Lo Pneumologo Andrea Vianello Fisiopatologia e Terapia Intensiva











- Slides: 42
Lo Pneumologo Andrea Vianello Fisiopatologia e Terapia Intensiva Respiratoria Ospedale-Università di Padova
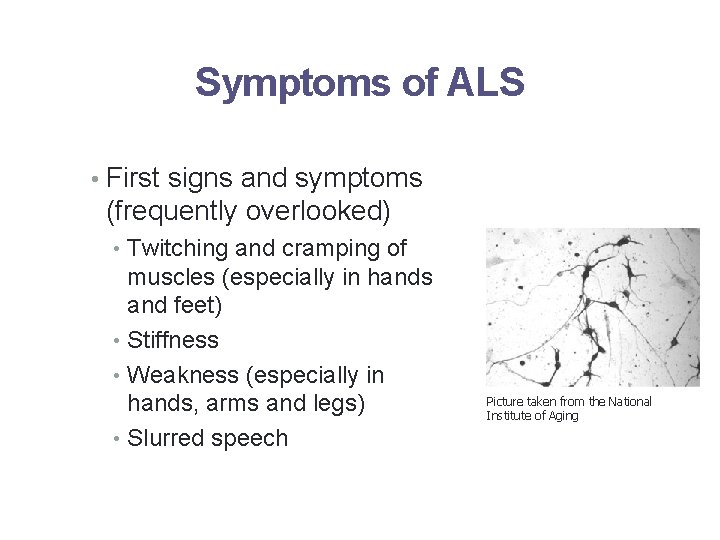
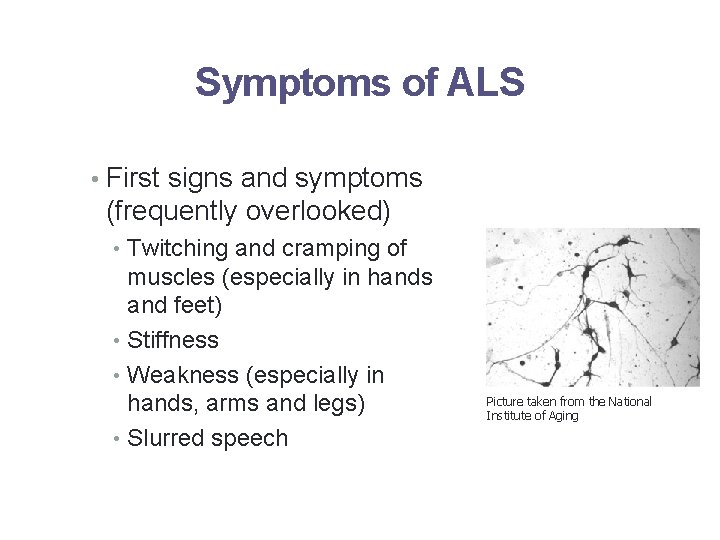
Symptoms of ALS • First signs and symptoms (frequently overlooked) • Twitching and cramping of muscles (especially in hands and feet) • Stiffness • Weakness (especially in hands, arms and legs) • Slurred speech Picture taken from the National Institute of Aging
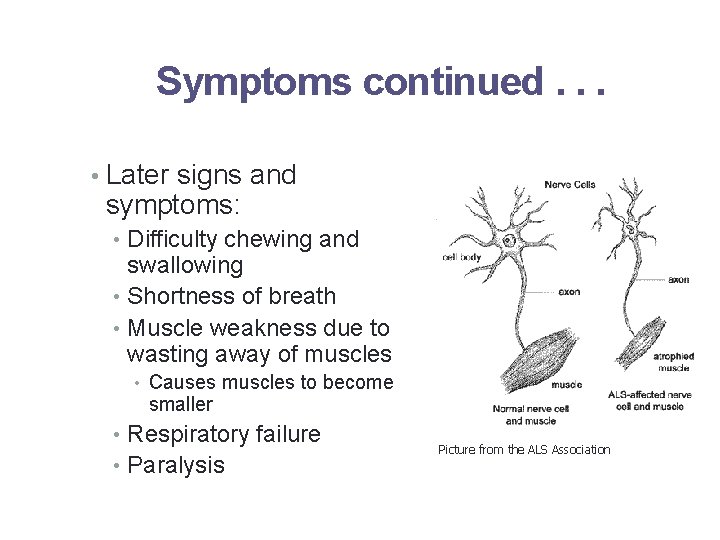
Symptoms continued. . . • Later signs and symptoms: • Difficulty chewing and swallowing • Shortness of breath • Muscle weakness due to wasting away of muscles • Causes muscles to become smaller • Respiratory failure • Paralysis Picture from the ALS Association

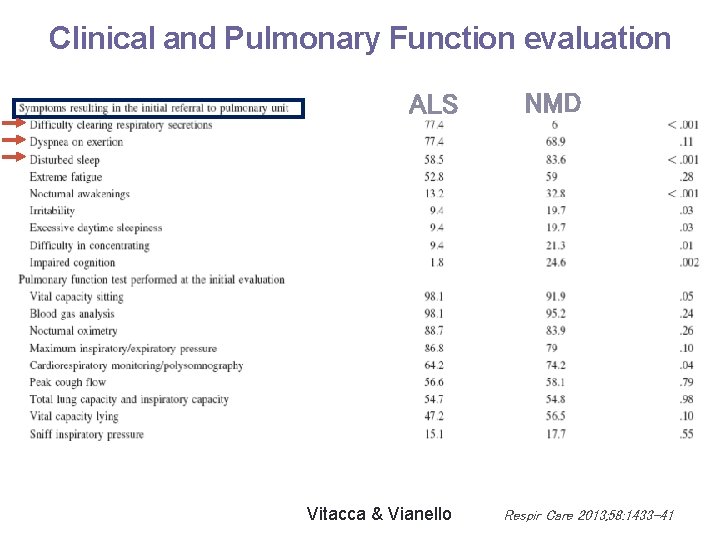
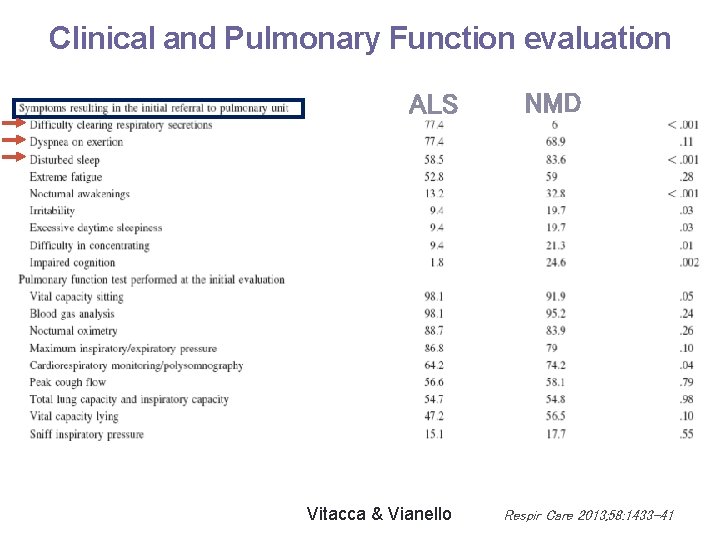
Clinical and Pulmonary Function evaluation ALS Vitacca & Vianello NMD Respir Care 2013; 58: 1433 -41

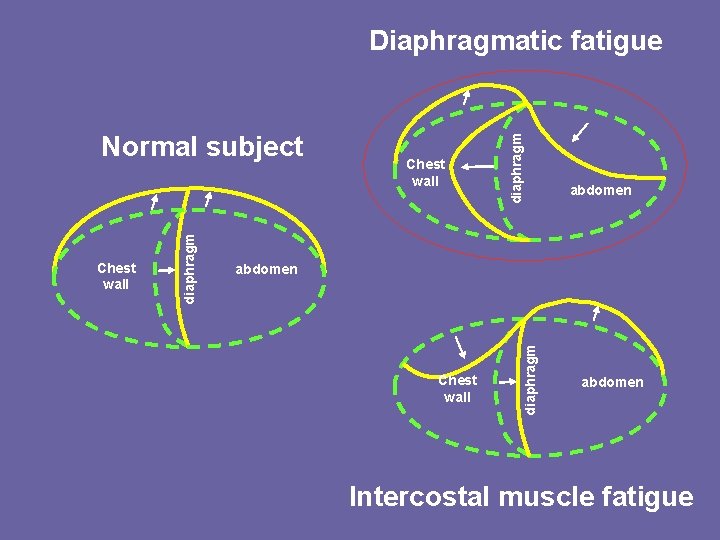
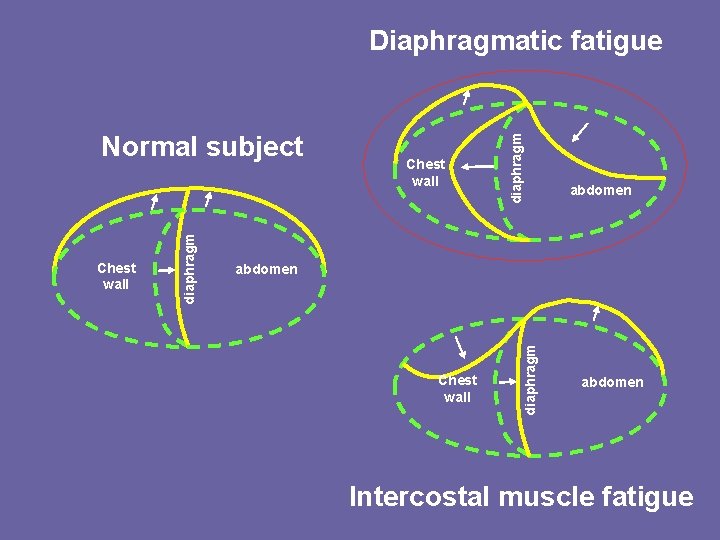
Chest wall abdomen Chest wall diaphragm Normal subject diaphragm Diaphragmatic fatigue abdomen Intercostal muscle fatigue
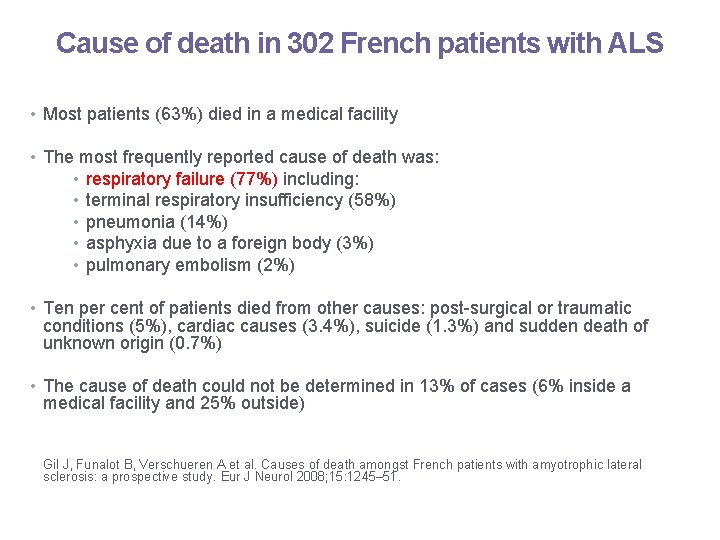
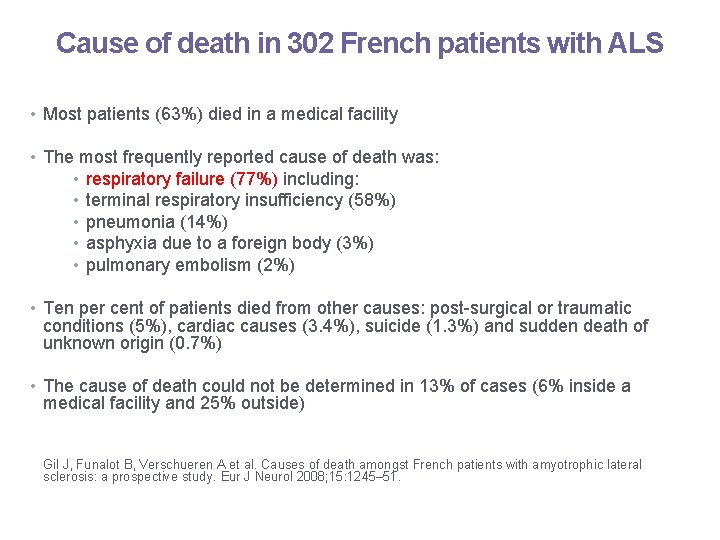
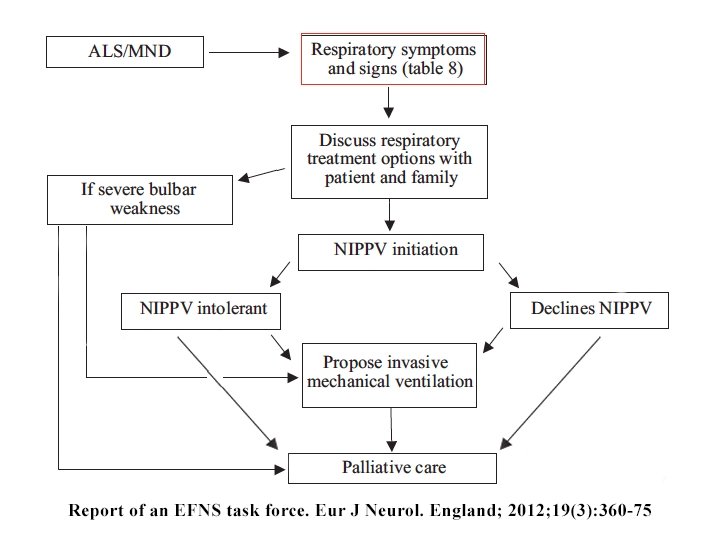
Cause of death in 302 French patients with ALS • Most patients (63%) died in a medical facility • The most frequently reported cause of death was: • • • respiratory failure (77%) including: terminal respiratory insufficiency (58%) pneumonia (14%) asphyxia due to a foreign body (3%) pulmonary embolism (2%) • Ten per cent of patients died from other causes: post-surgical or traumatic conditions (5%), cardiac causes (3. 4%), suicide (1. 3%) and sudden death of unknown origin (0. 7%) • The cause of death could not be determined in 13% of cases (6% inside a medical facility and 25% outside) Gil J, Funalot B, Verschueren A et al. Causes of death amongst French patients with amyotrophic lateral sclerosis: a prospective study. Eur J Neurol 2008; 15: 1245– 51.

Long-Term Noninvasive Ventilation
What is Noninvasive Ventilation? “A form of ventilatory support that avoids airway invasion”
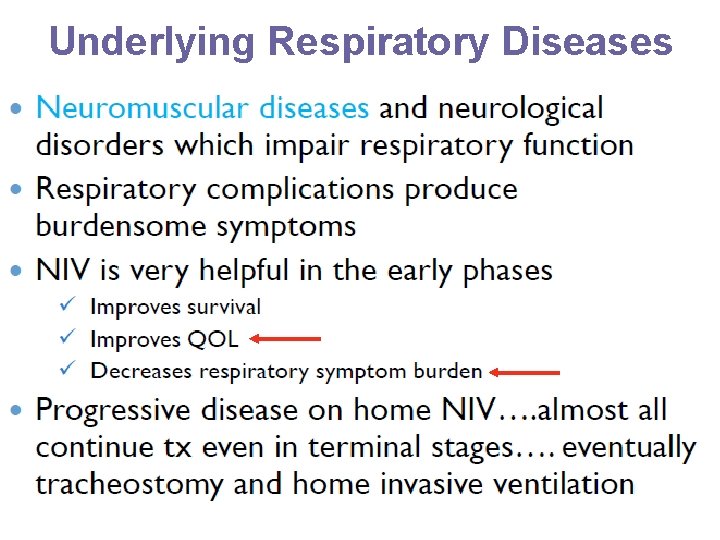
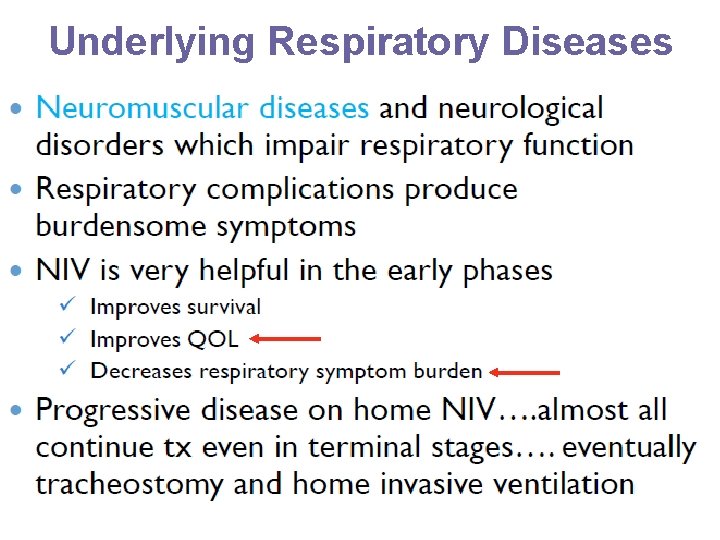
Underlying Respiratory Diseases
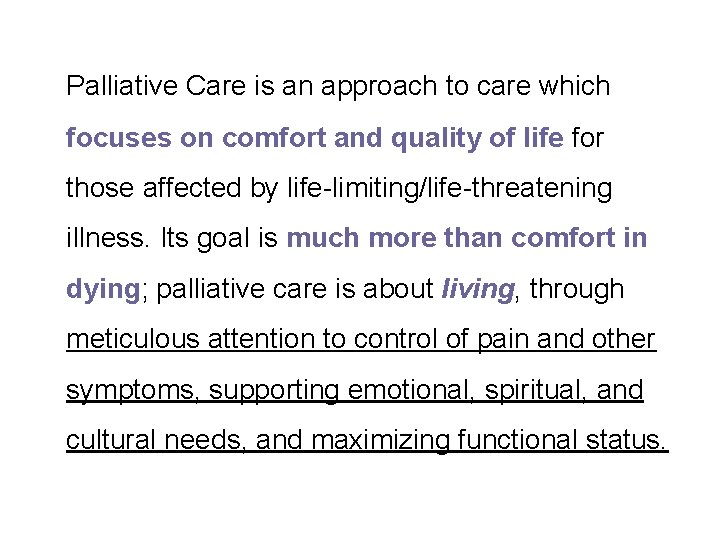
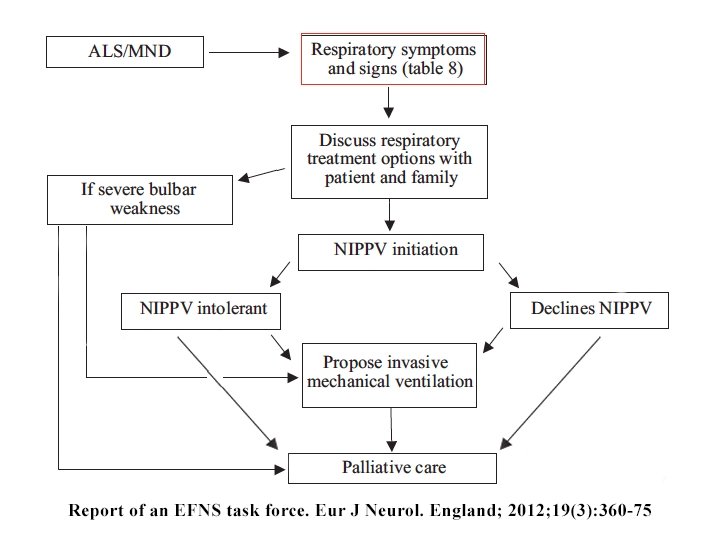
Palliative Care is an approach to care which focuses on comfort and quality of life for those affected by life-limiting/life-threatening illness. Its goal is much more than comfort in dying; palliative care is about living, through meticulous attention to control of pain and other symptoms, supporting emotional, spiritual, and cultural needs, and maximizing functional status.
Shared care 1. Role of O 2 therapy 2. Noninvasive ventilation 3. Role of opioids in palliation of dyspnea 4. Withdrawal of life-sustaining treatments – ventilatory support (invasive and noninvasive), oxygen
Shared care 1. Role of O 2 therapy 2. Noninvasive ventilation 3. Role of opioids in palliation of dyspnea 4. Withdrawal of life-sustaining treatments – ventilatory support (invasive and noninvasive), oxygen
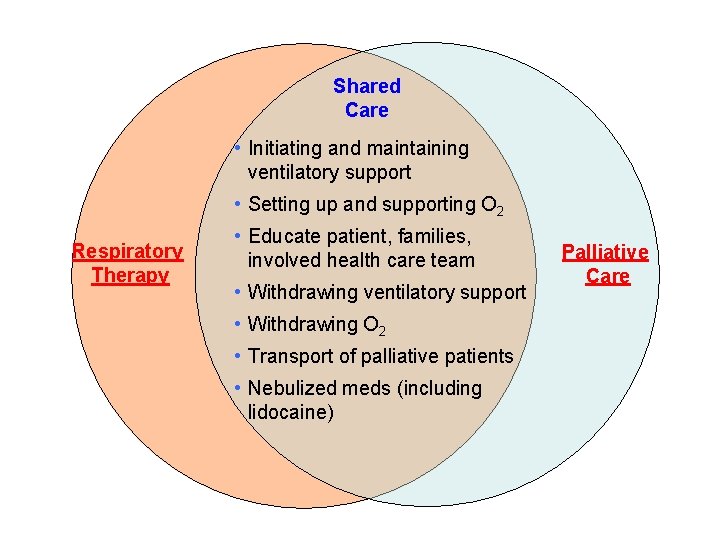
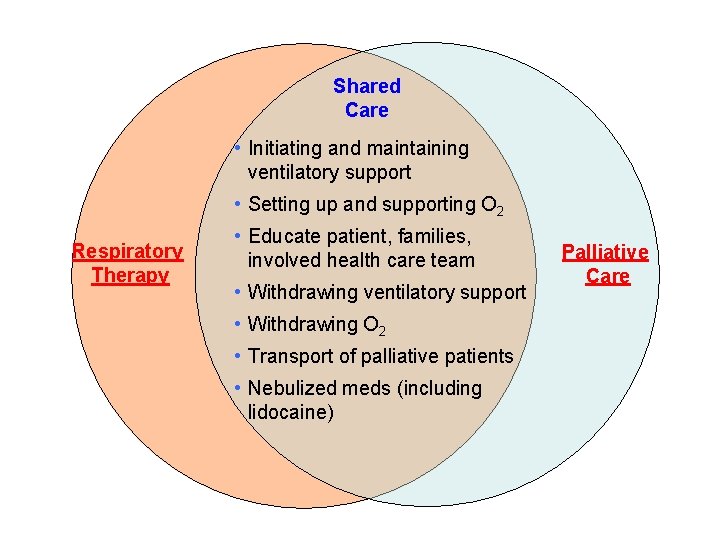
Shared Care • Initiating and maintaining ventilatory support • Setting up and supporting O 2 Respiratory Therapy • Educate patient, families, involved health care team • Withdrawing ventilatory support • Withdrawing O 2 • Transport of palliative patients • Nebulized meds (including lidocaine) Palliative Care
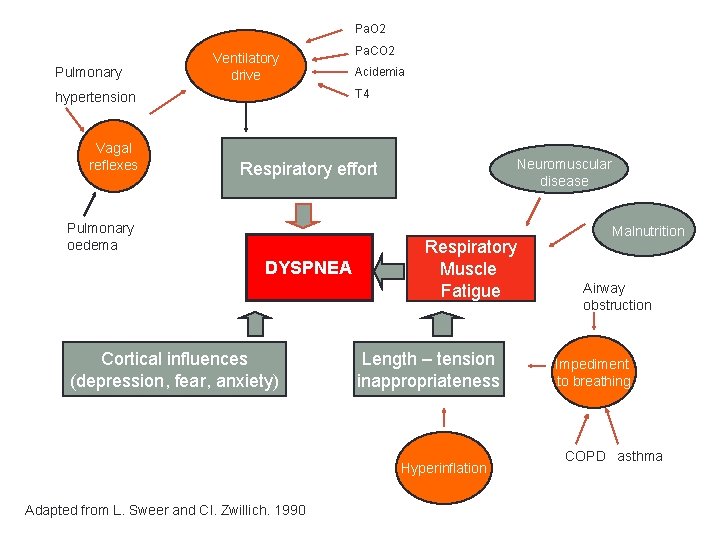
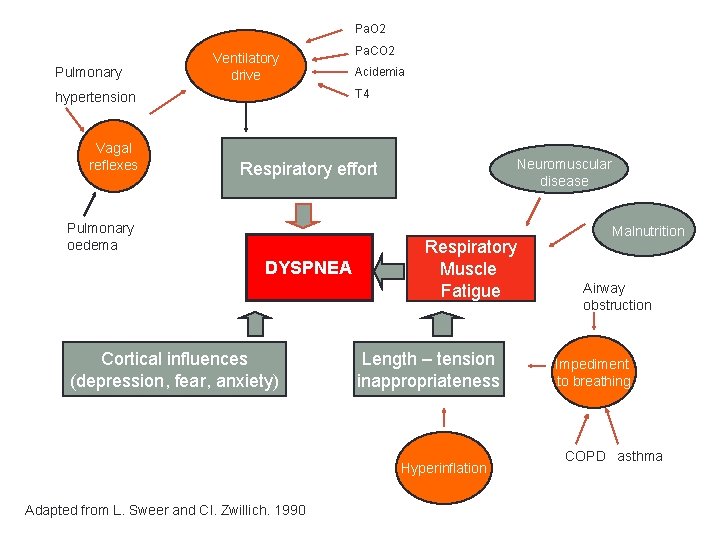
Pa. O 2 Pulmonary Ventilatory drive Acidemia T 4 hypertension Vagal reflexes Pa. CO 2 Neuromuscular disease Respiratory effort Pulmonary oedema DYSPNEA Cortical influences (depression, fear, anxiety) Respiratory Muscle Fatigue Length – tension inappropriateness Hyperinflation Adapted from L. Sweer and Cl. Zwillich. 1990 Malnutrition Airway obstruction Impediment to breathing COPD asthma
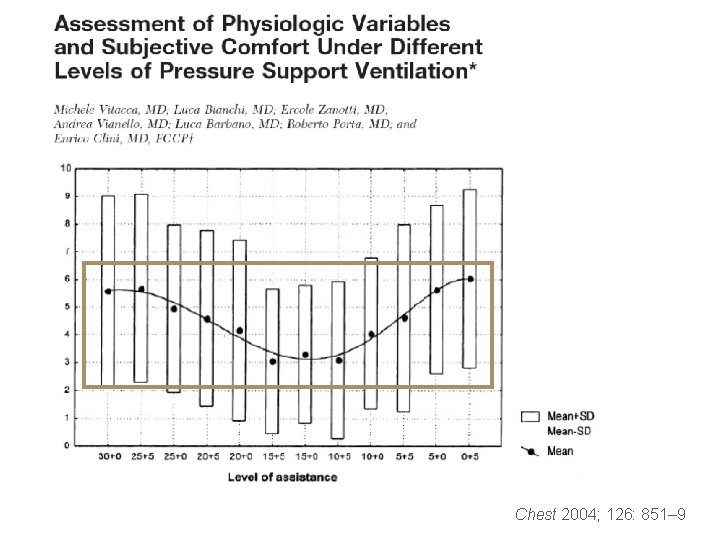
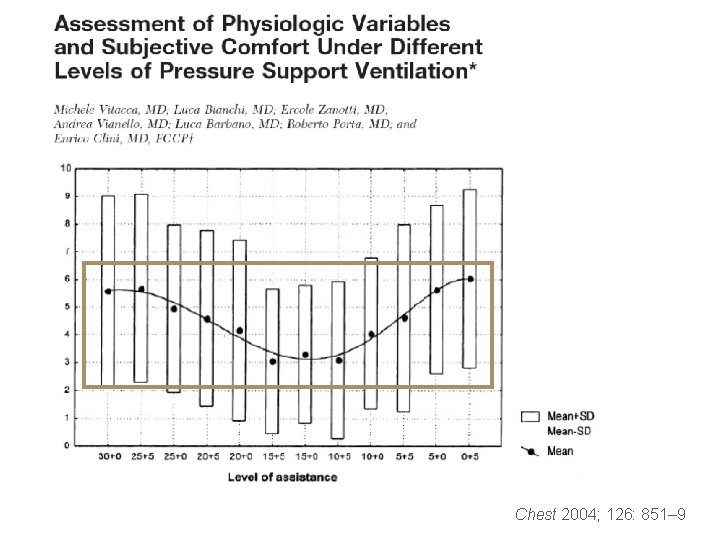
Chest 2004; 126: 851– 9
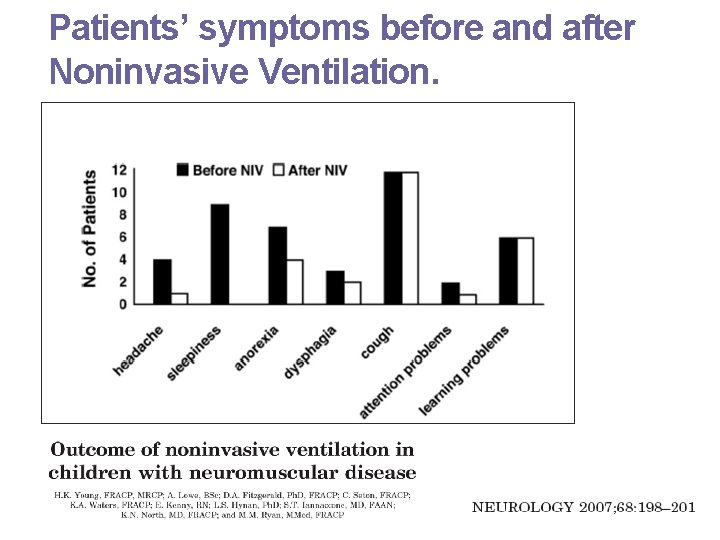
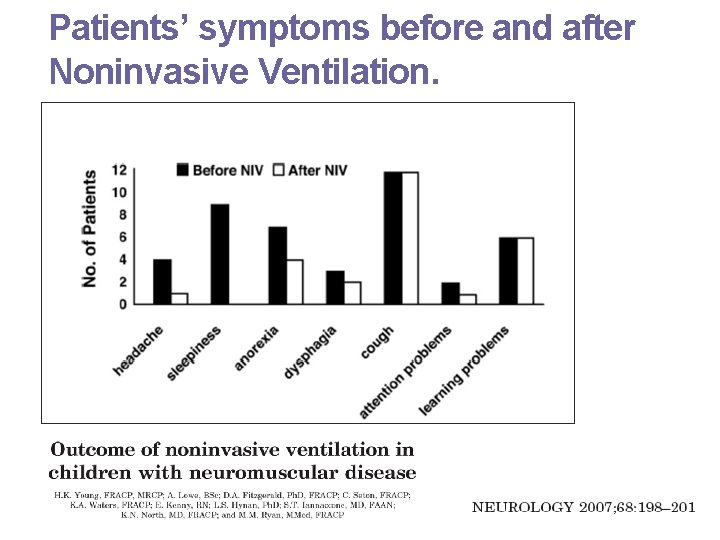
Patients’ symptoms before and after Noninvasive Ventilation.
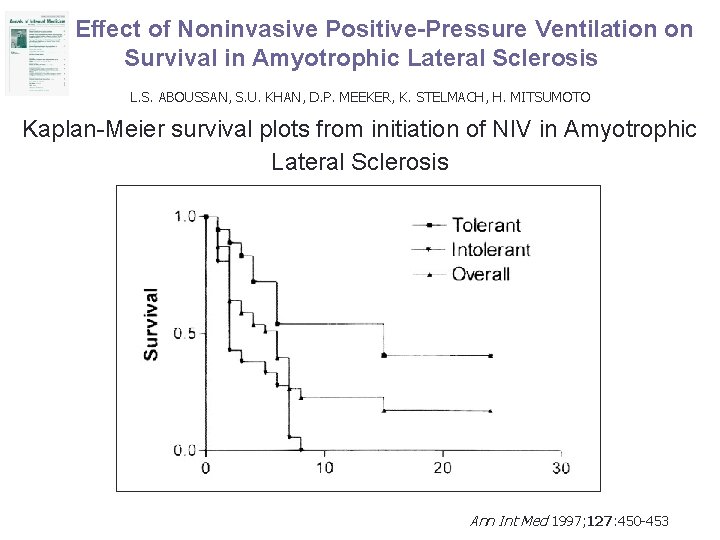
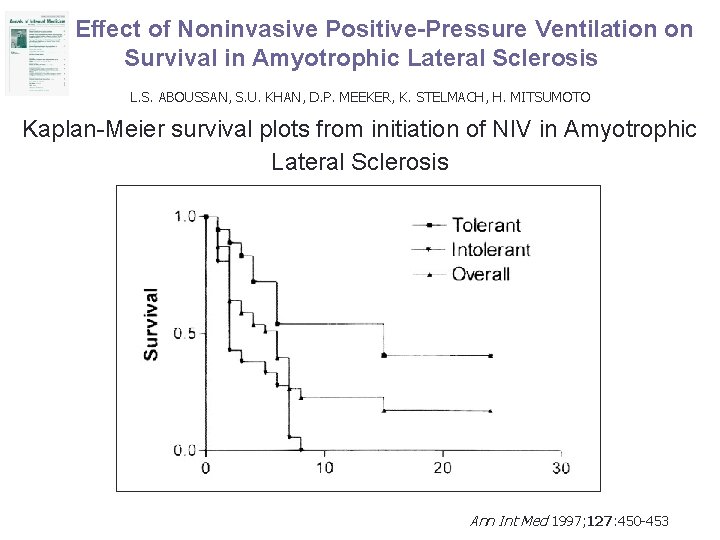
Effect of Noninvasive Positive-Pressure Ventilation on Survival in Amyotrophic Lateral Sclerosis L. S. ABOUSSAN, S. U. KHAN, D. P. MEEKER, K. STELMACH, H. MITSUMOTO Kaplan-Meier survival plots from initiation of NIV in Amyotrophic Lateral Sclerosis Ann Int Med 1997; 127: 450 -453
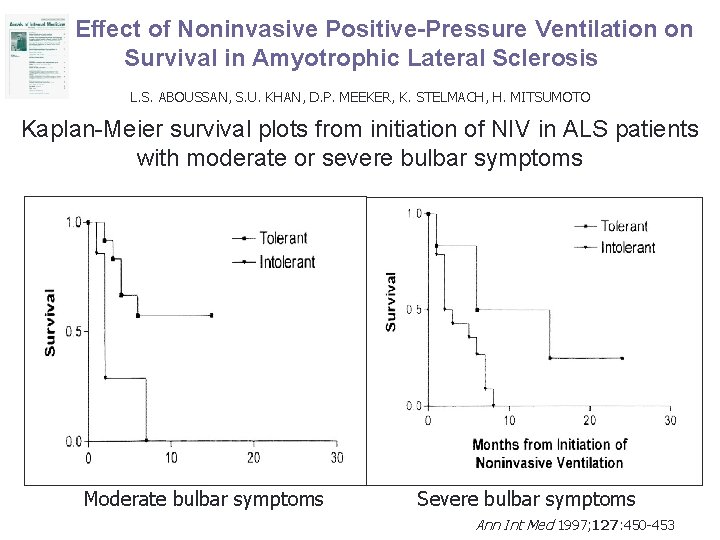
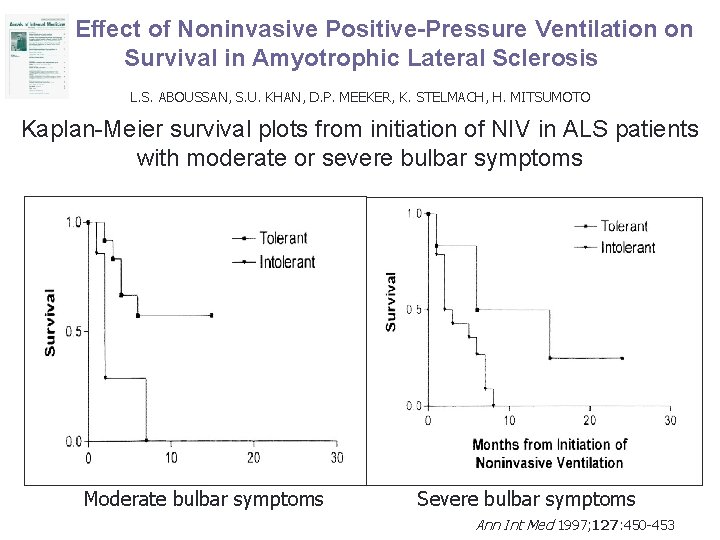
Effect of Noninvasive Positive-Pressure Ventilation on Survival in Amyotrophic Lateral Sclerosis L. S. ABOUSSAN, S. U. KHAN, D. P. MEEKER, K. STELMACH, H. MITSUMOTO Kaplan-Meier survival plots from initiation of NIV in ALS patients with moderate or severe bulbar symptoms Moderate bulbar symptoms Severe bulbar symptoms Ann Int Med 1997; 127: 450 -453
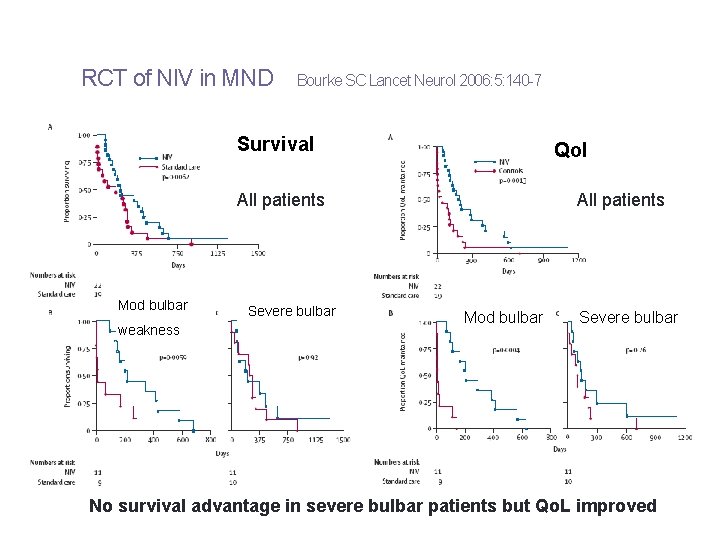
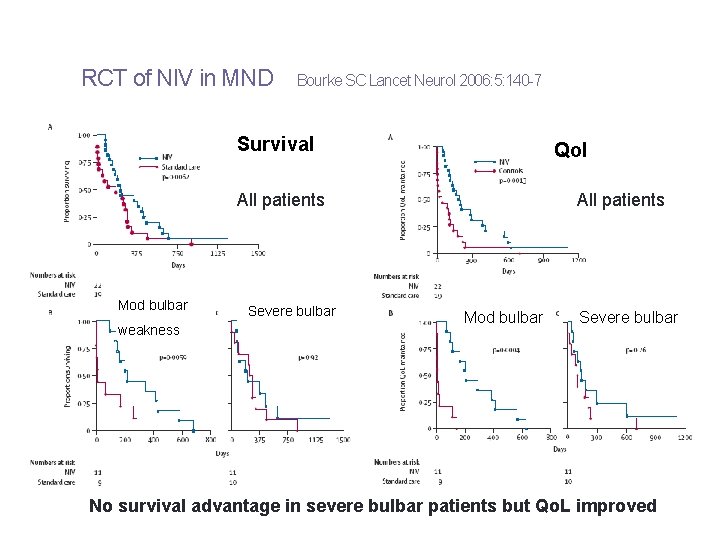
RCT of NIV in MND Bourke SC Lancet Neurol 2006: 5: 140 -7 Survival Qol All patients Mod bulbar weakness Severe bulbar All patients Mod bulbar Severe bulbar No survival advantage in severe bulbar patients but Qo. L improved
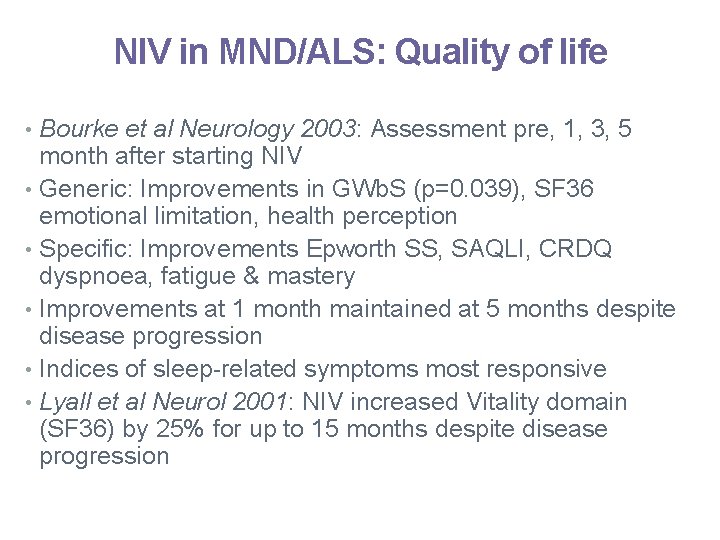
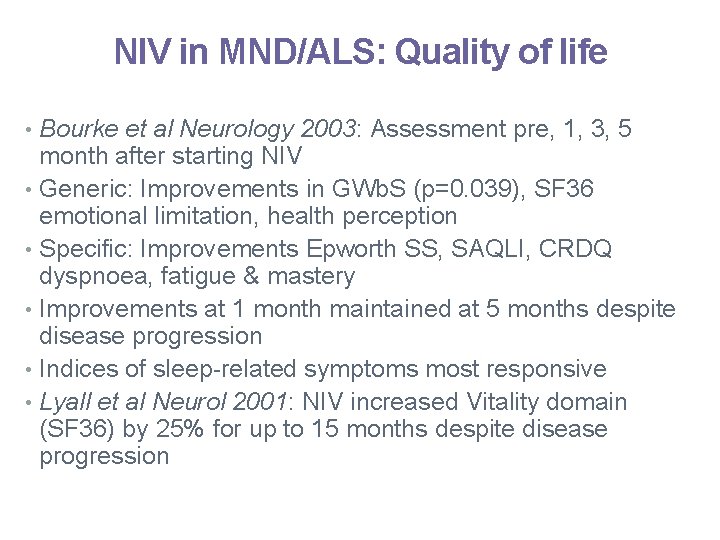
NIV in MND/ALS: Quality of life • Bourke et al Neurology 2003: Assessment pre, 1, 3, 5 month after starting NIV • Generic: Improvements in GWb. S (p=0. 039), SF 36 emotional limitation, health perception • Specific: Improvements Epworth SS, SAQLI, CRDQ dyspnoea, fatigue & mastery • Improvements at 1 month maintained at 5 months despite disease progression • Indices of sleep-related symptoms most responsive • Lyall et al Neurol 2001: NIV increased Vitality domain (SF 36) by 25% for up to 15 months despite disease progression
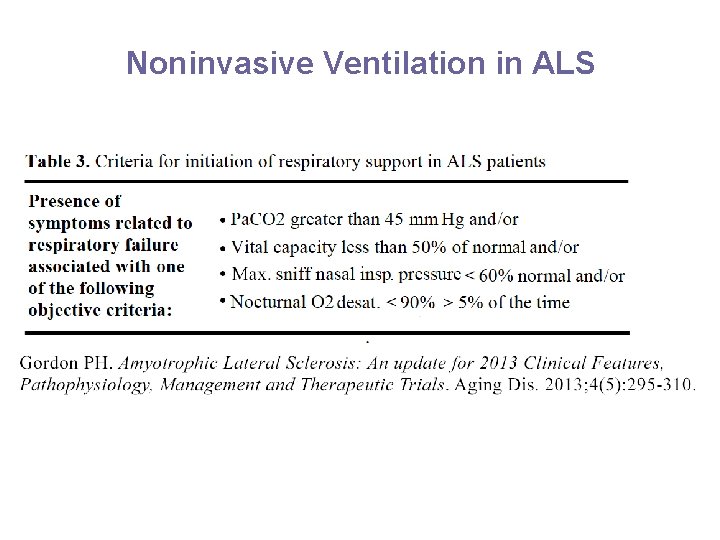
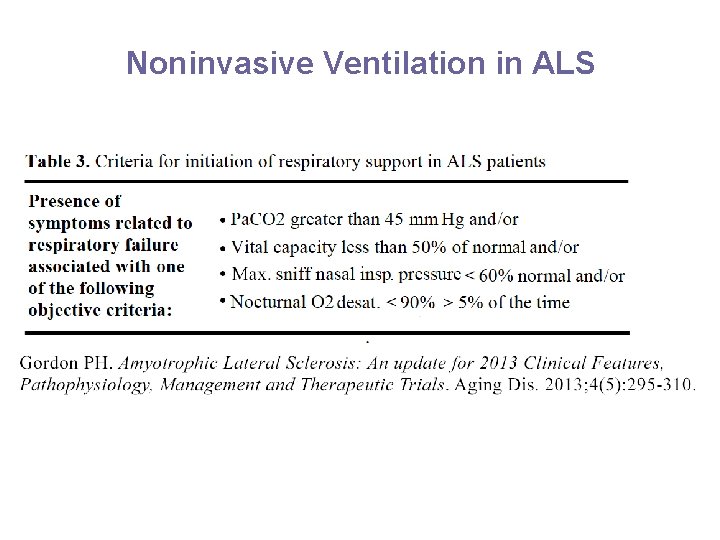
Noninvasive Ventilation in ALS

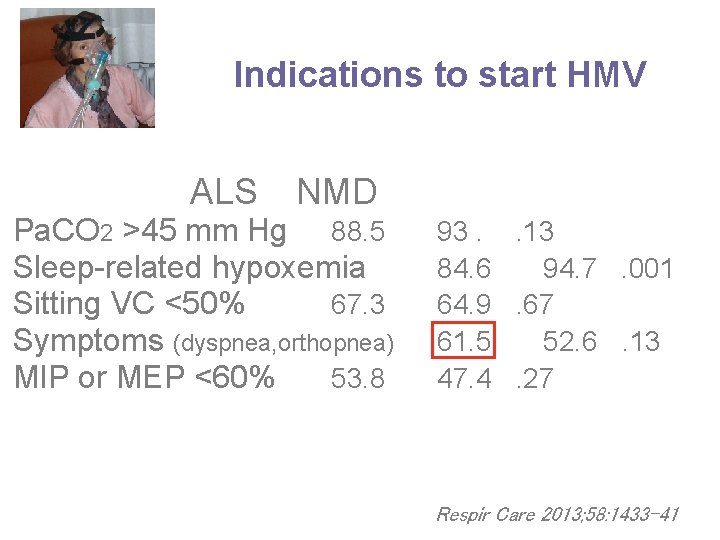
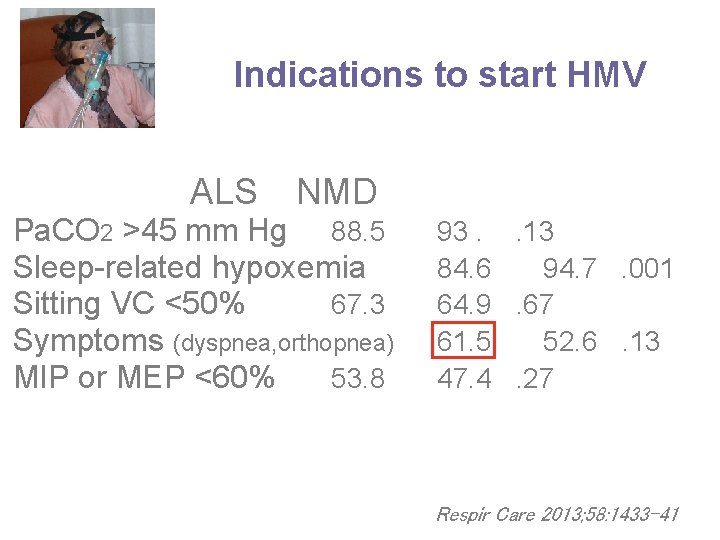
Indications to start HMV ALS NMD Pa. CO 2 >45 mm Hg 88. 5 Sleep-related hypoxemia Sitting VC <50% 67. 3 Symptoms (dyspnea, orthopnea) MIP or MEP <60% 53. 8 93. . 13 84. 6 94. 7. 001 64. 9. 67 61. 5 52. 6. 13 47. 4. 27 Respir Care 2013; 58: 1433 -41
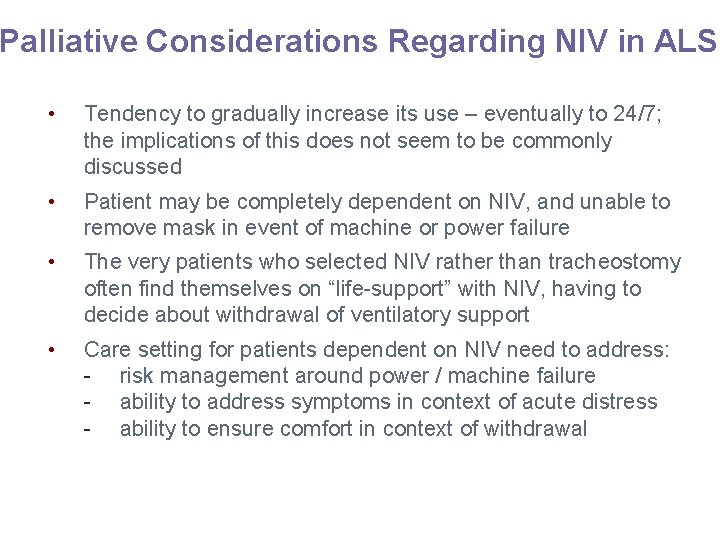
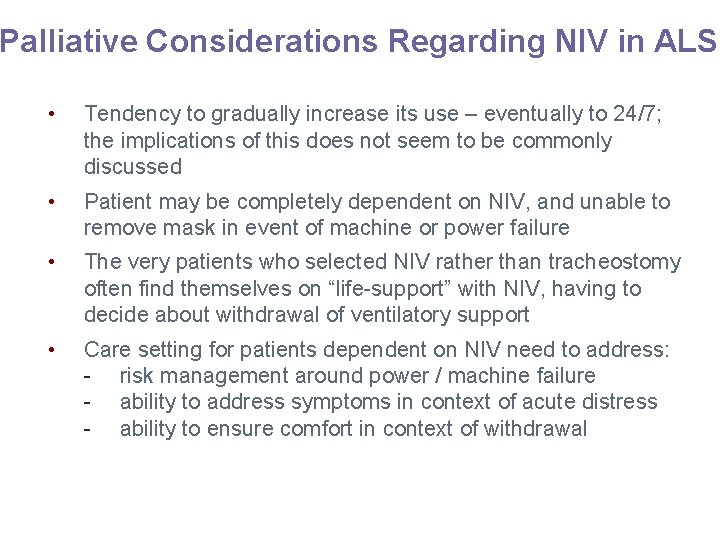
Palliative Considerations Regarding NIV in ALS • Tendency to gradually increase its use – eventually to 24/7; the implications of this does not seem to be commonly discussed • Patient may be completely dependent on NIV, and unable to remove mask in event of machine or power failure • The very patients who selected NIV rather than tracheostomy often find themselves on “life-support” with NIV, having to decide about withdrawal of ventilatory support • Care setting for patients dependent on NIV need to address: - risk management around power / machine failure - ability to address symptoms in context of acute distress - ability to ensure comfort in context of withdrawal


? Survival and Quality of Life after tracheotomy

The mean time between intubation and death was 7. 4 months, (median 2. 8 months, range 1 week to 3. 5 years)
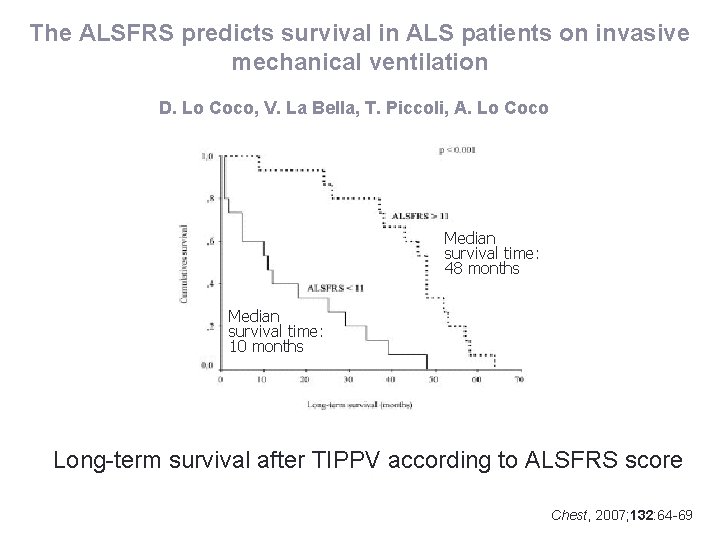
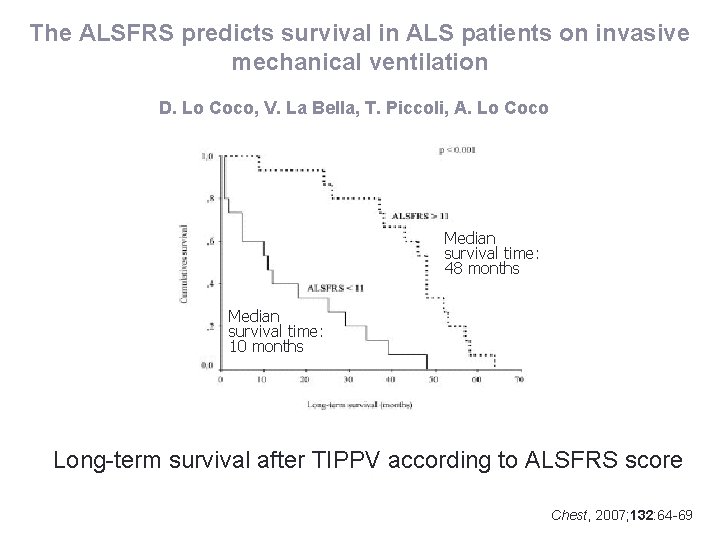
The ALSFRS predicts survival in ALS patients on invasive mechanical ventilation D. Lo Coco, V. La Bella, T. Piccoli, A. Lo Coco Median survival time: 48 months Median survival time: 10 months Long-term survival after TIPPV according to ALSFRS score Chest, 2007; 132: 64 -69
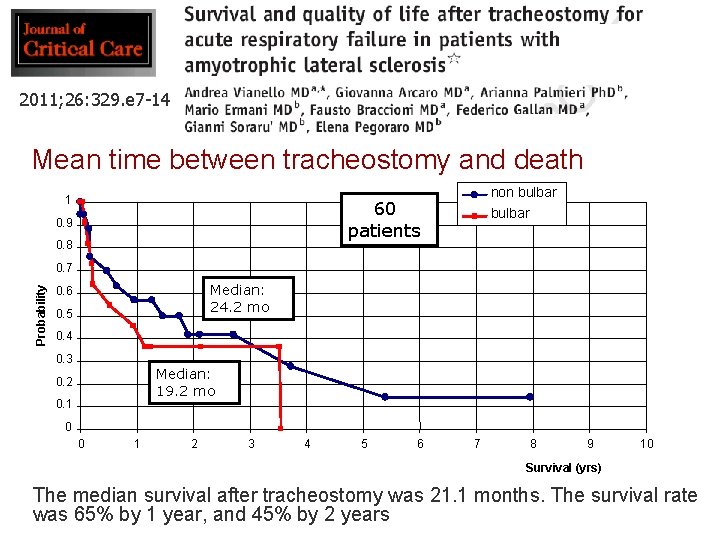
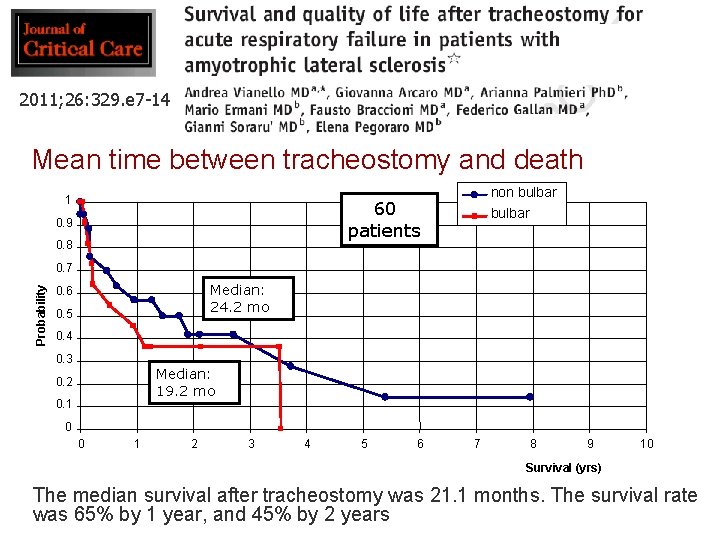
2011; 26: 329. e 7 -14 Mean time between tracheostomy and death 1 non bulbar 60 patients 0. 9 0. 8 bulbar Probability 0. 7 Median: 24. 2 mo 0. 6 0. 5 0. 4 0. 3 Median: 19. 2 mo 0. 2 0. 1 0 0 1 2 3 4 5 6 7 8 9 10 Survival (yrs) The median survival after tracheostomy was 21. 1 months. The survival rate was 65% by 1 year, and 45% by 2 years

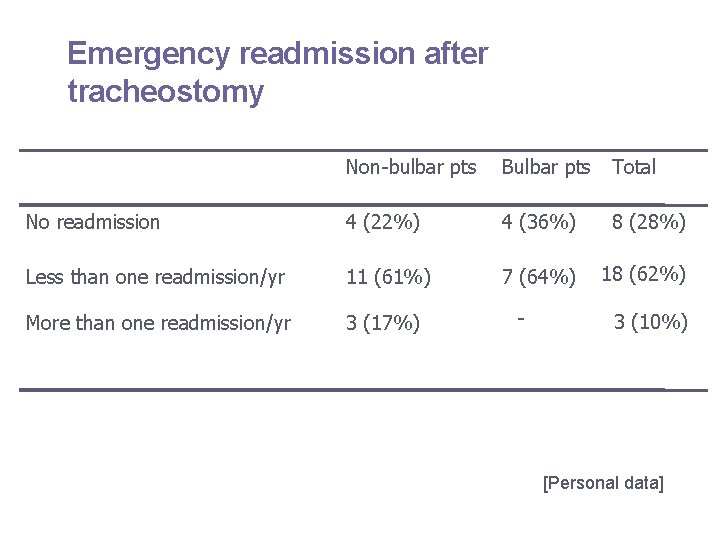
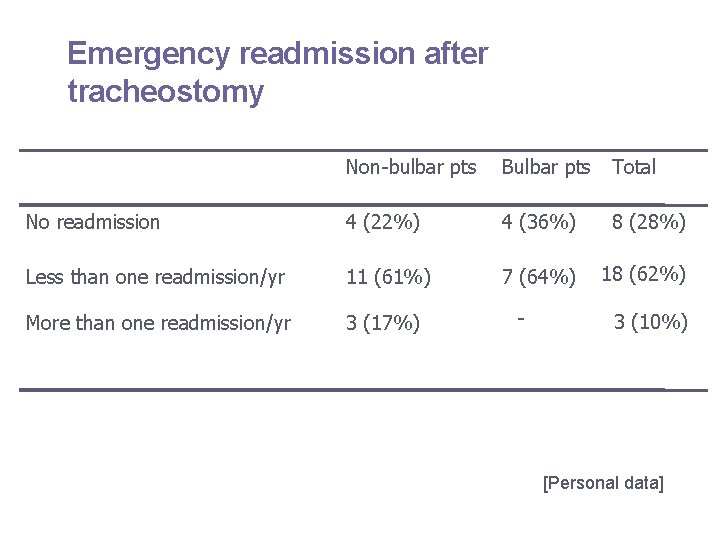
Emergency readmission after tracheostomy Non-bulbar pts Bulbar pts Total No readmission 4 (22%) 4 (36%) 8 (28%) Less than one readmission/yr 11 (61%) 7 (64%) 18 (62%) More than one readmission/yr 3 (17%) - 3 (10%) [Personal data]

Life Satisfaction Index – 11 (Italian Version) The Life Satisfaction Index – 11 is a short form of LSI questionnaire providing a cumulative score acknowledged as an index of quality of life
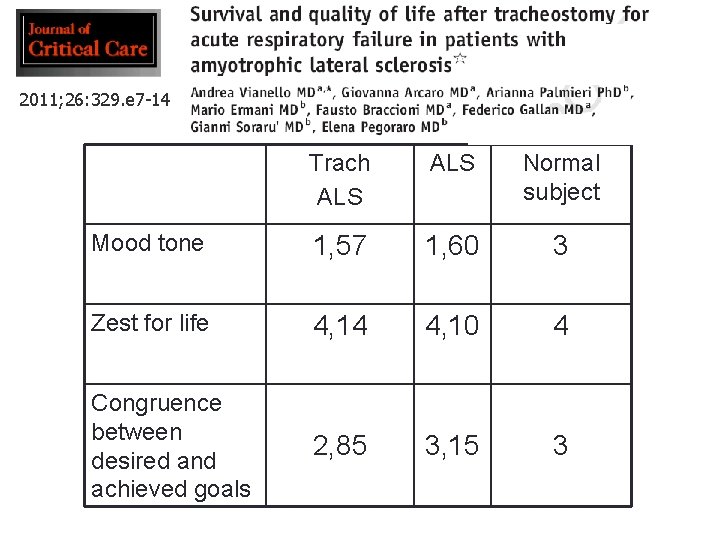
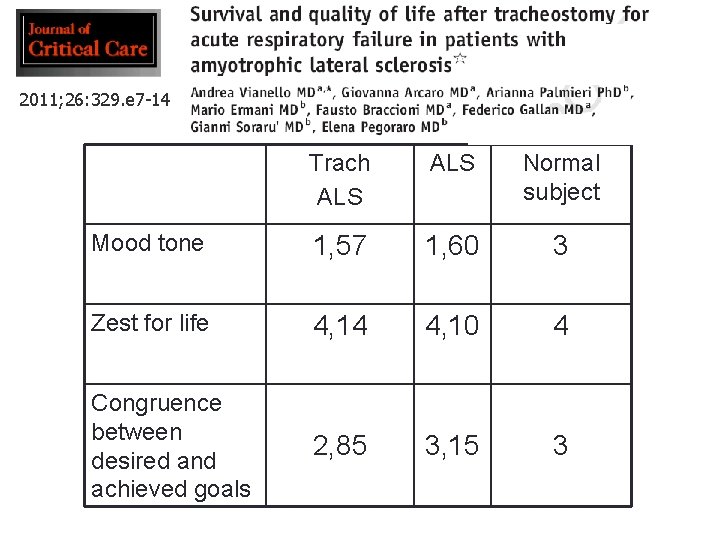
2011; 26: 329. e 7 -14 Trach ALS Normal subject Mood tone 1, 57 1, 60 3 Zest for life 4, 14 4, 10 4 Congruence between desired and achieved goals 2, 85 3, 15 3
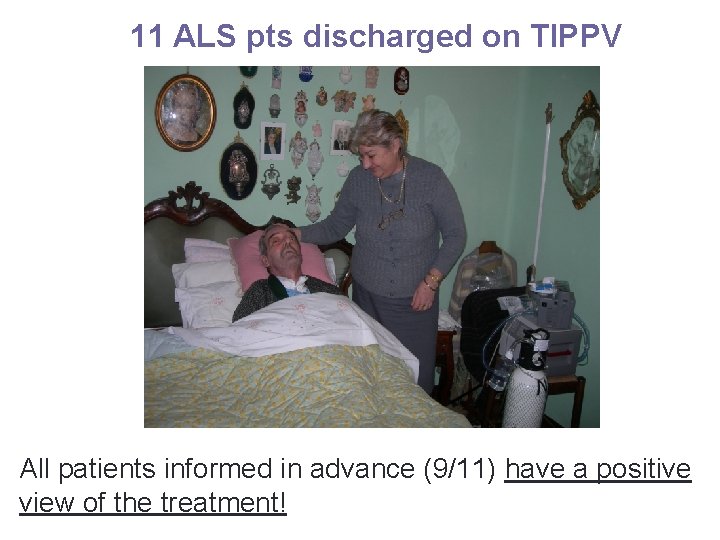
11 ALS pts discharged on TIPPV All patients informed in advance (9/11) have a positive view of the treatment!
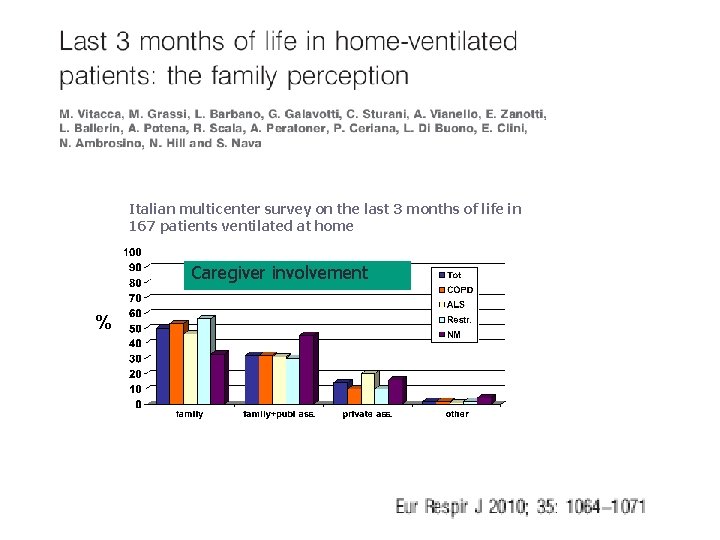
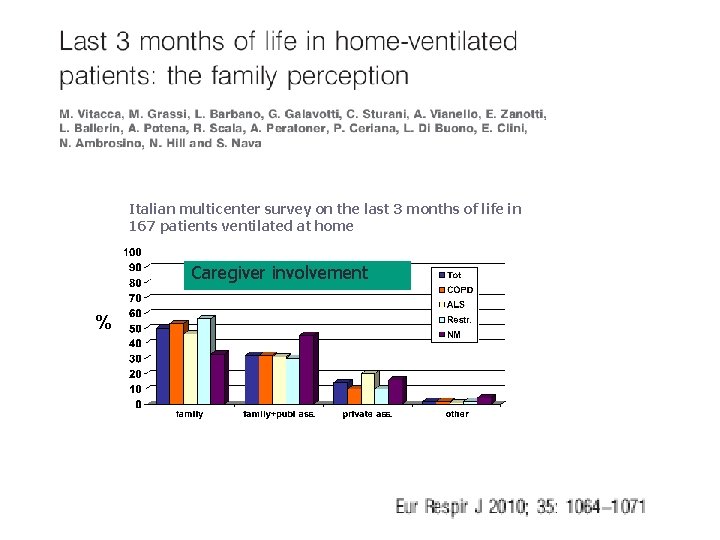
Italian multicenter survey on the last 3 months of life in 167 patients ventilated at home Caregiver involvement %
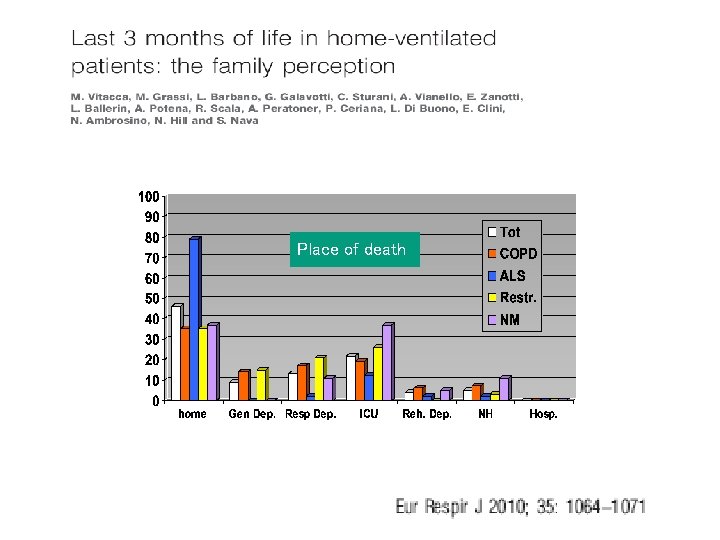
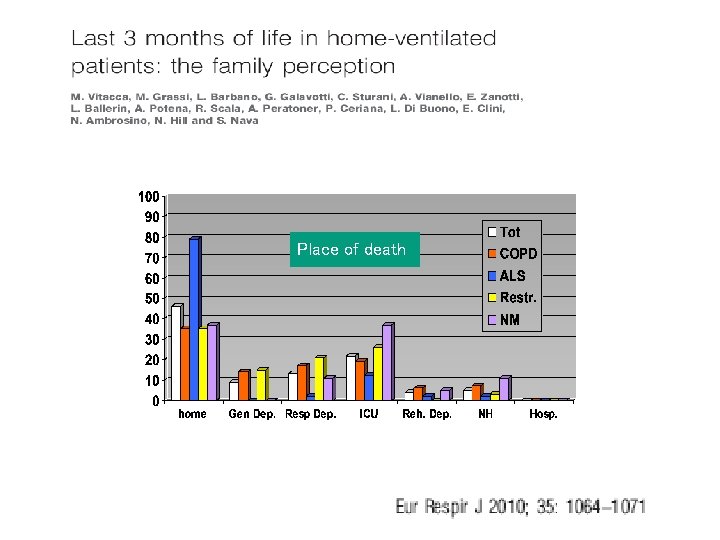
Place of death
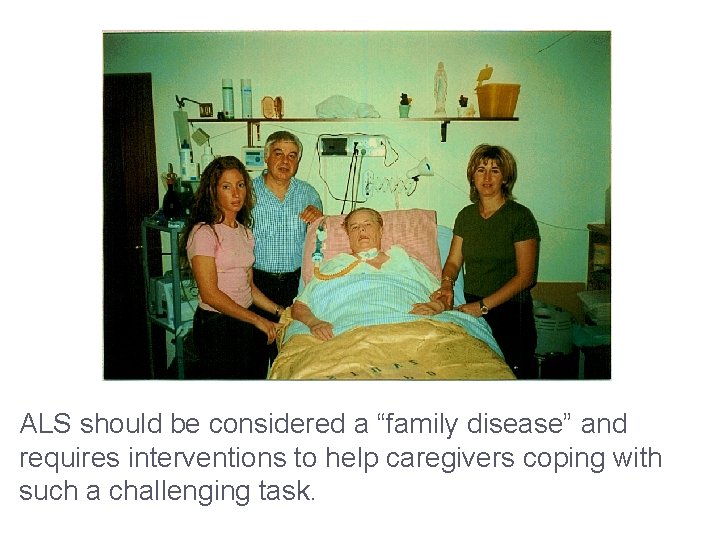
ALS should be considered a “family disease” and requires interventions to help caregivers coping with such a challenging task.

1. Most individuals with ALS develop respiratory complications; 2. NIV can be used to improve symptoms and health perception; however, patients may become increasingly dependent and unable to remove mask; 3. Patients transitioned to trach can live for many years and in a number of cases are happy with their choice.

Open questions • Which is the correct timing of starting NIV? • For which patients tracheostomy should be recommended?
 Niv terapia intensiva
Niv terapia intensiva Terapia intensiva cardiochirurgica monaldi
Terapia intensiva cardiochirurgica monaldi Ivan vianello
Ivan vianello Estrategia intensiva de penetración
Estrategia intensiva de penetración Propiedades intensivas
Propiedades intensivas Lectura intensiva concepto
Lectura intensiva concepto Rappresentazione intensiva di un insieme
Rappresentazione intensiva di un insieme Marco brunori pneumologo
Marco brunori pneumologo Filippo de marinis oncologo
Filippo de marinis oncologo Marco brunori pneumologo
Marco brunori pneumologo Dottor cottini bergamo
Dottor cottini bergamo Marco brunori pneumologo
Marco brunori pneumologo Scala di borg modificata
Scala di borg modificata Hidrorrea decidual
Hidrorrea decidual Nerofilia
Nerofilia Ligamento frenoesofágico
Ligamento frenoesofágico Maniobra de lyan
Maniobra de lyan Dmnid
Dmnid Sindrome polineuritico
Sindrome polineuritico Fisiopatologia hernia inguinal
Fisiopatologia hernia inguinal Fisiopatologia de la pancreatitis aguda
Fisiopatologia de la pancreatitis aguda Neuroglucopenia fases
Neuroglucopenia fases Etiologia de asma bronquial
Etiologia de asma bronquial Clasificacion de kramer ictericia
Clasificacion de kramer ictericia Neuroglucopenia
Neuroglucopenia Fisiopatologia pancreatitis
Fisiopatologia pancreatitis Dengue fisiopatologia
Dengue fisiopatologia Fisiopatologia intolerancia a lactose
Fisiopatologia intolerancia a lactose Cuadrilatero de fauchard
Cuadrilatero de fauchard Quemaduras fisiopatologia
Quemaduras fisiopatologia Fisiopatologia de la diarrea
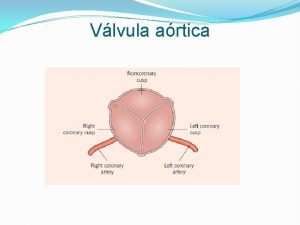
Fisiopatologia de la diarrea Right ventricle
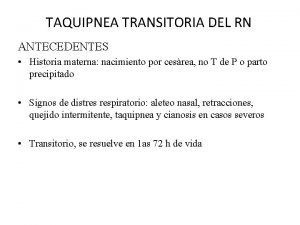
Right ventricle Fisiopatologia de taquipnea transitoria del recien nacido
Fisiopatologia de taquipnea transitoria del recien nacido Peptidos natriureticos
Peptidos natriureticos Mesangiocapilar
Mesangiocapilar Fisiopatologia de oclusion intestinal
Fisiopatologia de oclusion intestinal Edema agudo de pulmon fisiopatologia
Edema agudo de pulmon fisiopatologia Fisiopatologia de la apendicitis
Fisiopatologia de la apendicitis Www.laboratoriolacad.com.br
Www.laboratoriolacad.com.br Fisiopatologia estreñimiento
Fisiopatologia estreñimiento Clasificacion de la peritonitis
Clasificacion de la peritonitis Organofosforados fisiopatologia
Organofosforados fisiopatologia Fisiopatologia de obstruccion intestinal
Fisiopatologia de obstruccion intestinal