Clinical aspects of neoplasia Lecture 6 Clinical aspects


- Slides: 30
Clinical aspects of neoplasia Lecture 6
Clinical aspects of neoplasia Malignant tumors: More threatening on patients health than benign. Morbidity & mortality are associated with both. Benign tumor: A mass of cells that lacks the ability of invasion & metastastsis. Growth of benign tumors produces a mass effect: Can compress tissues: 1. Cause nerve damage. 2. Ischaemia: Reduction of blood to the area Tissue death (necrosis) & organ damage.
l Effects of Neoplasia are due to: (1). Location & impingement on adjacent structures. (2). Functional activity: Hormone synthesis. (3). Bleeding & infections. (4). Cachexia or wasting. (5). Paraneoplastic syndromes.
Effects of Tumor on Host: l 1. Location: l It has effect in both benign & malignant tumors. l A small (1 -cm) pituitary adenoma compress & destroy normal gland Hypopituitarism. l. A 0. 5 -cm leiomyoma in the wall of renal artery affects blood supply causing renal ischemia. l l Small carcinoma within the common bile duct induce fatal biliary tract obstruction.
l 2. Hormone production: l Seen in benign & well-differentiated malignant neoplasms arising in endocrine glands. l Ex. : l 1. In pancreas: Adenomas & carcinomas l Hyperinsulinism (sometimes fatal). 2. In adrenal gland: Adenomas & carcinomas: Elaborate corticosteroids: e. g. : Aldosterone Sodium retention, hypokalemia & hypertension.
l 3. Bleeding & secondary infection: l Occurs when tumor ulcerate through a surface. l 4. Cancer Cachexia: Loss of body fat & decrease body mass due to alteration in metabolism of carbohydrate, protein & fat. Basis of these metabolic abnormalities is unclear. Not results from reduced food intake. Results from: A- Action of cytokines: Produced by tumor & host. Patients have increased metabolic rate & high
l TNF produced by macrophages & tumor cell is responsible for: 1. Increase gluconeogenesis: A metabolic pathway results in generation of glucose from noncarbohydrate carbon substrates. 2. Loss of adipose tissue & protein. 3. Decrease in protein, lipid & glycogen synthesis. 4. Suppresses appetite. l B- Proteolysis & lipolysis inducing factor: l A protein mobilizing factor causes breakdown of skeletal muscle proteins & molecules with lipolytic action, detected in the serum of cancer patients.
5. Paraneoplastic Syndromes Symptom complexes occur in 10 -15% of patients with lung, breast & hematologic cancer. Not due to local or distant spread of tumor. Not due to elaboration of hormones. Not related to the tissue of origin of tumor. Their clinical recognition is important because it: • 1. Represent earliest manifestation of neoplasm. • 2. Associated with significant clinical illness & may be lethal. • 3. Mimic metastatic disease so disturbs treatment.


l The l 1. most common syndromes: Hypercalcemia. l 2. Cushing syndrome. l 3. Nonbacterial thrombotic endocarditis. l 1. Hypercalcemia is multifactorial: l 1 - Synthesis of parathyroid hormone (Responsible of bone remodling) by tumor cells. l 2 - Tumor cells produce T cell transcription factor (TCF-α) Activates osteoclasts Resorption l 3 - Osteolytic metastatic tumor of bone.
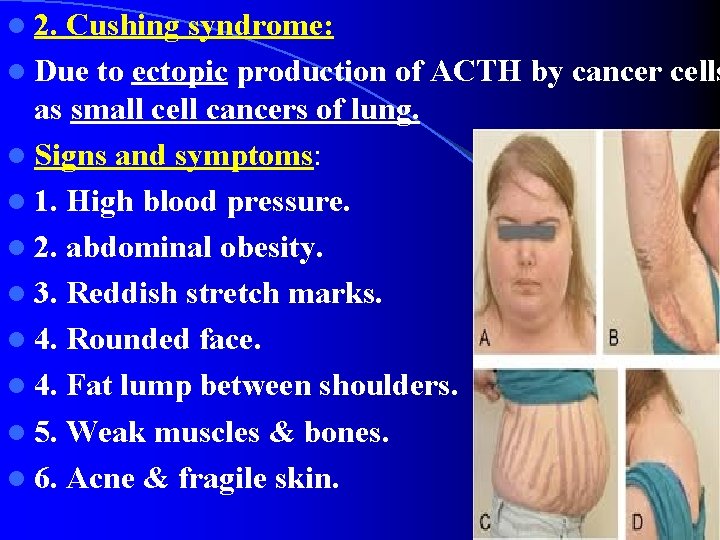
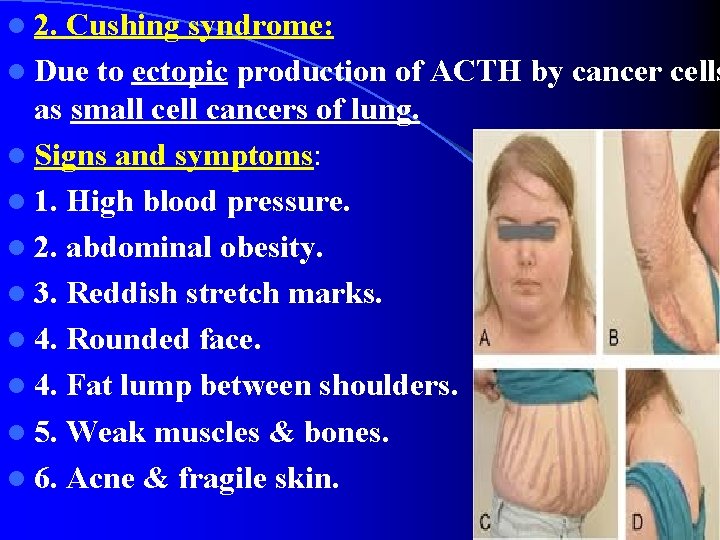
l 2. Cushing syndrome: l Due to ectopic production of ACTH by cancer cells as small cell cancers of lung. l Signs and symptoms: l 1. High blood pressure. l 2. abdominal obesity. l 3. Reddish stretch marks. l 4. Rounded face. l 4. Fat lump between shoulders. l 5. Weak muscles & bones. l 6. Acne & fragile skin.
l 3. Hypercoagulability: l Occurs due to the ability of tumor cells to activate the coagulation system venous thrombosis & nonbacterial thrombotic endocarditis. l Sometimes one tumor induces several syndromes. Ex. : Bronchogenic carcinomas : Elaborate products similar to: ACTH, antidiuretic & parathyroid hormone, serotonin, human chorionic gonadotropin.
Grading & Staging of Cancer: l Important methods in handling with cancer patients because they: l 1. Measure the clinical aggressiveness, extent & spread of neoplasm. l 2. Necessary for making accurate prognosis. l 3. Important in making a treatment plan. l Ex. : Treating plan is differ between: l Small differentiated thyroid adenocarcinoma localized to thyroid gland & highly anaplastic thyroid cancers invaded neck organs.
l Grading of cancer: l Give idea about aggressiveness or level of cancer. l Grading is based on: l 1. Cytologic differentiation of tumor cells. l (Degree of anaplasia). l 2. Number of mitoses within the tumor. l (Number of proliferating cells). l Cancer grading reflects the cytology of tumors: l Low-grade tumors: Well differentiated. l High-grade: Anaplastic, lack differentiated features that indicate the tissue of origin.
l Two l A. types of grading: According to increase anaplasia: l Grade I, III, & IV. l B. Descriptive characterizations: Ex. : l Well-differentiated cancer with no vascular or lymphatic invasion. l Highly anaplastic sarcoma with extensive vascular invasion.
l Cytologic & histologic grading is Subjective. l The severity of anaplasia is determined from: l 1. Shape & regularity of the cells. l 2. Presence of distinct differentiated features: Ex. : l Functioning glandular structures in adenocarc. l Epithelial pearls in squamous cell carcinomas. l The presence of such characteristics identifies the tumor as well differentiated or low grade.
l “Poorly differentiated” malignancies: l Have cells with little resemblance to their normal counterparts. (Cell of origin) l Evidence l (1) of rapid or abnormal growth: Large numbers of mitoses. l (2) Atypical mitoses. l (3) Nuclear pleomorphism. l (4) Tumor giant cells.
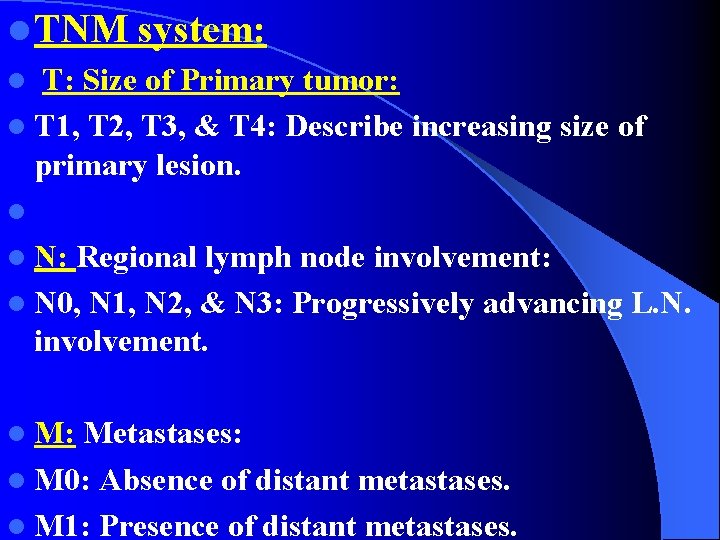
l Staging of cancers: Based on: l 1. Size of primary lesion. l 2. Extent of spread to the regional lymph nodes. l 3. Presence or absence of metastases. l Clinical staging is independent of cytologic grading & it refers to the extent of spread. l Two methods of staging: l 1. TNM system. l 2. AJC (American Joint Committee) system.
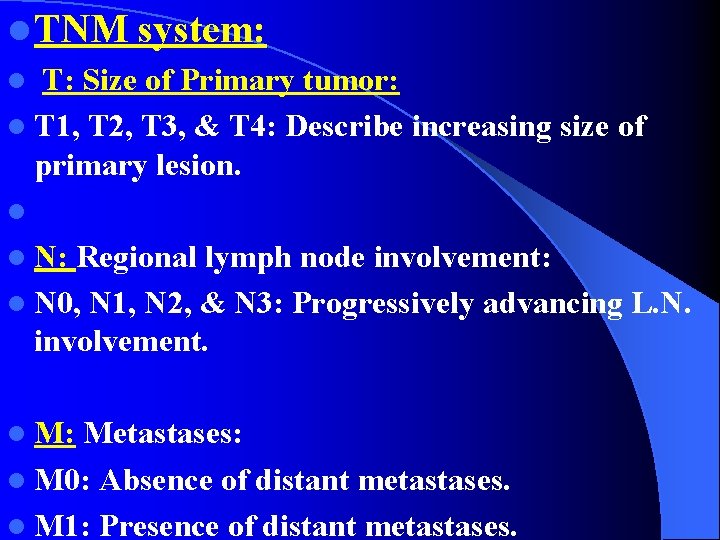
l TNM system: l T: Size of Primary tumor: l T 1, T 2, T 3, & T 4: Describe increasing size of primary lesion. l l N: Regional lymph node involvement: l N 0, N 1, N 2, & N 3: Progressively advancing L. N. involvement. l M: Metastases: l M 0: Absence of distant metastases. l M 1: Presence of distant metastases.
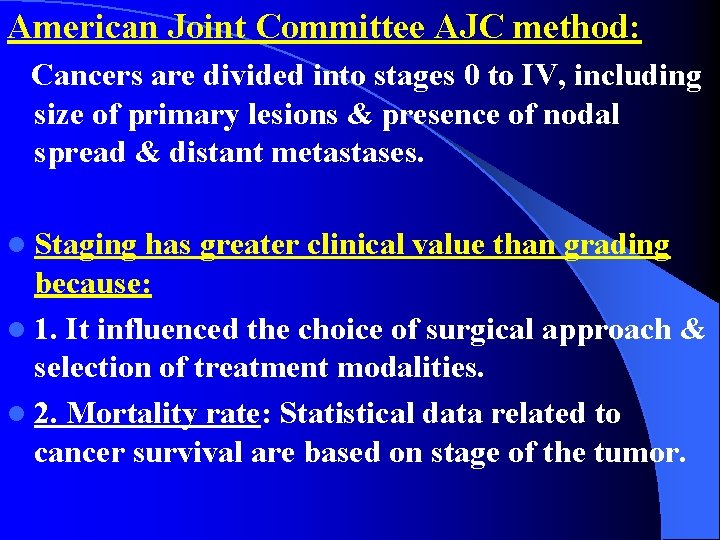
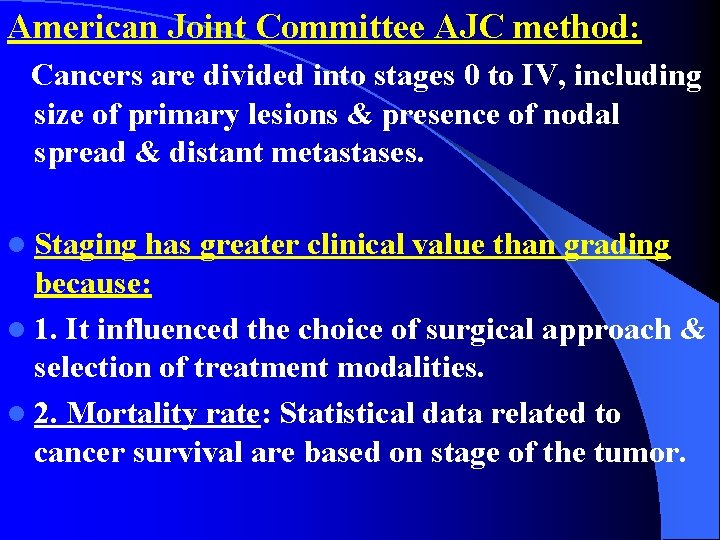
American Joint Committee AJC method: Cancers are divided into stages 0 to IV, including size of primary lesions & presence of nodal spread & distant metastases. l Staging has greater clinical value than grading because: l 1. It influenced the choice of surgical approach & selection of treatment modalities. l 2. Mortality rate: Statistical data related to cancer survival are based on stage of the tumor.
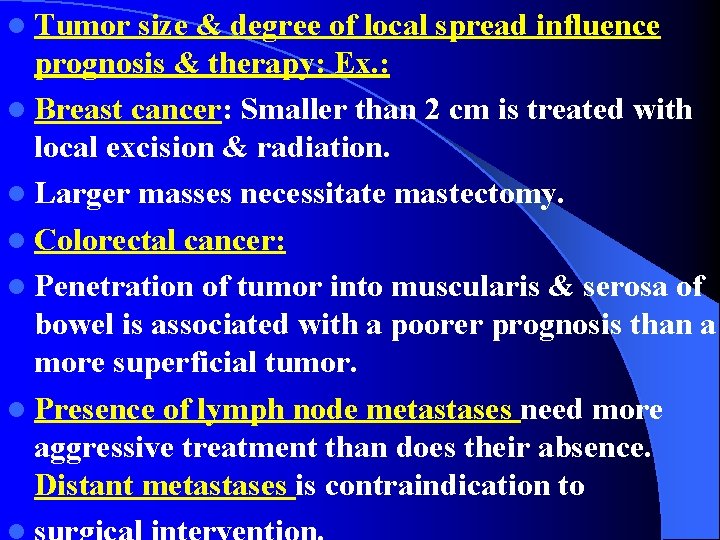
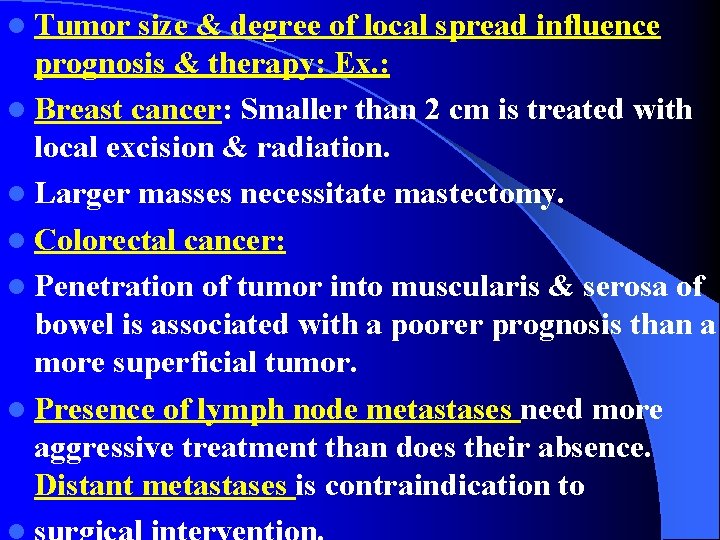
l Tumor size & degree of local spread influence prognosis & therapy: Ex. : l Breast cancer: Smaller than 2 cm is treated with local excision & radiation. l Larger masses necessitate mastectomy. l Colorectal cancer: l Penetration of tumor into muscularis & serosa of bowel is associated with a poorer prognosis than a more superficial tumor. l Presence of lymph node metastases need more aggressive treatment than does their absence. Distant metastases is contraindication to
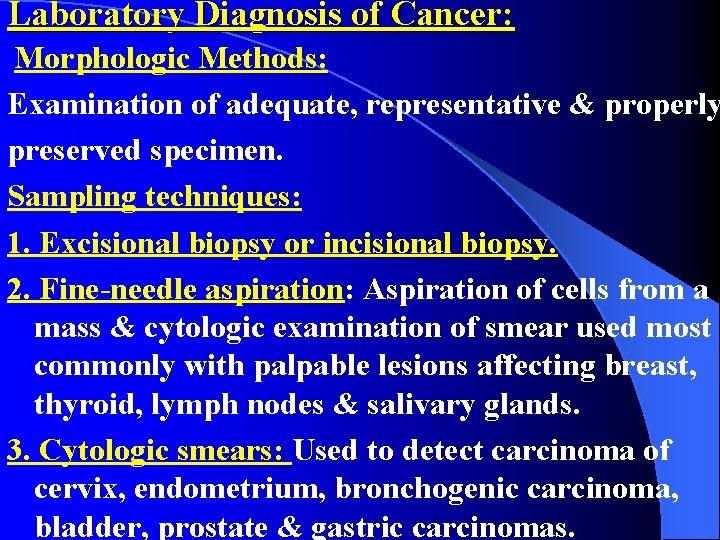
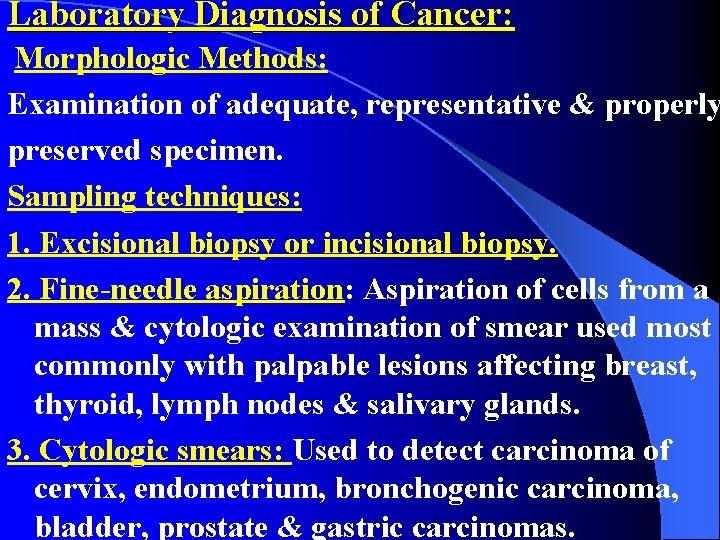
Laboratory Diagnosis of Cancer: Morphologic Methods: Examination of adequate, representative & properly preserved specimen. Sampling techniques: 1. Excisional biopsy or incisional biopsy. 2. Fine-needle aspiration: Aspiration of cells from a mass & cytologic examination of smear used most commonly with palpable lesions affecting breast, thyroid, lymph nodes & salivary glands. 3. Cytologic smears: Used to detect carcinoma of cervix, endometrium, bronchogenic carcinoma, bladder, prostate & gastric carcinomas.
l 4. Frozen section: The sample is quick-frozen and l sectioned, permits histological evaluation within minutes. l 5. Immunocytochemistry: Used in diagnosis of undifferentiated carcinoma. Ex. : l Detection of cytokeratin by specific monoclonal antibodies labeled with peroxidase. l 6. Flow cytometry: Fluorescent antibodies against cell surface molecules & differentiation antigens. Used to obtain the phenotype of malignant cells. Used in classification of leukemias & lymphomas.
Tumor Markers l They are tumor-associated enzymes, hormones, & proteins detected in blood. l Biochemical assays of tumor markers is useful screening tests but cannot be utilized for definitive diagnosis because it is: l 1. Produced in non-neoplastic conditions. l 2. Lack specificity & sensitivity required for early detection of cancers. l They are useful in detection of recurrences after successful excision of tumor because these markers disappear from serum.
Examples of tumor markers: 1. Prostate specific antigen PSA: Used to screen prostatic adenocarcinoma. l Elevated levels of PSA in blood prostatic carcinoma is suspected. 2. Carcinoembryonic antigen (CEA): l Elaborated by carcinomas of colon, pancreas, stomach & breast. 3. Alpha fetoprotein: l Produced by hepatocellular carcinomas.
Molecular diagnosis of Tumors l 1. Gene expression: l Measurements of expression levels of several thousand genes, begins by extraction of m. RNA from any two sources: l Normal & malignant tissues. l Normal & preneoplastic tissues. l Two tumors of the same histologic type. l 2. Whole Genome Sequencing: l Sequences of entire tumor genomes, compared with normal genome from the same patient, can reveal all somatic alterations present in tumor.
: l Uses of molecular techniques: l 1 • Diagnosis of malignancy: l Polymerase chain reaction (PCR): l A. PCR detects the specific antigen receptors rearrangement of T & B lymphocytes. l B. PCR detects translocations presents in hematopoietic neoplasm & solid tumors. l 2 • Prognosis & behavior: l Certain genetic alterations are associated with a poor prognosis so it determines tumor behavior.
l 3 • Detection of minimal residual disease: l By blood test. l All advanced tumors are associated with: l Intact circulating tumor cells. l Products derived from tumors. l 4 • Diagnosis of hereditary predisposition to cancer l Early detection of any mutated gene give the patient opportunity for prophylactic surgery. l 5 • Therapeutic decision-making: l Detection of mutations in a tumor can guide therapy by giving inhibitors against these mutated gene products.
Thank you
 Clinical features of neoplasia
Clinical features of neoplasia Colorectal
Colorectal Neoplasia
Neoplasia Neoplasia testicular
Neoplasia testicular Otorraggia
Otorraggia Multiple endocrine neoplasia type 2
Multiple endocrine neoplasia type 2 Malignancy
Malignancy New growth meaning
New growth meaning Anovulatory bleeding
Anovulatory bleeding Neoplasia
Neoplasia Que es una neoplasia
Que es una neoplasia Malignant neoplasm
Malignant neoplasm Que es una neoplasia
Que es una neoplasia Neoplasia
Neoplasia Neoplasia literally means
Neoplasia literally means Cin
Cin 01:640:244 lecture notes - lecture 15: plat, idah, farad
01:640:244 lecture notes - lecture 15: plat, idah, farad What are the three aspects of color
What are the three aspects of color Element of a plot
Element of a plot What aspects of minoan culture did the mycenaeans adopt
What aspects of minoan culture did the mycenaeans adopt Pegi media aspects covered
Pegi media aspects covered Security aspects
Security aspects Look at the pictures and answer the questions below.
Look at the pictures and answer the questions below. Discourse aspects of interlanguage
Discourse aspects of interlanguage Legal aspects of catering premises
Legal aspects of catering premises Components of lexical meaning
Components of lexical meaning Interlanguage and stylistic continuum
Interlanguage and stylistic continuum 4 aspects of research
4 aspects of research Palmer hayden jeunesse
Palmer hayden jeunesse Additional aspects of aqueous equilibria
Additional aspects of aqueous equilibria Psychosocial aspects of living with diabetes
Psychosocial aspects of living with diabetes