Clinical Informatics Its Our Time 2014 Clinical Informatics






- Slides: 81
Clinical Informatics: It’s Our Time! 2014 Clinical Informatics Academy Sponsored by DFW ANIA Chapter October 10 -11, 2014 Informatics & Quality: Pushing the Performance Envelope Debbie Schumann, RN-BC, BSN, MBA, CPHIMS Chief Nursing Informatics Officer Children’s Health. SM Children’s Medical Center 1
Conflict of Interest Disclosure Debbie Schumann, RN-BC, BSN, MBA, CPHIMS has no real or apparent conflicts of interest to report.
Session Objectives � Describe the intersection between the practice of informatics and quality/performance improvement in healthcare � Discuss examples of how informatics and quality practitioners collaborate to support the attributes of a high reliability organization � Describe the Davies Award experience at Children’s and THR and provide case studies 3
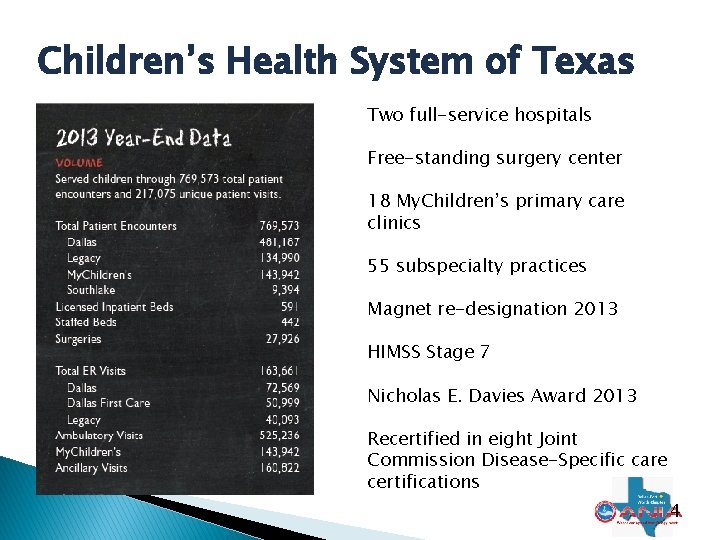
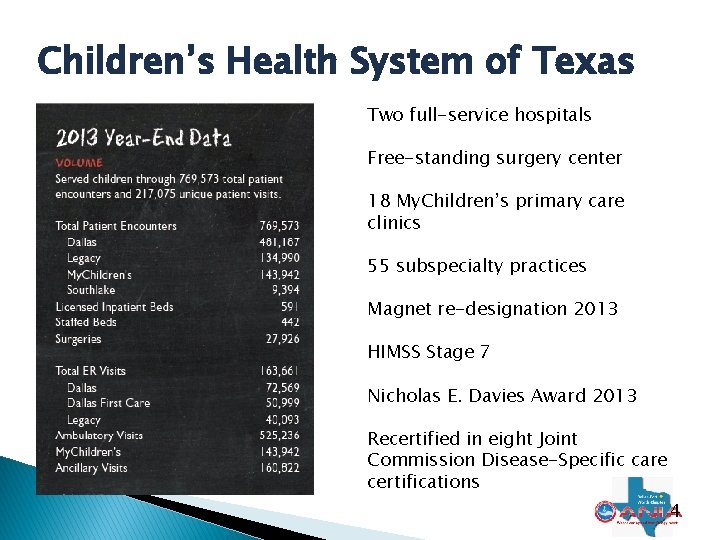
Children’s Health System of Texas Two full-service hospitals Free-standing surgery center 18 My. Children’s primary care clinics 55 subspecialty practices Magnet re-designation 2013 HIMSS Stage 7 Nicholas E. Davies Award 2013 Recertified in eight Joint Commission Disease-Specific care certifications 4

5
Guess What? � Informatics is not all about EHR Implementation ◦ Bar Coded Medication Administration ◦ Virtual Desktop with Tap and Go ◦ Davies Award ◦ Language Access Services Success ◦ Where are we going from here? 6
Bar Coded Medication Administration BCMA � Live on BCMA since 2001 � Currently on 3 rd vendor � Most kinks are worked out � How have we been successful? � Have errors been eliminated? 7
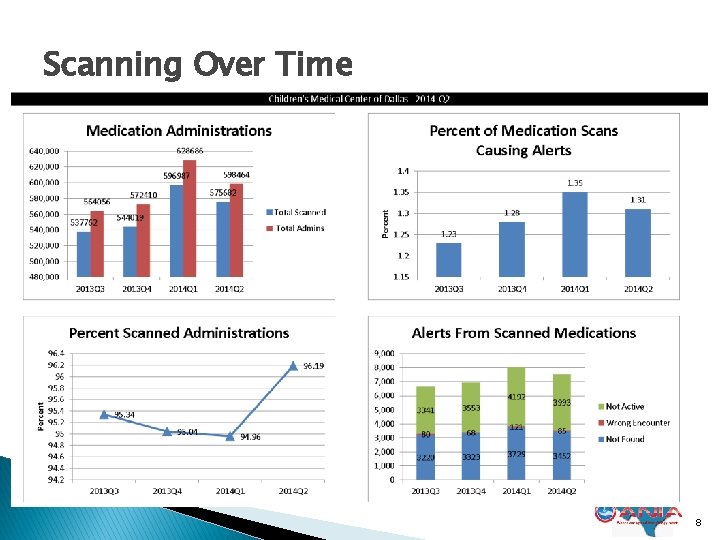
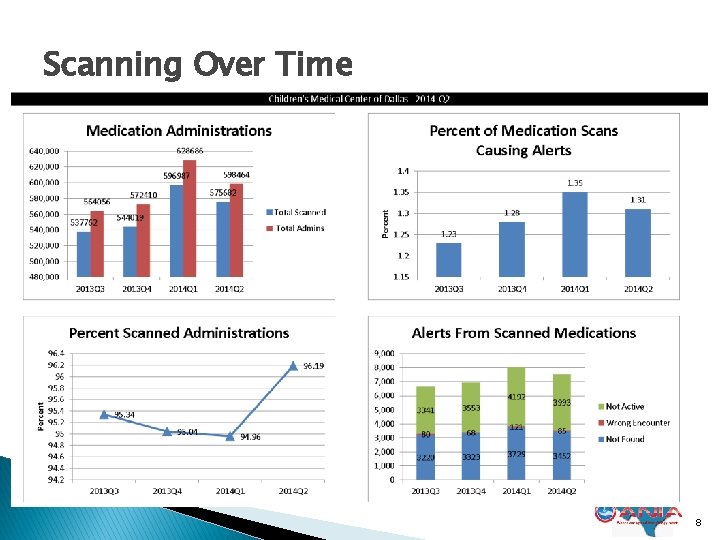
Scanning Over Time 8
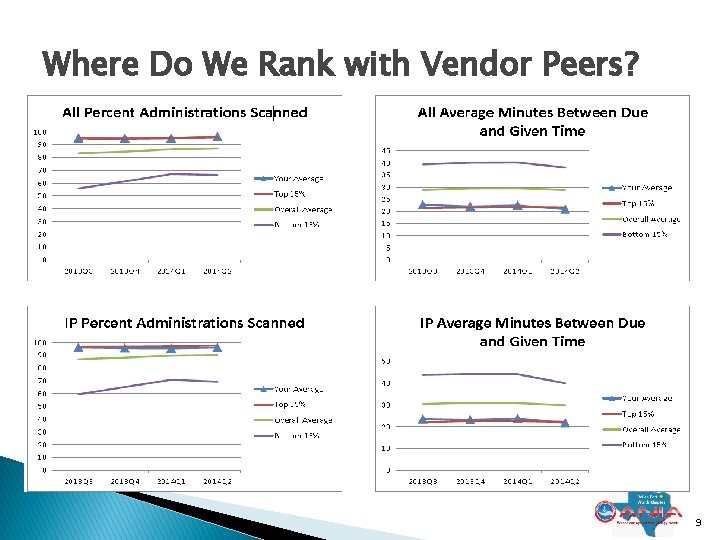
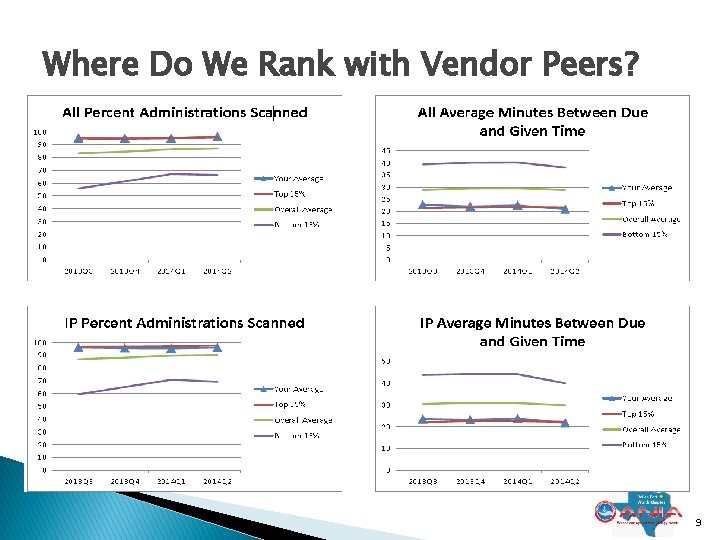
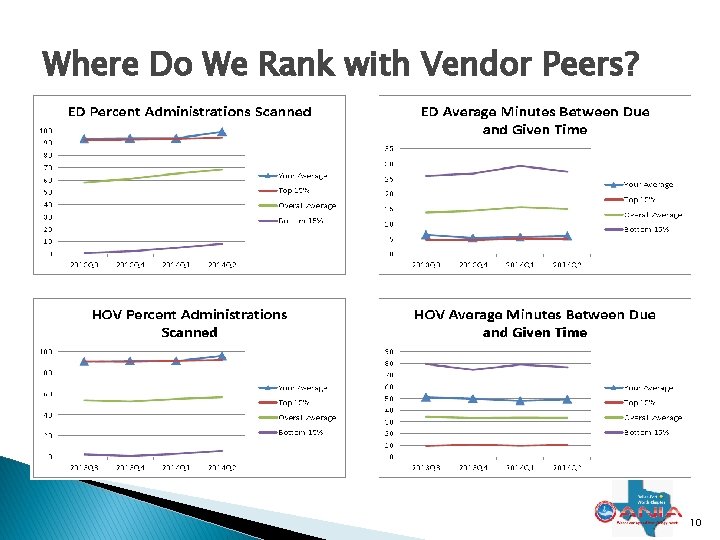
Where Do We Rank with Vendor Peers? � 9
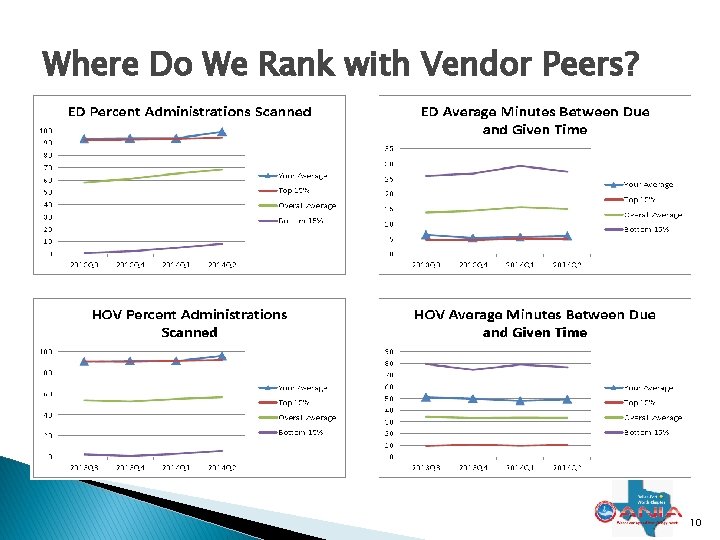
Where Do We Rank with Vendor Peers? 10
Near Miss Tracking: Good or Bad? � Instinct for a manager might be to whack for near miss � In reality the BCMA solution is doing it’s job, preventing a clinician from making an unrecognized error. � We distribute the Near Miss report with our Barcode compliance report monthly to all nursing radiology and respiratory leaders 11
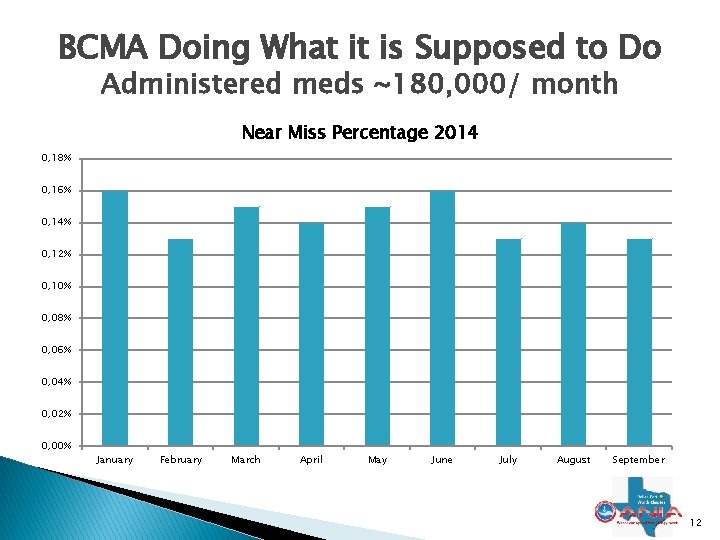
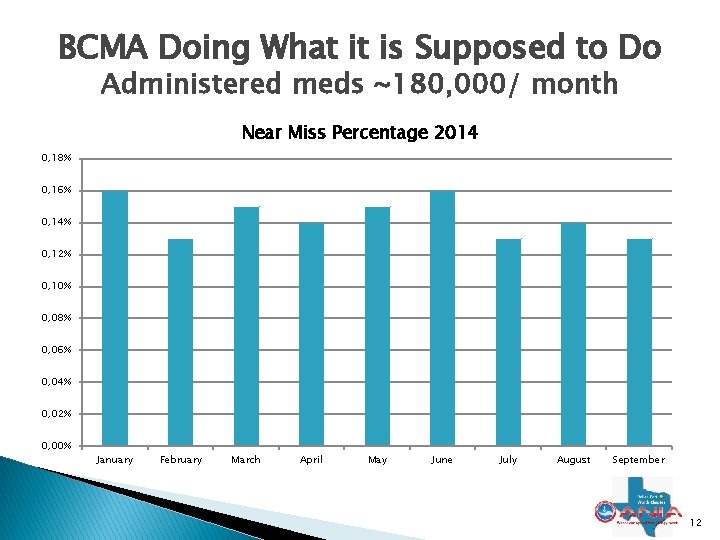
BCMA Doing What it is Supposed to Do Administered meds ~180, 000/ month Near Miss Percentage 2014 0, 18% 0, 16% 0, 14% 0, 12% 0, 10% 0, 08% 0, 06% 0, 04% 0, 02% 0, 00% January February March April May June July August September 12
Where Does Medication Safety Go Next � Medication Errors continue when programming a pump manually � Most of our serious safety events occur when �Humans do not follow the prescribed process �Humans are required to enter data � What do we do to push the quality envelope? � Infusion Pump Integration of Course! 13
Virtual Desktop Infrastructure (VDI) with Tap and Go Access • A virtual desktop infrastructure (VDI) is an architecture where core software is hosted in a central location and accessed by users via a thin or zero client
VDI continued • Thin or zero clients are small, streamlined operating systems used to access the VDI environment • No storage is available on these clients • Server side printing is generally required • Tap and Go technology allows users to log in and swap between thin/zero clients using their identification badge • Password is entered once per 24 hours • Uses existing ID badges 15
Clinical Informatics and VDI � The role of clinical informatics in VDI ◦ Proponents for the implementation ◦ Stakeholders in the vendor selection ◦ Coordinators of the initial introduction to clinical staff ◦ Coordinators of the pilot plan and subsequent production rollout schedule ◦ Testing, Testing and wait for it… Testing ◦ Teaching IS analysts what and how to test ◦ On site support for pilots 16
Additional Clinical Informatics Participation � Collaboration on the initial design of VDI to optimize clinician benefit � Testing clinical functions from VDI prior to piloting with first clinical audience � Liaising with clinicians on the added benefits of tap-and-go, a faster clinical workstation, and changes to Epic functionality � Facilitating conversations during clinician pilots ensure VDI is tuned to meet basic and optimal end user needs 17
The Value for Clinicians • • • Reduce time spent logging in “Follow me” desktops Consistent user experience More point of care/real time charting Easy, fast access to patient information
Clinical Informatics Pilot • • • Two-week hands-on experience for the Clinical Informatics team Enroll Children’s ID badges for Tap-and-Go Log in and swap between VDI clients with a badge tap Note reduction in time spent logging in and swapping between desktops Access One. Chart and Epic test environments Identify any further enhancement needs
Operational VDI Pilot � 2 weeks on 2 inpatient units and 1 ambulatory clinic � Great feedback from staff regarding speed and ease of access � Requested several desktop computers be reconfigured to zero clients with tap and go � Deployment to remainder of the inpatient units by end of 2014
Outcomes of Pilot � 90% acceptance of use of VDI and tap and go � Confirmation that project is ready to move to other units � Had to reconfigure all LWS records in order to print properly � Providers are anxious for phase two which will include access to shared drives 21
Nicholas E. Davies Award 2013 � Since 1994, the HIMSS Nicholas E. Davies Award of Excellence has recognized outstanding achievement in the implementation and value from health information technology, specifically EHRs. � Awarded in 2013 to ◦ Children’s Medical Center now Children’s Health. SM ◦ Texas Health Resources ◦ UC Davis Medical Center 22
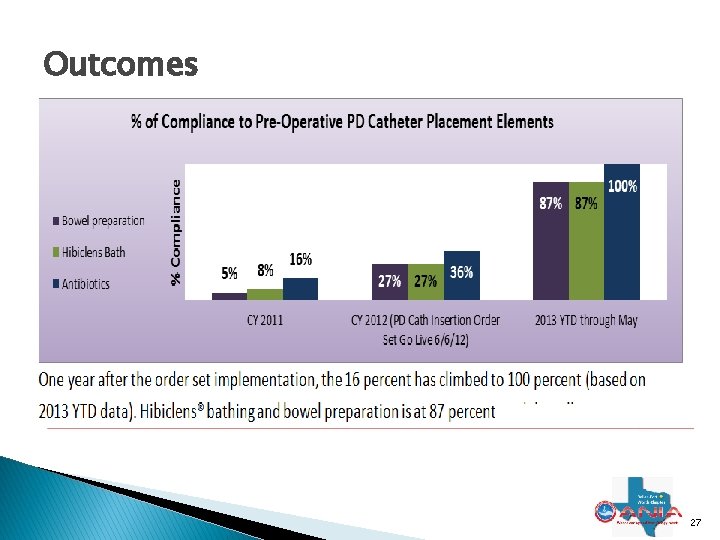
Davies Award Case Study • Conversion to CPOE did not translate always to increased safety and efficiency • The problem: • Fall of 2011 and into the spring of 2012, Children’s was experiencing about 20% more frequent than average cases of peritonitis in ESRD patients • The solution: • • • Consult with the clinical informatics department Understand the requirements, define success Analyze workflows for multiple roles Develop a plan Build and Implement the tools to drive to success Evaluate Outcomes
CPOE: a Menu Case Study: The Solution � Consult with the clinical informatics department • A clinical informaticist: • Developed understanding of the issue • Identified stakeholders and expectations • Drove the solution in conjunction with clinicians and IS analysts � Understand the requirements, define success • Documented the requirements and expected outcomes • IV antibiotics within 60 minutes of the surgical incision 100% compliance • Hibiclens® cleansing of patient’s trunk prior to surgery 100% compliance • Bowel cleanout prior to surgery (day prior) 100% compliance � Analyze workflows for multiple roles • In and outpatient workflows for nurses, providers and medical assistants • OR and peri op workflows for nurses and providers 24
CPOE: a Menu Case Study: The Solution � • • Develop a plan Order set available only to Nephrologists regardless of location One stop shop for order entry, highly intuitive Trigger required downstream events Integrate clinical decision support tools • Automatically suggest alternate antibiotic if patient had allergy to Penicillin • Automatically populate the Patient Education activity with appropriate topics • Real-time notification to PD nurse manager • Real-time pre op checklist driven by orders and documentation • Design a mechanism to reduce repetitive manual chart audits � � � Build and Implement the tools to drive to success Went live June 2012 Evaluate outcomes 25

CPOE: a Menu Case Study: The Solution � Build and Implement the tools to drive to success • Went live June 2012 with the orders and tools 26
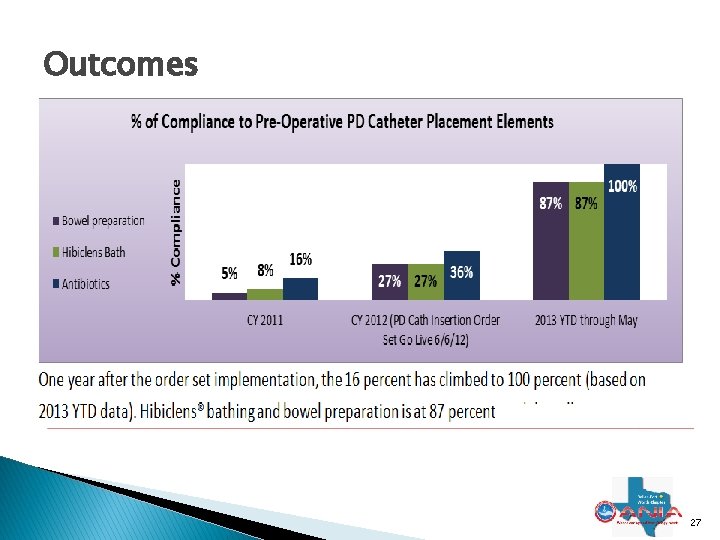
Outcomes t 27
What else is there? � Language Access Services Project � The never-ending list of requests for our expertise (more on that one) 28
Language Access Services (LAS) Success � Why did we need to improve access to LAS? � How was Clinical Informatics involved? � How did we improve access to LAS for clinicians? � What were the Outcomes? Did Clinical Informatics make a difference? 29
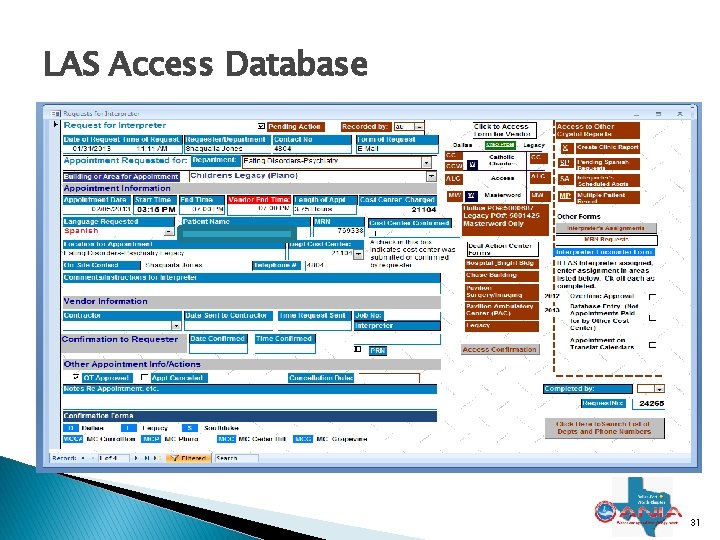
Why Improve Access to Language Access Services? � 24% of Children’s patients/families speak a language other than English ◦ 97% of those have Spanish as their primary or preferred language ◦ Spanish Language translation/interpretation is key to providing excellent care to patients � Translation needs were cited by clinicians as a reason for discharge delay � LAS tracked all translation/interpretation activities in an Access database ◦ Needed for them to produce the statistics 30
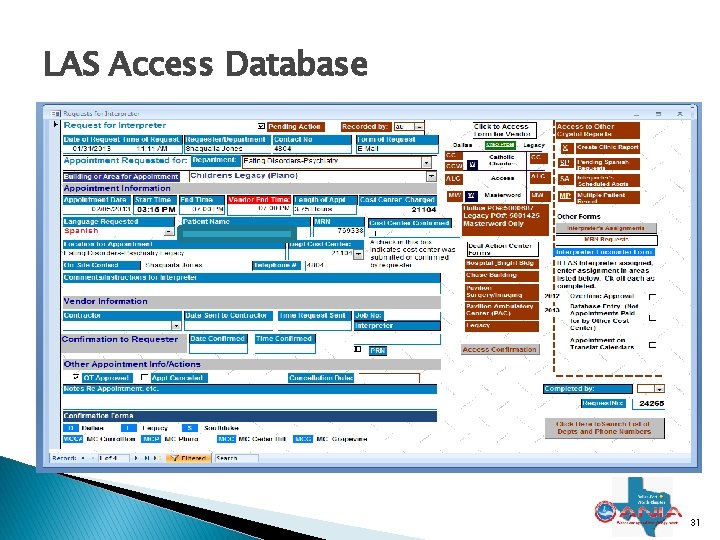
LAS Access Database 31
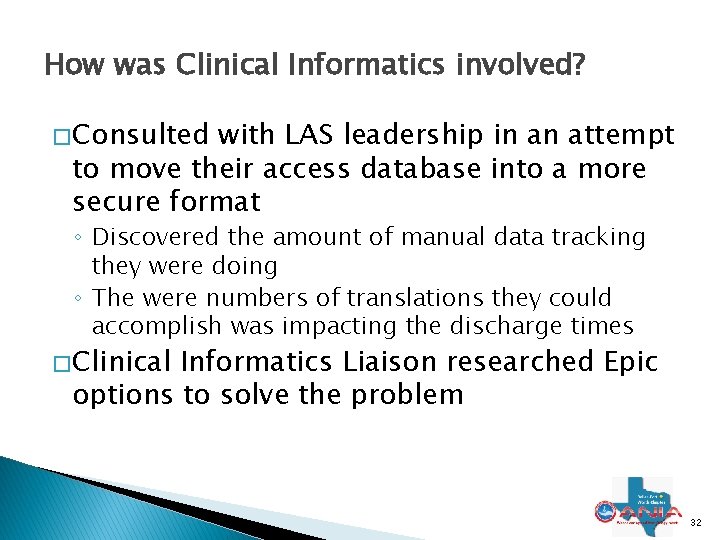
How was Clinical Informatics involved? � Consulted with LAS leadership in an attempt to move their access database into a more secure format ◦ Discovered the amount of manual data tracking they were doing ◦ The were numbers of translations they could accomplish was impacting the discharge times � Clinical Informatics Liaison researched Epic options to solve the problem 32
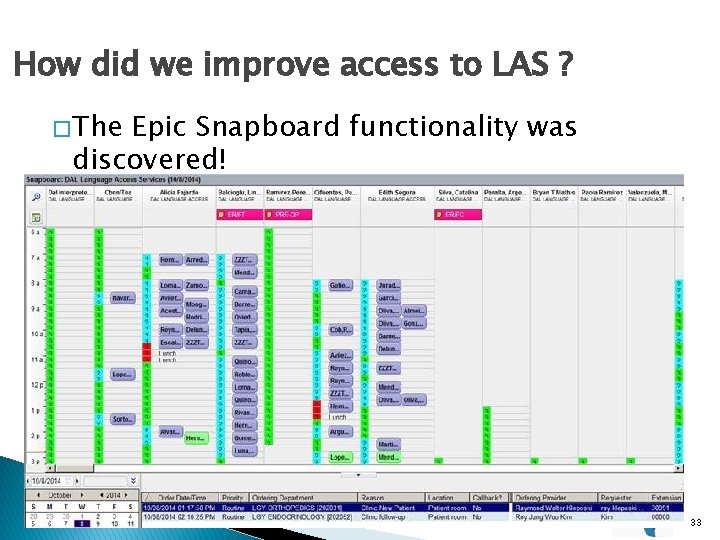
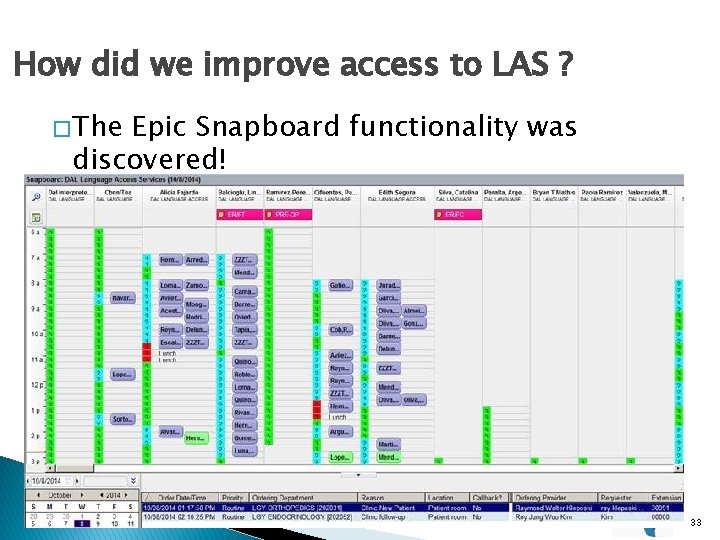
How did we improve access to LAS ? � The Epic Snapboard functionality was discovered! 33
What were the Outcomes? � Centralized service and resources by allowing the same dispatcher to assist several campuses at the same time � Reduced the cost associated with staffing by eliminating the need to have dispatcher coverage 24/7 � Increased efficiency by allowing the interpreters to see the orders and respond real time. � Reduced the time needed for the clinicians to enter a request for LAS � Increased patient, provider and interpreter’s satisfaction � eliminated the need to answer the pagers and phone during the encounter 34
What were the Outcomes? � Provides accurate reports with accurate times (no manual transcription of data) � Extra support can be provided from one team to another by reviewing Snapboard activity � Dispatcher can access interpreters from different campuses to support each other with discharge instructions � Automatic order confirmation: The provider receives a confirmation when the order has been assigned to an interpreter (including the name of the interpreter) � Reduces the length of encounter by eliminating interruption � Allows the interpreters to work with a virtual dispatcher 35
Other Quality Specific Impact � Participate in Clinical Guideline development � Review all safety events with quality team � Liaison between IS and Clinical operations for bundle development and build � Review all HIT, Clinical Device incidents as reported by staff… 8 -10 per month � Review all medication incidents weekly 36
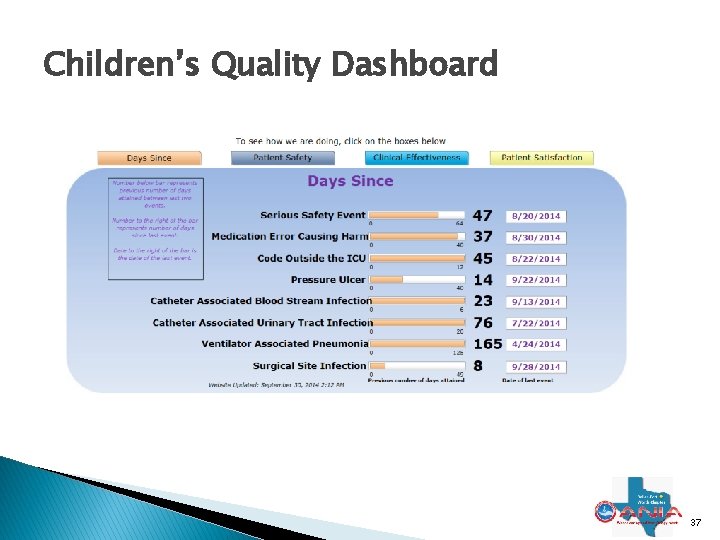
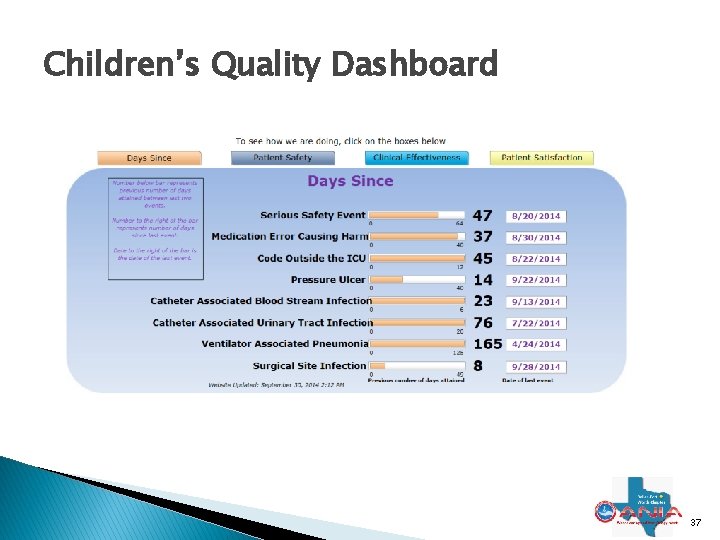
Children’s Quality Dashboard 37
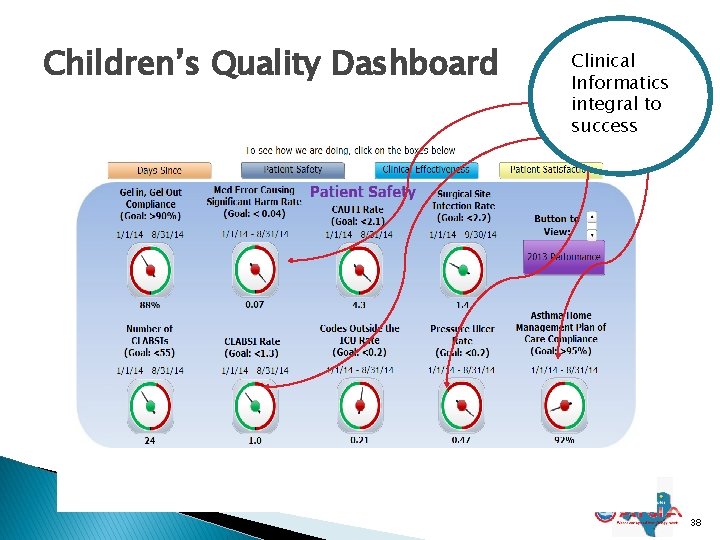
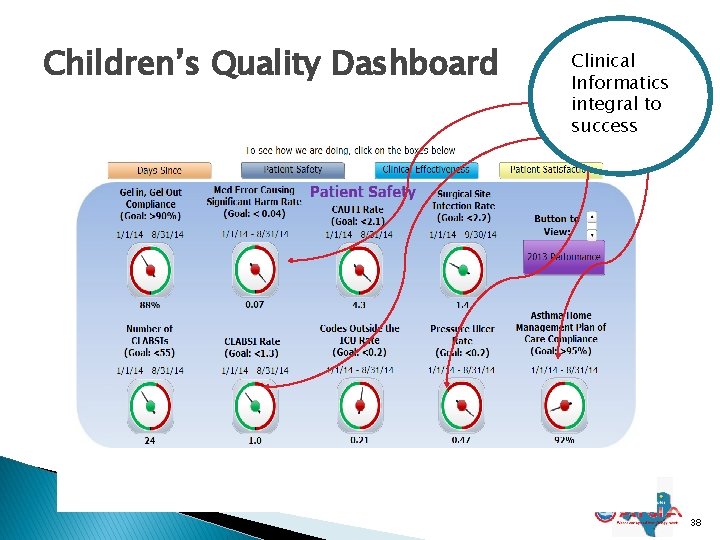
Children’s Quality Dashboard Clinical Informatics integral to success 38
Thank you for your time Questions after entire presentation � Debbie Schumann RN-BC, BSN, MBA, CPHIMSS ◦ CNIO ◦ Children’s Health. SM, Children’s Medical Center ◦ debra. schumann@childrens. com 39
Clinical Informatics: It’s Our Time! 2014 Clinical Informatics Academy Sponsored by DFW ANIA Chapter October 10 -11, 2014 Informatics & Quality: Pushing the Performance Envelope Mary Beth Mitchell, MSN, RN, BC, CPHIMS CNIO Texas Health Resources 40

Conflict of Interest Disclosure Mary Beth Mitchell has no real or apparent conflicts of interest to report.

Texas Health Mission To improve the health of the people in the communities we serve Texas Health Vision Texas Health Resources, a faith-based organization joining with physicians, will be the health care system of choice Innovative Technology Solutions Innovate, transform, and serve

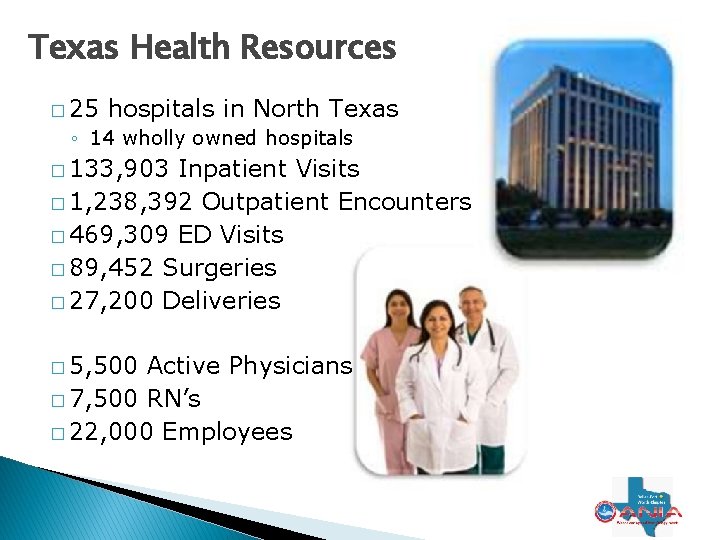
Texas Health Resources � 25 hospitals in North Texas ◦ 14 wholly owned hospitals � 133, 903 Inpatient Visits � 1, 238, 392 Outpatient Encounters � 469, 309 ED Visits � 89, 452 Surgeries � 27, 200 Deliveries � 5, 500 Active Physicians � 7, 500 RN’s � 22, 000 Employees
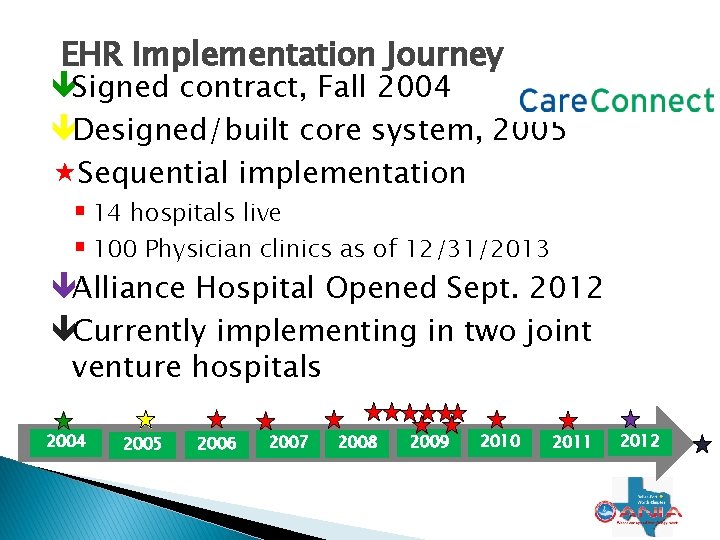
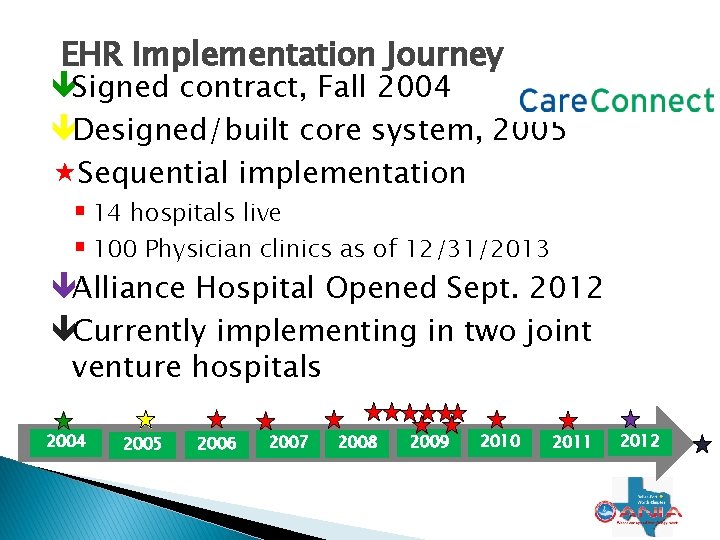
EHR Implementation Journey Signed contract, Fall 2004 Designed/built core system, 2005 Sequential implementation 14 hospitals live 100 Physician clinics as of 12/31/2013 Alliance Hospital Opened Sept. 2012 Currently implementing in two joint venture hospitals 2004 2005 2006 2007 2008 2009 2010 2011 2012
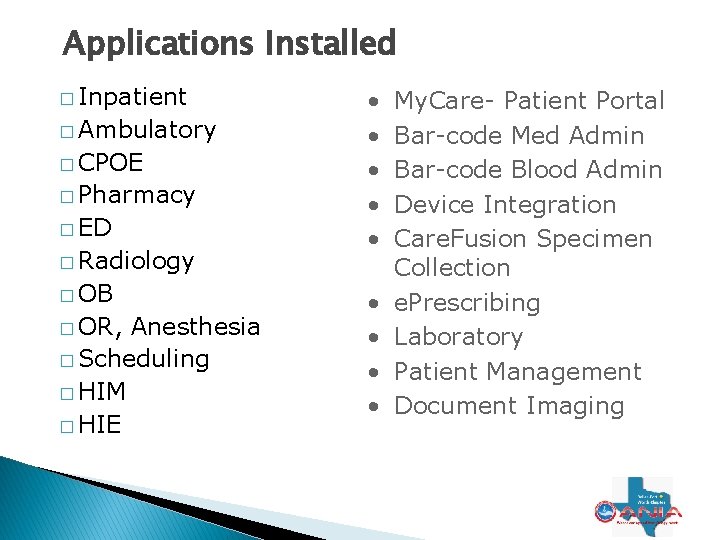
Applications Installed � Inpatient � Ambulatory � CPOE � Pharmacy � ED � Radiology � OB � OR, Anesthesia � Scheduling � HIM � HIE • • • My. Care- Patient Portal Bar-code Med Admin Bar-code Blood Admin Device Integration Care. Fusion Specimen Collection e. Prescribing Laboratory Patient Management Document Imaging
THR Value Proposition
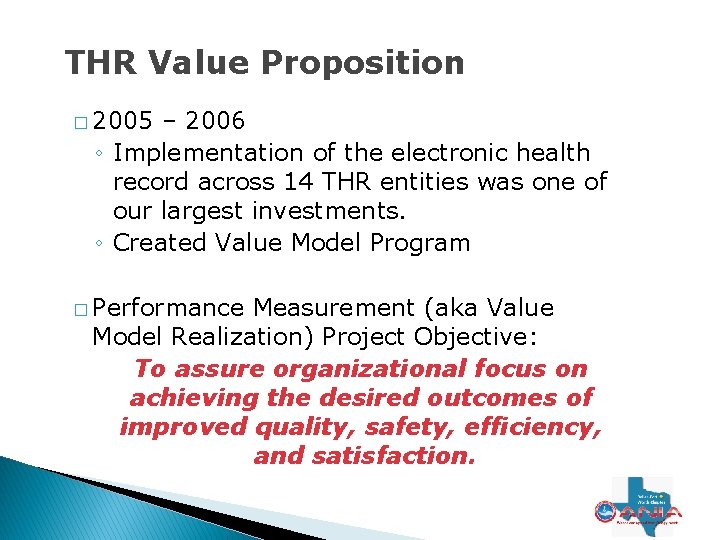
THR Value Proposition � 2005 – 2006 ◦ Implementation of the electronic health record across 14 THR entities was one of our largest investments. ◦ Created Value Model Program � Performance Measurement (aka Value Model Realization) Project Objective: To assure organizational focus on achieving the desired outcomes of improved quality, safety, efficiency, and satisfaction.
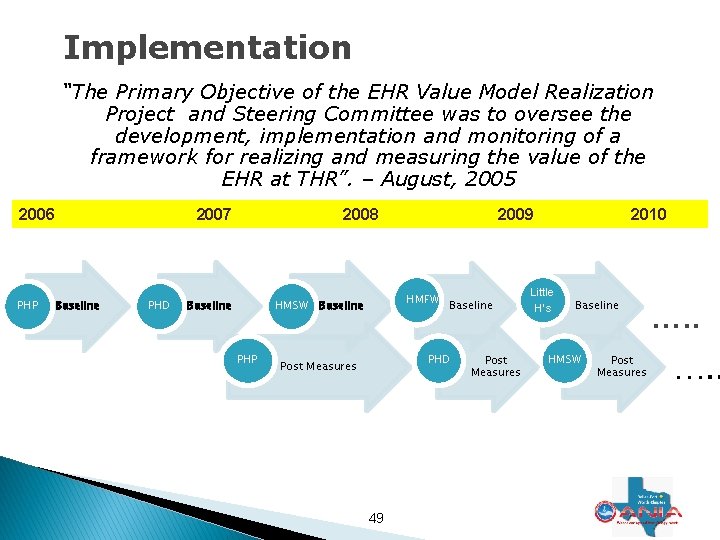
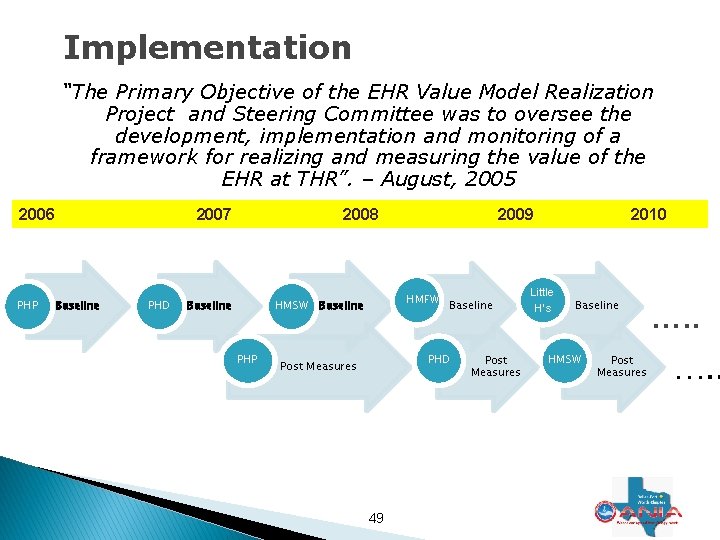
Implementation “The Primary Objective of the EHR Value Model Realization Project and Steering Committee was to oversee the development, implementation and monitoring of a framework for realizing and measuring the value of the EHR at THR”. – August, 2005 2006 PHP 2007 Baseline PHD 2008 Baseline HMSW PHP 2009 HMFW Baseline PHD Post Measures 49 Post Measures 2010 Little H’s Baseline HMSW Post Measures …. .
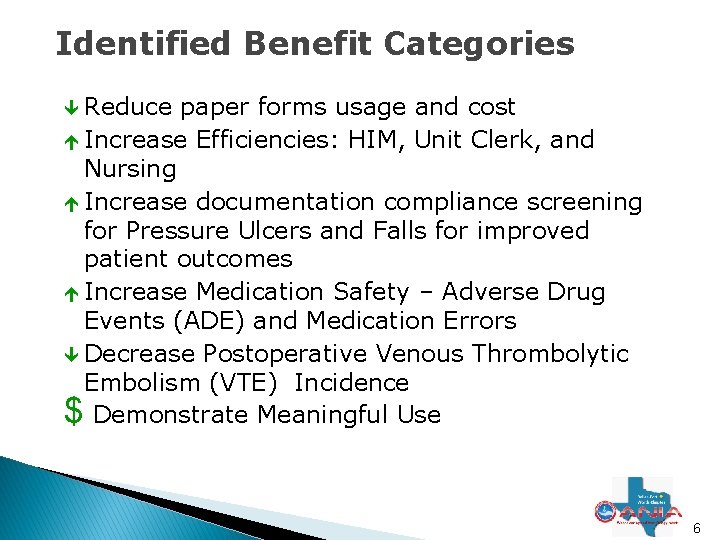
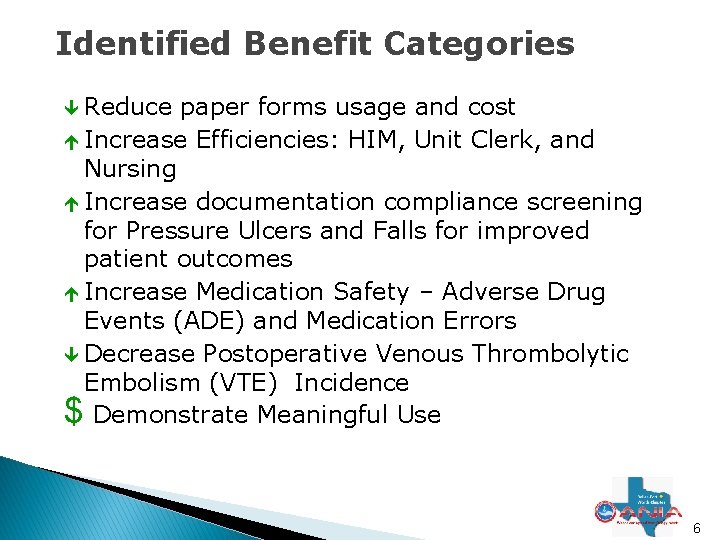
Identified Benefit Categories Reduce paper forms usage and cost é Increase Efficiencies: HIM, Unit Clerk, and Nursing é Increase documentation compliance screening for Pressure Ulcers and Falls for improved patient outcomes é Increase Medication Safety – Adverse Drug Events (ADE) and Medication Errors Decrease Postoperative Venous Thrombolytic Embolism (VTE) Incidence $ Demonstrate Meaningful Use 6
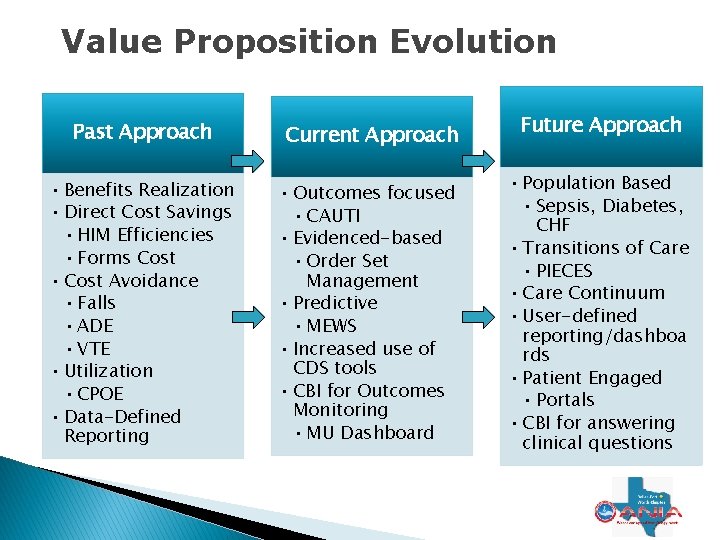
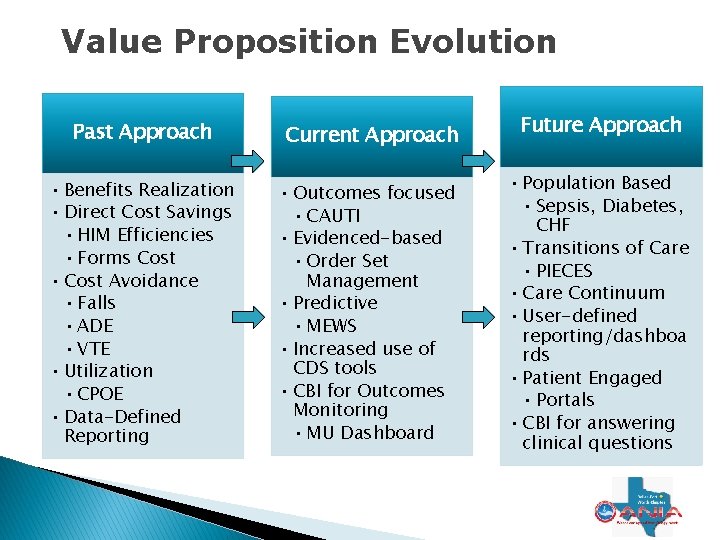
Value Proposition Evolution Past Approach Current Approach • Benefits Realization • Direct Cost Savings • HIM Efficiencies • Forms Cost • Cost Avoidance • Falls • ADE • VTE • Utilization • CPOE • Data-Defined Reporting • Outcomes focused • CAUTI • Evidenced-based • Order Set Management • Predictive • MEWS • Increased use of CDS tools • CBI for Outcomes Monitoring • MU Dashboard Future Approach • Population Based • Sepsis, Diabetes, CHF • Transitions of Care • PIECES • Care Continuum • User-defined reporting/dashboa rds • Patient Engaged • Portals • CBI for answering clinical questions
Clinical Value
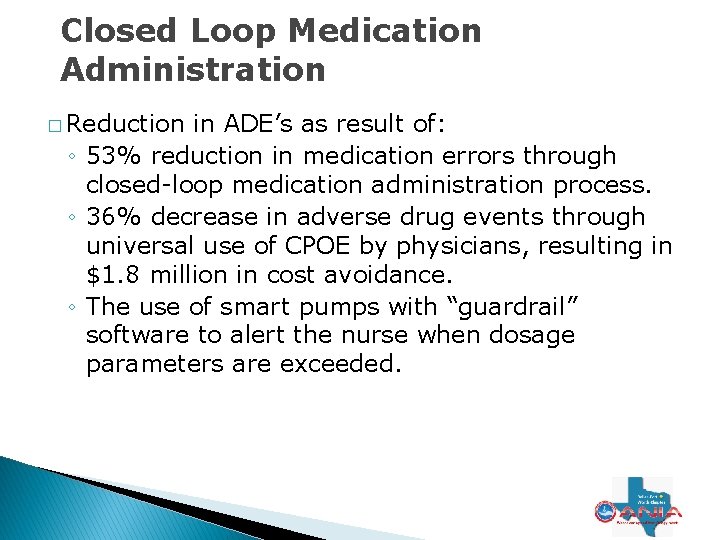
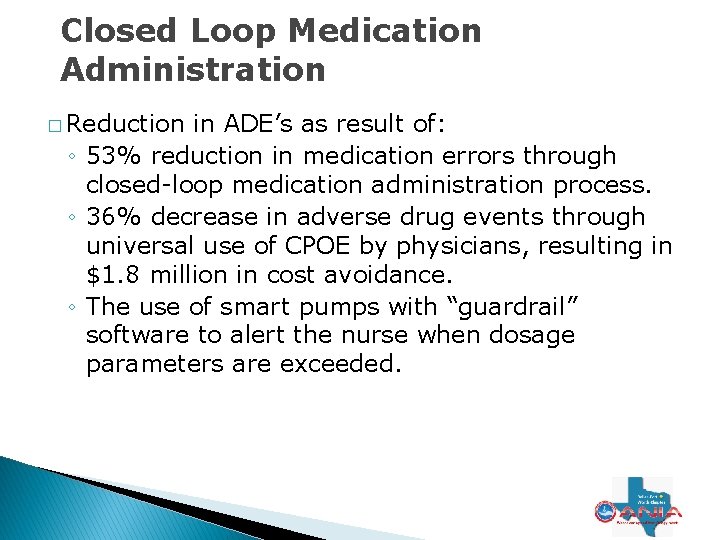
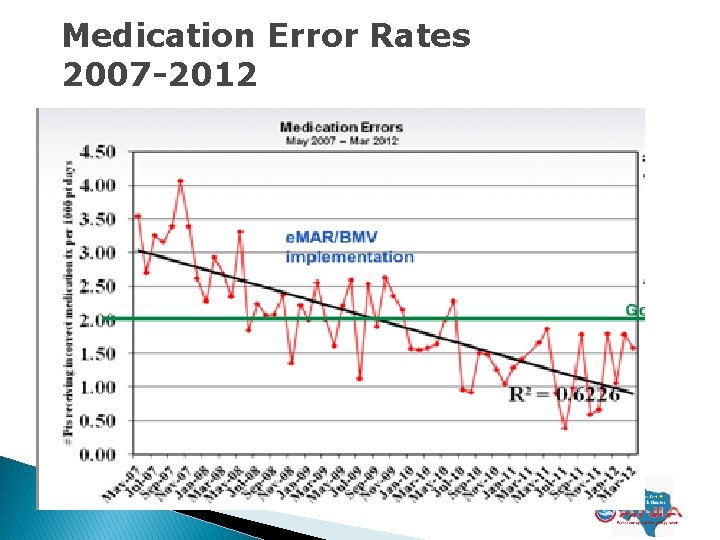
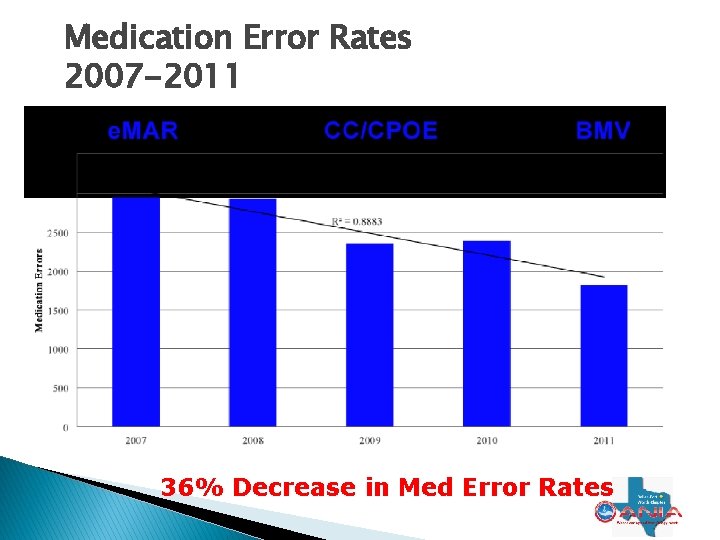
Closed Loop Medication Administration � Reduction in ADE’s as result of: ◦ 53% reduction in medication errors through closed-loop medication administration process. ◦ 36% decrease in adverse drug events through universal use of CPOE by physicians, resulting in $1. 8 million in cost avoidance. ◦ The use of smart pumps with “guardrail” software to alert the nurse when dosage parameters are exceeded.
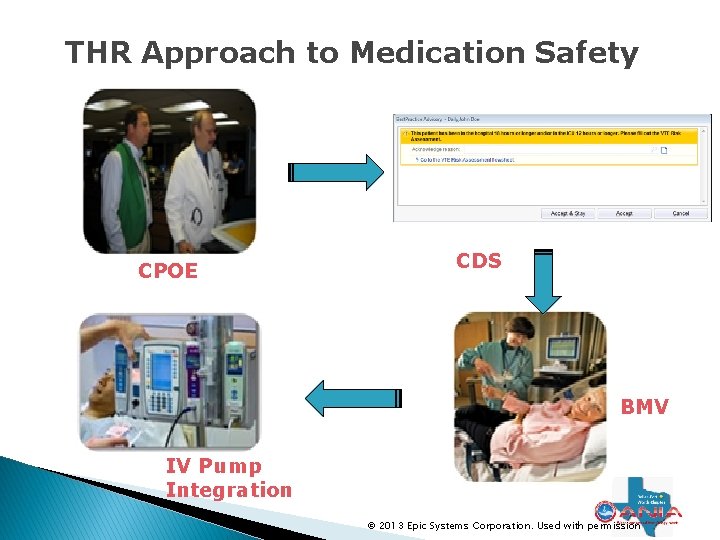
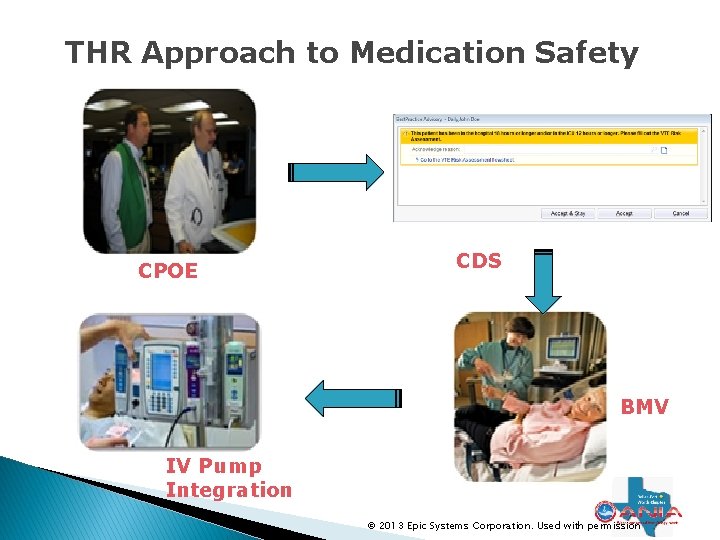
THR Approach to Medication Safety CPOE CDS BMV IV Pump Integration © 2013 Epic Systems Corporation. Used with permission
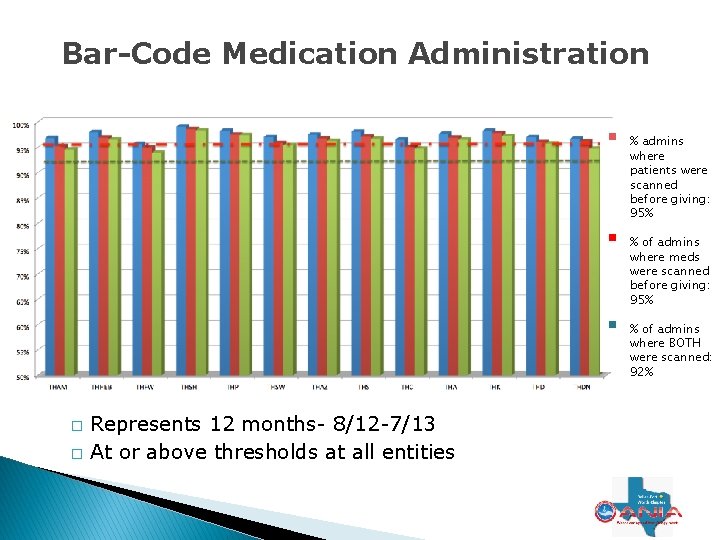
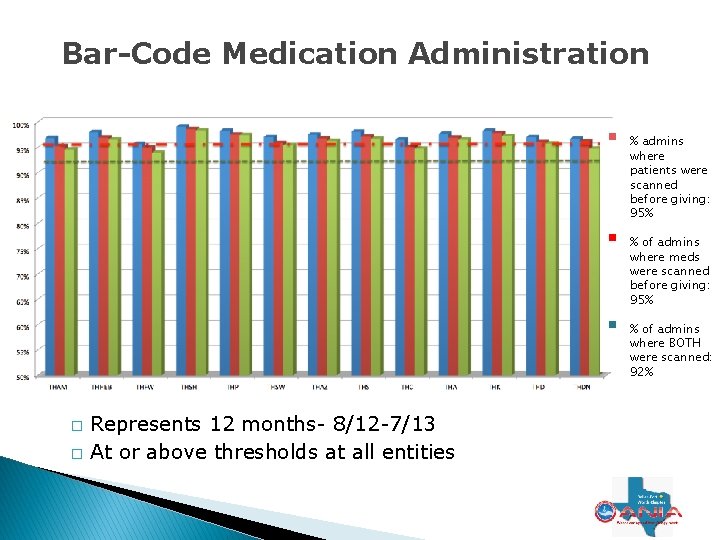
Bar-Code Medication Administration � � Represents 12 months- 8/12 -7/13 At or above thresholds at all entities % admins where patients were scanned before giving: 95% % of admins where meds were scanned before giving: 95% % of admins where BOTH were scanned: 92%
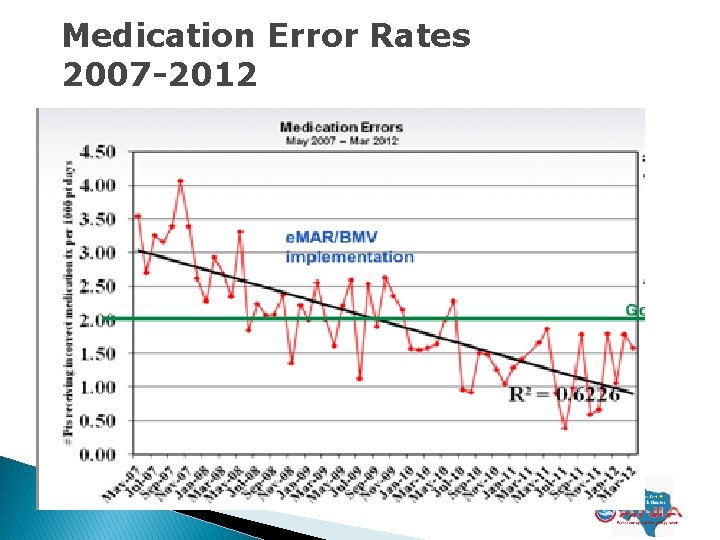
Medication Error Rates 2007 -2012
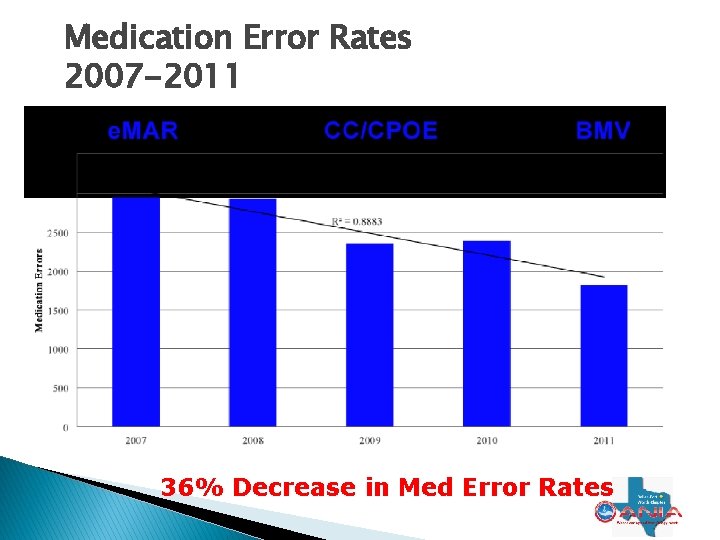
Medication Error Rates 2007 -2011 36% Decrease in Med Error Rates
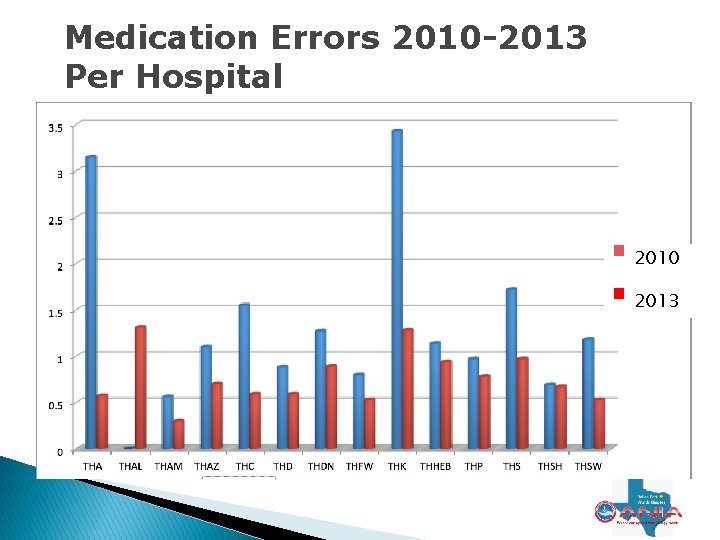
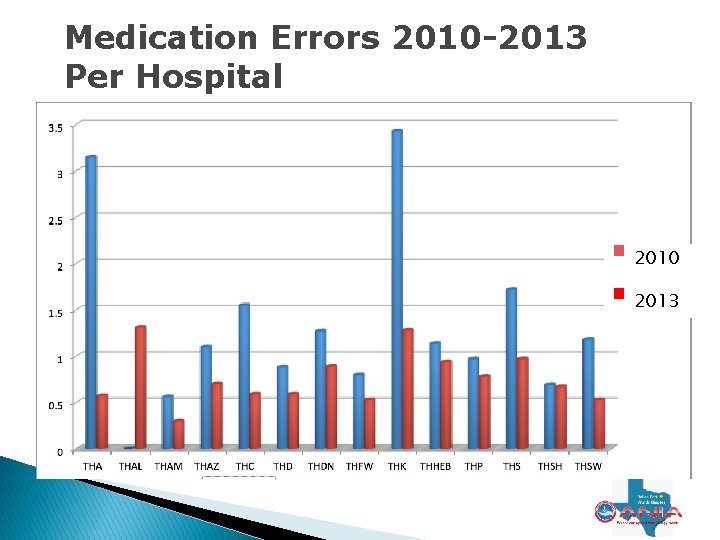
Medication Errors 2010 -2013 Per Hospital 2010 2013
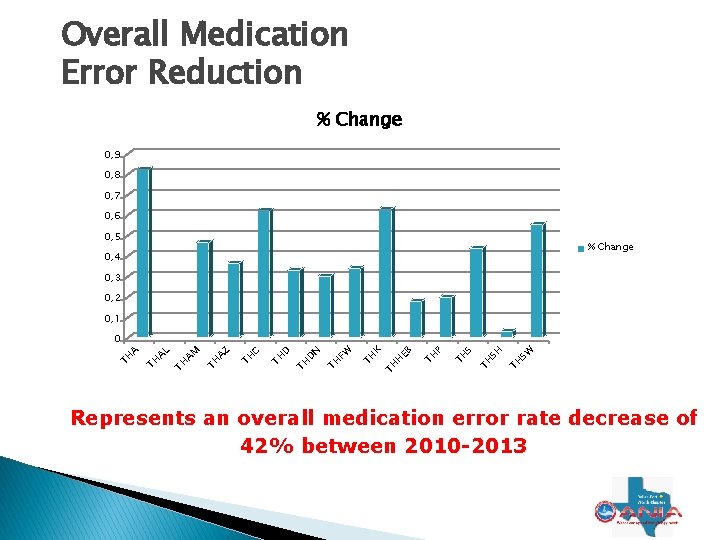
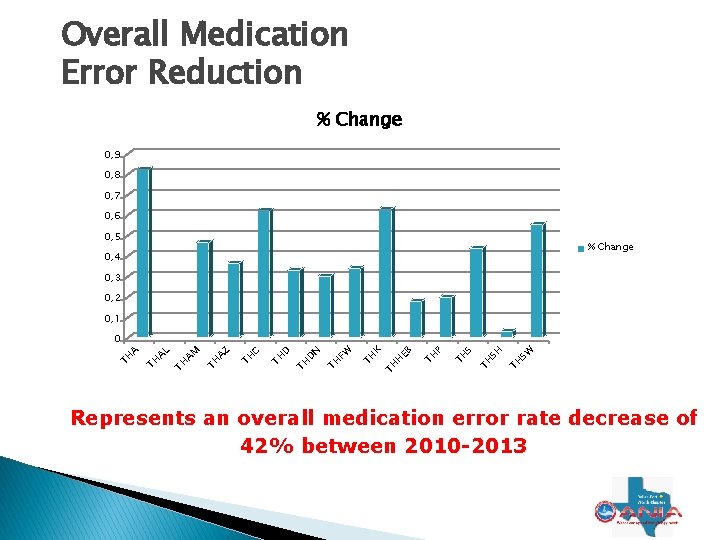
Overall Medication Error Reduction % Change 0, 9 0, 8 0, 7 0, 6 0, 5 % Change 0, 4 0, 3 0, 2 0, 1 SW TH SH TH S TH P TH H EB K TH TH FW TH N D TH C TH AZ TH AM TH AL TH TH A 0 Represents an overall medication error rate decrease of 42% between 2010 -2013
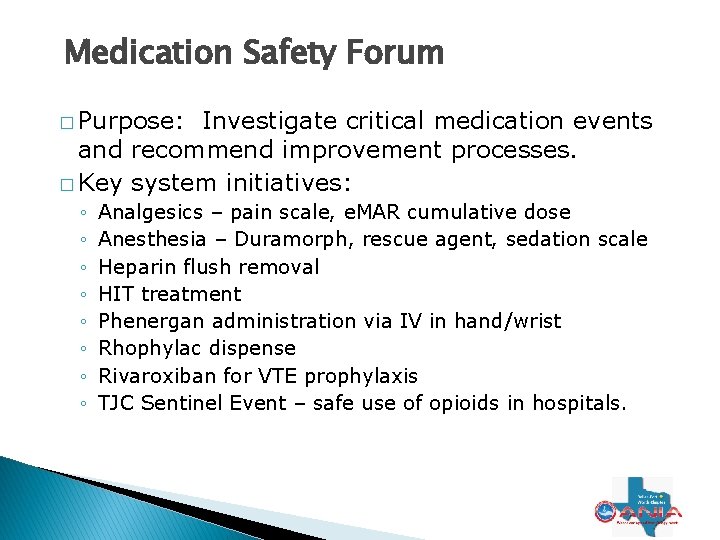
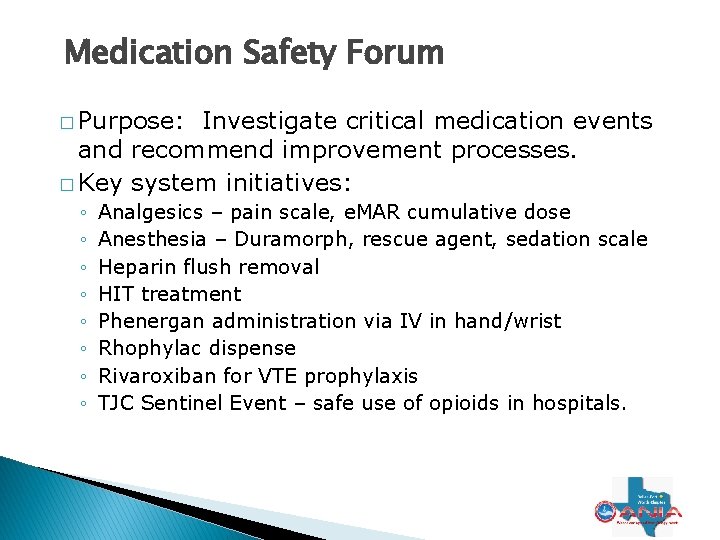
Medication Safety Forum � Purpose: Investigate critical medication events and recommend improvement processes. � Key system initiatives: ◦ ◦ ◦ ◦ Analgesics – pain scale, e. MAR cumulative dose Anesthesia – Duramorph, rescue agent, sedation scale Heparin flush removal HIT treatment Phenergan administration via IV in hand/wrist Rhophylac dispense Rivaroxiban for VTE prophylaxis TJC Sentinel Event – safe use of opioids in hospitals.
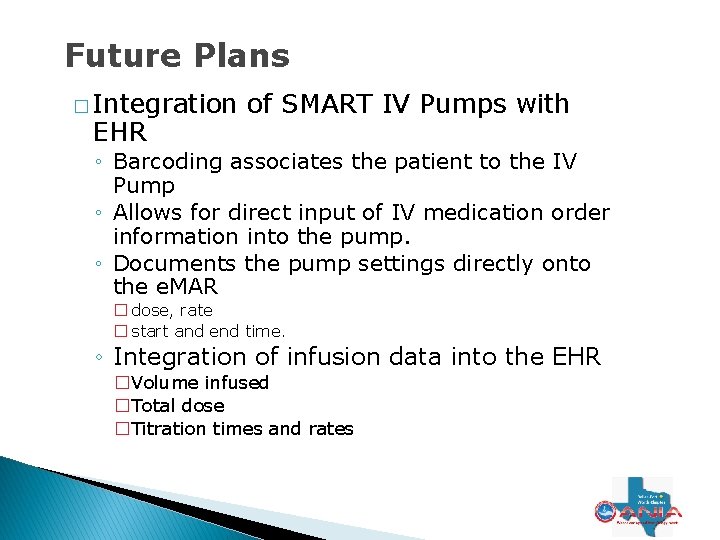
Future Plans � Integration EHR of SMART IV Pumps with ◦ Barcoding associates the patient to the IV Pump ◦ Allows for direct input of IV medication order information into the pump. ◦ Documents the pump settings directly onto the e. MAR � dose, rate � start and end time. ◦ Integration of infusion data into the EHR �Volume infused �Total dose �Titration times and rates
Modified Early Warning System
Modified Early Warning System - MEWS � � � Evidenced-based predictive tool that indicates patients at risk of cardiac arrest. Proactive management of patients before they experience significant clinical events that negatively impact their recovery. EHR facilitates clinician’s ability to aggregate patient information to make care decisions sooner. MEWS project designed to bring relevant information to the registered nurse with which to make immediate care decisions in critical situations. The success of this project has been beyond expectations.
MEWS � Cardiac arrest decreased by 38% in the first six months of use. � Cardiac arrest decreased 65% within 1 year(represents 22 at-risk patients) � Represents cost avoidance $640, 000* per year from increased MEWS surveillance So how does it work?
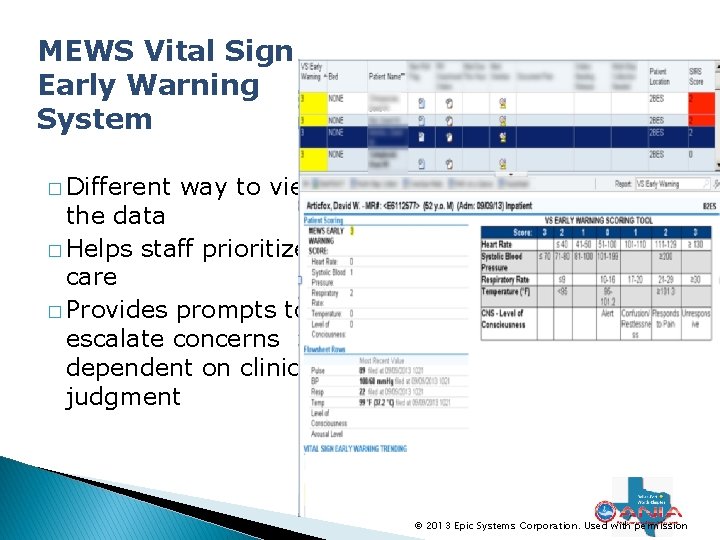
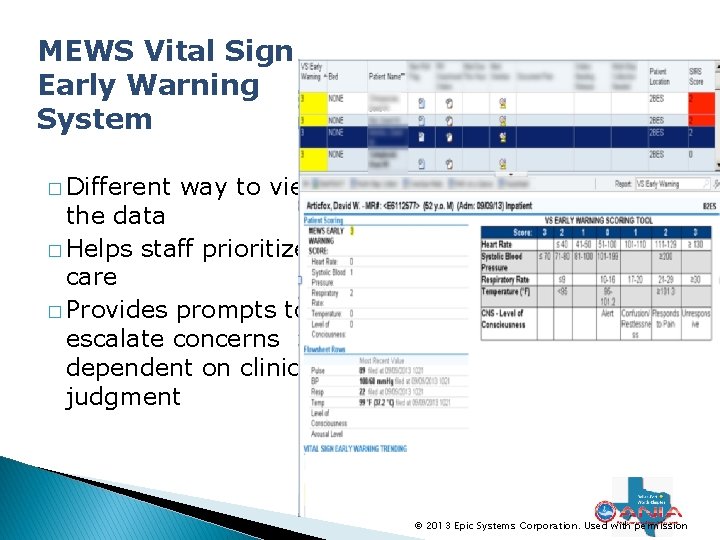
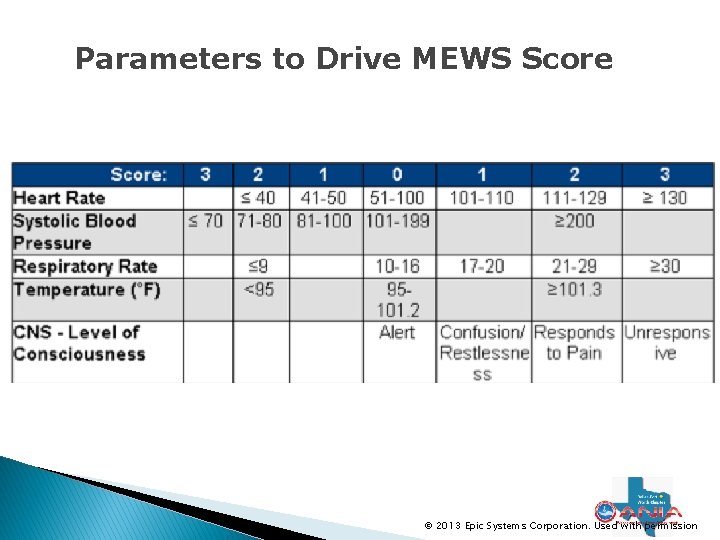
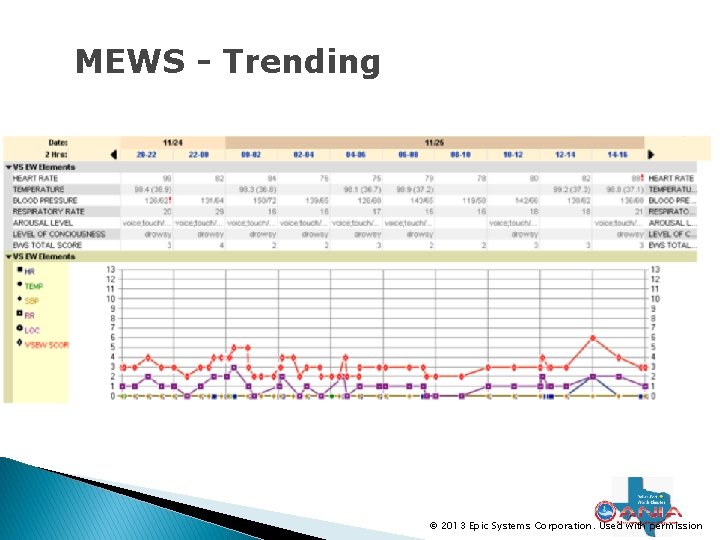
MEWS Vital Sign Early Warning System � Different way to view the data � Helps staff prioritize care � Provides prompts to escalate concerns dependent on clinical judgment © 2013 Epic Systems Corporation. Used with permission
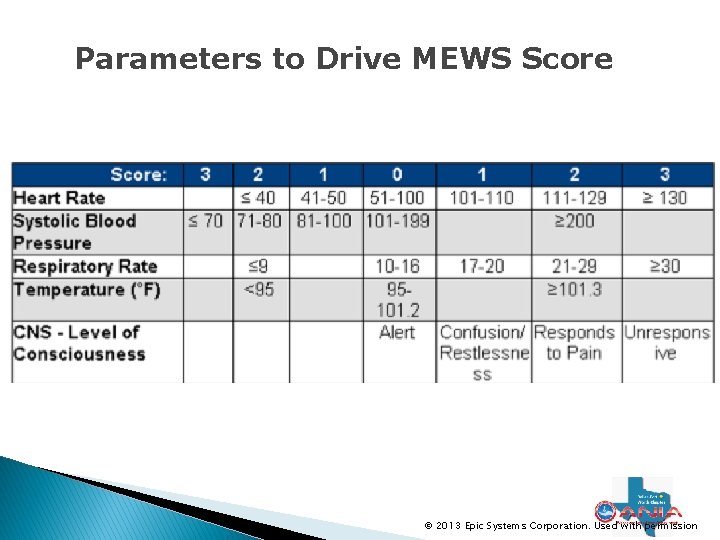
Parameters to Drive MEWS Score © 2013 Epic Systems Corporation. Used with permission
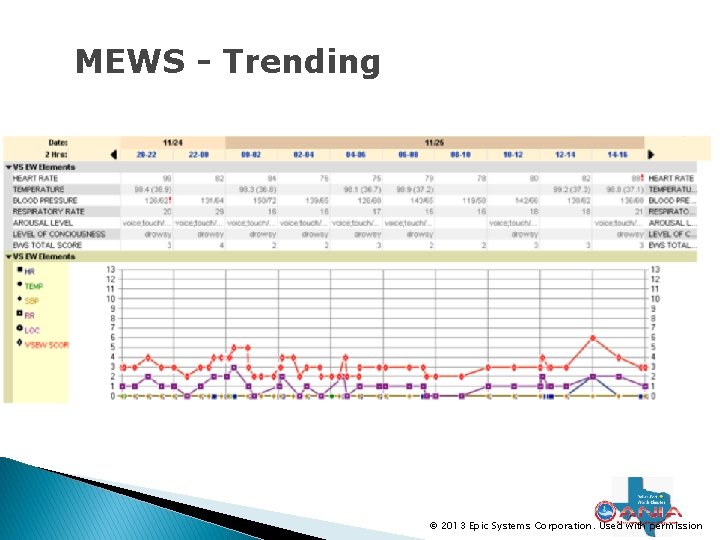
MEWS - Trending © 2013 Epic Systems Corporation. Used with permission
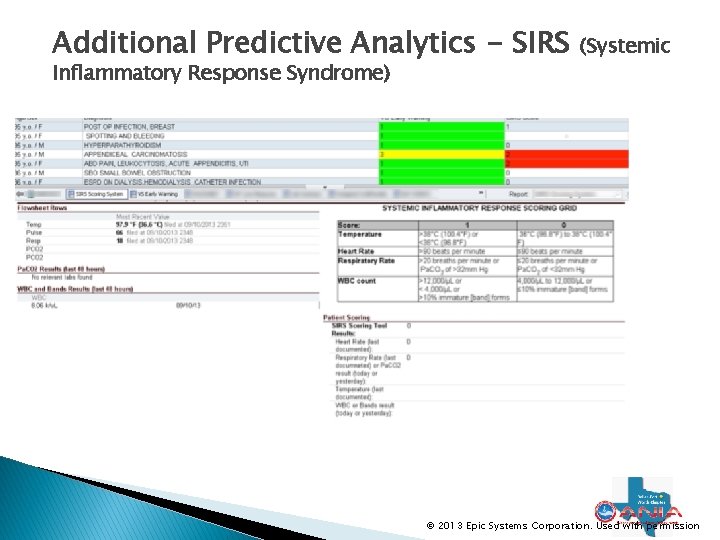
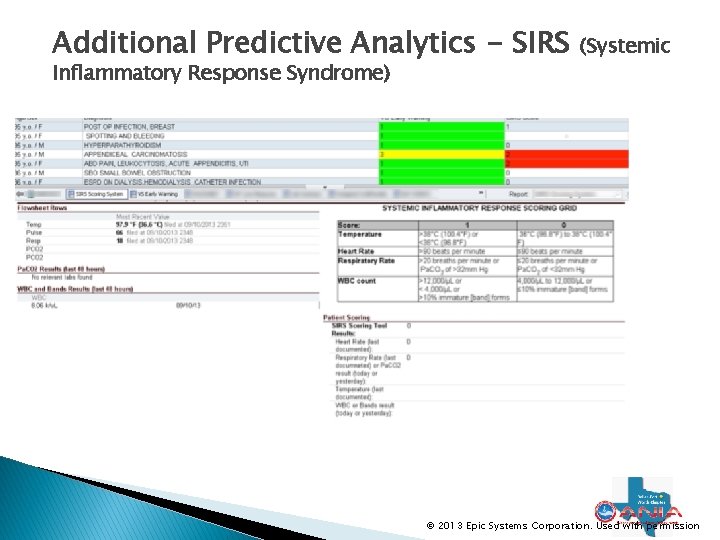
Additional Predictive Analytics - SIRS Inflammatory Response Syndrome) (Systemic © 2013 Epic Systems Corporation. Used with permission
Next Steps � Initially was not used/adopted in every unit in every hospital. � Nursing Leadership has stated this is now a patient-safety issue. ◦ Additional training – trending report emphasized. ◦ New policies in place ◦ All Cardiac Arrests will undergo Root Cause Analysis for compliance with MEWS monitoring. � New RRT and Code Navigators for documentation for all Med/Surg nurses. � Add MEWS to Nurse Leader Dashboard � Required
Venous Thromboembolism
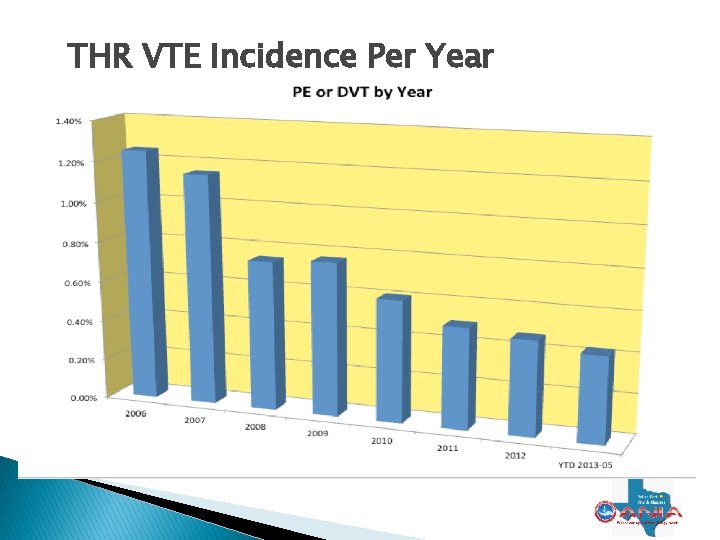
Venous Thromboembolism � � In 2008, Texas Health Resources launched a program to prevent venous thromboembolism (VTE). We saw immediate change in practices, and by 2011, post-operative VTE rates were less than half of preprogram rates. Lowering post-op VTE rates has helped Texas Health to satisfy Surgical Care Improvement Project requirements, and to meet measures set forth by the Centers for Medicare and Medicaid Services. The VTE prophylaxis program was awarded a 2011 HIMSS Story of Success, which also was used as a case study to show the effectiveness of the Texas Health electronic medical record for the Texas Health Alliance hospitals’ EMRAM Stage 7 award designation.
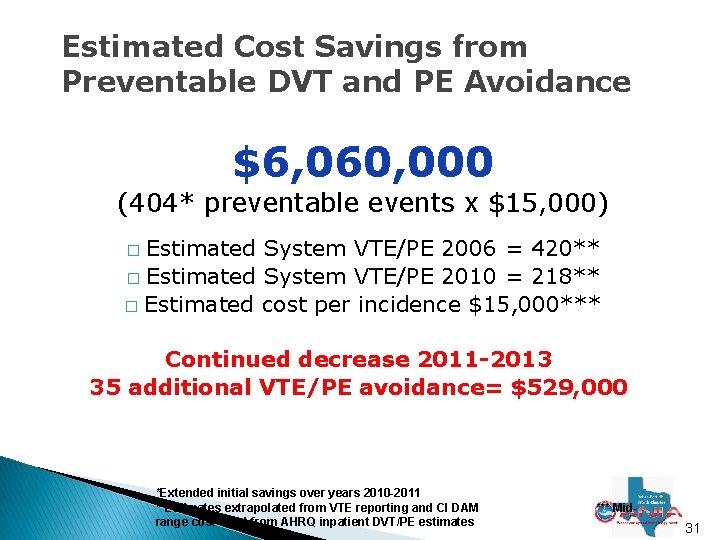
VTE- Highlights � Between 2008 and 2010, THR had 404 preventable VTE events � Resulted in a cost avoidance of more than $6 million. � The savings represents about a 50% decrease in the number of VTEs over four years.
Decrease Incidence of Deep Vein Thrombosis and Pulmonary Embolus � Care. Connect provides standardized CPOE Order Sets and Clinical Decision support tools for appropriate VTE Prophylaxis. � THR System VTE incidence steadily decreasing since implementation of Care. Connect. * � The Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Projects' estimates of inpatient cost are $10, 000 per DVT and $20, 000 per PE. ** * Data from CI DAM and VTE reporting **Data from AHRQ website 4/2011 29
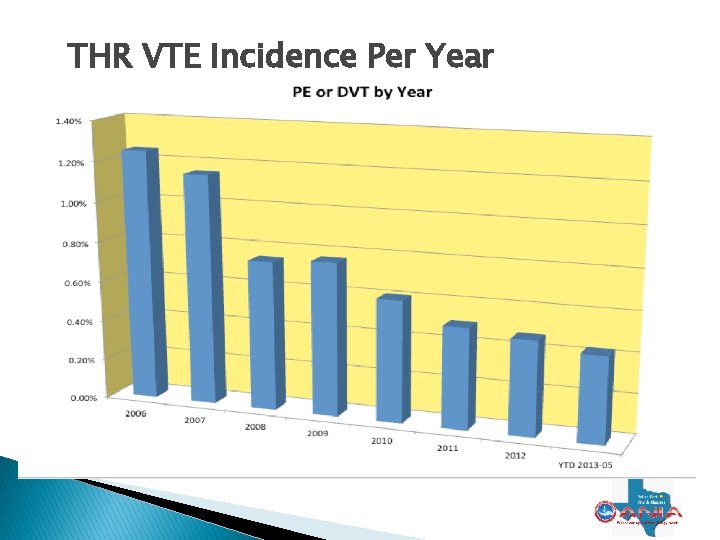
THR VTE Incidence Per Year
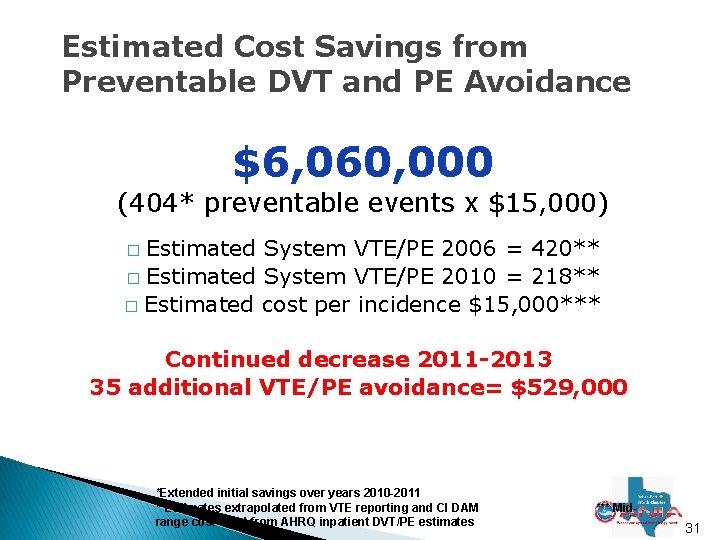
Estimated Cost Savings from Preventable DVT and PE Avoidance $6, 060, 000 (404* preventable events x $15, 000) Estimated System VTE/PE 2006 = 420** � Estimated System VTE/PE 2010 = 218** � Estimated cost per incidence $15, 000*** � Continued decrease 2011 -2013 35 additional VTE/PE avoidance= $529, 000 *Extended initial savings over years 2010 -2011 **Estimates extrapolated from VTE reporting and CI DAM range cost used from AHRQ inpatient DVT/PE estimates *** Mid- 31
Additional High-Impact Case Studies � CABG glycemic management ◦ Working with H&V Council to adopt standard insulin protocol and workflow; go-live in Dec 2013 � Global Immunizations ◦ Hospital MEC’s approved standard protocol; nursing workflow managed within Care. Connect � Antibiotic Stewardship- SCIP Measures ◦ Rules to move from IV to PO antibiotics. ◦ Initial work with Vancomycin � Sepsis ◦ SIRS and standardized Order Set currently in use ◦ Algorithm pilot to identify and manage potential sepsis patients.
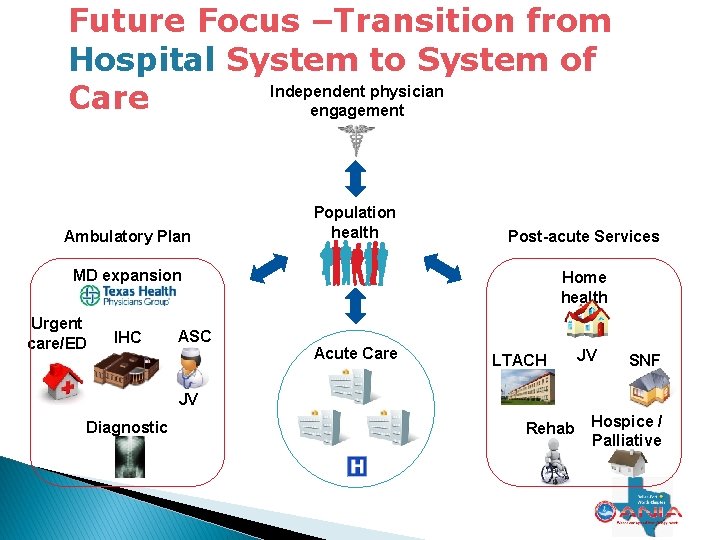
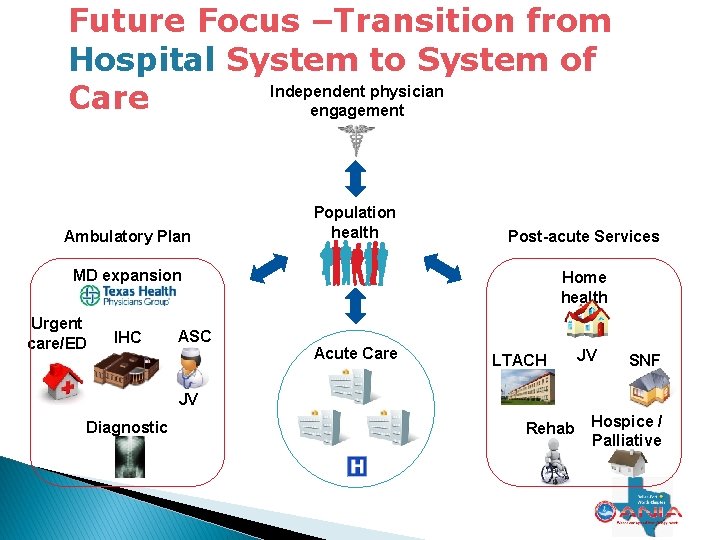
Future Focus –Transition from Hospital System to System of Independent physician Care engagement Ambulatory Plan Population health Post-acute Services MD expansion Urgent care/ED IHC ASC Home health Acute Care LTACH JV SNF JV Diagnostic s Rehab Hospice / Palliative
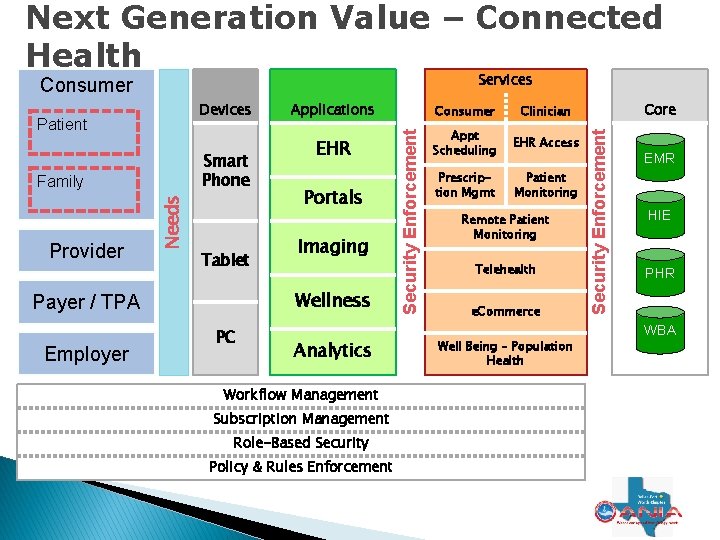
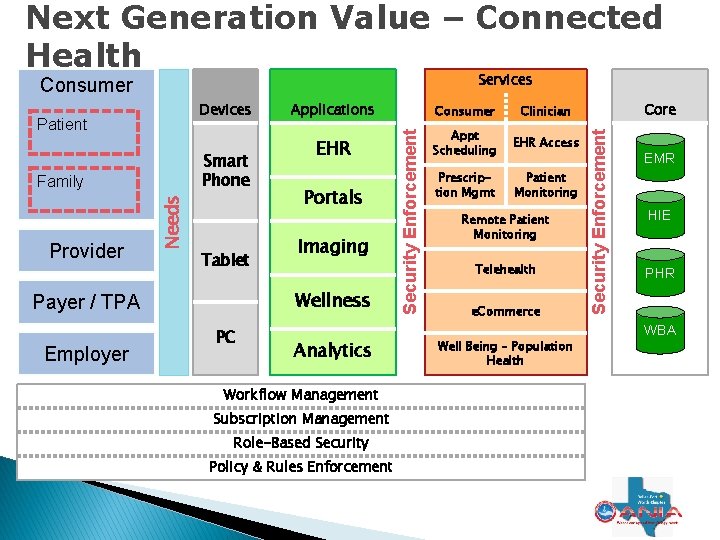
Next Generation Value – Connected Health Services Patient Smart Phone Provider Needs Family Tablet Consumer Clinician EHR Appt Scheduling EHR Access Prescription Mgmt Patient Monitoring Portals Imaging Wellness Payer / TPA Employer Applications PC Analytics Security Enforcement Devices Remote Patient Monitoring Telehealth e. Commerce Well Being – Population Health Core Security Enforcement Consumer EMR HIE PHR WBA Workflow Management Subscription Management Role-Based Security Policy & Rules Enforcement 78
In Summary Implementing an EHR • Big investment • Gets you in the game Value begins • Closing loops, gaps • Informing, monitoring Organizational Focus • Evolves • Leverage EHR to support Its a continuing Journey • To improve the health of the communities we serve A journey we are privileged to be on
Thank You! Mary Beth Mitchell Marybeth. Mitchell@Texashealth. org @mitchemtxtx

81