Cervical Spondylosis Cervical disc Cervical Spondylotic myelopathy Anatomy



- Slides: 38
Cervical Spondylosis Cervical disc Cervical Spondylotic myelopathy
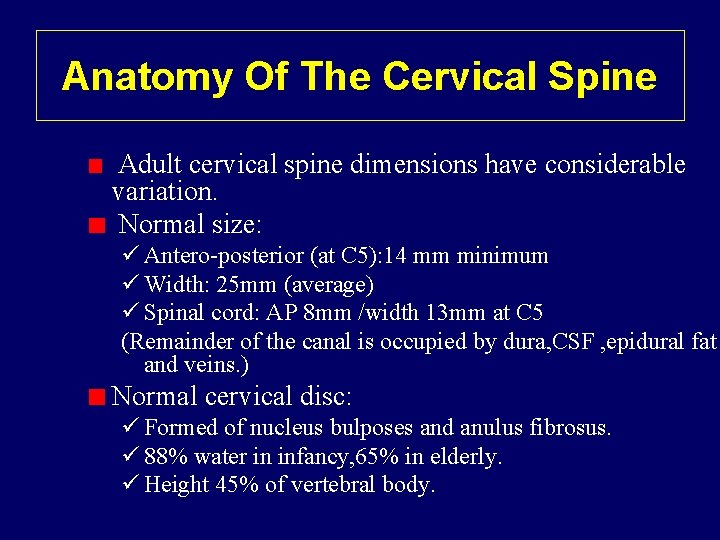
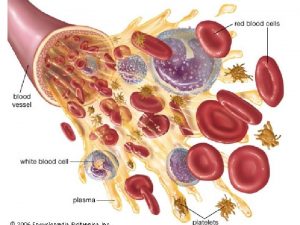
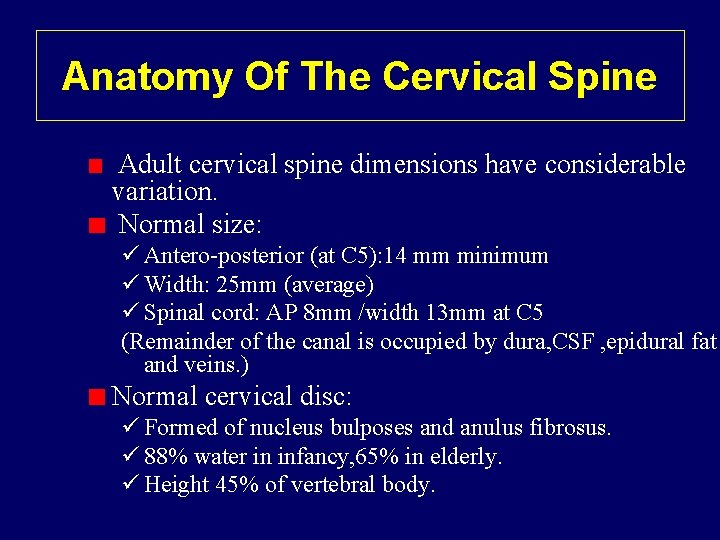
Anatomy Of The Cervical Spine Adult cervical spine dimensions have considerable variation. Normal size: ü Antero-posterior (at C 5): 14 mm minimum ü Width: 25 mm (average) ü Spinal cord: AP 8 mm /width 13 mm at C 5 (Remainder of the canal is occupied by dura, CSF , epidural fat and veins. ) Normal cervical disc: ü Formed of nucleus bulposes and anulus fibrosus. ü 88% water in infancy, 65% in elderly. ü Height 45% of vertebral body.
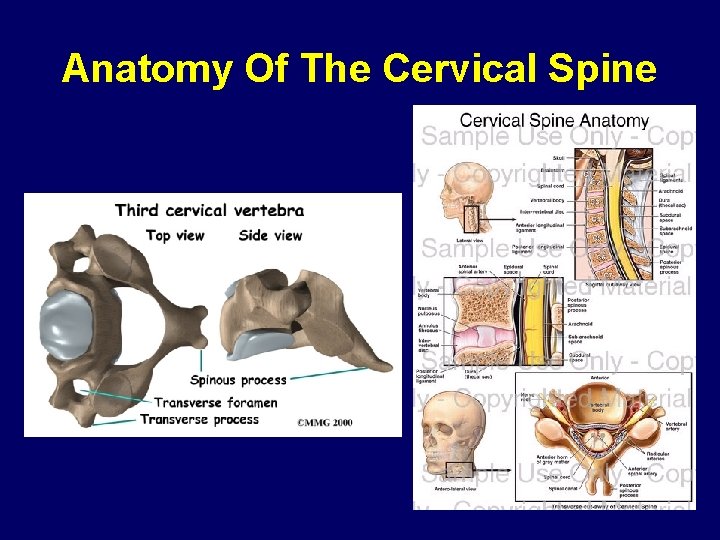
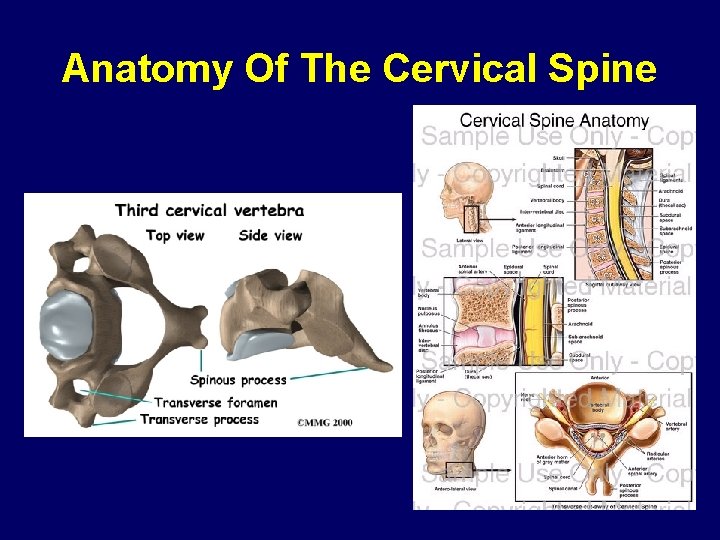
Anatomy Of The Cervical Spine
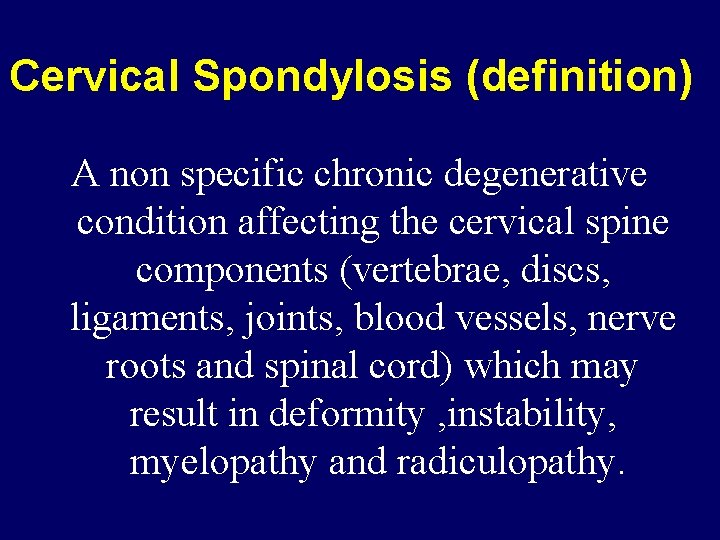
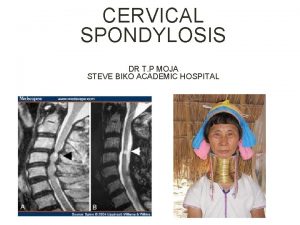
Cervical Spondylosis (definition) A non specific chronic degenerative condition affecting the cervical spine components (vertebrae, discs, ligaments, joints, blood vessels, nerve roots and spinal cord) which may result in deformity , instability, myelopathy and radiculopathy.
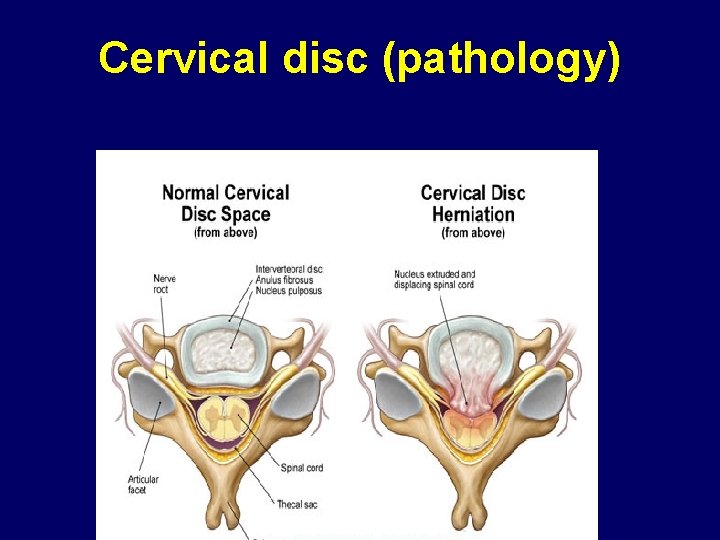
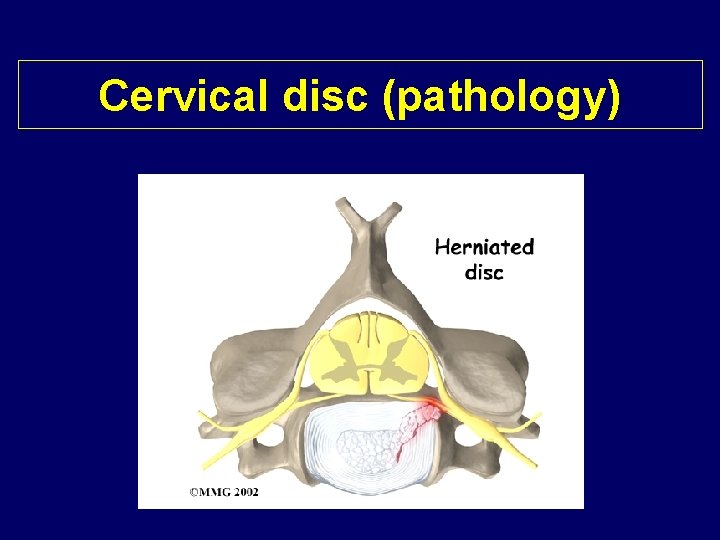
(Cervical disc disease (definition Rupture of fibrocartilagenous material (annulus fibrosis) that surrounds the intervertebral disk. This rupture involves the release of the disk's center portion containing a gelatinous substance called the nucleus pulposus. Pressure from the vertebrae above and below may cause the nucleus pulposus to be forced outward, placing pressure on a spinal nerve and causing considerable pain and damage to the nerve (compression of the cord or root)
Cervical Spondylosis (incidence) Radiographic evidence in 20 -25% of population by the age of 50 y and 70% by the age of 65 y Cervical spondylotic myelopathy is the commonest cause of acquired spstic paraparesis in middle and old age. Starts earlier in men than women C 5/6 &C 6/7 levels are commonest to be involved C 5&C 6 roots are comonly affected.
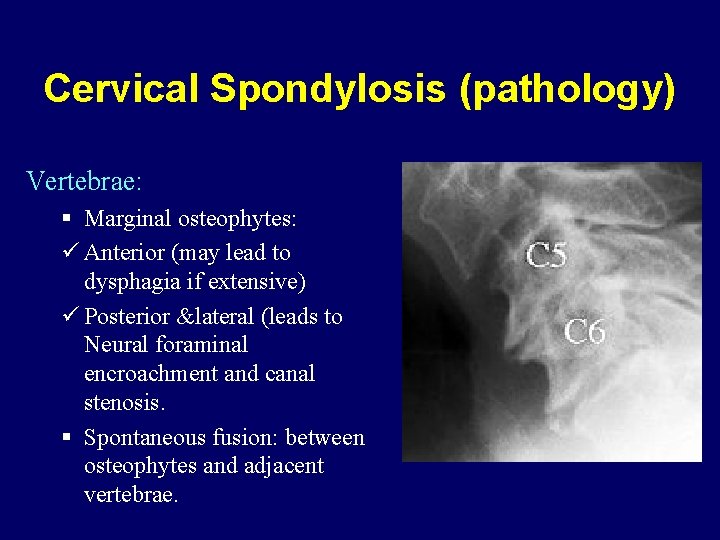
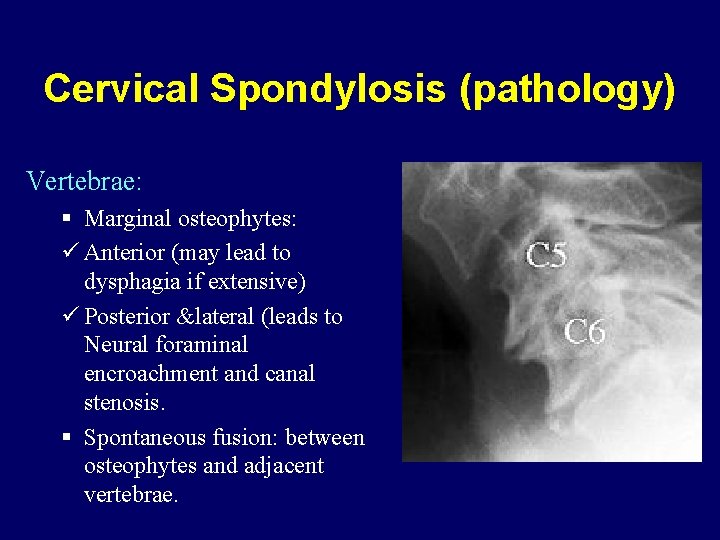
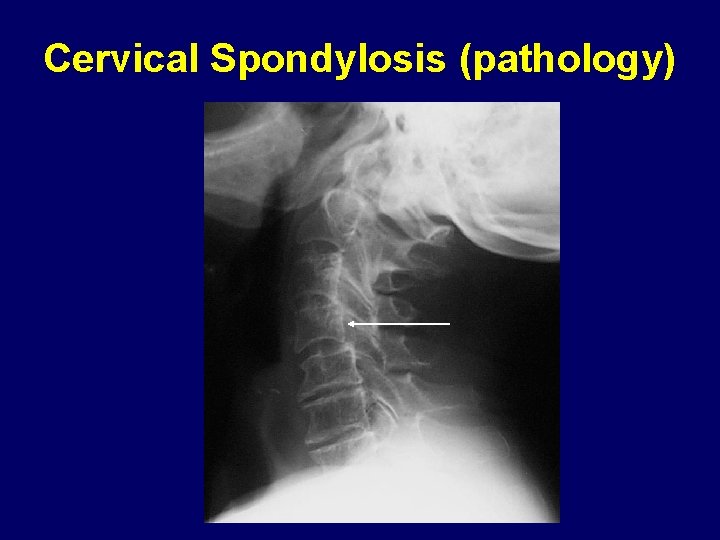
Cervical Spondylosis (pathology) Vertebrae: § Marginal osteophytes: ü Anterior (may lead to dysphagia if extensive) ü Posterior &lateral (leads to Neural foraminal encroachment and canal stenosis. § Spontaneous fusion: between osteophytes and adjacent vertebrae.
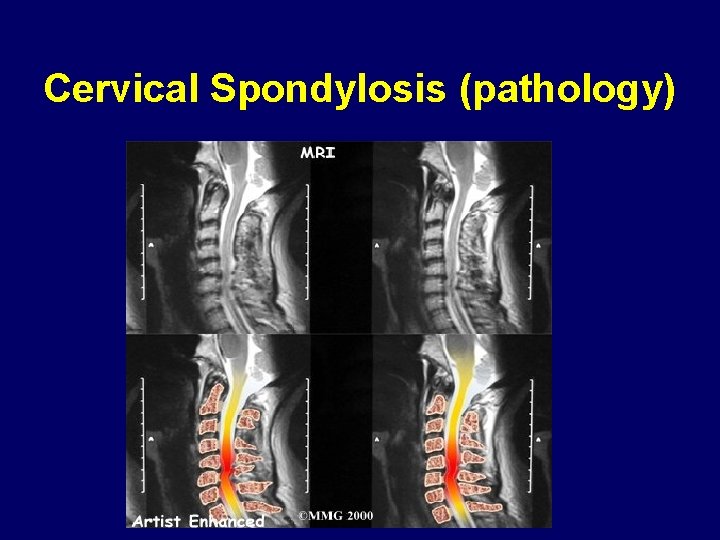
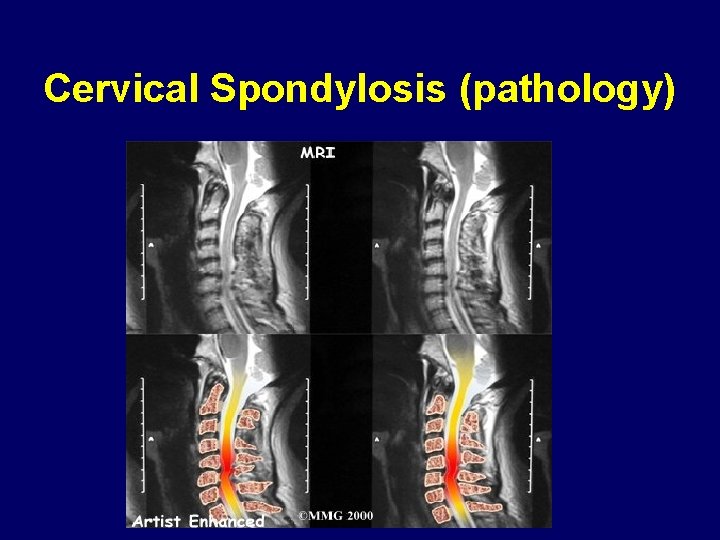
Cervical Spondylosis (pathology)
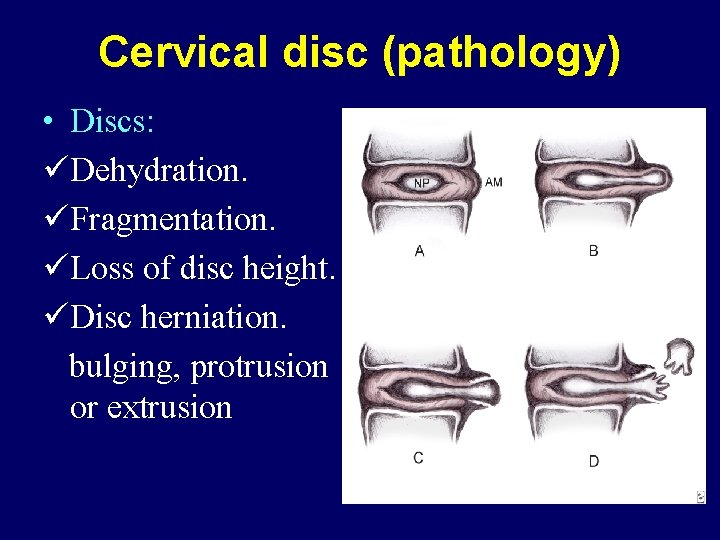
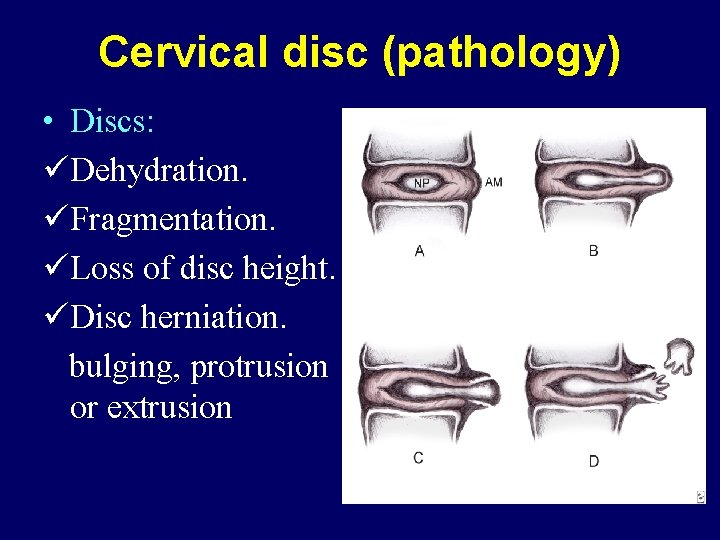
Cervical disc (pathology) • Discs: üDehydration. üFragmentation. üLoss of disc height. üDisc herniation. bulging, protrusion or extrusion
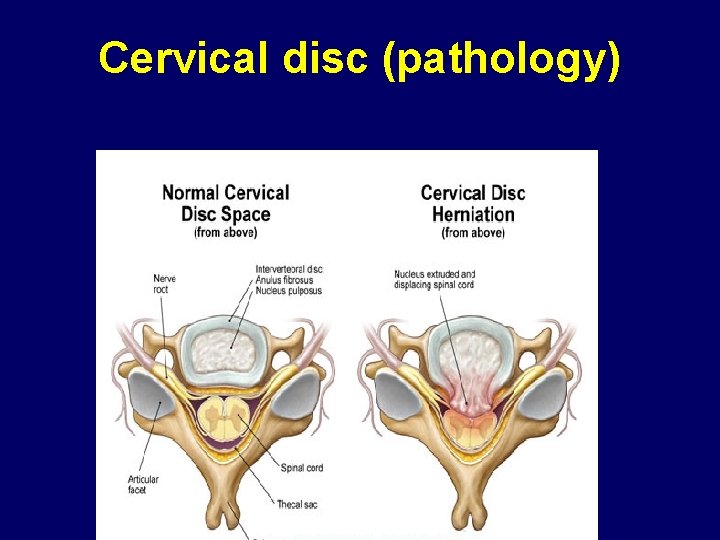
Cervical disc (pathology)
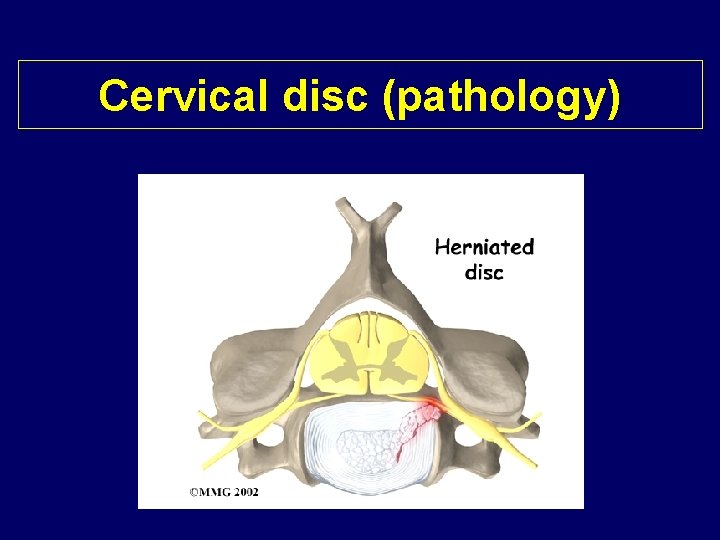
Cervical disc (pathology)
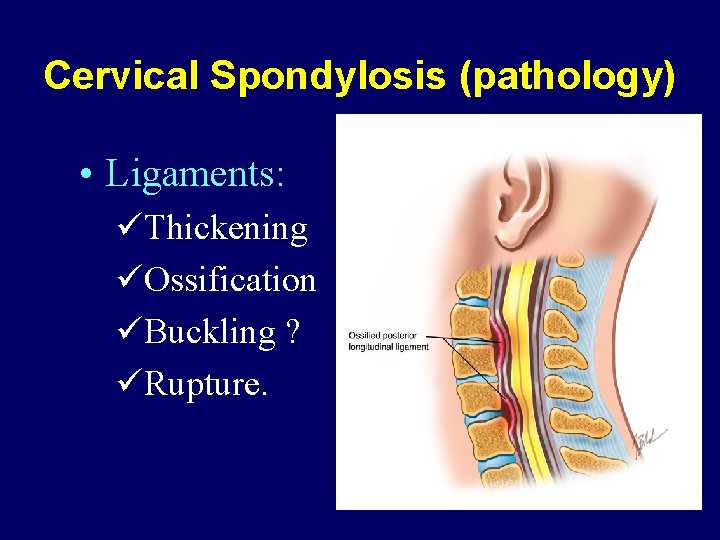
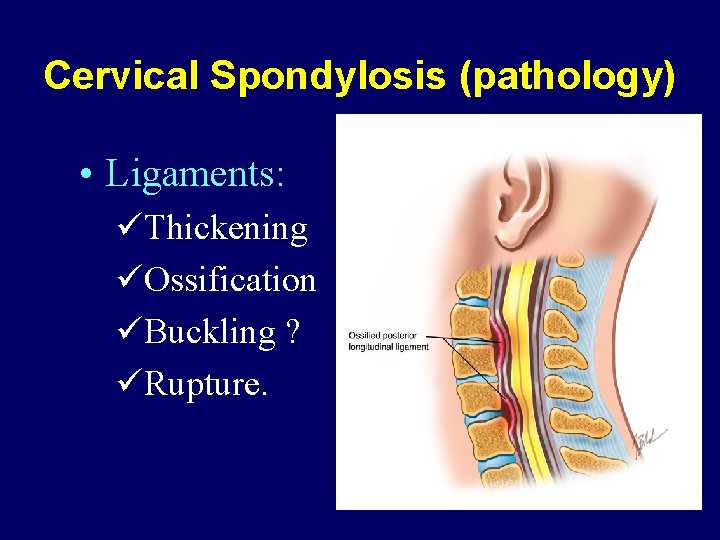
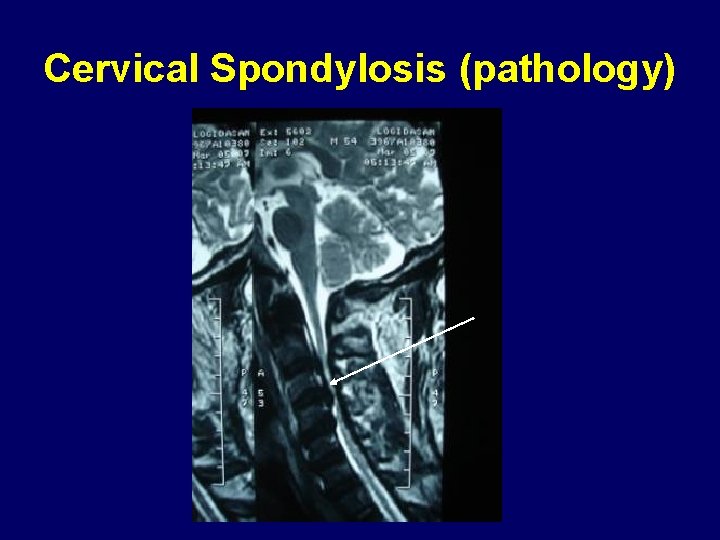
Cervical Spondylosis (pathology) • Ligaments: üThickening üOssification üBuckling ? üRupture.

Cervical Spondylosis (pathology)
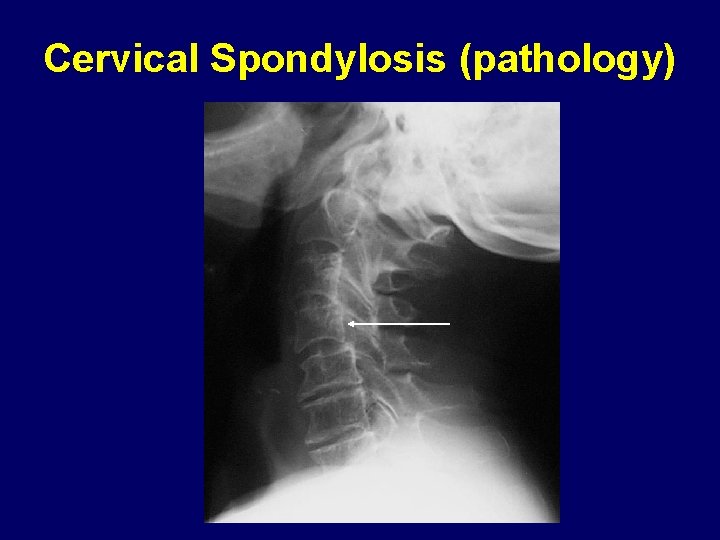
Cervical Spondylosis (pathology)

Cervical Spondylosis (pathology) • Joints: üReduced mobility üHypertrophy üSublaxation. üInflamation.
Cervical Spondylosis (pathology)
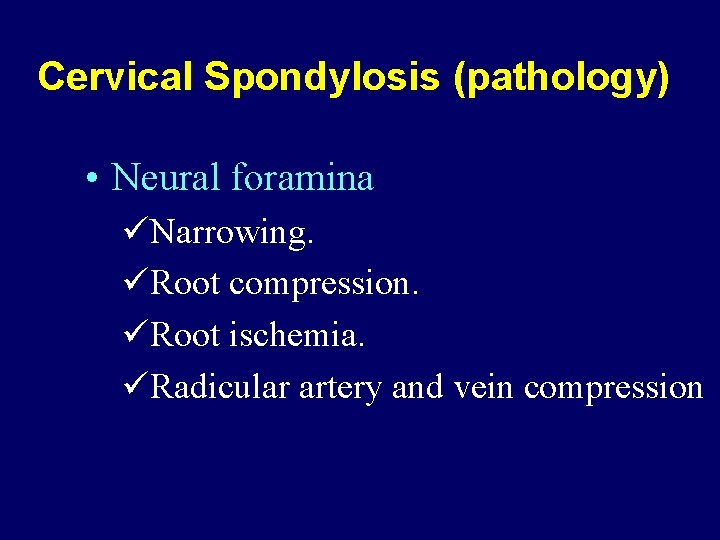
Cervical Spondylosis (pathology) • Neural foramina üNarrowing. üRoot compression. üRoot ischemia. üRadicular artery and vein compression
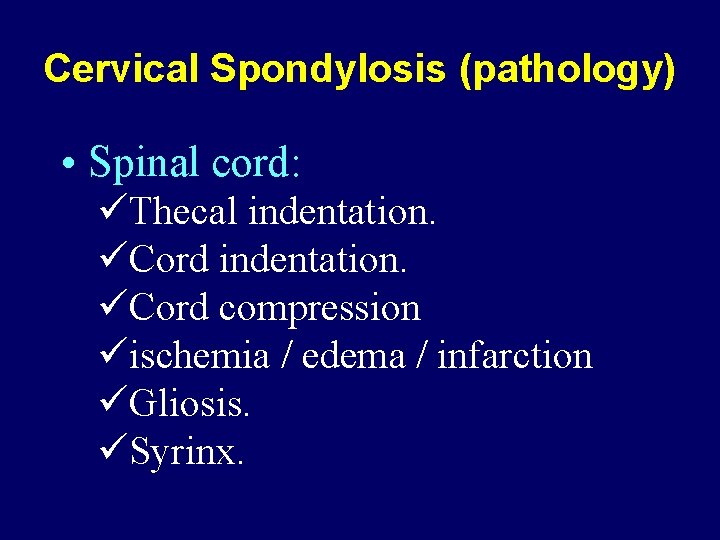
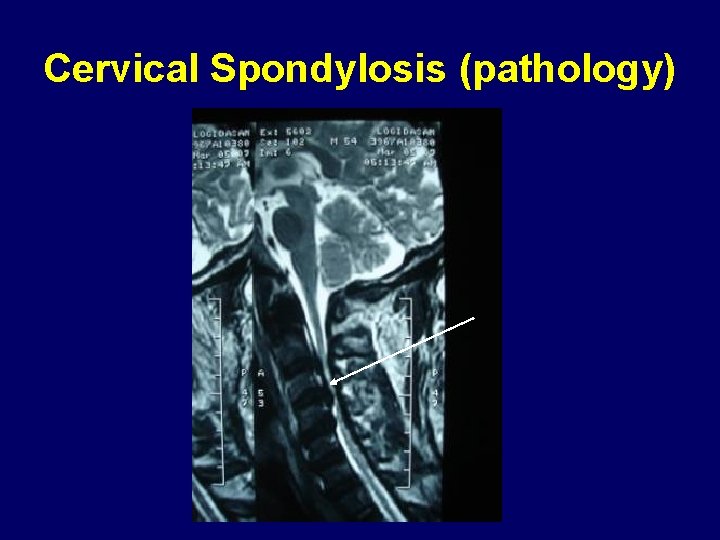
Cervical Spondylosis (pathology) • Spinal cord: üThecal indentation. üCord compression üischemia / edema / infarction üGliosis. üSyrinx.
Clinical presentation • History : üThe course may be slowly progressive , the patient may be asymptomatic or has mild neck pain. üAcute on top of chronic deterioration may occurs , and may be predisposed by trauma.
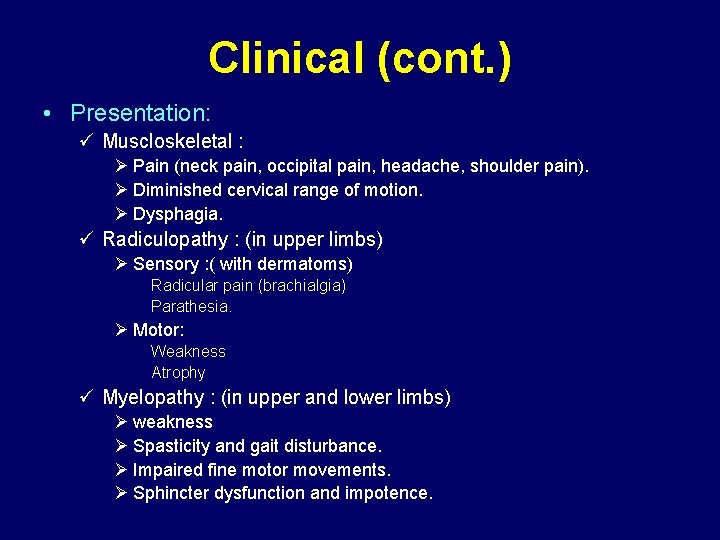
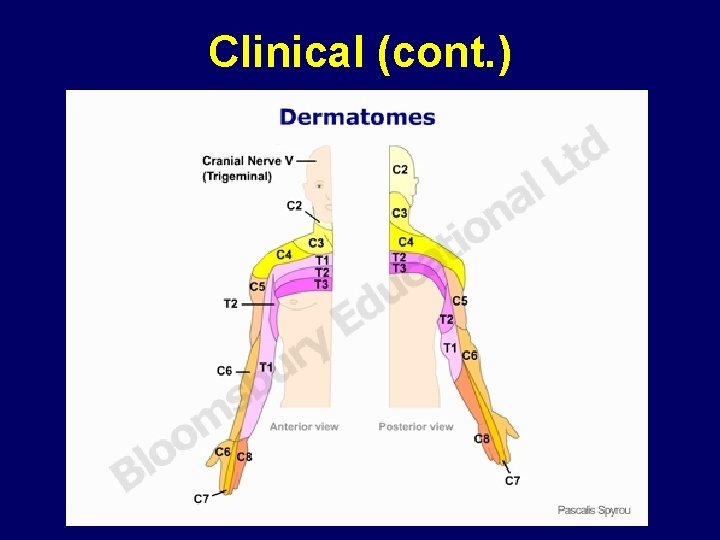
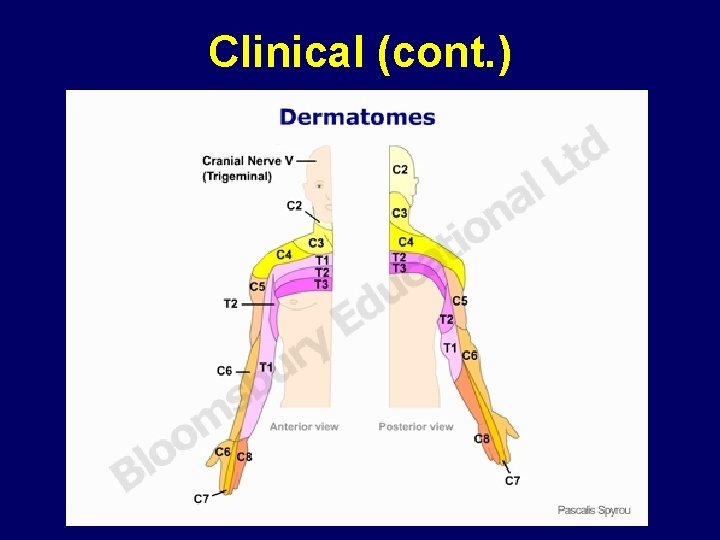
Clinical (cont. ) • Presentation: ü Muscloskeletal : Ø Pain (neck pain, occipital pain, headache, shoulder pain). Ø Diminished cervical range of motion. Ø Dysphagia. ü Radiculopathy : (in upper limbs) Ø Sensory : ( with dermatoms) Radicular pain (brachialgia) Parathesia. Ø Motor: Weakness Atrophy ü Myelopathy : (in upper and lower limbs) Ø weakness Ø Spasticity and gait disturbance. Ø Impaired fine motor movements. Ø Sphincter dysfunction and impotence.
Clinical (cont. )
Clinical (cont. ) • Examination: ü Local: Ø Decreased range of motion especially with neck extension Ø L’hermitte sign. ü Neurological : Ø Motor: - Spastic quadriparisis or paraparisis (below the level of compression) - Weakness taking myotomal distribution (according to level of compression) Ø Reflexes: - Hyper-reflexia , clonus (below the level). - Pathological reflexes (hoffman sign, pectoralis reflex, adductor reflex, babiniski reflex) - Hypo-reflexia (at the level) Ø Sensory: Hypothesia with dermatomal distribution or with sensory level
• Differential diagnosis
Correlation between radiological and clinical findings is mandatory.
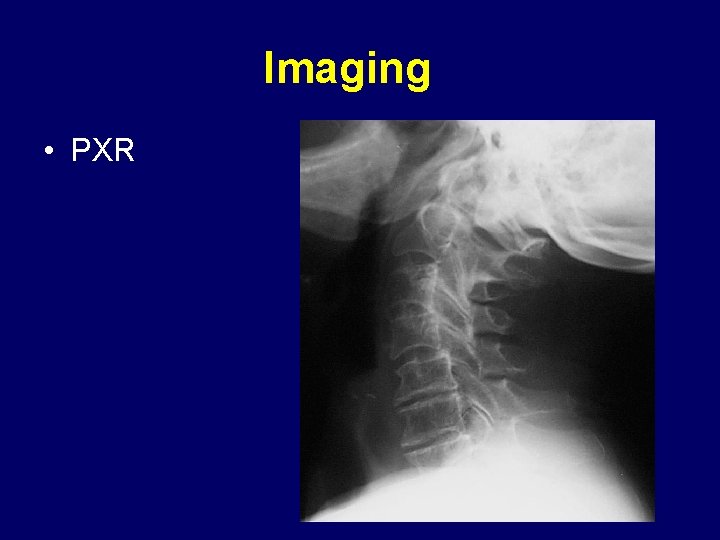
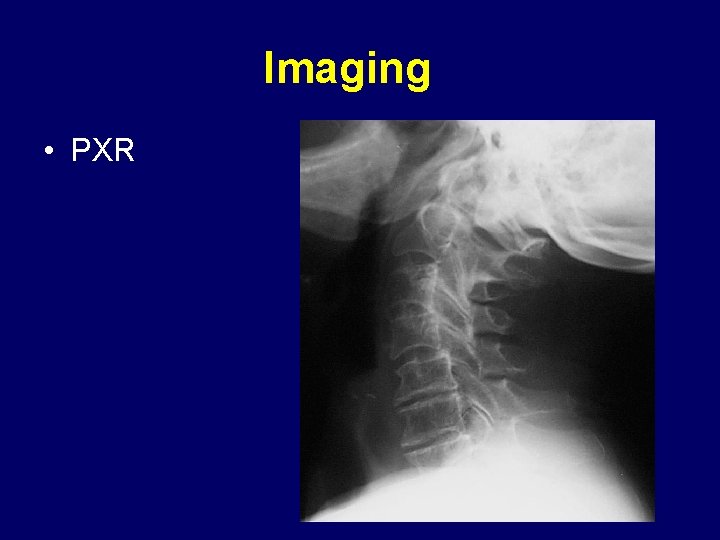
Imaging • PXR
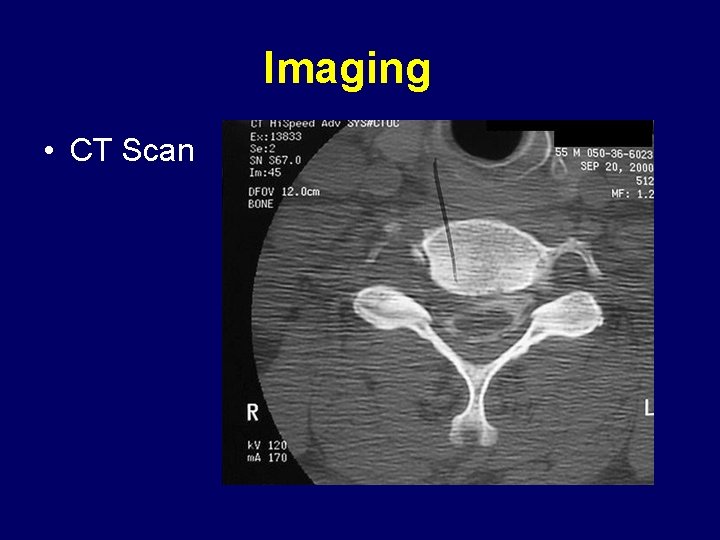
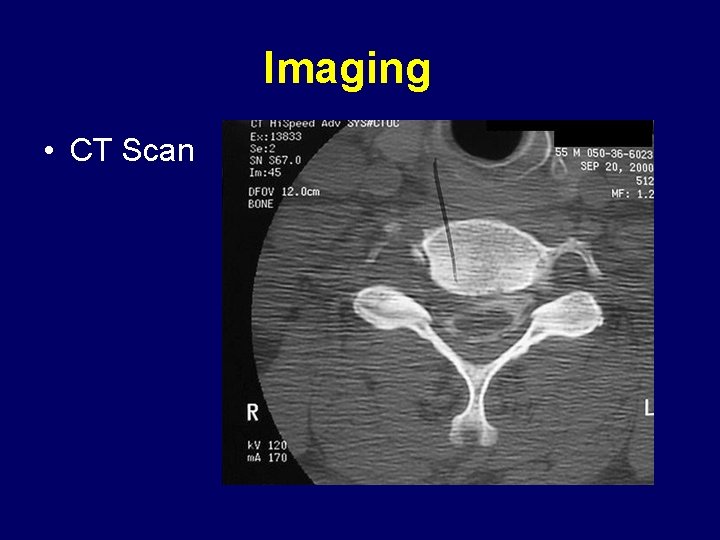
Imaging • CT Scan
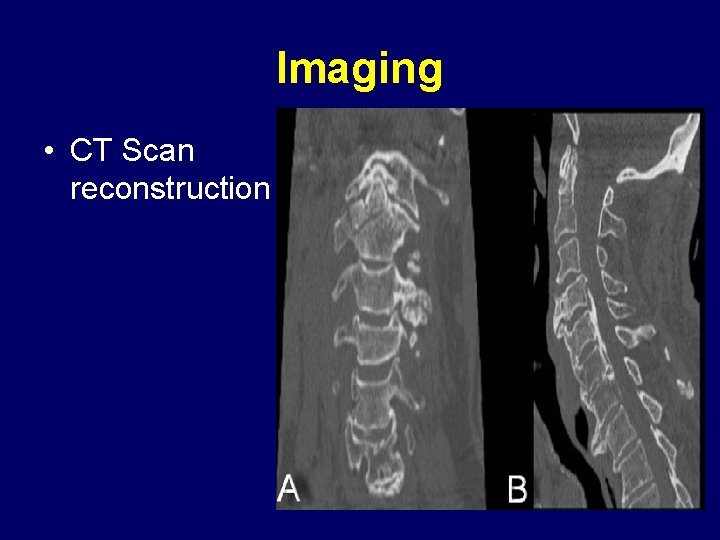
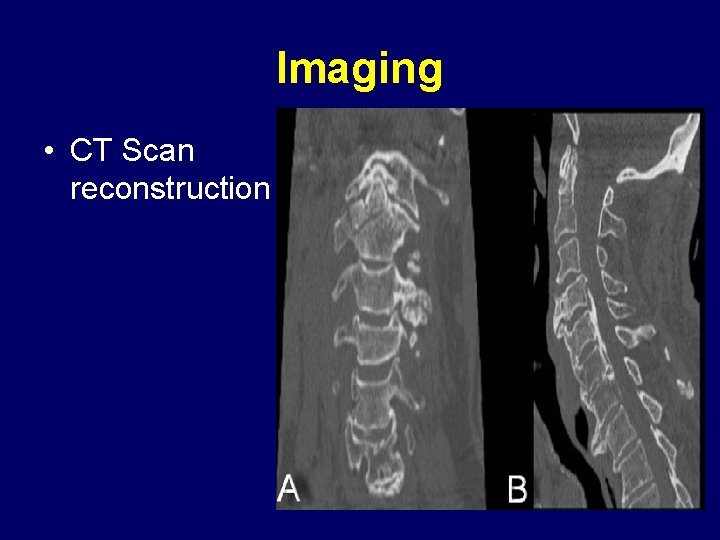
Imaging • CT Scan reconstruction
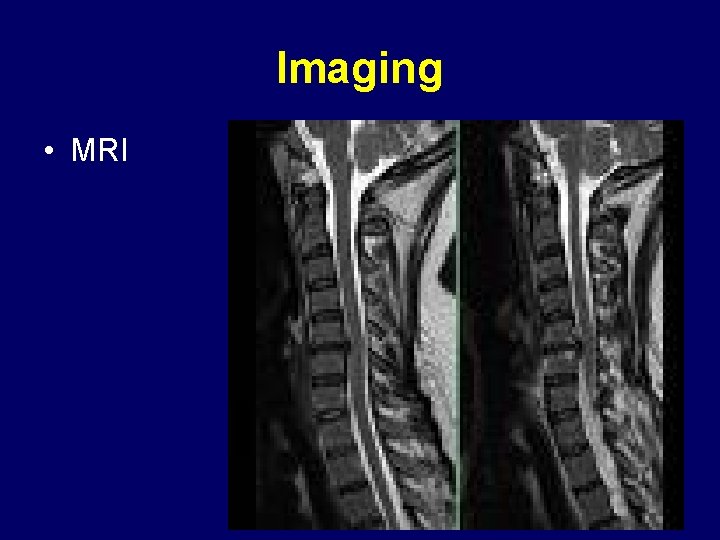
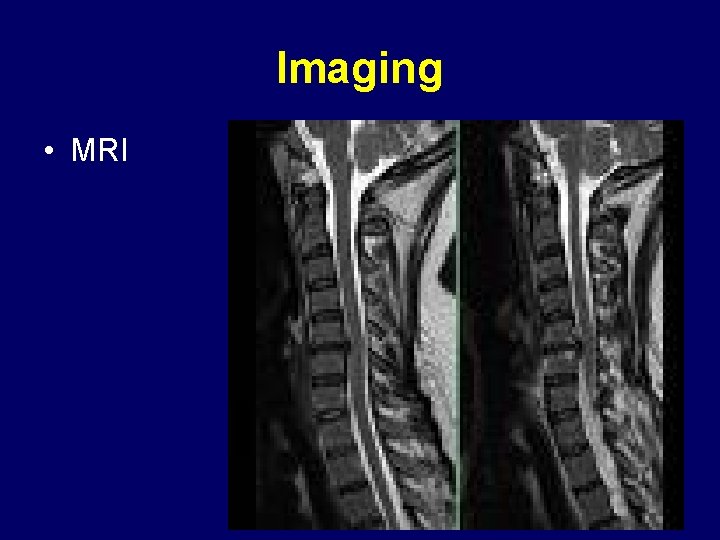
Imaging • MRI
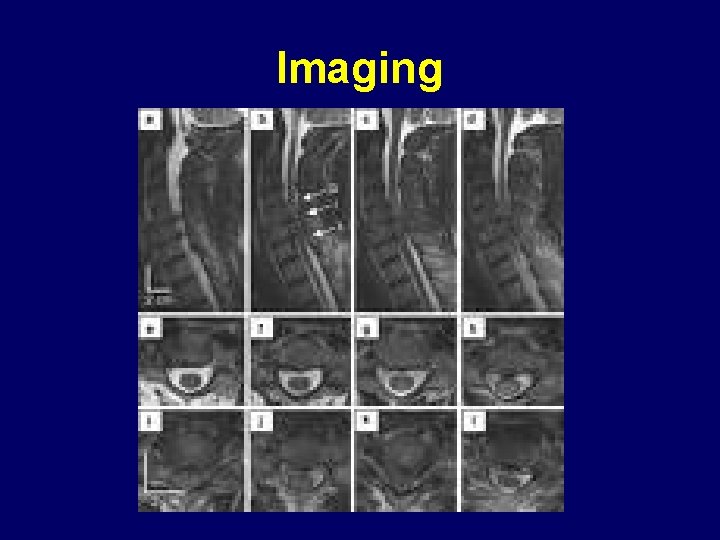
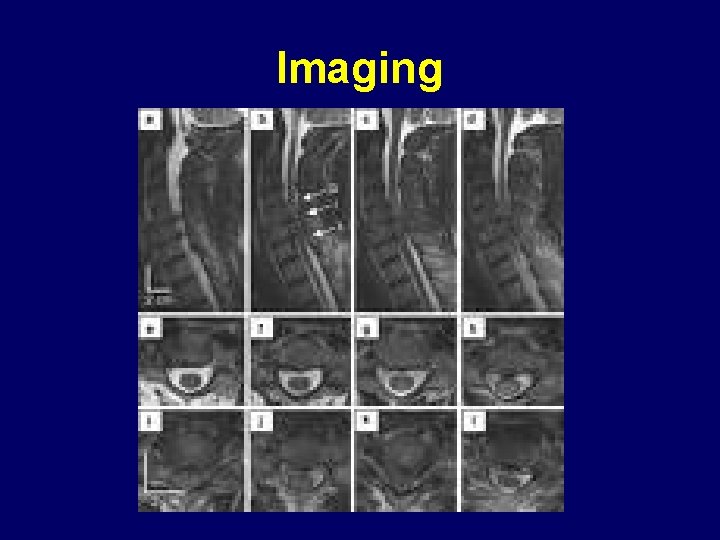
Imaging
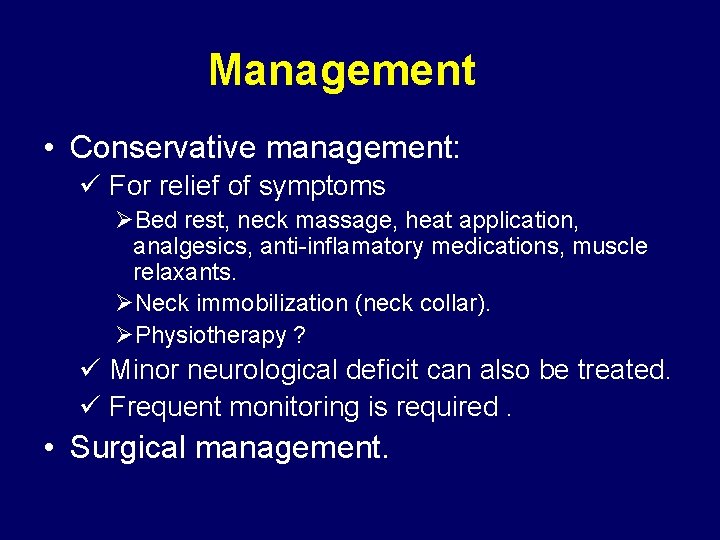
Management • Conservative management: ü For relief of symptoms ØBed rest, neck massage, heat application, analgesics, anti-inflamatory medications, muscle relaxants. ØNeck immobilization (neck collar). ØPhysiotherapy ? ü Minor neurological deficit can also be treated. ü Frequent monitoring is required. • Surgical management.
Management Surgical management • Indications: ü ü Intractable pain due to identified cause. Progressive neurologic deficite. Root compression clinicaly correlated to radiological finding. Instability • Aim of surgery ü Relieve pain and neuronal compression. ü Achieve stability. • Choice of procedure ü Depends upon findings on imaging ü Level of disease process. ü Extent of pathological changes.
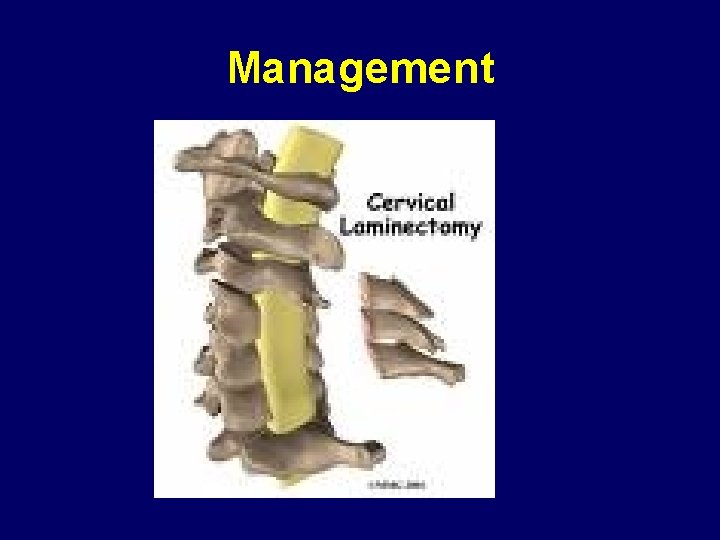
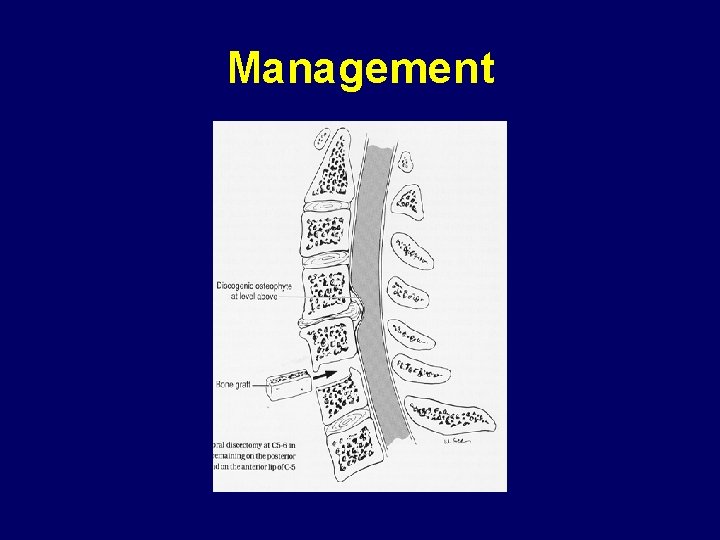
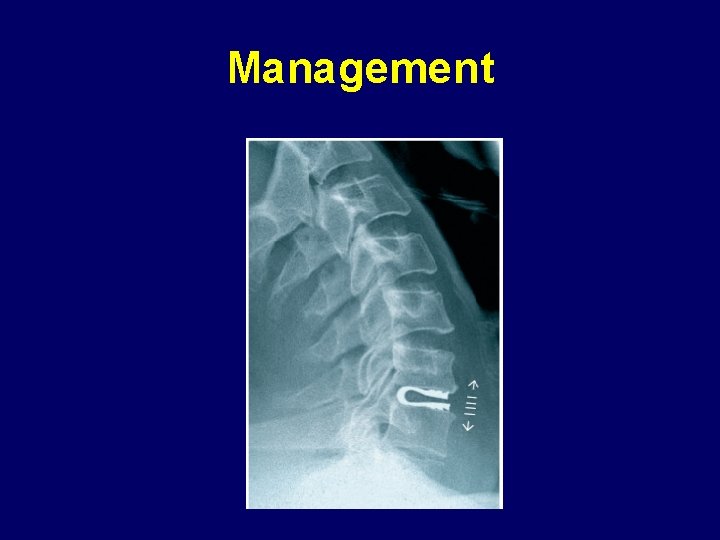
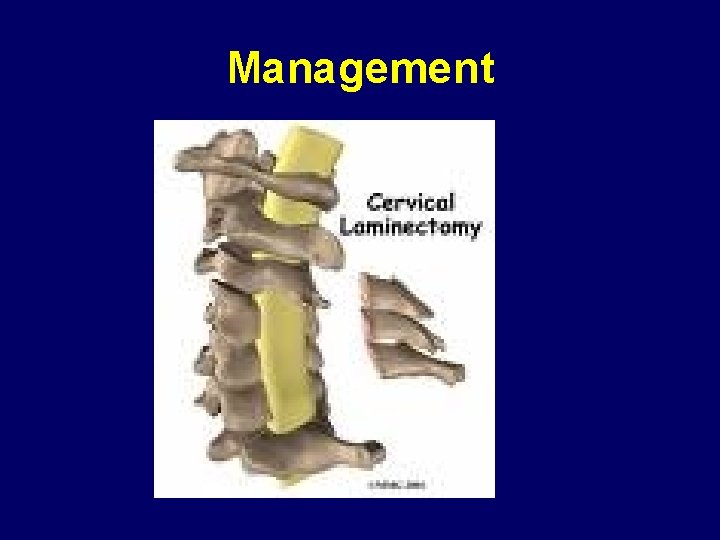
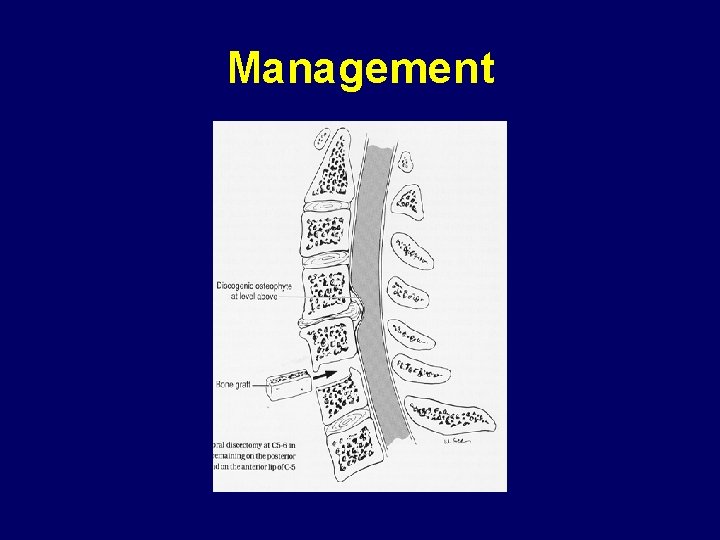
Management • Surgical procedures ü Posterior approaches: Ø Laminectomy. Ø Posterior foraminotomy. Ø Laminoplasty. Ø With or without fixation with plate and screws. NB. Posterior approaches for posterior pathology. ü Anterior approaches: Ø Anterior cervical discectomy/osteophytectomy and fusion. Ø Corpectomy with fusion and fixation. Ø Anterior foraminotomy. Ø Cervical arthroplasty. (artificial disc and dynamic implants) ü Percutaneous facet injection or radiofrequency.
Management
Management
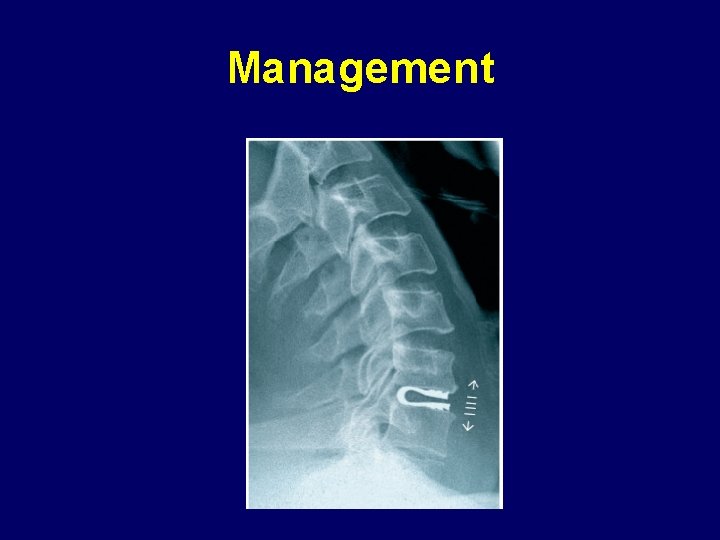
Management
Take home messages • Correlation • Diffrenttial • Different approaches acc to path

 Myelopathy vs radiculopathy
Myelopathy vs radiculopathy Cervical myelopathy wayne
Cervical myelopathy wayne L
L Uncovertebralis
Uncovertebralis Spondylolisthesis
Spondylolisthesis Spondylosis definition medical
Spondylosis definition medical Spinal cord spasticity
Spinal cord spasticity Surfer's myelopathy
Surfer's myelopathy Degenerative myelopathy wayne
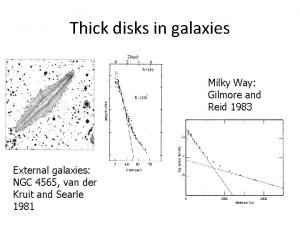
Degenerative myelopathy wayne Thick disc
Thick disc Platelets yellow
Platelets yellow Miller disc method
Miller disc method Tidewater disc golf course
Tidewater disc golf course Examples of optical storage devices
Examples of optical storage devices Aria totala con circular drept
Aria totala con circular drept Elliquence disc fx
Elliquence disc fx Reticulocyte normal
Reticulocyte normal Plasma disc decompression
Plasma disc decompression Extended disc sverige
Extended disc sverige Device handler seek strategies
Device handler seek strategies Hubless rotors are held onto the hub by
Hubless rotors are held onto the hub by Merkel disc receptor
Merkel disc receptor Ontario disc sports association
Ontario disc sports association Neurulation
Neurulation Parts of a compound light microscope and their functions
Parts of a compound light microscope and their functions Disc profil
Disc profil Dorsiflexion plantar
Dorsiflexion plantar Brown dwarf
Brown dwarf Champagne cork appearance of optic disc
Champagne cork appearance of optic disc Cow eye
Cow eye Www.123 test.com/disc-personality-test/
Www.123 test.com/disc-personality-test/ 123 disc personality test
123 disc personality test Sound-on-disc
Sound-on-disc Linear momentum in circular motion
Linear momentum in circular motion Bronze age sun disc
Bronze age sun disc Choroid in cow eye
Choroid in cow eye Taking flight with disc
Taking flight with disc Chorionic villus
Chorionic villus Broad-based disc bulge
Broad-based disc bulge