Come ventilare il paziente ipossiemico acuto Andrea Vianello

- Slides: 48
Come ventilare il paziente ipossiemico acuto Andrea Vianello Fisiopatologia e Terapia Intensiva Respiratoria Ospedale – Università di Padova
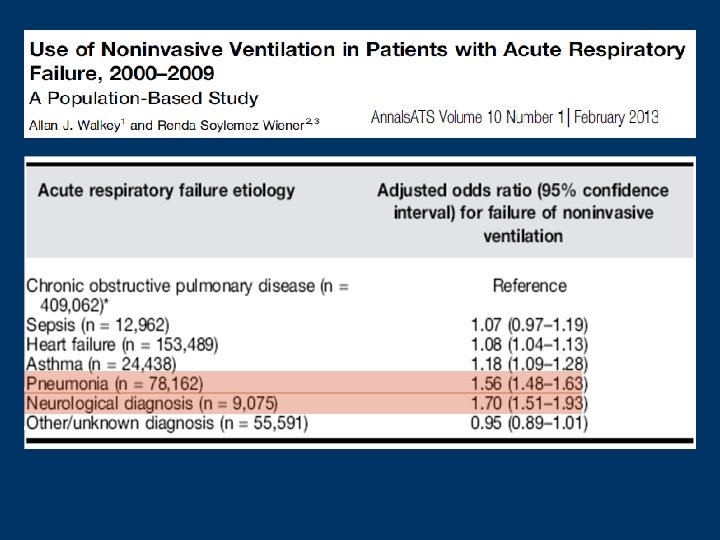
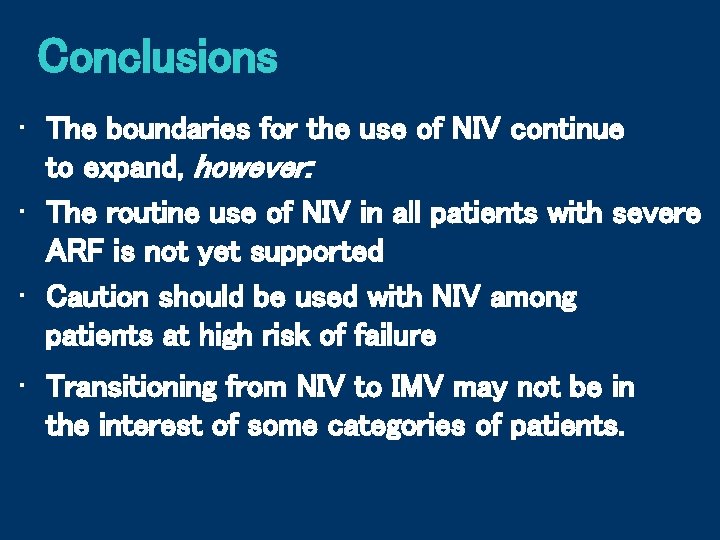
Non-Invasive Ventilation has demonstrated good efficacy in reducing risk of intubation and mortality; however, some potential etiologies of acute respiratory failure associated with a high risk of NIV failure, which may lead to great hospital mortality. Walkey AJ. Annals ATS 2013; 10: 10 -7
Talking about NIV failure: 1. Epidemiology & Aetiology 2. Remedies to avoid failure 3. Transition to IMV: dancing in the dark
Rate of NIV failure is extremely different according to study design, severity of illness and level of monitoring
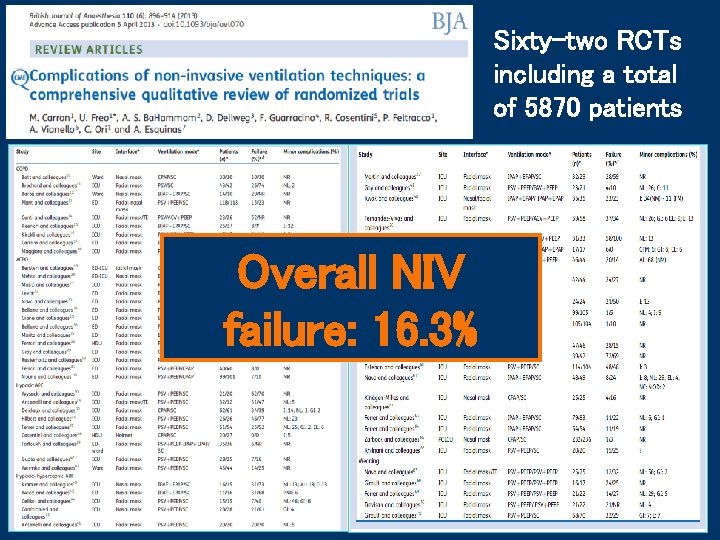
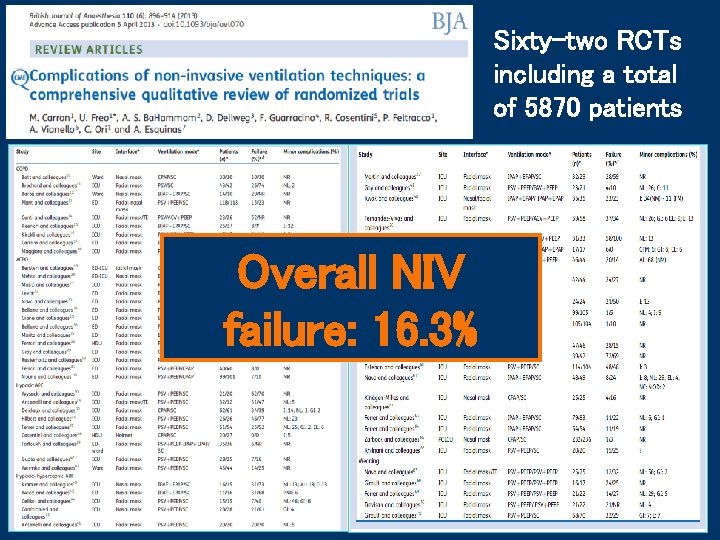
Sixty-two RCTs including a total of 5870 patients Overall NIV failure: 16. 3%
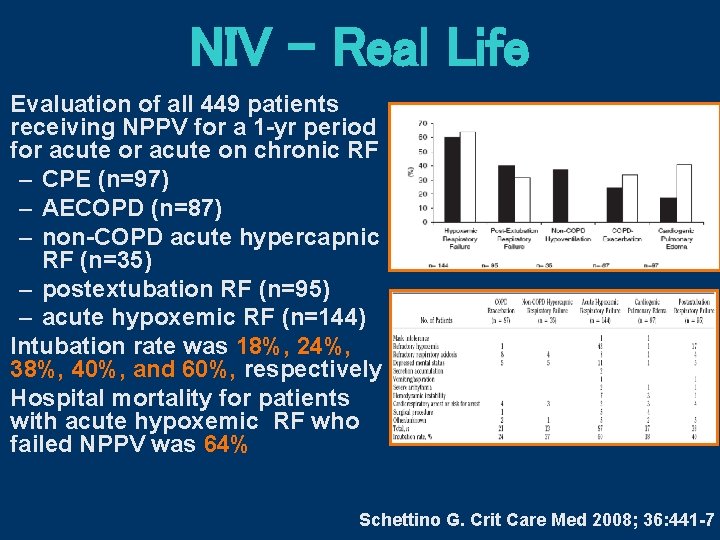
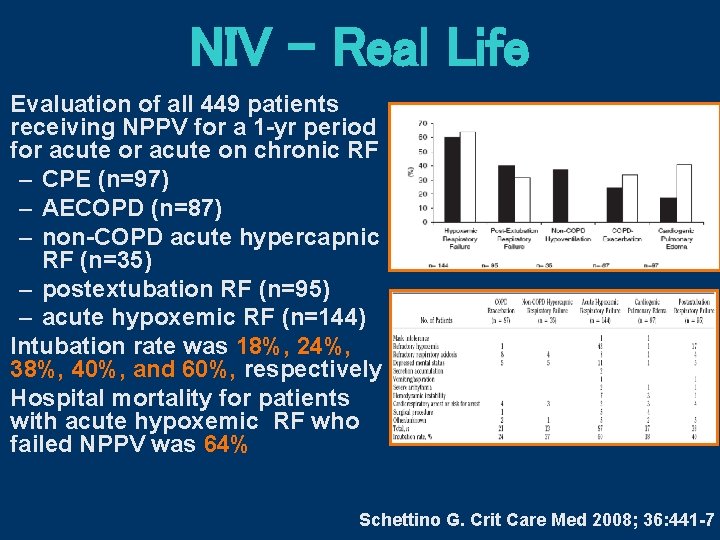
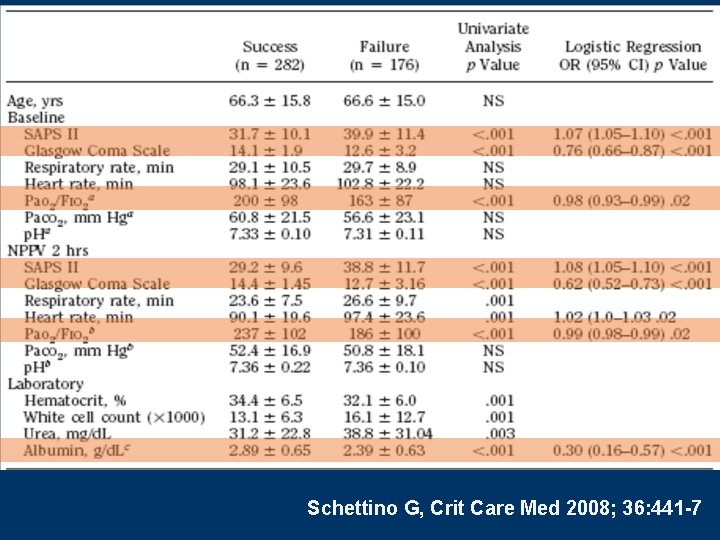
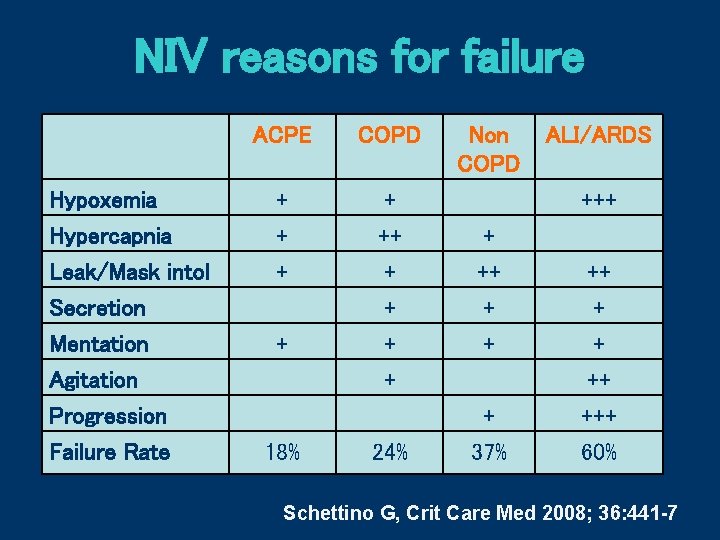
NIV – Real Life Evaluation of all 449 patients receiving NPPV for a 1 -yr period for acute on chronic RF – CPE (n=97) – AECOPD (n=87) – non-COPD acute hypercapnic RF (n=35) – postextubation RF (n=95) – acute hypoxemic RF (n=144) Intubation rate was 18%, 24%, 38%, 40%, and 60%, respectively Hospital mortality for patients with acute hypoxemic RF who failed NPPV was 64% Schettino G. Crit Care Med 2008; 36: 441 -7
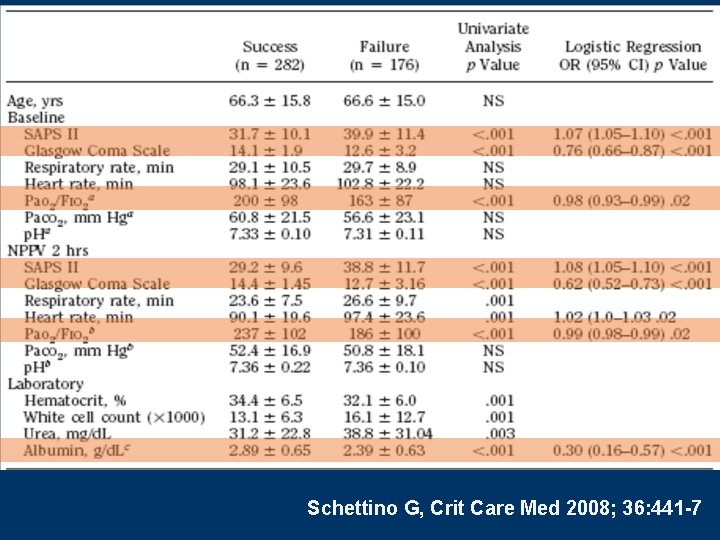
Schettino G, Crit Care Med 2008; 36: 441 -7
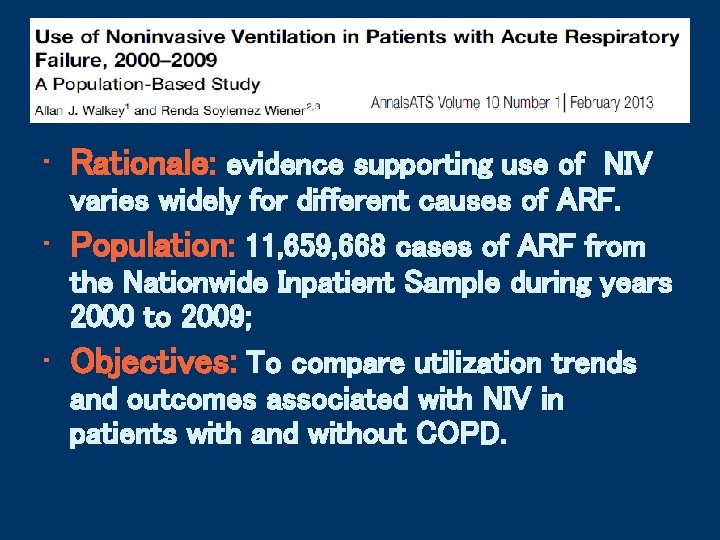
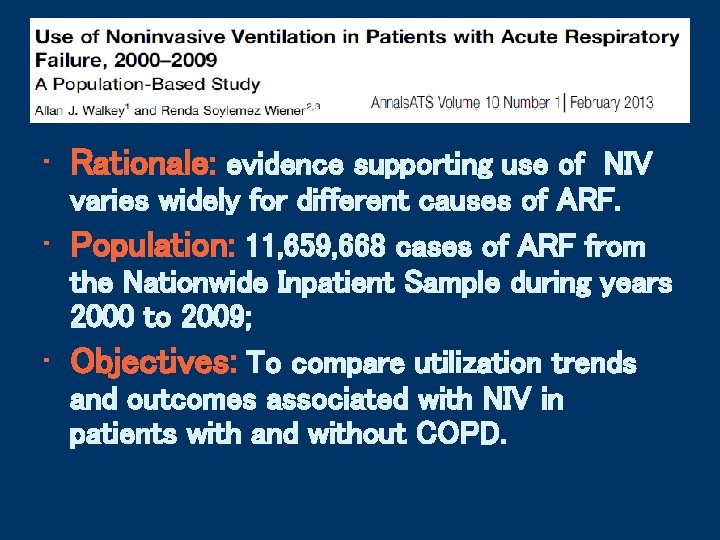
Epidemiology • Rationale: evidence supporting use of NIV varies widely for different causes of ARF. • Population: 11, 659, 668 cases of ARF from the Nationwide Inpatient Sample during years 2000 to 2009; • Objectives: To compare utilization trends and outcomes associated with NIV in patients with and without COPD.
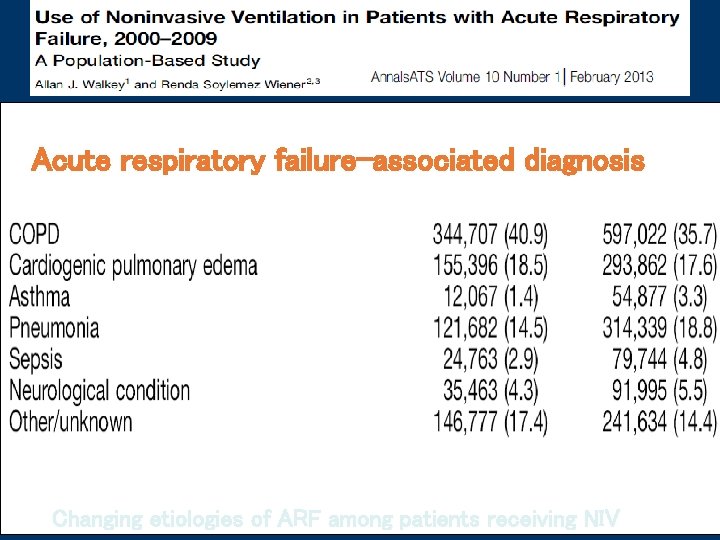
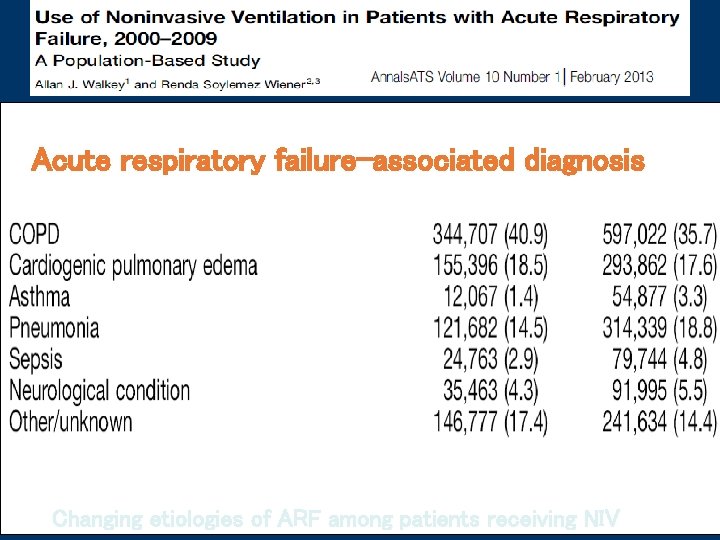
Acute respiratory failure-associated diagnosis Changing etiologies of ARF among patients receiving NIV
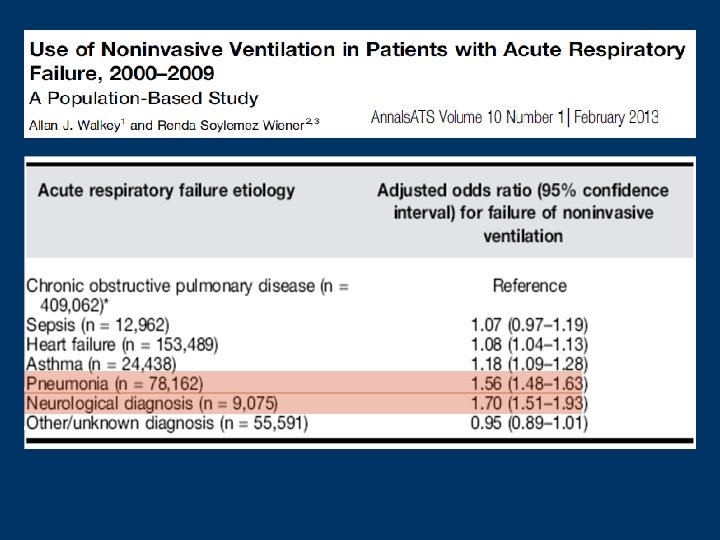
• 20% of patients without a COPD diagnosis who received NIV IMV; • 13. 4% of patients with COPD who received NIV IMV; • Patients experiencing NIV failure before transition to IMV had greater hospital mortality than those initially on IMV
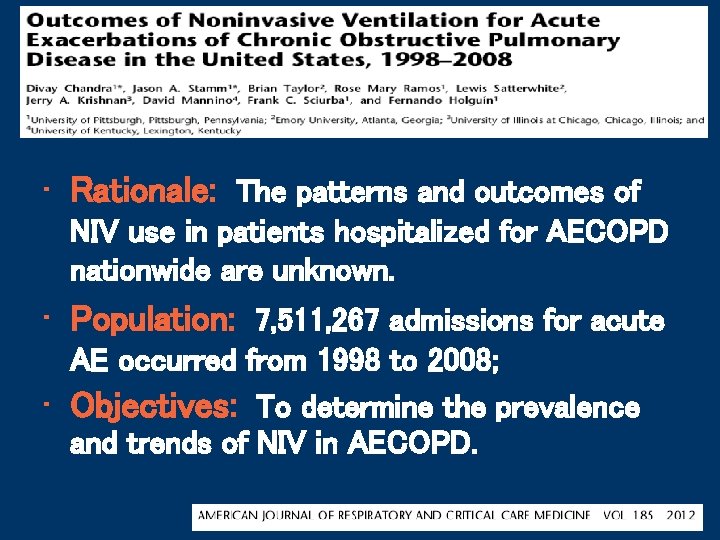
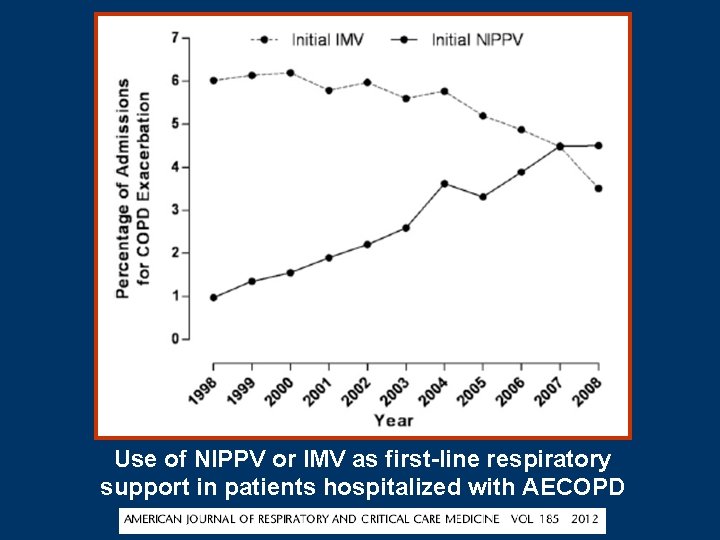
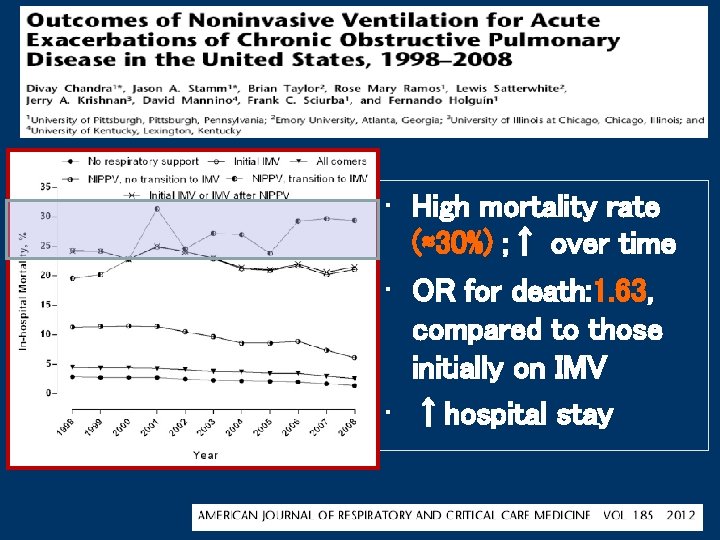
• Rationale: The patterns and outcomes of NIV use in patients hospitalized for AECOPD nationwide are unknown. • Population: 7, 511, 267 admissions for acute AE occurred from 1998 to 2008; • Objectives: To determine the prevalence and trends of NIV in AECOPD.
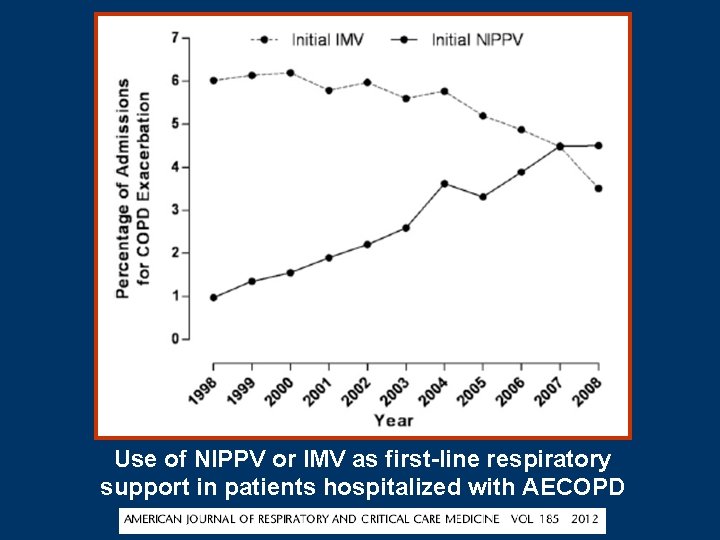
Use of NIPPV or IMV as first-line respiratory support in patients hospitalized with AECOPD
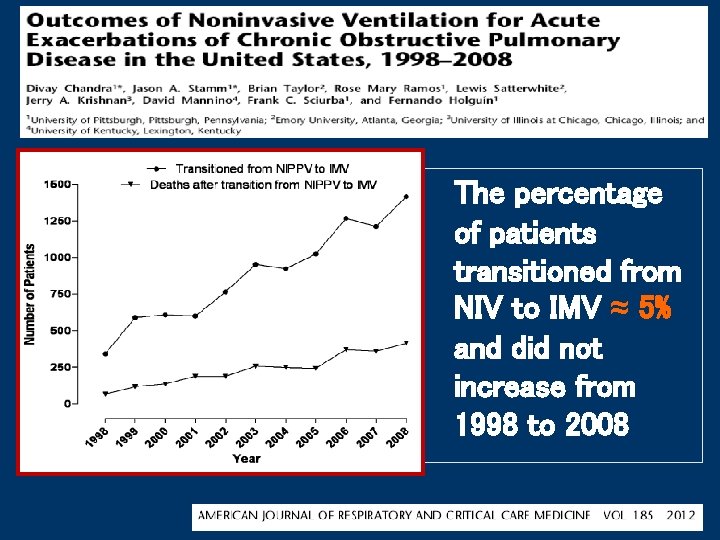
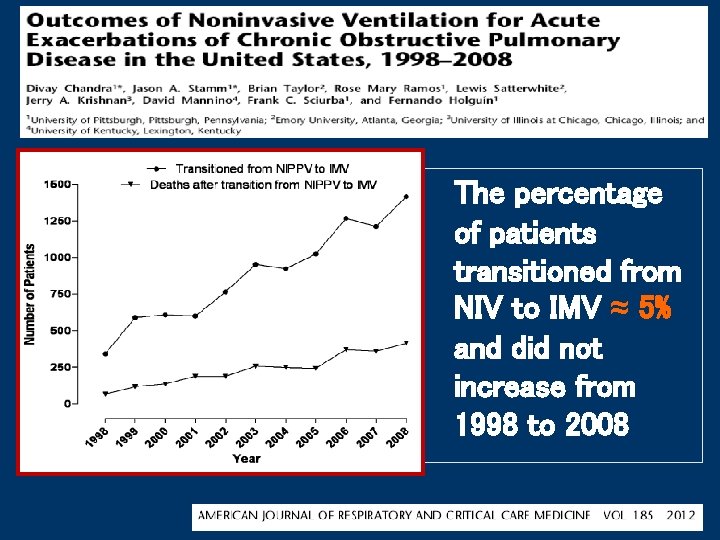
The percentage of patients transitioned from NIV to IMV ≈ 5% and did not increase from 1998 to 2008
Reasons for low rate of IMV use after NPPV, compared to clinical trial: • End of life decision to not accept IMV • Patients died before IMV could be started • Good selection of appropriate patients
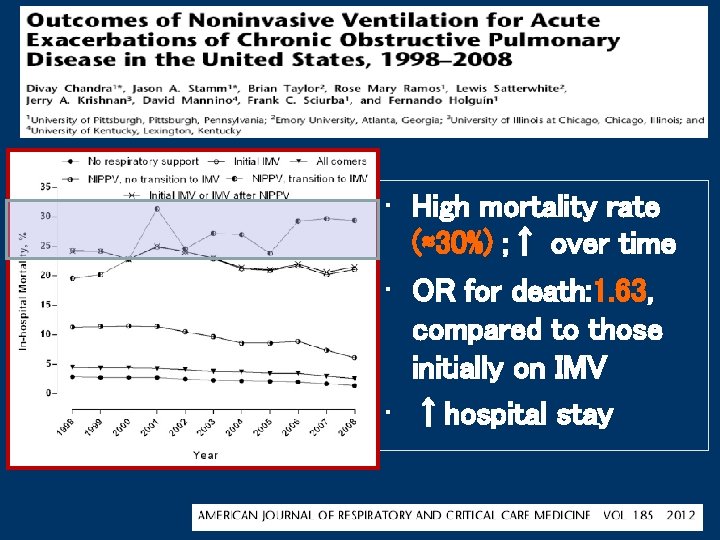
• High mortality rate (≈30%) ; ↑ over time • OR for death: 1. 63, compared to those initially on IMV • ↑hospital stay
Reasons for high mortality rate in patients transitioned to IMV • Increased use of NIPPV in patients difficult to ventilate? • Continuation of NIPPV despite a lack of early improvement?
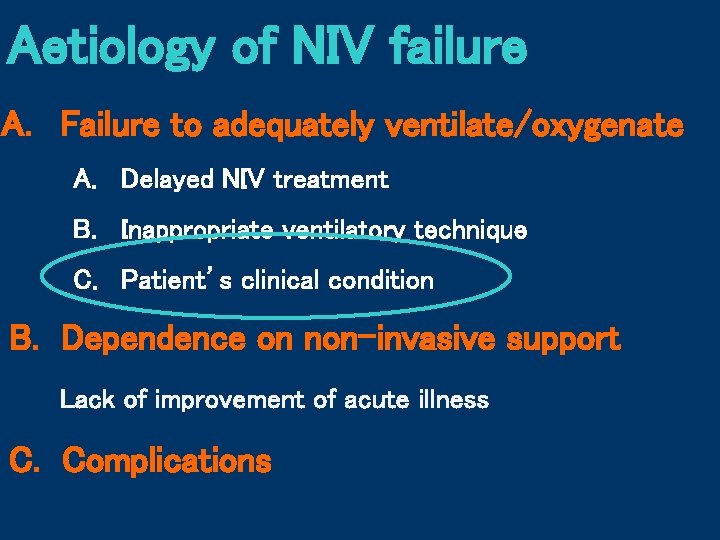
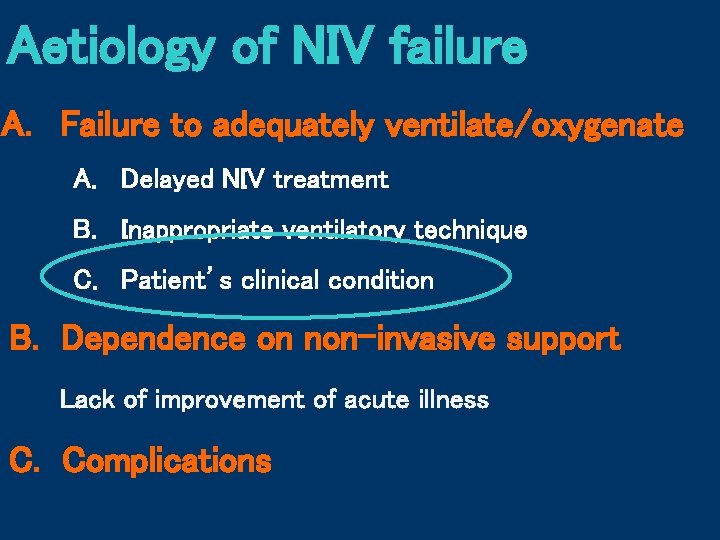
Aetiology of NIV failure A. Failure to adequately ventilate/oxygenate A. Delayed NIV treatment B. Inappropriate ventilatory technique C. Patient’s clinical condition B. Dependence on non-invasive support Lack of improvement of acute illness C. Complications
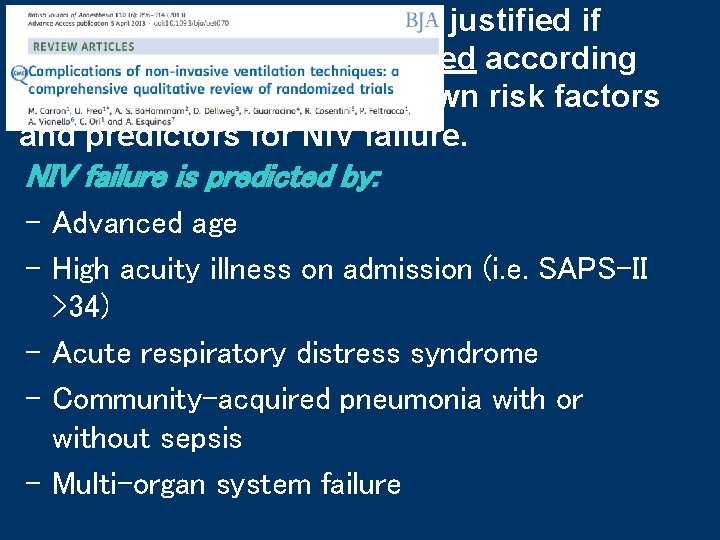
NIV trial in hypoxemic RF is justified if patients are carefully selected according to available guidelines, known risk factors and predictors for NIV failure is predicted by: - Advanced age - High acuity illness on admission (i. e. SAPS-II >34) - Acute respiratory distress syndrome - Community-acquired pneumonia with or without sepsis - Multi-organ system failure
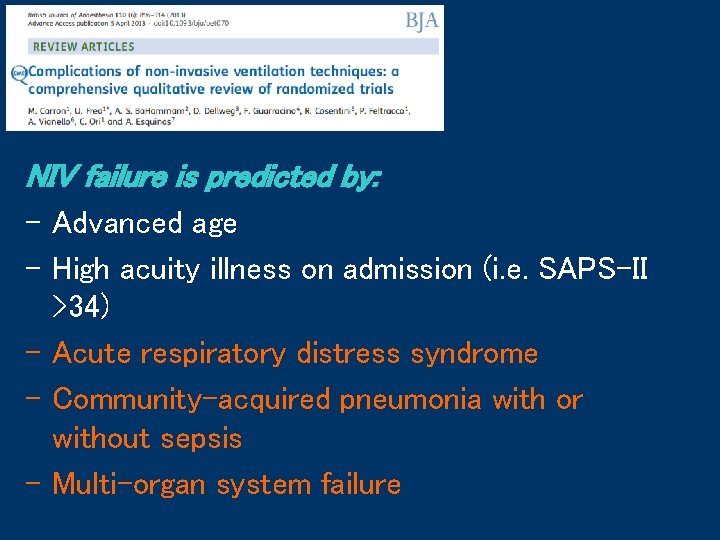
NIV failure is predicted by: - Advanced age - High acuity illness on admission (i. e. SAPS-II >34) - Acute respiratory distress syndrome - Community-acquired pneumonia with or without sepsis - Multi-organ system failure

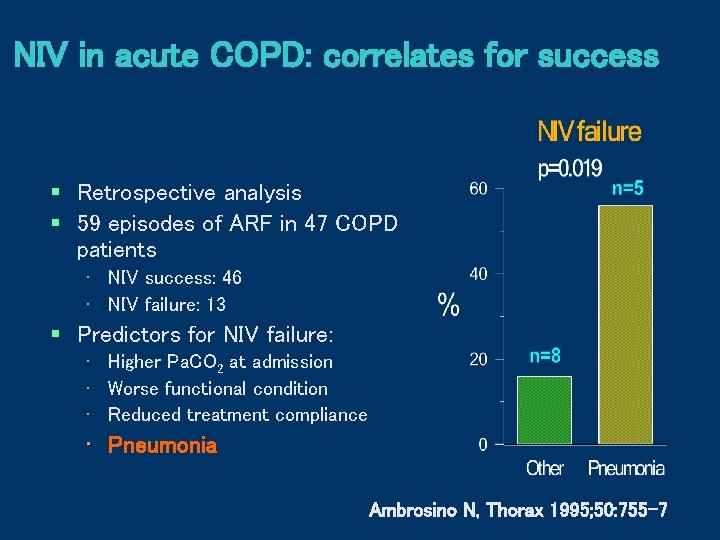
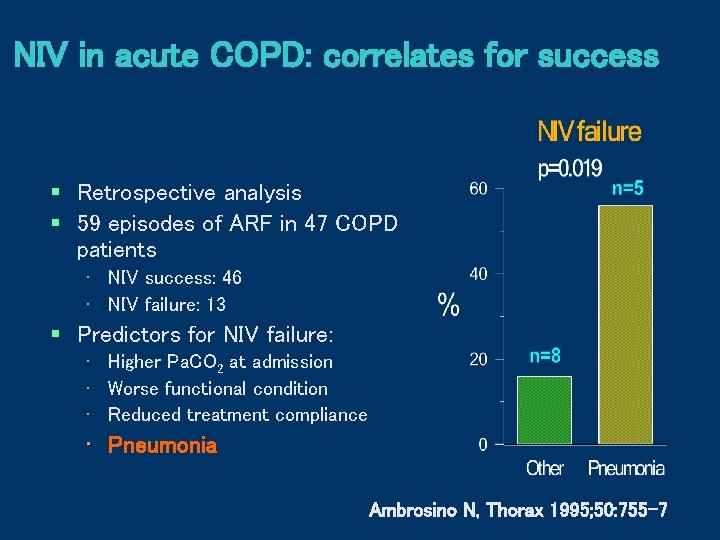
NIV in acute COPD: correlates for success § Retrospective analysis § 59 episodes of ARF in 47 COPD patients • NIV success: 46 • NIV failure: 13 § Predictors for NIV failure: • Higher Pa. CO 2 at admission • Worse functional condition • Reduced treatment compliance • Pneumonia Ambrosino N, Thorax 1995; 50: 755 -7
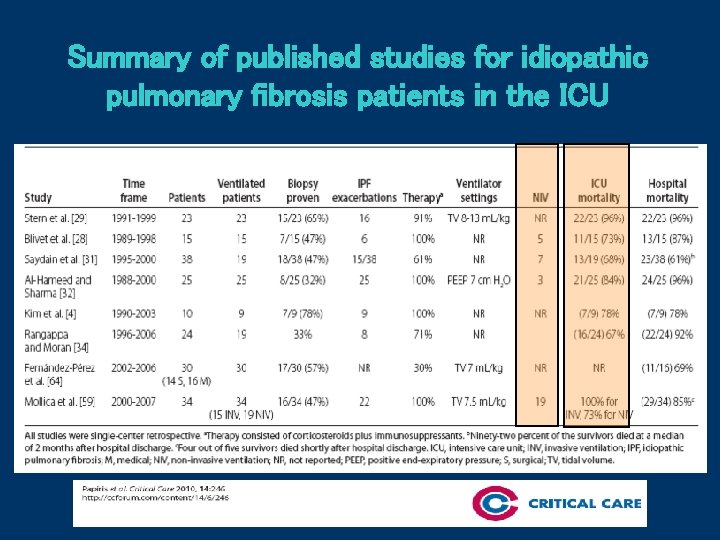
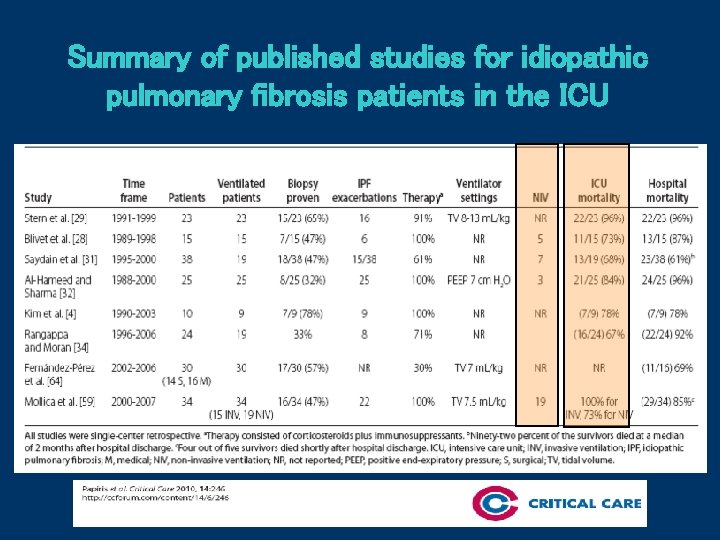
Summary of published studies for idiopathic pulmonary fibrosis patients in the ICU
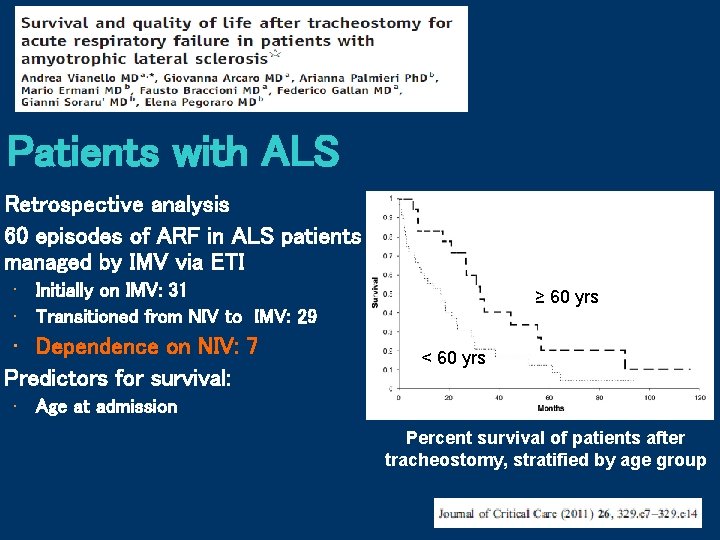
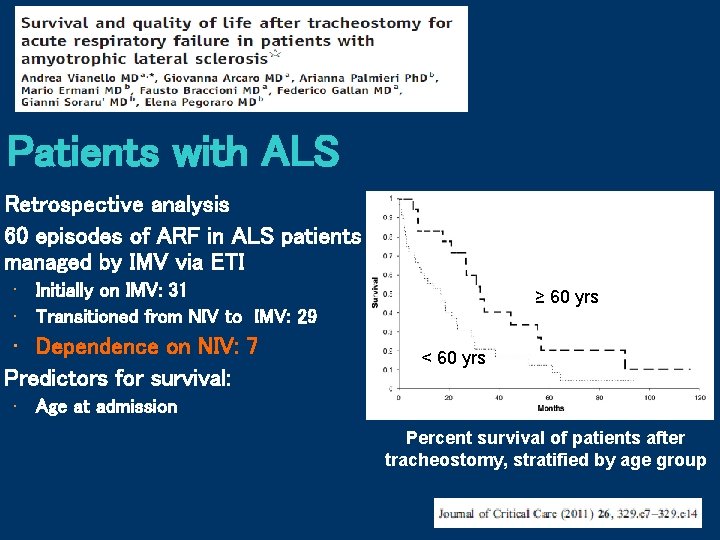
Patients with ALS Retrospective analysis 60 episodes of ARF in ALS patients managed by IMV via ETI • Initially on IMV: 31 • Transitioned from NIV to IMV: 29 • Dependence on NIV: 7 Predictors for survival: ≥ 60 yrs < 60 yrs • Age at admission Percent survival of patients after tracheostomy, stratified by age group
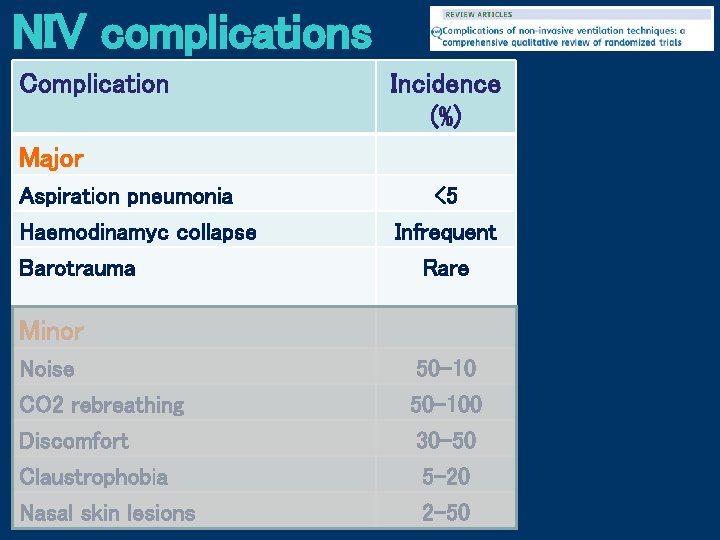
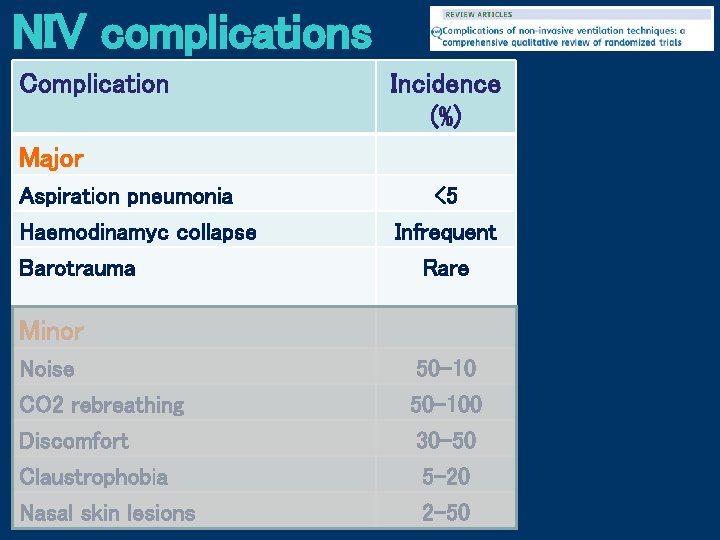
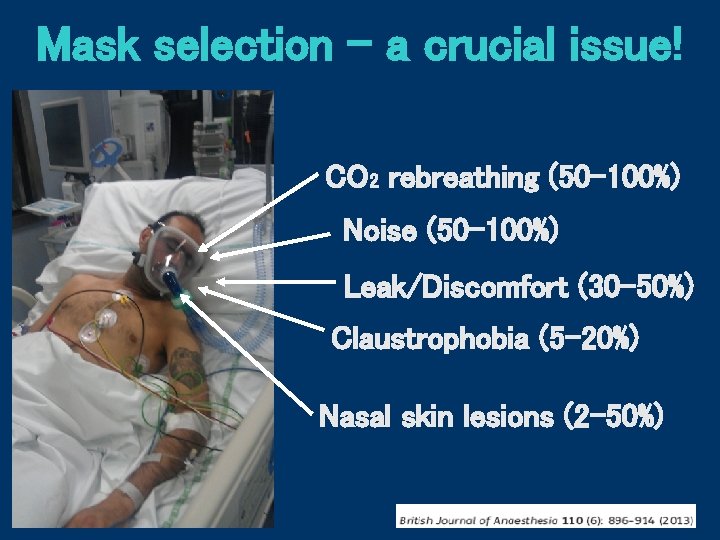
NIV complications Complication Incidence (%) Major Aspiration pneumonia Haemodinamyc collapse Barotrauma <5 Infrequent Rare Minor Noise CO 2 rebreathing Discomfort Claustrophobia Nasal skin lesions 50 -100 30 -50 5 -20 2 -50
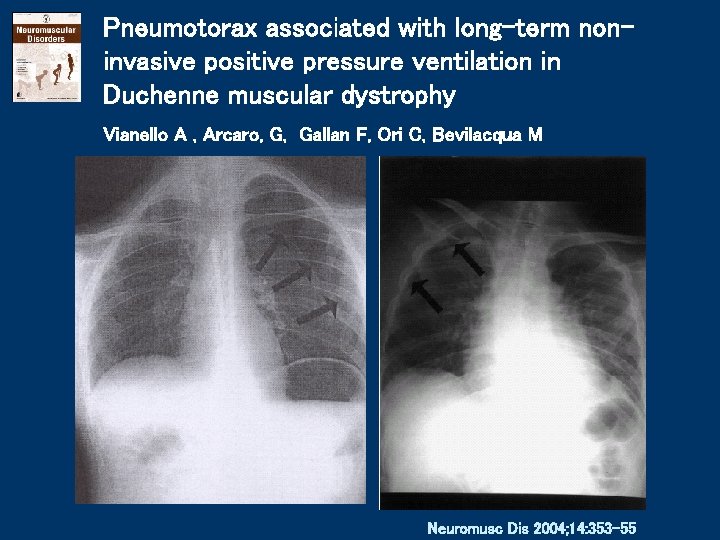
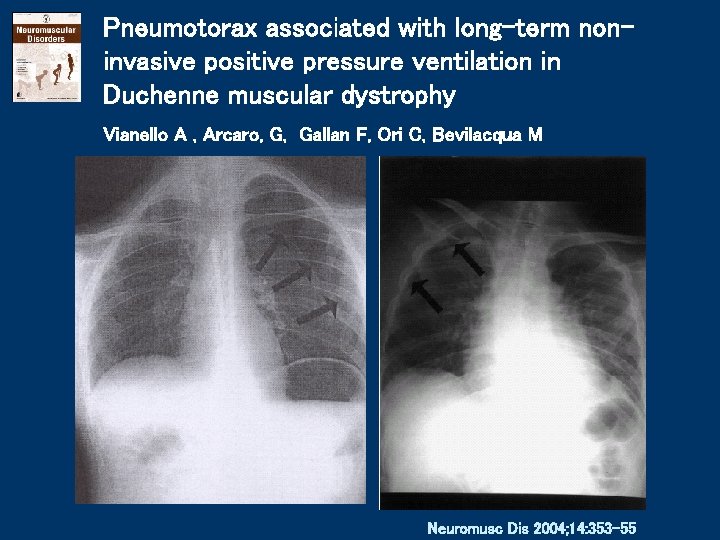
Pneumotorax associated with long-term noninvasive positive pressure ventilation in Duchenne muscular dystrophy Vianello A , Arcaro, G, Gallan F, Ori C, Bevilacqua M Neuromusc Dis 2004; 14: 353 -55
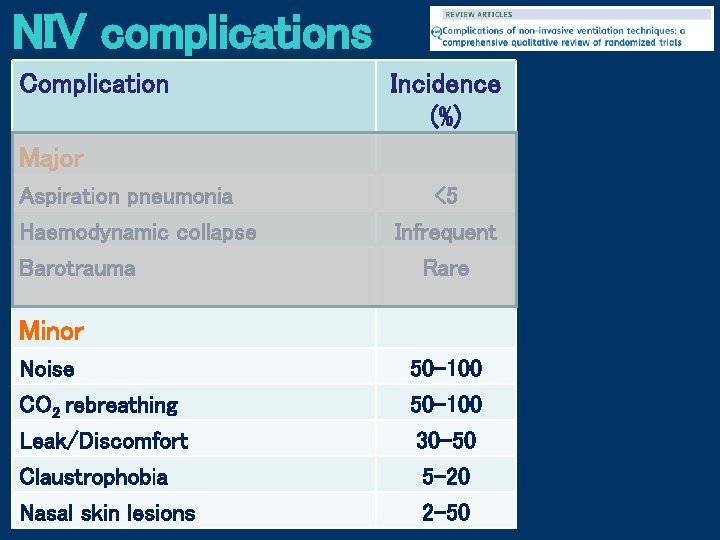
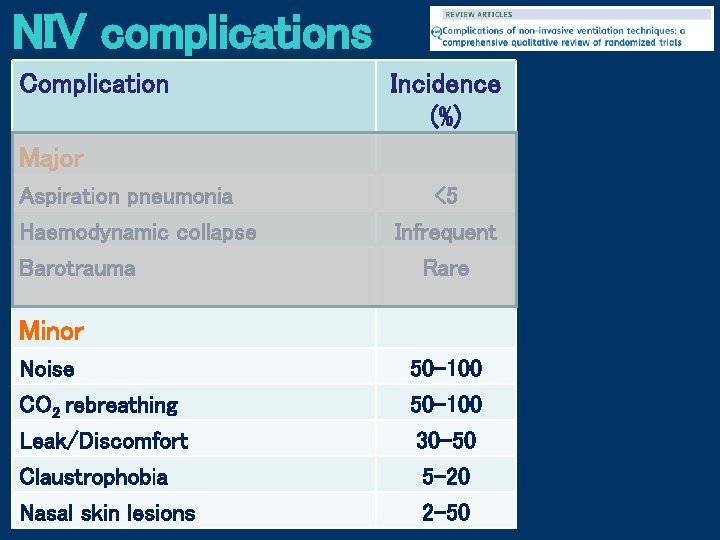
NIV complications Complication Incidence (%) Major Aspiration pneumonia Haemodynamic collapse Barotrauma <5 Infrequent Rare Minor Noise CO 2 rebreathing Leak/Discomfort Claustrophobia Nasal skin lesions 50 -100 30 -50 5 -20 2 -50
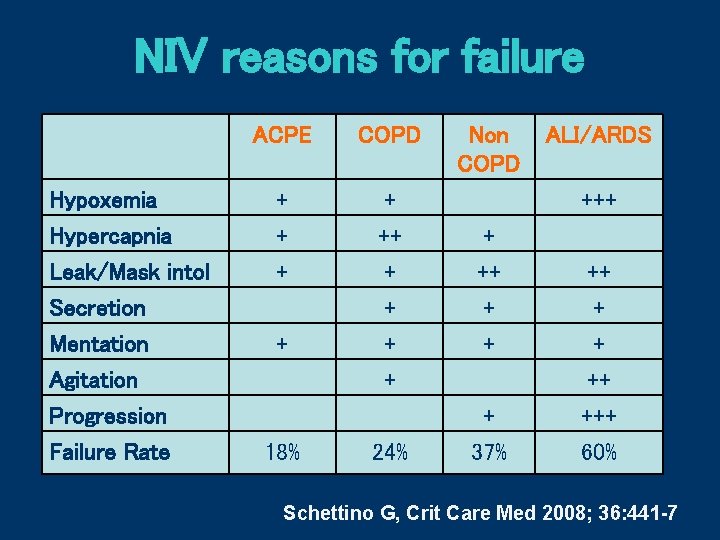
NIV reasons for failure ACPE COPD Hypoxemia Hypercapnia + ++ Leak/Mask intol Secretion Mentation Agitation Progression Failure Rate + + + 18% 24% Non COPD ALI/ARDS +++ + + + 37% ++ + + ++ +++ 60% Schettino G, Crit Care Med 2008; 36: 441 -7
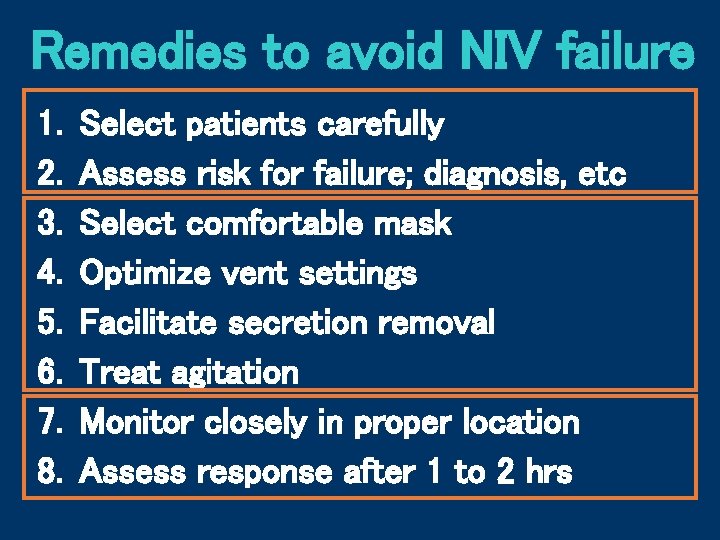
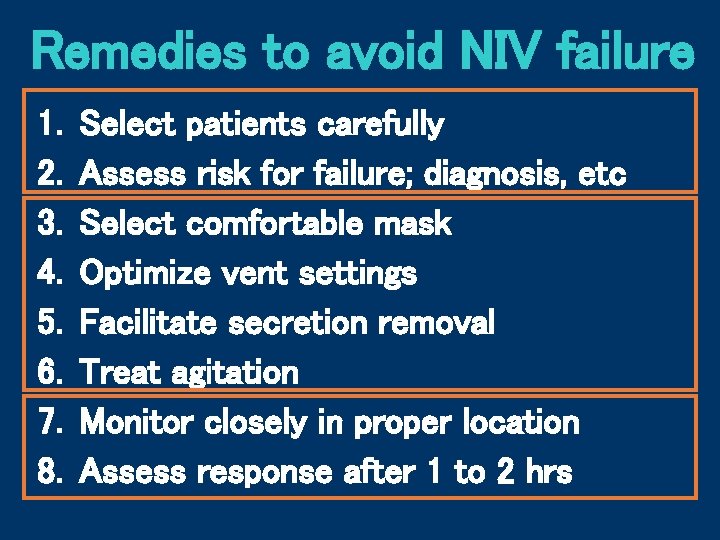
Remedies to avoid NIV failure 1. 2. 3. 4. 5. 6. 7. 8. Select patients carefully Assess risk for failure; diagnosis, etc Select comfortable mask Optimize vent settings Facilitate secretion removal Treat agitation Monitor closely in proper location Assess response after 1 to 2 hrs
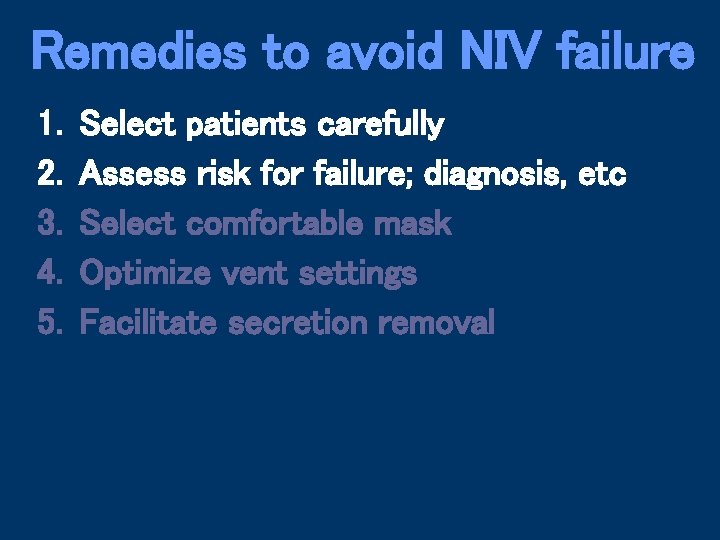
Remedies to avoid NIV failure 1. 2. 3. 4. 5. Select patients carefully Assess risk for failure; diagnosis, etc Select comfortable mask Optimize vent settings Facilitate secretion removal
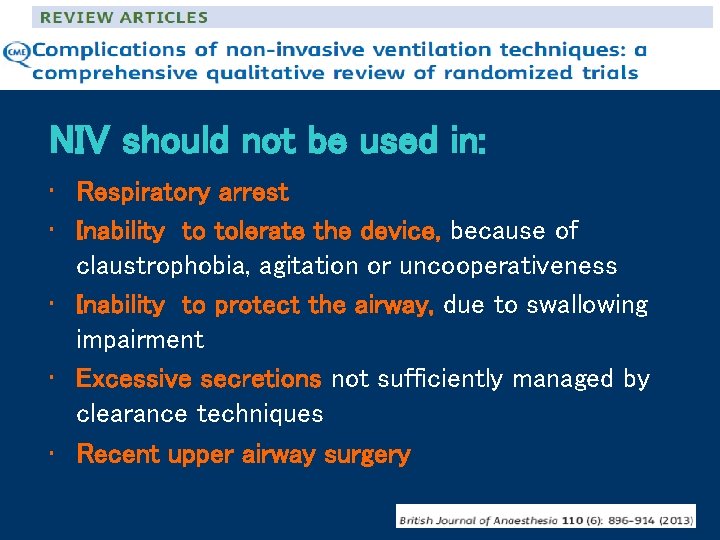
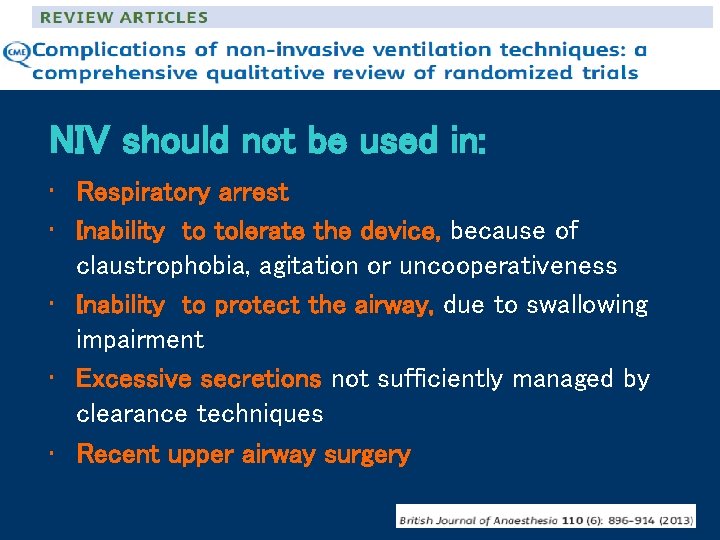
NIV should not be used in: • Respiratory arrest • Inability to tolerate the device, because of claustrophobia, agitation or uncooperativeness • Inability to protect the airway, due to swallowing impairment • Excessive secretions not sufficiently managed by clearance techniques • Recent upper airway surgery
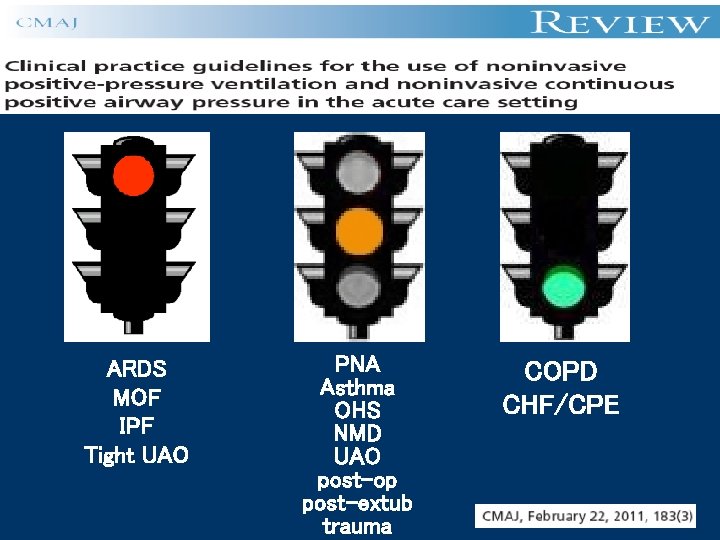
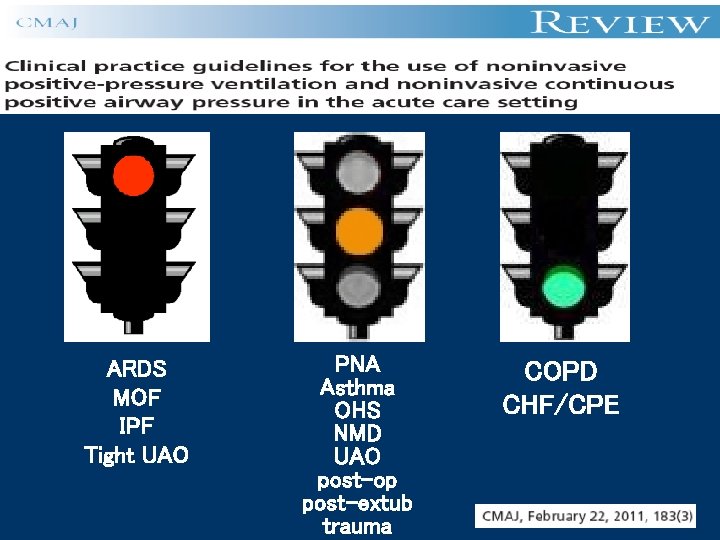
ARDS MOF IPF Tight UAO PNA Asthma OHS NMD UAO post-op post-extub trauma COPD CHF/CPE
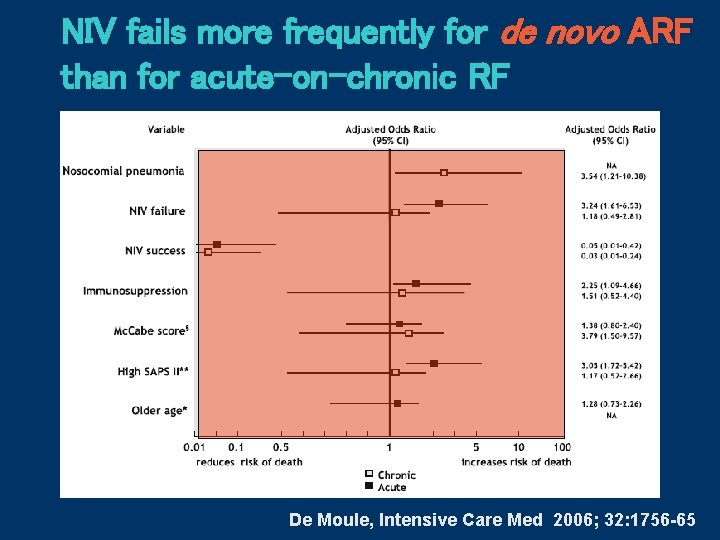
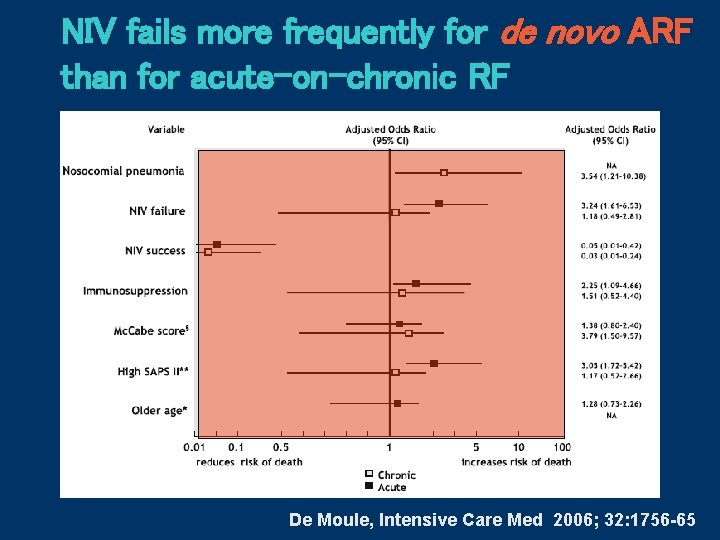
NIV fails more frequently for de novo ARF than for acute-on-chronic RF De Moule, Intensive Care Med 2006; 32: 1756 -65
Remedies to avoid NIV failure 1. 2. 3. 4. 5. Select patients carefully Assess risk for failure; diagnosis, etc Select comfortable mask Optimize vent settings Facilitate secretion removal
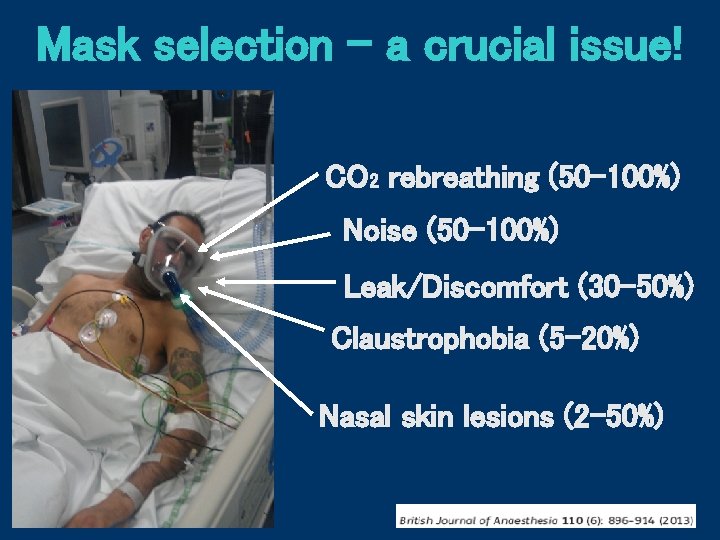
Mask selection - a crucial issue! CO 2 rebreathing (50 -100%) Noise (50 -100%) Leak/Discomfort (30 -50%) Claustrophobia (5 -20%) Nasal skin lesions (2 -50%)
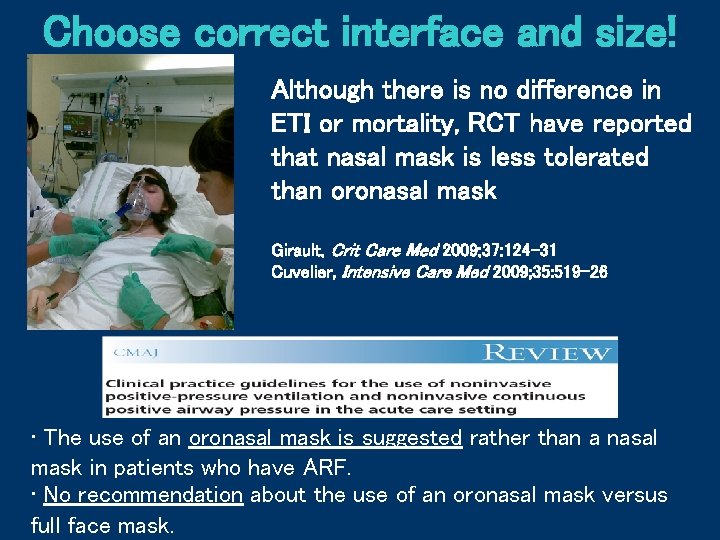
Choose correct interface and size! Although there is no difference in ETI or mortality, RCT have reported that nasal mask is less tolerated than oronasal mask Girault, Crit Care Med 2009; 37: 124 -31 Cuvelier, Intensive Care Med 2009; 35: 519 -26 • The use of an oronasal mask is suggested rather than a nasal mask in patients who have ARF. • No recommendation about the use of an oronasal mask versus full face mask.
Remedies to avoid NIV failure 1. 2. 3. 4. 5. Select patients carefully Assess risk for failure; diagnosis, etc Select comfortable mask Optimize vent settings Facilitate secretion removal
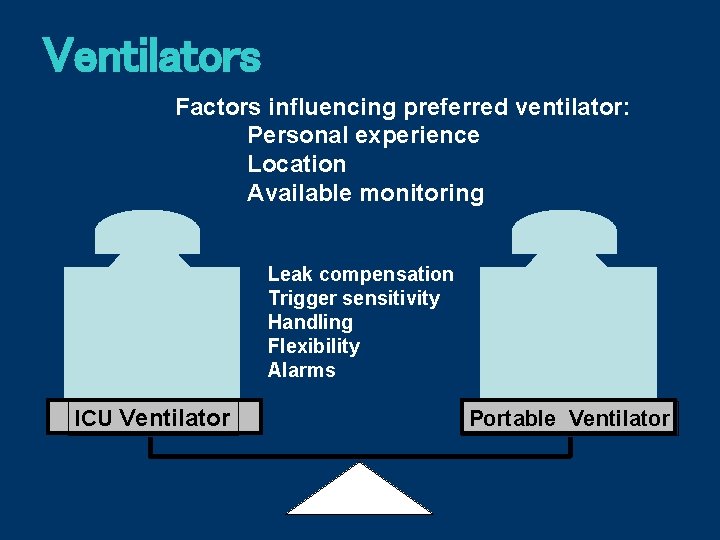
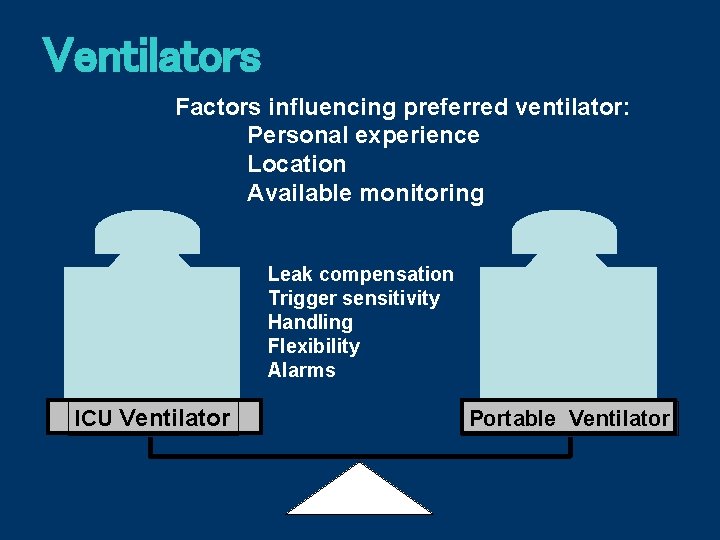
Ventilators Factors influencing preferred ventilator: Personal experience Location Available monitoring Leak compensation Trigger sensitivity Handling Flexibility Alarms ICU Ventilator Portable Ventilator
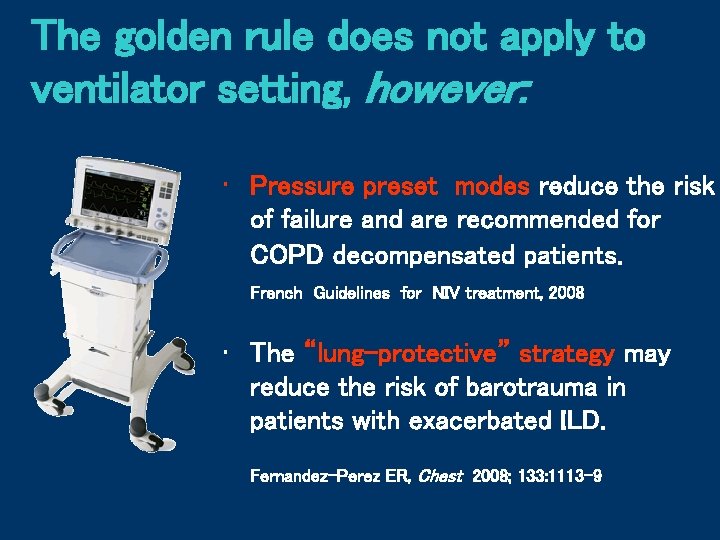
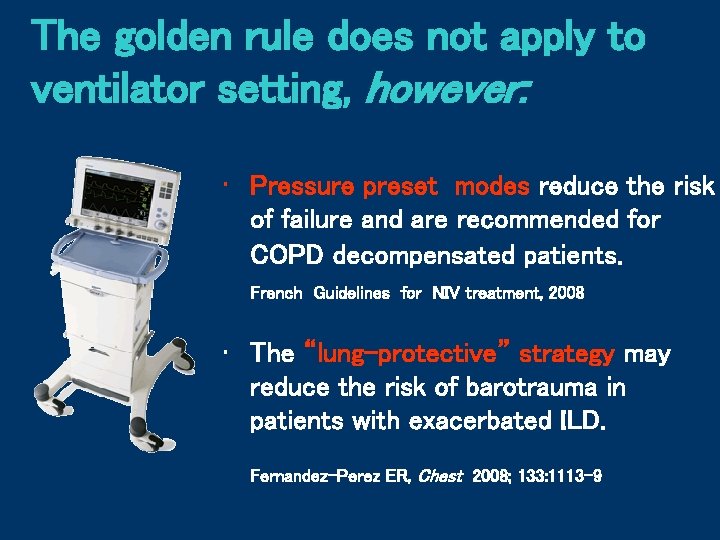
The golden rule does not apply to ventilator setting, however: • Pressure preset modes reduce the risk of failure and are recommended for COPD decompensated patients. French Guidelines for NIV treatment, 2008 • The “lung-protective” strategy may reduce the risk of barotrauma in patients with exacerbated ILD. Fernandez-Perez ER, Chest 2008; 133: 1113 -9
Remedies to avoid NIV failure 1. 2. 3. 4. 5. Select patients carefully Assess risk for failure; diagnosis, etc Select comfortable mask Optimize vent settings Facilitate secretion removal
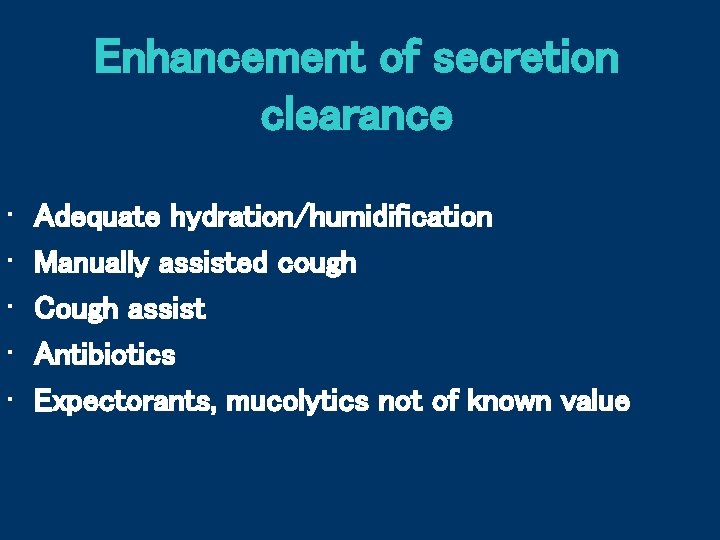
Enhancement of secretion clearance • • • Adequate hydration/humidification Manually assisted cough Cough assist Antibiotics Expectorants, mucolytics not of known value
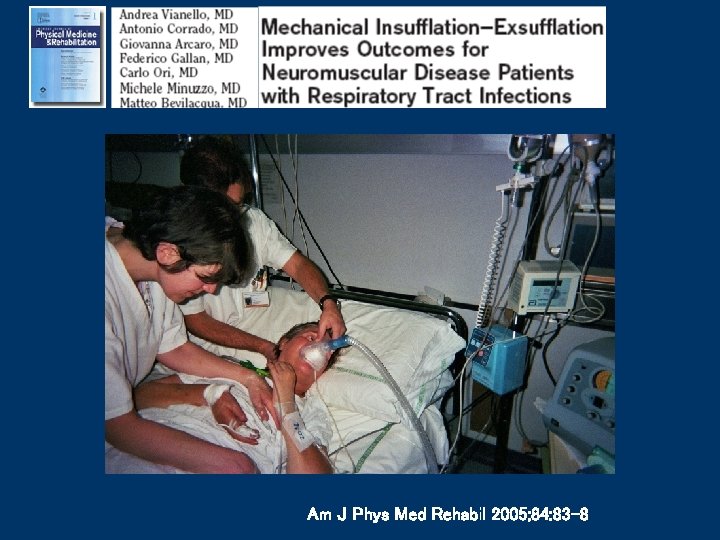
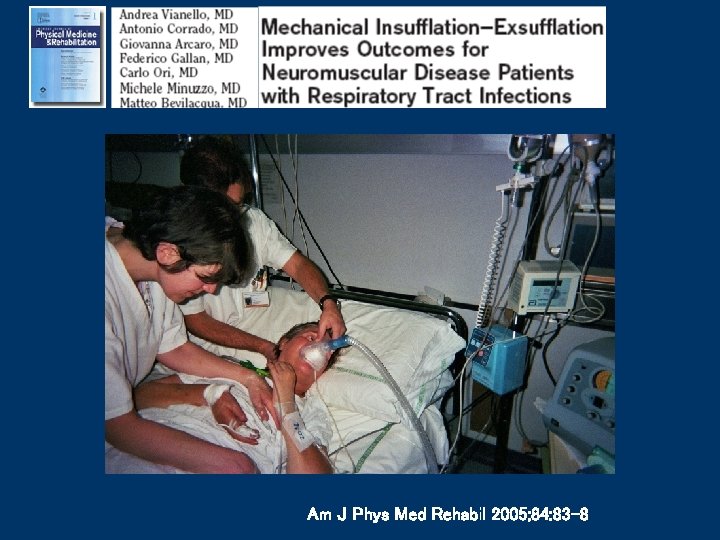
Am J Phys Med Rehabil 2005; 84: 83 -8
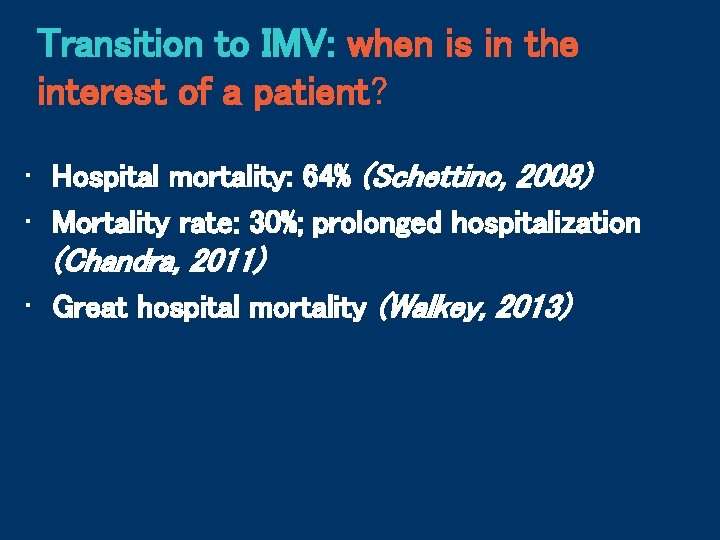
Transition to IMV: when is in the interest of a patient? • Hospital mortality: 64% (Schettino, 2008) • Mortality rate: 30%; prolonged hospitalization (Chandra, 2011) • Great hospital mortality (Walkey, 2013)
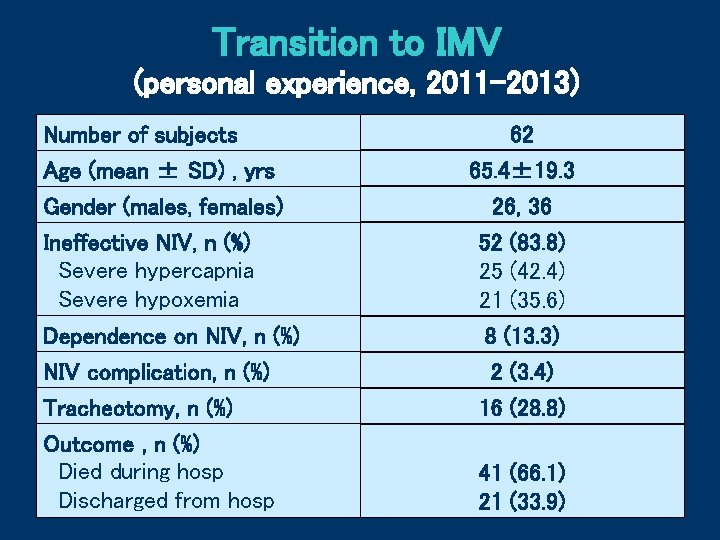
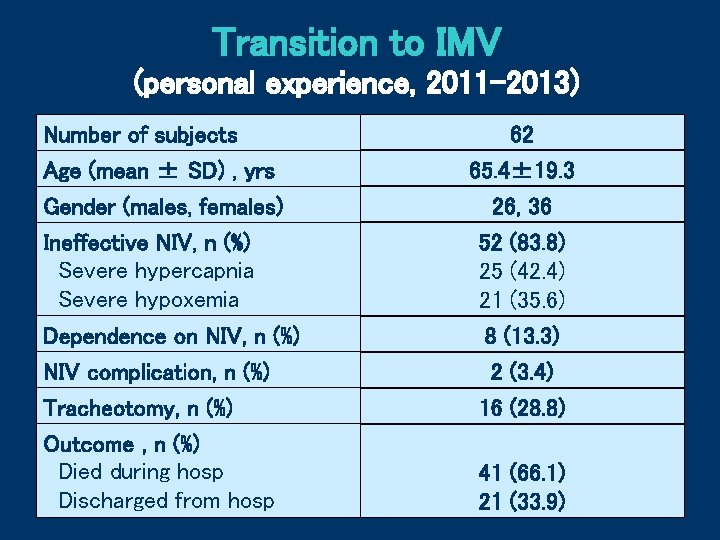
Transition to IMV (personal experience, 2011 -2013) Number of subjects Age (mean ± SD) , yrs Gender (males, females) Ineffective NIV, n (%) Severe hypercapnia Severe hypoxemia 62 65. 4± 19. 3 26, 36 52 (83. 8) 25 (42. 4) 21 (35. 6) Dependence on NIV, n (%) NIV complication, n (%) 8 (13. 3) 2 (3. 4) Tracheotomy, n (%) Outcome , n (%) Died during hosp Discharged from hosp 16 (28. 8) 41 (66. 1) 21 (33. 9)
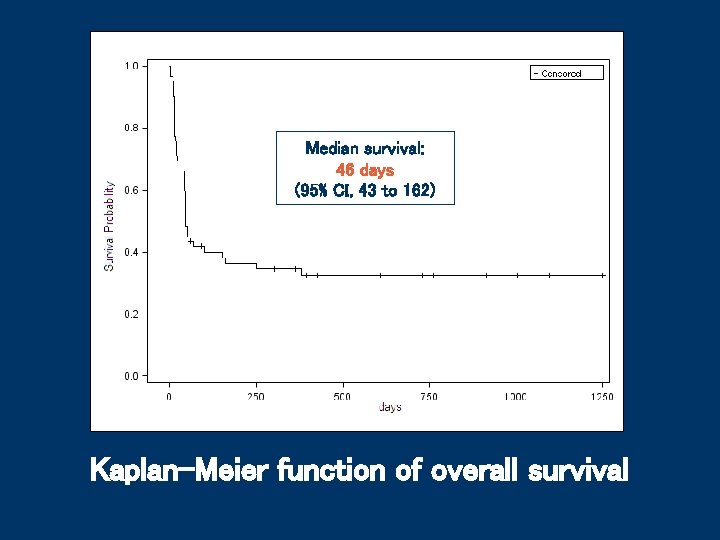
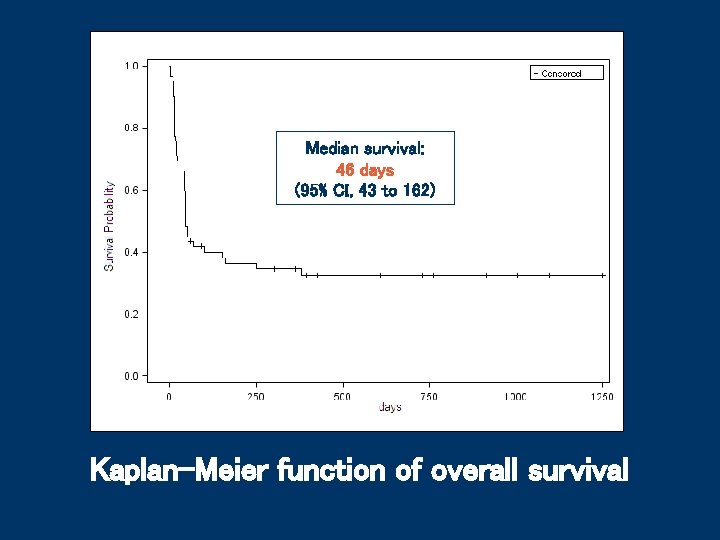
Median survival: 46 days (95% CI, 43 to 162) Kaplan-Meier function of overall survival
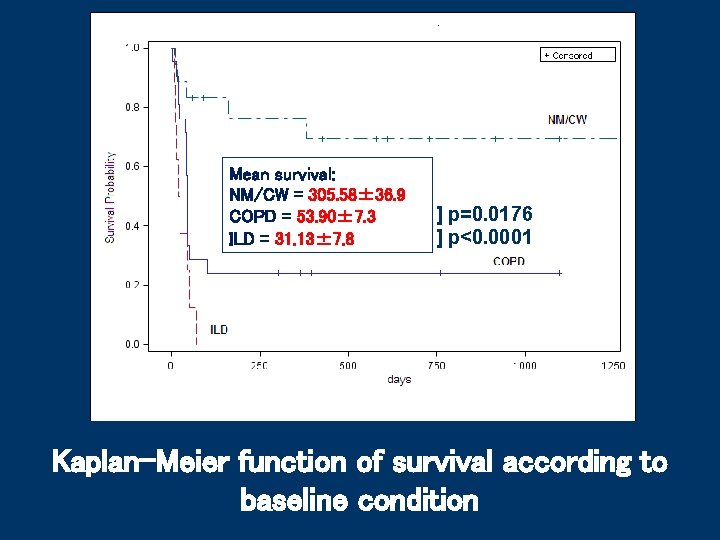
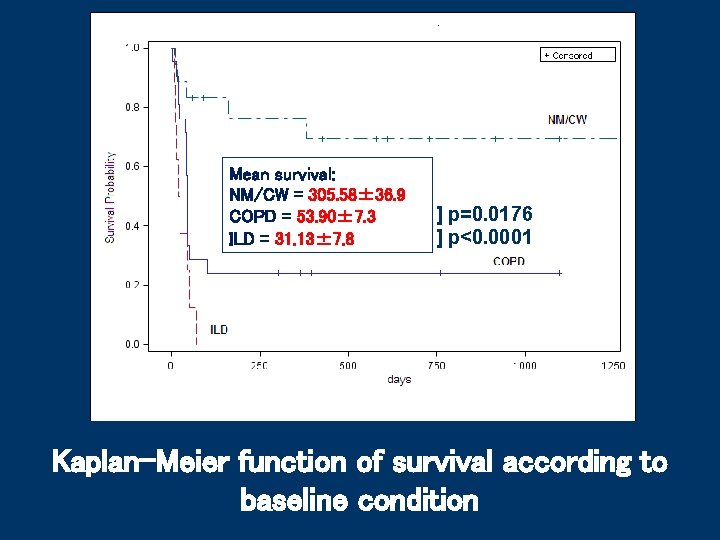
Mean survival: NM/CW = 305. 58± 36. 9 COPD = 53. 90± 7. 3 ILD = 31. 13± 7. 8 ] p=0. 0176 ] p<0. 0001 Kaplan-Meier function of survival according to baseline condition
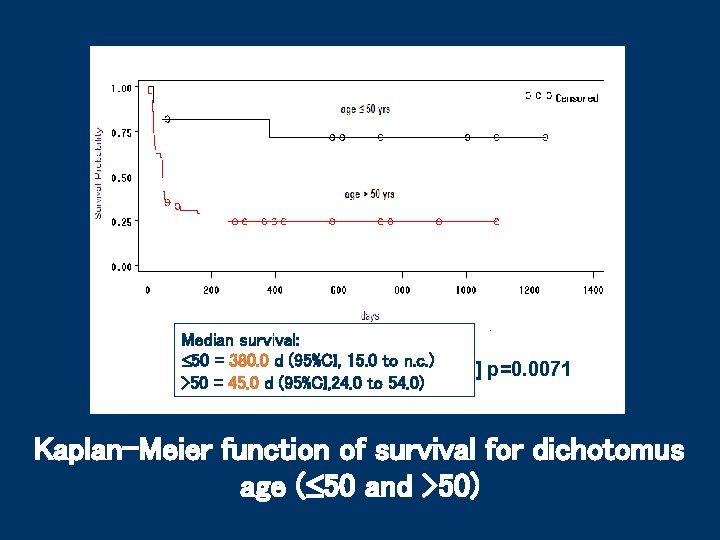
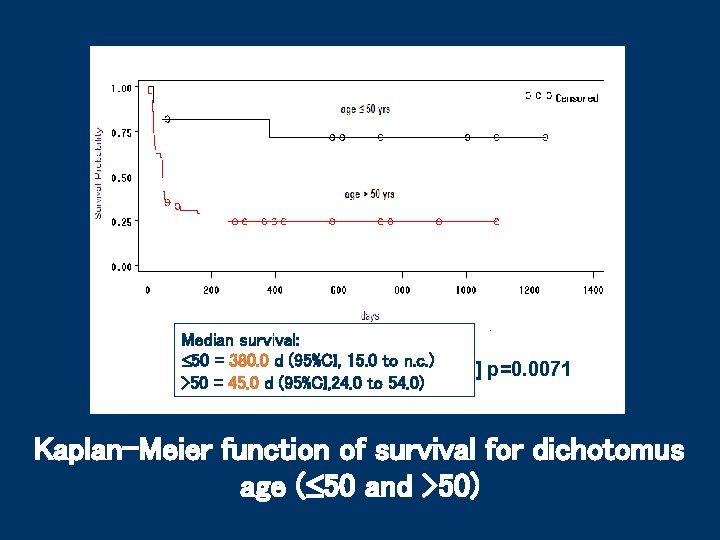
Median survival: 50 = 380. 0 d (95%CI, 15. 0 to n. c. ) >50 = 45. 0 d (95%CI, 24. 0 to 54. 0) ] p=0. 0071 Kaplan-Meier function of survival for dichotomus age ( 50 and >50)
Remarks • Mortality rate among patients transitioned to IMV is very high; • The outcome of patients with ILD is extremely poor. Should IPF/COPD patients be excluded from IMV after failing a NIV trial?
Conclusions • The boundaries for the use of NIV continue to expand, however: • The routine use of NIV in all patients with severe ARF is not yet supported • Caution should be used with NIV among patients at high risk of failure • Transitioning from NIV to IMV may not be in the interest of some categories of patients.
 Niv terapia intensiva
Niv terapia intensiva Ventilare
Ventilare Ipossiemica
Ipossiemica Paziente non collaborante
Paziente non collaborante Ivan vianello
Ivan vianello Mogans cevicheria
Mogans cevicheria Falso addome acuto
Falso addome acuto Attacco acuto glaucoma
Attacco acuto glaucoma Definizione di angoli
Definizione di angoli Etilismo acuto terapia
Etilismo acuto terapia Falso addome acuto
Falso addome acuto Quinto acuto
Quinto acuto Paziente confuso
Paziente confuso Osmolarità
Osmolarità Anestesia nel paziente tossicodipendente
Anestesia nel paziente tossicodipendente Mobilizzazione paziente emiplegico
Mobilizzazione paziente emiplegico Coumadin insufficienza renale
Coumadin insufficienza renale Paziente orientato lucido e collaborante
Paziente orientato lucido e collaborante Igiene cavo orale paziente incosciente posizione
Igiene cavo orale paziente incosciente posizione Paziente complesso definizione
Paziente complesso definizione Lettera di san paolo ai corinzi amore
Lettera di san paolo ai corinzi amore Monitoraggio paziente critico
Monitoraggio paziente critico E m m a n u e l
E m m a n u e l Past participle pensar
Past participle pensar Hey come on out by shinichi hoshi summary
Hey come on out by shinichi hoshi summary Come mi chiamo come mi chiamo
Come mi chiamo come mi chiamo Come mi vedo io come mi vedono gli altri
Come mi vedo io come mi vedono gli altri Come in come in and sit down
Come in come in and sit down Come thou fount come thou king
Come thou fount come thou king Come and listen
Come and listen Come lord jesus come and be born in our hearts lyrics
Come lord jesus come and be born in our hearts lyrics Come in come in and sit down
Come in come in and sit down Past perfect tense of ring
Past perfect tense of ring Come mi chiamo come mi chiamo
Come mi chiamo come mi chiamo Softly and tenderly jesus is calling
Softly and tenderly jesus is calling Come holy spirit, come hymn
Come holy spirit, come hymn Leader member exchange
Leader member exchange Title and author
Title and author Moc definicja
Moc definicja Fases de la alergia
Fases de la alergia Andrea omicini
Andrea omicini Andrea plesner
Andrea plesner Andrea suk
Andrea suk The probability that janice smokes is 3/10
The probability that janice smokes is 3/10 Kölner kommunikationsordner
Kölner kommunikationsordner Dr fodor andrea
Dr fodor andrea One24 webinar
One24 webinar Andrea de la puente
Andrea de la puente Maria claudia quintero lemus
Maria claudia quintero lemus