Cervical Intraepithelial Neoplasia CIN Cervical Intraepithelial Neoplasia v


- Slides: 18
Cervical Intraepithelial Neoplasia, CIN
Cervical Intraepithelial Neoplasia v Cervical intraepithelial neoplasia (CIN), also known as cervical dysplasia, is the abnormal growth of cells on the surface of the cervix that could potentially lead to cervical cancer. [1] More specifically, CIN refers to the potentially precancerous transformation of cells of the cervix.
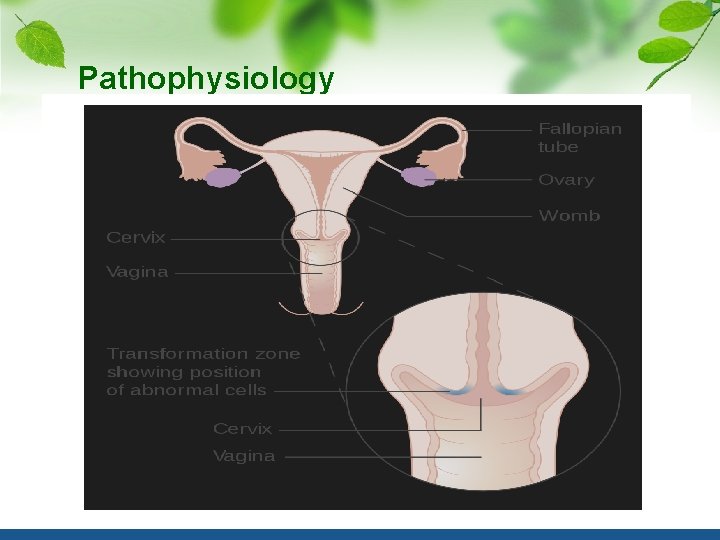
CIN most commonly occurs at the squamocolumnar junction of the cervix, a transitional area between the squamous epithelium of the vagina and the columnar epithelium of the endocervix. [2] It can also occur in vaginal walls and vulvar epithelium. CIN is graded on a 1 -3 scale, with 3 being the most abnormal (see classification section below) 84学时
Human papilloma virus (HPV) infection is necessary for the development of CIN, but not all with this infection develop cervical cancer. A large number of women with HPV infection never develop CIN or cervical cancer. Typically, HPV resolves on its own. However, those with an HPV infection that lasts more than 1 or 2 years have a higher risk of developing a higher grade of CIN. Like other intraepithelial neoplasias, CIN is not cancer and is usually curable. [3] Most cases of CIN either remain stable or are eliminated by the person's immune system without need for intervention. However, a small percentage of cases progress to cervical cancer, typically cervical squamous cell carcinoma (SCC), if left untreated.
Signs and symptoms There are no specific symptoms of CIN alone. Generally, signs and symptoms of cervical cancer include: [7] abnormal or post-menopausal bleeding abnormal discharge changes in bladder or bowel function pelvic pain on examination abnormal appearance or palpation of cervix. HPV infection of the vulva and vagina can cause genital warts or be asymptomatic.

Causes The cause of CIN is chronic infection of the cervix with HPV, especially infection with highrisk HPV types 16 or 18. It is thought that the high-risk HPV infections have the ability to inactivate tumor suppressor genes such as the p 53 gene and the RB gene, thus allowing the infected cells to grow unchecked and accumulate successive mutations, eventually leading to cancer. [1] Some groups of women have been found to be at a higher risk of developing CIN: [1][8]
Infection with a high risk type of HPV, such as 16, 18, 31, or 33 Immunodeficiency (e. g. HIV infection) Poor diet Multiple sex partners Lack of condom use Cigarette smoking Additionally, a number of risk factors have been shown to increase an individual's likelihood of developing CIN 3/carcinoma in situ (see below): Women who give birth before age 17; Women who with > 1 full term pregnancies
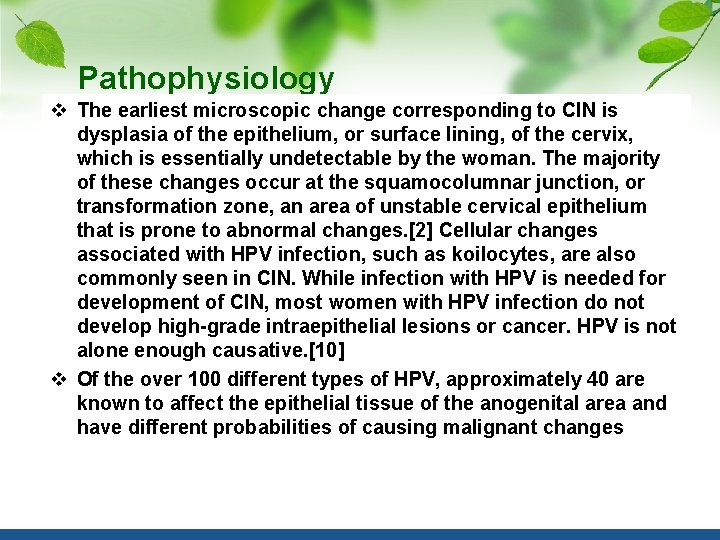
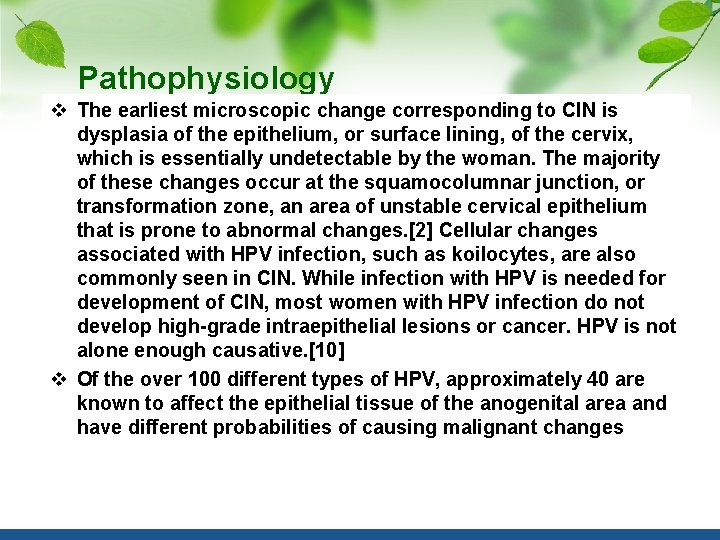
Pathophysiology v The earliest microscopic change corresponding to CIN is dysplasia of the epithelium, or surface lining, of the cervix, which is essentially undetectable by the woman. The majority of these changes occur at the squamocolumnar junction, or transformation zone, an area of unstable cervical epithelium that is prone to abnormal changes. [2] Cellular changes associated with HPV infection, such as koilocytes, are also commonly seen in CIN. While infection with HPV is needed for development of CIN, most women with HPV infection do not develop high-grade intraepithelial lesions or cancer. HPV is not alone enough causative. [10] v Of the over 100 different types of HPV, approximately 40 are known to affect the epithelial tissue of the anogenital area and have different probabilities of causing malignant changes
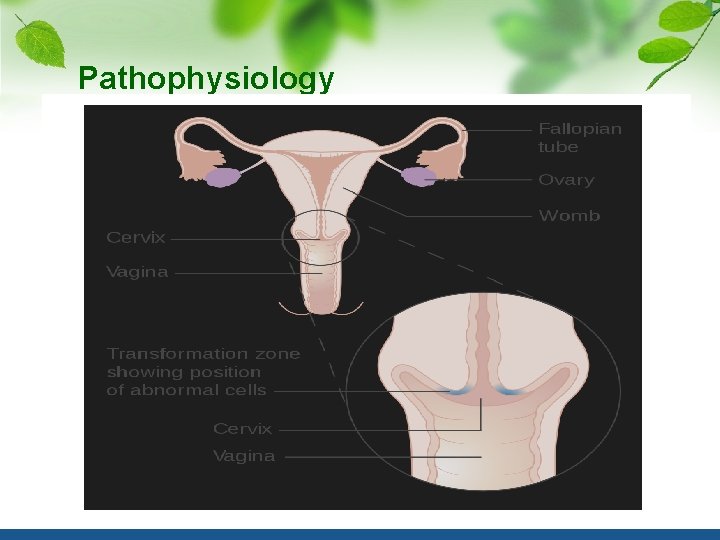
Pathophysiology
Diagnosis A test for HPV called the Digene HPV test is highly accurate and serves as both a direct diagnosis and adjuvant to the all-important Pap smear which is a screening device that allows for an examination of cells but not tissue structure, needed for diagnosis. A colposcopy with directed biopsy is the standard for disease detection. Endocervical brush sampling at the time of Pap smear to detect adenocarcinoma and its precursors is necessary along with doctor/patient vigilance on abdominal symptoms associated with uterine and ovarian carcinoma. The diagnosis of CIN or cervical carcinoma requires a biopsy for histological analysis.
Classification Historically, abnormal changes of cervical epithelial cells were described as mild, moderate, or severe dysplasia. In 1988 the National Cancer Institute developed "The Bethesda System for Reporting Cervical/Vaginal Cytologic Diagnoses. " [12] This system provides a uniform way to describe abnormal epithelial cells and determine specimen quality, thus providing clear guidance for clinical management. These abnormalities were classified as squamous or glandular and then further classified by the stage of dysplasia: atypical cells, mild, moderate, severe, and carcinoma. [13] Depending on several factors and the location of the lesion, CIN can start in any of the three stages and can either progress or regress. [1] The grade of squamous intraepithelial lesion can vary.
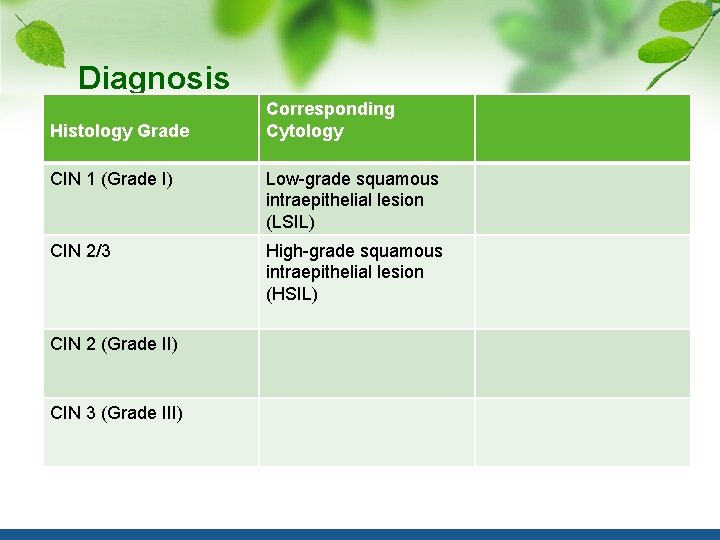
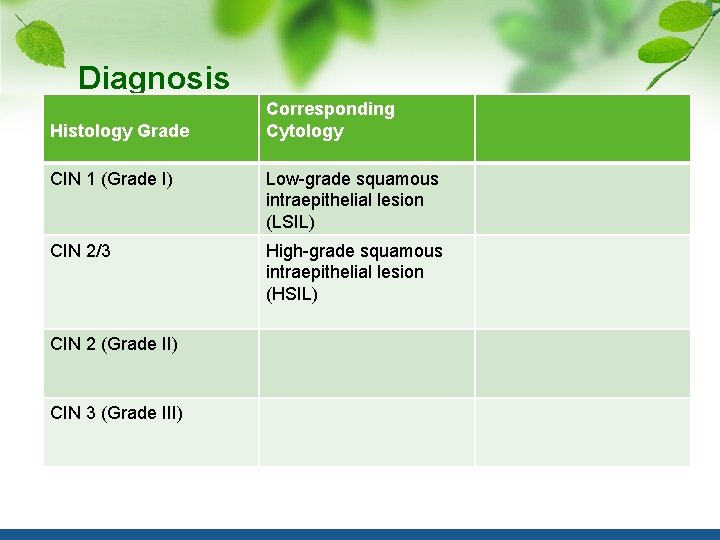
Diagnosis Histology Grade Corresponding Cytology CIN 1 (Grade I) Low-grade squamous intraepithelial lesion (LSIL) CIN 2/3 High-grade squamous intraepithelial lesion (HSIL) CIN 2 (Grade II) CIN 3 (Grade III)
Screening and prevention The two screening methods available are the Pap smear and testing for HPV. CIN is usually discovered by a screening test, the Pap smear. The purpose of this test is to detect potentially precancerous changes through random sampling of the transformation zone. Pap smear results may be reported using the Bethesda system (see above). The sensitivity and specificity of this test were variable in a systematic review looking at accuracy of the test. An abnormal Pap smear result may lead to a recommendation for colposcopy of the cervix, an in office procedure during which the cervix is examined under magnification. A biopsy is taken of any abnormal appearing areas
Screening and prevention HPV testing can identify most of the high risk HPV types responsible for CIN. HPV screening happens either as a co-test with the Pap smear or can be done after a Pap smear showing abnormal cells, called reflex testing. Frequency of screening changes based on guidelines from the Society of Lower Genital Tract Disorders (ASCCP). The World Health Organization also has screening and treatment guidelines for precancerous cervical lesions and prevention of cervical cancer.

Primary prevention HPV vaccination is the approach to primary prevention of both CIN and cervical cancer. Currently, only Gardasil 9 is available in the United States. Secondary prevention Appropriate management with monitoring and treatment is the approach to secondary prevention of cervical cancer in cases of persons with CIN.
Treatment Surgical treatment of CIN lesions is associated with an increased risk of infertility or subfertility. A case-control study found that there is an approximately two-fold increase in risk i. [17] Treatment of CIN during pregnancy increases the risk of premature birth. [18] People with HIV and CIN 2+ should be initially managed according to the recommendations for the general population according to the 2012 updated ASCCP consensus guidelines
Epidemiology Between 250, 000 and 1 million American women are diagnosed with CIN annually. Women can develop CIN at any age, however women generally develop it between the ages of 25 to 35. [1] The estimated annual incidence of CIN in the United States among persons who undergo screening is 4% for CIN 1 and 5% for CIN 2 and CIN 3
Outcomes It used to be thought that cases of CIN progressed through grades 1 -3 toward cancer in a linear fashion. However most CIN spontaneously regress. Left untreated, about 70% of CIN 1 will regress within one year; 90% will regress within two years. About 50% of CIN 2 will regress within 2 years without treatment. Progression to cervical carcinoma in situ (CIS) occurs in approximately 11% of CIN 1 and 22% of CIN 2 cases. Progression to invasive cancer occurs in approximately 1% of CIN 1, 5% in CIN 2 and at least 12% in CIN 3 cases. Progression to cancer typically takes 15 years with a range of 3 to 40 years. Also, evidence suggests that cancer can occur without first detectably progressing through CIN grades and that a high-grade intraepithelial neoplasia can occur without first existing as a lower grade. Treatment does not affect the chances of getting pregnant but does increase the risk of second trimester miscarriages
 Vulvar intraepithelial neoplasia (vin) grade 3
Vulvar intraepithelial neoplasia (vin) grade 3 Kippis englanniksi
Kippis englanniksi Hpv us
Hpv us Patho
Patho Burkitt lymphoma
Burkitt lymphoma Ciclo emorragico
Ciclo emorragico Valsava
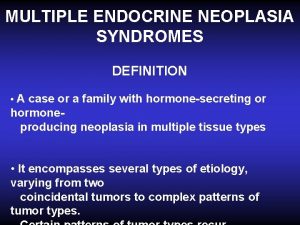
Valsava Multiple endocrine neoplasia type 2
Multiple endocrine neoplasia type 2 Patologia
Patologia Mamria
Mamria Anovulatory bleeding
Anovulatory bleeding Que es una neoplasia
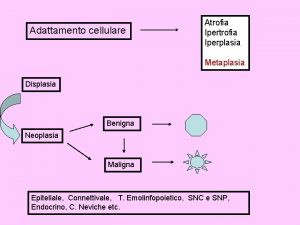
Que es una neoplasia Neoplasia
Neoplasia Enfermedades de la vulva
Enfermedades de la vulva Clinical features of neoplasia
Clinical features of neoplasia Neoplasia literally means
Neoplasia literally means New growth meaning
New growth meaning Md frcpc definition
Md frcpc definition Cin mafra
Cin mafra