the building of longer term skills § …stretching collectives aspiration for pace and § quality …ensuring some rapid, visible changes § …ensuring a change in personal mindsets and behaviours across the organisation § Key drivers of behavioural changes « I will change if … » ’ « I see leaders change… » « …I have the skills required for the new environment » « …I am convinced I need to change and that it will be worth the effort… » « The structures, processes and systems support the change »