Common Injection Techniques In PMR Se Won Lee
- Slides: 51
Common Injection Techniques In PM&R Se Won Lee MD
Learning Objectives • Learn basic anatomy and kinesiology of major joints • Learn indication, contraindication and complications of injection to major joints and bursae • Learn techniques of individual injections • Learn basic introduction to musculoskeletal ultrasound
Major Joints and Bursae • Common Injection sites for Upper Extremity Lower Extremity o o Shoulder and Elbow Joint Bursae in Shoulder Tendon in Elbow Carpal tunnel o Knee Joint o Bursae in hip and knee o Ankle Joint
General Indication for Injection in PM & R • Joint pathologies; symptomatic OA flare up, inflammatory arthropathy (crystal deposition disease, adjuvant Tx for rheumatoid arthropathy), adhesive capsulitis etc • Bursal pathologies; subacromial, trochanteric, pes anserine, retrocalcaneal bursitis etc • Tendon (Tenosynovium, paratendon) and ligament pathologies; dequevain tenosynovitis, trigger finger etc • Peripheral entrapment neuropathy; carpal tunnel syndrome • Others; ganglion cyst, fascial defect (tear) • Epidural/axial joint injection
Type of Injectate • • • Steroid Local anesthetics: lidocaine, bupivacaine Sclerosing therapy Viscosupplementation; hyaluronic acid Biologics; hyperosmolar agents, platelet rich plasma, stem cells etc
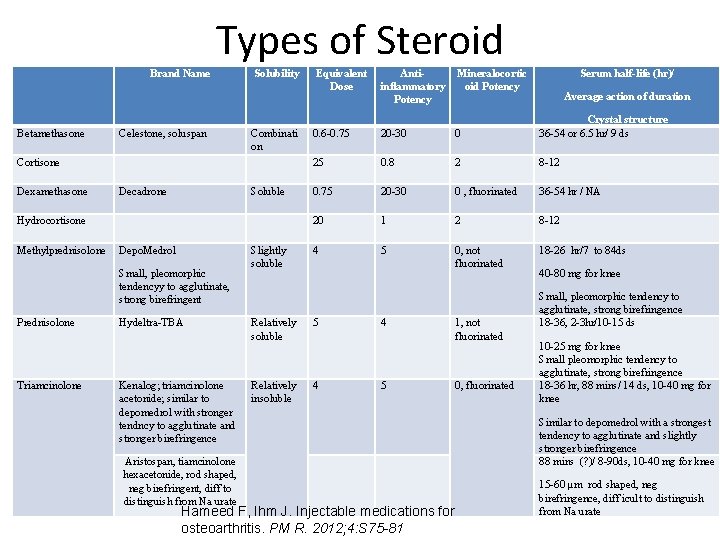
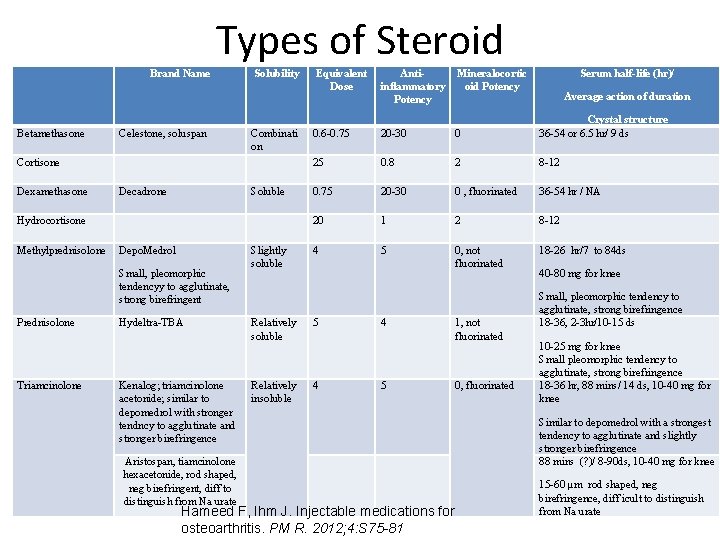
Types of Steroid Brand Name Betamethasone Celestone, soluspan Solubility Combinati on Cortisone Dexamethasone Decadrone Soluble Hydrocortisone Methylprednisolone Depo. Medrol Small, pleomorphic tendencyy to agglutinate, strong birefringent Prednisolone Triamcinolone Hydeltra-TBA Kenalog; triamcinolone acetonide; similar to depomedrol with stronger tendncy to agglutinate and stronger birefringence Aristospan, tiamcinolone hexacetonide, rod shaped, neg birefringent, diff to distinguish from Na urate Slightly soluble Equivalent Dose Antiinflammatory Potency Mineralocortic oid Potency Serum half-life (hr)/ Average action of duration 0. 6 -0. 75 20 -30 0 Crystal structure 36 -54 or 6. 5 hr/ 9 ds 25 0. 8 2 8 -12 0. 75 20 -30 0 , fluorinated 36 -54 hr / NA 20 1 2 8 -12 4 5 0, not fluorinated 18 -26 hr/7 to 84 ds Relatively soluble 5 Relatively insoluble 4 4 5 Hameed F, Ihm J. Injectable medications for osteoarthritis. PM R. 2012; 4: S 75 -81 1, not fluorinated 0, fluorinated 40 -80 mg for knee Small, pleomorphic tendency to agglutinate, strong birefringence 18 -36, 2 -3 hr/10 -15 ds 10 -25 mg for knee Small pleomorphic tendency to agglutinate, strong birefringence 18 -36 hr, 88 mins/ 14 ds, 10 -40 mg for knee Similar to depomedrol with a strongest tendency to agglutinate and slightly stronger birefringence 88 mins (? )/ 8 -90 ds, 10 -40 mg for knee 15 -60 µm rod shaped, neg birefringence, diff icult to distinguish from Na urate
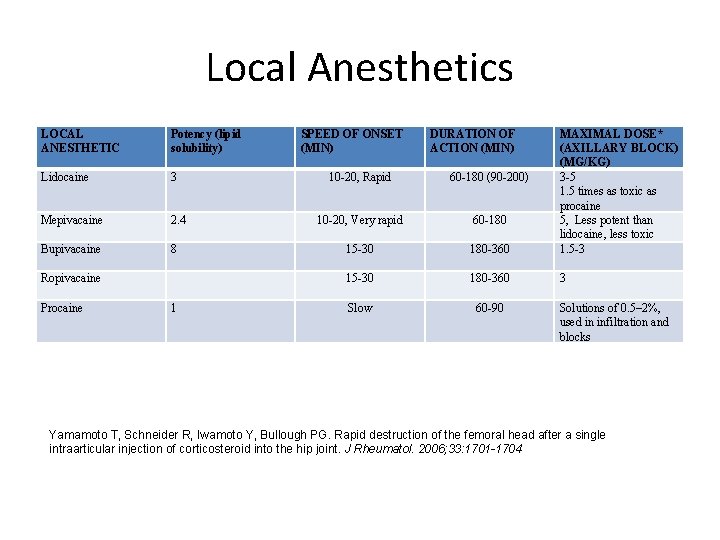
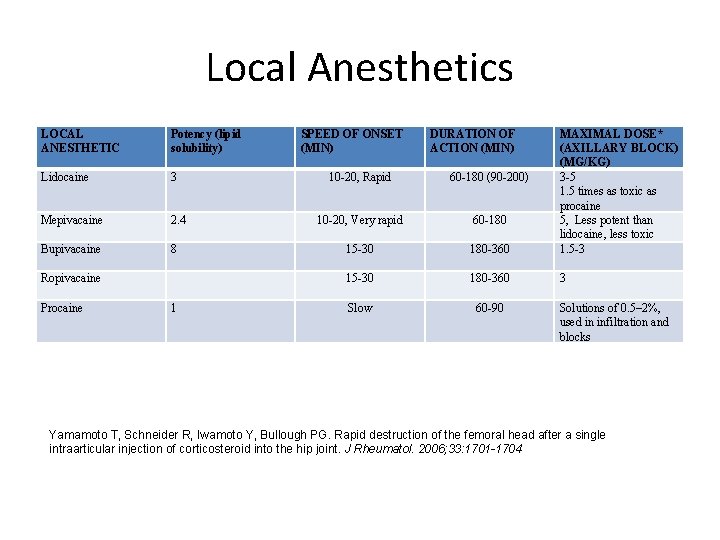
Local Anesthetics LOCAL ANESTHETIC Potency (lipid solubility) Lidocaine 3 Mepivacaine 2. 4 Bupivacaine 8 Ropivacaine Procaine 1 SPEED OF ONSET (MIN) DURATION OF ACTION (MIN) 10 -20, Rapid 60 -180 (90 -200) 10 -20, Very rapid 60 -180 15 -30 180 -360 MAXIMAL DOSE* (AXILLARY BLOCK) (MG/KG) 3 -5 1. 5 times as toxic as procaine 5, Less potent than lidocaine, less toxic 1. 5 -3 15 -30 180 -360 3 Slow 60 -90 Solutions of 0. 5– 2%, used in infiltration and blocks Yamamoto T, Schneider R, Iwamoto Y, Bullough PG. Rapid destruction of the femoral head after a single intraarticular injection of corticosteroid into the hip joint. J Rheumatol. 2006; 33: 1701 -1704
Precautions • Be cautious of cutaneous or peripheral nerves nearby structures; try to avoid (US may be useful in some conditions) • Subdeltoid bursa: deltoid artery (branch of thoracoacromial A) • Long head of biceps; anterior circumflex humeral artery • Lateral elbow; radial N and radial recurrent A • de. Quervain tenosynovitis/CMC joint; superficial radial nerve/ artery • Medial knee injection; infrapatellar branch of saphenous N • Tibio-fibular joint; common peroneal N, popliteus tendon/tenosynovium; common peroneal, lateral collateral lig • Retrocalcaneal bursa: sural N and Achilles tendon
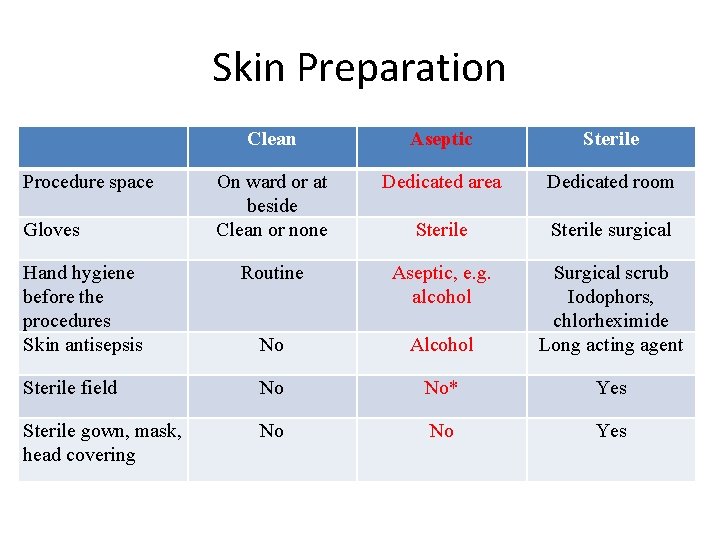
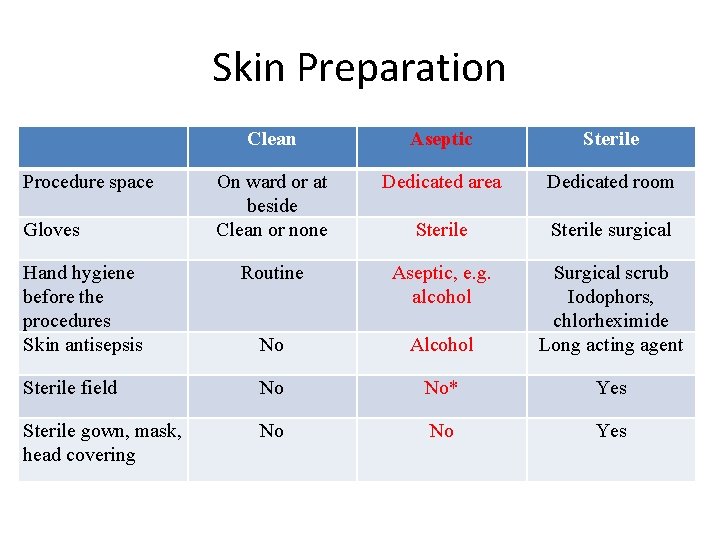
Skin Preparation Clean Aseptic Sterile On ward or at beside Clean or none Dedicated area Dedicated room Sterile surgical Routine Aseptic, e. g. alcohol No Alcohol Surgical scrub Iodophors, chlorheximide Long acting agent Sterile field No No* Yes Sterile gown, mask, head covering No No Yes Procedure space Gloves Hand hygiene before the procedures Skin antisepsis
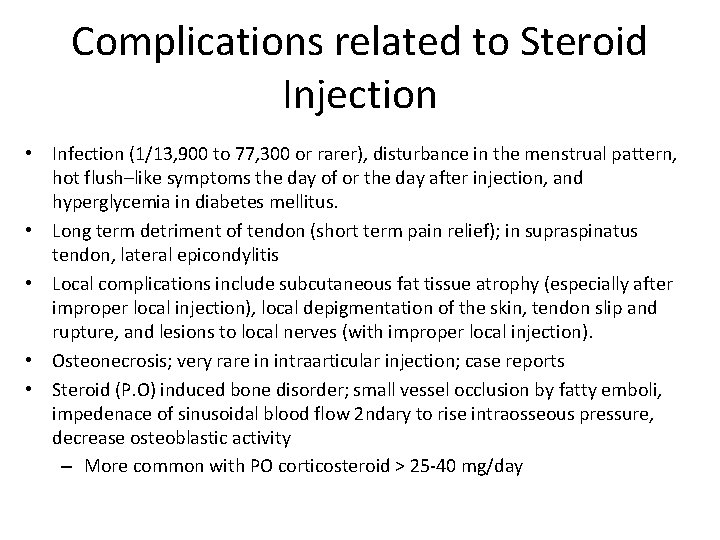
Complications related to Steroid Injection • Infection (1/13, 900 to 77, 300 or rarer), disturbance in the menstrual pattern, hot flush–like symptoms the day of or the day after injection, and hyperglycemia in diabetes mellitus. • Long term detriment of tendon (short term pain relief); in supraspinatus tendon, lateral epicondylitis • Local complications include subcutaneous fat tissue atrophy (especially after improper local injection), local depigmentation of the skin, tendon slip and rupture, and lesions to local nerves (with improper local injection). • Osteonecrosis; very rare in intraarticular injection; case reports • Steroid (P. O) induced bone disorder; small vessel occlusion by fatty emboli, impedenace of sinusoidal blood flow 2 ndary to rise intraosseous pressure, decrease osteoblastic activity – More common with PO corticosteroid > 25 -40 mg/day
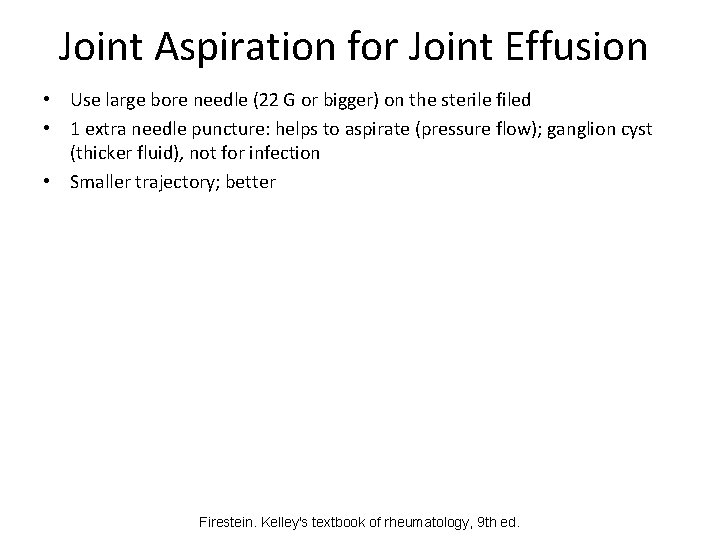
Joint Aspiration for Joint Effusion • Use large bore needle (22 G or bigger) on the sterile filed • 1 extra needle puncture: helps to aspirate (pressure flow); ganglion cyst (thicker fluid), not for infection • Smaller trajectory; better Firestein. Kelley's textbook of rheumatology, 9 th ed.
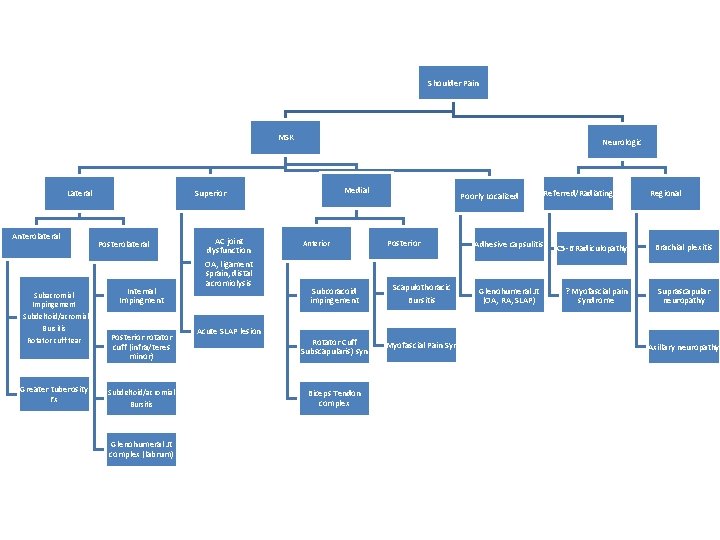
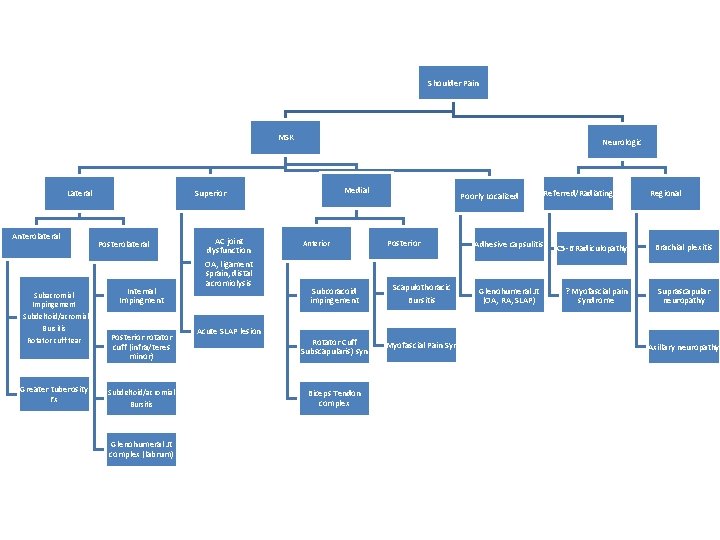
Shoulder Pain MSK Lateral Anterolateral Subacromial Impingement - Subdeltoid/acromial Bursitis Rotator cuff tear Greater tuberosity Fx Neurologic Medial Superior Posterolateral Internal Impingment Posterior rotator cuff (infra/teres minor) Subdeltoid/acromial Bursitis Glenohumeral Jt complex (labrum) AC joint dysfunction OA, ligament sprain, distal acromiolysis Acute SLAP lesion Anterior Poorly Localized Posterior Subcoracoid impingement Scapulothoracic Rotator Cuff (Subscapularis) syn. Myofascial Pain Syn Biceps Tendon complex Bursitis Referred/Radiating Adhesive capsulitis Glenohumeral Jt (OA, RA, SLAP) Regional C 5 -6 Radiculopathy Brachial plexitis ? Myofascial pain syndrome Suprascapular neuropathy Axillary neuropathy
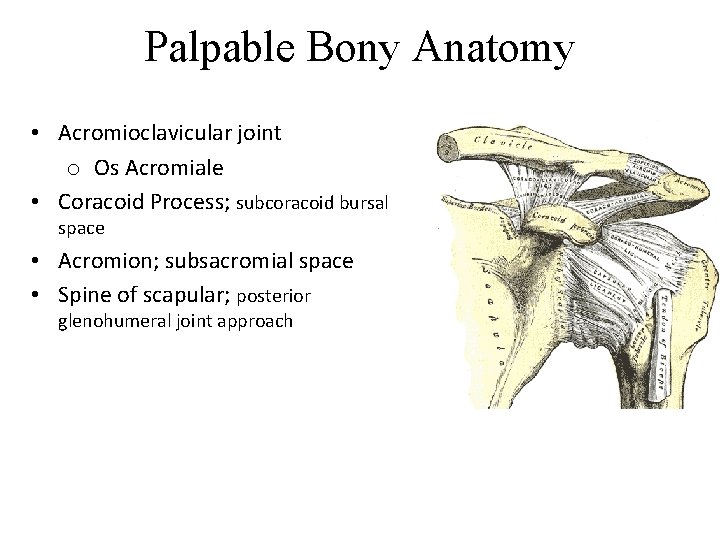
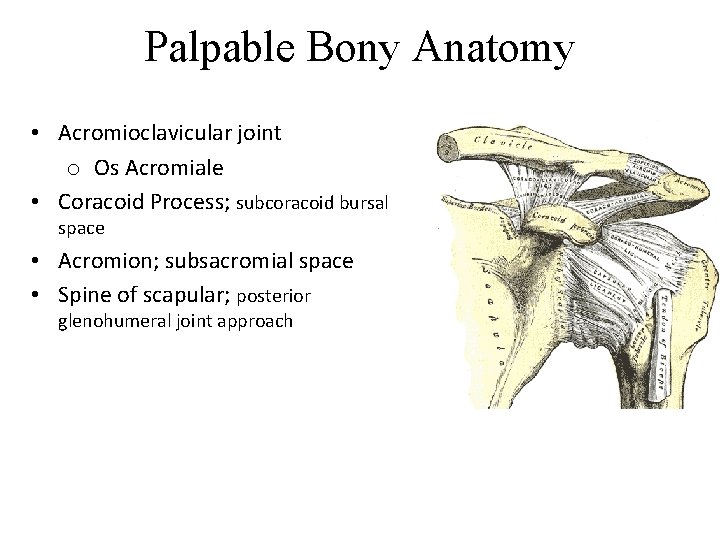
Palpable Bony Anatomy • Acromioclavicular joint o Os Acromiale • Coracoid Process; subcoracoid bursal space • Acromion; subsacromial space • Spine of scapular; posterior glenohumeral joint approach
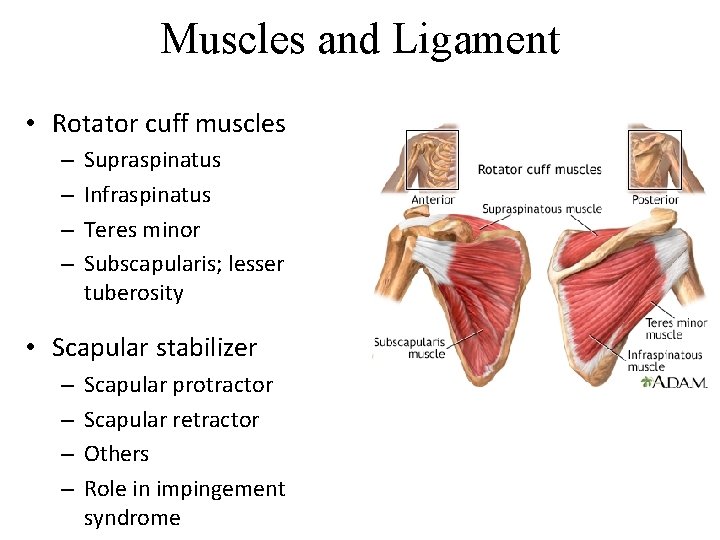
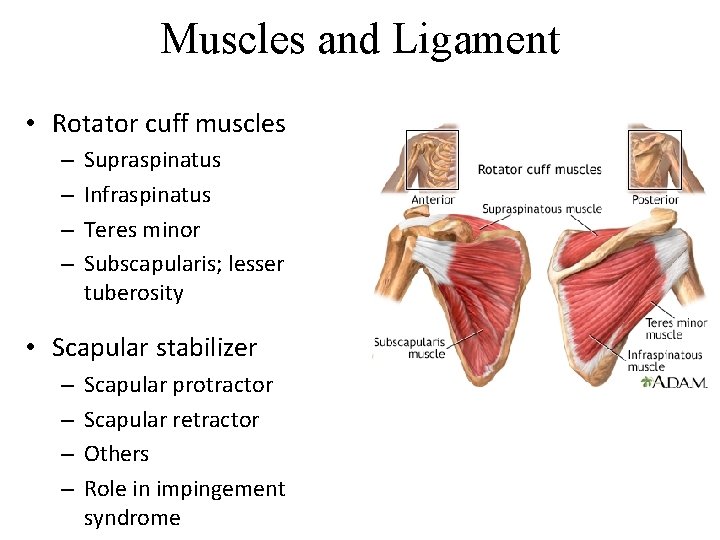
Muscles and Ligament • Rotator cuff muscles – – Supraspinatus Infraspinatus Teres minor Subscapularis; lesser tuberosity • Scapular stabilizer – – Scapular protractor Scapular retractor Others Role in impingement syndrome
Shoulder Biomechanics • Scapular positioning and movement – Shoulder abduction in asymptomatic patients; scapular rotates upwardly, rotates externally and tilts posteriorly – In impingement syndrome; decreased upward rotation and decreased posterior tilt – In glenohumeral instability; decreased upward rotation and increased internal rotation • Decreased distance between the humerus and coracoacromial arch: promoting impingement syndrome – Supraspinatus tendon tear: elevate the humeral head to coracoacromial arch (vicious cycle) – Scapular stabilizer weakness; scapular protract and depress it. Struyf F, Nijs J, Baeyens JP, Mottram S, Meeusen R. Scapular positioning and movement in unimpaired shoulders, shoulder impingement syndrome, and glenohumeral instability. Scandinavian journal of medicine & science in sports. 2011; 21: 352 -358
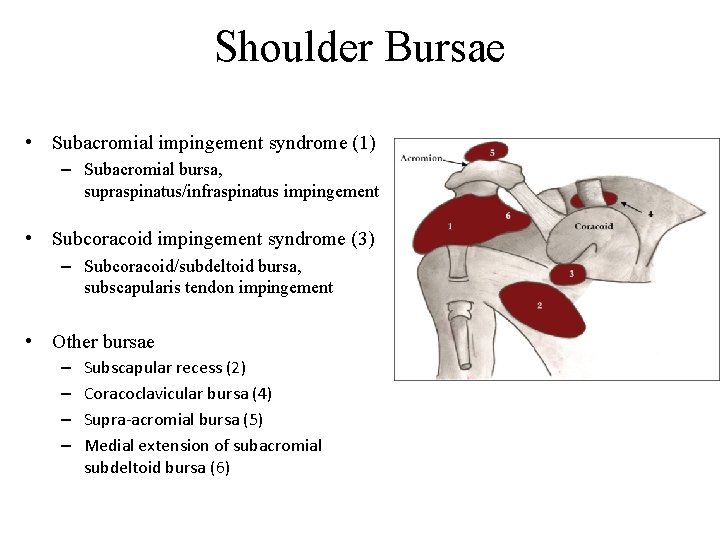
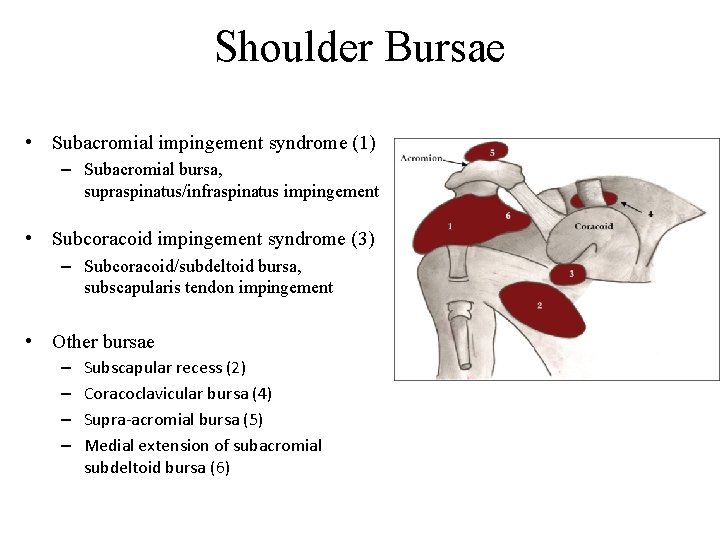
Shoulder Bursae • Subacromial impingement syndrome (1) – Subacromial bursa, supraspinatus/infraspinatus impingement • Subcoracoid impingement syndrome (3) – Subcoracoid/subdeltoid bursa, subscapularis tendon impingement • Other bursae – – Subscapular recess (2) Coracoclavicular bursa (4) Supra-acromial bursa (5) Medial extension of subacromial subdeltoid bursa (6)
Anatomy of Subaromial Space • The superior border (the roof): the coracoacromial arch • The inferior (the floor): the greater tuberosity of the humerus & the superior aspect of the humeral head. • The space between the acromion and the humeral head: 1. 0 - 1. 5 cm: the rotator cuff tendons, the long head of the biceps tendon, the bursa, and the coracoacromial ligament • The true height of this space is considerably less than that seen on radiographs
Physical Examination for Decision Making • Any signs of infection (erythema), wound, warmth (can be inflammatory) or uncontrolled BP, glucose especially with red flag; aspiration, no injection • Positive Impingement Signs; Neer and Hawkin’s test or coracoid impingement test Subacromial injection • Global decrease in Range of Motion – External rotation more or equal to internal rotation Glenohumeral joint injection
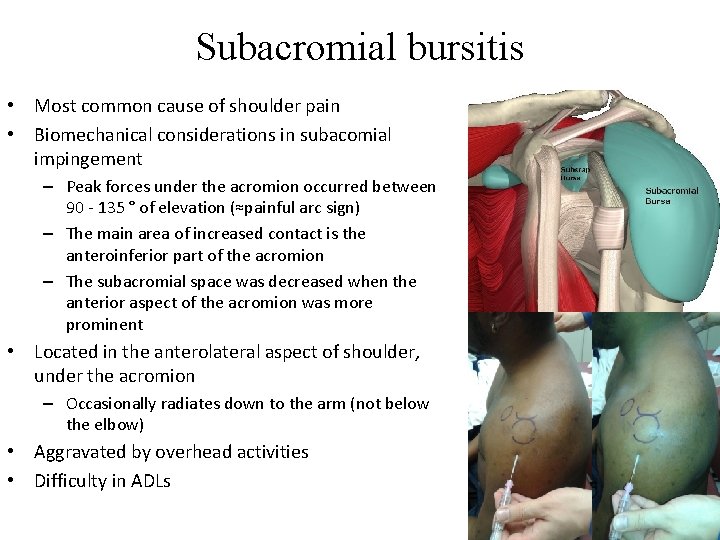
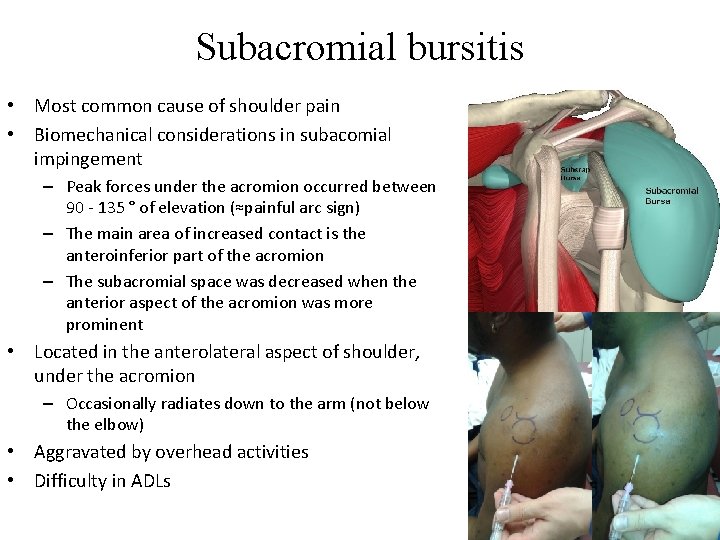
Subacromial bursitis • Most common cause of shoulder pain • Biomechanical considerations in subacomial impingement – Peak forces under the acromion occurred between 90 - 135 ° of elevation (≈painful arc sign) – The main area of increased contact is the anteroinferior part of the acromion – The subacromial space was decreased when the anterior aspect of the acromion was more prominent • Located in the anterolateral aspect of shoulder, under the acromion – Occasionally radiates down to the arm (not below the elbow) • Aggravated by overhead activities • Difficulty in ADLs
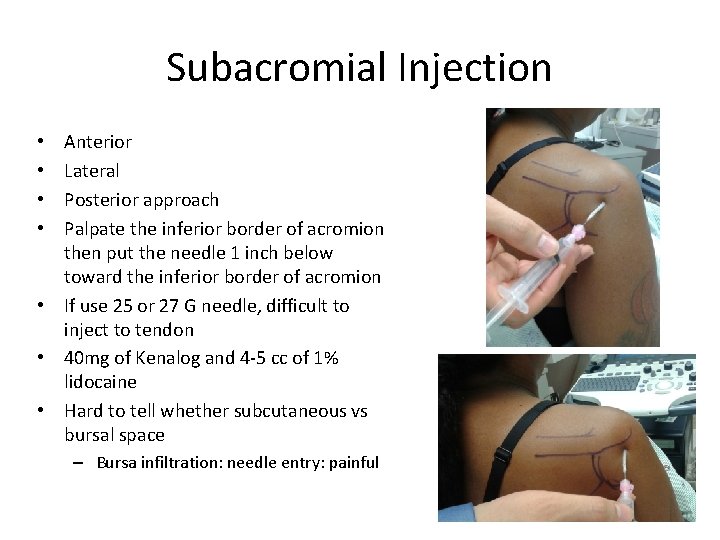
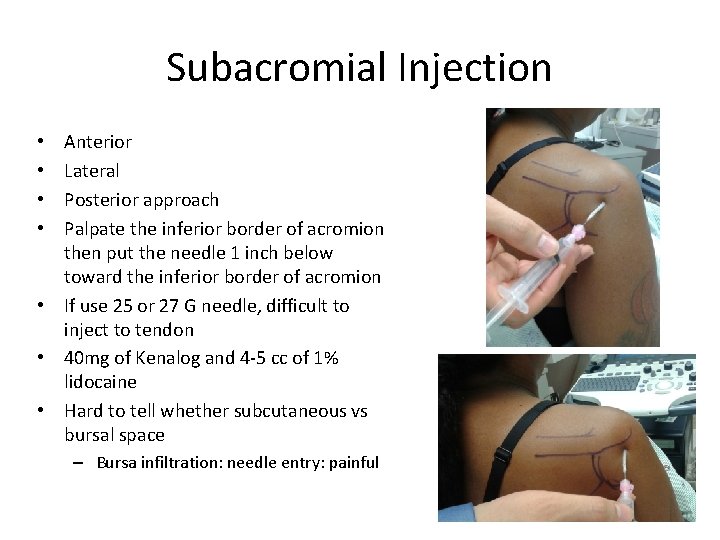
Subacromial Injection Anterior Lateral Posterior approach Palpate the inferior border of acromion then put the needle 1 inch below toward the inferior border of acromion • If use 25 or 27 G needle, difficult to inject to tendon • 40 mg of Kenalog and 4 -5 cc of 1% lidocaine • Hard to tell whether subcutaneous vs bursal space • • – Bursa infiltration: needle entry: painful
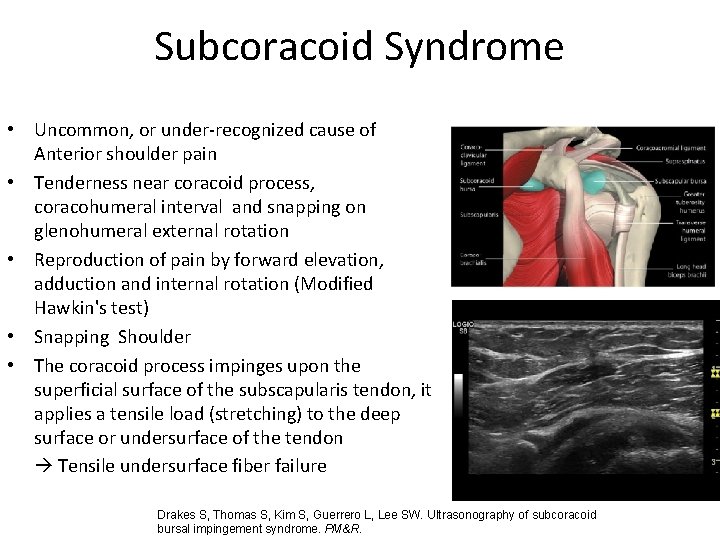
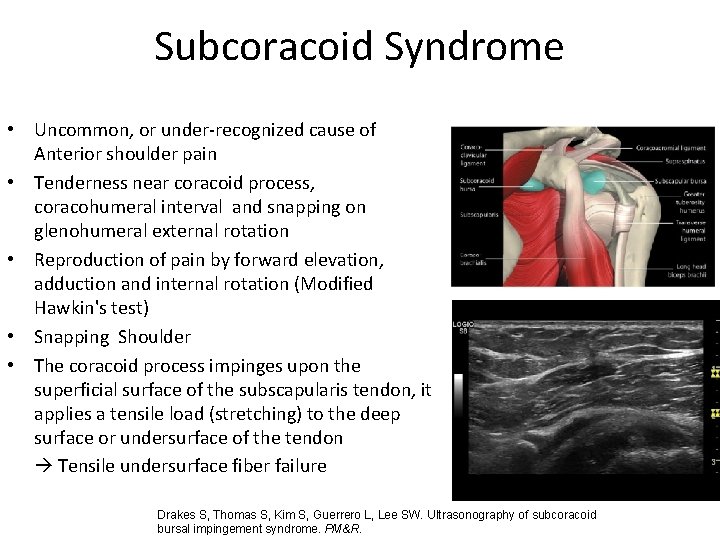
Subcoracoid Syndrome • Uncommon, or under-recognized cause of Anterior shoulder pain • Tenderness near coracoid process, coracohumeral interval and snapping on glenohumeral external rotation • Reproduction of pain by forward elevation, adduction and internal rotation (Modified Hawkin's test) • Snapping Shoulder • The coracoid process impinges upon the superficial surface of the subscapularis tendon, it applies a tensile load (stretching) to the deep surface or undersurface of the tendon Tensile undersurface fiber failure Drakes S, Thomas S, Kim S, Guerrero L, Lee SW. Ultrasonography of subcoracoid bursal impingement syndrome. PM&R.
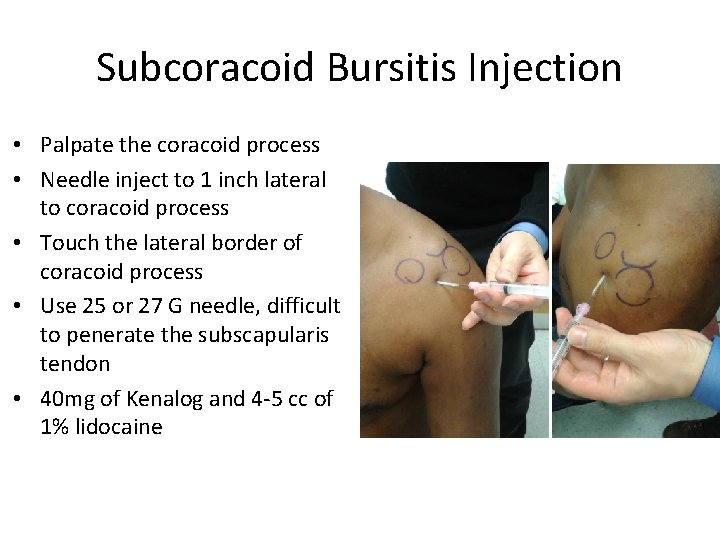
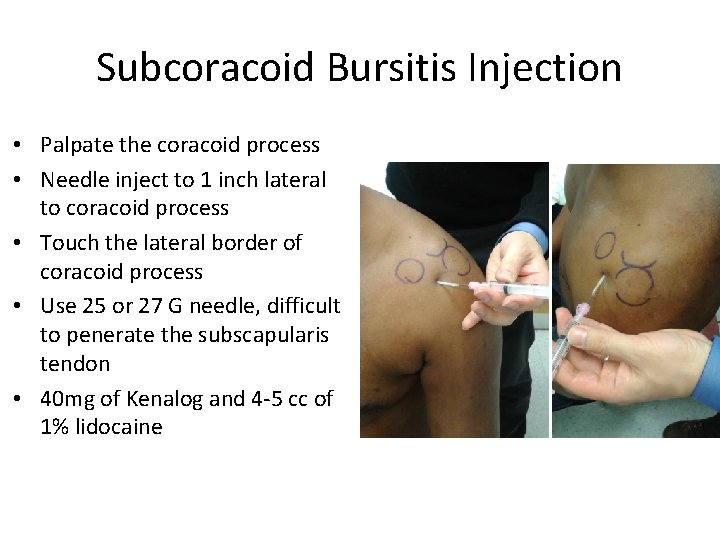
Subcoracoid Bursitis Injection • Palpate the coracoid process • Needle inject to 1 inch lateral to coracoid process • Touch the lateral border of coracoid process • Use 25 or 27 G needle, difficult to penerate the subscapularis tendon • 40 mg of Kenalog and 4 -5 cc of 1% lidocaine
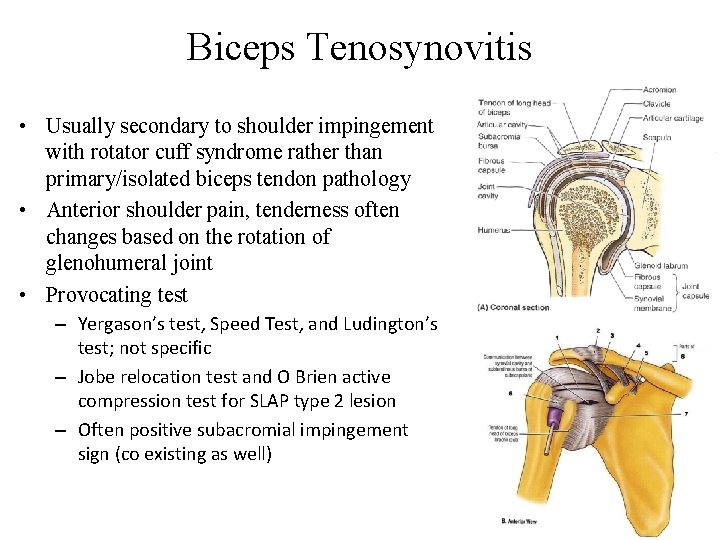
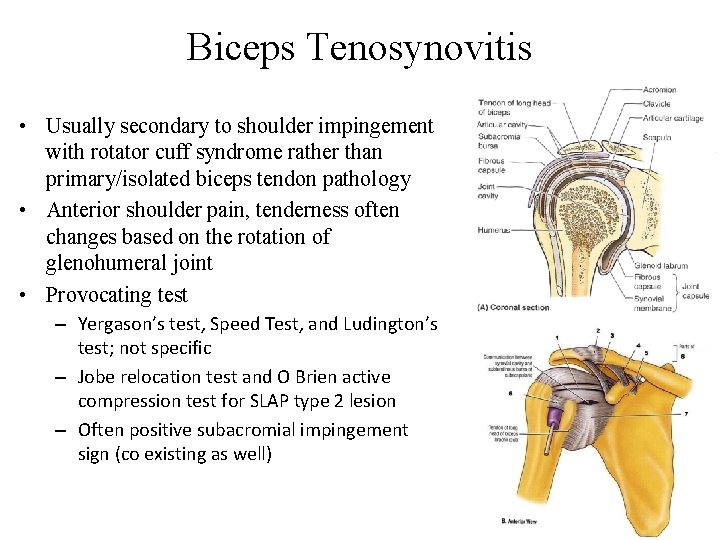
Biceps Tenosynovitis • Usually secondary to shoulder impingement with rotator cuff syndrome rather than primary/isolated biceps tendon pathology • Anterior shoulder pain, tenderness often changes based on the rotation of glenohumeral joint • Provocating test – Yergason’s test, Speed Test, and Ludington’s test; not specific – Jobe relocation test and O Brien active compression test for SLAP type 2 lesion – Often positive subacromial impingement sign (co existing as well)
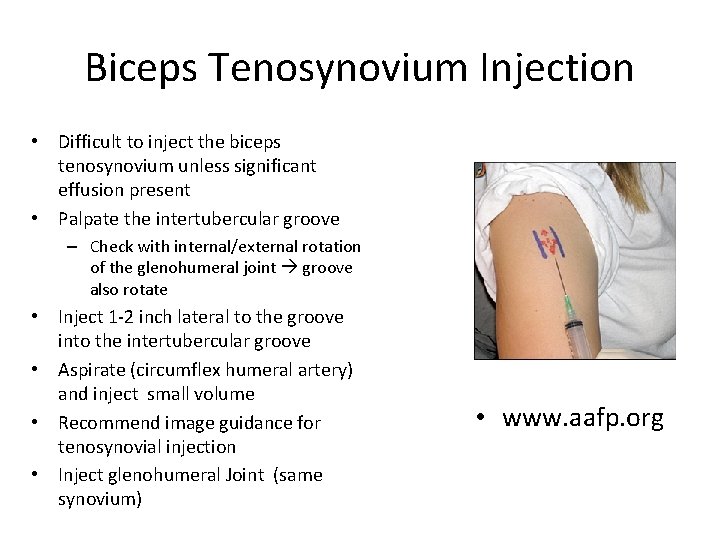
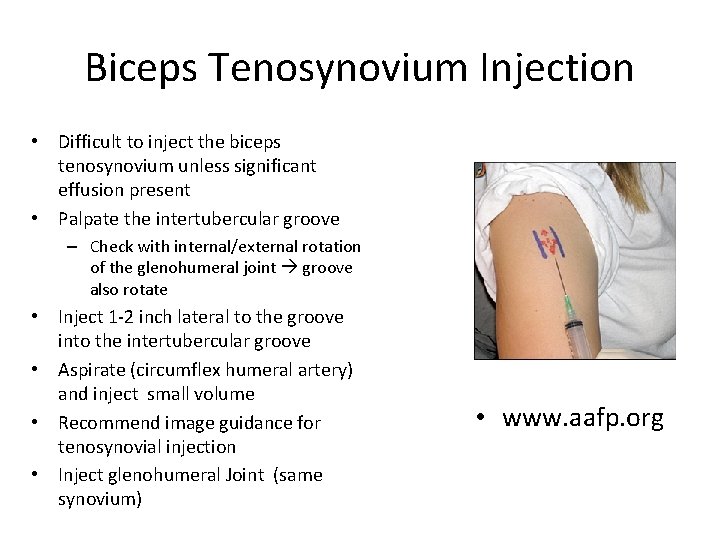
Biceps Tenosynovium Injection • Difficult to inject the biceps tenosynovium unless significant effusion present • Palpate the intertubercular groove – Check with internal/external rotation of the glenohumeral joint groove also rotate • Inject 1 -2 inch lateral to the groove into the intertubercular groove • Aspirate (circumflex humeral artery) and inject small volume • Recommend image guidance for tenosynovial injection • Inject glenohumeral Joint (same synovium) • www. aafp. org
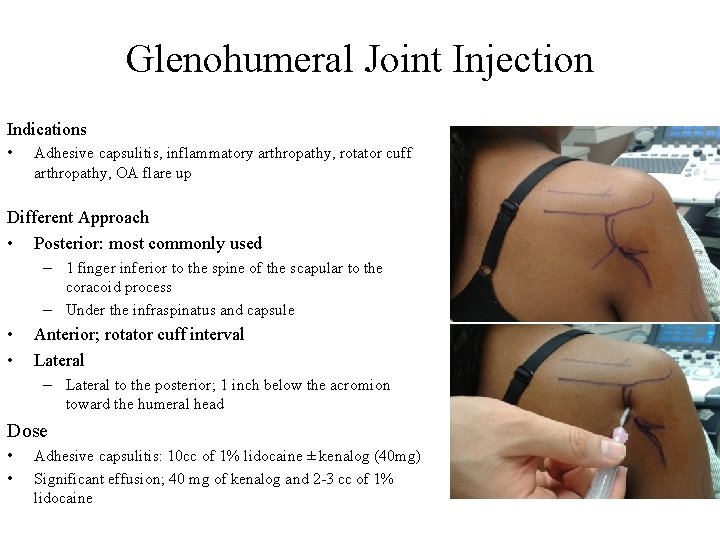
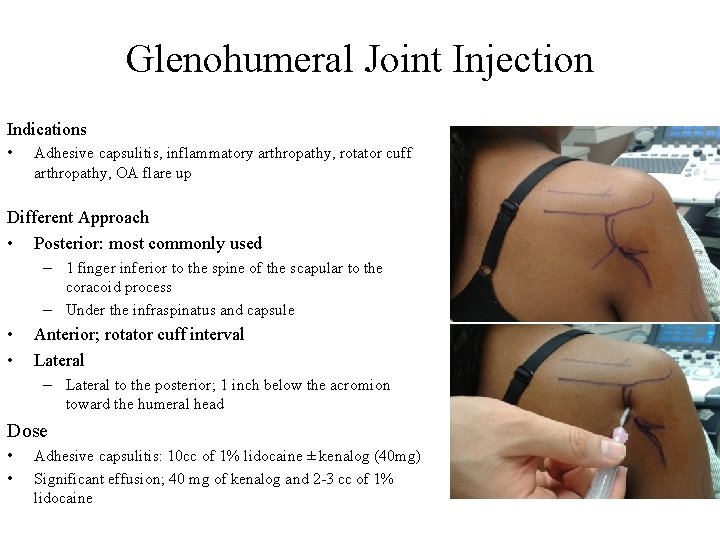
Glenohumeral Joint Injection Indications • Adhesive capsulitis, inflammatory arthropathy, rotator cuff arthropathy, OA flare up Different Approach • Posterior: most commonly used – 1 finger inferior to the spine of the scapular to the coracoid process – Under the infraspinatus and capsule • • Anterior; rotator cuff interval Lateral – Lateral to the posterior; 1 inch below the acromion toward the humeral head Dose • • Adhesive capsulitis: 10 cc of 1% lidocaine ± kenalog (40 mg) Significant effusion; 40 mg of kenalog and 2 -3 cc of 1% lidocaine
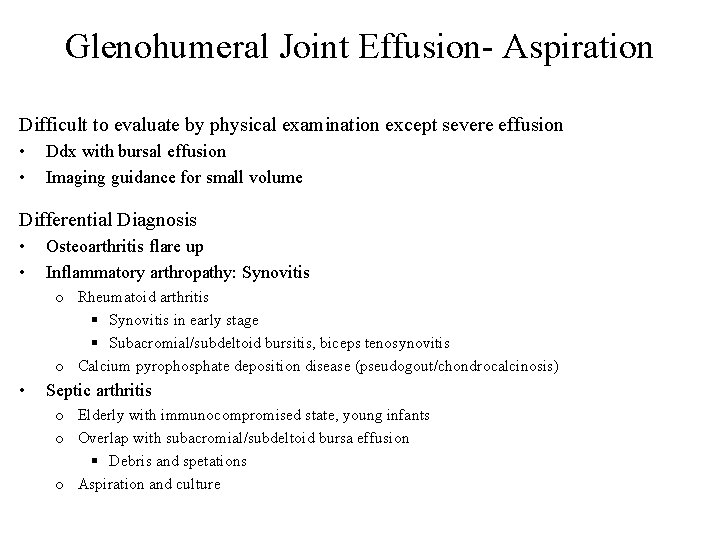
Glenohumeral Joint Effusion- Aspiration Difficult to evaluate by physical examination except severe effusion • • Ddx with bursal effusion Imaging guidance for small volume Differential Diagnosis • • Osteoarthritis flare up Inflammatory arthropathy: Synovitis o Rheumatoid arthritis § Synovitis in early stage § Subacromial/subdeltoid bursitis, biceps tenosynovitis o Calcium pyrophosphate deposition disease (pseudogout/chondrocalcinosis) • Septic arthritis o Elderly with immunocompromised state, young infants o Overlap with subacromial/subdeltoid bursa effusion § Debris and spetations o Aspiration and culture
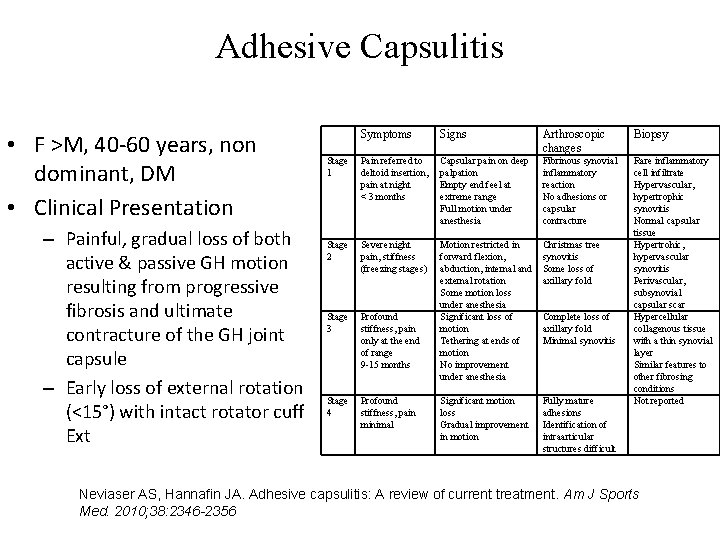
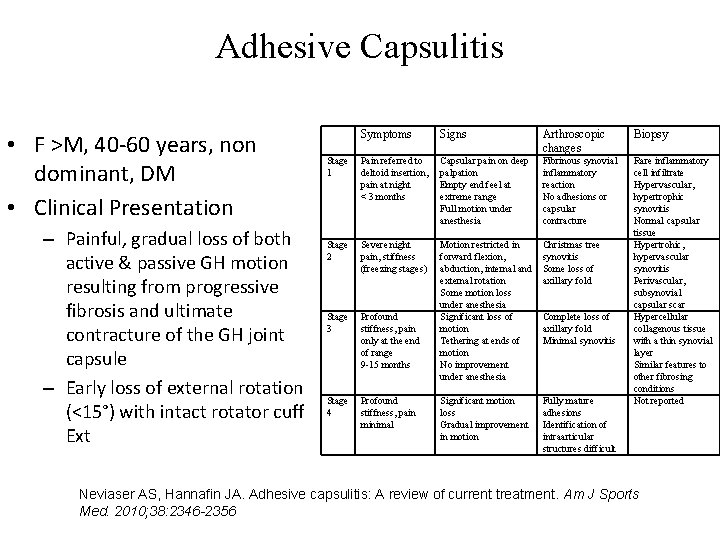
Adhesive Capsulitis • F >M, 40 -60 years, non dominant, DM • Clinical Presentation – Painful, gradual loss of both active & passive GH motion resulting from progressive fibrosis and ultimate contracture of the GH joint capsule – Early loss of external rotation (<15°) with intact rotator cuff Ext Symptoms Signs Arthroscopic changes Biopsy Stage Pain referred to 1 deltoid insertion, pain at night < 3 months Capsular pain on deep palpation Empty end feel at extreme range Full motion under anesthesia Fibrinous synovial inflammatory reaction No adhesions or capsular contracture Stage Severe night 2 pain, stiffness (freezing stages) Motion restricted in forward flexion, abduction, internal and external rotation Some motion loss under anesthesia Significant loss of motion Tethering at ends of motion No improvement under anesthesia Christmas tree synovitis Some loss of axillary fold Significant motion loss Gradual improvement in motion Fully mature adhesions Identification of intraarticular structures difficult Rare inflammatory cell infiltrate Hypervascular, hypertrophic synovitis Normal capsular tissue Hypertrohic, hypervascular synovitis Perivascular, subsynovial capsular scar Hypercellular collagenous tissue with a thin synovial layer Similar features to other fibrosing conditions Not reported Stage Profound 3 stiffness, pain only at the end of range 9 -15 months Stage Profound 4 stiffness, pain minimal Complete loss of axillary fold Minimal synovitis Neviaser AS, Hannafin JA. Adhesive capsulitis: A review of current treatment. Am J Sports Med. 2010; 38: 2346 -2356
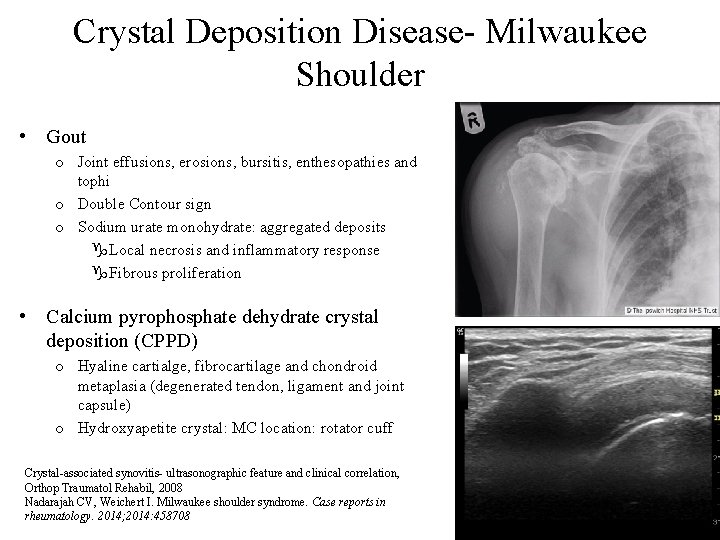
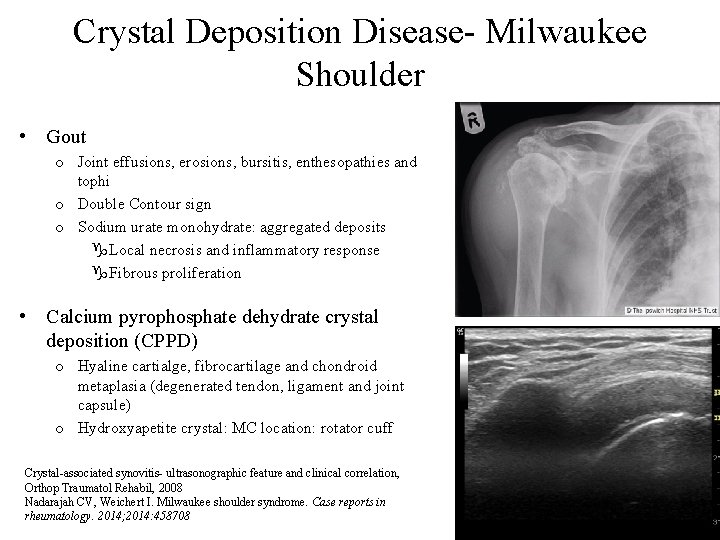
Crystal Deposition Disease- Milwaukee Shoulder • Gout o Joint effusions, erosions, bursitis, enthesopathies and tophi o Double Contour sign o Sodium urate monohydrate: aggregated deposits g. Local necrosis and inflammatory response g. Fibrous proliferation • Calcium pyrophosphate dehydrate crystal deposition (CPPD) o Hyaline cartialge, fibrocartilage and chondroid metaplasia (degenerated tendon, ligament and joint capsule) o Hydroxyapetite crystal: MC location: rotator cuff Crystal-associated synovitis- ultrasonographic feature and clinical correlation, Orthop Traumatol Rehabil, 2008 Nadarajah CV, Weichert I. Milwaukee shoulder syndrome. Case reports in rheumatology. 2014; 2014: 458708
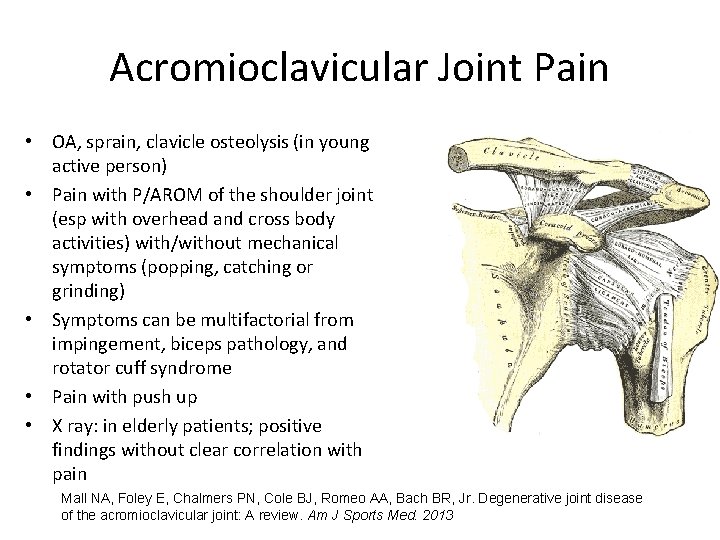
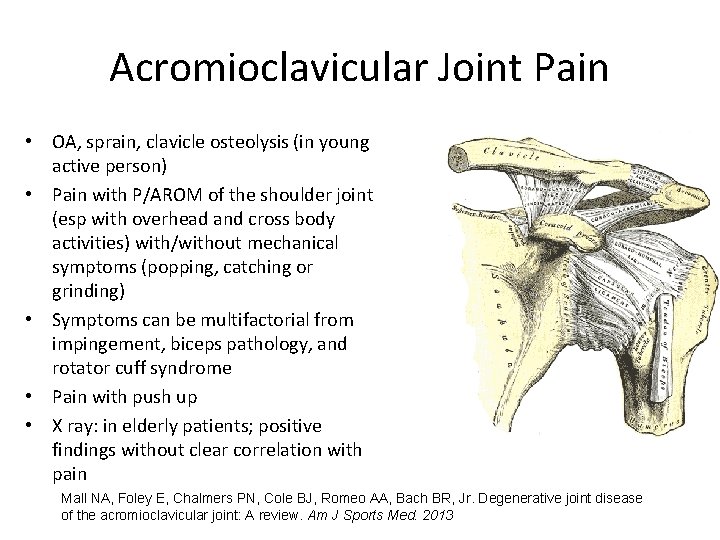
Acromioclavicular Joint Pain • OA, sprain, clavicle osteolysis (in young active person) • Pain with P/AROM of the shoulder joint (esp with overhead and cross body activities) with/without mechanical symptoms (popping, catching or grinding) • Symptoms can be multifactorial from impingement, biceps pathology, and rotator cuff syndrome • Pain with push up • X ray: in elderly patients; positive findings without clear correlation with pain Mall NA, Foley E, Chalmers PN, Cole BJ, Romeo AA, Bach BR, Jr. Degenerative joint disease of the acromioclavicular joint: A review. Am J Sports Med. 2013
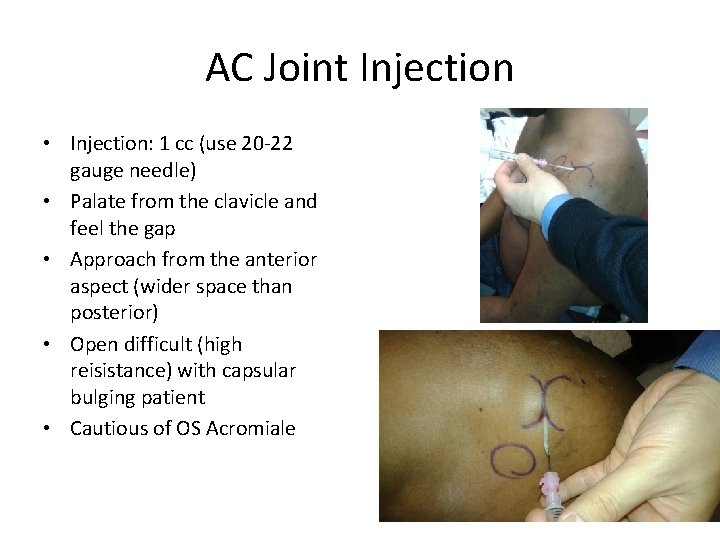
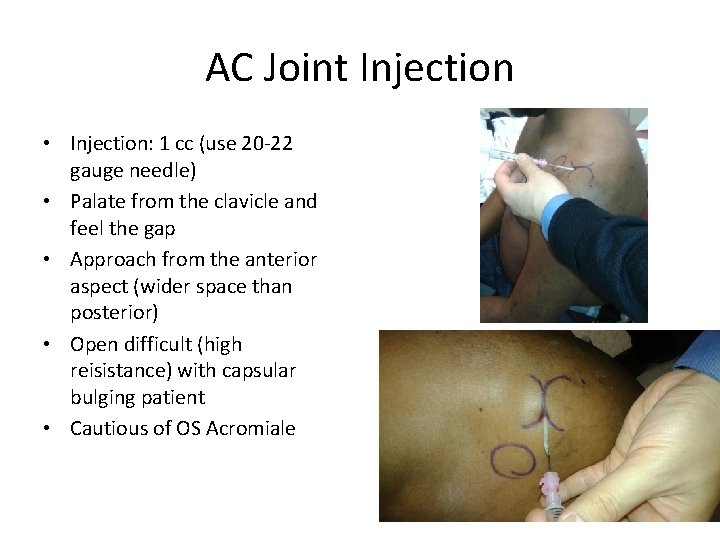
AC Joint Injection • Injection: 1 cc (use 20 -22 gauge needle) • Palate from the clavicle and feel the gap • Approach from the anterior aspect (wider space than posterior) • Open difficult (high reisistance) with capsular bulging patient • Cautious of OS Acromiale
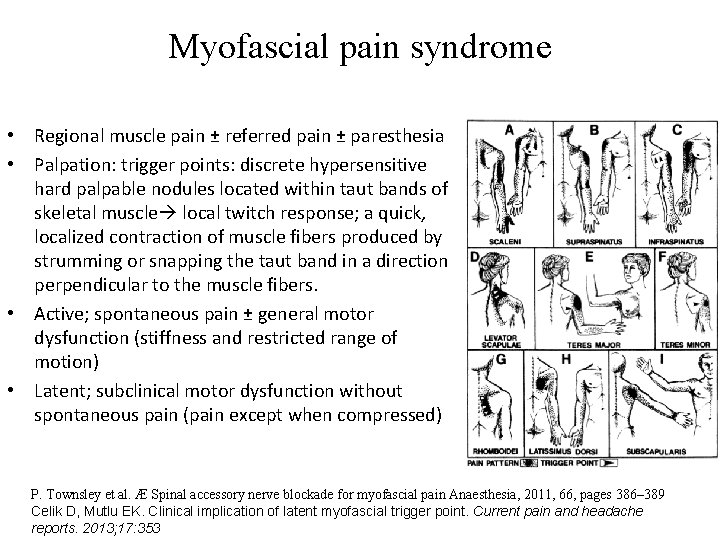
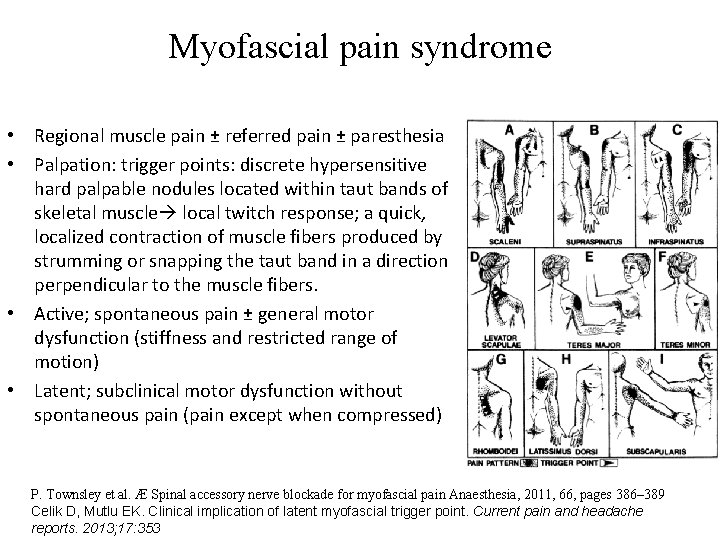
Myofascial pain syndrome • Regional muscle pain ± referred pain ± paresthesia • Palpation: trigger points: discrete hypersensitive hard palpable nodules located within taut bands of skeletal muscle local twitch response; a quick, localized contraction of muscle fibers produced by strumming or snapping the taut band in a direction perpendicular to the muscle fibers. • Active; spontaneous pain ± general motor dysfunction (stiffness and restricted range of motion) • Latent; subclinical motor dysfunction without spontaneous pain (pain except when compressed) P. Townsley et al. Æ Spinal accessory nerve blockade for myofascial pain Anaesthesia, 2011, 66, pages 386– 389 Celik D, Mutlu EK. Clinical implication of latent myofascial trigger point. Current pain and headache reports. 2013; 17: 353
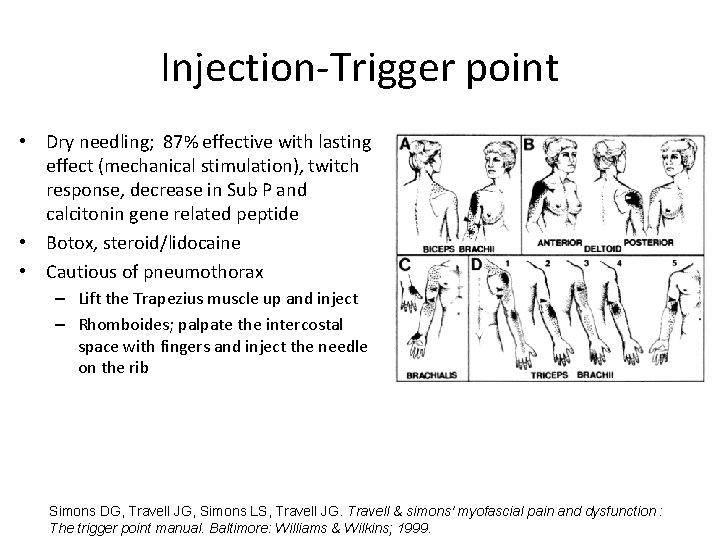
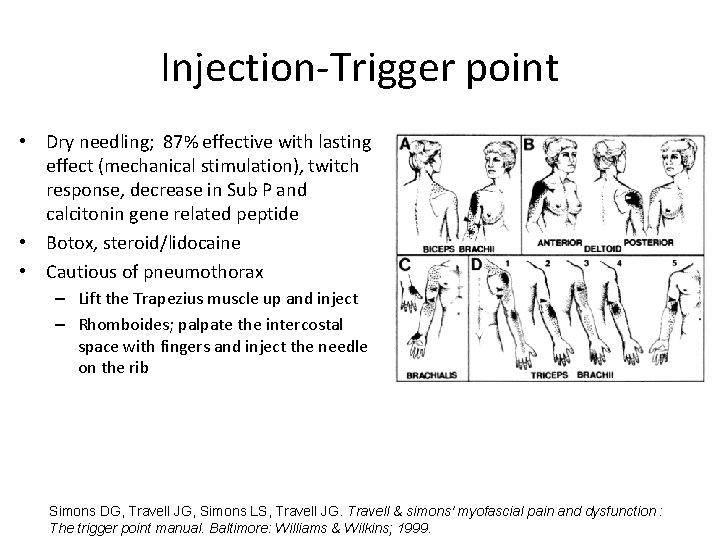
Injection-Trigger point • Dry needling; 87% effective with lasting effect (mechanical stimulation), twitch response, decrease in Sub P and calcitonin gene related peptide • Botox, steroid/lidocaine • Cautious of pneumothorax – Lift the Trapezius muscle up and inject – Rhomboides; palpate the intercostal space with fingers and inject the needle on the rib Simons DG, Travell JG, Simons LS, Travell JG. Travell & simons' myofascial pain and dysfunction : The trigger point manual. Baltimore: Williams & Wilkins; 1999.
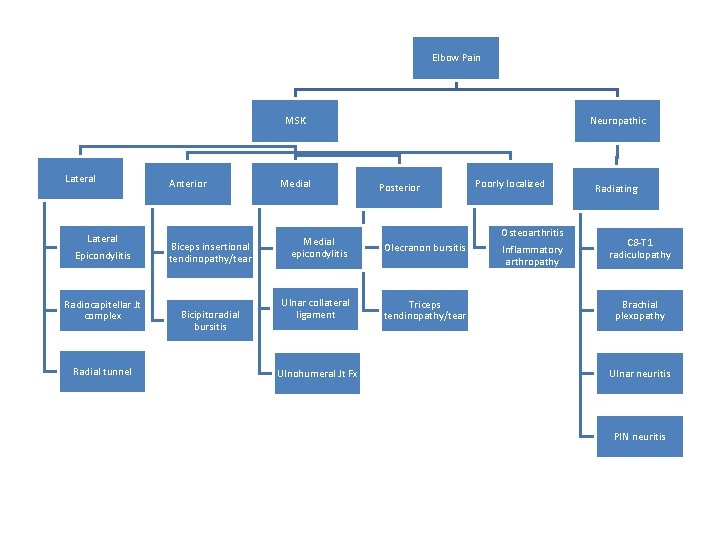
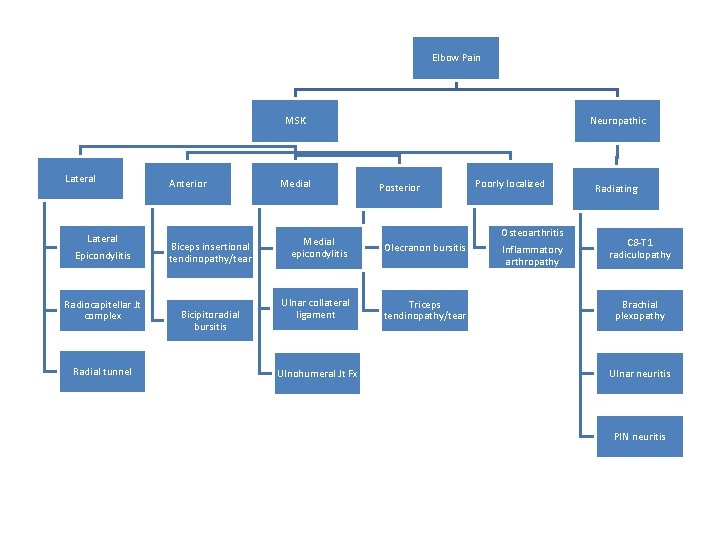
Elbow Pain MSK Lateral Epicondylitis Radiocapitellar Jt complex Radial tunnel Anterior Biceps insertional tendinopathy/tear Bicipitoradial bursitis Medial Neuropathic Posterior Medial epicondylitis Olecranon bursitis Ulnar collateral ligament Triceps tendinopathy/tear Ulnohumeral Jt Fx Poorly localized Osteoarthritis Inflammatory arthropathy Radiating C 8 -T 1 radiculopathy Brachial plexopathy Ulnar neuritis PIN neuritis
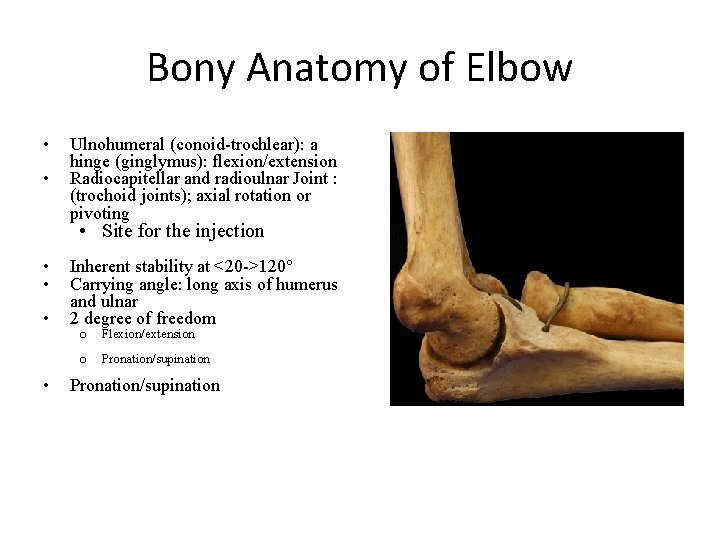
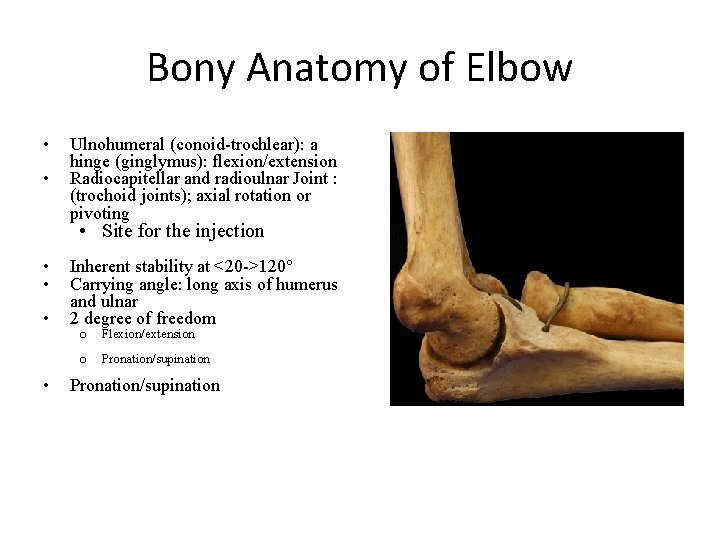
Bony Anatomy of Elbow • • Ulnohumeral (conoid-trochlear): a hinge (ginglymus): flexion/extension Radiocapitellar and radioulnar Joint : (trochoid joints); axial rotation or pivoting • Site for the injection • • Inherent stability at <20 ->120° Carrying angle: long axis of humerus and ulnar 2 degree of freedom o Flexion/extension o Pronation/supination
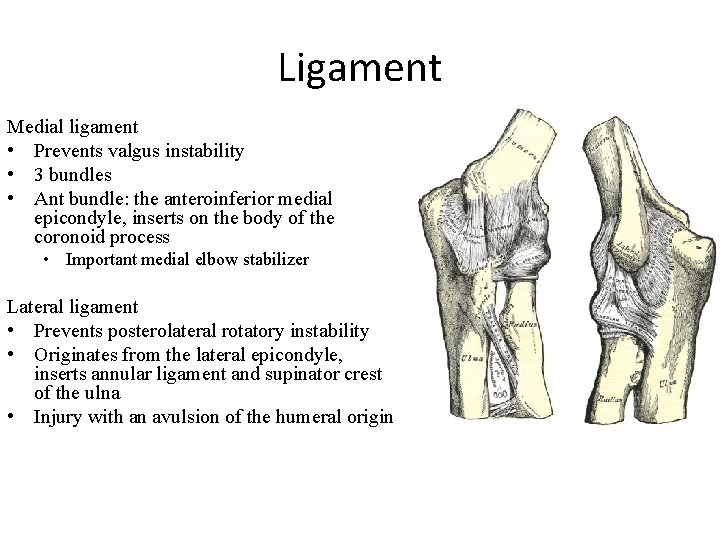
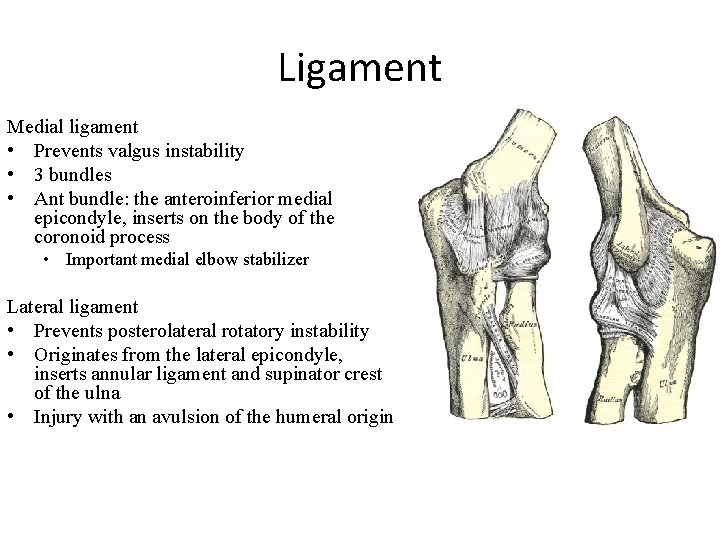
Ligament Medial ligament • Prevents valgus instability • 3 bundles • Ant bundle: the anteroinferior medial epicondyle, inserts on the body of the coronoid process • Important medial elbow stabilizer Lateral ligament • Prevents posterolateral rotatory instability • Originates from the lateral epicondyle, inserts annular ligament and supinator crest of the ulna • Injury with an avulsion of the humeral origin
Biomechanics • Weight bearing goes to ulnohumeral joint • Function ROM: 30 -130 degrees of flexion/extension • Most activities of daily living requires 100°of forearm rotation (50°of pronation & supination). • Loss of forearm pronation can be compensated to a certain extent by shoulder abduction, there are no effective mechanisms to replace supination • With passive flexion, the MCL-deficient elbow is more stable in supination, whereas the LCL-deficient elbow is more stable in pronation Bryce CD, Armstrong AD. Anatomy and biomechanics of the elbow. The Orthopedic clinics of North America. 2008; 39: 141 -154, v
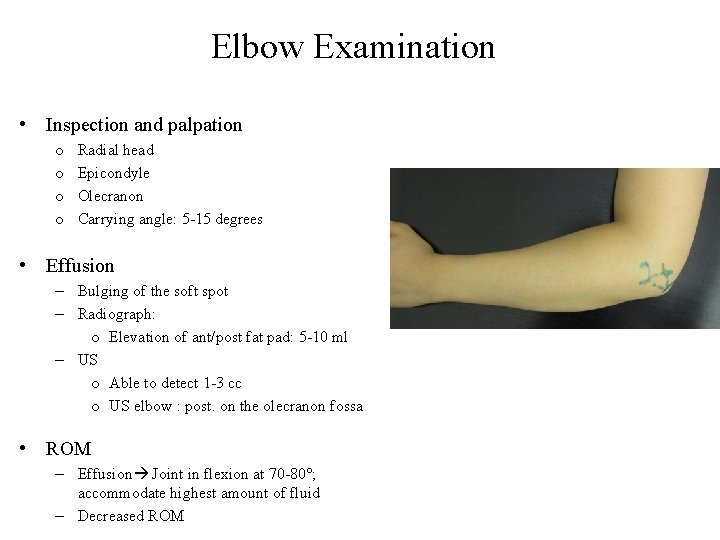
Elbow Examination • Inspection and palpation o o Radial head Epicondyle Olecranon Carrying angle: 5 -15 degrees • Effusion – Bulging of the soft spot – Radiograph: o Elevation of ant/post fat pad: 5 -10 ml – US o Able to detect 1 -3 cc o US elbow : post. on the olecranon fossa • ROM – Effusion Joint in flexion at 70 -80°; accommodate highest amount of fluid – Decreased ROM
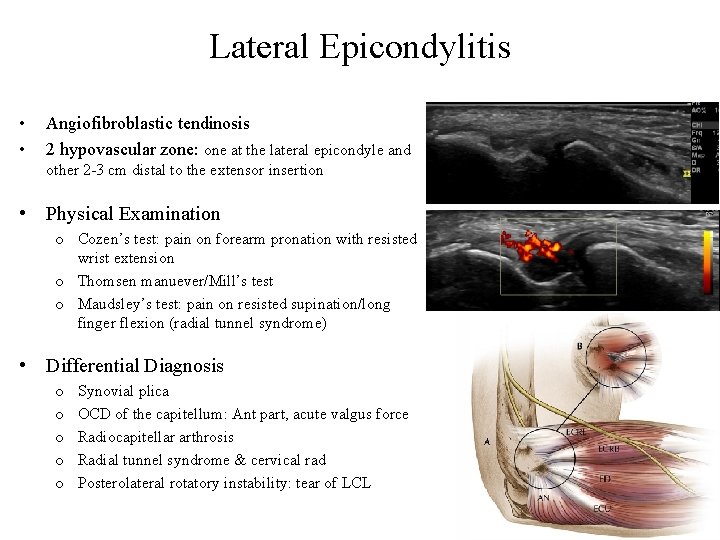
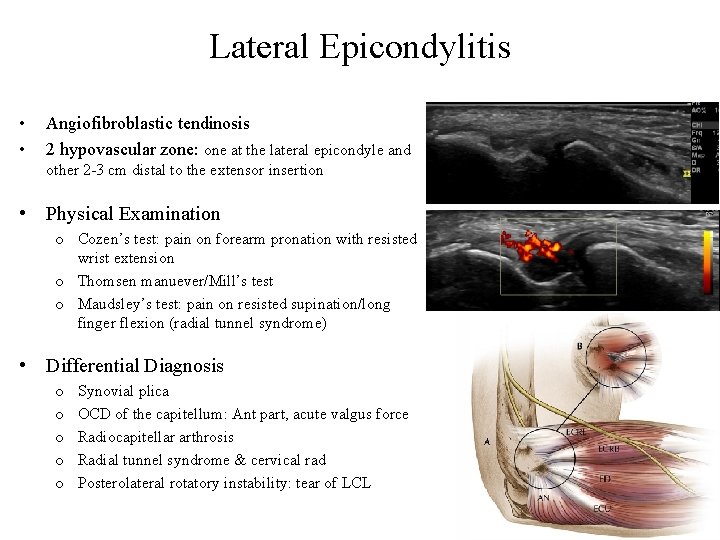
Lateral Epicondylitis • • Angiofibroblastic tendinosis 2 hypovascular zone: one at the lateral epicondyle and other 2 -3 cm distal to the extensor insertion • Physical Examination o Cozen’s test: pain on forearm pronation with resisted wrist extension o Thomsen manuever/Mill’s test o Maudsley’s test: pain on resisted supination/long finger flexion (radial tunnel syndrome) • Differential Diagnosis o o o Synovial plica OCD of the capitellum: Ant part, acute valgus force Radiocapitellar arthrosis Radial tunnel syndrome & cervical rad Posterolateral rotatory instability: tear of LCL
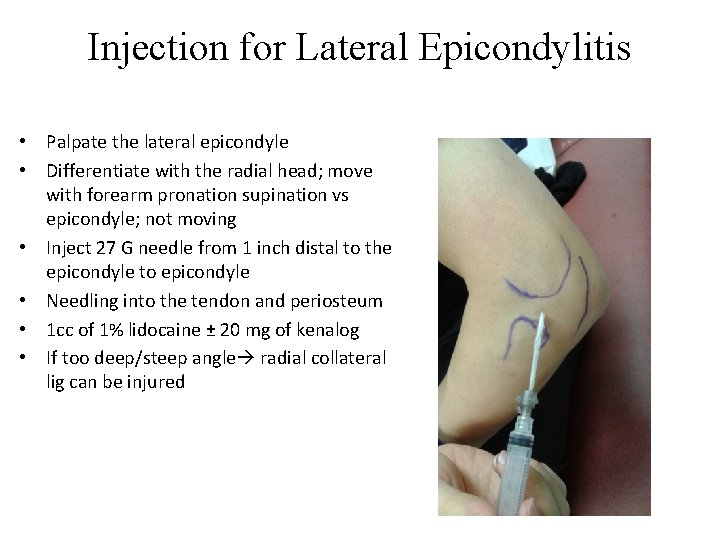
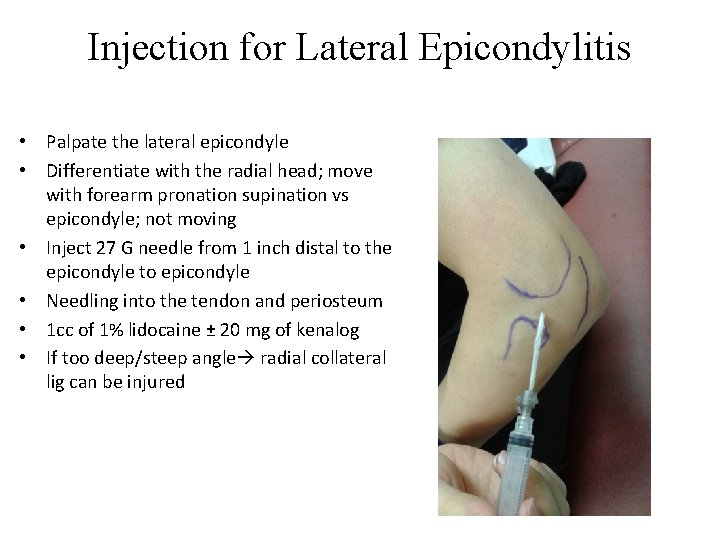
Injection for Lateral Epicondylitis • Palpate the lateral epicondyle • Differentiate with the radial head; move with forearm pronation supination vs epicondyle; not moving • Inject 27 G needle from 1 inch distal to the epicondyle to epicondyle • Needling into the tendon and periosteum • 1 cc of 1% lidocaine ± 20 mg of kenalog • If too deep/steep angle radial collateral lig can be injured
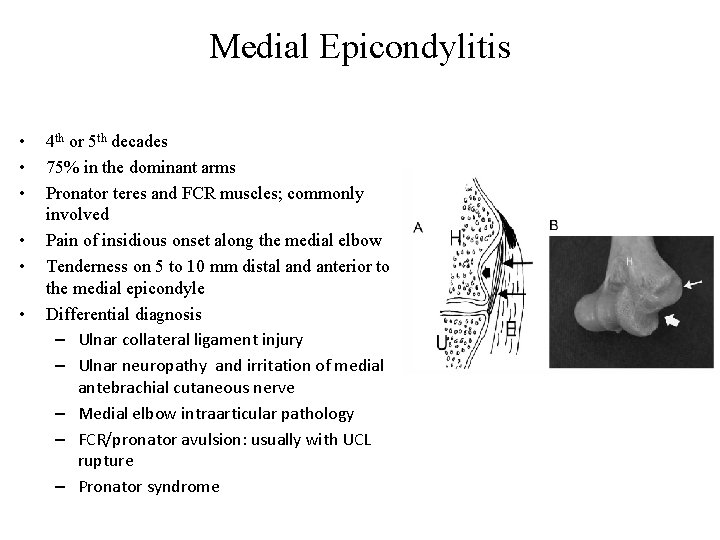
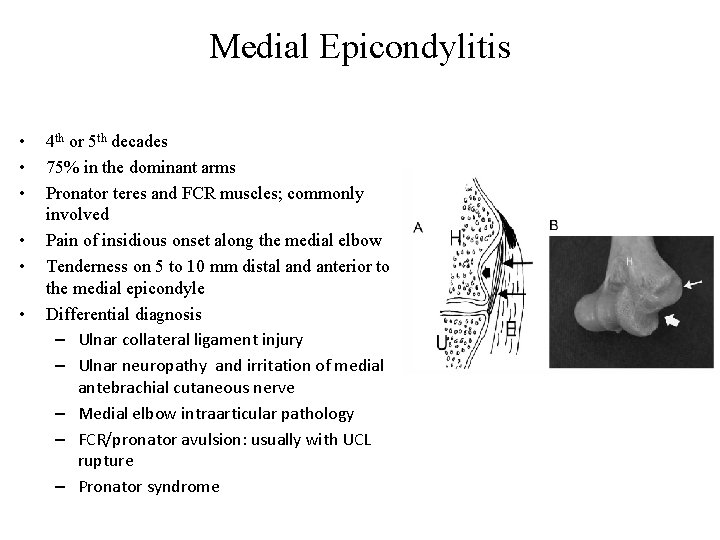
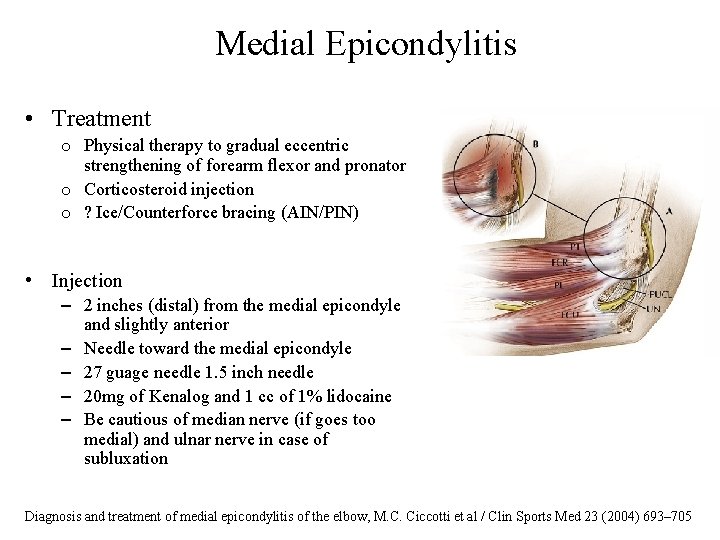
Medial Epicondylitis • • • 4 th or 5 th decades 75% in the dominant arms Pronator teres and FCR muscles; commonly involved Pain of insidious onset along the medial elbow Tenderness on 5 to 10 mm distal and anterior to the medial epicondyle Differential diagnosis – Ulnar collateral ligament injury – Ulnar neuropathy and irritation of medial antebrachial cutaneous nerve – Medial elbow intraarticular pathology – FCR/pronator avulsion: usually with UCL rupture – Pronator syndrome
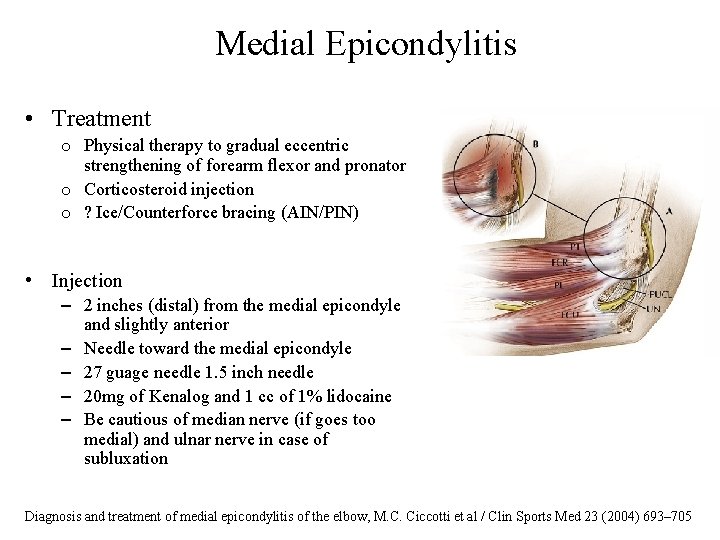
Medial Epicondylitis • Treatment o Physical therapy to gradual eccentric strengthening of forearm flexor and pronator o Corticosteroid injection o ? Ice/Counterforce bracing (AIN/PIN) • Injection – 2 inches (distal) from the medial epicondyle and slightly anterior – Needle toward the medial epicondyle – 27 guage needle 1. 5 inch needle – 20 mg of Kenalog and 1 cc of 1% lidocaine – Be cautious of median nerve (if goes too medial) and ulnar nerve in case of subluxation Diagnosis and treatment of medial epicondylitis of the elbow, M. C. Ciccotti et al / Clin Sports Med 23 (2004) 693– 705
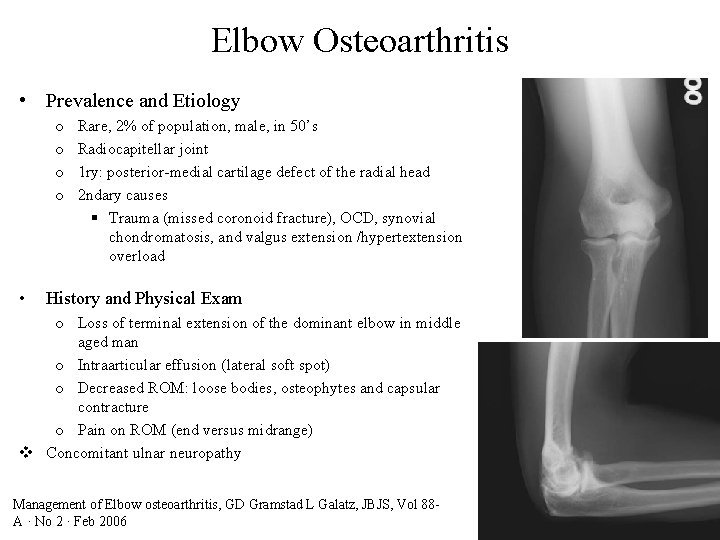
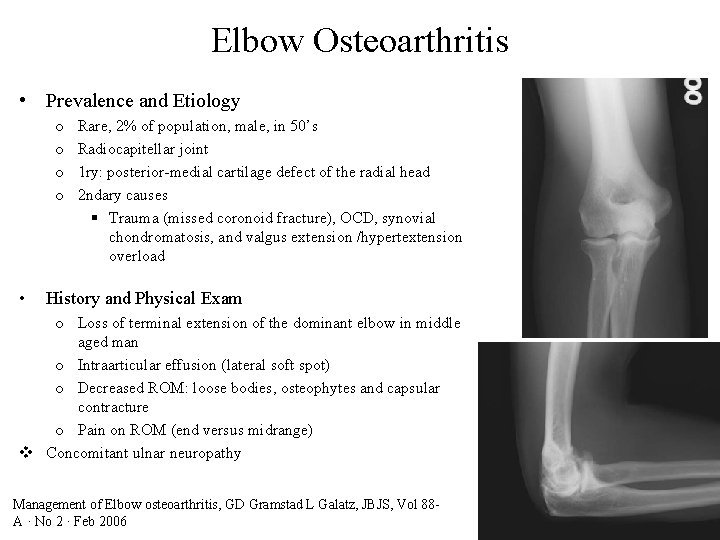
Elbow Osteoarthritis • Prevalence and Etiology o o • Rare, 2% of population, male, in 50’s Radiocapitellar joint 1 ry: posterior-medial cartilage defect of the radial head 2 ndary causes § Trauma (missed coronoid fracture), OCD, synovial chondromatosis, and valgus extension /hypertextension overload History and Physical Exam o Loss of terminal extension of the dominant elbow in middle aged man o Intraarticular effusion (lateral soft spot) o Decreased ROM: loose bodies, osteophytes and capsular contracture o Pain on ROM (end versus midrange) v Concomitant ulnar neuropathy Management of Elbow osteoarthritis, GD Gramstad L Galatz, JBJS, Vol 88 A · No 2 · Feb 2006
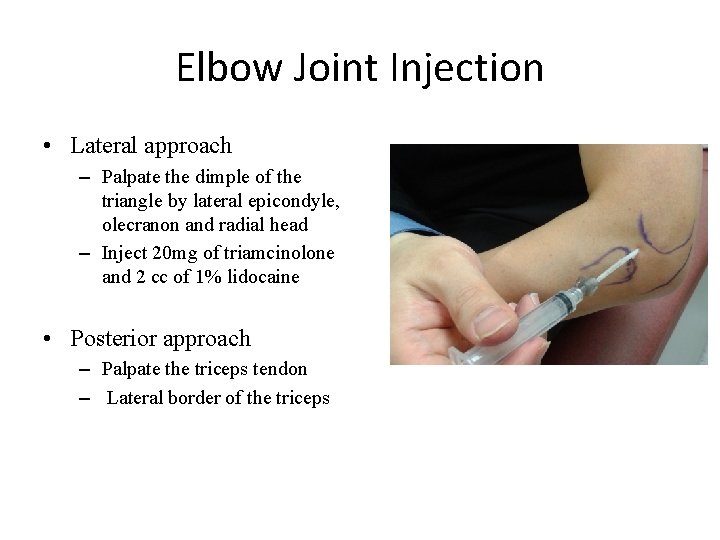
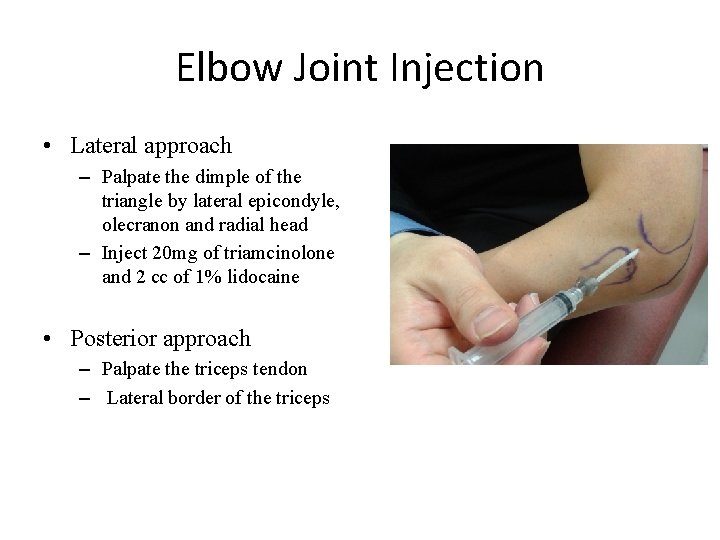
Elbow Joint Injection • Lateral approach – Palpate the dimple of the triangle by lateral epicondyle, olecranon and radial head – Inject 20 mg of triamcinolone and 2 cc of 1% lidocaine • Posterior approach – Palpate the triceps tendon – Lateral border of the triceps
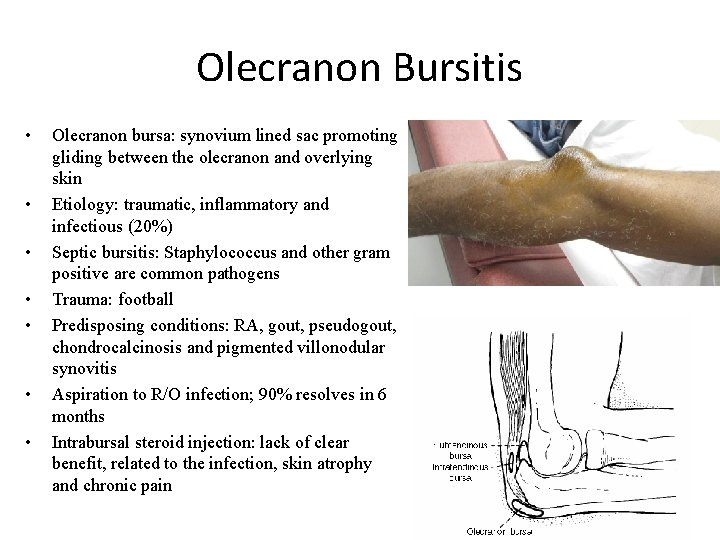
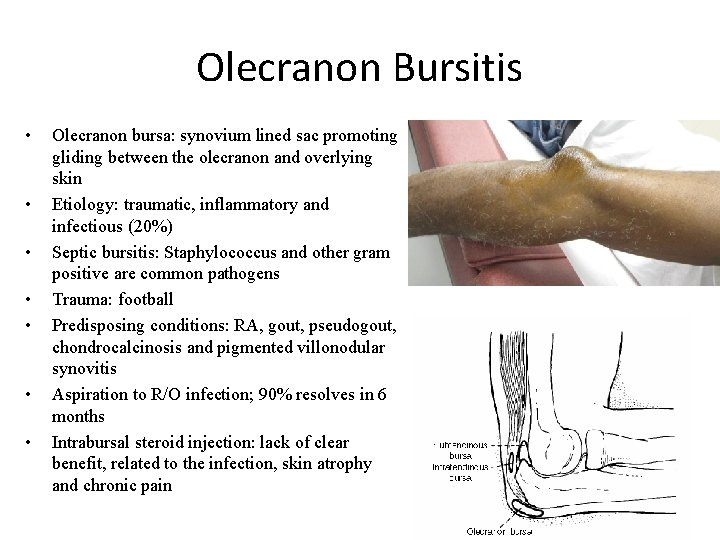
Olecranon Bursitis • • Olecranon bursa: synovium lined sac promoting gliding between the olecranon and overlying skin Etiology: traumatic, inflammatory and infectious (20%) Septic bursitis: Staphylococcus and other gram positive are common pathogens Trauma: football Predisposing conditions: RA, gout, pseudogout, chondrocalcinosis and pigmented villonodular synovitis Aspiration to R/O infection; 90% resolves in 6 months Intrabursal steroid injection: lack of clear benefit, related to the infection, skin atrophy and chronic pain
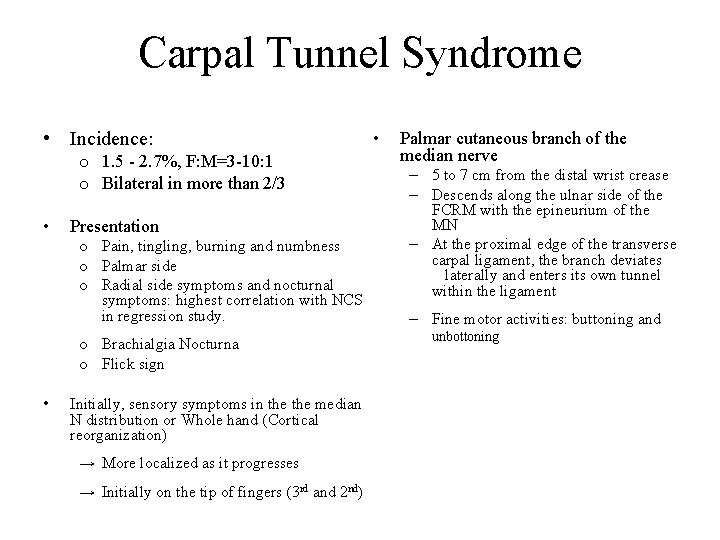
Carpal Tunnel Syndrome • Incidence: o 1. 5 - 2. 7%, F: M=3 -10: 1 o Bilateral in more than 2/3 • Presentation o Pain, tingling, burning and numbness o Palmar side o Radial side symptoms and nocturnal symptoms: highest correlation with NCS in regression study. o Brachialgia Nocturna o Flick sign • Initially, sensory symptoms in the median N distribution or Whole hand (Cortical reorganization) → More localized as it progresses → Initially on the tip of fingers (3 rd and 2 nd) • Palmar cutaneous branch of the median nerve – 5 to 7 cm from the distal wrist crease – Descends along the ulnar side of the FCRM with the epineurium of the MN – At the proximal edge of the transverse carpal ligament, the branch deviates laterally and enters its own tunnel within the ligament – Fine motor activities: buttoning and unbottoning
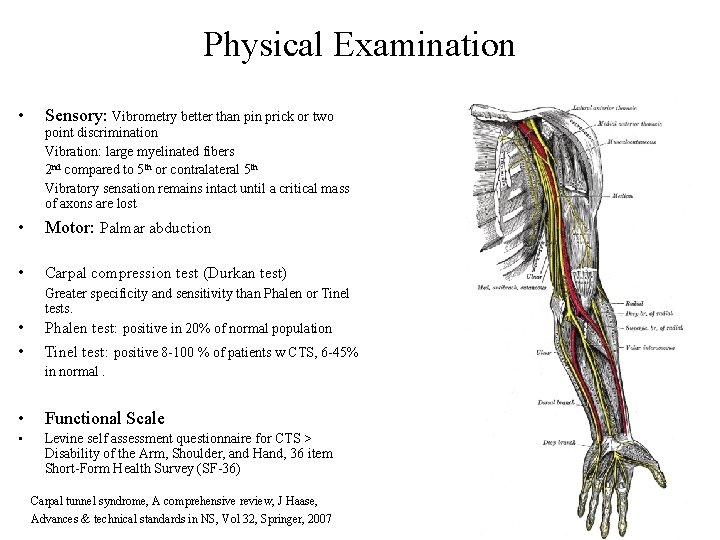
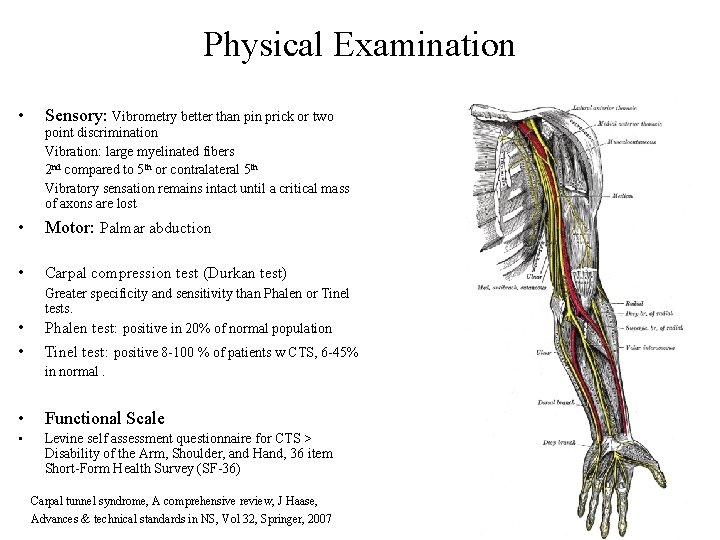
Physical Examination • Sensory: Vibrometry better than pin prick or two • Motor: Palmar abduction • Carpal compression test (Durkan test) point discrimination Vibration: large myelinated fibers 2 nd compared to 5 th or contralateral 5 th Vibratory sensation remains intact until a critical mass of axons are lost Greater specificity and sensitivity than Phalen or Tinel tests. • Phalen test: positive in 20% of normal population • Tinel test: positive 8 -100 % of patients w CTS, 6 -45% • Functional Scale • Levine self assessment questionnaire for CTS > Disability of the Arm, Shoulder, and Hand, 36 item Short-Form Health Survey (SF-36) in normal. Carpal tunnel syndrome, A comprehensive review, J Haase, Advances & technical standards in NS, Vol 32, Springer, 2007
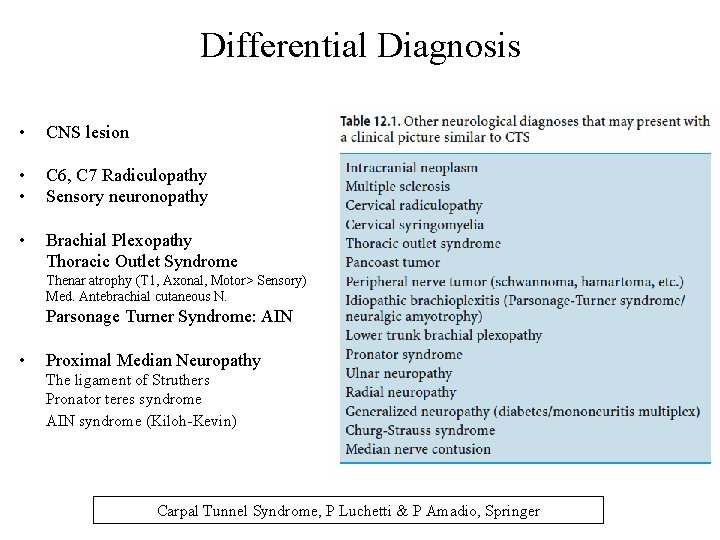
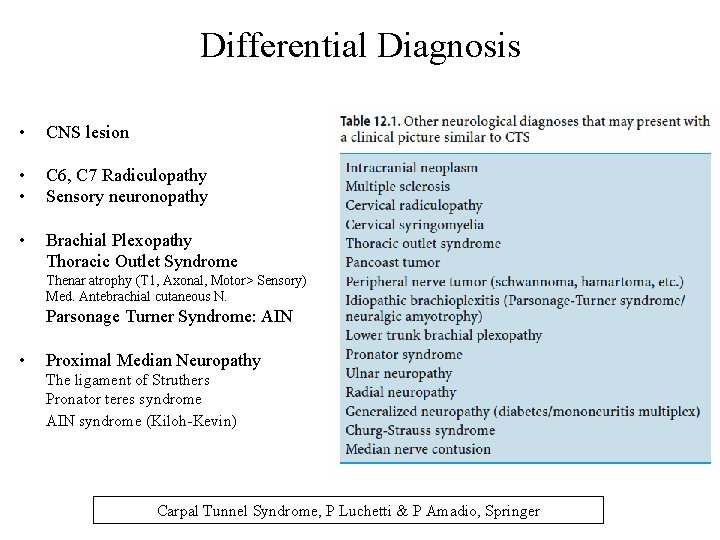
Differential Diagnosis • CNS lesion • • C 6, C 7 Radiculopathy Sensory neuronopathy • Brachial Plexopathy Thoracic Outlet Syndrome Thenar atrophy (T 1, Axonal, Motor> Sensory) Med. Antebrachial cutaneous N. Parsonage Turner Syndrome: AIN • Proximal Median Neuropathy The ligament of Struthers Pronator teres syndrome AIN syndrome (Kiloh-Kevin) Carpal Tunnel Syndrome, P Luchetti & P Amadio, Springer
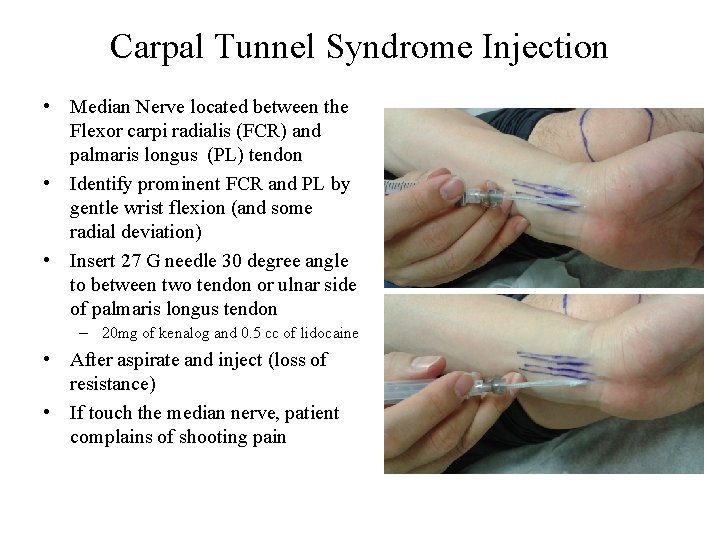
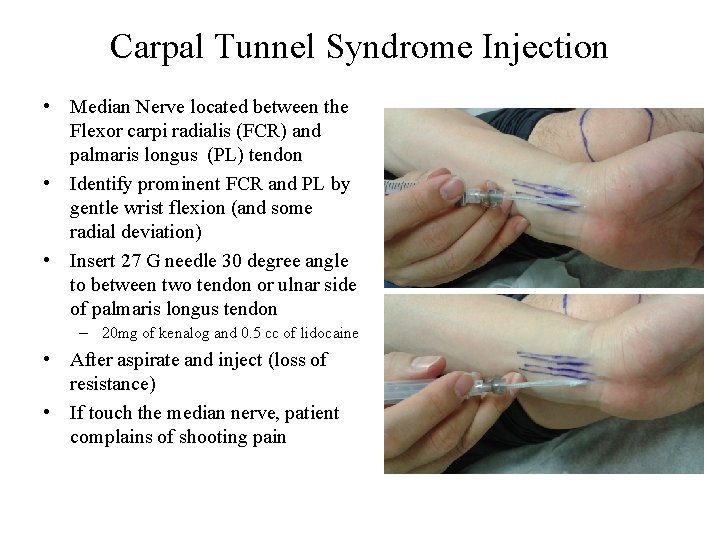
Carpal Tunnel Syndrome Injection • Median Nerve located between the Flexor carpi radialis (FCR) and palmaris longus (PL) tendon • Identify prominent FCR and PL by gentle wrist flexion (and some radial deviation) • Insert 27 G needle 30 degree angle to between two tendon or ulnar side of palmaris longus tendon – 20 mg of kenalog and 0. 5 cc of lidocaine • After aspirate and inject (loss of resistance) • If touch the median nerve, patient complains of shooting pain
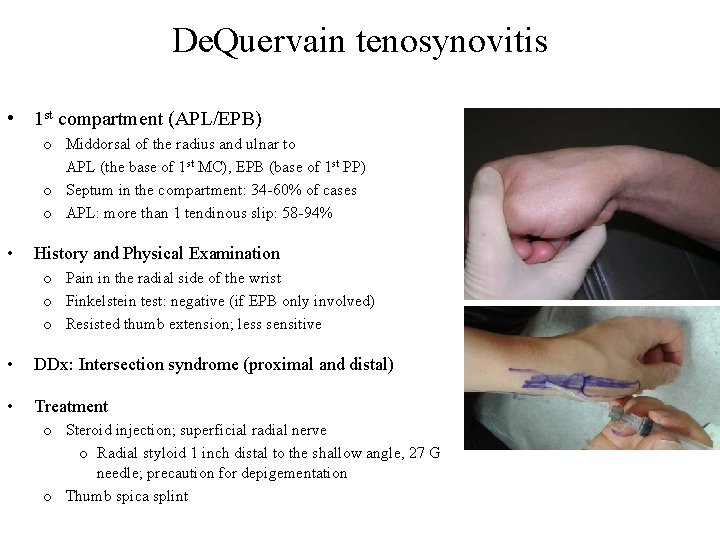
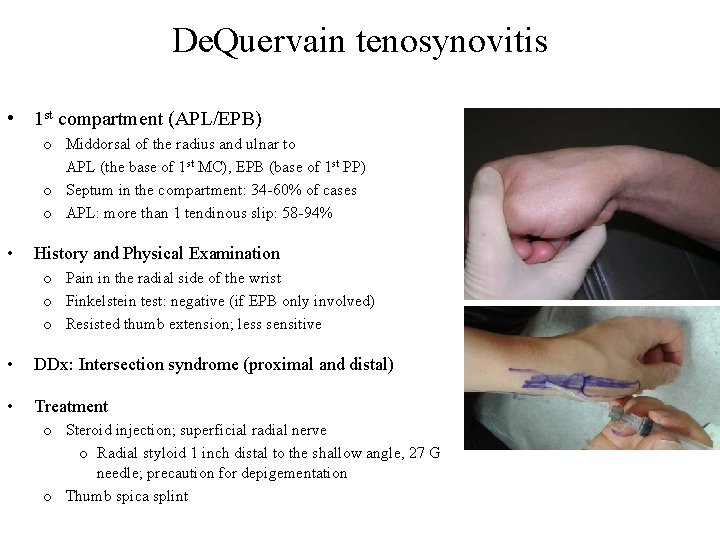
De. Quervain tenosynovitis • 1 st compartment (APL/EPB) o Middorsal of the radius and ulnar to APL (the base of 1 st MC), EPB (base of 1 st PP) o Septum in the compartment: 34 -60% of cases o APL: more than 1 tendinous slip: 58 -94% • History and Physical Examination o Pain in the radial side of the wrist o Finkelstein test: negative (if EPB only involved) o Resisted thumb extension; less sensitive • DDx: Intersection syndrome (proximal and distal) • Treatment o Steroid injection; superficial radial nerve o Radial styloid 1 inch distal to the shallow angle, 27 G needle; precaution for depigementation o Thumb spica splint
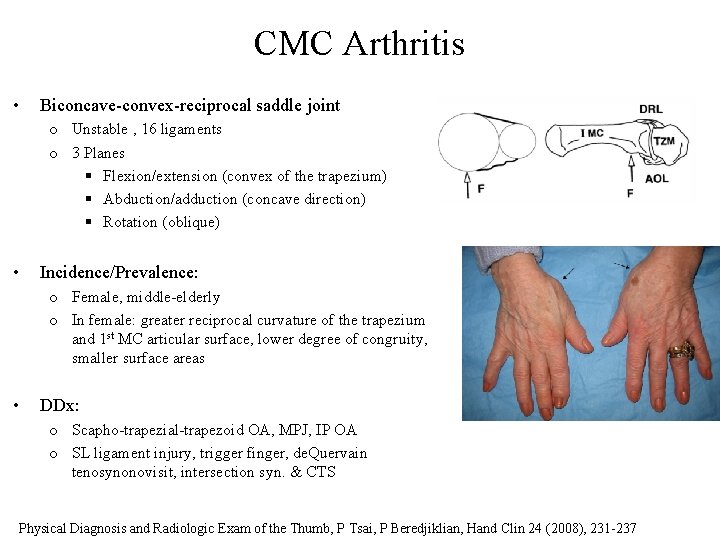
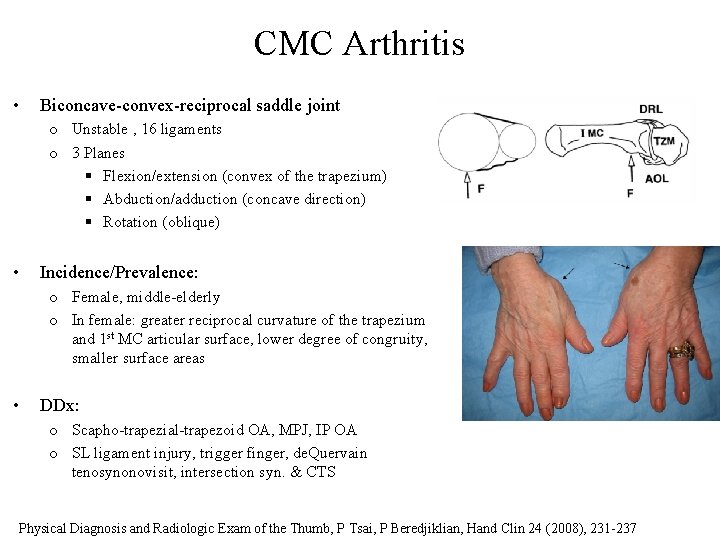
CMC Arthritis • Biconcave-convex-reciprocal saddle joint o Unstable , 16 ligaments o 3 Planes § Flexion/extension (convex of the trapezium) § Abduction/adduction (concave direction) § Rotation (oblique) • Incidence/Prevalence: o Female, middle-elderly o In female: greater reciprocal curvature of the trapezium and 1 st MC articular surface, lower degree of congruity, smaller surface areas • DDx: o Scapho-trapezial-trapezoid OA, MPJ, IP OA o SL ligament injury, trigger finger, de. Quervain tenosynonovisit, intersection syn. & CTS Physical Diagnosis and Radiologic Exam of the Thumb, P Tsai, P Beredjiklian, Hand Clin 24 (2008), 231 -237
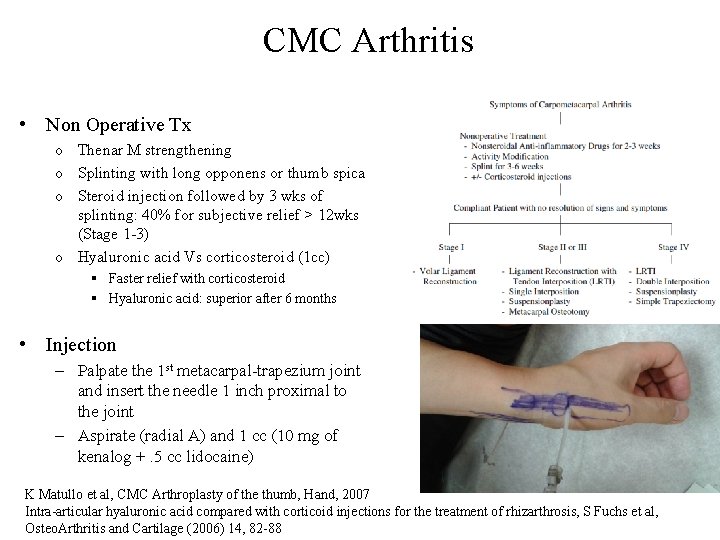
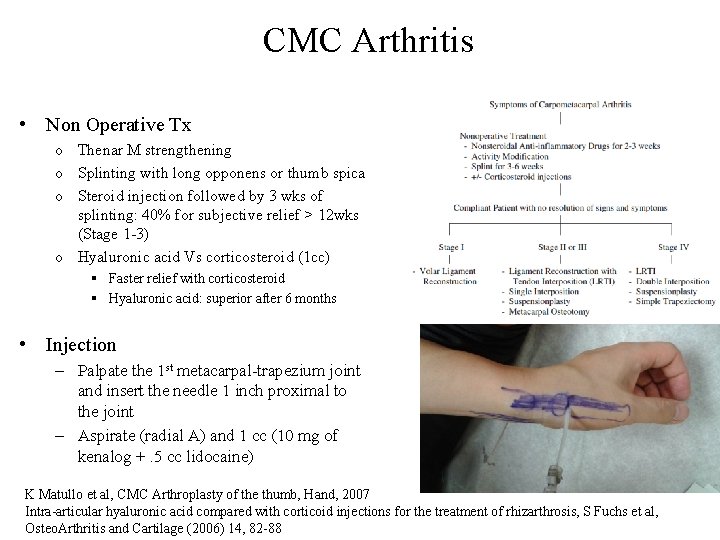
CMC Arthritis • Non Operative Tx o Thenar M strengthening o Splinting with long opponens or thumb spica o Steroid injection followed by 3 wks of splinting: 40% for subjective relief > 12 wks (Stage 1 -3) o Hyaluronic acid Vs corticosteroid (1 cc) § Faster relief with corticosteroid § Hyaluronic acid: superior after 6 months • Injection – Palpate the 1 st metacarpal-trapezium joint and insert the needle 1 inch proximal to the joint – Aspirate (radial A) and 1 cc (10 mg of kenalog +. 5 cc lidocaine) K Matullo et al, CMC Arthroplasty of the thumb, Hand, 2007 Intra-articular hyaluronic acid compared with corticoid injections for the treatment of rhizarthrosis, S Fuchs et al, Osteo. Arthritis and Cartilage (2006) 14, 82 -88