Condition that persists over time usually 3 months









- Slides: 43

Condition that persists over time, usually > 3 months, or one in which recovery is slow � Physical, psychosocial, or cognitive impairment that places limitations on child � Child and family rely on assistance from other caregivers � Congenital defect or problem that occurs during fetal development (e. g. , sepsis at birth, prematurity, or intraventricular hemorrhage) � Develops from genetic predisposition � Acquired sometime during child’s life as result of an illness, accident, or injury �
• • Brain: cerebral palsy or seizure disorder Heart: congenital or acquired heart disease Lungs: cystic fibrosis, bronchopulmonary dysplasia, asthma Muscular or skeletal: muscular dystrophy, skeletal malformations Abdominal organs: kidneys (renal failure), liver (cirrhosis), intestine (short bowel syndrome) Skin: eczema, dermatitis, or conditions such as Lyme disease (can cause chronic arthritis) Psychological: depression, bipolar disorder, autism Cognitive: Down syndrome, developmental and learning disabilities
• • Technology dependent indicates reliance on some type of medical device to compensate for loss of normal use of vital body function Main goal of Technology-Related Assistance for Individuals with Disabilities Act amendments is to examine barriers for children and adults who need to access and obtain assistive technology Assistive technology can enable individuals to participate in and contribute more fully to family, school, and community activities Assistive technology devices are used to increase, maintain, or improve functional capabilities of individuals with disabilities
� Creates threat of unknown, loss of control; can have long -term effects � Frequent visits to the hospital or clinic may be needed � Overwhelming lack of control � Social, financial, physical, and psychological strain � Child has to learn to cope with the condition
� Impact: � Impacts natural formation of the parent–child bonding process � Necessitates painful procedures; subsequent alteration in feeding and sleep–wake patterns can impact infant’s long-term overall condition � Disrupts normal growth and developmental milestones; long-tem impact � Nursing � Rock, care: hold, comfort, and use soothing voice � Provide visual and auditory stimulation � Implement group nursing care measures; protect nap time � Maintain crib as a safe place � Encourage parents to hold infant � Siblings can visit and participate in simple care-taking measures
� Impact: � Unable to accomplish autonomy � Pain, anxiety, and separation from parents � Sensitive to bodily harm � Hinders gross and fine motor development � Stress and regression � Nursing care: � Maintain bond between parents and child � Promote realistic developmental skills; do not react negatively to regression � Praise child for attempts at self-care � Instruct parents on realistic methods of discipline � Manage pain � Maintain home routine as much as possible � Allow child to express feelings through play
� Impact: � Child feels “punished” for real or imagined wrongdoing � Reacts aggressively; regresses; withdraws from others � May have difficulty sleeping (fear of going to sleep) � Nursing � Provide care: with opportunity to express fears and frustrations � Tell stories and read books � Allow preschooler to use play � Ask child-life specialist for assistance � Maintain normal home schedule as possible; enforce consistent limits � Reassure child that nothing he or she did caused illness � Be honest when explaining and preparing for the child for procedures � Understand child’s limited concept of time
• Impact: Altered autonomy and peer relationships; interrupts independence – Child refuses to comply with treatments or special diet – Child cannot completely comprehend all information (reluctant to answer questions) – May not understand significance of illness and lifelong consequences – • Nursing care: – – – Pain assessment and management Reassure that personal behavior has not caused illness Answer questions at level child can understand Use play as outlet; include peers or friends as much as possible Communicate to family about nonverbal cues Maintain open and honest dialogue

• Impact: – – – – • Where to place adolescent: on pediatric ward or adult floor? Dependence on caregivers Lack of privacy Maladaptive coping behaviors Refuses treatments Easily overwhelmed and may show regression Worries about condition, self-esteem, identity, and family Nursing care: – – – Provide solitary time Give realistic choices Include adolescent in medical-related matters when possible Use peer support and interaction May expand networks to include support groups and community programming
• Impact: – – – • Decreased self-esteem Receives less support from parents May have mood swings, lack understanding about condition May display negative attitude toward ill sibling Feelings of jealousy, embarrassment, resentment, loneliness, and isolation Thinks that he or she caused or might acquire the condition Nursing care: Promote family-centered care – Instruct parents to maintain familiar home routines as much as possible – Include sibling(s) in simple care – Encourage sibling visitation and share age-appropriate information –
• Children living with a chronic condition experience ≥ 1 of these symptoms: – – – – – Limitations Disfigurement, deformity, or scarring Dependence on technology Dependence on assistive devices Dependence on medication Dependence on a special diet Ongoing need for medical care appointments; treatments Ongoing need for special services Altered body image
�Dependence on others for basic daily needs �Not able to be or feel “normal” �Missed days at school �Not able to participate �Missing out on school functions �Lack of peer group or social support networks � Nursing �The care: nurse must communicate to the family that overwhelming feelings can be discussed with a health-care professional and that respite care is available
� Responses: �Initially, shock and chaos �Anger, fear, disbelief, anxiety, and confusion �If child has been ill for long period, parents may express relief at having an answer to child’s illness �Blame �Inability to bond with child � Nursing care: �Communication, support, and understanding �Sustain normal daily activity and incorporate treatment into new daily routine �Discuss important information (treatment, procedures, medicine or visits to hospital or clinic)
� Nursing �Listen care (cont’d): to parents �Teach parents about chronic sorrow �Reinforce continued involvement in the care of the child �Give parents information about community resources
� � It is important to establish a therapeutic relationship Nurse takes following actions when establishing trust: � Consider needs of entire family; do not forget siblings � Familiarize yourself with child’s condition and know about disease process � Be open and honest � Show family that burden of care is understood (burden of care includes combination of physical, psychological, social, and financial burdens family may face) � Take time to listen to child and caregiver � Arrange for continuity of nursing care � Assess family’s support systems and resources

� Nurse takes the following actions when establishing trust (cont’d): �Include parents in plan of care; some parents like to participate in child’s care while child is hospitalized �Maintain home rituals as much as possible while child is hospitalized �Treat each child as individual; essential that nurse not label child according to disease process �Allow child to make decisions about care when possible (especially important for adolescents) �Maintain confidentiality �Do not prematurely judge parents; some parents cannot stay with child in hospital based on personal needs and responsibilities
General growth failure means that child grows more slowly and that the height and weight are in lower percentile on growth charts than those for children the same age � Pathophysiology of the condition may also affect child’s growth � Treatment measures associated with chemotherapeutic agents may hinder growth or damage usual organ functioning � May see delayed development � Parents may positively or negatively affect child’s development � Plot growth on charts for the National Center for Health Statistics �
� Ensure adequate nutrition � Encourage parents to maintain realistic developmental milestones � Help child interact with same-age children � Create a social network
� Important to help family understand laws about educational services � The Individuals with Disabilities Education Act (IDEA) is the nation’s federal special education law that ensures public schools provide for the educational needs of students with disabilities
� Understanding cultural diversity of child who has chronic condition is paramount � Culturally diverse considerations emphasize cultural sensitivity in both hospital and community settings

Infant: based on degree of discomfort and reactions of parents others in the environment � Toddler: separation from parents or disruption in routine � Preschooler: �Magical thinker: illness or injury may be viewed as punishment for bad behaviors �Concrete thinker: death should not be described as “going to sleep” � School-aged child: understanding not precise until child understands concept of time; after age 8 or 9, children understand permanence of death � Adolescent: understands death at adult level, but has difficulty accepting it as reality and often thinks death can be defied �
� Complete the institution’s checklist to ensure policies and procedures are followed � Contact the bereavement team � Create a file and include community resources � Make a follow-up ledger and phone call

Loss of sensation � Loss of body’s ability to maintain thermoregulation � Skin color pale to, eventually, cyanotic (blue) � Loss of bowel and bladder function � Loss of awareness, consciousness; slurring of speech � Alteration in respiratory status � Cheyne–Stokes respirations � Noisy chest or respirations � Decreased, weak, or slow pulse rate � Drop in blood pressure � Confusion, delirium, or disorientation �
� Weakness, fatigue � Changes in pain perception � Restlessness and agitation � Alertness or alternation in sleep � Decreased oral intake � Seizures

� � � Shift from curative technological approach to providing care that enables child to move toward death accessing own inner resources Provide comfort measures Communicate genuine feelings of kindness and sympathy to family Be present Promote good communication with health-care team Manage pain and discomfort Assist child to die with dignity Cease unnecessary treatments Allow the family to express their end-of-life care wishes Use touch Give the family choices Create peaceful and supportive environment
� Palliative care for children is active, total care of the child’s mind, body, and spirit; also involves giving support to family � Hospice care uses variety of services provided by multidisciplinary group of health-care providers � End-of-life nursing care meant to provide best quality-of-life possible for child and family; holistic approach to care that includes physical, emotional, social, and spiritual interventions
� Managing discomfort and pain � Addressing questions and concerns � Communicating to family that child may not want to be left alone � Informing family about other resources, such as hospice nurses, child-life specialists, chaplains or spiritual leaders, home care agencies, social workers, and support groups
� Talk to family about child’s appearance and description of the death � Give family the choice of seeing the child alone or having the nurse accompany them into the room


� Somatic signs and symptoms of grief: Feelings of tightness in the throat or chest, sighing � Weakness or shortness of breath � Preoccupation with image of deceased � Inability to focus on anything other than loved one who died � Emotionally distancing self from others � Feelings of guilt �
� Feeling responsible for the loved one’s death Searching for what could have been done differently, thinking in terms of “if I only had done. . . ” � Hostile reactions that include feelings and expressions of anger � Inability to complete daily tasks �
A holistic nursing plan of care is essential when caring for the grieving family � After the child’s death, the family might ask the nurse questions such as “What did I do to deserve this? ” “Did I do something wrong? ” “Am I being punished? ” � Listen empathetically � Understand grief theories in order to provide proper care and support �
� Denial and isolation (numbness and disbelief) � Anger (awareness about the reality) � Bargaining (with self or “God”) � Depression (profound sadness) � Acceptance (look for meaning)
� Phase 1: State of numbness and shock � Phase 2: Period of intense grief � Phase 3: Period of reorganization
� Grief associated with sudden death or catastrophic loss: �High anxiety: emotional upheaval �Denial: protective emotional reaction �Anger: usually diffuse type of anger (lashing out) �Remorse: feelings of guilt and sorrow �Grief: period of overwhelming sadness �Reconciliation: endpoint to the family crisis (moving on)

� Grief reactions can differ � Recognize exhibited coping patterns and find ways to support family: � Listen, sit silently, refer family to pastoral care, offer spiritual care � If destructive behavior to self or others, call physician or professional counselor � Do not alter coping pattern completely � Pathological � Recognize grief: subtle indicators � Suicidal or homicidal ideation � Violent behavior � Grief influenced by drugs and alcohol � Extreme denial
Saying good-bye should not be rushed � Call the child by name � � What to say to the parents or caregiver: � “I’m sorry” � “This must be terribly hard for you” � “Is there anyone I can call for you? ” � “Would you like me to stay with you for a while? ” Keep the child covered up and as warm as possible � Allow parents to give the last bath and hold the child � Others may come to say good-bye � Be supportive and allow family to dictate the “goodbye” timeline �
�A visit from the sibling(s) is important � Include sibling(s) in the dying and grief process � Play is used as a coping mechanism � Keep routines to enhance safety and comfort � Parents can still set limits and enforce usual discipline parameters � School counselors may help � Give sibling(s) the opportunity to say goodbye and express personal wants and needs
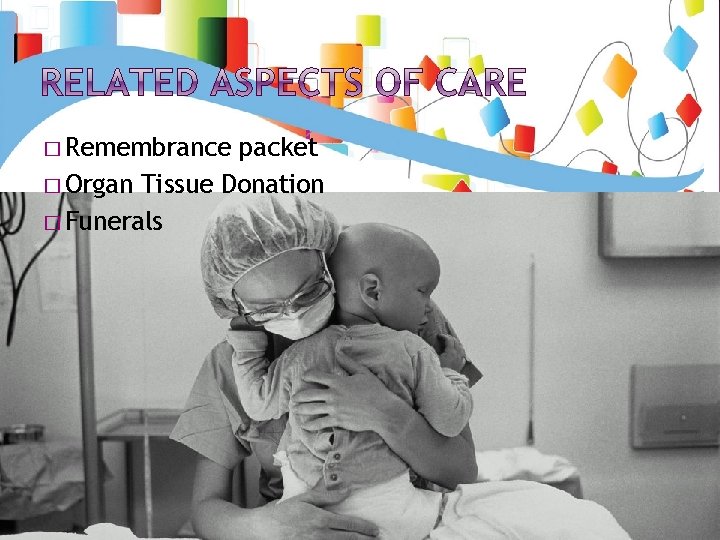
� Remembrance packet � Organ Tissue Donation � Funerals
�A nurse caring for the dying child can experience personal emotions � Burnout is a state of physical, emotional, and mental exhaustion � Compassion fatigue syndrome is characterized by a sense of helplessness, confusion, and isolation from supporters � Moral distress is when the nurse is unable to translate personal moral choices into action; the nurse acts in a manner contrary to personal or professional values, which undermines integrity � Pay attention to personal needs and take action