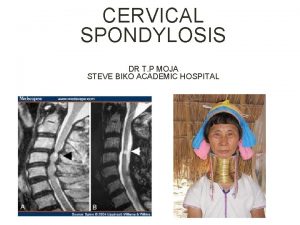
Cervical Spondylosis LIAO Hui MD Tongji Hospital HUST









- Slides: 37
Cervical Spondylosis LIAO Hui MD Tongji Hospital, HUST 2012. 11. 21

Degenerative Disease of the Spine Degenerative processes of aging occur at different rates, locations, and modalities, based on the unique attributes of individuals (factors known to influence degenerative diseases of the spine include lifestyle, work patterns, diet, and even genetics) Normal Degenerative

Cervical Spondylosis Cervical spondylosis is a general term encompassing a number of degenerative conditions ³ ³ ³ Degenerative disc disease (DDD) Spinal stenosis With or without degenerative facet joints With or without the formation of osteophytes With or without a herniated disc One single component as a diagnosis is rare
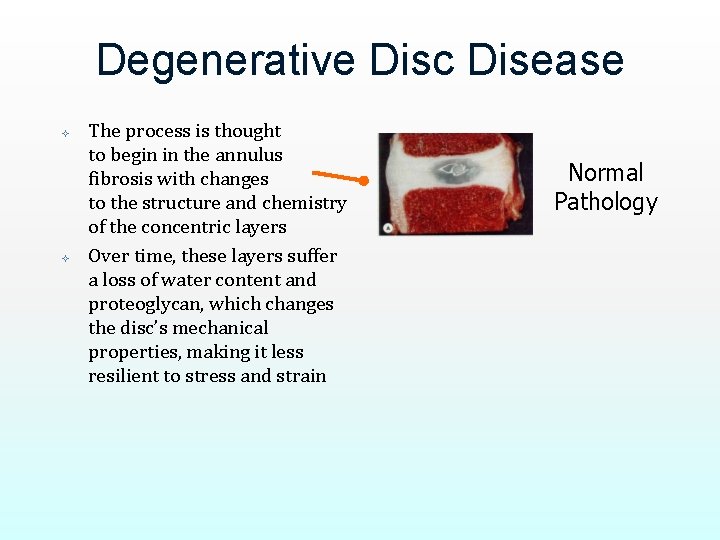
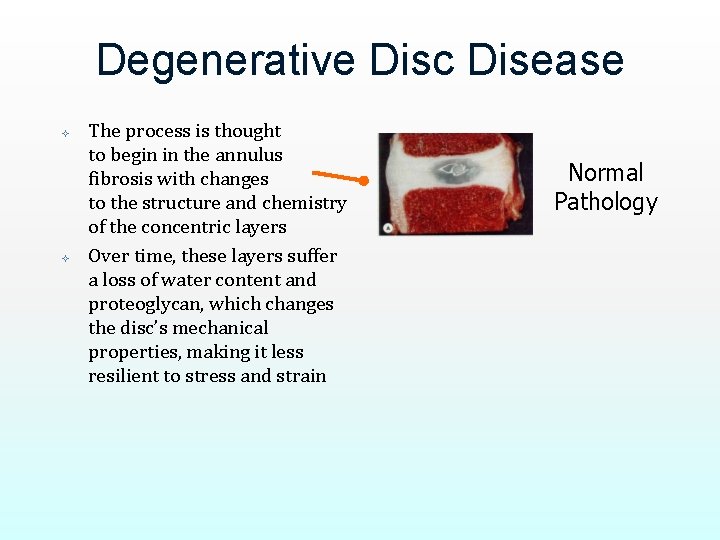
Degenerative Disc Disease The process is thought to begin in the annulus fibrosis with changes to the structure and chemistry of the concentric layers Over time, these layers suffer a loss of water content and proteoglycan, which changes the disc’s mechanical properties, making it less resilient to stress and strain Normal Pathology
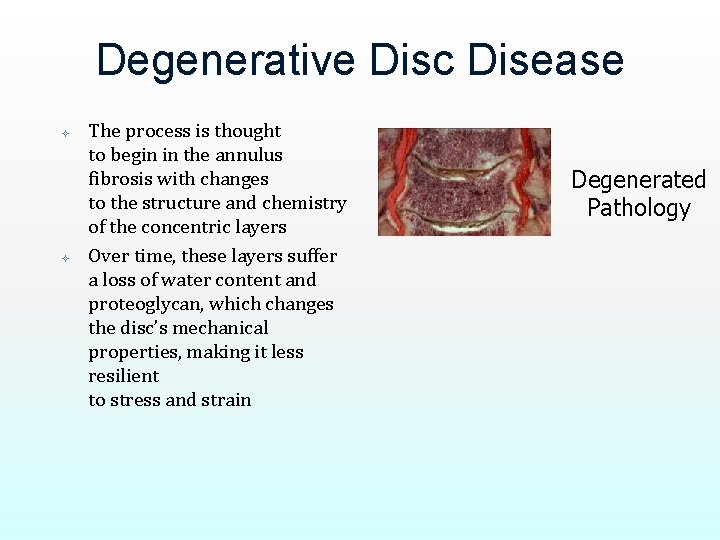
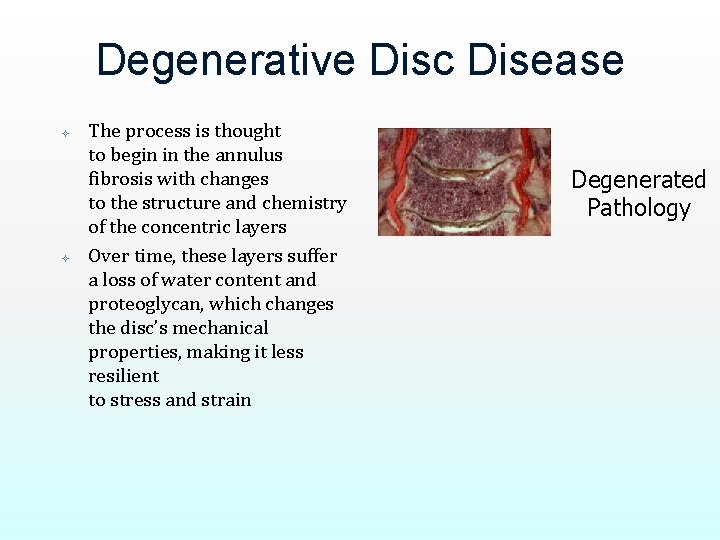
Degenerative Disc Disease The process is thought to begin in the annulus fibrosis with changes to the structure and chemistry of the concentric layers Over time, these layers suffer a loss of water content and proteoglycan, which changes the disc’s mechanical properties, making it less resilient to stress and strain Degenerated Pathology
Degenerative Disease: Facet Joints Changes in disc structure and function can lead to changes in the articular facets, especially hypertrophy (overgrowth), resulting from the redirection of compressive loads from the anterior and middle columns to the posterior elements
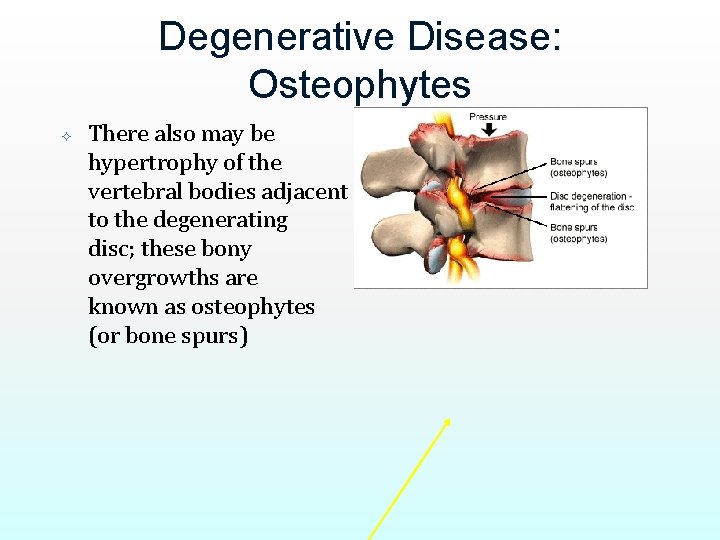
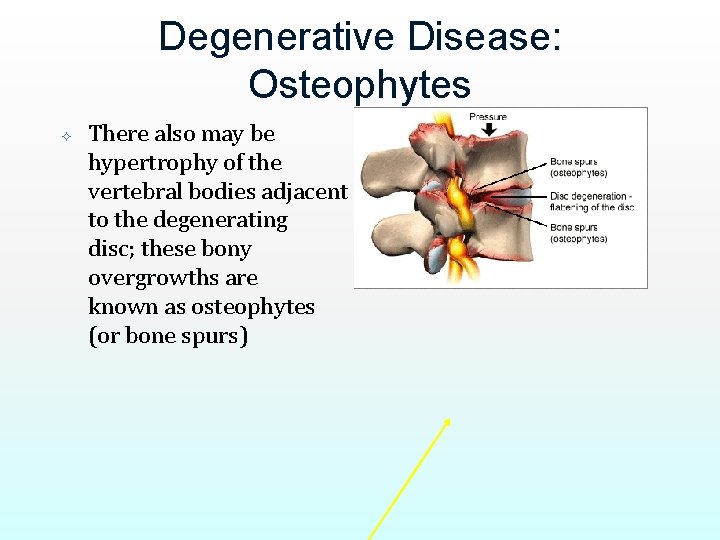
Degenerative Disease: Osteophytes There also may be hypertrophy of the vertebral bodies adjacent to the degenerating disc; these bony overgrowths are known as osteophytes (or bone spurs)
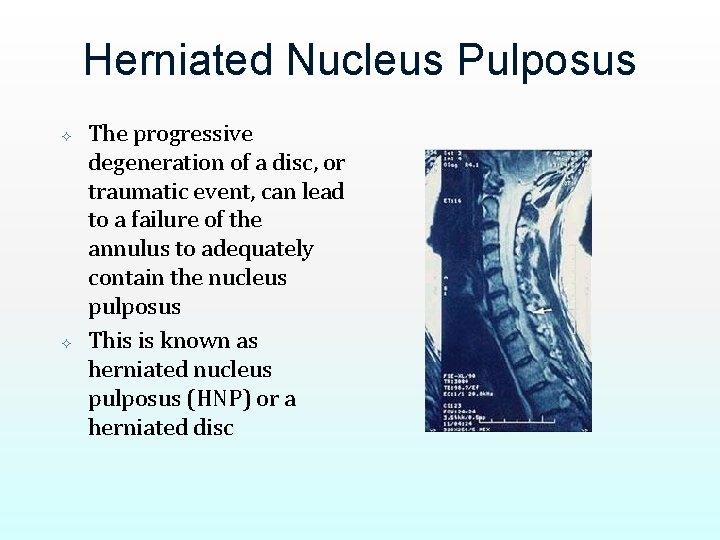
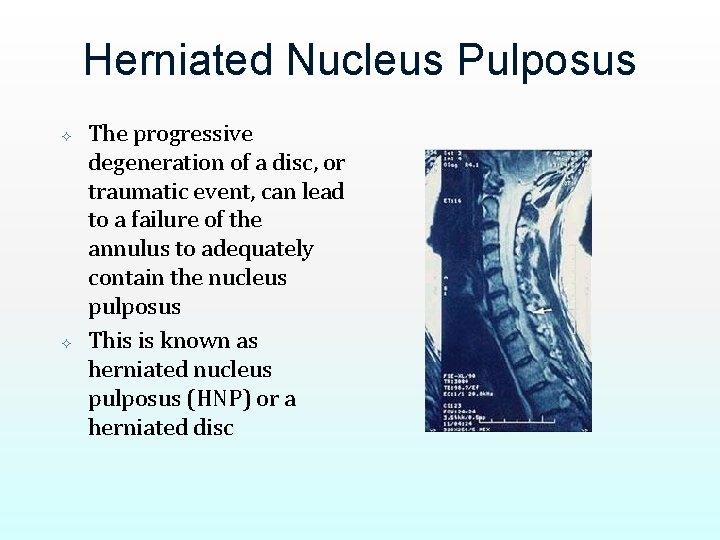
Herniated Nucleus Pulposus The progressive degeneration of a disc, or traumatic event, can lead to a failure of the annulus to adequately contain the nucleus pulposus This is known as herniated nucleus pulposus (HNP) or a herniated disc
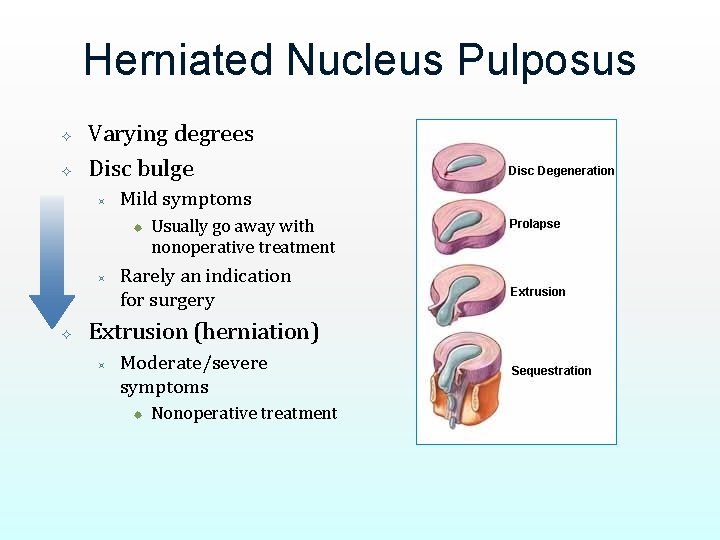
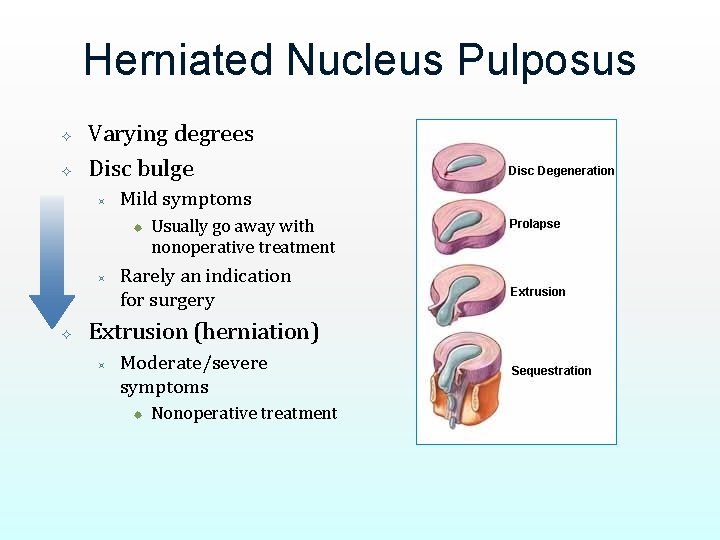
Herniated Nucleus Pulposus Varying degrees Disc bulge ³ Mild symptoms ® ³ Usually go away with nonoperative treatment Rarely an indication for surgery Extrusion (herniation) ³ Moderate/severe symptoms ® Nonoperative treatment
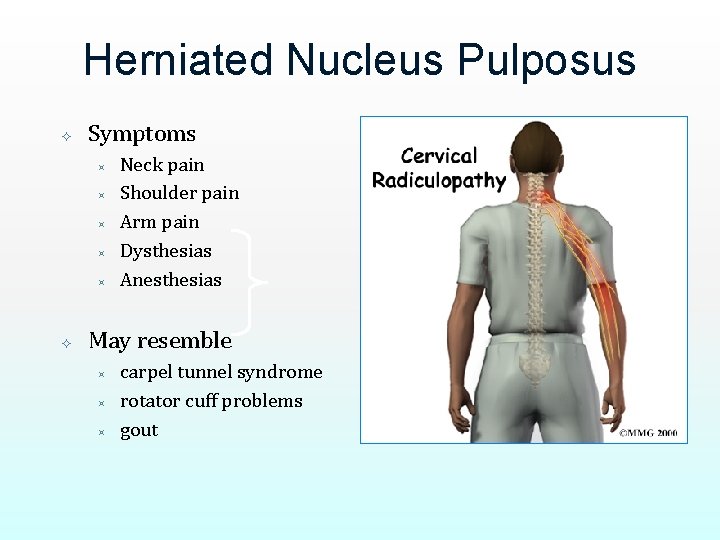
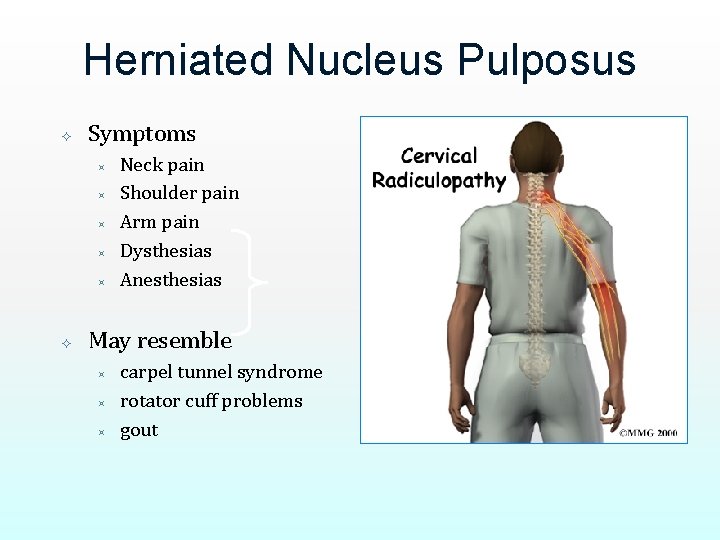
Herniated Nucleus Pulposus Symptoms ³ ³ ³ Neck pain Shoulder pain Arm pain Dysthesias Anesthesias May resemble ³ ³ ³ carpel tunnel syndrome rotator cuff problems gout
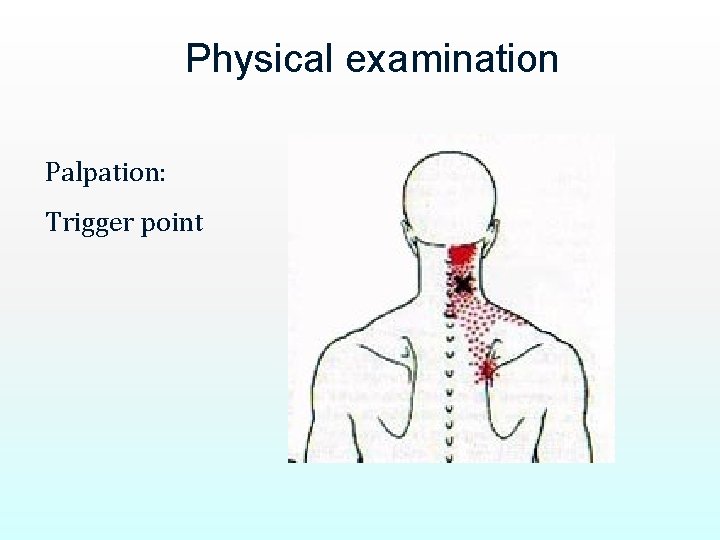
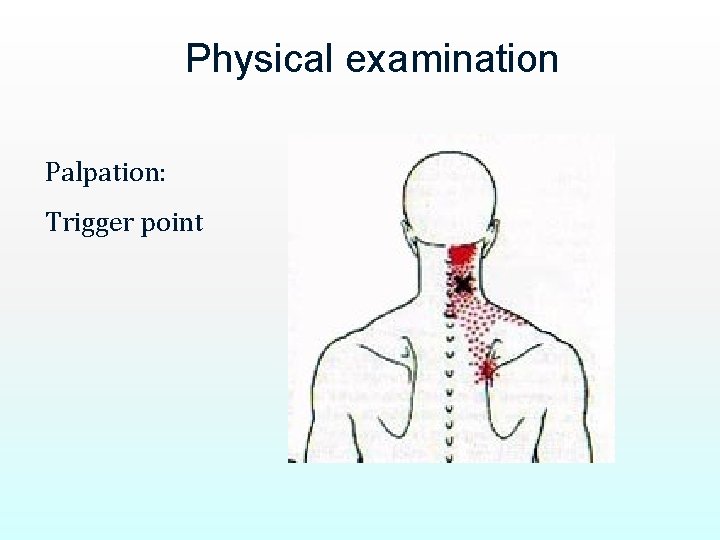
Physical examination Palpation: Trigger point
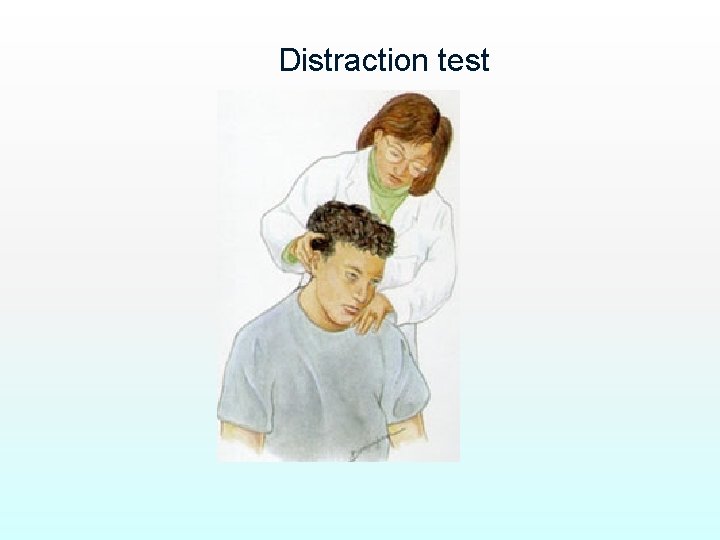
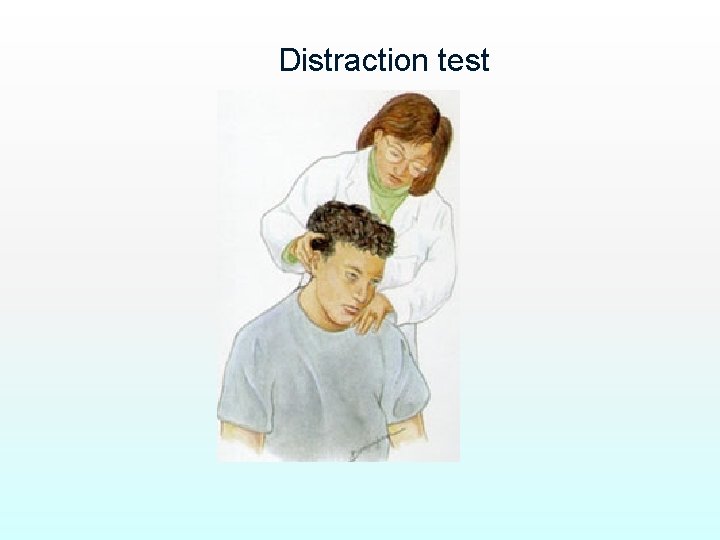
Distraction test
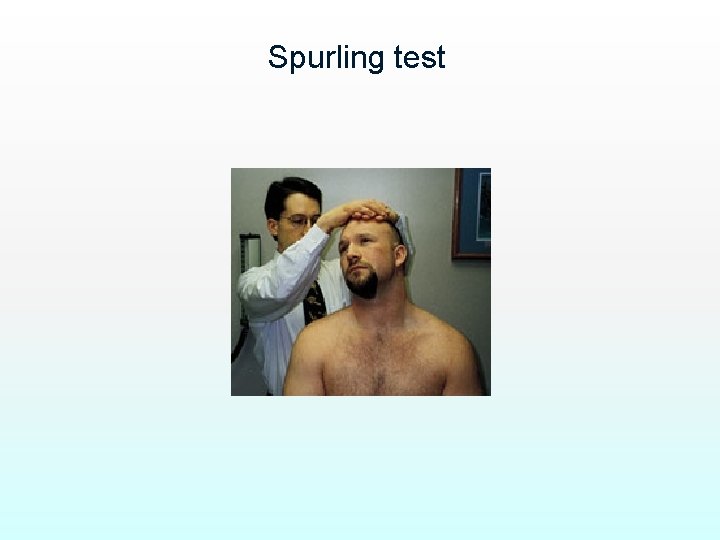
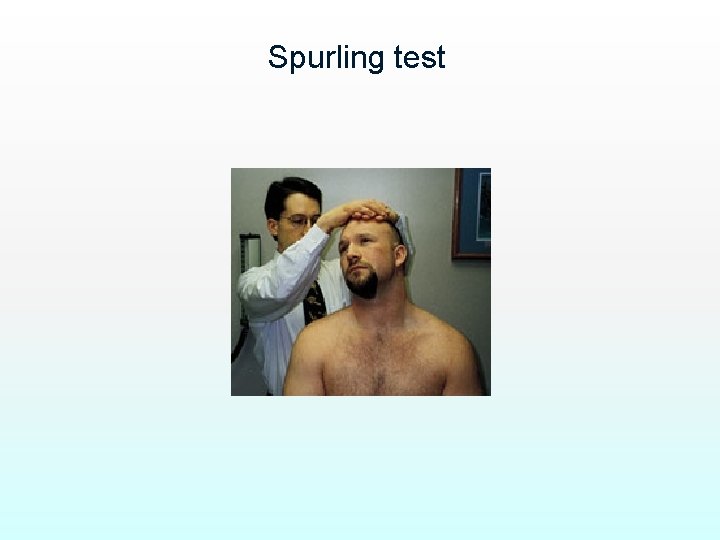
Spurling test
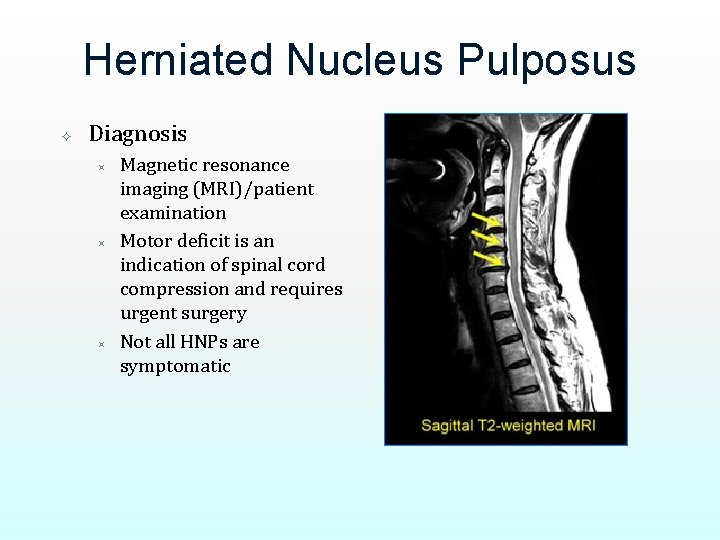
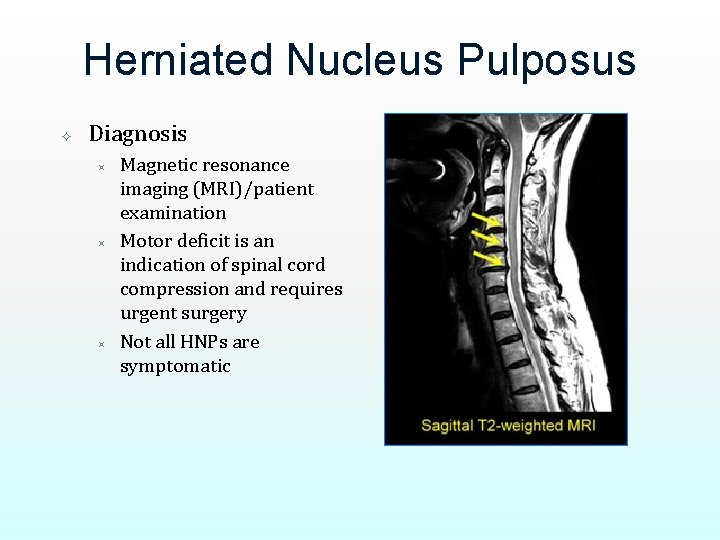
Herniated Nucleus Pulposus Diagnosis ³ ³ ³ Magnetic resonance imaging (MRI)/patient examination Motor deficit is an indication of spinal cord compression and requires urgent surgery Not all HNPs are symptomatic

Spinal Stenosis Spinal stenosis is the narrowing of the bony ring that surrounds the spinal cord. Causes include: ³ Bone spurs ³ Disc degeneration ³ Arthritis ³ Congenital This condition is most common in elderly people, who have had years of wear-and-tear on their spines
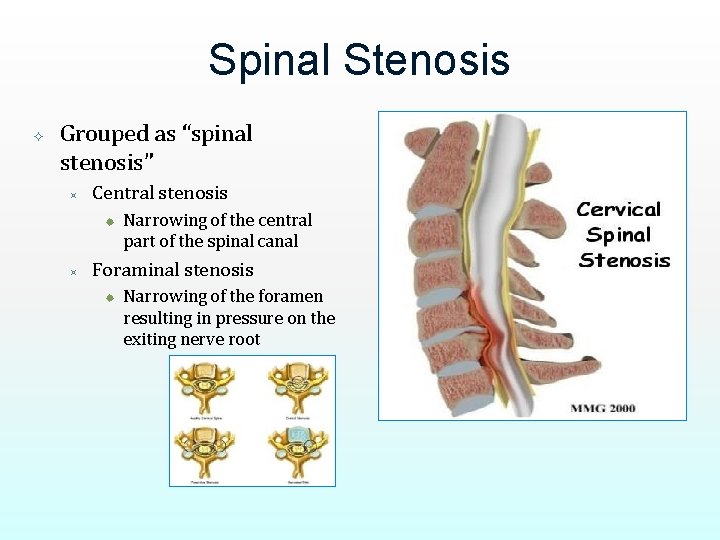
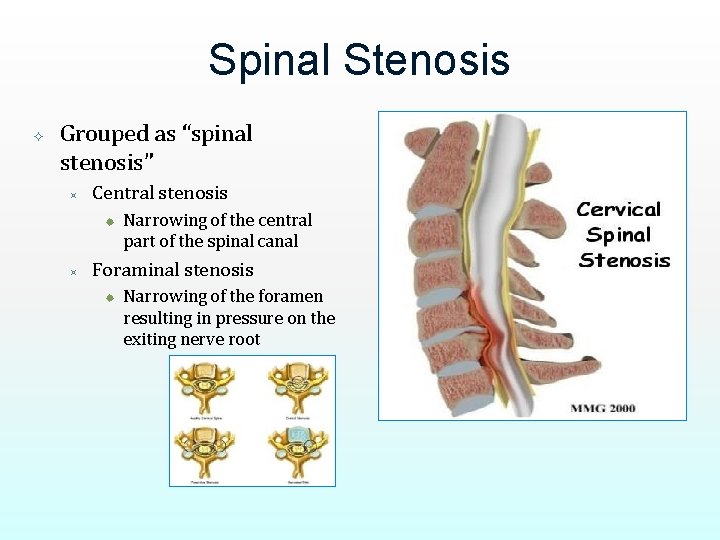
Spinal Stenosis Grouped as “spinal stenosis” ³ Central stenosis ® ³ Narrowing of the central part of the spinal canal Foraminal stenosis ® Narrowing of the foramen resulting in pressure on the exiting nerve root
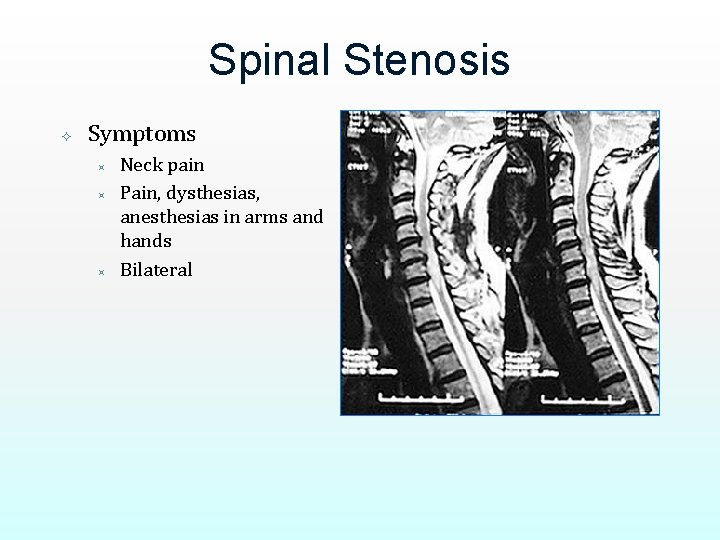
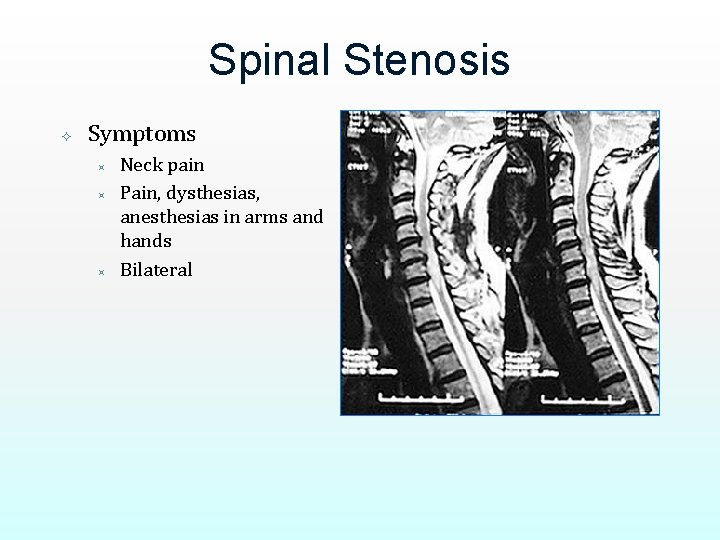
Spinal Stenosis Symptoms ³ ³ ³ Neck pain Pain, dysthesias, anesthesias in arms and hands Bilateral
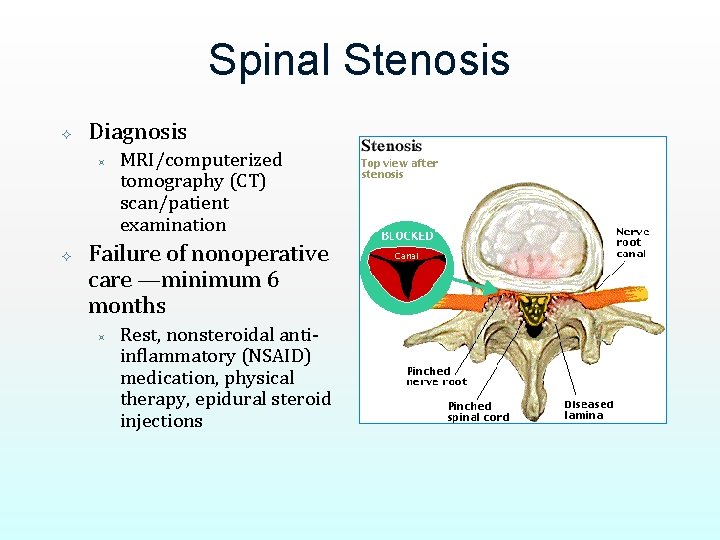
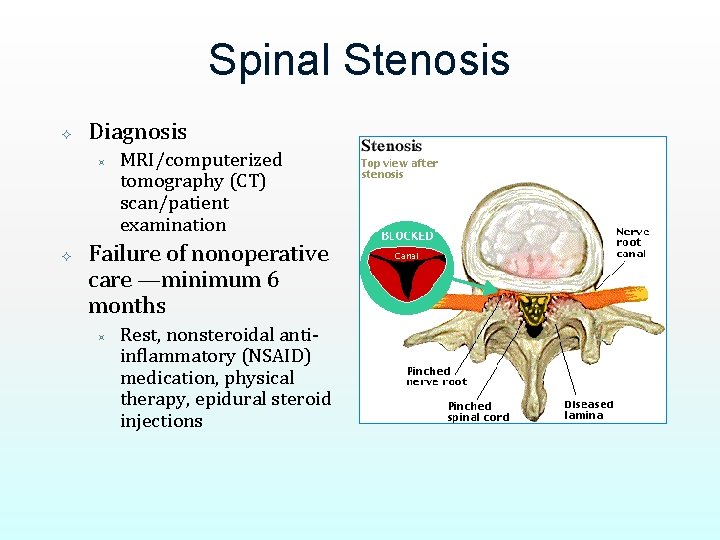
Spinal Stenosis Diagnosis ³ MRI/computerized tomography (CT) scan/patient examination Failure of nonoperative care —minimum 6 months ³ Rest, nonsteroidal antiinflammatory (NSAID) medication, physical therapy, epidural steroid injections
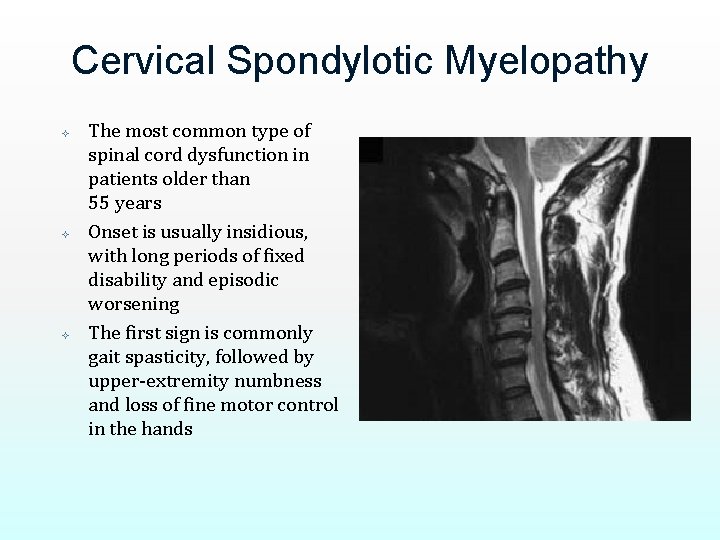
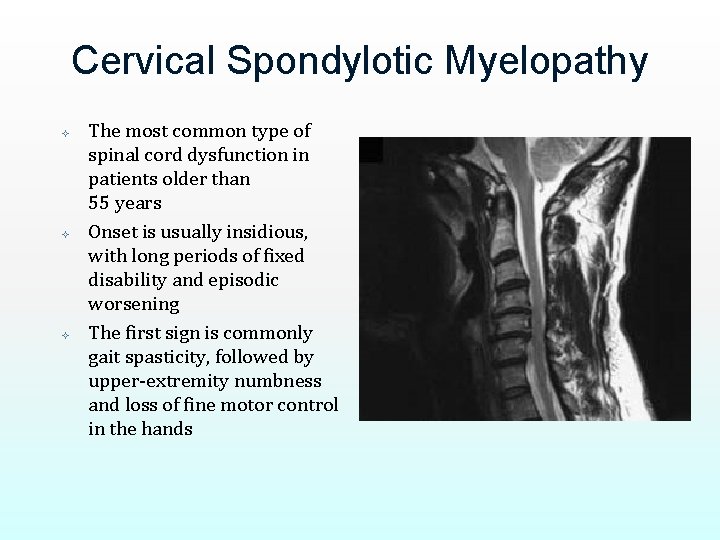
Cervical Spondylotic Myelopathy The most common type of spinal cord dysfunction in patients older than 55 years Onset is usually insidious, with long periods of fixed disability and episodic worsening The first sign is commonly gait spasticity, followed by upper-extremity numbness and loss of fine motor control in the hands
Cervical Spondylotic Myelopathy Unlike most degenerative conditions of the back and neck, conservative treatment is not indicated Performing surgery relatively early (within 1 year of symptom onset) is associated with a substantial improvement in neurologic prognosis Delay in surgical treatment can result in permanent impairment
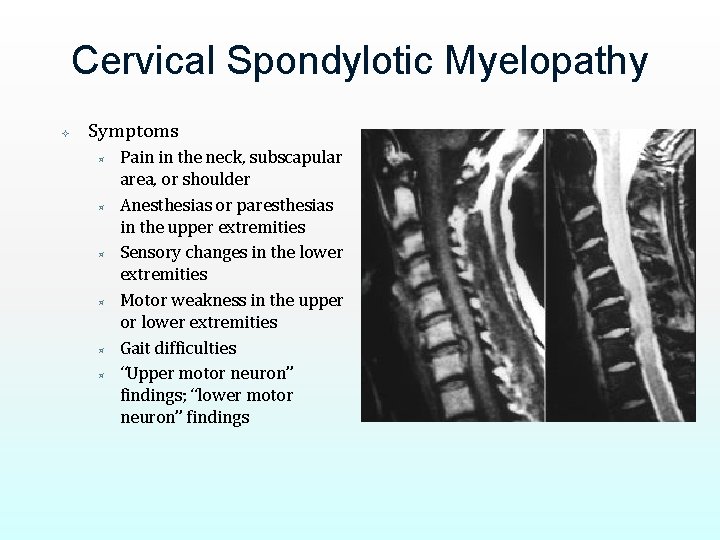
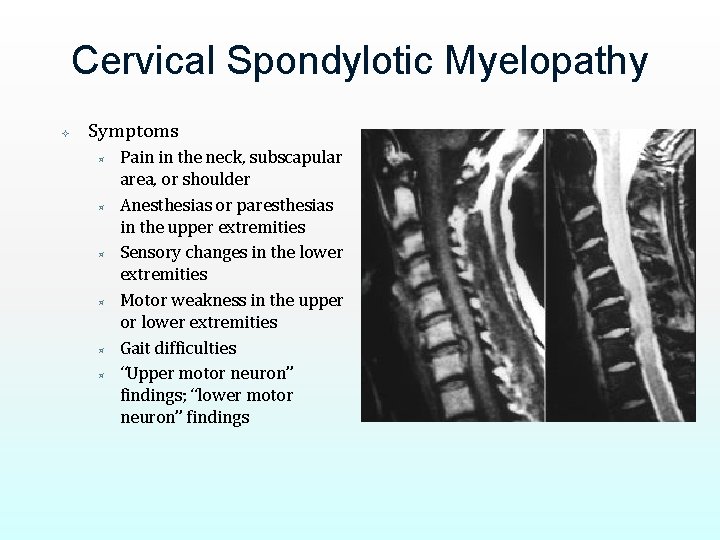
Cervical Spondylotic Myelopathy Symptoms ³ ³ ³ Pain in the neck, subscapular area, or shoulder Anesthesias or paresthesias in the upper extremities Sensory changes in the lower extremities Motor weakness in the upper or lower extremities Gait difficulties “Upper motor neuron” findings; “lower motor neuron” findings

Treatment The goal of treatment lrelief of pain lprevention of permanent spinal cord and nerve root injury. In mild cases, no treatment is required. l. Symptoms from cervical spondylosis usually stabilize or regress with simple lconservative therapy including a neck brace and NSAIDs.

Nonoperative treatment Halter traction Cervical support and collar Massage Physical therapy Analgesics and muscle relaxants Local block

Halter traction

Cervical collar
Massage

Analgesics ³ NSAIDS ® VOLTAREN ® Tramcontin Muscle relaxants
Cervical Spondylosis Without Myelopathy Surgical care ³ ³ ³ For radicular/neurologic symptoms Not for axial neck pain Dependent on the anatomy and the lordosis of the affected segments, and surgeon preference Anterior cervical discectomy and fusion ® Anterior cervical corpectomy (multiple levels) ® In some cases, adjunct posterior-instrumented fusion ®
Cervical Spondylotic Myelopathy Surgical care ³ ³ Posterior cervical fusion—instrumented Dependent upon the anatomy and the lordosis of the affected segments, and surgeon preference Posterior cervical fusion ® Laminoplasty ® May involve an adjunct anterior fusion procedure to address spondylosis ®

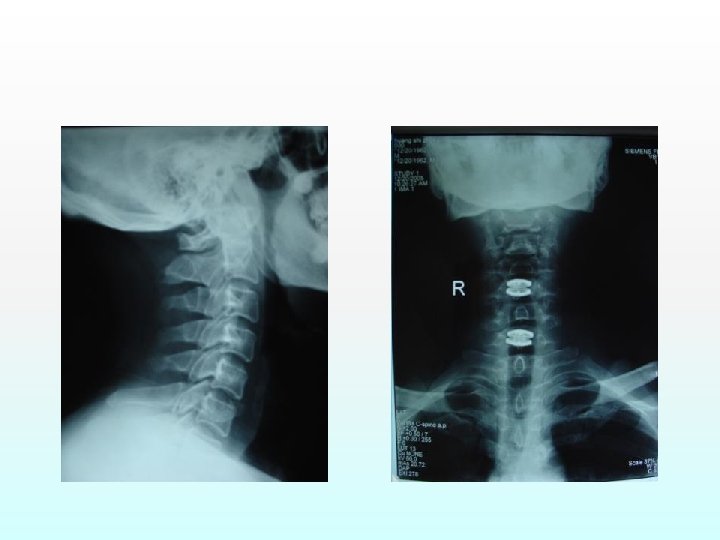
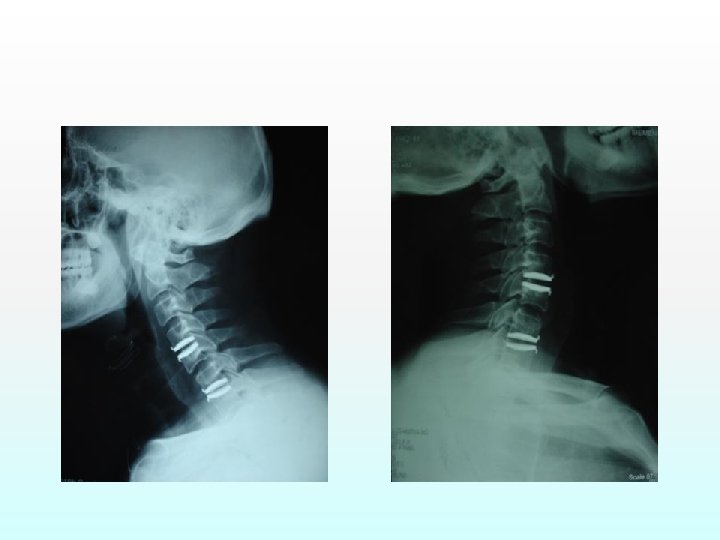
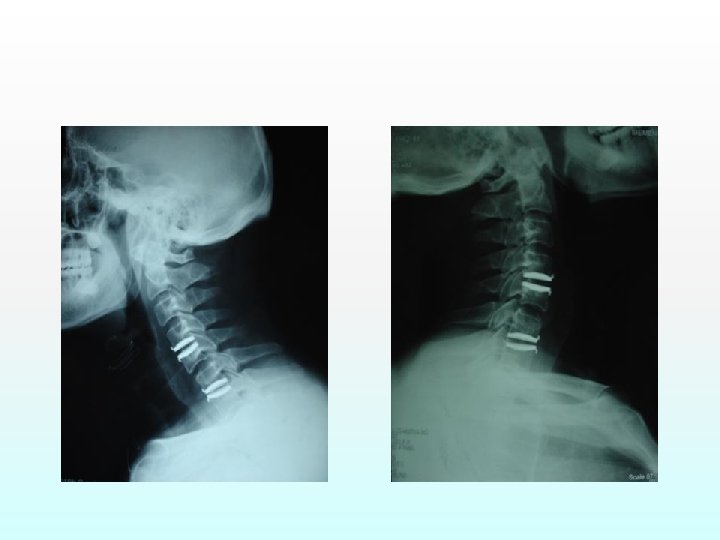
Anterior Cervical Discectomy and Fusion (ACDF) High success rate >90% for 1 level ³ ³ ³ Multilevels Disc removal/decompression Use of microscope Bone graft or other material for fusion Usually with plating
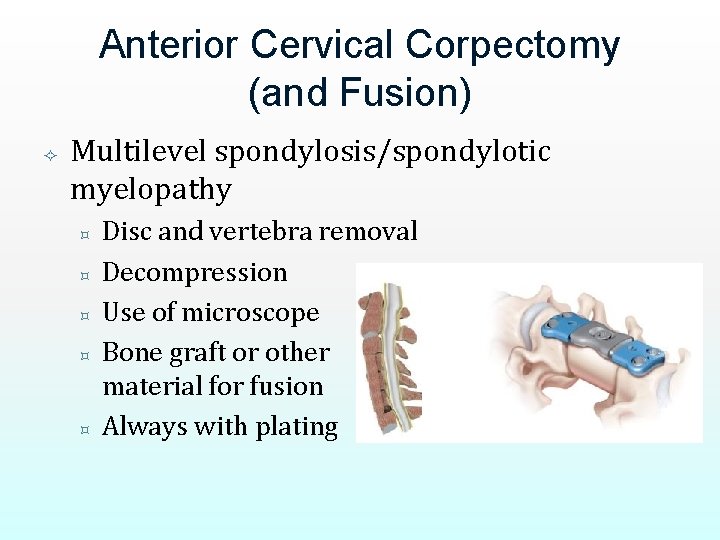
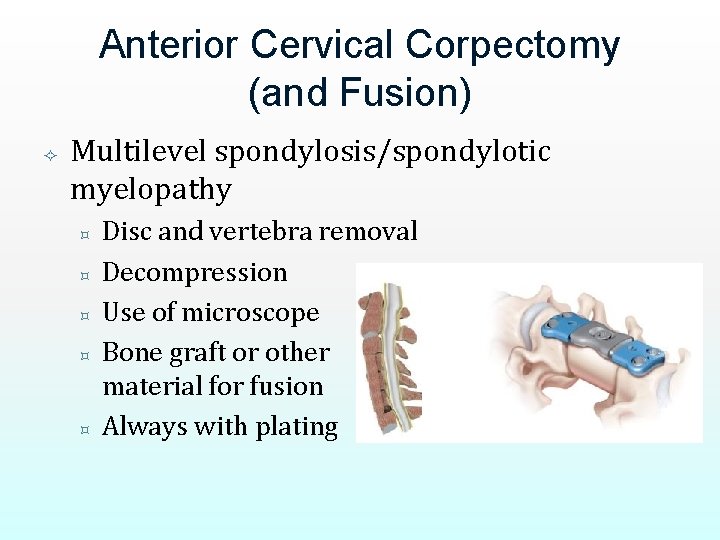
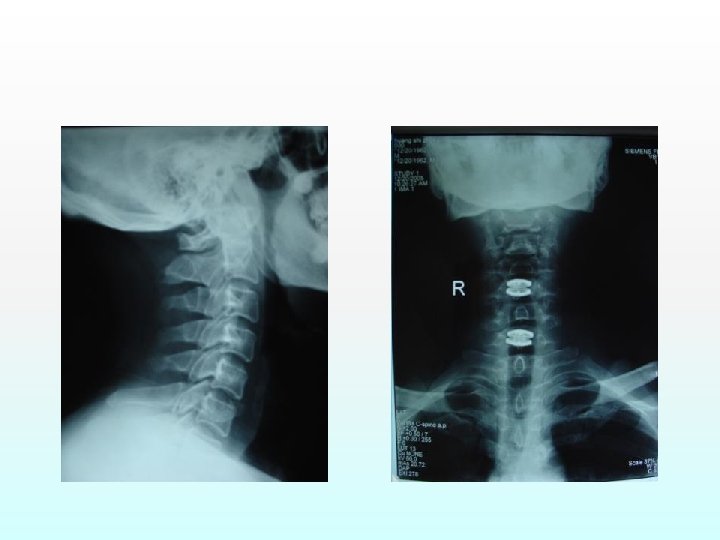
Anterior Cervical Corpectomy (and Fusion) Multilevel spondylosis/spondylotic myelopathy ³ ³ ³ Disc and vertebra removal Decompression Use of microscope Bone graft or other material for fusion Always with plating
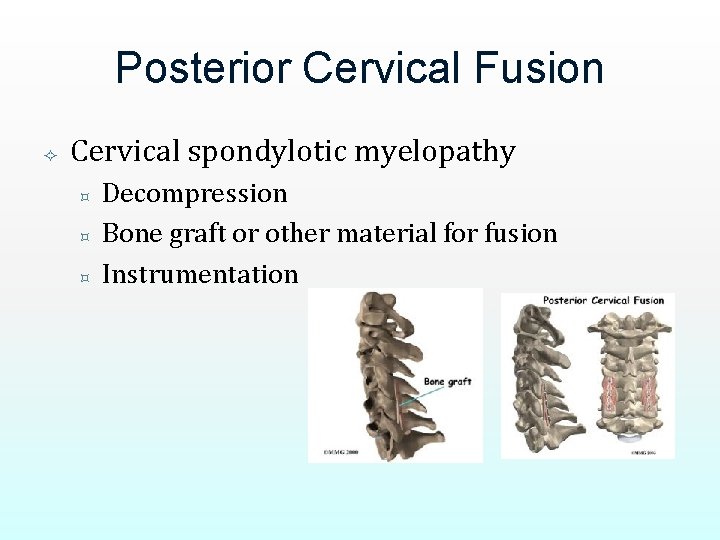
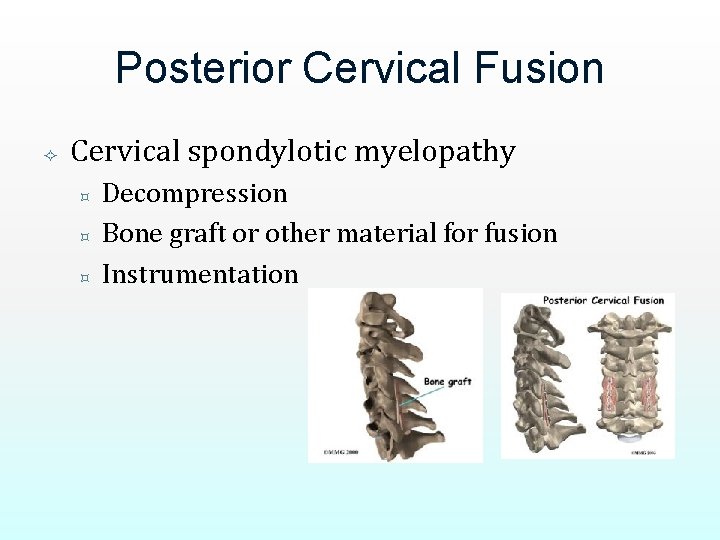
Posterior Cervical Fusion Cervical spondylotic myelopathy ³ ³ ³ Decompression Bone graft or other material for fusion Instrumentation
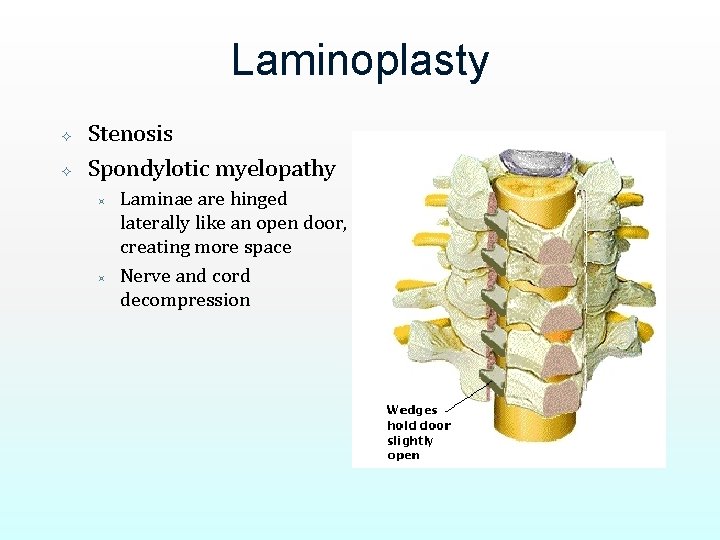
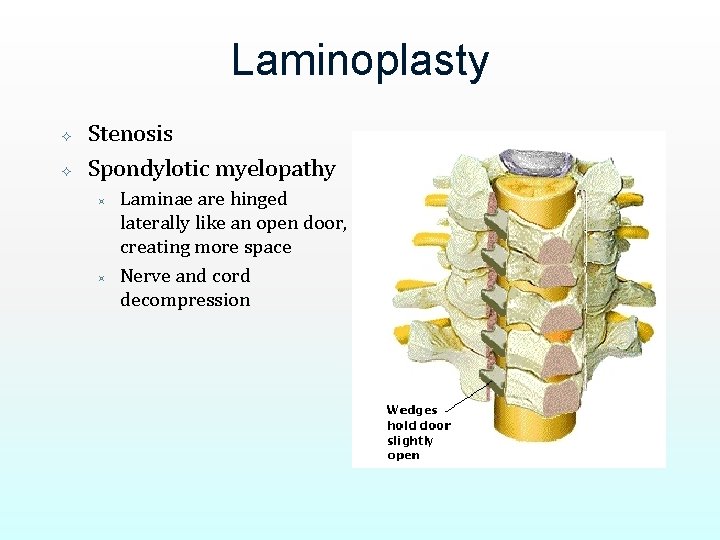
Laminoplasty Stenosis Spondylotic myelopathy ³ ³ Laminae are hinged laterally like an open door, creating more space Nerve and cord decompression
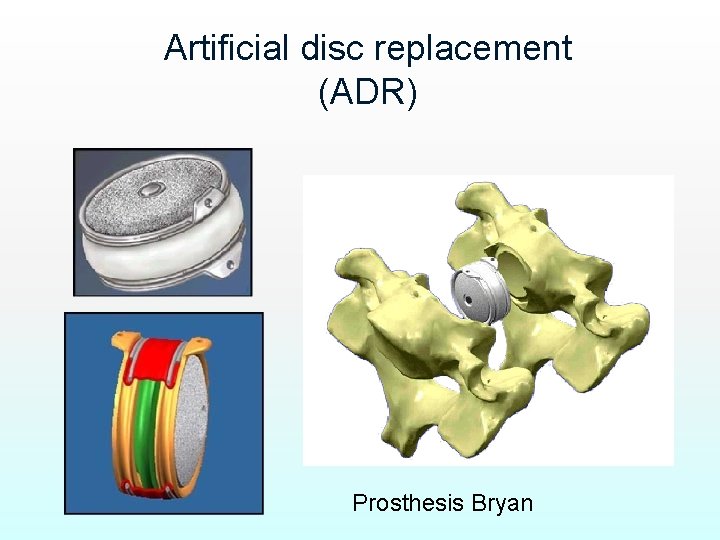
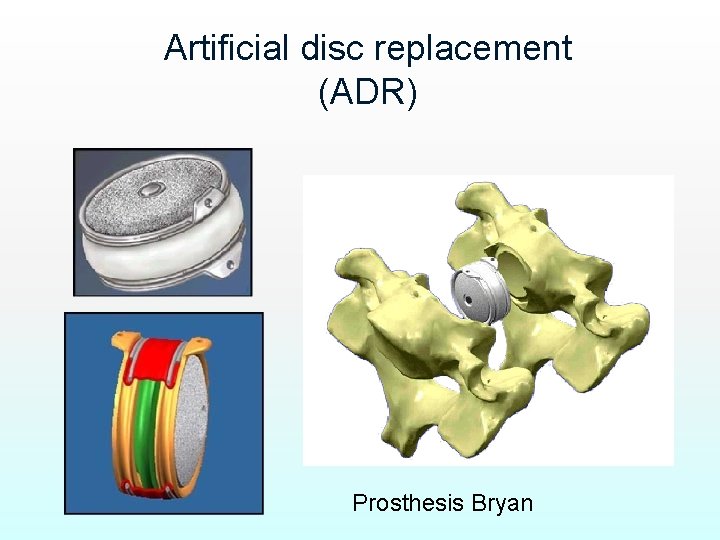
Artificial disc replacement (ADR) Prosthesis Bryan
Thank you
 Outlook hust
Outlook hust Caup tongji university
Caup tongji university Spondylosis definition medical
Spondylosis definition medical L
L Spondylarthrosis intervertebralis
Spondylarthrosis intervertebralis Rita m. lavelle
Rita m. lavelle Liao yuan
Liao yuan Allen liao
Allen liao Liao
Liao Liao yuan
Liao yuan Mei na liao
Mei na liao Shengcai liao
Shengcai liao Raymond liao
Raymond liao Dennis liao
Dennis liao Hospital pharmacy functions
Hospital pharmacy functions Cest mardi
Cest mardi Chia hui chang
Chia hui chang Shan gen acupuncture point
Shan gen acupuncture point Temsi europe
Temsi europe Seung-hui cho sister
Seung-hui cho sister The dwarf cho se hui
The dwarf cho se hui Nonepileptiform
Nonepileptiform Jacob tyler roberts
Jacob tyler roberts Hui zhang cmu
Hui zhang cmu Christ aujourd'hui nous appelle
Christ aujourd'hui nous appelle Hui lin financial services professional
Hui lin financial services professional Hui zhang cmu
Hui zhang cmu Jav huai yan
Jav huai yan Liu hui mathematician
Liu hui mathematician Sandy hui
Sandy hui Lam hui columbia
Lam hui columbia Harmony hui
Harmony hui Grace yang georgetown
Grace yang georgetown Hui whakaoranga
Hui whakaoranga Qu'est-ce qu'on va faire aujourd'hui
Qu'est-ce qu'on va faire aujourd'hui Aujourd'hui levons nous
Aujourd'hui levons nous Aujourd'hui dieu te fait prophète
Aujourd'hui dieu te fait prophète L'exposé de la musique tunisienne
L'exposé de la musique tunisienne